Abstract
The 2022 mpox virus (MPXV) outbreak was sustained by human-to-human transmission; however, it is currently unclear which factors lead to sustained transmission of MPXV. Here we present Mastomys natalensis as a model for MPXV transmission after intraperitoneal, rectal, vaginal, aerosol and transdermal inoculation with an early 2022 human outbreak isolate (Clade IIb). Virus shedding and tissue replication were route dependent and occurred in the presence of self-resolving localized skin, lung, reproductive tract or rectal lesions. Mucosal inoculation via the rectal, vaginal and aerosol routes led to increased shedding, replication and a pro-inflammatory T cell profile compared with skin inoculation. Contact transmission was higher from rectally inoculated animals. This suggests that transmission might be sustained by increased susceptibility of the anal and genital mucosae for infection and subsequent virus release.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
Data were deposited in figshare: https://doi.org/10.6084/m9.figshare.25105940. Source data are provided with this paper.
References
Adalja, A. & Inglesby, T. A novel international monkeypox outbreak. Ann. Intern. Med. 175, 1175–1176 (2022).
Happi, C. et al. Urgent need for a non-discriminatory and non-stigmatizing nomenclature for monkeypox virus. PLoS Biol. 20, e3001769 (2022).
Likos, A. M. et al. A tale of two clades: monkeypox viruses. J. Gen. Virol. 86, 2661–2672 (2005).
Alakunle, E., M, U., Nchinda, G. & Okeke, M. Monkeypox virus in Nigeria: infection biology, epidemiology, and evolution. Viruses 12, 1257 (2020).
Hobson, G. et al. Family cluster of three cases of monkeypox imported from Nigeria to the United Kingdom, May 2021. Euro Surveill. 26, 2100745 (2021).
Antinori, A. et al. Epidemiological, clinical, and virological characteristics of four cases of monkeypox support transmission through sexual contact, Italy, May 2022. Euro Surveill. 27, 2200421 (2022).
Adler, H. et al. Clinical features and management of human monkeypox: a retrospective observational study in the UK. Lancet Infect. Dis. 22, 1153–1162 (2022).
Nolen, L. et al. Introduction of monkeypox into a community and household: risk factors and zoonotic reservoirs in the Democratic Republic of the Congo. Am. J. Trop. Med. Hyg. 93, 410–415 (2015).
Jezek Z, M. S., Mutumbo, M., Nakano, J., Paluku, K. & Szczeniowski, M. Human monkeypox: a study of 2,510 contacts of 214 patients. J. Infect. Dis. 154, 551–555 (1986).
CDC in Centers for Disease Control and Prevention (2022). https://www.cdc.gov/poxvirus/mpox/response/2022/index.html
CDC Secondary and tertiary transmission of vaccinia virus after sexual contact with a smallpox vaccinee—San Diego, California, 2012. MMWR Morb. Mortal Wkly. Rep. 62, 145–147 (2013).
Chapman, J. L., Nichols, D. K., Martinez, M. J. & Raymond, J. W. Animal models of orthopoxvirus infection. Vet. Pathol. 47, 852–870 (2010).
Johnson, R. F. et al. Comparative analysis of monkeypox virus infection of cynomolgus macaques by the intravenous or intrabronchial inoculation route. J. Virol. 85, 2112–2125 (2011).
Parker, S. & Buller, R. M. A review of experimental and natural infections of animals with monkeypox virus between 1958 and 2012. Future Virol. 8, 129–157 (2013).
Hutson, C. L. et al. A prairie dog animal model of systemic orthopoxvirus disease using West African and Congo Basin strains of monkeypox virus. J. Gen. Virol. 90, 323–333 (2009).
Schultz, D. A., Sagartz, J. E., Huso, D. L. & Buller, R. M. Experimental infection of an African dormouse (Graphiurus kelleni) with monkeypox virus. Virology 383, 86–92 (2009).
Americo, J. L., Moss, B. & Earl, P. L. Identification of wild-derived inbred mouse strains highly susceptible to monkeypox virus infection for use as small animal models. J. Virol. 84, 8172–8180 (2010).
Hutson, C. L. & Damon, I. K. Monkeypox virus infections in small animal models for evaluation of anti-poxvirus agents. Viruses 2, 2763–2776 (2010).
Hutson, C. L. et al. Comparison of monkeypox virus clade kinetics and pathology within the prairie dog animal model using a serial sacrifice study design. Biomed. Res. Int. 2015, 965710 (2015).
