Abstract
Hair loss in early childhood represents a broad differential diagnosis which can be a diagnostic and therapeutic challenge for a physician. It is important to consider the diagnosis of a genetic hair disorder. Genetic hair disorders are a large group of inherited disorders, many of which are rare. Genetic hair abnormalities in children can be an isolated phenomenon or part of genetic syndromes. Hair changes may be a significant finding or even the initial presentation of a syndrome giving a clue to the diagnosis, such as Netherton syndrome and trichothiodystrophy. Detailed history including family history and physical examination of hair and other ectodermal structures such as nails, sweat glands, and sebaceous glands with the use of dermoscopic devices and biopsy all provide important clues to establish the correct diagnosis. Understanding the pathophysiology of genetic hair defects will allow for better comprehension of their treatment and prognosis. For example, in patients with an isolated hair defect, the main problem is aesthetic. In contrast, when the hair defect is associated with a syndrome, the prognosis will depend mainly on the associated condition. Treatment of many genetic hair disorders is focused on treating the primary cause and minimizing trauma to the hair.
Keywords: Alopecia, Children, Ectodermal dysplasias, Genetic hair disorders, Hair loss, Hair shaft disorders, Hypotrichosis
Introduction
Hair is a skin appendage that shares a common developmental pathway with other ectodermal tissue [1]. Human hair is a key phenotypic indicator of possible underlying metabolic or genetic syndromes.
Genetic hair disorders can cause severe alopecia in both adults and children and may occasionally present as part of a multisystem syndrome. So, the diagnosis of these genetic disorders is important not only for the initiation of proper therapy but also for the detection of other associated ectodermal anomalies and for appropriate genetic counselling. Affected children and their parents are usually psychologically impacted by such conditions.
In this review we summarize the main genetic hair disorders and discuss the clinical features, known associated genetic abnormalities, and current treatment modalities. The review will focus on hypotrichosis, hair shaft disorders (with and without increased fragility), and ectodermal dysplasia. Table 1 summarize the gene defect, clinical presentation, and treatment tried for each genetic hair disorder.
Table 1.
Summary table of gene defect, clinical presentation, and treatment of genetic hair disorders
| Tag | Genetic defect | Hair finding | Other clinical findings | Light or electron microscopy, or Trichoscopic finding | Treatment |
|---|---|---|---|---|---|
| Hypotrichosis | |||||
| Hereditary hypotrichosis simplex of the scalp |
AD Nonsense mutations in the CDSN gene |
Exclusively scalp hair loss Eyebrows, eyelashes, and other body hair are completely norma | Other ectodermal structures are normal and with no systemic abnormalities | Wiry, twisted scalp hair, resembling PT |
Unsatisfactory Topical minoxidil can improve the hair density and texture Wearing wig is the best option |
| Marie Unna hypotrichosis |
AD. Mutation of the U2HR gene, located in chromosome 8p21 |
Normal to adequate hairs at birth then develop pattern alopecia at puberty. Eyelashes, eyebrows, body hair and secondary sexual hair are sparse |
Nails, teeth, and sweat glands are normal. Milia-like facial lesions can occur | ||
| Autosomal recessive woolly hair/ hypotrichosis simplex | Mutation inMor lipase membrane H gene | Since infancy sparse, coarse, dry, and tightly curled hair, usually blond or lighter than other family members. | |||
| Hypotrichosis with juvenile macular dystrophy |
AR Gene defective in to 16q22.1. This region contains CDH3, encoding P-cadherin |
Early hair loss, heralding progressive degeneration of the retinal macula | Progressive degeneration of the retinal macula leading to early blindness during the second to third decade of life | Light and scanning electron microscopy of the hair shaft revealed PT | |
| Hair Shaft Disorders with Increases Fragility | |||||
| Arginosuccinic aciduria | Deficiency of arginosuccinic lyase | Normal hair at birth but then develop TN | Failure to thrive and mental retardation. | TN |
Managing the underlying disorder Zinc sulfate 45mg/day and 50 mg/day was tried – |
| Citrullinemia | Deficiency of arginosuccinate synthetase | Abnormally fragile hair with TN | TN | ||
| Netherton syndrome | AR mutations in the SPINK5 gene | short sparse fragile hair with TI | CIE or ILC, atopic athesis (elevated di IgE) | TI | Treatment is aimed to deal with the skin findings of Netherton syndrome more than the hair abnormality, and may include low dose oral steroids, etretinate,psoralen ultraviolet A therapy, topical tacrolimus, and lactate lotion 12% |
| Monilethrix |
AD (KRT81 , KRT83, and KRT86 gene coding for the type II hair keratins Hb1, Hb3, and Hb6) AR( mutation in the DSG4 gene, encoding for desmoglein 4 protein |
Normal hair at birth replaced by dull brittle hair.it commonly affect nape of the neck and accompanied with follicular keratosis. -Other body hair can be affected | keratosis pilaris, koilonychia, retarded growth and juvenile cataract | Light microscopy shows typical beaded or moniliform appearance of the hair |
systemic retinoid therapy where etretinate at 0.5 mg/kg/day and acitretin 0.5mg/kg/day were tried minoxidil 2% 1ml low dose oral minoxidil was tried gentle hair care |
| early onset pili torti | AD and AR have been reported |
Female born with abnormal or normal hair which then replaced with fragile light color hair Eybrows and eyelshes can be affected |
Can be associated with minor ectodermal abnormalities | PT | Improve with puberty |
| Late onset (Beare) Pili torti | AD | Eyebrows and off with an early age of onset, then the scalp hair after puberty become coarse, and jet black | |||
| Bjornstad syndrome |
AR mutations in the BCSIL gene |
PT | Sensorineural hearing loss | ||
| Crandall syndrome | AR | PT | Pituitary hormones dysfunction, hypogonadism, and deafness | ||
| Menkes syndrome | XLR. Mutation in the X‐linked ATP7A gene, which encodes a copper‐transporting ATPase |
Sparse, pale, lightly pigmented hair with a steel wool appearance Eyebrows are affected too |
Pale doughy skin Bowed upper lip Vascular, neurological and skeletal dysfunction |
||
| BDC syndrome | XLD | Congenital generalized hypotrichosis | Follicular atrophoderma, multiple basal cell carcinomas on the face, milia and hypohidrosis | Associated hair shaft abnormalities (PT, TN) | |
| Trichothiodystrophy |
AR Genetic defects involving the transcription factor TFIIH/XPB -XPB complex low sulfur or cysteine levels on the hair |
PIBIDS |
Light microscopy will show trichoschisis, TN Both trichoschisis and tiger tail are visible under polarizing light |
||
| Hair Shaft Disorders without Hair Fragility | |||||
| Pili annulati | AD | The hair shaft presents alternating light and dark bands | Non | Trichoscopy features include bright bands due to air filled cavities. These cavities appear dark on light microscopy | Hair growth was induced after two months of using topical minoxidil 2% solution twice daily |
| Hereditary woolly hair (HWH) |
AD A missense mutation within the helix initiation motif of the keratin K71 gene |
Variable degree of tight curling | Trichoscopic examination reveals that the hair shafts have waves at short intervals | Treatment with nonablative fractional lasers stimulated normal hair growth | |
| Carvajal syndrome |
AR Desmoplakin gene mutation |
Wooly hair at birth |
Striate PPK, left-sided ventricular cardiomyopathy. follicular keratoses on face, elbows, abdomen, and lower limbs, in finger clubbing, psoriasiform keratosis, and transient pruritic blisters |
Trichoscopic examination :the hair shafts have waves at short intervals | |
| Naxos syndrome | AR. Due to a plakoglobin gene mutation | Wooly hair at birth | Diffuse palmoplantar keratosis, arrhythmogenic right ventricular cardiomyopathy | ||
| Pili trianguli et canaliculi |
Commonly sporadic, AD, AR Mutations are located in three genes involving PADI3, TGM3 and TCHH |
Present in infancy with dry, curly, blond hair, resists to styling | Ectodermal dysplasia, retinal dysplasia/pigmentary dystrophy, juvenile cataract, tooth enamel anomalies, oligodontia, digit abnormalities, and phalangoepiphyseal dysplasia | Electron microscopy: irregularly shaped triangular shafts on cross section | Improves with ageing |
| Ectodermal Dysplasias | |||||
| Hypohidrotic ectodermal dysplasia (HED) |
Commonly XL pattern. AD and AR have been reported Mutations in the EDA1, EDAR, EDARADD, or WNT10A genes |
Scalp hair is thin, sparse, slow-growing, and lightly pigmented, though secondary sexual hair can be normal |
Inability to sweat, and abnormal or missing teeth Typical facies with prominent forehead, thick lips, and a flattened nasal bridge |
Variable shaft thickness, trichorrhexis nodosa, and pili torti |
Treatment is focused on managing symptoms. Topical minoxidil ± tretinoin (case reports) autologous hair transplantation has been used to replace eyebrows Tissue expansion surgery has been used |
| Hidrotic ectodermal dysplasia (Clouston syndrome) | AD. Missense mutations in the gap junction β6 gene (GJB6) | Short, thin sparse hair starting in infancy and progress to total alopecia at puberty | Nail thickening/shortening, palmoplantar keratoderma | Trichorrhexis nodosa, trichoptilosis, pili bifurcati |
Treatment involves management of symptoms. Topical minoxidil ± tretinoin (case reports) autologous hair transplantation has been used to replace eyebrows |
| AEC syndrome |
AD Mutation in the TP63 gene |
Newborn with scalp erosion that lead to alopecia Other body hair are sparse |
Ankyloblepharon ectodermal defects, and cleft lip/palate | Pili torti et canaliculi | Autologous hair transplantation has been used to replace eyebrows |
| Trichorhinophalangeal Syndrome | |||||
| Trichorhinophalangeal syndrome |
AD TRPS I and TRPS II |
Fine, sparse hair. May have sparse lateral eyebrows and eyelashes | Large pear-shaped nose, thick and broad eyebrows, prominent ears, short stature, short digits, cone-shaped epiphyses, dystrophic nails | Light microscopy may show thinning of the distal end of the hair shaft, TN, and trichoptilosis |
Hair transplant has been shown to be an option The use of wigs can be considered if desired |
| Atrichia with Papular Lesions | |||||
| Atrichia with papular lesions |
AR Mutation in zinc finger domain of (HL) gene |
Irreversible alopecia of the scalp, eyebrows, axillary, and pubic hair, which starts a few months after birth | Keratin cysts over the body | Light microscopy shows the infundibular part of the hair follicle with replacement of the middle and lower part by keratinizing cysts | |
AD Autosomal dominant, AR Autosomal recessive, CDSN corneodesmosin, PT Pili torti, TI Trichorrhexis invaginate, ILC Icthyosis linearis circumflexa, CIE Congenital icthysiform erythroderma, XLR X linked recessive, BDC syndrome, Bazex-Dupre-Christol syndrome, XLD X linked dominant, PIBIDS photosensitivity, ichthyosis, brittle hair, intellectual impairment, decrease fertility and short stature, PPK Palmoplanter keratoderma, PADI3 peptidylarginine deiminase 3 TGM3 transglutaminase3 ,TCHH trichohyalin, AEC syndrome: ankyloblepharon, ectodermal defects, and cleft lip/palate. TRPS Trichorhinophalangeal syndrome, HL Human hairless gene
Methods
We searched keywords using PubMed and Medline to identify all relevant publications. The terms “Hair loss,” “Alopecia,” “Hypotrichosis,” “Trichorrhexis nodosa,” “Trichorrhexis invaginate,” “Bamboo hair,” “Pili torti,” “Trichothiodystrophy,” “Monilethrix,” “Pili annulati,” “Woolly hair,” “Uncombable hair syndrome,” “Pili trianguli et canaliculi,” “Ectodermal dysplasias,” “Trichorhinophalangeal syndrome,” “pediatric,” “congenital,” “genetic,” and “children” were included as a search terms to identify all relevant publications.
Three independent researchers performed a literature search to identify all relevant studies. Only published articles written in English were chosen. A total of 159 articles within the last 50 years were selected to be included in this review.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors. Tables/figures are original and have been produced by the authors for this particular publication. The authors have consent from the patients for using their images in this publication.
