Abstract
Background:
At the end of 2019, a novel coronavirus outbreak causative organism has been subsequently designated the 2019 novel coronavirus (2019-nCoV). The effectiveness of adjunctive glucocorticoid therapy in the management of 2019-nCoV-infected patients with severe lower respiratory tract infections is not clear, and warrants further investigation.
Methods:
The present study will be conducted as an open-labeled, randomized, controlled trial. We will enrol 48 subjects from Chongqing Public Health Medical Center. Each eligible subject will be assigned to an intervention group (methylprednisolone via intravenous injection at a dose of 1–2 mg/kg/day for 3 days) or a control group (no glucocorticoid use) randomly, at a 1:1 ratio. Subjects in both groups will be invited for 28 days of follow-up which will be scheduled at four consecutive visit points. We will use the clinical improvement rate as our primary endpoint. Secondary endpoints include the timing of clinical improvement after intervention, duration of mechanical ventilation, duration of hospitalization, overall incidence of adverse events, as well as rate of adverse events at each visit, and mortality at 2 and 4 weeks.
Discussion:
The present coronavirus outbreak is the third serious global coronavirus outbreak in the past two decades. Oral and parenteral glucocorticoids have been used in the management of severe respiratory symptoms in coronavirus-infected patients in the past. However, there remains no definitive evidence in the literature for or against the utilization of systemic glucocorticoids in seriously ill patients with coronavirus-related severe respiratory disease, or indeed in other types of severe respiratory disease. In this study, we hope to discover evidence either supporting or opposing the systemic therapeutic administration of glucocorticoids in patients with severe coronavirus disease 2019.
Trial registration:
ClinicalTrials.gov, ChiCTR2000029386, http://www.chictr.org.cn/showproj.aspx?proj=48777.
Keywords: 2019 Novel coronavirus, Coronavirus disease 2019, Glucocorticoids, Severe pneumonia, Acute respiratory distress syndrome
Introduction
Coronaviruses are RNA viruses, and may infect the respiratory, gastrointestinal, hepatic and central nervous systems of humans, livestock species, avian species, many mammals, and wild animals.[1] In humans, infection by four coronaviruses, namely HCoV-229E, HCoV-OC43, HCoV-NL63, and HCoV-HKU1, usually lead to mild, self-limiting upper respiratory tract infections.[2] However, other coronaviruses, such as those associated with severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), may cause severe respiratory disease, and have caused a total of more than 10,000 laboratory-confirmed cases globally in the past two decades, with a 10% and 34.4% case-fatality rate, respectively.[3,4] In December 2019, the 2019 novel coronavirus (2019-nCoV), present with clinical manifestations in humans resembling that of viral pneumonia.[5] By February 25, 2020, about 77,780 confirmed cases have been identified in China, with 2666 deaths. Worryingly, 2459 confirmed cases of coronavirus disease 2019 (COVID-19) have now been identified outside of China.[6]
Symptoms of infection are non-specific, and include fever, cough, and myalgia,[7] with diarrhea, with or without the subsequent development of dyspnea.[8] Severe cases with respiratory distress, sepsis, and septic shock have been reported.[9]
During the SARS epidemic of 2003, therapeutic systemic glucocorticoids were widely administered in patients who were infected with the severe acute respiratory syndrome coronavirus (SARS-CV), and who subsequently developed severe respiratory disease. One cohort study of patients during the SARS outbreak showed that the use of pulsed high-dose methylprednisolone was associated with clinical improvement in patients with SARS.[10] In another study of 20 patients with SARS, certain cytokine levels (interleukin-8, monocyte chemoattractant protein-1, and Th1 chemokine interferon-γ-inducible protein-10) were found to be reduced after 5 to 8 days of glucocorticoid therapy.[11] However, a previous retrospective study indicated that pulsed doses of methylprednisolone was a risk factor associated with increased 30-day mortality (adjusted odds ratio 26.0; 95% confidence interval, 4.4–154.8; P = 0.001).[12] In addition, a further retrospective observational study found that glucocorticoid therapy in patients with MERS was associated with delayed Middle East respiratory syndrome coronavirus (MERS-CoV) RNA clearance.[13] The clinical, therapeutic, and other effects of systemic glucocorticoid therapy in patients with COVID-19 is not currently clear, and the case for and against the use of systemic glucocorticoids in severe cases of COVID-19 warrants further investigation.
Our study proposes to investigate the effectiveness of glucocorticoid therapy in patients with severe COVID-19. Our major objective is to observe whether there is a clinical necessity, or therapeutic justification, for the use of systemic glucocorticoids in patients with severe COVID-19.
Methods
Ethics and dissemination
The study was approved by the Ethics Committee of the Chongqing Public Health Medical Center (No. 2020-003-01-KY). We will publish the results of our study in medical journals at the conclusion of the study. No patient names will appear in any published articles, and no access to the data may be obtained, with the exception of the researchers and members of the Hospital Ethics Committee.
