Key Points
-
During blood-stage infections, Plasmodium parasites infect erythrocytes and can cause a variety of acute and chronic complications, some of which can be fatal. Although malaria complications are often attributed to sepsis-like systemic inflammation, the parasites in the circulation reach and interact with host tissues locally and specifically.
-
The brain, eye (retina), gastrointestinal tract, bones, lungs, kidneys and placenta are the organs that are specifically affected both during and even long after malaria infection. The unique anatomical structure of the vessels, parenchyma and lymphatics in each organ shapes the interaction with Plasmodium parasites and their products.
-
In the brain, unique areas such as the olfactory bulb, retina and perivascular spaces share similar anatomical and immunological features; Plasmodium parasites and their associated inflammation cause blood–brain barrier disruption in these areas.
-
The gastrointestinal tract microenvironment is a target of Plasmodium parasites and related events. Malaria infection causes the disruption of blood vessels and epithelial barriers in the gut.
-
Plasmodium parasites can reside in the bone marrow. At this site, the parasites and their products, such as haemozoin, interact with bone marrow niches and with cells resident in the bone tissue, including osteoblasts and osteoclasts, causing long-term effects in the host, such as bone loss.
-
The interactions that occur between Plasmodium parasites and the specific host tissues alter the outcome of malaria disease. A better understanding of malaria pathology in the context of host–parasite interactions at the various tissue levels of each organ will allow for better diagnostics and treatments for malaria.
Abstract
Systemic inflammation mediated by Plasmodium parasites is central to malaria disease and its complications. Plasmodium parasites reside in erythrocytes and can theoretically reach all host tissues via the circulation. However, actual interactions between parasitized erythrocytes and host tissues, along with the consequent damage and pathological changes, are limited locally to specific tissue sites. Such tissue specificity of the parasite can alter the outcome of malaria disease, determining whether acute or chronic complications occur. Here, we give an overview of the recent progress that has been made in understanding tissue-specific immunopathology during Plasmodium infection. As knowledge on tissue-specific host–parasite interactions accumulates, better treatment modalities and targets may emerge for intervention in malaria disease.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Murray, C. J. L. et al. Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384, 1005–1070 (2014).
Hempelmann, E. & Krafts, K. Bad air, amulets and mosquitoes: 2,000 years of changing perspectives on malaria. Malar. J. 12, 232 (2013).
Gething, P. W. et al. Mapping Plasmodium falciparum mortality in Africa between 1990 and 2015. N. Engl. J. Med. 375, 2435–2445 (2016).
World Health Organization. World Malaria Report 2015 (WHO, 2015).
Pigott, D. M. et al. Prioritising infectious disease mapping. PLoS Negl. Trop. Dis. 9, e0003756 (2015).
Naing, C., Whittaker, M. A., Nyunt Wai, V. & Mak, J. W. Is Plasmodium vivax malaria a severe malaria?: a systematic review and meta-analysis. PLoS Negl. Trop. Dis. 8, e3071 (2014).
Arévalo-Herrera, M. et al. Clinical profile of Plasmodium falciparum and Plasmodium vivax infections in low and unstable malaria transmission settings of Colombia. Malar. J. 14, 154 (2015).
Millar, S. B. & Cox-Singh, J. Human infections with Plasmodium knowlesi — zoonotic malaria. Clin. Microbiol. Infect. 21, 640–648 (2015).
Seilmaier, M. et al. Severe Plasmodium knowlesi infection with multi-organ failure imported to Germany from Thailand/Myanmar. Malar. J. 13, 422 (2014).
Storm, J. & Craig, A. G. Pathogenesis of cerebral malaria — inflammation and cytoadherence. Front. Cell. Infect. Microbiol. 4, 100 (2014).
Milner, D. A. et al. The systemic pathology of cerebral malaria in African children. Front. Cell. Infect. Microbiol. 4, 104 (2014). This is an important human study that systematically identifies the sequestration of parasites in not only the brain, but also many other parts of the human body during cerebral malaria.
Milner, D. et al. Pulmonary pathology in pediatric cerebral malaria. Hum. Pathol. 44, 2719–2726 (2013).
Milner, D. A. et al. Quantitative assessment of multiorgan sequestration of parasites in fatal pediatric cerebral malaria. J. Infect. Dis. 212, 1317–1321 (2015). This is an important study that quantifies multi-organ sequestration of parasites in fatal human malaria.
