Abstract
Background
Although adolescent and young adult (AYA) cancers represent a unique spectrum of malignancies, epidemiological studies of cancer incidence often group AYAs together with younger or older populations, obscuring patterns specific to this population.
Methods
We examined AYA cancer incidence trends in 41 countries over a 15-year period using the CI5plus database. Truncated age-standardized incidence rates were calculated and the annual percentage change was assessed, with statistical significance corresponding to a 95% confidence interval that does not include zero.
Results
From 1998 to 2012, the 41 included countries contributed a total of 1 846 588 cancer cases and 3.1 billion person-years among AYAs. Although statistically significant increases in the overall cancer burden were observed in 23 countries, the magnitude varied considerably, with the greatest increase in incidence observed in South Korea (annual percentage change2002–2012 = 8.5%, 95% confidence interval = 7.6% to 9.4%) due to thyroid cancer. Notable trends included sharp increases in the incidence of obesity-related malignancies among AYAs; indeed, statistically significant increases were observed among AYAs for 10 of 11 and 9 of 11 obesity-related cancer sites in the US and UK, respectively, with at least five obesity-related cancers statistically significantly increasing in Canada, Japan, South Korea, Australia, and the Netherlands. Other striking trends were noted for thyroid and testicular cancer, with statistically significantly increasing rates observed in 33 and 22 countries, respectively, whereas statistically significant declines in incidence were observed for smoking-related cancers, cervical cancer, and Kaposi sarcoma in many countries.
Conclusions
Our results highlight the future health-care needs related to treatment as well as the urgency for public health initiatives that can mitigate the increasing burden of cancer in AYAs.
Cancer during adolescence and young adulthood represents a substantial disease burden, with an estimated 1.2 million cancer cases and 400 000 cancer-related deaths occurring among 15- to 39-year olds in 2018 (1). Although it is well recognized that adolescent and young adult (AYA) cancers represent a unique spectrum of malignancies (2), epidemiological studies often obscure patterns specific to this population by grouping AYAs with children or older adults. As prior work examining the global burden of cancer incidence and mortality among young adults found not only differences compared with older and younger groups but also substantial variation by age, sex, and geographical region (3), a broad analysis of international trends in the incidence of AYA cancers is needed to plan and evaluate health-care initiatives, including prevention and detection strategies. Thus, in this study, we characterize the changing cancer burden by examining trends in AYA cancer incidence over a 15-year period across 41 countries in order to inform clinicians and researchers and identify priorities for health-care policy.
Methods
Data Sources
Following the recommendations of the Adolescent and Young Adult Oncology Progress Review Group, we define AYA cancers as those that occur between the ages of 15 and 39 years (4). Cancer incidence data, and corresponding population at risk data, for this age range were obtained from the International Agency for Research on Cancer’s CI5plus database (http://ci5.iarc.fr/CI5plus). Data were available for all cancers combined except nonmelanoma skin cancer (ICD-10: C00-96, except C44) and the following 29 cancer sites/types: lip, oral cavity, and pharynx (C00-14); esophagus (C15); stomach (C16); colon (C18); rectum and anus (C19-21); liver and intrahepatic bile ducts (C22); gallbladder and extrahepatic ducts (C23-24); pancreas (C25); larynx (C32); trachea, bronchus, and lung (C33-34); bone (C40-41); melanoma of skin (C43); Kaposi sarcoma (C46); connective and soft tissue (C47 and C49); female breast (C50); cervix uteri (C53); corpus uteri (C54); ovary (C56); prostate (C61); testis (C62); kidney and renal pelvis (C64-65); bladder (C67); eye (C69); brain and central nervous system (C70-72); thyroid (C73); Hodgkin lymphoma (C81); non-Hodgkin lymphoma (C82-86, C96, B21); multiple myeloma and immunoproliferative diseases (C88 and C90), and leukemia (C91-95).
Because the purpose of this study was to assess trends in AYA cancer incidence, we included only registries with data for the entire 15-year study period of 1998–2012. Ultimately, 41 of the 43 countries in CI5plus were included (Supplementary Table 1, available online); 18 of these countries were covered nationally and 23 countries were represented by one or more subnational registries, which combined covered various proportions of the AYA population in the defined area.
Statistical Analyses
Incidence was calculated by summing the number of new cases occurring during our study period by cancer type, country, sex, and ethnicity where appropriate. Truncated age-standardized incidence rates (ASR), by cancer type, country, sex, and ethnicity, were calculated as the number of cases among individuals aged 15–39 years divided by the corresponding number of person-years at risk per 100 000 using the World Standard Population as proposed by Segi (5) and modified by Doll and colleagues (6).
To assess the average annual percentage change (AAPC) in cancer incidence among AYAs, we used Stata 15.1 statistical software to fit the natural logarithm of the incidence with incidence year using generalized linear regression models with a Poisson distribution in which 95% confidence intervals (CI) were used to determine statistically significant changes; trends were considered stable if they did not reject the null hypothesis, which corresponded to zero lying within the AAPC 95% confidence interval. Additionally, the Joinpoint Regression Program (version 3.5.3) was used to check for statistically significant changes in the AAPC during the study period. Because it is recommended that at least seven data points be observed to consider allowing a joinpoint (7), a maximum of two joinpoints was allowed in this 15-year analysis. The Monte Carlo Permutation method was used to test for statistically significant differences between each segment (8). Differences in the AAPC between sexes, or the average percentage change (APC) across joinpoints, were assessed by comparing 95% confidence intervals, where nonoverlapping 95% confidence intervals were statistically significantly different.
Results
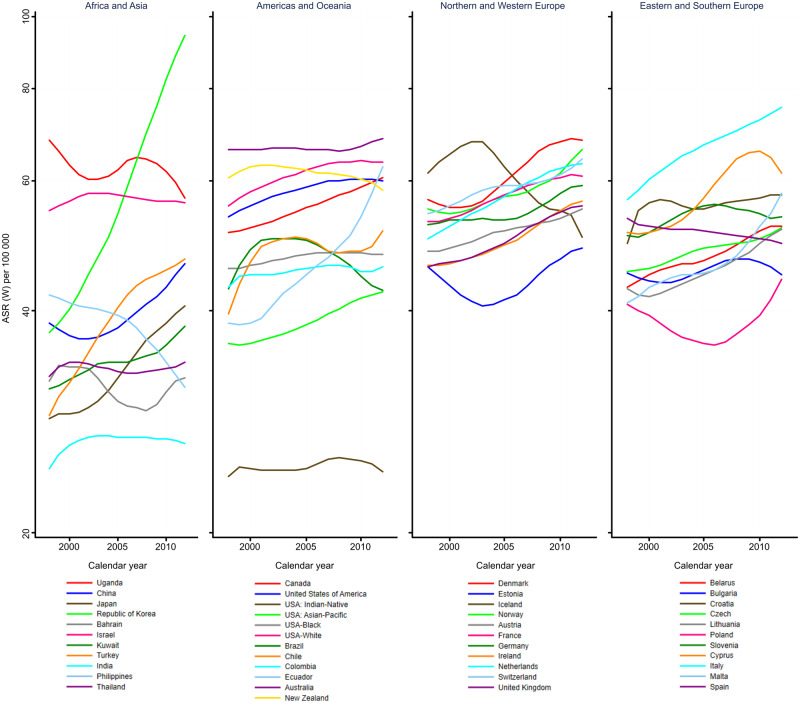
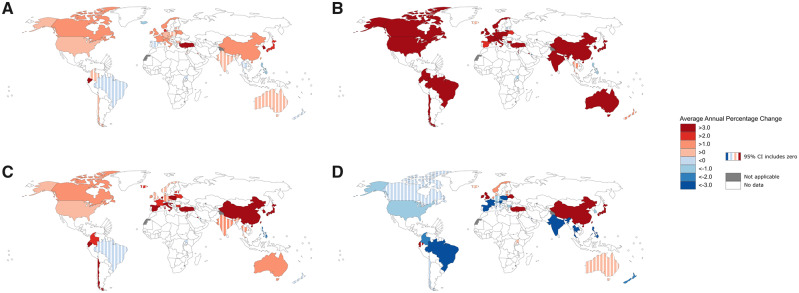
From 1998 to 2012, the 41 included countries contributed a total of 1 846 588 new cancer cases and 3.1 billion person-years among 15- to 39-year olds, with exact numbers of cases and average ASR for the study period shown in Table 1. When the annual ASRs were assessed for all cancer combined, vast differences were observed in the incidence trend for all cancers combined (Figure 1). Overall, the incidence of AYA cancer rose over the study period in 23 countries, decreased in two countries, and remained stable in the other 16 (Figure 2A; Supplementary Table 5, available online). The sharpest increase in incidence was seen in the Republic of Korea beginning in 2002 (APC2002–2012 = 8.5%, 95% CI = 7.6% to 9.4%) (Supplementary Table 6, available online). When assessed by sex (Tables 2 and 3), the AAPCs generally corresponded with the overall AAPC in each country.