Study design
This study will be conducted as an open-labeled, randomized, controlled trial. We will enroll 48 subjects from the Chongqing Public Health Medical Center for this study. This protocol has been written and devised in accordance with the Standard Protocol Items: Recommendations for Interventional Trials statement.[14] The enrolment, intervention, and assessment processes are described in Figure 1.
Figure 1.
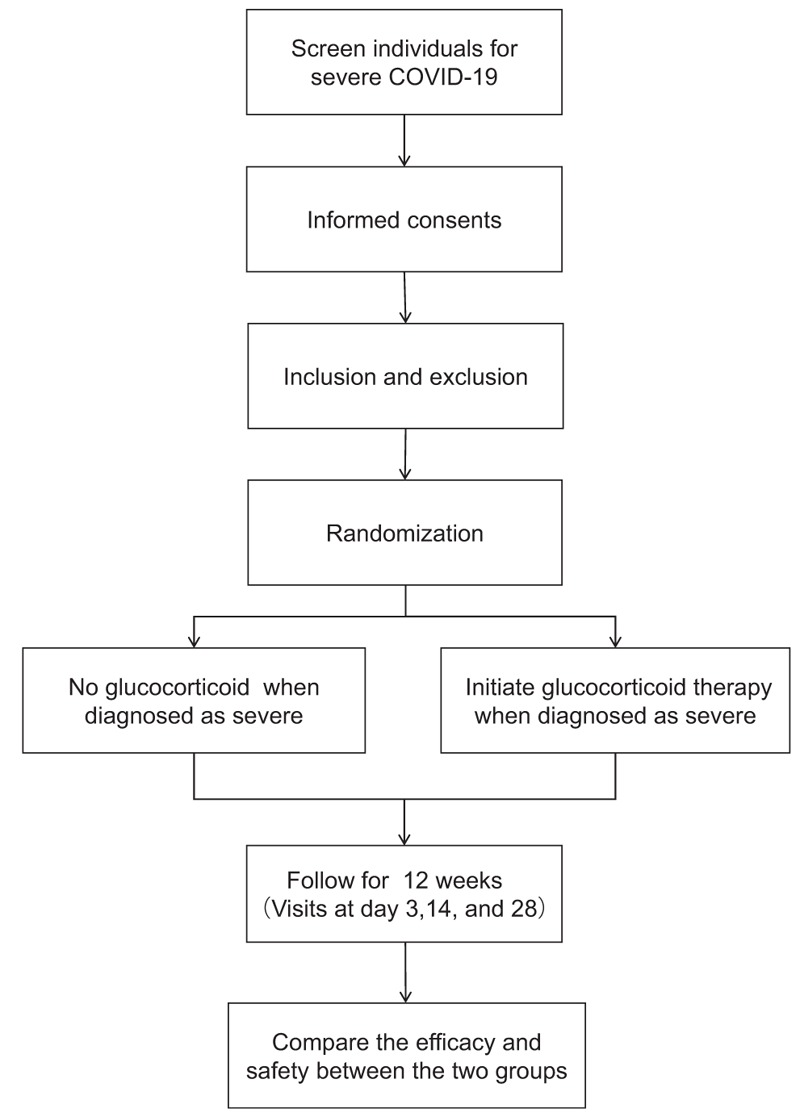
Stratification flowchart of selection, randomization and follow-up of subjects with severe coronavirus disease 2019 (COVID-19) with or without glucocorticoid therapy.
