Abstract
Antiviral properties of different oxa- and aza-heterocycles are identified and properly correlated with their structural features and discussed in this review article. The primary objective is to explore the activity of such ring systems as antiviral agents, as well as their synthetic routes and biological significance. Eventually, the structure–activity relationship (SAR) of the heterocyclic compounds, along with their salient characteristics are exhibited to build a suitable platform for medicinal chemists and biotechnologists. The synergistic conclusions are extremely important for the introduction of a newer tool for the future drug discovery program.
Keywords: antiviral agents, heterocycles, natural products, Structure Activity Relationship (SAR), synthetic methods
1. Introduction
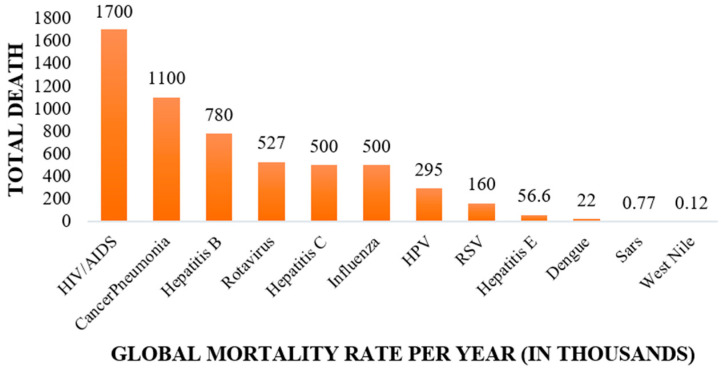
The terrible impact of viral diseases has become a severe concern for the whole animal kingdom, including human beings, during the last few decades [1,2,3]. Several categories of viruses, given their diverse behavior against biological systems, are the major reasons for the incidence of chronic health issues. It is indeed extremely important to address the epidemic nature and the corresponding mortality rate of such diseases in comparison to other fatal infections [4,5]. According to recent reports, the highest number of deaths have been caused by cardiovascular diseases throughout the globe [6], but still, viral infections also have been responsible for millions of human casualties every year (Figure 1). Human immunodeficiency virus (HIV) is considered to be very fatal in nature [7], but it is also very important to note the pervasive nature of other viruses with respect to geographic and economic diversity [8]. As, for example, Rabies disease (originated from domestic dogs) is 100% fatal to humans, but not a pandemic [9]. Disease due to the Ebola virus is a global pandemic with very high average fatality rate (~55%), but it varies depending upon the region [10,11,12].
Figure 1.
Global mortality rate per year due to different viral infections [13].
In the year of 1918, there was an outbreak of the H1N1 Influenza virus, which is definitely considered to be the world’s biggest pandemic, known as the Spanish flu [14,15]. It was exceptionally severe; 50 million people (~2% of the world’s population) become infected during 1918–1920 [16,17]. In recent times, the entire world has gone through a catastrophic situation due to the rapid spread of a newly emerged COVID-19, or severe acute respiratory syndrome CoV-2 (SARS-CoV-2) virus [18]. The existence of this highly contagious virus was first reported in December 2019 in Wuhan, China. The World Health Organization (WHO) began immediate special surveillance on this particular issue and effectively framed several protocols throughout the globe. But to the present day, there are very limited remedies available to fight against this COVID-19 [19,20,21,22,23]. The vaccines listed and recommended by WHO are the only solutions to combat these deadly infections [24]. After facing such situations, it is undoubtedly needed to develop libraries of newer drug candidates corresponding to each and every virus, in order to control their fatal outcomes.
In drug discovery research, the role of heterocyclic moieties is extremely significant in order to make stable interactions with the targeted proteins [25,26]. Such ring systems offer suitable coordination with the specific proteins by tailoring the bulk size and pertinent electron density to modulate the efficacy of the drug compounds in the biological environments [27,28,29,30,31,32]. For these reasons, the synthetic and biological studies of structurally designed heterocyclic moieties are really a crucial measure for the development of future generation drug candidates [33,34,35,36,37]. In this review article, our main focus will be on the structural features, along with the synthetic routes, of oxygen- and nitrogen-containing ring systems (saturated/unsaturated derivatives) present in several natural products, marketed drugs and synthetic analogues having prominent antiviral activities.
2. Overview of the Viral Diseases
Based on its genomic aspects, a virus could be classified as a DNA virus [38] (DNA as a genetic material), which replicates with the help of DNA polymerase (e.g., HSV and HCMV). Secondly, it could be categorized as an RNA virus (RNA as a genetic material), which replicates in the presence of RNA polymerase (e.g., HCV, HBV, RSV and Ebola virus) [39]. Thirdly, it could be categorized as a reverse-transcribing virus [40]; for these viruses, the genome is RNA, but by using a reverse transcriptase enzyme, it is able to form DNA (e.g., HIV) [41].
2.1. Human Immunodeficiency Virus (HIV)
This retrovirus was discovered in the year 1983 [42] and is mainly transmitted through bodily fluids or by bodily contacts of HIV-positive patients. According to the WHO global health survey, there are 38.0 million people living with HIV, and 690,000 people had died by the year 2021 [43]. There is no specific vaccine or medicine available to cure AIDS, but there are some natural and synthetic drug candidates available [44,45]. Dolutegravir, sold under the brand name of Tivicay, was the bestselling anti-HIV drug in 2018 [46]. Some other synthetic drugs like zalcitabine [47], zidovudine [48] and emtricitabine [49] terminate the viral DNA chain by inhibiting the reverse transcriptase.
2.2. Hepatitis C Virus (HCV)
This is a blood-borne virus, discovered in 1989, which generally is transmitted in a similar way to HIV [50]. According to the WHO global health survey, hepatitis C generates chronic diseases like liver cirrhosis and jaundice. Till now there is no specific vaccine or medicine available for the treatment of hepatitis C. There are some marketed drugs available for the general treatment of HCV.
Mavyret, which is the composition of glecaprevir and pibrentasvir, was the best-selling anti-HCV drug in 2018 [51]. Asunaprevir, boceprevir and grazoprevir inhibit the proteolytic activity of HCV NS3/4A protease and show promising anti-HCV properties [52,53,54].
2.3. Hepatitis B Virus (HBV)
The existence of this virus was confirmed in the year of 1963; it generally is transmitted through sexual contact, blood transfusion or by bodily fluids [55]. According to the WHO global health survey, HBV causes approximately 780,000 deaths every year. The vaccine that corresponds to HBV is available in the market as a hepatitis B surface antigen (HBsAg) [56]; along with that, there are several other drugs that are also available in the market for the treatment of hepatitis B, with the names entecavir, telbivudine and lamivudine [57,58,59].
2.4. Respiratory Syncytial Virus (RSV)
The World Health Organization (WHO) has reported that RSV causes a significant number of casualties each year, ranging from 66,000 to 199,000 [60]. Moreover, in the year 2005, it was estimated that RSV had infected around 33.8 million children [61,62]. This virus is transmitted through the respiratory systems, by droplets, or from contaminated substances [63].
2.5. Human Cytomegalovirus (HCMV)
HCMV, a member of the herpes virus family, is a prevalent virus that often presents with mild or no symptoms in healthy individuals [64]. Moreover, individuals with weakened immune systems, including newborns, pregnant women and immune compromised individuals can experience severe complications. This infectious virus generally spreads with the help of bodily fluids; it causes serious organ damage, including gastrointestinal problems and colitis [65]. The management of HCMV infection involves the use of antiviral medications which effectively control the virus and alleviate symptoms [66].
2.6. Herpes Simplex Virus (HSV)
Herpes simplex virus (HSV) is a highly contagious virus that causes recurrent infections. The virus is transmitted through direct contact with an infected person’s skin, mucous membranes, or bodily fluids [67]. Although there is no cure for HSV, antiviral medications can help to manage symptoms and reduce the frequency and severity of outbreaks. According to the WHO global health survey (2016), over half a billion people worldwide are estimated to have genital herpes caused by herpes simplex virus type 1 (HSV-1) or type 2 (HSV-2) [68].
2.7. Ebola Virus (EBOV)
The existence of the Ebola virus was first understood in the year of 1976 [69]. The primary mode of transmission for the Ebola virus is through direct contact with infected blood, bodily fluids, or tissues [70]. In the year 2018, WHO documented approximately 11,500 deaths globally attributed to Ebola. However, it is important to note that these figures are not fixed and can fluctuate over time and across different regions. The impact of Ebola outbreaks can vary depending on factors such as healthcare infrastructure, access to resources, and public health interventions. Efforts are continuously underway to improve surveillance and response capabilities and institute preventive measures to minimize the spread of the virus and reduce the number of Ebola-related fatalities.
2.8. Severe Acute Respiratory Syndrome CoV-2 (SARS-CoV-2) Virus
Coronaviruses are positive single-stranded RNA viruses that have an enveloped structure and can infect humans and various animals [71]. In 1965, Tyrrell and Bynoe made a significant contribution to the history of human coronaviruses [72]. They discovered that a virus named B814, obtained from the respiratory tract of an adult with a common cold, could be successfully propagated in human embryonic tracheal organ cultures. This discovery paved the way for further research on coronaviruses and their potential impact on human health [73]. These viruses have a spherical shape, with surface projections resembling the solar corona, hence their name “coronaviruses” (derived from the Latin word “corona”, meaning “crown”). There are four subfamilies of coronaviruses, including alpha, beta, gamma and delta. The alpha and beta variants likely originate from mammals, predominantly bats, while gamma and delta are associated with pigs and birds. Coronaviruses have genome sizes ranging from 26 to 32 kb. Among the seven subtypes of coronaviruses that can infect humans, beta-coronaviruses can lead to severe illness and fatalities, whereas alpha-coronaviruses typically result in mild or asymptomatic infections [74].
2.9. The Human Papillomavirus (HPV)
The human papillomavirus is a common virus that can infect the body’s skin and mucous membranes. It is usually transferred through sexual contact or skin-to-skin contact [75]. According to the WHO report, the consequence of this virus is very much prominent in patients with cervical cancer; the majority of the deaths of such women patients are due to a HPV infection [76].
2.10. Rabies Virus
Rabies virus is a deadly virus that affects the central nervous system of mammals, including humans. It primarily spreads through the saliva of infected animals, usually through a bite. The virus is believed to have originated from bats, but is also found in other animals such as dogs, cats and other wild animals (e.g., fox, raccoon and skunk) [77].
2.11. Zika Virus
The Zika virus is a mosquito-borne virus that was first identified in the Zika Forest of Uganda in 1947 [78]. It remained relatively unknown until a major outbreak occurred in the year 2015 in Brazil, which rapidly spread throughout the Americas and the Caribbean [79].
Most people infected by the Zika virus experience mild symptoms, and the incidence of casualties is also rare, but the viral infection is found to link with birth defects in newborn babies. In most cases, it causes microcephaly, in which the infants are born with abnormally small or underdeveloped brains [80]. The exact number of deaths related to the Zika virus is difficult to determine, as many deaths may have been caused by co-infections or other complications [81].
2.12. The Poliovirus
The poliovirus was first isolated in 1909 by Karl Landsteiner and Erwin Popper; it is a highly contagious virus that primarily affects young children and can lead to paralysis, and even death [82]. It is believed to have originated in ancient times and has been a major public health concern worldwide since the early 20th century [83].
Polio generally is transmitted through contaminated food and water or direct contact with an infected person’s saliva [84]. As per the WHO report, the Global Polio Eradication Initiative has led to an impressive 99% reduction in polio infections. In 2020, only 140 polio cases were found worldwide [85].
2.13. West Nile Virus
West Nile virus (WNV) is a virus that generally enters into humans through the bite of infected mosquitoes. The virus originated in Africa, and was first identified in the West Nile district of Uganda in 1937 [86]. The virus can cause a range of symptoms, from mild flu to more severe neurological problems like meningitis and encephalitis [87].
2.14. The Chickenpox Virus
The virus that corresponds to chickenpox is known as varicella–zoster virus (VZV), which is a highly contagious virus that causes a characteristic itchy rash and fever. The virus mostly spreads through respiratory droplets or direct contact with the fluid from the blisters of infected individuals [88].
2.15. The Influenza Virus
The influenza virus is a highly infectious respiratory virus that can cause mild to severe illness, and even death. It is believed that this virus originated in birds and transmitted to humans through close contact with the infected birds or contaminated surfaces [89]. The severity of the illness varies from a mild fever to severe symptoms, or even death. Globally, this annual epidemic leads to approximately three to five million cases of severe illness each year [90].
2.16. Yellow Fever
Yellow fever virus is a Flavivirus which originated in Africa and is transmitted by the Aedes aegypti mosquito. The virus can cause a wide range of symptoms, from mild flu to hemorrhagic fever [91]. Yellow fever is endemic in tropical regions of Africa and South America, where it affects thousands of people every year. The majority of infections are asymptomatic, but in severe cases, the virus can cause liver damage, kidney failure and death. According to the WHO report, yellow fever still causes an estimated 200,000 cases and 30,000 deaths per year, mostly in the tropical regions where it is endemic [92].
3. Overview of the Antiviral Drugs
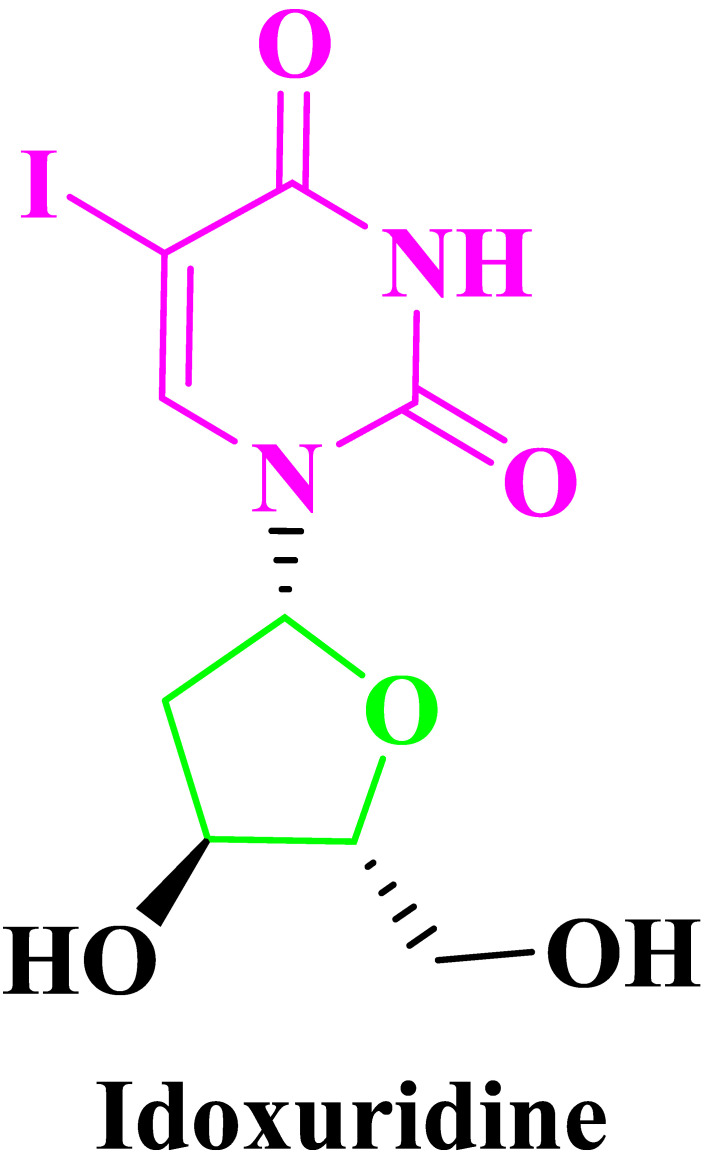
The period of antiviral drugs begins from the year 1959 with the introduction of Idoxuridine (5-iodo-2′-deoxyuridine) (Figure 2), the first antiviral drug (Figure 2), by the American pharmacologist William H. Prusoff for the treatment of HSV keratitis in humans [93,94,95]. This drug was formally approved by FDA in June of 1963; subsequently, different categories of drugs have been discovered and marketed to combat other viral infections [96].
Figure 2.
First FDA-approved antiviral drug Idoxuridine.
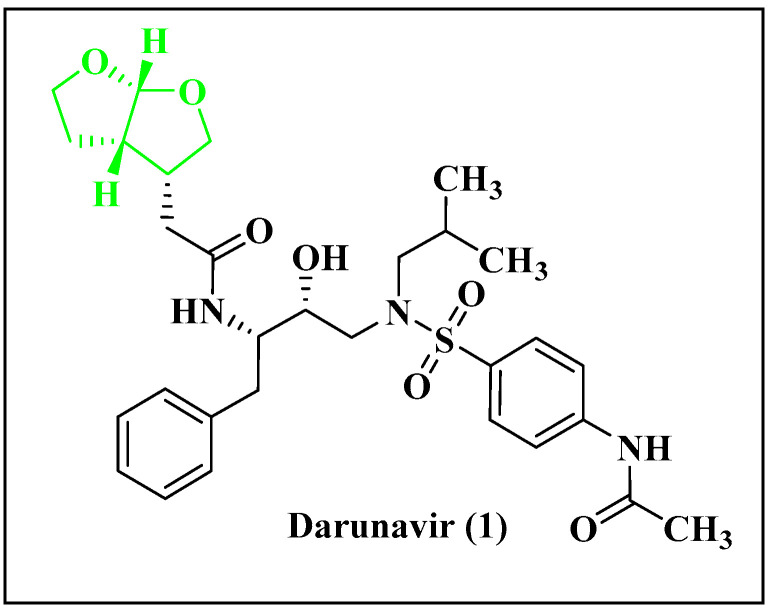
3.1. Representative Antiviral Drug Candidates
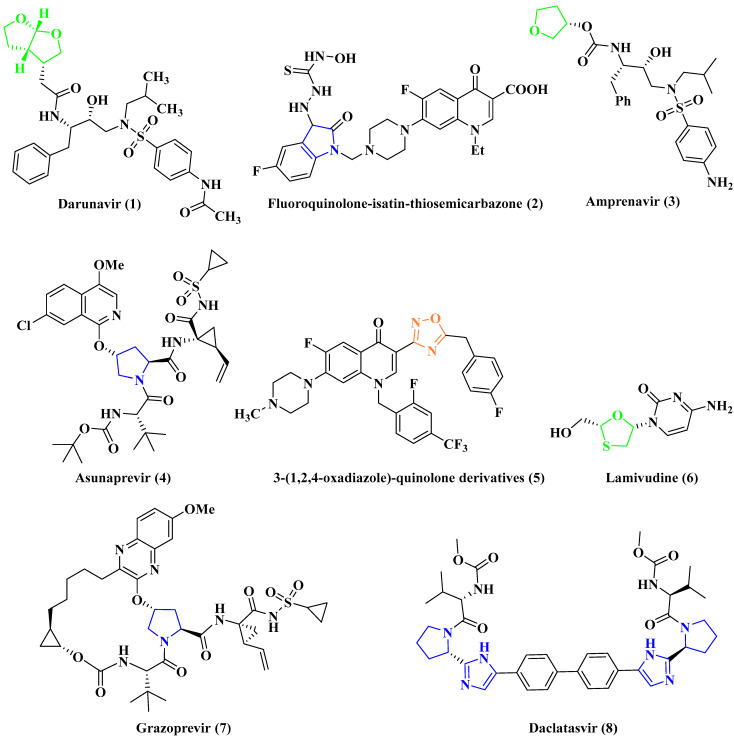
Antiviral drugs (Figure 3) target specific enzymes and proteins involved in the viral life cycle, such as RNA-dependent DNA polymerase, RNA-dependent RNA polymerase, proteases and neuraminidases. RNA-dependent DNA polymerase inhibitors are used for retroviral infections like HIV, while RNA-dependent RNA polymerase inhibitors are efficient against RNA viral infections. Protease inhibitors are effective against viruses that require proteases, and neuraminidase inhibitors treat influenza [97].
Figure 3.
Representative examples of antiviral drug candidates.
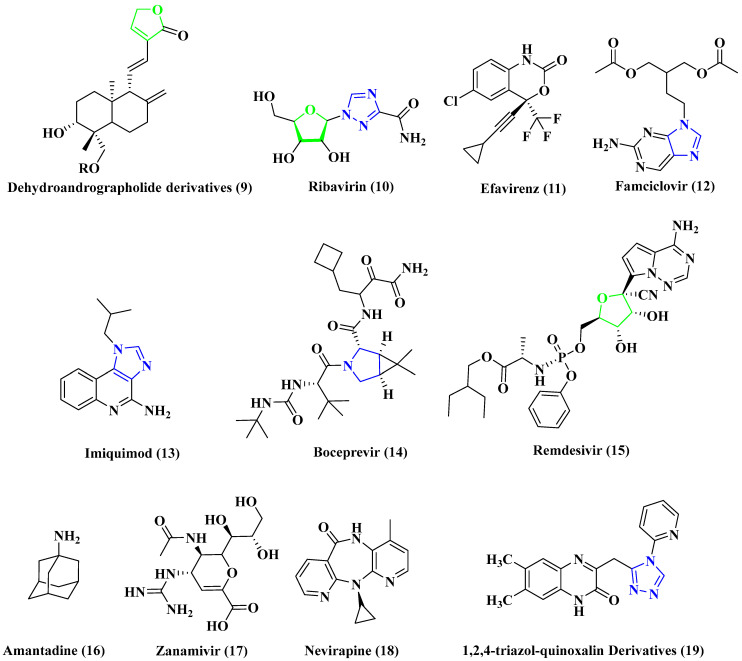
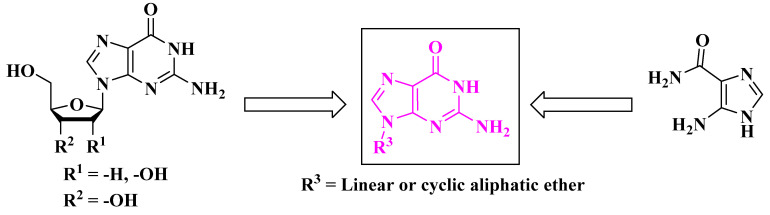
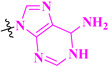
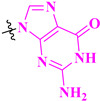
3.2. Antiviral Drugs Containing Nucleoside Subunit
These drugs contain nucleobase/substituted nucleobase and a sugar derivative (Figure 4) having prominent antiviral properties. Arabinosyl nucleoside analogues were isolated initially from sponges [98].
Figure 4.
Representative nucleoside drugs.
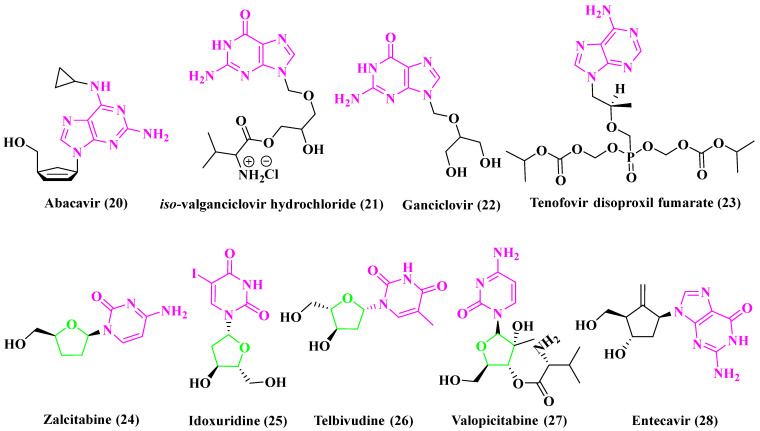
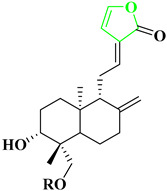
3.3. Examples of Natural Products with Antiviral Properties
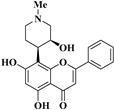
Nature is a continuous source for the provision of different kinds of natural products having excellent biological activities (Figure 5). The alkaloids found in numerous plants and marine algae show important antiviral properties.
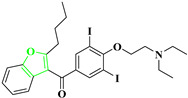
Chalepin (29), from a Ruta angustifolia species plant, shows a good inhibitory effect against HCV [99].
Lamellarin α-20 sulfate (30) is an alkaloid found in marine Lamellarins [100], and is responsible for inhibiting the integration of HIV-1 replication in its very early stages.
Lycogarubins (A, B and C) are isolated from fruit bodies of Myxomycetes Lycogala epidendnrm, and contain two indole groups connected with dimethyl pyrrole-dicarboxylate, in which Lycogarubin C (31) shows activity against HSV [101].
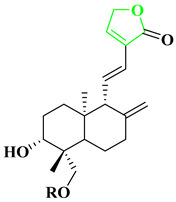
Silvestrol (32), from the bark of the Aglaia foveolate type of plants, contains a substituted dioxane and acts as a potent inhibitor of the Ebola virus [102].
Manassantin B (33), extracted from Saururus chinensis Baill plants, shows inhibitory properties against the Epstein–Barr virus [103].
Harmaline (34) is an indole alkaloid from Peganum harmala, and shows antiviral properties against HSV-1 [104].
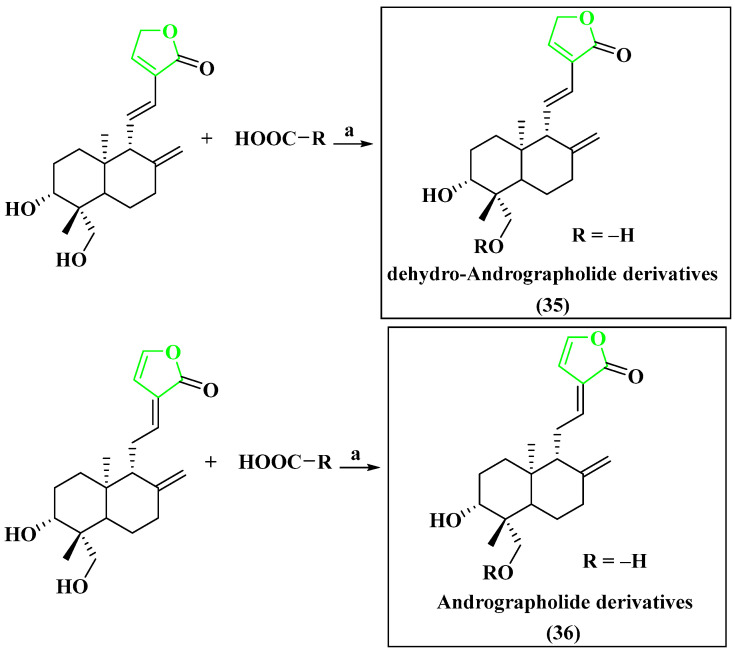
Dehydro-Andrographolide (35) and Andrographolide (36) are two types of natural diterpenoids that have been extracted from Andrographis paniculata. These compounds have demonstrated the ability to inhibit the replication of HBV DNA [105].
(+)-Dehydrod-iconiferyl alcohol (37) that has been isolated from Swertia patens shows inhibitory activities on the secretion of HBsAg, with IC50 value of 1.94 mM [106].
Syringaresinol 4″-O-β-D-glucopyranoside (38), which was extracted from Swertia chirayita, exhibited an inhibitory effect on the secretion of HBsAg, with IC50 values of 1.49 ± 0.033 mM [107].
Figure 5.
Representative natural products having antiviral activities.
4. Importance of Heterocyclic Ring Systems as Antiviral Agents
Nitrogen- and oxygen-containing ring systems offer significant activities as antiviral candidates [108,109,110,111]. These ring systems have either been constructed by linear synthetic steps or could be present from particular starting substrates (like sugar or aza-sugar derivatives). Several research groups have made immense efforts seeking the development of such heterocyclic subunits. Here, the heterocyclic moieties have been screened based on their profound antiviral properties and the corresponding synthetic protocols have been discussed.
5. Synthetic Outlines of Representative Antiviral Drug Candidates
5.1. Anti-HIV Agent
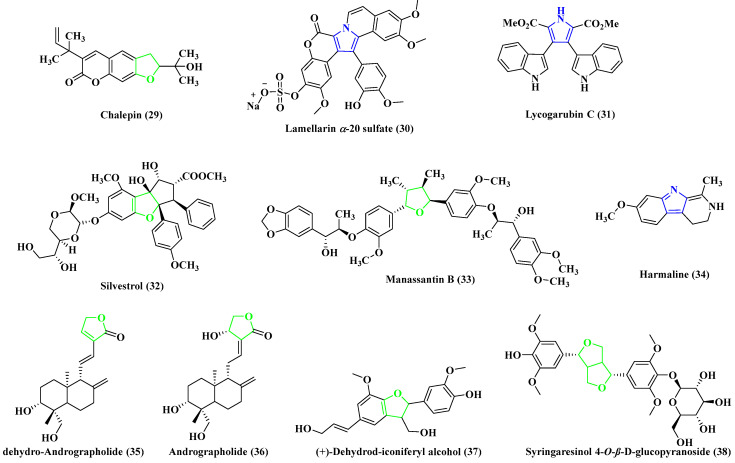
5.1.1. Anti-HIV Agent Darunavir
Kate et al. have demonstrated the synthesis of darunavir (Figure 6), which is considered to be a protease inhibitor [112] and used in low doses for the treatment of HIV. Raltegravir [113] and stavudine [114] are the other available drugs which also show similar properties in this particular domain.
Figure 6.
Chemical structure of darunavir (1).
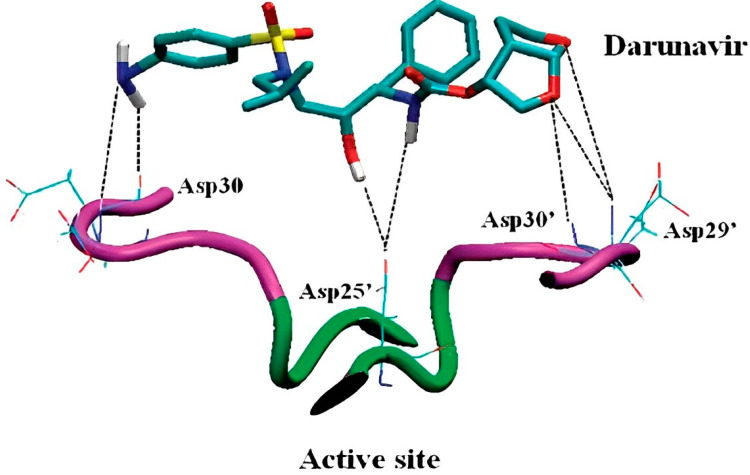
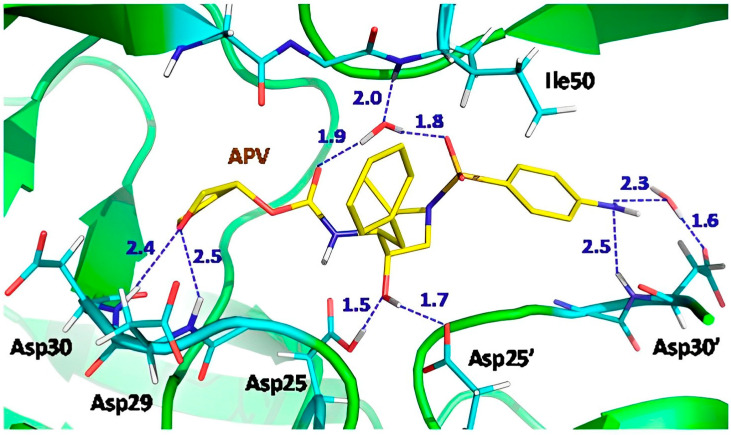
Darunavir becomes stabilized inside the cavity of the enzyme by making a hydrogen bonding interaction through the coordination of the hydroxyl group, 4-amino phenyl and tetrahydrofuran ring system with the active site (Asp25′) or near to the active site (Asp29/29′, Asp30/30′) of the amino acid residues as present in HIV-1 PR (Figure 7) [115].
Figure 7.
The interaction of darunavir with HIV-1 PR.
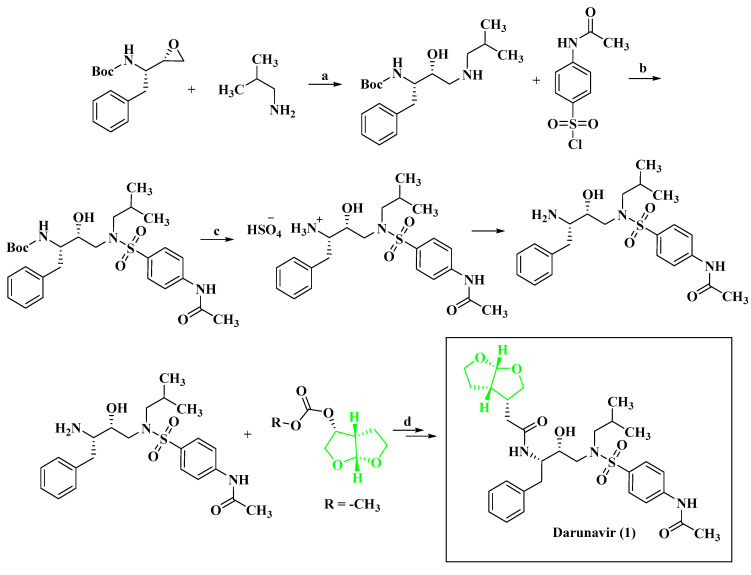
Key synthetic steps for Scheme 1 [116]: (a) ring opening of epoxide with primary amine; (b) N-protected 4-aminobenzenesulfonyl halide; (c) Boc deprotection; and (d) nucleophilic addition followed by separation of the product 1.
Scheme 1.
Synthesis of darunavir.
Reagents and conditions: (a) A mixture of (2S,3S)-1,2-Epoxy-3-(Boc-amino)–4-phenylbutane and isobutyl amine was heated at 65–75 °C and (b) N-acetyl sulphanilyl chloride was added at 5–15 °C to the pre-cooled mixture of (1S,2R)-(1-Benzyl-2-hydroxy-3-(isobutyl-amino) propyl) carbamic acid tert-butyl ester in N, N-dimethylacetamide. Then, triethyl amine was added to the reaction mixture at a temperature below 30 °C and (c) Boc deprotection was done by taking the corresponding carbamic acid tert-butyl ester in isopropyl alcohol at 25–35 °C; after that, aqueous sulphuric acid solution was added to the reaction mixture at 25–35 °C. Then, the amino- N-((2R,3S)-3-amino-2-hydroxy-4-phenylbutyl)-N-isobutylbenzene sulfonamide sulphate salt was treated with potassium carbonate solution in water and 4-Amino-N-((2R,3S)-3-amino–2-hydroxy-4-phenylbutyl)-N–isobutylbenzenesulfonamide was obtained above in water. Then, to a stirred mixture of (d) potassium carbonate, isopropyl acetate and water, 4-amino-N-((2R,3S)-3-amino-2-hydroxy-4-phenylbutyl)-N-isobutyl benzene sulphonamide was added at 25–35 °C, and the reaction mixture was cooled to 15–25 °C; after that, (3R,3aS,6aR)-Hydroxyhexa hydrofuro [2,3-b] furanyl succinimidyl carbonate was added at 15–25 °C. After completion of the reaction, the crude reaction mixture was purified to obtain the final product 1.
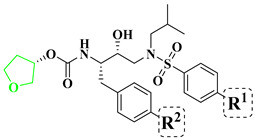
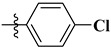
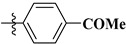
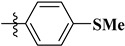
Structure–Activity Relationship of Darunavir: The structure–activity relationship of darunavir analogues is shown in Table 1, in which the incorporation of thiazole and ethyl phosphonate subunit as R1, along with benzo[d][1,3]dioxole moiety as R2, increases its activity significantly [117]. Darunavir and its corresponding synthetic analogues show a distinctive mechanism of action, as characterized by dual functionality. It works as HIV-1 protease inhibitor and also hinders the dimerization process of the HIV-1 protease [118]. Mostly, the Darunavir class of compounds exhibits a binding affinity towards plasma proteins such as alpha-1-acid glycoprotein (AAG or AGP) [119]. The CheckMateTM Mammalian Two-Hybrid System was utilized to establish a dual luciferase assay. This assay was employed to assess the susceptibility of HIV-1LAI to a variety of drugs and evaluate the cytotoxic effects of the drugs.
Table 1.
SAR analysis of darunavir.
| Compound | Substitution | Activity | ||
|---|---|---|---|---|
| −R1 | −R2 | Inhibition Concentration (nM) | Inhibitor Constant (Ki) | |
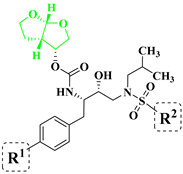
|

