Abstract
PURPOSE
Worldwide, Indigenous people often have disproportionally worse health and lower life expectancy than their non-Indigenous counterparts. Despite the impact of cancer on life expectancy, little is known about the burden of cancer for Indigenous people primarily because of the paucity of data. We investigated the collection and reporting of Indigenous status information among a global sample of population-based cancer registries (PBCRs).
PARTICIPANTS AND METHODS
An online survey was e-mailed to eligible registries using set inclusion criteria. Respondents were asked questions on the collection, reporting, and quality assessment of Indigenous status in their registers.
RESULTS
Eighty-three PBCRs from 25 countries were included. Of these, 66% reported that their registry collected Indigenous status data, although the quality of this variable had been assessed in less than half in terms of completeness (38%) and accuracy (47%). Two thirds of PBCRs who collected Indigenous status data (67%), from nine of 25 countries responded that cancer statistics for Indigenous people were reported using registry data. Key barriers to the collection of Indigenous status information included the lack of data collection at the point of care (79%), lack of transfer of Indigenous status to the cancer registry (46%), inadequate information systems (43%), and legislative limitations (32%). Important variations existed among world regions, although the lack of Indigenous status data collection at the point of care was commonly reported across all regions.
CONCLUSION
High-quality data collection is lacking for Indigenous peoples in many countries. To ensure the design and implementation of cancer control activities required to reduce disparities for Indigenous populations, health information systems, including cancer registries, need to be strengthened, and this must be done in dialogue with Indigenous leaders.
INTRODUCTION
The global burden of cancer is predicted to rise with the aging and growth of the world’s population alongside changing risk patterns.1 Subsequently, cancer surveillance systems are becoming increasingly critical for cancer control. Despite Indigenous peoples representing 5% of the world population in more than 70 countries,2,3 data related to Indigenous people are scarce. The rights of Indigenous peoples have become a focus of the United Nations, including their right to health and well-being4 and to be counted in population and health data collections.5 Evidence from Australia, New Zealand, Canada, and the United States demonstrates that cancer is a leading cause of death among Indigenous people,6-9 and Indigenous people are more likely than non-Indigenous people to be diagnosed with and die as a result of the most preventable cancers.10-14 Little has been published on cancer disparities between Indigenous and non-Indigenous people elsewhere. With cancer an increasingly major health priority for Indigenous populations, targeted, comprehensive, and adequately resourced cancer control action is imperative.15
Reliable and accurate cancer surveillance is critical for developing, monitoring, and evaluating cancer control strategies, and population-based cancer registries (PBCRs) play a central role.16 Such data also are necessary to monitor cancer disparities between populations.17,18 Internationally, a number of collaborative activities have occurred to improve the health measurement of Indigenous peoples17,19 in a way that respects Indigenous data sovereignty20 and Indigenous peoples’ right to count and be counted in official statistics.17 Few PBCRs worldwide are believed to collect Indigenous status information,21,22 although such figures have not been assessed. Thus, an assessment of the capacity of PBCRs to conduct cancer surveillance for Indigenous peoples is overdue and is a critical step in gaining a comprehensive picture of the burden of cancer among Indigenous populations and enabling the monitoring of trends over time. We report the practices in collection, recording, and reporting of Indigenous status information by PBCRs and examine the variation across world regions to gain insight into the perceived barriers to these activities.
CONTEXT
Key Objective
Assess the extent to which cancer registries collect and report data for Indigenous populations and gain insight into perceived barriers and solutions of such data collection.
Knowledge Generated
There is a lack of high-quality cancer data for many Indigenous populations, which is perceived to be largely due to health care staff not asking patients how they identify at the point of care. Other barriers include an inability of information systems to capture and transfer required information through the cancer surveillance system, prohibitive legislation, and a lack of societal-level recognition of Indigenous peoples.
Relevance
Reliable and accurate data are critical for identifying and monitoring disparities in cancer outcomes within populations and developing and implementing targeted cancer control actions. The development and implementation of any strategies to overcome barriers to the collection of Indigenous status information should be done within Indigenous data governance frameworks and in dialogue with Indigenous leaders, and support from international cancer control agencies may be required.
