Abstract
OBJECTIVES:
The present study aimed to assess the level of mothers’ knowledge toward cleft lip and palate and their experience concerning presurgical orthopedic management.
MATERIALS AND METHODS:
This was a cross-sectional study where the mothers were invited to complete a self-administered validated and reliable questionnaire. The questionnaire included questions that aimed to assess mother's knowledge related to the most prevalent aspects of cleft lip and palate anomaly itself and additionally, questions associated with presurgical orthopedic treatment as an adjunct therapy. Descriptive statistics were used to define the characteristics of the study variables. Chi-square test was utilized to assess relationships between categorical variables.
RESULTS:
Totally, 145 mothers completed the survey (response rate was 73%). Forty-six (46%) of the mothers provided an incomplete or improper definition of the anomaly and 35 (24%) claimed that they know the cause of the anomaly. The majority of mothers did not identify family history as a risk factor; consanguinity was identified in 29% (n = 42). Of the total, 58 mothers (40%) agreed that dental management of CLP requires teamwork and the majority (n = 126, 87%) recognized the plastic surgeon as the most important specialist. Mothers aged 20-30 years old (n = 42, 53%), and those who are university graduates (n = 38, 48%), as well as employed mothers (n = 52, 66%) have in general a higher degree of knowledge regarding cleft lip and palate (P < 0.001). More than half of the mothers (n = 70, 57%) reported that presurgical orthopedic treatment was useful and needed for their infants.
CONCLUSIONS:
Most of the mothers reported a high level of knowledge about cleft lip and palate and they experienced the usefulness of the orthopedic appliances for their infants. However, there was uncertainty in some parts such as definition, diagnosis, causes, and risk factors for cleft lip and palate. Therefore, understanding the causes of cleft lip and palate, as well as comprehensive education concerning the essential role of the orthopedic appliances to improve cleft lip and palate are crucial for mothers to improve their infants’ quality of life.
Keywords: Cleft lip and palate, mother's experience, mother's knowledge, orthopedics management
Introduction
Cleft lip and palate (CLP) is a common congenital anomaly with an estimated incidence of 1-7 per 1000 births.[1,2] It is one of the most heterogeneous orofacial malformations and it accounts for 65% of head and neck anomalies.[3,4] The definite cause of CLP is still unclear and not completely understood yet; however, it is believed that environmental and genetic causative factors play an essential role in the complex aetiology.[5] Undoubtedly, the exposure of the mother to harmful extrinsic factors may increase the likelihood of congenital anomalies including CLP.[6] Combined feeding, speech, hearing and psychological problems are often seen in individuals with CLP, and these can be corrected to varying degrees by surgical, orthodontic, speech, and psychological interventions.[7]
Orthodontic management for infants diagnosed with CLP comprises a series of therapeutic schemes, which involves three stages of treatment being provided for the first two decades of life.[8] Despite being a debatable stage, presurgical orthopedic (PSO) treatment is considered a crucial part in interdisciplinary management of CLP[9,10,11] due to its main advantages, such as facilitating feeding and narrowing of the cleft width, which in turn have an impact on improving the outcome of lip and palate repair.[12]
Variable levels of CLP knowledge have been reported in different countries in various urban and rural areas.[13,14,15,16] In fact, previous studies elucidated the importance of parents’ education toward the successful management of CLP. This might include comprehensive information and treatment options explanations.[17,18] An obvious association between parents’ awareness/knowledge and high incidence of unrepaired cleft cases was reported, which may result, in extreme cases, in death.[13,19] Schwarz and Khadka observed that one of the most important reasons for late presentation of CLP patients is the lack of sufficient knowledge.[20] Also, late surgical procedures can lead to poor outcomes and have a potential impact on the child's and family's quality of life (QoL).[21] Therefore, adequate levels of knowledge about the anomaly, cause and treatment options can have a significant impact on the social, health, and psychological support of CLP patients.[14] Since it is well established that parents play a crucial role in the child's development, the present study aimed to assess the level of mothers’ knowledge of CLP and their experience regarding PSO management. The study further aims to assess their experience with the use of orthopedic appliances.
Materials and Methods
Study design and setting
This was a cross-sectional study at the cleft center at the College of Dentistry (Baghdad University). Figure 1 presents the study flowchart.
Figure 1.
