Abstract
Mitochondrial dysfunction is not only a hallmark of rare inherited mitochondrial disorders, but is also implicated in age-related diseases, including those that affect the metabolic and nervous system, such as type 2 diabetes and Parkinson’s disease. Numerous pathways maintain and/or restore proper mitochondrial function, including mitochondrial biogenesis, mitochondrial dynamics, mitophagy, and the mitochondrial unfolded protein response. New and powerful phenotypic assays in cell-based models, as well as multicellular organisms, have been developed to explore these different aspects of mitochondrial function. Modulating mitochondrial function has therefore emerged as an attractive therapeutic strategy for a range of diseases, which has spurred active drug discovery efforts in this area.
Introduction
Mitochondria — the intracellular powerhouse in which energy from nutrients is converted into ATP — are thought to be evolutionarily derived from alphaproteobacteria that operated within cells in endosymbiosis1. Consequently, mitochondria have unique characteristics that pose several challenges to the host cell. During evolution, most of the genes of the endosymbiont were transferred to the nucleus (nuclear DNA; nDNA) of the host cell. In human cells, mitochondrial DNA (mtDNA) — in the form of multiple copies of circular double-stranded DNA molecules — encodes only 13 key proteins, which require separate transcription and translation machinery. Furthermore, as ~1,500 additional nDNA-encoded proteins2 are essential for proper mitochondrial function, a complex system is required for importing, processing and surveying these other proteins3–6.
To perform their key roles in cellular energy production, mitochondria use an intricate system that encompasses the breakdown of fatty acids and glucose, which is coupled to oxidative phosphorylation. Mitochondria are highly dynamic structures that undergo rapid remodeling through fusion and fission to adapt to changes in the cellular context7. When mitochondria are damaged, mitophagy — a specific autophagic response confined to mitochondria — regulates their controlled degradation8; furthermore, following extensive damage or specific triggers, mitochondria are central to the initiation of apoptosis9. Given the complex balance between the nuclear and mitochondrial genome, and the fact that mitochondria are the site of metabolic transformation and hence a hotspot of metabolic stress, it is not surprising that mitochondrial dysfunction is involved in a broad spectrum of diseases, both inherited and acquired. Prototypical inherited mitochondrial diseases can be caused by mutations in either mtDNA or nDNA, and typically result in very severe multisystem disease from birth. Conversely, mitochondrial dysfunction is important, or at least implicated, in a diverse range of acquired diseases, including cancer, metabolic diseases and neurodegenerative disorders, which are often associated with ageing. Here, we first provide an overview of diseases that affect mitochondria and then present key mitochondrial pathways that are amenable to therapeutic intervention, focusing on mitochondrial biogenesis and quality control circuits as the most tractable targets. Finally, we discuss state-of-the-art screening strategies that can be applied to identify drugs targeting these pathways.
Mitochondrial diseases
Mitochondrial diseases can narrowly be defined as inherited disorders resulting from mutations in mtDNA or nDNA that impair mitochondrial function. However, in a broader sense, ageing-associated disorders in which defective mitochondrial function has been pathophysiologically could also be considered as mitochondrial diseases. Below, we briefly discuss these different aspects of mitochondrial dysfunction in diseases, which have recently been extensively reviewed in the literature (see REFS 10–12).
Inherited mitochondrial diseases
Many inborn errors in metabolism are characterized by a primary defect in mitochondrial processes, such as fatty acid oxidation, haem biosynthesis or oxidative phosphorylation13. Most of these mitochondrial diseases follow a Mendelian mode of inheritance, meaning that a mutation in a single genetic locus is responsible for the phenotype in either a dominant or recessive fashion (BOX 1). For example, defects in oxidative phosphorylation can be caused by mutations in genes encoding subunits of the electron transport chain (ETC), as well as by mutations in genes involved in mtDNA replication, maintenance and repair, mitochondrial translation, respiratory complex assembly and processes that affect mitochondrial biogenesis, dynamics and homeostasis in general. The pleiotropic origin of defects in oxidative phosphorylation is illustrated by cytochrome c oxidase (complex IV) deficiency, which can be caused by mutations in over 15 different genes encoding complex IV subunits or its assembly proteins14 (TABLE 1).
Box 1. Towards a network approach for mitochondrial diseases.
The symptoms and age of onset of mitochondrial diseases caused by mutations in mitochondrial DNA (mtDNA) can be variable even within the same family. This can be partially explained by the variation in the number of copies of normal and mutated forms of mtDNA within a cell (termed heteroplasmy). This is not observed for diseases caused by nuclear DNA mutations because they are inherited in a Mendelian fashion. Furthermore, the variability among patients from the same family carrying the same mutation is affected by environmental contributions, epigenetic factors and the presence of other genetic polymorphisms that ultimately modify the nature and expression of the disease phenotype. These modifier genes often work within large interaction networks, similar to those observed in complex multigenic diseases.
Complex diseases are associated with changes at several genetic loci, termed quantitative trait loci (QTLs), and each locus contributes quantitatively to the phenotype. For example, genetic studies suggest that common diseases in which mitochondrial dysfunction is involved, such as type 2 diabetes, are caused by small changes in many genes rather than large effects produced by mutations in a few genes236–238. Likewise, in the case of Parkinson’s disease, mutations in PTEN-induced putative kinase 1 (PINK1) and parkin are only associated with the early-onset form of the disease, which represents a small fraction of all Parkinson’s disease cases (TABLE 2), whereas other forms of Parkinson’s disease follow a complex disease inheritance pattern that is modified by gene–gene and gene–environment interactions. One could therefore hypothesize that although rare inherited mitochondrial diseases differ from common diseases in which mitochondrial dysfunction is implicated, with respect to the severity of impact of the mutations (affecting either one or several genes), both types of diseases could benefit from a network approach to identify novel target genes and pathways that modulate mitochondrial function.
Table 1. Selected typical inherited mitochondrial diseases.
| Genome | Gene | Gene function | Clinical description |
|---|---|---|---|
| mtDNA |
MTND1, MTND2, MTND4 and MTND6 |
Complex I subunits | Leber hereditary optic neuropathy (LHON) |
| MTATP6 | Complex V subunit | Neuropathy, ataxia, retinis pigmentosa (NARP) or maternally inherited Leigh’s syndrome (MILS) |
|
| MTTL1 | Mitochondrial protein translation |
Mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes (MELAS) |
|
| MTTK | Mitochondrial protein translation |
Myoclonic epilepsy, muscle weakness and wasting with red-ragged fibres (MERFF), cerebellar ataxia, deafness and dementia |
|
|
MTCO1, MTCO2 and MTCO3 |
Complex IV subunits | Complex IV deficiency: clinically very variable, from single-organ defects (such as motor neuron deficiency or myopathy) to multisystem defects (for example, encephalomyopathy) |
|
| nDNA |
COX10, COX6B1, SCO1 and SCO2 |
Complex IV subunit or assembly |
|
|
SURF1
COX15 |
Complex IV biogenesis or assembly |
Leigh syndrome characterized by loss of motor milestones, hypotonia, movement disorders, nystagmus, breathing disorders, ophthalmoplegia, peripheral neuropathy and cardiomyopathy |
|
| MFN2 | Mitochondrial fusion | Charcot–Marie–Tooth disease type 2A; peripheral sensorimotor neuropathy characterized by motor and sensory deficits and postural tremors |
|
| OPA1 | Mitochondrial fusion | Optic atrophy |
COX10, cytochrome c oxidase assembly homolog 10; COX15, cytochrome c oxidase assembly homolog 15; COX6B1, cytochrome c oxidase subunit 6B1; MFN2, mitofusin 2; MTATP6, mitochondrially encoded ATP synthase 6; MTCO1, mitochondrially encoded cytochrome c oxidase 1; MTND1, mitochondrially encoded NADH dehydrogenase subunit 1; MTTK, mitochondrially encoded tRNA lysine; MTTL1, mitochondrially encoded tRNA leucine 1 (UUA/G); OPA1, optic atrophy protein 1; SCO1, cytochrome c oxidase assembly protein SCO1; SURF1, surfeit 1.
Another hallmark of inherited mitochondrial diseases is that their phenotypic presentation is highly heterogeneous, with some diseases affecting single tissues (such as the cochlea in maternally inherited deafness) and others affecting multiple systems (such as encephalomyopathies), and with disease onset ranging from the neonatal phase to adulthood15. In the case of diseases caused by mutations in mtDNA, this heterogeneity can be partially explained by the phenomenon of heteroplasmy — in which both native and mutated mtDNA coexist within the same cell — which can arise because mitochondria contain multiple copies of mtDNA16. This means that the mutational load could vary substantially among tissues or among members of the same family17.
Despite this variability, tissues that rely heavily on mitochondria for the generation of ATP — such as the sensory, nervous, cardiac and muscle systems — are more frequently affected than others18 (TABLE 1). Furthermore, the segregation capacity of mtDNA varies in different tissues. In fact, studies have reported that heteroplasmy is maintained in the brain, muscle and heart of NZB-BALB/c or NZB-129S6 heteroplasmic mice, whereas DNA segregation occurs over time in the ovary, liver and spleen16,17. It was also demonstrated that simply carrying two types of normal mtDNA from different inbred strains — that is, NZB-BALB/c and NZB- 129S6 mice — leads to abnormal metabolism, activity and behaviour16. Although further work is necessary to understand the underlying genetic causes of this phenomenon, these observations indicate that reducing heteroplasmy in patients with mtDNA mutations could be a therapeutic objective (reviewed in REFS 19,20).
Mitochondrial dysfunction in common diseases
Although the origin of many inherited mitochondrial diseases has been identified, this is not straightforward for common diseases in which mitochondrial dysfunction is involved. Such common diseases are rarely caused by single genetic defects; rather, they result from a combination of factors, including the quantitative contribution of several genes (so-called quantitative trait loci; QTLs) and environmental factors such as exercise, stress, diet and age21 (BOX 1). Deregulation of various signalling pathways, such as the insulin–IGF1 (insulin-like growth factor 1) pathway22, the mammalian target of rapamycin (mTOR) pathway23, the AMP-activated protein kinase (AMPK) pathway24 and the sirtuin25 pathways, can induce mitochondrial dysfunction26. The phenotypic signs of reduced mitochondrial function — such as impaired fitness, metabolism, cognitive function and memory — that herald underlying organ dysfunction also typify ageing27–30. The multiscalar regulatory network that governs mitochondrial homeostasis may therefore be involved in the development of some of the most common age-related diseases, including type 2 diabetes, obesity, Alzheimer’s disease and Parkinson’s disease.
Metabolic disorders
Type 2 diabetes is a complex multisystem metabolic disease that is characterized by elevated glucose levels. A common early feature in the pathogenesis of type 2 diabetes is the accumulation of lipids in skeletal muscle, adipose tissue and the liver owing to mitochondrial dysfunction31,32. This is likely to be caused by an inability to maintain metabolic flexibility — that is, the ability to switch from one fuel source to another. In fact, several studies have shown that there is a global reduction in oxidative capacity within the skeletal muscle of patients with type 2 diabetes33,34. This was linked to reduced expression and activity of PPARγ coactivator 1α (PGC1α) and its target genes35–37. Similarly, the mitochondrial content of white adipose tissue is lower in patients with insulin resistance, type 2 diabetes and severe obesity38,39. The situation is less clear in the liver, as both increased and decreased (as well as unaltered) expression of oxidative phosphorylation genes has been observed in the liver of humans and mice with metabolic disease40–42.
In addition, a reduction in the oxidative capacity of mitochondria seems to be linked to the development of insulin resistance in the context of type 2 diabetes and obesity11,43. This hypothesis goes hand in hand with the fact that exercise and caloric restriction both promote mitochondrial biogenesis and oxidative capacity as well as improving insulin sensitivity in patients who are obese and/or have type 2 diabetes44,45. Conversely, moderate dysfunction in oxidative phosphorylation following the deletion of apoptosis-inducing factor (AIF) in the liver and muscle, or deletion of mitochondrial transcription factor A (TFAM) in adipose tissue, was shown to protect mice from diet-induced obesity and type 2 diabetes46,47. Despite these apparent opposing effects on oxidative phosphorylation overall, these examples support the general concept that mitochondrial function has a role in type 2 diabetes. Further work is needed to establish whether the link between dysfunctional oxidative phosphorylation and type 2 diabetes is causal or consequential, which could clarify how mitochondrial metabolism might be modulated to prevent or treat type 2 diabetes.
Neurodegenerative disorders
Abnormal protein folding homeostasis and subsequent protein aggregation — a phenomenon termed proteotoxicity — is a common feature of neurodegenerative diseases such as Alzheimer’s disease and Parkinson’s disease48. Senile plaques, composed of amyloid-β (Aβ) peptide in the case of Alzheimer’s disease and Lewy bodies that stain positive for α-synuclein and ubiquitin in the case of Parkinson’s disease, are examples of this phenomenon10. Defective mitochondrial proteostasis has also been implicated in such diseases48. In addition, several proteins associated with early-onset neurodegenerative disease have been directly or indirectly connected to mitochondrial function10 (TABLE 2). Two genes associated with familial Parkinson’s disease, the E3 ubiquitin protein ligase Parkinson’s disease protein 2 (PARK2; also known as parkin) and PTEN-induced putative kinase 1 (PINK1)49,50, have a crucial role in mitophagy, partly by modulating mitochondrial fusion and fission51,52 (TABLE 2). Likewise, the proteotoxic α-synuclein and the Parkinson’s disease-associated protein DJ1 (also known as PARK7) control mitochondrial morphology as well as fusion and/or fission events in the same pathway as parkin and PINK1 (REFS 53–55).
Table 2. Selected rare diseases associated with mitochondrial dysfunction*.
| Gene | Gene function | Clinical description |
|---|---|---|
| Parkin PARK7 (also known as DJ1) PINK1 |
Mitophagy and/or mitochondrial dynamics |
Early onset form of Parkinson’s disease, characterized by tremor, bradykinesia, rigidity and postural instability |
| FXN | Mitochondrial iron metabolism | Friedreich’s ataxia, characterized by difficulties in coordinating movements, associated with neurological signs, cardiomyopathy and (sometimes) type 1 diabetes |
| Paraplegin | Mitochondrial protease | Spastic paraplegia; characterized by progressive spasticity and weakness of the lower legs owing to axonal degeneration |
| HSP60 | Mitochondrial quality control, mitochondrial UPR |
FXN, frataxin; HSP60, mitochondrial chaperonin heat shock protein 60; PARK7, Parkinson’s disease protein 7; PINK1, PTEN-induced putative kinase 1; UPR, unfolded protein response.
Nuclear DNA only.
The potential involvement of mitochondrial dysfunction in Alzheimer’s disease is currently less clear. Aβ was shown to translocate to mitochondria56, resulting in reduced ETC activity. This may occur following the induction of mitochondrial fragmentation57, an increase in mitochondrial membrane viscosity58 and/or direct inhibition of complex IV activity59, and involve mitochondria-associated endoplasmic reticulum membranes (MAMs) in the processing of amyloid precursor protein60. Additional evidence supporting the potential involvement of mitochondria in Alzheimer’s disease has come from mtDNA haplogroup association studies, in which mtDNA haplogroups that have a greater likelihood of predisposing individuals to Alzheimer’s disease seem to be associated with defects in oxidative phosphorylation61.
Following these observations, it was suggested and shown that boosting mitochondrial function by dietary restriction or using the caloric restriction mimetic resveratrol can counteract neurodegeneration in worms and mice (reviewed in REF. 48). Conversely, inhibiting mitochondrial function by knocking out the cytochrome c oxidase assembly protein (Cox10) gene — which encodes an enzyme that is required for the function of mitochondrial cytochrome c oxidase (COX) — in the brain62 delayed the onset of neurodegeneration in a mouse model of Alzheimer’s disease. Even though the approach to knock out Cox10 appears to be counterintuitive, these two types of interventions may be connected through a common induction of protective mitochondrial quality control systems, as discussed below.
Pathways to restore mitochondrial function
The treatment of inherited mitochondrial diseases typically involves general measures, such as the optimization of nutrition and administration of vitamins and food supplements, along with symptom-based management. Other specific approaches are focused on establishing a heteroplasmic shift towards a higher proportion of nonmutated mtDNA in diseases that are caused by mutations in mtDNA rather than nDNA (reviewed in REFS 19,20). Specific novel interventions to improve mitochondrial function in rare and common diseases are in their infancy but could provide benefit in several disease settings. With the growing understanding of mitochondrial function, it has become clear that several aspects could be therapeutically targeted. We focus here on the main pathways that have been demonstrated to maintain and/or restore proper mitochondrial function, such as: mitochondrial biogenesis and metabolic flexibility; mitochondrial dynamics, including fusion and fission; and mitochondrial quality control through proteostasis and mitophagy. We do not cover apoptosis, which is another important aspect of mitochondrial function, but this topic has been extensively reviewed in REFS 63,64.