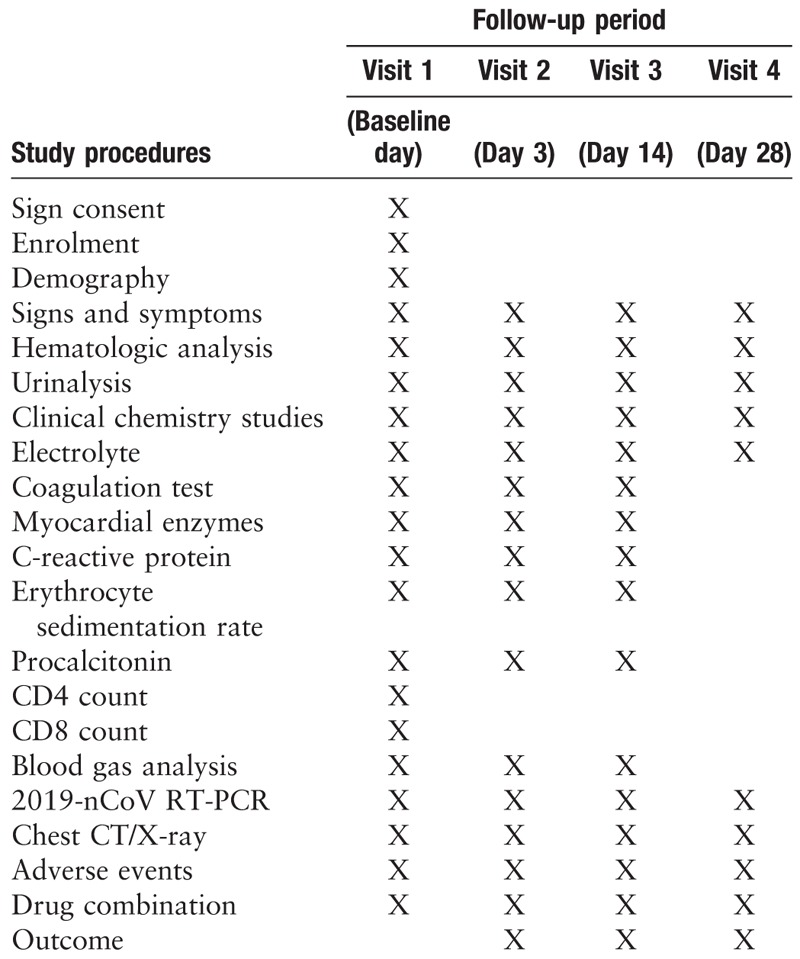
After obtaining informed consent, all subjects in each group will be invited for 28 days of follow-up, which will be scheduled at four consecutive visit points [Table 1]. Blood and urine samples will be collected for laboratory testing, including hematologic analysis, urinalysis, clinical chemistry studies, electrolytes, coagulation testing, myocardial enzymes, C-reactive protein, erythrocyte sedimentation rate, procalcitonin, cluster of differentiation 4 (CD4) cell counts, CD8 cell counts, blood gas analysis, and 2019-nCoV real-time reverse transcription-polymerase chain reaction (RT-PCR). All items considered and tested for during the follow-up period are listed in Table 1.
Table 1.
Follow-up schedule for patients with or without glucocorticoid therapy in severe novel coronavirus pneumonia reflecting epidemiologic, clinical, hematologic, and radiologic patient data.
Adverse events
Adverse events (AEs) are defined as undesirable outcomes experienced by patients during the study, whether or not related to treatment with glucocorticoids. All AEs described by patients or observed by the medical team will be duly documented. All serious AEs will be documented in detail, and the investigators will be notified as soon as possible. AEs will be recorded in both the clinical history of the patient and the case report form, with appropriate medical terminology. All AEs will be expeditiously resolved. Short-term glucocorticoid therapy usually causes mild side effects, including hypokalemia, glucose intolerance, hypertension, pancreatitis, cutaneous, hematologic, immunologic, and neuropsychologic effects.[15] The above mild side effects are reversible upon discontinuation of glucocorticoids. Side effects associated with long-term glucocorticoid use are not considered relevant for this study, because of the short duration of the glucocorticoids prescribed in this study (3 days).
Participants
Diagnostic criteria
The diagnosis of severe COVID-19 in subjects will have to meet the following criteria[16]:
-
(1)
Identification of 2019-nCoV via RT-PCR in blood samples, sputum samples, bronchoalveolar lavage fluid or nasopharyngeal swab samples.
-
(2)
Having at least one of the following conditions:
-
a.
respiratory distress (≥30 times/min);
-
b.
oxygen saturation ≤93% at rest;
-
c.
arterial partial pressure of oxygen (PaO2)/fraction of inspiration O2 (FiO2) ≤300 mmHg (1 mmHg = 0.133 kPa);
-
d.
respiratory failure requiring mechanical ventilation;
-
e.
septic shock development;
-
f.
critical organ failure requiring intensive care unit care.
-
a.
Inclusion criteria
Subjects will be included in our study if they satisfy the following criteria:
-
(1)
Aged 18 years or over;
-
(2)
Severe COVID-19;
-
(3)
Be willing to give informed consent.
Exclusion criteria
Subjects will be excluded from the study if they satisfy the following criteria:
-
(1)
Are allergic or intolerant to any therapeutic drugs used in this study;
-
(2)
Pregnant or lactating women;
-
(3)
Presence of severe systemic illness that may affect the effectiveness or safety evaluation for this study.
Randomization
Microsoft Excel 2013 (Microsoft Corporation, Redmond, WA, USA) will be used to generate random numbers for each subject with consent. Once eligibility has been confirmed, the investigators or designers will randomize the subjects into a control group and an intervention group, at a 1:1 ratio.
Data collection and quality assurance
All results will be recorded and entered twice independently. All data will be documented on case report forms and immediately recorded in the Excel database. Any missing values will be verified to ensure completeness and accuracy of data as much as possible. Data that are obviously abnormal or beyond the upper limit of normal (laboratory items exceeding 20% of the normal value) must be explained, and the necessary explanation must be given by the physician. Drop-outs and AEs will be recorded in a timely manner, and drugs used for trial will be supplied, stored, distributed, and recycled according to relevant regulations. After the data lock record is signed by the principal researcher, sponsor, statistical analyst, and data manager, the data administrator will perform a database lock.