PARTICIPANTS AND METHODS
Design and Participants
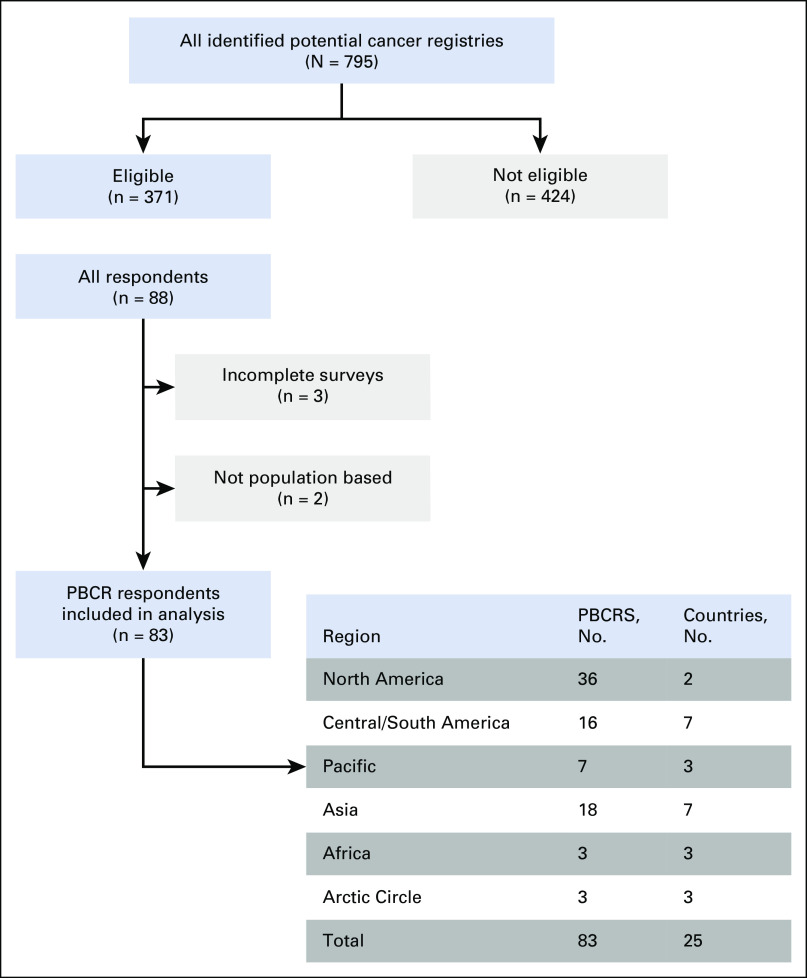
A rapid review of cancer registry practices for collecting and reporting Indigenous status information was conducted through an online cross-sectional survey from February to June 2019. A list of world population–based and nonpopulation-based cancer registries were compiled using the International Association for Cancer Registries online member list (n = 539), complemented by a search of publications of the International Agency for Research on Cancer, such as GLOBOCAN reports, and suggestions from the project team (n = 256). From the initial list of 795 organizations, duplicate records (n = 7), registries from countries not listed in the 2018 and 2019 Indigenous World yearbooks23,24 (n = 324), tumor- or age-specific registries (n = 31), and registries without current contact information (n = 61) were excluded. In total, 371 registries were invited to participate (Fig 1). The Indigenous World yearbooks list 69 countries with Indigenous populations; we identified registries in 61 of these, and eligible registries were invited from across 54 countries.
FIG 1.
Eligibility and recruitment process. PBCR, population-based cancer registry.
Topics of interest were determined by the research team, which is experienced in both Indigenous health and cancer registry data collection. Questions were formulated, structured using branch logic and trialed by the research team members for face validity and readability. Topics were kept to a minimum to reduce the burden for registry staff. Up to 19 questions were asked dependent on respondent’s previous answers. The survey took approximately 10 to 20 minutes to complete.
The questions focused on collection of Indigenous status, reasons for noncollection, methods and sources for collection, the assessment of the quality and/or completeness of Indigenous status information, and whether Indigenous cancer statistics had been reported. To avoid confusion over the two concepts, we referred to collection as entailing both collection (capture of data) and recording (documenting of data) of Indigenous status information. Open-ended questions sought to gain additional insight into the barriers to data collection and reporting.
The survey was administered online using the data collection software program REDCap25 and in two waves (February to March and May to June 2019) because the updated 2019 Indigenous World yearbook became available during the first wave. For both waves, an e-mail invitation to complete the survey was sent to all registries. Where e-mails were undeliverable, all attempts were made to identify updated contact information and resend the e-mail. Two reminders were automatically sent to registries that had not yet responded, approximately 1 week apart. Consenting respondents could download the survey and return through e-mail, complete it online, or complete it through telephone, although no one took the telephone option. Online results were automatically stored in REDCap, and e-mailed survey responses were entered manually.