Mitochondrial biogenesis and metabolic flexibility
Mitochondrial biogenesis is a complex process, driven by a set of nuclear-encoded transcription factors and assisted by transcriptional co-factors, through which the cell equilibrates its energy-harvesting capacity to meet its energetic demands (BOX 2). Considering this transcriptional network, one can distinguish two approaches to induce mitochondrial biogenesis: targeting the upstream regulators (for example, sensors), or targeting their downstream effector pathways (for example, transcription factors and cofactors) (FIG. 1). It should be noted, however, that for most of the therapeutic strategies it is impossible to discriminate between beneficial effects that arise within the mitochondria and those that arise from other subcellular compartments.
Box 2. Metabolic flexibility and the upstream sensors of mitochondrial biogenesis.
Evolution favoured the survival of organisms that were capable of adapting to environmental challenges, such as a non-continuous supply of energy. This explains why proteins that are involved in pathways governing metabolic flexibility and the shift between anabolism and catabolism, such as AMP-activated protein kinase (AMPK) and mammalian target of rapamycin (mTOR), are incredibly well conserved from yeast to mammals239. When energy is abundant, mTOR stimulates anabolic pathways110, whereas sufficient ATP levels keep AMPK activity low107. On the contrary, when energy is limited, mTOR activity is low110 and AMPK is activated by the high AMP/ATP ratio, which promotes catabolic energy-generating pathways107. AMPK activates mitochondrial energy production by activating transcription factors, such as the forkhead box O (FOXO) proteins, through both direct (that is, phosphorylation) and indirect mechanisms, which involve metabolic changes leading to increased NAD+ levels and subsequent sirtuin 1 (SIRT1)-mediated FOXO deacetylation78.
Aside from these well-conserved kinases, which act as cell-autonomous fuel sensors and effectors, other pathways involving transcription factors and their co-factors regulate metabolic flexibility at the organismal scale. In vertebrates, mitochondrial biogenesis and activity are controlled in part by a ‘yin-yang’ between co-repressors, such as nuclear receptor co-repressor 1 (NCOR1)70, and co-activators, such as steroid receptor co-activator protein 1 (SRC1; also known as NCOA1)151 and PPARγ co-activator 1α (PGC1α)240,241, which fine-tune transcriptional networks controlling oxidative metabolism. For example, increased cellular NAD+ levels during energy stress lead to deacetylation and activation of PGC1α74,77,78,105, which, together with reduced activity of NCOR1 (REF. 70), favours oxidation and enhances the use of stored energy during caloric restriction. These processes are reversed by excessive caloric intake at both the enzymatic and gene expression level. In fact, a high-fat diet leads to high ATP and low NAD+ levels, which attenuates AMPK and SIRT1 activity242 and induces the expression of SRC3 (also known as NCOA3) and the histone acetyltransferase GCN5 (REF. 152). This results in the acetylation and inhibition of transcription factors, such as the tumour suppressor p53 (REF. 69), FOXO71–73 and PGC1α74, which in turn attenuates mitochondrial activity242. Furthermore, NCOR1 is activated70, which accentuates the decreased transcription of genes governing mitochondrial activity and contributes to the storage of excess calories152,243. These co-factor networks target and fine-tune a limited number of transcription factors, including nuclear respiratory factor 1 (NRF1), NRF2 and several nuclear receptors, such as the peroxisome proliferator-activated receptors (PPARs) and oestrogen-related receptors (ERRs)244–246. Each of these transcription factors binds to a specific motif, promoting the transcription of different gene sets in the tissues where they are expressed.
One interesting point to underscore is that in invertebrates, including yeast and worms, mitochondrial biogenesis and metabolic flexibility are regulated through similar transcriptional regulatory networks that govern these processes in vertebrates, even though invertebrates lack homologues of some of the transcription factors (for example, nuclear receptors in yeast) and co-factors (for example, PGC1α in yeast and worms) that are present in vertebrates. By contrast, the kinases (mTOR and AMPK), sirtuins and NCOR1 are conserved throughout evolution.
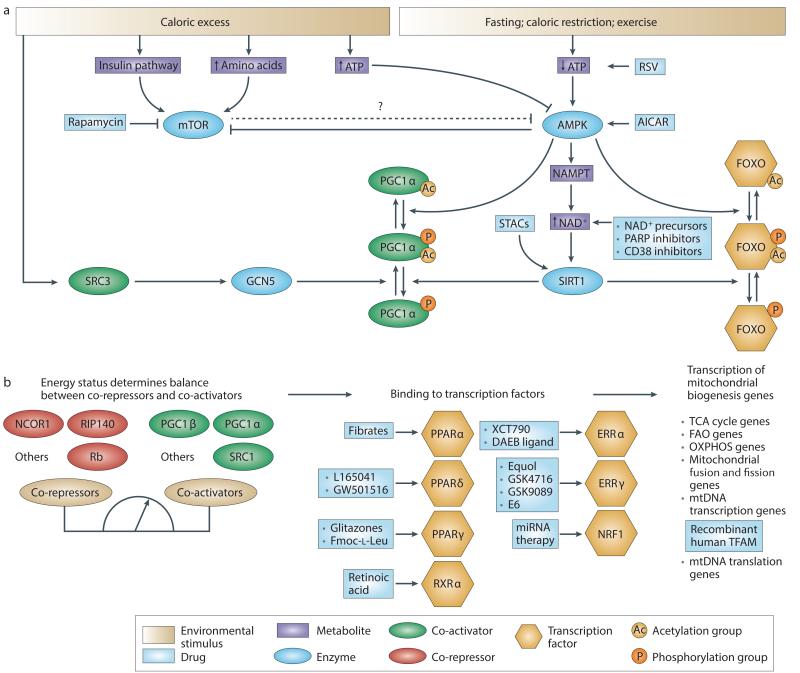
Figure 1. Pharmacological approaches targeting mitochondrial biogenesis.
Pharmacological approaches for targeting mitochondrial biogenesis. a | Upstream sensors of energy status. Energy stress promotes the activation of AMP-activated protein kinase (AMPK) via an increase in the AMP/ATP ratio, whereas energy excess activates the mammalian target of rapamycin (mTOR) pathway either via an increase in levels of amino acids or via the activation of insulin signalling. Rapamycin, 5-aminoimidazole-4-carboxamide riboside (AICAR) and resveratrol (RSV) simulate energy crisis by inhibiting mTOR or activating AMPK. AMPK-mediated phosphorylation of co-factors (such as PPARγ co-activator 1α (PGC1α)) and transcription factors (such as forkhead box O (FOXO) proteins) is a preliminary step required for their activation. AMPK also increases levels of NAD+, which is a substrate for sirtuins. NAD+ levels can be increased either by supplying precursors or by inhibiting NAD+-consuming enzymes such as CD38 and poly(ADP-ribose) polymerases (PARPs). The increase in NAD+ levels activates sirtuin 1 (SIRT1), which subsequently deacetylates PGC1α and FOXO. The acetylation status of PGC1α is counterbalanced by the activity of the histone acetyltransferase GCN5, which is activated by feeding and via the recruitment of steroid receptor co-activator protein 3 (SRC3). Sirtuin-activating compounds (STACs) can also activate SIRT1 directly. b | Downstream transcriptional factors and co-factors. The balance between the activity of co-repressors and co-activators determines the activation of transcription factors involved in mitochondrial biogenesis. Nuclear receptors such as peroxisome proliferator-activated receptors (PPARs) are ideal drug targets as they are activated upon ligand binding. Likewise, agonist ligands for retinoid X receptor-α (RXRα), the heterodimerization partner of the PPARs, enhance mitochondrial function. Also, several compounds can induce the transcriptional activity of the oestrogen-related receptors (ERRs). The only approach described to modulate the activity of the transcription factor nuclear respiratory factor 1 (NRF1) was a microRNA (miRNA)-based approach. Finally, a recombinant form of human mitochondrial transcription factor A (TFAM) was designed to stimulate the processing of mitochondrial DNA (mtDNA). FAO, fatty acid oxidation; NAMPT, nicotinamide phosphoribosyltransferase; NCOR1, nuclear receptor corepressor 1; OXPHOS, oxidative phosphorylation; RIP140, receptor-interacting protein 140; Rb, retinoblastoma protein; TCA, tricarboxylic acid.
Upstream sensors - caloric restriction, AMPK, mTOR, NAD+ boosters and sirtuins
Caloric restriction is the only physiological intervention that has so far been shown to increase lifespan in a range of species65. Although it is uncertain whether this effect also occurs in primates, caloric restriction does improve metabolic health and prevent pathological decline associated with ageing in such species66,67. The molecular network underlying the effects of caloric restriction comprises the key nutrientsensing pathways, such as those involving insulin–IGF1, mTOR, AMPK and the sirtuins26. As a caloric restriction diet is very difficult to apply and maintain, the search for caloric restriction mimetics has intensified in the past decade.
The sirtuin family of histone deacetylases has emerged as a prime target to mimic caloric restriction25. This was based on the critical dependence of sirtuins on the metabolic co-factor NAD+ (REF. 68), and on the fact that sirtuin 1 (SIRT1) controls the activity of various transcription factors and co-factors — such as the tumour suppressor p53 (REF. 69), myocyte-specific enhancer factor 2 (MEF2)70, forkhead box O (FOXO) proteins71–73 and PGC1α74 — which are known to govern mitochondrial biogenesis and function. The best-characterized sirtuinactivating compound is resveratrol, which is present in low levels in red grapes and red wine75. Resveratrol, however, does not directly activate SIRT1; rather, it acts indirectly via the activation of AMPK and the subsequent induction of NAD+ levels, which stimulate the activity of SIRT1 (REFS 76–80). Regardless of its mechanism of action, resveratrol enhances mitochondrial biogenesis and oxidative capacity in rodent models of diet-induced obesity, which translates into improved muscle function and protection against obesity and insulin resistance, ultimately improving healthspan81,82.
In humans, resveratrol improved mitochondrial function and lipid levels in obese patients at a 200-fold lower dose than that used in mice (150 mg per day)83, although differences in the study design and the resveratrol dose used may lead to variable results84–86. Resveratrol also improved glycaemic control in patients with type 2 diabetes when it was administered alone or in combination with other hypoglycaemic agents84,87. Together, these clinical trials indicated the therapeutic potential of resveratrol in the context of metabolic diseases, although further pharmacokinetic studies will be needed to optimize resveratrol’s therapeutic efficiency88.
Spurred by these beneficial effects of resveratrol, a search for more potent SIRT1-activating compounds (STACs) that are structurally unrelated to resveratrol led to the identification of SRT1720 and SRT2104 (REFS 89,90). The exact mechanism of action of these compounds is the subject of intense controversy, as studies have shown that these STACs only seem to be active on artificial substrates that contain a fluorophore tag79,91,92. However, it was recently shown that STACs also activate SIRT1 when certain structural features that mimic the large fluorophore are present in natural SIRT1 substrates (for example, on PGC1α-K778 and FOXO3A-K290)93. Despite the controversy regarding the capacity of STACs to directly induce the deacetylase activity of SIRT1, SRT1720 has been reported to improve glucose homeostasis and insulin sensitivity in rodents89, which translated into improved healthspan and increased lifespan in dietinduced obese (DIO) mice; these findings are consistent with SIRT1 activation94. SRT2104, which has similar beneficial effects in DIO mouse models95,96, was recently assessed for its safety and pharmacokinetics in humans97. Besides SRT1720 and SRT2104, several new potent SIRT1 agonists have been reported98–100. The outcomes of clinical efficacy studies of these STACs in various diseases are eagerly awaited.
Considering the crucial dependence of sirtuins on the enzymatic co-factor NAD+ (REF. 101), modulation of NAD+ levels should activate SIRT1 signalling and promote mitochondrial biogenesis and function. NAD+ levels can be increased by directly stimulating NAD+ synthesis or by inhibiting NAD+-consuming enzymes102. Indeed, dietary supplementation with the NAD+ precursors nicotinamide mononucleotide (NMN) or nicotinamide riboside increased NAD+ levels in several tissues in mice103,104. This effect on NAD+ levels led to SIRT1-dependent mitochondrial activation and improved exercise endurance and insulin sensitivity103,104. Strikingly, nicotinamide riboside also activated the mitochondrial SIRT3 (REF. 103). Although SIRT1 and SIRT3 both regulate important aspects of mitochondrial metabolism, non-mitochondrial targets of these regulators may also contribute to the beneficial phenotype. Similarly, NAD+ levels and SIRT1 activity were increased in the tissues of mice treated with inhibitors of poly(ADP-ribose) polymerases (PARPs) or ADPribosyl cyclase 1 (also known as CD38), two enzymes that consume NAD+, leading to a boost in mitochondrial function and metabolic fitness105,106. The activation of AMPK, which enhances mitochondrial energy production following an increase in the AMP/ATP ratio107, also mimics caloric restriction24. In healthy animals, the AMPK agonist 5-aminoimidazole- 4-carboxamide riboside (AICAR) increases exercise endurance by activating a gene programme that is normally induced after exercise108. AMPK activation by AICAR also rescued mitochondrial dysfunction and the limited exercise capacity of mice deficient in cytochrome c oxidase109. Alternatively, inhibition of mTOR, a conserved kinase that promotes cell growth and anabolism in the presence of nutrients and growth factors110, simulates a state of energy crisis and thereby activates AMPK and boosts mitochondrial activity through an as yet unknown mechanism (BOX 2). In fact, the mTOR inhibitor rapamycin increases lifespan in various organisms including mice111–113. Importantly, the beneficial effects of mTOR inhibition in mice seem to be tissuespecific, as adipose-specific knockout of the mTOR complex protein Raptor (regulatory associated protein of mTOR) enhances mitochondrial respiration114, whereas muscle-specific knockout of Raptor results in muscular dystrophy115.
Downstream effectors – nuclear receptors, NRF1, TFAM
Nuclear receptors are popular targets for drug discovery as many nuclear receptors can be activated by small-molecule ligands. Ligand binding changes the conformation of nuclear receptors, facilitating the exchange of transcriptional co-repressors for co-activators and inducing the transcription of their target genes. The three peroxisome proliferator-activated receptors (PPARs), PPARα, PPARδ (also known as PPARβ) and PPARγ, constitute a small subfamily of the large nuclear receptor gene family116–118. Although fatty acids are natural PPAR ligands, several synthetic PPAR ligands have been identified. PPARα has a crucial role in the adaptive response to fasting, by inducing the expression of genes that are involved in fatty acid oxidation119. Consequently, activation of PPARα by fibrates has been shown to reduce hyperlipidaemia and improve insulin sensitivity in patients with type 2 diabetes116,117. Similarly, synthetic PPARδ agonists such as L-165041 or GW501516 improve hyperlipidaemia and insulin sensitivity and reduce adiposity in mice120,121 and obese patients122, an effect that is linked to enhanced mitochondrial biogenesis and activity108,121.
Recently, it was proposed that this effect of PPARδ on mitochondria could improve fatty acid oxidation in the context of inherited mitochondrial disorders. Cells derived from patients with a deficiency in very-longchain-acyl-CoA dehydrogenase (VLCAD; also known as ACADVL) were treated with the PPARδ agonist bezafibrate, which restored VLCAD gene expression123,124. In patients with carnitine O-palmitoyltransferase 2 (CPT2) deficiency, bezafibrate substantially increased the rates of fatty acid oxidation and CPT2 gene expression in muscle125. When administered to mouse models of complex IV deficiency, bezafibrate was unable to fully restore complex IV activity109. The final member of the PPAR family, PPARγ, also has a pleiotropic role in metabolic homeostasis126. Although potent PPARγ agonists such as rosiglitazone have been successfully used to treat type 2 diabetes, they became sidelined owing to their potential adverse effects127. It became clear that less potent PPARγ modulators that selectively modify the recruitment of specific co-factors exhibit fewer side effects than the traditional PPARγ agonists but maintain beneficial effects on energy homeostasis128,129 (reviewed in REF. 130).
Interestingly, one of the heterodimerization partners of PPARs, the retinoid X receptor-α (RXRα), was recently shown to be involved in mitochondrial retrograde signalling in cybrid cells containing different loads of mt3243, an mtDNA carrying a mutation in the gene encoding tRNALeu (tRNA recognizing a triplet codon for leucine)131. The oxidative phosphorylation deficiency in these cybrid cells was accompanied by a decrease in the expression of RXRα and of mitochondrial genes, and was reversed by the RXR agonist retinoic acid131. The decrease in RXRα activity was also dependent on JUN N-terminal kinase (JNK) activation by reactive oxygen species (ROS) and reversed by JNK inhibitors131. These data suggest that increasing the transcriptional activity of RXRα, either using a direct activator such as retinoic acid or using JNK inhibitors, might restore the efficiency of oxidative phosphorylation. Further work is required to determine whether this also applies to other types of mtDNA mutations or nDNA mutations.