|
|
IC90 = 4.1 | 16 pM |

|
|
IC90 = 1.4 | 14 pM | |

|
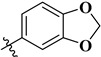
|
IC50 = 0.22 | 14 pM | |
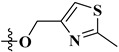
|
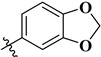
|
IC50 = 0.7 | 15 fM | |
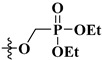
|
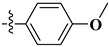
|
IC50 = 1 | 8 pM | |
A 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide assay was employed for determining drug susceptibility and cytotoxicity [120]. The chromogenic substrate Lys-Ala-Arg-Val-Nle-paranitro-Phe-Glu-Ala-Nle-amide was used to determine the kinetic parameters [121].
Mechanism of Action of Darunavir: Darunavir interacts with the protease enzyme of HIV-1 to prevent the dimerization and enhance the catalytic activity. As a result, the cleavage of the proteins is disturbed, and ultimately the replication of the virus is stopped, after the application of this drug to HIV-infected cells [122]. Generally, the interaction takes place with the primary chains of Asp-29 and Asp-30 amino acids present in the active site of the protease enzyme.
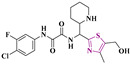
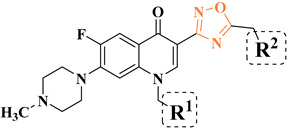
5.1.2. Anti-HIV Agent Fluoroquinolone-Isatin-Thiosemicarbazone Hybrids
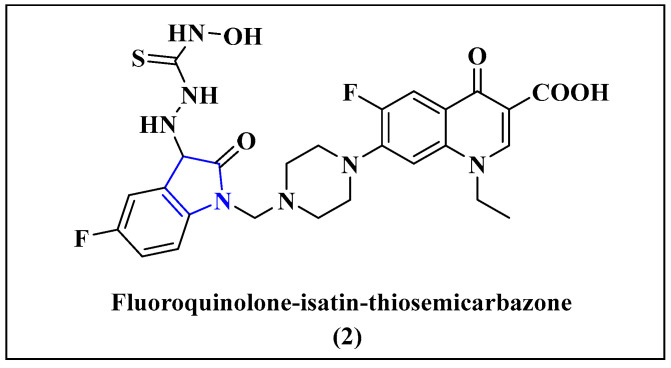
The molecular-hybrid approach was introduced to understand the synergistic effects of the two compounds in order to generate a new structural entity with superior properties [123] for inhibiting the viral replication. Isatin derivatives have been shown to exhibit antiviral activity against a range of viruses, including HIV-1. Recently, hybrid fluoroquinolone-isatin derivatives have attracted attention due to their promising anti-HIV properties (Figure 8) [124].
Figure 8.
Fluoroquinolone-isatin-thiosemicarbazone hybrid (2), a potential anti-HIV agent.
Key synthetic steps for Scheme 2 [125]: (a) A solution of N-hydroxylamine in absolute ethanol was added to potassium hydroxide and carbon disulphide, and the mixture was stirred at 0−5 °C to form the corresponding potassium salt of dithiocarbamates; (b) hydrazine hydrate was added to the reaction mixture and stirred at 80 °C; after completion of the reaction, it was cooled to 0 °C to obtain the corresponding thiosemicarbazide; (c) to a hot dispersion of thiosemicarbazide in ethanol was added an equimolar aqueous solution of sodium acetate, and to this solution a further equimolar ethanolic solution of 5-F-isatin was added, and the mixture was stirred while being heated on a hot plate for 4−15 min. The resultant precipitate was filtered off and dried. The product was recrystallized from 95% ethanol; (d) the N-Mannich bases were further synthesized by condensing the acidic imino group of isatin derivatives with formaldehyde and secondary amine (4-ethyl-7-fluoro-1-oxo-6-(piperazin-1-yl)-1,4-dihydronaphthalene-2-carboxylic acid) by irradiating the reaction vessel in a microwave reactor for 3−15 min at 455 W, followed by purification to obtain the corresponding product 2.
Scheme 2.
Synthesis of fluoroquinolone-isatin-thiosemicarbazone hybrid.
Reagents and conditions: (a) CS2, KOH, C2H5OH, 0−5 °C; (b) NH2NH2.H2O, 80 °C, conc. HCl; (c) 5-F-Isatin, CH3COONa; (d) 30% HCHO, 455 W, 3−15 min.
Mechanism of Action of Fluoroquinolone-isatin-thiosemicarbazone: Isatinyl thiosemicarbazone derivatives have been found to exhibit anti-HIV activity by hindering the viral protease enzyme’s function. The viral protease enzyme plays a pivotal role in the maturation of the HIV virion by interrupting its activity; as a result, the production of the corresponding infectious virions stops. Isatinyl thiosemicarbazone derivatives interact with the active site of the viral protease enzyme, and hence its activity is stopped [126,127].
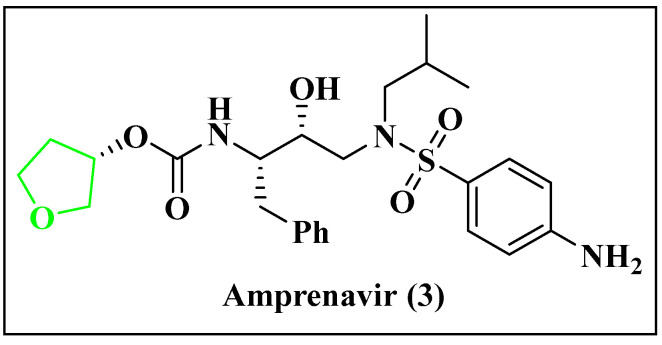
5.1.3. Anti-HIV Agent Amprenavir
The drug amprenavir (Figure 9) is primarily used to treat HIV infections; it acts as a protease inhibitor. It binds to the active site of the enzyme and inhibits its activity. It prevents the cleavage of viral polyproteins, which leads to the development of immature non-infectious viruses [128]. Amprenavir’s hydroxyl group interacts with Asp25 and Asp25′ residues of the protein at the catalytic site. Along with that, there are stable H-bonding interactions between the hydroxyl group of the drug with the catalytic site of the aspartic acid side chains (Figure 10) [129].
Figure 9.
Chemical structure of amprenavir (3).
Figure 10.
H-bonds and water-mediated interactions formed by amprenavir with the active site.
Key synthetic steps for Scheme 3 [130]: (a) Formation of chalcone by the reaction of 2-phenylacetaldehyde and Ph3PCHCO2Et at 90 °C in toluene; (b) reduction of the ester by lithium aluminium hydride and AlCl3 in diethyl ether; (c) chiral epoxidation; (d) epoxide ring opening, followed by (e) epoxide ring closing and further(f) ring opening; and formation of gem-diol derivatives which formed product 3 by reacting with (g) isobutyl amine and (h) N-hydroxysuccinimidyl carbonate of (S)-3-hydroxytetrahydrofuran.
Scheme 3.
Synthesis of amprenavir.
Reagents and conditions: (a) Ph3PCHCO2Et, PhH, 90 °C; (b) LiAlH4, AlCl3 (30 mol %), Et2O, 0 °C; (c) mCPBA, CH2Cl2, 0 °C; (d) Ti(OiPr)4, TMSN3, C6H6, 70 °C; (e) p-TsCl, Bu2SnO (2 mol %), Et3N, DMAP (10 mol %), CH2Cl2, 0 °C; (f) K2CO3, MeOH, 0 °C; (g) (S,S)-Co(salen)OAc (0.5 mol %), THF, H2O (0.5 equiv), 25 °C; (h) (1) iBuNH2, iPrOH, 50 °C, (2) PPh3, H2O, THF, 25 °C; (2) N-hydroxysuccinimidyl carbonate of (S)-3-hydroxytetrahydrofuran, Et3N, CH2Cl2, 25 °C.
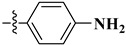
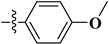
Structure–Activity Relationship of Amprenavir: It shows antiviral properties against the HIV-1 virus in an in vitro study against the C8166 cell line [131]. The efficacy of HIV-1 protease inhibitors was assessed using the fluorescence resonance energy transfer (FRET) technique. A specific protease substrate [Arg-Glu(EDANS)-Ser-Gln-Asn-Tyr-Pro-Ile-Val-Gln-Lys(DABCYL)-Arg], was employed. The determination of the inhibitor’s binding dissociation constant (Ki) involved fitting the initial velocity plot against inhibitor concentrations to the Morrison equation through non-linear regression analysis [132]. The EC50 values were compared with those of amprenavir, resulting in the conclusion that the biaryl subunit with varying substituents showed lower efficiency. However, compounds that featured substituents of –NH2 for R1 and 3-pyridyl or 4-pyridyl for R2 exhibited increased solubility and stronger enzyme inhibitory activity at a sub-nanomolar level. These compounds were found to be 2–10 times more active than amprenavir, as described in Table 2 [133].
Table 2.
SAR analysis of amprenavir.
| Compound | Substitution | Activity | ||
|---|---|---|---|---|
| −R1 | −R2 | EC50 (nM) | Inhibitor Constant (Ki) (nM) | |
|

|

|
2.93 | 0.84 |

|

|
4.29 | 5.8 | |

|
|
2.32 | 6.4 | |

|
|
6.89 | 5.8 | |

|
|
6.04 | 7.4 | |

|
|
3.63 | 5.2 | |

|
|
5.53 | 1.8 | |

|
|
4.30 | 1.9 | |

|

|
3.46 | 4.3 | |

|
|
9.2 | 1.6 | |

|

|
4.48 | 8.1 | |

|

|
3.08 | 3.5 | |

|
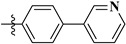
|
2.68 | 1.6 | |

|
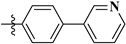
|
2.25 | 3.8 | |

|

|
0.10 | 1.95 | |

|
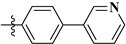
|
0.10 | 0.33 | |

|
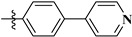
|
2.93 | 0.086 | |
Mechanism of Action of Amprenavir: Amprenavir binds to the active site of the protease and inhibits the activity of the enzyme. This inhibition prevents the cleavage of the gag-pol polyprotein. Amprenavir competes with the natural substrate of the viral protease enzyme, which is a precursor protein of the viral genome. This competition leads to the formation of a stable complex between the drug and the enzyme, preventing the enzyme from cleaving the protein. As a result, non-infectious viral particles are produced, leading to a reduction in the number of viral particles in the body [134]. In Table 3 other marketed anti-HIV drugs are listed with their mechanism of action, ways of use and side effects.
Table 3.
Anti-HIV drugs.
| Sl. No. | Drug Name | Drug Target | Mechanism of Action | Ways of Use | Side Effect | Brand Name |
|---|---|---|---|---|---|---|
| 1. | Zalcitabine [135] | Reverse transcriptase/RNase H (Human immunodeficiency virus 1) |
Inhibiting reverse transcriptase and terminating the viral DNA chain | Oral | Liver failure, inflammation of the pancreas | Hivid |
| 2. | Amprenavir [136] | Human immunodeficiency virus type 1 protease | Blocks the active site of HIV protease to prevent cleavage of the viral precursor proteins |
Oral | Diarrhea, kidney failure, weakness |
Agenerase |
| 3. | Maraviroc [137] | C-C chemokine receptor type 5 |
Blocks GP120-CCR5 interaction to inhibit HIV entry |
Oral | Liver problems, nausea, allergic reactions | Selzentry |
| 4. | Tenofovir disoproxil Fumarate [138] |
Reverse transcriptase/RNaseH (Human immunodeficiency virus 1) |
Competes with dATP and inhibits the activity of HIV RT | Oral | Trouble sleeping, dizziness, diarrhea | Viread |
| 5. | Emtricitabine [139] | Reverse transcriptase/RNase H (Human immunodeficiency virus 1) |
Through nucleoside reverse transcriptase inhibition | Oral | Body aches, ough, diarrhea, fever |
Truvada |
| 6. | Cabotegravir [140] | Integrase (Human immunodeficiency virus 1) |
By HIV-1 integrase inhibition | Oral | Abnormal dreams, dark urine, difficulty in breathing |
Vocabria |
| 7. | Lenacapavir [141] | Gag-Pol polyprotein |
Lenacapavir works by blocking the HIV-1 virus’ protein shell (the capsid), thereby interfering with multiple essential steps of the viral lifecycle | Oral/subcutaneous injection |
Nausea |
Sunlenca |
Some other synthesized compounds that show activity against HIV are given in Table 4.
Table 4.
Synthesized anti-HIV compounds.
| Sl. No. | Antiviral Agent | Drug Target | Activity |
|---|---|---|---|
| 1. |
|
HIV [142] | Methylthiazole derivatives effectively inhibit HIV-1 entry into cells, demonstrating low micromolar potency (IC50 = 1.6 µM) and a favorable selectivity index (SI) in both single-cycle TZM-bl cell assays and multicycle MT-2 cell assays. |
| 2. |
|
HIV-1 and HIV-2 [143] |
3″-alkenyl-substituted TSAO derivatives exhibit anti-HIV-1 and anti-HIV-2 activity at subtoxic concentrations against HIV-2 RT involved the RNA-dependent DNA polymerase assay with EC50(HIV-1MT-4) = 0.06 ± 0.03 µM and EC50(HIV-2MT-4) >10 µM. |
| 3. |
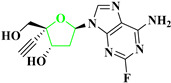
|
HIV [144] | 4′-ethynyl-2-fluoro-2′-deoxyadenosine demonstrates exceptional potency in inhibiting HIV-1 replication in phytohemagglutinin-activated peripheral blood mononuclear cells with EC50(HIV-1NL4-3) = 50 pM. |
| 4. |
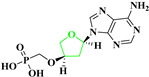
|
HIV-1 [145] | Deoxythreosyl phosphonate nucleosides exhibit potent anti-HIV-1 activity (EC50(HIV-1) = 2.53 μM) by binding effectively to the active site pocket of HIV-1 reverse transcriptase. These compounds show no cytotoxicity, even at high concentrations (CC50 > 316 µM). The incorporation kinetics of these compounds into DNA were studied using their diphosphate form as a substrate and HIV-1 reverse transcriptase as the catalyst. |
| 5. |
|
HIV-1 [146] | Flavopiridol, a cyclin-dependent kinase (CDK) inhibitor, blocks HIV-1 Tat transactivation and viral replication by inhibiting P-TEFb kinase activity. The cytotoxicity of Flavopiridol and its analogues was evaluated using an MTT-based cell viability assay, demonstrating their potential as anti-HIV-1 therapeutics with EC50 = 7.4 nM. |
5.2. Anti-HCV Agent
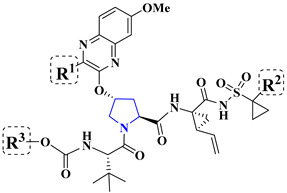
5.2.1. Anti-HCV Agent Asunaprevir
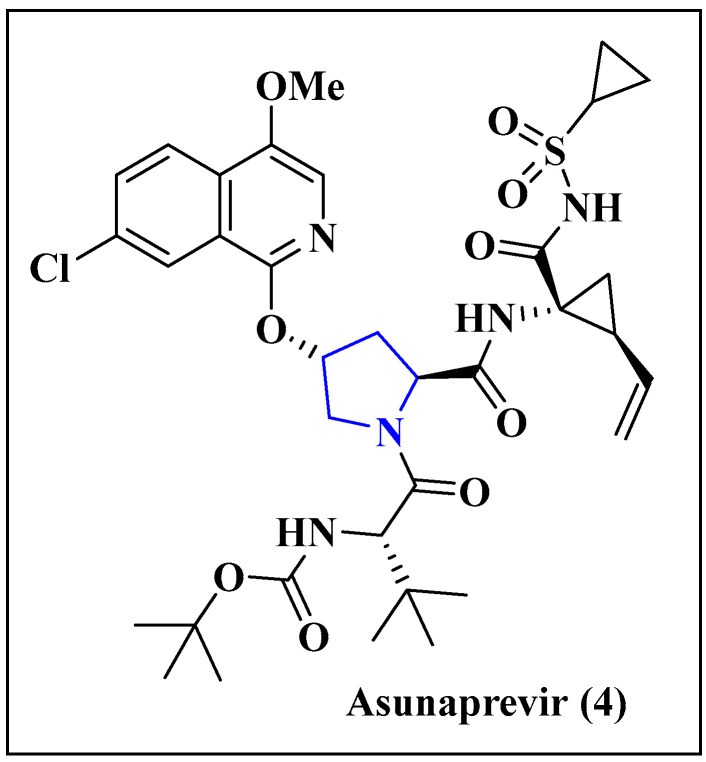
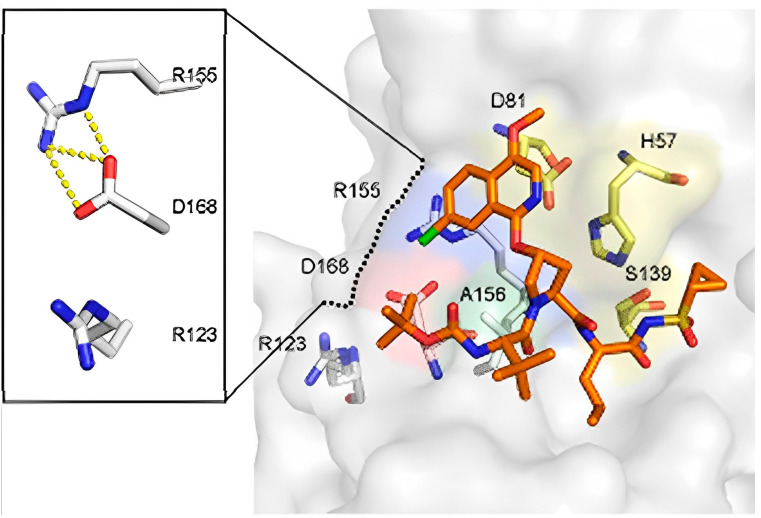
Asunaprevir (Figure 11) is an orally efficacious NS3 protease inhibitor used for the treatment of hepatitis C virus infection. This tripeptidic acyl sulfonamide is an inhibitor of the enzyme NS3/4A, and is now in phase III clinical trials for the treatment of hepatitis C virus infection. The activity of asunaprevir showed a robust antiviral response in early clinical trials. Suzuki et al. have studied the antiviral activity and toxicological profile of asunaprevir [147]. It inhibits the activity of proteases by binding to the active site. Viral polyproteins cannot be cleaved by this inhibition, which produces undeveloped and non-infectious viral particles (Figure 12) [148].
Figure 11.
Chemical structure of asunaprevir (4).
Figure 12.
Structure of HCV NS3/4A protease in complex with asunaprevir.
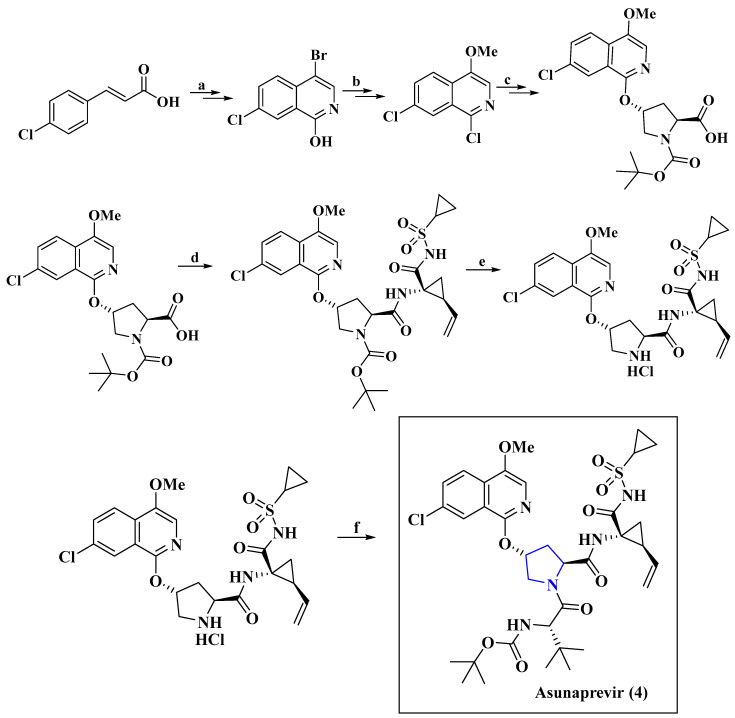
Key synthetic steps for the Scheme 4 [149]: (a,b) (E)-3-(4-chlorophenyl)acrylic acid is cyclized, and the derivatization (c) reacts with N-Boc-3-(R)-hydroxy-L-proline via nucleophilic addition (d) by peptide coupling reaction. The synthesized fragment reacts with (1R,2S)-1-amino-N-(cyclopropylsulfonyl)-2-vinylcyclopropanecarboxamide (TsOH salt), followed by (e) deprotection of proline nitrogen. (f) The final product 4 was obtained by the peptide coupling reaction with N-Boc-t-butyl-L-glycine.
Scheme 4.
Synthesis of anti-HCV agent asunaprevir.
Reagents and conditions: (a) (i) DPPA, Et3N, benzene, rt; (ii) Ph2CH2, reflux; (iii) NBS, MeCN, reflux. (b) (i) POCl3, reflux; (ii) (1) n-Bu-Li, THF, −78 °C, (2) (i-PrO)3B, −78 °C; (3) 50% H2O2, Na2SO3 −78 °C; (iii) MeOH, MeCN, TMSCHN2, 0 °C–rt. (c) N-Boc-3-(R)-hydroxy-L-proline, t-BuOK, DMSO, 10 °C. (d) HATU, Hunig’s base i-Pr2Net, (1R,2S)-1-amino-N-(cyclopropylsulfonyl)-2-vinylcyclopropanecarboxamide (TsOH salt), rt; (e) HCl (conc.), MeOH, reflux; (f) HATU, Hunig’s base, N-Boc-t-butyl-L-glycine, DCM, 0 °C–rt.
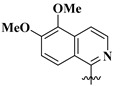
Structure–Activity Relationship of Asunaprevir: The structure-activity relationship studies show that the incorporation of a hydroxyl group at the R1 position decreases its antiviral activity (Table 5). The isoquinoline series with methoxy and chlorinated analogues proved to be potent inhibitors of the NS3/4A protease (GT-1a NS3/4A enzyme) which extended to excellent inhibitory activity in the replicon at the R2 substituent. The antiviral activity of the drug was evaluated through a two-part study. Initially, a single ascending dose (SAD) study was conducted in patients infected with genotype 1, followed by a subsequent multiple ascending dose (MAD) study [149].
Table 5.
SAR analysis of asunaprevir derivatives.
| Compound | Substitution | Activity | |||
|---|---|---|---|---|---|
| −R1 | −R2 | −R3 | −R4 | IC50 (nM) | |
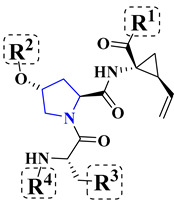
|