Hypotrichosis
In hypotrichosis, sparse hair is the result of a hair regeneration defect, caused by impairment in hair cycling and anchoring of the hair shaft in the skin [2]. Mutations in different genes have been associated with non-syndromic as well as syndromic forms [3], including hypotrichosis simplex, hypotrichosis with juvenile macular dystrophy (HJMD), Marie Unna hypotrichosis (MUH), and autosomal recessive woolly hair/hypotrichosis simplex.
Hypotrichosis Simplex
Hypotrichosis simplex (HS) (Mendelian Inheritance in Man (MIM) 146520, MIM 278150, MIM 146550, MIM 613981, and MIM 605389) [4] is a descriptive term for the clinical manifestations related to diffuse hair thinning without any morphological abnormalities of the hair shaft. Several hereditary hypotrichosis simplex (HHS) pedigrees have been published showing autosomal dominant inheritance, while others show autosomal recessive inheritance. Clinical variability can be observed on the basis of patient’s age of onset, as well as eyebrow and eyelash involvement [5]. Mutations in six genes have been identified for isolated HS, and mutations in three of them—CDSN (MIM 602593), APCDD1 (MIM 607479), and RPL21 (MIM 603636)—are responsible for autosomal dominant forms [4].
When the hypotrichosis simplex is only limited to the scalp, it is called hereditary hypotrichosis simplex of the scalp (HHSS) (MIM 146520), which is a rare non-syndromic autosomal dominant condition characterized by exclusively scalp hair loss, sparing other ectodermal structures and with no systemic abnormalities [6]. It is caused by nonsense mutations in the corneodesmosin gene (CDSN) which leads to expression of a truncated protein probably toxic to hair growth [7].
Patients present with normal hair at birth, then a gradually progressive scalp hair loss begins in the middle of the first decade ending with almost complete hair loss by the third decade. Eyebrows, eyelashes, and other body hair beside teeth and nails are completely normal. Developmental and intellectual development are normal [8]. Hypotrichosis simplex of the scalp was first described by Toribio and Quinones [9]. Males and females are affected equally [9].
Marine Unna Hypotrichosis
Marie Unna hypotrichosis, also known as Marie Unna hereditary hypotrichosis (MUHH) (OMIM ID #146550) is a rare autosomal dominant condition characterized by scalp hair that is sparse or absent at birth [10], with variable coarse, wiry hair regrowth in childhood, and potential loss again at puberty causing non-scarring alopecia [11]. It was first described by Marie-Unna in a German family, where individuals over seven generations were affected by a previously unreported type of congenital hypotrichosis. The exact mechanism of hair loss is not yet known, and genetic factors may play a role. There are hypotheses that might contribute to the pathogenesis including decreased number of functional follicles, altered hair shaft morphology, and abnormal follicle cycling [12]. Mutation of the U2HR gene, located in chromosome 8p21 is responsible for MUH. Several mutations in the U2HR gene that have been reported in the literature [10, 13, 14].
Patients have normal to adequate hair at birth and develop pattern alopecia resembling severe androgenetic alopecia at puberty [15]. Eyelashes, eyebrows, body hair, and secondary sexual hair are sparse or absent. Loss of eyebrows and presence of wiry, twisted scalp hair, resembling pili torti, is important for diagnosis [16]. Nails, teeth, and sweat glands are normal. Milia-like facial lesions can occur [17].
The hair shaft shows irregular twisting at odd angles and diameter variability along its length on light microscopy. Peeling of the cuticle and longitudinal grooves are noticeable on scanning electron microscopy [15]. Histologically, the number of hair follicles is decreased and there is a mild to moderate inflammatory infiltrate, but no fibrosis and scarring. The distinctive pattern of hair loss and twisted hair shaft provides a clue to the diagnosis of MUH. Unfortunately, there is no effective treatment available [17].
Autosomal Recessive Wooly Hair/Hypotrichosis Simplex (ARWH/H) or Familial Woolly Hair (WFH)
Autosomal recessive woolly hair/hypotrichosis simplex (ARWH/H) (OMIM ID #604379) is rare disorder characterized by tightly curled hair with variable light color (woolly hair) since infancy and variable degree of hypotrichosis [18]. It is caused by a mutation in P2RY5 or lipase membrane H gene (LIPH) [18]. LIPH encodes PA-PLA1a, a phospholipase A1 family member that produces lysophosphatidic acid (LPA) from phosphatidic acid, and plays a crucial role in hair growth in humans. LPA is an extracellular mediator that has many biological functions [19]. A mutation in P2RY5 gene (which is expressed in both Henle’s and Huxley’s layers of the inner root sheath of the hair follicle) had been identified in six consanguineous Pakistani families [20]. Patients have sparse, coarse, dry, and tightly curled hair, usually blond or lighter than other family members [21, 22] (Fig. 1).
Fig. 1.

Autosomal recessive woolly hair/hypotrichosis. Note sparse blond curled hair
Hypotrichosis with Juvenile Macular Dystrophy
Congenital hypotrichosis associated with juvenile macular dystrophy (MIM 601553) is a rare autosomal recessive disorder characterized by early hair loss, heralding progressive degeneration of the retinal macula leading to early blindness during the second to third decade of life [23, 24]. HJMD prevalence is unknown and has only been reported in approximately 30 patients [25–30].
Sprecher et al. [23] used mapping in four consanguineous families to localize the gene defective in HJMD to 16q22.1. This region contains CDH3, encoding P-cadherin, which is expressed in the hair follicles and retinal pigment epithelium. Mutation analysis shows in all families a common homozygous deletion in exon 8 of CDH3. These findings establish for the first time the molecular etiology of HJMD and link a cadherin molecule in the pathogenesis of this hair and retinal disorder [23]. Furthermore, Indelman et al. reported another four members of a consanguineous family with HJMD. Light and scanning electron microscopy of the hair shaft revealed pili torti. Fundus examination of the eyes showed marked degeneration of the macular pigment epithelium. DNA analysis of the entire coding sequence of CDH3 revealed, in all affected individuals, a homozygous missense mutation resulting in a single amino acid substitution at position 503 of P-cadherin sequence (R503H). This is considered the first missense mutation reported in CDH3 and second mutation found to underlie HJMD [31].
Additionally, Indelman and his colleagues assessed nine patients belonging to five families to further characterize the CDH3 mutation spectrum and delineate possible phenotype–genotype correlations. Significant inter- and intrafamilial differences in hair morphology were found, as well as differences in associated skin findings, severity, and age of onset of visual disability [32]. It has been recommended that all patients with congenital hypotrichosis should undergo a thorough fundus examination [26, 27, 33, 33]. A therapeutic window for gene augmentation therapy to preserve visual acuity was suggested. More novel mutations in the CDH3 gene in HJMD have been reported afterwards [25, 28–30, 35–40].
Therapy for Hypotrichosis
The treatment of this type of alopecia is unsatisfactory. Topical minoxidil can improve the hair density and texture but for most patients wearing a wig is the best option [7].
Hair Shaft Disorders
Hair Shaft Disorders with Increased Fragility
Trichorrhexis Nodosa
Trichorrhexis nodosa (TN) refers to the light microscopic appearance of a fracture with splaying out of individual cortical cells from the main body of the hair shaft, producing an appearance suggestive of two brushes pushed together [41]. The condition can be classified into three variants: primary congenital form, trichorrhexis nodosa as part of other syndromes, and acquired trichorrhexis nodosa [42]. The acquired form of trichorrhexis nodosa is due to repeated trauma to the hair shaft, and it is beyond the scope of this review.
The primary genetic form of TN (congenital trichorrhexis nodosa) is inherited in an autosomal dominant pattern. The hair is usually normal at birth, then it is replaced with fragile hair a few months later. This condition may improve with time [41].
The forms of TN as part of syndromes include argininosuccinic aciduria, citrullinemia, and trichohepatoenteric syndrome [43]. TN can occurs in association with monilethrix, trichothiodystrophy, Netherton syndrome, and Menkes syndrome as a response to injury of otherwise damaged hair shaft [41].
Argininosuccinic aciduria and citrullinemia are a group of urea cycle disorders caused by a deficiency of enzymes required to convert toxic ammonia into urea. Clinical manifestations of these diseases are mostly due to hyperammonemia, which affects the central nervous system. Affected individuals may also develop hepatic dysfunction [44].
Argininosuccinic aciduria is an inborn error of urea synthesis. It is due to deficiency of argininosuccinic lyase. If untreated, it may present with failure to thrive and mental retardation. The hair finding of TN is an important diagnostic clue in this syndrome. These patients have normal hair at birth but then develop TN when they are 1–2 years of age [45].
Citrullinemia is also a rare genetic error of the urea cycle. There is a deficiency of argininosuccinate synthetase, resulting in increased blood ammonia, citrullinemia, and decreased arginine level [46]. Patients with this syndrome have abnormally fragile hair with TN [46].
Treatment of TN is challenging in its genetic form and it is dependent mainly on managing the underlying disorder. Zinc sulfate 45 mg/day and 50 mg/day was given to two children with TN for 2 years. They had associated alopecia and dry scaly skin. The treatment enhanced the hair growth, despite persistence of TN microscopically. One of them had normal zinc level at initiation of the therapy [47].
Trichorrhexis Invaginata
In trichorrhexis invaginata (TI), also known as Bamboo hair, the hair shaft invaginates at several point along its length (Fig. 2). Low magnification trichoscopy shows multiple small nodules spaced at irregular intervals. With high magnification trichoscopy, it is possible to see invagination of the distal part of the shaft into its proximal part, forming a ball in a cup appearance. Sometimes the proximal cupped end may be seen after the distal end has fractured (golf tee sign) [48] (Fig. 3).
Fig. 2.
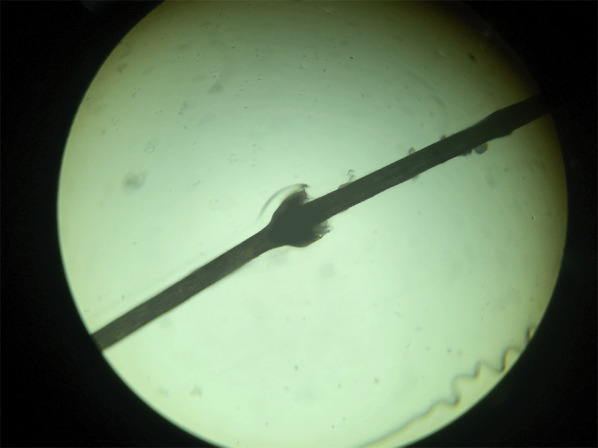
Trichorrhexis invaginate under microscopy. Invagination of the distal part of the hair shaft into its proximal part forming a ball in a cup appearance
Fig. 3.
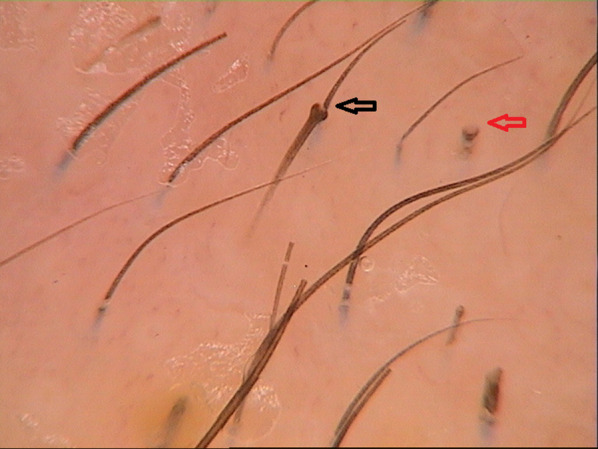
Trichoscopic finding in trichorrhexis invaginate. Note the invagination of the distal part of the shaft into its proximal part forming a ball in a cup appearance (black arrow). Proximal cupped end also seen after the distal end has fractured (golf tee sign) (red arrow)
TI is a pathognomonic finding of Netherton syndrome, a rare autosomal recessive condition caused by mutations in the SPINK5 gene. Netherton syndrome is characterized by a triad of congenital ichthyosiform erythroderma (CIE) or ichthyosis linearis circumflexa (ILC), atopic diathesis (elevated serum IgE), and short sparse fragile hair with trichorrhexis invaginata [49].
