Abstract
The World Bank will publish the nine volumes of Disease Control Priorities, 3rd edition, in 2015–16. Volume 1—Essential Surgery—identifies 44 surgical procedures as essential on the basis that they address substantial needs, are cost effective, and are feasible to implement. This report summarises and critically assesses the volume’s five key findings. First, provision of essential surgical procedures would avert about 1.5 million deaths a year, or 6–7% of all avertable deaths in low-income and middle-income countries. Second, essential surgical procedures rank among the most cost effective of all health interventions. The surgical platform of the first-level hospital delivers 28 of the 44 essential procedures, making investment in this platform also highly cost effective. Third, measures to expand access to surgery, such as task sharing, have been shown to be safe and effective while countries make long-term investments in building surgical and anaesthesia workforces. Because emergency procedures constitute 23 of the 28 procedures provided at first-level hospitals, expansion of access requires that such facilities be widely geographically diffused. Fourth, substantial disparities remain in the safety of surgical care, driven by high perioperative mortality rates including anaesthesia-related deaths in low-income and middle-income countries. Feasible measures, such as WHO’s Surgical Safety Checklist, have led to improvements in safety and quality. Fifth, the large burden of surgical disorders, cost-effectiveness of essential surgery, and strong public demand for surgical services suggest that universal coverage of essential surgery should be financed early on the path to universal health coverage. We point to estimates that full coverage of the component of universal coverage of essential surgery applicable to first-level hospitals would require just over US$3 billion annually of additional spending and yield a benefit–cost ratio of more than 10:1. It would efficiently and equitably provide health benefits, financial protection, and contributions to stronger health systems.
Introduction
Disorders that are treated mainly or frequently by surgery constitute a substantial portion of the global burden of disease. Each year, injuries kill nearly 5 million people and about 270 000 women die from complications of pregnancy.1 Many of these injury-related and obstetric-related deaths, as well as deaths from other causes (eg, abdominal emergencies and congenital anomalies), could be prevented by improved access to surgical care.
Despite this large burden, surgical services are not being delivered to many of the individuals who need them most. An estimated 2 billion people lack access to even the most basic of surgical care.2 This need has not been widely acknowledged, and priorities for investment in health systems’ surgical capacities have therefore only recently been investigated. Indeed, until the 1990s, health policy in resource-constrained settings focused sharply on infectious diseases and undernutrition, especially in children. Surgical capacity was developing in urban areas but was often viewed as a secondary priority that mainly served socioeconomically advantaged people.
In the 1990s, several studies began to question the perception that surgery was costly and low in effectiveness. Economic evaluations of cataract surgery showed the procedure to be cost effective even under resource-constrained circumstances; Javitt3 pioneered cost-effectiveness analysis for surgery, including his chapter on cataract in the first edition of Disease Control Priorities in Developing Countries in 1993. In 2003, McCord and Chowdhury4 enriched the approach to economic evaluation in surgery in a report assessing the overall cost-effectiveness of a surgical platform in Bangladesh. The design of Disease Control Priorities in Developing Countries, 2nd edition (DCP2), published in 2006, placed much more substantial emphasis on surgery than had previous health policy documents. DCP2 included a dedicated chapter on surgery that amplified the approach of McCord and Chowdhury and provided an initial estimate of the amount of disease burden that could be addressed by surgical intervention in low-income and middle-income countries. The design of the Disease Control Priorities, 3rd edition (DCP3), places still-greater emphasis on surgery by dedication of an entire volume (out of nine in total) to the topic. There is also a growing academic literature on surgery’s importance in health system development—for example, as described by Paul Farmer and Jim Kim,5 who noted that “surgery may be thought of as the neglected stepchild of global public health”. Likewise, WHO is paying increasing attention to surgical care, such as through its Global Initiative for Emergency and Essential Surgical Care.6 Finally, the creation of a Lancet Commission on Global Surgery,7 now well into its work, points to a major change in the perceived importance of surgery.
This report summarises the main findings of Essential Surgery.8 We attempt to better define the health burden of disorders requiring surgery, identify those surgical procedures that are the most cost effective and cost beneficial, and describe the health-care policies and platforms that can universally deliver these procedures at high quality. In particular, Essential Surgery seeks to define and study a package of so-called essential surgical procedures that would lead to substantial improvements in health if they were universally delivered (ie, universal coverage of essential surgery). This report and the volume focus on the situation in low-income and lower-middle-income countries. In a companion Comment, Dean Jamison9 discusses the history, objectives, and contents of DCP3, of which Essential Surgery constitutes Volume 1.xx.
Definitions
Health disorders cannot be neatly dichotomised into disorders that need surgery and those that do not. Different diagnoses range widely in the proportion of patients who need some type of surgical procedure. At the upper end are admissions for musculoskeletal disorders (84% of which involved some type of surgical procedure in an operating room in the USA in 2010) and at the lower end are admissions for mental health disorders (0·4%).10
The surgical capabilities required are not only those related to surgical operations. Surgical care also includes preoperative assessment (including the decision of whether to operate or not), provision of safe anaesthesia, and postoperative care. Even when patients do not need a surgical procedure, surgical providers often provide care, such as management of severe head injuries, and resuscitation for airway compromise and shock in patients with trauma. Such care occurs in contexts in which clinicians must be prepared to intervene operatively as complications arise or conditions deteriorate.
Within the limitations inherent in the definition of surgical disorders, DCP3 has outlined, by consensus, a group of essential surgical disorders and the procedures (and other surgical care) needed to treat them. Essential surgical disorders can be defined as those that are mainly or extensively treated by surgery (procedures and other surgical care), have a large health burden, and can be successfully treated by a surgical procedure (and other surgical care) that is cost effective and feasible to promote globally.11,12
In most situations, procedures to treat these disorders (eg, caesarean section) can be done at first-level hospitals—ie, those that have about 50–200 beds, serve roughly 50 000–200 000 people, and have basic surgical capabilities. However, for some disorders, the treatments (eg, cataract extraction) are mainly provided at higher-level or specialised facilities. In table 1, we have listed the procedures that we define to be essential. This report addresses those disorders listed in table 1. We acknowledge that the list is not exhaustive, and other procedures might also be considered as essential. For many countries, however, table 1 will provide a reasonable starting point for an essential surgical package, although there will be country-specific variations. Safe anaesthesia and perioperative care are necessary components of all of these procedures.
Table 1. The essential surgery package—procedures and platforms.