Oestrogen-related receptor-α (ERRα) and ERRγ also regulate mitochondrial biogenesis132, as shown by genome-wide location analyses identifying ERRα- and ERRγ-binding sites in several genes encoding mitochondrial proteins133, and by studies in mouse models showing that these receptors coordinate many aspects of oxidative metabolism in muscle tissue134,135. Given the beneficial effects of these receptors on mitochondrial function, efforts to develop specific ligands for ERRs — which have long been considered to be constitutively active orphan nuclear receptors132 — have intensified. Indeed, the finding that 4-hydroxytamoxifen can specifically antagonize ERRγ shows that it is possible to modulate the activity of these receptors using exogenous compounds136. ERRγ agonists have been identified137,138, but no data on their effects in mitochondrial disease models are yet available. However, only inverse agonists have been described for ERRα139–141, which is congruent with the outcome of structural activity studies indicating that it is challenging to activate ERRα using small molecules142,143.
Interestingly, a diaryl ether-based ERRα inverse agonist improved glucose homeostasis in rodent models of type 2 diabetes and stimulated the expression of genes involved in mitochondrial metabolism and insulin sensitization in the liver141. In the same vein, treatment of leptin-receptor-deficient (db/db) mice with GSK5182, an inverse agonist of ERRγ, reduced hyperglycaemia through inhibition of hepatic gluconeogenesis144. These observations could possibly be explained by the promiscuity of ERRα and ERRγ for target genes and their compensatory induction when one ERR is inhibited133. Further studies are required to elucidate the crosstalk among the ERRs and to define whether inverse agonists or agonists are desired to modulate mitochondrial function and manage metabolic diseases.
Finally, nuclear respiratory factor 1 (NRF1) and TFAM are two nDNA-encoded transcription factors that have a crucial impact on mitochondrial function. NRF1 promotes, among others, the transcription of ETC subunits and nDNA-encoded mitochondrial transcription factors, including TFAM145. The stabilization and activation of NRF1 was achieved by inhibiting its natural antisense transcript146. A recombinant form of human TFAM was designed, in which an exogenous amino-terminal domain allows rapid translocation across cell membranes, whereas its mitochondrial targeting signal stimulates mitochondrial uptake147. Treatment of aged mice with recombinant human TFAM stimulated oxidative metabolism and improved memory148. In addition, treatment of cells derived from patients with Leber’s hereditary optic neuropathy (LHON) and Leigh syndrome using recombinant human TFAM and non-mutated mtDNA restored mitochondrial biogenesis and respiration149. However, although these studies indicate that TFAM activation may represent a promising strategy for the treatment of mitochondrial diseases147–149, it should be noted that aged Tfam-transgenic mice displayed an increased mtDNA copy number that was associated with unexpected mtDNA deletions and ETC deficiency150. Further work is therefore required to determine the safety window of this approach.
Downstream effectors – cofactors
The activity of transcription factors results from the delicate balance between inhibitory effects of co-repressors and stimulatory effects of co-activators. This balance can be exploited for therapeutic purposes by fine-tuning or directing the activity of co-factors towards specific transcription factors, pathways or cells and tissues. For instance, selective recruitment of the co-factor steroid receptor co-activator protein (SRC1; also known as NCOA1) instead of its family members SRC2 (also known as NCOA2 or GRIP1)151 or SRC3 (also known as NCOA3)152 orients PPARγ activity towards an oxidative programme, resulting in enhanced thermogenesis and protection against obesity and type 2 diabetes in mice151,153. Specific PPARγ ligands such as Fmoc-l-Leu induce a particular conformational change in PPARγ that translates into selective SRC1 recruitment and insulin sensitization, without the induction of the weight gain that is commonly associated with PPARγ activation128.
The similar effects observed with SR1664 and SR1824, two PPARγ ligands that lack classical transcriptional agonist activity but mediate their effects via the inhibition of cyclin-dependent kinase 5 (CDK5) phosphorylation, were probably also due to selective recruitment of the oxidative co-factor PGC1α129,154. The induction of PGC1α levels has also been explored as a strategy to boost mitochondrial biogenesis. In a screen performed in mouse white adipocytes, antagonists of transient receptor potential vanilloid 4 (TRPV4) induced PGC1α expression, mitochondrial biogenesis and fat browning155. Similarly, irisin, a hormone (and so-called myokine) that is secreted by muscle tissue following exercise, stimulated a broad PGC1α-mediated gene expression programme leading to the browning of white fat156. Bile acids can also stimulate oxidative metabolism in brown adipose tissue and skeletal muscle through the activation of G protein-coupled bile acid receptor 1 (GPBAR1; also known as TGR5)157. Activated TGR5 induces the cyclic AMP-dependent thyroid hormone-activating enzyme type 2 iodothyronine deiodinase (DIO2), which leads to activation of the thyroid hormone receptor and subsequent induction of PGC1α157.
Inhibition of transcriptional co-repressors of the PPARs and ERRs also enhances mitochondrial function. For example, in muscle-specific nuclear receptor corepressor 1 (Ncor1)-mutant mice there was an observed increase in both muscle mass and in mitochondrial number and activity, a phenotype that is also conserved in worms70. In line with these results, reduced NCOR1 function in mice has been linked to ketogenesis in the liver158 and to reduced fat accumulation in adipose tissue159, in a manner reminiscent of PGC1α activation. Furthermore, these tissue-specific loss-of-NCOR1-function studies suggest that inhibiting mTOR complex 1 (mTORC1)158 and/or insulin signalling70 may be a pharmacologically viable way to attenuate NCOR1 signalling. Alternatively, inhibition of deacetylases (such as histone deacetylase 3 (HDAC3)), which interact with NCOR1, can result in similar beneficial effects on oxidative metabolism, as indicated by the improved muscle function observed after pharmacological inhibition of HDAC3 in mice160, reduced adipogenesis after pharmacological inhibition of HDAC3 in cells161 and reduced gluconeogenesis in liver-specific Hdac3-knockout mice162.
Other co-factors that are capable of affecting oxidative metabolism include receptor-interacting protein 140 (RIP140; also known as NRIP1), which functions as a corepressor for several nuclear receptors such as PPARs and ERRα163. Genetic ablation of RIP140 increases mitochondrial biogenesis and oxidative metabolism in muscle164 and adipose tissue163, and protects mice against metabolic diseases165,166. The retinoblastoma protein Rb can also have a major impact on oxidative metabolism through its repressive actions on the transcription factor E2F1, which is a key regulator of cell proliferation and metabolism167. In fact, the absence of Rb favours the development of more oxidative programmes in brown adipose tissue161,168–170 and muscle167, as evidenced through both in vitro and in vivo studies. Intervening in either the RIP140–nuclear receptor or E2F1–Rb pathways may therefore represent another approach to modulate mitochondrial function, but the potential tumour-promoting effects of Rb inhibition as well as the induction of sterility resulting from the loss of RIP140 function in female mice171 must be considered.
Mitochondrial quality control
The central position of mitochondria in metabolism makes them vulnerable to damage. First, mitochondria are a site of oxidative stress generation, in particular at the level of complex I and III of the ETC, where electrons might react prematurely with oxygen, leading to the accumulation of ROS172. Although ROS may have a signalling function in healthy cells173, they can also damage lipids, proteins and DNA. Mammalian cells have therefore developed a battery of protective systems to tightly regulate ROS levels. This includes the presence of uncoupling proteins, which dissipate the proton gradient across the mitochondrial inner membrane174, the production of antioxidant enzymes that dampen ROS accumulation and the induction of mitophagy or even apoptosis if ROS levels become too high (FIG. 2).
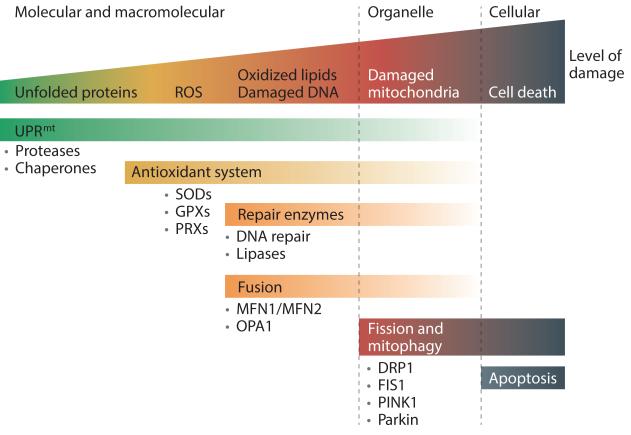
Figure 2. Mitochondrial quality control processes.
A graphical model of the different steps involved in mitochondrial quality control. At a basal level, cells maintain proteostasis within their mitochondria with the help of the mitochondrial unfolded protein response (UPRmt) machinery. If proteostasis is not properly maintained, levels of reactive oxygen species (ROS) might increase following electron transport chain dysfunction and be downregulated by antioxidant enzymes such as superoxide dismutases (SODs), which convert superoxide (O2 −•) into hydrogen peroxide (H2O2), or peroxiredoxins (PRXs) and glutathione peroxidases (GPXs), which remove H2O2. When antioxidant levels are not sufficient, and/or ROS levels are excessive, ROS damage the mitochondrial microenvironment (for example, proteins, mitochondrial DNA (mtDNA) and lipids), resulting in the loss of membrane potential and ATP synthesis efficiency, thereby increasing ROS production in a feedforward reaction. A second line of defence consists of enzymes that repair or eliminate the damaged components: that is, DNA repair enzymes for mtDNA, and lipases for the digestion of oxidized lipids. In parallel, mitochondria can restore their efficiency through fusion– fission cycles235. One hypothesis is that fusion enables mitochondria to exchange their content, and thereby dilute the damaged materials to facilitate their repair or removal. When these mechanisms are insufficient and damage has affected a great portion of the mitochondrion, fission helps to eliminate damaged mitochondria that are beyond repair through mitophagy. Finally, when damage reaches too many mitochondria, these undergo fragmentation followed by apoptosis. DRP1, dynamin-related protein 1; FIS1, mitochondrial fission 1 protein; MFN1, mitofusin 1; OPA1, optic atrophy protein 1; PINK1, PTEN-induced putative kinase 1.
Second, the import of proteins into mitochondria involves the unfolding and refolding of the ~1,500 nuclearencoded mitochondrial proteins when they pass through the two mitochondrial membranes. This poses a major challenge for maintaining proteostasis. Furthermore, the number of proteins encoded by both the nDNA and mtDNA needs to be stoichiometrically matched in the complexes and supercomplexes of the ETC. Both of these challenges make the mitochondria particularly vulnerable to proteotoxic stress. In the mitochondria, proteostasis is maintained by fine-tuning the expression of mitochondrial chaperones in the mitochondrial unfolded protein response (UPR). Abnormal ROS production or proteostasis render the mitochondria vulnerable to the accumulation of damage. Several mitochondrial quality control pathways, which include fusion, fission, mitophagy and protein folding homeostasis, have evolved to efficiently protect mitochondria against these insults. These mitochondrial quality control pathways also open up new opportunities for drug discovery, as summarized below.
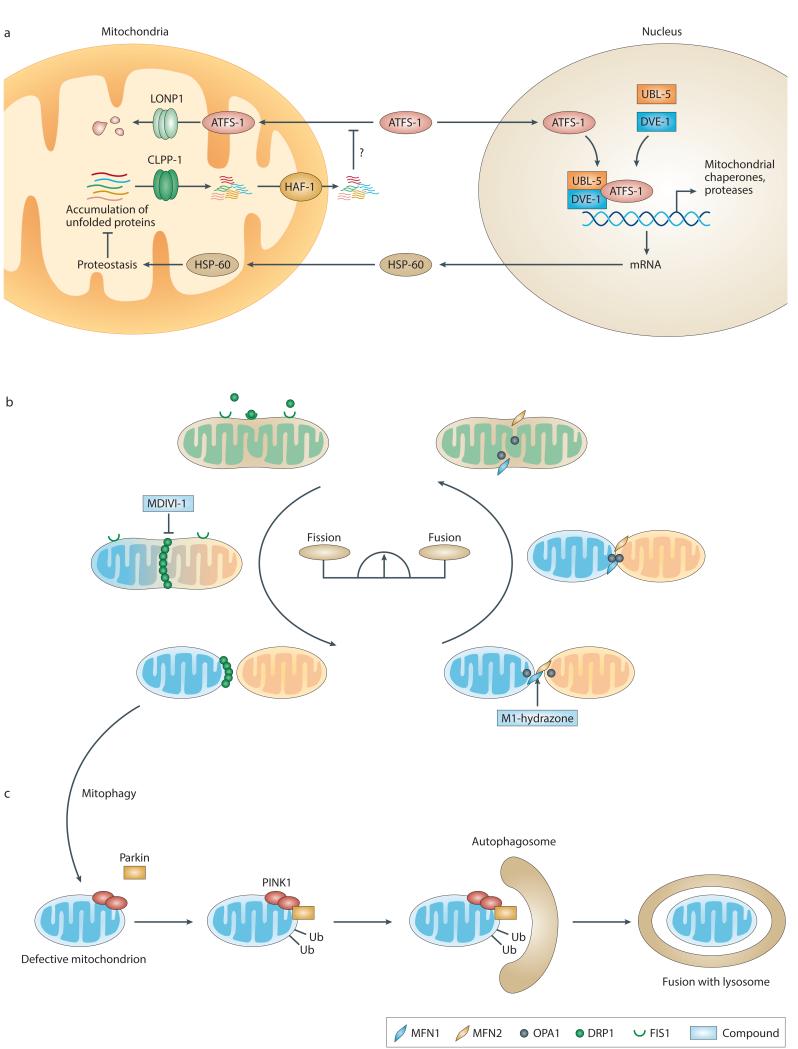
Fusion and fission
Live-imaging technology has revealed the dynamic nature of mitochondria175. Their shape results from the balance between fusion and fission events and involves concerted and balanced actions of fusion proteins (such as mitofusin 1 (MFN1), MFN2 and optic atrophy protein 1 (OPA1)) and fission proteins (such as dynaminrelated protein 1 (DRP1) and mitochondrial fission 1 protein (FIS1))7,9,176. In humans, mutations in fusion proteins lead to the development of neurodegenerative diseases; an OPA1 mutation is associated with autosomal dominant optic atrophy, whereas MFN2 mutations lead to Charcot–Marie–Tooth disease type 2A177,178 (TABLE 1). Diseases caused by mutations in fission proteins are extremely rare in humans179, probably because these proteins are crucial for embryonic development, as illustrated by the embryonic lethality observed as a result of knocking out Drp1 in mice180. Likewise, suppression of either fusion or fission in cultured cells is associated with a deficiency in oxidative phosphorylation, mtDNA loss and mitochondrial heterogeneity (that is, concomitant presence of both abnormal and functional mitochondria)181,182. These data underline the importance of a proper balance between mitochondrial fusion and fission.
Furthermore, there is some evidence to indicate that fusion has a role in physiological processes. MFN2 expression is induced in skeletal muscle and brown adipose tissue of mice exposed to cold temperatures, following the administration of β3-adrenergic receptor agonists or after exercise — conditions that induce energy expenditure183,184. The extent to which the changes in mitochondrial biogenesis, which also occur in these conditions, translate into the modulation of mitochondrial dynamics, however, requires further investigation. Although our understanding of the regulation of fusion and fission is still in its infancy, novel compounds have been identified that are capable of either promoting fusion (that is, M1 hydrazone) 185 or inhibiting fission (that is, the DRP1 inhibitor MDIVI-1)186 (FIG. 3). These two compounds have been mostly tested for their effects on apoptosis in the context of neurodegenerative diseases185,187 and further results on their potential beneficial effects in disease models of fusion and fission are awaited.
Figure 3. Current models of mitochondrial quality control processes.
a | A model of the mitochondrial unfolded protein response in Caenorhabditis elegans. In basal conditions, the transcription factor ATFS-1 (activating transcription factor associated with stress 1) is imported into the mitochondrial matrix via the translocase of the outer membrane (TOM) complex and the translocase of the inner membrane 23 (TIM23) complex, where it is degraded by the mitochondrial Lon peptidase 1 (LONP1). When unfolded proteins accumulate, the CLPP-1 protease generates peptide fragments, which are exported to the cytosol via the HAF-1 transporter. The presence of these peptides in the cytosol inhibits the import of ATFS-1 into mitochondria, which subsequently accumulates in the nucleus through an as yet uncharacterized translocation step. In complex with ubiquitin-like protein 5 (UBL-5) and DVE-1, ATFS-1 then induces the transcription of proteases and mitochondrial chaperones that translocate back into the mitochondria to restore local proteostasis. b | A model of fusion and fission in mammalian cells. The balance between fusion and fission events determines the shape of the mitochondrial network. Fusion of the outer mitochondrial membrane is achieved by the tethering of mitofusin 1 (MFN1) and MFN2, whereas optic atrophy protein 1 (OPA1) is required for the fusion of the inner mitochondrial membrane. The compound M1-hydrazone promotes fusion in an MFN1- and/or MFN2-dependent manner. Fission occurs through the GTPase dynamin-related protein 1 (DRP1), which is recruited by mitochondrial fission 1 protein (FIS1) and is specifically inhibited by the compound MDIVI-1. c | Model of mitophagy in mammalian cells. Defective mitochondria are isolated from the mitochondrial pool by fission (as marked by the arrow). They are characterized by a loss of mitochondrial membrane potential, which is accompanied by the accumulation of PTEN-induced putative kinase 1 (PINK1) at the surface of the mitochondrion. This leads to the recruitment of parkin, which ubiquitylates mitochondrial outer membrane proteins, thereby triggering the recruitment of autophagosomes. The defective mitochondrion is then engulfed in an autophagosome before its fusion with a lysosome and digestion. HSP-60, mitochondrial chaperonin heat shock protein 60 (C. elegans).
