Abstract
The British Society of Echocardiography has previously outlined a minimum dataset for a standard transthoracic echocardiogram, and this remains the basis on which an echocardiographic study should be performed. The importance of ultrasound in excluding critical conditions that may require urgent treatment is well known. Several point-of-care echo protocols have been developed for use by non-echocardiography specialists. However, these protocols are often only used in specific circumstances and are usually limited to 2D echocardiography. Furthermore, although the uptake in training for these protocols has been reasonable, there is little in the way of structured support available from accredited sonographers in the ongoing training and re-accreditation of those undertaking these point-of-care scans. In addition, it is well recognised that the provision of echocardiography on a 24/7 basis is extremely challenging, particularly outside of tertiary cardiac centres. Consequently, following discussions with NHS England, the British Society of Echocardiography has developed the Level 1 echocardiogram in order to support the rapid identification of critical cardiac pathology that may require emergency treatment. It is intended that these scans will be performed by non-specialists in echocardiography and crucially are not designed to replace a full standard transthoracic echocardiogram. Indeed, it is expected that a significant number of patients, in whom a Level 1 echocardiogram is required, will need to have a full echocardiogram performed as soon as is practically possible. This document outlines the minimum dataset for a Level 1 echocardiogram. The accreditation process for Level 1 echo is described separately.
Keywords: echocardiogram, point of care, emergency
Introduction
The British Society of Echocardiography (BSE) has previously outlined a minimum dataset for a standard (Level 2) transthoracic echocardiogram (1), and this remains the basis on which a complete echocardiographic study should be performed. However, the importance of ultrasound in excluding critical conditions that may require urgent treatment is well known, and over the last decade there has been a growing demand for point-of-care assessment of the heart in patients who are critically unwell (2, 3). In the United Kingdom (UK), this has coincided with a political drive to deliver high quality and timely access to care 24 hours a day, 7 days a week (4).
In 2017, NHS England outlined standards of care that should be achieved for diagnostic imaging. According to these standards, diagnostics, including echocardiography, should be available within 1 h in an emergency situation, 12 h for urgent scans and within 24 h of non-urgent in-patient requests (4). There are significant challenges for echocardiographic departments in meeting these standards. First, in the UK, the majority of echocardiograms are performed within echocardiography departments by highly trained cardiac physiologists. Many of these departments are already stretched and there is a national shortage of cardiac physiologists. Consequently, relying solely on cardiac physiologists to support echocardiography services 24 hours a day and 7 days a week is not practical. Secondly, the actual demand for emergency echocardiography, particularly overnight in most hospitals, is relatively small and an audit has suggested that it is not an efficient use of resources to keep fully trained echocardiographers on-call 24/7. Even in larger tertiary cardiac centres, out-of-hours echocardiography is usually provided by other staff groups such as cardiologists, intensivists and anaesthetists. Finally, the requests for emergency echo out of hours tend to be for specific indications rather than for a complete echocardiographic study. Consequently, the BSE felt that these standards could not be met by cardiac physiologists alone and that a different approach was required.
Several point-of-care echo programmes are already available for those working in acute specialties. Examples include Focussed Intensive Care Echo (FICE), Focussed Echocardiography in Emergency Life Support (FEEL) and Point-of-Care Ultrasound (PoCUS). There is evidence that essential echo skills can be learnt to an adequate standard with relative ease and in a short time frame (5), with further evidence backing the clinical usefulness of focussed studies within the context of standardised datasets (6, 7, 8). However, the existing point-of-care programmes are limited to specific scenarios, for example FEEL, which is used in the peri-arrest patient. In addition, these point-of-care protocols utilise only 2D echocardiography, meaning that important pathology that may require urgent treatment may be missed. Although the take up of training in point-of-care echocardiography has been reasonable, the utility of this in clinical practice has been limited, in part, by the lack of integration with echocardiographic departments, a lack of image sharing and archiving, robust quality assurance process and ongoing training and recertification. There is, therefore, a requirement for a point-of-care focussed study that can be applied in the more general emergency scenario, which can cover emergency clinical situations where echo may be useful, whether at the front door, in acute medicine or in surgery. Furthermore, there needs to be a supportive structure in place that enables archiving, image sharing, options for experienced review, prompt access to formal Level 2 and Level 3 echocardiography and includes standards for re-accreditation, audit and service review.
It is against this backdrop that the British Society of Echocardiography has developed the Level 1 echocardiographic protocol and accreditation process (9).