Intervention
All subjects will receive conventional treatment for COVID-19 according to the guidelines for diagnosis and treatment of COVID-19 (version 6). Patients randomized to the intervention group will receive methylprednisolone (intravenous injection, 1–2 mg/kg/day for 3 days), whereas those in the control group will not receive glucocorticoid therapy. Discontinuation of the regimen may occur for those participants who have no substantial improvement after a full course of treatment, or for those subjects whose clinical condition deteriorate during the course of treatment.
Study endpoints
The primary endpoint is the change in sequential organ failure assessment (SOFA) at 3 days after randomization.[17] The secondary endpoints are: proportion of mechanical ventilation use at 2 and 4 weeks, mortality at 2 and 4 weeks, and duration of hospitalization.
Sample size
This trial is a randomized controlled trial with two parallel groups, without masking, and with a 1:1 allocation ratio. Up to now, no randomized controlled trials have evaluated changes in SOFA scores in patients with 2019-nCoV infection with or without glucocorticoid therapy. The sample-size calculation is based on the primary hypothesis of detecting a reduction of 40% in SOFA scores between the treatment and non-treatment groups after 3 days of glucocorticoid therapy. PASS software version 15 (NCSS, LLC; Kaysville, UT, USA) will be used with a power of 80% and a level of 95% confidence. Considering a dropout rate of 5%, the sample size is estimated to be 24 cases in each group. A randomized controlled trial in 2003 aimed to compare the plasma SARS-CoV RNA concentrations in patients in an early hydrocortisone-treated group with patients in a placebo group.[18] This study only enrolled a total of 17 subjects because it was conducted at the end of the SARS outbreak, and fewer appropriate patients were available to be recruited. Taking into account the uncertainty of the duration of the outbreak, the final sample size may be adjusted. Currently, Chongqing has a relatively small number of confirmed cases of COVID-19, and an even smaller number of severe cases of COVID-19. It is hoped that we do eventually recruit a cohort of 48 patients for our study, but we may have to settle for an even smaller cohort, should suitable subjects not be available.
Statistical analysis
The primary outcome analysis will be presented for the intervention group and control group using descriptive statistics. The normality of the data distribution will be evaluated by the Kolmogorov-Smirnov test. Continuous variables will be described as mean values with standard deviation (mean ± standard deviation), and will be analyzed using the t test for independent samples. Categorical variables will be analyzed using the Chi-squared test or Fisher's exact test. To verify the magnitude of the difference, the relative risk of success will be estimated in the intervention group and control group, and its confidence interval will be set at 95%. Values of P < 0.05 will be considered to be statistically significance. All the analyses will be performed using the SPSS software version 24 (SPSS Inc., Chicago, IL, USA).
Discussion
Since 2019-nCoV was first reported in December 2019,[19] it has attracted global attention owing to its similarity to SARS-CoV and MERS-CoV in causing fatal respiratory disease, and its potential for propagating large-scale human infection and economic disruption. Systemic glucocorticoid therapy could be considered for critically ill patients with COVID-19, but their impact on clinical outcomes is uncertain.[16] Available data on systemic glucocorticoid therapy among coronavirus-infected patients mainly comes from studies of patients with SARS and MERS, but whether glucocorticoid therapy is definitively beneficial in the clinical management of these two coronavirus infections is still being debated.[13,20,21]
Glucocorticoid therapy was used in the treatment of severe SARS because early anecdotal experience supported it, and radiologic findings and histologic features of critically ill patients with SARS were similar to those of patients with acute respiratory distress syndrome (ARDS).[22–25] As early as March 2003, China first summarized its experience in the management of SARS, and suggested that high-dose glucocorticoids should be used if patients had fever persisting for more than 3 days, or radiologic findings were suggestive of persistent lung involvement or progressive deterioration.[26] There were three different regimens used by physicians in Hong Kong, China including methylprednisolone (1–2 mg/kg qid or 2–4 mg/kg tid IV followed by oral prednisolone for varying periods and of disparate dosages, as per clinical evaluation), hydrocortisone (2 mg/kg qid or 4 mg/kg tid IV followed by oral prednisolone for varying periods and doses as per clinical evaluation), and pulsed methylprednisolone (500 mg IV daily for 5 days followed by maintenance oral prednisolone 50 mg bid, reduced to 20–30 mg daily on day 21 and as per clinical evaluation).[27]