Boivin, M. J. et al. Cognitive impairment after cerebral malaria in children: a prospective study. Pediatrics 119, e360–e366 (2007).
Roze, E. et al. Neurologic sequelae after severe falciparum malaria in adult travelers. Eur. Neurol. 46, 192–197 (2001).
Marsh, K. & Kinyanjui, S. Immune effector mechanisms in malaria. Parasite Immunol. 28, 51–60 (2006).
Illingworth, J. et al. Chronic exposure to Plasmodium falciparum is associated with phenotypic evidence of B and T cell exhaustion. J. Immunol. 190, 1038–1047 (2013).
Portugal, S. et al. Malaria-associated atypical memory B cells exhibit markedly reduced B cell receptor signaling and effector function. eLife 4, e07218 (2015).
Portugal, S., Pierce, S. K. & Crompton, P. D. Young lives lost as B cells falter: what we are learning about antibody responses in malaria. J. Immunol. 190, 3039–3046 (2013).
Chen, I. et al. “Asymptomatic” malaria: a chronic and debilitating infection that should be treated. PLoS Med. 13, e1001942 (2016).
Magrath, I. Epidemiology: clues to the pathogenesis of Burkitt lymphoma. Br. J. Haematol. 156, 744–756 (2012).
Thorley-Lawson, D., Deitsch, K. W., Duca, K. a. & Torgbor, C. The link between Plasmodium falciparum malaria and endemic Burkitt'slymphoma — new insight into a 50-year-old enigma. PLoS Pathog. 12, 12–16 (2016).
Torgbor, C. et al. A multifactorial role for P. falciparum malaria in endemic Burkitt's lymphoma pathogenesis. PLoS Pathog. 10, e1004170 (2014).
Robbiani, D. F. et al. Plasmodium infection promotes genomic instability and AID-dependent B cell lymphoma. Cell 162, 727–737 (2015). This study shows that murine Plasmodium infections can promote the development of mature B cell lymphoma by inducing AID expression in lymphoid tissues.
Lewis, C. P., Lavy, C. B. D. & Harrison, W. J. Delay in skeletal maturity in Malawian children. J. Bone Joint Surg. Br. 84, 732–734 (2002).
LaBeaud, A. D. et al. Parasitism in children aged three years and under: relationship between infection and growth in rural coastal Kenya. PLoS Negl. Trop. Dis. 9, e0003721 (2015).
Lee, M. S. J. et al. Plasmodium products persist in the bone marrow and promote chronic bone loss. Sci. Immunol. 2, eaam8093 (2017). This study shows experimentally for the first time that Plasmodium metabolic products, including haemozoin, cause chronic bone loss.
Liehl, P. & Mota, M. M. Innate recognition of malarial parasites by mammalian hosts. Int. J. Parasitol. 42, 557–566 (2012).
Gazzinelli, R. T., Kalantari, P., Fitzgerald, K. A. & Golenbock, D. T. Innate sensing of malaria parasites. Nat. Rev. Immunol. 14, 744–757 (2014).
Egan, E. S. et al. A forward genetic screen identifies erythrocyte CD55 as essential for Plasmodium falciparum invasion. Science 348, 711–714 (2015).
Zenonos, Z. A. et al. Basigin is a druggable target for host-oriented antimalarial interventions. J. Exp. Med. 212, 1145–1151 (2015).
Langhorne, J. & Duffy, P. E. Expanding the antimalarial toolkit: targeting host-parasite interactions. J. Exp. Med. 213, 143–153 (2016).
Sturm, A. et al. Manipulation of host hepatocytes by the malaria parasite for delivery into liver sinusoids. Science 313, 1287–1290 (2006).
Haldar, K. & Mohandas, N. Malaria, erythrocytic infection, and anemia. Hematology Am. Soc. Hematol. Educ. Program 2009, 87–93 (2009).
Miller, L. H., Ackerman, H. C., Su, X.-Z. & Wellems, T. E. Malaria biology and disease pathogenesis: insights for new treatments. Nat. Med. 19, 156–167 (2013).
Evans, K. J., Hansen, D. S., Van Rooijen, N., Buckingham, L. A. & Schofield, L. Severe malarial anemia of low parasite burden in rodent models results from accelerated clearance of uninfected erythrocytes. Blood 107, 1192–1199 (2006).