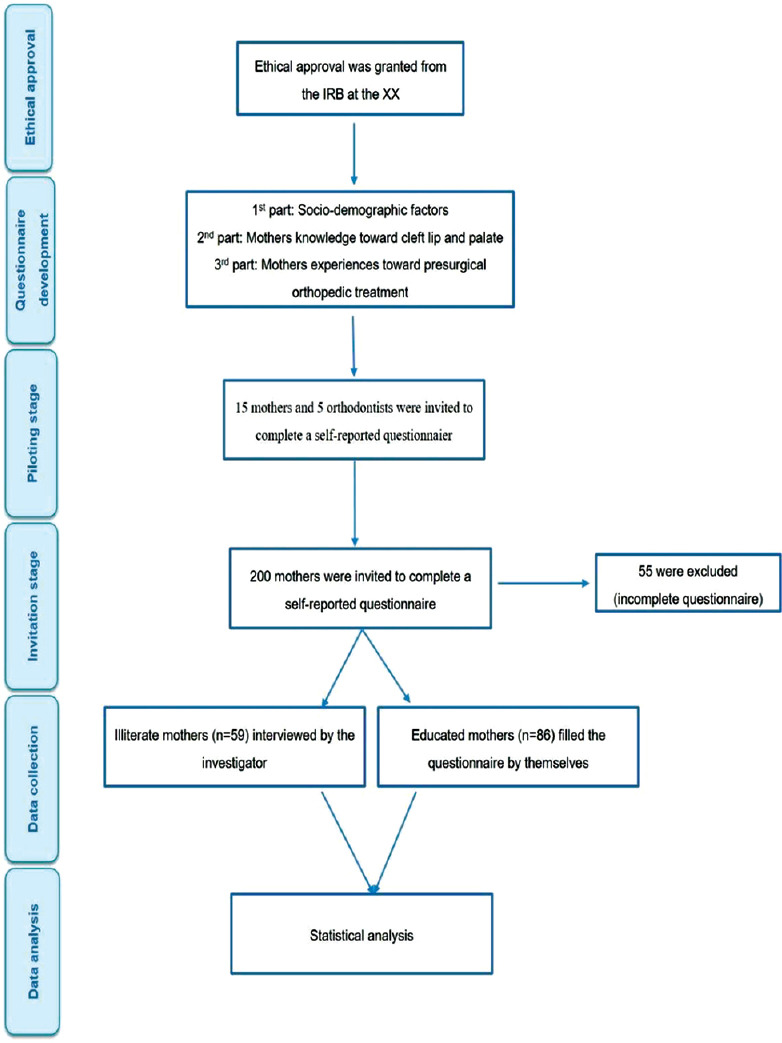
Study flowchart
Study participants and sampling technique
The participants included in the study were mothers, at any age, of infants with unilateral or bilateral CLP. Overall, 200 questionnaires were distributed, and data were collected from January 2019 to January 2020.
Study measures
Mothers were invited to complete a self-administered questionnaire; illiterate mothers were interviewed either by the investigator or another family member. The survey included three parts. The first part elicited information on the age, occupation, level of education, and the number of children. The second part included questions to assess the mother's knowledge of CLP. It was composed of 20 closed-ended questions about the general knowledge of CLP, diagnosis, aetiology, risk factors, and management. These questions were adapted and customized from a questionnaire developed by Alnujaim et al.,[15,18] who used 33 questions. However, this study included 20 closed-ended questions about general knowledge of CLP, diagnosis, aetiology, risk factors, and management, as the remaining 13 questions are not relevant to this study. The level of knowledge was estimated using a scoring system validated by a previous study.[15] For example, the level of knowledge was scored as follows: one point was given to each correct answer, while no points were given to incorrect or unknown answers. Accordingly, the participants were classified into high knowledge (when the score was above the mean) and low knowledge (when the score was below the mean). Lastly, the third part aimed to assess the mother's experience using 10 closed-ended, non-validated questions, concerning the appliances used to treat their infants. Accordingly, this part was piloted with 15 mothers and five orthodontists, and they recommended some modifications. Ethical approval was granted from the Institutional Review Board (IRB) at the College of Dentistry-Baghdad University (Reference no. 191420). The study was conducted according to the principles of the World Medical Association Declaration of Helsinki. Written, informed consent was obtained from participants and identifiable data were kept anonymously.
Study size
A Chi-square test was used to determine the sample size of the study. Assuming a moderate effect size of 0.3, a study with 80% power will require a total sample size of 143 to test the difference in average value between two groups (low knowledge versus high knowledge) using a two-tailed test at 5% level of significance. The power verification was carried out using G power version 3.1.9.2.