Table 1.
Number of cases and truncated ASR per 100 000 person-years for all cancers excluding NMSC, and cancers of the breast, cervix uteri, colon, kidney and renal pelvis, rectum and anus, testis, and thyroid
| All cancer cases excl. NMSC | Breast cancer cases | Cervix uteri cancer cases | Colon cancer cases | Kidney and renal pelvis cancer cases | Rectum and anus cancer cases | Testis cancer cases | Thyroid cancer cases | |
|---|---|---|---|---|---|---|---|---|
| Country | No. (ASR per 100 000) | No. (ASR per 100 000) | No. (ASR per 100 000) | No. (ASR per 100 000) | No. (ASR per 100 000) | No. (ASR per 100 000) | No. (ASR per 100 000) | No. (ASR per 100 000) |
| Africa | ||||||||
| Uganda* | 7395 (62·14) | 461 (8·75) | 863 (17·07) | 52 (0·45) | 43 (0·36) | 81 (0·71) | 17 (0·25) | 67 (0·54) |
| South America | ||||||||
| Brazil* | 4143 (47·41) | 620 (13·05) | 541 (11·52) | 143 (1·61) | 55 (0·62) | 130 (1·47) | 99 (2·42) | 537 (6·16) |
| Chile* | 1084 (48·23) | 78 (6·62) | 178 (15·50) | 31 (1·36) | 16 (0·68) | 15 (0·65) | 259 (23·50) | 90 (4·06) |
| Colombia* | 6101 (45·23) | 771 (10·46) | 774 (10·55) | 198 (1·46) | 62 (0·46) | 151 (1·10) | 301 (4·80) | 601 (4·46) |
| Ecuador* | 4724 (45·99) | 398 (7·31) | 426 (7·81) | 125 (1·22) | 35 (0·34) | 84 (0·82) | 442 (8·97) | 828 (8·01) |
| North America | ||||||||
| Canada* | 80 414 (55·19) | 11 282 (13·88) | 4832 (6·36) | 2388 (1·57) | 1656 (1·06) | 1521 (0·97) | 6730 (9·86) | 12137 (8·34) |
| United States of America* | 952 752 (58·29) | 142 475 (15·96) | 49 273 (5·81) | 29 953 (1·75) | 23 407 (1·36) | 20 805 (1·20) | 73 327 (9·43) | 119 770 (7·41) |
| USA-American, Indian, Alaskan Native* | 5166 (24·75) | 707 (6·57) | 382 (3·69) | 186 (0·88) | 215 (0·99) | 144 (0·67) | 404 (3·90) | 590 (2·86) |
| USA-Asian-Pacific Islander* | 37 246 (38·96) | 7236 (13·25) | 1270 (2·36) | 1291 (1·30) | 600 (0·60) | 941 (0·93) | 1171 (2·74) | 6939 (7·28) |
| USA-Black* | 112 079 (47·22) | 24 886 (19·05) | 6699 (5·30) | 4928 (2·02) | 3538 (1·47) | 3159 (1·29) | 2304 (2·11) | 8306 (3·54) |
| USA-White* | 783 260 (61·21) | 108 658 (15·59) | 40 118 (6·10) | 23 283 (1·73) | 18 859 (1·38) | 16 316 (1·19) | 68 421 (11·14) | 102 318 (8·09) |
| Asia | ||||||||
| Bahrain* | 937 (31·42) | 249 (16·40) | 13 (0·85) | 37 (1·24) | 16 (0·54) | 25 (0·84) | 19 (1·28) | 91 (3·07) |
| China* | 40 275 (39·27) | 6300 (10·69) | 2023 (3·48) | 1377 (1·30) | 658 (0·62) | 1081 (0·99) | 835 (1·85) | 5264 (5·33) |
| India* | 8947 (26·70) | 1385 (8·01) | 632 (3·64) | 177 (0·52) | 70 (0·21) | 299 (0·88) | 144 (0·87) | 421 (1·26) |
| Israel | 22 408 (56·75) | 3838 (18·85) | 708 (3·49) | 576 (1·43) | 377 (0·94) | 370 (0·92) | 1520 (7·71) | 2946 (7·46) |
| Japan* | 21 402 (33·02) | 4346 (12·12) | 2330 (6·71) | 895 (1·32) | 344 (0·50) | 642 (0·93) | 954 (3·09) | 1406 (2·26) |
| Kuwait* | 2009 (34·35) | 336 (11·26) | 37 (1·23) | 82 (1·43) | 36 (0·61) | 46 (0·81) | 91 (3·16) | 344 (5·91) |
| Philippines* | 15 678 (38·02) | 2525 (12·24) | 1083 (5·26) | 613 (1·49) | 167 (0·41) | 449 (1·08) | 229 (1·14) | 1955 (4·66) |
| Republic of Korea* | 77486 (57·73) | 9885 (13·93) | 4431 (6·30) | 2155 (1·55) | 1261 (0·91) | 2230 (1·59) | 716 (1·17) | 27 130 (20·04) |
| Thailand* | 11 889 (33·50) | 1571 (7·98) | 1471 (7·47) | 416 (1·17) | 67 (0·19) | 247 (0·69) | 123 (0·74) | 913 (2·69) |
| Turkey* | 14 791 (39·80) | 2493 (12·67) | 327 (1·67) | 405 (1·05) | 225 (0·58) | 315 (0·82) | 1098 (6·11) | 2296 (6·15) |
| Europe | ||||||||
| Austria | 24 839 (51·07) | 3812 (13·67) | 1452 (5·55) | 589 (1·14) | 480 (0·89) | 434 (0·78) | 3318 (14·19) | 2201 (4·63) |
| Belarus | 28005 (47·51) | 3178 (9·78) | 2532 (8·16) | 618 (0·99) | 877 (1·40) | 412 (0·66) | 1058 (3·69) | 4630 (8·21) |
| Bulgaria | 20 644 (45·28) | 3 161 (13·13) | 3131 (13·14) | 595 (1·26) | 389 (0·82) | 381 (0·80) | 1817 (8·18) | 909 (2·05) |
| Croatia | 13 781 (55·86) | 1 633 (12·10) | 1042 (7·89) | 362 (1·37) | 266 (1·02) | 299 (1·14) | 1652 (13·99) | 1436 (5·80) |
| Cyprus | 2690 (58·38) | 439 (16·81) | 85 (3·33) | 78 (1·63) | 31 (0·66) | 19 (0·38) | 268 (12·29) | 596 (13·02) |
| Czech Republic | 30 523 (48·15) | 3459 (10·33) | 3 638 (11·03) | 901 (1·40) | 757 (1·13) | 593 (0·87) | 4269 (13·51) | 2371 (3·83) |
| Denmark | 18 376 (60·65) | 2493 (14·45) | 1840 (11·76) | 367 (1·14) | 187 (0·56) | 265 (0·78) | 2725 (18·72) | 693 (2·34) |
| Estonia | 3401 (43·75) | 415 (9·88) | 413 (10·10) | 70 (0·84) | 87 (1·05) | 49 (0·59) | 209 (5·59) | 145 (1·91) |
| France* | 21 614 (57·08) | 4200 (20·04) | 1049 (5·10) | 544 (1·39) | 468 (1·18) | 321 (0·78) | 2091 (11·77) | 2472 (6·62) |
| Germany* | 9002 (54·32) | 1481 (15·78) | 573 (6·20) | 266 (1·53) | 172 (0·97) | 186 (0·96) | 1245 (15·57) | 423 (2·55) |
| Iceland | 1068 (60·63) | 132 (14·06) | 115 (12·94) | 22 (1·18) | 15 (0·78) | 17 (0·88) | 91 (10·38) | 110 (6·32) |
| Ireland | 13 443 (50·27) | 2 185 (15·07) | 1212 (8·60) | 350 (1·26) | 230 (0·82) | 252 (0·89) | 1684 (12·96) | 632 (2·38) |
| Italy* | 12 734 (66·47) | 2080 (18·45) | 366 (3·36) | 297 (1·47) | 263 (1·21) | 150 (0·68) | 1013 (11·55) | 2266 (11·86) |
| Lithuania | 9028 (44·92) | 1118 (10·18) | 1388 (13·15) | 182 (0·86) | 231 (1·10) | 135 (0·64) | 385 (4·06) | 777 (3·92) |
| Malta | 1056 (46·80) | 143 (12·09) | 50 (4·41) | 32 (1·38) | 28 (1·20) | 17 (0·72) | 102 (8·99) | 137 (5·96) |
| Netherlands | 53 763 (56·97) | 10 438 (19·60) | 3018 (5·93) | 1874 (2·02) | 605 (0·59) | 900 (0·86) | 6445 (14·82) | 1843 (2·03) |
| Norway | 15 405 (57·53) | 1878 (12·57) | 1416 (10·07) | 486 (1·78) | 224 (0·79) | 266 (0·90) | 2729 (21·23) | 850 (3·18) |
| Poland* | 2812 (38·27) | 320 (8·66) | 171 (4·65) | 74 (0·98) | 64 (0·86) | 59 (0·78) | 263 (7·18) | 315 (4·25) |
| Slovenia | 6482 (53·62) | 831 (12·60) | 674 (10·59) | 143 (1·12) | 120 (0·91) | 122 (0·92) | 1,041 (17·42) | 476 (4·15) |
| Spain* | 14 045 (50·96) | 2360 (15·25) | 501 (3·29) | 397 (1·32) | 331 (1·08) | 236 (0·77) | 1293 (9·83) | 1142 (4·22) |
| Switzerland* | 8210 (58·55) | 1272 (15·21) | 257 (3·31) | 194 (1·41) | 107 (0·72) | 122 (0·81) | 1096 (16·48) | 653 (4·68) |
| United Kingdom* | 167 412 (50·11) | 30 451 (16·09) | 15 817 (9·25) | 4744 (1·41) | 2430 (0·68) | 2916 (0·81) | 18 576 (11·74) | 7902 (2·42) |
| Oceania | ||||||||
| Australia | 81 024 (66·38) | 10 945 (16·17) | 3536 (5·60) | 2735 (2·23) | 1413 (1·09) | 1798 (1·39) | 6774 (11·60) | 6599 (5·41) |
| New Zealand | 14 796 (61·52) | 2371 (17·23) | 850 (6·78) | 4·52 (1·80) | 210 (0·83) | 288 (1·15) | 1413 (12·72) | 849 (3·62) |
Subnational. ASR = age-standardized incidence rate; NMSC = nonmelanoma skin cancer.