Hair improves with aging, but the eyebrows usually exhibit some hairs with the abnormality and should be checked for diagnosis [50]. Trichoscopy allows fast diagnosis of this condition as the affected hairs might be difficult to detect, as only 20–50% of hair is affected [49]. Other hair findings in patients with Netherton syndrome may resemble pili torti-like, trichorrhexis nodosa-like, and helical hairs [51].
Treatment aims to deal with the skin findings of Netherton syndrome more than the hair abnormality, and may include low dose oral steroids, etretinate [52], psoralen ultraviolet A therapy, topical tacrolimus [53], and lactate lotion 12% [54].
Monilethrix
Monilethrix (beaded hair) comes from monile (necklace, in Latin) and thrix (hair, in Greek). It is most commonly transmitted as an autosomal dominant disease [55], with high penetrance and variable severity [56].
Three genes have been associated with monilethrix (KRT81, KRT83, and KRT86, coding for the type II hair keratins Hb1, Hb3, and Hb6) [57]. An autosomal recessive form has been described, caused by a mutation in the DSG4 gene, encoding for desmoglein 4 protein [58].
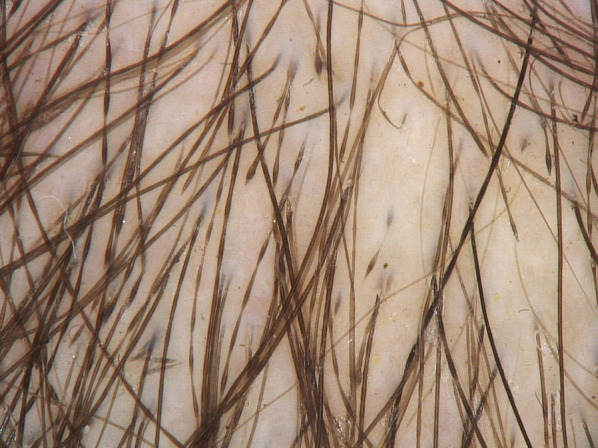
The scalp hair is usually normal at birth. Within a few weeks to months, the hair is then replaced by dull, dry, and brittle hair which break easily, leaving a stubble-like appearance. The hair on the nape of the neck and occipital area are the most commonly affected areas and is usually accompanied by follicular keratosis [59] (Fig. 4). Lanugo hair is normal in the neonatal period, and clinical signs of monilethrix appear when the terminal hair begins to form [60]. In most cases, hair growth will be a maximum of 8 cm in length, but mild cases with hair of almost normal length can occur [41]. Eyebrows, eyelashes, and body hair can be affected, too [61]. The condition can be associated with keratosis pilaris, koilonychia, retarded growth, and juvenile cataract [62].
Fig. 4.

Clinical picture of monilethrix. Alopecia is more severe in the occipital region that also presents keratotic follicular papules
Trichoscopy will show normal medullated nodes of hair, along with non-medullated internodal thin hair at regular intervals (Fig. 5). The internode represents the diseased abnormal hair where it can be easily fractured [63]. Light microscopy shows typical beaded or moniliform appearance of the hair.
Fig. 5.
Trichoscopic finding in monilethrix. Typical beaded or moniliform appearance of the hair
Monilethrix usually persists into adulthood but may improve at puberty, pregnancy, or with an oral contraceptive [64]. Variable results have been obtained from systemic retinoid therapy where etretinate at 0.5 mg/kg/day and acitretin 0.5 mg/kg/day were tried with satisfactory results, but relapse occurred after discontinuation of these medications [65, 66].
Daily topical minoxidil 2% 1 mL for 1 year showed a good response in four patients [67]. Low dose of oral minoxidil was tried on two women with good treatment response after 6 months [68]. Gentle hair care may diminish weathering and improve the condition [68].
Pili Torti
Pili torti (PT) is a hair shaft disorder characterized by a flattened hair shaft that irregularly twists over its own axis. This finding can be seen via light microscopy and trichoscopy [69] (Fig. 6). Although a few pili torti hairs are commonly seen in association with other hair shaft disorders, there are rare conditions where pili torti is the exclusive finding [41]. In classic early onset pili torti, it can be associated with other, usually minor, ectodermal abnormalities. Both autosomal dominant and recessive forms have been reported. Females are most commonly affected, where they are born with abnormal hair or normal hair that is replaced with fragile, spangled, easily broken hair at different levels. The hair color is usually lighter than the unaffected relative’s hair color. Eyebrows and eyelashes can be affected. This condition improves with puberty [70].
Fig. 6.

Trichoscopic feature of pili torti. Note the flattened hair shaft that twists over its own axis
Late onset (Beare) pili torti is an autosomal dominant condition in which the eyebrows and eyelashes are broken off with an early age of onset, then the scalp hair after puberty becomes coarse, stiff, and jet black [71].
Pili torti can be part of other syndromes:
Bjornstad syndrome: Autosomal recessive condition. The patient will have both pili torti and sensorineural hearing loss. It is caused by mutations in the BCS1L gene [72].
Crandall syndrome: Autosomal recessive condition. The patient will have pituitary hormones dysfunction, hypogonadism, pili torti, and deafness [73].
Menkes syndrome: X-linked recessive condition. It is due to a mutation in the X-linked ATP7A gene, which encodes a copper-transporting ATPase. In this syndrome there is a maldistribution of the body’s copper leading to dysfunctions of all processes that need this element. The patient will have sparse, pale, lightly pigmented hair with a steel wool appearance. Eyebrows are affected, too. The skin is pale and doughy with a bowed upper lip. There will be associated vascular, neurological, and skeletal dysfunction due to decrease in activity of copper-dependent enzymes [74].
Bazex–Dupré–Christol syndrome (BDC syndrome) is a rare X-liked dominant disorder. It is characterized by triad of (1) follicular atrophoderma, especially on the dorsum of hands and feet, (2) multiple basal cell carcinomas on the face, occurring mainly during the second decade of life, and (3) congenital generalized hypotrichosis with associated hair shaft abnormalities (pili torti, trichorrhexis nodosa) [75]. The expression of these main features may vary [76]. Common associated symptoms are milia and hypohidrosis [77].
Trichothiodystrophy
Trichothiodystrophy (TTD) is an autosomal recessive condition characterized by low sulfur or cysteine levels on the hair. Varying degrees of clinical presentations from isolated hair shaft abnormality to a more severe developmental delay, intellectual disability, recurrent infections, and even death at early childhood [78]. The PIBIDS acronym refer to photosensitivity, ichthyosis, brittle hair, intellectual impairment, decrease fertility, and short stature [79].
About half of the cases with TTD have photosensitivity. Light microscopy will show trichoschisis (transverse fracture through the hair shaft) with or without trichorrhexisis nodosa [80]. Both trichoschisis and alternating light and dark bands (tiger tail) are visible under polarized light [81].
Trichothiodystrophy is caused by several functionally related genetic defects involving the transcription factor TFIIH/XPD-XPB complex. Current thinking is that transcription factor IIH has a dual function—transcription and DNA repair [82].
Hair Shaft Disorders Without Hair Fragility
Pili Annulati
Pili annulati (PA) is sporadic or autosomal dominant, and clinically presents as speckled-appearing or shiny spangled scalp hair. The PA locus has been mapped to chromosome 12q24.32–24.33, and recombination events define a critical region of 2.9 Mb containing 36 genes [83]. The hair shaft presents alternating light and dark bands. Trichoscopy features include bright bands caused by light scattered from clusters of air-filled cavities in the hair [84] (Fig. 7). These air-filled cavities appear dark on light microscopy [85]. Usually PA is not associated with hair fragility; however, a few cases associated with severe hair fragility have been reported [86, 87].
Fig. 7.

Trichoscopic feature of pili annulati with bright band along the hair shaft
Furthermore, two patients were described in the literature with pili annulati in whom fragility of hair developed in a causal relationship with the onset of androgenetic alopecia [88]. There are a few diseases that have been reported to be associated with PA including autoimmune thyroid disease and primary immunoglobulin A deficiency [85].
PA carries excellent prognosis and treatment is usually unnecessary [89]. Cases of PA in association with alopecia areata have been reported even though the association is possibly coincidental. In a case treatment with topical minoxidil 2% solution twice daily, hair growth was induced after 2 months and the new hair lacked the ringed appearance [90].
Woolly Hair
Woolly hair (WH) is a group of hair shaft disorders characterized by short, kinked, tightly curled hair [91] (Fig. 1). Trichoscopic examination reveals that the hair shafts have waves at short intervals [69]. WH has three different subtypes: hereditary woolly hair (HWH), familial woolly hair (FWH), and woolly hair nevus (WHN) [92]. HWH is an autosomal dominant form with a variable degree of tight curling. It presents in hairs all over the scalp. Usually the hair density is normal in HWH and hair color is variable. A missense mutation within the helix initiation motif of the keratin K71 gene causes the dominant form [91]. Moreover, the dominant form has been described with disruption of keratin 74 [93].
FWH is an autosomal recessive type which is known as autosomal recessive woolly hair/hypotrichosis simplex (ARWH/H) and presents with tightly curled, sparse, thin, short white or blond hair since birth [94, 95]. This disease was discussed in detail under the “Hypotrichosis” section. WHN is considered the isolated or localized type of WH and characterized by a well-demarcated area that is lighter than the normal hair and has a smaller diameter [92].
When WH is accompanied by palmoplantar keratoderma, it may be associated with fatal cardiomyopathy like Carvajal syndrome or Naxos syndrome [96], and hence this condition should alert the physician to a cardiac disease [97–99].
Carvajal syndrome is an autosomal recessive disorder due to a desmoplakin gene mutation. It is characterized by wooly hair at birth, striate palmoplantar keratoderma which develops after infancy, and left-sided ventricular cardiomyopathy. Other features include follicular keratoses on face, elbows, abdomen, and lower limbs, in addition to finger clubbing, psoriasiform keratosis, and transient pruritic blisters. The main cause of death is heart failure which can occur in adolescence. Early cardiac intervention can decrease mortality and improve prognosis [100].
Naxos syndrome is an autosomal recessive disorder due to a plakoglobin gene mutation. The clinical features include wooly hair at birth, diffuse palmoplantar keratosis developing during the first year of life, and arrhythmogenic right ventricular cardiomyopathy. The last of these presents by adolescence with arrhythmia and automatic implantable cardioverter defibrillator is usually indicated which may prevent sudden death [101].
WH may be an isolated finding or associated with additional clinical symptoms. WH has been reported with keratosis pilaris [69], congenital ichthyosis [99], Noonan syndrome, cardiofaciocutaneous syndrome [102], osteoma cutis [103], nail dystrophy [104], and severe neurologic disorders [105].
WH is most evident during childhood; the appearances can become less severe in adulthood since the manageability improves with age [106]. However, some individuals do not improve with age [107]. Treatment with nonablative fractional lasers stimulated normal hair growth in three adult men with autosomal recessive WH [108].
Pili Trianguli et Canaliculi, “Uncombable Hair Syndrome” or “Spun Glass Hair Syndrome”
Pili trianguli et canaliculi most often presents in infancy or early childhood, with spun-glass-appearing scalp hairs that are dry, curly, blond, and totally resist all efforts of styling [109]. Hair is not fragile and grows normally [110]. Most reported cases are sporadic, but autosomal dominant and autosomal recessive inheritance has been described [111]. Mutations are located in three genes involving PADI3 (peptidylarginine deiminase 3), TGM3 (transglutaminase 3), and TCHH (trichohyalin) [112]. Electron microscopy reveals irregularly shaped triangular shafts on cross section, which are areas of the internal root sheath that have been abnormally keratinized. Several conditions have been reported in association with uncombable hair, such as ectodermal dysplasia, retinal dysplasia/pigmentary dystrophy, juvenile cataract, tooth enamel anomalies, oligodontia, digit abnormalities, and phalangoepiphyseal dysplasia [109].
In most cases of uncombable hair syndrome, the hair texture and manageability improve with ageing [111].
