Abstract
Background and objective
Dopamine plays an important role in the disease pathology of Parkinson’s disease and schizophrenia. These two neuropsychiatric disorders represent disease end points of the dopaminergic spectrum where Parkinson’s disease represents dopamine deficit and schizophrenia represents dopamine hyperactivity in the mid-brain. Therefore, current treatment strategies aim to restore normal dopamine levels. However, during treatment patients develop adverse effects due to overshooting of physiological levels of dopamine leading to psychosis in Parkinson’s disease, and extrapyramidal symptoms in schizophrenia. Absence of any laboratory tests hampers modulation of pharmacotherapy. Apolipoprotein E and α-synuclein have an important role in the neuropathology of these two diseases. The objective of this study was to evaluate cerebrospinal fluid (CSF) concentrations of apolipoprotein E and α-synuclein in patients with these two diseases so that they may serve as biomarkers to monitor therapy in Parkinson’s disease and schizophrenia.
Methods
Drug-naïve Parkinson’s disease patients and Parkinson’s disease patients treated with dopaminergic therapy, neurological controls, schizophrenic patients treated with antidopaminergic therapy, and drug-naïve schizophrenic patients were recruited for the study and CSF was collected. Enzyme-linked immunosorbent assays were carried out to estimate the concentrations of apolipoprotein E and α-synuclein. Pathway analysis was done to establish a possible role of these two proteins in various pathways in these two dopamine dictated diseases.
Results
Apolipoprotein E and α-synuclein CSF concentrations have an inverse correlation along the entire dopaminergic clinical spectrum. Pathway analysis convincingly establishes a plausible hypothesis for their co-regulation in the pathogenesis of Parkinson’s disease and schizophrenia. Each protein by itself or as a combination has encouraging sensitivity and specificity values of more than 55%.
Conclusion
The dynamic variation of these two proteins along the spectrum is ideal for them to be pursued as pharmacotherapeutic biomarkers in CSF to monitor pharmacological efficacy in Parkinson’s disease and schizophrenia.
Keywords: cerebrospinal fluid, Parkinson’s disease, schizophrenia, dopamine, apolipoprotein E, α-synuclein, biomarkers, treatment monitoring
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Parkinson’s disease is a progressive neurodegenerative disorder diagnosed based on the presence of motor symptoms like tremor, rigidity, bradykinesia, and postural instability.1 The prevalence increases with age and around 1–2% of the population over the age of 60 years is affected by Parkinson’s disease.2,3 Schizophrenia is a chronic mental disorder characterized by delusions, hallucinations, disorganized speech, or behavior and impaired cognitive ability.4 The worldwide prevalence of schizophrenia is 1%.1,5,6 Dopamine is an important neurotransmitter produced in the substantia nigra and ventral tegmental regions of the brain and its dysfunction plays a crucial role in both Parkinson’s disease and schizophrenia.7 In Parkinson’s disease, the decrease in dopamine in the substantia nigra of the mid-brain caused by selective loss of dopaminergic neurons has been implicated in disease pathology.8 On the contrary, dopamine hyperactivity is associated with schizophrenia.9 The treatment strategies for both the diseases exploit the difference in dopamine level from the baseline. In Parkinson’s disease, clinical intervention is aimed at increasing the concentration of dopamine in mid-brain.10 On the other hand, in schizophrenia, neuroleptics are prescribed which block dopamine receptors and decrease overall dopamine activity.11 However, there is a strong chance that during the treatment period patients develop symptoms related to the other extreme of dopamine spectrum, wherein Parkinson’s disease patients tend to develop psychosis, and schizophrenia patients tend to develop extrapyramidal side effects.12 This clinical scenario is depicted by the patients recruited in this study (Table 1).
Table 1.
Clinical profile of patients receiving pharmacological therapy and showing side effects
| Patient ID | Age (years) |
Gender | Clinical phenotype | Treatment (Generic) | Side effects |
|---|---|---|---|---|---|
| 01MA | 48 | Female | Schizophrenia | Olanzapine, risperidone | Tremor of hands, slow walking, no proper body balance for 4 years |
| 02RA | 34 | Male | Schizophrenia | Olanzapine, pramipexole, haloperidol | Impaired voice, body stiffness, fatigue, dizziness, slow body movements for 1.5 years |
| 03MA | 45 | Female | Schizophrenia | Olanzapine, risperidone | Unable to write, tremor of hands, dizziness, poor balance for 3 years |
| 04SH | 56 | Male | Schizophrenia | Olanzapine, haloperidol | Fatigue, daytime sleepiness, difficulty in walking, jaw stiffness for 3 years |
| 05AM | 79 | Male | Parkinson’s disease | Levodopa, carbidopa ropinirole, rasagiline | Depression and visual hallucinations for 2 years |
| 06TA | 56 | Male | Parkinson’s disease | Levodopa, carbidopa, ropinirole | Auditory hallucinations for 2 years |
| 07LA | 58 | Female | Parkinson’s disease | Levodopa, carbidopa, ropinirole | Claustrophobia, auditory hallucinations and delusions for 2.5 years |
| 08SI | 52 | Female | Parkinson’s disease | Levodopa, carbidopa, ropinirole | Visual hallucinations for 1 year |
| 09SA | 57 | Male | Parkinson’s disease | Levodopa, carbidopa, ropinirole | Delusion and hallucinations for 1 year |
Currently, there is no definite parameter to monitor the treatment and assist the clinicians to modulate therapy to avoid adverse effects. In this regard, biomarkers provide a convenient tool that can be objectively evaluated and used as an indicator of biological processes and pharmacologic response in the human body.13–15 Biomarker discovery for various diseases including neurological conditions has provided an efficient medium to monitor various disease conditions.16–18 Despite the discovery of many protein biomarkers for diagnosis or prognosis of Parkinson’s disease and schizophrenia, there is no significant clinical proteomic study to monitor drug therapy in these two diseases.19,20 The unavailability of reliable biomarkers to monitor drug therapy in Parkinson’s disease and schizophrenia provides opportunities for clinical proteomic-based biomarker discovery in this field. In the recent past, our group has been dedicatedly involved in protein biomarker discovery to assess treatment in both Parkinson’s disease and schizophrenia.21,22
Apolipoprotein E is a ligand for low-density lipoprotein receptors and is the most important lipid transport protein present in the brain.23 The gene is located on the chromosome19q13.2 with three alleles e2, e3, and e4.24 It is involved in many complex biological processes such as regulation of intracellular signaling, lipid metabolism, modulation of nitric oxide synthase-mediated cell proliferation, immune system regulation, and extracellular signaling.25–27 Apolipoprotein E is mainly synthesized by astrocytes in the brain and is known to be associated with various neurodegenerative disorders including Alzheimer’s disease and Parkinson's disease.28,29 It is a predominant genetic risk factor for Parkinson’s disease as it imparts vulnerability to early semantic memory impairment.30 In schizophrenia, aberrant apolipoprotein E signaling and the evidence of common receptors with schizophrenia susceptibility gene, reelin, supports its role in the disease pathology.31
α-synuclein is encoded by the SNCA gene located on the chromosome 4q22.1.32 It is abundantly expressed in the brain and is known to interact with lipids, presynaptic vesicles, and plasma membrane by lipid rafts.33–35 It is a core component of Lewy bodies which is a clinical hallmark for Parkinson’s disease.36 In addition, point mutations in the α-synuclein gene are known to be a risk factor for Parkinson’s disease.37 The association between α-synuclein expression and schizophrenia has been shown by a previous study.38 α-synuclein expression at the mRNA level is down regulated in lymphocytes of schizophrenic patients.39
The intricate association of apolipoprotein E and α-synuclein, with neuropsychiatric disorders, prompted us to study the expression of these proteins in cerebrospinal fluid (CSF) along the clinical dopaminergic spectrum, with a view to developing them as therapeutic efficacy monitoring biomarkers in Parkinson’s disease and schizophrenia.