| Platform for delivery of procedure | |||
|---|---|---|---|
| Community facility and primary health centres | First-level hospitals | Referral and specialised hospitals | |
| Dental procedures | Extraction Drainage of dental abscess Treatment for caries* |
·· | ·· |
| Obstetric, gynaecological, and family planning | Normal delivery† | Caesarean birth† Vacuum extraction or forceps delivery† Ectopic pregnancy† Manual vacuum aspiration and dilation and curettage† Tubal ligation Vasectomy Hysterectomy for uterine rupture or intractable post-partum haemorrhage† Visual inspection with acetic acid and cryotherapy for precancerous cervical lesions |
Repair obstetric fistula |
| General surgical | Drainage of superfi cial abscess† Male circumcision |
Repair of perforations (perforated peptic ulcer, typhoid ileal perforation, etc)† Appendectomy† Bowel obstruction† Colostomy† Gallbladder disease (including emergency surgery for acute cholecystitis†) Hernia (including incarceration†) Hydrocelectomy Relief of urinary obstruction; catheterisation or suprapubic cystostomy (tube into bladder through skin)† |
·· |
| Injury‡ | Resuscitation with basic life support measures† Suturing laceration† Management of non-displaced fractures† |
Resuscitation with advanced life support measures, including surgical airway† Tube thoracostomy (chest drain)† Trauma laparotomy†§ Fracture reduction† Irrigation and debridement of open fractures† Placement of external fi xator; use of traction† Escharotomy or fasciotomy (cutting of constricting tissue to relieve pressure from swelling)† Trauma-related amputations† Skin grafting Burr hole† |
·· |
| Congenital | ·· | ·· | Cleft lip and palate repair Club foot repair Shunt for hydrocephalus Repair of anorectal malformations and Hirschsprung’s disease |
| Visual impairment | ·· | ·· | Cataract extraction and insertion of intraocular lens Eyelid surgery for trachoma |
| Non-trauma orthopaedic | ·· | Drainage of septic arthritis† Debridement of osteomyelitis† |
·· |
All procedures listed in this table are discussed in DCP3 (Volume 1: Essential Surgery), with the following three exceptions, which will be covered in other DCP volumes: male circumcision, visual inspection and treatment of precancerous cervical lesions, and eyelid surgery for ocular trachoma. All of the procedures listed under community facility and primary health centres are also frequently provided at first-level and referral hospitals. All of the procedures under first-level hospitals are also frequently provided at referral hospitals. The column in which a procedure is listed is the lowest level of the health system in which it would usually be provided. Not included in the table are prehospital interventions, such as first aid, basic life support procedures, or advanced life support procedures done in the prehospital setting. Health systems in different countries are structured differently and what might be suitable at the various levels of facilities will differ. Likewise, each facility level represents a spectrum of capabilities. In this table, community facility implies mainly outpatient capabilities (as would be used to provide the elective procedures such as dental care), whereas primary health centre implies a facility with overnight beds and 24 h staff (as would be needed for procedures such as normal delivery). First-level hospital implies fairly well-developed surgical capabilities with doctors with surgical expertise, otherwise many of the procedures would need to be done at higher-level facilities. Referral and specialised hospitals imply facilities that have advanced or subspecialised expertise for treatment of one or more surgical disorders, not usually found at lower-level facilities. This list of essential surgical procedures is based on the authors’ judgment in light of the burden, implementation feasibility, and cost-effectiveness information contained in DCP3 (Volume 1: Essential Surgery). Earlier assessments of essential surgical interventions also provide useful information. 6,11–13 DCP3=Disease Control Priorities, 3rd edition.
Treatment for caries can include one or more of the following, depending on local capabilites: silver-diamine-fluoride application, atraumatic restoration, or fillings.
Emergency procedure or disorder.
Trauma (injury) care includes a wide variety of procedures. Not included in the list of essential procedures would be procedures that are more applicable at higher-level facilities: repair of vascular injury, open reduction and internal fixation, drainage of intracranial haematoma (other than through burr hole), or exploration of neck or chest.
Trauma laparotomy applicable at first-level hospitals: exploratory laparotomy for haemoperitoneum, pneumoperitoneum, or bowel injury; specific procedures include splenectomy, splenic repair, packing of hepatic injury, and repair of bowel perforation.
Key messages
Overview
This report synthesises the main results of the individual chapters of Essential Surgery to provide broad directions for policy. The key messages deriving from our analysis are summarised and explained in further detail below, concerning five categories of results: surgically avertable disease burden, cost-effectiveness and economics, improvements to access, improvements to quality, and essential surgery in the context of universal health coverage. The appendix lists the titles, authors, and main messages of each individual chapter of Essential Surgery.
Disease burden avertable by essential surgery
The disorders treated at least partly by the procedures in table 1 account for 4·7 million deaths (or 10% of all deaths) in low-income and middle-income countries (table 2). This figure is probably an underestimate, because the burden of several common surgical disorders represented in table 1 (eg, bowel obstruction and gallbladder disease) are not estimated as distinct entities in WHO’s Global Health Estimates and hence are not included in table 2. With universal coverage of essential surgery in low-income and middle-income countries, 1·5 million deaths per year could be averted (table 3), representing 6·5% of all avertable deaths in these countries.
Table 2. Total burden of disorders addressed by essential surgery in low-income and middle-income countries, 2011.
| Deaths (1000) | DALYs (1000) | |
|---|---|---|
| Category 1: communicable, maternal, perinatal, and nutritional | ||
| Maternal disorders | 280 | 19 000 |
| Birth asphyxia and birth trauma | 780 | 78 000 |
| Category 2: non-communicable diseases | ||
| Cataracts | <1 | 7000 |
| Peptic ulcer disease | 230 | 7000 |
| Appendicitis | 38 | 2000 |
| Skin diseases* | 90 | 16 000 |
| Cleft lip and palate | 5 | <1000 |
| Oral disorders† | <1 | 13 000 |
| Category 3: injuries Road traffic crash | ||
| Road traffic crash | 1160 | 72 000 |
| Other unintentional injury‡ | 1550 | 96 000 |
| Intentional injury§ | 540 | 34 000 |
| Burden from these disorders | 4700 | 340 000 |
| Total burden from all causes in low-income and middle-income countries | 45 000 | 2 400 000 |
| Percent of burden due to disorders addressed by essential surgery | 10·4% | 14·2% |
DALY=disability-adjusted life-year.
Skin diseases include abscess and cellulitis.
Oral disorders include caries, periodontal disease, and edentulism. Data from WHO Global Health Estimates.1
Other unintentional injury includes falls, fires (and heat and hot substances), and exposure to forces of nature; it excludes drowning and poisoning.
Intentional injury includes violence and collective violence or legal intervention; it excludes self-harm.
Table 3. Disease burden avertable by essential surgery in low-income and middle-income countries, 2011.
| Deaths (1000) | DALYs (1000) | |
|---|---|---|
| Total burden | 45 000 | 2 400 000 |
| Total avertable burden* | 23 000 | 1 300 000 |
| Burden from disorders addressed by essential surgery† | 4700 | 340 000 |
| Burden avertable by essential surgery‡ | 1500 | 87 000 |
| Burden avertable by essential surgery (proportion of total burden) | 3·3% | 3·6% |
| Burden avertable by essential surgery (proportion of avertable burden) | 6·5% | 6·6% |
DALY=disability-adjusted life-year.
Total avertable burden refers to the number of deaths and DALYs that would be averted if all-cause, age-adjusted rates of death and disability in high-income countries pertained in low-income and middle-income countries.
From table 2.
From Essential Surgery, chapter 2.14 The burden avertable from essential disorders as reported in this table is adjusted downward from that estimated in Essential Surgery because the figure here does not categorise as essential the surgery to address congenital cardiac disease or neural tube defects.
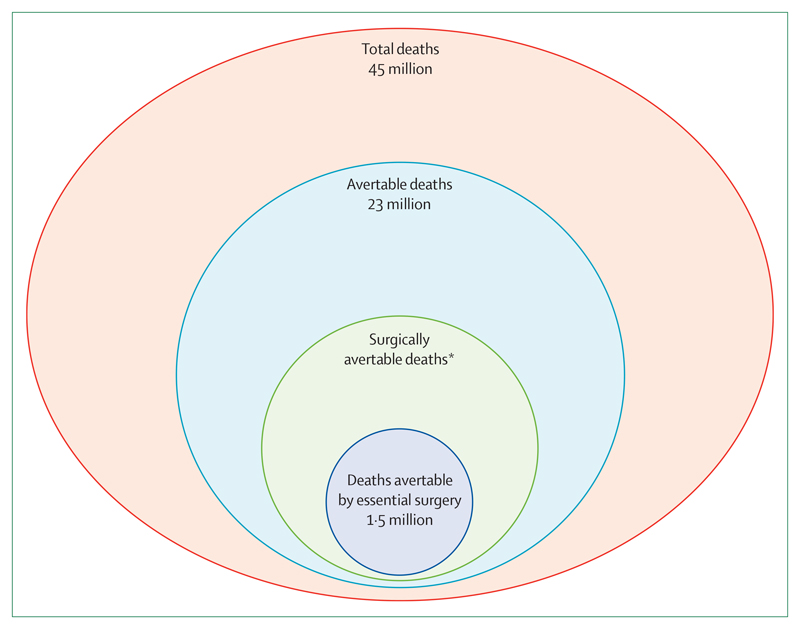
By comparison, DCP2 previously estimated that 11% of the total global burden of death and disability was from disorders that were very likely to need surgery.15,16 The current estimates are based on a more rigorous estimation method and a more narrowly defined subset of essential surgical disorders (figure 1), excluding other highly prevalent disorders often treated by surgery (eg, cancer and vascular disease). Further details about the estimation of burden avertable by essential surgery are provided in panel 1.