Ectodermal Dysplasias
Ectodermal dysplasias include a big group of disorders characterized by isolated or associated abnormalities in the teeth, hair, nails, and sweating function [113]. These disorders may also include abnormalities in other ectoderm-derived structures such as the meibomian glands, mammary glands, branchial arch cartilages, and pigment cells, anterior pituitary, thymus, and melanocytes [114, 115].
Hair is the most frequent appendage affected by ectodermal dysplasias [115], with manifestations of alopecia and hypotrichosis. Common trichoscopic findings in ectodermal dysplasia include follicular units with a single hair, abnormalities in hair shaft pigmentation, pili torti, trichoschisis, pili canaliculi, trichorrhexis nodosa, and pseudomonilethrix [116].
Hypohidrotic Ectodermal Dysplasia (Christ–Siemens–Touraine Syndrome)
Hypohidrotic ectodermal dysplasia (HED) is an ectodermal dysplasia which principally causes sparse hair, the inability to sweat, and abnormal or missing teeth (Fig. 8). The X-linked form is the most common, occurring in approximately 1 in 17,000 live births [117]. Males are disproportionately affected by the X-linked HED; however, approximately one-third of cases are inherited in either an autosomal recessive or autosomal dominant pattern, of which males and females are affected equally [114]. Approximately 90% of cases are due to mutations in the EDA1, EDAR, EDARADD, or WNT10A genes [118]. These genes encode for proteins utilized in the tumor necrosis factor α (TNFα) signaling pathway [117]. These mutations disrupt communication between surface epithelial cells and the underlying mesenchyme during embryonic development, thereby impairing the development of skin appendages [119].
Fig. 8.

Hypohidrotic ectodermal dysplasia. Scalp hair is thin, sparse, slow-growing, and lightly pigmented. Note the flat nasal bridge
Hypohidrosis due to hypoplasia of sweat glands leads to fevers as a child and heat intolerance throughout life, especially during exercise [120]. Hypodontia is seen with an average of nine permanent teeth in patients with HED, which are frequently smaller than normal and with altered shape [121]. Patients with HED exhibit a typical facies with prominent forehead, thick lips, and a flattened nasal bridge [122].
Scalp hair is thin, sparse, slow-growing, and lightly pigmented, though secondary sexual hair can be normal [122]. In microscopic hair analysis of 22 patients with HED, investigators found an increased incidence of variable shaft thickness, trichorrhexis nodosa, and pili torti compared to normal controls [123]. Phototrichogram analysis in a control-matched group of 12 patients with HED showed significantly decreased number of terminal hairs, decreased number of follicular units, decreased number of hairs per follicular unit, decreased terminal hair width, and decreased hair growth rate [124].
No specific guidelines for diagnosing HED have been published. Individuals are typically diagnosed during infancy as a result of the characteristic features of hypotrichosis, hypohidrosis, and hypodontia and typical facies [122]. Hypohidrosis can be confirmed with the starch–iodine test.
Biopsy is not routinely performed; however, horizontally sectioned 4-mm punch biopsy specimens of the scalp or palms that lack eccrine structures are diagnostic of HED; scalp biopsy is much more sensitive than palmar biopsy [123].
Genetic testing for mutations in the EDAR, EDARADD, or WNT10A genes can be done to confirm diagnosis.
There is currently no cure for HED, so treatment is focused on managing symptoms. It is important for HED patients to control their exposure to heat in light of their hypohidrosis. During hot weather, they should have access to a cool environment and plenty of water. A dentist can help treat the patient’s dental symptoms.
There is some promising data regarding EDA-A1 replacement protein that binds to the EDA-A1 receptor (EDAR) called EDI200 developed by Edimer Pharmaceuticals. EDI200 is a targeted therapy that has been shown to be effective in preventing manifestation of the disease when administered to newborn X-linked HED dog and mouse animal models [125]. These benefits persisted through adulthood in these animals. However, a phase II clinical trial (ClinicalTrials.gov Identifier NCT01775462) showed inconclusive results in humans [122].
Management of hair symptoms is discussed below.
Hidrotic Ectodermal Dysplasia (Clouston Syndrome)
Hidrotic ectodermal dysplasia (Clouston syndrome) is a rare autosomal dominant disorder characterized by nail thickening/shortening, palmoplantar keratoderma, and short, thin sparse hair. It is caused by different missense mutations in the gap junction β6 gene (GJB6), which encodes for connexin-30 [126]. The disease is most frequently associated with those of French–Canadian descent [127], but has been seen in other ethnicities. Unlike hypohidrotic ectodermal dysplasia, patients with Clouston syndrome have the ability to sweat and have normal dentition.
Patients with Clouston exhibit pale-colored, patchy, wiry, and brittle scalp hair during infancy, with progressive hair loss typically leading to total alopecia by puberty. Eyebrows, axillary, and pubic hair are sparse or absent, and eyelashes are short and sparse [128]. Hair abnormalities under light microscopy include trichorrhexis nodosa, trichoptilosis, pili bifurcati, variable diameter, damaged cuticles, and irregular helical twists [129, 130]. Electron microscopy of the abnormal hair shows a square shape in transverse section and longitudinal grooving [131].
Clouston syndrome should be suspected in individuals with nail dystrophy, hypotrichosis, and palmoplantar hyperkeratosis starting early in life [128]. The diagnosis can be confirmed by genetic analysis. The best initial genetic test is targeted analysis for the four known GJB6 pathogenic variants, and if initial testing is inconclusive, sequence analysis can be done [126].
There is no cure for Clouston disease; its treatment involves management of symptoms. Artificial nails may be used to improve appearance of nails. Skin emollients may improve palmoplantar hyperkeratosis [128].
Management of hair symptoms is discussed below.
AEC Syndrome/Rapp–Hodgkin Syndrome
AEC syndrome is an ectodermal dysplasia characterized by ankyloblepharon (partial or complete fusion of the eyelids), ectodermal defects, and cleft lip/palate. Rapp–Hodgkin syndrome is distinguished from AEC syndrome by the absence of ankyloblepharon [132]. Once thought to be separate disorders, the two diseases are now considered to be varying presentations of the same genetic disease [132–135]. AEC syndrome is due to a mutation in the TP63 gene, coding for the p63 protein, which is involved in epidermal differentiation [136]. The disease has an autosomal dominant pattern of inheritance, though approximately 70% of mutations arise de novo [137]. Additional symptoms include dental hypoplasia, nail dysplasia, decreased sweating, and hair symptoms described below [137].
Virtually 100% of newborns with AEC syndrome have skin erosions of the scalp of varying severity, with severe erosions leading to scarring alopecia and hypotrichosis (Fig. 9) [137]. In a review of 72 cases of Rapp–Hodgkin syndrome, 82% of cases exhibited hair described as dry, wiry, and sparse; 36% showed pili torti et canaliculi, 24% had hypopigmented hair, 21% had scalp dermatitis, and 18% had a prominent forehead or high frontal hairline [138]. Scalp hair loss frequently begins at puberty and continues through the 20s and 30s, and typically affects the frontal hairline to the crown, with relative sparing of the occipital and temporal regions, but often leads to almost complete hair loss [138]. Absence or thinning of eyebrows and eyelashes is common, and body hair is usually sparse. Varying severity of Rapp–Hodgkin syndrome can manifest with different degrees of hair symptoms.
Fig. 9.

Clinical picture of AEC syndrome with scalp erosions leading to scarring alopecia and hypotrichosis
Diagnosis can be suspected owing to the characteristic clinical features described above, and can be confirmed with sequence analysis of the TP63 gene [137].
Treatment focuses on management of symptoms. Neonatal scalp skin erosions should be treatment with dilute bleach soaks in order to prevent secondary infection [137], perhaps decreasing incidence of scarring alopecia after healing. Cleft lip and palate can be corrected by surgery, and ankyloblepharon typically resolves on its own but may be corrected by an ophthalmologist if necessary [137].
Management of hair symptoms is discussed below.
Managing Hair Symptoms of Ectodermal Dysplasias
The use of topical minoxidil has been proposed and its effectiveness in certain types of epidermal dysplasia is supported by isolated case reports, used either on its own [139] or in combination with topical tretinoin [140]. Using only topical minoxidil is probably the safer option due to possibility of side effects when used in combination with tretinoin, such as eruptive pyogenic granuloma [141]. The cases supporting the effectiveness of minoxidil involved HED and Clouston syndrome [142]; it is unknown whether minoxidil’s effectiveness is generalizable to other forms of ectodermal dysplasia.
Some surgical techniques have been used with success. Patients are generally poor candidates for hair transplant because of lack of sufficient donor sites [143]. However, autologous hair transplantation has been used to replace eyebrows in a patient with ectodermal dysplasia [144]. Tissue expansion surgery has been successfully used to correct areas of alopecia in a patient with hypohidrotic ectodermal dysplasia [145].
Patients may opt for use of a wig. A great resource for education and support meant for patients with ectodermal dysplasia is The National Foundation for Ectodermal Dysplasias (http://www.NFED.org).
Trichorhinophalangeal Syndrome (TRPS)
Trichorhinophalangeal syndrome (TRPS) is a group of two autosomal dominant genetic diseases (TRPS I and TRPS II) characterized by skeletal abnormalities, distinct facial features, and ectodermal features. TRPS I is caused by a pathogenic variant of the TRPS1 gene, and TRPS II is caused by a continuous 8q23.3–q24.11 deletion including the TRPS1, RAD21, and EXT1 genes. Clinical features include a large pear-shaped nose, thick and broad eyebrows, prominent ears, short stature, short digits, cone-shaped epiphyses, dystrophic nails, and fine, sparse hair. TRPS II may be accompanied by mild to moderate intellectual disability [146].
The hair of patients with TRPS is typically fine, sparse, slow-growing, and not very pigmented [146]. The pathologic change and pattern of hair loss is similar to that seen in male pattern baldness, with recession of the frontotemporal hairline and thinning of hair diameter [147]. Approximately one-third of males go nearly or completely bald within a few years after puberty, while women typically keep most of their hair but have a high frontal hairline [148]. Patients may have sparse lateral eyebrows and eyelashes [149].
Scanning electron microscopy of the hair shaft may be normal or show changes in cuticular pattern and hair shaft structure [150]. Light microscopy may show thinning of the distal end of the hair shaft, trichorrhexis nodosa, and trichoptilosis [149, 151].
In mice, the TRPS1 gene has been shown to be involved in the Wnt signaling pathway, involved in follicle morphogenesis. In humans with TRPS, two keratin-related genes (KRT6C and KRTAP3-1) were found to be downregulated in balding areas of the scalp as compared to nonbalding areas. TRPS1 protein expression has been shown to be regulated by androgens [152], providing a possible mechanism for why hair loss seen in TRPS can mimic male pattern baldness.
Diagnosis can typically be made clinically on the basis of typical findings. Many cases, especially in TRPS II, arise de novo and thus family history is not necessary to make a diagnosis. Sequence analysis can typically confirm the diagnosis of TRPS I, and chromosomal microarray analysis can be used to diagnose TRPS II.
Despite similarities in appearance to male pattern baldness, topical minoxidil and oral finasteride have not been shown to be effective in patients with TRPS. Hair transplant has been shown to be a viable option in these patients, with favorable results seen at 3-year follow-up [147]. In patients for whom hair transplant is not an option, the use of wigs can be considered if desired [146].
Atrichia with Papular Lesions
Atrichia with papular lesions (APL) is a rare autosomal recessive disease with irreversible alopecia of the scalp, eyebrows, axillary, and pubic hair, which starts a few months after birth and is associated with development keratin cysts over the body [153].
It is due to mutation in the zinc finger domain of human hairless gene (HL) on chromosome region 8p12 [154]. The hair matrix cells in APL undergo premature apoptosis associated with loss of neural cell adhesion molecule positivity and disconnection from overlying epithelial sheath. This results in loss of messages between dermal papillae and the bulge’s stem cells leading to disruption in hair growth [155]. Lanugo hairs are present at birth, but the alopecia is complete within the first year of life as the catagen follicles are unable to re-enter the anagen phase. Progressive keratin retention into follicular structures results in cyst formation, clinically evident as papules [156].