Respondents were advised that they could stop the survey at any time, pause and resume later, or withdraw from the study. Ethical approval was obtained from the International Agency for Research on Cancer Ethics Committee (IEC No. 18-22) and the Human Research Ethics Committee of the Northern Territory Department of Health and Menzies School of Health Research (HREC No. 2019-3326).
Analysis
Data were imported from REDCap to Stata 14.25,26 Frequencies and proportions were calculated for questions with ordinal or nominal response categories. Proportions were rounded to the nearest whole number, given the small numbers within each region. Common and divergent themes that arose from the qualitative responses to open-ended questions were identified through thematic analysis by the lead author and discussed with a second author to obtain consensus.
RESULTS
PBCR Respondents
Of the 371 cancer registries invited, 88 responded (24% response rate) from 27 countries (50% of the 54 countries invited). Three registries with high levels of missing data were excluded. Of the remaining 85 registers, 18 were national, 65 subnational (55 state/province based, 10 city, district, or region based), and two were hospital based. The two nonpopulation-based registers were excluded to increase the homogeneity of the sample, which left 83 PBCRs from 25 countries (Fig 1).
Collection of Indigenous Status
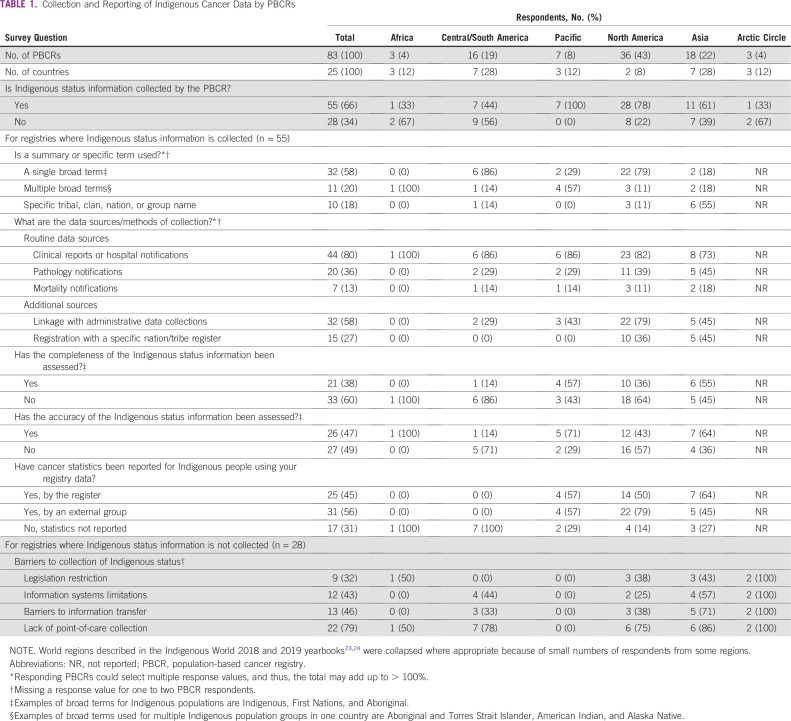
Key findings are listed by region in Table 1. In total, 55 PBCRs (66%) reported that they collect Indigenous status information, with the lowest proportion in Africa and Central and South America. Similarly, 64% of included countries had at least one participating PBCR that routinely collected Indigenous status information (n = 16). Broad terms were most commonly used to identify Indigenous populations, and specific tribal names were used by 18% of PBCRs, most commonly by Asian registries. Proxy measures of identification were described by some, including religion, geographical area, registration status, or reservation residence. The primary sources of Indigenous status information were clinical and hospital notifications (80%), pathology notifications (36%), and data linkages (58%). Linkage to specific tribal registers was used mostly in India and the United States.
TABLE 1.