Figure 1. Deaths, avertable deaths, and surgically avertable deaths in low-income and middle-income countries in 2011.
Surgically avertable deaths refers to 2011 deaths in low-income and middle-income countries that would have been averted by the universal coverage of essential surgery. *Estimate not available.
Panel 1. Estimation of burden and avertable burden.
The burden of a particular health disorder can be measured in several ways. Most straightforward is the number of deaths it causes. In table 2, disorders that are addressed by essential surgery are listed, along with the numbers of deaths they each caused in 2011.
Other measures of burden include:
Years of life lost
In this measure, age of death is considered and years of life lost are calculated from life tables on the basis of the best-performing country in the world at a particular time. Disorders that result in more deaths at earlier ages (ie, more premature deaths) lead to a higher burden of years of life lost. Because this measure (and others) takes into account the years of life lost, it is on a larger scale than the measure of number of deaths.
Years lost due to disability
Also referred to as years lived with disability, this measure assesses years lived in states of less-than-optimum health (ie, disability). Different degrees of disability are calculated as disability weights applied to the number of years lived with a particular disorder.
Disability-adjusted life-years
A summary measure adding years of life lost and years lost due to disability for a particular disorder. In table 2, the disability-adjusted life-years for each of the disorders addressed by essential surgery are listed.
Avertable burden
Avertable burden implies the number of deaths (or other burden measure) that would not have occurred if a different (or counterfactual) state pertained. In table 3 and figure 1, the total avertable health burden is included as the numbers of deaths that would be averted if all-cause, age-adjusted rates of death (and disability) in high-income countries pertained in low-income and middle-income countries. Avertable burden for a particular intervention can also be estimated and is classified as what would be achieved with universal availability of that intervention. Chapter 2 in Essential Surgery14 goes into detail in estimating the avertable burden that would be achieved if all low-income and middle-income countries had access to several surgical interventions at the same level as in the best-performing high-income countries. These interventions include caesarean birth or related procedures for obstructed labour, haemorrhage, or fetal distress; surgery for four gastrointestinal disorders (appendicitis, intestinal obstruction, hernia, and gallbladder disease); surgery for trauma; cataract extraction; repair of obstetric fistula; and surgery for several congenital anomalies (eg, cleft lip and palate). In table 3 and figure 1, this avertable burden from universal coverage of essential surgery is estimated at 1·5 million deaths, accounting for 6·5% of the total avertable burden of deaths in low-income and middle-income countries. A similar figure for all of surgical care has not yet been derived by the research community.
Obtaining more accurate estimates of avertable burden from surgically treatable disorders will need broad agreement on a definition of the concept of avertable burden and on methods for its measurement. The steps taken in Essential Surgery should be regarded as preliminary. Improved estimates of avertable burden will need systematic data gathering from hospitals and population-based surveys to establish the proportion of the world’s population that lacks access to surgical care. Such a survey was recently done in Sierra Leone,17 showing that 25% of deaths might have been prevented with timely surgical care. Similar studies need to be repeated more widely. In addition to individual research studies, the international community could contribute to development and promotion of metrics for ongoing monitoring of the burden of essential surgical disorders, as is currently done for maternal mortality.
Economic evaluation of essential surgery
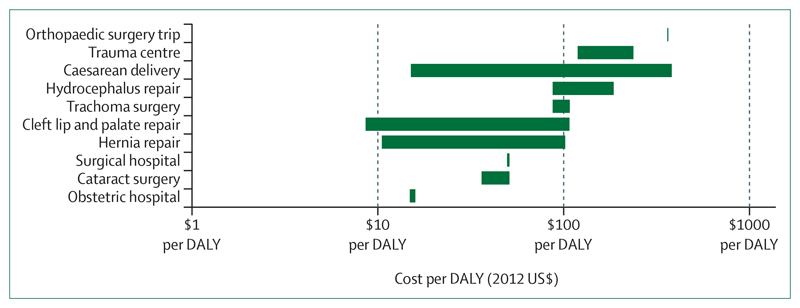
At the time of DCP2, a small number of cost-effectiveness analyses had shown specific surgical procedures to be very cost effective. Since then, the scientific literature has expanded and consistently documented that many of the essential surgical services identified in this report rank among health care’s most cost-effective interventions (figure 2). A few examples (all context specific) include cleft lip repair (US$10–110 per disability-adjusted life-year [DALY] averted), inguinal hernia repair ($10–100 per DALY averted), cataract surgery (about $50 per DALY averted), and emergency caesarean section ($15–380 per DALY averted). By comparison, many of the widely disseminated public health measures are of similar cost-effectiveness, for example vitamin A supplementation (about $10 per DALY averted), oral rehydration solution (more than $1000 per DALY averted), and antiretroviral therapy for HIV/AIDS (about $900 per DALY averted).19,20
Figure 2. Cost-effectiveness of surgical interventions.
Figure summarises the cost-effectiveness of surgical interventions in low-income and middle-income countries according to available evidence. The data are presented in cost per DALY averted, in 2012 USD$.18 Orthopaedic surgery trip refers to a mission or outside group visiting a location and undertaking a set of surgical procedures. DALY=disability-adjusted life-year.
Benefit–cost analyses have shown similar findings. An analysis of the benefits from cleft lip repair evaluated the costs needed to run a specialised cleft clinic in India and the resulting health benefits, to which a monetary benefit was ascribed. Cleft surgery had a cost of about $300 per DALY averted and had a benefit–cost ratio of 12:1.21 This puts cleft repair within the benefit–cost ratio range for the key investment priorities for disease control established by the Copenhagen Consensus, an organisation that asks experts to rank global health and development interventions.22 The benefit–cost ratio for cleft surgery is also very high, similar to the range across different development sectors. Panel 2 provides an overview of approaches to economic evaluation of surgical procedures and an overview of findings.
Panel 2. Economic evaluation of investments in surgery.
Economic evaluations aim to inform decision making by quantifying the tradeoffs between resource inputs needed for alternative investments and the resulting outcomes. Four approaches to economic evaluation in health are particularly prominent:
Assessment of how much of a specific health outcome (eg, HIV infections averted) can be attained for a particular level of resource input.
Assessment of how much of an aggregate measure of health (eg, deaths, disability, or quality-adjusted life-years such as disability-adjusted life-years or quality-adjusted life-years) can be attained from a particular level of resource inputs applied to alternative interventions; this approach of cost-effectiveness analysis enables comparison of the attractiveness of interventions addressing many different health outcomes (eg, tuberculosis treatment vs caesarean section).
Assessment of how much health and financial risk protection can be attained for a particular level of public-sector finance of a particular intervention; this approach (extended cost-effectiveness analysis) enables assessment not only of efficiency in improving the health of a population, but also of efficiency in achieving the other major goal of a health system (ie, protection of the population from financial risk).