Histology of this disorder shows the infundibular part of the hair follicle with replacement of the middle and lower part by keratinizing cysts. Differential diagnosis includes vitamin D-resistant rickets type II, which also causes total alopecia in early life. It is due to a mutation of vitamin D receptor (VDR), suggesting that VDR and HL gene, both of which are zinc finger proteins, may be involved in the same genetic pathway of hair follicle control [157].
Another clinical differential diagnosis of APL is alopecia universalis (AU), so AU should be excluded to avoid the need for systemic steroid and immunosuppressive medication [158].
Diagnostic criteria of this disorder were revised by Yip et al. (Tables 1, 2) [159].
Table 2.
Revision of diagnostic criteria for atrichia with popular lesions
|
Major criteria (4 out of 5 required for diagnosis) Permanent and complete absence of scalp hairs by the first few months of life Few to widespread smooth, whitish, or milia-like papules on the face, scalp, arms, elbows, thighs, or knees from infancy or childhood Replacement of mature hair follicle structures by follicular cysts filled with cornified material in scalp histology Mutation(s) in the human hairless gene through genetic testing Clinical and/or molecular exclusion of vitamin D-dependent rickets |
|
Minor criteria (supplementary criteria) Family history of consanguinity Absence of secondary axillary, pubic, or body hair growth and/or sparse eyebrows and eyelashes Normal growth and development, including normal bones, teeth, nails, and sweating Whitish hypopigmented streaks on the scalp Lack of response to any treatment modality |
Acknowledgements
Special thanks to the staff of the clinics at the University of Miami Hospital for their help and support.
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Dr. Antonella Tosti: Consultant P&G, DS Laboratories, Monat, PI: Incyte, Pfeizer, Aclaris, Nutrifol. Azhar Ahmed, Hind Almohanna and Jacob Griggs have nothing to disclose. Dr. Antonella Tosti is a member of the journals Editorial Board.
Compliance with Ethics Guidelines
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors. Tables/figures are original and have been produced by the authors for this particular publication. The authors have consent from the patients for using their images in this publication.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Footnotes
Enhanced Digital Features
To view enhanced digital features for this article go to 10.6084/m9.figshare.8578415.
References
- 1.Cui C-Y, Schlessinger D. EDA signaling and skin appendage development. Cell Cycle. 2006;5(21):2477–2483. doi: 10.4161/cc.5.21.3403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Basel-Vanagaite L, Pasmanik-Chor M, Lurie R, Yeheskel A, Kjaer KW. CDH3-related syndromes: report on a new mutation and overview of the genotype-phenotype correlations. Mol Syndromol. 2010;1(5):223–230. doi: 10.1159/000327156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Duverger O, Morasso MI. To grow or not to grow: hair morphogenesis and human genetic hair disorders. Semin Cell Dev Biol. 2014;25–26:22–33. doi: 10.1016/j.semcdb.2013.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pasternack SM, Refke M, Paknia E, et al. Mutations in SNRPE, which encodes a core protein of the spliceosome, cause autosomal-dominant hypotrichosis simplex. Am J Hum Genet. 2013;92(1):81–87. doi: 10.1016/j.ajhg.2012.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xu C, Zhang L, Chen N, et al. A new locus for hereditary hypotrichosis simplex maps to chromosome 13q12.12 approximately 12.3 in a Chinese family. J Cutan Pathol. 2010;37(7):758–763. doi: 10.1111/j.1600-0560.2009.01415.x. [DOI] [PubMed] [Google Scholar]
- 6.Cambiaghi S, Barbareschi M. A sporadic case of congenital hypotrichosis simplex of the scalp: difficulties in diagnosis and classification. Pediatr Dermatol. 16(4):301–4. http://www.ncbi.nlm.nih.gov/pubmed/10469417. Accessed 21 Nov 2018. [DOI] [PubMed]
- 7.Betz RC. Alopezien und Hypotrichosen im Kindesalter. Der Hautarzt. 2014;65(6):520–526. doi: 10.1007/s00105-013-2714-y. [DOI] [PubMed] [Google Scholar]
- 8.Betz RC, Lee YA, Bygum A, et al. A gene for hypotrichosis simplex of the scalp maps to chromosome 6p21.3. Am J Hum Genet. 2000;66(6):1979–1983. doi: 10.1086/302934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Toribio J, Quinones PA. Hereditary hypotrichosis simplex of the scalp. Br J Dermatol. 1974;91(6):687–696. doi: 10.1111/j.1365-2133.1974.tb12455.x. [DOI] [PubMed] [Google Scholar]
- 10.Mende B, Kreysel HW. [Hypotrichosis congenita hereditaria Marie Unna with Ehlers-Danlos syndrome and atopy]. Hautarzt. 1987;38(9):532–5. http://www.ncbi.nlm.nih.gov/pubmed/3692855. Accessed 20 Nov 2018. [PubMed]
- 11.Yan KL, He PP, Yang S, et al. Marie Unna hereditary hypotrichosis: report of a Chinese family and evidence for genetic heterogeneity. Clin Exp Dermatol. 2004;29(5):460–463. doi: 10.1111/j.1365-2230.2004.01570.x. [DOI] [PubMed] [Google Scholar]
- 12.Podjasek JO, Hand JL. Marie-Unna hereditary hypotrichosis: case report and review of the literature. Pediatr Dermatol. 2011;28(2):202–204. doi: 10.1111/j.1525-1470.2011.01387.x. [DOI] [PubMed] [Google Scholar]
- 13.Yun S-K, Cho Y-G, Song KH, et al. Identification of a novel U2HR mutation in a Korean woman with Marie Unna hereditary hypotrichosis. Int J Dermatol. 2014;53(11):1358–1361. doi: 10.1111/ijd.12545. [DOI] [PubMed] [Google Scholar]
- 14.Yoshida K, Hayashi R, Shimomura Y, Niizeki H. Novel heterozygous mutation, c.74C>G (p.Pro25Arg), in the U2HR gene underlies Marie Unna hereditary hypotrichosis in a Japanese family. J Dermatol. 2017;44(8):e184–e185. doi: 10.1111/1346-8138.13868. [DOI] [PubMed] [Google Scholar]
- 15.Roberts JL, Whiting DA, Henry D, Basler G, Woolf L. Marie Unna congenital hypotrichosis: clinical description, histopathology, scanning electron microscopy of a previously unreported large pedigree. J Investig Dermatol Symp Proc. 1999;4(3):261–7. http://www.ncbi.nlm.nih.gov/pubmed/10674378. Accessed 20 Nov 2018. [DOI] [PubMed]
- 16.Mansur AT, Elcioglu NH, Redler S, et al. Marie Unna hereditary hypotrichosis: a Turkish family with loss of eyebrows and a U2HR mutation. Am J Med Genet A. 2010;152A(10):2628–2633. doi: 10.1002/ajmg.a.33649. [DOI] [PubMed] [Google Scholar]
- 17.Srinivas SM, Hiremagalore R. Marie-Unna hereditary hypotrichosis. Int J Trichol. 2014;6(4):182–184. doi: 10.4103/0974-7753.142873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Horev L, Tosti A, Rosen I, et al. Mutations in lipase H cause autosomal recessive hypotrichosis simplex with woolly hair. J Am Acad Dermatol. 2009;61(5):813–818. doi: 10.1016/j.jaad.2009.04.020. [DOI] [PubMed] [Google Scholar]
- 19.Shinkuma S, Akiyama M, Inoue A, et al. Prevalent LIPH founder mutations lead to loss of P2Y5 activation ability of PA-PLA1alpha in autosomal recessive hypotrichosis. Hum Mutat. 2010;31(5):602–610. doi: 10.1002/humu.21235. [DOI] [PubMed] [Google Scholar]
- 20.Shimomura Y, Wajid M, Ishii Y, et al. Disruption of P2RY5, an orphan G protein-coupled receptor, underlies autosomal recessive woolly hair. Nat Genet. 2008;40(3):335–339. doi: 10.1038/ng.100. [DOI] [PubMed] [Google Scholar]
- 21.Salamon T. On a family with the recessive trait of woolly hair, hypotrichosis and other anomalies. Hautarzt. 1963;14:540–4. http://www.ncbi.nlm.nih.gov/pubmed/14113527. Accessed 20 Nov 2018. [PubMed]
- 22.Itoh E, Nakahara T, Furumura M, Furue M, Shimomura Y. Case of autosomal recessive woolly hair/hypotrichosis with atopic dermatitis. J Dermatol. 2017;44(10):1185–1186. doi: 10.1111/1346-8138.13660. [DOI] [PubMed] [Google Scholar]
- 23.Sprecher E, Bergman R, Richard G, et al. Hypotrichosis with juvenile macular dystrophy is caused by a mutation in CDH3, encoding P-cadherin. Nat Genet. 2001;29(2):134–136. doi: 10.1038/ng716. [DOI] [PubMed] [Google Scholar]
- 24.Wagner H. Makulaaffektion vergesellschaftet mit Haarabnormalitat von anugotypus, beide vielleicht angeboren bei zwei Geschwistern. Graefes Arch Klin Exp Ophthalmol. 1935;134:71. doi: 10.1007/BF01854763. [DOI] [Google Scholar]
- 25.Karti O, Abali S, Ayhan Z, et al. CDH3 gene related hypotrichosis and juvenile macular dystrophy—a case with a novel mutation. Am J Ophthalmol Case Rep. 2017;7:129–133. doi: 10.1016/j.ajoc.2017.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khan AO, Bolz HJ. Phenotypic observations in “hypotrichosis with juvenile macular dystrophy” (recessive CDH3 mutations) Ophthalmic Genet. 2016;37(3):301–306. doi: 10.3109/13816810.2015.1071411. [DOI] [PubMed] [Google Scholar]
- 27.Elfatoiki FZ, Cordoliani F, Pascal Regane P, Afforitit-Demoge A. Hypotrichosis with juvenile macular dystrophy: Portuguese case. Dermatol Online J. 2016;22(5). http://www.ncbi.nlm.nih.gov/pubmed/27617529. Accessed 20 Nov 2018. [PubMed]
- 28.Indelman M, Eason J, Hummel M, et al. Novel CDH3 mutations in hypotrichosis with juvenile macular dystrophy. Clin Exp Dermatol. 2007;32(2):191–6. http://www.ncbi.nlm.nih.gov/pubmed/17342797. Accessed 20 Nov 2018. [DOI] [PubMed]
- 29.Jelani M, Salman Chishti M, Ahmad W. A novel splice-site mutation in the CDH3 gene in hypotrichosis with juvenile macular dystrophy. Clin Exp Dermatol. 2009;34(1):68–73. doi: 10.1111/j.1365-2230.2008.02933.x. [DOI] [PubMed] [Google Scholar]
- 30.Kamran-ul-Hassan Naqvi S, Azeem Z, Ali G, Ahmad W. A novel splice-acceptor site mutation in CDH3 gene in a consanguineous family exhibiting hypotrichosis with juvenile macular dystrophy. Arch Dermatol Res. 2010;302(9):701–703. doi: 10.1007/s00403-010-1035-6. [DOI] [PubMed] [Google Scholar]
- 31.Indelman M, Bergman R, Lurie R, et al. A missense mutation in CDH3, encoding P-cadherin, causes hypotrichosis with juvenile macular dystrophy. J Investig Dermatol. 2002;119(5):1210–1213. doi: 10.1046/j.1523-1747.2002.19528.x. [DOI] [PubMed] [Google Scholar]
