Abstract
Objectives:
Gan Mai Da Zao (GMDZ) decoction is widely used for the treatment of various diseases of the internal organ and of the central nervous system. The aim of this study is to investigate the effects of GMDZ decoction on neuropsychiatric disorders in an animal model.
Methods:
We searched seven databases for randomized animal studies published until April 2015: Pubmed, four Korean databases (DBpia, Oriental Medicine Advanced Searching Integrated System, Korean Studies Information Service System, and Research Information Sharing Service), and one Chinese database (China National Knowledge Infrastructure). The randomized animal studies were included if the effects of GMDZ decoction were tested on neuropsychiatric disorders. All articles were read in full and extracted predefined criteria by two independent reviewers.
Results:
From a total of 258 hits, six randomized controlled animal studies were included. Five studies used a Sprague Dawley rat model for acute psychological stress, post-traumatic stress disorders, and unpredictable mild stress depression whereas one study used a Kunming mouse model for prenatal depression. The results of the studies showed that GMDZ decoction improved the related outcomes.
Conclusion:
Regardless of the dose and concentration used, GMDZ decoction significantly improved neuropsychiatric disease-related outcomes in animal models. However, additional systematic and extensive studies should be conducted to establish a strong conclusion.
Keywords: animal model, depression, Gan Mai Da Zao decoction, neuropsychiatric disease, stress
1. Introduction
Gan Mai Da Zao (GMDZ) decoction is a prescription first described as having the capability to “treat hysteric psychoneurosis-sad and prone to crying, frequently yawning, as if haunted by spirits” in Jin Gui Yao Lue - Treatment of Various Female Diseases by Zhang Zhong Jing in the Later Han Dynasty [1]. It is also called Zhong Jing Da Zao Tang [2] or Da Zao Tang [3] and has been commonly used by practitioners for many generations as a restorative herbal medicine for diseases that cause complications, convulsions, palpitations, and spasms. This prescription consists of three medicinal ingredients, licorice, wheat, and jujube, and has a sweet and plain taste. According to Lingshu - Five Tastes, wheat was used as a royal medicine; it was “advisable for patients with cardiac disease”. It cures the heart and the spleen and controls self-consciousness and sub-consciousness, and in combination with licorice and jujube, which protect the heart and the liver, it decreases excessive female energy, stabilizes the heart, decreases anxiety, protects the heart and the spleen, and relaxes irritability.
GMDZ decoction is widely used for the treatment of various diseases of the internal organ and of the central nervous system (e.g., depression, irritability, anxiety, post-traumatic stress disorders (PTSDs), and acute psychological stress); it is also used in surgery, gynecology, and pediatrics [4]. Although several clinical studies and systematic reviews of GMDZ decoction have been conducted, a systematic analysis of experimental studies has yet to be made. Therefore, the aim of this study is to summarize current evidence from experimental studies on the effects of GMDZ decoction in the treatment of neuropsychiatric diseases.
2. Materials and Methods
The following seven electronic databases were searched: Pubmed, four Korean databases (DBpia, Oriental Medicine Advanced Searching Integrated System, Korean Studies Information Service System, and Research Information Sharing Service), and one Chinese database (China National Knowledge Infrastructure). Our search strategy included the following main keywords in English, Korean, and Chinese: Gan Mai Da Zao, depression, insomnia, stress, neuropsychiatry, central nerve.
All randomized experimental studies in which any animals in neuropsychiatric disease models were treated with GMDZ decoction were included regardless of the control treatments involved. Studies that compared two different forms of herbal decoctions were excluded. No language restrictions were imposed. Thesis and dissertations were included, and articles with insufficient content were excluded. All biochemical or behavioral outcomes were included.
Hard copies of all articles were obtained and read in full by two independent reviewers (SRK, JHJ). Data from the articles were validated and extracted according to pre-defined criteria, such as the prescriptive formula, year, study model, treatment method, and experiment results (Table 1). Discrepancies were resolved through a discussion between the two reviewers (SRK, JHJ) and, as needed, through the opinion of a third reviewer (HWL).