Purpose of the Level 1 echocardiogram
The purpose of the Level 1 study is to provide rapid assessment at the bedside, allowing global and largely qualitative assessment of structure and function to direct the acute management of the unstable patient. In particular, it is designed to rule in, or rule out, critical pathology and to direct further investigation and/or specialist referral if critical pathology is found or not adequately excluded. It is important to note that the Level 1 echo is not intended to replace a full standard (Level 2) transthoracic echocardiogram. Where indicated by senior review, identified pathology may need deeper investigation either by a Level 2 study or by another modality as appropriate. For example, identification of a regional wall motion abnormality, ventricular dysfunction or significant valvular abnormality would necessitate further evaluation and should be considered for the patient who remains unwell despite no clear abnormality was found on a Level 1 study. Furthermore, it is not designed as a ‘quick’ echo or a screening tool to relieve the burden of a fuller assessment with a Level 2 study.
A Level 1 study should be viewed as a stand-alone test in the context for which it is intended. It should be selected as a ‘best fit test’ and where a different test may be more appropriate to the patient, that test should be done instead, whether this is a Level 2 transthoracic echo, a transoesophageal echo or a CT/MRI scan.
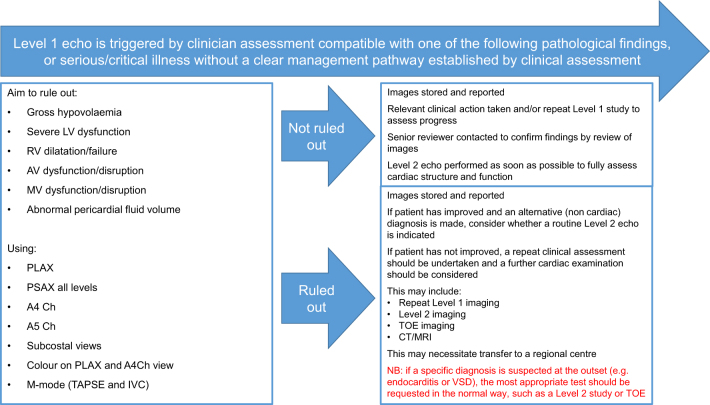
Figure 1 shows a summary overview of how a Level 1 study is intended to fit in with the overall echo service provision.
Figure 1.
Requirements for a Level 1 echocardiogram.
Requirements for a Level 1 echocardiogram
1. Benefits and general principles
It is intended that the images are acquired in a standardised manner according to a clearly defined protocol to ensure that important images are not missed. In addition, the reporting of the study should be consistent and reported according to a standard template.
The views chosen as part of the Level 1 protocol have been specified to strike a balance in ensuring that significant life-threatening pathology can be ruled in or out, but the scan can be performed by non-expert sonographers with appropriate training and support.
The intended benefits of this guideline are:
To support healthcare professionals in developing Level 1 echocardiographic services and implementing these locally.
To define the core ’minimum dataset’ for a Level 1 study.
To define the local processes, quality control and support arrangements for implementing Level 1 echo.
2. Identifying information
All images acquired should be clearly labelled with patient identifiers, including the following:
Patient name.
A second unique identifier such as hospital number or date of birth.
Identification of the operator
3. Electrocardiogram (ECG)
An ECG should be attached to the patient and used routinely to ensure acquisition of complete digital loops.
4. Archiving of images
All images obtained should be archived onto digital storage and be available for subsequent review. Ideally, the ability should be in place to upload the images for remote review by a Level 2 certified expert on a 24/7 basis.
5. Reporting
A structured report should be completed and stored either in the patient clinical record or within a dedicated reporting system depending on local requirements. Given the clinical urgency of these scans, the report must be completed immediately and the results communicated directly to the clinical team.
Systems should be in place, whereby reports can be reviewed by an experienced Level 2 certified sonographer either immediately when necessary or when practical with appropriate feedback provided to the person performing the Level 1 scan to support ongoing development.
The Level 1 minimum data set
A Level 1 study comprises 17 images and includes the standard 2D parasternal long axis, parasternal short axis, apical 4 chamber, apical 5 chamber and subcostal views.
The dataset comprises 2D images, with colour flow mapping across the aortic and mitral valves, as well as M-mode assessments of right heart function and IVC variation (Table 1). The focus, however, remains on global assessment and contextualising findings to the clinical picture.
Table 1.