Assessment of the economic benefits, measured in monetary terms, from investment in a health intervention and weighing that benefit against its cost (benefit–cost analysis); this analysis enables comparison of the attractiveness of health investments compared with those in other sectors.
Cost-effectiveness analyses predominate among economic evaluations in surgery (and for health interventions more generally). Three recent overviews of cost-effectiveness analysis findings for surgery (one in Essential Surgery) underpin this report’s conclusion that many essential surgical procedures are highly cost effective even in resource-constrained environments.18–20 Chapter 18 of Essential Surgery also assesses the cost-effectiveness of the district hospital surgical platform.18
The Lancet Commission on Investing in Health applied benefit–cost analysis to broad investments in health and showed ratios often in excess of 10:1.23 Essential Surgery contains benefit–cost evaluations of selected surgical procedures reporting similarly high ratios,21 and the Copenhagen Consensus for 2012 used benefit–cost analysis to rank “strengthening surgical capacity” as number eight in a list of 30 attractive priorities for investment in development across all sectors.22,24
Extended cost-effectiveness analyses remain a fairly new evaluation approach (developed for Disease Control Priorities, 3rd edition). In Essential Surgery, Shrime and colleagues25 apply extended cost-effectiveness analysis to surgical intervention in Ethiopia, showing substantial financial protection as well as health benefits.
The cost-effectiveness of some platforms or facility-types for provision of surgical care also needs to be considered. Essential Surgery includes a chapter on cost-effectiveness analysis.18 Basic essential procedures are likely to be cost effective when delivered at any level of the health-care system. However, the first-level hospital has been found to be especially cost effective as a surgical delivery platform, with costs of $10–220 per DALY averted for all surgical care delivered in this setting, across a wide range of low-income and middle-income countries.4,26–28 Most surgery in the first-level hospital is emergency surgery. Therefore, health systems need to disperse surgical facilities widely in the population, and surgical teams working in first-level hospitals should have a broad array of basic emergency skills rather than a narrow range of specialised skills.
A range of other surgical platforms were considered in our analysis. Short-term surgical missions by outside surgeons (ie, surgeons not living and working in that area) seem beneficial only if no other option is available; otherwise suboptimum outcomes, unfavourable cost-effectiveness, and lack of sustainability reduce their usefulness. Self-contained mobile platforms, such as hospital ships, seem to offer good outcomes for people who can reach them, but there are no data about their cost-effectiveness and obvious limitations for scale-up and national ownership. Specialised hospitals, including those providing surgery for cataract and obstetric fistula, seem to be among the most cost effective of the competing options for specialised platforms.29 Such specialised hospitals would be most sustainable if they also developed strong links with local practitioners (ie, those living and working in that country) to promote training and to ensure appropriate postsurgical care, and eventually evolved to be led by these local professionals. Because essential procedures done in specialised hospitals are elective, not urgent, patients can be scheduled over space and time to achieve high volumes, contain costs, and improve technical quality.
Many people with surgical disorders, especially trauma, die in the prehospital setting. For example, findings from a study30 showed that 81% of trauma deaths in Kumasi, Ghana, were in the prehospital setting. Most prehospital deaths occur in areas of low-income and middle-income countries where formal emergency medical services are rudimentary or absent. Improvement in the first aid skills of lay first responders can cost less than $10 per year of life gained, making it one of the most cost effective of all health interventions. Likewise, basic ambulance services can cost less than $300 per year of life gained, which is still highly cost effective.31
In 2013, Jamison and colleagues22 estimated that it would cost just over $3 billion annually to scale-up delivery of the component of the essential surgery package shown in table 1 that is applicable to first-level hospitals, so that this package is available universally. This development would have a benefit–cost ratio of 10:1, which is broadly consistent with that of other surgical procedures as described by Alkire and colleagues.21
Measures to improve access
The substantial avertable burden from surgical disorders is directly related to the low capacity for surgical care in many low-income and middle-income countries, as shown in the numbers of surgical procedures done globally. Most operations (60%) take place in wealthier countries, where 15% of the world’s population lives. Only 3·5% of operations take place in poorer countries, where 35% of the world’s people live.32 This low capacity for surgery in low-income and middle-income countries is in turn related to shortages of both human resources (eg, skills and staffing) and physical resources (eg, equipment and supplies).
In terms of human resources, across 23 low-income and middle-income countries the ratio of general surgeons per population was shown to range from 0·13 to 1·57 per 100 000, whereas the ratio of anaesthesiologists per population ranged from 0 to 4·9 per 100 000.33 By contrast, the USA has nine general surgeons and 11·4 anaesthesiologists per 100 000.34 There are also striking differences in the ratio of operating theatres per population across high-income and low-income settings: 25 per 100 000 in eastern Europe, 14–15 in North America and western Europe, 4–14 in Latin America, 4·7 in east Asia, but just 1·3 in south Asia and 1–1·2 in sub-Saharan Africa.2
There are examples of institutions and health systems successfully overcoming these barriers. For example, establishment of the Ghana College of Physicians and Surgeons in 2003 created the first in-country credentialing process for surgeons and led to an expansion of the workforce of fully trained general surgeons and obstetricians. As of June, 2014, 284 specialist surgeons and obstetrician-gynaecologists have graduated from the College and been posted to regional and district hospitals throughout the country to serve as both providers and trainers.
Expansion of access to essential surgical services in rural areas of low-income and middle-income countries will probably be impossible in the foreseeable future with dependence on only fully certified surgeons and anaesthesiologists. Innovative solutions to the surgical workforce crisis are thus imperative. Evidence shows that midlevel operators can safely do several essential surgical procedures, provided that they are properly trained and supervised and perform the operations frequently.35,36 In some locations these operators are general practitioners. In other areas, they are non-physician clinicians, such as técnicos de cirurgia in Mozambique or assistant medical officers in Tanzania.
Outcomes such as maternal and neonatal mortality after caesarean section and other emergency obstetric procedures for assistant medical officers were similar to those of doctors in Tanzania.35,36 Although cost studies are few, preliminary evidence shows the cost-effectiveness of task sharing. For example, in Mozambique, it was three times more cost effective to train and deploy técnicos de cirurgia than to train and deploy physicians to provide obstetric surgery; the 30-year cost per major operation was about $40 for técnicos de cirurgia and about $140 for physicians.37 Likewise, emergency obstetric care provided by general practitioners was found to be more cost effective than that provided by fully trained obstetricians in Burkina Faso.38
Non-physician clinicians are more likely than physicians to stay in under-served rural areas, and are less likely to emigrate to other countries; their deployment therefore substantially increases the availability of surgical services in under-served rural areas. In Mozambique and Tanzania, non-physician clinicians do about 90% of major emergency obstetric surgeries in rural areas where most of the population live, as explained in more detail in the DCP3 chapter on workforce innovations.39 Challenges continue for many countries in terms of physicians’ acceptance of non-physician clinicians, standardisation of their training, supervision, regulatory mechanisms, continuing skills improvement, and remuneration as well as non-financial incentives. The long-range goal is expansion of the number of fully trained surgeons. However, general practitioners and non-physician clinicians, with appropriate support from surgeons, can be an important intermediate solution to the problem of access to basic surgery.
Surgical training has traditionally emphasised decision making and operative technique for individual patient care, which is appropriate in view of the clinical role that most surgeons have. However, those surgeons who wish to address the system-level barriers to achievement of universal coverage of essential surgery will need additional skills in management and supervision of health-care systems, quality improvement, and public health.