Table. 1. Summary of randomized controlled animal studies of GMDZ decoction for neuropsychiatric diseases.
| Study Author (year) [Ref] | Disease model | Animal model Treatment period | Intervention group Control group | Outcomes | Results |
|---|---|---|---|---|---|
| Tong et al (2005) [5] | Acute psychological stress | SD rat | A) Normal (n = 11) | 1) Thymus index, Spleen index, Adrenal index | 1) Spleen index ↑ |
| B1) Sham (n = 11) | |||||
| 180 - 220 g | B2) Control (n = 11) | ||||
| C1) GMDZ (1 g/mL, n = 11) | |||||
| C2) GCLGML (1 g/mL, n = 11) | 2) Leucocytic mediator (IL-1B, IL-2) | 2) 1L-1B ↓ | |||
| 17 days | C3) SNS (1 g/mL, n = 11) | ||||
| C4) BXHP (1 g/mL ,n = 11) | |||||
| Liu (2013) [6] | PTSD | SD rat | A) Normal (n = 11) | ACTH, COR | ACTH, COR ↓ |
| B) Control (n = 11) | |||||
| 180 - 220 g | C1) GMDZ (0.02 mL/g, n = 11) | ||||
| C2) ZZC (0.02 mL/g, n = 11) | |||||
| 14 days | C3) TMS (0.02 mL/g, n = 11) | ||||
| Liu et al (2013) [7] | PTSD | SD rat | A) Normal (n = 8) | 1) OF | 1) Vertical motion count ↓ |
| B) Control (n = 8) | 2) MWM | 2) 4,5 day escape incubation period ↓ |
|||
| 180 - 220 g | C1) GMDZ (0.02 mL/g, n = 8) | 3) IL-1B, IL-6 | 3) TNF-a, ACTH, COR, TSH, T4, T3, LH, testosterone ↓ |
||
| C2) ZZC (0.02 mL/g, n = 8) | 4) TNF-a, ACTH, COR, TSH, T4, T3, LH, testosterone | ||||
| 14 days | C3) TMS (0.02 mL/g, n = 8) | ||||
| Bi (2012) [8] | CUMS Depression | SD rat | A) Normal (n = 10) | 1) OF | 1) Horizontal movement, vertical movement ↑ |
| B1) Control (n = 10) | 2) Sugar water test | 2) Sugar consumption ↑ | |||
| 180 – 200 g | B2) Positive control (Venlafaxine, n = 10) | ||||
| C1) GMDZ (38 g/kg/d, n = 10) | 3) Amount of food consumed | 3) Amount of food consumed↑ | |||
| 21 days | C2) GMDZ (19 g/kg/d, n = 10) | 4) NE, 5-HT | 4) NE, 5-HT in C2↑ | ||
| C3) GMDZ (9.5 g/kg/d, n = 10) | |||||
| Qin et al (1994) [9] | CUMS Depression | SD rat | A) Normal (n = 10) | 1) OF | 1) Horizontal movement, vertical movement ↑ |
| B1) Control (n = 10) | |||||
| 180 - 200 g | B2) Positive control (Venlafaxine, n = 10) | 2) Sugar water test | 2) Sugar consumption ↑ | ||
| C1) GMDZ (4 g/mL, n = 10) | |||||
| 21 days | C2) GMDZ (2 g/mL, n = 10) | 3) NE, 5-HT | 3) NE, 5-HT in C2 ↑ | ||
| C3) GMDZ (1 g/mL, n = 10) | |||||
| Zhong et al (2012) [10] | Prenatal depression | KM mouse | A) Non-pregnancy control (n = 10) | 1) FST | 1) Underwater down stop time ↓ |
| B) pregnancy control (n = 10) | |||||
| 20 – 25 g | C1) GMDZT (30 g/kg/d, n = 10) | 2) TST | 2) In Tail hang time, stop time ↓ | ||
| 8 days | C2) GMDZ (7.5 g/kg/d, n = 10) |
GMDZ, Gan Mai Da Zao decoction; SD, Sprague Dawley; GZGCLGML, Gui Zhi Gan Cao Long Gu Mu Lv decoction; SNS, Si Ni San; BXHP, Ban Xia Hou Pu decoction; PTSD, post-traumatic stress disorder; ZZC, Zhi Zi Chi decoction; TMS, Tian Ma Su; ACTH, adrenocorticotropic hormone; COR, cortisol; OF, open field test; MWM, Morris water test; NE, norepinephrine; TST, tail suspension test; CUMS, chronic unpredictable mild stress; KM, Kun Ming; FST, forced swim test.