The minimum data set for a Level 1 echocardiogram.
| View/modality | Explanatory note | Image |
|---|---|---|
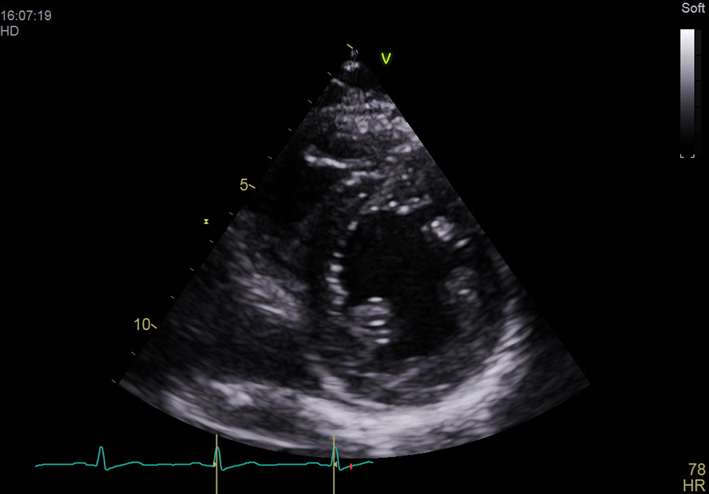
| PLAX deep (2D) | Visual assessment of pleural and pericardial effusions | 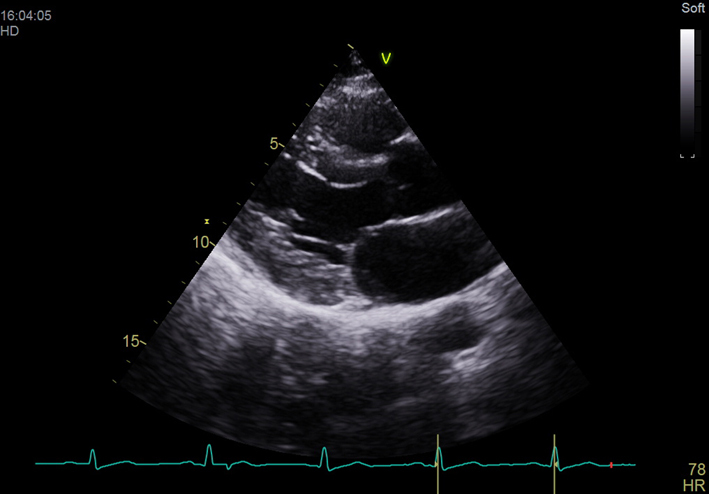 |
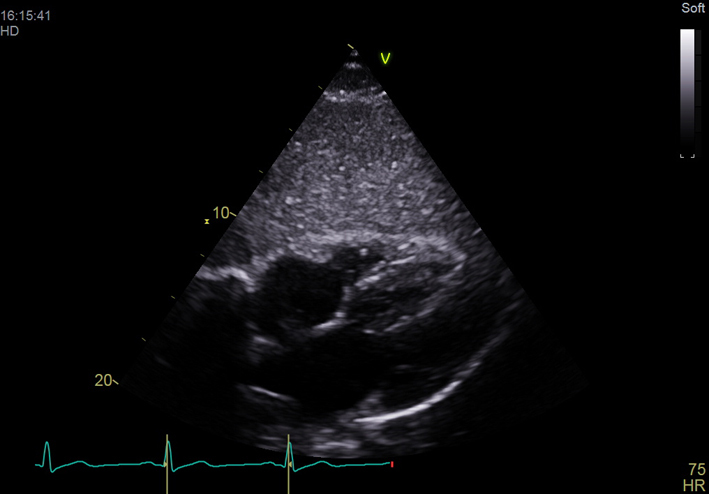
| PLAX (2D) | Optimise depth to look at cardiac structures Visual assessment of LV size and function Visual assessment of RV AV appearance and movement MV appearance and movement Major regional wall motion abnormalities |
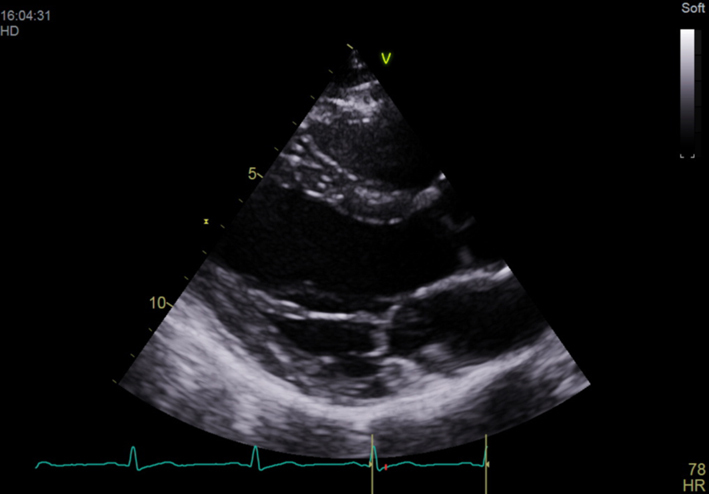 |
| PLAX (2D) LVIDd | Measurement of left ventricular internal diameter (LVID) in diastole Visual assessment of aortic root size |
