Abstract
An impaired ability to evacuate the urinary bladder is commonly seen in both men and women with aging. Usually, patients present with a range of storage, voiding, and post-micturition urinary symptoms. It may eventually lead to urinary retention. These symptoms may have a considerable effect on the patient’s quality of life. Despite its common prevalence with advancing age, the etiopathogenesis of the underactive urinary bladder is incompletely understood. There are no widely agreed diagnostic criteria. The urodynamic study (UDS), an invasive investigation is the only accepted modality to diagnose underactive detrusor. There is a lack of effective treatments to improve bladder emptying. The goals of treatment are to improve symptoms and reduce the risk for the complications of impaired bladder emptying. We report a case of a 73 year male who came to us with a history of urinary symptoms and a distended abdomen.
Keywords: Distended abdomen, underactive, urinary bladder, urinary retention
Introduction
An underactive urinary bladder is a form of urinary bladder dysfunction that affects approximately 20% to 25% of all patients who present with urinary symptoms.[1] It is a symptom complex that is characterized by hesitancy, slow urinary stream, prolonged voiding time with or without the sensation of incomplete bladder emptying.[2] Currently, an invasive urodynamic study is the only investigation to estimate detrusor voiding function.[3] Management commonly involves bladder drainage techniques or drugs aimed at reducing bladder outflow resistance. We report an uncommon presentation of the underactive urinary bladder in a 73 years old male.
Case History
A male aged 73 years came to the emergency room with a history of abdominal distension for 2 months and frequency of micturition for 3-4 months. No history of fever, dysuria, hematuria, abdominal pain, vomiting, or constipation. No history of diabetes mellitus, neurological disorder, weight loss, or surgical intervention in the past. No history of drug intake except irregular antihypertensive treatment. There was a history of alcohol intake for more than 20 years.
Physical examination revealed a non-tender, distended abdomen. The fluid thrill was present. Shifting dullness was absent. Bowel sounds were normal. There was no pallor, Icterus, or cyanosis. External genitalia were normal. Digital rectal examination revealed Grade 1 prostate, normal anal tone, and empty rectum. Blood pressure was 180/110 mm of Hg. A clinical diagnosis of abdominal ascites with hypertension was made and the patient was admitted under the medicine department for further management. Blood investigations revealed hemoglobin 15.1 g/dl, Serum creatinine of 2.16 mg/dl. Serum electrolytes and Liver function tests were normal. The urine routine showed no evidence of proteinuria or pyuria. Urine culture showed no growth. Ultrasound abdomen showed hugely distended urinary bladder with bilateral hydroureteronephrosis, Prostate 35 g, and 1700 cc of post-void residual urine. CT scan of the abdomen showed a distended urinary bladder [Figure 1]. The rest of the abdominal organs were normal.
Figure 1.
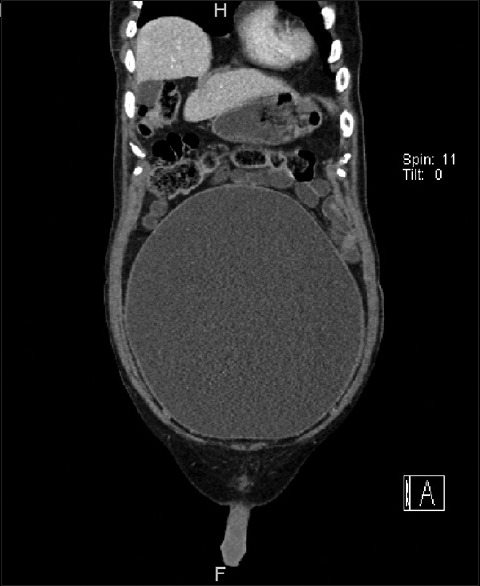
CT scan shows distended bladder
The urologist’s opinion was taken. The patient was catheterized, approximately 6 liters of clear urine was drained. Serum creatinine, after 2 days of catheterization came down to 1.6 mg/dl, Serum electrolytes remained normal. He was discharged, with a catheter.
During follow-up, Serum creatinine was 1.3 mg/dl. Micturating Cystourethrogram revealed significant post-void residual urine [Figure 2]. The urodynamic evaluation showed detrusor underactivity [Figure 3]. The neurologist’s opinion was taken. Neurological examination was unremarkable. MRI lumbosacral spine showed no significant abnormality. Diagnosis of underactive urinary bladder was made. He was started on Tamsulosin 0.4 mg at night and Bethanechol 25 mg Q8H. He failed to void even after multiple trials without a catheter. Finally, he was advised to start clean intermittent self-catheterization (CISC) or continuous bladder drainage. He is doing well with CISC.