|

|

|

|
2 |

|

|

|

|
247 | |

|

|

|

|
2 | |

|

|

|
|
4 | |

|
|

|

|
4 | |

|

|

|

|
2 | |

|

|

|

|
7 | |

|

|

|

|
1 | |

|
|

|

|
7 | |

|
|

|

|
2 | |
Mechanism of Action of Asunaprevir: Asunaprevir is highly active against HCV NS3 protease [150], which is responsible for processing the HCV polyprotein into individual viral proteins. The production of new viral proteins is prevented with the use of this drug compound, and as a result, the progression of HCV-related liver disease is reduced. It is typically used in combination with other antiviral drugs to enhance efficacy and minimize drug resistance [52].
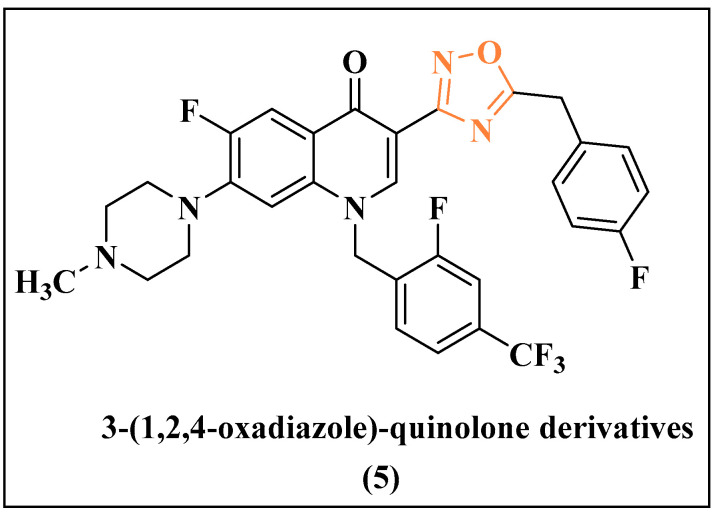
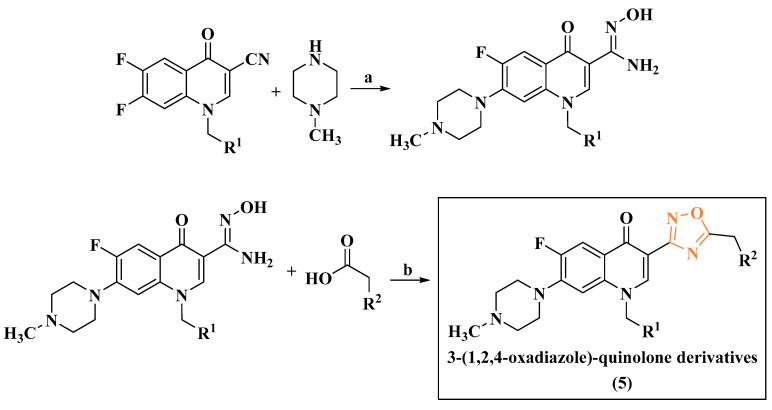
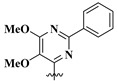
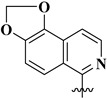
5.2.2. Anti-HCV Agent 3-(1,2,4-oxadiazole)-quinolone
Studies have shown that 3-heterocyclic quinolones (Figure 13) can inhibit NS5B polymerase activity by binding to an allosteric site. This binding triggers a change in the protein’s structure, resulting in the inhibition of RNA replication. In vitro and in vivo studies have demonstrated the significant antiviral activity of these compounds against HCV and indicated their roles as promising lead candidates for further development [151].
Figure 13.
3-(1,2,4-oxadiazole)-quinolone derivative (5) with anti-HCV activities.
Key synthetic steps for Scheme 5 [151]: (a) The nitrile moiety of quinolone is converted to the intermediate hydroxyamidine through reaction with hydroxyl amine; (b) the resulting hydroxyamidine intermediates are converted to a variety of 1,2,4-oxadiazole target compounds by reacting with appropriate carboxylic acids to obtain product 5.
Scheme 5.
Synthesis of 3-(1,2,4-oxadiazole)-quinolone derivatives.
Reagents and conditions: (a) CH3CN, reflux (b) NH2OH, DIEA, aq. EtOH; (c) HBTU, DIPEA, 200 °C, microwave.
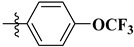
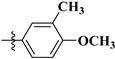
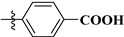
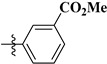
Structure–Activity Relationship of 3-(1,2,4-oxadiazole)-quinolone derivatives: The activity (IC50) against the NS5B polymerase enzyme (Table 6) was determined by scintillation proximity assays (SPA) [152]. For a high-throughput screening (HTS) campaign to identify inhibitors of NS5B polymerase, a scintillation proximity assay (SPA) format was employed. Scintillation proximity assays (SPAs) are an efficient technique that can be used to detect enzymes, receptors, radioimmunoassays and molecular interac-tions. This assay format allowed for the screening of compounds that effectively inhibited the enzymatic function of NS5B polymerase, specifically targeting the wild-type (genotype 1b) enzyme. The IC50 values of the compounds were assessed against NS5B polymerase, and their efficacy was determined in using a cell-based viral replication surrogate assay called the replicon system [152]. R1 and R2 mainly stabilize the compounds in the hydrophobic pockets. The inhibition activity of these two functionalities present in the quinolone moiety is shown in Table 6 [153]. It is clearly found that the presence of the –F or –CF3 group in either R1 or R2 is very much responsible for modulating the corresponding activity [153].
Table 6.
SAR analysis of 3-(1,2,4-oxadiazole)-quinolone derivatives.
| Compound | Ubstitution | Activity | |
|---|---|---|---|
|
−R1 | −R2 | IC50 (μM) |
| 4-Cl-C6H4 | 4-F4-C6H4 | 0.019 | |
| 4-Cl-C6H4 | 2,4-DiF-C6H3 | 0.075 | |
| 4-CF3-C6H4 | C6H5 | 0.024 | |
| 2-F,4-CF3-C6H3 | C6H5 | 0.014 | |
| 2-F,4-CF3-C6H3 | 4-F4-C6H4 | 0.015 | |
Mechanism of Action of 3-(1,2,4-oxadiazole)-quinolone derivatives: 3-(1,2,4-oxadiazole)-quinolone derivatives show promising inhibitory activity against HCV NS5B polymerase and NS3 protease. Cyclophilin, a protein present in the host cell of HCV, also is affected by the interaction of such heterocyclic compounds; consequently, the replication process of this virus becomes affected. By targeting multiple stages of the HCV life-cycle, these compounds can reduce the amount of virus and slow or stop the progression of HCV-related liver diseases [154].
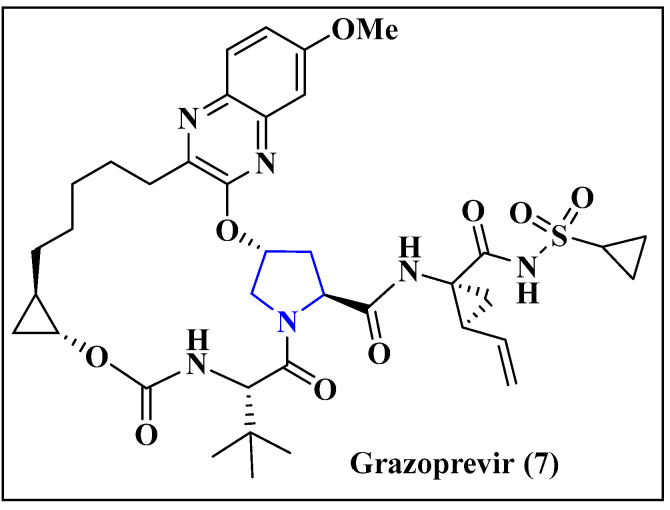
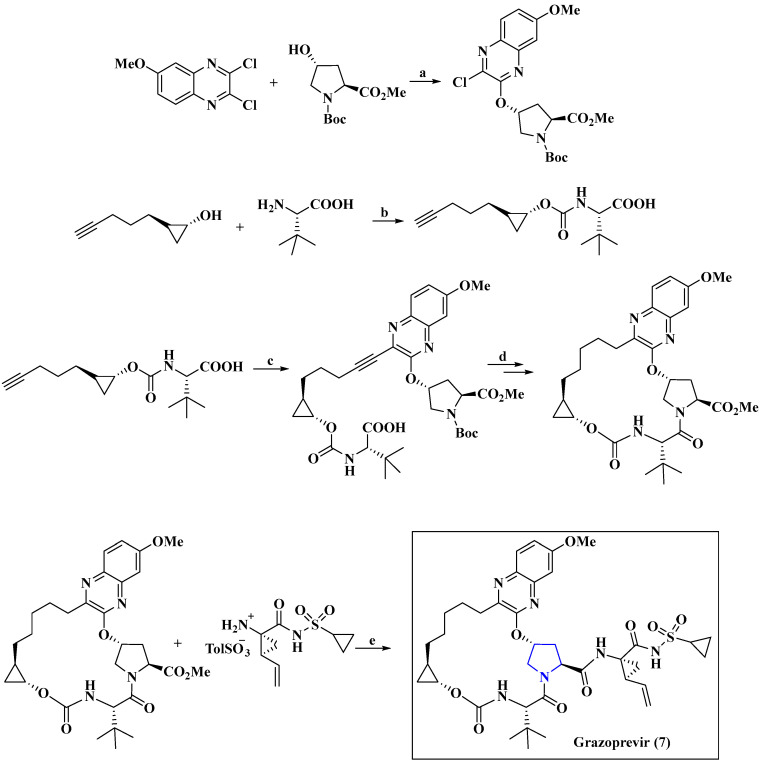
5.2.3. Anti-HCV Agent Grazoprevir
Grazoprevir (Figure 14) is a potent inhibitor of RNA synthesis in HCV (due to the action of two different DAAs as NS5A and NS3/4A inhibitors), representing high genetic barriers to resistance. The mechanism of action and pharmacodynamic properties, as well as the pharmacokinetics, clinical uses, safety and efficacy of elbasvir/grazoprevir in managing a large variety of conditions, including cases in the presence of cirrhosis, co-infection with HIV and patients having inherited blood disorders, were nicely reviewed by Kassas et al. [155]. Sofosbuvir [156], ledipasvir [157] and telaprevir [158] are the reported anti-HCV drugs with similar synthetic procedures.
Figure 14.
Chemical structure of grazoprevir (7).
Key synthetic steps for Scheme 6 [159]: Grazoprevir was synthesized starting from the (a) cross coupling strategy of 2,3-dichloro-6-methoxyquinoxaline with substituted proline derivative to obtain the corresponding five membered heterocyclic core followed by (b) esterification of the (1R,2R)-2-(pent-4-yn-1-yl)cyclopropan-1-ol with (S)-2-amino-3,3-dimethylbutanoic acid and (c) metal catalyzed coupling reactions of the fragments, followed by (d) cyclization through intramolecular peptide coupling (e). The final product 7 was obtained by the peptide coupling with the allylic sulfonamide, as shown in Scheme 6.
Scheme 6.
Synthesis of grazoprevir.
Reagents and conditions: (a) DBU (1.05 equiv.), DMAc, 50 °C; (b) CDI, Hunig’s base, 95 °C, 2.5 h; (c) Pb(OAc)2, P(t-Bu)3BF4, K2CO3, CPME/MeCN; (d) (1) Pd/C, H2, IPAc/MeOH; (2) (i) PhSO3H, (ii) HATU, NEt3, MeCN; (e) DEC, pyridine, MeCN.
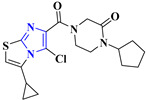
Structure–Activity Relationship of Grazoprevir: A group of linear HCV NS3/4A protease inhibitors was created by removing the macrocyclic linker found in grazoprevir. This allows for the exploration of diverse quinoxalines while conferring conformational flexibility. Inhibitors with small substituents at the 3-position (R1) of quinoxaline were found to be effective in maintaining potency. The 3-chloroquinoxaline demonstrated outstanding potency against wild-type HCV NS3/4A protease. Replacing the cyclopropyl-sulfonamide with a more hydrophobic 1-methyl cyclopropyl-sulfonamide group (R2) generally enhances the potency of the resulting analogues. Similarly, substituting the tert-butyl group (R3) with a bulkier cyclopentyl moiety led to the development of compounds with improved potency (Table 7) [160]. The enzyme inhibition constants (Ki) were determined for the wild-type genotype 1a NS3/4A protease, as well as the resistant variants R155K and D168A. Additionally, a subset of compounds underwent testing to determine their cellular antiviral potencies (EC50) using replicon-based antiviral assays. These assays, which assessed the efficacy of the compounds, were not only run against the wild-type HCV strain but also against the drug-resistant variants R155K, A156T, D168A, and D168V [161].
Table 7.
SAR Analysis of grazoprevir derivatives.
| Compound | Substitution | Activity | |||
|---|---|---|---|---|---|
| −R1 | −R2 | −R3 | EC50 (nM) | Inhibitor Constant (Ki) (nM) | |
|

|

|

|
24 | 19 ± 2.7 |

|

|

|
6.6 | 7.8 ± 1.1 | |

|

|

|
6.3 | 6.1 ± 1.1 | |

|

|

|
10 | 9.2 ± 0.9 | |

|

|

|
4.5 | 7.1 ± 1.1 | |

|

|

|
3.1 | 3.9 ± 0.7 | |
Mechanism of Action of Grazoprevir: Grazoprevir is a potent and selective inhibitor of the NS3/4A protease enzyme in the hepatitis C virus (HCV). The NS3/4A protease enzyme plays a critical role in HCV replication by cleaving the HCV polyprotein into the individual functional proteins necessary for the virus to replicate and propagate. Grazoprevir’s mechanism of action has been extensively studied and documented. Grazoprevir effectively inhibited the NS3/4A protease enzyme by binding to the enzyme’s active site, thereby preventing the cleavage of the HCV polyprotein and inhibiting HCV replication [162]. There are other drugs available on the market for the treatment of HCV, such as boceprevir, sofosbuvir, etc. Their mechanisms of action, ways of use and side effects are given in Table 8.
Table 8.
Anti-HCV drugs.
| Sl. No. | Drug Name | Drug Target | Mechanism of Action | Ways of Use | Side Effect | Brand Name |
|---|---|---|---|---|---|---|
| 1. | Asunaprevir [147] | Genome polyprotein (Hepatitis C virus genotype 1b) |
Inhibits the proteolytic activity of HCV NS3/4A protease | Oral | Flu-like symptoms, skin rash, irritability, headache | Sunvepra |
| 2. | Boceprevir [163] | NS3/4A protein (Hepatitis C Virus) |
Inhibits the proteolytic activity of HCV NS3/4A protease | Oral | Vomiting, dry skin, fever, sore throat | Victrelis |
| 3. | Grazoprevir [164] |
NS3/4A protein (Hepatitis C Virus) |
Inhibits the proteolytic activity of HCV NS3/4A protease | Oral | Headache, nausea, trouble breathing | Zepatier |
| 4. | Sofosbuvir [165] | RNA-dependent RNA-polymerase (Hepatitis C Virus) |
Inhibits RNA-dependent RNA polymerases of HCV NS5B (non-structural protein 5B) | Oral | Fatigue, headache, decreased appetite | Vosevi |
| 5. | Daclatasvir [166] | Nonstructural protein 5A (Hepatitis C Virus) |
Disrupts the NS5A proteins that have undergone hyperphosphorylation; interferes with the functioning of newly formed HCV replication complexes. | Oral | Headache, feeling tired, nausea | Daklinza |
Some other synthesized compounds that show activity against HCV are given in Table 9.
Table 9.
Synthesized anti-HCV compounds.
| Sl. No. | Antiviral Agent | Drug Target | Activity |
|---|---|---|---|
| 1. |
|
Hepatitis C Virus (HCV) [167] | The fatty acid synthase inhibitors showed good antiviral activity in a cell-based HCV replicon assay and an acceptable selectivity index. Their observed cell permeability in an MDCK permeability assay supports these findings. The antiviral activities align with the biochemical inhibition (IC50 values > 30 μM) of Hfasn [168]. |
| 2. |

|
HCV [169] | Imidazo[2,1-b]thiazole targets HCV NS4B, specifically the second amphipathic α helix (4BAH2). The effectiveness of the compound against Huh-7 cells was assessed, screening an EC50 value of 18 nM [170]. |
| 3. |
|
HCV [171] | The efficacy of the compound against Huh-7 cells shows promising activity, which reflects in the EC50 value (16 nM). |
5.3. Anti-HBV Agent
5.3.1. Anti-HBV Agent Lamivudine
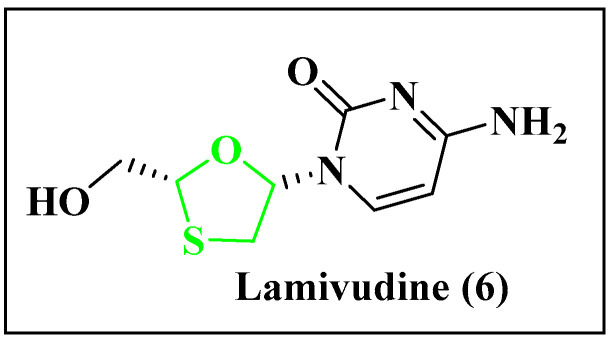
Lamivudine (Figure 15) is a nucleoside reverse transcriptase inhibitor that inhibits the reverse transcriptase of the human hepatitis B virus (HBV). It is a safe medicine with minimal side effects and can be prescribed for pregnant women and children over five years of age [172].
Figure 15.
Chemical structure of lamivudine (6).
Key synthetic steps for Scheme 7 [173,174]: Formation of mixture of diastereomer at 0 °C (b) separation of diastereomers is done by recrystallization, (c) diastereo pure compound is treated with methanolic K2CO3 to obtain product 6.
Scheme 7.
Synthesis of anti-HBV agent lamivudine.
Reagents and conditions: (a) Reactants are mixed and cooled to 0 °C in MeOH; (b) separation of diastereomers; (c) MeOH, K2CO3.
Mechanism of Action of Lamivudine: Lamivudine is a nucleoside analogue that is used in the treatment of hepatitis B virus (HBV) infection. The mechanism of action of lamivudine is based on its ability to inhibit HBV reverse transcriptase, which is a critical enzyme for viral replication. Once inside the infected cell, lamivudine is phosphorylated by cellular enzymes into its active triphosphate form. This active form of lamivudine competes with the natural nucleotide building blocks for incorporation into the growing viral DNA chain. However, lamivudine lacks the 3′-OH group required for further chain extension, thereby resulting in the termination of viral DNA synthesis [175].
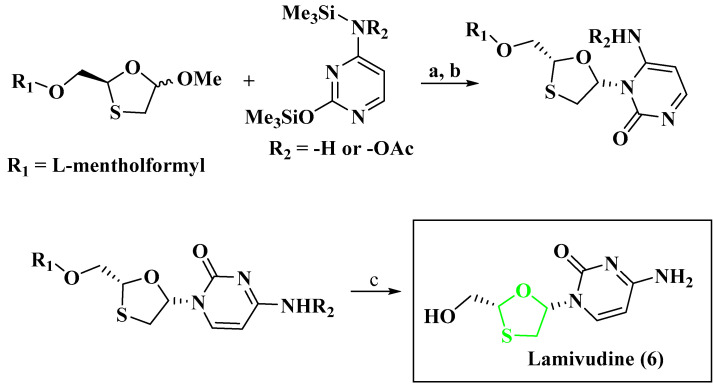
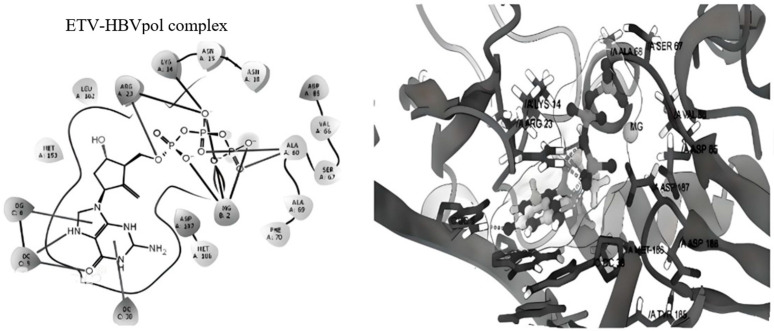
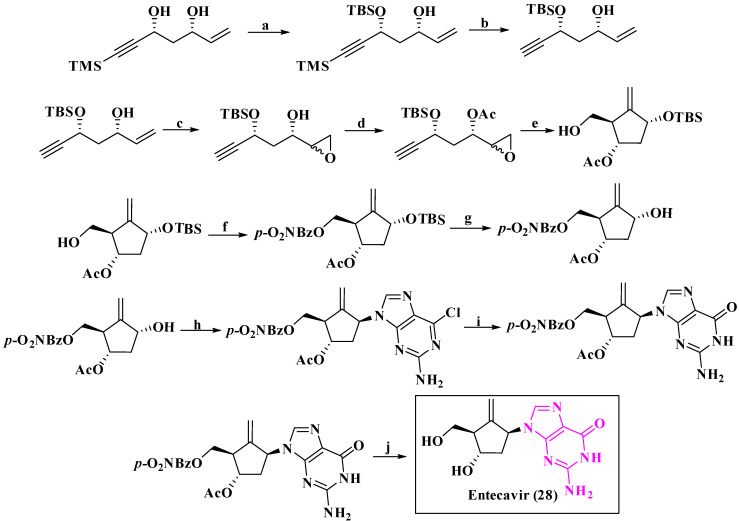
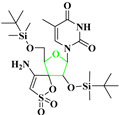
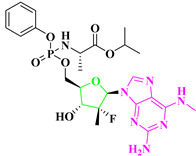
5.3.2. Anti-HBV Agent Entecavir
Entecavir (Figure 16) is a guanosine nucleoside analogue active against hepatitis B (HBV). It is highly efficient in preventing all stages of replication. Compared to the other Hepatitis B drugs, lamivudine and entecavir are more effective; the corresponding triphosphate binds with HBVpol with amino acid residues ARG A: 23, LYS A: 14, ASN A: 18 and ALA A: 68 and effectively inhibits its activity (Figure 17) [176,177].
Figure 16.
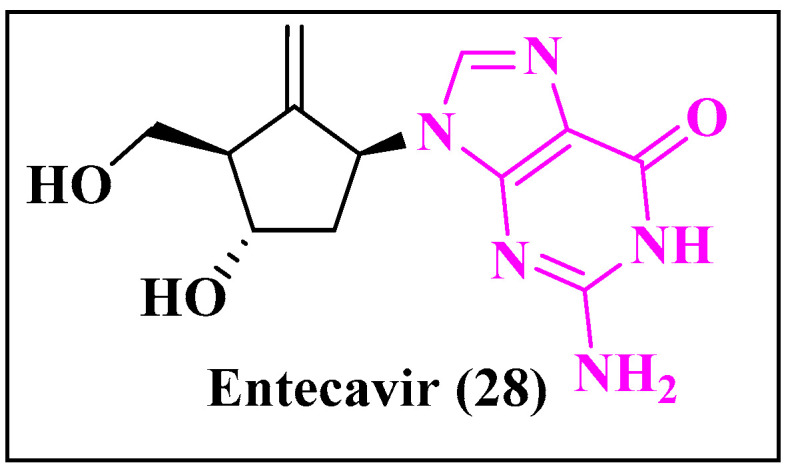
Chemical structure of entecavir (28).
Figure 17.
Entecavir triphosphate docking with HBVpol.
Key synthetic steps for Scheme 8 [178]: (a) Protection of aliphatic alcohol; (b) activation of the terminal alkyne; (c,d) synthesis of the epoxide followed by (e) intramolecular cyclization; (f,g) protection and deprotection of the alcohols; (h) Mitsunobu reaction with 2-amino-6-chloropurine; followed by (i) acid treatment; and (j) saponification to obtain the Entecavir 28.
Scheme 8.
Synthesis of entecavir.
Reagents and conditions: (a) TBSCI (1.1 equiv.), imidazole, THF, rt; (b) K2CO3 cat., MeOH; (c) m-CPBA, CH2Cl2; (d) Ac2O, NEt3, DMAP cat., CH2Cl2; (e) Cp2TiCl2 20 mol%, IrCl(CO)(PPh3)2 10 mol%, Mn (2 equiv.), collidine, TMSCl, H2 (4 bar), THF; (f) p-O2NBzCl, NEt3, CH2Cl2; (g) 5% (+)-CSA, MeOH; (h) 2-amino-6-chloropurine, DIAD, PPh3, THF, −10 °C; (i) HCOOH, 50 °C; (j) MeONa, MeOH.
Structure–Activity Relationship of Entecavir: An extensive investigation of the structure–activity relationship (SAR) of entecavir and its analogues is shown in Table 10. It was discovered that these compounds are the most potent inhibitors of HBV replication, with the ability to effectively inhibit lamivudine-resistant HBV. These compounds are carbocyclic guanosine nucleoside analogues (R1) and are highly effective when tested against HBV in HepG2.2.15 cells [179]. The plasma half-life of entecavir in rats and dogs is 4–9 h. It is metabolized by HepG2 cells to the corresponding mono-, di-, and triphosphates.
Table 10.
SAR analysis of entecavir derivatives.
| Compound | Substitution | Activity | |
|---|---|---|---|
| −R1 | −R2 | IC50 (μM) | |
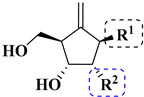
|