Methods
Ethics, patient selection criteria, and consent
The study was approved by the ethics committee of All India Institute of Medical Sciences, New Delhi (Reference no.: IESC/T-418/26.08.2015), and the methods followed were as per the ethical standard formulated in the Helsinki declaration. The Parkinson’s disease and schizophrenia patients were screened and recruited for the study at the Department of Neurology and Department of Psychiatry, All India Institute of Medical Sciences, New Delhi, respectively. The neurological control group comprised of patients with bladder, prostate, and uterine pathologies, who were screened at urology and gynecology clinics at the institute. These patients were recruited for surgeries under spinal anesthesia. Before enrolling the patients in the study written informed consent was obtained. Briefly, 1.5 mL of CSF was collected under sterile conditions in microfuge tubes and was centrifuged at 4°C for 5 min at 3,000 rpm. The supernatant was taken in a separate microfuge tube and stored in −80°C until further experiments. Proper care was taken while collecting the CSF samples to avoid blood contamination, and samples with even minute contamination with blood were excluded from the study.
Patient inclusion and exclusion criteria
Inclusion criteria: The Unified Parkinson's Disease Rating Scale was used for screening patients with Parkinson’s disease according to which a score of zero represents no disability and a score of 199 represents complete disability.40 For describing the progress of symptoms in Parkinson’s disease patients, the Hoehn and Yahr scale was used and was graded from stage 1 to stage 5.41 ICD 10 was used to diagnose schizophrenia.42 Exclusion criteria: The patients with other disease or coexisting pathology or those under any therapeutic interventions were excluded from the study.
Enzyme-linked immunosorbent assay (ELISA)
The estimation of apolipoprotein E and α-synuclein in the recruited patients was done using ELISA kits (Elabscience, China). The methodology used was as per the manufacturer’s instruction protocol. The concentrations of apolipoprotein E and α-synuclein were extrapolated from the standard curves.
Statistical analysis
The mean concentrations for all the five groups were plotted and a linear curve with line equations and R2 value was obtained. Correlation coefficient and p-value (<0.05) for CSF apolipoprotein E and α-synuclein were obtained using Student’s t-test. Receiver operating characteristic (ROC) curve was obtained using GraphPad Prism (GraphPad Prism software, San Diego, CA, USA) to derive cut-off levels and area-under-the-curve for apolipoprotein E and α-synuclein in Parkinson’s disease and schizophrenia.
Pathway analysis
The entire information of genes corresponding to the identified proteins, their related functions were obtained from UniProt and from published literature in PubMed. Using this information, the proteins were analyzed for their biological interactions in Parkinson’s disease and schizophrenia pathways using KEGG and Schizo-Pi database.43 For visualizing the interaction and pathways of identified proteins and its interactors Cytoscape v2.8.0 software was used.44,45 Michigan Molecular Interactions plugin was used to collect the human gene regulatory interactome obtained from the public databases including STRING, MINT, MENTHA, and HPRD and merge the information.46–50 From this complete network, sub-networks for Parkinson’s disease and schizophrenia were obtained up to the first neighboring nodes using the plugin BiNoM v2.5. The resulting networks were merged using Cytoscape. Venn/Euler diagram was used to analyze the intersection between Parkinson’s disease and schizophrenia. The corresponding interactions of the identified proteins were noted and analyzed.
Results
Clinical profile
A total of 61 CSF samples of patients with Parkinson’s disease and schizophrenia were obtained from the neurology and psychiatry out-patient departments. The sample group included drug- naïve patients and those treated for Parkinson’s disease and schizophrenia and neurological controls. The demographic profile of the patients recruited for the study is mentioned in Table 2. The sex distribution of the patients has fewer females as compared to males. Also, the mean age of Parkinson’s disease patients is almost twice that of schizophrenia patients, and the mean age of the neurological control group is 61.4 years.
Table 2.
Demographic profile of patients recruited in the study
| Clinical phenotype | Average age (years) | Gender | Total | |
|---|---|---|---|---|
| Female | Male | |||
| Parkinson | 47.25 | 1 | 7 | 8 |
| Parkinson Treated | 52.75 | 3 | 25 | 28 |
| Neurological Control | 61.4 | 6 | 9 | 15 |
| Schizophrenia Treated | 27 | 1 | 5 | 6 |
| Schizophrenia | 25 | 0 | 4 | 4 |
| Total | 61 | |||
Apolipoprotein E and α-synuclein expression in CSF of Parkinson’s disease and schizophrenia
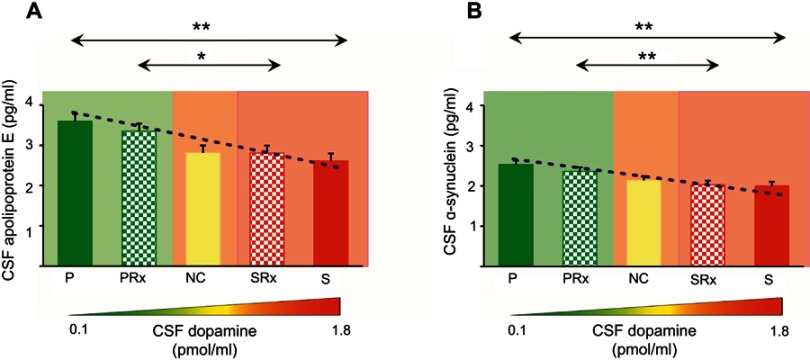
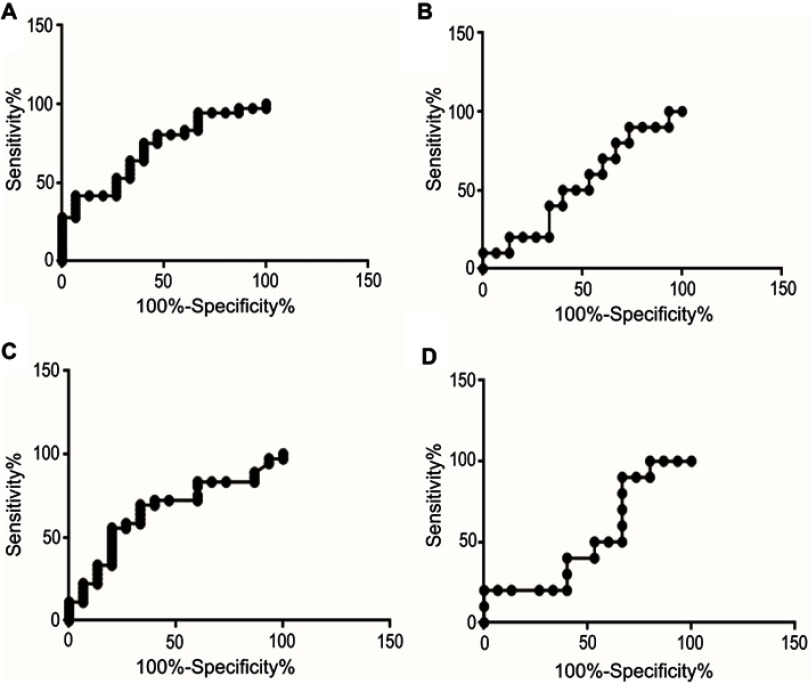
ELISA was done to determine the CSF concentrations of apolipoprotein E and α-synuclein across five groups; (1) drug-naïve Parkinson’s disease, (2) treated Parkinson’s disease, (3) neurological controls, (4) drug-naïve schizophrenia and, (5) treated schizophrenia. The relationship between apolipoprotein E and α-synuclein concentrations and dopamine level in CSF is represented in Figure 1. It should also be noted that the concentrations of both apolipoprotein E and α-synuclein correlate with each other as indicated by a positive correlation coefficient value of 0.5 in Figure 2. ROC curve was plotted for apolipoprotein E and α-synuclein levels in CSF in Parkinson’s disease, neurological control, and schizophrenia as shown in Figure 3. Individual values corresponding to the cut-off values, sensitivity, and specificity are given in Table 3. It can be observed that when either of the two proteins, apolipoprotein E and α-synuclein, were considered for evaluation with the individual estimated cut-off values, the sensitivity and specificity values ranged from 53.3% to 79.3%.