Statistical analysis
The data were analyzed using Statistical Package for Social Science (SPSS) version 24 (SPSS Inc., Chicago. Illinois, USA). Descriptive statistics were used to define the characteristics of the study variables in the form of raw counts and percentages. A Chi-square test was used to assess relationships between categorical variables. A conventional P value of less than 0.05 was the criterion for rejecting the null hypothesis.
Results
Out of 200 distributed questionnaires, 145 surveys were eligible for data analysis as they were fully completed; while 55 surveys were incompletely or in appropriately filled; hence they have been excluded to avoid response bias.
Characteristics of the study participants
Table 1 presents the characteristics of the study participants. The survey showed that almost half of the mothers were in the range of 20-30 years (n = 71, 49%). More than half of mothers (n = 78, 54%) were employees, while the rest were housewives (n = 67, 46%). The majority of mothers (n = 59, 41%) were illiterate, followed by university graduates (n = 45, 31%) and last, those with secondary school qualifications (n = 25, 17%). More than half of the respondents (n = 77, 53%) have had their first ever born.
Table 1.
Characteristics of the study participants
| Category | n | % | |
|---|---|---|---|
| Age | < 20 years | 24 | 16.6 |
| 20-30 years old | 71 | 48.9 | |
| 31-35 years old | 36 | 24.8 | |
| 36-44 years old | 14 | 9.7 | |
| Occupational status | Housewife | 67 | 46.2 |
| Employee | 78 | 53.8 | |
| Level of education | Illiterate | 59 | 40.7 |
| Intermediate | 14 | 9.7 | |
| Secondary | 25 | 17.2 | |
| College | 45 | 31.0 | |
| Higher degree | 2 | 1.4 | |
| Number of children | First child | 77 | 53.1 |
| Three and fewer | 25 | 17.2 | |
| More than three | 43 | 29.7 |
Mothers’ knowledge
The level of knowledge was assessed according to the mean knowledge score of the mothers, which was 12.5 (SD = ±2.5). In response to the definition of CLP, 66 (46%) of the mothers provided an incomplete or improper definition of the anomaly, while 34 (23%) defined it as opening in the CLP. In regard to the diagnosis, about half of the participants (74, 51%) responded that it cannot be diagnosed during pregnancy and 77 (53%) agreed that it is not preventable.
Nearly a quarter of mothers (n = 35, 24%) claimed that they know the cause of the anomaly, while 22 mothers (15%) believed in the role of a supernatural entity. The majority of mothers did not identify the family history as a risk factor; consanguinity was identified in 29% (n = 42). For example, some mothers reported foliate deficiency (n = 65, 45%), drug intake (n = 42, 29%), smoking (n = 16, 11%), and diabetes mellitus (n = 17, 12%) as risk factors for CLP.
The respondents reported the following complication and symptoms of CLP: feeding difficulty (n = 121, 83%), speech difficulty (n = 83, 57%), facial deformity (n = 129, 89%), dental deformity (n = 34, 23%), and occlusal deformity (n = 39, 27%). Furthermore, 58 mothers (40%) agreed that dental management of CLP requires teamwork and the majority (n = 126, 87%) recognized the plastic surgeon as the most important specialist. In regard to the prognosis of CLP treatment, almost half of the participants (48%) reported that the treatment of CLP has a good prognosis.
The association between mothers’ demographic characteristics and their knowledge
Table 2 presents the association between mothers’ characteristics and their knowledge. It was observed that mothers aged 20-30 years old (n = 42, 53%), university graduates (n = 38, 48%) and employed mothers (n = 52, 66%) showed a high degree of knowledge regarding CLP (P-value <0.001). On the other hand, first child mothers (n = 43, 65%) showed a significantly lower level of knowledge (P-value = 0.028) in comparison to mothers that had more than one child.
Table 2.