Figure 2.

MCUG shows significant post-void residual urine
Figure 3.
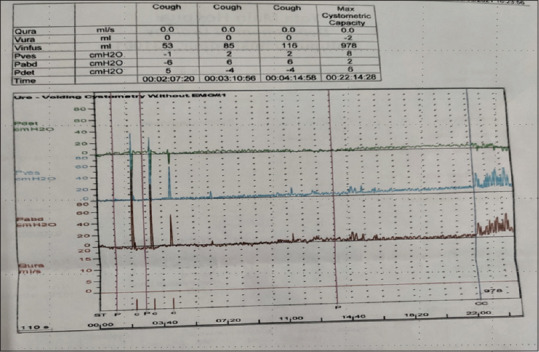
Urodynamic evaluation shows detrusor underactivity
Discussion
An impaired ability to empty the urinary bladder is a common urological problem. It may due to an increase in bladder outlet resistance or lack of efficient bladder contraction, referred to as detrusor underactivity (DUA) by the International Continence Society (ICS). ICS standardization document in 2002 defined DUA as a contraction of reduced strength and/or duration, resulting in prolonged or incomplete bladder emptying within a normal time span.[4] Various epidemiologic studies have shown that lower urinary tract symptoms (LUTS) have a high prevalence in both men and women, increasing significantly with age. However, the contribution of the hypotonic bladder to these symptoms remains unknown because of the lack of a simple noninvasive marker.
Detrusor underactivity is seen in 9% to 28% of men less than 50 years of age and 48% of men over 70 years undergoing urodynamic study (UDS). Similarly, 12% to 45% of women undergoing UDS will have features of detrusor underactivity.[5] This is more prevalent among institutionalized elderly patients.[6] Jeong et al.[7] showed that detrusor underactivity often coexists with other lower urinary tract dysfunctions.
Etiopathogenesis appears to be multifactorial.[8] An etiologic factor may be Neurogenic, Myogenic, Iatrogenic, Functional, or Drugs with anticholinergic side effects. In clinical practice, many patients do not have any apparent cause for underactive bladder suggesting that this may occur secondary to age-related changes, although it has not been conclusively proved.
The only accepted modality to diagnose detrusor underactivity is a urodynamic study. The urodynamic study focuses mainly on strength of detrusor contraction.
Management of underactive bladder usually involves bladder drainage measures like catheterization (either clean intermittent catheterization or indwelling catheter), pharmacotherapy to facilitate bladder emptying, and reducing bladder outlet resistance. There are no effective pharmacotherapies for the treatment of underactive bladder. Drugs used to facilitate bladder emptying are parasympathomimetic agents including muscarinic receptor agonist (e.g., Bethanechol and Carbachol) and anticholinesterases (e.g., Distigmine). The level of evidence to support their use is minimal, especially when their side effect profile is considered.[9] Alpha adrenoceptor antagonists (alpha-blockers) are the most commonly used drugs to reduce bladder outlet resistance. The combination of an alpha-blocker and a cholinergic drug has been found to be more effective.[10]
Various other treatment modalities that have been used with variable success rates are Intravesical electrotherapy, Sacral neuromodulation. Surgical intervention in the form of bladder outlet surgery and reconstructive surgery has a high risk of failure. There are several potential future treatments like Gene therapy, Stem cells, and regenerative techniques for the treatment of hypotonic bladder.[11] We need to have long-term studies to ensure the safety and efficacy of these treatments.
In addition, behavioral interventions like timed voiding, double voiding have been used to reduce symptoms and complications of incomplete bladder emptying. Pelvic floor physiotherapy and biofeedback have been used to treat adults and children with dysfunctional voiding.[12,13]
The hypotonic bladder is a poorly understood bladder dysfunction. Patients may present to a primary care physician with a history of abdominal distension. Ultrasound may be misleading. The possibility of a hypotonic bladder should be kept in mind especially when abdominal distention is associated with urinary symptoms.
Declaration of patient consent
Patient has given his consent regarding use of images and clinical material without using his name.