Figure 1.
Annual truncated age-standardized incidence rates for all cancers combined, excluding nonmelanoma skin cancer, among 15- to 39-year olds by world region.
Figure 2.
Average annual percentage change for all cancers, thyroid cancer, testicular cancer, and cervical cancer. A) All cancers combined, excluding nonmelanoma skin cancer for both sexes combined. B) Thyroid cancer for both sexes combined. C) Testicular cancer for males. D) Cervical cancer for females.
Table 2.
AAPC for cancers occurring among 15- to 39-year-old males during 1998–2012 for each country for all cancers excluding NMSC, and cancers of the colon, kidney and renal pelvis, rectum and anus, testis, and thyroid†
| Country | All cancers excluding nonmelanoma skin | Colon | Kidney and renal pelvis | Rectum and anus | Testis | Thyroid |
|---|---|---|---|---|---|---|
| Africa | ||||||
| Uganda* | 0·38 (−1·30, 2·09) | 2·58 (−3·62, 9·19) | −2·72 (−7·47, 2·28) | −1·17 (−7·76, 5·89) | −0·13 (−5·88, 5·96) | −5·43 (−12·20, 1·86) |
| South America | ||||||
| Brazil* | −0·40 (−1·71, 0·93) | −1·55 (−8·63, 6·08) | 4·56 (−3·10, 12·82) | −2·73 (−9·75, 4·83) | −0·59 (−5·86, 4·96) | 3·90 (−1·16, 9·21) |
| Chile* | 1·48 (−0·69, 3·70) | −4·37 (−8·20, -0·38) | 11·17 (−0·20, 23·84) | −2·09 (−4·78, 0·68) | 3·13 (−1·37, 7·82) | 1·78 (−7·97, 12·56) |
| Colombia* | −0·07 (−1·02, 0·89) | 4·57 (−0·75, 10·18) | −0·03 (−5·95, 6·27) | −0·43 (−5·37, 4·75) | 2·67 (0·23, 5·16) | 0·21 (−4·09, 4·71) |
| Ecuador* | 2·67 (1·44, 3·92) | −2·67 (−7·65, 2·58) | 0·64 (−5·74, 7·45) | −2·52 (−7·63, 2·87) | 3·24 (1·30, 5·22) | 10·39 (6·49, 14·43) |
| North America | ||||||
| Canada* | 1·05 (0·73, 1·37) | 4·04 (2·79, 5·31) | 2·75 (1·55, 3·96) | 3·87 (1·44, 6·35) | 2·00 (1·37, 2·62) | 6·01 (4·81, 7·22) |
| United States of America* | 0·43 (0·25, 0·60) | 1·77 (1·42, 2·13) | 5·96 (5·21, 6·71) | 1·53 (1·10, 1·97) | 0·62 (0·37, 0·88) | 5·20 (4·78, 5·62) |
| USA-American, Indian, Alaskan Native* | 0·72 (−0·47, 1·93) | 3·58 (−0·91, 8·28) | 7·60 (2·95, 12·46) | 3·75 (−4·43, 12·62) | 3·85 (0·31, 7·52) | 5·53 (0·86, 10·42) |
| USA-Asian-Pacific Islander* | 0·53 (0·12, 0·95) | −1·34 (−2·87, 0·22) | 5·31 (2·02, 8·70) | −0·72 (−2·78, 1·39) | 2·14 (0·69, 3·62) | 4·82 (2·94, 6·73) |
| USA-Black* | 0·06 (−0·16, 0·28) | 0·64 (−0·31, 1·60) | 3·92 (2·85, 5·01) | 1·31 (0·09, 2·55) | 0·78 (−0·22, 1·79) | 5·07 (3·32, 6·85) |
| USA-White* | 0·58 (0·39, 0·78) | 2·16 (1·81, 2·51) | 6·50 (5·68, 7·33) | 1·66 (1·21, 2·11) | 0·81 (0·53, 1·09) | 5·39 (4·97, 5·82) |
| Asia | ||||||
| Bahrain* | 1·40 (−0·80, 3·65) | 1·04 (−4·09, 6·44) | 1·39 (−7·65, 11·32) | 0·15 (−6·32, 7·08) | −2·50 (−11·94, 7·95) | 5·04 (−0·17, 10·53) |
| China* | 0·75 (0·24, 1·26) | −1·16 (−3·74, 1·49) | 10·75 (9·21, 12·31) | 2·80 (0·50, 5·15) | 4·19 (2·77, 5·63) | 14·79 (11·68, 17·99) |
| India* | 1·06 (0·16, 1·98) | 4·12 (−2·81, 11·54) | 2·67 (−4·93, 10·88) | −1·75 (−4·41, 0·99) | 1·71 (−2·81, 6·45) | 3·80 (−1·03, 8·88) |
| Israel | −0·17 (−0·59, 0·25) | 4·10 (1·06, 7·23) | 3·79 (1·84, 5·76) | −0·29 (−2·93, 2·43) | 1·16 (−0·39, 2·74) | 4·57 (2·07, 7·12) |
| Japan* | 2·25 (1·63, 2·88) | 1·62 (0·15, 3·10) | 4·97 (1·63, 8·41) | 2·10 (−0·98, 5·28) | 6·19 (4·13, 8·29) | 6·56 (3·81, 9·38) |
| Kuwait* | 1·55 (−1·21, 4·38) | 8·11 (2·39, 14·15) | −0·63 (−5·80, 4·82) | −0·38 (−5·88, 5·44) | 10·47 (2·81, 18·70) | −1·40 (−7·00, 4·53) |
| Philippines* | −2·24 (−2·79, -1·70) | 0·04 (−2·77, 2·94) | −8·19 (−13·89, -2·12) | −0·69 (−3·58, 2·29) | −2·35 (−5·45, 0·85) | −0·13 (−2·48, 2·27) |
| Republic of Korea* | 4·89 (4·09, 5·69) | 3·19 (1·68, 4·73) | 6·50 (5·33, 7·68) | 7·99 (6·90, 9·09) | 6·90 (5·73, 8·08) | 26·30 (23·25, 29·43) |
| Thailand* | 0·27 (−0·47, 1·01) | 2·36 (−0·84, 5·66) | −2·94 (−9·70, 4·33) | 2·31 (−3·51, 8·48) | 1·76 (−1·64, 5·28) | −0·08 (−3·77, 3·75) |