Mitophagy
In response to prolonged nutrient deprivation, cells start to digest themselves to recycle intracellular components — a process known as autophagy188. Non-selective macroautophagy is one particular type of autophagy that is triggered by energy stress. During this process, proteins and organelles such as endoplasmic reticulum (ER) or mitochondria are targeted to autophagosomes for subsequent fusion with lysosomes, where they are degraded via acidic lysosomal hydrolases189.
By contrast, mitochondrial autophagy — also called mitophagy — is a type of selective macroautophagy that occurs under nutrient-rich conditions and is central to controlling the number and quality of mitochondria8. The specific recruitment of autophagosomes to mitochondria is mediated by different proteins in mammals according to the cell type and process. For instance, during the maturation of reticulocytes into red blood cells, the expression of the mitochondrial outer membrane NIP3-like protein X (NIX) increases, and NIX directly binds to microtubule-associated protein 1 light chain 3 (MAP1LC3; also known as LC3) to allow the removal of mitochondria by mitophagy190.
In many cultured cell lines, including neurons and HeLa cells, PINK1 and parkin are the key mediators of mitophagy. The loss of mitochondrial membrane potential leads to PINK1 accumulation at the surface of the mitochondria and the recruitment of parkin, which in turn ubiquitylates mitochondrial outer membrane proteins for their recognition by autophagosomes55,191 (FIG. 3). Mutations in parkin or PINK1, which are found in Parkinson’s disease, disrupt parkin recruitment and parkin-induced mitophagy at distinct steps and therefore result in the accumulation of dysfunctional mitochondria191–194. Conversely, in a mouse model of Parkinson’s disease in which Tfam is specifically knocked out in dopaminergic neurons, defective mitochondria accumulate and are not cleared by mitophagy195, although it should be noted that the mitochondrial dysfunction in this model may not fully reflect the pathophysiology of Parkinson’s disease.
Other studies have also demonstrated how mitophagy is dependent on mitochondrial dynamics by showing that overexpression of PINK1 or parkin promotes fission, most probably via the ubiquitylation of MFN1 or MFN2 (REFS 196,197). Although our understanding of this pathway is still evolving, these data suggest that modulation of fusion and fission may be a way to modulate mitophagy. Unravelling the exact mechanisms and links between mitophagy and fusion or fission will probably allow the identification of novel targets that are more specific to mitophagy.
Protein folding homeostasis
Proteotoxicity is often associated with the accumulation of misfolded or unfolded proteins. Cells respond to this accumulation by increasing the level of protein quality control effectors, including chaperones and proteases198. Depending on the subcellular localization of the damage, an organelle-specific UPR is activated: for instance, UPR in the ER (often referred to as ER stress), and UPR in mitochondria3,4.
The mitochondrial UPR reduces the amount of unfolded proteins in the mitochondria by stimulating the transcription of nuclear-encoded mitochondrial chaperones such as heat shock 70 kDa protein 9 (HSPA9; also known as mtHSP70) and the mitochondrial chaperonin heat shock protein 60 (HSP60; also known as HSPD1)3,4 (FIG. 3). In Caenorhabditis elegans, the triggering signal for the mitochondrial UPR is the cleavage of unfolded proteins by the CLPP-1 protease into smaller peptides, which are exported by the HAF-1 transporter in the cytosol. These peptides, through an as yet unknown mechanism, activate the transcription factor ATFS-1 (activating transcription factor associated with stress 1; also known as ZC376.7)199, which — together with co-factors such as ubiquitin-like protein 5 (UBL-5) and DVE-1 (REF. 200) — induces the transcription of genes encoding mitochondrial chaperones and proteases: that is, hsp-6 and hsp-60 (FIG. 3). The mitochondrial UPR is crucial for the longevity of worms with defective oxidative phosphorylation, as the long lifespan of cco-1 worms, which are deficient in cytochrome c oxidase activity, was suppressed in the absence of a functional mitochondrial UPR, as induced by ubl-5 RNA interference (RNAi)201. This response involves noncell-autonomous signalling engaging as yet unidentified mitokines, as selective RNAi of cco-1 in sensory neurons was sufficient to activate the mitochondrial UPR in the worm intestine201.
Interestingly, fibroblast growth factor 21 (FGF21) was recently identified as a biomarker that is secreted by muscle tissue in individuals with mitochondrial respiratory chain deficiencies, which suggests that such non-cell-autonomous signalling might also be conserved in humans202–204. Likewise, the mitochondrial-derived peptide (MDP) humanin, which was initially identified as having a protective effect against neurodegeneration, was shown to be elevated in the skeletal muscle of patients with mtDNA mutations, which indicates that it could be acting as a mitokine (reviewed in REF. 205). Although it is not yet clear what triggers the activation of the mitochondrial UPR, the evidence from cco-1 worms201 and worms treated with the mtDNA depleting agent ethidium bromide206 suggests that it is crucial to maintain a balance in the levels of expression of different proteins in complexes and supercomplexes of the respiratory chain. This was further confirmed by a study in which stoichiometric imbalance between ETC subunits, induced either by inhibiting the translation of mtDNA-encoded proteins (for example, using doxycycline) or by stimulating the translation of nDNA-encoded proteins (for example, using resveratrol or rapamycin), resulted in an induction of the mitochondrial UPR in both worms and mammals207. Such an imbalance was shown to contribute to the beneficial effects of resveratrol and rapamycin, which induce mitochondrial biogenesis and extend fitness and lifespan207.
Potential evidence for a beneficial role of the mitochondrial UPR comes from the inherited disease spastic paraplegia. This rare neurodegenerative disorder is caused by mutations in the HSP60 gene208 and in the paraplegin gene, which encodes a subunit of the m-AAA protease that degrades misfolded proteins and regulates mitochondrial ribosome assembly209,210 (TABLE 2). Two groups have further reported that the mitochondrial UPR is induced in a C. elegans models of Friedriech’s ataxia, a neurodegenerative disease in which the assembly and function of Fe–S cluster-containing subunits of ETC complexes I, II and III is impaired as a result of a mutation in the frataxin gene211–213. Whether it is possible to further increase the mitochondrial UPR in such disease contexts and whether this would be sufficient to restore proteostasis remains to be addressed. Such a strategy may potentially be beneficial for all inherited mitochondrial diseases in which mutations lead to proteotoxicity.
Identifying drugs to treat mitochondrial diseases
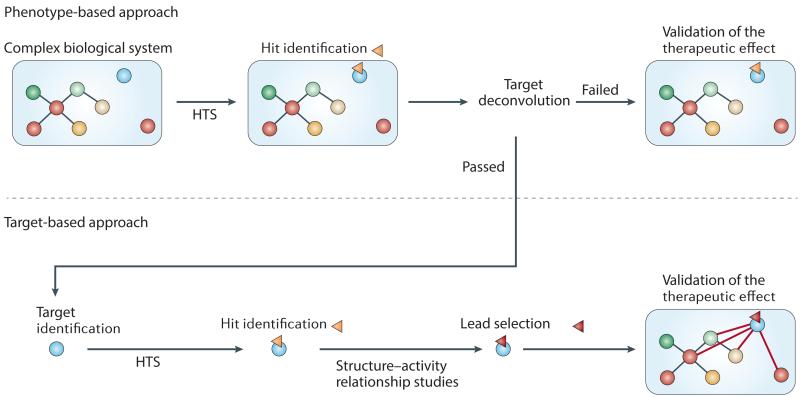
Several compounds that modulate mitochondrial function have been identified via target-based screens (FIG. 4), including compounds that bind to and modulate specific G protein-coupled receptors, nuclear receptors and other transcription factors as well as kinases. Hallmark compounds identified via such a targeted approach include natural, semisynthetic and synthetic agonists for the PPARs128–130 and ERRs137–141,144, SIRT1 (REFS 89,93,95,96, 98–100,214), TGR5 (REFS 215–221) and AMPK222,223. An important advantage of target-based strategies is that they enable structure–activity relationship (SAR) optimization of hits from primary screens. However, in the context of mitochondrial diseases, a target-based drug discovery approach has considerable limitations because a given target is only a small part of the large pleiotropic regulatory networks that govern mitochondrial homeostasis. By contrast, a phenotypic screen allows the identification of novel compounds that do not just modulate a single target or pathway but instead modulate a more global phenotype, without knowing the specific target (FIG. 4). In addition, phenotypic screens can be powerful in identifying novel pathways or proteins involved in the regulatory network of mitochondrial function (FIG. 4). Although phenotypic screens for mitochondrial function are only beginning to emerge, in the section below we assess the various models that may be used for such screens and consider the limitations associated with their design and application.
Figure 4. Models and approaches for mitochondrial screens.
Phenotype-based versus target-based screening approaches are shown. A phenotypic screen aims to identify hit compounds that are able to modulate the activity of a complex biological system that is only partially characterized. When a hit (yellow triangle) is identified, its target may not always be known. Validation of its therapeutic effect can be performed without knowledge of the pathway. If the target can be identified, this can aid the optimization of hits into lead compounds (red triangle) with improved properties and eventually expand knowledge of the pathway, as depicted by the new connections in the network. See TABLE 3 for drawbacks and advantages of model systems for mitochondrial screens. HTS, high-throughput screening.
Models for mitochondrial phenotypic screens
Although immortalized cell lines are convenient because they can be grown in large quantities, these cell lines often lose the physiological features of an in vivo eukaryotic cell, including senescence and cell cycle regulation, and thereby instead resemble transformed cancer cells. This is a major drawback for the identification of drugs targeting mitochondrial function, as most transformed cells are metabolically reprogrammed to address their particular energetic needs: for example, overactivation of the phosphoinositide 3-kinase (PI3K)–mTOR pathway or inhibition of AMPK signalling224. Despite such caveats, immortalized cells have been used for the identification of mitochondrial modulators, as exemplified by the discovery of the fusion promoter M1 hydrazone using an image-based screen in mouse embryonic fibroblasts (MEFs)171 (TABLE 3). Two other studies have identified the hitherto unknown mitochondrial effects of several US Food and Drug Administration (FDA)-approved drugs using phenotypic screens in human fibroblasts206 and in C2C12 myotubes (a mouse muscle cell line)205, as discussed below (TABLE 3).
Table 3. Drawbacks and advantages of model systems for mitochondrial screens*.
| Suitability for high-throughput screening format |
Conservation with human proteins |
Multi-organ physiology readout |
Feasibility of genome-wide screen |
Examples of drug discovery |
|
|---|---|---|---|---|---|
|
Target-based
approach |
|||||
| Isolated target | ++++ | ++++ | NA | NA | |
|
Phenotype-
based approach |
|||||
| Yeast | +++ | ++ | + | ++++ | |
| Immortalized cell lines |
+++ | +++ | + | ++ | |
| Primary cells | −/+ | ++++ | + | −/+ |
|
|
Caenorhabditis
elegans |
++ | ++ | ++++ | +++ |
AMPK, AMP-activated protein kinase; ERR, oestrogen-related receptor; GPBAR1, G protein-coupled bile acid receptor 1; NA, not applicable; PPAR, peroxisome proliferator-activated receptor; SIRT1, sirtuin 1.
Although targeted approaches use isolated targets and directly assess the change in target activity, phenotypic screening approaches can use different models with variable degrees of complexity. Models are ranked by degree of complexity from top to bottom in this table. Several criteria can help to determine the choice of the model. For example, the worm C. elegans is less suitable for high-throughput screening than an assay using isolated proteins or immortalized cell lines, but it models multi-organ physiology and is amenable to high-content screens. The last column provides examples of compounds and drugs that have been discovered using the different models and that are discussed in this article. The ‘−’ and ‘+’ signs are relative comparisons of the different models for each criteria, ranging from not suitable (−/+) to highly suitable (++++).
Primary cell cultures represent an interesting alternative to immortalized cell lines, as they more closely resemble the in vivo metabolic milieu and can be isolated from patients or disease models and thereby even mimic complex genetic diseases (TABLE 3). An image-based screen in human umbilical vein endothelial cells (HUVECs) led to the identification of BRD6897, a compound that seems to govern mitochondrial biogenesis and turnover through a mechanism that is independent of known transcriptional programmes225 (TABLE 3). Primary cells have also been used to identify mitochondrial toxins226–228.
Other approaches using more primitive but intact organisms have proven to be valuable for identifying and functionally characterizing compounds that affect mitochondria. The budding yeast Saccharomyces cerevisiae is particularly interesting owing to the high level of conservation of mitochondrial genes and function (TABLE 3). For example, the mitochondrial division inhibitor MDIVI-1 was identified in a yeast screen by its capacity to suppress the growth defect of mitochondrial fusion mutants186. Likewise, chlorhexidine was identified as being able to rescue yeast ATP synthase mutants, which phenotypically resemble human inherited mitochondrial diseases such as the NARP (neuropathy, ataxia and retinitis pigmentosa) syndrome229 (TABLE 3). Nevertheless, owing to the simplicity of the unicellular yeast, it cannot be used to model a disease at the scale of an organ or an intact organism. However, this can be partly achieved in invertebrate animal models such as the nematode C. elegans, which has the advantage of modelling physiology at the multi-organ level while now being manageable at the scale of high-throughput screening230 (TABLE 3). Like in yeast, most biological processes and genes involved in mitochondrial function are conserved in C. elegans, and the convenience of performing genome-wide RNAi screens aids the identification of the pathways that underlie the effects of the compounds231 (TABLE 3).
Design of mitochondrial phenotypic screens
The use of phenotypic screens for drug discovery requires careful design, especially in the context of mitochondria. In fact, owing to the high metabolic flexibility of higher organisms, multiple readouts and complementary tests are required to elucidate the mechanism of action of a given compound. For example, glycolysis activators and oxidative phosphorylation inhibitors both reduce cellular respiration. If respiration is the only measured parameter, the only way to distinguish between these two compounds is to test them at different concentrations; a glycolysis activator should be harmless compared to an oxidative phosphorylation inhibitor at a high dose. Alternatively, these two types of compounds could be compared in a pro-glycolytic (for example, glucose) and pro-oxidative (for example, galactose) culture medium; a respiration inhibitor will be more toxic under pro-oxidative conditions but it may have no effect under pro-glycolytic conditions. This latter strategy (comparing compounds in pro-glycolytic or pro-oxidative culture medium) was used to assess the impact of compounds on the viability of human fibroblasts and led to the characterization of the metabolic effect of the antiemetic drug meclizine232.
Another way to distinguish between two different classes of drugs that have the same effect on a given metabolic aspect is to analyse several parameters in parallel to obtain a so-called footprint of the effect of each compound on mitochondrial activity. For example, simultaneous measurement of mitochondrial and related viability parameters, combined with a gene expression survey, of mouse C2C12 myotubes treated with FDA-approved drugs led to the identification of negative modulators of mitochondrial function, such as the HMG-CoA reductase inhibitors, as well as stimulants of the transcription of genes involved in oxidative phosphorylation, such as microtubule destabilizers (for example, podophyllotoxin)233.
A further improvement would be to obtain more comprehensive and complex mitochondrial footprints of compounds and drugs by measuring as many parameters as possible at a given time. For example, one of the gaps in our understanding of mitochondrial function is why both inhibition and stimulation of respiration can improve health and extend lifespan in primitive organisms such as yeast and worms. Such a question could be addressed by aligning respiration, biogenesis, mitochondrial dynamics and viability profiles in cells with metabolic characterization and lifespan assays in yeast and worms. In our own studies, we selected a set of mitochondrial function assays to construct a detailed atlas of mitochondrial footprints or signatures of known drugs with mitochondrial activity (BOX 3). This strategy could enable the accurate mapping of mitochondrial pathways affected by new compounds and provide a biochemical approach to further define mitochondrial regulatory networks.
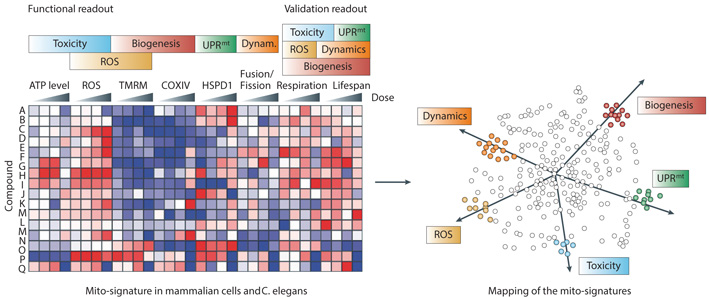
Box 3. Functional readouts to obtain mitochondrial fingerprints.