Lamikanra, A. A. et al. Malarial anemia: of mice and men. Blood 110, 18–28 (2007).
Lamb, T. J., Brown, D. E., Potocnik, A. J. & Langhorne, J. Insights into the immunopathogenesis of malaria using mouse models. Expert Rev. Mol. Med. 8, 1–22 (2006).
Collins, W. E., Jeffery, G. M. & Roberts, J. M. A retrospective examination of anemia during infection of humans with Plasmodium vivax. Am. J. Trop. Med. Hyg. 68, 410–412 (2003).
Jakeman, G. N., Saul, A., Hogarth, W. L. & Collins, W. E. Anaemia of acute malaria infections in non-immune patients primarily results from destruction of uninfected erythrocytes. Parasitology 119, 127–133 (1999).
White, N. J. Malaria parasite clearance. Malar. J. 16, 88 (2017).
Fernandez-Arias, C. et al. Anti-self phosphatidylserine antibodies recognize uninfected erythrocytes promoting malarial anemia. Cell Host Microbe 19, 194–203 (2016).
Sosale, N. G., Spinler, K. R., Alvey, C. & Discher, D. E. Macrophage engulfment of a cell or nanoparticle is regulated by unavoidable opsonization, a species-specific 'Marker of Self' CD47, and target physical properties. Curr. Opin. Immunol. 35, 107–112 (2015).
Segawa, K. & Nagata, S. An apoptotic 'eat me' signal: phosphatidylserine exposure. Trends Cell Biol. 25, 639–650 (2015).
Cunnington, A. J. A., de Souza, J. B., Walther, M. & Riley, E. E. M. Malaria impairs resistance to Salmonella through heme- and heme oxygenase–dependent dysfunctional granulocyte mobilization. Nat. Med. 18, 120–127 (2011).
Ferreira, A., Balla, J., Jeney, V., Balla, G. & Soares, M. P. A central role for free heme in the pathogenesis of severe malaria: the missing link? J. Mol. Med. 86, 1097–1111 (2008).
Zhao, H. et al. Lipocalin 2 bolsters innate and adaptive immune responses to blood-stage malaria infection by reinforcing host iron metabolism. Cell Host Microbe 12, 705–716 (2012).
Langhorne, J., Ndungu, F. M. M., Sponaas, A.-M. & Marsh, K. Immunity to malaria: more questions than answers. Nat. Immunol. 9, 725–732 (2008).
Riley, E. M. & Stewart, V. A. Immune mechanisms in malaria: new insights in vaccine development. Nat. Med. 19, 168–178 (2013).
Tiburcio, M., Sauerwein, R., Lavazec, C. & Alano, P. Erythrocyte remodeling by Plasmodium falciparum gametocytes in the human host interplay. Trends Parasitol. 31, 270–278 (2015).
Goel, S. et al. RIFINs are adhesins implicated in severe Plasmodium falciparum malaria. Nat. Med. 21, 314–317 (2015).
Franke-Fayard, B., Fonager, J., Braks, A., Khan, S. M. & Janse, C. J. Sequestration and tissue accumulation of human malaria parasites: can we learn anything from rodent models of malaria? PLoS Pathog. 6, e1001032 (2010).
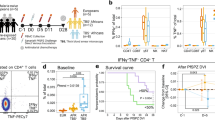
Zhao, H. et al. Olfactory plays a key role in spatiotemporal pathogenesis of cerebral malaria. Cell Host Microbe 15, 551–563 (2014). This is the first study to show that the blood–brain barrier is disrupted at the olfactory bulb during experimental cerebral malaria.
Claser, C. et al. CD8+ T cells and IFN-γ mediate the time-dependent accumulation of infected red blood cells in deep organs during experimental cerebral malaria. PLoS ONE 6, e18720 (2011).
Rénia, L. & Howland, S. W. Targeting the olfactory bulb during experimental cerebral malaria. Trends Parasitol. 30, 375–376 (2014).
Fonager, J. et al. Reduced CD36-dependent tissue sequestration of Plasmodium-infected erythrocytes is detrimental to malaria parasite growth in vivo. J. Exp. Med. 209, 93–107 (2012).
Dorovini-Zis, K. et al. The neuropathology of fatal cerebral malaria in Malawian children. Am. J. Pathol. 178, 2146–2158 (2011).
