Abstract
Purpose of review:
An increasing trend in obesity prevalence since the early 1980s has posed a significant population health burden across the globe. We conducted a systematic review for studies using measured anthropometry to examine trends in obesity in the US published from 2012 to 2018 and for systematic reviews to document trends in obesity across the globe published from 2014 to 2018.
Recent findings:
For the US, the only nationally representative data source capturing trends in obesity in this period was the National Health and Nutrition Examination Survey, which uses repeated cross-sectional data to document national trends in obesity in the US.. For global trends, the only systematic reviews of obesity across the globe were the Global Burden of Disease Obesity study and the Non-communicable Disease Risk Factor Collaboration study. In general, the population distribution of Body Mass Index (BMI) in the US has shifted towards the upper end of its distribution over the past three decades. The global distribution has similarly increased, albeit with large regional differences.
Summary:
US and global studies suggest an increasing trend in obesity since the 1980s, and there is a dearth of nationally representative longitudinal studies using measured anthropometry to capture trends in adult obesity in the US for the same individuals over time. Greater efforts are needed to identify factors contributing to the continued increases in obesity.
Keywords: Obesity, Prevalence, Population Health, Body Mass Index
Introduction
Obesity is linked with elevated risk of non-communicable diseases (NCDs) [1]. An increasing trend in obesity prevalence since the early 1980s has posed a significant population health burden across the globe [2] while obesity prevalence varies by region and country [1, 3].
Country-specific trends in obesity are generally tracked using longitudinal panel or repeated cross-sectional data, with the highest quality studies using measured anthropometry. In the US, the National Health and Nutrition Examination Survey (NHANES), which is a nationally representative, repeated cross-sectional survey of the civilian, noninstitutionalized US population [4], is the predominant dataset used to track changes in obesity over time. There are a set of national- or population-representative longitudinal studies following the same individuals over time or repeated cross-sections, some of which use self-reported height and weight (e.g., National Longitudinal Survey of Youth [5]; Health Information National Trends Survey [6]; California Health Interview Survey [7]; Medical Expenditure Panel Survey-Household Component [8]; Panel Study of Income Dynamics [9]; Behavioral Risk Factor Surveillance System [10]; and National Health Interview Survey [11]) while others capture specific subpopulations or portions of the lifecycle (e.g, Early Childhood Longitudinal Study [12]; National Longitudinal Study of Adolescent to Adult Health (Add Health) [13]; National Hospital Ambulatory Medical Care Survey [14]). For global studies, the predominant data sources include the Global Burden of Disease (GBD) study [2, 3, 15] and the Non-communicable Disease Risk Factor Collaboration (NCD-RisC) [16, 17], both of which include approximately 200 countries, allowing comparisons over time, across age groups, and among populations [2, 15–17].
We conducted a systematic review to examine trends in obesity in the US for studies providing nationally or sub-nationally representative estimates of body mass index (BMI), obesity, or abdominal obesity using measured anthropometry and published from 2012 to 2018. In addition, we reviewed the literature on global trends in obesity, restricting our search to systematic reviews or meta-analyses of global obesity in adults. In this review, we present findings on trends in obesity in the US and across the globe and discuss future research directions.
Methods
Search strategy
We used the following cut-off values to define overweight/obesity: overweight (BMI: 25–29.9), class I obesity (BMI: 30–34.9), class II obesity (BMI: 35–39.9) and class III obesity (BMI: ≥ 40) [18]. We defined abdominal obesity (i.e., cut-off values of waist circumference (WC) ≥ 102 cm (40 in) for men and WC ≥ 88 cm (35 in) for women) [19]. In addition, we considered the non-Hispanic Asian cut-points of WC ≥ 90 cm for men and WC ≥ 80 cm for women [20].
We systematically reviewed the literature using a protocol informed by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. We searched for articles published in English, peer-reviewed journals in PubMed. For the global study, we further restricted studies to systematic reviews or meta-analyses. We developed the search syntax in collaboration with a reference librarian (Supplementary Tables 1 and 2). Our query included the following terms, their cognates, and synonyms: obesity AND trend AND United States AND adults AND nationally representative (US studies); obesity AND trend AND global AND adults (global studies).
Inclusion/exclusion criteria
For the search of domestic studies, articles had to fit the following inclusion criteria: 1) estimates of obesity following our criteria above; 2) sampling to be nationally representative or sub-nationally representative of the US; 3) include adults over the age of 18 years; 4) measured (rather than self-report) anthropometry; 5) repeated cross-sectional or longitudinal study design; 6) peer-reviewed; 7) available in English; and 8) published between January 1, 2012 and July 1, 2018 (Supplementary table 1).
For the search of global studies, we restricted studies to systematic reviews and began with the seminal GBD paper [2] as a model and searched for studies that evaluated the prevalence or incidence of obesity using measured height and weight in countries outside the United States. To be included, articles had to fit the following inclusion criteria: 1) estimates of obesity following our criteria above; 2) estimates for areas outside the US; 3) adults over the age of 18 years; 4) measured (rather than self-report) anthropometry; 5) systematic review or meta-analysis; 6) peer-reviewed; 7) available in English; and 8) published between January 1, 2014 and July 1, 2018 (Supplementary table 2).
Study selection and data extraction
We used Covidence, an online platform, to manage screening and selection of studies. A single reviewer completed an initial independent screen of all titles and abstracts retrieved from the database searches. A second reviewer checked a random sampling of titles to guarantee no articles were falsely excluded at this stage, and the second reviewer found no such discrepancies. Three separate reviewers independently reviewed the full texts of studies, whereby each study was dually screened, to determine final study inclusion. All conflicts in the full text review were resolved via discussion with the authorship team.
