Abstract
Kaposi's sarcoma (KS) is an endothelial neoplasm, originally reported by Moritz Kaposi in 1872. It most commonly involves the lower extremities. Its clinical presentation and course can be quite variable. We present a rare case of solitary incidental primary KS of the glans penis in a circumcised, immunocompetent male who is human immunodeficiency virus seronegative. The lesion was discovered incidentally when the otherwise asymptomatic male presented to our outpatient department for an unrelated issue and was given a physical examination. To our knowledge, this is the first incidentally discovered case of primary penile KS.
Keywords: Glans, Kaposi’s, penis, sarcoma
INTRODUCTION
In 2003, Morelli et al. reported the first case of solitary penile Kaposi's sarcoma (KS) in an human immunodeficiency virus (HIV)-seronegative patient.[1] Penile KS otherwise usually occurs in HIV-positive men. We present a case of this rare condition, which might provide some insight into at least one form of natural progression of the disease.
CASE REPORT
A 59-year-old heterosexual male from Yemen presented to the urology clinic for prostate cancer screening. His past medical history was positive for hypertension, dyslipidemia, and remote schistosomiasis, which was treated. He did not smoke nor consume alcohol or illicit drugs. He had no family history of prostate cancer. His prostate was normal on digital rectal examination. However, on genital examination, a firm, nontender, spherical nodule was noted in the glans penis. The overlying skin was intact and normal in color and appearance. No palpable lymph nodes were detected.
Upon further questioning, the patient stated that the nodule had been there for “years.” He first noted it after a night spent outdoors in Yemen. He was wearing a traditional Yemeni “Futah” (a sarong-like garment that is worn without underwear beneath it). He thought that an insect bit him while he was asleep. The nodule persisted since he first noticed it, but was not bothersome. He never thought to seek medical attention for it.
Preoperative serological testing, including for HIV, was negative. An excisional biopsy was carried out as a day procedure, with negative margins on frozen section. Pathological assessment revealed “plump spindle cells, arranged in slit-like spaces containing red blood cells.” The tumor cells showed small nucleoli and scattered mitotic figures. The tumor stained positive for human herpes virus-8 (HHV-8) and CD31 and negative for desmin. Immunostaining for ki-67 revealed positive nuclear staining in 10% of tumor cells. The final histopathological report was consistent with a diagnosis of KS [Figures 1-3]. The patient's postoperative recovery was unremarkable. Follow-up at up to 18 months revealed no disease recurrence. He maintained adequate erectile function.
Figure 1.
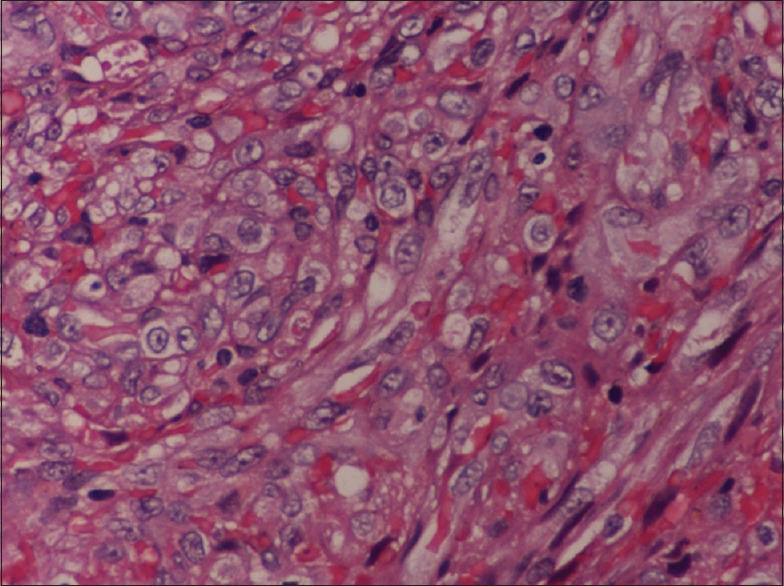
High-power original image of hematoxylin and eosin-stained section of the lesion showing plump spindle cells, arranged in slit-like spaces containing red blood cells
Figure 3.