Some suggested glucocorticoid therapeutic doses during the SARS outbreak were very high, approximating the treatment doses for acute severe asthma, and some prescribed doses were similar to those prescribed for organ rejection in transplant patients, or for ARDS.[23] One study compared pulsed glucocorticoid therapy (methylprednisolone ≥500 mg/day) with non-pulsed glucocorticoid (methylprednisolone <500 mg/day) therapy, finding that pulsed glucocorticoid therapy appeared to be a more efficacious, with patients using pulsed glucocorticoid therapy having lower oxygen requirements, better radiographic outcomes, and decreased likelihood of requiring rescue. Unfortunately, the stated study was not a randomized controlled trial, and is thus open to the possibility of bias having an impact on outcomes.[23] However, there were also staunch advocates for not using systemic glucocorticoids in these patients. One systematic review of studies on patients with SARS-CoV, including 29 studies documenting glucocorticoid use, found 25 studies that were inconclusive regarding the role of the adjunctive use of glucocorticoids, and four studies demonstrated that the use of systemic glucocorticoids in patients with SARS may cause possible harm.[28] A prospective, randomized double-blinded, placebo-controlled trial compared early hydrocortisone treatment (before day 7 of the illness) with placebo, finding that early hydrocortisone therapy was associated with a higher subsequent plasma viral load.[18] Meanwhile, many possible complications of glucocorticoid use, such as profound immunosuppression, with the possible emergence of severe commensal and other viral and bacterial infections, invasive fungal infections, osteonecrosis, and psychosis may occur with prolonged and high-dose glucocorticoid therapy.[29–34]
Glucocorticoid therapy was also commonly used for critically ill patients with MERS. In one study, hypoxemic patients with MERS-CoV pneumonia who had moderate levels of positive end-expiratory pressure were initiated on glucocorticoid therapy.[13] In these patients, there was no difference in 90-day mortality, and these patients were associated with delayed MERS-CoV RNA clearance. Many patients with severe MERS were treated with systemic high-dose glucocorticoids intending to reverse the progression of respiratory distress and to prevent lung fibrosis. However, this approach has not been proven to be successful.[35] One study, including a total of 314 patients with symptomatic MERS-CoV, found that glucocorticoid use was associated with increased mortality in these patients.[36] A retrospective cohort study compared 151 patients in the glucocorticoid group with 158 patients in the non-glucocorticoid group, finding that mortality in the glucocorticoid group was similar to that of the non-glucocorticoid group, but that glucocorticoid therapy was associated with delayed MERS-CoV RNA clearance, after adjustment for baseline and time-varying confounding factors.[13]
After infection with 2019-nCoV occurs, some patients develop mild symptoms, but a significant fraction of patients progress to severe ARDS and require intensive care.[7,37] The use of glucocorticoids in patients with ARDS is still controversial because of divergent results in the existing literature.[38] High-dose glucocorticoid is one of the most frequently used adjuncts in ARDS (17.9%) in 50 countries, even though their effectiveness in the management of acute lung injury is not yet clear.[39] One systematic review conducted an analysis of individual patient data from randomized trials, and demonstrated that compared with the placebo group, prolonged glucocorticoid treatment did improve clinical outcomes.[40] Another randomized controlled trial showed that glucocorticoid therapy could down-regulate ARDS-related inflammation, and was associated with significant improvements in lung and extrapulmonary organ dysfunction, as well as reduce mechanical ventilation duration and intensive care unit hospital admission duration.[41] Studies by Meduri et al[42,43] found that prolonged methylprednisolone treatment may complement positive modulation of systemic inflammation by inducing recovery from induced glucocorticoid resistance, and co-existing decreased production of endogenous glucocorticoids.[42,43] Animal experiments in recent years have provided evidence for the use of glucocorticoids to reduce inflammation, the attenuation of acute lung injury, and reduction in mortality during the acute phase of severe disease.[44,45] However, other studies have suggested that glucocorticoid therapy in ARDS is not necessary, and may even aggravate the clinical picture. The use of hydrocortisone improves lung function in sepsis-associated ARDS, but no significant survival benefit has been observed in these patients.[46] A higher mortality rate has been observed in patients with ARDS who took high-dose glucocorticoids within 7 days after hospital admission, compared with those who were treated without high-dose glucocorticoid.[47]
Existing studies on ARDS have not assessed the effects of glucocorticoids in identical types of patients, or identical processes of the disease.[48] Therefore, the results for these studies cannot be considered to be congruent. Adjunctive glucocorticoid therapy in specific diseases causing ARDS, such as Pneumocystis jirovecii pneumonia, has been shown to reduce mortality in adult patients.[49]Additionally, the dosage of the glucocorticoid used needs to be factored in. High-dose glucocorticoid therapy may increase ventilator dependence, and may possibly induce a worse outcome.[50] The development of osteonecrosis was discovered in patients receiving high-dose glucocorticoids during the SARS epidemic in 2003, and the number of osteonecrotic lesions was directly related to the dosage of the glucocorticoid prescribed.[51,52] Additionally, high-dose glucocorticoid use is one of the causes for neuropsychiatric outcomes in patients with SARS.[53] It has been noted that if lung injury has been effectively controlled, appropriate doses of glucocorticoids based on disease severity may be beneficial for better outcomes of SARS.[10,21] In our study, we will investigate whether the use of mid-dose and short-course adjunctive glucocorticoid therapy to treat severe COVID-19 is advantageous, safe, and effective.