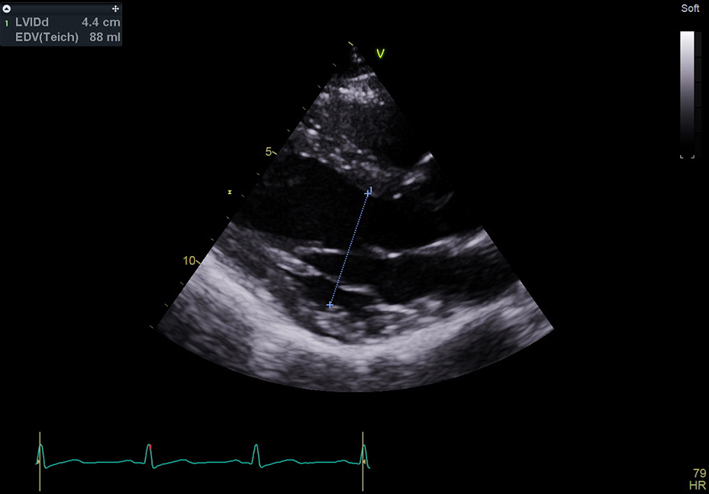 |
| PLAX (2D)with colour Doppler over aortic valve (AV) | Check colour Doppler settings Colour box over AV Look for abnormal flow over AV |
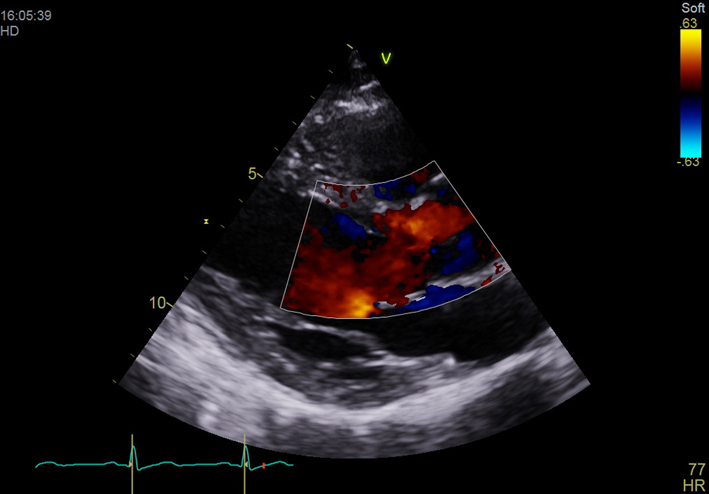 |
| PLAX (2D) with colour Doppler over mitral valve (MV) | Check colour Doppler settings Colour box over MV Look for abnormal flow over MV |
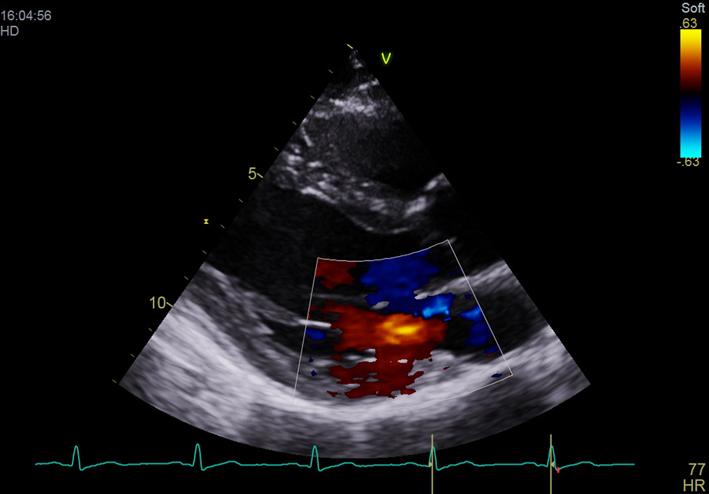 |
| PSAX Outflow (2D) | AV appearance and function | 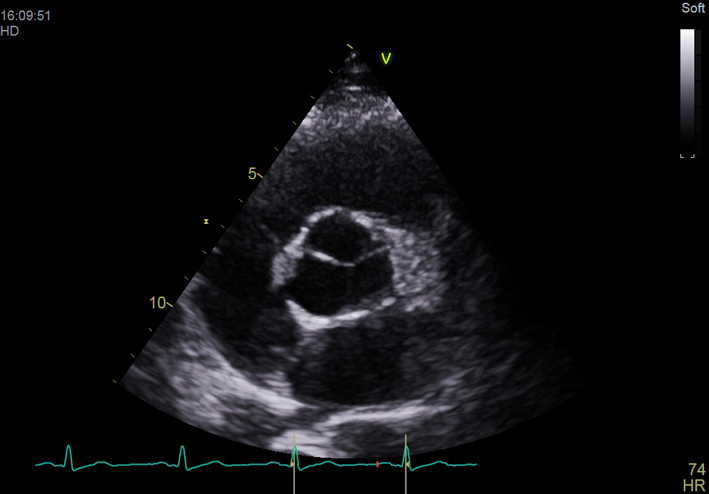 |
| PSAX Base (2D) | MV appearance and function Radial systolic function Major regional wall motion abnormalities |