Figure 1.
ELISA for expression of (A) apolipoprotein E and (B) α-synuclein in the cerebrospinal fluid (CSF) of Parkinson’s disease, neurological controls, and schizophrenia patients. Clinical phenotypes comprise of Parkinson’s disease naïve (P), Parkinson’s treated (PRx), neurological controls of patients with urological and gynecological diseases needing surgical intervention (NC), schizophrenia treated (SRx), and schizophrenia naïve patients (S). Mean ± Standard error of mean of the values is shown by horizontal lines. The bars represent the concentrations as the average of duplicate readings of each patient sample. Trend lines of apolipoprotein E (y=−0.25x+3.78; R2=0.91) and α-synuclein (y=−0.14x+2.63; R2=0.94) across the five clinical phenotypes is shown as a blue dotted line in (A) and (B), respectively. Diagrammatic representation of the dopamine concentration in cerebrospinal fluid (CSF) is shown along the x-axis. Concentrations of dopamine in the CSF across the clinical phenotypes has been estimated in Gao et al and Jensen et al.47,48 * indicates statistical significance with p<0.05.
Figure 2.
Correlation analysis for apolipoprotein E expression and alpha-synuclein. The correlation coefficient (R2) has a value of 0.5 and a statistical significance (p) of 0.05. Abbreviation: CSF, cerebrospinal fluid.
Figure 3.
Receiver Operating Characteristic (ROC) for cut-offs that best differentiate disease from controls. (A) Apolipoprotein E for Parkinson’s disease and neurological control; (B) Apolipoprotein E for schizophrenia and control; (C) α-synuclein for Parkinson’s disease and control; and, (D) α-synuclein for schizophrenia and control.
Table 3.
Pharmacotherapeutic monitoring value of Apolipoprotein E and α-synuclein in Parkinson’s disease and schizophrenia
| Biomarker | Cut-off values to differentiate neurological controls from the disease | Parameters | |
|---|---|---|---|
| Sensitivity (%) | Specificity (%) | ||
| Apolipoprotein E | >3.4 pg (Parkinson’s disease) | 41.7 | 86.7 |
| Apolipoprotein E | <2.6 pg (Schizophrenia) | 50.0 | 60.0 |
| α-synuclein | >2.2 pg (Parkinson’s disease) | 55.6 | 80.0 |
| α-synuclein | <1.9 pg (Schizophrenia) | 20.0 | 93.3 |
| Apolipoprotein E or α-synuclein | >3.4 pg (Parkinson’s disease) | 79.3 | 66.6 |
| >2.2 pg (Parkinson’s disease) | |||
| Apolipoprotein E or α-synuclein | <2.6 pg (Schizophrenia) | 60.0 | 53.3 |
| <1.9 pg (Schizophrenia) | |||
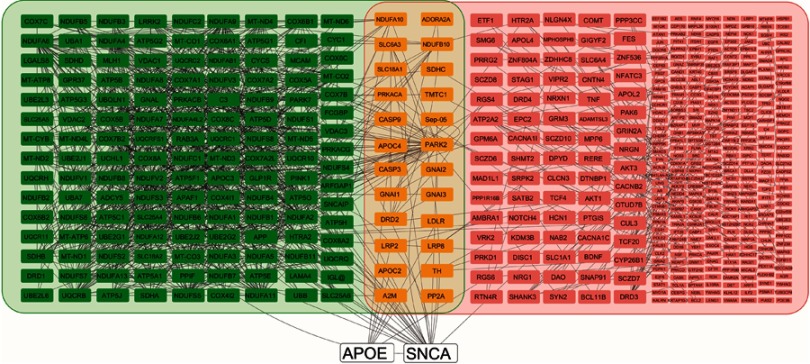
Pathway analysis
Pathway analysis was carried out to study the interactions of these proteins in these dopamine dictated diseases. A total of 25 proteins were found to be directly interacting with apolipoprotein E and α-synuclein in Parkinson’s disease, and 18 proteins were found to be directly interacting with apolipoprotein E and α-synuclein in schizophrenia, with 13 proteins being common amongst the two groups (Figure 4). The functions of these proteins and their relevance in this study have been delineated in Table 4. A hypothesis has been proposed based on the ELISA results, highlights of the pathway analysis, information from previous studies, and the same has been diagrammatically represented in Figure 5.
Figure 4.
Pathway analysis shows apolipoprotein E and alpha-synuclein, and their respective interactions. apolipoprotein E and alpha-synuclein are shown in white nodes, interacting nodes in Parkinson’s disease pathway are highlighted in green, interacting nodes in schizophrenia pathway are highlighted in pink, and nodes that common to both the groups are highlighted in yellow. Those nodes in the schizophrenia group that have four or more than four interactions are indicated in larger size boxes and those less than four are indicated by smaller boxes. All the interactions are shown by gray lines.
Table 4.
Interactions of apolipoprotein E and α-synuclein in the pathogenesis of Parkinson’s disease and schizophrenia
| Protein | Function | Relevance in this study | References |
|---|---|---|---|
| Voltage-dependent anion channels |
|
|
51–57 |
| NADH:ubiquinone oxidoreductase subunit S3 |
|
|
58 |
| Synphilin-1 |
|
|
59, 60 |
| ADP-ribosylation factor GTPase-activating protein 1 |
|
|
61 |
| Protein phosphatase-2A |
|
|
62–64 |
| Sodium-dependent dopamine transporter |
|
|
65, 66 |
| Microtubule-associated protein tau |
|
|
67 |
| AKT_Serine/threonine kinase-1 |
|
|
68 |
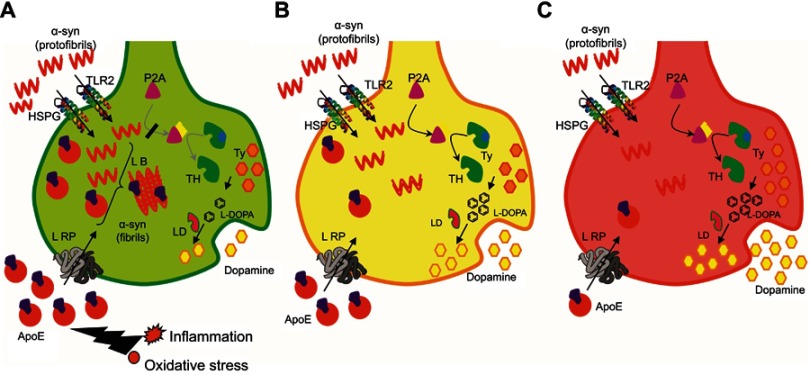
Figure 5.