|

|
0.03 |
|

|
0.128 | |
|

|
>100 | |
Mechanism of Action of Entecavir: Entecavir is a nucleoside analogue that inhibits hepatitis B virus (HBV) DNA replication by interfering with the activity of viral polymerase, an enzyme essential for the virus to replicate its genetic material. In HBV-infected cells, it is phosphorylated into its active form, entecavir triphosphate, which competes with the natural substrate, deoxyguanosine triphosphate, for incorporation into the elongating viral DNA chain. The incorporation of entecavir triphosphate into the viral DNA chain leads to chain termination, preventing further extension of the viral DNA and ultimately inhibiting HBV replication. Entecavir’s mechanism of action has been extensively studied and has been shown to be highly effective in suppressing HBV replication and reducing liver damage. Due to its high potency and low risk of developing viral resistance, entecavir has become one of the preferred first-line treatments for chronic HBV infection [180,181].
5.3.3. Anti-HBV Agent Dehydro-Andrographolide and Andrographolide Derivatives
Dehydro-andrographolide and andrographolide compounds have demonstrated the ability to inhibit the replication of HBV DNA, with IC50 values of 22.58 and 54.07 μM, respectively [172].
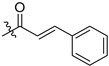
Key synthetic steps for Scheme 9 [172]: (a) Compounds are obtained with the help of esterification reaction with acids in the presence of 4-dimethylaminopyridine (DMAP) and N′,N′-dicyclohexylcarbodiimide (DCC) in anhydrous dichloromethane to obtain the product 35.
Scheme 9.
Synthesis of dehydro-andrographolide (35) and andrographolide (36) derivatives.
Reagents and conditions: (a) corresponding acids, DMAP, DCC, CH2Cl2, rt.
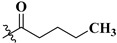
Structure–Activity Relationship of dehydro-Andrographolide: The SARs of the derivatives indicate that having a free hydroxyl group at C-2 can result in enhanced anti-HBV properties. Additionally, maintaining the double bond between C-8 and C-17, as well as the conjugated double bonds between C-11 and C-14, or C-12 and C-15, is crucial for preserving anti-HBV activity and decreasing cytotoxicity. To improve the anti-HBV activity, it is useful to incorporate the 3-methoxycinnamoyl, nicotinoyl, 2-furoyl, or 2-thenoyl groups shown in Table 11 [105]. The anti-HBV activity of the compounds derived from dehydro-andrographolide and andrographolide were investigated. Specifically, their ability to inhibit the secretion of HBsAg and HBeAg, as well as HBV DNA replication, was evaluated using HepG 2.2.15 cells in vitro. Tenofovir, a known antiviral agent, was used as the positive control in the study [182].
Table 11.
SAR analysis of dehydro-andrographolide and andrographolide derivatives.
| Compound | Substitution | Activity |
|---|---|---|
| −R | IC50 (μM) | |
|

|
18 |
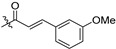
|
1970 | |

|
207 | |

|
40 | |

|
2313 | |

|
19.2 | |

|
162 | |
|
|
210 |

|
1137 | |

|
121 | |

|
880 | |

|
280 | |
|
565 | |

|
1317 |
Mechanism of Action of dehydro-Andrographolide: Dehydro-andrographolide inhibits HBV replication by blocking the binding of the HBV core protein to viral RNA. It also activates the host immune response, which can help control HBV replication and clear infected cells [183]. Overall, dehydro-andrographolide has shown promising anti-HBV activity through its ability to inhibit viral replication and enhance the host immune response. However, further studies are needed to fully understand its mechanisms of action and potential clinical applications [184]. The details of other anti-HBV drugs, along with their mechanisms of action, are mentioned in Table 12.
Table 12.
Anti-HBV drugs.
| Sl. No. | Drug Name | Drug Target | Mechanism of Action |
Ways of Use | Side Effect | Brand Name |
|---|---|---|---|---|---|---|
| 1. | Entecavir [185] | DNA polymerase |
Inhibits the activity of HBV DNA polymerase |
Oral | Headache, dizziness, nausea | Baraclude |
| 2. | Telbivudine [186] | DNA polymerase |
Inhibits the activity of HBV DNA polymerase | Oral | Diarrhea, cough, headache, dizziness | Tyzeka |
| 3. | Lamivudine [187] | Protein P (HBV-F) |
Inhibits reverse transcriptase | Oral | Nausea, diarrhea, headaches | Lamivudine |
Some other synthesized compounds with activity against HBV are tabulated below (Table 13).
Capsid assembly modulators (CpAMs) belong to a novel category of antiviral compounds that specifically target the core protein of the hepatitis B virus (HBV) to interfere with the assembly process. HepG2.2.15 cells are a type of human hepatoblastoma cells that have been genetically modified to stably express the hepatitis B virus (HBV). The compounds under investigation inhibit HBV replication by interfering with the assembly of the HBV capsid protein [188].
Table 13.
Synthesized anti-HBV compounds.
| Sl. No. | Antiviral Agent | Drug Target | Activity |
|---|---|---|---|
| 1. |
|
HBV [189] | Capsid assembly modulators (CpAMs) are antiviral compounds that target the core protein of the hepatitis B virus (HBV) to disrupt assembly. In HepG2.2.15 cells, which express HBV, these compounds inhibit HBV replication by interfering with capsid protein assembly with EC50 = 511 nM. |
| 2. |

|
HBV [190] | The anti-HCV activities were tested in the Huh-Luc/neo cell line and cytotoxicity of the test compound was determined on both MT-2 cell lines with EC50 = 10 µM. |
5.4. Anti-RSV Agent
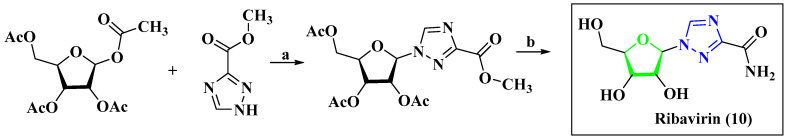
Anti-RSV Agent Ribavirin
The antiviral property of this drug (Figure 18) was studied in 1972 [191]. This drug is presently used for the treatment of RSV. DeVincenzo et al. have studied the inhibitory activities of ribavirin against the RSV F-protein [192].
Figure 18.
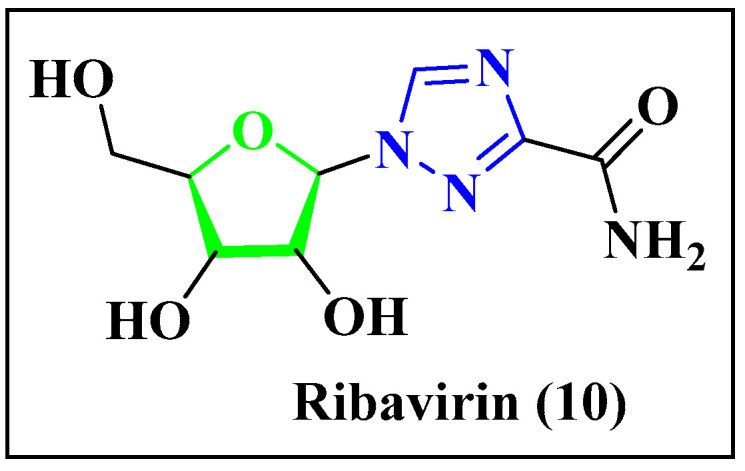
Chemical structure of ribavirin (10).
Key synthetic step for the Scheme 10 [193]: (a) Nucleophilic substitution in the presence of bio-catalyst, (b) amide formation in the presence of NH3 to obtain product 10.
Scheme 10.
Synthesis of ribavirin.
Reagents and conditions: (a) Purine nucleoside phosphorylase, buffer solution of pH = 7; (b) NH3, MeOH.
Mechanism of Action of Ribavirin: Ribavirin is a broad-spectrum antiviral agent that has activity against a range of RNA and DNA viruses, including respiratory syncytial virus (RSV). The mechanism of action of ribavirin is not completely understood, but it is believed to involve several different mechanisms [194]. One proposed mechanism is that ribavirin interferes with the synthesis of viral RNA by inhibiting the activity of the viral RNA-dependent RNA polymerase. Another proposed mechanism is that ribavirin induces mutations in the viral genome, leading to non-functional or less-virulent viral particles. Additionally, ribavirin has been shown to stimulate the host’s immune response, which may contribute to its antiviral effects [195,196,197]. RSV-IGIV and palivizumab are the available drugs on the market for the treatment of RSV. Their mechanisms of action, ways of use and side effects are given in Table 14.
Table 14.
Anti-RSV drugs.
| Sl. No. | Drug Name | Drug Target | Mechanism of Action |
Ways of Use | Side Effect | Brand Name |
|---|---|---|---|---|---|---|
| 1. | Ribavirin [198] | RNA-directed RNA polymerase L (HPIV-2) |
Targets viral RNA polymerase to inhibit mRNA synthesis |
Oral or inhaled | Hemolytic anemia, asthenia, rigors, fevers | Rebetol |
| 2. | RSV-IGIV [199] | RSV G protein | Prevents the binding of RSV surface glycoproteins F and G |
- | - | RespiGam |
| 3. | Palivizumab [200] | Fusion glycoprotein F0 (Human respiratory syncytial virus B) |
Prevents the binding of RSV surface glycoprotein F |
Injection | Sore throat, runny nose, vomiting |
Synagis |
Some other synthesized compounds that show activity against RSV are given in Table 15.
Table 15.
Synthesized anti-RSV compounds.
| Sl. No. | Antiviral Agent | Drug Target | Activity |
|---|---|---|---|
| 1. |
|
Respiratory syncytial virus [201] | The anti-RSV property of the compound tested with Hep2 cells with IC50 = 1.2 nM. The cell viability was measured using MTT reagents and cell cytotoxicity was evaluated through parallel assessments with plaque reduction assays. |
| 2. |
|
Respiratory syncytial virus [202] | The screening of the compounds against nonattenuated respiratory syncytial virus was done by high-throughput protocol with EC50 = 0.36–0.55 μM. |
5.5. Anti-HCMV Agent
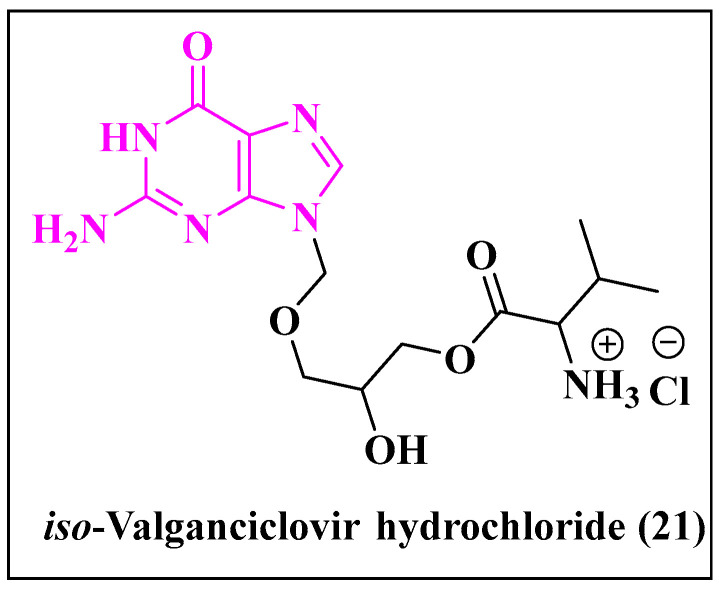
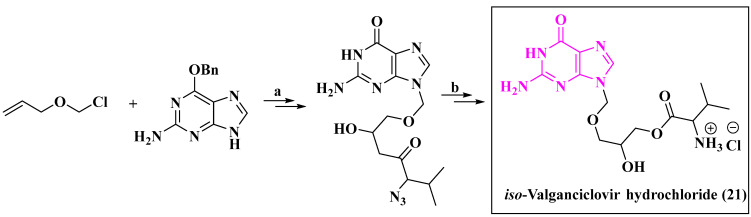
5.5.1. Anti-HCMV Agent Iso-Valganciclovir Hydrochloride
Iso-Valganciclovir hydrochloride (Figure 19) is used for the treatment of cytomegalovirus (CMV). It is a type of nucleoside analogue and is the cutting-edge drug candidate against CMV [203].
Figure 19.
Chemical structure of iso-Valganciclovir hydrochloride (21).
Key synthetic step for Scheme 11 [204]: (a) Addition of reaction of 3-(chloromethoxy)prop-1-ene to o-benzyl guanine in the presence of a base, followed by oxidation; (b) addition reaction with S-2-azido-3-methylbutanoic acid and further reduction gives the final product 21, as shown in Scheme 11.
Scheme 11.
Synthesis of iso-valganciclovir hydrochloride.
Reagents and conditions: (a) (i) NaH, DMF; (ii) KMnO4, acetone; (ii) 10% Pd/C, MeOH; (iv) (S)-2-azido-3-methylbutanoic acid, DCC, DMSO; (b) 10% Pd/C, MeOH.
Mechanism of Action of Iso-Valganciclovir Hydrochloride: Iso-Valganciclovir hydrochloride is a prodrug of the antiviral agent ganciclovir, which is converted to its active form by hydrolysis of the valine ester in the liver and blood. The active form of ganciclovir works by inhibiting the viral DNA polymerase, which is essential for the replication of HCMV. By inhibiting the viral DNA polymerase, ganciclovir prevents the formation of new viral DNA chains, which ultimately inhibits HCMV replication [205].
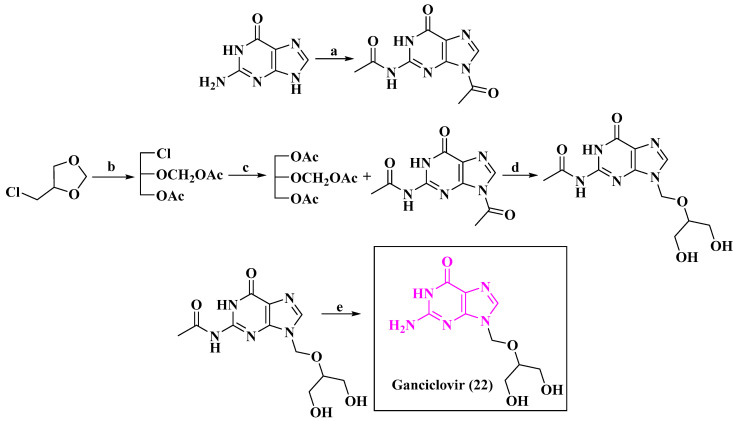
5.5.2. Anti-HCMV Agent Ganciclovir
Ganciclovir (Figure 20) is a marketed drug for the treatment of HCMV; it acts as a DNA polymerase to inhibit synthesis of viral DNA [206].
Figure 20.
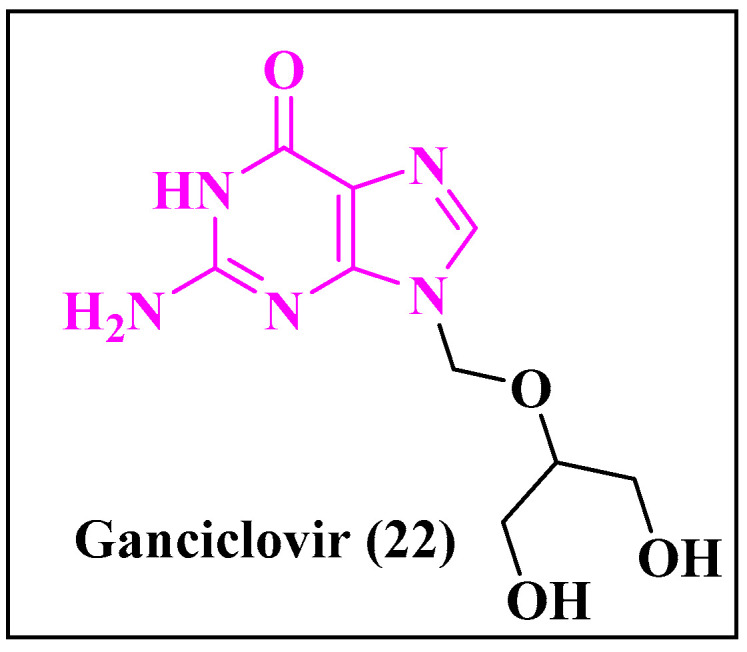
Chemical structure of ganciclovir (22).
Key synthetic steps for Scheme 12 [207]: (a) N-Acylation of the guanine then (d) reacts with 2-(acetoxymethoxy)propane-1,3-diyl diacetate to form N-(9-(((1,3-dihydroxypropan-2-yl)oxy)methyl)-6-oxo-6,9-dihydro-1H-purin-2-yl)acetamide (prepared from 4-(chloromethyl)-1,3-dioxolane) (e) by the deprotection of the amine and alcohol group; the final product 22 was thereby obtained.
Scheme 12.
Synthesis of Ganciclovir.
Reagents and conditions: (a) Ac2O/HOAc, 140 °C; (b) Ac2O/HOAc/ZnCl2, r.t.; (c) KOAc/DMF, 150 °C; (d) EtSO3H, 165–170 °C; (e) 40% aq. MeNH2, 75 °C.
Mechanism of Action of Ganciclovir: Ganciclovir is an antiviral drug used to treat HCMV infections. It stops viral DNA synthesis by acting as a chain terminator, which inhibits the elongation of the viral DNA strand. Ganciclovir triphosphate, its active form, is similar to guanosine and is selectively toxic to infected cells as it is preferentially incorporated into viral DNA, reducing viral replication and controlling infections [206].
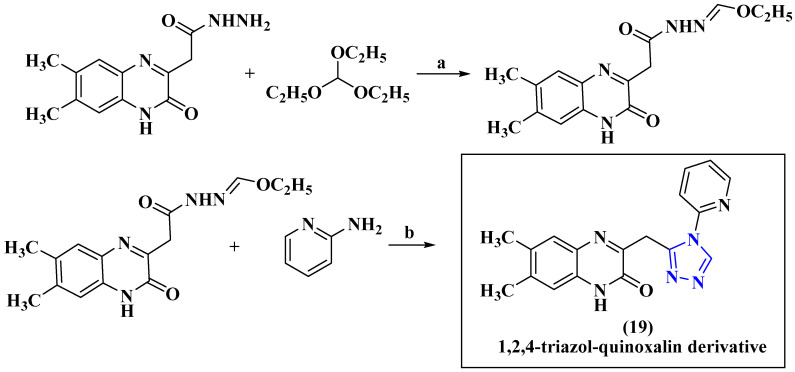
5.5.3. Anti-HCMV Agent 1,2,4-Triazol-Quinoxalin Derivative
Another potential anti-HCMV agent is represented by quinoxaline derivatives, which have been found in recent research studies. Quinoxaline is a heterocyclic compound containing a benzene ring fused to a pyrazine ring, and its derivatives have diverse biological activities, including antiviral properties. These compounds have exhibited greater antiviral activity against HCMV compared to the standard drug ganciclovir [208]. The triazole and quinoxaline moieties in 1,2,4-triazoloquinoxaline (Figure 21) have been reported to exhibit antiviral activity against HCMV. The triazole moiety is a five-membered heterocyclic ring containing three nitrogen atoms, which has been reported to possess antiviral activity. The quinoxaline moiety is a bicyclic aromatic ring system that has also been reported to exhibit antiviral activity. Studies have shown that 1,2,4-triazoloquinoxaline derivatives can inhibit HCMV replication by targeting the viral DNA polymerase, which is a key enzyme involved in viral replication. These compounds have also been reported to have low cytotoxicity toward human cells, making them potentially useful as antiviral agents [209].
Figure 21.
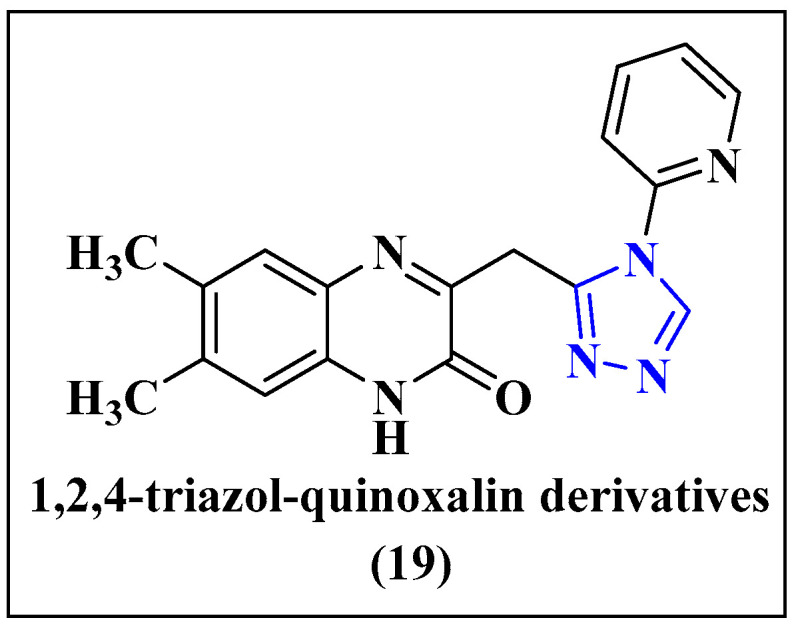
1,2,4-triazol-quinoxalin derivative (19), a new anti-human-cytomegalovirus (HCMV) agent.
Key synthetic steps for Scheme 13 [210]: (a) The compound 2-(6,7-dimethyl-3-oxo-3,4-dihydroquinoxalin-2-yl)acetohydrazide was reacted with triethylorthoformate in ethanol to afford ethyl [(6,7-dimethyl-3-oxo-3,4- dihydroquinoxalin-2-yl)acetyl]hydrazonoformate; further, (b) treatment of the hydrazonoformate with 2-aminopyridine in acetic acid reflux afforded 6,7-dimethyl-3-{[4-(pyridin-2-yl)- 4H-1,2,4-triazol-3-yl]methyl}quinoxalin-2(1H)-one to obtain the product 19.
Scheme 13.
Synthesis of 1,2,4-triazol-quinoxalin derivative.
Reagents and conditions: (a) C2H5OH, rt; (b) CH3COOH, reflux.
Mechanism of Action of 1,2,4-triazol-quinoxalin Derivatives: 1,2,4-triazol-quinoxalin derivatives have potential as antiviral agents against HCMV, but their exact mechanism of action is not fully understood. They may inhibit viral DNA replication and interfere with viral gene expression or virion assembly. Additionally, they may have immunomodulatory effects that enhance antiviral activity or inhibit immune evasion strategies against HCMV [211]. Valganciclovir is another available drug for the treatment of HCMV. The mechanism of action, ways of use and side effects of valganciclovir and ganciclovir are given in Table 16.
Table 16.
Anti-HCMV drugs.
| Sl. No. | Drug Name | Drug Target | Mechanism of Action | Ways of Use | Side Effects | Brand Name |
|---|---|---|---|---|---|---|
| 1. | Valganciclovir [212] | DNA polymerase | Inhibits the activity of viral DNA polymerase | Oral | Diarrhea, upset stomach, dizziness | Valcyte |
| 2. | Ganciclovir [213] | DNA polymerase catalytic subunit | DNA polymerase to inhibit viral DNA synthesis |
Oral | Diarrhea, loss of appetite, increased sweating | Cytovene |
Some other synthesized compounds that show activity against HCMV are given in the Table 17.
Table 17.
Synthesized anti-HCMV compounds.
| Sl. No. | Antiviral Agent | Drug Target | Activity |
|---|---|---|---|
| 1. |
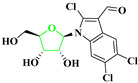
|
HCMV [214] | Synthesized trichlorinated indole nucleosides were tested for activity against human cytomegalovirus (HCMV). Cytotoxicity was assessed using two methods: microscopic inspection of uninfected HFF cells [215] and crystal violet staining with spectrophotometric quantitation in KB cells [216]. The IC50 was found to be 0.23 µM. |
| 2. |
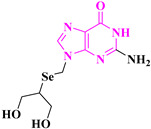
|
HCMV [217] | The compound was assayed for antiviral activity against HCMV (Davis, VR-807) cells in a cytotoxic assay. The EC50 value of 53.1 µM showed only moderate antiviral activity against HCMV. |
5.6. Anti-HSV Agent
Lycogarubins have been reported as the first naturally occurring dimethyl pyrrole-dicarboxylate attached to two indole moieties [218]. These compounds were isolated from the fruit bodies of the slime molds Arcyria denudate, and are closely related to Arcyriarubins and Arycyriaflavins. Three novel dimethyl pyrrole dicarboxylates named Lycogarubins A–C were isolated by Haahimoto et al. from the Myxomycetes Lycogala epidendrum, among which Lycogarubin C showed the effective potency against HSV-I [219]. Idoxuridine, trifluridine and brivudine are marketed anti-HSV drugs used as ointments for the treatment of eye infections due to HSV. They act by inhibiting DNA polymerase of HSV and interrupting viral DNA synthesis. The mechanisms of action, ways of use, and side effects of idoxuridine, trifluridine and brivudine are given in Table 18.
Table 18.
Anti-HSV drugs.
| Sl. No. | Drug Name | Drug Target | Mechanism of Action | Ways of Use | Side Effect | Brand Name |
|---|---|---|---|---|---|---|
| 1. | Idoxuridine [95] | DNA polymerase | HSV DNA polymerase to inhibit viral DNA synthesis | Used as an ointment | Eye irritation or pain, swelling of the eye | Dendrid |
| 2. | Trifluridine [220] | DNA polymerase | Inhibits HSV DNA replication | Eye drop | Eye pain, mild burning of eyes | Viroptic |
| 3. | Brivudine [221] | DNA polymerase | Inhibits HSV DNA replication | Oral | No side effect | Zostex |
Mechanism of Action of Anti-HSV Drugs: Anti-HSV drugs target the herpes simplex virus (HSV) and work by inhibiting viral replication and/or reducing the severity and duration of HSV symptoms. There are three main classes of anti-HSV drugs:
Nucleoside analogues: These drugs mimic the structure of the nucleotides that the virus needs to replicate its DNA. When the virus interacts with the DNA part of the nucleoside, it disrupts the replication process, preventing the virus from making new copies of it. Examples of nucleoside derivatives used to treat HSV include acyclovir, valacyclovir, and famciclovir [58].
Non-nucleoside inhibitors: These drugs target specific viral enzymes that are essential for viral replication. They work by binding to the enzyme and blocking its activity, thereby preventing the virus from replicating. Examples of non-nucleoside inhibitors used to treat HSV include foscarnet and cidofovir [222].
Interferons: These drugs are proteins that the body naturally produces in response to viral infections. They provoke activity by stimulating the immune system to produce antiviral proteins that can inhibit viral replication. Examples of interferons used to treat HSV include interferon alpha and interferon beta [223]. Here, it is important to note that while these drugs can help reduce the severity and duration of HSV symptoms, they do not cure the infection. The virus remains in the body and can reactivate, causing recurrent outbreaks.
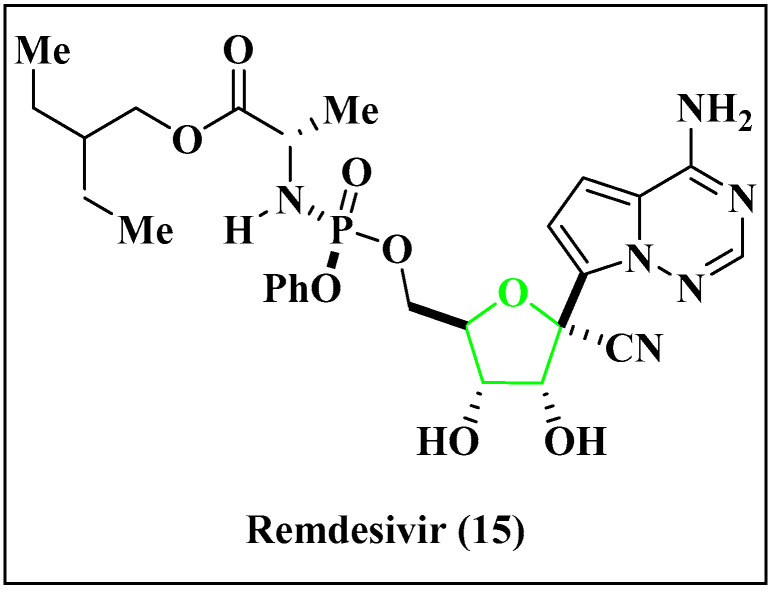
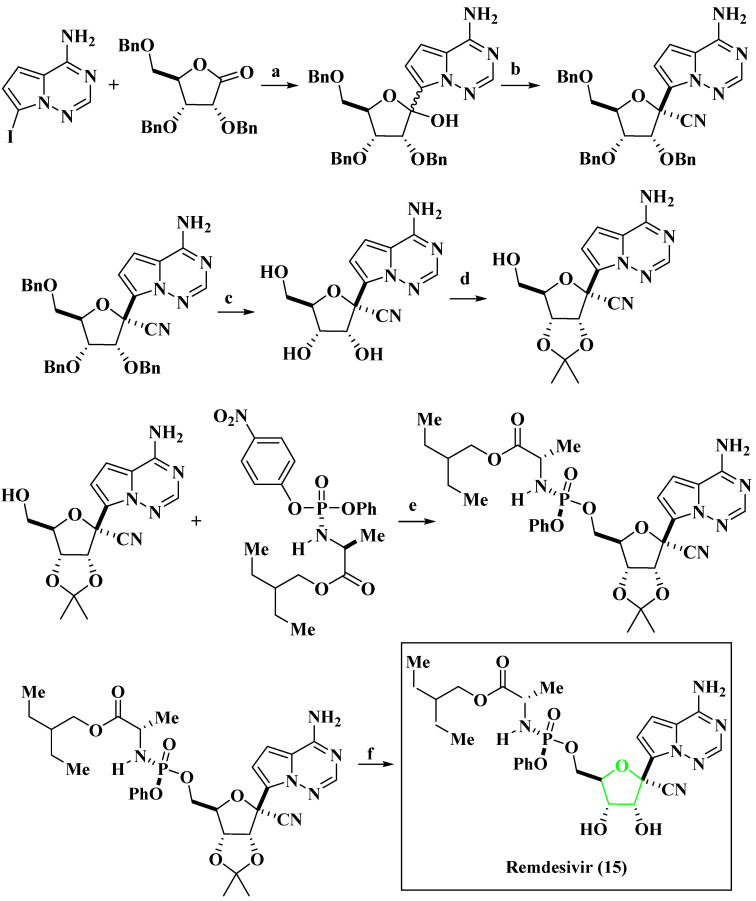
5.7. Anti-Ebola Agent
Anti-Ebola agents are drugs that target the Ebola virus by preventing its replication or entry into human cells. Examples include ZMapp, a combination of three monoclonal antibodies, and remdesivir (Figure 22) [224,225], which is used as a broad-spectrum antiviral drug. The other treatments developed include RNA-based therapies and gene therapies. Such advanced treatments offer genuine hope for a better future, in which EVD will not be considered to be a major concern of public health.
Figure 22.
Anti Ebola agent remdesivir (15).
Key synthetic steps for Scheme 14 [226]: (a) The iodopyrazole was dissolved in THF and cooled to 0 °C, TMSCl was added, and after 1 h, phenylmagnesium chloride was added. The reaction mixture was cooled to −20 °C and iso-propylmagnesium chloride was added slowly to (b) a pre-cooled (−40 °C.) solution of (3R,4R,5R)-2-(4-aminopyrrolo[2,1-f][1.2.4]triazin-7-yl)-3,4-bis(benzyloxy)-5-((benzyloxy)methyl)tetrahydrofuran-2-ol in DCM trifluoroacetic acid was added, followed by a pre-cooled (−30 °C.) solution of TMSOTf and TMSCN in DCM at rt; (c) the tribenzyl cyano nucleoside was dissolved in anhydrous CH2Cl2 and cooled to about −20 °C. A solution of BCl3, the reaction mixture, was stirred for 1 h at about −20 °C. MeOH was added dropwise (d) to a mixture of (2R,3R,4S.5R)-2-(4-aminopyrrolo[2,1-f][1.2.4] triazin-7-yl)-3,4-dihydroxy-5-(hydroxymethyl)tetrahydrofuran-2-carbonitrile, 2,2-dimethoxypropane and acetone at ambient temperature, to which sulfuric acid was added. The mixture was warmed to about 45 °C and (e) N,N-dimethylacetamide was added to a mixture of (2R,3R,4S.5R)-2-(4-aminopyrrolo[2,1-f][1.2.4]triazin-7-yl)-3,4-dihydroxy-5-(hydroxymethyl)tetrahydrofuran-2-carbonitrile, (S)-2-ethylbutyl2-(((S)-(4-nitrophenoxy)(phenoxy)phosphoryl)amino)propanoate and MgCl2. Then the resulting reaction mixture was warmed at 30 °C with constant stirring and N,N-diisopropylethylamine was added slowly, (f) the deprotection of the alcohols was performed by conc. HCl to obtain the product 15.
Scheme 14.
Synthesis of remdesivir.
Reagents and conditions: (a) TMSCl, PhMgCl, iPrMgCl·LiCl, THF, −20 °C; (b) TMSCN, TMSOTf, TfOH, CH2Cl2, −78 °C; (c) (1) BCl3, CH2Cl2, −40 °C; (2) Et3N, MeOH, −78 °C–rt; (d) 2,2-DMP, H2SO4, Me2CO, rt; 45 °C; (e) MgCl2, DIPEA, MeCN, 50 °C; (f) 12 N HCl, THF (1:5), rt.
Mechanism of Action of Remdesivir: Remdesivir interferes with the Ebola virus’s replication by inhibiting its RNA-dependent RNA polymerase enzyme. It acts as a chain terminator, preventing the virus from replicating further and causing harm to the host [97]. The mechanism of action and ways of use are given in Table 19.
Table 19.
Anti-EBOV drugs.
| Sl. No. | Drug Name | Drug Target | Mechanism of Action | Ways of Use | Side Effect | Brand Name |
|---|---|---|---|---|---|---|
| 1. | BCX4430 [227] | RNA-directed RNA polymerase L | Acts as a nonobligate RNA chain terminator upon incorporation into viral RNA |
Intramuscular or oral |
- | BioCryst |
| 2. | Neplanocin A [228] |
S-adenosyl-l-homocysteine (SAH) hydrolase inhibitor | - | - | - | - |
| 3. | Lectins [229] | - | - | - | - | - |
| 4. | Remdesivir [230] | RNA-directed RNA polymerase L | Inhibits the viral RNA polymerase enzyme, which is essential for the replication of the virus | Intravenously | Nausea, vomiting, diarrhea, and elevated liver enzymes | Veklury |
| 5. | TKM-130803 [231] | mRNA of EBOV | Degrades the viral RNA of the Ebola virus | Intravenous infusion | Immune reactions, off-target effects, and toxicity due to high doses | - |
Synthesized compounds that show activity against the Ebola virus are given in Table 20.
Table 20.
Synthesized anti-Ebola compounds.
| Sl. No. | Antiviral Agent | Drug Target | Activity |
|---|---|---|---|
| 1. |
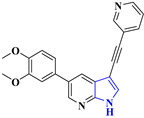
|
Ebola virus [232] | 3,5-Disubstitutedpyrrolo[2,3 b]pyridines demonstrate potent activity against DENV-infected primary dendritic cells and exhibit anti-EBOV activity. A LanthaScreen binding assay was conducted to assess their effectiveness against the Ebola virus (EC50 = 0.59 μM). |
| 2. |
|
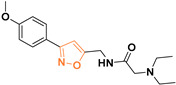
Ebola virus [233] | Isoxazole analogues were tested as inhibitors of Ebola GP-mediated cell entry, with a promising IC50 value in the range of 30 μM. |
| 3. |
|
Ebola virus [200] | - |
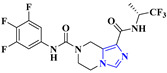
5.8. Anti-SARS-COV-2 Agent
SARS-CoV-2 is a beta-coronavirus in the B lineage that is closely related to the SARS-CoV virus [234]. The major structural genes include N, S, SM and M, while an additional glycoprotein HE occurs in HCoV-OC43 and HKU1 beta-coronaviruses. SARS-CoV-2 shares 96% of its genome with a bat coronavirus. There are several types of anti-SARS-CoV-2 medications, each with its own mechanism of action. The examples are mentioned below:
Vaccines: Vaccines stimulate the immune system to produce antibodies that can neutralize the virus before it can cause an infection. There are currently several COVID-19 vaccines available, including mRNA vaccines, viral vector vaccines, and inactivated or protein subunit vaccines [235].
As of 12 January 2022, the following vaccines have been granted Emergency Use Listing:
Comirnaty vaccine by Pfizer/BioNTech, approved 31 December 2020.
SII/COVISHIELD and AstraZeneca/AZD1222 vaccines, approved 16 February 2021.
Janssen/Ad26.COV 2.S vaccine developed by Johnson & Johnson, approved 12 March 2021.
Moderna COVID-19 vaccine (mRNA 1273), approved 30 April 2021.
Sinopharm COVID-19 vaccine, approved 7 May 2021.
Sinovac-CoronaVac vaccine, approved 1 June 2021.
Bharat Biotech BBV152 COVAXIN vaccine, approved 3 November 2021.
Covovax (NVX-CoV2373) vaccine, approved 17 December 2021.
Nuvaxovid (NVX-CoV2373) vaccine, approved 20 December 2021.
Monoclonal antibodies: Monoclonal antibodies are laboratory-made proteins that mimic the immune system’s ability to fight off harmful pathogens. They can neutralize the virus by binding to specific proteins on its surface and preventing it from entering host cells [236].
Antiviral drugs (Table 21): Antiviral drugs can inhibit viral replication by targeting specific viral proteins or enzymes. For example, remdesivir is an antiviral drug that inhibits the viral RNA polymerase enzyme which is essential for the replication of the virus [237].
Immune-modulators: Immune modulators help modulate the immune response to the virus. For example, dexamethasone is a corticosteroid drug that reduces inflammation and has been shown to improve outcomes in severe COVID-19 cases [238].
Table 21.
Anti-SARS-CoV-2 drugs.
| Sl. No. | Drug Name | Drug Target | Mechanism of Action | Ways of Use | Side Effect | Brand Name |
|---|---|---|---|---|---|---|
| 1. |
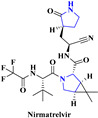
|
SARS-CoV-2 [239] | Nirmatrelvir inhibits cysteine residue in the 3C-like protease (3CLPRO) of SARS-CoV-2 | Oral | There is no such side effect observed | Paxlovid |
| 2. |
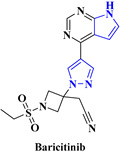
|
COVID-19 [240] | Baricitinib inhibits the activity of JAK proteins and modulates the signaling pathway of various interleukins, interferons | Oral | There is no such side effect observed | Olumiant |
Some other synthesized compounds that show activity against SARS-COV-2 are given in Table 22.
Table 22.
Synthesized anti-SARS-COV-2 compounds.
| Sl. No. | Antiviral Agent | Drug Target | Activity |
|---|---|---|---|
| 1. |
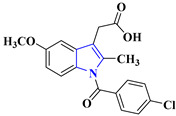
|
SARS-CoV-2 [241] | Indomethacin exhibits potent antiviral activity against SARS coronavirus by selectively inhibiting viral RNA synthesis, independent of its COX inhibition and anti-inflammatory properties [242], with a promising EC50 value of 50 μM. |
| 2. |
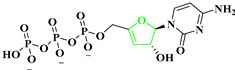
|
SARS-CoV-2 [243] | 3′-Deoxy-3′,4′-didehydro-cytidine triphosphate (ddhCTP) is a novel antiviral molecule that specifically targets non-native RNA polymerases. Its production does not affect cell viability or growth rate. |
| 3. |
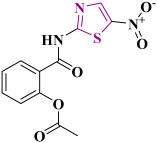
|
SARS-CoV-2 [244] | Nitazoxanide (NTZ), originally an antiparasitic agent, shows potent activity against various RNA and DNA viruses, including SARS-CoV-2 (EC50 = 3.16 μM). Further studies are needed to understand its mode of action and specificity [245]. |
| 4. |
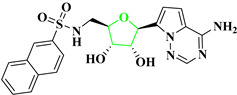
|
SARS-CoV-2 [246] | This compound targets the SARS-CoV-2 methyltransferases MTase and Nsp14. Which demonstrates superior anti-SARS-CoV-2 inhibition (EC50 = 0.72 μM), as evidenced by the compound’s high antiviral activity and low cytotoxicity. |
5.9. Anti-HPV Agent
HPV can infect both men and women, and it is predicted that most sexually active adults will become infected at some point in their lives. It can cause genital warts and certain types of cancer, including cervical, anal and oropharyngeal cancer [247]. There is no cure for HPV; however, there are various treatment options available (as below) to minimize the symptoms in a controlled way [248].
Imiquimod (Aldara): This topical cream stimulates the immune system to fight the virus and is used to treat external genital warts and certain pre-cancerous skin lesions caused by HPV.
Podofilox (Condylox): This topical solution works by destroying the skin cells infected with HPV and is used to treat external genital warts.
Trichloroacetic acid (TCA): This topical solution is used to treat genital warts and certain pre-cancerous skin lesions caused by HPV.
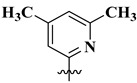
Cidofovir (Vistide): This antiviral drug is used to treat severe cases of HPV infections, including those that have spread to other parts of the body.
Gardasil and Cervarix: These are vaccines that protect against several strains of HPV, including those that are known to cause most cases of cervical cancer.
A synthesized compound that shows activity as an anti-HPV agent is given in Table 23.
Table 23.
Synthesized anti-HPV compound.
| Sl. No. | Antiviral Agent | Drug Target | Activity |
|---|---|---|---|
| 1. |
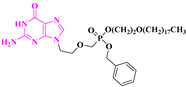
|
Human papillomavirus (HPV-18) [249] | The compound octadecyloxyethyl benzyl 9-[(2-phosphonomethoxy)ethyl]guanine effectively inhibited the amplification of HPV-11 plasmid DNA in transfected cells (EC50 = 0.10 μM). Cell viability was assessed using CellTiter-Glo reagent (Promega) and measured with a luminometer. |
5.10. Anti-Rabies Agent
There are two main ways to prevent and treat rabies virus infection: vaccination and post-exposure prophylaxis (PEP) with immunoglobulin and vaccines. In the case of suspected rabies virus exposure, PEP is recommended to prevent the virus from causing an infection. PEP typically involves the administration of both rabies immunoglobulin (RIG), which contains antibodies against the virus, and a series of rabies vaccine injections [250].
5.11. Anti-Zika Agent
There is currently no specific antiviral treatment for Zika virus infection, and treatment is generally supportive. For example, drugs that are used to treat other Flaviviruses, such as dengue and yellow fever, are being tested in clinical trials to see if they can also be effective against the Zika virus [251,252]. In addition, multiple vaccine candidates, such as DNA vaccines and RNA vaccines, are in various stages of development. These vaccines are being tested in preclinical and clinical trials to determine their safety and effectiveness in preventing Zika virus infection [253].
Synthesized compounds that show activity against the Zika virus are given in Table 24.
Table 24.
Synthesized anti-Zika compounds.
| Sl. No. | Antiviral Agent | Drug Target | Activity |
|---|---|---|---|
| 1. |
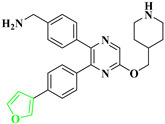
|
Zika virus [254] | These compounds have demonstrated significant efficacy in both cellular and in vivo studies, particularly in U87 glioma cells infected with the ZIKV FLR strain [255], with IC50 values ranging from 200–790 nM. Their mode of action involves binding to an allosteric pocket of NS3, which is a viable target within the Flavivirus protease. This binding occurs in contrast to the shallow active site, which typically recognizes polar and positively charged residues in the substrate, such as arginine (Arg) or lysine (Lys) [256]. |
| 2. |
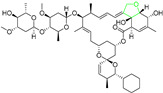
|
Zika virus [257] | Doramectin has been investigated as a potential broad-spectrum antiviral agent against ZIKV. It has shown strong inhibitory effects against ZIKV infection in SNB19 cells. It shows an EC50 value of less than 3 μM. |
| 3. |
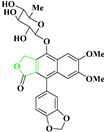
|
Zika virus [258] | Another substituted Glycosylated diphyllin has shown strong inhibitory effects against ZIKV infection in various cell lines, including CHME3 cells (human microglia cells), with IC50 values ranging from 10–70 Nm. |
| 4. |
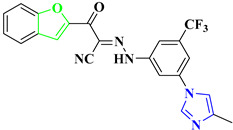
|
Zika virus [259] | Cyanohydrazones have also exhibited noteworthy antiviral activity against ZIKV, with an IC90 value of 4.2 ± 0.2. These compounds target the E-mediated membrane fusion process, effectively inhibiting ZIKV infection [260]. |
Several compounds have shown a broad inhibition activity against Flavivirus proteases and have been extensively studied.
5.12. Anti-Polio Agent
Remediation of polio involves immunization through the administration of the oral polio vaccine (OPV) or the inactivated polio vaccine (IPV). OPV is the preferred vaccine for most countries, as it is easy to administer and can also provide herd immunity by interrupting the transmission of the virus from person to person [261].
5.13. Anti-West Nile Agent
There is currently no specific treatment or vaccine for West Nile virus, but several vaccines are being developed and tested in clinical trials. Nonetheless, several promising vaccine candidates are currently being studied, and ongoing research in this area is very promising and provides hope for the future [262].
5.14. Anti-Chickenpox Agent
Remediation for chickenpox includes management of the symptoms, such as the use of antihistamines to alleviate itching and pain relievers to reduce fever. There are two major ways to prevent and treat chickenpox: through vaccination and antiviral medications. The chickenpox vaccine is a live, attenuated vaccine that contains a weakened form of the varicella–zoster virus [263]. Antiviral medications such as acyclovir, valacyclovir, and famciclovir can also be used to treat chickenpox. These drugs work by inhibiting the replication of the virus and are typically used in individuals who are at high risk of complications, such as pregnant women, immunocompromised individuals, and those with severe symptoms [264].
5.15. Anti-Influenza Agent
The most commonly used drugs for the treatment of the flu disease are neuraminidase inhibitors, which generally work by blocking the intracellular spread of the virus in the body. The two main neuraminidase inhibitors used for this purpose are oseltamivir (Tamiflu) [265] and zanamivir (Relenza) [266]. These drugs are effective in reducing the duration and severity of flu symptoms, as well as preventing complications.
Synthesized compounds with prominent activity against the influenza virus are mentioned in Table 25.
Table 25.
Synthesized anti-influenza compounds.
| Sl. No. | Antiviral Agent | Drug Target | Activity |
|---|---|---|---|
| 1. |
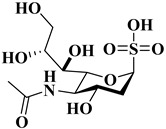
|
Influenza virus [267] | Sialosyl sulfonate is a potent inhibitor of influenza virus replication. Sialosyl sulfonates have shown their ability to block influenza A virus H3N2 (Perth/16/2009) infection of MDCK cells in vitro, using an in-situ ELISA method with IC50 > 1000 μM. |
| 2. |