Collection and Reporting of Indigenous Cancer Data by PBCRs
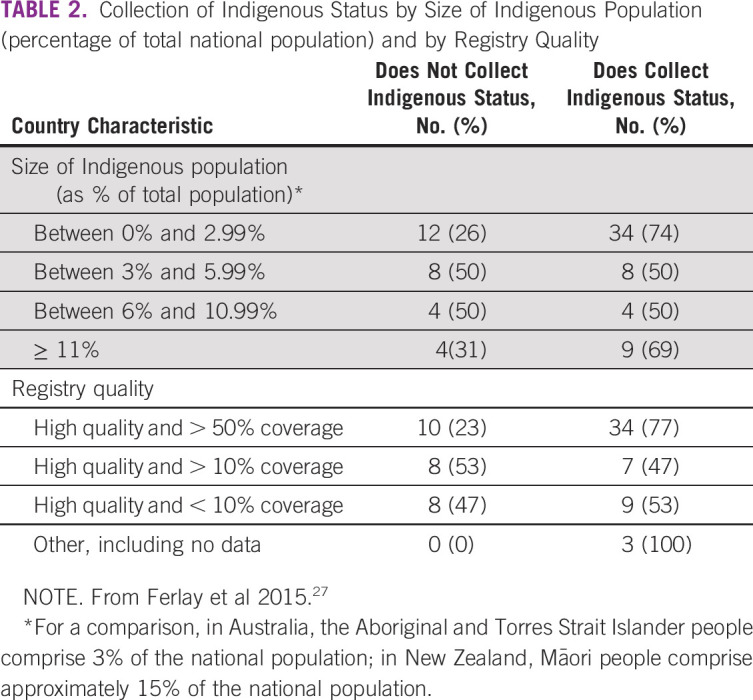
Less than half of PBCRs that captured Indigenous status were aware of completeness (38%) or accuracy (47%) assessments of these data. Such assessments were more commonly reported among PBCRs in the Pacific and Asia (Table1). In response to open-ended questions, data linkage commonly arose as a means of verifying the completeness and/or accuracy of the Indigenous status variable in the cancer registry. One PBCR described the need for best practice business rules to guide the assessment of data completeness and accuracy, especially when multiple sources of Indigenous status were available. Another noted that accurate ascertainment of Indigenous status using linked data is challenging but that continued improvement is ongoing through close collaboration with Indigenous groups. There seemed to be little relation between collecting Indigenous status and the relative size of the Indigenous population; however, participating PBCRs with high-quality data and broad population coverage seemed to be more likely to capture this information than those with lower data quality (Table 2).
TABLE 2.
Collection of Indigenous Status by Size of Indigenous Population (percentage of total national population) and by Registry Quality
Barriers to the Collection of Indigenous Status
In total, 28 PBCRs (34%) advised that Indigenous status information was not collected by their register (Table 1). The primary barriers were information not being routinely collected at the point of care (79%), information not being transferred through the cancer reporting pathway (46%), incapacity of the registry’s information system to collect or store these data (43%), and lack of legislative support (32%). For all regions, the lack of Indigenous status collection at the point of care was the most commonly identified barrier (Table 1). PBCRs were given the opportunity, through an open-ended question, to identify additional perceived barriers (Table 3).
TABLE 3.
Additional Perceived Reasons for Noncollection of Indigenous Status Information
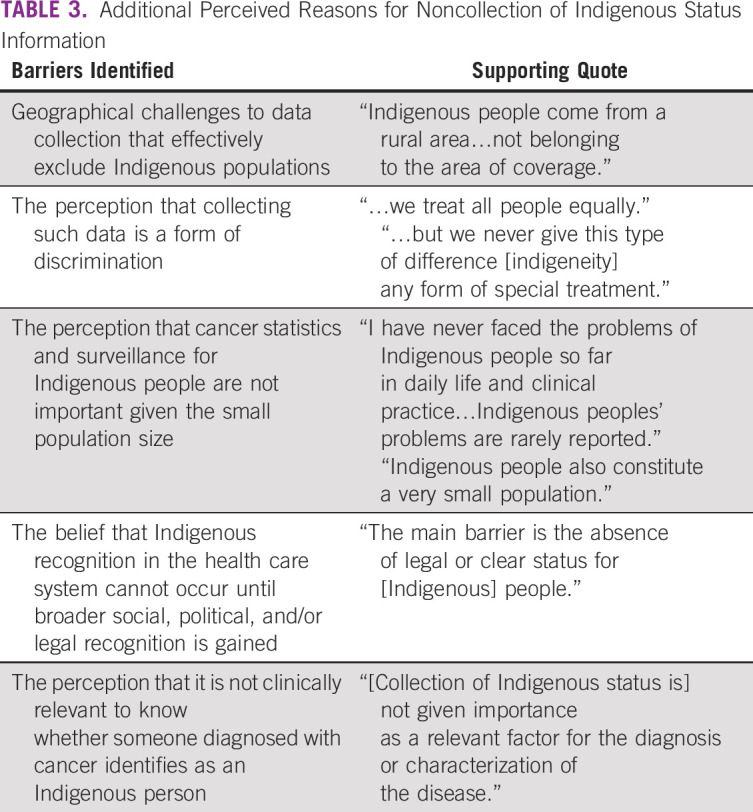
Many PBCRs provided suggestions on how to overcome the key barriers to the collection of Indigenous status information in their register. These focused on societal-level (eg, obtaining political support to increase the recognition of Indigenous peoples, changing legislation to allow health services to collect this information at point of care), system-level (eg, developing and implementing guidelines to ensure and standardize the collection and reporting of Indigenous status information, developing and implementing information systems that can capture and transfer Indigenous status information), and professional- and patient-level (eg, education for health care professionals, administration staff, and patients on the importance of asking for, recording, and transferring Indigenous status information) approaches. Many PBCRs recognized that multiple approaches would be required to enable reporting of cancer statistics for Indigenous populations.