Diagrammatic representation of neuronal synapse depicting experimental result-based hypotheses that explain molecular events in Parkinson’s disease, neurological controls, and schizophrenia.
Abbreviations: HSPG, Heparan Sulphate Proteo-Glycan; TLR2, Toll-Like Receptor 2; LRP, Low density lipid Receptor Protein; L-DOPA, Levo-Dopa; P2A, phosphatase 2A; LB, Lewy body; LD, L-decarboxylase; TH, tyrosine hydroxylase; Ty, tyrosine.
Discussion
Clinical profile
The incidence of Parkinson’s disease and schizophrenia majorly affects the male population; therefore, the sex distribution of the patients has fewer females as compared to males.69 Secondly, the mean age of Parkinson’s disease patients is almost double that of schizophrenia patients because the incidence of Parkinson’s disease increases above the age of 60 years, with only 4% of the affected being under the age of 50 years.70 On the other hand, the incidence of schizophrenia occurs between 16 and 25 years.71 The mean age of the neurological control group is 61.4 years since the patients selected as neurological controls were those requiring surgical intervention for urological disorders which presents around this age.72 The drug-naïve patients of Parkinson’s disease and schizophrenia represent the extreme end points of dopamine spectrum, patients who have been treated represent time frames within this spectrum, and neurological controls represent the mid-point of the spectrum that defines the physiological range of dopamine.
Correlation of apolipoprotein E and α-synuclein expression in CSF of Parkinson’s disease and schizophrenia
The concentrations of both apolipoprotein E and α-synuclein inversely correlate with the dopamine concentrations. It is higher in drug-naïve Parkinson’s disease patients and linearly decreases through treated Parkinson’s disease, neurological controls, treated schizophrenia patients and drug-naïve schizophrenia patients. Such a relationship of apolipoprotein E and α-synuclein concentrations with the dopamine levels provides a window of opportunity to modulate treatment in a way that patients do not develop side effects. According to the ROC curve each protein, apolipoprotein E and α-synuclein, individually or as a combination has sensitivity and specificity values of around 54%. This would, therefore, mean that using these protein biomarkers for monitoring therapeutic efficacy would help to reduce the number of patients affected by drug-induced side effects in these two diseases by more than half. These results and data are very encouraging from a translational point of view in the field of neuropsychiatry. It may be noted that though the patients were phenotypes and grouped based on certain clinical criteria, there exists a vast heterogeneity among the patients with respect to the age of onset of the disease, stage of the disease, quality of drug intervention, duration of therapy, personal habits, and habitat. This explains the subtle variations in the concentrations of these two proteins.
Interaction-based pathway analysis involving apolipoprotein E and α-synuclein in Parkinson’s disease and schizophrenia
In order to understand the role of apolipoprotein E and α-synuclein in the pathogenesis of Parkinson’s disease and schizophrenia, it becomes important to study the interaction of these proteins in the dopaminergic pathway and subsequent cellular damage. Based on these interactions, pathway analysis was carried out to place the observed experimental outcomes in the right perspective. The protein interactions and cellular mechanisms explaining the observed results are shown in Figure 5 and is discussed below.
(A) Apolipoprotein E is the most abundant apolipoprotein present in the brain and is mostly synthesized by the astrocytes.73 It is a cholesterol transport protein which is found associated with high-density lipoprotein (HDL).74,75 The most common apolipoprotein E receptor is low-density lipoprotein receptor-related protein (LRP) which is involved in its uptake across the plasma membrane.25 Apolipoprotein E and LRP play a major role in cholesterol regulation which affects processes related to abnormal turnover of synaptic proteins.76 This turnover is a response mechanism to counter the damage at synaptic terminals because of inflammation or oxidative stress, both of which are elevated in Parkinson’s disease.77 In a previous study by our group, the level of alpha-2-macroglobulin was found to be elevated in Parkinson’s disease as compared to schizophrenia.22 Interestingly, LRP is a common receptor for apolipoprotein E, alpha-2-macroglobulin and amyloid precursor protein.78 This further strengthens the combined role of neuronal damage induced compensatory response involving LRP, apolipoprotein E, and α-synuclein.
(B) α-synuclein is majorly a cytosolic protein; however, its secretion into extracellular space has been established.79 Extracellular α-synuclein has a heterogeneous population including both monomeric and oligomeric forms that interact with Toll-like receptor 2 which is involved in its uptake.80,81 Cell surface heparan sulfate proteoglycans are also known to be involved in apolipoprotein E-mediated uptake of α-synuclein.82 α-synuclein binds to cholesterol and modulates α-synuclein aggregation and its association with HDL.83–85 Apolipoprotein E increases aggregation of α-synuclein which is a known component of Lewy bodies and promotes neurodegeneration.86
(C) α-synuclein also interacts with protein phosphatase 2A (PP2A) and increases its activity, activated PP2A is involved in dephosphorylation of tyrosine hydroxylase, which is a critical enzyme in dopamine metabolism, therefore leads to a reduction of dopamine levels.66 α-synuclein is also known to bind to tyrosine hydroxylase gene promoter and down regulate its expression.87 This is substantiated by the fact that there is a decreased level of tyrosine hydroxylase mRNA in Parkinson’s disease.88
(D) The inverse relationship between apolipoprotein E and α-synuclein to the dopamine spectrum represented by clinical phenotypes including Parkinson’s disease, neurological controls, and schizophrenia is very interesting. β2-adrenergic receptor agonists (β2AR) are known to mimic endogenous catecholamines like dopamine, norepinephrine, and epinephrine.89 β2AR activation decreases histone acetylation of the α-synuclein gene and suppresses its transcription.90 α-synuclein in association with ATP-binding cassette sub-family A member 1 (ABCA1), a plasma membrane transporter protein, is known to increase the cholesterol efflux mechanism.91 In the brain, deficiency of ABCA1 which is required for cholesterol efflux to apolipoprotein E leads to reduced lipidation and an overall decrease of apolipoprotein E levels.92
(E) In addition, psychotropic drugs up-regulate the expression of apolipoprotein E by activation of sterol regulatory element-binding protein transcription factors through an intracellular oxysterol sensor, liver X-receptor.93 Liver X-receptor has been shown to positively regulate α-synuclein expression.94 On the contrary, levodopa-induced lipogenesis inhibition has only been shown in certain non-neurological tissues.95
(F) Oxidative stress is another important parameter that regulates apolipoprotein E and α-synuclein in Parkinson’s disease and schizophrenia. Oxidative stress is known to be elevated in Parkinson’s disease and is decreased in schizophrenia.96 The increased formation of reactive oxygen species in dopaminergic neurons in Parkinson’s disease leads to the formation of cholesterol aldehydes that enable α-synuclein aggregation, leading to a pathologic cycle.97 Alterations in lipid metabolism have an important role in the pathogenesis of Parkinson’s disease since there is direct cross-talk between lipids and α-synuclein, influencing both lipid metabolism and α-synuclein aggregation.98,99 In the brain, apolipoprotein E is expressed by astrocytes and perivascular cells under normal conditions. However, it has also been found to be intra-neuronally expressed. Such a pattern of apolipoprotein E expression is seen when neurons are under stress conditions.100 Increased apolipoprotein E formation under such conditions can affect neuronal survival due to the formation of a C-terminal truncated form which causes mitochondrial impairment in neurons.101
Conclusion
Apolipoprotein E and α-synuclein CSF concentrations have an inverse correlation along the entire dopaminergic clinical spectrum comprising of Parkinson’s disease and schizophrenia. Each protein by itself or as a combination has the ability to differentiate either of the pathological states from the physiological state. Pathway analysis supports the mechanism of coregulation in the pathogenesis of the two diseases. The dynamic variation of these two proteins along the spectrum is ideal for them to be pursued as pharmacotherapeutic biomarkers in CSF to monitor pharmacological efficacy in Parkinson’s disease and schizophrenia with a reasonable accuracy. Outcome of this study will be helpful for the clinicians and patients to monitor pharmacotherapy and make informed treatment decisions in Parkinson’s disease and schizophrenia.