3. Results
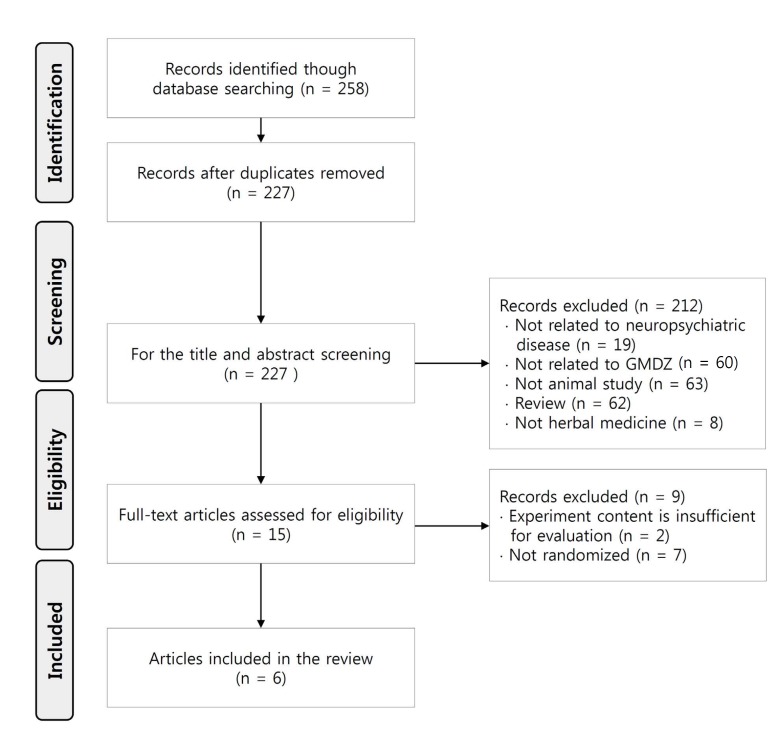
Our search identified 258 studies, of which 6 met the inclusion criteria (Fig. 1) [5-10]. The key data of the included studies are summarized in (Table 1) Two studies tested the effects of GMDZ decoction on PTSD [6, 7], one its effects on acute psychological stress [5], two its effects on chronic unpredictable mild stress (CUMS) depression [8, 9], and one its effects on prenatal depression [10].
Fig. 1. Flow diagram of the selection process.
The details of the medicinal ingredients and prescriptions of the GMDZ decoction used in each study are listed in (Table 2). GMDZ decoction consists of three pieces of licorice, one cup of wheat, and five to seven jujubes according to Jin Gui Yao Lue - Treatment of Various Female Diseases. All of the included studies used a dose adjusted on the basis of the original prescription. Two studies [8, 10] utilized grilled licorice instead of raw licorice in a different preparation method whereas the two other studies [6, 7] used trtici immaturi semen instead of wheat.