Reporting of Cancer Statistics for Indigenous Peoples
Of the PBCRs that collected Indigenous status, more than half (69%) advised that cancer statistics for Indigenous people were produced using their data (Table 1). Nine countries from the Pacific, North America, and Asia had at least one registry that reported routine collection and reporting of Indigenous cancer data. For some PBCRs, Indigenous statistics often were aggregated by year or jurisdiction to overcome the small population numbers and patients with cancer. In addition, some reported that although they collected Indigenous status data, they did not report it for various reasons, including poor data quality, inadequate denominator data to allow the calculation of rates, lack of interest and/or funds from national health authorities to produce such reports, and concerns about privacy and potential discrimination through the identification of Indigenous people in population-based data.
While several PBCRs recognized the need to collect and report on Indigenous cancer statistics, these registers reported feeling disempowered to do so and advocated for more support to conduct the required analyses to produce such reports. Others acknowledged that decisions about the way in which data are collected and reported required leadership from and collaboration with Indigenous people, communities, and health organizations, and how this is done is likely to vary by community.
DISCUSSION
This study provides a comprehensive overview of the collection and reporting practices of Indigenous status information in cancer registries worldwide. Although two thirds of PBCRs collect Indigenous status, substantial identification gaps persist for some registries and countries. None of the registries from Africa, Central and South America, and the Nordic countries said that they routinely collect and report data for Indigenous populations. PBCRs identified a range of barriers to including Indigenous status in their data sets and proposed multiple and complementary approaches to overcome these challenges.
Of note, although some PBCRs believed that their Indigenous population was too small to report on, others suggested the aggregation of multiple years or jurisdictions to overcome this. The size of the Indigenous population, in terms of the proportion of the total country population, did not seem to be related to the PBCR’s propensity to collect Indigenous status. While small population size and geographical isolation are characteristic of many Indigenous populations globally and thus present a challenge for high-quality statistical analysis, methods for overcoming these concerns exist.28
Legislation was perceived to be a barrier to the collection of Indigenous status by 32% of respondents, and although not the most common reported barrier, it is potentially the most critical. In some countries, including the Nordic countries (Denmark, Finland, Norway, and Sweden), Japan, and New Caledonia, Indigenous status information cannot be collected by law.5 However, some may use geographical or religion-based proxies to enable cancer surveillance for Indigenous populations. In the survey, concern about identification leading to discrimination or a privacy breach emerged. It is important that registries balance the right to privacy with the right to be counted.17 In other countries, legislative changes are required to mandate the routine collection of this information, which may improve the quality of such data. For example, a US study found consistently high levels of completeness for ethnicity data in hospital records in states that have a legal reporting requirement (93% to 100% complete) compared with those that do not (23% to 100%).29
The most common barrier identified was the lack of collection and recording of Indigenous status information at the point of care (79%). Education to improve the capability of staff to ask for Indigenous identification and record this was identified as an important step in capturing relevant information. In Australia, for example, to improve the completeness and accuracy of Indigenous status, hospital and other health-related staff have been trained to use a Standard Indigenous Question,30 which was introduced by the Australian Bureau of Statistics in 1996 and currently is used for census data collection (population denominator) and across Australia’s health, education, and criminal justice systems.20,31 The implementation of the Standard Indigenous Question has led to a notable improvement in the completeness and accuracy of these data. The 2017 national cancer report initially estimated that 1,189 Indigenous Australians had been diagnosed with cancer during 2008 to 2012; this estimate was revised in 2019 to 1,549 in the same time period using an improved Indigenous status variable.32
PBCRs identified the need for enhanced information systems across the cancer surveillance system that can capture and transfer Indigenous status information from general practices to pathology laboratories and cancer registries. Implementation of such systems would require financial investment. Initiatives to improve point-of-care collection of Indigenous status would require collaboration with practice managers, software vendors, and national health authorities and would need investment in staff capacity building to ensure the effective use of new systems.