| Turkey* | 2·11 (1·20, 3·03) | 1·05 (−2·78, 5·03) | 7·71 (2·92, 12·72) | 1·33 (−4·97, 8·05) | 5·43 (3·74, 7·16) | 17·24 (13·31, 21·30) |
| Europe | ||||||
| Austria | 0·41 (0·06, 0·76) | 3·25 (0·50, 6·08) | −1·00 (−2·85, 0·89) | −1·69 (−4·58, 1·28) | −0·57 (−1·32, 0·19) | 7·48 (5·23, 9·78) |
| Belarus | 0·62 (0·00, 1·24) | 0·20 (−2·53, 3·02) | 4·38 (2·40, 6·40) | 2·72 (0·04, 5·47) | 2·44 (1·10, 3·80) | −0·31 (−2·02, 1·43) |
| Bulgaria | 0·44 (−0·16, 1·03) | −0·43 (−2·68, 1·88) | 0·99 (−0·88, 2·90) | −0·95 (−4·01, 2·22) | 2·71 (1·07, 4·39) | 6·06 (1·99, 10·30) |
| Croatia | 0·93 (−1·06, 2·95) | 0·38 (−4·40, 5·41) | 2·49 (−1·26, 6·39) | −0·93 (−4·22, 2·48) | 4·33 (2·20, 6·49) | 7·38 (3·44, 11·47) |
| Cyprus | 2·18 (1·09, 3·28) | 1·38 (−5·34, 8·57) | −3·49 (−8·19, 1·45) | −0·99 (−8·06, 6·62) | 3·19 (0·28, 6·18) | 12·73 (6·79, 18·99) |
| Czech Republic | 0·64 (0·23, 1·05) | 0·53 (−0·91, 1·98) | −0·39 (−2·66, 1·93) | 0·38 (−2·52, 3·37) | 0·82 (0·12, 1·51) | 6·96 (5·29, 8·64) |
| Denmark | 1·34 (0·54, 2·15) | 3·09 (−0·09, 6·38) | 4·55 (1·27, 7·92) | 1·50 (−2·77, 5·95) | 0·19 (−0·56, 0·94) | 4·07 (−1·82, 10·31) |
| Estonia | 1·07 (−0·79, 2·97) | 4·56 (−3·92, 13·78) | 0·73 (−7·60, 9·80) | −0·82 (−8·39, 7·38) | 2·27 (−2·49, 7·27) | 3·63 (−5·09, 13·16) |
| France* | 1·03 (0·60, 1·47) | 1·65 (−0·91, 4·27) | 6·30 (1·99, 10·79) | −3·71 (−6·71, -0·61) | 2·68 (1·64, 3·73) | 1·73 (−0·16, 3·64) |
| Germany* | 0·51 (−0·22, 1·25) | 1·06 (−5·61, 8·20) | −2·52 (−6·85, 2·01) | 3·47 (−0·64, 7·75) | 1·16 (−0·39, 2·72) | 2·14 (−3·43, 8·03) |
| Iceland | −0·65 (−2·33, 1·07) | −0·08 (−4·47, 4·50) | −2·38 (−5·78, 1·13) | 1·05 (−2·02, 4·22) | 2·67 (−3·93, 9·72) | 2·84 (−5·62, 12·06) |
| Ireland | 1·05 (0·44, 1·67) | 4·39 (−0·76, 9·81) | 6·85 (1·44, 12·56) | 2·49 (−2·11, 7·30) | 1·29 (0·29, 2·30) | 7·23 (2·23, 12·48) |
| Italy* | 1·96 (1·50, 2·42) | 1·72 (−3·25, 6·94) | 2·34 (−2·14, 7·01) | 0·68 (−4·99, 6·68) | 3·49 (2·12, 4·89) | 6·72 (4·06, 9·46) |
| Lithuania | 1·25 (0·32, 2·20) | −0·50 (−3·80, 2·91) | 4·62 (1·53, 7·80) | 3·45 (−0·12, 7·15) | 2·99 (0·82, 5·20) | 13·53 (6·49, 21·02) |
| Malta | 1·21 (−0·93, 3·39) | 1·64 (−8·15, 12·48) | 2·85 (−2·02, 7·96) | — | 4·03 (−0·40, 8·65) | 4·40 (−4·98, 14·72) |
| Netherlands | 2·04 (1·82, 2·26) | 2·68 (1·04, 4·36) | 4·54 (1·27, 7·92) | 3·51 (1·76, 5·30) | 3·39 (2·91, 3·87) | 4·53 (1·43, 7·72) |
| Norway | 0·88 (0·32, 1·46) | 3·86 (1·10, 6·70) | 8·44 (3·23, 13·92) | 5·62 (1·65, 9·75) | 0·61 (−0·27, 1·50) | 3·83 (0·80, 6·96) |
| Poland* | 0·67 (−0·36, 1·70) | 0·57 (−7·38, 9·21) | −3·15 (−9·63, 3·78) | −5·17 (−10·99, 1·04) | 5·74 (2·68, 8·88) | 6·83 (−0·19, 14·35) |
| Slovenia | 0·14 (−0·81, 1·10) | −1·87 (−7·27, 3·83) | 2·38 (−2·81, 7·85) | 1·82 (−2·94, 6·81) | 0·70 (−0·71, 2·13) | 7·30 (1·58, 13·33) |
| Spain* | −0·29 (−0·91, 0·32) | −0·99 (−3·71, 1·80) | −1·65 (−5·93, 2·81) | 0·44 (−3·64, 4·70) | 3·63 (1·98, 5·30) | 4·24 (2·20, 6·31) |
| Switzerland* | 0·74 (−0·18, 1·66) | 6·38 (0·74, 12·34) | 7·01 (2·58, 11·63) | −0·92 (−8·5, 7·28) | −0·01 (−1·17, 1·17) | 2·76 (−1·20, 6·88) |
| United Kingdom* | 1·22 (0·85, 1·60) | 5·58 (3·91, 7·27) | 4·76 (3·35, 6·19) | 4·59 (3·13, 6·08) | 0·45 (−0·03, 0·93) | 5·96 (4·84, 7·09) |
| Oceania | ||||||
| Australia | −0·17 (−0·43, 0·10) | 3·72 (2·05, 5·42) | 3·82 (1·74, 5·94) | 3·53 (2·01, 5·07) | 1·20 (0·58, 1·82) | 3·03 (1·61, 4·47) |
| New Zealand | −0·23 (−1·04, 0·59) | 3·39 (−0·60, 7·55) | 2·15 (−2·07, 6·56) | 7·41 (3·69, 11·27) | −0·20 (−1·28, 0·89) | 2·57 (−0·58, 5·83) |
Subnational. AAPC = average annual percentage change; NMSC = nonmelanoma skin cancer.
An em-dash (—) denotes that too few cancer cases were observed to calculate the AAPC.
Table 3.