The association between mothers’ characteristics and their knowledge (n=145)
| Participant characteristics | Low knowledge (n=66) | High knowledge (n=79) | Statistical analysis | ||||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| n | % | n | % | X 2 | df | P | |
| Age | |||||||
| < 20 years | 15 | 22.8 | 9 | 11.4 | |||
| 20-30 years old | 29 | 43.9 | 42 | 53.2 | |||
| 31-35 years old | 9 | 13.6 | 27 | 34.2 | 22.2 | 3 | <0.001 |
| 36-44 years old | 13 | 19.7 | 1 | 1.2 | |||
| Occupational status | |||||||
| Housewife | 40 | 60.1 | 27 | 34.2 | 10.1 | 1 | <0.001 |
| Employee | 26 | 39.9 | 52 | 65.8 | |||
| Level of education | |||||||
| Illiterate | 42 | 63.6 | 17 | 21.5 | |||
| Intermediate | 8 | 12.2 | 6 | 7.6 | 35.3 | 4 | <0.001 |
| Secondary | 9 | 13.6 | 16 | 20.3 | |||
| College | 7 | 10.6 | 38 | 48.1 | |||
| Higher degree | 0 | 0.0 | 2 | 2.5 | |||
| Number of children | |||||||
| First child | 43 | 65.2 | 34 | 43 | |||
| Three and fewer | 9 | 13.6 | 16 | 20.3 | 7.1 | 2 | 0.028 |
| More than three | 14 | 21.2 | 29 | 36.7 | |||
Mothers’ experiences with orthopedic appliances
Upon clinical examination, 122 infants (84%) were identified to undergo treatment using orthopedic appliances. Table 3 shows the mothers’ experience toward orthopedic treatment. The results revealed that almost half of the mothers recognized the important role of orthodontists (n = 58, 48%), and 69 mothers (56.6%) thought that the CLP anomaly always requires orthopedic treatment. However, 40% of the respondents use the internet for information related to CLP treatment. Regarding treatment experience, 70 mothers (57%) found that orthopedic treatment was useful. Moreover, mothers reported that orthopedic treatment improved infants’ feeding (n = 50, 41%), facial appearance (n = 69, 57%) and speedier surgical repair appointments (n = 29, 19%). More than two-thirds of the participants (n = 52, 43%) did not report difficulty in dealing with the appliance and almost half of the respondents (49%) revealed that they would encourage other parents to undergo orthopedic treatment (n = 60, 49%).
Table 3.
Mothers’ experience toward presurgical orthopaedic management (n=122)*
| Question | Yes n % | No n % | I don’t know n % | |||
|---|---|---|---|---|---|---|
| 1. Do you think that the orthodontist is an important member of the team? | 58 | 47.5 | 35 | 28.7 | 29 | 23.8 |
| 2. Do think that CLP babies always need presurgical orthopaedic treatment? | 69 | 56.6 | 24 | 19.7 | 29 | 23.7 |
| 3. Did you search the web looking for information about presurgical orthopaedic treatment? | 49 | 40.1 | 73 | 59.9 | 0 | 0.0 |
| 4. Did you find orthopaedic treatment useful for your baby? | 70 | 57.4 | 33 | 27.0 | 19 | 15.6 |
| 5. Did it improve the baby’s feeding? | 50 | 40.9 | 54 | 44.3 | 18 | 14.8 |
| 6. Did it improve the baby’s facial appearance? | 69 | 56.6 | 37 | 30.3 | 16 | 13.1 |
| 7. Did it make the appointment for surgical repair earlier? | 23 | 18.9 | 25 | 20.5 | 74 | 60.6 |
| 8. Did you find difficulty in dealing with presurgical orthopaedic appliances? | 39 | 31.9 | 83 | 68.1 | 0 | 0.0 |
| 9. Did you find it embarrassing for you that your baby was wearing the appliance? | 52 | 42.6 | 41 | 33.6 | 29 | 23.8 |
| 10. Would you encourage other parents to do presurgical orthopaedic treatment? | 60 | 49.2 | 39 | 31.9 | 23 | 18.9 |
* 122 infants used presurgical orthopaedic appliances.
The association between mothers’ knowledge and their experience toward presurgical orthopedic treatment for CLP
The data revealed that there was a significant difference between the level of participants’ knowledge in four questions. These questions were related to the need for appliances (n = 40, 64%), internet search for professional information (n = 37, 60%), the appliance being embarrassing (n = 30, 48%) and encouraging the treatment (n = 36, 58%), P < 0.05. Table 4 shows the association between mothers’ knowledge and their experience toward PSO appliances.
Table 4.