Turner, L. et al. Severe malaria is associated with parasite binding to endothelial protein C receptor. Nature 498, 502–505 (2013).
Wassmer, S. C. et al. Investigating the pathogenesis of severe malaria: a multidisciplinary and cross-geographical approach. Am. J. Trop. Med. Hyg. 93, 42–56 (2015).
Lennartz, F. et al. Structure-guided identification of a family of dual receptor-binding PfEMP1 that is associated with cerebral malaria. Cell Host Microbe 21, 403–414 (2017).
Howland, S. W. et al. Brain microvessel cross-presentation is a hallmark of experimental cerebral malaria. EMBO Mol. Med. 5, 916–931 (2013).
Jambou, R. et al. Plasmodium falciparum adhesion on human brain microvascular endothelial cells involves transmigration-like cup formation and induces opening of intercellular junctions. PLoS Pathog. 6, e1001021 (2010).
Mantel, P. Y. & Marti, M. The role of extracellular vesicles in Plasmodium and other protozoan parasites. Cell. Microbiol. 16, 344–354 (2014).
Mantel, P. Y. et al. Malaria-infected erythrocyte-derived microvesicles mediate cellular communication within the parasite population and with the host immune system. Cell Host Microbe 13, 521–534 (2013).
van der Heyde, H. C., Nolan, J., Combes, V., Gramaglia, I. & Grau, G. E. A unified hypothesis for the genesis of cerebral malaria: sequestration, inflammation and hemostasis leading to microcirculatory dysfunction. Trends Parasitol. 22, 503–508 (2006).
Frevert, U. & Nacer, A. Immunobiology of Plasmodium in liver and brain. Parasite Immunol. 35, 267–282 (2013).
Owens, T., Bechmann, I. & Engelhardt, B. Perivascular spaces and the two steps to neuroinflammation. J. Neuropathol. Exp. Neurol. 67, 1113–1121 (2008).
Abbott, N. J., Patabendige, A. A. K., Dolman, D. E. M., Yusof, S. R. & Begley, D. J. Structure and function of the blood–brain barrier. Neurobiol. Dis. 37, 13–25 (2010).
Taylor, T. E. et al. Differentiating the pathologies of cerebral malaria by postmortem parasite counts. Nat. Med. 10, 143–145 (2004).
Idro, R., Jenkins, N. E. & Newton, C. R. J. C. Pathogenesis, clinical features, and neurological outcome of cerebral malaria. Lancet Neurol. 4, 827–840 (2005).
Newton, C. R., Hien, T. T. & White, N. Cerebral malaria. J. Neurol. Neurosurg. Psychiatry 69, 433–441 (2000).
Seydel, K. B. et al. Brain swelling and death in children with cerebral malaria. N. Engl. J. Med. 372, 1126–1137 (2015). This study shows that death occurs in humans during cerebral malaria owing to brain swelling and oedema.
Penet, M. F. et al. Imaging experimental cerebral malaria in vivo: significant role of ischemic brain edema. J. Neurosci. 25, 7352–7358 (2005).
Medana, I. M., Hunt, N. H. & Chan-Ling, T. Early activation of microglia in the pathogenesis of fatal murine cerebral malaria. Glia 19, 91–103 (1997).
Coban, C. et al. Pathological role of Toll-like receptor signaling in cerebral malaria. Int. Immunol. 19, 67–79 (2007).
Hoffman, A. et al. Experimental cerebral malaria spreads along the rostral migratory stream. PLoS Pathog. 12, e1005470 (2016).
Shrivastava, S. K. et al. Uptake of parasite-derived vesicles by astrocytes and microglial phagocytosis of infected erythrocytes may drive neuroinflammation in cerebral malaria. Glia 65, 75–92 (2017).
Medana, I. M., Chan-Ling, T. & Hunt, N. H. Redistribution and degeneration of retinal astrocytes in experimental murine cerebral malaria: relationship to disruption of the blood-retinal barrier. Glia 16, 51–64 (1996).
Medana, I. M. et al. Axonal Injury in cerebral malaria. Am. J. Pathol. 160, 655–666 (2002).
Medana, I. M., Idro, R. & Newton, C. R. J. C. Axonal and astrocyte injury markers in the cerebrospinal fluid of Kenyan children with severe malaria. J. Neurol. Sci. 258, 93–98 (2007).