- 32.Indelman M, Hamel CP, Bergman R, et al. Phenotypic diversity and mutation spectrum in hypotrichosis with juvenile macular dystrophy. J Investig Dermatol. 2003;121(5):1217–1220. doi: 10.1046/j.1523-1747.2003.12550_1.x. [DOI] [PubMed] [Google Scholar]
- 33.Indelman M, Leibu R, Jammal A, Bergman R, Sprecher E. Molecular basis of hypotrichosis with juvenile macular dystrophy in two siblings. Br J Dermatol. 2005;153(3):635–638. doi: 10.1111/j.1365-2133.2005.06734.x. [DOI] [PubMed] [Google Scholar]
- 34.Mason JO, Patel SA. A case of hypotrichosis with juvenile macular dystrophy. Retin Cases Brief Rep. 2015;9(2):164–167. doi: 10.1097/ICB.0000000000000127. [DOI] [PubMed] [Google Scholar]
- 35.Shimomura Y, Wajid M, Kurban M, Christiano AM. Splice site mutations in the P-cadherin gene underlie hypotrichosis with juvenile macular dystrophy. Dermatology. 2010;220(3):208–212. doi: 10.1159/000275673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Avitan-Hersh E, Indelman M, Khamaysi Z, Leibu R, Bergman R. A novel nonsense CDH3 mutation in hypotrichosis with juvenile macular dystrophy. Int J Dermatol. 2012;51(3):325–327. doi: 10.1111/j.1365-4632.2011.04973.x. [DOI] [PubMed] [Google Scholar]
- 37.Halford S, Holt R, Németh AH, Downes SM. Homozygous deletion in CDH3 and hypotrichosis with juvenile macular dystrophy. Arch Ophthalmol. 2012;130(11):1490–1492. doi: 10.1001/archophthalmol.2012.708. [DOI] [PubMed] [Google Scholar]
- 38.Ahmad F, Ali RH, Muhammad D, et al. Novel homozygous sequence variants in the CDH3 gene encoding P-cadherin underlying hypotrichosis with juvenile macular dystrophy in consanguineous families. Eur J Dermatol. 2016;26(6):610–612. doi: 10.1684/ejd.2016.2848. [DOI] [PubMed] [Google Scholar]
- 39.Blanco-Kelly F, Rodrigues-Jacy da Silva L, Sanchez-Navarro I, et al. New CDH3 mutation in the first Spanish case of hypotrichosis with juvenile macular dystrophy, a case report. BMC Med Genet. 2017;18(1):1. doi: 10.1186/s12881-016-0364-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vicente LP, Finzi S, Susanna R, Young TL. Hypotrichosis with juvenile macular dystrophy: a case report with molecular study. Arq Bras Oftalmol. 2017;80(1):49–51. doi: 10.5935/0004-2749.20170013. [DOI] [PubMed] [Google Scholar]
- 41.Rogers M. Hair shaft abnormalities: part I. Australas J Dermatol. 1995;36(4):179–84. http://www.ncbi.nlm.nih.gov/pubmed/8593104. Accessed 13 Nov 2018 (quiz 185–6). [DOI] [PubMed]
- 42.Martin AM, Sugathan P. Localised acquired trichorrhexis nodosa of the scalp hair induced by a specific comb and combing habit—a report of three cases. Int J Trichol. 2011;3(1):34–37. doi: 10.4103/0974-7753.82138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hwang ST, Park BC. Trichorrhexis nodosa after hair transplantation: dermoscopic, pathologic and electron microscopy analyses. Dermatol Surg. 2013;39(11):1721–1724. doi: 10.1111/dsu.12325. [DOI] [PubMed] [Google Scholar]
- 44.Summar ML, Dobbelaere D, Brusilow S, Lee B. Diagnosis, symptoms, frequency and mortality of 260 patients with urea cycle disorders from a 21-year, multicentre study of acute hyperammonaemic episodes. Acta Paediatr. 2008;97(10):1420–1425. doi: 10.1111/j.1651-2227.2008.00952.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Urea Cycle Disorders Conference group. Consensus statement from a conference for the management of patients with urea cycle disorders. J Pediatr. 2001;138(1 Suppl):S1–5. http://www.ncbi.nlm.nih.gov/pubmed/11148543. Accessed 13 Nov 2018. [DOI] [PubMed]
- 46.Patel HP, Unis ME. Pili torti in association with citrullinemia. J Am Acad Dermatol. 1985;12(1 Pt 2):203–6. http://www.ncbi.nlm.nih.gov/pubmed/3973120. Accessed 8 Feb 2019. [DOI] [PubMed]
- 47.Slonim AE, Sadick N, Pugliese M, Meyers-Seifer CH. Clinical response of alopecia, trichorrhexis nodosa, and dry, scaly skin to zinc supplementation. J Pediatr. 1992;121(6):890–5. http://www.ncbi.nlm.nih.gov/pubmed/1447651. Accessed 13 Nov 2018. [DOI] [PubMed]
- 48.Rudnicka L, Rakowska A, Kurzeja M, Olszewska M. Hair shafts in trichoscopy. Dermatol Clin. 2013;31(4):695–708. doi: 10.1016/j.det.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 49.Saleem HMK, Shahid MF, Shahbaz A, Sohail A, Shahid MA, Sachmechi I. Netherton syndrome: a case report and review of literature. Cureus. 2018;10(7):e3070. doi: 10.7759/cureus.3070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Powell J, Dawber RP, Ferguson DJ, Griffiths WA. Netherton’s syndrome: increased likelihood of diagnosis by examining eyebrow hairs. Br J Dermatol. 1999;141(3):544–6. http://www.ncbi.nlm.nih.gov/pubmed/10583065. Accessed 13 Nov 2018. [DOI] [PubMed]
- 51.Ito M, Ito K, Hashimoto K. Pathogenesis in trichorrhexis invaginata (bamboo hair). J Investig Dermatol. 1984;83(1):1–6. http://www.ncbi.nlm.nih.gov/pubmed/6547464. Accessed 14 Nov 2018. [DOI] [PubMed]
- 52.Caputo R, Vanotti P, Bertani E. Netherton’s syndrome in two adult brothers. Arch Dermatol. 1984;120(2):220–2. http://www.ncbi.nlm.nih.gov/pubmed/6696474. Accessed 14 Nov 2018. [PubMed]
- 53.Suga Y, Tsuboi R, Hashimoto Y, Yoshiike T, Ogawa H. A case of ichthyosis linearis circumflexa successfully treated with topical tacrolimus. J Am Acad Dermatol. 2000;42(3):520–2. http://www.ncbi.nlm.nih.gov/pubmed/10688732. Accessed 14 Nov 2018. [DOI] [PubMed]
- 54.Wehr RF, Hickman J, Krochmal L. Effective treatment of Netherton’s syndrome with 12% lactate lotion. J Am Acad Dermatol. 1988;19(1 Pt 1):140–2. http://www.ncbi.nlm.nih.gov/pubmed/3403739. Accessed 14 Nov 2018. [DOI] [PubMed]
- 55.de Oliveira EF, de Araripe ALCA. Monilethrix: a typical case report with microscopic and dermatoscopic findings. An Bras Dermatol. 2015;90(1):126–127. doi: 10.1590/abd1806-4841.20153357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Amichai B, Metzker A. Hair loss in a 6-month-old child. Monilethrix. Arch Dermatol. 1996;132(5):574–5, 577–8. http://www.ncbi.nlm.nih.gov/pubmed/8624158. Accessed 8 Feb 2019. [DOI] [PubMed]
- 57.van Steensel M, Vreeburg M, Urbina MT, López P, Morice-Picard F, van Geel M. Novel KRT83 and KRT86 mutations associated with monilethrix. Exp Dermatol. 2015;24(3):222–224. doi: 10.1111/exd.12624. [DOI] [PubMed] [Google Scholar]
- 58.Ullah A, Raza SI, Ali RH, et al. A novel deletion mutation in the DSG4 gene underlies autosomal recessive hypotrichosis with variable phenotype in two unrelated consanguineous families. Clin Exp Dermatol. 2015;40(1):78–84. doi: 10.1111/ced.12457. [DOI] [PubMed] [Google Scholar]
- 59.Narmatha GR, Chithra S, Balasubramanian N. Monilethrix. Indian J Dermatol Venereol Leprol. 68(4):220–1. http://www.ncbi.nlm.nih.gov/pubmed/17656942. Accessed 8 Feb 2019. [PubMed]
- 60.Singh G, Siddalingappa K, Nischal KC, Naik LC, Lokanatha K. Monilethrix in three generations. Indian J Dermatol. 2008;53(2):99–100. doi: 10.4103/0019-5154.41660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ferrando J, Galve J, Torres-Puente M, Santillán S, Nogués S, Grimalt R. Monilethrix: a new family with the novel mutation in KRT81 gene. Int J Trichol. 2012;4(1):53–55. doi: 10.4103/0974-7753.96105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shah V, Tharini GK, Manoharan K. Monilethrix with Holt-Oram syndrome: case report of a rare association. Int J Trichol. 2015;7(1):33–35. doi: 10.4103/0974-7753.153455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bentley-Phillips B, Bayles MA. A previously undescribed hereditary hair anomaly (pseudo-monilethrix). Br J Dermatol. 1973;89(2):159–67. http://www.ncbi.nlm.nih.gov/pubmed/4726892. Accessed 14 Nov 2018. [DOI] [PubMed]
- 64.Mirmirani P, Huang KP, Price VH. A practical, algorithmic approach to diagnosing hair shaft disorders. Int J Dermatol. 2011;50(1):1–12. doi: 10.1111/j.1365-4632.2010.04768.x. [DOI] [PubMed] [Google Scholar]
- 65.de Berker D, Dawber RP. Monilethrix treated with oral retinoids. Clin Exp Dermatol. 1991;16(3):226–8. http://www.ncbi.nlm.nih.gov/pubmed/1934581. Accessed 20 Nov 2018. [DOI] [PubMed]
- 66.Karincaoglu Y, Coskun BK, Seyhan ME, Bayram N. Monilethrix: improvement with acitretin. Am J Clin Dermatol. 2005;6(6):407–410. doi: 10.2165/00128071-200506060-00008. [DOI] [PubMed] [Google Scholar]
- 67.Rossi A, Iorio A, Scali E, et al. Monilethrix treated with minoxidil. Int J Immunopathol Pharmacol. 2011;24(1):239–242. doi: 10.1177/039463201102400129. [DOI] [PubMed] [Google Scholar]
- 68.Sinclair R. Treatment of monilethrix with oral minoxidil. JAAD Case Rep. 2016;2(3):212–215. doi: 10.1016/j.jdcr.2016.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rudnicka L, Rakowska A, Kerzeja M, Olszewska M. Hair shafts in trichoscopy: clues for diagnosis of hair and scalp diseases. Dermatol Clin. 2013;31(4):695–708. doi: 10.1016/j.det.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 70.Choudhary S, Tarafdar P, Jawade S, Singh A. A point to note in pili torti. Int J Trichol. 2018;10(2):95. doi: 10.4103/ijt.ijt_111_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Martin-Scott I. Congenital pilar defect showing features of pili torti. Br J Dermatol. 1953;65(1):35–6. http://www.ncbi.nlm.nih.gov/pubmed/13019001. Accessed 20 Nov 2018. [DOI] [PubMed]
- 72.Marubashi Y, Yanagishita T, Muto J, et al. Morphological analyses in fragility of pili torti with Björnstad syndrome. J Dermatol. 2017;44(4):455–458. doi: 10.1111/1346-8138.13700. [DOI] [PubMed] [Google Scholar]
- 73.Crandall BF, Samec L, Sparkes RS, Wright SW. A familial syndrome of deafness, alopecia, and hypogonadism. J Pediatr. 1973;82(3):461–5. http://www.ncbi.nlm.nih.gov/pubmed/4698933. Accessed 20 Nov 2018. [DOI] [PubMed]
- 74.Cosimo QC, Daniela L, Elsa B, Carlo D-V, Giuseppe F. Kinky hair, kinky vessels, and bladder diverticula in Menkes disease. J Neuroimaging. 2011;21(2):e114–e116. doi: 10.1111/j.1552-6569.2010.00476.x. [DOI] [PubMed] [Google Scholar]