The association between mothers’ knowledge and their experiences toward presurgical orthopaedic treatment (n=122).*
| Question | Low knowledge (n=60) | High knowledge (n=62) | Statistical analysis | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| n | % | n | % | X2 (df=2) | P | |
| 1. Do you think that the orthodontist is an important member of the team? | ||||||
| Yes | 23 | 38.3 | 35 | 56.5 | 4.3 | 0.111 |
| No | 19 | 31.7 | 16 | 25.8 | ||
| I don’t know | 18 | 30 | 11 | 17.7 | ||
| 2. Do you think that CLP babies always need presurgical orthopaedic management? | ||||||
| Yes | 29 | 48.3 | 40 | 64.5 | 0.048 | |
| No | 11 | 18.3 | 13 | 20.9 | 6.0 | |
| I don’t know | 20 | 33.4 | 9 | 14.6 | ||
| 3. Did you search the web looking for information about presurgical orthopaedic management? | ||||||
| Yes | 12 | 20.0 | 37 | 59.7 | 19.9 | 0.010 |
| No | 48 | 80.0 | 25 | 40.3 | ||
| 4. Did you find presurgical orthopaedic treatment useful for your baby? | ||||||
| Yes | 29 | 48.3 | 41 | 66.2 | ||
| No | 20 | 33.3 | 13 | 20.9 | 3.9 | 0.136 |
| I don’t know | 11 | 18.4 | 8 | 12.9 | ||
| 5. Did it improve the baby’s feeding? | ||||||
| Yes | 22 | 36.7 | 28 | 45.2 | ||
| No | 32 | 53.3 | 22 | 35.4 | 4.5 | 0.100 |
| I don’t know | 6 | 10.0 | 12 | 19.4 | ||
| 6. Did it improve the baby’s facial appearance? | ||||||
| Yes | 30 | 50.0 | 28 | 45.1 | ||
| No | 33.3 | 22 | 35.5 | 1.6 | 0.400 | |
| I don’t know | 20 | 16.7 | 12 | 19.4 | ||
| 7. Did it make the appointment for surgical repair earlier? | ||||||
| Yes | 9 | 15.0 | 14 | 22.6 | ||
| No | 17 | 28.3 | 8 | 12.9 | 4.7 | 0.090 |
| I don’t know | 34 | 56.7 | 40 | 64.5 | ||
| 8. Did you find difficulty in dealing with the presurgical orthopaedic appliances? | ||||||
| Yes | 22 | 36.7 | 17 | 27.4 | ||
| No | 38 | 63.3 | 45 | 72.6 | 1.1 | 0.270 |
| 9. Did you find it embarrassing for you that your baby was wearing the appliance? | ||||||
| Yes | 22 | 36.7 | 30 | 48.4 | ||
| No | 17 | 28.3 | 24 | 38.7 | 8.2 | 0.011 |
| I don’t know | 21 | 35 | 8 | 12.9 | ||
| 10. Would you encourage other parents to do presurgical orthopaedic treatment? | ||||||
| Yes | 24 | 40 | 36 | 58.0 | ||
| No | 19 | 31.7 | 20 | 32.3 | 7.6 | 0.021 |
| I don’t know | 17 | 28.3 | 6 | 9.7 | ||
122 infants used presurgical orthopaedic appliances.
Discussion
It is indisputable that the level of knowledge regarding different health conditions such as CLP varies between different individuals. Information provided to the parents or patients regarding the aetiology, complications, and treatment planning about CLP may have a significant impact on understanding the impact of treatment on their QoL.[21]
The results of this study showed that almost half of the mothers (46%) did not define CLP properly and gave an incomplete definition, while others defined it as an opening in the mouth or congenital anomaly. The results are similar to those reported in other investigation,[15] while a cross-sectional study by Middleton et al. found that 18.4% of mothers could not define CLP properly. On the other hand, two studies conducted on pregnant women in Nigeria and Saudi Arabia reported a high percentage of a proper definition of CLP.[15,22]
The findings of this study revealed that the majority of the mothers did not show a great deal of knowledge and awareness of most of the risk factors, such as family history, consanguinity, diabetes, and smoking. This disagrees with previous studies that reported the important role of exogenous risk factors such as mothers’ illness, medication intake, and smoking in the aetiology of CLP.[23,24,25] The difference could be attributed to the difference in the questionnaire perception, cultural background and educational and health programs in each country.
On the contrary, the majority of the respondents (75%) ruled out the involvement of supernatural entities (witchcraft) in such anomalies, in contrast to a previous African study where these beliefs are dominant.[26] Therefore, there is a need to raise mothers’ knowledge regarding CLP and how the orthopedic treatment impacts on their infants’ short- and long-term QoL.