Aspelund, a. et al. A dural lymphatic vascular system that drains brain interstitial fluid and macromolecules. J. Exp. Med. 212, 991–999 (2015).
Louveau, A. et al. Structural and functional features of central nervous system lymphatic vessels. Nature 523, 337–341 (2015). References 81 and 82 describe the presence of dural lymphatics.
Coureuil, M., Lécuyer, H., Bourdoulous, S. & Nassif, X. A journey into the brain: insight into how bacterial pathogens cross blood–brain barriers. Nat. Rev. Microbiol. 15, 149–159 (2017).
Zhao, Z., Nelson, A. R., Betsholtz, C. & Zlokovic, B. V. Establishment and dysfunction of the blood-brain barrier. Cell 163, 1064–1078 (2015).
Louveau, A., Harris, T. H. & Kipnis, J. Revisiting the mechanisms of CNS immune privilege. Trends Immunol. 36, 569–577 (2015).
Ransohoff, R. M. & Engelhardt, B. The anatomical and cellular basis of immune surveillance in the central nervous system. Nat. Rev. Immunol. 12, 623–635 (2012).
Iliff, J. J., Goldman, S. a. & Nedergaard, M. Implications of the discovery of brain lymphatic pathways. Lancet Neurol. 14, 977–979 (2015).
Iliff, J. J. et al. Brain-wide pathway for waste clearance captured by contrast-enhanced MRI. J. Clin. Invest. 123, 1299–1309 (2013).
Ampawong, S. et al. Electron microscopic features of brain edema in rodent cerebral malaria in relation to glial fibrillary acidic protein expression. Int. J. Clin. Exp. Pathol. 7, 2056–2067 (2014).
Promeneur, D., Lunde, L. K., Amiry-Moghaddam, M. & Agre, P. Protective role of brain water channel AQP4 in murine cerebral malaria. Proc. Natl Acad. Sci. USA 110, 1035–1040 (2013).
Bartholomäus, I. et al. Effector T cell interactions with meningeal vascular structures in nascent autoimmune CNS lesions. Nature 462, 94–98 (2009).
Shaw, T. N. et al. Perivascular arrest of CD8+ T cells is a signature of experimental cerebral malaria. PLoS Pathog. 11, e1005210 (2015).
Lackner, P. et al. Scanning electron microscopy of the neuropathology of murine cerebral malaria. Malar. J. 5, 116 (2006).
Ampawong, S. et al. Quantitation of brain edema and localisation of aquaporin 4 expression in relation to susceptibility to experimental cerebral malaria. Int. J. Clin. Exp. Pathol. 4, 566–574 (2011).
Nacer, A. et al. Experimental cerebral malaria pathogenesis — hemodynamics at the blood brain barrier. PLoS Pathog. 10, e1004528 (2014).
Howland, S. W., Poh, C. M. & Rénia, L. Activated brain endothelial cells cross-present malaria antigen. PLoS Pathog. 11, e1004963 (2015).
Howland, S. W., Gun, S. Y., Claser, C., Poh, C. M. & Rénia, L. Measuring antigen presentation in mouse brain endothelial cells ex vivo and in vitro. Nat. Protoc. 10, 2016–2026 (2015).
Swanson, P. a. et al. CD8+ T cells induce fatal brainstem pathology during cerebral malaria via luminal antigen-specific engagement of brain vasculature. PLoS Pathog. 12, e1006022 (2016).
Combes, V., Guillemin, G. J., Chan-Ling, T., Hunt, N. H. & Grau, G. E. R. The crossroads of neuroinflammation in infectious diseases: endothelial cells and astrocytes. Trends Parasitol. 28, 311–319 (2012).
Greiner, J. et al. Correlation of hemorrhage, axonal damage, and blood-tissue barrier disruption in brain and retina of Malawian children with fatal cerebral malaria. Front. Cell. Infect. Microbiol. 5, 18 (2015).
Saeki, N. et al. Histologic characteristics of normal perivascular spaces along the optic tract: new pathogenetic mechanism for edema in tumors in the pituitary region. Am. J. Neuroradiol. 25, 1218–1222 (2004).
Kwee, R. M. & Kwee, T. C. Virchow–Robin spaces at MR imaging. Radiographics 27, 1071–1086 (2007).