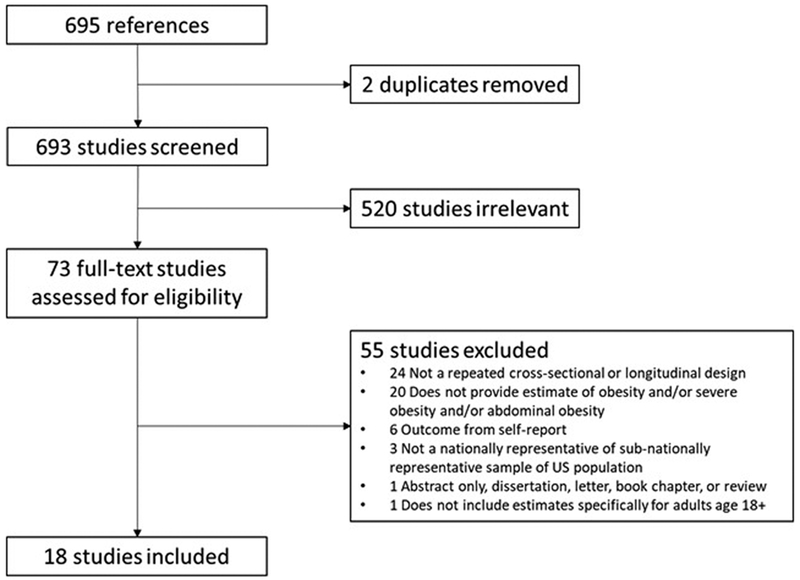
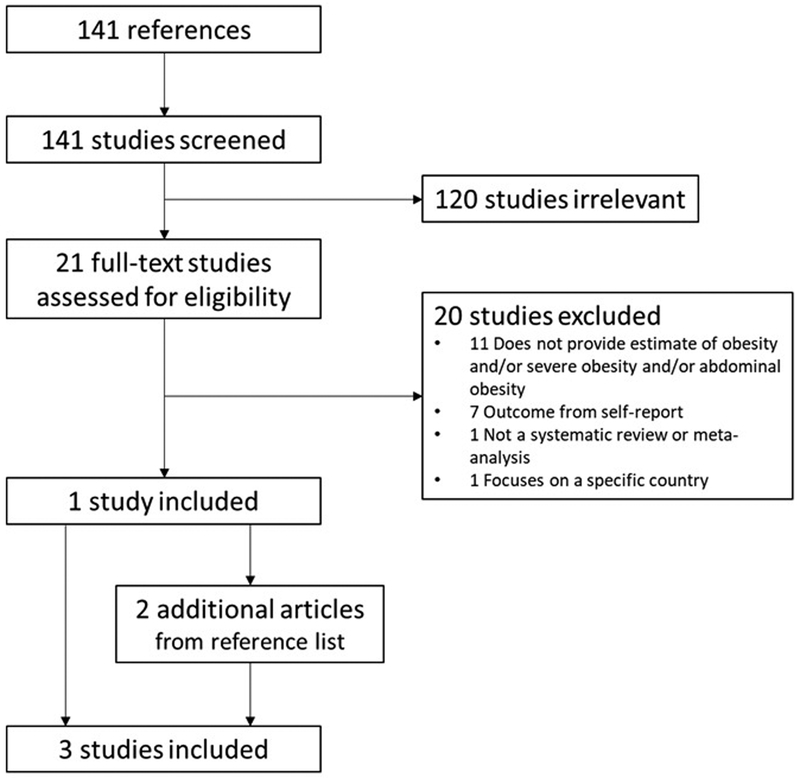
In our electronic search for the domestic studies, we found 695 references, two of which were duplicates, resulting in a total of 693 studies. In the initial title and abstract screen, the research team deemed 620 studies irrelevant, leaving 73 full-texts to review. We retained and extracted data from 18 studies that met inclusion criteria (Figure 1). Our search for the global studies returned 141 references, of which we deemed 120 studies irrelevant on the basis of initial title and abstract screen, leaving 21 full-texts to review of which one fit inclusion criteria. In addition, we included the GBD study published in July 2017 [2] and used the reference lists of the papers captured in our search to add one NCD-RisC paper [17] (Figure 2).
Figure 1.
PRISMA diagram for US studies that used nationally representative adult samples with measured anthropometry, published between Jan 2012 and July 2018.
Figure 2.
PRISMA diagram for global studies that were systematic review published between Jan 2014 and July 2018.
Results
We identified 18 US studies and three global studies that fit search criteria (Table 1). All the US studies used information collected in the NHANES and one also used information collected in the National Health Examination Survey (predecessor to the NHANES) [21]. Periods of time covered in each study differed; Hales et al. [38] provided the most updated information covering the period between 2013 and 2016 while Ljungvall et al. [21] presented data across the longest timespan (i.e., 1959 – 2008) among the studies extracted in our search. Three studies examined abdominal obesity, one of which used different cut-off points as their study participants were confined to non-Hispanic Asian Americans [36]. In relation to the global obesity trends, the GBD study used information obtained from 1514 sources [2] while the NCD RisC studies used information collected in 1698 population-based studies [16] and 1820 studies [17].
Table 1.
Eighteen US studies reviewing obesity prevalence in the US published from January 2012 to July 2018 and three studies of global obesity published from January 2014 to July 2018
| Authors | Data source | Study period |
Age range | BMI cut-off points |
Waist circumference cut-off points |
|---|---|---|---|---|---|
| Studies in the US | |||||
| Ljungvall et al., 2012 [21] | NHANES | 1959-2008 | 20-74 | ≥ 30 and ≥ 35 | |
| Romero et al., 2012 [22] | NHANES | 1988-2004 | 25-84 | ≥ 30 | |
| Yu, 2012 [23] | NHANES | 1971-2006 | 25-64 | ≥ 30 | |
| Huffman et al., 2012 [24] | NHANES | 1988-2008 | 20+ | ≥ 30 | |
| Robinson et al., 2013 [25] | NHANES | 1971-2008 | 2-74 | ≥ 30 for respondents aged 20-74 years ≥ the 95th percentile values of the sex- and age-specific CDC standards or BMI ≥ 30 for respondents aged 2-19 years |
|
| Robinson et al., 2013 [26] | NHANES | 1988-2008 | 20-74 | ≥ 102 cm (40 in) for men ≥ 88 cm (35 in) for women |
|
| Saydah et al., 2014 [27] | NHANES | 1999-2010 | 18+ | BMI ≥ 30 and BMI ≥ 35 | |
| Ladabaum et al., 2014 [28] | NHANES | 1988-2010 | 18+ | BMI ≥ 30 | |
| Cohen et al., 2015 [29] | NHANES | 1965-2011 | 18-64 | ≥ 102 cm (40 in) for men ≥ 88 cm (35 in) for women |
|
| Flegal et al., 2016 [30] | NHANES | 2005-2014 | 20+ | ≥ 30 and ≥ 40 | |
| Mehta et al., 2016 [31] | NHANES | 1971-1994 | 25-60 | ≥ 30 and ≥ 35 | |
| Kranjac et al. 2016 [32] | NHANES | 1971-2012 | 20+ | 30 to < 40 and ≥ 40 | |
| Yu, 2016 [33] | NHANES | 1971-2012 | 25-74 | ≥ 30 | |
| Yu, 2016 [34] | NHANES | 1971-2006 | 25-74 | 30 to < 35 and ≥ 35 | |
| Casagrande et al., 2016 [35] | NHANES | 1971-2012 | 20-49 | ≥ 30 | |
| Liu et al., 2017 [36] | NHANES | 2011-2014 | 20+ | ≥ 90 cm for men ≥ 80 cm for women |
|
| Ogden et al. 2017 [37] | NHANES | 2011-2014 | 20+ | ≥ 30 | |
| Hales et al., 2018 [38] | NHENES | 2013-2016 | 20+ | ≥ 30 and ≥ 40 | |
| Studies across the globe | |||||
| GBD 2015 Obesity Collaborators, 2017 [2] | 1514 studies | 1980-2015 | 20+ | ≥ 30 | |
| NCD RisC, 2016 [16] | 1698 studies | 1975-2014 | 18+ | 30 to < 35; 35 to < 40; ≥ 40 | |
| NCD RisC, 2017 [17] | 1820 studies | 1975-2016 | 20+ | 30 to < 35; 35 to < 40; ≥ 40 (online) |
BMI: Body Mass Index; GBD: Global Burden of Disease; NCD RisC: NCD Risk Factor Collaboration; NHANES: National Health and Nutrition Survey.