Moreover, due to the disruption of the normal anatomical relations, individuals with CLP may experience various degrees of problems such as feeding difficulty and speech and psychological problems.[27] The mothers in this study demonstrated a good understanding of these common complications as reflected in the data gathered. The highest percentages were reported with feeding and facial deformity, while the lowest percentages were reported with dental and occlusal problems. The mothers might not recognize these two functioning problems at this stage of the patient's life, probably due to the fact that teeth erupt at later stages of life. This is in accordance with a previous study in which dental problems were identified in 6.3% of the public.[18]
Less than half of the mothers were aware that management by a multidisciplinary team is required to manage the CLP anomaly. Similarly, Alnujaim et al. found that more than half of the specialists were not identified by the participants.[15] The majority of the mothers believed that the plastic surgeon is the most important member of the management team, which agrees with other studies.[15,16,18]
Interestingly, more than half of the mothers revealed an appropriate knowledge above the mean score, which can be justified in the context that almost half of the mothers are educated. This is in contrast to a previous study on a Nigerian population;[22] however, it is consistent with a Saudi population.[15] The difference could be attributed to the difference in the questionnaire perception, geographic areas, cultural background, and educational programs in each country.
Since the introduction of the PSO treatment, it has become an integrated part of the treatment protocol dedicated to infants with unilateral or bilateral CLP.[28,29] In our study, the majority of infants required PSO appliances to align the two palatal segments and proximate the premaxilla. Delay in the surgical repair of CLP may be attributed to different reasons, such as cultural and socio-economic factors.[30] Moreover, delay in closing the gap or aligning the cleft segments may result in postponing the time for reconstructive surgery. Interestingly, most of the mothers in the present study stated that PSO for their babies started as early as within the first two weeks, and their surgeries were performed on time.
It is noteworthy to mention that about half of the respondents recognized the important role of orthodontists in the management of CLP. Almost two-thirds of the mothers did not search the web looking for information about this modality of treatment. This is probably due to the lack of cleft-related information published in the population's language and seems to be coherent with a previous study that reported that the quality of web-based information about CLP is low.[31] Another finding is that more than half of the mothers found the PSO management improved feeding and facial appearance for their infants.[8,32,33]
The generalizability of the single study center findings may not be applicable; however, to provide comparable findings, this study used validated and reliable measures assessing mothers’ knowledge regarding CLP. Although non-validated measures were utilized to assess mothers’ experience about PSO appliances, this study was pre-surveyed with a pilot assessment of 15 mothers who have infants with CLP and, in addition, five orthodontists were involved to develop clear and valid questions. There is a possibility that some answers are adversely linked to cultural background or treatment-seeking purposes, which may raise an issue regarding selection bias. Lastly, this study concluded that mothers who had experiences having CLP infants generally knew well the PSO treatment; however, a comparative study involving the mothers who had no experience having CLP infants might give different findings and this should be investigated in future research.
Conclusions and Clinical Implications
This study indicated that mothers reported a high level of knowledge about cleft lip and palate. However, there was uncertainty in some parts such as definition, diagnosis, causes and risk factors for cleft lip and palate. The majority of mothers reported the usefulness of orthopedic appliances for their infants’ feeding, facial appearance, and speedier surgical repair appointment.
The efficient management of CLP requires a multidisciplinary approach, understanding the causes of CLP, as well as comprehensive education concerning the essential role of the PSO treatment to improve CLP infants’ QoL. For example, pregnant mothers should receive preparatory information about the possibility of their infants having CLP, and also additional support to initiate treatment with the PSO appliances without delay, thus improving clinical outcome in infants’ life, and enhancing a successful prognosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We would like to acknowledge the College of Dentistry/Baghdad University for sponsoring the study. Special thanks to assistant professor Ali Abbas for doing the statistical analysis of the study.