Beare, N. A. V., Taylor, T. E., Harding, S. P., Lewallen, S. & Molyneux, M. E. Malarial retinopathy: a newly established diagnostic sign in severe malaria. Am. J. Trop. Med. Hyg. 75, 790–797 (2006). This is the first study to describe malarial retinopathy in human cerebral malaria.
Idro, R., Marsh, K., John, C. C. & Newton, C. R. J. Cerebral malaria: mechanisms of brain injury and strategies for improved neurocognitive outcome. Pediatr. Res. 68, 267–274 (2010).
Maude, R. J. et al. Magnetic resonance imaging of the brain in adults with severe falciparum malaria. Malar. J. 13, 177 (2014).
Grau, G. E. et al. Platelet accumulation in brain microvessels in fatal pediatric cerebral malaria. J. Infect. Dis. 187, 461–466 (2003).
White, V. A., Lewallen, S., Beare, N. A. V., Molyneux, M. E. & Taylor, T. E. Retinal pathology of pediatric cerebral malaria in Malawi. PLoS ONE 4, e4317 (2009).
Beare, N. A., Lewallen, S., Taylor, T. E. & Molyneux, M. E. Redefining cerebral malaria by including malaria retinopathy. Future Microbiol. 6, 349–355 (2011).
Maccormick, I. J. C. et al. Cerebral malaria in children: using the retina to study the brain. Brain 137, 2119–2142 (2014).
Barrera, V. et al. Severity of retinopathy parallels the degree of parasite sequestration in the eyes and brains of Malawian children with fatal cerebral malaria. J. Infect. Dis. 211, 1977–1986 (2015).
Vecino, E., Rodriguez, F. D., Ruzafa, N., Pereiro, X. & Sharma, S. C. Glia–neuron interactions in the mammalian retina. Prog. Retin. Eye Res. 51, 1–40 (2016).
Saggu, R., Faille, D., Grau, G. E., Cozzone, P. J. & Viola, A. In the eye of experimental cerebral malaria. Am. J. Pathol. 179, 1104–1109 (2011).
Danielyan, L. et al. Intranasal delivery of cells to the brain. Eur. J. Cell Biol. 88, 315–324 (2009).
Chaigneau, E. et al. Two-photon imaging of capillary blood flow in olfactory bulb glomeruli. Proc. Natl Acad. Sci. USA 100, 13081–13086 (2003).
Ueno, M. & Dobrogowska, D. H. & Vorbrodt, A. W. Immunocytochemical evaluation of the blood-brain barrier to endogenous albumin in the olfactory bulb and pons of senescence-accelerated mice (SAM). Histochem. Cell Biol. 105, 203–212 (1996).
Ioannidis, L. J., Nie, C. Q. & Hansen, D. S. The role of chemokines in severe malaria: more than meets the eye. Parasitology 141, 602–613 (2014).
Abkallo, H. M. et al. DNA from pre-erythrocytic stage malaria parasites is detectable by PCR in the faeces and blood of hosts. Int. J. Parasitol. 44, 467–473 (2014).
Taniguchi, T. et al. Plasmodium berghei ANKA causes intestinal malaria associated with dysbiosis. Sci. Rep. 5, 15699 (2015). This study shows that P. berghei parasites may promote gut pathology and dysbiosis of the intestinal microbiota.
Feasey, N. A., Dougan, G., Kingsley, R. A., Heyderman, R. S. & Gordon, M. A. Invasive non-typhoidal salmonella disease: an emerging and neglected tropical disease in Africa. Lancet 379, 2489–2499 (2012).
Chau, J. Y. et al. Malaria-associated L-arginine deficiency induces mast cell-associated disruption to intestinal barrier defenses against nontyphoidal salmonella bacteremia. Infect. Immun. 81, 3515–3526 (2013).
Adegnika, A. a & Kremsner, P. G. Epidemiology of malaria and helminth interaction: a review from 2001 to 2011. Curr. Opin. HIV AIDS 7, 221–224 (2012).
Potts, R. A. et al. Mast cells and histamine alter intestinal permeability during malaria parasite infection. Immunobiology 221, 468–474 (2015).
Mastelic, B. et al. IL-22 protects against liver pathology and lethality of an experimental blood-stage malaria infection. Front. Immunol. 3, 85 (2012).
Mooney, J. P. et al. The mucosal inflammatory response to non-typhoidal Salmonella in the intestine is blunted by IL-10 during concurrent malaria parasite infection. Mucosal Immunol. 7, 1302–1311 (2014).