Acknowledgments
An abstract of this paper titled ‘Evaluation of apolipoprotein E and α-synuclein as potential biomarkers in CSF to monitor pharmaco-therapeutic efficacy in dopamine dictated disease states of Parkinson’s disease and schizophrenia’ was published in the 2019 Science Program, by the American Academy of Neurology as a part of the Annual Meeting held in Philadelphia, PA, USA, in May 2019 ((http://indexsmart.mirasmart.com/AAN2019/PDFfiles/AAN2019-000045.pdf).
GH acknowledges Department of Science and Technology, Government of India for the grant SO/BB-0122/2013 (D-348). The work was partly carried out at the Proteomics Division at Central Core Research Facility at AIIMS, New Delhi, India.
Disclosure
The authors report no conflicts of interest in regard to this work.
References
- 1.Mollenhauer B, Weintraub D. The depressed brain in Parkinson’s disease: implications for an inflammatory biomarker. Proc Natl Acad Sci U S A. 2017;114(12):3004–3005. doi: 10.1073/pnas.1700737114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Lau LM, Breteler MM. Epidemiology of Parkinson’s disease. Lancet Neurol. 2006;5(6):525–535. doi: 10.1016/S1474-4422(06)70471-9 [DOI] [PubMed] [Google Scholar]
- 3.Mehanna R, Moore S, Hou JG, Sarwar AI, Lai EC. Comparing clinical features of young onset, middle onset and late-onset Parkinson’s disease. Parkinsonism Relat Disord. 2014;20(5):530–534. doi: 10.1016/j.parkreldis.2014.02.013 [DOI] [PubMed] [Google Scholar]
- 4.Patel KR, Cherian J, Gohil K, Atkinson D. Schizophrenia: overview and treatment options. PT. 2014;39(9):638–645. [PMC free article] [PubMed] [Google Scholar]
- 5.Gore FM, Bloem PJ, Patton GC, et al. Global burden of disease in young people aged 10–24 years: a systematic analysis. Lancet. 2011;377(9783):2093–2102. doi: 10.1016/S0140-6736(11)60512-6 [DOI] [PubMed] [Google Scholar]
- 6.Millan MJ, Andrieux A, Bartzokis G, et al. Altering the course of schizophrenia: progress and perspectives. Nat Rev Drug Discov. 2016;15(7):485–515. doi: 10.1038/nrd.2016.28 [DOI] [PubMed] [Google Scholar]
- 7.Bogerts B, Häntsch J, Herzer M. A morphometric study of the dopamine-containing cell groups in the mesencephalon of normals, Parkinson patients, and schizophrenics. BiolPsychiatry. 1983;18(9):951–969. [PubMed] [Google Scholar]
- 8.Kinoshita K, Tada Y, Muroi Y. Selective loss of dopaminergic neurons in the substantia nigra pars compacta after systemic administration of MPTP facilitates extinction learning. Life Sci. 2015;137:28–36. doi: 10.1016/j.lfs.2015.07.017 [DOI] [PubMed] [Google Scholar]
- 9.Grace A. Dopamine system dysregulation by the hippocampus: implications for the pathophysiology and treatment of schizophrenia. Neuropharmacology. 2012;62(3):1342–1348. doi: 10.1016/j.neuropharm.2011.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jankovic J, Aguilar LG. Current approaches to the treatment of Parkinson’s disease. Neuropsychiatr Dis Treat. 2008;4(4):743–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li P, Snyder GL, Vanover KE. Dopamine targeting drugs for the treatment of schizophrenia: past, present, and future. Curr Top Med Chem. 2016;16(29):3385–3403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Caroff SN, Hurford I, Lybrand J, Campbell EC. Movement disorders induced by antipsychotic drugs: implications of the CATIE schizophrenia trial. Neurol Clin. 2011;29(1):127–128. doi: 10.1016/j.ncl.2010.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hariprasad G, Hariprasad R, Kumar L, Srinivasan A, Kola S, Kaushik A. Apolipoprotein A1 as a potential biomarker in the ascitic fluid for the differentiation of advanced ovarian cancers. Biomarkers. 2013;18(6):532–541. doi: 10.3109/1354750X.2013.822561 [DOI] [PubMed] [Google Scholar]
- 14.Rukmangadachar LA, Makharia GK, Mishra A, et al. Proteome analysis of the macroscopically affected colonic mucosa of Crohn’s disease and intestinal tuberculosis. Sci Rep. 2016;6:23162. doi: 10.1038/srep23162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sehrawat U, Pokhriyal R, Gupta AK, et al. Proteomic analysis of advanced ovarian cancer tissue to identify potential biomarkers of responders and nonresponders to first-line chemotherapy of carboplatin and paclitaxel. Biomark Cancer. 2016;16(8):43–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kataria J, Rukmangadachar LA, Hariprasad G, et al. Two-dimensional difference gel electrophoresis analysis of cerebrospinal fluid in tuberculous meningitis patients. J Proteomics. 2011;74(10):2194–2203. doi: 10.1016/j.jprot.2011.06.020 [DOI] [PubMed] [Google Scholar]
- 17.Rukmangadachar LA, Kataria J, Hariprasad G, Samantaray JC, Srinivasan A. Two-dimensional difference gel electrophoresis (DIGE) analysis of sera from visceral leishmaniasis patients. Clin Proteomics. 2011;8(1):4. doi: 10.1186/1559-0275-8-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Manral P, Sharma P, Hariprasad G, Chandralekha TM, Srinivasan A. Can apolipoproteins and complement factors be biomarkers of Alzheimer’s disease? CurrAlzheimer Res. 2012;9(8):935–943. [DOI] [PubMed] [Google Scholar]
- 19.Chahine LM, Stern MB, Chen-Plotkin A. Blood-based biomarkers for Parkinson’s disease. ParkinsonismRelatDisord. 2014;20:S99–S103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sabherwal S, English JA, Föcking M, Cagney G, Cotter DR. Blood biomarker discovery in drug-free schizophrenia: the contribution of proteomics and multiplex immunoassays. Expert Rev Proteomics. 2016;13(12):1141–1155. doi: 10.1080/14789450.2016.1252262 [DOI] [PubMed] [Google Scholar]
- 21.Gupta AK, Rani K, Swarnkar S, et al. Evaluation of serum apolipoprotein E as a potential biomarker for pharmacological therapeutic efficacy monitoring in dopamine dictated disease spectrum of schizophrenia and Parkinson’s disease. J Cent NervSyst Dis. 2018;10:1179573518803585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gupta AK, Kumar GK, Rani K, et al. 2D-DIGE as a strategy to identify serum protein biomarkers to monitor pharmacological efficacy in dopamine dictated states of Parkinson’s disease and schizophrenia. Neuropsychiatr Dis Treat. 2019;15:1031–1044. doi: 10.2147/NDT.S198559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mahley RW. Apolipoprotein E: cholesterol transport protein with expanding role in cell biology. Science. 1988;240(4852):622–630. [DOI] [PubMed] [Google Scholar]