- 75.Yung A, Newton-Bishop JA. A case of Bazex–Dupré–Christol syndrome associated with multiple genital trichoepitheliomas. Br J Dermatol. 2005;153(3):682–684. doi: 10.1111/j.1365-2133.2005.06819.x. [DOI] [PubMed] [Google Scholar]
- 76.Yesenia Arévalo N, Buján MM, Cervini AB, Pierini AM. Bazex–Dupré–Christol syndrome: case series. Arch Argent Pediatr. 2015;113(5):e256–e259. doi: 10.5546/aap.2015.e256. [DOI] [PubMed] [Google Scholar]
- 77.Herges A, Stieler W, Stadler R. [Bazex-Dupré-Christol syndrome. Follicular atrophoderma, multiple basal cell carcinomas and hypotrichosis]. Hautarzt. 1993;44(6):385–91. http://www.ncbi.nlm.nih.gov/pubmed/8335462. Accessed 8 Feb 2019. [PubMed]
- 78.Singh G, Miteva M. Prognosis and management of congenital hair shaft disorders with fragility-part I. Pediatr Dermatol. 2016;33(5):473–480. doi: 10.1111/pde.12894. [DOI] [PubMed] [Google Scholar]
- 79.Lambert WC, Gagna CE, Lambert MW. Trichothiodystrophy: photosensitive, TTD-P, TTD, Tay syndrome. Adv Exp Med Biol. 2010;685:106–10. http://www.ncbi.nlm.nih.gov/pubmed/20687499. Accessed 26 Nov 2018. [DOI] [PubMed]
- 80.Hashimoto S, Egly JM. Trichothiodystrophy view from the molecular basis of DNA repair/transcription factor TFIIH. Hum Mol Genet. 2009;18(R2):R224–R230. doi: 10.1093/hmg/ddp390. [DOI] [PubMed] [Google Scholar]
- 81.Yang YW, Yarbrough K, Mitkov M, Russi D, Price HN, Swanson DL. Polarized transilluminating dermoscopy: bedside trichoscopic diagnosis of trichothiodystrophy. Pediatr Dermatol. 2018;35(1):147–149. doi: 10.1111/pde.13290. [DOI] [PubMed] [Google Scholar]
- 82.Theil AF, Mandemaker IK, van den Akker E, et al. Trichothiodystrophy causative TFIIEβ mutation affects transcription in highly differentiated tissue. Hum Mol Genet. 2017;26(23):4689–4698. doi: 10.1093/hmg/ddx351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Giehl KA, Eckstein GN, Benet-Pagès A, et al. A gene locus responsible for the familial hair shaft abnormality pili annulati maps to chromosome 12q24.32–24.33. J Investig Dermatol. 2004;123(6):1073–1077. doi: 10.1111/j.0022-202x.2004.23423.x. [DOI] [PubMed] [Google Scholar]
- 84.Akoglu G, Emre S, Metin A, et al. Pili annulati with fragility: electron microscopic findings of a case. Int J Trichol. 2012;4(2):89–92. doi: 10.4103/0974-7753.96909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Castelli E, Fiorella S, Caputo V. Pili annulati coincident with alopecia areata, autoimmune thyroid disease, and primary IgA deficiency: case report and considerations on the literature. Case Rep Dermatol. 2012;4(3):250–255. doi: 10.1159/000345469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Werner K, St-Surin-Lord S, Sperling LC. Pili annulati associated with hair fragility: cause or coincidence? Cutis. 2013;91(1):36–8. http://www.ncbi.nlm.nih.gov/pubmed/23461057. Accessed 21 Nov 2018. [PubMed]
- 87.Gonzalez AM, Borda LJ, Tosti A. Pili annulati with severe trichorrhexis nodosa: a case report and review of the literature. Skin Appendage Disord. 2019;5(2):114–116. doi: 10.1159/000491910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hofbauer GF, Tsambaos D, Spycher MA, Trüeb RM. Acquired hair fragility in pili anulati: causal relationship with androgenetic alopecia. Dermatology. 2001;203(1):60–62. doi: 10.1159/000051706. [DOI] [PubMed] [Google Scholar]
- 89.Berk DR, Bayliss SJ, Giehl KA. Pili annulati: a report of 2 American families. Cutis. 2013;91(5):254–57. http://www.ncbi.nlm.nih.gov/pubmed/23772432. Accessed 21 Nov 2018. [PubMed]
- 90.Smith SR, Kirkpatrick RC, Kerr JH, Mezebich D. Alopecia areata in a patient with pili annulati. J Am Acad Dermatol. 1995;32(5 Pt 1):816–8. http://www.ncbi.nlm.nih.gov/pubmed/7722034. Accessed 21 Nov 2018. [DOI] [PubMed]
- 91.Fujimoto A, Farooq M, Fujikawa H, et al. A missense mutation within the helix initiation motif of the keratin K71 gene underlies autosomal dominant woolly hair/hypotrichosis. J Investig Dermatol. 2012;132(10):2342–2349. doi: 10.1038/jid.2012.154. [DOI] [PubMed] [Google Scholar]
- 92.Hutchinson PE, Cairns RJ, Wells RS. Woolly hair. Clinical and general aspects. Trans St Johns Hosp Dermatol Soc. 1974;60(2):160–77. http://www.ncbi.nlm.nih.gov/pubmed/4467886. Accessed 20 Nov 2018. [PubMed]
- 93.Shimomura Y, Wajid M, Petukhova L, Kurban M, Christiano AM. Autosomal-dominant woolly hair resulting from disruption of keratin 74 (KRT74), a potential determinant of human hair texture. Am J Hum Genet. 2010;86(4):632–638. doi: 10.1016/j.ajhg.2010.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Nakamura M, Tokura Y. Congenital woolly hair without P2RY5 mutation. Dermatoendocrinol. 2009;1(1):58–9. http://www.ncbi.nlm.nih.gov/pubmed/20046591. Accessed 21 Nov 2018. [DOI] [PMC free article] [PubMed]
- 95.Hayashi R, Inoue A, Suga Y, Aoki J, Shimomura Y. Analysis of unique mutations in the LPAR6 gene identified in a Japanese family with autosomal recessive woolly hair/hypotrichosis: establishment of a useful assay system for LPA6. J Dermatol Sci. 2015;78(3):197–205. doi: 10.1016/j.jdermsci.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 96.Baykan A, Olgar Ş, Argun M, et al. Different clinical presentations of Naxos disease and Carvajal syndrome: case series from a single tertiary center and review of the literature. Anatol J Cardiol. 2015;15(5):404–408. doi: 10.5152/akd.2014.5413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ramot Y, Zlotogorski A. The twisting tale of woolly hair: a trait with many causes. J Med Genet. 2015;52(4):217–223. doi: 10.1136/jmedgenet-2014-102630. [DOI] [PubMed] [Google Scholar]
- 98.Polivka L, Bodemer C, Hadj-Rabia S. Combination of palmoplantar keratoderma and hair shaft anomalies, the warning signal of severe arrhythmogenic cardiomyopathy: a systematic review on genetic desmosomal diseases. J Med Genet. 2016;53(5):289–295. doi: 10.1136/jmedgenet-2015-103403. [DOI] [PubMed] [Google Scholar]
- 99.Tursen U, Kaya TI, Ikizoglu G, Aktekin M, Aras N. Genetic syndrome with ichthyosis: congenital ichthyosis, follicular atrophoderma, hypotrichosis, and woolly hair; second report. Br J Dermatol. 2002;147(3):604–6. http://www.ncbi.nlm.nih.gov/pubmed/12207612. Accessed 21 Nov 2018. [DOI] [PubMed]
- 100.Srinivas SM, Kumar P, Basavaraja GV. Carvajal syndrome. Int J Trichol. 2016;8(1):53–55. doi: 10.4103/0974-7753.179400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Islam AM, Rahman MT, Chowdhury AH. Cardiocutaneous syndrome (Naxos disease) in a Bangladeshi boy. Cardiovasc Diagn Ther. 2016;6(5):462–465. doi: 10.21037/cdt.2016.03.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Venugopal V, Karthikeyan S, Gnanaraj P, Narasimhan M. Woolly hair nevus: a rare entity. Int J Trichol. 2012;4(1):42–43. doi: 10.4103/0974-7753.96090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ruggieri M, Pavone V, Smilari P, Rizzo R, Sorge G. Primary osteoma cutis—multiple café-au-lait spots and woolly hair anomaly. Pediatr Radiol. 1995;25(1):34–6. http://www.ncbi.nlm.nih.gov/pubmed/7761159. Accessed 21 Nov 2018. [DOI] [PubMed]
- 104.Vasudevan B, Verma R, Pragasam V, Badad A. A rare case of woolly hair with unusual associations. Indian Dermatol Online J. 2013;4(3):222–224. doi: 10.4103/2229-5178.115524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Pavone P, Falsaperla R, Barbagallo M, Polizzi A, Praticò AD, Ruggieri M. Clinical spectrum of woolly hair: indications for cerebral involvement. Ital J Pediatr. 2017;43(1):99. doi: 10.1186/s13052-017-0417-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tanahashi K, Sugiura K, Takeichi T, et al. Prevalent founder mutation c.736T>A of LIPH in autosomal recessive woolly hair of Japanese leads to variable severity of hypotrichosis in adulthood. J Eur Acad Dermatol Venereol. 2013;27(9):1182–1184. doi: 10.1111/j.1468-3083.2012.04526.x. [DOI] [PubMed] [Google Scholar]
- 107.Gonzalez FCG, Hernandez REG, Galilea ON. Woolly hair nevus in a toddler. Int J Trichol. 2014;6(4):187–188. doi: 10.4103/0974-7753.142890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Cho S, Choi MJ, Zheng Z, Goo B, Kim D-Y, Cho SB. Clinical effects of non-ablative and ablative fractional lasers on various hair disorders: a case series of 17 patients. J Cosmet Laser Ther. 2013;15(2):74–79. doi: 10.3109/14764172.2013.764436. [DOI] [PubMed] [Google Scholar]
- 109.Hicks J, Metry DW, Barrish J, Levy M. Uncombable hair (cheveux incoiffables, pili trianguli et canaliculi) syndrome: brief review and role of scanning electron microscopy in diagnosis. Ultrastruct Pathol. 25(2):99–103. http://www.ncbi.nlm.nih.gov/pubmed/11407534. Accessed 21 Nov 2018. [PubMed]
- 110.Garty B, Metzker A, Mimouni M, Varsano I. Uncombable hair: a condition with autosomal dominant inheritance. Arch Dis Child. 1982;57(9):710–2. http://www.ncbi.nlm.nih.gov/pubmed/7125692. Accessed 21 Nov 2018. [DOI] [PMC free article] [PubMed]
- 111.Hebert AA, Charrow J, Esterly NB, Fretzin DF, Opitz JM, Reynolds JF. Uncombable hair (pili trianguli et canaliculi): evidence for dominant inheritance with complete penetrance based on scanning electron microscopy. Am J Med Genet. 1987;28(1):185–193. doi: 10.1002/ajmg.1320280126. [DOI] [PubMed] [Google Scholar]
- 112.Basmanav FBÜ, Cau L, Tafazzoli A, et al. Mutations in three genes encoding proteins involved in hair shaft formation cause uncombable hair syndrome. Am J Hum Genet. 2016;99(6):1292–1304. doi: 10.1016/j.ajhg.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Itin PH. Etiology and pathogenesis of ectodermal dysplasias. Am J Med Genet Part A. 2014;164(10):2472–2477. doi: 10.1002/ajmg.a.36550. [DOI] [PubMed] [Google Scholar]
- 114.Fete TJ, Grange DK. Ectodermal dysplasias. In: Hand JL, Corona R, editors. UpToDate. UpToDate, Waltham, MA. Accessed 22 Oct 2018.