Sellau, J., Alvarado, C., Hoenow, S. & Mackroth, M. IL-22 dampens the T cell response in experimental malaria. Sci. Rep. 6, 28058 (2016).
Yilmaz, B. et al. Gut microbiota elicits a protective immune response against malaria transmission. Cell 159, 1277–1289 (2014).
Villarino, N. F. et al. Composition of the gut microbiota modulates the severity of malaria. Proc. Natl Acad. Sci. USA 113, 2235–2240 (2016). This study shows that the gut microbiota modulates the severity of malaria.
Yooseph, S. et al. Stool microbiota composition is associated with the prospective risk of Plasmodium falciparum infection. BMC Genomics 16, 631 (2015).
Bernier-Latmani, J. et al. DLL4 promotes continuous adult intestinal lacteal regeneration and dietary fat transport. J. Clin. Invest. 125, 4572–4586 (2015).
Spadoni, I., Fornasa, G. & Rescigno, M. Organ-specific protection mediated by cooperation between vascular and epithelial barriers. Nat. Rev. Immunol. 17, 761–773 (2017).
Morrison, S. J. & Scadden, D. T. The bone marrow niche for haematopoietic stem cells. Nature 505, 327–334 (2014).
Imai, T. et al. Cytotoxic activities of CD8+ T cells collaborate with macrophages to protect against blood-stage murine malaria. eLife 2015, e04232 (2015).
Panichakul, T. et al. Production of erythropoietic cells in vitro for continuous culture of Plasmodium vivax. Int. J. Parasitol. 37, 1551–1557 (2007).
Tamez, P. A., Liu, H., Fernandez-Pol, S., Haldar, K. & Wickrema, A. Stage-specific susceptibility of human erythroblasts to Plasmodium falciparum malaria infection. Blood 114, 3652–3655 (2009).
Farfour, E., Charlotte, F., Settegrana, C., Miyara, M. & Buffet, P. The extravascular compartment of the bone marrow: a niche for Plasmodium falciparum gametocyte maturation? Malar. J. 11, 285 (2012).
Joice, R. et al. Plasmodium falciparum transmission stages accumulate in the human bone marrow. Sci. Transl Med. 6, 244re5 (2014).
Aguilar, R. et al. Molecular evidence for the localization of Plasmodium falciparum immature gametocytes in bone marrow. Blood 123, 959–966 (2014).
Chasis, J. A. & Mohandas, N. Erythroblastic islands: niches for erythropoiesis. Blood 112, 470–478 (2008).
Imai, T. et al. CD8+ T cell activation by murine erythroblasts infected with malaria parasites. Sci. Rep. 3, 1572 (2013).
Mercier, F. E., Ragu, C. & Scadden, D. T. The bone marrow at the crossroads of blood and immunity. Nat. Rev. Immunol. 12, 49–60 (2011).
Omatsu, Y. & Nagasawa, T. The critical and specific transcriptional regulator of the microenvironmental niche for hematopoietic stem and progenitor cells. Curr. Opin. Hematol. 22, 330–336 (2015).
Taylor, W. R. J., Hanson, J., Turner, G. D. H., White, N. J. & Dondorp, A. M. Respiratory manifestations of malaria. Chest 142, 492–505 (2012).
Ehrich, J. H. H. & Eke, F. U. Malaria-induced renal damage: facts and myths. Pediatr. Nephrol. 22, 626–637 (2007).
Brabin, B. J. et al. The sick placenta — the role of malaria. Placenta 25, 359–378 (2004).
Shechter, R., London, A. & Schwartz, M. Orchestrated leukocyte recruitment to immune-privileged sites: absolute barriers versus educational gates. Nat. Rev. Immunol. 13, 206–218 (2013).
Aspelund, A. et al. The Schlemm's canal is a VEGF-C/VEGFR-3-responsive lymphatic-like vessel. J. Clin. Invest. 124, 3975–3986 (2014).
Maitland, K. & Marsh, K. Pathophysiology of severe malaria in children. Acta Trop. 90, 131–140 (2004).
Wilairatana, P., Meddings, J. B., Ho, M., Vannaphan, S. & Looareesuwan, S. Increased gastrointestinal permeability in patients with Plasmodium falciparum malaria. Clin. Infect. Dis. 24, 430–435 (1997).