Funding
This work was supported by the Chongqing Special Research Project for Prevention and Control of Novel Coronavirus Pneumonia (No. cstc2020jscx-fyzx0074).
Conflicts of interest
None.
Footnotes
How to cite this article: Qin YY, Zhou YH, Lu YQ, Sun F, Yang S, Harypursat V, Chen YK. Effectiveness of glucocorticoid therapy in patients with severe coronavirus disease 2019: protocol of a randomized controlled trial. Chin Med J 2020;133:1080–1086. doi: 10.1097/CM9.0000000000000791
References
- 1.Chen Y, Liu Q, Guo D. Emerging coronaviruses: genome structure, replication, and pathogenesis. J Med Virol 2020; 92:418–423. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zumla A, Chan JF, Azhar EI, Hui DS, Yuen KY. Coronaviruses - drug discovery and therapeutic options. Nat Rev Drug Discov 2016; 15:327–347. doi: 10.1038/nrd.2015.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO. Summary of probable SARS cases with onset of illness from November 1, 2002 to July 31, 2003. WHO, 2003. Available from: https://www.who.int/csr/sars/country/table2004_04_21/en/. [Accessed on February 2, 2020] [Google Scholar]
- 4.WHO. Middle East respiratory syndrome coronavirus (MERS-CoV). 2019. Available from: http://www.who.int/emergencies/mers-cov/en/. [Accessed on February 2, 2020] [Google Scholar]
- 5.WHO. Novel Coronavirus(2019-nCoV)SITUATION REPORT-121 JANUARY 2020. 2020. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf?sfvrsn=20a99c10_4. [Accessed January 20, 2020] [Google Scholar]
- 6.WHO. Novel Coronavirus(2019-nCoV) Situation Report – 36 - ERRATUM. 2020. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200225-sitrep-36-covid-19.pdf?sfvrsn=2791b4e0_2. [Accessed February 25, 2020] [Google Scholar]
- 7.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 2020; 395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet 2020; 395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sung JJ, Wu A, Joynt GM, Yuen KY, Lee N, Chan PK, et al. Severe acute respiratory syndrome: report of treatment and outcome after a major outbreak. Thorax 2004; 59:414–420. doi: 10.1136/thx.2003.014076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wong CK, Lam CW, Wu AK, Ip WK, Lee NL, Chan IH, et al. Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome. Clin Exp Immunol 2004; 136:95–103. doi: 10.1111/j.1365-2249.2004.02415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tsang OT, Chau TN, Choi KW, Tso EY, Lim W, Chiu MC, et al. Coronavirus-positive nasopharyngeal aspirate as predictor for severe acute respiratory syndrome mortality. Emerg Infect Dis 2003; 9:1381–1387. doi: 10.3201/eid0911.030400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arabi YM, Mandourah Y, Al-Hameed F, Sindi AA, Almekhlafi GA, Hussein MA, et al. Corticosteroid therapy for critically ill patients with Middle East respiratory syndrome. Am J Respir Crit Care Med 2018; 197:757–767. doi: 10.1164/rccm.201706-1172OC. [DOI] [PubMed] [Google Scholar]
- 14.Chan AW, Tetzlaff JM, Gotzsche PC, Altman DG, Mann H, Berlin JA, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013; 346:e7586.doi: 10.1136/bmj.e7586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buchman AL. Side effects of corticosteroid therapy. J Clin Gastroenterol 2001; 33:289–294. doi: 10.1097/00004836-200110000-00006. [DOI] [PubMed] [Google Scholar]
- 16.National Health Commission of the People's Republic of China. Guidelines for the Diagnosis and Treatment of Novel Coronavirus (2019-nCoV) Infection by the National Health Commission (Trial Version 6) 2020. Available from: http://www.nhc.gov.cn/yzygj/s7653p/202002/8334a8326dd94d329df351d7da8aefc2/files/b218cfeb1bc54639af227f922bf6b817.pdf. [Accessed February 18, 2020] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus definitions for sepsis and septic shock (Sepsis-3). Jama 2016; 315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee N, Allen Chan KC, Hui DS, Ng EK, Wu A, Chiu RW, et al. Effects of early corticosteroid treatment on plasma SARS-associated Coronavirus RNA concentrations in adult patients. J Clin Virol 2004; 31:304–309. doi: 10.1016/j.jcv.2004.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu J, Zheng X, Tong Q, Li W, Wang B, Sutter K, et al. Overlapping and discrete aspects of the pathology and pathogenesis of the emerging human pathogenic coronaviruses SARS-CoV, MERS-CoV, and 2019-nCoV. J Med Virol 2020; 1–4. doi: 10.1002/jmv.25709 [E-pub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Booth CM, Matukas LM, Tomlinson GA, Rachlis AR, Rose DB, Dwosh HA, et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA 2003; 289:2801–2809. doi: 10.1001/jama.289.21.JOC30885. [DOI] [PubMed] [Google Scholar]