The development and capacity building needs of cancer registries will vary among countries dependent on the current and historical sociopolitical recognition of Indigenous people,5 legislation around collection and reporting, capability and capacity of staff at the point of care to ask for Indigenous status, and ability of information systems to record and transfer this information to the cancer registry. Here, international agencies or associations, such as the International Association of Cancer Registries,33 may prove essential for the strategic development of tools, guidelines, educational materials, advocacy, and networks for better collection of Indigenous status within registries. The Global Initiative of Cancer Registry development,34 which aims to support local cancer actions and ensure improvements in cancer data, may well promote the expansion of cancer registry data collection to include Indigenous status. Importantly, Indigenous leadership and governance can ensure the appropriate and ethical collection and use of data to support Indigenous health, improve health systems, and promote opportunities for Indigenous people to meaningfully engage in all aspects of data collection and reporting for their community,21,35,36 which will inextricably link data sovereignty to self-determination.20
From some PBCRs, data linkage was used as a means to overcome the lack of Indigenous status data in the registry. Linkage to specific tribal registries may allow more nuanced epidemiologic investigations of cancer trends and better informed cancer policies. Integrated registry systems, which use ongoing linkages, may provide an efficient method of cancer surveillance for Indigenous peoples and other minority populations. However, Indigenous people have the right to choose when and to whom they identify, and data linkage practices should be devised by or in collaboration with Indigenous leaders and communities. Data linkage also was suggested as a means to assess the quality of the Indigenous status variable used by the cancer registry, as has been done before.37,38 Even though the right to self-identify in the health care system is an important element of self-determination and adopted as best practice in increasingly more countries, it can create a challenge to the reporting of cancer statistics for Indigenous people.20,28 The propensity to identify as Indigenous may vary over time and across settings, which can affect the reliability of the Indigenous status measure.29,30 In Australia, where Indigenous status information is largely drawn from hospital separations data, best-practice algorithms have been derived to established reliable cancer data for Indigenous Australians.39 Data linkage also may overcome the discordance in how numerator and denominator data are collected for Indigenous people.15,22,30
This study provides evidence on the routine collection and reporting of Indigenous status information by a global sample of cancer registries. The findings may inform the development or strengthening of guidelines for these activities. Regional variations in the barriers to collection and reporting highlight the need for tailored guidelines and mechanisms to achieve the aim of improved Indigenous identification in cancer data. We acknowledge that respondents from the PBCRs offered their personal views, which may not reflect the official view or practices of the cancer registry. In addition, future research should include in-depth interviews with representatives across the cancer data system to gain a richer understanding of the point-of-care and information transfer barriers and potential solutions. Our response rate was low (24%), although encouragingly, at least one registry from half of the included countries responded. The response rate was particularly low in Africa and notably large in North America, which in part is a reflection of the large number of state and province-based PBCRs in the United States and Canada. It is plausible that registries may have been more inclined to participate if they collected Indigenous status and/or believed that this was important for their population. As such, we may have overestimated the number of registries that collect this information.
In conclusion, few countries seem to routinely collect and report cancer data for Indigenous peoples. Disaggregation of health and well-being indicators by Indigenous status is important to highlight within-country inequalities and to inform priority-driven policy.5 Given that a core pledge of the Sustainable Development Goals is to leave no one behind, it is fundamental that cancer registries are supported to collect and report such data.35,40
Clear variations exist across world regions in the extent to which Indigenous status is collected and reported, as were the priorities to overcome barriers to these activities. To support registries in collecting this information, locally tailored strategies may be required alongside discussions to raise awareness of the importance of Indigenous cancer statistics. Any approaches to improve the collection and reporting of cancer data for Indigenous populations must be done within Indigenous data governance frameworks and in collaboration with Indigenous communities and leaders.
ACKNOWLEDGMENT
Where authors are identified as personnel of the International Agency for Research on Cancer/WHO, the authors alone are responsible for the views expressed in this article and do not necessarily represent the decisions, policy, or views of the International Agency for Research on Cancer/WHO.
Footnotes
Supported by the National Health and Medical Research Council (NHMRC)–funded Centre of Research Excellence in Targeted Approaches to Improve Cancer Services for Aboriginal and Torres Strait Islander Australians (TACTICS; #1153027). The views expressed in this publication are those of the authors and do not reflect the views of the NHMRC. A.D. is funded by a Menzies Early Career Support Fellowship. L.J.W. was supported by an NHMRC Early Career Fellowship (#1142035), as was G.G. (#1105399).