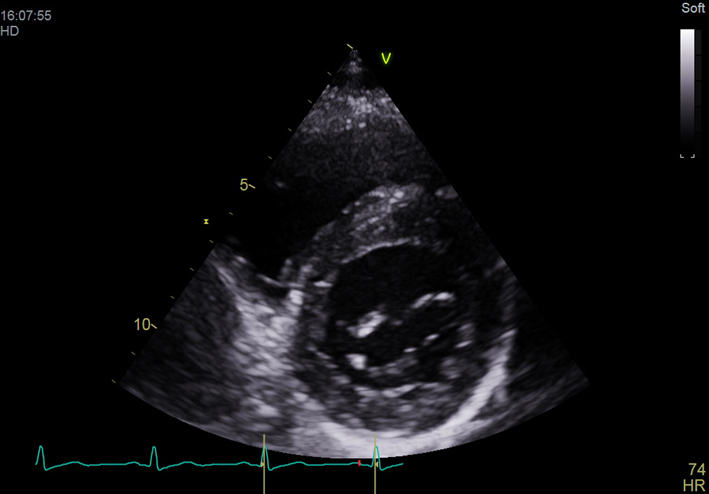 |
| PSAX Mid (2D) | Radial systolic function Major regional wall abnormalities |
 |
| PSAX Apex (2D) | Radial systolic function Major regional wall abnormalities |
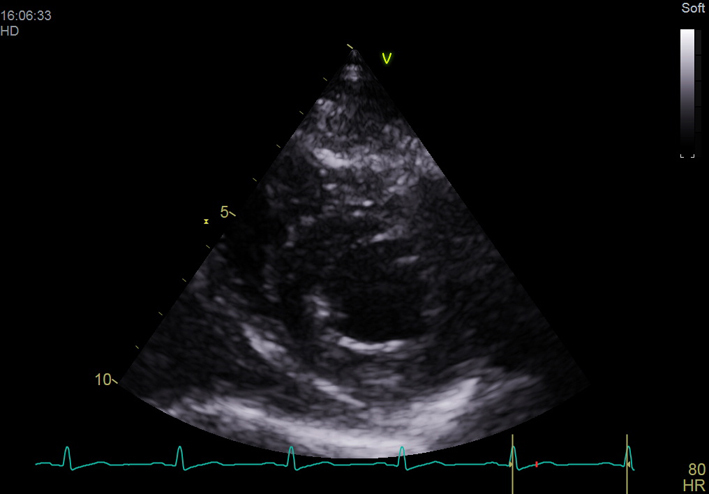 |
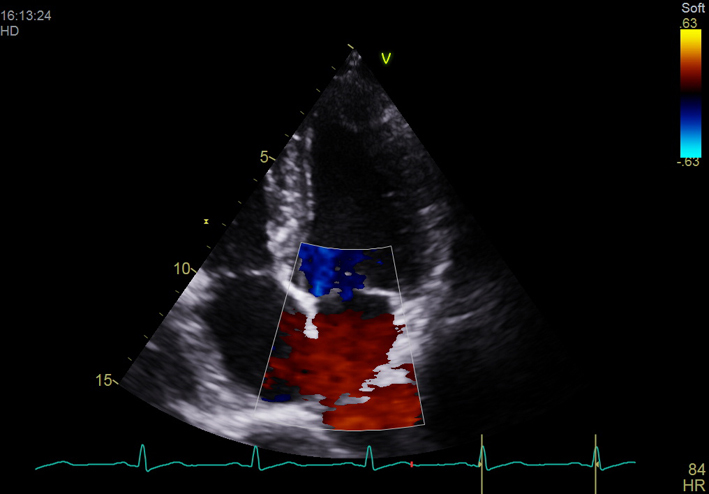
| Apical 4 chamber (2D) | LV cavity size (visual assessment) Visual assessment of longitudinal and radial function Major regional wall abnormalities MV appearance and function TV appearance and function RV cavity size (compared with LV size) RV free wall motion (visual assessment) Visual assessment of RV free wall hypertrophy Observe atrial septal position/mobility |