Overall obesity trends in the US
Flegal et al. [30] estimated obesity prevalence to be 34.6% (men: 33.5%; women: 35.7%) in 2005–2006, which decreased in 2007–2008 to 33.9% (men: 32.2%; women: 35.5%) but then increased to 37.9% (men: 35.2%; women: 40.5%) in 2013–2014 (Table 2). Hales et al. [38], including the most recent cycle of the NHANES, reported that obesity prevalence in 2013–2016 to be 36.5% for men and 40.8% for women.
Table 2.
Summary of findings reported in the Eighteen US studies reviewing obesity prevalence in the US published from January 2012 to July 2018 and three studies of global obesity published from January 2014 to July 2018.
| Authors | Study objectives | Statistical analysis | Selected findings / conclusions (related to obesity) |
|---|---|---|---|
| US studies | |||
| Ljungvall et al., 2012 [21] | • To analyze how obesity prevalence and the adjusted distribution of BMI have changed over time while paying attention to differences among population subgroups (i.e., race/ethnicity, education attainment and income). | • Probability linear models using obesity and BMI ≥ 35 as the outcomes. • Quantile regression models using BMI as the outcome. • Models were stratified by gender. |
• Increases in obesity, BMI ≥ 35 and BMI were similar across the different population subgroups while the additional increases among Blacks merit further investigation. • The obesity epidemic is not limited to low socioeconomic and minority groups. |
| Romero et al., 2012 [22] | • To examine trends in the prevalence of obesity and other CVD risk factors by race/ethnic groups. • To test whether the prevalence and trends differ according to race/ethnicity. |
• Absolute changes in the prevalence estimates within each race/ethnic group were calculated for each period (1988-1994 and 1999-2004) and over time (1988-1994 vs. 1999-2004). | • The prevalence of obesity increased significantly in non-Hispanic white and non-Hispanic black, both in men and women. • Among Mexican American, the prevalence of obesity increased only among men. • There existed persistent race/ethnic differences for all CVD risk factors, with non-Hispanic black and Mexican American generally having worse profiles than non-Hispanic white. |
| Yu, 2012 [23] | • To examine the time trends in educational differences in obesity by gender and race (non-Hispanic white and non-Hispanic black). | • The prevalence model; interaction terms between time (1971-1980 vs. 1999-2006) and education categories (< high school; high school degree; some college; at least 4-year college) were incorporated to indicate the change in the education-obesity association. • The analysis is done separately for each of the four gender-race groups. |
• The increase in obesity was similar for most educational groups, but significantly greater for younger women with some college and smaller for younger white men without a high-school degree. |
| Huffman et al., 2012 [24] | • To evaluate recent trends in composite cardiovascular health metrics • To estimate future levels of cardiovascular health behaviors and factors among adults in the US to determine whether the American Heart Association 2020 goals will be met if current trends continue. |
• Weighted linear regression using prevalence as the dependent variables and survey time as independent variables. • The coefficient based on the regression (i.e., the average annual change in the prevalence) was used to project the obesity prevalence and trends of other components for 2020 by assuming that trends would be the same. |
• Prevalence of obesity and dysglycemia increase as opposed to prevalence of smoking, hypercholesterolemia and hypertension that declined over the study periods. • The obesity prevalence was projected to increase up to 43.4% among men and 42.2% among women in 2020. |
| Robinson et al., 2013 [25] | • To estimate cohort-specific propensity to obesity for those born in the US in the 1980s. | • Age-period-cohort analysis | • Cohorts born in the 1980s had increased propensity to obesity versus those born in the late 1960s. |
| Robinson et al., 2013 [26] | • To estimate cohort-specific risks for abdominal obesity. | • Age-period-cohort effect | • The birth cohorts of the post-World War II Baby Boom appeared to have low cohort-specific risks of abdominal obesity. • The cohorts preceding and succeeding the Baby Boom showed evidence of birth cohort effects that increased prevalence of abdominal obesity. • These generational differences were more pronounced in women than in men. |
| Saydah et al., 2014 [27] | • To assess whether trends in CVD risk factors have improved by weight status (normal, overweight and obese). | • Data was grouped into 4-year periods (1999-2002, 2003-2006 and 2007-2010). • Prevalence of risk factors (total and undiagnosed diabetes, total and untreated hypertension, total and untreated dyslipidemia, self-reported smoking and moderate to heavy smoking exposure (cotinine levels ≥ 10ng/ml)) was calculated overall and for each BMI group. • Absolute change in prevalence was calculated as the percent estimate for 2007-2010 minus the percent estimate for 1999-2002. |
• The prevalence of cardiovascular risk factors increases as people become overweight and obese. • The prevalence of CVD risk factors has remained the same or declined over time. • From 1999-2002 to 2007-2010, untreated hypertension decreased among obese and overweight adults and untreated dyslipidemia decreased for all weight groups. • The proportion of those with 3 or more CVD risk factors increased over time among the obese population. |
| Ladabaum et al., 2014 [28] | • To characterize trends in and associations among overweight and obesity, abdominal obesity, physical activity and caloric intake in the US adults in the last 2 decades. | • Linear regression to assess trends in log-transformed BMI, WC and daily energy intake. • Logistic regression to assess the trends in the prevalence of obesity and abdominal obesity. |
• The prevalence of obesity and abdominal obesity increased substantially during the period between 1988 and 2010. • The proportion of people who reported no leisure time physical activity increased while average daily caloric intake did not change significantly. |
| Cohen et al., 2015 [29] | • To determine how macronutrient consumption patterns and body mass index in the US adult population have changed since the 1960s. | • Descriptive. | • Americans in general have been following the official nutrition advice for more than 40 years. • General adherence to recommendations to reduce fat consumption has coincided with a substantial increase in obesity. |
| Flegal et al., 2016 [30] | • To examine prevalence of obesity and Class 3 obesity (BMI ≥ 40) in 2013-2014. • To examine trends over the decade from 2005 through 2014. |
• Sex-stratified logistic regression models to assess the associations of age group, race/Hispanic origin, smoking status, and education with obesity prevalence. • When examining the trends, 5 cycles of the NHANES survey (2005-2014) were treated as a categorical variable. • Predicted margins are calculated. |
• The age-adjusted prevalence of obesity in 2013-2014 was 35.0% among men and 40.4% among women. • The prevalence of overall and class 3 obesity both showed a significant linear trend between 2005 and 2014, while there were no significant trends for men. |
| Mehta et al., 2016 [31] | • To test the hypothesis that even if the true effect of BMI as a continuous variable on mortality has not changed, changes in the BMI distribution could affect the calculated estimates of the effects for specific BMI categories. | • The NHANES I dataset (1971-1975) linked with mortality data was used to fit a Cox proportional hazards model incorporating BMI as a continuous variable. • Coefficients obtained from this model were used to simulate mortality for participants in the NHANES III (1988-1994). • Hazard ratios of mortality by BMI categories were compared between the NHANES I and the NHANES III with simulated mortality data. |