Key message
An impaired ability to evacuate the urinary bladder is often seen in both men and women. It has a wide variety of manifesting symptoms. There is a lack of effective treatment. Management usually involves bladder drainage techniques like catheterization, pharmacotherapy to facilitate bladder emptying and reducing bladder outlet resistance.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Seki N, Kai N, Seguchi H, Takei M, Yamaguchi A, Naito S. Predictives regarding outcome after transurethral resection for prostatic adenoma associated with detrusor underactivity. Urology. 2006;67:306–10. doi: 10.1016/j.urology.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 2.Chappel CR, Osman NI, Birder L, van Koeveringe GA, Oelke M, Nitti VW, et al. The underactive bladder:A new clinical concept? Eur Urol. 2015;68:351–3. doi: 10.1016/j.eururo.2015.02.030. [DOI] [PubMed] [Google Scholar]
- 3.Yoshida M, Sekido N, Matsukawa Y, Yono M, Yamaguchi O. Clinical diagnostic criteria for detrusor underactivity:A report from the Japanese Continence Society working group on underactive bladder. Low Urin Tract Symptoms. 2021;13:13–6. doi: 10.1111/luts.12356. [DOI] [PubMed] [Google Scholar]
- 4.Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology in lower urinary tract function:Report from the standardisation sub-committee of the International continence society. Urology. 2003;61:37–49. doi: 10.1016/s0090-4295(02)02243-4. [DOI] [PubMed] [Google Scholar]
- 5.Osman NI, Chapple CR, Abrams P, Dmochowski R, Haab F, Nitti V, et al. Detrusor underactivity and the underactive bladder:A new clinical entity? A review of current terminology, definitions, epidemiology, aetiology, and diagnosis. Eur Urol. 2014;65:389–98. doi: 10.1016/j.eururo.2013.10.015. [DOI] [PubMed] [Google Scholar]
- 6.Sawaqed F, Abughosh Z, Suoub M. The prevalence of detrusor underactivity and its symptoms co-relation with urodynamic study findings in patients with lower urinary tract symptoms. Res Rep Urol. 2020;12:415–22. doi: 10.2147/RRU.S264237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jeong SJ, Kim HJ, Lee YJ, Lee JK, Lee BK, Choo YM, et al. Prevalence and clinical features of detrusor underactivity among elderly with lower urinary tract symptoms:A comparison between men and women. Korean J Urol. 2012;53:342–8. doi: 10.4111/kju.2012.53.5.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Osman N, Mangera A, Hillary C, Inman R, Chapple C. The underactive bladder:Detection and diagnosis. F1000Res. 2016;5 doi: 10.12688/f1000research.7344.1. F1000 Faculty Rev-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barendrecht MM, Oelke M, Laguna MP, Michel MC. Is the use of parasympathomimetics for treating an underactive urinary bladder evidence-based? BJU Int. 2007;99:749–52. doi: 10.1111/j.1464-410X.2006.06742.x. [DOI] [PubMed] [Google Scholar]
- 10.Yamanishi T, Yasuda K, Kamai T, Tsujii T, Sakakibara R, Uchiyama T, et al. Combination of a cholinergic drug and an alpha-blocker is more effective than monotherapy for the treatment of voiding difficulty in patients with underactive detrusor. Int J Urol. 2004;11:88–96. doi: 10.1111/j.1442-2042.2004.00753.x. [DOI] [PubMed] [Google Scholar]
- 11.Toby C, Kudze T. New therapeutic directions to treat underactive bladder. Investig Clin Urol. 2017;58(Suppl 2):S99–106. doi: 10.4111/icu.2017.58.S2.S99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Jong TPVM, Klijn AJ, Vijverberg MAW, de Kort LM, van Empelen R, Schoenmakers MAGC. Effect of biofeedback training on paradoxical pelvic floor movement in children with dysfunctional voiding. Urology. 2007;70:790–3. doi: 10.1016/j.urology.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 13.Minardi D, d'Anzeo G, Parri G, Polito M, Jr, Piergallina M, El Asmar Z, et al. The role of uroflowmetry biofeedback and biofeedback training of the pelvic floor muscles in the treatment of recurrent urinary tract infections in women with dysfunctional voiding:A randomized controlled prospective study. Urology. 2010;75:1299–304. doi: 10.1016/j.urology.2009.11.019. [DOI] [PubMed] [Google Scholar]