AAPC for cancers occurring among 15- to 39-year-old females during 1998–2012 for each country for all cancers excluding NMSC, and cancers of the breast, cervix uteri, colon, kidney and renal pelvis, rectum and anus, and thyroid
| Country | All cancers excluding nonmelanoma skin | Breast | Cervix uteri | Colon | Kidney and renal pelvis | Rectum and anus | Thyroid |
|---|---|---|---|---|---|---|---|
| Africa | |||||||
| Uganda* | −0·81 (−1·60, -0·02) | 1·01 (−3·44, 5·66) | 0·29 (−2·27, 2·91) | −6·08 (−13·13, 1·54) | −5·32 (−12·60, 2·56) | 0·34 (−6·84, 8·07) | −1·35 (−8·57, 6·43) |
| South America | |||||||
| Brazil* | −0·68 (−2·27, 0·95) | 0·19 (−1·67, 2·09) | −5·16 (−8·02, -2·22) | 0·29 (−4·71, 5·54) | −1·22 (−7·03, 4·95) | −0·50 (−7·20, 6·67) | 4·87 (2·52, 7·27) |
| Chile* | −0·17 (−2·87, 2·61) | −3·30 (−9·14, 2·92) | −0·91 (−4·83, 3·17) | 4·83 (−3·80, 14·23) | 1·85 (−1·78, 5·61) | −0·61 (−4·47, 3·40) | 10·66 (3·89, 17·86) |
| Colombia* | 0·44 (−0·42, 1·30) | 1·42 (−0·10, 2·97) | −2·38 (−3·68, -1·06) | 0·00 (−4·70, 4·94) | 9·15 (1·24, 17·68) | 5·41 (−0·45, 11·61) | 5·86 (3·65, 8·12) |
| Ecuador* | 3·76 (2·51, 5·03) | 3·12 (−0·40, 6·77) | 3·27 (−0·00, 6·64) | 2·70 (−2·48, 8·16) | −6·26 (−11·93, -0·24) | −0·37 (−7·03, 6·77) | 9·33 (6·74, 11·99) |
| North America | |||||||
| Canada* | 1·38 (1·08, 1·69) | 0·95 (0·50, 1·40) | −0·45 (−1·14, 0·25) | 4·32 (2·68, 5·98) | 2·71 (0·87, 4·58) | 4·83 (3·06, 6·63) | 5·18 (4·07, 6·30) |
| United States of America* | 1·10 (0·89, 1·31) | −0·05 (−0·17, 0·06) | −1·86 (−2·14, -1·58) | 2·16 (1·66, 2·67) | 6·34 (5·57, 7·11) | 2·31 (1·85, 2·77) | 5·27 (4·92, 5·61) |
| USA-American, Indian, Alaskan Native* | 0·13 (−0·67, 0·94) | −0·35 (−1·73, 1·04) | −2·49 (−4·98, 0·07) | 3·18 (−1·91, 8·54) | 4·95 (−1·44, 11·75) | −0·56 (−5·59, 4·73) | 2·91 (0·65, 5·22) |
| USA-Asian-Pacific Islander* | 1·74 (1·39, 2·09) | 0·47 (−0·03, 0·98) | −0·59 (−1·67, 0·50) | 1·02 (−1·27, 3·36) | 4·29 (2·19, 6·43) | 0·59 (−1·38, 2·59) | 5·71 (5·29, 6·13) |
| USA-Black* | 0·57 (0·33, 0·81) | −0·09 (−0·30, 0·13) | −2·45 (−3·11, -1·78) | 0·99 (−0·06, 2·05) | 3·81 (2·80, 4·83) | 2·72 (1·56, 3·89) | 5·28 (4·55, 6·02) |
| USA-White* | 1·26 (1·02, 1·50) | −0·04 (−0·18, 0·11) | −1·63 (−1·95, -1·31) | 2·59 (2·06, 3·11) | 7·13 (6·27, 8·00) | 2·35 (1·81, 2·88) | 5·36 (4·99, 5·74) |
| Asia | |||||||
| Bahrain* | −1·85 (−4·17, 0·52) | −2·58 (−5·27, 0·20) | −6·48 (−12·99, 0·51) | −2·22 (−8·90, 4·96) | −2·76 (−10·66, 5·84) | 4·21 (−1·40, 10·15) | −5·46 (−11·86, 1·40) |
| China* | 1·82 (1·16, 2·48) | 1·42 (0·56, 2·29) | 3·73 (2·26, 5·23) | −0·89 (−2·74, 0·99) | 4·30 (1·64, 7·02) | −1·31 (−3·70, 1·14) | 9·69 (7·93, 11·47) |
| India* | −0·41 (−1·11, 0·29) | −0·69 (−2·53, 1·20) | −7·97 (−9·95, -5·94) | 7·68 (1·94, 13·73) | −3·25 (−10·03, 4·05) | −1·68 (−6·55, 3·43) | 4·37 (0·84, 8·01) |
| Israel | 0·12 (−0·31, 0·54) | 0·31 (−0·64, 1·27) | 0·21 (−1·32, 1·77) | 3·36 (1·07, 5·70) | 3·89 (−0·21, 8·17) | 0·31 (−2·36, 3·06) | 3·20 (2·13, 4·27) |
| Japan* | 3·19 (2·52, 3·87) | 2·17 (1·13, 3·23) | 4·96 (3·52, 6·43) | 1·15 (−0·67, 3·00) | 3·19 (−1·39, 7·97) | 3·94 (0·75, 7·23) | 7·75 (5·49, 10·06) |
| Kuwait* | 0·70 (−0·61, 2·02) | −0·72 (−3·72, 2·38) | −1·59 (−7·77, 5·01) | −8·40 (−14·72, -1·60) | −4·70 (−11·27, 2·35) | −0·01 (−8·33, 9·06) | 5·90 (3·17, 8·70) |
| Philippines* | −1·66 (−2·34, -0·98) | −1·00 (−1·83, -0·17) | −3·51 (−4·52, -2·50) | 1·72 (−0·77, 4·28) | −3·84 (−7·52, -0·01) | −1·32 (−5·10, 2·61) | −1·77 (−3·42, -0·09) |
| Republic of Korea* | 8·47 (7·80, 9·14) | 4·99 (4·16, 5·84) | −1·39 (−2·15, -0·63) | 3·66 (1·98, 5·37) | 8·52 (6·19, 10·91) | 5·64 (4·08, 7·23) | 21·28 (19·73, 22·85) |
| Thailand* | −0·33 (−0·82, 0·16) | 2·15 (0·58, 3·74) | −3·70 (−5·31, -2·07) | 0·15 (−2·21, 2·57) | 8·50 (2·10, 15·29) | 4·06 (−0·23, 8·54) | 1·25 (−0·27, 2·81) |
| Turkey* | 4·73 (4·04, 5·43) | 2·16 (1·10, 3·23) | 6·27 (3·65, 8·95) | 6·03 (0·26, 12·14) | 3·18 (0·08, 6·38) | −1·05 (−6·38, 4·58) | 14·32 (11·71, 16·99) |
| Europe | |||||||
| Austria | 1·34 (0·95, 1·73) | 0·96 (0·32, 1·61) | −3·27 (−4·47, -2·07) | 6·20 (2·87, 9·64) | 1·43 (−1·82, 4·79) | 1·21 (−2·92, 5·50) | 7·59 (6·08, 9·11) |
| Belarus | 1·78 (1·25, 2·31) | 0·95 (0·21, 1·71) | 3·48 (2·19, 4·79) | 0·36 (−2·60, 3·41) | 1·82 (−0·54, 4·24) | −0·72 (−4·16, 2·83) | 2·35 (1·16, 3·55) |
| Bulgaria | 0·68 (0·13, 1·23) | 1·34 (0·30, 2·40) | −1·50 (−2·78, -0·21) | 1·01 (−2·21, 4·34) | 1·06 (−1·86, 4·06) | −0·43 (−4·32, 3·62) | 5·38 (3·85, 6·94) |
| Croatia | 0·39 (−1·10, 1·91) | 1·56 (−0·71, 3·88) | −1·54 (−3·32, 0·28) | 4·28 (−0·35, 9·14) | −1·11 (−7·24, 5·42) | 1·96 (−1·74, 5·79) | 6·31 (5·14, 7·50) |
| Cyprus | 2·53 (0·97, 4·11) | 0·39 (−2·17, 3·01) | 1·45 (−6·20, 9·72) | −3·34 (−10·34, 4·22) | 4·86 (−5·43, 16·26) | 3·80 (−0·21, 7·97) | 7·58 (5·24, 9·97) |
| Czech Republic | 1·18 (0·80, 1·57) | 3·98 (3·18, 4·79) | −1·68 (−2·52, -0·83) | 2·10 (−0·30, 4·55) | 2·03 (−1·56, 5·74) | −1·26 (−3·23, 0·76) | 7·63 (6·18, 9·10) |
| Denmark | 2·49 (1·80, 3·18) | 2·22 (1·19, 3·27) | 0·78 (−0·62, 2·20) | 3·35 (−0·21, 7·04) | 7·77 (0·60, 15·45) | 0·34 (−4·30, 5·21) | 3·66 (1·61, 5·75) |
| Estonia | 0·79 (−0·50, 2·09) | 0·80 (−2·43, 4·12) | 0·94 (−2·07, 4·04) | 5·47 (−2·20, 13·73) | 5·57 (−2·63, 14·46) | −2·07 (−9·31, 5·74) | −0·76 (−4·68, 3·31) |
| France* | 1·45 (1·01, 1·89) | 1·54 (1·12, 1·96) | −3·83 (−5·80, -1·82) | 5·53 (2·50, 8·65) | 2·01 (0·11, 3·96) | 6·20 (1·82, 10·76) | 4·07 (2·99, 5·17) |
| Germany* | 1·02 (0·27, 1·78) | 1·77 (0·90, 2·66) | −1·01 (−2·97, 1·00) | 5·96 (1·98, 10·09) | 0·55 (−8·29, 10·23) | −0·39 (−6·41, 6·03) | 6·61 (2·69, 10·69) |
| Iceland | −2·41 (−4·57, -0·21) | 0·69 (−4·36, 6·01) | 0·14 (−3·84, 4·28) | 0·23 (−6·25, 7·14) | −10·43 (−14·48, -6·19) | −1·79 (−9·48, 6·55) | 0·11 (−6·09, 6·72) |
| Ireland | 2·09 (1·62, 2·55) | 0·70 (−0·07, 1·48) | 4·68 (2·92, 6·48) | 9·65 (5·32, 14·16) | 4·28 (0·19, 8·53) | 3·58 (−1·79, 9·24) | 12·72 (8·84, 16·75) |
| Italy* | 1·83 (1·26, 2·40) | −0·01 (−1·21, 1·20) | −0·44 (−3·00, 2·19) | 3·01 (−2·10, 8·40) | 1·97 (−1·70, 5·78) | −3·28 (−9·94, 3·87) | 6·86 (5·09, 8·67) |
| Lithuania | 1·74 (1·09, 2·40) | 2·04 (0·81, 3·28) | 1·17 (−0·20, 2·56) | 0·16 (−5·50, 6·17) | 1·45 (−1·47, 4·46) | 2·32 (−6·75, 12·28) | 8·18 (4·92, 11·55) |
| Malta | 2·31 (−0·19, 4·86) | 1·72 (−0·86, 4·36) | 1·89 (−3·72, 7·82) | 3·56 (−7·17, 15·53) | 2·78 (−0·19, 5·84) | 7·31 (4·73, 9·95) | −1·30 (−4·98, 2·51) |
| Netherlands | 1·57 (1·21, 1·94) | 1·62 (1·13, 2·11) | 1·16 (−0·03, 2·37) | 3·93 (2·54, 5·33) | 3·73 (0·59, 6·98) | 2·42 (−0·41, 5·34) | 3·56 (2·48, 4·65) |