Phenotypic screens offer the possibility to simultaneously record several parameters and hence obtain a more global footprint of the activity of a compound on mitochondria (see the figure). Ideally, these different parameters should be representative of the array of functions of interest and should first be performed with mitochondrial benchmark compounds. Below, we highlight a compendium of mitochondrial tests that could be used to define a multiscalar mitochondrial signature for a given compound. A representative example of results obtained using this array of tests performed in our laboratory is shown in the left panel of the figure. The heat map represents changes (blue for decrease and red for increase compared to vehicle control) in the different signals after treatment with increasing doses of mitochondrial benchmark compounds.
Determination of ATP levels is an effective and robust way to assess compound toxicity in cells233. Reactive oxygen species (ROS) are important signalling molecules but high levels are deleterious. ROS can therefore be used to assess both toxicity and ROS homeostasis. Several methods to directly measure ROS using fluorescent probes have been described in cells247. The most promising tools for specific and quantitative ROS measurements are fluorescent protein-based redox probes248, but their use requires a transfection step, which can be limiting. The mitochondrial membrane potential (ΔψM) can be assessed by fluorescent probes, such as tetramethylrhodamine (TMRM), that accumulate inside mitochondria proportionally to ΔψM without having any impact on mitochondrial respiration. TMRM can also provide information about mitochondrial abundance and thereby both mitochondrial biogenesis and efficiency. Several parameters of mitochondrial function, including mitochondrial biogenesis and the mitochondrial unfolded protein response (UPRmt) can also be monitored either directly by measuring gene expression or by using luciferase reporter assays. In the case of mitochondrial biogenesis, appropriate readouts include levels of expression of one of the respiratory complex subunits, such as the cytochrome c oxidase subunit IV (COXIV), measured either directly (for example, at the mRNA level) or indirectly (for example, using a promoter reporter activity assay). A similar approach can be applied to measure the activation of the UPRmt by measuring changes in mRNA levels of mitochondrial chaperonin heat shock protein 60 (HSP60) or HSP60 promoter reporter activity. The only way to assess mitochondrial dynamics is by cellular imaging. Systematic image analysis software now makes it possible to quantify mitochondrial networks in cells transfected with mitochondrially targeted green fluorescent protein (GFP) in a high-throughput manner185. Furthermore, through the development of multiwell format oxygen-dependent fluorescence quenching systems, it has become possible to evaluate respiration in a high-throughput format225,232. Importantly, this technology can also be applied to measure respiration in Caenorhabditis elegans207. Finally, lifespan, activity and fitness assays in worms are good surrogates to assess the general impact of compounds on mitochondria and physiological homeostasis249. Importantly, such tests already indicate the potential effect of a compound at the scale of an entire organism.
It is important to underscore that the combination of several of these assays is desirable and most valuable to characterize new compounds. By combining the results of several tests for all compounds, it is possible to define a comprehensive set of mitochondrial signatures that enable the clustering of novel chemical entities according to their footprint on mitochondrial function (see right panel of figure). Such a signature will also provide insight into the particular mitochondrial signalling pathways that are affected, facilitating downstream target deconvolution.
Conclusion/Perspectives
Understanding how proteins that are encoded by mitochondrial and nuclear genomes work together with metabolites to maintain mitochondrial homeostasis continues to be a major research challenge. Mitochondrial function is regulated by a complex network of sensors and effectors, and so a multigenic and holistic approach is best suited for understanding the physiology and the pathophysiology associated with this organelle. At present, by far the best-characterized aspect of the mitochondrial regulatory network is how sensors of the nutrient and energy status (such as AMPK, NAD+ and SIRT1) and their downstream transcriptional effectors govern mitochondrial biogenesis. However, other key features that regulate mitochondrial function, such as fusion and fission, mitophagy and the mitochondrial UPR, have recently also been elucidated.
Several lines of evidence have suggested that mitochondrial biogenesis and other processes should not be seen as independent but instead as concomitant and interdependent phenomena. A few examples illustrate this interdependency. First, the mitochondrial UPR is induced during the L3–L4 stage of larval development of C. elegans, a phase during which mitochondrial biogenesis also takes place4,234. This is further supported by the fact that resveratrol and rapamycin, two compounds that induce mitochondrial biogenesis and extend fitness and lifespan, also induce the mitochondrial UPR207. Second, the balance between fusion and fission events affects the structure of the inner boundary membrane, which is a site that is enriched in proteins involved in translocation235. Therefore, processes that require massive protein translocation within mitochondria, such as mitochondrial biogenesis or the mitochondrial UPR, are also likely to be linked to fusion and fission events. The intertwined nature of these mitochondrial homeostatic processes also underscores that our understanding of the mitochondrial regulatory network is only in its infancy, and suggests that phenotypic screens, coupled with subsequent deconvolution of the targets of hit compounds, might be the best way to not only recognize new compounds that restore mitochondrial function but also identify existing compounds that are toxic to mitochondria. Using this approach, we can expect the emergence of new targets and compounds that could lead to the development of drugs for both rare and common diseases in which dysfunctional mitochondria are implicated.
Acknowledgements
The authors thank R. Wanders for critically reading the manuscript. R.H.H. is financially supported by an AMC Postdoctoral fellowship and a ZonMw-VENI grant (number 91613050). J.A. is the Nestlé Chair in Energy Metabolism and work in his laboratory is supported by the École polytechnique fédérale de Lausanne (EPFL), the EU Ideas program (ERC-2008-AdG-231138), the US National Institutes of Health (grants 1R01HL 106511-01A1 and R01AG043930), the Velux Stiftung Research Grant Program and the Swiss National Science Foundation (grants 31003A-124713 and CRSII3-136201).
Glossary
- Mitochondrial DNA (mtDNA)
A 16.5kb circular DNA sequence carried within mitochondria, composed of a light and heavy strand. Both strands contain 37 genes, including 13 that encode protein subunits of the OXPHOS complexes, while the remaining code for rRNA and tRNA molecules that are essential for transcription and synthesis of mitochondrially encoded proteins.
- Oxydative phosphorylation
Enzymatic phosphorylation of ADP to ATP, which is coupled to electron transfer from a substrate to molecular oxygen in the electron transport chain.
- Heteroplasmy
A mixture of different forms of mitochondrial DNA within a single cell
- Quantitative trait loci (QTLs)
Genetic loci contributing quantitatively to a trait or phenotype. A QTL partly explains the genetic contribution to a given phenotype.
- Proteostasis
Homeostasis of the protein folding landscape.
- Caloric restriction diet
A diet that involves the consumption of 20-50% less calories than normal without causing malnutrition: that is, with maintainance of proper vitamin and mineral intake.
- NAD+
The oxidized version of NAD; serves as a co-factor in oxidation-reduction reactions. NAD+ also acts as an obligatory co-substrate for sirtuin-mediated deacylation reactions.
- Inverse agonists
Compounds that bind to the same receptor binding-site as a prototypical agonist for that given receptor. Through this binding, inverse agonists reverse the basal or constitutive activity of the receptor. Oestrogen-related receptor-α is an example of constitutively active nuclear receptor for which inverse agonists exist.
- mtDNA haplogroup
A group sharing the same single nucleotide polymorphism (SNP) on mitochondrial DNA (mtDNA). Some haplogroups have been suggested to have a greater likelihood of predisposing individuals to Alzheimer’s disease.
- Mitokine
A signalling molecule that is produced by mitochondria in a given tissue and affects mitochondrial function in a distinct tissue.
- Myokine
A signalling molecule that is produced by the muscle and has cytokine-like properties.
References
- 1.Wallin IE, Wallin Ivan E. Symbionticism and the origin of species. Williams & Wilkins Company; Baltimore: 1927. [Google Scholar]
- 2.Pagliarini DJ, et al. A mitochondrial protein compendium elucidates complex I disease biology. Cell. 2008;134:112–23. doi: 10.1016/j.cell.2008.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study provides the list of mitochondrial proteins
- 3.Ryan MT, Hoogenraad NJ. Mitochondrial-nuclear communications. Annu Rev Biochem. 2007;76:701–22. doi: 10.1146/annurev.biochem.76.052305.091720. [DOI] [PubMed] [Google Scholar]
- 4.Haynes CM, Ron D. The mitochondrial UPR - protecting organelle protein homeostasis. J Cell Sci. 2010;123:3849–55. doi: 10.1242/jcs.075119. [DOI] [PubMed] [Google Scholar]
- 5.Schmidt O, Pfanner N, Meisinger C. Mitochondrial protein import: from proteomics to functional mechanisms. Nat Rev Mol Cell Biol. 2010;11:655–67. doi: 10.1038/nrm2959. [DOI] [PubMed] [Google Scholar]
- 6.Rugarli EI, Langer T. Mitochondrial quality control: a matter of life and death for neurons. EMBO J. 2012;31:1336–49. doi: 10.1038/emboj.2012.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Westermann B. Mitochondrial fusion and fission in cell life and death. Nat Rev Mol Cell Biol. 2010;11:872–84. doi: 10.1038/nrm3013. [DOI] [PubMed] [Google Scholar]
- 8.Youle RJ, Narendra DP. Mechanisms of mitophagy. Nat Rev Mol Cell Biol. 2011;12:9–14. doi: 10.1038/nrm3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nunnari J, Suomalainen A. Mitochondria: in sickness and in health. Cell. 2012;148:1145–59. doi: 10.1016/j.cell.2012.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lin MT, Beal MF. Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature. 2006;443:787–95. doi: 10.1038/nature05292. [DOI] [PubMed] [Google Scholar]
- 11.Patti ME, Corvera S. The role of mitochondria in the pathogenesis of type 2 diabetes. Endocr Rev. 2010;31:364–95. doi: 10.1210/er.2009-0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vafai SB, Mootha VK. Mitochondrial disorders as windows into an ancient organelle. Nature. 2012;491:374–83. doi: 10.1038/nature11707. [DOI] [PubMed] [Google Scholar]
- 13.Wallace DC. Mitochondrial diseases in man and mouse. Science. 1999;283:1482–8. doi: 10.1126/science.283.5407.1482. [DOI] [PubMed] [Google Scholar]
- 14.Shoubridge EA. Cytochrome c oxidase deficiency. Am J Med Genet. 2001;106:46–52. doi: 10.1002/ajmg.1378. [DOI] [PubMed] [Google Scholar]
- 15.Kerstann K, Brown M, Vockley I, Wallace D. Metabolic and Molecular Bases of Inherited Disease. McGraw-Hill; New York: 2001. (ed. al., V.e.) [Google Scholar]
- 16.Sharpley MS, et al. Heteroplasmy of Mouse mtDNA Is Genetically Unstable and Results in Altered Behavior and Cognition. Cell. 2012;151:333–43. doi: 10.1016/j.cell.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]; This paper demonstrates that heteroplasmy for two wild-type mtDNAs is sufficient to alter metabolism and cognitive function in mice.
- 17.Jenuth JP, Peterson AC, Shoubridge EA. Tissue-specific selection for different mtDNA genotypes in heteroplasmic mice. Nat Genet. 1997;16:93–5. doi: 10.1038/ng0597-93. [DOI] [PubMed] [Google Scholar]; This study reports that mtDNA segregates differently from one tissue to another.
- 18.Zeviani M, Di Donato S. Mitochondrial disorders. Brain. 2004;127:2153–72. doi: 10.1093/brain/awh259. [DOI] [PubMed] [Google Scholar]
- 19.Koene S, Smeitink J. Mitochondrial medicine: entering the era of treatment. J Intern Med. 2009;265:193–209. doi: 10.1111/j.1365-2796.2008.02058.x. [DOI] [PubMed] [Google Scholar]
- 20.Wallace DC, Fan W, Procaccio V. Mitochondrial energetics and therapeutics. Annu Rev Pathol. 2010;5:297–348. doi: 10.1146/annurev.pathol.4.110807.092314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Andreux PA, et al. Systems genetics of metabolism: the use of the BXD murine reference panel for multiscalar integration of traits. Cell. 2012;150:1287–99. doi: 10.1016/j.cell.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]; This paper exploits the BXD strains as a potential resource for the complex genetics underlying metabolic phenotypes related to mitochondrial dysfunction.
- 22.Kenyon CJ. The genetics of ageing. Nature. 2010;464:504–12. doi: 10.1038/nature08980. [DOI] [PubMed] [Google Scholar]
- 23.Laplante M, Sabatini DM. mTOR signaling in growth control and disease. Cell. 2012;149:274–93. doi: 10.1016/j.cell.2012.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hardie DG, Ross FA, Hawley SA. AMPK: a nutrient and energy sensor that maintains energy homeostasis. Nat Rev Mol Cell Biol. 2012;13:251–62. doi: 10.1038/nrm3311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Houtkooper RH, Pirinen E, Auwerx J. Sirtuins as regulators of metabolism and healthspan. Nat Rev Mol Cell Biol. 2012;13:225–38. doi: 10.1038/nrm3293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Houtkooper RH, Williams RW, Auwerx J. Metabolic networks of longevity. Cell. 2010;142:9–14. doi: 10.1016/j.cell.2010.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Corsetti G, et al. Morphometric changes induced by amino acid supplementation in skeletal and cardiac muscles of old mice. Am J Cardiol. 2008;101:26E–34E. doi: 10.1016/j.amjcard.2008.02.078. [DOI] [PubMed] [Google Scholar]
- 28.Boudina S, et al. Contribution of impaired myocardial insulin signaling to mitochondrial dysfunction and oxidative stress in the heart. Circulation. 2009;119:1272–83. doi: 10.1161/CIRCULATIONAHA.108.792101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hyyti OM, Ledee D, Ning XH, Ge M, Portman MA. Aging impairs myocardial fatty acid and ketone oxidation and modifies cardiac functional and metabolic responses to insulin in mice. Am J Physiol Heart Circ Physiol. 2010;299:H868–75. doi: 10.1152/ajpheart.00931.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Houtkooper RH, et al. The metabolic footprint of aging in mice. Scientific Reports. 2011;1 doi: 10.1038/srep00134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sinha R, et al. Assessment of skeletal muscle triglyceride content by (1)H nuclear magnetic resonance spectroscopy in lean and obese adolescents: relationships to insulin sensitivity, total body fat, and central adiposity. Diabetes. 2002;51:1022–7. doi: 10.2337/diabetes.51.4.1022. [DOI] [PubMed] [Google Scholar]
- 32.Kotronen A, Seppala-Lindroos A, Bergholm R, Yki-Jarvinen H. Tissue specificity of insulin resistance in humans: fat in the liver rather than muscle is associated with features of the metabolic syndrome. Diabetologia. 2008;51:130–8. doi: 10.1007/s00125-007-0867-x. [DOI] [PubMed] [Google Scholar]
- 33.Kelley DE, He J, Menshikova EV, Ritov VB. Dysfunction of mitochondria in human skeletal muscle in type 2 diabetes. Diabetes. 2002;51:2944–50. doi: 10.2337/diabetes.51.10.2944. [DOI] [PubMed] [Google Scholar]
- 34.Petersen KF, Dufour S, Befroy D, Garcia R, Shulman GI. Impaired mitochondrial activity in the insulin-resistant offspring of patients with type 2 diabetes. N Engl J Med. 2004;350:664–71. doi: 10.1056/NEJMoa031314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hwang H, et al. Proteomics analysis of human skeletal muscle reveals novel abnormalities in obesity and type 2 diabetes. Diabetes. 2010;59:33–42. doi: 10.2337/db09-0214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mootha VK, et al. Integrated analysis of protein composition, tissue diversity, and gene regulation in mouse mitochondria. Cell. 2003;115:629–40. doi: 10.1016/s0092-8674(03)00926-7. [DOI] [PubMed] [Google Scholar]