- 21.Yam LY, Lau AC, Lai FY, Shung E, Chan J, Wong V, et al. Corticosteroid treatment of severe acute respiratory syndrome in Hong Kong. J Infect 2007; 54:28–39. doi: 10.1016/j.jinf.2006.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.So LK, Lau AC, Yam LY, Cheung TM, Poon E, Yung RW, et al. Development of a standard treatment protocol for severe acute respiratory syndrome. Lancet 2003; 361:1615–1617. doi: 10.1016/s0140-6736(03)13265-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ho JC, Ooi GC, Mok TY, Chan JW, Hung I, Lam B, et al. High-dose pulse versus nonpulse corticosteroid regimens in severe acute respiratory syndrome. Am J Respir Crit Care Med 2003; 168:1449–1456. doi: 10.1164/rccm.200306-766OC. [DOI] [PubMed] [Google Scholar]
- 24.Lee N, Hui D, Wu A, Chan P, Cameron P, Joynt GM, et al. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med 2003; 348:1986–1994. doi: 10.1056/NEJMoa030685. [DOI] [PubMed] [Google Scholar]
- 25.Tsang KW, Ho PL, Ooi GC, Yee WK, Wang T, Chan-Yeung M, et al. A cluster of cases of severe acute respiratory syndrome in Hong Kong. N Engl J Med 2003; 348:1977–1985. doi: 10.1056/NEJMoa030666. [DOI] [PubMed] [Google Scholar]
- 26.Zhong NS, Zeng GQ. Our strategies for fighting severe acute respiratory syndrome (SARS). Am J Respir Crit Care Med 2003; 168:7–9. doi: 10.1164/rccm.200305-707OE. [DOI] [PubMed] [Google Scholar]
- 27.Tsang K, Zhong NS. SARS: pharmacotherapy. Respirology 2003; 8: Suppl: S25–S30. doi: 10.1046/j.1440-1843.2003.00525.x. [DOI] [PubMed] [Google Scholar]
- 28.Stockman LJ, Bellamy R, Garner P. SARS: systematic review of treatment effects. PLoS Med 2006; 3:e343.doi: 10.1371/journal.pmed.0030343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tsang KW, Lam WK. Management of severe acute respiratory syndrome: the Hong Kong University experience. Am J Respir Crit Care Med 2003; 168:417–424. doi: 10.1164/rccm.2305012. [DOI] [PubMed] [Google Scholar]
- 30.Wang H, Ding Y, Li X, Yang L, Zhang W, Kang W. Fatal aspergillosis in a patient with SARS who was treated with corticosteroids. N Engl J Med 2003; 349:507–508. doi: 10.1056/NEJM200307313490519. [DOI] [PubMed] [Google Scholar]
- 31.Griffith JF, Antonio GE, Kumta SM, Hui DS, Wong JK, Joynt GM, et al. Osteonecrosis of hip and knee in patients with severe acute respiratory syndrome treated with steroids. Radiology 2005; 235:168–175. doi: 10.1148/radiol.2351040100. [DOI] [PubMed] [Google Scholar]
- 32.Hong N, Du XK. Avascular necrosis of bone in severe acute respiratory syndrome. Clin Radiol 2004; 59:602–608. doi: 10.1016/j.crad.2003.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee DT, Wing YK, Leung HC, Sung JJ, Ng YK, Yiu GC, et al. Factors associated with psychosis among patients with severe acute respiratory syndrome: a case-control study. Clin Infect Dis 2004; 39:1247–1249. doi: 10.1086/424016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tai DY. Pharmacologic treatment of SARS: current knowledge and recommendations. Ann Acad Med Singapore 2007; 36:438–443. [PubMed] [Google Scholar]
- 35.Who Mers-Cov Research G. State of knowledge and data gaps of Middle East respiratory syndrome coronavirus (MERS-CoV) in humans. PLoS Curr 2013; 5: doi: 10.1371/currents.outbreaks.0bf719e352e7478f8ad85fa30127ddb8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alfaraj SH, Al-Tawfiq JA, Assiri AY, Alzahrani NA, Alanazi AA, Memish ZA. Clinical predictors of mortality of Middle East respiratory syndrome coronavirus (MERS-CoV) infection: a cohort study. Travel Med Infect Dis 2019; 29:48–50. doi: 10.1016/j.tmaid.2019.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Heymann DL. Data sharing and outbreaks: best practice exemplified. Lancet 2020; 395:469–470. doi: 10.1016/S0140-6736(20)30184-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Matthay MA, Zemans RL, Zimmerman GA, Arabi YM, Beitler JR, Mercat A, et al. Acute respiratory distress syndrome. Nat Rev Dis Primers 2019; 5:18.doi: 10.1038/s41572-019-0069-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA 2016; 315:788–800. doi: 10.1001/jama.2016.0291. [DOI] [PubMed] [Google Scholar]