| Norway | 1·61 (0·74, 2·48) | 2·21 (0·65, 3·79) | 1·74 (0·37, 3·14) | 7·09 (3·77, 10·51) | 5·57 (−0·43, 11·93) | 4·01 (0·72, 7·40) | 3·28 (1·54, 5·05) |
| Poland* | −0·25 (−1·80, 1·31) | −0·73 (−2·53, 1·11) | −7·35 (−11·39, -3·13) | −2·88 (−9·15, 3·82) | −0·66 (−7·34, 6·49) | −0·80 (−8·37, 7·38) | 7·17 (3·37, 11·11) |
| Slovenia | 1·01 (0·17, 1·85) | 2·53 (1·00, 4·09) | −7·26 (−9·30, -5·17) | 5·21 (−1·48, 12·36) | 2·63 (−3·51, 9·16) | 1·29 (−7·24, 10·59) | 7·87 (4·12, 11·75) |
| Spain* | −0·40 (−0·95, 0·15) | 0·64 (−0·38, 1·67) | −4·79 (−7·34, -2·16) | 2·13 (−2·04, 6·47) | 0·52 (−3·50, 4·71) | −0·19 (−3·55, 3·29) | 2·67 (0·92, 4·46) |
| Switzerland* | 1·18 (0·49, 1·88) | 1·69 (0·51, 2·88) | −1·52 (−3·43, 0·42) | 7·73 (1·28, 14·59) | 2·90 (−5·08, 11·56) | 0·06 (−7·05, 7·72) | 5·50 (3·17, 7·87) |
| United Kingdom* | 1·80 (1·55, 2·04) | 0·09 (−0·19, 0·37) | 3·03 (2·06, 4·02) | 6·27 (4·30, 8·27) | 4·05 (2·84, 5·27) | 3·42 (1·82, 5·04) | 6·35 (5·89, 6·80) |
| Oceania | |||||||
| Australia | 0·31 (0·05, 0·57) | 0·36 (0·01, 0·72) | 0·90 (−0·32, 2·13) | 3·95 (2·46, 5·45) | 0·20 (−2·23, 2·69) | 4·08 (2·38, 5·81) | 3·46 (2·96, 3·97) |
| New Zealand | −0·47 (−1·03, 0·09) | −0·45 (−1·35, 0·46) | −2·53 (−4·55, -0·46) | 3·71 (0·38, 7·16) | −2·15 (−6·00, 1·86) | 1·19 (−1·59, 4·05) | 1·56 (−1·17, 4·37) |
Subnational. AAPC = average annual percentage change; NMSC = nonmelanoma skin cancer.
Increases in the incidence of thyroid cancer were seen in 33 of the 41 countries studied (Figure 2B; Supplementary Table 5, available online); of these 33 countries, the significant increases observed for thyroid cancer were noted for females in all countries, and in males for 22 countries (Table 2). Among the countries that experienced a statistically significant increase in thyroid cancer incidence, the lowest AAPC was observed in females in Belarus (2.4%, 95% CI = 1.2% to 3.6%). AAPCs of 10–20% were seen in Chile (females), Ecuador (males), China (males), Turkey (males and females), Cyprus (males), Ireland (females), and Lithuania (males), and an AAPC greater than 20% was seen in both males and females in the Republic of Korea. Interestingly, the AAPC increased at a higher rate in males than females only in China and the Republic of Korea. When assessed using joinpoint regressions, there was an indication of a deceleration in the increase of thyroid cancer incidence in Canadian females, and the initial increase was replaced by a stable trend in both sexes in the USA (white), Lithuania, and Slovenia (Supplementary Table 6, available online). Conversely, the percentage change increased towards the end of the period assessed for Chinese females and Norwegian males.
For testicular cancer, incidence increased among AYA males in 22 countries (Figure 2C; Table 2); these countries were from South and North America, Asia, all parts of Europe, and Oceania. Statistically significant increases ranged from an AAPC of 0.6% (95% CI = 0.4% to 0.9%) in American AYAs to over 5% in Japan (AAPC = 6.2%), Kuwait (AAPC = 10.5%), the Republic of Korea (AAPC = 6.9%), Turkey (AAPC = 5.4%), and Poland (AAPC = 5.7%).
Results pertaining to the incidence of cervical cancer were mixed (Figure 2D; Table 3). The incidence of cervical cancer decreased among AYA females in Brazil, Colombia, the United States, India, the Philippines, the Republic of Korea, Thailand, Austria, Bulgaria, the Czech Republic, France, Poland, Slovenia, Spain, and New Zealand. The sharpest declines (ie, at least −5% per year) were seen in Brazil, India, Poland, and Slovenia. In contrast, increases in cervical cancer incidence among AYAs were seen in China, Japan, Turkey, Belarus, Ireland, Norway, and the UK. In joinpoint regressions, there was also some indication that the incidence of cervical cancer started to increase more recently among young females in the Netherlands (APC2002–2012 = 3.1%, 95% CI = 1.3% to 4.9%) and Australia (APC2001–2012 = 2.7%, 95% CI = 1.4% to 4.0%) (Supplementary Table 6, available online).
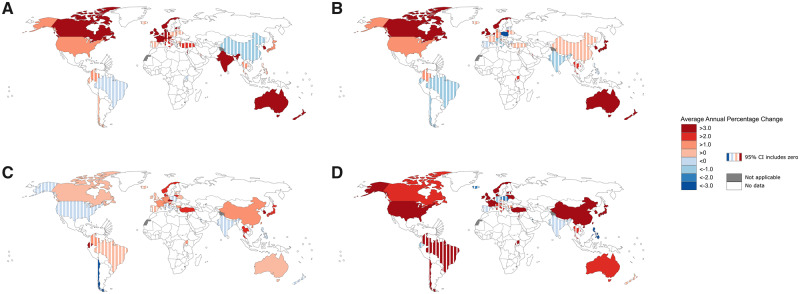
When assessed for both sexes combined, the incidence of colon cancer was either stable (n = 24) or increasing (n = 17) for all countries investigated (Figure 3A; Supplementary Table 5, available online). When assessed by ethnicity, the statistically significantly increasing incidence in the United States was observed only in white Americans (AAPC = 2.4%, 95% CI = 2.0% to 2.7%). Colon cancer in the UK was observed to increase at a particularly rapid rate, with the APC increasing from −2.4% (95% CI = −11.3% to 7.5%) in 1998–2001 to 27.6% (95% CI = 12.3% to 45.1%) in 2010–2012 (Supplementary Table 6, available online). Similarly, in Australia the increase was limited to the period of 2006–2012 (AAPC = 9.0%, 95% CI = 5.0% = 13.2%). Although the majority of these increases were observed in both sexes, in Kuwait colon cancer was statistically significantly increasing among males (AAPC = 8.1%, 95% CI = 2.4% to 14.2%) (Table 2) and statistically significantly decreasing among females (AAPC = −8.4%, 95% CI = −14.7% to −1.6) (Table 3).
Figure 3.
Average annual percentage change of colon cancer, rectoanal cancer, breast cancer, and kidney and renal cancer. A) Colon cancer for both sexes combined. B) Rectoanal cancer for both sexes combined. C) Breast cancer among females. D) Kidney and renal for both sexes combined.
A similar pattern was seen for the incidence of rectal and anal (rectoanal) cancers, where 10 of the countries that experienced increases in colon cancer also observed increases for this cancer (Figure 3B; Supplementary Table 5, available online). In the United States, the increase in rectoanal cancers was observed in both black and white populations. Interestingly, when assessed by subtype for both sexes combined, there was an indication that the increases were primarily due to rectal cancers (ICD-10: C19-20), with 10 countries observing increasing incidence rates. Increases in anal cancers (ICD-10: C21) were observed in only Uganda and Japan, with the United States, Spain, and Thailand observing statistically significant declines in anal cancer (Supplementary Table 7, available online). Although most countries observed a linear pattern in the AAPC for our study period, the rectoanal trend switched from a declining or stable rate to an increasing rate more recently in Thailand (both sexes), Japan (females), and Lithuania (females), and for American males the rates was observed to stabilize from 2008 onwards (Supplementary Table 6, available online).