- 37.Patti ME, et al. Coordinated reduction of genes of oxidative metabolism in humans with insulin resistance and diabetes: Potential role of PGC1 and NRF1. Proc Natl Acad Sci U S A. 2003;100:8466–71. doi: 10.1073/pnas.1032913100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Krishnan J, et al. Dietary obesity-associated Hif1alpha activation in adipocytes restricts fatty acid oxidation and energy expenditure via suppression of the Sirt2-NAD+ system. Genes Dev. 2012;26:259–70. doi: 10.1101/gad.180406.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mustelin L, et al. Acquired obesity and poor physical fitness impair expression of genes of mitochondrial oxidative phosphorylation in monozygotic twins discordant for obesity. Am J Physiol Endocrinol Metab. 2008;295:E148–54. doi: 10.1152/ajpendo.00580.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pihlajamaki J, et al. Thyroid hormone-related regulation of gene expression in human fatty liver. J Clin Endocrinol Metab. 2009;94:3521–9. doi: 10.1210/jc.2009-0212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Takamura T, et al. Obesity upregulates genes involved in oxidative phosphorylation in livers of diabetic patients. Obesity (Silver Spring) 2008;16:2601–9. doi: 10.1038/oby.2008.419. [DOI] [PubMed] [Google Scholar]
- 42.Poussin C, et al. Oxidative phosphorylation flexibility in the liver of mice resistant to high-fat diet-induced hepatic steatosis. Diabetes. 2011;60:2216–24. doi: 10.2337/db11-0338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Auwerx J. Improving metabolism by increasing energy expenditure. Nat Med. 2006;12:44–5. doi: 10.1038/nm0106-44. discussion 45. [DOI] [PubMed] [Google Scholar]
- 44.Meex RC, et al. Restoration of muscle mitochondrial function and metabolic flexibility in type 2 diabetes by exercise training is paralleled by increased myocellular fat storage and improved insulin sensitivity. Diabetes. 2010;59:572–9. doi: 10.2337/db09-1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Phielix E, Meex R, Moonen-Kornips E, Hesselink MK, Schrauwen P. Exercise training increases mitochondrial content and ex vivo mitochondrial function similarly in patients with type 2 diabetes and in control individuals. Diabetologia. 2010;53:1714–21. doi: 10.1007/s00125-010-1764-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pospisilik JA, et al. Targeted deletion of AIF decreases mitochondrial oxidative phosphorylation and protects from obesity and diabetes. Cell. 2007;131:476–91. doi: 10.1016/j.cell.2007.08.047. [DOI] [PubMed] [Google Scholar]
- 47.Vernochet C, et al. Adipose-Specific Deletion of TFAM Increases Mitochondrial Oxidation and Protects Mice against Obesity and Insulin Resistance. Cell Metab. 2012 doi: 10.1016/j.cmet.2012.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Douglas PM, Dillin A. Protein homeostasis and aging in neurodegeneration. J Cell Biol. 2010;190:719–29. doi: 10.1083/jcb.201005144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Valente EM, et al. Localization of a novel locus for autosomal recessive early-onset parkinsonism, PARK6, on human chromosome 1p35-p36. Am J Hum Genet. 2001;68:895–900. doi: 10.1086/319522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kitada T, et al. Mutations in the parkin gene cause autosomal recessive juvenile parkinsonism. Nature. 1998;392:605–8. doi: 10.1038/33416. [DOI] [PubMed] [Google Scholar]
- 51.Dagda RK, et al. Loss of PINK1 function promotes mitophagy through effects on oxidative stress and mitochondrial fission. J Biol Chem. 2009;284:13843–55. doi: 10.1074/jbc.M808515200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cui M, Tang X, Christian WV, Yoon Y, Tieu K. Perturbations in mitochondrial dynamics induced by human mutant PINK1 can be rescued by the mitochondrial division inhibitor mdivi-1. J Biol Chem. 2010;285:11740–52. doi: 10.1074/jbc.M109.066662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kamp F, et al. Inhibition of mitochondrial fusion by alpha-synuclein is rescued by PINK1, Parkin and DJ-1. EMBO J. 2010;29:3571–89. doi: 10.1038/emboj.2010.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Krebiehl G, et al. Reduced basal autophagy and impaired mitochondrial dynamics due to loss of Parkinson’s disease-associated protein DJ-1. PLoS One. 2010;5:e9367. doi: 10.1371/journal.pone.0009367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vives-Bauza C, et al. PINK1-dependent recruitment of Parkin to mitochondria in mitophagy. Proc Natl Acad Sci U S A. 2010;107:378–83. doi: 10.1073/pnas.0911187107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hansson Petersen CA, et al. The amyloid beta-peptide is imported into mitochondria via the TOM import machinery and localized to mitochondrial cristae. Proc Natl Acad Sci U S A. 2008;105:13145–50. doi: 10.1073/pnas.0806192105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Barsoum MJ, et al. Nitric oxide-induced mitochondrial fission is regulated by dynamin-related GTPases in neurons. EMBO J. 2006;25:3900–11. doi: 10.1038/sj.emboj.7601253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Aleardi AM, et al. Gradual alteration of mitochondrial structure and function by beta-amyloids: importance of membrane viscosity changes, energy deprivation, reactive oxygen species production, and cytochrome c release. J Bioenerg Biomembr. 2005;37:207–25. doi: 10.1007/s10863-005-6631-3. [DOI] [PubMed] [Google Scholar]
- 59.Crouch PJ, et al. Copper-dependent inhibition of human cytochrome c oxidase by a dimeric conformer of amyloid-beta1-42. J Neurosci. 2005;25:672–9. doi: 10.1523/JNEUROSCI.4276-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Area-Gomez E, et al. Upregulated function of mitochondria-associated ER membranes in Alzheimer disease. EMBO J. 2012;31:4106–23. doi: 10.1038/emboj.2012.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Coskun P, et al. A mitochondrial etiology of Alzheimer and Parkinson disease. Biochim Biophys Acta. 2012;1820:553–64. doi: 10.1016/j.bbagen.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fukui H, Diaz F, Garcia S, Moraes CT. Cytochrome c oxidase deficiency in neurons decreases both oxidative stress and amyloid formation in a mouse model of Alzheimer’s disease. Proc Natl Acad Sci U S A. 2007;104:14163–8. doi: 10.1073/pnas.0705738104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fulda S, Galluzzi L, Kroemer G. Targeting mitochondria for cancer therapy. Nat Rev Drug Discov. 2010;9:447–64. doi: 10.1038/nrd3137. [DOI] [PubMed] [Google Scholar]
- 64.Green DR, Galluzzi L, Kroemer G. Mitochondria and the autophagy-inflammation-cell death axis in organismal aging. Science. 2011;333:1109–12. doi: 10.1126/science.1201940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fontana L, Partridge L, Longo VD. Extending healthy life span--from yeast to humans. Science. 2010;328:321–6. doi: 10.1126/science.1172539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Colman RJ, et al. Caloric restriction delays disease onset and mortality in rhesus monkeys. Science. 2009;325:201–4. doi: 10.1126/science.1173635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mattison JA, et al. Impact of caloric restriction on health and survival in rhesus monkeys from the NIA study. Nature. 2012;489:318–21. doi: 10.1038/nature11432. [DOI] [PMC free article] [PubMed] [Google Scholar]; References 66 and 67 show divergent results of the impact of caloric restriction on health and lifespan in non-human primates.
- 68.Imai S, Armstrong CM, Kaeberlein M, Guarente L. Transcriptional silencing and longevity protein Sir2 is an NAD-dependent histone deacetylase. Nature. 2000;403:795–800. doi: 10.1038/35001622. [DOI] [PubMed] [Google Scholar]
- 69.Matoba S, et al. p53 regulates mitochondrial respiration. Science. 2006;312:1650–3. doi: 10.1126/science.1126863. [DOI] [PubMed] [Google Scholar]
- 70.Yamamoto H, et al. NCoR1 Is a Conserved Physiological Modulator of Muscle Mass and Oxidative Function. Cell. 2011;147:827–839. doi: 10.1016/j.cell.2011.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Brunet A, et al. Stress-dependent regulation of FOXO transcription factors by the SIRT1 deacetylase. Science. 2004;303:2011–5. doi: 10.1126/science.1094637. [DOI] [PubMed] [Google Scholar]
- 72.Motta MC, et al. Mammalian SIRT1 represses forkhead transcription factors. Cell. 2004;116:551–63. doi: 10.1016/s0092-8674(04)00126-6. [DOI] [PubMed] [Google Scholar]
- 73.van der Horst A, et al. FOXO4 is acetylated upon peroxide stress and deacetylated by the longevity protein hSir2(SIRT1) J Biol Chem. 2004;279:28873–9. doi: 10.1074/jbc.M401138200. [DOI] [PubMed] [Google Scholar]
- 74.Rodgers JT, et al. Nutrient control of glucose homeostasis through a complex of PGC-1alpha and SIRT1. Nature. 2005;434:113–8. doi: 10.1038/nature03354. [DOI] [PubMed] [Google Scholar]
- 75.Howitz KT, et al. Small molecule activators of sirtuins extend Saccharomyces cerevisiae lifespan. Nature. 2003;425:191–6. doi: 10.1038/nature01960. [DOI] [PubMed] [Google Scholar]
- 76.Beher D, et al. Resveratrol is not a direct activator of SIRT1 enzyme activity. Chem Biol Drug Des. 2009;74:619–24. doi: 10.1111/j.1747-0285.2009.00901.x. [DOI] [PubMed] [Google Scholar]
- 77.Canto C, et al. AMPK regulates energy expenditure by modulating NAD+ metabolism and SIRT1 activity. Nature. 2009;458:1056–60. doi: 10.1038/nature07813. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study defines the importance of the AMPK/SIRT1/PGC1-α signaling axis in mitochondrial function.
- 78.Canto C, et al. Interdependence of AMPK and SIRT1 for Metabolic Adaptation to Fasting and Exercise in Skeletal Muscle. Cell Metab. 2010;11:213–219. doi: 10.1016/j.cmet.2010.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pacholec M, et al. SRT1720, SRT2183, SRT1460, and resveratrol are not direct activators of SIRT1. J Biol Chem. 2010;285:8340–51. doi: 10.1074/jbc.M109.088682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Um JH, et al. AMP-activated protein kinase-deficient mice are resistant to the metabolic effects of resveratrol. Diabetes. 2010;59:554–63. doi: 10.2337/db09-0482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Baur JA, et al. Resveratrol improves health and survival of mice on a high-calorie diet. Nature. 2006;444:337–42. doi: 10.1038/nature05354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lagouge M, et al. Resveratrol improves mitochondrial function and protects against metabolic disease by activating SIRT1 and PGC-1alpha. Cell. 2006;127:1109–22. doi: 10.1016/j.cell.2006.11.013. [DOI] [PubMed] [Google Scholar]; References 81 and 82 provide the first evidence of a beneficial impact of resveratrol on mitochondrial function and healthspan in mice.
- 83.Timmers S, et al. Calorie restriction-like effects of 30 days of resveratrol supplementation on energy metabolism and metabolic profile in obese humans. Cell Metab. 2011;14:612–22. doi: 10.1016/j.cmet.2011.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Brasnyo P, et al. Resveratrol improves insulin sensitivity, reduces oxidative stress and activates the Akt pathway in type 2 diabetic patients. Br J Nutr. 2011;106:383–9. doi: 10.1017/S0007114511000316. [DOI] [PubMed] [Google Scholar]
- 85.Poulsen MM, et al. High-Dose Resveratrol Supplementation in Obese Men: An Investigator-Initiated, Randomized, Placebo-Controlled Clinical Trial of Substrate Metabolism, Insulin Sensitivity, and Body Composition. Diabetes. 2012 doi: 10.2337/db12-0975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yoshino J, et al. Resveratrol supplementation does not improve metabolic function in nonobese women with normal glucose tolerance. Cell Metab. 2012;16:658–64. doi: 10.1016/j.cmet.2012.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bhatt JK, Thomas S, Nanjan MJ. Resveratrol supplementation improves glycemic control in type 2 diabetes mellitus. Nutr Res. 2012;32:537–41. doi: 10.1016/j.nutres.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 88.Patel KR, et al. Clinical trials of resveratrol. Ann N Y Acad Sci. 2011;1215:161–9. doi: 10.1111/j.1749-6632.2010.05853.x. [DOI] [PubMed] [Google Scholar]
- 89.Milne JC, et al. Small molecule activators of SIRT1 as therapeutics for the treatment of type 2 diabetes. Nature. 2007;450:712–6. doi: 10.1038/nature06261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Feige JN, et al. Specific SIRT1 activation mimics low energy levels and protects against diet-induced metabolic disorders by enhancing fat oxidation. Cell Metab. 2008;8:347–58. doi: 10.1016/j.cmet.2008.08.017. [DOI] [PubMed] [Google Scholar]
- 91.Dai H, et al. SIRT1 activation by small molecules: kinetic and biophysical evidence for direct interaction of enzyme and activator. J Biol Chem. 2010;285:32695–703. doi: 10.1074/jbc.M110.133892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Baur JA, Ungvari Z, Minor RK, Le Couteur DG, de Cabo R. Are sirtuins viable targets for improving healthspan and lifespan? Nat Rev Drug Discov. 2012;11:443–61. doi: 10.1038/nrd3738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hubbard BP, et al. Evidence for a common mechanism of SIRT1 regulation by allosteric activators. Science. 2013;339:1216–9. doi: 10.1126/science.1231097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Minor RK, et al. SRT1720 improves survival and healthspan of obese mice. Sci. Rep. 2011 doi: 10.1038/srep00070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Qi Y, et al. SRT2104, a Novel Small Molecule SIRT1 Activator Ameliorates Insulin Resistance and Promotes Glucose utilization Measured under a Hyperinsulinemic-Euglycemic Clamp by Enhancing Both Glycolysis and Carbohydrate Oxidation in Mice Fed a High Fat Diet (2011). 71st Scientific Sessions (San Diego, CA, USA) published in Diabetes. 60:A235–A352. [Google Scholar]
- 96.Suri V, et al. The Metabolomic Profile of SRT2104, a Selective SIRT1 Activator in High Fat Diet Fed Mice Reveals Significant Improvements in Metabolic Function in Liver, Heart and Skeletal Muscle (2011). 71st Scientific Sessions (San Diego, CA, USA) published in Diabetes. 60:A442–A521. [Google Scholar]
- 97.Hoffmann E, et al. Pharmacokinetics and tolerability of SRT2104, a first-in-class small molecule activator of SIRT1, after single and repeated oral administration in man. Br J Clin Pharmacol. 2013;75:186–96. doi: 10.1111/j.1365-2125.2012.04340.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bemis JE, et al. Discovery of oxazolo[4,5-b]pyridines and related heterocyclic analogs as novel SIRT1 activators. Bioorg Med Chem Lett. 2009;19:2350–3. doi: 10.1016/j.bmcl.2008.11.106. [DOI] [PubMed] [Google Scholar]
- 99.Mai A, et al. Study of 1,4-dihydropyridine structural scaffold: discovery of novel sirtuin activators and inhibitors. J Med Chem. 2009;52:5496–504. doi: 10.1021/jm9008289. [DOI] [PubMed] [Google Scholar]
- 100.Vu CB, et al. Discovery of imidazo[1,2-b]thiazole derivatives as novel SIRT1 activators. J Med Chem. 2009;52:1275–83. doi: 10.1021/jm8012954. [DOI] [PubMed] [Google Scholar]
- 101.Houtkooper RH, Canto C, Wanders RJ, Auwerx J. The Secret Life of NAD+: An Old Metabolite Controlling New Metabolic Signaling Pathways. Endocr Rev. 2010;31(2):194–223. doi: 10.1210/er.2009-0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Houtkooper RH, Auwerx J. Exploring the therapeutic space around NAD+ J Cell Biol. 2012;199:205–9. doi: 10.1083/jcb.201207019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Canto C, et al. The NAD(+) precursor nicotinamide riboside enhances oxidative metabolism and protects against high-fat diet-induced obesity. Cell Metab. 2012;15:838–47. doi: 10.1016/j.cmet.2012.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Yoshino J, Mills KF, Yoon MJ, Imai S. Nicotinamide mononucleotide, a key NAD(+) intermediate, treats the pathophysiology of diet- and age-induced diabetes in mice. Cell Metab. 2011;14:528–36. doi: 10.1016/j.cmet.2011.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Bai P, et al. PARP-1 inhibition increases mitochondrial metabolism through SIRT1 activation. Cell Metab. 2011;13:461–8. doi: 10.1016/j.cmet.2011.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Barbosa MT, et al. The enzyme CD38 (a NAD glycohydrolase, EC 3.2.2.5) is necessary for the development of diet-induced obesity. Faseb J. 2007;21:3629–39. doi: 10.1096/fj.07-8290com. [DOI] [PubMed] [Google Scholar]; References 103–106 (four independent studies) define the importance of NAD+ levels and SIRTs activation in mitochondrial homeostasis.
- 107.Canto C, Auwerx J. AMP-activated protein kinase and its downstream transcriptional pathways. Cell Mol Life Sci. 2010;67:3407–23. doi: 10.1007/s00018-010-0454-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Narkar VA, et al. AMPK and PPARdelta agonists are exercise mimetics. Cell. 2008;134:405–15. doi: 10.1016/j.cell.2008.06.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Viscomi C, et al. In vivo correction of COX deficiency by activation of the AMPK/PGC-1alpha axis. Cell Metab. 2011;14:80–90. doi: 10.1016/j.cmet.2011.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]; This paper shows that the AMPK agonist AICAR is beneficial for this form of inherited mitochondrial disease in mice.
- 110.Zoncu R, Efeyan A, Sabatini DM. mTOR: from growth signal integration to cancer, diabetes and ageing. Nat Rev Mol Cell Biol. 2011;12:21–35. doi: 10.1038/nrm3025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Harrison DE, et al. Rapamycin fed late in life extends lifespan in genetically heterogeneous mice. Nature. 2009;460:392–5. doi: 10.1038/nature08221. [DOI] [PMC free article] [PubMed] [Google Scholar]; This key report demonstrates the beneficial impact of the mTOR inhibitor rapamycin on mouse lifespan.