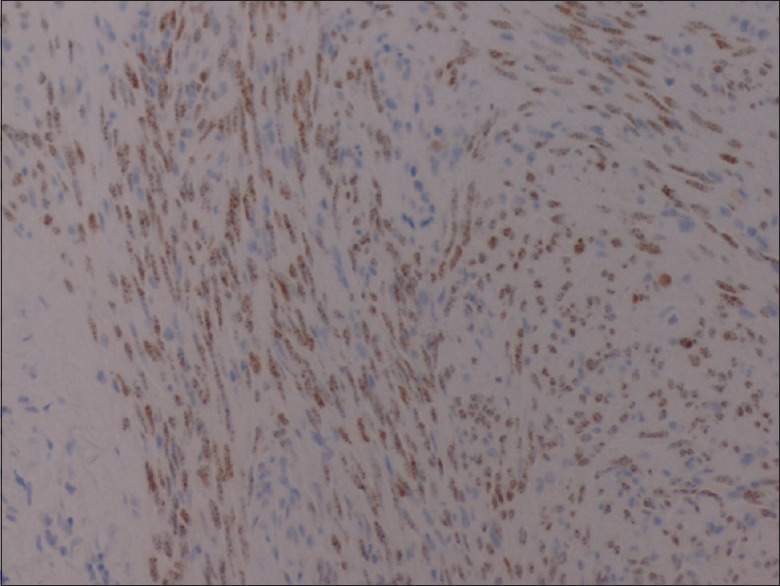
Section of the lesion showing positive human herpes virus-8 immunohistochemical staining
Figure 2.
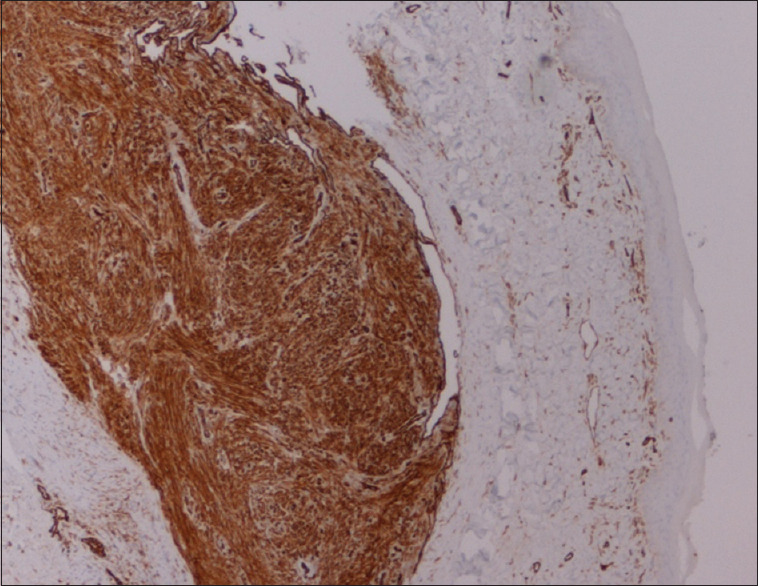
Section of the lesion showing positive CD31 immunohistochemistry staining
DISCUSSION
Conventionally, KS has been classified into four clinical categories: classic, epidemic (HIV associated), endemic (occurring in young African men), and iatrogenic (related to immunosuppressive therapy use).[2] Classic KS is described as an indolent illness that is rarely fatal. It has traditionally been described in individuals of Mediterranean and Ashkenazi Jewish descents. More recently, all of these forms of the disease are believed to be related to HHV-8 infection.[3] Indeed, HHV-8 viremia levels might reflect tumor burden and progression, even in forms that are not associated with immunocompromisation (i.e., endemic and classic forms).[4]
Primary KS of the penis is a rare presentation, especially in circumcised men. It usually involves the glans, as in the present case.[1,5] KS presenting as usually discolored (blue, violet purple, violet, red, or brown) nodules has been previously described.[5] Other lesion forms such as papules, macules, plaques, pedunculated lesions, and exophytic, ulcerating lesions have been described.[1,6,7,8]
Most cases of KS of the penis are seen in HIV-positive men. Solitary, primary KS of the penis has only rarely been reported in HIV-seronegative patients.[1,5,6,7,8] And usually, it is the patients who seek medical attention for what they deem worrisome lesions which persist for weeks to months. In the present case of what would qualify as classic KS, the patient was aware of the nodule for an extended period of time, which underlines the potentially indolent course of the disease. At least in some cases, the natural history of the disease might start off as a subcutaneous nodule with no skin changes before causing the previously reported discoloration and/or ulceration. It also highlights the importance of performing a careful physical examination.