With the exception of the Philippines, breast cancer among AYAs was increasing (n = 19) or stable (n = 21) in all countries assessed (Figure 3C; Table 3), with increases primarily observed in Western and Eastern Europe and Asia. Among countries experiencing statistically significantly increasing breast cancer rates, the AAPC ranged from 0.4% (95% CI = 0.0% to 0.7%) in Australia to 5.0% (95% CI = 4.2% to 5.8%) in the Republic of Korea.
The incidence of kidney and renal pelvis cancer among AYAs increased in 17 countries, decreased in the Philippines, and remained stable in 23 countries (Figure 3D; Supplementary Table 5, available online). For each of the countries experiencing statistically significant increases, incidence increased on average by at least 2% each year when sexes were combined, with the greatest increase occurring in China (AAPC = 7.9%, 95% CI = 6.3% to 9.5%). When assessed by sex, the AAPC was comparable for all countries, except China where males (AAPC = 10.8%, 95% CI = 9.2% to 12.3%) had a statistically significantly higher AAPC compared with females (AAPC = 4.3%, 95% CI = 1.6% to 7.0%) (Tables 2 and 3). Interestingly, the increasing incidence in the United States stabilized from 2008 onwards, with a deceleration observed among white American males and females (Supplementary Table 6, available online).
Increases were also observed in other obesity-related cancers, including uterine (12 countries), pancreatic (10 countries), gallbladder (seven countries), and liver (six countries) cancer (Supplementary Table 5, available online). No statistically significant differences in the AAPCs were observed between sexes (Supplementary Tables 8 and 9, available online).
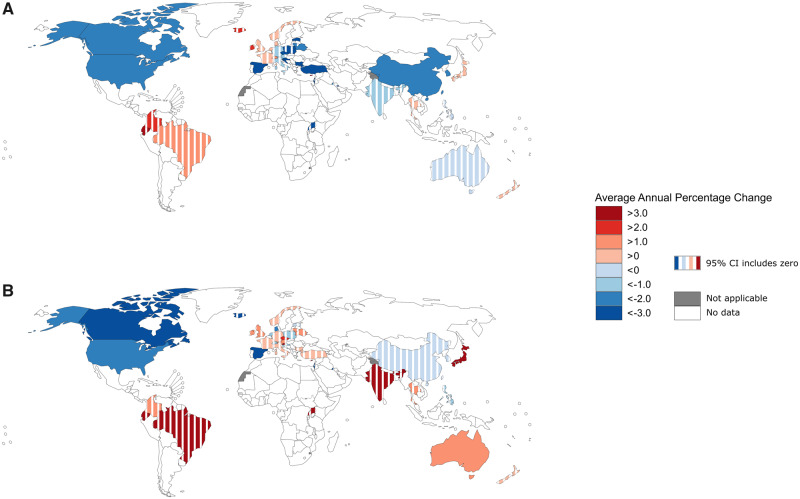
Substantial decreases in the incidence of lung cancer were seen for both sexes in Canada, the United States, Bahrain, China, Israel, the Republic of Korea, Turkey, Bulgaria, Croatia, the Czech Republic, and Spain (Supplementary Table 5, available online). This decrease was largely restricted to male AYAs (Figure 4, A and B; Supplementary Table 7, available online), although the AAPC was only statistically significantly different between males and females in Bahrain, China, Turkey, and the Czech Republic. Notably, in the United States, the decreasing AAPC was more substantial among blacks than whites when assessed overall and in females only (Supplementary Tables 5, 8, 9, available online). For females, statistically significant increases in lung cancer incidence were observed only in Australia (AAPC = 2.0%, 95% CI = 0.1% to 3.8%) and Japan (AAPC = 3.0%, 95% CI = 0.3% to 5.8%), although, again, the AAPC was not statistically significantly different than that observed in males (Supplementary Table 9, available online).
Figure 4.
Average annual percentage change of lung cancer: A) males and B) females.
Declines for other smoking-related cancers were also noted in AYAs (Supplementary Table 5, available online). In particular, 12 countries experienced declines in laryngeal cancer, and nine countries experienced statistically significant declines in bladder cancer. Results were less consistent for lip, oral cavity, and pharyngeal cancers, however, with four countries experiencing declines and 10 countries experiencing increases in incidence over our study period.
Declines were also noted for Kaposi sarcoma in eight countries for both sexes (Supplementary Table 5, available online). Within the United States, the rate of Kaposi sarcoma among AYAs decreased more substantially in whites (AAPC = −5.6%, 95% CI = −6.5% to −4.7%) than in blacks (AAPC = −2.2%, 95% CI = −3.1% to −1.3%). Conversely, Kaposi sarcoma statistically significantly increased among AYAs in the Republic of Korea, Thailand, and Ecuador by 10.9% (95% CI = 1.6% to 20.9%), 9.0% (95% CI = 1.6% to 17.0%), and 8.1% (95% CI = 1.2% to 15.4%) on average annually, respectively.
The final notable finding is the wide variation in trends for skin melanoma by sex and country. Whereas 12 European countries and Turkey experienced increases in the burden of this cancer for both sexes, notable annual decreases ranging from 2.3% to 6.7% were observed in the United States (black), Israel, Kuwait, Germany, Iceland, Australia, and New Zealand (Supplementary Table 5, available online).
Discussion
Examining variations in international trends of cancer incidence allows for the anticipation of the future cancer burden, generation of hypotheses regarding etiology, and evaluation of both primary prevention strategies and changes in diagnostic practice. These are important for AYAs, a population that is underrepresented in cancer research despite their unique health-care needs (9). Studying AYAs separately thus ensures that trends specific to this population are not masked by the larger absolute burden of cancer in older adults.
An important example concerns rates of colorectal cancer, which in the general population have stabilized or are decreasing in most high-income countries (10). Previous studies have noted, however, that these declines are restricted to older adults and that rates among young adults are increasing sharply (11). Our results indicate that a similar pattern is seen across multiple countries in Northern Europe, North America, and Oceania. Obesity is a well-known risk factor for colorectal cancer (12), and thus increasing rates of both childhood and adult obesity (13,14) are likely to be one driving factor behind increasing AYA rates (12,13,15).
Consistent with this hypothesis, our results show that the incidence of other obesity-related malignancies have also statistically significantly increased in AYAs in a number of countries. Currently, as classified by the International Agency for Research on Cancer in 2016, there is strong evidence that excess body weight is causally linked to the following cancer sites: esophagus, gastric cardia, colon and rectum, liver, gallbladder, pancreas, postmenopausal breast, corpus uteri, ovary, kidney, meningioma, thyroid, and multiple myeloma (12). Indeed, among the 11 obesity-linked cancer sites that can occur among AYAs and were investigated in this study (ie, excluding postmenopausal breast cancer and meningioma), statistically significant increases were observed in the United States and UK for 10 and nine cancer sites, respectively, with at least five obesity-related cancers statistically significantly increasing in Canada, Japan, the Republic of Korea, Australia, and the Netherlands. Our findings thus support the hypothesis that the etiology of these cancers may be related to obesity or related risk factors (eg, low physical activity, poor nutrition). Prevention or treatment of obesity in both childhood and early adulthood may blunt future increases in AYA cancer incidence.
Substantial increases in thyroid cancer rates were also seen in AYA across the clear majority of countries studied. Previous studies have attributed this alarming explosion of cases to overdiagnosis, citing the large increases in indolent cases, widespread use of diagnostic ultrasounds and fine-needle aspiration biopsies (16), and generally stable mortality rates. In the case of the Republic of Korea, overdiagnosis is almost certainly a contributing cause of the rising thyroid cancer burden among AYA as thyroid cancer screening was added as an inexpensive add-on to the list of screening tests offered nationally by the government (17); indeed, when thyroid cancers are excluded, we observe a substantial decrease in the overall AAPC of AYA cancers in the Republic of Korea, from 22.1% to 1.9%. Overdiagnosis may not be the only relevant factor, however, as recent findings demonstrated that mortality rates for thyroid cancer, overall and for advanced-stage cases, are statistically significantly increasing in the United States (18). Thus, additional AYA-specific studies of thyroid cancer mortality trends and treatment patterns are warranted.
Statistically significant increases in testicular cancer were also seen in many countries, the etiology of which is unknown (19). These increases may relate to prenatal exposures, particularly estrogens that can affect gonadal development in utero (20–22). Further work is needed to understand the increasing incidence of testicular cancer, which affected countries on all continents except Africa. Similarly, it is unclear why breast cancers are increasing among AYA, particularly as obesity has been cited as a protective factor against the development of premenopausal breast cancer (23). Potential factors include changes in reproductive behaviors, such as having fewer children and at later stages in life (24).