In terms of physical resources, two related WHO efforts have defined optimum infrastructure needs for first-level hospitals for surgical care generally (the WHO Programme for Emergency and Essential Surgical Care) and for trauma care at all levels of the health-care system (the Essential Trauma Care Project). Surveys done with these WHO guidelines and tools have shown consistent lack of many low-cost pieces of equipment and supplies (eg, chest tubes, oxygen, and equipment for airway management and anaesthesia) in many locations, but especially in low-income countries and at first-level hospitals. In some cases, items are physically present but non-functional—for instance, equipment awaiting repairs. Often equipment is functional, but available only to those who can pay, sometimes in advance, and thus many patients who need the services are unable to access them.6,13,40–46
As with human resources, there are examples of health systems successfully confronting these barriers. For example, the Hanoi Health Department, Vietnam, steadily improved its physical resources for trauma care in its network of clinics and hospitals. Such improvements have been stimulated partly by research defining substantial gaps in availability of low-cost items recommended in WHO’s Guidelines for Essential Trauma Care, and by advocacy to remedy those gaps.47,48
Many essential physical resources are low cost and could be better supplied through improved planning and logistics. However, availability of some of the more expensive items (eg, x-ray machines, ventilators) would be improved by research into product development. Such research should address improved durability, low cost (both for purchase and operation), and increased ease of operation. Likewise, availability of many items could be improved by increased capabilities for local manufacture.49,50 However, international assistance for provision of basic essential equipment and supplies will be needed for the immediate future for the poorest countries. An often-overlooked component is the need to ensure local capacity to maintain and repair equipment.
For both human and physical resources, population, policy, and implementation research could contribute by identifying more-efficient and lower-cost delivery methods. WHO has already made substantial contributions by establishing norms for human and physical resources for surgical and trauma care and by documenting success stories of individual countries,6,13,47 a role that should be expanded.
A large additional barrier to access to surgical care is financial, especially in situations in which user fees are high or where out-of-pocket payments are required. Cost of surgical care is also a substantial contributor to medical impoverishment, as explained in more detail in the DCP3 chapter on surgery and poverty.51 Inclusion of universal coverage of essential surgery within universal public finance would remove financial barriers to access to essential surgical care, and would offer financial risk protection, as discussed further at the end of this report.
Improving the safety and quality of surgery and anaesthesia
In all settings, surgical care is fraught with hazards, including risks from the diseases themselves, from the operation, and from anaesthesia. These hazards translate into strikingly different risks of death and other complications in different settings. For example, compared with Sweden’s rate of 0·04 deaths per 1000 caesarean sections, mortality is at least 2–4 times higher in Latin America, 6–10 times higher in South Asia, and 100 times higher in sub-Saharan Africa.52,53
A large component of the differences in mortality after operations is caused by differences in mortality due to anaesthesia. Major advances have occurred in anaesthesia safety in high-income countries, mainly as a result of improved monitoring and increased standardisation and professionalisation. In wealthier countries, mortality per million anaesthetics has decreased from 357 deaths per million before 1970 to 25 deaths per million in the 1990s and 2000s. However, high rates of anaesthetic deaths are still prevalent in most low-income and middle-income countries. Deaths solely attributable to anaesthesia are estimated to occur at a rate of 141 deaths per million anaesthetics in poorer countries, by comparison with the noted 25 deaths per million anaesthetics in wealthier countries.54
Many of the deaths and complications from surgery in low-income and middle-income countries are potentially preventable with three specific affordable and sustainable improvements: use of a surgical safety checklist, improved monitoring and related safety practices during anaesthesia, and improved systems-wide monitoring and assessment of surgical care overall.
Use of the simple, 19-item WHO Surgical Safety Checklist across eight countries was reported to double adherence to basic perioperative safety standards,55,56 such as confirmation of the procedure and operative site, objective airway assessment, and completion of instrument and sponge counts at the end of the procedure. Use of the checklist reduced deaths by 47% (the postoperative death rate fell from 1·5% before introduction of the checklist to 0·8% afterwards) and inpatient complications by 35% (from 11% to 7%). The checklist improved outcomes in high-income, middle-income, and low-income countries and in elective and emergency cases.
The safety of anaesthesia in high-income countries has been achieved through adoption of standards of care, such as continuous presence of a trained anaesthesia provider and uninterrupted monitoring of oxygenation, ventilation, and perfusion.57 Anaesthesia delivery systems have been better standardised with safety features engineered into the machines. One crucial technology is pulse oximetry, an essential standard in high-income countries, which allows ongoing monitoring of oxygenation status so that problems can be corrected early on, before they lead to serious or lethal consequences. In one study in Moldova,58 introduction of a surgical safety checklist and pulse oximetry cut the number of hypoxic episodes and the complication rate by more than half. A barrier to pulse oximetry availability has been its cost, although a concerted global effort is underway to reduce these costs and increase availability of pulse oximetry in low-income and middle-income countries. With lower-cost options now available, the cost-effectiveness of pulse oximetry introduction seems very favourable.59
Improved monitoring and evaluation of surgical care across institutions, such as through quality improvement programmes, help to better inform administration and management. Quality improvement programmes range from very simple outcome assessments (eg, morbidity and mortality conferences) to more complex monitoring, such as surveillance of complications and use of risk-adjusted mortality. Many hospitals in low-income and middle-income countries have some type of basic quality improvement activities, such as periodic morbidity and mortality conferences. The effectiveness of these activities could be increased by simple measures such as more systematic recording of proceedings, more purposeful enactment of corrective action, and monitoring of the outcome of this corrective action. A WHO review of quality improvement programmes for trauma care showed that most programmes led to improvements in patient outcomes (including mortality) or process of care, with some centres also reporting cost savings.60 Although most of the programmes were from high-income countries, two were from Thailand, where a model programme for quality improvement led to sustained improvements in both process of care and mortality. Despite their effectiveness, simplicity, and affordability, quality improvement programmes are at a very rudimentary level of development and implementation in most low-income and middle-income countries.41,60
An important role for the international community is to support population, policy, and implementation research that addresses affordable and sustainable methods to improve quality of care, and documents and disseminates specific case studies of good practices being sustained.23 WHO has already made substantial contributions by establishing norms such as the WHO Surgical Safety Checklist. This role needs to be expanded further, such as through establishment and promotion of standards for safe, low-cost anaesthesia machines, and norms for monitoring and evaluation of procedures for surgical care. There also needs to be better definition and tracking of a variety of quality indicators globally, such as the perioperative mortality rate.54,61,62
Surgery as a core component of universal health coverage
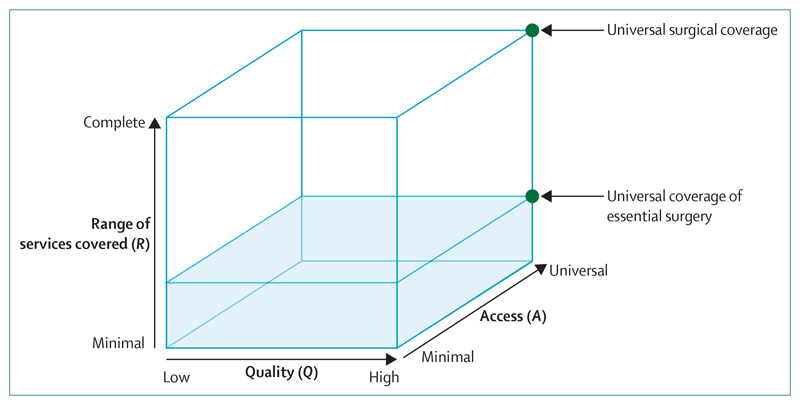
Our results point to the potential for essential surgery to cost-effectively address a large burden of disease. Moreover, there are several viable short-term and longer-term options for improvement of access, safety, and quality of surgical care. Figure 3 shows alternative uses for incremental resources in light of these findings. A country’s situation today could be portrayed as a point in the cube: its position on dimension Q depicts the current average quality of care, its position on dimension A represents the proportion of the population with access to care, and its position on dimension R shows the range of services available. Investment choice requires assessment of whether to put incremental money into improvements in access, improvements in average quality, or improvements in the range of services to be offered. Our interpretation is that it will generally prove both equitable and effcient to achieve full access to essential surgery at high quality rather than committing public resources to expanding the range of services for a smaller proportion of the population. The shading in figure 3 depicts this situation, which we have labelled universal coverage of essential surgery. Achievement of universal coverage of essential surgery should appear early on the pathway to universal health coverage as discussed by Jamison and colleagues.23
Figure 3. The dimensions of universal coverage of essential surgery.