- 40.Meduri GU, Bridges L, Shih MC, Marik PE, Siemieniuk RAC, Kocak M. Prolonged glucocorticoid treatment is associated with improved ARDS outcomes: analysis of individual patients’ data from four randomized trials and trial-level meta-analysis of the updated literature. Intensive Care Med 2016; 42:829–840. doi: 10.1007/s00134-015-4095-4. [DOI] [PubMed] [Google Scholar]
- 41.Meduri GU, Golden E, Freire AX, Taylor E, Zaman M, Carson SJ, et al. Methylprednisolone infusion in early severe ARDS: results of a randomized controlled trial. Chest 2007; 131:954–963. doi: 10.1378/chest.06-2100. [DOI] [PubMed] [Google Scholar]
- 42.Meduri GU, Tolley EA, Chrousos GP, Stentz F. Prolonged methylprednisolone treatment suppresses systemic inflammation in patients with unresolving acute respiratory distress syndrome: evidence for inadequate endogenous glucocorticoid secretion and inflammation-induced immune cell resistance to glucocorticoids. Am J Respir Crit Care Med 2002; 165:983–991. doi: 10.1164/ajrccm.165.7.2106014. [DOI] [PubMed] [Google Scholar]
- 43.Meduri GU, Muthiah MP, Carratu P, Eltorky M, Chrousos GP. Nuclear factor-kappaB- and glucocorticoid receptor alpha-mediated mechanisms in the regulation of systemic and pulmonary inflammation during sepsis and acute respiratory distress syndrome. Evidence for inflammation-induced target tissue resistance to glucocorticoids. Neuroimmunomodulation 2005; 12:321–338. doi: 10.1159/000091126. [DOI] [PubMed] [Google Scholar]
- 44.Tu GW, Shi Y, Zheng YJ, Ju MJ, He HY, Ma GG, et al. Glucocorticoid attenuates acute lung injury through induction of type 2 macrophage. J Transl Med 2017; 15:181.doi: 10.1186/s12967-017-1284-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Song LC, Chen XX, Meng JG, Hu M, Huan JB, Wu J, et al. Effects of different corticosteroid doses and durations on smoke inhalation-induced acute lung injury and pulmonary fibrosis in the rat. Int Immunopharmacol 2019; 71:392–403. doi: 10.1016/j.intimp.2019.03.051. [DOI] [PubMed] [Google Scholar]
- 46.Tongyoo S, Permpikul C, Mongkolpun W, Vattanavanit V, Udompanturak S, Kocak M, et al. Hydrocortisone treatment in early sepsis-associated acute respiratory distress syndrome: results of a randomized controlled trial. Crit Care 2016; 20:329.doi: 10.1186/s13054-016-1511-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kido T, Muramatsu K, Asakawa T, Otsubo H, Ogoshi T, Oda K, et al. The relationship between high-dose corticosteroid treatment and mortality in acute respiratory distress syndrome: a retrospective and observational study using a nationwide administrative database in Japan. BMC Pulm Med 2018; 18:28.doi: 10.1186/s12890-018-0597-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Seam N, Suffredini AF. Steroids are part of rescue therapy in ARDS patients with refractory hypoxemia: we are not sure. Intensive Care Med 2016; 42:924–927. doi: 10.1007/s00134-015-4160-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ewald H, Raatz H, Boscacci R, Furrer H, Bucher HC, Briel M. Adjunctive corticosteroids for Pneumocystis jiroveci pneumonia in patients with HIV infection. Cochrane Database Syst Rev 2015; CD006150.doi: 10.1002/14651858CD006150ub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Takaki M, Ichikado K, Kawamura K, Gushima Y, Suga M. The negative effect of initial high-dose methylprednisolone and tapering regimen for acute respiratory distress syndrome: a retrospective propensity matched cohort study. Crit Care 2017; 21:135.doi: 10.1186/s13054-017-1723-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang NF, Li ZR, Wei HY, Liu ZH, Hernigou P. Steroid-induced osteonecrosis: the number of lesions is related to the dosage. J Bone Joint Surg Br 2008; 90:1239–1243. doi: 10.1302/0301-620X.90B9.20056. [DOI] [PubMed] [Google Scholar]
- 52.Chan MH, Chan PK, Griffith JF, Chan IH, Lit LC, Wong CK, et al. Steroid-induced osteonecrosis in severe acute respiratory syndrome: a retrospective analysis of biochemical markers of bone metabolism and corticosteroid therapy. Pathology 2006; 38:229–235. doi: 10.1080/00313020600696231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sheng B, Cheng SK, Lau KK, Li HL, Chan EL. The effects of disease severity, use of corticosteroids and social factors on neuropsychiatric complaints in severe acute respiratory syndrome (SARS) patients at acute and convalescent phases. Eur Psychiatry 2005; 20:236–242. doi: 10.1016/j.eurpsy.2004.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]