Cervical cancer trends in AYAs varied internationally. Over one-third of the countries studied experienced statistically significant decreases more recently, while China, Japan, Turkey, Belarus, Ireland, and the UK experienced annual increases of over 3%. Although some of these countries (eg, Japan, Ireland) offer national HPV vaccination programs, it may be too early to see the impact on AYA cervical cancer rates, with changing sexual behaviors likely accounting for the increases observed (25,26). HPV vaccination programs nonetheless play an important role in controlling cervical cancer in AYA and will also likely affect the incidence of other HPV-related cancers in the future (27).
Although AYA melanoma rates were highest in Australia, statistically significant progress was made over the study period, with an annual average decrease of 2.8%. This stands in contrast to the increasing trends seen in 12 European countries. Primary prevention efforts seeking to change childhood and teenage behaviors regarding sun protection and tanning bed use in Australia are now warranted across much of Europe as well (28,29).
Our results also highlight encouraging international trends. For example, declines in Kaposi sarcoma are likely the result of HIV control and improved medications, and declining rates of smoking-related cancers in AYAs are likely a result of successful tobacco control initiatives. Further research is nonetheless urgently needed to understand the impact of increasing rates of e-cigarette use on the incidence of these cancer types (30).
Study strengths include the large number of populations included from geographically diverse regions, the standardized quality-assured data, and the ability to track annual incidence rates over a 15-year period. In addition, we were able to report incidence rates for certain groups of cancer common in the AYA age range that are rarely reported, such as bone and connective tissue cancers. One limitation is the inability to align cancer categories with those proposed by Barr et al. (2) Second, our study was limited to countries able to provide high-quality data, representing predominately high- or upper-middle income economies. Substantial improvements in cancer registration are required in most low- and middle-income countries, without which efforts to characterize and address the global burden of AYA cancer will remain limited. Finally, only some of the included registries were national and thus our results may misrepresent the patterns in a given country.
In conclusion, our results have demonstrated unique trends in the incidence of AYA cancer. These data advocate for prevention and screening strategies that are of most relevance in the represented AYA population and indicate future health-care needs related to treatment. Efforts targeting obesity prevention, widespread access to HPV vaccination, smoking cessation, and appropriate prevention of sun exposure and tanning bed use are potential pathways to decrease AYA cancer incidence rates in many countries.
Notes
All authors declare no conflicts of interests.
Cancer Incidence in Five Continents data are freely available for download at ci5.iarc.fr.
MMF-B and SG contributed to the conception and design of the study. JF coassessed all raw incidence data for inclusion in Cancer Incidence in Five Continents. YR and AH analyzed the clean CI5plus data. MMF-B and SG drafted the first manuscript. All authors contributed to the interpretation of the data, the critical revision of the manuscript, and agreed to the submission of the manuscript.
Where authors are identified as personnel of the International Agency for Research on Cancer/World Health Organization, the authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policy or views of the International Agency for Research on Cancer/World Health Organization.
Supplementary Material
References
- 1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. [DOI] [PubMed] [Google Scholar]
- 2. Barr RD, Holowaty EJ, Birch JM. Classification schemes for tumors diagnosed in adolescents and young adults. Cancer. 2006;106(7):1425–1430. [DOI] [PubMed] [Google Scholar]
- 3. Fidler MM, Gupta S, Soerjomataram I, Ferlay J, Steliarova-Foucher E, Bray F. Cancer incidence and mortality among young adults aged 20–39 years worldwide in 2012: a population-based study. Lancet Oncol. 2017;18(12):1579–1589. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Department of Health and Human Services. Closing the Gap: Research and Care Imperatives for Adolescents and Young Adults with Cancer – Report of the Adolescent and Young Adult Oncology - Progress Review Group National Cancer Institute of the National Institutes of Health; 2006.
- 5. Segi M. Cancer Mortality for Selected Sites in 24 Countries (1950-1957). Sendai, Japan: Department of Public Health, Tohoku University of Medicine; 1960. [Google Scholar]
- 6. Doll R, Payne P, Waterhouse J, eds. Cancer Incidence in Five Continents: A Technical Report. Berlin: Springer; 1966. [Google Scholar]
- 7.National Cancer Institute - Surveillance Research Program. Number of Joinpoints—Joinpoint Help System 4.4.0.0. https://surveillance.cancer.gov/help/joinpoint/setting-parameters/advanced-tab/number-of-joinpoints. Accessed November 4, 2019.
- 8. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates [Erratum in: Stat Med 2001;20:655]. Stat Med. 2000;19(3):335–351. [DOI] [PubMed] [Google Scholar]
- 9. Hay AE, Rae C, Fraser GA, et al. Accrual of adolescents and young adults with cancer to clinical trials. Curr Oncol. 2016;23(2):e81–e85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66(4):683–691. [DOI] [PubMed] [Google Scholar]
- 11. Siegel RL, Jemal A, Ward EM. Increase in incidence of colorectal cancer among young men and women in the United States. Cancer Epidemiol Biomarkers Prev. 2009;18(6):1695–1698. [DOI] [PubMed] [Google Scholar]
- 12. Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K. Body fatness and cancer—viewpoint of the IARC Working Group. N Engl J Med. 2016;375(8):794–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Keum N, Greenwood DC, Lee DH, et al. Adult weight gain and adiposity-related cancers: a dose-response meta-analysis of prospective observational studies. J Natl Cancer Inst. 2015;107(2): djv088. [DOI] [PubMed] [Google Scholar]
- 14. Swinburn BA, Kraak VI, Allender S, et al. The global syndemic of obesity, undernutrition, and climate change: The Lancet Commission report. Lancet. 2019;393(10173):791–846. [DOI] [PubMed] [Google Scholar]
- 15. Liu P-H, Wu K, Ng K, et al. Association of obesity with risk of early-onset colorectal cancer among women. JAMA Oncol. 2019;5(1):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Davies L, Welch HG. Current thyroid cancer trends in the United States. JAMA Otolaryngol - Head Neck Surg. 2014;140(4):317–322. [DOI] [PubMed] [Google Scholar]
- 17. Ahn HS, Kim HJ, Welch HG. Korea’s thyroid-cancer “Epidemic”—screening and overdiagnosis. N Engl J Med. 2014;371(19):1765–1767. [DOI] [PubMed] [Google Scholar]
- 18. Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM. Trends in thyroid cancer incidence and mortality in the United States, 1974-2013. JAMA. 2017;317(13):1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Znaor A, Lortet-Tieulent J, Jemal A, Bray F. International variations and trends in testicular cancer incidence and mortality. Eur Urol. 2014;65(6):1095–1106. [DOI] [PubMed] [Google Scholar]
- 20. Giannandrea F, Paoli D, Fig-Talamanca I, Lombardo F, Lenzi A, Gandini L. Effect of endogenous and exogenous hormones on testicular cancer: the epidemiological evidence. Int J Dev Biol. 2013;57(2–4):255–263. [DOI] [PubMed] [Google Scholar]
- 21. Morimoto LM, Zava D, McGlynn KA, et al. Neonatal hormone concentrations and risk of testicular germ cell tumors (TGCT). Cancer Epidemiol Biomarkers Prev. 2018;27(4):488–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McGlynn KA, Quraishi SM, Graubard BI, Weber JP, Rubertone MV, Erickson RL. Persistent organochlorine pesticides and risk of testicular germ cell tumors. J Natl Cancer Inst. 2008;100(9):663–671. [DOI] [PubMed] [Google Scholar]
- 23. Carmichael AR, Bates T. Obesity and breast cancer: a review of the literature. Breast. 2004;13(2):85–92. [DOI] [PubMed] [Google Scholar]
- 24. Key TJ, Verkasalo PK, Banks E. Epidemiology of breast cancer. Lancet Oncol. 2001;2(3):133–140. [DOI] [PubMed] [Google Scholar]
- 25. Layte R, McGee H, Quail A, et al. The Irish Study of Sexual Health and Relationships Dublin, Ireland: Crisis Pregnancy and the Department of Health and Children; 2006.
- 26. Utada M, Chernyavskiy P, Lee WJ, et al. Increasing risk of uterine cervical cancer among young Japanese women: comparison of incidence trends in Japan, South Korea and Japanese-Americans between 1985 and 2012. Int J Cancer. 2019;144(9):2144–2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Stier EA, Chigurupati NL, Fung L. Prophylactic HPV vaccination and anal cancer. Hum Vaccines Immunother. 2016;12(6):1349–1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Baade PD, Balanda KP, Lowe JB. Changes in skin protection behaviors, attitudes, and sunburn: in a population with the highest incidence of skin cancer in the world. Cancer Detect Prev. 1996;20(6):566–575. [PubMed] [Google Scholar]
- 29. Boniol M, Autier P, Boyle P, Gandini S. Cutaneous melanoma attributable to sunbed use: systematic review and meta-analysis. BMJ. 2012;345(2):e4757–e4757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Grana R, Benowitz N, Glantz SA. E-cigarettes. Circulation. 2014;129(19):1972–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.