Falendysz, E. A. et al. Further assessment of monkeypox virus infection in Gambian pouched rats (Cricetomys gambianus) using in vivo bioluminescent imaging. PLoS Negl. Trop. Dis. https://doi.org/10.1371/journal.pntd.0004130 (2015).
Falendysz, E. A. et al. Characterization of Monkeypox virus infection in African rope squirrels (Funisciurus sp.). PLoS Negl. Trop. Dis. https://doi.org/10.1371/journal.pntd.0005809 (2017).
Earl, P. L., Americo, J. L., Cotter, C. A. & Moss, B. Comparative live bioluminescence imaging of monkeypox virus dissemination in a wild-derived inbred mouse (Mus musculus castaneus) and outbred African dormouse (Graphiurus kelleni). Virology 475, 150–158 (2015).
Shchelkunov, S. N., Marennikova, S. S. & Moyer, R. W. Orthopoxviruses Pathogenic for Humans (Springer Science+Business Media, 2006).
Isaäcson, M. The ecology of Praomys (Mastomys) natalensis in southern Africa. Bull. World Health Organ. 52, 629–636 (1975).
Wozniak, D. M. et al. Inoculation route-dependent Lassa virus dissemination and shedding dynamics in the natural reservoir—Mastomys natalensis. Emerg. Microbes Infect. 10, 2313–2325 (2021).
Safronetz, D. et al. Temporal analysis of Lassa virus infection and transmission in experimentally infected Mastomys natalensis. PNAS Nexus 1, pgac114 (2022).
Bragazzi, N. et al. Epidemiological trends and clinical features of the ongoing monkeypox epidemic: a preliminary pooled data analysis and literature review. J. Med. Virol. 95, e27931 (2022).
Perez Duque, M. et al. Ongoing monkeypox virus outbreak, Portugal, 29 April to 23 May 2022. Euro Surveill. 27, 2200424 (2022).
Kibungu, E. M. et al. Clade I-associated mpox cases associated with sexual contact, the Democratic Republic of the Congo. Emerg. Infect. Dis. 30, 172–176 (2024).
Mpox (monkeypox) in the Democratic Republic of the Congo. World Health Organization https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON493 (2023).
Breman, J. et al. Human monkeypox, 1970-79. Bull. World Health Organ. 58, 165–182 (1980).
Hammerschlag, Y. et al. Monkeypox infection presenting as genital rash, Australia, May 2022. Euro Surveill. https://doi.org/10.2807/1560-7917.Es.2022.27.22.2200411 (2022).
Lum, F. M. et al. Monkeypox: disease epidemiology, host immunity and clinical interventions. Nat. Rev. Immunol. 22, 597–613 (2022).
Davido, B., D’Anglejan, E., Jourdan, J., Robinault, A. & Davido, G. Monkeypox 2022 outbreak: cases with exclusive genital lesions. J. Travel Med. https://doi.org/10.1093/jtm/taac077 (2022).
Kelley, C. F. et al. The rectal mucosa and condomless receptive anal intercourse in HIV-negative MSM: implications for HIV transmission and prevention. Mucosal Immunol. 10, 996–1007 (2017).
Zingaropoli, M. A. et al. Longitudinal virological and immunological profile in a case of human monkeypox infection. Open Forum Infect. Dis. 9, ofac569 (2022).
Hammarlund, E. et al. Monkeypox virus evades antiviral CD4+ and CD8+ T cell responses by suppressing cognate T cell activation. Proc. Natl Acad. Sci. USA 105, 14567–14572 (2008).
Xiao, S. Y. et al. Experimental infection of prairie dogs with monkeypox virus. Emerg. Infect. Dis. 11, 539–545 (2005).
Hutson, C. L. et al. Monkeypox disease transmission in an experimental setting: prairie dog animal model. PLoS ONE 6, e28295 (2011).
Hoffmann, C. et al. Experimental Morogoro virus infection in its natural host, Mastomys natalensis. Viruses https://doi.org/10.3390/v13050851 (2021).
Meyer, B. J. & Schmaljohn, C. S. Persistent hantavirus infections: characteristics and mechanisms. Trends Microbiol. 8, 61–67 (2000).
Deschambault, Y. et al. Experimental infection of North American deer mice with clade I and II monkeypox virus isolates. Emerg. Infect. Dis. 29, 858–860 (2023).