- 112.Bjedov I, et al. Mechanisms of life span extension by rapamycin in the fruit fly Drosophila melanogaster. Cell Metab. 2010;11:35–46. doi: 10.1016/j.cmet.2009.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Robida-Stubbs S, et al. TOR signaling and rapamycin influence longevity by regulating SKN-1/Nrf and DAF-16/FoxO. Cell Metab. 2012;15:713–24. doi: 10.1016/j.cmet.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Polak P, et al. Adipose-specific knockout of raptor results in lean mice with enhanced mitochondrial respiration. Cell Metab. 2008;8:399–410. doi: 10.1016/j.cmet.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 115.Bentzinger CF, et al. Skeletal muscle-specific ablation of raptor, but not of rictor, causes metabolic changes and results in muscle dystrophy. Cell Metab. 2008;8:411–24. doi: 10.1016/j.cmet.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 116.Schoonjans K, Staels B, Auwerx J. Role of the peroxisome proliferator-activated receptor (PPAR) in mediating the effects of fibrates and fatty acids on gene expression. J Lipid Res. 1996;37:907–25. [PubMed] [Google Scholar]
- 117.Evans RM, Barish GD, Wang YX. PPARs and the complex journey to obesity. Nat Med. 2004;10:355–61. doi: 10.1038/nm1025. [DOI] [PubMed] [Google Scholar]
- 118.Michalik L, et al. International Union of Pharmacology. LXI. Peroxisome proliferator-activated receptors. Pharmacol Rev. 2006;58:726–41. doi: 10.1124/pr.58.4.5. [DOI] [PubMed] [Google Scholar]
- 119.Kersten S, et al. Peroxisome proliferator-activated receptor alpha mediates the adaptive response to fasting. J Clin Invest. 1999;103:1489–98. doi: 10.1172/JCI6223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Leibowitz MD, et al. Activation of PPARdelta alters lipid metabolism in db/db mice. FEBS Lett. 2000;473:333–6. doi: 10.1016/s0014-5793(00)01554-4. [DOI] [PubMed] [Google Scholar]
- 121.Tanaka T, et al. Activation of peroxisome proliferator-activated receptor delta induces fatty acid beta-oxidation in skeletal muscle and attenuates metabolic syndrome. Proc Natl Acad Sci U S A. 2003;100:15924–9. doi: 10.1073/pnas.0306981100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Riserus U, et al. Activation of peroxisome proliferator-activated receptor (PPAR)delta promotes reversal of multiple metabolic abnormalities, reduces oxidative stress, and increases fatty acid oxidation in moderately obese men. Diabetes. 2008;57:332–9. doi: 10.2337/db07-1318. [DOI] [PubMed] [Google Scholar]
- 123.Djouadi F, et al. Bezafibrate increases very-long-chain acyl-CoA dehydrogenase protein and mRNA expression in deficient fibroblasts and is a potential therapy for fatty acid oxidation disorders. Hum Mol Genet. 2005;14:2695–703. doi: 10.1093/hmg/ddi303. [DOI] [PubMed] [Google Scholar]
- 124.Gobin-Limballe S, et al. Genetic basis for correction of very-long-chain acyl coenzyme A dehydrogenase deficiency by bezafibrate in patient fibroblasts: toward a genotype-based therapy. Am J Hum Genet. 2007;81:1133–43. doi: 10.1086/522375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bonnefont JP, et al. Long-term follow-up of bezafibrate treatment in patients with the myopathic form of carnitine palmitoyltransferase 2 deficiency. Clin Pharmacol Ther. 2010;88:101–8. doi: 10.1038/clpt.2010.55. [DOI] [PubMed] [Google Scholar]; This study shows that PPARδ activation with bezafibrate has beneficial therapeutic effects in patients with fatty acid oxidation deficiciency.
- 126.Heikkinen S, Auwerx J, Argmann CA. PPARgamma in human and mouse physiology. Biochim Biophys Acta. 2007;1771:999–1013. doi: 10.1016/j.bbalip.2007.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kung J, Henry RR. Thiazolidinedione safety. Expert Opin Drug Saf. 2012;11:565–79. doi: 10.1517/14740338.2012.691963. [DOI] [PubMed] [Google Scholar]
- 128.Rocchi S, et al. A unique PPARγ ligand with potent insulin-sensitizing yet weak adipogenic activity. Mol Cell. 2001;8:737–747. doi: 10.1016/s1097-2765(01)00353-7. [DOI] [PubMed] [Google Scholar]
- 129.Choi JH, et al. Antidiabetic actions of a non-agonist PPARgamma ligand blocking Cdk5-mediated phosphorylation. Nature. 2011;477:477–81. doi: 10.1038/nature10383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Knouff C, Auwerx J. Peroxisome proliferator-activated receptor-gamma calls for activation in moderation: lessons from genetics and pharmacology. Endocr Rev. 2004;25:899–918. doi: 10.1210/er.2003-0036. [DOI] [PubMed] [Google Scholar]
- 131.Chae S, et al. A systems approach for decoding mitochondrial retrograde signaling pathways. Sci Signal. 2013;6:rs4. doi: 10.1126/scisignal.2003266. [DOI] [PubMed] [Google Scholar]
- 132.Giguere V. Transcriptional control of energy homeostasis by the estrogen-related receptors. Endocr Rev. 2008;29:677–96. doi: 10.1210/er.2008-0017. [DOI] [PubMed] [Google Scholar]
- 133.Dufour CR, et al. Genome-wide orchestration of cardiac functions by the orphan nuclear receptors ERRalpha and gamma. Cell Metab. 2007;5:345–56. doi: 10.1016/j.cmet.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 134.Schreiber SN, et al. The estrogen-related receptor alpha (ERRalpha) functions in PPARgamma coactivator 1alpha (PGC-1alpha)-induced mitochondrial biogenesis. Proc Natl Acad Sci U S A. 2004;101:6472–7. doi: 10.1073/pnas.0308686101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Alaynick WA, et al. ERRgamma directs and maintains the transition to oxidative metabolism in the postnatal heart. Cell Metab. 2007;6:13–24. doi: 10.1016/j.cmet.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 136.Coward P, Lee D, Hull MV, Lehmann JM. 4-Hydroxytamoxifen binds to and deactivates the estrogen-related receptor gamma. Proc Natl Acad Sci U S A. 2001;98:8880–4. doi: 10.1073/pnas.151244398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Zuercher WJ, et al. Identification and structure-activity relationship of phenolic acyl hydrazones as selective agonists for the estrogen-related orphan nuclear receptors ERRbeta and ERRgamma. J Med Chem. 2005;48:3107–9. doi: 10.1021/jm050161j. [DOI] [PubMed] [Google Scholar]
- 138.Kim Y, Koh M, Kim DK, Choi HS, Park SB. Efficient discovery of selective small molecule agonists of estrogen-related receptor gamma using combinatorial approach. J Comb Chem. 2009;11:928–37. doi: 10.1021/cc900081j. [DOI] [PubMed] [Google Scholar]
- 139.Willy PJ, et al. Regulation of PPARgamma coactivator 1alpha (PGC-1alpha) signaling by an estrogen-related receptor alpha (ERRalpha) ligand. Proc Natl Acad Sci U S A. 2004;101:8912–7. doi: 10.1073/pnas.0401420101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Chisamore MJ, Cunningham ME, Flores O, Wilkinson HA, Chen JD. Characterization of a novel small molecule subtype specific estrogen-related receptor alpha antagonist in MCF-7 breast cancer cells. PLoS One. 2009;4:e5624. doi: 10.1371/journal.pone.0005624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Patch RJ, et al. Identification of diaryl ether-based ligands for estrogen-related receptor alpha as potential antidiabetic agents. J Med Chem. 2011;54:788–808. doi: 10.1021/jm101063h. [DOI] [PubMed] [Google Scholar]
- 142.Kallen J, et al. Crystal structure of human estrogen-related receptor alpha in complex with a synthetic inverse agonist reveals its novel molecular mechanism. J Biol Chem. 2007;282:23231–9. doi: 10.1074/jbc.M703337200. [DOI] [PubMed] [Google Scholar]
- 143.Hyatt SM, et al. On the intractability of estrogen-related receptor alpha as a target for activation by small molecules. J Med Chem. 2007;50:6722–4. doi: 10.1021/jm7012387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Kim DK, et al. Orphan nuclear receptor estrogen-related receptor gamma (ERRgamma) is key regulator of hepatic gluconeogenesis. J Biol Chem. 2012;287:21628–39. doi: 10.1074/jbc.M111.315168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Kelly DP, Scarpulla RC. Transcriptional regulatory circuits controlling mitochondrial biogenesis and function. Genes Dev. 2004;18:357–68. doi: 10.1101/gad.1177604. [DOI] [PubMed] [Google Scholar]
- 146.Collard J, Khorkova Sherman O. Treatment of nuclear respiratory factor 1 (NRF1) related diseases by inhibition of natural antisense transcript to NRF1. CuRNA, Inc.; 2010. http://patents.com/us-20120264812.html. [Google Scholar]
- 147.Iyer S, et al. Recombinant mitochondrial transcription factor A with N-terminal mitochondrial transduction domain increases respiration and mitochondrial gene expression. Mitochondrion. 2009;9:196–203. doi: 10.1016/j.mito.2009.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Thomas RR, et al. RhTFAM treatment stimulates mitochondrial oxidative metabolism and improves memory in aged mice. Aging (Albany NY) 2012;4:620–35. doi: 10.18632/aging.100488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Iyer S, et al. Mitochondrial gene therapy improves respiration, biogenesis, and transcription in G11778A Leber’s hereditary optic neuropathy and T8993G Leigh’s syndrome cells. Hum Gene Ther. 2012;23:647–57. doi: 10.1089/hum.2011.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Ylikallio E, Tyynismaa H, Tsutsui H, Ide T, Suomalainen A. High mitochondrial DNA copy number has detrimental effects in mice. Hum Mol Genet. 2010;19:2695–705. doi: 10.1093/hmg/ddq163. [DOI] [PubMed] [Google Scholar]
- 151.Picard F, et al. SRC-1 and TIF2 control energy balance between white and brown adipose tissues. Cell. 2002;111:931–941. doi: 10.1016/s0092-8674(02)01169-8. [DOI] [PubMed] [Google Scholar]
- 152.Coste A, et al. The genetic ablation of SRC-3 protects against obesity and improves insulin sensitivity by reducing the acetylation of PGC-1{alpha} Proc Natl Acad Sci U S A. 2008;105:17187–92. doi: 10.1073/pnas.0808207105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Coste A, et al. Absence of the steroid receptor coactivator-3 induces B-cell lymphoma. EMBO J. 2006;25:2453–64. doi: 10.1038/sj.emboj.7601106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Choi JH, et al. Anti-diabetic drugs inhibit obesity-linked phosphorylation of PPARgamma by Cdk5. Nature. 2010;466:451–6. doi: 10.1038/nature09291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Ye L, et al. TRPV4 Is a Regulator of Adipose Oxidative Metabolism, Inflammation, and Energy Homeostasis. Cell. 2012;151:96–110. doi: 10.1016/j.cell.2012.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Bostrom P, et al. A PGC1-alpha-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature. 2012;481:463–8. doi: 10.1038/nature10777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Watanabe M, et al. Bile acids induce energy expenditure by promoting intracellular thyroid hormone activation. Nature. 2006;439:484–9. doi: 10.1038/nature04330. [DOI] [PubMed] [Google Scholar]
- 158.Sengupta S, Peterson TR, Laplante M, Oh S, Sabatini DM. mTORC1 controls fasting-induced ketogenesis and its modulation by ageing. Nature. 2010;468:1100–4. doi: 10.1038/nature09584. [DOI] [PubMed] [Google Scholar]
- 159.Li P, et al. Adipocyte NCoR knockout decreases PPARgamma phosphorylation and enhances PPARgamma activity and insulin sensitivity. Cell. 2011;147:815–26. doi: 10.1016/j.cell.2011.09.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Iezzi S, et al. Deacetylase inhibitors increase muscle cell size by promoting myoblast recruitment and fusion through induction of follistatin. Dev Cell. 2004;6:673–84. doi: 10.1016/s1534-5807(04)00107-8. [DOI] [PubMed] [Google Scholar]
- 161.Fajas L, et al. The retinoblastoma-histone deacetylase 3 complex inhibits PPARgamma and adipocyte differentiation. Dev Cell. 2002;3:903–10. doi: 10.1016/s1534-5807(02)00360-x. [DOI] [PubMed] [Google Scholar]
- 162.Sun Z, et al. Hepatic Hdac3 promotes gluconeogenesis by repressing lipid synthesis and sequestration. Nat Med. 2012;18:934–42. doi: 10.1038/nm.2744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Debevec D, et al. Receptor interacting protein 140 regulates expression of uncoupling protein 1 in adipocytes through specific peroxisome proliferator activated receptor isoforms and estrogen-related receptor alpha. Mol Endocrinol. 2007;21:1581–92. doi: 10.1210/me.2007-0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Seth A, et al. The transcriptional corepressor RIP140 regulates oxidative metabolism in skeletal muscle. Cell Metab. 2007;6:236–45. doi: 10.1016/j.cmet.2007.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Leonardsson G, et al. Nuclear receptor corepressor RIP140 regulates fat accumulation. Proc Natl Acad Sci U S A. 2004;101:8437–42. doi: 10.1073/pnas.0401013101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Powelka AM, et al. Suppression of oxidative metabolism and mitochondrial biogenesis by the transcriptional corepressor RIP140 in mouse adipocytes. J Clin Invest. 2006;116:125–36. doi: 10.1172/JCI26040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Blanchet E, et al. E2F transcription factor-1 regulates oxidative metabolism. Nat Cell Biol. 2011;13:1146–52. doi: 10.1038/ncb2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Scime A, et al. Rb and p107 regulate preadipocyte differentiation into white versus brown fat through repression of PGC-1alpha. Cell Metab. 2005;2:283–95. doi: 10.1016/j.cmet.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 169.Dali-Youcef N, et al. Adipose tissue-specific inactivation of the retinoblastoma protein protects against diabesity because of increased energy expenditure. Proc Natl Acad Sci U S A. 2007;104:10703–8. doi: 10.1073/pnas.0611568104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Calo E, et al. Rb regulates fate choice and lineage commitment in vivo. Nature. 2010;466:1110–4. doi: 10.1038/nature09264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.White R, et al. The nuclear receptor co-repressor nrip1 (RIP140) is essential for female fertility. Nat Med. 2000;6:1368–74. doi: 10.1038/82183. [DOI] [PubMed] [Google Scholar]
- 172.Brand MD. The sites and topology of mitochondrial superoxide production. Exp Gerontol. 2010;45:466–72. doi: 10.1016/j.exger.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Sena LA, Chandel NS. Physiological roles of mitochondrial reactive oxygen species. Mol Cell. 2012;48:158–67. doi: 10.1016/j.molcel.2012.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Brand MD. Uncoupling to survive? The role of mitochondrial inefficiency in ageing. Exp Gerontol. 2000;35:811–20. doi: 10.1016/s0531-5565(00)00135-2. [DOI] [PubMed] [Google Scholar]
- 175.Chen H, et al. Mitofusins Mfn1 and Mfn2 coordinately regulate mitochondrial fusion and are essential for embryonic development. J Cell Biol. 2003;160:189–200. doi: 10.1083/jcb.200211046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Chan DC. Mitochondria: dynamic organelles in disease, aging, and development. Cell. 2006;125:1241–52. doi: 10.1016/j.cell.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 177.Alexander C, et al. OPA1, encoding a dynamin-related GTPase, is mutated in autosomal dominant optic atrophy linked to chromosome 3q28. Nat Genet. 2000;26:211–5. doi: 10.1038/79944. [DOI] [PubMed] [Google Scholar]
- 178.Zuchner S, et al. Mutations in the mitochondrial GTPase mitofusin 2 cause Charcot-Marie-Tooth neuropathy type 2A. Nat Genet. 2004;36:449–51. doi: 10.1038/ng1341. [DOI] [PubMed] [Google Scholar]
- 179.Waterham HR, et al. A lethal defect of mitochondrial and peroxisomal fission. N Engl J Med. 2007;356:1736–41. doi: 10.1056/NEJMoa064436. [DOI] [PubMed] [Google Scholar]
- 180.Ishihara N, et al. Mitochondrial fission factor Drp1 is essential for embryonic development and synapse formation in mice. Nat Cell Biol. 2009;11:958–66. doi: 10.1038/ncb1907. [DOI] [PubMed] [Google Scholar]
- 181.Chen H, Chomyn A, Chan DC. Disruption of fusion results in mitochondrial heterogeneity and dysfunction. J Biol Chem. 2005;280:26185–92. doi: 10.1074/jbc.M503062200. [DOI] [PubMed] [Google Scholar]
- 182.Parone PA, et al. Preventing mitochondrial fission impairs mitochondrial function and leads to loss of mitochondrial DNA. PLoS One. 2008;3:e3257. doi: 10.1371/journal.pone.0003257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Soriano FX, et al. Evidence for a mitochondrial regulatory pathway defined by peroxisome proliferator-activated receptor-gamma coactivator-1 alpha, estrogen-related receptor-alpha, and mitofusin 2. Diabetes. 2006;55:1783–91. doi: 10.2337/db05-0509. [DOI] [PubMed] [Google Scholar]
- 184.Cartoni R, et al. Mitofusins 1/2 and ERRalpha expression are increased in human skeletal muscle after physical exercise. J Physiol. 2005;567:349–58. doi: 10.1113/jphysiol.2005.092031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Wang D, et al. A small molecule promotes mitochondrial fusion in mammalian cells. Angew Chem Int Ed Engl. 2012;51:9302–5. doi: 10.1002/anie.201204589. [DOI] [PubMed] [Google Scholar]; This paper reports the identification of a small molecule that stimulates mitochondrial fusion in mammalian cells.