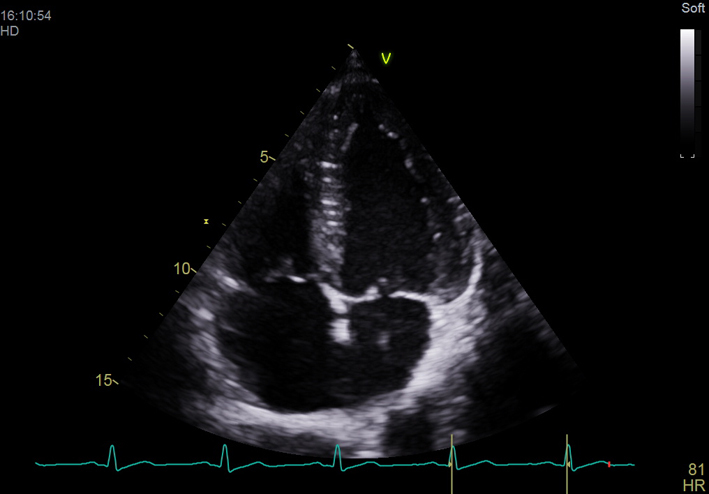 |
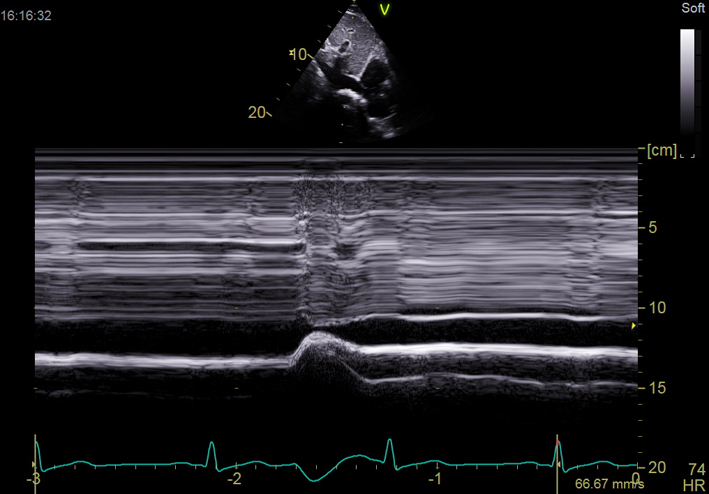
| A4C (M-Mode) TAPSE | M-mode through the lateral tricuspid valve annulus Measure tricuspid annular plane systolic excursion (TAPSE) |
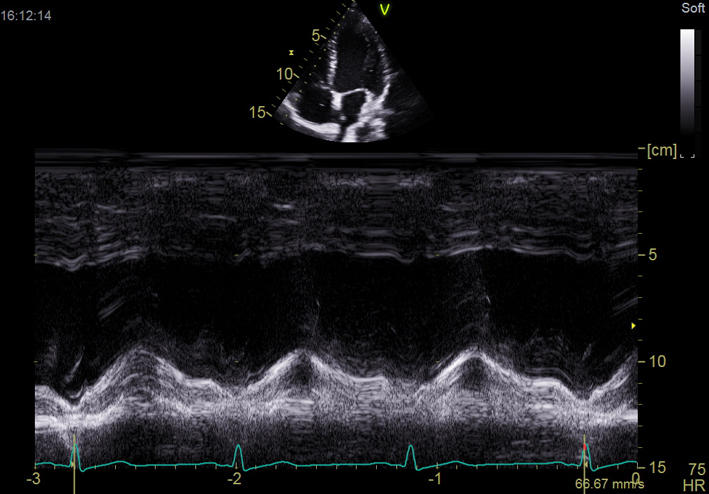 |
| A4C (2D) with CFM TV | Check colour Doppler settings Look for abnormal colour flow over TV |
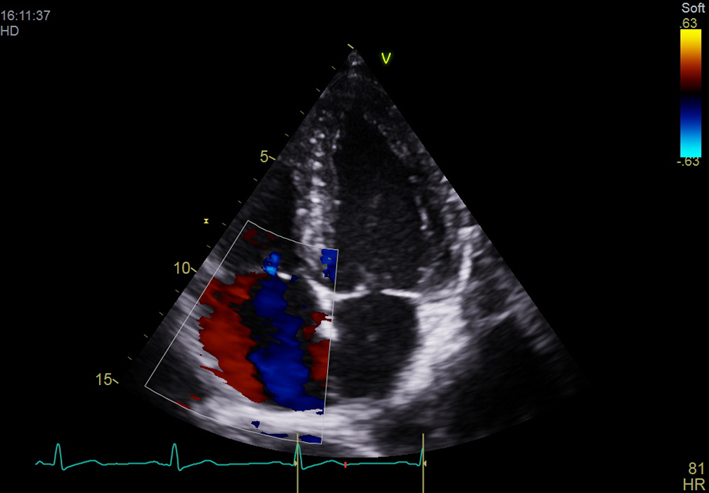 |
| A4C (2D) with CFM MV | Check colour Doppler settings Look for abnormal colour flow over MV |
 |
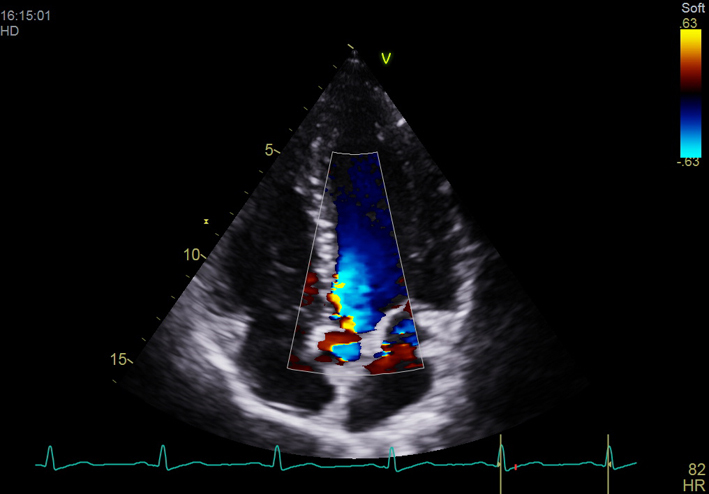
| A5C (2D) | AV appearance and function | 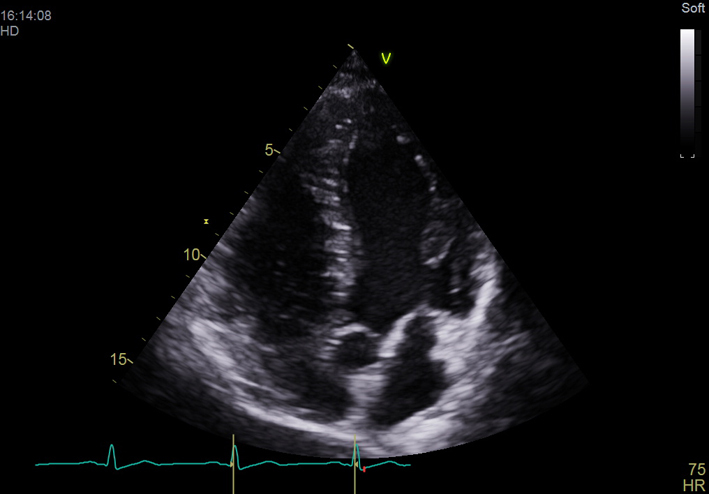 |
| A5C (2D) with CFM AV | Check colour Doppler settings Look for abnormal flow over AV |