• Some of the diminution of the association between obesity and mortality may be an artifact of treating BMI as a categorical variable. |
| Kranjac et al. 2016 [32] | • To decompose change in body mass index, obesity and severe obesity from 1971 through 2012 into parts attributable to (1) older, fitter cohorts in the population being replaced by newer, less fit cohorts (between-cohort change) and cohort members becoming less fit over time (within-cohort change). | • Glenn Firebaugh’s linear decomposition technique and Kitagawa’s algebraic decomposition method to decompose aggregate change into two components (i.e., intracohort change and cohort replacement [i.e., intercohort change]). | • The rise in mean BMI and rates of obesity and severe obesity was primarily a consequence of intracohort change driven by variation in the demographic and socioeconomic composition and in the diet of the population overtime. • Obesity and BMI in the population rose largely because of individual increases in weight status that were broadly distributed across age and cohort groups. |
| Yu, 2016 [33] | • To analyze the influences of educational attainment on obesity trends. | • The linear probability model that included education (< high school; high school degree; some college; at least 4-year college), survey year, and interactions between education and survey year. • Obesity prevalence was simulated under several scenarios (different age distribution, educational distribution or educational inequality in obesity prevalence.) |
• Educational inequality in obesity was generally larger for women than men and for non-Hispanic white than non-Hispanic black. No difference was observed among non-Hispanic black men. • Obesity prevalence among some college group experienced the largest increase compared to other groups, except for non-Hispanic black men. |
| Yu, 2016 [34] | • To estimate model for year-of-birth (cohort) and year-of-observation (period) trends in how age-specific mortality rates differ across BMI categories. | • Logistic regression model • Models were compared to determine which temporal patterns provided a better fit to the data (age, period and /or cohort) • The final model includes interactions between birth cohort and BMI categories. |
• Among women, those who were born later were more likely to die when they were overweight, obese and severe obese (BMI ≥ 35) compared to normal weight. • Among men, those who were born later were less likely to die when they were overweight and were more likely to die when they were severely obese, compared to those with normal weight. |
| Casagrande et al., 2016 [35] | • To examine generational differences in cardiovascular risk factors of younger adults over the past 40 years. | • Logistic regression was used to calculate the odds of health conditions among adults aged 20-49 years. | • Cardiovascular risk factors in younger adults have worsened over the past 40 years. • Participants in 2009-2012 were more likely to be obese than those in 1971-1975 (OR = 4.98) |
| Liu et al., 2017 [36] | • To examine the prevalence of central obesity and the difference in the prevalence across demographic and socioeconomic groups were examined among US non-Hispanic Asian adults. | • Chi-squared tests were used to examine the difference in the prevalence of central obesity over time (2011-2012 vs. 2013-2014). | • Overall prevalence of central obesity (2011-2014) was 58.1%, with higher prevalence observed in women than in men. • Significant increases in central obesity were observed in younger adults (20-39 years), men, those with higher education and non-poor population. |
| Ogden et al., 2017 [37] | • To analyze trends in obesity prevalence by household income levels and individual education level during 1999-2002 to 2011-2014, | • No information on models provided. • Household income level was defined based on percentage of the federal poverty level (≤130%; >130 to 350%; and >350%) and education level was categorized into high school graduate or less; some college; and college graduate. |
• The prevalence of obesity increased among women in the two lower income groups. Among men, obesity prevalence increased among men in all three income groups. • Obesity prevalence increased among both sexes in all education groups except for men who were college graduates. |
| Hales et al., 2018 [38] | • To estimate obesity prevalence and examine trends in the prevalence by urbanization level. | • Logistic regression models were used to calculate obesity prevalence by urbanization level and 4-year period (2001-2004, 2005-2008, 2009-2012, 2013-2016). • Urbanization level was based on the National Center for Health Statistics classification schemes (large metropolitan statistical areas [MSAs]; medium or small MSAs; and non-MSAs). |
• Men living in medium or small MSAs had a higher obesity prevalence compared to those living in large MSAs. Women living in medium or smalle MSAs and non-MSAs had a higher prevalence compared to women living in large MSAs. • Obesity prevalence increased across all the urbanization level between 2001-2004 and 2013-2016. |
| Global studies | |||
| GBD 2015 Obesity Collaboration, 2017 [2] | • To assess the trends in the obesity and overweight prevalence during the period between 1980 and 2015. • To quantify the burden of disease related to high BMI (1990 – 2015). |
• Mixed-effects linear regression models (Bayesian meta-regression model and spatiotemporal Gaussian process regression model) |
• In 2015, overall obesity prevalence was 12.0%. • Since 1980, obesity prevalence has doubled in more than 70 countries. |
| NCD RisC, 2016 [16] | • To estimate trends in adult body mass index and trends in the prevalence of underweight, overweight and obesity from 1975 to 2014 in the world | • Bayesian hierarchical model | • During the period between 1975 and 2014, age-adjusted obesity prevalence increased from 3.2% to 10.8% in men and from 6.4% to 14.9 in women. |
| NCD RisC, 2017 [17] | • To estimates trends in mean BMI and the prevalence of underweight, overweight and obesity from 1975 to 2016 in children, adolescents and adults in the world. | • Bayesian hierarchical model | • Adult results were not presented in the manuscript while the updated results are available on the NCD-RisC website. |
BMI: Body mass index; CVD: cardiovascular disease; GBD: Global Burden of Disease; NCD-RisC: NCD Risk Factor Collaboration; WC: waist circumference
Ljungvall et al. [21] reported an obesity prevalence of 10% for men and 16% for women in 1959–1962, which increased to 18% for men and 23% for women in 1988–91, 27% for men and 34% for women in 1999–2000, and again to 32% for men and 36% for women in NHANES 2007 – 2008. The increasing trend in obesity prevalence was featured in the other studies in our search as well [22–24, 33, 35].
Several studies that used BMI cut-offs higher than 30 suggest a shift in population distribution for BMI towards the upper end of the BMI distribution. [21, 27, 30, 32]. For example, Ljungvall et al. [21] reported that prevalence of BMI ≥ 35, which was 1% and 5% for men and women, respectively in 1959, increased to 5% and 9% in 1988–1991 and finally to 11% and 19% in 2007–2008. Kranjac et al. [32] reported that the prevalence of BMI ≥ 40 was 1% in 1971, rising to 6% in 2012, with higher prevalence reported in women than in men. The prevalence of BMI ≥ 40 for men and women was 5.5% and 9.9% in 2013–2014 [30] and 5.5% and 9.8% in 2013–2016 [38].
Between 1988–1994 and 2009–2010, abdominal obesity prevalence increased from 29.1% to 42.0% among men and from 46.0% to 61.5% among women [28]. Robinson et al. [26] reported that in 1986–1990 abdominal obesity prevalence was 36.0% (27.5% for men and 44.3% for women) increasing to 52.5% (43.1% for men and 61.5% for women) in 2006–2010. Liu et al. [36] reported that central obesity among US non-Hispanic Asian adults in 2011–2014 was 55.3% and 60.9% for men and women, respectively.