- 186.Cassidy-Stone A, et al. Chemical inhibition of the mitochondrial division dynamin reveals its role in Bax/Bak-dependent mitochondrial outer membrane permeabilization. Dev Cell. 2008;14:193–204. doi: 10.1016/j.devcel.2007.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study identifies a small molecule that inhibits mitochondrial fission in yeast.
- 187.Lackner LL, Nunnari J. Small molecule inhibitors of mitochondrial division: tools that translate basic biological research into medicine. Chem Biol. 2010;17:578–83. doi: 10.1016/j.chembiol.2010.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Nakatogawa H, Suzuki K, Kamada Y, Ohsumi Y. Dynamics and diversity in autophagy mechanisms: lessons from yeast. Nat Rev Mol Cell Biol. 2009;10:458–67. doi: 10.1038/nrm2708. [DOI] [PubMed] [Google Scholar]
- 189.Yang Z, Klionsky DJ. Eaten alive: a history of macroautophagy. Nat Cell Biol. 2010;12:814–22. doi: 10.1038/ncb0910-814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Sandoval H, et al. Essential role for Nix in autophagic maturation of erythroid cells. Nature. 2008;454:232–5. doi: 10.1038/nature07006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Narendra DP, et al. PINK1 is selectively stabilized on impaired mitochondria to activate Parkin. PLoS Biol. 2010;8:e1000298. doi: 10.1371/journal.pbio.1000298. [DOI] [PMC free article] [PubMed] [Google Scholar]; This key paper demonstrates the recruitment of PINK1 as a stimulator of mitophagy.
- 192.Geisler S, et al. PINK1/Parkin-mediated mitophagy is dependent on VDAC1 and p62/SQSTM1. Nat Cell Biol. 2010;12:119–31. doi: 10.1038/ncb2012. [DOI] [PubMed] [Google Scholar]
- 193.Lee JY, Nagano Y, Taylor JP, Lim KL, Yao TP. Disease-causing mutations in parkin impair mitochondrial ubiquitination, aggregation, and HDAC6-dependent mitophagy. J Cell Biol. 2010;189:671–9. doi: 10.1083/jcb.201001039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Matsuda N, et al. PINK1 stabilized by mitochondrial depolarization recruits Parkin to damaged mitochondria and activates latent Parkin for mitophagy. J Cell Biol. 2010;189:211–21. doi: 10.1083/jcb.200910140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Sterky FH, Lee S, Wibom R, Olson L, Larsson NG. Impaired mitochondrial transport and Parkin-independent degeneration of respiratory chain-deficient dopamine neurons in vivo. Proc Natl Acad Sci U S A. 2011;108:12937–42. doi: 10.1073/pnas.1103295108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Gegg ME, et al. Mitofusin 1 and mitofusin 2 are ubiquitinated in a PINK1/parkin-dependent manner upon induction of mitophagy. Hum Mol Genet. 2010;19:4861–70. doi: 10.1093/hmg/ddq419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Tanaka A, et al. Proteasome and p97 mediate mitophagy and degradation of mitofusins induced by Parkin. J Cell Biol. 2010;191:1367–80. doi: 10.1083/jcb.201007013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Hartl FU, Bracher A, Hayer-Hartl M. Molecular chaperones in protein folding and proteostasis. Nature. 2011;475:324–32. doi: 10.1038/nature10317. [DOI] [PubMed] [Google Scholar]
- 199.Nargund AM, Pellegrino MW, Fiorese CJ, Baker BM, Haynes CM. Mitochondrial import efficiency of ATFS-1 regulates mitochondrial UPR activation. Science. 2012;337:587–90. doi: 10.1126/science.1223560. [DOI] [PMC free article] [PubMed] [Google Scholar]; This report describes another layer of transcriptional control of the mitochondrial UPR by regulating the subcellular distribution of ATFS-1.
- 200.Benedetti C, Haynes CM, Yang Y, Harding HP, Ron D. Ubiquitin-like protein 5 positively regulates chaperone gene expression in the mitochondrial unfolded protein response. Genetics. 2006;174:229–39. doi: 10.1534/genetics.106.061580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Durieux J, Wolff S, Dillin A. The cell-non-autonomous nature of electron transport chain-mediated longevity. Cell. 2011;144:79–91. doi: 10.1016/j.cell.2010.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrates that lifespan extension in C. elegans following mitochondrial dysfunction in the neurons requires mitochondrial UPR in distal tissues. It also defines the concept of mitokine.
- 202.Tyynismaa H, et al. Mitochondrial myopathy induces a starvation-like response. Hum Mol Genet. 2010;19:3948–58. doi: 10.1093/hmg/ddq310. [DOI] [PubMed] [Google Scholar]
- 203.Suomalainen A, et al. FGF-21 as a biomarker for muscle-manifesting mitochondrial respiratory chain deficiencies: a diagnostic study. Lancet Neurol. 2011;10:806–18. doi: 10.1016/S1474-4422(11)70155-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Kim KH, et al. Autophagy deficiency leads to protection from obesity and insulin resistance by inducing Fgf21 as a mitokine. Nat Med. 2012 doi: 10.1038/nm.3014. [DOI] [PubMed] [Google Scholar]; References 203 and 204 suggest that FGF-21 can function as a mitokine.
- 205.Lee C, Yen K, Cohen P. Humanin: a harbinger of mitochondrial-derived peptides? Trends Endocrinol Metab. 2013 doi: 10.1016/j.tem.2013.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Martinus RD, et al. Selective induction of mitochondrial chaperones in response to loss of the mitochondrial genome. Eur J Biochem. 1996;240:98–103. doi: 10.1111/j.1432-1033.1996.0098h.x. [DOI] [PubMed] [Google Scholar]
- 207.Houtkooper RH, et al. Mitonuclear protein imbalance as a conserved longevity mechanism. Nature. 2013;497:451–7. doi: 10.1038/nature12188. [DOI] [PMC free article] [PubMed] [Google Scholar]; This recently published paper shows that the imbalance between mitochondrial and nuclear proteins triggers the mitochondrial UPR, which is an overarching mechanism that enhances lifespan
- 208.Fontaine B, et al. A new locus for autosomal dominant pure spastic paraplegia, on chromosome 2q24-q34. Am J Hum Genet. 2000;66:702–7. doi: 10.1086/302776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Casari G, et al. Spastic paraplegia and OXPHOS impairment caused by mutations in paraplegin, a nuclear-encoded mitochondrial metalloprotease. Cell. 1998;93:973–83. doi: 10.1016/s0092-8674(00)81203-9. [DOI] [PubMed] [Google Scholar]
- 210.Nolden M, et al. The m-AAA protease defective in hereditary spastic paraplegia controls ribosome assembly in mitochondria. Cell. 2005;123:277–89. doi: 10.1016/j.cell.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 211.Ventura N, et al. p53/CEP-1 increases or decreases lifespan, depending on level of mitochondrial bioenergetic stress. Aging Cell. 2009;8:380–93. doi: 10.1111/j.1474-9726.2009.00482.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Guillon B, et al. Frataxin deficiency causes upregulation of mitochondrial Lon and ClpP proteases and severe loss of mitochondrial Fe-S proteins. FEBS J. 2009;276:1036–47. doi: 10.1111/j.1742-4658.2008.06847.x. [DOI] [PubMed] [Google Scholar]
- 213.Rotig A, et al. Aconitase and mitochondrial iron-sulphur protein deficiency in Friedreich ataxia. Nat Genet. 1997;17:215–7. doi: 10.1038/ng1097-215. [DOI] [PubMed] [Google Scholar]
- 214.Bieganowski P, Brenner C. Discoveries of nicotinamide riboside as a nutrient and conserved NRK genes establish a Preiss-Handler independent route to NAD+ in fungi and humans. Cell. 2004;117:495–502. doi: 10.1016/s0092-8674(04)00416-7. [DOI] [PubMed] [Google Scholar]
- 215.Sato H, et al. Anti-hyperglycemic activity of a TGR5 agonist isolated from Olea europaea. Biochem Biophys Res Commun. 2007;362:793–8. doi: 10.1016/j.bbrc.2007.06.130. [DOI] [PubMed] [Google Scholar]
- 216.Sato H, et al. Novel potent and selective bile acid derivatives as TGR5 agonists: biological screening, structure-activity relationships, and molecular modeling studies. J Med Chem. 2008;51:1831–41. doi: 10.1021/jm7015864. [DOI] [PubMed] [Google Scholar]
- 217.Evans KA, et al. Discovery of 3-aryl-4-isoxazolecarboxamides as TGR5 receptor agonists. J Med Chem. 2009;52:7962–5. doi: 10.1021/jm901434t. [DOI] [PubMed] [Google Scholar]
- 218.Pellicciari R, et al. Discovery of 6alpha-ethyl-23(S)-methylcholic acid (S-EMCA, INT-777) as a potent and selective agonist for the TGR5 receptor, a novel target for diabesity. J Med Chem. 2009;52:7958–61. doi: 10.1021/jm901390p. [DOI] [PubMed] [Google Scholar]
- 219.Genet C, et al. Structure-activity relationship study of betulinic acid, a novel and selective TGR5 agonist, and its synthetic derivatives: potential impact in diabetes. J Med Chem. 2010;53:178–90. doi: 10.1021/jm900872z. [DOI] [PubMed] [Google Scholar]
- 220.Herbert MR, et al. Synthesis and SAR of 2-aryl-3-aminomethylquinolines as agonists of the bile acid receptor TGR5. Bioorg Med Chem Lett. 2010;20:5718–21. doi: 10.1016/j.bmcl.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 221.Londregan AT, et al. Discovery of 5-phenoxy-1,3-dimethyl-1H-pyrazole-4-carboxamides as potent agonists of TGR5 via sequential combinatorial libraries. Bioorg Med Chem Lett. 2013 doi: 10.1016/j.bmcl.2012.12.076. [DOI] [PubMed] [Google Scholar]
- 222.Moreno D, Knecht E, Viollet B, Sanz P. A769662, a novel activator of AMP-activated protein kinase, inhibits non-proteolytic components of the 26S proteasome by an AMPK-independent mechanism. FEBS Lett. 2008;582:2650–4. doi: 10.1016/j.febslet.2008.06.044. [DOI] [PubMed] [Google Scholar]
- 223.Hawley SA, et al. The ancient drug salicylate directly activates AMP-activated protein kinase. Science. 2012;336:918–22. doi: 10.1126/science.1215327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Cairns RA, Harris IS, Mak TW. Regulation of cancer cell metabolism. Nat Rev Cancer. 2011;11:85–95. doi: 10.1038/nrc2981. [DOI] [PubMed] [Google Scholar]
- 225.Kitami T, et al. A chemical screen probing the relationship between mitochondrial content and cell size. PLoS One. 2012;7:e33755. doi: 10.1371/journal.pone.0033755. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study reports the set up of an image-based phenotypic screen for the identification of compounds that increase mitochondrial content per cell using a primary cell line.
- 226.Beeson CC, Beeson GC, Schnellmann RG. A high-throughput respirometric assay for mitochondrial biogenesis and toxicity. Anal Biochem. 2010;404:75–81. doi: 10.1016/j.ab.2010.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Kikkawa R, Yamamoto T, Fukushima T, Yamada H, Horii I. Investigation of a hepatotoxicity screening system in primary cell cultures --“what biomarkers would need to be addressed to estimate toxicity in conventional and new approaches?”. J Toxicol Sci. 2005;30:61–72. doi: 10.2131/jts.30.61. [DOI] [PubMed] [Google Scholar]
- 228.Li AP. Screening for human ADME/Tox drug properties in drug discovery. Drug Discov Today. 2001;6:357–366. doi: 10.1016/s1359-6446(01)01712-3. [DOI] [PubMed] [Google Scholar]
- 229.Couplan E, et al. A yeast-based assay identifies drugs active against human mitochondrial disorders. Proc Natl Acad Sci U S A. 2011;108:11989–94. doi: 10.1073/pnas.1101478108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Burns AR, et al. High-throughput screening of small molecules for bioactivity and target identification in Caenorhabditis elegans. Nat Protoc. 2006;1:1906–14. doi: 10.1038/nprot.2006.283. [DOI] [PubMed] [Google Scholar]; References 229 and 230 are examples of phenotypic screens for mitochondrial function performed in C. elegans and yeast.
- 231.Segalat L. Invertebrate animal models of diseases as screening tools in drug discovery. ACS Chem Biol. 2007;2:231–6. doi: 10.1021/cb700009m. [DOI] [PubMed] [Google Scholar]
- 232.Gohil VM, et al. Nutrient-sensitized screening for drugs that shift energy metabolism from mitochondrial respiration to glycolysis. Nat Biotechnol. 2010;28:249–55. doi: 10.1038/nbt.1606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Wagner BK, et al. Large-scale chemical dissection of mitochondrial function. Nat Biotechnol. 2008;26:343–51. doi: 10.1038/nbt1387. [DOI] [PMC free article] [PubMed] [Google Scholar]; References 232 and 233 describe two examplary phenotypic screens for mitochondrial function in mammalian cells.
- 234.Tsang WY, Lemire BD. Mitochondrial genome content is regulated during nematode development. Biochem Biophys Res Commun. 2002;291:8–16. doi: 10.1006/bbrc.2002.6394. [DOI] [PubMed] [Google Scholar]
- 235.Detmer SA, Chan DC. Functions and dysfunctions of mitochondrial dynamics. Nat Rev Mol Cell Biol. 2007;8:870–9. doi: 10.1038/nrm2275. [DOI] [PubMed] [Google Scholar]
- 236.Wellcome Trust Case Control Consortium Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature. 2007;447:661–78. doi: 10.1038/nature05911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Frayling TM. Genome-wide association studies provide new insights into type 2 diabetes aetiology. Nat Rev Genet. 2007;8:657–62. doi: 10.1038/nrg2178. [DOI] [PubMed] [Google Scholar]
- 238.Zeggini E, et al. Meta-analysis of genome-wide association data and large-scale replication identifies additional susceptibility loci for type 2 diabetes. Nat Genet. 2008;40:638–45. doi: 10.1038/ng.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Mair W, Dillin A. Aging and survival: the genetics of life span extension by dietary restriction. Annu Rev Biochem. 2008;77:727–54. doi: 10.1146/annurev.biochem.77.061206.171059. [DOI] [PubMed] [Google Scholar]
- 240.Handschin C, Spiegelman BM. Peroxisome proliferator-activated receptor gamma coactivator 1 coactivators, energy homeostasis, and metabolism. Endocr Rev. 2006;27:728–35. doi: 10.1210/er.2006-0037. [DOI] [PubMed] [Google Scholar]
- 241.Fernandez-Marcos PJ, Auwerx J. Regulation of PGC-1alpha, a nodal regulator of mitochondrial biogenesis. Am J Clin Nutr. 2011;93:884S–90. doi: 10.3945/ajcn.110.001917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Canto C, Auwerx J. PGC-1alpha, SIRT1 and AMPK, an energy sensing network that controls energy expenditure. Curr Opin Lipidol. 2009;20:98–105. doi: 10.1097/MOL.0b013e328328d0a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Jeninga EH, Schoonjans K, Auwerx J. Reversible acetylation of PGC-1: connecting energy sensors and effectors to guarantee metabolic flexibility. Oncogene. 2010;29:4617–4624. doi: 10.1038/onc.2010.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Feige JN, Gelman L, Michalik L, Desvergne B, Wahli W. From molecular action to physiological outputs: peroxisome proliferator-activated receptors are nuclear receptors at the crossroads of key cellular functions. Prog Lipid Res. 2006;45:120–59. doi: 10.1016/j.plipres.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 245.Feige JN, Auwerx J. Transcriptional coregulators in the control of energy homeostasis. Trends Cell Biol. 2007;17:292–301. doi: 10.1016/j.tcb.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 246.Scarpulla RC, Vega RB, Kelly DP. Transcriptional integration of mitochondrial biogenesis. Trends Endocrinol Metab. 2012;23:459–66. doi: 10.1016/j.tem.2012.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Kalyanaraman B, et al. Measuring reactive oxygen and nitrogen species with fluorescent probes: challenges and limitations. Free Radic Biol Med. 2012;52:1–6. doi: 10.1016/j.freeradbiomed.2011.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Meyer AJ, Dick TP. Fluorescent protein-based redox probes. Antioxid Redox Signal. 2010;13:621–50. doi: 10.1089/ars.2009.2948. [DOI] [PubMed] [Google Scholar]
- 249.Greer EL, et al. An AMPK-FOXO pathway mediates longevity induced by a novel method of dietary restriction in C. elegans. Curr Biol. 2007;17:1646–56. doi: 10.1016/j.cub.2007.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]