Table. 2. Composition of Gan Mai Da Zao decoction in included studies.
| Chinese name | Gan cao | Shi gan cao | Xiao mai | Fu xiao mai | Da zao |
|---|---|---|---|---|---|
| Latin name | Glycyrrhiza uralensis FISCH | Glycyrrhiza uralensis FISCH | Triticum satuurum Lamarck | Triticum aestivum. L | Zizyphus jujube MILL. Var inermis (BUNGE) REHD |
| Tong et al (2005) [5] | 9 g | - | 20 g | - | 5 units |
| Liu (2013) [6] | 10 g | - | - | 30 g | 10 g |
| Liu et al (2013) [7] | 10 g | - | - | 30 g | 10 g |
| Bi (2012) [8] | - | 66 g | 100 g | - | 45 g |
| Qin et al (2013) [9] | - | 66 g | 100 g | - | 45 g |
| Zhong et al (2012) [10] | - | 12 g | 18 g | - | 9 units |
Five studies [5-9] used a Sprague Dawley (SD) rat model for acute psychological stress, PTSD, and CUMS depression whereas one study [10] used a Kunming (KM) mouse model for prenatal depression. Regarding the number of experiment models, 60 to less than 100 animals was the most common range, as shown in three studies [5, 8, 9], whereas less than 60 animals were used in three studies [6, 7, 10]. GMDZ decoction was used at a ratio of 4:2:1 for large, moderate, and small doses in one study [8] whereas the dose was divided into large and small ones at various ratios, such as 4:1 [10] and 1.3:1, in two studies [9]. In addition, GMDZ decoction was observed and compared with other prescriptions used to treat neuropsychiatric symptoms in three studies [5-7].
One study used the sugar-water test or food intake [8] whereas another study used the same test, together with the Morris water test (MWM) [6]. A third study utilized the forced swim test (FST) and the tail suspension test (TST) together [10]. Pentobarbital, amphetamine, N-Aminothiourea, picrotoxin, and pentetrazole were used to investigate central nervous control reactions, such as hypnosis, sedation and anti-convulsion, and swoon [9]. Three studies measured the norepinephrine (NE), or 5-hydroxytryptamine receptors (5-HT), adrenocorticotropic hormone (ACTH), and cortisol (COR) levels in tissue and blood after having observed behavioral changes. [6-8]. Two studies measured serum IL-1β and IL-2 levels, which affect inflammatory response, human body immunity, and metabolic control [5, 6].
GMDZ decoction increased the spleen index and reduced the IL-1β content in the IL-1 level in SD rats with acute psychological stress [5]. Not only did it cause an improvement in the imbalanced hypothalamic-pituitary-adrenal (HPA) axis hormone, it also has a positive effect on IL-1 (IL-a and IL-1B) inflammatory response, human body immunity, and metabolism affected by stress. GMDZ decoction (0.2 mL/g for 14 days) also lowered the levels of ACTH, COR, thyroid-stimulating hormone, thyroxine (T4) and triiodothyronine (T3), luteinizing hormone (LH), and testosterone in the blood, as well as the levels of IL-1β, IL-6, and TNF-a in the hippocampus [6, 7]. These results indicated that GMZD decoction improved the imbalance between the HPA neuro-endocrine axis hormone and inflammatory factors, as well as decreased the escape latency of 4 - 5 days as a result of the MWM test [6, 7]. GMDZ decoction also increased the horizontal and the vertical movements in test models of CUMS depression, the intake of sugared water and food, the weight, and the contents of brain neurotransmitters, such as NE and 5-HT [8].
A prenatal depression study likewise showed that regardless of the concentration of GMDZ decoction used, abnormal behaviors were improved, including the swimming time of test models during the FST; the suspension duration of the dangled tail of the test model during the TST was also decreased [10]. GMDZ decoction extended sleeping hours in animal models in which sleeping was induced with pentobarbital to observe central nerve inhibition effects [9]. The sedative effects on convulsions induced with pentetrazol and ECT were also shown [9]. Spontaneous behavioral inhibition effects, including a decrease in the number of lifting forelegs, were likewise observed [9].