Sociodemographic disparities
Several of the US studies examined differences in obesity prevalence by race/ethnicity, educational attainment, income and urbanization level. For example, Ljungvall et al. [21] reported that probability of obesity in 1960 was higher in non-Hispanic black women than non-Hispanic white women by 10 percentage points and that total increase during the study period (1960 – 2008) was also larger in non-Hispanic black women than non-Hispanic white women (by 5 – 10 percentage points). Romero et al. [22] studied a shorter period of time (1988 – 2004) and showed that a baseline difference observed between non-Hispanic white and non-Hispanic black did not change over time, while a difference between non-Hispanic black and Hispanic increased over time.
Yu et al [33] concluded that educational inequalities in relation to obesity prevalence from 1971 to 2012 were generally larger in women than men and larger in non-Hispanic white than non-Hispanic black and that obesity prevalence did not differ by educational attainment among non-Hispanic black men. In addition, individuals with some college education (i.e., 13 – 15 years of school or associate’s degree) experienced the most rapid increase in obesity prevalence among the four educational attainment categories in non-Hispanic white men, non-Hispanic white women and non-Hispanic black women. Ogden et al. [37], which also examined the trends by educational attainment (high school graduates or less; some college; and college graduates) between 1999–2002 and 2011–2014, showed that obesity prevalence among men with some college tended to increase at a faster pace than other two groups. On the other hand, such difference was not observed among women.
Ljungvall et al. [21] found an initial disparity by income, with higher prevalence observed among women in the lower (versus higher) income groups in 1959; this difference did not diverge over the full period captured (1959–2008). The initial income disparity for men in 1960 disappeared by the 1970s. When Ogden et al. [37] examined trends in obesity prevalence by three categories of household income from 1999–2002 to 2011–2014, obesity prevalence increased among women in the bottom two income groups, but it did not among women in the highest income group. Among men, obesity prevalence in the three income groups increased during the same period.
Hales et al. [38] examined if obesity prevalence differed by urbanization level (large metropolitan statistical areas [MSAs]; medium or small MSAs; and non-MSAs), showing that in 2013–2016, participants living in medium or small MSAs had a higher obesity prevalence compared to those living in large MSAs in both sexes. In addition, women living in non-MSAs also had a higher prevalence compared to women living in large MSAs.
Given less change in obesity prevalence in the first decade of the 2000s compared to previous years, several authors suggested that the increase in obesity prevalence among US adults may be leveling off [39, 40]. Robinson et al. examined differences in obesity prevalence [25] and abdominal obesity prevalence [26] by birth cohort using an age-period-cohort analysis. Robinson et al. [25] found that cohorts born in the 1980s had increased propensity to obesity compared to previous generations, suggesting obesity prevalence may continue to increase as this younger generation reaches the ages of peak prevalence of obesity. Robinson et al. [26] reported that the baby boomers (those born in 1946–1964) seemed to have low cohort effects on abdominal obesity.
Differences in obesity and abdominal obesity patterns
The authors of two studies reported trends in obesity defined using BMI and abdominal obesity (per waist circumference). Robinson et al. [26] reported that in 1986–1990 abdominal obesity prevalence was 27.5% for men and 44.3% for women and increased up to 43.1% for men and 61.5% for women in 2006–2010. During the same period, obesity defined with BMI increased from 18.5% to 32.6% and from 23.6% to 36.0% among men and women, respectively. Ladabaum et al. [28] reported that between 1988–1994 and 2009–2010, obesity prevalence increased from 19.9% to 34.6% among men and 24.9% to 35.4% among women while abdominal obesity prevalence increased from 29.1% to 42.0% among men and 46.0% to 61.5% among women.
Global trends in adult obesity prevalence
The GBD 2015 Obesity Collaborators based their study on a systematic literature search in Medline for studies providing nationally or sub-nationally representative estimates of BMI, overweight, or obesity among children or adults. Information came from 1514 data sources from 174 countries (713 measured and 801 self-report data) between 1980 and 2015. On the other hand, the NCD-RisC estimated global trends of BMI and obesity prevalence between 1975 and 2014 using data collected from 1698 population-based studies (e.g., nationally or sub-nationally representative studies and community-based studies) that used measured height and weight [16]. Following this initial paper, they expanded their study period to 2016 using data collected from 1820 population-based studies [17].
Both research groups described how obesity prevalence has increased in the last few decades. The GBD study showed that between 1980 and 2015 obesity prevalence doubled in 73 countries and showed an increase in most of the other countries as well. The NCD-RisC [16, 17] found that between 1975 and 2014, age-standardized prevalence of obesity increased from 3.2% to 10.8% in men and from 6.4% to 14.9% in women. In 2014, 2.3% and 5.0% of men and women from these 200 countries had BMI ≥35 and 0.64% and 1.6% had BMI ≥ 40.
The GBD study also showed trends in adult obesity prevalence by country’s sociodemographic development quintiles (categorized into quintiles: low, low-middle, middle, high-middle, and high). The GBD study showed that between 1980 and 2015, men aged 25 to 29 and living in countries with a low-middle degree of development experienced the largest relative increase in obesity prevalence (1.1% in 1980 to 3.8% in 2015) among population subgroups stratified by sex, age and country’s level of sociodemographic level.
The NCD RisC [16, 17] emphasized large regional differences in obesity prevalence. Areas with obesity prevalence of ≥25% or higher in 2016 included High-income Western countries (men: 29.6%; women: 29.6%), Central and Eastern Europe (women: 26.1%), Central Asia, Middle East and North Africa (women: 35.2%), Latin America and Caribbean (women: 29.2%), and Oceania (women: 30.0%), while several areas had obesity prevalence of <10%, i.e., East and South East Asia (men: 5.9%; women: 7.4%), High-income Asia Pacific (men: 4.9%; women: 4.3%), South Asia (men: 3.2%; women: 6.0%); and Sub-Saharan Africa (men: 4.8%).
Discussion
Synthesis of findings
We extracted 18 US studies from the NHANES in our search, which indicate an increase in obesity prevalence over the past 40 years, with the latest prevalence estimates from the NHANES 2013–2016 at 36.6% (men) and 41.0% (women) [38]. In addition, Hales et al. [41], which was published as a letter and thus not included in our search, reported obesity prevalence in 2015–2016 to be 37.9% (men) and 41.1% (women).