- 24.Yu CE, Cudaback E, Foraker J, et al. Epigenetic signature and enhancer activity of the human APOE gene. Hum Mol Genet. 2013;22(24):5036–5047. doi: 10.1093/hmg/ddt354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mahley RW, Ji ZS. Remnant lipoprotein metabolism: key pathways involving cell-surface heparan sulfate proteoglycans and apolipoprotein E. J Lipid Res. 1999;40(1):1–6. [PubMed] [Google Scholar]
- 26.Mahley RW, Rall SC Jr. Apolipoprotein E: far more than a lipid transport protein. Annu Re Genomics Hum Genet. 2000;1:507–537. doi: 10.1146/annurev.genom.1.1.507 [DOI] [PubMed] [Google Scholar]
- 27.Zerba KE, Ferrell RE, Sing CF. Complex adaptive systems and human health: the influence of common genotypes of the apolipoprotein E (ApoE) gene polymorphism and age on the relational order within a field of lipid metabolism traits. Hum Genet. 2000;107(5):466–475. [DOI] [PubMed] [Google Scholar]
- 28.Harhangi BS, de Rijk MC, Van Duijn CM, et al. APOE and the risk of PD with or without dementia in a population-based study. Neurology. 2000;54(6):1272–1276. doi: 10.1212/wnl.54.6.1272 [DOI] [PubMed] [Google Scholar]
- 29.Souza DR, de Godoy MR, Hotta J, et al. Association of apolipoprotein E polymorphism in late-onset Alzheimer’s disease and vascular dementia in Brazilians. Braz J Med Biol Res. 2003;36(7):919–923. doi: 10.1590/s0100-879x2003000700013 [DOI] [PubMed] [Google Scholar]
- 30.Mata IF, Leverenz JB, Weintraub D, et al. APOE, MAPT, SNCA, and cognitive performance in Parkinson disease. JAMA Neurol. 2014;71(11):1405–1412. doi: 10.1001/jamaneurol.2014.1455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gibbons AS, Udawela M, Jeon WJ, Seo MS, Brooks L, Dean B. The neurobiology of APOE in schizophrenia and mood disorders. Front Biosci. 2011;16:962–979. doi: 10.2741/3729 [DOI] [PubMed] [Google Scholar]
- 32.Chen X, de Silva HA, Pettenati MJ, et al. The human NACP/α-synuclein gene: chromosome assignment to 4q21.3-q22 and TaqI RFLP analysis. Genomics. 1995;26(2):425–427. [DOI] [PubMed] [Google Scholar]
- 33.Withers GS, George JM, Banker GA, Clayton DF. Delayed localization of synelfin (synuclein, NACP) to presynaptic terminals in cultured rat hippocampal neurons. Brain Res Dev Brain Res. 1997;99:87–94. [DOI] [PubMed] [Google Scholar]
- 34.Jo E, McLaurin J, Yip CM, St George-Hyslop P, Fraser PE. α-synuclein-membrane interactions and lipid specificity. J Biol Chem. 2000;275(44):34328–34334. doi: 10.1074/jbc.M004345200 [DOI] [PubMed] [Google Scholar]
- 35.Fortin DL, Troyer MD, Nakamura K, Kubo S, Anthony MD, Edwards RH. Lipid rafts mediate the synaptic localization of α-synuclein. J Neurosci. 2004;24(30):6715–6723. doi: 10.1523/JNEUROSCI.1594-04.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xu L, Pu J. α-synuclein in Parkinson’s disease: from pathogenetic dysfunction to potential clinical application. Parkinsons Dis. 2016;2016:1720621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Olanow CW, Brundin P. Parkinson’s disease and alpha-synuclein: is Parkinson’s disease a prion-like disorder? Mov Disord. 2013;28(1):31–40. doi: 10.1002/mds.25373 [DOI] [PubMed] [Google Scholar]
- 38.Demirel ÖF, Cetin İ, Turan Ş, Sağlam T, Yıldız N, Duran A. Decreased expression of α-Synuclein, Nogo-A, and UCH-L1 in patients with schizophrenia: a preliminary serum study. Psychiatry Investig. 2017;14(3):344–349. doi: 10.4306/pi.2017.14.3.344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Noori-Daloii MR, Kheirollahi M, Mahbod P, et al. Alpha- and beta-synucleins mRNA expression in lymphocytes of schizophrenia patients. Genet Test Mol Biomarkers. 2010;14(5):725–729. doi: 10.1089/gtmb.2010.0050 [DOI] [PubMed] [Google Scholar]
- 40.Chou KL, Taylor JL, Patil PG. The MDS–UPDRS tracks motor and non– a motor improvement due to subthalamic nucleus deep brain stimulation in Parkinson disease. Parkinsonism Relat Disord. 2013;19(11):966–969. doi: 10.1016/j.parkreldis.2013.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Goetz CG, Poewe W, Rascol O, et al. Movement disorder society task force report on the Hoehn and Yahr staging scale: status and recommendation. Mov Disord. 2004;19:1020–1028. doi: 10.1002/mds.20213 [DOI] [PubMed] [Google Scholar]
- 42.World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders. Clinical descriptions and diagnostic guidelines. Available from: https://apps.who.int/iris/handle/10665/37958. Accessed June 28, 2019. [Google Scholar]
- 43.Ganapathiraju MK, Thahir M, Handen A, et al. Schizophrenia interactome with 504 novel protein-protein interactions. NPJ Schizophr. 2016;2:16012. doi: 10.1038/npjschz.2016.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shannon P, Markiel A, Ozier O, et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 2003;13(11):2498–2504. doi: 10.1101/gr.1239303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Smoot ME, Ono K, Ruscheinski J, Wang PL, Ideker T. Cytoscape 2.8: new features for data integration and network visualization. Bioinformatics. 2011;27(3):431–432. doi: 10.1093/bioinformatics/btq675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chatr-Aryamontri A, Ceol A, Palazzi LM, et al. MINT: the Molecular INTeraction database. Nucleic Acids Res. 2007;35:D572–D574. doi: 10.1093/nar/gkl950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gao J, Ade AS, Tarcea VG, et al. Integrating and annotating the interactome using the MiMI plugin for Cytoscape. Bioinformatics. 2009;5(1):137–138. doi: 10.1093/bioinformatics/btn501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jensen LJ, Kuhn M, Stark M, et al. STRING 8-a global view on proteins and their functional interactions in 630 organisms. Nucleic Acids Res. 2009;37:D412–D416. doi: 10.1093/nar/gkn760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Keshava Prasad TS, Goel R, Kandasamy K, et al. Human protein reference database-2009 update. Nucleic Acids Res. 2009;37(Database issue):D767–D772. doi: 10.1093/nar/gkn892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Calderone A, Castagnoli L, Cesareni G. Mentha: a resource for browsing integrated protein-interaction networks. Nat Methods. 2013;10(8):690–691. doi: 10.1038/nmeth.2561 [DOI] [PubMed] [Google Scholar]