References
- 1.Mossey P, Little J, Munger R, Dixon M, Shaw W. Cleft lip and palate. Lancet. 2009;374:1773–85. doi: 10.1016/S0140-6736(09)60695-4. [DOI] [PubMed] [Google Scholar]
- 2.Magdalenić-Meštrović M, Bagatin M. An epidemiological study of orofacial clefts in Croatia 1988-1998. J Cranio-Maxillofacial Surg. 2005;33:85–90. doi: 10.1016/j.jcms.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 3.Gorlin R, Cohen M, Hannekam R. 4th ed. New York: Oxford University Press; 2001. Syndromes of the Head and Neck. [Google Scholar]
- 4.Dixon MJ, Marazita ML, Beaty TH, Murray JC. Cleft lip and palate: Understanding genetic and environmental influences. Nat Rev Genet. 2011;12:167–78. doi: 10.1038/nrg2933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang B, Jiao X, Mao L, Xue J. Maternal cigarette smoking and the associated risk of having a child with orofacial clefts in China: A case-control study. J Cranio-Maxillofacial Surg. 2011;39:313–8. doi: 10.1016/j.jcms.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 6.Altoé SR, Borges AH, Neves AT, Aranha AM, Borba AM, Espinosa MM. Influence of parental exposure to risk factors in the occurrence of oral clefts. J Dent. 2020;21:119–26. doi: 10.30476/DENTJODS.2019.77620.0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Semb G, Enemark H, Friede H, Paulin G, Lilja J, Rautio J, et al. A Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: 1. Planning and management. J Plast Surg Hand Surg. 2017;51:2–13. doi: 10.1080/2000656X.2016.1263202. [DOI] [PubMed] [Google Scholar]
- 8.Uzel A, Alparslan ZN. Long-term effects of presurgical infant orthopedics in patients with cleft lip and palate: A systematic review. Cleft Palate-Craniofacial J. 2011;48:587–95. doi: 10.1597/10-008. [DOI] [PubMed] [Google Scholar]
- 9.Hotz M, Gnoinski W. Comprehensive care of cleft lip and palate children at Zurich University: A preliminary report. Am J Orthod. 1976;70:481–504. doi: 10.1016/0002-9416(76)90274-8. [DOI] [PubMed] [Google Scholar]
- 10.Margaret M, Gnoiinski W. Effects of early maxillary orthopaedics in coordination with delayed surgery for cleft lip and palate. J Maxillofac Surg. 1979;7:201–10. doi: 10.1016/s0301-0503(79)80041-7. [DOI] [PubMed] [Google Scholar]
- 11.Weil J. Orthopaedic growth guidanceand stimulation for patients with cleft lip and palate. Scand J Plas Reconstr Surg Hand Surg. 1987;21:57–63. doi: 10.3109/02844318709083581. [DOI] [PubMed] [Google Scholar]
- 12.Shetty V, Thakral A, Sreekumar C. Comparison of early onset Nasoalveolar molding with patients who presented for molding up to 1 year of age. J Oral Maxillofac Surg. 2016;74:811–27. doi: 10.1016/j.joms.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 13.Kwari DY, Chinda J, Olasoji H, Adeosun O. Cleft lip and palate surgery in children: Anesthetic considerations. Afr J Paediatr Surg. 2010;7:174–7. doi: 10.4103/0189-6725.70420. [DOI] [PubMed] [Google Scholar]
- 14.Chan RKK, McPherson B, Whitehill TL. Chinese attitudes toward cleft lip and palate: Effects of personal contact. Cleft Palate-Craniofacial J. 2006;43:731–9. doi: 10.1597/05-111. [DOI] [PubMed] [Google Scholar]
- 15.Alnujaim NH, Albedaie ES, Alyahya LS, Adosary MA, Alotaibi FF, Alnujaim MH, et al. Awareness, knowledge and attitudes of Saudi pregnant women towards cleft lip and palate. Curr Pediatr Res. 2017;21:595–603. [Google Scholar]
- 16.Weatherley-White RCA, Eiserman W, Beddoe M, Vanderberg R. Perceptions, expectations, and reactions to cleft lip and palate surgery in native populations: A pilot study in rural India. Cleft Palate-Craniofacial J. 2005;42:560–4. doi: 10.1597/04-003.1. [DOI] [PubMed] [Google Scholar]
- 17.Ortiz-Monasterio F. A mobile unit for the detection and care of craniofacial anomalies. Plast Reconstr Surg. 1975;55:186–9. doi: 10.1097/00006534-197502000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Middleton GF, Lass NJ, Starr P, Pannbacker M. Survey of public awareness and knowledge of cleft palate. Cleft Palate J. 1986;23:58–62. [PubMed] [Google Scholar]