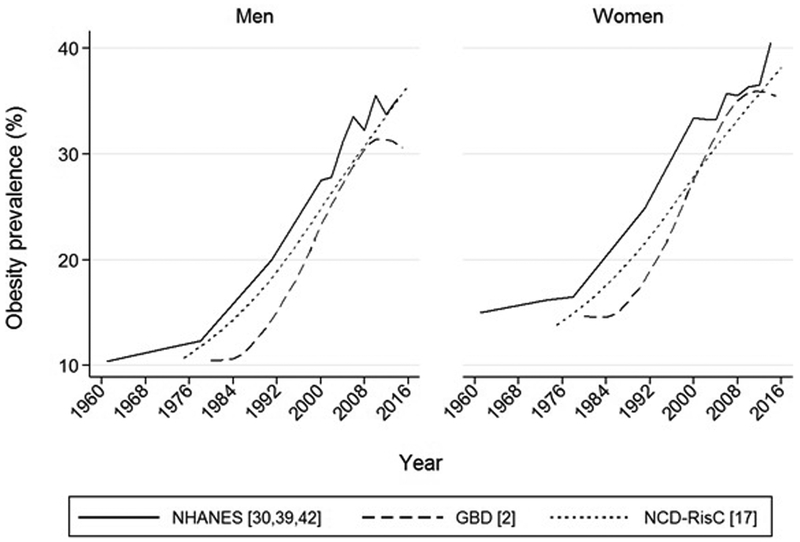
Several papers by Flegal and her colleagues published outside of our inclusion window, and thus not included in our search, reported obesity prevalence during the periods between 1960 and 1988–1994 [42], 1988–1994 to 1999–2000 [43], and 1999–2000 and 2007–2008 [39, 44–47]. The earlier two studies showed that obesity prevalence increased significantly from 14.5% to 22.5% to 30.5% between NHANES II (1976–1980), NHANES III (1988–1994), and the first cycle of the continuous NHANES (1999–2000), while the more recent studies suggested a stabilized trend in obesity prevalence in the early 2000s. Whereas some authors report that the increase in adult obesity prevalence may be slowing over time [39, 40], the 18 more recent studies included in our review do not support such trend. In particular, Flegal et al. [30] found a significant increasing linear trend in the prevalence between 2005–2006 and 2013–2014 among women. Significant increases were reported between 2001–2004 and 2013–2016 [38] and between 2007–2008 and 2015–2016 [41]. In addition, US-specific estimates provided by the GBD [2] and the NCD-RisC [17] also suggest an increase in US obesity prevalence (Figure 3).
Figure 3.
Trends in US adult obesity prevalence based on data from the National Health and Nutrition Survey (NHANES), and US data included in the Global Burden of Disease (GBD), the NCD Risk Factor Collaborations (NCD-RisC).
The studies that examined obesity trends suggest particularly high risk among non-Hispanic black women [21, 22], individuals with some college education versus the other educational attainment categories [33], those whose communities were classified as the intermediate category of urbanization [38] and cohort differences in obesity prevalence. [25, 26].
Our findings for global obesity trends indicate that obesity prevalence has increased in the last few decades across the world. The GBD study showed that between 1980 and 2015 obesity prevalence doubled in 73 countries and the NCD-RisC [16, 17] found that age-standardized prevalence of obesity increased from 3.2% to 10.8% in men and from 6.4% to 14.9% in women across 200 countries between 1975 and 2014 [16].
Differences in surveillance
The NHANES is a repeated cross-sectional survey, in which different participants were randomly sampled from population at several time points. Thus, unlike in longitudinal studies, it is not possible to track within-person changes in weight over time. While there are several representative longitudinal cohort studies in the US that collect measured height and weight (e.g., Add Health [13], the Longitudinal Health and Retirement Study [48], the National Social Life, Health, and Aging Project [49] and the Wisconsin Longitudinal Study [50]), none had data published in the date range that fit our inclusion criteria.
The GBD study and the NCD-RisC study based their estimates on many population-based studies, some of which were cross-sectional and the others were longitudinal follow-up. Rather than looking at the longitudinal association, the GBD and NCD-RisC studies estimated obesity prevalence for each country and year using data collected in each given country and the year of data collection, but allowed for inclusion of data from other years in the same country or from data in other countries across similar time periods within regions.
Analytical issues
Several aspects of the analysis of obesity prevalence trends can impact the magnitude and direction of estimated effects, potentially resulting in inconsistent conclusions across studies. Conclusions in relation to the trends in obesity prevalence differed by time periods covered by each study. Studies that covered a longer period (e.g., 1959–2008 [21]; 1988–2008 [28]) documented increases in obesity prevalence, while Flegal et al. [43] suggested that obesity prevalence from 1999 to 2008 did not continue to increase at the same rate as that observed in the prior 10 years. Another example is a difference between Ljungvall et al. [21] that covered the period between 1959–2008 and Romero et al. [22] that used information collected in 1988–2004. While the former described that the increases in obesity prevalence during the study periods (1960–2008) were similar across the racial/ethnic subgroups (or, at least, smaller than the increase experienced by the whole population), the latter emphasized that non-Hispanic black were at higher risk of obesity compared to non-Hispanic white.
The time point used as baseline for evaluating obesity prevalence trends can also have an important impact on findings [47]. A notable example comes from studies of recent childhood obesity trends; evaluations using 2003–2004 as the baseline time point reported decreases in the prevalence of obesity among 2–5 year old children through 2011–2014 [47, 51], while studies using 1999–2000 as baseline reported no evidence of a decline in obesity prevalence in this or any age group through 2011–2014 [52–54]. Because prevalence estimates can fluctuate substantially between study waves, inclusion of data from several prior years and subsequent years can aid in determining whether prevalence changes at any given time point reflect a transient anomalous dip or a true downward trend [53]. The need to place data in context and see the bigger picture underscores the need for ongoing, consistent monitoring of obesity prevalence and trends in the US and worldwide.
One must consider exclusion criteria for each specific study, even when based on the same study source. For example, in the 18 studies we reviewed, three studies explicitly excluded BMI < 18.5 [23, 27, 34]. Studies also varied greatly in the exclusion of older adults, with some studies excluding adults in their late 60s or 70s while others making no exclusions of older adults, and also varied in exclusion of younger adults aged 18–24 years old. Because obesity prevalence varies across the lifespan and some evidence suggests that obesity trends differ by age [30, 47], the age range of included participants could potentially impact estimated trends or limit comparability across studies. The analytical approaches used to evaluate obesity trends also varied, with methods including pairwise difference testing, linear trend tests, regression modeling to evaluate linear and quadratic trends, and age-period-cohort analysis. Studies using multivariable regression modeling to evaluate changes over time also differed in the selection of covariates used for adjustment in regression models. However, regardless of these differences, studies of US trends included in our review consistently found significant long-term increases in the prevalence of obesity.
There are also analytical issues related to future obesity projections. Flegal et al. [30] cautioned that several previous attempts to use past data to extrapolate to future trends in obesity prevalence may not have provided valid estimates [55–57]. Mehta et al. [31] conducted simulations using NHANES I to simulate mortality for NHANES III participants to test whether a decline in association between BMI and mortality related to statistical nuisance issues, finding that these nuisance contributors, such as the usage of categorical BMI variable (vs. continuous variable) and changes in population distribution altered findings.