Although the reported patient vaguely relates the disease onset to a possible insect bite, such an association cannot be made with any degree of certainty and at present can only be described as speculative. HHV-8 is currently believed to be transmitted through body fluids.[9] Up to our knowledge, no reports have suggested vector transmission of HHV-8.
No precise guidelines have been described for the management of KS. However, local excision is generally advised for localized small lesions. Localized radiotherapy can be utilized for larger lesions. Systemic chemotherapy can be considered when treating more widespread disease.[10] Carbon dioxide laser therapy has also been described to treat localized penile KS. Other methods described for local control of KS include local chemotherapy and topical agents (e.g., alitretinoin gel).[8] Adjustment of medication dosages can be used to manage iatrogenic KS.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Morelli L, Pusiol T, Piscioli F, Höfler H, Weirich G, Werner M, et al. Herpesvirus 8-associated penile Kaposi's sarcoma in an HIV-negative patient:First report of a solitary lesion. Am J Dermatopathol. 2003;25:28–31. doi: 10.1097/00000372-200302000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Baykal C, Atci T, Buyukbabani N, Kutlay A. The spectrum of underlying causes of iatrogenic Kaposi's sarcoma in a large series: A retrospective study. Indian J Dermatol. 2019;64:392–9. doi: 10.4103/ijd.IJD_217_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dupin N, Grange PA. Looking for the target cell of Kaposi's sarcoma-associated herpesvirus. J Invest Dermatol. 2006;126:545–7. doi: 10.1038/sj.jid.5700132. [DOI] [PubMed] [Google Scholar]
- 4.Pellet C, Kerob D, Dupuy A, Carmagnat MV, Mourah S, Podgorniak MP, et al. Kaposi's sarcoma-associated herpesvirus viremia is associated with the progression of classic and endemic Kaposi's sarcoma. J Invest Dermatol. 2006;126:621–7. doi: 10.1038/sj.jid.5700083. [DOI] [PubMed] [Google Scholar]
- 5.Seleit I, Attia A, Maraee A, Samaka R, Bakry O, Eid E. Isolated Kaposi Sarcoma in two HIV negative patients. J Dermatol Case Rep. 2011;5:24–6. doi: 10.3315/jdcr.2011.1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gönen M, Cenker A, Kiyici H, Kalkan M. Penile Kaposi's sarcomas in a circumcised and HIV-seronegative patient. Int J Urol. 2006;13:318–20. doi: 10.1111/j.1442-2042.2006.01282.x. [DOI] [PubMed] [Google Scholar]
- 7.Micali G, Nasca MR, De Pasquale R, Innocenzi D. Primary classic Kaposi's sarcoma of the penis: Report of a case and review. J Eur Acad Dermatol Venereol. 2003;17:320–3. doi: 10.1046/j.1468-3083.2003.00747.x. [DOI] [PubMed] [Google Scholar]
- 8.Soufiane M, Fadl TM, Nawfel M, Ouafae M, Kawtar Z, Afaf L, et al. Kaposi's sarcoma: HIV-negative man with isolated penile localization. Indian J Pathol Microbiol. 2010;53:535–6. doi: 10.4103/0377-4929.68294. [DOI] [PubMed] [Google Scholar]
- 9.Pica F, Volpi A. Transmission of human herpesvirus 8: An update. Curr Opin Infect Dis. 2007;20:152–6. doi: 10.1097/QCO.0b013e3280143919. [DOI] [PubMed] [Google Scholar]
- 10.Lowe FC, Lattimer DG, Metroka CE. Kaposi's sarcoma of the penis in patients with acquired immunodeficiency syndrome. J Urol. 1989;142:1475–7. doi: 10.1016/s0022-5347(17)39129-2. [DOI] [PubMed] [Google Scholar]