- 51.Rostovtseva TK, Gurnev PA, Protchenko O, et al. α-synuclein shows high-affinity interaction with voltage-dependent anion channel, suggesting mechanisms of mitochondrial regulation and toxicity in Parkinson disease. J Biol Chem. 2015;290(30):18467–18477. doi: 10.1074/jbc.M115.641746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lu L, Zhang C, Cai Q, et al. Voltage-dependent anion channel involved in the α-synuclein-induced dopaminergic neuron toxicity in rats. Acta Biochim Biophys Sin. 2013;45(3):170–178. doi: 10.1093/abbs/gms114 [DOI] [PubMed] [Google Scholar]
- 53.Halestrap AP. What is the mitochondrial permeability transition pore? J Mol Cell Cardiol. 2009;46(6):821–831. doi: 10.1016/j.yjmcc.2009.02.021 [DOI] [PubMed] [Google Scholar]
- 54.Beutner G, Rück A, Riede B, Brdiczka D. Complexes between porin, hexokinase, mitochondrial creatine kinase and adenylate translocator display properties of the permeability transition pore. The implication for regulation of permeability transition by the kinases. Biochim Biophys Acta. 1998;1368(1):7–18. [DOI] [PubMed] [Google Scholar]
- 55.Tsujimoto Y, Shimizu S. Role of the mitochondrial membrane permeability transition in cell death. Apoptosis. 2007;12(5):835–840. doi: 10.1007/s10495-006-0525-7 [DOI] [PubMed] [Google Scholar]
- 56.Schinzel AC, Takeuchi O, Huang Z, et al. Cyclophilin D is a component of mitochondrial permeability transition and mediates neuronal cell death after focal cerebral ischemia. Proc Natl Acad Sci USA. 2005;102(34):12005–12010. doi: 10.1073/pnas.0505294102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gincel D, Shoshan-Barmatz V. Glutamate interacts with VDAC and modulates the opening of the mitochondrial permeability transition pore. J Bioenerg Biomembr. 2004;36(2):179–186. [DOI] [PubMed] [Google Scholar]
- 58.McFarland MA, Ellis CE, Markey SP, Nussbaum RL. Proteomics analysis identifies phosphorylation-dependent α-synuclein protein interactions. Mol Cell Proteomics. 2008;7(11):2123–2137. doi: 10.1074/mcp.M800116-MCP200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liani E, Eyal A, Avraham E, et al. Ubiquitylation of synphilin-1 and α-synuclein by SIAH and its presence in cellular inclusions and Lewy bodies imply a role in Parkinson’s disease. Proc Natl Acad Sci. 2004;101(15):5500–5555. doi: 10.1073/pnas.0401081101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dashtipour K, Tafreshi A, Adler C, et al. Hypermethylation of synphilin-1, Α-synuclein-interacting protein (SNCAIP) gene in the cerebral cortex of patients with sporadic Parkinson’s disease. Brain Sci. 2017;7:7. doi: 10.3390/brainsci7070074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stafa K, Trancikova A, Webber PJ, Glauser L, West AB, Moore DJ. GTPase activity and neuronal toxicity of Parkinson’s disease-associated LRRK2 is regulated by ArfGAP1. GTPase activity and neuronal toxicity of Parkinson’s disease-associated LRRK2 is regulated by ArfGAP1. PLoS Genet. 2012;8(2):e1002526. doi: 10.1371/journal.pgen.1002526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wu J, Lou H, Alerte TN, et al. Lewy-like aggregation of α-synuclein reduces protein phosphatase 2A activity in vitro and in vivo. Neuroscience. 2012;07:288–297. doi: 10.1016/j.neuroscience.2012.01.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hua G, Xiaolei L, Weiwei Y, et al. Protein phosphatase 2A is involved in the tyrosine hydroxylase phosphorylation regulated by α-synuclein. Neurochem Res. 2015;40(3):428–437. doi: 10.1007/s11064-014-1477-x [DOI] [PubMed] [Google Scholar]
- 64.Peng X, Tehranian R, Dietrich P, Stefanis L, Perez RG. α-Synuclein activation of protein phosphatase 2A reduces tyrosine hydroxylase phosphorylation in dopaminergic cells. J Cell Sci. 2005;118(15):3523–3530. doi: 10.1242/jcs.02481 [DOI] [PubMed] [Google Scholar]
- 65.Lee FJ, Liu F, Pristupa ZB, Niznik HB. Direct binding and functional coupling of α-synuclein to the dopamine transporters accelerate dopamine-induced apoptosis. Faseb J. 2001;15(6):916–926. doi: 10.1096/fj.00-0334com [DOI] [PubMed] [Google Scholar]
- 66.Wersinger C, Sidhu A. Attenuation of dopamine transporter activity by α-synuclein. Neurosci Lett. 2003;340(3):189–192. [DOI] [PubMed] [Google Scholar]
- 67.Kawakami F, Yabata T, Ohta E, et al. LRRK2 phosphorylates tubulin-associated tau but not the free molecule: LRRK2-mediated regulation of the tau-tubulin association and neurite outgrowth. PLoS One. 2012;7(1):e30834. doi: 10.1371/journal.pone.0030834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ohi K, Hashimoto R, Yasuda Y, et al. The AKT1 gene is associated with attention and brain morphology in schizophrenia. World J Biol Psychiatry. 2013;14(2):100–113. doi: 10.3109/15622975.2011.591826 [DOI] [PubMed] [Google Scholar]
- 69.Loke H, Harley V, Lee J. Biological factors underlying sex differences in neurological disorders. Int J Biochem Cell Biol. 2015;65:139–150. doi: 10.1016/j.biocel.2015.05.024 [DOI] [PubMed] [Google Scholar]
- 70.Van Den Eeden SK, Tanner CM, Bernstein AL, et al. The incidence of Parkinson’s disease: variation by age, gender, and race/ethnicity. Am J Epidemiol. 2003;157(11):1015–1022. doi: 10.1093/aje/kwg068 [DOI] [PubMed] [Google Scholar]
- 71.Sham PC, MacLean CJ, Kendler KS. A typological model of schizophrenia based on age at onset, sex, and familial morbidity. Acta Psychiatr Scand. 1994;89(2):135–141. [DOI] [PubMed] [Google Scholar]
- 72.Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL. Harrisons Principles of Internal Medicine. 16th ed. London: Mcgraw Hill Medical Publishing Division; 2005. [Google Scholar]
- 73.Wilhelmus MM, Bol JG, Van Haastert ES, et al. Apolipoprotein E and LRP1 increase early in Parkinson’s disease pathogenesis. Am J Pathol. 2011;179(5):2152–2156. doi: 10.1016/j.ajpath.2011.07.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Vance JE, Hayashi H. Formation and function of apolipoprotein E-containing lipoproteins in the nervous system. Biochim Biophys Acta. 2010;1801(8):806–818. doi: 10.1016/j.bbalip.2010.02.007 [DOI] [PubMed] [Google Scholar]