|
[267] | The above-mentioned method (Table 25, Sl. No. 1) was used to determine the activity of the compound. The IC50 value was found to be 0.7 μM. |
| 3. |
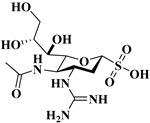
|
[267] | The above-mentioned method (Table 25, Sl. No. 1) was used to determine the activity of the compound. It showed an IC50 > 0.02 μM. |
| 4. |
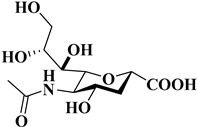
|
[267] | The above-mentioned method (Table 25, Sl. No. 1) was used to determine the activity of the compound. The IC50 value for this compound was found to be 550 μM. |
| 5. |
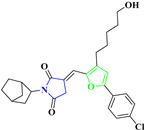
|
Influenza virus [268] | Through intervention in these host–virus interactions, the substituted furan-succinimide derivative can successfully impede viral replication and restrict the advancement of the infection, with the EC50 value determined to be 50 pM [269]. |
| 6. |
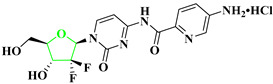
|
Influenza virus [270] | In human cells (HeLa), the compound was evaluated for its antiviral activity (EC90 = 11.4–15.9 μM), more precisely the polymerase activity of influenza A virus PR8. To assess this, a negative-sense EGFP gene, flanked with 5′ and 3′ UTRs derived from the NS segment, was cloned under the control of the human RNA polymerase I promoter. |
| 7. |
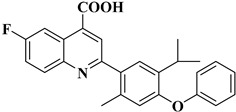
|
Influenza virus [271] | The compound inhibits human dihydroorotate dehydrogenase (DHODH) and viral replication of WSN-Influenza, with an EC50 of 41 nM. |
5.16. Anti-Yellow Fever Agent
Currently, there is no specific antiviral drug available to treat yellow fever. Treatment is primarily supportive, with measures such as fluid replacement, pain relief and management of other symptoms [272].
6. Conclusions
In this review article, we have precisely discussed the antiviral activities of structurally diverse oxa- and aza-cycles with respect to different diseases. We have highlighted the role of representative small molecules, from natural products to synthetic compounds with heterocyclic subunits, and demonstrated their antiviral features. Taking into consideration of the severity of the viral infections, it is undoubtedly necessary to have a complete data set, along with the structure–activity relationship (SAR) of various drug candidates against the infectious viruses. In this regard, this review article could definitely play a crucial role in the discovery of antiviral drugs.
7. Scope, Limitation and the Presentation of the Future Trend of Antiviral Drugs
Antiviral drugs have revolutionized the treatment and control of infections caused by viral diseases. They target specific viral mechanisms, by such means as inhibiting replication, preventing viral entry into cells and blocking the activity of the viral enzyme. These drugs have significantly improved patient outcomes and reduced the spread of contagions. They are capable enough to tackle infections like HIV, hepatitis, influenza, herpes, and more. In spite of the suitability of such drugs in terms of the proper treatment and control of viral infections, they do have limitations. Viruses can develop resistance to certain drugs, necessitating the development of new classes of drugs or combination therapies. Moreover, antiviral drugs may cause side effects and interact with other medications, a situation which requires careful management. The challenges are even greater when facing the newly emerged viruses, and the lack of specific and effective treatment options becomes apparent. The development of drugs targeting such viruses is very complicated and involves extensive research and development, advanced computational support and dedicated clinical trials. Additionally, viral mutations and the potential for drug resistance further impede the effectiveness of existing therapies against newly arrived viruses.
Furthermore, emerging technologies like CRISPR/Cas9-based gene editing hold the potential for targeted viral genome disruption, offering innovative approaches to combat viral infections. The ongoing research and development of antiviral drugs aim to address current limitations, including drug resistance, side effects and access issues, while providing more effective, safer and accessible treatments for viral infections in the future.
Acknowledgments
S.H. is thankful to SERB, India (grant no. ECR/2017/000966) and DST, India (grant no. INT/RUS/RFBR/P-293/G) for the financial support. S. Santra and G.V. Zyryanov are grateful to the Ministry of Science and Higher Education of the Russian Federation (Agreement # 075-15-2022-1118 dated 29.06.2022) for funding. S.M. thanks VNIT Nagpur, India, for the research fellowship. K.D. is grateful to DST, India for providing a research fellowship. We all are thankful to the department of Chemistry VNIT Nagpur for providing infrastructure and a research facility.
Abbreviations
| Abbreviation | Full Name |
| DNA | Deoxyribonucleic Acid |
| RNA | Ribonucleic Acid |
| AIDS | Acquired Immune Deficiency Syndrome |
| HIV | Human Immunodeficiency Virus |
| HCV | Hepatitis C Virus |
| HBV | Hepatitis B Virus |
| RSV | Respiratory Syncytial Virus |
| HCMV | Human Cytomegalovirus |
| HSV | Herpes Simplex Virus |
| EBOV | Ebola Virus |
| SARS-CoV-2 | Severe Acute Respiratory Syndrome CoV-2 |
| PNBA | Para Nitro Benzoic Acid |
| GP120-CCR5 | Beta chemokine receptors |
| dATP | Deoxyadenosine triphosphate |
| mRNA | Messenger Ribonucleic Acid |
| eIF4A | Eukaryotic initiation factor 4A |
| ToS | Toluenesulfonyl |
| OiPr | Isopropoxide |
| OSBT | O-(Tert-Butyldimethylsilyl)hydroxylamine |
| Boc | tert-butoxycarbonyl |
| PMP | Polymethylpentene |
| OBn | Benzyl group |
| mCPBA | meta-chloroperoxybenzoic acid |
| DMSO | Dimethyldioxirane |
| TFAA | Trifluoroacetic anhydride |
| TFA | Trifluoroacetic acid |
| DSC | N,N′-Disuccinimidyl carbonate |
| DEC | Diethylcarbamazine |
| DMAP | 4-Dimethylaminopyridine |
| LDA | Lithium diisopropylamide |
| DDQ | 2,3-Dichloro-5,6-Dicyanobenzoquinone |
| THF | Tetrahydrofuran |
| NBS | N-Bromosuccinimide |
| DPPA | Diphenylphosphoryl azide |
| HATU | Hexafluorophosphate Azabenzotriazole Tetramethyl Uronium |
| DCM | Dichloromethane |
| DMAc | N,N-Dimethylacetamide |
| DBU | 1,8-Diazabicyclo(5.4.0)undec-7-ene |
| CDI | Carbonyldiimidazole |
| CPME | Cyclopentyl methyl ether |
| DIAD | Diisopropyl azodicarboxylate |
| IPAc | Isopropyl acetate |
| DMF | Dimethylformamide |
| DCC | N,N′-Dicyclohexylcarbodiimide |
| DEAD | Diethyl azodicarboxylate |
| TBAF | Tetra-n-butylammonium fluoride |
| 4Å MS | 4Å Molecular Sieve |
Author Contributions
Investigation, S.S. and E.V.N.; resources, S.S. and E.V.N.; writing—original draft preparation, K.D. and S.H.; writing—review and editing, S.S.; E.V.N. and G.V.Z.; literature Search, S.M. and K.D.; structure Draw, S.M. and K.D.; referencing, S.H.; editing, S.H. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
Science and Engineering Research Board; ECR/2017/000966.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Parvez M.K., Parveen S. Evolution and Emergence of Pathogenic Viruses: Past, Present, and Future. Intervirology. 2017;60:1–7. doi: 10.1159/000478729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gaba A., Ayalew L.E., Tikoo S.K. Animal Adenoviruses. In: Malik Y.S., Singh R.K., Yadav M.P., editors. Recent Advances in Animal Virology. Springer; Singapore: 2019. [DOI] [Google Scholar]
- 3.Zhu Z., Lian X., Su X., Wu W., Marraro G.A., Zeng Y. From SARS and MERS to COVID-19: A brief summary and comparison of severe acute respiratory infections caused by threeighly pathogenic human coronaviruses. Respir. Res. 2020;21:224. doi: 10.1186/s12931-020-01479-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wirth T. Biodiversity and Evolution. Volume 3. Elsevier; Amsterdam, The Netherlands: 2018. pp. 123–137. [DOI] [Google Scholar]
- 5.Morens D.M., Fauci A.S. Emerging Pandemic Diseases: How We Got to COVID-19. Cell. 2020;182:1077–1092. doi: 10.1016/j.cell.2020.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pagidipati N.J., Gaziano T.A. Estimating Deaths From Cardiovascular Disease: A Review of Global Methodologies of Mortality Measurement. Circulation. 2013;127:749–756. doi: 10.1161/CIRCULATIONAHA.112.128413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Joint United Nations Programme on HIV/AIDS (UNAIDS) 2006 Report on the Global AIDS Epidemic. UNAIDS; Geneva, Switzerland: 2006. [Google Scholar]
- 8.Mathers C.D., Boerma T., Ma Fat D. Global and regional causes of death. Br. Med. Bull. 2009;92:7–32. doi: 10.1093/bmb/ldp028. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization . Division of Emerging and Other Communicable Diseases Surveillance and Control. World Survey of Rabies: No. 30: For the Year 1994. World Health Organization; Geneva, Switzerland: 1996. [Google Scholar]
- 10.Piot P., Muyembe J.J., Edmunds W.J. Ebola in west Africa: From disease outbreak to humanitarian crisis. Lancet Infect. Dis. 2014;14:1034–1035. doi: 10.1016/S1473-3099(14)70956-9. [DOI] [PubMed] [Google Scholar]
- 11.Gostin L.O., Lucey D., Phelan A. The Ebola Epidemic A Global Health Emergency. JAMA J. Am. Med. Assoc. 2014;312:1095–1096. doi: 10.1001/jama.2014.11176. [DOI] [PubMed] [Google Scholar]
- 12.Meyers L., Frawley T., Goss S., Kang C. Ebola Virus Outbreak 2014: Clinical Review for Emergency Physicians. Ann. Emerg. Med. 2015;65:101–108. doi: 10.1016/j.annemergmed.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 13.Gogineni V., Schinazi R.F., Hamann M.T. Role of Marine Natural Products in the Genesis of Antiviral Agents. Chem. Rev. 2015;115:9655–9706. doi: 10.1021/cr4006318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.More A.F., Loveluck C.P., Clifford H., Handley M.J., Korotkikh E.V., Kurbatov A.V., McCormick M., Mayewski P.A. The health benefit of physical exercise on COVID-19 pandemic: Evidence from mainland China. GeoHealth. 2020;4:277–284. doi: 10.1371/journal.pone.0275425. [DOI] [Google Scholar]
- 15.Mammas I., Spandidos D.A. [Comment] COVID-19 threat and the 1918 Spanish flu outbreak: The following day. Exp. Ther. Med. 2019;20:292. doi: 10.3892/etm.2020.9422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taubenberger J.K., Morens D.M. 1918 Influenza: The mother of all pandemics. Emerg. Infect. Dis. 2006;12:15–22. doi: 10.3201/eid1209.05-0979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trilla A., Trilla G., Daer C. The 1918 “Spanish Flu” in Spain. Clin. Infect. Dis. 2008;47:668–673. doi: 10.1086/590567. [DOI] [PubMed] [Google Scholar]
- 18.Li L., Huang T., Wang Y., Wang Z., Liang Y., Huang T., Zhang H., Sun W., Wang Y.J. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. Med. Virol. 2020;92:577–583. doi: 10.1002/jmv.25757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dagan N., Barda N., Kepten E., Miron O., Perchik S., Katz M.A., Hernán M.A., Lipsitch M., Reis B., Balicer R.D. BNT162b2 mRNA COVID-19 Vaccine in a Nationwide Mass Vaccination Setting. N. Engl. J. Med. 2021;384:1412–1423. doi: 10.1056/NEJMoa2101765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haynes B.F., Corey L., Fernandes P., Gilbert P.B., Hotez P.J., Rao S., Santos M.R., Schuitemaker H., Watson M., Arvin A. Prospects for a safe COVID-19 vaccine. Sci. Transl. Med. 2020;12:eabe0948. doi: 10.1126/scitranslmed.abe0948. [DOI] [PubMed] [Google Scholar]
- 21.Corey L., Mascola J.R., Fauci A.S., Collins F.S. A strategic approach to COVID-19 vaccine R&D. Science. 2020;368:948–950. doi: 10.1126/science.abc5312. [DOI] [PubMed] [Google Scholar]
- 22.Kim J.H., Marks F., Clemens J.D. Looking beyond COVID-19 vaccine phase 3 trials. Nat. Med. 2021;27:205–211. doi: 10.1038/s41591-021-01230-y. [DOI] [PubMed] [Google Scholar]
- 23.Cao Y., Deng Q., Dai S. Remdesivir for severe acute respiratory syndrome coronavirus 2 causing COVID-19: An evaluation of the evidence. Travel Med. Infect. Dis. 2020;35:101647–101677. doi: 10.1016/j.tmaid.2020.101647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization Newsroom: Coronavirus Disease (COVID-19): Vaccines. [(accessed on 15 August 2021)]. Available online: https://www.who.int/news-room/q-a-detail/coronavirus-disease-(COVID-19)-vaccines.
- 25.Onnuswamy M.N., Gromiha M.M., Sony S.M.M., Saraboji K. QSAR and Molecular Modeling Studies in Heterocyclic Drugs I. Volume 3. Springer; Berlin/Heidelberg, Germany: 2006. pp. 81–147. [DOI] [Google Scholar]
- 26.Sliwoski G.R., Meiler J., Lowe E.W. Computational methods in drug discovery. Comput. Methods Drug Discov. 2014;66:334–395. doi: 10.1124/pr.112.007336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jambhekar S.S., Breen P.J. Drug dissolution: Significance of physicochemical properties and physiological conditions. Drug Discov. Today. 2013;18:1173–1184. doi: 10.1016/j.drudis.2013.08.013. [DOI] [PubMed] [Google Scholar]
- 28.Syam Y., Kamel M. Structure and physicochemical properties in relation to drug action. Egypt. Pharm. J. 2013;12:95–108. doi: 10.4103/1687-4315.124000. [DOI] [Google Scholar]
- 29.Martin-Benlloch X., Haid S., Novodomska A., Rominger F., Pietschmann T., Davioud-Charvet E., Elhabiri M. Physicochemical properties govern the activity of potent antiviral flavones. ACS Omega. 2019;4:4871–4887. doi: 10.1021/acsomega.8b03332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Klimenko K., Marcou G., Horvath D., Varnek A.J. Chemical Space Mapping and Structure–Activity Analysis of the ChEMBL Antiviral Compound Set. Chem. Inf. Model. 2016;56:1438–1454. doi: 10.1021/acs.jcim.6b00192. [DOI] [PubMed] [Google Scholar]
- 31.Prashantha Kumar B.R., Soni M., Bharvi Bhikhalal U., Kakkot I.R., Jagadeesh M., Bommu P., Nanjan M.J. Analysis of physicochemical properties for drugs from nature. Nat. Med. Chem. Res. 2010;19:984–992. doi: 10.1007/s00044-009-9244-2. [DOI] [Google Scholar]
- 32.Evstigneev M.P. Physicochemical mechanisms of synergistic biological action of combinations of aromatic heterocyclic compounds. Org. Chem. Int. 2013;2013:278143. doi: 10.1155/2013/278143. [DOI] [Google Scholar]
- 33.Kerru N., Gummidi L., Maddila S., Gangu K.K., Jonnalagadda S.B. A review on recent advances in nitrogen-containing molecules and their biological applications. Molecules. 2020;25:1909. doi: 10.3390/molecules25081909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gomtsyan, AHeterocycles in drugs and drug discovery. Chem. Heterocycl. Compd. 2012;48:7–10. doi: 10.1007/s10593-012-0960-z. [DOI] [Google Scholar]
- 35.De Vivo M., Masetti M., Bottegoni G., Cavalli A. Role of molecular dynamics and related methods in drug discovery. J. Med. Chem. 2016;59:4035–4061. doi: 10.1021/acs.jmedchem.5b01684. [DOI] [PubMed] [Google Scholar]
- 36.Pastorino B., Nougairède A., Wurtz N., Gould E., de Lamballerie X. Role of host cell factors in flavivirus infection: Implications for pathogenesis and development of antiviral drugs. Antivir. Res. 2010;87:281–294. doi: 10.1016/j.antiviral.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 37.Monto A.S. Vaccines and antiviral drugs in pandemic preparedness. Emerg. Infect. Dis. 2006;12:55–60. doi: 10.3201/eid1201.051068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schmid M., Speiseder T., Dobner T., Gonzalez R.A. DNA virus replication compartments. J. Virol. 2014;88:1404–1420. doi: 10.1128/JVI.02046-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schwartz M., Chen J., Janda M., Sullivan M., Den Boon J., Ahlquist P. A positive-strand RNA virus replication complex parallels form and function of retrovirus capsids. Mol. Cell. 2002;9:505–514. doi: 10.1016/S1097-2765(02)00474-4. [DOI] [PubMed] [Google Scholar]
- 40.Vahlne A. A historical reflection on the discovery of human retroviruses. Retrovirology. 2009;6:40. doi: 10.1186/1742-4690-6-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Levin J.G., Mitra M., Mascarenhas A., Musier-Forsyth K. Role of HIV-1 nucleocapsid protein in HIV-1 reverse transcription. RNA Biol. 2010;7:754–774. doi: 10.4161/rna.7.6.14115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gallo R.C., Montagnier L. The discovery of HIV as the cause of AIDS. N. Engl. J. Med. 2003;349:2283–2285. doi: 10.1056/NEJMp038194. [DOI] [PubMed] [Google Scholar]
- 43.World Health Organization Newsroom: HIV and AIDS. [(accessed on 4 May 2023)]. Available online: https://www.who.int/news-room/fact-sheets/detail/hiv-aids.
- 44.Ghosh A.K., Fyvie W.S., Brindisi M., Steffey M., Agniswamy J., Wang Y.F., Aoki M., Amano M., Weber I.T., Mitsuya H. Design, Synthesis, Biological Evaluation, and X-ray Studies of HIV-1 Protease Inhibitors with Modified P2′ Ligands of Darunavir. ChemMedChem. 2017;12:1942–1952. doi: 10.1002/cmdc.201700614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Du L., Jia J., Ge P., Jin Y. Self-assemblies of 5′-cholesteryl-ethyl-phosphoryl zidovudine. Colloids Surf. B. 2016;148:385–391. doi: 10.1016/j.colsurfb.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 46.Belk D., Belk P. The Great American Healthcare Scam: How Kickbacks, Collusion and Propaganda Have Exploded Healthcare Costs in the United States Paperback. David Belk; Greensboro, NC, USA: 2020. [Google Scholar]
- 47.Vasilyeva S.V., Shtil A.A., Petrova A.S., Balakhnin S.M., Achigecheva P.Y., Stetsenko D.A., Silnikov V.N. Conjugates of phosphorylated zalcitabine and lamivudine with SiO2 nanoparticles: Synthesis by CuAAC click chemistry and preliminary assessment of anti-HIV and antiproliferative activity. Bioorg. Med. Chem. 2017;25:1696–1702. doi: 10.1016/j.bmc.2017.01.038. [DOI] [PubMed] [Google Scholar]
- 48.Paton N.I., Musaazi J., Kityo C., Walimbwa S., Hoppe A., Balyegisawa A., Kaimal A., Mirembe G., Tukamushabe P., Ategeka G. Dolutegravir or darunavir in combination with zidovudine or tenofovir to treat HIV. N. Engl. J. Med. 2021;385:330–341. doi: 10.1056/NEJMoa2101609. [DOI] [PubMed] [Google Scholar]
- 49.Mayer K.H., Molina J.-M., Thompson M.A., Anderson P.L., Mounzer K.C., De Wet J.J., DeJesus E., Jessen H., Grant R.M., Ruane P.J. Emtricitabine and tenofovir alafenamide vs emtricitabine and tenofovir disoproxil fumarate for HIV pre-exposure prophylaxis (DISCOVER): Primary results from a randomised, double-blind, multicentre, active-controlled, phase 3, non-inferiority trial. Lancet. 2020;396:239–254. doi: 10.1016/S0140-6736(20)31065-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alter M.J. Epidemiology of hepatitis C virus infection. World J. Gastroenterol. 2007;13:2436–2441. doi: 10.3748/wjg.v13.i17.2436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Massengill M.T., Park J.C., McAnany J.J., Hyde R.A. Occult retinopathy following treatment of Hepatitis C with glecaprevir/pibrentasvir (Mavyret) Doc. Ophthalmol. 2023;146:191–197. doi: 10.1007/s10633-023-09923-0. [DOI] [PubMed] [Google Scholar]
- 52.Gentile I., Buonomo A.R., Zappulo E., Minei G., Morisco F., Borrelli F., Coppola N., Borgia G. Asunaprevir, a protease inhibitor for the treatment of hepatitis C infection. Ther. Clin. Risk Manag. 2014;10:493–504. doi: 10.2147/TCRM.S66731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chang M.H., Gordon L.A., Fung H.B. Infection of common marmosets with GB virus B chimeric virus encoding the major nonstructural proteins NS2 to NS4A of hepatitis C virus. Clin. Ther. 2012;34:2021–2038. doi: 10.1016/j.clinthera.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 54.Kiang T.K.L. Clinical pharmacokinetics and drug–drug interactions of elbasvir/grazoprevir. Eur. J. Drug Metab. Pharmacokinet. 2018;43:509–531. doi: 10.1007/s13318-018-0471-0. [DOI] [PubMed] [Google Scholar]
- 55.Blumberg B.S. Hepatitis B virus, the vaccine, and the control of primary cancer of the liver. Proc. Natl. Acad. Sci. USA. 1997;94:7121–7125. doi: 10.1073/pnas.94.14.7121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liu J., Li T., Zhang L., Xu A. The role of hepatitis B surface antigen in nucleos (t) ide analogues cessation among asian patients with chronic hepatitis B: A systematic review. Hepatology. 2019;70:1045–1055. doi: 10.1002/hep.30474. [DOI] [PubMed] [Google Scholar]
- 57.Sulkowski M.S., Agarwal K., Ma X., Nguyen T.T., Schiff E.R., Hann H.W.L., Dieterich D.T., Nahass R.G., Park J.S., Chan S.J. Safety and efficacy of vebicorvir administered with entecavir in treatment-naïve patients with chronic hepatitis B virus infection. Hepatol. 2022;77:1265–1275. doi: 10.1016/j.jhep.2022.05.027. [DOI] [PubMed] [Google Scholar]
- 58.Zenchenko A.A., Drenichev M.S., Il’icheva I.A., Mikhailov S.N. Antiviral and antimicrobial nucleoside derivatives: Structural features and mechanisms of action. Mol. Biol. 2021;55:786–812. doi: 10.1134/S0026893321040105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Menéndez-Arias L., Álvarez M., Pacheco B. Nucleoside/nucleotide analog inhibitors of hepatitis B virus polymerase: Mechanism of action and resistance. Curr. Opin. Virol. 2014;8:1–9. doi: 10.1016/j.coviro.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 60.Acosta P.L., Caballero M.T., Polack F.P. Brief history and characterization of enhanced respiratory syncytial virus disease. Clin. Vaccine Immunol. 2016;23:189–195. doi: 10.1128/CVI.00609-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Li Y., Wang X., Blau D.M., Caballero M.T., Feikin D.R., Gill C.J., Madhi S.A., Omer S.B., Simões E.A.F., Campbell H. Brief history and characterization of enhanced respiratory syncytial virus disease. Lancet. 2022;399:2047–2064. doi: 10.1016/S0140-6736(22)00478-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shi T., Vennard S., Mahdy S., Nair H.J. Risk factors for RSV associated acute lower respiratory infection poor outcome and mortality in young children: A systematic review and meta-analysis. Infect. Dis. 2022;226:S10–S16. doi: 10.1093/infdis/jiaa751. [DOI] [PubMed] [Google Scholar]
- 63.Nair H., Nokes D.J., Gessner B.D., Dherani M., Madhi S.A., Singleton R.J., O’Brien K.L., Roca A., Wright P.F., Bruce N., et al. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: A systematic review and meta-analysis. Lancet. 2010;375:1545–1555. doi: 10.1016/S0140-6736(10)60206-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang Y.Q., Zhao X.Y. Human cytomegalovirus primary infection and reactivation: Insights from virion-carried molecules. Front. Microbiol. 2020;11:1511. doi: 10.3389/fmicb.2020.01511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Stoelben S., Arns W., Renders L., Hummel J., Mühlfeld A., Stangl M., Fischereder M., Gwinner W., Suwelack B., Witzke O., et al. Preemptive treatment of Cytomegalovirus infection in kidney transplant recipients with letermovir: Results of a Phase 2a study. Transpl. Int. 2014;27:77–86. doi: 10.1111/tri.12225. [DOI] [PubMed] [Google Scholar]
- 66.Biron K.K. Antiviral drugs for cytomegalovirus diseases. Antivir. Res. 2006;71:154–163. doi: 10.1016/j.antiviral.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 67.Corey L., Sper P.G. Infections with herpes simplex viruses. N. Engl. J. Med. 1986;314:686–691. doi: 10.1056/NEJM198603133141105. [DOI] [PubMed] [Google Scholar]
- 68.Gottlieb S.L., Giersing B.K., Hickling J., Jones R., Deal C., Kaslow D.C. Meeting report: Initial World Health Organization consultation on herpes simplex virus (HSV) vaccine preferred product characteristics, March 2017. Vaccine. 2019;37:7408–7418. doi: 10.1016/j.vaccine.2017.10.084. [DOI] [PubMed] [Google Scholar]
- 69.Feldmann H., Jones S., Klenk H.-D., Schnittler H.-J. Ebola virus: From discovery to vaccine. Nat. Rev. Immunol. 2003;3:677–685. doi: 10.1038/nri1154. [DOI] [PubMed] [Google Scholar]
- 70.Mirza M.U., Vanmeert M., Ali A., Iman K., Froeyen M., Idrees M. Perspectives towards antiviral drug discovery against Ebola virus. J. Med. Virol. 2019;91:2029–2048. doi: 10.1002/jmv.25357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Grellet E., Goulet A., Imbert I. Replication of the Coronavirus Genome: A Paradox among Positive-Strand RNA Viruses. J. Biol. Chem. 2022;5:101923–101938. doi: 10.1016/j.jbc.2022.101923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tyrrell D.A.J., Bynoe M.L. Cultivation of viruses from a high proportion of patients with colds. Lancet. 1966;287:76–77. doi: 10.1016/S0140-6736(66)92364-6. [DOI] [PubMed] [Google Scholar]
- 73.Kahn J.S., McIntosh K. History and Recent Advances in Coronavirus Discovery. Pediatr. Infect. Dis. J. 2005;24:S223–S227. doi: 10.1097/01.inf.0000188166.17324.60. [DOI] [PubMed] [Google Scholar]
- 74.Hu B., Guo H., Zhou P., Shi Z.L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021;19:141–154. doi: 10.1038/s41579-020-00459-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chang F., Syrjänen S., Kellokoski J., Syrjänen K. Human Papillomavirus (HPV) Infections and Their Associations with Oral Disease. J. Oral Pathol. Med. 1991;20:305–317. doi: 10.1111/j.1600-0714.1991.tb00936.x. [DOI] [PubMed] [Google Scholar]
- 76.World Health Organization Newsroom: Fact Sheets. Cervical Cancer. [(accessed on 1 May 2023)]. Available online: https://www.who.int/news-room/fact-sheets/detail/cervical-cancer.
- 77.Fekadu M., Shaddock J.H., Chandler F.W., Baer G.M. Rabies Virus in the Tonsils of a Carrier Dog. Arch. Virol. 1983;78:37–47. doi: 10.1007/BF01310857. [DOI] [PubMed] [Google Scholar]
- 78.Dick G.W.A., Kitchen S.F., Haddow A.J. zika virus (i). Isolations and serological specificity. Trans. R. Soc. Trop. Med. Hyg. 1952;46:509–520. doi: 10.1016/0035-9203(52)90042-4. [DOI] [PubMed] [Google Scholar]