Access is defined as the extent to which services are available to the population—geographically, socially, and financially (eg, with little or no out-of-pocket payments at the point of service).
There are other surgical disorders and procedures to consider, such as those for cancer, vascular disease, and disorders requiring more advanced treatments such as transplantation. Improving access to these procedures will also have benefit. But, in terms of sequencing and use of public funds, efforts to assure greater access to quality essential services should be undertaken before increased investment in disorders that are more expensive to treat or that have a smaller health effect.
Conclusions
There is a high burden of avertable death and disability from disorders that can be successfully treated by surgery. Many of the surgical procedures and capabilities needed to treat these disorders are among the most cost effective of all health interventions and most in demand from the population. These interventions include procedures to treat injuries, obstetric complications, abdominal emergencies, cataracts, obstetric fistula, and congenital anomalies. Many of the most needed procedures are affordable and feasible to deliver, but improving their coverage and quality will need a focused effort to strengthen the health system, particularly at first-level hospitals. With the exception of obstetric care, the global health community has largely failed to address the unmet need for surgery. The surgical community in turn has not tackled broader requirements for incorporating surgery into resource-constrained health systems (with the important exceptions of exploring task-sharing and improving quality of care).
Assurance of essential surgical services to everyone who needs them, when they need them, is deliverable partly through improved training in safe surgical care and technique, and partly through improved functioning of health systems—including better monitoring and evaluation, development of appropriate financing mechanisms, and promotion of equity, social justice, and human rights. The global system can play an important part in these efforts through informed leadership and advocacy, support for population, policy, and implementation research, and financial transfers to low-income countries to assist attainment of universal coverage of essential surgery.
Improved access to essential surgery should be implemented early in the path to universal health coverage, as part of the overall essential benefit package advocated by the Lancet Commission on Investing in Health.23 Implementation would include measures such as use of public funds to ensure access to essential surgery, safely and effectively, and inclusion of in the packages covered by national health insurance schemes. Such measures would also offer financial risk protection against medical impoverishment from the costs of surgical care. Surgery should be viewed as an indispensable component of a properly functioning health system, and can be a means to strengthen the entire system, thus increasing the return on investment.23,63 Investments to provide and maintain equipment and to ensure a steady flow of supplies required for a functioning surgical service can strengthen the supply chain for an entire facility. The early literature in this area also suggests positive spillovers between surgical investments and the functioning of and demand for health care. For example, upgrading of facilities to provide surgery has improved providers’ confidence in their facility and their own clinical skills in Uganda.64 Findings from several studies have shown that availability of surgical services has increased demand for health care in potentially high-risk conditions, such as labour and delivery or emergency care.64–66
National governments and the international community should commit themselves to universal coverage of essential surgery, to substantially reduce mortality and morbidity from treatable surgical disorders, protect populations from financial risk, and contribute to the development of the broader health system.
Acknowledgments
The Bill & Melinda Gates Foundation provides financial support for the Disease Control Priorities Network project, of which this volume is a part. The following individuals provided valuable comments and assistance on this report: Elizabeth Brouwer, Rachel Cox, Anna Dare, Sarah Greenberg, Andrew Leather, Rachel Nugent, and Gavin Yamey.
Footnotes
For the Bellagio Essential Surgery Group see http://essentialsurgery.org/bellagio/index.html
Contributors
HTD, DTJ, and CNM generated the basic plan for this study. CNM prepared the first draft with input and revisions from all authors. All authors approved the final draft. HTD, DTJ, and CNM had responsibility for submitting for publication.
Declaration of interests
DTJ reports grants from the Bill & Melinda Gates Foundation during conduct of the study. AG reports receiving royalties from personal publications on health-care improvement, including surgery and use of checklists. MEK, HTD, PD, and CNM declare no competing interests.
Contributor Information
Prof Charles N Mock, Departments of Surgery and of Global Health, University of Washington, Seattle, WA, USA.
Prof Peter Donkor, Department of Surgery, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana.
Prof Atul Gawande, Ariadne Labs: A Joint Center for Health System Innovation at Brigham and Women’s Hospital and Harvard T H Chan School of Public Health, Boston, MA, USA.
Prof Dean T Jamison, Department of Global Health, University of Washington, Seattle, WA, USA.
Margaret E Kruk, Department of Global Health and Population, Harvard T H Chan School of Public Health, Harvard University, Boston, MA, USA.
Prof Haile T Debas, Global Health Sciences and Department of Surgery, University of California, San Francisco.
References
- 1.Global Health Estimates. Geneva: World Health Organization; 2011. [accessed Jan 27, 2015]. http://www.who.int/healthinfo/global_burden_disease/en/ [Google Scholar]
- 2.Funk LM, Weiser TG, Berry WR, et al. Global operating theatre distribution and pulse oximetry supply: an estimation from reported data. Lancet. 2010;376:1055–61. doi: 10.1016/S0140-6736(10)60392-3. [DOI] [PubMed] [Google Scholar]
- 3.Javitt JC. The cost-effectiveness of restoring sight. Arch Ophthalmol. 1993;111:1615. doi: 10.1001/archopht.1993.01090120037015. [DOI] [PubMed] [Google Scholar]
- 4.McCord C, Chowdhury Q. A cost effective small hospital in Bangladesh: what it can mean for emergency obstetric care. Int J Gynaecol Obstet. 2003;81:83–92. doi: 10.1016/s0020-7292(03)00072-9. [DOI] [PubMed] [Google Scholar]
- 5.Farmer PE, Kim JY. Surgery and global health: a view from beyond the OR. World J Surg. 2008;32:533–36. doi: 10.1007/s00268-008-9525-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Global Initiative for Emergency and Essential Surgical Care. Geneva: World Health Organization; 2014. [accessed Jan 27, 2015]. Available from: http://www.who.int/surgery/en/ [Google Scholar]
- 7.Meara JG, Leather AJM, Hagander L, et al. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. doi: 10.1016/j.surg.2015.02.009. (in press) [DOI] [PubMed] [Google Scholar]
- 8.Mock CN, Donkor P, Gawande A, et al. Disease Control Priorities. 3rd edn. Volume 1: essential surgery. Washington, DC: World Bank; (in press) [PubMed] [Google Scholar]