Heberling, R. L. & Kalter, S. S. Induction, course, and transmissibility of monkeypox in the baboon (Papio cynocephalus). J. Infect. Dis. 124, 33–38 (1971).
Hánová, A. et al. Historical demography and climatic niches of the Natal multimammate mouse (Mastomys natalensis) in the Zambezian region. Mamm. Biol. 103, 239–251 (2023).
Hutson, C. L. et al. Dosage comparison of Congo Basin and West African strains of monkeypox virus using a prairie dog animal model of systemic orthopoxvirus disease. Virology 402, 72–82 (2010).
Osorio, J. E., Iams, K. P., Meteyer, C. U. & Rocke, T. E. Comparison of monkeypox viruses pathogenesis in mice by in vivo imaging. PLoS ONE 4, e6592 (2009).
Americo, J. L., Earl, P. L. & Moss, B. Virulence differences of mpox (monkeypox) virus clades I, IIa, and IIb.1 in a small animal model. Proc. Natl Acad. Sci. USA 120, e2220415120 (2023).
Safronetz, D. et al. Establishment of a genetically confirmed breeding colony of Mastomys natalensis from wild-caught founders from West Africa. Viruses https://doi.org/10.3390/v13040590 (2021).
de Wit, E. et al. The Middle East respiratory syndrome coronavirus (MERS-CoV) does not replicate in Syrian hamsters. PLoS ONE 8, e69127 (2013).
Alexander, D. J. et al. Association of Inhalation Toxicologists (AIT) working party recommendation for standard delivered dose calculation and expression in non-clinical aerosol inhalation toxicology studies with pharmaceuticals. Inhal. Toxicol. 20, 1179–1189 (2008).
Hartings, J. M. & Roy, C. J. The automated bioaerosol exposure system: preclinical platform development and a respiratory dosimetry application with nonhuman primates. J. Pharmacol. Toxicol. Methods 49, 39–55 (2004).
Li, Y., Zhao, H., Wilkins, K., Hughes, C. & Damon, I. K. Real-time PCR assays for the specific detection of monkeypox virus West African and Congo Basin strain DNA. J. Virol. Methods 169, 223–227 (2010).
Liu, J. et al. Retrospective detection of monkeypox virus in the testes of nonhuman primate survivors. Nat. Microbiol. 7, 1980–1986 (2022).
Acknowledgements
We want to thank Z. Wiener, T. Smith, N. Baird, C. Hutson, F. Atif and I. Damon of the CDC for rapidly sharing the MPXV strain used in this study, A. Chowdhury and D. Douek of the Vaccine Research Center for sharing protein used in the ELISA, and X. Zeng of the United States Army Medical Research Institute of Infectious Diseases for sharing positive control tissues for histology. We would also like to thank B. Moss, P. Earl, E. Haddock, R. Fischer, the RML Institutional Biosafety Committee and the biosafety office for helpful suggestions and support. We would like to thank the animal caretakers for their assistance during the study. We want to thank A. Athman, R. Perry-Gottschalk and A. Mora from the VMA for assisting with image compilation. Lastly, we want to thank N. van Doremalen for helpful feedback on the paper.
This work was supported by the Intramural Research Program of the National Institute of Allergy and Infectious Diseases (NIAID), National Institutes of Health (NIH) (1ZIAAI001179-01). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the paper. This paper has been deposited as a preprint with bioRxiv under a CC0 license for government authors.
Author information
Authors and Affiliations
Contributions
J.R.P. and K.R. designed the studies. J.R.P., J.C.R., S.G.S., F.K.K., M.C.L., S.G., A.O., T.B., J.E.S., R.R., J.P.-S., A.C., S.B., B.J.S. and K.R. performed the experiments. J.R.P., K.R., J.C.R., S.G.S., L.M., F.K.K. and G.S. analysed results. J.R.P., K.R. and V.J.M. wrote the paper. V.J.M. and H.F. secured funding for the study. All co-authors reviewed the paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Microbiology thanks Eric Mucker and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Lesion formation after inoculation of Mastomys natalensis with MPXV.
M. natalensis were challenged with 105 PFU MPXV (2022 isolate, Clade IIb) using one of the transdermal, rectal, vaginal, or intraperitoneal routes (N = 8; 4 males and 4 females). (a-c) Exemplary skin lesions. (d-f) Exemplary irritation of the vagina and the rectum.