- 79.Posen H.J., Keystone J.S., Gubbay J.B., Morris S.K. Epidemiology of Zika Virus, 1947–2007. BMJ Glob. Health. 2016;1:e000087. doi: 10.1136/bmjgh-2016-000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chen H.L., Tang R.B.J. Why Zika virus infection has become a public health concern? Chin. Med. Assoc. 2016;79:174–178. doi: 10.1016/j.jcma.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 81.Gorshkov K., Shiryaev S.A., Fertel S., Lin Y.W., Huang C.T., Pinto A., Farhy C., Strongin A.Y., Zheng W., Terskikh A.V. Transdermal permeation of bacteriophage particles by choline oleate: Potential for treatment of soft-tissue infections. Front. Microbiol. 2019;9:3252–3296. doi: 10.3389/fmicb.2018.03252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Skern T. 100 years poliovirus: From discovery to eradication. A meeting report. Arch. Virol. 2010;155:1371–1381. doi: 10.1007/s00705-010-0778-x. [DOI] [PubMed] [Google Scholar]
- 83.Melnick J.L. Current Status of Poliovirus Infections. Clin. Microbiol. Rev. 1996;9:293–300. doi: 10.1128/CMR.9.3.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dowdle W.R., Birmingham M.E. The Biologic Principles of Poliovirus Eradication. J. Infect. Dis. 1997;175:S286–S292. doi: 10.1093/infdis/175.Supplement_1.S286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.World Health Organization Health Topics: Poliomyelitis. [(accessed on 1 May 2023)]. Available online: https://www.who.int/health-topics/poliomyelitis.
- 86.Smithburn K.C., Hughes T.P., Burke A.W., Paul J.H. A neurotropic virus isolated from the blood of a native of Uganda. Am. J. Trop. Med. 1940;20:471–472. doi: 10.4269/ajtmh.1940.s1-20.471. [DOI] [Google Scholar]
- 87.World Health Organization Newsroom: Fact Sheets. West Nile Virus. [(accessed on 1 May 2023)]. Available online: https://www.who.int/news-room/fact-sheets/detail/west-nile-virus.
- 88.Takahashi M. Chickenpox Virus. Adv. Virus Res. 1983;28:285–356. doi: 10.1016/S0065-3527(08)60726-5. [DOI] [PubMed] [Google Scholar]
- 89.Hutchinson E.C. Influenza Virus. Trends Microbiol. 2018;26:809–810. doi: 10.1016/j.tim.2018.05.013. [DOI] [PubMed] [Google Scholar]
- 90.World Health Organization Newsroom: Fact Sheets. Detail. Influenza (Seasonal) [(accessed on 1 May 2023)]. Available online: https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal)
- 91.Monath T.P., Vasconcelos P.F.C. Yellow Fever. J. Clin. Virol. 2015;64:160–173. doi: 10.1016/j.jcv.2014.08.030. [DOI] [PubMed] [Google Scholar]
- 92.World Health Organization Health Topics: Yellow-Fever. [(accessed on 1 May 2023)]. Available online: https://www.who.int/health-topics/yellow-fever.
- 93.Prusoff W.H. Synthesis and biological activities of iododeoxyuridine, an analog of thymidine. BBA—Biochim. Biophys. Acta. 1959;32:295–296. doi: 10.1016/0006-3002(59)90597-9. [DOI] [PubMed] [Google Scholar]
- 94.Cheng Y., Prusoff W.H. Relationship between the inhibition constant (&) and the concentration of inhibitor which causes 50 per cent inhibition (iso) of an enzymatic reaction. Biochem. Pharmacol. 1973;22:3099–3108. doi: 10.1016/0006-2952(73)90196-2. [DOI] [PubMed] [Google Scholar]
- 95.Kaufman H.E., Martola E.-L., Dohlman C. Use of 5-Iodo-2’-Deoxyuridine(IDU) in Treatment of Herpes Simplex Keratitis. Arch. Ophthalmol. 1962;68:235–239. doi: 10.1001/archopht.1962.00960030239015. [DOI] [PubMed] [Google Scholar]
- 96.De Clercq E., Li G. Approved Antiviral Drugs over the Past 50 Years. Clin. Microbiol. Rev. 2016;29:695–747. doi: 10.1128/CMR.00102-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Tchesnokov E.P., Feng J.Y., Porter D.P., Götte M. Mechanism of Inhibition of Ebola Virus RNA-Dependent RNA Polymerase by Remdesivir. Viruses. 2019;11:326. doi: 10.3390/v11040326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bergmann W., Feeney R.J.J. The isolation of a new thymine pentoside from sponges. J. Am. Chem. Soc. 1950;72:2809–2810. doi: 10.1021/ja01162a543. [DOI] [Google Scholar]
- 99.Wahyuni T.S., Widyawaruyanti A., Lusida M.I., Fuad A., Soetjipto, Fuchino H., Kawahara N., Hayashi Y., Aoki C., Hotta H. Inhibition of hepatitis C virus replication by chalepin and pseudane IX isolated from Ruta angustifolia leaves. Fitoterapia. 2014;99:276–283. doi: 10.1016/j.fitote.2014.10.011. [DOI] [PubMed] [Google Scholar]
- 100.Andersen R.J., Faulkner D.J., He C.H., Van Duyne G.D., Clardy J.J. Metabolites of the Marine Prosobranch Mollusc Lamellaria sp. Am. Chem. Soc. 1985;107:5492–5495. doi: 10.1021/ja00305a027. [DOI] [Google Scholar]
- 101.Hashimoto T., Akiyo Y., Akazawa K., Takaoka S., Tori M., Asakawa Y. Three novel dimethyl pyrroledicarboxylate, lycogarubins A C, from the myxomycetes lycogala epidendrum. Tetrahedron Lett. 1994;35:2559–2560. doi: 10.1016/S0040-4039(00)77170-X. [DOI] [Google Scholar]
- 102.Biedenkopf N., Lange-Grünweller K., Schulte F.W., Weiber A., Muller C., Becker D., Becker S., Hartmann R.K., Grünweller A. The natural compound silvestrol is a potent inhibitor of Ebola virus replication. Antivir. Res. 2017;137:76–81. doi: 10.1016/j.antiviral.2016.11.011. [DOI] [PubMed] [Google Scholar]
- 103.Cui H., Xu B., Wu T., Xu J., Yuan Y., Gu Q.J. Potential Antiviral Lignans from the Roots of Saururus chinensis with Activity against Epstein−Barr Virus Lytic Replication. Nat. Prod. 2014;77:100–110. doi: 10.1021/np400757k. [DOI] [PubMed] [Google Scholar]
- 104.Perez R.M. Antiviral Activity of Compounds Isolated From Plants. Pharm. Biol. 2003;41:107–157. doi: 10.1076/phbi.41.2.107.14240. [DOI] [Google Scholar]
- 105.Chen H., Ma Y.B., Huang X.Y., Geng C.A., Zhao Y., Wang L.J., Guo R.H., Liang W.J., Zhang X.M., Chen J.J. Synthesis, structure–activity relationships and biological evaluation of dehydroandrographolide and andrographolide derivatives as novel anti-hepatitis B virus agents. Bioorg. Med. Chem. Lett. 2014;24:2353–2359. doi: 10.1016/j.bmcl.2014.03.060. [DOI] [PubMed] [Google Scholar]
- 106.Geng C.A., Chen J.J. The Progress of Anti-HBV Constituents from Medicinal Plants in China. Nat. Prod. Bioprospect. 2018;8:227–244. doi: 10.1007/s13659-018-0178-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Zhou N.J., Geng C.A., Huang X.Y., Ma Y.-B., Zhang X.M., Wang J.L., Chen J.J. Anti-Hepatitis B Virus Active Constituents from Swertia Chirayita. Fitoterapia. 2015;100:27–34. doi: 10.1016/j.fitote.2014.11.011. [DOI] [PubMed] [Google Scholar]
- 108.Baumann M., Baxendale I.R., Ley S.V., Nikbin N. An overview of the key routes to the best selling 5-membered ring heterocyclic pharmaceuticals. Beilstein J. Org. Chem. 2011;7:442–495. doi: 10.3762/bjoc.7.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Vitaku E., Smith D.T., Njardarson J.T. Analysis of the Structural Diversity, Substitution Patterns, and Frequency of Nitrogen Heterocycles among U.S. FDA Approved Pharmaceuticals. J. Med. Chem. 2014;57:10257–10274. doi: 10.1021/jm501100b. [DOI] [PubMed] [Google Scholar]
- 110.Delost M.D., Smith D.T., Anderson B.J., Njardarson J.T. From Oxiranes to Oligomers: Architectures of U.S. FDA Approved Pharmaceuticals Containing Oxygen Heterocycles. J. Med. Chem. 2018;61:10996–11020. doi: 10.1021/acs.jmedchem.8b00876. [DOI] [PubMed] [Google Scholar]
- 111.De Clercq E. Fifty Years in Search of Selective Antiviral Drugs. J. Med. Chem. 2019;62:7322–7339. doi: 10.1021/acs.jmedchem.9b00175. [DOI] [PubMed] [Google Scholar]
- 112.McKeage K., Perry C.M., Keam S.J. Darunavir: A review of its use in the management of HIV infection in adults. Drugs. 2009;69:477–503. doi: 10.2165/00003495-200969040-00007. [DOI] [PubMed] [Google Scholar]
- 113.Kevin M., BelykHenry G., MorrisonAmar J., MahajanDaniel J. KumkeHsien-Hsin TungLawrence WaiVanessa Pruzinsky. Potassium Salt of an HIV Integrase Inhibitor. U.S. Patent No.: US 7,754,731 B2. 2006 July 8;
- 114.Ray P.C., Tummanapalli J.M.C., Gorantla S.R. Process for the Largescale Production of Stavudine. U.S. Patent No.: US 8,026,356 B2. 2007 May 31;
- 115.Leonis G., Czyżnikowska Ż., Megariotis G., Reis H., Papadopoulos M.G.J. Computational Studies of Darunavir into HIV-1 Protease and DMPC Bilayer: Necessary Conditions for Effective Binding and the Role of the Flaps. Chem. Inf. Model. 2012;52:1542–1558. doi: 10.1021/ci300014z. [DOI] [PubMed] [Google Scholar]
- 116.Vellanki S.R.P., Sahu A., Katukuri A.K., Vanama V., Kothari S., Ponnekanti V.S., Datta D. Process for the Preparation of Darunavir. U.S. Patent No. US8703980B2. 2019 September 17;
- 117.Ghosh A.K., Martyr C.D. Modern Drug Synthesis. John Wiley & Sons, Inc.; Hoboken, NJ, USA: 2010. Darunavir (Prezista): A HIV-1 Protease Inhibitor for Treatment of Multidrug-Resistant HIV; pp. 29–44. [DOI] [Google Scholar]
- 118.Koh Y., Matsumi S., Das D., Amano M., Davis D.A., Li J.F., Leschenko S., Baldridge A., Shioda T., Yarchoan R., et al. Potent Inhibition of HIV-1 Replication by Novel Non-peptidyl Small Molecule Inhibitors of Protease Dimerization. J. Biol Chem. 2007;282:28709–28720. doi: 10.1074/jbc.M703938200. [DOI] [PubMed] [Google Scholar]
- 119.Fujimoto H., Higuchi M., Watanabe H., Koh Y., Ghosh A.K., Mitsuya H., Tanoue N., Hamada A., Saito H. P-Glycoprotein Mediates Efflux Transport of Darunavir in Human Intestinal Caco-2 and ABCB1 Gene-Transfected Renal LLC-PK1 Cell Lines. Biol. Pharm. Bull. 2009;32:1588–1593. doi: 10.1248/bpb.32.1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Koh Y., Nakata H., Maeda K., Ogata H., Bilcer G., Devasamudram T., Kincaid J.F., Boross P., Wang Y.F., Tie Y., et al. Novel bis-Tetrahydrofuranylurethane-Containing Nonpeptidic Protease Inhibitor (PI) UIC-94017 (TMC114) with Potent Activity against Multi-PI-Resistant Human Immunodeficiency Virus In Vitro. Antimicrob. Agents Chemother. 2003;47:3123–3129. doi: 10.1128/AAC.47.10.3123-3129.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Ghosh A.K., Sridhar P.R., Leshchenko S., Hussain A.K., Li J., Kovalevsky A.Y., Walters D.E., Wedekind J.E., Grum-Tokars V., Das D., et al. Structure-Based Design of Novel HIV-1 Protease Inhibitors To Combat Drug Resistance. J. Med. Chem. 2006;49:5252–5261. doi: 10.1021/jm060561m. [DOI] [PubMed] [Google Scholar]
- 122.Davis D.A., Soule E.E., Davidoff K.S., Daniels S.I., Naiman N.E., Yarchoan R. Activity of Human Immunodeficiency Virus Type 1 Protease Inhibitors against the Initial Autocleavage in Gag-Pol Polyprotein Processing. Antimicrob. Agents Chemother. 2012;56:3620–3628. doi: 10.1128/AAC.00055-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Modh R.P., De Clercq E., Pannecouque C., Chikhalia K.H.J. Design, synthesis, antimicrobial activity and anti-HIV activity evaluation of novel hybrid quinazoline–triazine derivatives. Enzym. Inhib. Med. Chem. 2014;29:100–108. doi: 10.3109/14756366.2012.755622. [DOI] [PubMed] [Google Scholar]
- 124.Xu Z., Zhao S.J., Lv Z.S., Gao F., Wang Y., Zhang F., Bai L., Deng J.L. Fluoroquinolone-isatin hybrids and their biological activities. Eur. J. Med. Chem. 2019;162:396–406. doi: 10.1016/j.ejmech.2018.11.032. [DOI] [PubMed] [Google Scholar]
- 125.Banerjee D., Yogeeswari P., Bhat P., Thomas A., Srividya M., Sriram D. Novel isatinyl thiosemicarbazones derivatives as potential molecule to combat HIV-TB co-infection. Eur. J. Med. Chem. 2011;46:106–121. doi: 10.1016/j.ejmech.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 126.Pandeya S.N., Sriram D., Nath G., DeClercq E. Synthesis, antibacterial, antifungal and anti-HIV activities of Schiff and Mannich bases derived from isatin derivatives and N-[4-(49-chlorophenyl)thiazol-2-yl] thiosemicarbazide. Eur. J. Pharm. Sci. 1999;9:25–31. doi: 10.1016/S0928-0987(99)00038-X. [DOI] [PubMed] [Google Scholar]
- 127.Bal T.R., Anand B., Yogeeswari P., Sriram D. Synthesis and evaluation of anti-HIV activity of isatin b-thiosemicarbazone derivatives. Bioorg. Med. Chem. Lett. 2005;15:4451–4455. doi: 10.1016/j.bmcl.2005.07.046. [DOI] [PubMed] [Google Scholar]
- 128.Shen C.-H., Wang Y.-F., Kovalevsky A.Y., Harrison R.W., Weber I.T. Amprenavir complexes with HIV-1 protease and its drug-resistant mutants altering hydrophobic clusters. FEBS J. 2010;277:3699–3714. doi: 10.1111/j.1742-4658.2010.07771.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Weber I.T., Waltman M.J., Mustyakimov M., Blakeley M.P., Keen D.A., Ghosh A.K., Langan P., Kovalevsky A.Y. Joint X-ray/Neutron Crystallographic Study of HIV-1 Protease with Clinical Inhibitor Amprenavir: Insights for Drug Design. J. Med. Chem. 2013;56:5631–5635. doi: 10.1021/jm400684f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Gadakh S.K., Santhosh Reddy R., Sudalai A. Enantioselective synthesis of HIV protease inhibitor amprenavir via Co-catalyzed HKR of 2-(1-azido-2-phenylethyl)oxirane. Tetrahedron Asymmetry. 2012;23:898–903. doi: 10.1016/j.tetasy.2012.06.003. [DOI] [Google Scholar]
- 131.Fan L.L., Liu W.Q., Xu H., Yang L.M., Lv M., Zheng Y.T. Anti Human Immunodeficiency Virus-1 (HIV-1) Agents 3. Synthesis and in Vitro Anti-HIV-1 Activity of Some N-Arylsulfonylindoles. Chem. Pharm. Bull. 2009;57:797–800. doi: 10.1248/cpb.57.797. [DOI] [PubMed] [Google Scholar]
- 132.Ali A., Reddy G.S.K.K., Cao H., Anjum S.G., Nalam M.N.L., Schiffer C.A., Rana T.M. Discovery of HIV-1 Protease Inhibitors with Picomolar Affinities Incorporating N-Aryl-oxazolidinone-5-carboxamides as Novel P2 Ligands. J. Med. Chem. 2006;49:7342–7356. doi: 10.1021/jm060666p. [DOI] [PubMed] [Google Scholar]
- 133.Yan J., Huang N., Li S., Yang L.M., Xing W., Zheng Y.T., Hu Y. Synthesis and biological evaluation of novel amprenavir-based P1-substituted bi-aryl derivatives as ultra-potent HIV-1 protease inhibitors. Bioorg. Med. Chem. Lett. 2012;22:1976–1979. doi: 10.1016/j.bmcl.2012.01.037. [DOI] [PubMed] [Google Scholar]
- 134.Tie Y., Boross P.I., Wang Y.F., Gaddis L., Hussain A.K., Leshchenko S., Ghosh A.K., Louis J.M., Harrison R.W., Weber I.T.J. High Resolution Crystal Structures of HIV-1 Protease with a Potent Non-peptide Inhibitor (UIC-94017) Active Against Multi-drug-resistant Clinical Strains. Mol. Biol. 2004;338:341–352. doi: 10.1016/j.jmb.2004.02.052. [DOI] [PubMed] [Google Scholar]
- 135.Shahabadi N., Abbasi A.R., Moshtkob A., Shiri F.J. DNA-binding studies of a new Cu(II) complex containing reverse transcriptase inhibitor and anti-HIV drug zalcitabine. Coord. Chem. 2019;72:1957–1972. doi: 10.1080/00958972.2019.1620216. [DOI] [Google Scholar]
- 136.Brower E.T., Bacha U.M., Kawasaki Y., Freire E. Title of article. Chem. Biol. Drug Des. 2008;71:298–305. doi: 10.1111/j.1747-0285.2008.00647.x. [DOI] [PubMed] [Google Scholar]
- 137.Gulick R.M., Lalezari J., Goodrich J., Clumeck N., DeJesus E., Horban A., Nadler J., Clotet B., Karlsson A., Wohlfeiler M., et al. Maraviroc for Previously Treated Patients with R5 HIV-1 Infection. N. Engl. J. Med. 2008;359:1429–1441. doi: 10.1056/NEJMoa0803152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.De Clercq E. Where rilpivirine meets with tenofovir, the start of a new anti-HIV drug combination era. Biochem. Pharmacol. 2012;84:241–248. doi: 10.1016/j.bcp.2012.03.024. [DOI] [PubMed] [Google Scholar]
- 139.Orkin C., Llibre J.M., Gallien S., Antinori A., Behrens G.M.N., Carr A. Nucleoside reverse transcriptase inhibitor-reducing strategies in HIV treatment: Assessing the evidence. HIV Med. 2018;19:18–32. doi: 10.1111/hiv.12534. [DOI] [PubMed] [Google Scholar]
- 140.Clement M.E., Kofron R., Landovitz R.J. Long-acting injectable cabotegravir for the prevention of HIV infection. Curr. Opin. HIV AIDS. 2020;15:19. doi: 10.1097/COH.0000000000000597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Molina J.-M., Segal-Maurer S., Stellbrink H.J., Castagna A., Berhe M., Richmond G.J., Ruane P.J., Sinclair G.I., Siripassorn K., Wang H.J., et al. Efficacy and Safety of Long-Acting Subcutaneous Lenacapavir in Phase 2/3 in Heavily Treatment-Experienced People with HIV: Week 26 Results (Capella Study) [(accessed on 29 November 2021)]. Available online: https://theprogramme.ias2021.org/Abstract/Abstract/2605.
- 142.Curreli F., Choudhury S., Pyatkin I., Zagorodnikov V.P., Bulay A.K., Altieri A., Kwon Y.D., Kwong P.D., Debnath A.K.J. Design, Synthesis, and Antiviral Activity of Entry Inhibitors That Target the CD4-Binding Site of HIV-1. Med. Chem. 2012;55:4764–4775. doi: 10.1021/jm3002247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Lobatón E., Rodríguez-Barrios F., Gago F., Pérez-Pérez M.-J., De Clercq E., Balzarini J., Camarasa M.-J., Velázquez S. Synthesis of 3′′-Substituted TSAO Derivatives with Anti-HIV-1 and Anti-HIV-2 Activity through an Efficient Palladium-Catalyzed Cross-Coupling Approach. J. Med. Chem. 2002;45:3934–3945. doi: 10.1021/jm020820h. [DOI] [PubMed] [Google Scholar]
- 144.Kageyama M., Nagasawa T., Yoshida M., Ohrui H., Kuwahara S. Enantioselective Total Synthesis of the Potent Anti-HIV Nucleoside EFdA. Org. Lett. 2011;13:5264–5266. doi: 10.1021/ol202116k. [DOI] [PubMed] [Google Scholar]
- 145.Wu T., Froeyen M., Kempeneers V., Pannecouque C., Wang J., Busson R., De Clercq E., Herdewijn P.J. Deoxythreosyl Phosphonate Nucleosides as Selective Anti-HIV Agents. Am. Chem. Soc. 2005;127:5056–5065. doi: 10.1021/ja043045z. [DOI] [PubMed] [Google Scholar]
- 146.Ali A., Ghosh A., Nathans R.S., Sharova N., O’Brien S., Cao H., Stevenson M., Rana T.M. Identification of Flavopiridol Analogues that Selectively Inhibit Positive Transcription Elongation Factor (P-TEFb) and Block HIV-1 Replication. ChemBioChem. 2009;10:2072–2080. doi: 10.1002/cbic.200900303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Suzuki Y., Ikeda K., Suzuki F., Toyota J., Karino Y., Chayama K., Kawakami Y., Ishikawa H., Watanabe H., Hu W., et al. Dual oral therapy with daclatasvir and asunaprevir for patients with HCV genotype 1b infection and limited treatment options. J. Hepatol. 2013;58:655–662. doi: 10.1016/j.jhep.2012.09.037. [DOI] [PubMed] [Google Scholar]
- 148.Soumana D.I., Ali A., Schiffer C.A. Structural Analysis of Asunaprevir Resistance in HCV NS3/4A Protease. ACS Chem. Biol. 2014;9:2485–2490. doi: 10.1021/cb5006118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Scola P.M., Sun L.Q., Wang A.X., Chen J., Sin N., Venables B.L., Sit S.Y., Chen Y., Cocuzza A., Bilder D.M., et al. The Discovery of Asunaprevir (BMS-650032), An Orally Efficacious NS3 Protease Inhibitor for the Treatment of Hepatitis C Virus Infection. J. Med. Chem. 2014;57:1730–1752. doi: 10.1021/jm500297k. [DOI] [PubMed] [Google Scholar]
- 150.Lok A.S., Gardiner D.F., Lawitz E., Martorell C., Everson G.T., Ghalib R., Reindollar R., Rustgi V., McPhee F., Wind-Rotolo M. Preliminary Study of Two Antiviral Agents for Hepatitis C Genotype 1. N. Engl. J. Med. 2012;366:216–224. doi: 10.1056/NEJMoa1104430. [DOI] [PubMed] [Google Scholar]
- 151.Kumar D.V., Rai R., Brameld K.A., Riggs J., Somoza J.R., Rajagopalan R., Janc J.W., Xia Y.M., Ton T.L., Hu H., et al. 3-Heterocyclyl quinolone inhibitors of the HCV NS5B polymerase. Bioorg. Med. Chem. Lett. 2012;22:300–304. doi: 10.1016/j.bmcl.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 152.McKercher G., Beaulieu P.L., Lamarre D., LaPlante S., Lefebvre S., Pellerin C., Thauvette L., Kukolj G. Specific inhibitors of HCV polymerase identified using an NS5B with lower affinity for template/primer substrate. Nucleic Acids Res. 2004;32:422–431. doi: 10.1093/nar/gkh160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Kumar D.V., Rai R., Brameld K.A., Somoza J.R., Rajagopalan R., Janc J.W., Xia Y.M., Ton T.L., Shaghafi M.B., Hu H. Quinolones as HCV NS5B polymerase inhibitors. Bioorg. Med. Chem. Lett. 2011;21:82–87. doi: 10.1016/j.bmcl.2010.11.068. [DOI] [PubMed] [Google Scholar]
- 154.Han J., Lee M.K., Jang Y., Cho W.J., Kim M. Repurposing of cyclophilin A inhibitors as broad-spectrum antiviral agents. Drug Discov. Today. 2022;27:1895–1912. doi: 10.1016/j.drudis.2022.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.El Kassas M., Elbaz T., Abd El Latif Y., Esmat G. Elbasvir and grazoprevir for chronic hepatitis C genotypes 1 and 4. Expert Rev. Clin. Pharmacol. 2016;9:1413–1421. doi: 10.1080/17512433.2016.1233813. [DOI] [PubMed] [Google Scholar]
- 156.Sofia M.J., Bao D., Chang W., Du J., Nagarathnam D., Rachakonda S., Reddy P.G., Ross B.S., Wang P., Zhang H.R., et al. Discovery of a β-D-20 -Deoxy-20 -r-fluoro-20 -β-C-methyluridine Nucleotide Prodrug (PSI-7977) for the Treatment of Hepatitis C Virus. J. Med. Chem. 2010;53:7202–7218. doi: 10.1021/jm100863x. [DOI] [PubMed] [Google Scholar]
- 157.Link J.O., Taylor J.G., Xu L., Mitchell M., Guo H., Liu H., Kato D., Kirschberg T., Sun J., Squires N., et al. Discovery of Ledipasvir (GS-5885): A Potent, Once-Daily Oral NS5A Inhibitor for the Treatment of Hepatitis C Virus Infection. J. Med. Chem. 2014;57:2033–2046. doi: 10.1021/jm401499g. [DOI] [PubMed] [Google Scholar]
- 158.Znabet A., Polak M.M., Janssen E., De Kanter F.J.J., Turner N.J., Orru R.V.A., Ruijter E. A highly efficient synthesis of telaprevir by strategic use of biocatalysis and multicomponent reactions. Chem. Commun. 2010;46:7918–7920. doi: 10.1039/c0cc02823a. [DOI] [PubMed] [Google Scholar]
- 159.Xu F., Kim J., Waldman J., Wang T., Devine P. Synthesis of Grazoprevir, a Potent NS3/4a Protease Inhibitor for the Treatment of Hepatitis C Virus. Org. Lett. 2018;20:7261–7265. doi: 10.1021/acs.orglett.8b03173. [DOI] [PubMed] [Google Scholar]
- 160.Rusere L.N., Matthew A.N., Lockbaum G.J., Jahangir M., Newton A., Petropoulos C.J., Huang W., Kurt Yilmaz N., Schiffer C.A., Ali A. Quinoxaline-Based Linear HCV NS3/4A Protease Inhibitors Exhibit Potent Activity Against Drug Resistant Variants. ACS Med. Chem. Lett. 2018;9:691–696. doi: 10.1021/acsmedchemlett.8b00150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Matthew A.N., Zephyr J., Hill C.J., Jahangir M., Newton A., Petropoulos C.J., Huang W., Kurt-Yilmaz N., Schiffer C.A., Ali A. Hepatitis C Virus NS3/4A Protease Inhibitors Incorporating Flexible P2 Quinoxalines Target Drug Resistant Viral Variants. J. Med. Chem. 2017;60:5699–5716. doi: 10.1021/acs.jmedchem.7b00426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Roth D., Nelson D.R., Bruchfeld A., Liapakis A., Silva M., Monsour H., Martin P., Pol S., Londoño M.C., Hassanein T. Grazoprevir plus elbasvir in treatment-naive and treatment-experienced patients with hepatitis C virus genotype 1 infection and stage 4–5 chronic kidney disease (the C-SURFER study): A combination phase 3 study. Lancet. 2015;386:1537–1545. doi: 10.1016/S0140-6736(15)00349-9. [DOI] [PubMed] [Google Scholar]
- 163.De Clercq E. Current race in the development of DAAs (direct-acting antivirals) against HCV. Biochem. Pharmacol. 2014;89:441–452. doi: 10.1016/j.bcp.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 164.DeCarolis D.D., Chen Y.C., Westanmo A.D., Conley C., Gravely A.A., Khan F.B. Decreased warfarin sensitivity among patients treated with elbasvir and grazoprevir for hepatitis C infection. Am. J. Health Pharm. 2019;76:1273–1280. doi: 10.1093/ajhp/zxz127. [DOI] [PubMed] [Google Scholar]
- 165.Keating G.M., Vaidya A. Sofosbuvir: First Global Approval. Drugs. 2014;74:273–282. doi: 10.1007/s40265-014-0179-7. [DOI] [PubMed] [Google Scholar]
- 166.Lee C. Daclatasvir: Potential role in hepatitis C. Drug Des. Dev. Ther. 2013;7:1223–1233. doi: 10.2147/DDDT.S40310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Shannon A., Fattorini V., Sama B., Selisko B., Feracci M., Falcou C., Gauffre P., El Kazzi P., Delpal A., Decroly E., et al. A dual mechanism of action of AT-527 against SARS-CoV-2 polymerase. Nat. Commun. 2022;13:621–630. doi: 10.1038/s41467-022-28113-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Abdel-Magid A.F. Fatty Acid Synthase Inhibitors as Possible Treatment for Cancer. ACS Med. Chem. Lett. 2012;3:612–613. doi: 10.1021/ml3001566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Oslob J.D., Johnson R.J., Cai H., Feng S.Q., Hu L., Kosaka Y., Lai J., Sivaraja M., Tep S., Yang H., et al. Imidazopyridine-Based Fatty Acid Synthase Inhibitors That Show Anti-HCV Activity and in Vivo Target Modulation. ACS Med. Chem. Lett. 2013;4:113–117. doi: 10.1021/ml300335r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Lohmann V., Korner F., Koch J., Herian U., Theilmann L., Bartenschlager R. Replication of Subgenomic Hepatitis C Virus RNAs in a Hepatoma Cell Line. Science. 1999;285:110–113. doi: 10.1126/science.285.5424.110. [DOI] [PubMed] [Google Scholar]
- 171.Wang N.Y., Xu Y., Zuo W.Q., Xiao K.J., Liu L., Zeng X.X., You X.Y., Zhang L.D., Gao C., Liu Z.H., et al. Discovery of imidazo[2,1-b]thiazole HCV NS4B inhibitors exhibiting synergistic effect with other direct-acting antiviral agents. J. Med. Chem. 2015;58:2764–2778. doi: 10.1021/jm501934n. [DOI] [PubMed] [Google Scholar]
- 172.Matthews G.V., Seaberg E., Dore G.J., Bowden S., Lewin S.R., Sasadeusz J., Marks P., Goodman Z., Philp F.H., Tang Y. Combination HBV therapy is linked to greater HBV DNA suppression in a cohort of lamivudineexperienced HIV/HBV coinfected individuals. AIDS. 2009;23:1707–1715. doi: 10.1097/QAD.0b013e32832b43f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Li J., Lv F. Process for Stereoselective Synthesis of Lamvudine. U.S. Patent No.: US 8,304,540 B2. 2007 May 18;
- 174.Caso M.F., Dalonzo D., Derrico S., Palumbo G., Guaragna A. Highly Stereoselective Synthesis of Lamivudine (3TC) and Emtricitabine (FTC) by a Novel N-Glycosidation Procedure. Org. Lett. 2015;17:2626–2629. doi: 10.1021/acs.orglett.5b00982. [DOI] [PubMed] [Google Scholar]
- 175.Lok A.S.F., McMahon B.J. Chronic Hepatitis B: Update 2009. Hepatology. 2009;50:661–662. doi: 10.1002/hep.23190. [DOI] [PubMed] [Google Scholar]