- 9.Jamison DT. Disease Control Priorities, 3rd edition: improving health and reducing poverty. Lancet. 2015 doi: 10.1016/S0140-6736(15)60097-6. published online Feb 5. [DOI] [PubMed] [Google Scholar]
- 10.Rose J, Chang DC, Weiser TG, Kassebaum NJ, Bickler SW. The role of surgery in global health: analysis of United States inpatient procedure frequency by condition using the Global Burden of Disease 2010 framework. PLoS One. 2014;9:e89693. doi: 10.1371/journal.pone.0089693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mock C, Cherian M, Juillard C, et al. Developing priorities for addressing surgical conditions globally: furthering the link between surgery and public health policy. World J Surg. 2010;34:381–85. doi: 10.1007/s00268-009-0263-4. [DOI] [PubMed] [Google Scholar]
- 12.Luboga S, Macfarlane SB, von Schreeb J, et al. the Bellagio Essential Surgery Group (BESG) Increasing access to surgical services in sub-saharan Africa: priorities for national and international agencies recommended by the Bellagio Essential Surgery Group. PLoS Med. 2009;6:e1000200. doi: 10.1371/journal.pmed.1000200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mock CN, Lormand JD, Goosen J, Joshipura M, Peden M. Guidelines for essential trauma care. Geneva: World Health Organization; 2004. [Google Scholar]
- 14.Bickler S, Weiser T, Kassenbaum N, et al. Chapter 2. Global burden of surgical conditions. In: Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN, editors. Disease Control Priorities. Volume 1: essential surgery. Washington, DC: World Bank; (in press) [Google Scholar]
- 15.Laxminarayan R, Mills AJ, Breman JG, et al. Advancement of global health: key messages from the Disease Control Priorities Project. Lancet. 2006;367:1193–208. doi: 10.1016/S0140-6736(06)68440-7. [DOI] [PubMed] [Google Scholar]
- 16.Haile T. Debas, Richard Gosselin, Colin McCord, Amardeep Thind. Surgery. In: Jamison D, Breman J, Measham A, et al., editors. Disease control priorities in developing countries. 2nd edn. New York, NY: Oxford University Press; 2006. pp. 1245–60. [Google Scholar]
- 17.Groen RS, Samai M, Stewart KA, et al. Untreated surgical conditions in Sierra Leone: a cluster randomised, cross-sectional, countrywide survey. Lancet. 2012;380:1082–87. doi: 10.1016/S0140-6736(12)61081-2. [DOI] [PubMed] [Google Scholar]
- 18.Prinja S, Nandi A, Horton S, Levin C, Olson Z, Laxminarayan R. Chapter 18. Costs, effectiveness, and cost-effectiveness of selected surgical procedures and platforms: a summary. In: Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN, editors. Disease Control Priorities. 3rd edn. Volume 1: essential surgery. Washington, DC: World Bank; (in press) [PubMed] [Google Scholar]
- 19.Grimes CE, Henry JA, Maraka J, Mkandawire NC, Cotton M. Cost-effectiveness of surgery in low- and middle-income countries: a systematic review. World J Surg. 2014;38:252–63. doi: 10.1007/s00268-013-2243-y. [DOI] [PubMed] [Google Scholar]
- 20.Chao TE, Sharma K, Mandigo M, et al. Cost-effectiveness of surgery and its policy implications for global health: a systematic review and analysis. Lancet Glob Health. 2014;2:e334–45. doi: 10.1016/S2214-109X(14)70213-X. [DOI] [PubMed] [Google Scholar]
- 21.Alkire B, Vincent J, Meara J. Chapter 21. Benefit-cost analysis for selected surgical interventions in low and middle income countries. In: Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN, editors. Disease Control Priorities. 3rd edn. Volume 1: essential surgery. Washington, DC; World Bank: (in press) [Google Scholar]
- 22.Jamison DT, Jha P, Laxminarayan R, Ord T. Infectious disease, injury, and reproductive health. In: Lomborg B, editor. Global problems, smart solutions: costs and benefits. Cambridge: Cambridge University Press for Copenhagen Consensus Center; 2013. [Google Scholar]
- 23.Jamison DT, Summers LH, Alleyne G, et al. Global health 2035: a world converging within a generation. Lancet. 2013;382:1898–955. doi: 10.1016/S0140-6736(13)62105-4. [DOI] [PubMed] [Google Scholar]
- 24.Kydland F, Mundell R, Schelling T, Smith V, Stokey N. Expert panel ranking. In: Lomborg B, editor. Global problems, smart solutions: costs and benefits. Cambridge: Cambridge University Press; 2013. pp. 701–16. [Google Scholar]
- 25.Shrime M, Verguet S, Johansson KA, Desalegne D, Jamison DT, Kruk ME. Chapter 19. Task-sharing or public finance for the expansion of surgical access in rural Ethiopia: an extended cost-effectiveness analysis. In: Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN, editors. Disease Control Priorities. Volume 1: essential surgery. Washington, DC: World Bank; (in press) [Google Scholar]
- 26.Gosselin RA, Heitto M. Cost-effectiveness of a district trauma hospital in Battambang, Cambodia. World J Surg. 2008;32:2450–53. doi: 10.1007/s00268-008-9708-4. [DOI] [PubMed] [Google Scholar]
- 27.Gosselin RA, Maldonado A, Elder G. Comparative cost-effectiveness analysis of two MSF surgical trauma centers. World J Surg. 2010;34:415–19. doi: 10.1007/s00268-009-0230-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gosselin RA, Thind A, Bellardinelli A. Cost/DALY averted in a small hospital in Sierra Leone: what is the relative contribution of different services? World J Surg. 2006;30:505–11. doi: 10.1007/s00268-005-0609-5. [DOI] [PubMed] [Google Scholar]
- 29.Shrime M, Sleemi A, Ravilla T. Chapter 13. Specialized surgical platforms. In: Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN, editors. Disease Control Priorities. 3rd edn. Volume 1: essential surgery. Washington, DC: World Bank; (in press) [Google Scholar]
- 30.Mock CN, Jurkovich GJ, nii-Amon-Kotei D, Arreola-Risa C, Maier RV. Trauma mortality patterns in three nations at different economic levels: implications for global trauma system development. J Trauma. 1998;44:804–12. doi: 10.1097/00005373-199805000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Thind A, Hsia R, Mabweijano J, Hicks ER, Zakariah A, Mock C. Chapter 14. Prehospital and emergency care. In: Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN, editors. Disease Control Priorities. 3rd edn. Volume 1: essential surgery. Washington, DC: World Bank; (in press) [Google Scholar]
- 32.Weiser TG, Regenbogen SE, Thompson KD, et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet. 2008;372:139–44. doi: 10.1016/S0140-6736(08)60878-8. [DOI] [PubMed] [Google Scholar]
- 33.Hoyler M, Finlayson SR, McClain CD, Meara JG, Hagander L. Shortage of doctors, shortage of data: a review of the global surgery, obstetrics, and anesthesia workforce literature. World J Surg. 2014;38:269–80. doi: 10.1007/s00268-013-2324-y. [DOI] [PubMed] [Google Scholar]
- 34.Stewart B, Khanduri P, McCord C, et al. Global disease burden of conditions requiring emergency surgery. Br J Surg. 2014;101:e9–22. doi: 10.1002/bjs.9329. [DOI] [PubMed] [Google Scholar]
- 35.McCord C, Mbaruku G, Pereira C, Nzabuhakwa C, Bergstrom S. The quality of emergency obstetrical surgery by assistant medical officers in Tanzanian district hospitals. Health Aff (Millwood) 2009;28:w876–85. doi: 10.1377/hlthaff.28.5.w876. [DOI] [PubMed] [Google Scholar]