Extended Data Fig. 2 Representative gating strategy for flow cytometric analysis of splenocytes.
In the first experiment with rectal and transdermal infection, splenocytes were first gated on SSC-A vs FSC-A (a), followed by a Time gate to exclude possible erratic sample flow (b), followed by a single cell gate using FSC-H vs FSC-A (c), which was followed by a dead cell exclusion gate using Fixable Blue vs Time (d). In the second experiment with aerosol infection, counting beads were included and first EDF3excluded from the analysis (e), followed by a lymphocyte gate (f), followed by a single cell gate (g), which was followed by a dead cell and Time gate (h). This population was further analyzed by gating on B cells or T cells using CD19 PE-CF594 vs CD3 FITC as represented in Fig. 4a. CD19+ and CD3+ cells were then further analyzed for expression of Ki-67 R718, Granzyme B APC, MHCII PE, TNFα eF450 and IFNγ PE as represented in Fig. 4e.
Extended Data Fig. 3 Polyfunctionality of T-cell response after rectal, aerosol, or transdermal inoculation.
M. natalensis were inoculated with MPXV by the rectal, aerosol, or transdermal route. Uninfected age-matched animals served as controls. Splenocytes were analyzed by flow cytometry at day 14. Splenocytes were cultured in vitro for 24 hours in the presence of IL-2. a CD3+ T-cells were then analyzed by intracellular flow cytometry for expression of Ki-67, Granzyme B, TNFα, and IFNγ. Boolean gating was performed. Bar graph depicting median, 95% CI, and individuals. Rectal N = 6, transdermal N = 6, aerosol N = 8. b Comparison of expression of Ki-67, Granzyme B, TNFα, and IFNγ after in vitro culture in the presence of IL-2 alone and when stimulated by MPXV-specific peptides. Rectal N = 6, transdermal N = 6, control N = 11, aerosol N = 8. Bar graph depicting median, 95% CI, and individuals. Two-way ANOVA, followed by Šídák’s multiple comparisons test. P-values indicated where significant.
Extended Data Fig. 4 Cell infiltration to the lesion sites after transdermal, aerosol, and rectal inoculation.
M. natalensis were challenged with 105 PFU MPXV (2022 isolate, Clade IIb) using one of the transdermal, aerosol, or rectal routes and tissues were collected on day 8 (N = 4). Immunohistochemical staining for CD3 as a marker for T-cells. PAX5 as a marker for B-cells, IBA-1 as a marker for macrophages. Transdermal (skin) (a, b, c), aerosol (nasal turbinates) (j, k, l) & rectal (rectum) (d, e, f) 40x: bar = 200 µm; vaginal (vagina and uterus) (g, h, i) 20x: bar = 500 µm; aerosol (lungs) (m, n, o) 200x: bar = 50 µm.
Extended Data Fig. 5 Rectal shedding dynamics of individual contact transmission pairs after rectal and transdermal inoculation.
M. natalensis were challenged with 105 PFU MPXV (2022 isolate, Clade IIb) using either the rectal (a) or transdermal (b) route (N = 8; 4 males and 4 females). On day 2, eight donor animals were co-housed with eight naïve sentinels (sex-matched, 2:2 ratio) and co-housed for 12 days. Rectal swabs were collected on days 3, 5, 7, 9, 11, and 14 post-inoculation/-exposure. Median of N = 2 swabs collected per time point (dark continuous = donors, light dotted = sentinels). M = male, F = female.
Extended Data Fig. 6 Oral shedding dynamics of individual contact transmission pairs after rectal and transdermal inoculation.
M. natalensis were challenged with 105 PFU MPXV (2022 isolate, Clade IIb) using either the rectal (a) or transdermal (b) route (N = 8; 4 males and 4 females). On day 2, eight donor animals were co-housed with eight naïve sentinels (sex-matched, 2:2 ratio) and co-housed for 12 days. Oral swabs were collected on days 3, 5, 7, 9, 11, and 14 post-inoculation/-exposure. Median of N = 2 swabs collected per time point (dark continuous = donors, light dotted = sentinels). M = male, F = female.
Extended Data Fig. 7 Rectal shedding dynamics of individual contact transmission pairs after rectal and transdermal inoculation.