 |
| Subcostal 4Ch (2D) | Relative chamber sizes and function Visual assessment of RV free wall hypertrophy Atrial septal position and hypertrophy Pericardial effusion |
 |
| Subcostal IVC (2D) | Observe size and collapsibility with respiration | 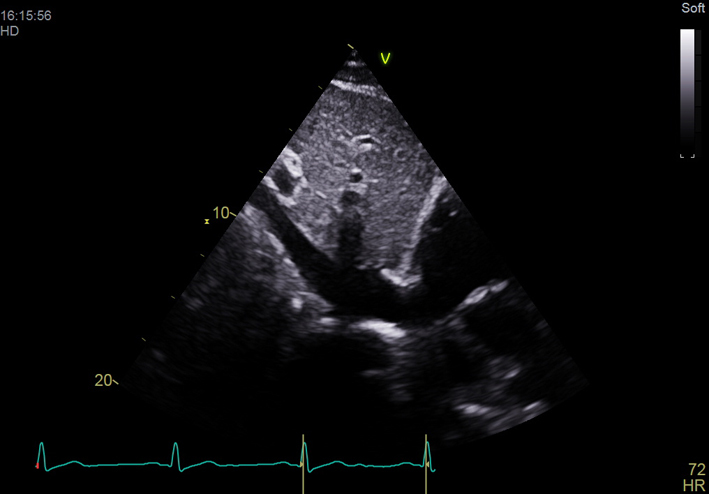 |
| Subcostal IVC (M-mode) | Assess IVC size and variation with respiration Dilated IVC may indicate high right atrial pressure |
 |
The dataset provides the necessary information required to identify clinically relevant pathology and to allow the study to be readily repeated at the bedside to assess progress or effectiveness of intervention.