Limitations
There are several limitations that should be addressed. First, only studies based on the NHANES data were captured with our inclusion criteria. While the NHANES is nationally representative sample and designed to estimate obesity prevalence in the US, it is a repeated cross sectional, which precludes within-individual change in BMI/obesity. Second, although NHANES is nationally representative, the subpopulation groups can get quite small by sex, race/ethnicity and socioeconomic groups. Third, we only included systematic reviews and meta analyses for our global search. Thus, some smaller within country studies that were not a part of GBD and NCD RisC might have been missed. Fourth, the GBD study and the NCD-RisC studies estimated obesity prevalence in each country as a whole, thus ignoring within-country heterogeneity by region, SES, or other subpopulations.
Conclusions and Future directions
It would be ideal to use longitudinal studies that allow intra-individual changes between study waves for surveillance. Surveillance that can fully address age-period-cohort differences are needed to identify whether obesity trajectories by age are different by cohort. For example, the Global Burden of Disease Study [3] presented obesity prevalence by age across birth cohorts, suggesting that obesity prevalence tended to increase at a faster pace among those who were born in later cohorts than in earlier cohorts (e.g., those born in 1985 vs. those born in 1960). Age-period-cohort analyses might be particularly relevant in countries undergoing dramatic changes in social and economic environment. There remains a need for studies that allow within-country differences in obesity prevalence.
Although significant increases in the prevalence of obesity since the 1980s are well-documented, relatively little is known about the causes for these population-level trends [30]. Future studies are needed to identify the factors contributing to the continued increases in obesity. Moreover, there is a need for evaluation of the effectiveness of programs and policies to prevent obesity, as well as to understand the reasons for limited progress in reversing obesity trends [58–61]. Because of the large inter-individual heterogeneity in the efficacy of obesity intervention and treatment approaches, further studies are warranted to identify individual factors that predict response and to evaluate personalized precision approaches based on genetic and phenotypic characterization [62]. In addition, given the established relations between central obesity and cardiometabolic risk, a close monitoring of trends in central obesity prevalence may be necessary.
Supplementary Material
Footnotes
Conflict of Interest
Yosuke Inoue declares that he has no conflict of interest.
Bo Qin declares that she has no conflict of interest.
Jennifer Poti declares that she has no conflict of interest.
Rebeccah Sokol declares that she has no conflict of interest.
Penny Gordon-Larsen is supported by grants from the National Institutes of Health (NIH) and the Office of the Vice Chancellor for Research at the University of North Carolina at Chapel Hill.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
- 1.World Health Organization. Obesity and overweight. http://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
- 2.• Global Burden of Disease Obesity Collaborators, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, Marczak L, Mokdad AH, Moradi-Lakeh M et al. : Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Engl J Med. 2017, 377(1):13–27. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study used information on body mass index, overweight and obesity obtained from 1514 sources from 174 countries, documenting an overall increase in global obesity.
- 3.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF et al. : Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384(9945):766–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. http://www.cdc.gov/nchs/nhanes/index.htm.
- 5.Bureau of Labor Statistics. National Longitudinal Survey of Youth 1997 cohort. http://www.nlsinfo.org/content/cohorts/nlsy97.
- 6.Nelson DE, Kreps GL, Hesse BW, Croyle RT, Willis G, Arora NK, Rimer BK, Viswanath KV, Weinstein N, Alden S: The Health Information National Trends Survey (HINTS): development, design, and dissemination. J Health Commun. 2004, 9(5):443–460; discussion 481–444. [DOI] [PubMed] [Google Scholar]
- 7.UCLA Center for Health Policy Research. California Health Interview Survey. http://healthpolicy.ucla.edu/chis/Pages/default.aspx.
- 8.Cohen JW, Cohen SB, Banthin JS: The medical expenditure panel survey: a national information resource to support healthcare cost research and inform policy and practice. Med Care. 2009, 47(7 Suppl 1):S44–50. [DOI] [PubMed] [Google Scholar]
- 9.McGonagle KA, Schoeni RF, Sastry N, Freedman VA: The Panel Study of Income Dynamics: Overview, Recent Innovations, and Potential for Life Course Research. Longit Life Course Stud. 2012, 3(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. http://www.cdc.gov/brfss/.
- 11.Centers for Disease Control and Prevention. National Health Interview Survey. https://www.cdc.gov/nchs/nhis/index.htm.
- 12.National Center for eucation Statistics. Early childhood longitudinal study, birth cohort (ECLS-B). http://nces.ed.gov/ecls/birth.asp.
- 13.The NS, Suchindran C, North KE, Popkin BM, Gordon-Larsen P: Association of adolescent obesity with risk of severe obesity in adulthood. JAMA. 2010, 304(18):2042–2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevantion. Ambulatory Health Care Data. http://www.cdc.gov/nchs/ahcd/index.htm.
- 15.Institute for Health Metrics and Evaluation. Global Burden of Disease Data. http://www.healthdata.org/gbd/data.
- 16.NCD Risk Factor Collaboration: Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet 2016, 387(10026):1377–1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.• NCD Risk Factor Collaboration: Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390(10113):2627–2642. [DOI] [PMC free article] [PubMed] [Google Scholar]; While the main focus of this study was the global obesity prevalence among children and adolescents, the manuscript also includes updated information on adult obesity prevalence (1975 to 2016), which is availbale on the project’s website.
- 18.American College of Cardiology/American Heart Association Task Force on Practice Guidelines OEP: Executive summary: Guidelines (2013) for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Obesity Society published by the Obesity Society and American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Based on a systematic review from the The Obesity Expert Panel, 2013. Obesity. 2014, 22 Suppl 2:S5–39. [DOI] [PubMed] [Google Scholar]
- 19.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Executive Summary of the Third Report of The National Cholesterol Education Program (NCEP). JAMA. 2001, 285(19):2486–2497. [DOI] [PubMed] [Google Scholar]
- 20.Alberti KG, Zimmet P, Shaw J: Metabolic syndrome--a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006, 23(5):469–480. [DOI] [PubMed] [Google Scholar]
- 21.Ljungvall A, Zimmerman FJ: Bigger bodies: long-term trends and disparities in obesity and body-mass index among U.S. adults, 1960–2008. Soc Sci Med. 2012, 75(1):109–119. [DOI] [PubMed] [Google Scholar]
- 22.Romero CX, Romero TE, Shlay JC, Ogden LG, Dabelea D: Changing trends in the prevalence and disparities of obesity and other cardiovascular disease risk factors in three racial/ethnic groups of USA adults. Adv Prev Med. 2012, 2012:172423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yu Y: Educational differences in obesity in the United States: a closer look at the trends. Obesity. 2012, 20(4):904–908. [DOI] [PubMed] [Google Scholar]
- 24.Huffman MD, Capewell S, Ning H, Shay CM, Ford ES, Lloyd-Jones DM: Cardiovascular health behavior and health factor changes (1988–2008) and projections to 2020: results from the National Health and Nutrition Examination Surveys. Circulation 2012, 125(21):2595–2602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robinson WR, Keyes KM, Utz RL, Martin CL, Yang Y: Birth cohort effects among US-born adults born in the 1980s: foreshadowing future trends in US obesity prevalence. Int J Obes. 2013, 37(3):448–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robinson WR, Utz RL, Keyes KM, Martin CL, Yang Y: Birth cohort effects on abdominal obesity in the United States: the Silent Generation, Baby Boomers and Generation X. Int J Obes. 2013, 37(8):1129–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saydah S, Bullard KM, Cheng Y, Ali MK, Gregg EW, Geiss L, Imperatore G: Trends in cardiovascular disease risk factors by obesity level in adults in the United States, NHANES 1999–2010. Obesity. 2014, 22(8):1888–1895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ladabaum U, Mannalithara A, Myer PA, Singh G: Obesity, abdominal obesity, physical activity, and caloric intake in US adults: 1988 to 2010. Am J Med. 2014, 127(8):717–727.e712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cohen E, Cragg M, deFonseka J, Hite A, Rosenberg M, Zhou B: Statistical review of US macronutrient consumption data, 1965–2011: Americans have been following dietary guidelines, coincident with the rise in obesity. Nutrition. 2015, 31(5):727–732. [DOI] [PubMed] [Google Scholar]
- 30.•• Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL: Trends in Obesity Among Adults in the United States, 2005 to 2014. JAMA. 2016, 315(21):2284–2291. [DOI] [PMC free article] [PubMed] [Google Scholar]; Flegal and her colleagues have published a series of articles using data from the NHANES. This study is one of this group’s most recent papers to document US obesity prevalence during the period between 2005 – 2014.