- 19.Mzezewa S, Muchemwa FC. Reaction to the birth of a child with cleft lip or cleft palate in Zimbabwe. Trop Doct. 2010;40:138–40. doi: 10.1258/td.2010.090329. [DOI] [PubMed] [Google Scholar]
- 20.Schwarz R, Khadka SB. Reasons for late presentation of cleft deformity in Nepal. Cleft Palate-Craniofacial J. 2004;41:199–201. doi: 10.1597/03-016. [DOI] [PubMed] [Google Scholar]
- 21.Pelchat D, Bisson J, Ricard N, Perreault M, Bouchard JM. Longitudinal effects of an early family intervention programme on the adaptation of parents of children with a disability. Int J Nurs Stud. 1999;36:465–77. doi: 10.1016/s0020-7489(99)00047-4. [DOI] [PubMed] [Google Scholar]
- 22.Owotade FJ, Ogundipe OK, Ugboko VI, Okoje VN, Olasoji HO, Makinde ON, et al. Awareness, knowledge and attitude on cleft lip and palate among antenatal clinic attendees of tertiary hospitals in Nigeria. Niger J Clin Pract. 2014;17:6–9. doi: 10.4103/1119-3077.122822. [DOI] [PubMed] [Google Scholar]
- 23.Jones M. Etiology of facial clefts: Prospective evaluation of 428 patients. Cleft Palate J. 1988;25:16–20. [PubMed] [Google Scholar]
- 24.Al-Janabi M, Al-Zubaydi A, Al-Mulla A. Cleft lip and palate: Cross-sectional study part II. J Baghdad Coll Dent. 2004;16:92–4. [Google Scholar]
- 25.Sabbagh H, Alamoudi N, Abdulhameed F, Innes NPT, Al-Aama JY, Hummaida T, et al. Environmental risk factors in the etiology of nonsyndromic orofacial clefts in the Western Region of Saudi Arabia. Cleft Palate-Craniofacial J. 2016;53:435–43. doi: 10.1597/14-136. [DOI] [PubMed] [Google Scholar]
- 26.Dagher D, Ross E. Approaches of South African traditional healers regarding the treatment of cleft lip and palate. Cleft Palate-Craniofacial J. 2004;41:461–9. doi: 10.1597/03-153.1. [DOI] [PubMed] [Google Scholar]
- 27.Jamilian A, Sarkarat F, Jafari M, Neshandar M, Amini E, Khosravi S, et al. Family history and risk factors for cleft lip and palate patients and their associated anomalies. Stomatologija. 2017;19:78–83. [PubMed] [Google Scholar]
- 28.Grill FD, Ritschl LM, Dikel H, Rau A, Roth M, Eblenkamp M, et al. Facilitating CAD/CAM nasoalveolar molding therapy with a novel click-in system for nasal stents ensuring a quick and user-friendly chairside nasal stent exchange. Sci Rep. 2018;8:1–9. doi: 10.1038/s41598-018-29960-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Agrawal R, Patel D, Vora P. Orthopaedic traction with passive nasoalveolar moulding in a bilateral cleft lip and palate patient – Rediscovering the old. JPRAS Open. 2019;19:50–5. doi: 10.1016/j.jpra.2018.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rebekah Z, Rodby K, Perry B, Kirstie D, Pravin P, Janine R. Delay in cleft lip and palate surgical repair an institutional review on cleft health disparities in an urban population. J Craniofac Surg. 2019;30:2328–31. doi: 10.1097/SCS.0000000000005740. [DOI] [PubMed] [Google Scholar]
- 31.Karamitros GA, Kitsos NA. Clefts of the lip and palate: Is the Internet a trustworthy source of information for patients? Int J Oral Maxillofac Surg. 2018;47:1114–20. doi: 10.1016/j.ijom.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 32.Papadopoulos MA, Koumpridou EN, Vakalis ML, Papageorgiou SN. Effectiveness of pre-surgical infant orthopedic treatment for cleft lip and palate patients: A systematic review and meta-analysis. Orthod Craniofac Res. 2012;15:207–36. doi: 10.1111/j.1601-6343.2012.01552.x. [DOI] [PubMed] [Google Scholar]
- 33.Niranjane PP, Kamble RH, Diagavane SP, Shrivastav SS, Batra P, Vasudevan SD, et al. Current status of presurgical infant orthopaedic treatment for cleft lip and palate patients: A critical review. Indian J Plast Surg. 2014;47:293–302. doi: 10.4103/0970-0358.146573. [DOI] [PMC free article] [PubMed] [Google Scholar]