Visual recognition or suspicion of other significant abnormalities may warrant further assessment with a Level 2 transthoracic or transoesophageal study and a referral to specialist cardiology services. It is for this reason that Level 1 echocardiograms must be performed within a wider service with imaging providers subject to and learning from service review processes including immediate senior review if required.
Conclusion
This guideline outlines the requirements and minimum dataset for a Level 1 echocardiogram. This protocol is designed to support non-expert and expert sonographers in identifying or excluding important pathology in critically unwell patients. The protocol is also designed to facilitate efficient use of personnel and services to deliver a 24/7 service; it is also appropriate for use when patient contact needs to be minimised, for example, when managing patients with highly contagious respiratory infections such as COVID-19. Level 1 echocardiography should be viewed as a separate test from a Level 2 echocardiogram, with clear indications and contraindications which are patient- and pathology-specific.
Declaration of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of this guideline.
Funding
This work did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
References
- 1.Wharton G, Steeds R, Allen J, Phillips H, Jones R, Kanagala P, Lloyd G, Masani N, Mathew T, Oxborough D, et al. A minimum dataset for a standard standard transthoracic echocardiogram: a guideline protocol from the British Society of Echocardiography. Echo Research and Practice 2015. 2 G9–G24. ( 10.1530/ERP-14-0079) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heiberg J, El-Ansary D, Canty DJ, Royse AG & Royse CF. Focussed echocardiography: a systematic review of diagnostic and clinical decision-making in anaesthesia and critical care. Anaesthesia 2016. 17 1091–1100. ( 10.1111/anae.13525) [DOI] [PubMed] [Google Scholar]
- 3.Hall DP, Jordan H, Alam S, Gillies MA. The impact of focussed echocardiography using the Focussed Intensive Care Echo protocol on the management of critically ill patients, and comparison with full echocardiographic studies by BSE-accredited sonographers. Journal of the Intensive Care Society 2017. 18 206–211. ( 10.1177/1751143717700911) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.NHS England.Seven Day Services Clinical Standards. London, UK, NHS England, 2017. (available at: https://www.england.nhs.uk/wp-content/uploads/2017/09/seven-day-service-clinical-standards-september-2017.pdf) [Google Scholar]
- 5.Senthilnathan M, Kundra P, Mishra SK, Velayudhan S, Pillai AA. Competence of intensivists in focussed transthoracic echocardiography in intensive care unit: a prospective observational study. Indian Journal of Critical Care Medicine 2018. 22 340–345. ( 10.4103/ijccm.IJCCM_401_17) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alam SR, Docherty A, Mackle I, Gillies MA. The introduction of intensive care-led echocardiography into a tertiary care unit. Journal of the Intensive Care Society 2013. 14 15–19. ( 10.1177/175114371301400105) [DOI] [Google Scholar]
- 7.Orme RM, Oram MP, McKinstry CE. Impact of Echocardiography on patient management in the intensive care unit: an audit of district general hospital practice. British Journal of Anaesthesia 2009. 102 340–344. ( 10.1093/bja/aen378) [DOI] [PubMed] [Google Scholar]
- 8.Stanko LK, Jacobson E, Tam JW, De Wet CJ & Avidan M. Impact of echocardiography: impact on diagnosis and management in tertiary intensive care units. Anaesthesiology and Intensive Care 2005. 33 492–496. ( 10.1177/0310057X0503300411) [DOI] [PubMed] [Google Scholar]
- 9.Colebourn C, Pierce K, Sharma V, Steeds R. Delivering 7-Day Services in Echocardiography – A Proposal for Level 1 Emergency Echocardiography from the British Society of Echocardiography. London, UK: British Society of Echocardiography, 2017. [Google Scholar]



 This work is licensed under a
This work is licensed under a