Romero, A. et al. Changes in gastric mucosa in acute malaria [Spanish]. Gen 47, 123–128 (1993).
Anstey, N. M., Douglas, N. M., Poespoprodjo, J. R. & Price, R. N. Plasmodium vivax: clinical spectrum, risk factors and pathogenesis. Adv. Parasitol. 80, 151–201 (2012).
Collins, W. E. & Jeffery, G. M. Plasmodium ovale: parasite and disease. Clin. Microbiol. Rev. 18, 570–581 (2005).
Strydom, K.-A., Ismail, F. & Frean, J. Plasmodium ovale: a case of not-so-benign tertian malaria. Malar. J. 13, 85 (2014).
Collins, W. E. & Jeffery, G. M. Plasmodium malariae: parasite and disease. Clin. Microbiol. Rev. 20, 579–592 (2007).
Singh, B. & Daneshvar, C. Human infections and detection of Plasmodium knowlesi. Clin. Microbiol. Rev. 26, 165–184 (2013).
Acknowledgements
The authors are supported by Grants-in-Aid for Scientific Research (B grant no. 16H05181 to C.C.) and by the Japan Agency for Medical Research and Development (AMED J-PRIDE 17fm0208021h0001 to C.C.).
Author information
Authors and Affiliations
Contributions
C.C. wrote the manuscript; all authors contributed to researching data, discussing the content and reviewing and editing the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Glossary
- Malaria
-
A disease caused by Plasmodium parasites belonging to the Apicomplexa phylum, which consists of several obligate intracellular parasites. The term was originally used in Italian folk medicine to mean poisonous or bad air.
- Activation-induced cytidine deaminase
-
(AID). An enzyme that is required for two crucial B cell events in the germinal centre: somatic hypermutation and class-switch recombination.
- Connective tissue
-
A connecting and supporting tissue composed of collagen and/or elastin fibres and interstitial fluid. Blood, bone and adipose tissue are some of the connective tissue components.
- Perivascular spaces
-
Also known as Virchow–Robin spaces. Spaces located between brain-penetrating pial vessels and the brain tissue grey matter.
- Interstitial fluid
-
(ISF). The solution present extracellularly, that fills the spaces between cells and tissues.
- Cerebrospinal fluid
-
(CSF). The solution surrounding the brain and spinal cord, which mainly serves to protect these two important organs.
- Olfactory bulb
-
An organ located on the cribriform plate, which functions in smell. The bulb surface is surrounded by complex olfactory nerve structures that originate from the nasal cavity and project to the brain. Small trabecular capillary structures are the main vessel structures inside the bulb.
- Cribriform plate
-
A small, perforated bone structure that lies on top of the nasal cavity and supports the olfactory bulb. Olfactory nerves running from the nasal cavity to the olfactory bulb pass thorough cribriform plate.
- Neurovascular coupling
-
A mechanism explaining the relationship between neuronal activity and the cerebral blood vessels and the blood flow.
- Lacteals
-
Small lymphatic capillaries located in the villi of the small intestine.
- Sinusoids
-
Vessels with a structure similar to capillaries but that have larger diameters and porous endothelial cells, which allow for permeability and exchange of materials; they are located in bone marrow, liver and spleen.
- Haemozoin
-
A unique by-product of Plasmodium parasites that accumulates in several organs, including spleen, liver and bone marrow, even after the infection resolves.
Rights and permissions
About this article
Cite this article
Coban, C., Lee, M. & Ishii, K. Tissue-specific immunopathology during malaria infection. Nat Rev Immunol 18, 266–278 (2018). https://doi.org/10.1038/nri.2017.138
Published:
Issue Date:
DOI: https://doi.org/10.1038/nri.2017.138
This article is cited by
-
Avian malaria in a feral-pet pigeon: a case report
Malaria Journal (2024)
-
Kidney involvement in Plasmodium falciparum infection in a pregnant patient
Malaria Journal (2024)
-
Genome-wide liver transcriptomic profiling of a malaria mouse model reveals disturbed immune and metabolic responses
Parasites & Vectors (2023)
-
Xylopic acid-amodiaquine and xylopic acid-artesunate combinations are effective in managing malaria in Plasmodium berghei-infected mice
Malaria Journal (2021)
-
Constitutive immune mechanisms: mediators of host defence and immune regulation
Nature Reviews Immunology (2021)