- 115.Visinoni ÁF, Lisboa-Costa T, Pagnan NAB, Chautard-Freire-Maia EA. Ectodermal dysplasias: clinical and molecular review. Am J Med Genet Part A. 2009;149A(9):1980–2002. doi: 10.1002/ajmg.a.32864. [DOI] [PubMed] [Google Scholar]
- 116.Rakowska A, Górska R, Rudnicka L, Zadurska M. Trichoscopic hair evaluation in patients with ectodermal dysplasia. J Pediatr. 2015;167(1):193–195. doi: 10.1016/j.jpeds.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 117.Trzeciak WH, Koczorowski R. Molecular basis of hypohidrotic ectodermal dysplasia: an update. J Appl Genet. 2016;57(1):51–61. doi: 10.1007/s13353-015-0307-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Cluzeau C, Hadj-Rabia S, Jambou M, et al. Only four genes (EDA1, EDAR, EDARADD, and WNT10A) account for 90% of hypohidrotic/anhidrotic ectodermal dysplasia cases. Hum Mutat. 2011;32(1):70–72. doi: 10.1002/humu.21384. [DOI] [PubMed] [Google Scholar]
- 119.Schmidt-Ullrich R, Paus R. Molecular principles of hair follicle induction and morphogenesis. Bioessays. 2005;27(3):247–261. doi: 10.1002/bies.20184. [DOI] [PubMed] [Google Scholar]
- 120.Hammersen JE, Neukam V, NüSken K-D, Schneider H. Systematic evaluation of exertional hyperthermia in children and adolescents with hypohidrotic ectodermal dysplasia: an observational study. Pediatr Res. 2011;70(3):297–301. doi: 10.1203/PDR.0b013e318227503b. [DOI] [PubMed] [Google Scholar]
- 121.Lexner MO, Bardow A, Hertz JM, Nielsen LA, Kreiborg S. Anomalies of tooth formation in hypohidrotic ectodermal dysplasia. Int J Paediatr Dent. 2007;17(1):10–18. doi: 10.1111/j.1365-263X.2006.00801.x. [DOI] [PubMed] [Google Scholar]
- 122.Wright JT, Grange DK, Fete M. Hypohidrotic ectodermal dysplasia. 2003 Apr 28 [Updated 2017 Jun 1]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle: University of Washington; 1993–2018. [PubMed]
- 123.Rouse C, Siegfried E, Breer W, Nahass G. Hair and sweat glands in families with hypohidrotic ectodermal dysplasia. Arch Dermatol. 2004;140(7):850–855. doi: 10.1001/archderm.140.7.850. [DOI] [PubMed] [Google Scholar]
- 124.Jones KB, Goodwin AF, Landan M, et al. Characterization of X-linked hypohidrotic ectodermal dysplasia (XL-HED) hair and sweat gland phenotypes using phototrichogram analysis and live confocal imaging. Am J Med Genet A. 2013;161A(7):1585–1593. doi: 10.1002/ajmg.a.35959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Huttner K. Future developments in XLHED treatment approaches. Am J Med Genet Part A. 2014;164(10):2433–2436. doi: 10.1002/ajmg.a.36499. [DOI] [PubMed] [Google Scholar]
- 126.Lamartine J, Munhoz Essenfelder G, Kibar Z, et al. Mutations in GJB6 cause hidrotic ectodermal dysplasia. Nat Genet. 2000;26(2):142–144. doi: 10.1038/79851. [DOI] [PubMed] [Google Scholar]
- 127.Clouston HR. A hereditary ectodermal dystrophy. Can Med Assoc J. 1929;21(1):18–31. [PMC free article] [PubMed] [Google Scholar]
- 128.Der Kaloustian VM. Hidrotic ectodermal dysplasia 2. 2005 Apr 25 [Updated 2015 Jan 22]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle: University of Washington; 1993–2018.
- 129.Hirano SA, Mason AR, Salkey K, Williams JV, Pariser DM. Light microscopic hair shaft analysis in ectodermal dysplasia syndromes. Pediatr Dermatol. 2012;29(4):414–420. doi: 10.1111/j.1525-1470.2011.01606.x. [DOI] [PubMed] [Google Scholar]
- 130.Sanches S, Rebellato PRO, Fabre AB, de Campos GLM. Do you know this syndrome? Clouston syndrome. An Bras Dermatol. 2017;92(3):417–418. doi: 10.1590/abd1806-4841.20175716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Escobar V, Goldblatt LI, Bixler D, Weaver D. Clouston syndrome: an ultrastructural study. Clin Genet. 1983;24(2):140–146. doi: 10.1111/j.1399-0004.1983.tb02225.x. [DOI] [PubMed] [Google Scholar]
- 132.Kannu P, Savarirayan R, Ozoemena L, White SM, McGrath JA. Rapp-Hodgkin ectodermal dysplasia syndrome: the clinical and molecular overlap with Hay–Wells syndrome. Am J Med Genet Part A. 2006;140A(8):887–891. doi: 10.1002/ajmg.a.31187. [DOI] [PubMed] [Google Scholar]
- 133.Clements SE, Techanukul T, Holden ST, et al. Rapp–Hodgkin and Hay–Wells ectodermal dysplasia syndromes represent a variable spectrum of the same genetic disorder. Br J Dermatol. 2010;163(3):624–629. doi: 10.1111/j.1365-2133.2010.09859.x. [DOI] [PubMed] [Google Scholar]
- 134.Cambiaghi S, Tadini G, Barbareschi M, Menni S, Caputo R. Rapp–Hodgkin syndrome and AEC syndrome: are they the same entity? Br J Dermatol. 1994;130(1):97–101. doi: 10.1111/j.1365-2133.1994.tb06891.x. [DOI] [PubMed] [Google Scholar]
- 135.Bertola DR, Kim CA, Albano LMJ, Scheffer H, Meijer R, van Bokhoven H. Molecular evidence that AEC syndrome and Rapp–Hodgkin syndrome are variable expression of a single genetic disorder. Clin Genet. 2004;66(1):79–80. doi: 10.1111/j.0009-9163.2004.00278.x. [DOI] [PubMed] [Google Scholar]
- 136.Zarnegar BJ, Webster DE, Lopez-Pajares V, et al. Genomic profiling of a human organotypic model of AEC syndrome reveals ZNF750 as an essential downstream target of mutant TP63. Am J Hum Genet. 2012;91(3):435–443. doi: 10.1016/j.ajhg.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Sutton VR, van Bokhoven H. TP63-related disorders. 2010 Jun 8 [Updated 2015 Aug 6]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews®. Seattle: University of Washington; 1993–2018. [PubMed]
- 138.Park S-W, Yong SL, Martinka M, Shapiro J. Rapp-Hodgkin syndrome: a review of the aspects of hair and hair color. J Am Acad Dermatol. 2005;53(4):729–735. doi: 10.1016/j.jaad.2005.05.038. [DOI] [PubMed] [Google Scholar]
- 139.Lee H-E, Chang I-K, Im M, Seo Y-J, Lee J-H, Lee Y. Topical minoxidil treatment for congenital alopecia in hypohidrotic ectodermal dysplasia. J Am Acad Dermatol. 2013;68(4):e139–e140. doi: 10.1016/j.jaad.2012.10.019. [DOI] [PubMed] [Google Scholar]
- 140.Melkote S, Dhurat RS, Palav A, Jerajani HR. Alopecia in congenital hidrotic ectodermal dysplasia responding to treatment with a combination of topical minoxidil and tretinoin. Int J Dermatol. 2009;48(2):184–185. doi: 10.1111/j.1365-4632.2009.03907.x. [DOI] [PubMed] [Google Scholar]
- 141.Baran R. Explosive eruption of pyogenic granuloma on the scalp due to topical combination therapy of minoxidil and retinoic acid. Dermatologica. 1989;179(2):76–78. doi: 10.1159/000248316. [DOI] [PubMed] [Google Scholar]
- 142.Harrison S, Sinclair R. Hypotrichosis and nail dysplasia: a novel hidrotic ectodermal dysplasia. Australas J Dermatol. 2004;45(2):103–105. doi: 10.1111/j.1440-0960.2004.00055.x. [DOI] [PubMed] [Google Scholar]
- 143.National Foundation for Ectodermal Dysplasias. Treating hair problems in ectodermal dysplasias. 2016. https://juyhw1n8m4a3a6yng24eww91-wpengine.netdna-ssl.com/wp-content/uploads/2016/06/Treating-Hair-Problems-in-Ectodermal-Dysplasias.pdf. Accessed 22 Oct 2018.
- 144.Nilforoushzadeh MA, Adibi N, Mirbagher L. A novel treatment strategy for eyebrow transplantation in an ectodermal dysplasia patient. J Res Med Sci. 2012;17(4):407–411. [PMC free article] [PubMed] [Google Scholar]
- 145.Mitsukawa N, Omori N, Tominaga M, et al. Tissue expansion for correction of alopecia in a child with hypohidrotic ectodermal dysplasia. J Dermatol. 2016;43(11):1382–1384. doi: 10.1111/1346-8138.13415. [DOI] [PubMed] [Google Scholar]
- 146.Maas S, Shaw A, Bikker H, Hennekam RC. Trichorhinophalangeal syndrome. 2017 Apr 20. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington; 1993–2018.
- 147.Choi MS, Park MJ, Park M, et al. Treatment of hair loss in the trichorhinophalangeal syndrome. Ann Dermatol. 2018;30(3):382. doi: 10.5021/ad.2018.30.3.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Rudnicka L, Olszewska M, Waśkiel A, Rakowska A. Trichoscopy in hair shaft disorders. Dermatol Clin. 2018;36(4):421–430. doi: 10.1016/j.det.2018.05.009. [DOI] [PubMed] [Google Scholar]
- 149.Seitz CS, Lüdecke H-J, Wagner N, Bröcker E-B, Hamm H. Trichorhinophalangeal syndrome type I. Arch Dermatol. 2001;137(11):1437–1442. doi: 10.1001/archderm.137.11.1437. [DOI] [PubMed] [Google Scholar]
- 150.Oh C, Jeon J, Kim J. Trichorhinophalangeal syndrome type I—clinical, microscopic, and molecular features. Indian J Dermatol Venereol Leprol. 2014;80(1):54. doi: 10.4103/0378-6323.125515. [DOI] [PubMed] [Google Scholar]
- 151.Lalević-Vasić BM, Nikolić MM, Polić DJ. Study of hair in type I tricho-rhino-phalangeal syndrome. Ann Dermatol Venereol. 1994;121(9):618–622. [PubMed] [Google Scholar]
- 152.Chang GTG, Jhamai M, van Weerden WM, Jenster G, Brinkmann AO. The TRPS1 transcription factor: androgenic regulation in prostate cancer and high expression in breast cancer. Endocr Relat Cancer. 2004;11(4):815–822. doi: 10.1677/erc.1.00853. [DOI] [PubMed] [Google Scholar]
- 153.Bansal M, Manchanda K, Lamba S, Pandey S. Atrichia with papular lesions. Int J Trichol. 2011;3(2):112–114. doi: 10.4103/0974-7753.90827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Thomas M, Daniel S. Atrichia congenita with papular lesions. Indian J Dermatol Venereol Leprol. 2011;77(1):70–72. doi: 10.4103/0378-6323.74994. [DOI] [PubMed] [Google Scholar]
- 155.Verma R, Vasudevan B, Pragasam V, Badad A, Mitra D, Neema S. Congenital atrichia with papular lesions. Indian J Paediatr Dermatology. 2014;15(2):94–4. http://go.galegroup.com.access.library.miami.edu/ps/retrieve.do?tabID=T002&resultListType=RESULT_LIST&searchResultsType=SingleTab&searchType=AdvancedSearchForm¤tPosition=1&docId=GALE%7CA381469477&docType=Case+study&sort=RELEVANCE&contentSegment=&prodId=AONE&contentSet=GALE%7CA381469477&searchId=R1&userGroupName=miami_richter&inPS=true. Accessed 21 Nov 2018.
- 156.Rocha VB, Michalany N, Valente NYS, Pereira LB, Donati A. Atrichia with papular lesions: importance of histology at an early disease stage. Ski Appendage Disord. 2018;4(3):129–130. doi: 10.1159/000480519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Miller J, Djabali K, Chen T, et al. Atrichia caused by mutations in the vitamin D receptor gene is a phenocopy of generalized atrichia caused by mutations in the hairless gene. J Investig Dermatol. 2001;117(3):612–617. doi: 10.1046/j.0022-202x.2001.01438.x. [DOI] [PubMed] [Google Scholar]
- 158.Zlotogorski A, Panteleyev AA, Aita VM, Christiano AM. Clinical and molecular diagnostic criteria of congenital atrichia with papular lesions. J Investig Dermatol. 2001;117(6):1662–1665. doi: 10.1046/j.0022-202x.2001.01618.x. [DOI] [PubMed] [Google Scholar]
- 159.Yip L, Horev L, Sinclair R, Zlotogorski A. Atrichia with papular lesions: a report of three novel human hairless gene mutations and a revision of diagnostic criteria. Acta Derm Venereol. 2008;88(4):346–349. doi: 10.2340/00015555-0466. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.