- 36.Pereira C, Mbaruku G, Nzabuhakwa C, Bergström S, McCord C. Emergency obstetric surgery by non-physician clinicians in Tanzania. Int J Gynaecol Obstet. 2011;114:180–83. doi: 10.1016/j.ijgo.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 37.Kruk ME, Pereira C, Vaz F, Bergström S, Galea S. Economic evaluation of surgically trained assistant medical officers in performing major obstetric surgery in Mozambique. BJOG. 2007;114:1253–60. doi: 10.1111/j.1471-0528.2007.01443.x. [DOI] [PubMed] [Google Scholar]
- 38.Hounton SH, Newlands D, Meda N, De Brouwere V. A cost-effectiveness study of caesarean-section deliveries by clinical officers, general practitioners and obstetricians in Burkina Faso. Hum Resour Health. 2009;7:34. doi: 10.1186/1478-4491-7-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bergström S, McPake B, Pereira C, Dovlo D. Chapter 17. Workforce innovations to expand the capacity for surgical services. In: Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN, editors. Disease Control Priorities. 3rd edn. Volume 1: essential surgery. Washington, DC: World Bank; (in press) [Google Scholar]
- 40.Essential trauma care project. Geneva: World Health Organization; 2014. [accessed March 23, 2014]. http://www.who.int/violence_injury_prevention/services/traumacare/en/ [Google Scholar]
- 41.Mock C, Nguyen S, Quansah R, Arreola-Risa C, Viradia R, Joshipura M. Evaluation of trauma care capabilities in four countries using the WHO-IATSIC Guidelines for Essential Trauma Care. World J Surg. 2006;30:946–56. doi: 10.1007/s00268-005-0768-4. [DOI] [PubMed] [Google Scholar]
- 42.Belle J, Cohen H, Shindo N, et al. Influenza preparedness in low-resource settings: a look at oxygen delivery in 12 African countries. J Infect Dev Ctries. 2010;4:419–24. doi: 10.3855/jidc.859. [DOI] [PubMed] [Google Scholar]
- 43.Kushner AL, Cherian MN, Noel L, Spiegel DA, Groth S, Etienne C. Addressing the Millennium Development Goals from a surgical perspective: essential surgery and anesthesia in 8 low- and middle-income countries. Arch Surg. 2010;145:154–59. doi: 10.1001/archsurg.2009.263. [DOI] [PubMed] [Google Scholar]
- 44.Ologunde R, Vogel J, Cherian M, Sbaiti M, Merialdi M, Yeats J. Assessment of cesarean delivery availability in 26 low- and middle-income countries: a cross-sectional study. Am J Obstet Gynecol. 2014;5:504. e1–504. e12. doi: 10.1016/j.ajog.2014.05.022. [DOI] [PubMed] [Google Scholar]
- 45.Vo D, Cherian M, Bianchi S, et al. Anesthesia capacity in 22 low- and middle-income countries. J Anesth Clin Res. 2012;3:207. [Google Scholar]
- 46.Surgical care at the district hospital. Geneva: World Health Organization; 2003. [accessed Nov 1, 2014]. http://www.who.int/surgery/publications/scdh_manual/en/ [Google Scholar]
- 47.Mock C, Juillard C, Joshipura M, Goosen J. Strengthening care for the injured: success stories and lessons learned from around the world. Geneva: World Health Organization; 2010. [Google Scholar]
- 48.Son NT, Mock C. Improvements in trauma care capabilities in Vietnam through use of the WHO-IATSIC Guidelines for Essential Trauma Care. Int J Inj Contr Saf Promot. 2006;13:125–27. doi: 10.1080/17457300500310152. [DOI] [PubMed] [Google Scholar]
- 49.Local production and technology transfer to increase access to medical devices. Geneva: World Health Organization; 2012. [accessed Jan 27, 2015]. www.who.int/medical_devices/1240EHT_final.pdf. [Google Scholar]
- 50.Local production for access to medical products. Geneva: World Health Organization; 2011. [accessed Jan 27, 2015]. http://www.who.int/phi/publications/Local_Production_Policy_Framework.pdf. [Google Scholar]
- 51.Schecter W, Adhikari S. Chapter 20. Global surgery and poverty. In: Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, CN M, editors. Disease Control Priorities. 3rd edn. Volume 1: essential surgery. Washington, DC: World Bank; (in press) [Google Scholar]
- 52.Högberg U. Maternal deaths related to cesarean section in Sweden, 1951–1980. Acta Obstet Gynecol Scand. 1989;68:351–57. doi: 10.3109/00016348909028671. [DOI] [PubMed] [Google Scholar]
- 53.Weiser T, Gawande A. Chapter 16. Excess surgical mortality: strategies for improving quality of care. In: Debas HT, Gawande A, Jamison DT, Kruk ME, Mock CN, editors. Disease Control Priorities. 3rd edn. Volume 1: essential surgery. Washington, DC: World Bank; (in press) [Google Scholar]
- 54.Bainbridge D, Martin J, Arango M, Cheng D, for the Evidence-based Peri-operative Clinical Outcomes Research (EPiCOR) Group Perioperative and anaesthetic-related mortality in developed and developing countries: a systematic review and meta-analysis. Lancet. 2012;380:1075–81. doi: 10.1016/S0140-6736(12)60990-8. [DOI] [PubMed] [Google Scholar]
- 55.Haynes AB, Weiser TG, Berry WR, et al. the Safe Surgery Saves Lives Study Group A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360:491–99. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 56.WHO surgical safety checklist and implementation manual. Geneva: World Health Organization; 2008. [accessed Jan 27, 2015]. http://www.who.int/patientsafety/safesurgery/tools_resources/SSSL_Checklist_finalJun08.pdf?ua=1. [Google Scholar]
- 57.Eichhorn JH, Cooper JB, Cullen DJ, Maier WR, Philip JH, Seeman RG. Standards for patient monitoring during anesthesia at Harvard Medical School. JAMA. 1986;256:1017–20. [PubMed] [Google Scholar]
- 58.Kwok AC, Funk LM, Baltaga R, et al. Implementation of the World Health Organization surgical safety checklist, including introduction of pulse oximetry, in a resource-limited setting. Ann Surg. 2013;257:633–39. doi: 10.1097/SLA.0b013e3182777fa4. [DOI] [PubMed] [Google Scholar]
- 59.Burn SL, Chilton PJ, Gawande AA, Lilford RJ. Peri-operative pulse oximetry in low-income countries: a cost-effectiveness analysis. Bull World Health Organ. 2014;92:858–67. doi: 10.2471/BLT.14.137315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Juillard CJ, Mock C, Goosen J, Joshipura M, Civil I. Establishing the evidence base for trauma quality improvement: a collaborative WHO-IATSIC review. World J Surg. 2009;33:1075–86. doi: 10.1007/s00268-009-9959-8. [DOI] [PubMed] [Google Scholar]
- 61.McQueen KA. Editorial perspective: global surgery: measuring the impact. World J Surg. 2013;37:2505–06. doi: 10.1007/s00268-013-2198-z. [DOI] [PubMed] [Google Scholar]
- 62.Weiser TG, Makary MA, Haynes AB, Dziekan G, Berry WR, Gawande AA, for the Safe Surgery Saves Lives Measurement and Study Groups Standardised metrics for global surgical surveillance. Lancet. 2009;374:1113–17. doi: 10.1016/S0140-6736(09)61161-2. [DOI] [PubMed] [Google Scholar]
- 63.World Health Report 2008: Primary health care—now more than ever. Geneva: World Health Organization; 2008. [accessed Jan 27, 2015]. http://www.who.int/whr/2008/en/ [Google Scholar]
- 64.Kruk ME, Rabkin M, Grépin KA, et al. ‘Big push’ to reduce maternal mortality in Uganda and Zambia enhanced health systems but lacked a sustainability plan. Health Aff (Millwood) 2014;33:1058–66. doi: 10.1377/hlthaff.2013.0637. [DOI] [PubMed] [Google Scholar]
- 65.Yaffee AQ, Whiteside LK, Oteng RA, et al. Bypassing proximal health care facilities for acute care: a survey of patients in a Ghanaian Accident and Emergency Centre. Trop Med Int Health. 2012;17:775–81. doi: 10.1111/j.1365-3156.2012.02984.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kruk ME, Hermosilla S, Larson E, Mbaruku GM. Bypassing primary care clinics for childbirth: a cross-sectional study in the Pwani region, United Republic of Tanzania. Bull World Health Organ. 2014;92:246–53. doi: 10.2471/BLT.13.126417. [DOI] [PMC free article] [PubMed] [Google Scholar]