M. natalensis were challenged with 105 PFU MPXV (2022 isolate, Clade IIb) using the aerosol route and exposure occurred either continuously (a) or was limited to the peak oral shedding phase of the donors (b). (N = 8; 4 males and 4 females). On day 2, eight donor animals were co-housed with eight naïve sentinels (sex-matched, 2:2 ratio) and co-housed for 12 days for continuous exposure. For the limited exposure window, sentinels were exposed between day 3 and 6. Rectal swabs were collected on days 3, 5, 7, 9, 11, and 14- post inoculation/-exposure. Median of N = 2 swabs collected per time point (dark continuous = donors, light dotted = sentinels). M = male, F = female.
Extended Data Fig. 8 Oral shedding dynamics of individual contact transmission pairs after continues or limited exposure to aerosol inoculated donors.
M. natalensis were challenged with 105 PFU MPXV (2022 isolate, Clade IIb) using the aerosol route and exposure occurred either continuously (a) or was limited to the peak oral shedding phase of the donors (b). (N = 8; 4 males and 4 females). On day 2, eight donor animals were co-housed with eight naïve sentinels (sex-matched, 2:2 ratio) and co-housed for 12 days for continuous exposure. For the limited exposure window, sentinels were exposed between day 3 and 6. Oral swabs were collected on days 3, 5, 7, 9, 11, and 14- post inoculation/-exposure. Median of N = 2 swabs collected per time point (dark continuous = donors, light dotted = sentinels). M = male, F = female.
Extended Data Fig. 9 Contact transmission in Mastomys natalensis.
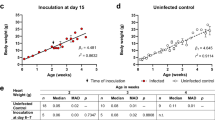
M. natalensis were challenged with 105 PFU MPXV (2022 isolate, Clade IIb) using either the transdermal, rectal, or aerosol route (N = 8; 4 males and 4 females). On day 2, eight donor animals were co-housed with eight naïve sentinels (sex-matched, 2:2 ratio) for 12 days. a Oral and rectal swabs were collected on days 3, 5, 7, 9, 11, and 14 post-inoculation/-exposure. Averaged percentage of swabs positive for each group depicted as pie charts. Black = positive PCR result, white = negative PCR result. b, c Correlation between the number of positive rectal and oral donors swab samples and the total of positive sentinel swabs. Median individual values for each cage are depicted, as well as simple linear regression line across all transmission cages. Spearman r values are depicted. Teal = rectal, black = transdermal, and orange = aerosol inoculated donors. d Correlation between the number of all positive donor swabs and all positive sentinel swabs, separated by sex. Median individual values for each cage are depicted, as well as simple linear regression lines across all transmission cages. Spearman r values are depicted. Black = males, pink = females. e M. natalensis were challenged using one of the transdermal, rectal, vaginal, intraperitoneal, or aerosol routes. Viral genetic copies (left) and infectious virus (right) measured in oral, rectal, or urogenital skin swabs on days 1, 3, 5, 7, 9, 11, and 14 post-inoculation. Cumulative shedding (day 1 to day 14) across all routes, separated by sex, calculated as area under the curve (AUC), N = 16. Bar chart, mean and SEM, and individuals are depicted. Light grey = vaginally inoculated females.
Supplementary information
Supplementary Information
Supplementary Tables 1–3.
Source data
Source Data Fig. 1
Statistical source data.
Source Data Fig. 2
Unprocessed images.
Source Data Fig. 3
Statistical source data.
Source Data Fig. 4
Statistical source data.
Source Data Fig. 4
Unprocessed images.
Source Data Fig. 5
Statistical source data.
Source Data Fig. 6
Statistical source data.
Source Data Extended Data Fig. 1
Unprocessed images.
Source Data Extended Data Fig. 2
Unprocessed images.
Source Data Extended Data Fig. 3
Statistical source data.
Source Data Extended Data Fig. 4
Unprocessed images.
Source Data Extended Data Fig. 5
Statistical source data.
Source Data Extended Data Fig. 6
Statistical source data.
Source Data Extended Data Fig. 7
Statistical source data.
Source Data Extended Data Fig. 8
Statistical source data.
Source Data Extended Data Fig. 9
Statistical source data.
Rights and permissions
About this article
Cite this article
Port, J.R., Riopelle, J.C., Smith, S.G. et al. Infection with mpox virus via the genital mucosae increases shedding and transmission in the multimammate rat (Mastomys natalensis). Nat Microbiol 9, 1231–1243 (2024). https://doi.org/10.1038/s41564-024-01666-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41564-024-01666-1