- 75.Vitali C, Wellington CL, Calabresi L. HDL and cholesterol handling in the brain. Cardiovasc Res. 2014;103(3):405–413. doi: 10.1093/cvr/cvu148 [DOI] [PubMed] [Google Scholar]
- 76.de Chaves EP, Narayanaswami V. Apolipoprotein E and cholesterol in aging and disease in the brain. Future Lipidol. 2008;3(5):505–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Iwai A. Properties of NACP/α-synuclein and its role in Alzheimer’s disease. Biochim Biophys Acta. 2000;1502(1):95–109. [DOI] [PubMed] [Google Scholar]
- 78.Marzolo MP, von Bernhardi R, Bu G, Inestrosa NC. Expression of alpha(2)-macroglobulin receptor/low-density lipoprotein receptor-related protein (LRP) in rat microglial cells. J Neurosci Res. 2000;60(3):401–411. doi: [DOI] [PubMed] [Google Scholar]
- 79.Lee HJ, Bae EJ, Lee SJ. Extracellular α–synuclein-a novel and the crucial factor in Lewy body diseases. Nat Rev Neurol. 2014;10(2):92–98. doi: 10.1038/nrneurol.2013.275 [DOI] [PubMed] [Google Scholar]
- 80.Danzer KM, Kranich LR, Ruf WP, et al. Exosomal cell-to-cell transmission of alpha-synuclein oligomers. Mol Neurodegener. 2012;24:7–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Dzamko N, Gysbers A, Perera G, et al. Toll-like receptor 2 is increased in neurons in Parkinson’s disease brain and may contribute to α-synuclein pathology. Acta Neuropathological. 2017;133(2):303–319. doi: 10.1007/s00401-016-1648-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Holmes BB, DeVos SL, Kfoury N, et al. Heparan sulfate proteoglycans mediate internalization and propagation of specific proteopathic seeds. Proc Natl Acad Sci U S A. 2013;110(33):E3138. doi: 10.1073/pnas.1301440110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Fantini J, Carlus D, Yahi N. The fusogenic tilted peptide (67–78) of α-synuclein is a cholesterol binding domain. Biochim Biophys Acta. 2011;1808(10):2343–2351. doi: 10.1016/j.bbamem.2011.06.017 [DOI] [PubMed] [Google Scholar]
- 84.Bar-On P, Crews L, Koob AO, et al. Statins reduce neuronal α-synuclein aggregation in vitro models of Parkinson’s disease. J Neurochem. 2008;105(5):1656–1667. doi: 10.1111/j.1471-4159.2008.05254.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Emamzadeh FN, Allsop D. α-Synuclein interacts with lipoproteins in plasma. J Mol Neurosci. 2017b;63(2):165–172. doi: 10.1007/s12031-017-0967-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Emamzadeh FN. Role of apolipoproteins and α-synuclein in Parkinson’s disease. J Mol Neurosci. 2017a;62(3–4):344–355. doi: 10.1007/s12031-017-0942-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gao N, Li YH, Li X, et al. Effect of α-synuclein on the promoter activity of the tyrosine hydroxylase gene. Neurosci Bull. 2007;23(1):53–57. doi: 10.1007/s12264-007-0008-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kastner A, Hirsch EC, Herrero MT, Javoy-Agid F, Agid Y. Immunocytochemical quantification of tyrosine hydroxylase at a cellular level in the mesencephalon of control subjects and patients with Parkinson’s and Alzheimer’s disease. J Neurochem. 1993;61(3):1024–1034. [DOI] [PubMed] [Google Scholar]
- 89.Peterson L, Ismond KP, Chapman E, Flood P. Potential benefits of the therapeutic use of β2-adrenergic receptor agonists in neuroprotection and Parkinson’s disease. J Immunol Res. 2014;2014:103780. doi: 10.1155/2014/394127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mittal S, Bjørnevik K, Im DS, et al. β2-Adrenoreceptor is a regulator of the α-synuclein gene driving the risk of Parkinson’s disease. Science. 2017;357(6354):891–898. doi: 10.1126/science.aaf3934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hsiao JT, Halliday GM, Kim WS. α-synuclein regulates neuronal cholesterol efflux. Molecules. 2017;19(22):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hirsch-Reinshagen V, Zhou S, Burgess BL, et al. Deficiency of ABCA1 impairs apolipoprotein E metabolism in the brain. J Biol Chem. 2004;279(39):41197–41207. doi: 10.1074/jbc.M407962200 [DOI] [PubMed] [Google Scholar]
- 93.Kamisuki S, Mao Q, Abu-Elheiga L, et al. A small molecule that blocks fat synthesis by inhibiting the activation of SREBP. Chem Biol. 2009;16(8):882–892. doi: 10.1016/j.chembiol.2009.07.007 [DOI] [PubMed] [Google Scholar]
- 94.Cheng D, Kim WS, Garner B. Regulation of α-synuclein expression by liver X receptor ligands in vitro. Neuroreport. 2008;19(17):1685–1689. doi: 10.1097/WNR.0b013e32831578b2 [DOI] [PubMed] [Google Scholar]
- 95.Wheatley VR, Brind JL. Sebaceous gland differentiation: III. The uses and limitations of freshly isolated mouse preputial gland cells for the in vitro study of hormone and drug action. J Invest Dermatol. 1981;76(4):293–296. [DOI] [PubMed] [Google Scholar]
- 96.Beal MF. Mitochondria, oxidative damage, and inflammation in Parkinson’s disease. Ann N YAcad Sci. 2003;991(1):120–131. doi: 10.1111/j.1749-6632.2003.tb07470.x [DOI] [PubMed] [Google Scholar]
- 97.Bosco DA, Fowler DM, Zhang Q, et al. Elevated levels of oxidized cholesterol metabolites in Lewy body disease brains accelerate α-synuclein fibrilization. Nat Chem Biol. 2006;2(5):249–253. doi: 10.1038/nchembio782 [DOI] [PubMed] [Google Scholar]
- 98.Gallardo G, Schlüter OM, Südhof TC. A molecular pathway of neurodegeneration linking α-synuclein to ApoE and Aβ peptides. Nature Neurosci. 2008;11(3):301. doi: 10.1038/nn2058 [DOI] [PubMed] [Google Scholar]
- 99.Ruipérez V, Darios F, Davletov B. α-synuclein, lipids and Parkinson’s disease. Prog Lipid Res. 2010;49(4):420–428. doi: 10.1016/j.plipres.2010.05.004 [DOI] [PubMed] [Google Scholar]
- 100.Mahley RW, Weisgraber KH, Huang Y. Apolipoprotein E4: a causative factor and therapeutic target in neuropathology, including Alzheimer’s disease. Proc Natl Acad Sci. 2006;103(15):5644–5651. doi: 10.1073/pnas.0600549103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Chang S, Ran Ma T, Miranda RD, et al. Lipid- and receptor-binding regions of apolipoprotein E4 fragments act in concert to cause mitochondrial dysfunction and neurotoxicity. Proc Natl Acad Sci. 2005;102(51):18694–18699. doi: 10.1073/pnas.0508254102 [DOI] [PMC free article] [PubMed] [Google Scholar]