AUTHOR CONTRIBUTIONS
Conception and design: Abbey Diaz, Isabelle Soerjomataram, Suzanne Moore, Lisa J. Whop, Freddie Bray, Gail Garvey
Collection and assembly of data: Abbey Diaz, Hana Hoberg, Gail Garvey
Data analysis and interpretation: Abbey Diaz, Isabelle Soerjomataram, Suzanne Moore, Lisa J. Whop, Freddie Bray, Gail Garvey
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jgo/site/misc/authors.html.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
No potential conflicts of interest were reported.
REFERENCES
- 1.Brawley OW. Avoidable cancer deaths globally. CA Cancer J Clin. 2011;61:67–68. doi: 10.3322/caac.20108. [DOI] [PubMed] [Google Scholar]
- 2.The World Bank Indigenous Peoples. 2019 https://www.worldbank.org/en/topic/indigenouspeoples
- 3. United Nations Department of Economic and Social Affairs: State of the World’s Indigenous Peoples, New York, NY, United Nations, 2015.
- 4. United Nations: United Nations Declaration on the Rights of Indigenous Peoples. New York, NY, United Nations Publications, 2008. [Google Scholar]
- 5. Balestra C, Fleischer L: Diversity statistics in the OECD: How do OECD countries collect data on ethnic, racial and indigenous identity, OECD Statistics Working Papers, No. 2018/09, OECD Publishing, Paris, France, 2018 . [DOI]
- 6. New Zealand Ministry of Health: Major causes of death, 2018. https://www.health.govt.nz/our-work/populations/maori-health/tatau-kahukura-maori-health-statistics/nga-mana-hauora-tutohu-health-status-indicators/major-causes-death.
- 7. Australian Institute of Health and Welfare: The Health and Wellbeing of Australia’s Aboriginal and Torres Strait Islander peoples (2015 Cat. No.: IHW 147). Canberra, Australian Capital Territory, Australia, Australian Institute of Health and Welfare, 2015. [Google Scholar]
- 8. Health Canada: A Statistical Profile of the Health of First Nations in Canada: Vital Statistics for Atlantic and Western Canada, 2003-2007. Ottawa, Ontario, Canada, Health Canada, 2014. [Google Scholar]
- 9.Kochanek KD, Xu J, Murphy SL, et al. Deaths: Final data for 2009. Natl Vital Stat Rep. 2011;60:1–116. [PubMed] [Google Scholar]
- 10. Australian Institute of Health and Welfare: Cancer in Aboriginal & Torres Strait Islander People of Australia. Canberra, Australian Capital Territory, Australia, Australian Institute of Health and Welfare, 2018. [Google Scholar]
- 11.Mazereeuw MV, Withrow DR, Nishri ED, et al. Cancer incidence among First Nations adults in Canada: Follow-up of the 1991 Census Mortality Cohort (1992-2009) Can J Public Health. 2018;109:700–709. doi: 10.17269/s41997-018-0091-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moore SP, Antoni S, Colquhoun A, et al. Cancer incidence in indigenous people in Australia, New Zealand, Canada, and the USA: A comparative population-based study. Lancet Oncol. 2015;16:1483–1492. doi: 10.1016/S1470-2045(15)00232-6. [DOI] [PubMed] [Google Scholar]
- 13.Teng AM, Atkinson J, Disney G, et al. Ethnic inequalities in cancer incidence and mortality: Census-linked cohort studies with 87 million years of person-time follow-up. BMC Cancer. 2016;16:755. doi: 10.1186/s12885-016-2781-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Withrow DR, Pole JD, Nishri ED, et al. Cancer survival disparities between First Nation and non-Aboriginal adults in Canada: Follow-up of the 1991 Census Mortality Cohort. Cancer Epidemiol Biomarkers Prev. 2017;26:145–151. doi: 10.1158/1055-9965.EPI-16-0706. [DOI] [PubMed] [Google Scholar]
- 15.Sarfati D, Robson B. Equitable cancer control: Better data needed for indigenous people. Lancet Oncol. 2015;16:1442–1444. doi: 10.1016/S1470-2045(15)00295-8. [DOI] [PubMed] [Google Scholar]
- 16.Parkin DM. The role of cancer registries in cancer control. Int J Clin Oncol. 2008;13:102–111. doi: 10.1007/s10147-008-0762-6. [DOI] [PubMed] [Google Scholar]
- 17. Chino M, Ring I, Pluver LJ, et al: Improving health data for indigenous populations: The international group for indigenous health measurement. Stat J IAOS 35:15-21, 2019. [Google Scholar]
- 18. doi: 10.1016/S0140-6736(16)00345-7. Anderson I, Robson B, Connolly M, et al: Indigenous and tribal people’s health (the Lancet-Lowitja Institute Global Collaboration): A population study. Lancet 388:P131-P157, 2016. [DOI] [PubMed] [Google Scholar]