- 176.Yasutake Y., Hattori S., Hayashi H., Matsuda K., Tamura N., Kohgo S., Maeda K., Mitsuya H. HIV-1 with HBV-associated Q151M substitution in RT becomes highly susceptible to entecavir: Structural insights into HBV-RT inhibition by entecavir. Sci. Rep. 2018;8:1624–1636. doi: 10.1038/s41598-018-19602-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Parvez M.K., Al-Dosari M.S., Abdelwahid M.A.S., Alqahtani A.S., Alanzi A.R. Novel anti-hepatitis B virus-active catechin and epicatechin from Rhus tripartita. Exp. Ther. Med. 2022;23:398. doi: 10.3892/etm.2022.11325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Velasco J., Ariza X., Badía L., Bartra M., Berenguer R., Farràs J., Gallardo J., Garcia J., Gasanz Y.J. Total Synthesis of Entecavir. Org. Chem. 2013;78:5482–5491. doi: 10.1021/jo400607v. [DOI] [PubMed] [Google Scholar]
- 179.Li J.J. Innovative Drug Synthesis. John Wiley & Sons, Inc.; Hoboken, NJ, USA: 2015. pp. 1–14. [DOI] [Google Scholar]
- 180.Shaw T., Locarnini S. Entecavir for the treatment of chronic hepatitis B. Expert Rev. Anti. Infect. Ther. 2004;2:853–871. doi: 10.1586/14789072.2.6.853. [DOI] [PubMed] [Google Scholar]
- 181.Matthews S.J. Entecavir for the Treatment of Chronic Hepatitis B Virus Infection. Clin. Ther. 2006;28:184–203. doi: 10.1016/j.clinthera.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 182.Dai G.F., Xu H.W., Wang J.F., Liu F.W., Liu H.M. Studies on the novel a-glucosidase inhibitory activity and structure–activity relationships for andrographolide analogues. Bioorg. Med. Chem. Lett. 2006;16:2710–2713. doi: 10.1016/j.bmcl.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 183.Wu Y.H. Naturally derived anti-hepatitis B virus agents and their mechanism of action. World J. Gastroenterol. 2016;22:188–204. doi: 10.3748/wjg.v22.i1.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Sadiea R.Z., Sultana S., Chaki B.M., Islam T., Dash S., Akter S., Islam M.S., Kazi T., Nagata A., Spagnuolo R. Phytomedicines to Target Hepatitis B Virus DNA Replication: Current Limitations and Future Approaches. Int. J. Mol. Sci. 2022;23:1617. doi: 10.3390/ijms23031617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Poordad F., Sievert W., Mollison L., Bennett M., Tse E., Bräu N., Levin J., Sepe T., Lee S.S., Angus P., et al. Fixed-Dose Combination Therapy With Daclatasvir, Asunaprevir, and Beclabuvir for Noncirrhotic Patients With HCV Genotype 1 Infection. JAMA. 2015;313:1728–1735. doi: 10.1001/jama.2015.3860. [DOI] [PubMed] [Google Scholar]
- 186.Lai C.L., Gane E., Liaw Y.F., Hsu C.W., Thongsawat S., Wang Y., Chen Y., Heathcote E.J., Rasenack J., Bzowej N., et al. Telbivudine versus Lamivudine in Patients with Chronic Hepatitis B. N. Engl. J. Med. 2007;357:2576–2588. doi: 10.1056/NEJMoa066422. [DOI] [PubMed] [Google Scholar]
- 187.Lai C.L., Shouval D., Lok A.S., Chang T.T., Cheinquer H., Goodman Z., DeHertogh D., Wilber R., Zink R.C., Cross A., et al. Entecavir versus Lamivudine for Patients with HBeAg-Negative Chronic Hepatitis B. N. Engl. J. Med. 2006;354:1011–1020. doi: 10.1056/NEJMoa051287. [DOI] [PubMed] [Google Scholar]
- 188.Testoni B., Durantel D., Zoulim F. Novel targets for hepatitis B virus therapy. Liver Int. 2017;37:33–39. doi: 10.1111/liv.13307. [DOI] [PubMed] [Google Scholar]
- 189.Li X., Zhang Z., Chen Y., Wang B., Yang G., Xu X., Yechao B., Bai D., Feng B., Mao Y., et al. Discovery of SHR5133, a Highly Potent and Novel HBV Capsid Assembly Modulator. ACS Med. Chem. Lett. 2022;13:507–512. doi: 10.1021/acsmedchemlett.2c00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Yeo H., Li Y., Fu L., Zhu J.L., Gullen E.A., Dutschman G.E., Lee Y., Chung R., Huang E.-S., Austin D.J., et al. Synthesis and Antiviral Activity of Helioxanthin Analogues. J. Med. Chem. 2005;48:534–546. doi: 10.1021/jm034265a. [DOI] [PubMed] [Google Scholar]
- 191.Crotty S., Maag D., Arnold J.J., Zhong W., Lau J.Y.N., Hong Z., Andino R., Cameron C.E. The broad-spectrum antiviral ribonucleoside ribavirin is an RNA virus mutagen. Nat. Med. 2000;6:1375–1379. doi: 10.1038/82191. [DOI] [PubMed] [Google Scholar]
- 192.Kim Y.-I., Pareek R., Murphy R., Harrison L., Farrell E., Cook R., DeVincenzo J. The antiviral effects of RSV fusion inhibitor, MDT-637, on clinical isolates, versus its achievable concentrations in the human respiratory tract and comparison to ribavirin. Influenza Other Respi. Viruses. 2017;11:525–530. doi: 10.1111/irv.12503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Sakharov V., Baykov S., Konstantinova I., Esipov R., Dorogov M. An Efficient Chemoenzymatic Process for Preparation of Ribavirin. Int. J. Chem. Eng. 2015;2015:734851. doi: 10.1155/2015/734851. [DOI] [Google Scholar]
- 194.Feld J.J., Hoofnagle J.H. Mechanism of action of interferon and ribavirin in treatment of hepatitis C. Nature. 2005;436:967–972. doi: 10.1038/nature04082. [DOI] [PubMed] [Google Scholar]
- 195.Yang Y., Rijnbrand R., McKnight K.L., Wimmer E., Paul A., Martin A., Lemon S.M. Sequence Requirements for Viral RNA Replication and VPg Uridylylation Directed by the Internal cis-Acting Replication Element (cre) of Human Rhinovirus Type 14. J. Virol. 2002;76:7485–7494. doi: 10.1128/JVI.76.15.7485-7494.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Nyström K., Waldenström J., Tang K.W., Lagging M. Ribavirin: Pharmacology, Multiple Modes of Action and Possible Future Perspectives. Sequence Requirements for Viral RNA Replication and VPg Uridylylation Directed by the Internal cis-Acting Replication Element (cre) of Human Rhinovirus Type 14. Future Virol. 2019;14:153–160. doi: 10.2217/fvl-2018-0166. [DOI] [Google Scholar]
- 197.Cameron C.E., Castro C. The mechanism of action of ribavirin: Lethal mutagenesis of RNA virus genomes mediated by the viral RNA-dependent RNA polymerase. Curr. Opin. Infect. Dis. 2001;14:757–764. doi: 10.1097/00001432-200112000-00015. [DOI] [PubMed] [Google Scholar]
- 198.Thomas E., Ghany M.G., Liang T.J. The application and mechanism of action of ribavirin in therapy of hepatitis C. Antivir. Chem. Chemother. 2012;23:1–12. doi: 10.3851/IMP2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Robinson R.F., Nahata M.C. Respiratory syncytial virus (RSV) immune globulin and palivizumab for prevention of RSV infection. Am. J. Health Pharm. 2000;57:259–264. doi: 10.1093/ajhp/57.3.259. [DOI] [PubMed] [Google Scholar]
- 200.Wright M., Piedimonte G. Respiratory Syncytial Virus Prevention and Therapy: Past, Present, and Future. Pediatr. Pulmonol. 2011;46:324–347. doi: 10.1002/ppul.21377. [DOI] [PubMed] [Google Scholar]
- 201.Cockerill G.S., Angell R.M., Bedernjak A., Chuckowree I., Fraser I., Gascon-Simorte J., Gilman M.S.A., Good J.A.D., Harland R., Johnson S.M., et al. Discovery of Sisunatovir (RV521), an Inhibitor of Respiratory Syncytial Virus Fusion. J. Med. Chem. 2021;64:3658–3676. doi: 10.1021/acs.jmedchem.0c01882. [DOI] [PubMed] [Google Scholar]
- 202.Yoon J.J., Chawla D., Paal T., Ndungu M., Du Y.H., Kurtkaya S., Sun A.M., Snyder J.P., Plemper R.K.J. High-Throughput Screening–Based Identification of Paramyxovirus Inhibitors. Biomol. Screen. 2008;13:591–608. doi: 10.1177/1087057108321089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Yust I., Fox Z., Burke M., Johnson A., Turner D., Mocroft A., Katlama C., Ledergerber B., Reiss P., Kirk O. Retinal and extraocular cytomegalovirus end-organ disease in HIV-infected patients in Europe: A EuroSIDA study, 1994–2001. Eur. J. Clin. Microbiol. Infect. Dis. 2004;23:550–559. doi: 10.1007/s10096-004-1160-2. [DOI] [PubMed] [Google Scholar]
- 204.Babu K.S., Rao M.R., Goverdhan G., Srinivas P., Reddy P.P., Venkateswarlu G., Anand R.V. Synthesis of Valganciclovir Hydrochloride Congeners. Synth. Commun. 2013;43:1751–1758. doi: 10.1080/00397911.2011.651249. [DOI] [Google Scholar]
- 205.Wiltshire H., Paya C.V., Pescovitz M.D., Humar A., Dominguez E., Washburn K., Blumberg E., Alexander B., Freeman R., Heaton N. Pharmacodynamics of Oral Ganciclovir and Valganciclovir in Solid Organ Transplant Recipients. Transplantation. 2005;79:1477–1483. doi: 10.1097/01.TP.0000164512.99703.AD. [DOI] [PubMed] [Google Scholar]
- 206.Matthews T., Boehme R. Antiviral Activity and Mechanism of Action of Ganciclovir. Rev. Infect. Dis. 1988;10:490–494. doi: 10.1093/clinids/10.Supplement_3.S490. [DOI] [PubMed] [Google Scholar]
- 207.Gao H., Mitra A.K. Synthesis of Acyclovir, Ganciclovir and Their Prodrugs: A Review. Synthesis. 2000;2000:329–351. doi: 10.1055/s-2000-6333. [DOI] [Google Scholar]
- 208.Montana M., Montero V., Khoumeri O., Vanelle P. Quinoxaline Derivatives as Antiviral Agents: A Systematic Review. Molecules. 2020;25:2784. doi: 10.3390/molecules25122784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Wang Y., Mukhopadhyay R., Roy S., Kapoor A., Su Y.-P., Charman S.A., Chen G., Wu J., Wang X., Vennerstrom J.L. Inhibition of Cytomegalovirus Replication with Extended-HalfLife Synthetic Ozonides. Antimicrob. Agents Chemother. 2019;63:e01735-18. doi: 10.1128/AAC.01735-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.El-Zahab H.S.A. Synthesis, Characterization, and Biological Evaluation of Some Novel Quinoxaline Derivatives as Antiviral Agents. Arch. Pharm. Chem. Life Sci. 2017;350:1700028. doi: 10.1002/ardp.201700028. [DOI] [PubMed] [Google Scholar]
- 211.El-Sebaey S.A. Recent Advances in 1,2,4-Triazole Scaffolds as Antiviral Agents. ChemistrySelect. 2020;5:11654–11680. doi: 10.1002/slct.202002830. [DOI] [Google Scholar]
- 212.Kimberlin D.W., Jester P.M., Sánchez P.J., Ahmed A., Arav-Boger R., Michaels M.G., Ashouri N., Englund J.A., Estrada B., Jacobs R.F., et al. Valganciclovir for Symptomatic Congenital Cytomegalovirus Disease. N. Engl. J. Med. 2015;372:933–943. doi: 10.1056/NEJMoa1404599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Martin D.F., Kuppermann B.D., Wolitz R.A., Palestine A.G., Li H., Robinson C.A. Oral ganciclovir for patients with cytomegalovirus retinitis treated with a ganciclovir implant. N. Engl. J. Med. 1999;340:1063–1070. doi: 10.1056/NEJM199904083401402. [DOI] [PubMed] [Google Scholar]
- 214.Williams J.D., Chen J.J., Drach J.C., Townsend L.B. Design, Synthesis, and Antiviral Activity of Certain 3-Substituted 2,5,6-Trichloroindole Nucleosides. J. Med. Chem. 2004;47:5753–5765. doi: 10.1021/jm0400146. [DOI] [PubMed] [Google Scholar]
- 215.Turk S.R., Shipman C., Jr., Nassiri M.R., Genzlinger G., Krawczyk S.H., Townsend L.B., Drach J.C. Pyrrolo[2,3-d]Pyrimidine Nucleosides as Inhibitors of Human Cytomegalovirus. Antimicrob. Agents Chemother. 1987;31:544–550. doi: 10.1128/AAC.31.4.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Prichard M.N., Prichard L.E., Baguley W.A., Nassiri M.R., Shipman C., Jr. Three-Dimensional Analysis of the Synergistic Cytotoxicity of Ganciclovir and Zidovudine. Antivir. Res. 1991;35:1060–1065. doi: 10.1128/AAC.35.6.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Sahu P.K., Umme T., Yu J., Nayak A., Kim G., Noh M., Lee J.Y., Kim D.-D., Jeong L.S. Seleno-acyclovir and –ganciclovir: A Discovery of a New Template for Antiviral Agents. J. Med. Chem. 2015;58:8734–8738. doi: 10.1021/acs.jmedchem.5b00804. [DOI] [PubMed] [Google Scholar]
- 218.Zhou N., Xie T., Liu L., Xie Z.J. Cu/Mn Co-oxidized Cyclization for the Synthesis of Highly Substituted Pyrrole Derivatives from Amino Acid Esters: A Strategy for the Biomimetic Syntheses of Lycogarubin C and Chromopyrrolic Acid. Org. Chem. 2014;79:6061–6068. doi: 10.1021/jo500740w. [DOI] [PubMed] [Google Scholar]
- 219.Lin Z.Q., Li C.D., Zhou Z.C., Xue S., Gao J.R., Ye Q., Li Y.J. Copper(II)-Promoted Oxidation/[3+2]Cycloaddition/Aromatization Cascade: Efficient Synthesis of Tetrasubstituted NH-Pyrrole from Chalcones and Iminodiacetates. Synlett. 2019;30:1442–1446. doi: 10.1055/s-0039-1689972. [DOI] [Google Scholar]
- 220.Kaufman H.E., Heidelberger C. Therapeutic Antiviral Action of 5-Trifluoromethyl-2’-deoxyuridine in Herpes Simplex Keratitis. Science. 1964;145:585–586. doi: 10.1126/science.145.3632.585. [DOI] [PubMed] [Google Scholar]
- 221.De Clercq E. Discovery and development of BVDU (brivudin) as a therapeutic for the treatment of herpes zoster. Biochem. Pharmacol. 2004;68:2301–2315. doi: 10.1016/j.bcp.2004.07.039. [DOI] [PubMed] [Google Scholar]
- 222.McClain L., Zhi Y., Cheng H., Ghosh A., Piazza P., Yee M.B., Kumar S., Milosevic J., Bloom D.C., Arav-Boger R. Broad-spectrum non-nucleoside inhibitors of human herpesviruses. Antivir. Res. 2015;121:16–23. doi: 10.1016/j.antiviral.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Taylor J.L., Punda-Polic V., O’brien W.J. Combined anti-herpes virus activity of nucleoside analogs and interferon. Curr. Eye Res. 1991;10:205–211. doi: 10.3109/02713689109020381. [DOI] [PubMed] [Google Scholar]
- 224.Warren T.K., Jordan R., Lo M.K., Ray A.S., Mackman R.L., Soloveva V., Siegel D., Perron M., Bannister R., Hui H.C., et al. Therapeutic efficacy of the small molecule GS-5734 against Ebola virus in rhesus monkeys. Nature. 2016;531:381–385. doi: 10.1038/nature17180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Pardo J., Shukla A.M., Chamarthi G., Gupte A. The journey of remdesivir: From Ebola to COVID-19. Drugs Context. 2020;9:1–9. doi: 10.7573/dic.2020-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Chun B.K., Clarke M.O.H., Doerffler E., Hui H.C., Jordan R., Mackman R.L., Parrish J.P., Ray A.S., Siegel D., Gilead Sciences, Inc. Methods for Treating Filoviridae Virus Infections. Patent WO 2016069826 A1. 2016 July 5;
- 227.Taylor R., Kotian P., Warren T., Panchal R., Bavari S., Julander J., Dobo S., Rose A., El-Kattan Y., Taubenheim B., et al. BCX4430 – A broad-spectrum antiviral adenosine nucleoside analog under development for the treatment of Ebola virus disease. Infect. Public Health. 2016;9:220–226. doi: 10.1016/j.jiph.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.De Clercq E. Ebola virus (EBOV) infection: Therapeutic strategies. Biochem. Pharmacol. 2015;93:1–10. doi: 10.1016/j.bcp.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Picazo E., Giordanetto F. Small molecule inhibitors of ebola virus infection. Drug Discov. Today. 2015;20:277–286. doi: 10.1016/j.drudis.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 230.Shannon A., Canard B. Development of a robust and convenient dual-reporter high-throughput screening assay for SARS-CoV-2 antiviral drug discovery. Antivir. Res. 2023;210:105501–105516. doi: 10.1016/j.antiviral.2022.105501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Scott J.T., Sharma R., Meredith L.W., Dunning J., Moore C.E., Sahr F., Ward S., Goodfellow I., Horby P. Pharmacokinetics of TKM-130803 in Sierra Leonean patients with Ebola virus disease: Plasma concentrations exceed target levels, with drug accumulation in the most severe patients. EBioMedicine. 2020;52:102601–102611. doi: 10.1016/j.ebiom.2019.102601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Verdonck S., Pu S.Y., Sorrell F.J., Elkins J.M., Froeyen M., Gao L.J., Prugar L.I., Dorosky D.E., Brannan J.M., Barouch-Bentov R., et al. Synthesis and Structure−Activity Relationships of 3,5-Disubstitutedpyrrolo[2,3-b]pyridines as Inhibitors of Adaptor-Associated Kinase 1 with Antiviral Activity. J. Med. Chem. 2019;62:5810–5831. doi: 10.1021/acs.jmedchem.9b00136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Janeba Z. Development of Small-Molecule Antivirals for Ebola. Med. Res. Rev. 2015;35:1175–1194. doi: 10.1002/med.21355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W., Si H.R., Zhu Y., Li B., Huang C.L., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Mascellino M.T., Di Timoteo F., De Angelis M., Oliva A. Overview of the Main Anti-SARS-CoV-2 Vaccines: Mechanism of Action, Efficacy and Safety. Infect. Drug Resist. 2021;14:3459–3476. doi: 10.2147/IDR.S315727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Quiros-Roldan E., Amadasi S., Zanella I., Degli Antoni M., Storti S., Tiecco G., Castelli F. Monoclonal Antibodies against SARS-CoV-2: Current Scenario and Future Perspectives. Pharmaceuticals. 2021;14:1272. doi: 10.3390/ph14121272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Wang X., Sacramento C.Q., Jockusch S., Chaves O.A., Tao C., Fintelman-Rodrigues N., Chien M., Temerozo J.R., Li X., Kumar S., et al. Combination of antiviral drugs inhibits SARS-CoV-2 polymerase and exonuclease and demonstrates COVID-19 therapeutic potential in viral cell culture. Commun. Biol. 2022;5:154–168. doi: 10.1038/s42003-022-03101-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Dube T., Ghosh A., Mishra J., Kompella U.B., Panda J.J. Repurposed Drugs, Molecular Vaccines, Immune-Modulators, and Nanotherapeutics to Treat and Prevent COVID-19 Associated with SARS-CoV-2, a Deadly Nanovector. Adv. Ther. 2021;4:2000172–2000202. doi: 10.1002/adtp.202000172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Marzolini C., Kuritzkes D.R., Marra F., Boyle A., Gibbons S., Flexner C., Pozniak A., Boffito M., Waters L., Burger D. Recommendations for the Management of Drug–Drug Interactions Between the COVID-19 Antiviral Nirmatrelvir/Ritonavir (Paxlovid) and Comedications. Clin. Pharmacol. Ther. 2022;112:1191–1200. doi: 10.1002/cpt.2646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Rubin R. Baricitinib Is First Approved COVID-19 Immunomodulatory Treatment. JAMA. 2022;327:2281. doi: 10.1001/jama.2022.9846. [DOI] [PubMed] [Google Scholar]
- 241.Amici C., Di Caro A., Ciucci A., Chiappa L., Castilletti C., Martella V., Decaro N., Buonavoglia C., Capobianchi M.R., Santoro M.G. Indomethacin has a potent antiviral activity against SARS coronavirus. Antivir. Ther. 2006;11:1021–1030. doi: 10.1177/135965350601100803. [DOI] [PubMed] [Google Scholar]
- 242.Tegeder I., Pfeilschifter J., Geisslinger G. Cyclooxygenase-independent actions of cyclooxygenase inhibitors. FASEB J. 2001;15:2057–2072. doi: 10.1096/fj.01-0390rev. [DOI] [PubMed] [Google Scholar]
- 243.Wood J.M., Evans G.B., Grove T.L., Almo S.C., Cameron S.A., Furneaux R.H., Harris L.D.J. Chemical Synthesis of the Antiviral Nucleotide Analogue ddhCTP. Org. Chem. 2021;86:8843–8850. doi: 10.1021/acs.joc.1c00761. [DOI] [PubMed] [Google Scholar]
- 244.Stachulski A.V., Taujanskas J., Pate S.L., Rajoli R.K.R., Aljayyoussi G., Pennington S.H., Ward S.A., Hong W.D., Biagini G.A., Owen A., et al. Therapeutic Potential of Nitazoxanide: An Appropriate Choice for Repurposing versus SARS-CoV-2? ACS Infect. Dis. 2021;7:1317–1331. doi: 10.1021/acsinfecdis.0c00478. [DOI] [PubMed] [Google Scholar]
- 245.Gizzi A.S., Grove T.L., Arnold J.J., Jose J., Jangra R.K., Garforth S.J., Du Q., Cahill S.M., Dulyaninova N.G., Love J.D., et al. A naturally occurring antiviral ribonucleotide encoded by the human genome. Nature. 2018;558:610–614. doi: 10.1038/s41586-018-0238-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Jung E., Soto-Acosta R., Xie J., Wilson D.J., Dreis C.D., Majima R., Edwards T.C., Geraghty R.J., Chen L. Bisubstrate Inhibitors of Severe Acute Respiratory Syndrome Coronavirus-2 Nsp14 Methyltransferase. ACS Med. Chem. Lett. 2022;13:1477–1484. doi: 10.1021/acsmedchemlett.2c00265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Braaten K.P., Laufer M.R. Human Papillomavirus (HPV), HPV-Related Disease, and the HPV Vaccine. Rev. Obstet. Gynecol. 2008;1:2–10. [PMC free article] [PubMed] [Google Scholar]
- 248.Rivera A., Tyring S.K. Therapy of cutaneous human Papillomavirus infections. Dermatol. Ther. 2004;17:441–448. doi: 10.1111/j.1396-0296.2004.04047.x. [DOI] [PubMed] [Google Scholar]
- 249.Beadle J.R., Valiaeva N., Yang G., Yu J.H., Broker T.R., Aldern K.A., Harden E.A., Keith K.A., Prichard M.N., Hartman T., et al. Synthesis and Antiviral Evaluation of Octadecyloxyethyl Benzyl 9-[(2- Phosphonomethoxy)ethyl]guanine (ODE-Bn-PMEG), a Potent Inhibitor of Transient HPV DNA Amplification. J. Med. Chem. 2016;59:10470–10478. doi: 10.1021/acs.jmedchem.6b00659. [DOI] [PubMed] [Google Scholar]
- 250.Briggs D.J. The role of vaccination in rabies prevention. Curr. Opin. Virol. 2012;2:309–314. doi: 10.1016/j.coviro.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 251.Da Silva S., Oliveira Silva Martins D., Jardim A.C. A Review of the Ongoing Research on Zika Virus Treatment. Viruses. 2018;10:255. doi: 10.3390/v10050255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Barrows N.J., Campos R.K., Powell S.T., Prasanth K.R., Schott-Lerner G., Soto-Acosta R., Galarza-Muñoz G., McGrath E.L., Urrabaz-Garza R., Gao J. A Screen of FDA-Approved Drugs for Inhibitors of Zika Virus Infection. Cell Host Microbe. 2016;20:259–270. doi: 10.1016/j.chom.2016.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Zhou K., Li C., Shi W., Hu X., Nandakumar K.S., Jiang S., Zhang N. Current Progress in the Development of Zika Virus Vaccines. Vaccines. 2021;9:1004. doi: 10.3390/vaccines9091004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Yao Y., Huo T., Lin Y.L., Nie S., Wu F., Hua Y., Wu J., Kneubehl A.R., Vogt M.B., Rico-Hesse R., et al. Discovery, X-ray Crystallography and Antiviral Activity of Allosteric Inhibitors of Flavivirus NS2B-NS3 Protease. Am. Chem. Soc. 2019;141:6832–6836. doi: 10.1021/jacs.9b02505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Tricarico P.M., Caracciolo I., Crovella S., D’Agaro P. Zika virus induces inflammasome activation in the glial cell line U87-MG. Biochem. Biophys. Res. Commun. 2017;492:597–602. doi: 10.1016/j.bbrc.2017.01.158. [DOI] [PubMed] [Google Scholar]
- 256.Lahon A., Arya R.P., Kneubehl A.R., Vogt M.B., Dailey Garnes N.J.M., Rico-Hesse R. Characterization of a Zika Virus Isolate from Colombia. PLoS Negl. Trop. Dis. 2016;10:e0005019. doi: 10.1371/journal.pntd.0005019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Zhu Y., Liang M., Yu J., Zhang B., Zhu G., Huang Y., He Z., Yuan J. Repurposing of Doramectin as a New Anti-Zika Virus Agent. Viruses. 2023;15:1068. doi: 10.3390/v15051068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Martinez-Lopez A., Persaud M., Chavez M.P., Zhang H., Rong L., Liu S., Wang T.T., Sarafianos S.G., Diaz-Griffero F. Glycosylated diphyllin as a broad-spectrum antiviral agent against Zika virus. EBioMedicine. 2019;47:269–283. doi: 10.1016/j.ebiom.2019.08.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Li P.C., Jang J., Hsia C.Y., Groomes P.V., Lian W., de Wispelaere M., Pitts J.D., Wang J., Kwiatkowski N., Gray N.S., et al. Small Molecules Targeting the Flavivirus E Protein with Broad-Spectrum Activity and Antiviral Efficacy in Vivo. ACS Infect. Dis. 2019;5:460–472. doi: 10.1021/acsinfecdis.8b00322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Lian W., Jang J., Potisopon S., Li P.C., Rahmeh A., Wang J., Kwiatkowski N.P., Gray N.S., Yang P.L. Discovery of Immunologically Inspired Small Molecules That Target the Viral Envelope Protein. ACS Infect. Dis. 2018;4:1395–1406. doi: 10.1021/acsinfecdis.8b00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Murdin A.D., Barreto L., Plotkin S. Inactivated poliovirus vaccine: Past and present experience. Vaccine. 1996;14:735–746. doi: 10.1016/0264-410X(95)00211-I. [DOI] [PubMed] [Google Scholar]
- 262.Amanna I.J., Slifka M.K. Current trends in West Nile virus vaccine development. Expert Rev. Vaccines. 2014;13:589–608. doi: 10.1586/14760584.2014.906309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Harder T., Siedler A. Systematic Review and Meta-analysis of Chickenpox Vaccination and Risk of Herpes Zoster: A Quantitative View on the “Exogenous Boosting Hypothesis”. Clin. Infect. Dis. 2019;69:1329–1338. doi: 10.1093/cid/ciy1099. [DOI] [PubMed] [Google Scholar]
- 264.Davidson R.N., Lynn W., Savage P., Wansbrough-Jones M.H. Chickenpox pneumonia: Experience with antiviral treatment. Thorax. 1988;43:627–630. doi: 10.1136/thx.43.8.627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Ward P., Small I., Smith J., Suter P., Dutkowski R.J. Oseltamivir (Tamiflu®) and its potential for use in the event of an influenza pandemic. Antimicrob. Chemother. 2005;55:5–21. doi: 10.1093/jac/dki018. [DOI] [PubMed] [Google Scholar]
- 266.Lin L.Z., Fang J.M. Total Synthesis of Anti-Influenza Agents Zanamivir and Zanaphosphor via Asymmetric Aza-Henry Reaction. Org. Lett. 2016;18:4400–4403. doi: 10.1021/acs.orglett.6b02131. [DOI] [PubMed] [Google Scholar]
- 267.Shie J.J., Fang J.M.J. Development of effective anti-influenza drugs: Congeners and conjugates – a review. Biomed. Sci. 2019;26:84–104. doi: 10.1186/s12929-019-0567-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Rowse M., Qiu S., Tsao J., Yamauchi Y., Wang G., Luo M. Reduction of Influenza Virus Envelope’s Fusogenicity by Viral Fusion Inhibitors. ACS Infect. Dis. 2016;2:47–53. doi: 10.1021/acsinfecdis.5b00109. [DOI] [PubMed] [Google Scholar]
- 269.DeFilippis V., Früh K. Host cell targets for antiviral therapy: An update. Future Virol. 2006;1:509–518. doi: 10.2217/17460794.1.4.509. [DOI] [Google Scholar]
- 270.Cha H.M., Kim U.I., Ahn S.B., Lee M.K., Lee H., Bang H., Jang Y., Kim S.S., Bae M.A., Kim K., et al. Evaluation of Antiviral Activity of Gemcitabine Derivatives against Influenza Virus and Severe Acute Respiratory Syndrome Coronavirus. ACS Infect. Dis. 2023;9:1033–1045. doi: 10.1021/acsinfecdis.3c00034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Das P., Deng X., Zhang L., Roth M.G., Fontoura B.M.A., Phillips M.A., De Brabander J.K. SAR-Based Optimization of a 4-Quinoline Carboxylic Acid Analogue with Potent Antiviral Activity. ACS Med. Chem. Lett. 2013;4:517–521. doi: 10.1021/ml300464h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Monath T.P. SAR-Based Optimization of a 4-Quinoline Carboxylic Acid Analogue with Potent Antiviral Activity. Lancet Infect. Dis. 2001;1:11–20. doi: 10.1016/S1473-3099(01)00016-0. [DOI] [PubMed] [Google Scholar]