4. Discussion
Few animal studies have focused on the effects of GMDZ decoction on neuropsychiatric diseases. This review showed the positive effects of GMDZ decoction on neurohormones, cytokines, behavioral improvement, and the autonomic nervous system. The recent trends in animal studies on GMDZ decoction suggest prospects for such experimental studies in the future through a comparison and analysis of each study and for the preparation of herbal ingredients that will contribute to the treatment of neuropsychiatric diseases. The fact that 54.5% of such articles have been published since 2000 shows that studies on neuropsychiatric diseases using GMDZ decoction have been actively conducted in the past five years. This reflects social interest in not only physical health but also mental health, as the social costs related to depression and stress continue to increase.
Our review has a number of significant limitations. We expended considerable effort to retrieve all relevant randomized controlled animal studies, but we may still have missed identifying all relevant trials. Moreover, several negative studies exist, but remain unpublished. Studies that validate the side effects or safety of the decoction are also lacking. Because of the limitations in experimental studies, differences in the concentrations and the quality of the extracts may exist, depending on the packaging method used and the source of the herbal medicinal ingredient. The probability of error is also present for the drugs used in each study, depending on their formulation ratio, their packaging method, and the concentration and duration of drug administration. All of these limitations affect the delivery of objective test results.
Furthermore, the items examined through tests were possibly not divided according to the established criteria for each disease. The concentration or period of drug administration may have been improperly set for test animals, but was readily applied in actual clinical settings. These issues should be investigated to increase the objectivity of experimental studies and the connection between clinical studies. Further rigorous research should be conducted to achieve a strong conclusion and determine the mechanism of action of GMDZ decoction.
5. Conclusion
Collectively, this review shows that regardless of the dosage and the formulation used, GMDZ decoction has positive effects on several types of neuropsychiatric diseases. However, additional systematic and extensive studies should be conducted to establish a strong conclusion.
Acknowledgments
This study was supported by grants from the Korea Institute of Oriental Medicine (K16291 and K16292).
Footnotes
Conflict of interest The authors declare that there are no conflicts of interest.
References
- 1.Zhang ZJ. Treatise on febrile diseases caused by cold (Shanghan lun) New World Press; NY: 1986. 442 [Google Scholar]
- 2.Wang KD. Liuke Zhunsheng. Xin Wen Publishing; Taipei: 1979. [Google Scholar]
- 3.Chen ZM. Fugui liangfang daquan. Wen Kuang Publishing Company; Taiwan: 1987. [Google Scholar]
- 4.Guo ZG. Ganmai dazao decotion in treatment of post stroke depresssion. Nei Mongol J Tradit Chin Med. 2001;3:6–7. [Google Scholar]
- 5.Tong Y, Zou J, Liu P, Ni LQ, Cao BY, Liang SH et al. [Effects of four herbal compound formulae on the contents of IL- 1β and IL-2 in acute psychological stress rats] J Shanghai Univ Tradit Chin Med. 2005;19(2):32–34. Chinese. [Google Scholar]
- 6.Liu M. The effect of drugs on behavior, neuroendocrine hormones and hippocampal cytokines of rats with PTSD. The foruth Mlitary Medical University; Xian: 2013. [Google Scholar]
- 7.Min LIU, Hong Y, Jinhong C, Chunxiu Z, Zhenwen Z, Liwu L et al. The effect of different drugs on plasma ACTH and COR of rat with posttraumatic stress disorder. Med J Chin Peop Armed Poli Forc. 2013;24(5):422–424. [Google Scholar]
- 8.Bi XH. Experimental study on the effect of monoamine neurotransmitter ganmaidazao decoction on behavior of depression rats and brain. Yunnan University of TCM; Yunnan: 2012. [Google Scholar]
- 9.Qin WC, Hong GX, Rao F. The inhibitory effect of gan mai da zao tang (GMDZT) on the central nervous systems. Pharmacol Clin Chin Mater Med. 1994;5:9–11. [Google Scholar]
- 10.Zhong Y, Liu GH, Wang RR et al. Effects of ganmaidazao decoction on the behavior of prenatal depression model mice. 39Nei Mongol J Tradit Chin Med. 2012 [Google Scholar]