- 19.West K. Editorial. Stat J IAOS. 2019;35:1–3. [Google Scholar]
- 20. Griffiths K, Coleman C, Al-Yaman F, et al: The identification of Aboriginal and Torres Strait Islander people in official statistics and other data: Critical issues of international significance. Stat J IAOS 35:91-106, 2019. [Google Scholar]
- 21.Sarfati D, Robson B, Garvey G, et al. Improving the health of Indigenous people globally. Lancet Oncol. 2018;19:e276. doi: 10.1016/S1470-2045(18)30336-X. [DOI] [PubMed] [Google Scholar]
- 22.Sarfati D, Garvey G, Robson B, et al. Measuring cancer in indigenous populations. Ann Epidemiol. 2018;28:335–342. doi: 10.1016/j.annepidem.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 23. Jacquelin-Andersen P (ed): The Indigenous World 2018. Copenhagen, Denmark, International Work Group for Indigenous Affairs, 2018. [Google Scholar]
- 24. Berger DN (ed): The Indigenous World 2019. Copenhagen, Denmark, International Work Group for Indigenous Affairs, 2019. [Google Scholar]
- 25.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. StataCorp: Stata statistical software: Release 15. College Station, TX, StataCorp, 2017. [Google Scholar]
- 27.Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 28. Connolly M, Gallagher M, Hodge F, et al: Identification in a time of invisibility for American Indians and Alaska Natives in the United States. Stat J IAOS 35:71-89, 2019. [Google Scholar]
- 29. National Research Council (US) Panel on DHHS Collection of Race and Ethnicity Data: Improving Racial and Ethnic Data on Health: Report of a Workshop. Washington, DC, National Academies Press, 2003. [PubMed] [Google Scholar]
- 30.Madden R, Coleman C, Mashford-Pringle A, et al. Indigenous identification: Past, present, and a possible future. Stat J IAOS. 2019;35:23–27. [Google Scholar]
- 31. Australian Bureau of Statistics: 2077.0 - Census of Population and Housing: Understanding the Increase in Aboriginal and Torres Strait Islander Counts, 2016. Technical Note 1 - Aboriginal and Torres Strait Islander Status and the Census, 2018. https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/2077.0~2016~Main%20Features~Technical%20Note%201%20-%20Aboriginal%20and%20Torres%20Strait%20Islander%20Status%20and%20the%20Census~127.
- 32. Australian Institute of Health and Welfare: Cancer in Australia 2019 (Cancer Series No. 119; Cat. No.: CAN 123). Canberra, Australian Capital Territory, Australia, Australian Institute of Health and Welfare, 2019. [Google Scholar]
- 33. International Association of Cancer Registries (IACR): Welcome to IACR. http://www.iacr.com.fr.
- 34. International Agency for Research on Cancer; WHO: Global Initiative for Cancer Registry Development (GICR). http://gicr.iarc.fr.
- 35.Garvey G, Cunningham J. National cancer control plans. Lancet Oncol. 2018;19:e666. doi: 10.1016/S1470-2045(18)30834-9. [DOI] [PubMed] [Google Scholar]
- 36.Walker J, Lovett R, Kukutai T, et al. Indigenous health data and the path to healing. Lancet. 2017;390:2022–2023. doi: 10.1016/S0140-6736(17)32755-1. [DOI] [PubMed] [Google Scholar]
- 37.Espey DK, Wiggins CL, Jim MA, et al. Methods for improving cancer surveillance data in American Indian and Alaska Native populations. Cancer. 2008;113:1120–1130. doi: 10.1002/cncr.23724. [DOI] [PubMed] [Google Scholar]
- 38.Jim MA, Arias E, Seneca DS, et al. Racial misclassification of American Indians and Alaska Natives by Indian Health Service Contract Health Service Delivery Area. Am J Public Health. 2014;104:S295–S302. doi: 10.2105/AJPH.2014.301933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Randall DA, Lujic S, Leyland AH, et al. Statistical methods to enhance reporting of Aboriginal Australians in routine hospital records using data linkage affect estimates of health disparities. Aust N Z J Public Health. 2013;37:442–449. doi: 10.1111/1753-6405.12114. [DOI] [PubMed] [Google Scholar]
- 40.Romero Y, Trapani D, Johnson S, et al. National cancer control plans: A global analysis. Lancet Oncol. 2018;19:e546–e555. doi: 10.1016/S1470-2045(18)30681-8. [DOI] [PubMed] [Google Scholar]