- 31.• Mehta T, Pajewski NM, Keith SW, Fontaine K, Allison DB: Role of a plausible nuisance contributor in the declining obesity-mortality risks over time. Exp Gerontol. 2016, 86:14–21. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this paper, the authors address critical methodological issues related to understanding the issues in the estimation of the association between BMI and mortality. The authors found that nuisance contributors, such as the use of categorical (vs. continuous) BMI variables and changes in population distribution over time, altered findings.
- 32.Kranjac AW, Wagmiller RL: Decomposing trends in adult body mass index, obesity, and morbid obesity, 1971–2012. Soc Sci Med. 2016, 167:37–44. [DOI] [PubMed] [Google Scholar]
- 33.Yu Y: Four Decades of Obesity Trends among Non-Hispanic Whites and Blacks in the United States: Analyzing the Influences of Educational Inequalities in Obesity and Population Improvements in Education. PLOS ONE. 2016, 11(11):e0167193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yu Y: The Changing Body Mass-Mortality Association in the United States: Evidence of Sex-Specific Cohort Trends from Three National Health and Nutrition Examination Surveys. Biodemography Soc Biol. 2016, 62(2):143–163. [DOI] [PubMed] [Google Scholar]
- 35.Casagrande SS, Menke A, Cowie CC: Cardiovascular Risk Factors of Adults Age 20–49 Years in the United States, 1971–2012: A Series of Cross-Sectional Studies. PLOS ONE. 2016, 11(8):e0161770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu X, Chen Y, Boucher NL, Rothberg AE: Prevalence and change of central obesity among US Asian adults: NHANES 2011–2014. BMC Public Health. 2017, 17(1):678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ogden CL, Fakhouri TH, Carroll MD, Hales CM, Fryar CD, Li X, Freedman DS: Prevalence of obesity among adults, by household income and education—United States, 2011–2014. MMWR Morb Mortal Wkly Rep. 2017, 66(50):1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.• Hales CM, Fryar CD, Carroll MD, Freedman DS, Aoki Y, Ogden CL: Differences in Obesity Prevalence by Demographic Characteristics and Urbanization Level Among Adults in the United States, 2013–2016. JAMA. 2018, 319(23):2419–2429. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study provided the most recent obesity prevalence from the NHANES (2013–2016) among the studies in our search, including examination of trends in obesity prevalence by urbanization level during this period.
- 39.Flegal KM, Carroll MD, Ogden CL, Curtin LR: Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010, 303(3):235–241. [DOI] [PubMed] [Google Scholar]
- 40.Rokholm B, Baker JL, Sørensen TIA: The levelling off of the obesity epidemic since the year 1999--a review of evidence and perspectives. Obes Rev. 2010, 11(12):835–846. [DOI] [PubMed] [Google Scholar]
- 41.Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL: Trends in Obesity and Severe Obesity Prevalence in US Youth and Adults by Sex and Age, 2007–2008 to 2015–2016. JAMA. 2018, 319(16):1723–1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL: Overweight and obesity in the United States: prevalence and trends, 1960–1994. Int J Obes. 1998, 22(1):39–47. [DOI] [PubMed] [Google Scholar]
- 43.Flegal KM, Carroll MD, Ogden CL, Johnson CL: Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002, 288(14):1723–1727. [DOI] [PubMed] [Google Scholar]
- 44.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM: Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004, 291(23):2847–2850. [DOI] [PubMed] [Google Scholar]
- 45.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM: Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006, 295(13):1549–1555. [DOI] [PubMed] [Google Scholar]
- 46.Flegal KM, Carroll MD, Kit BK, Ogden CL: Prevalence of Obesity and Trends in the Distribution of Body Mass Index Among US Adults, 1999–2010. JAMA. 2012, 307(5):491–497. [DOI] [PubMed] [Google Scholar]
- 47.Ogden CL, Carroll MD, Kit BK, Flegal KM: Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014, 311(8):806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, Weir DR: Cohort Profile: the Health and Retirement Study (HRS). Int J Epidemiol. 2014, 43(2):576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Suzman R: The National Social Life, Health, and Aging Project: an introduction. J Gerontol B Psychol Sci Soc Sci. 2009, 64 Suppl 1:i5–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Herd P, Carr D, Roan C: Cohort profile: Wisconsin longitudinal study (WLS). Int J Epidemiol. 2014, 43(1):34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, Flegal KM: Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988–1994 Through 2013–2014. JAMA. 2016, 315(21):2292–2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Skinner AC, Skelton JA: Prevalence and trends in obesity and severe obesity among children in the United States, 1999–2012. JAMA Pediatr. 2014, 168(6):561–566. [DOI] [PubMed] [Google Scholar]
- 53.Skinner AC, Perrin EM, Skelton JA: Prevalence of obesity and severe obesity in US children, 1999–2014. Obesity. 2016, 24(5):1116–1123. [DOI] [PubMed] [Google Scholar]
- 54.Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC: Prevalence of Obesity and Severe Obesity in US Children, 1999–2016. Pediatrics. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Finkelstein EA, Khavjou OA, Thompson H, Trogdon JG, Pan L, Sherry B, Dietz W: Obesity and severe obesity forecasts through 2030. Am J Prev Med. 2012, 42(6):563–570. [DOI] [PubMed] [Google Scholar]
- 56.Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M: Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011, 378(9793):815–825. [DOI] [PubMed] [Google Scholar]
- 57.Kelly T, Yang W, Chen CS, Reynolds K, He J: Global burden of obesity in 2005 and projections to 2030. Int J Obes. 2008, 32(9):1431–1437. [DOI] [PubMed] [Google Scholar]
- 58.Roberto CA, Swinburn B, Hawkes C, Huang TT, Costa SA, Ashe M, Zwicker L, Cawley JH, Brownell KD: Patchy progress on obesity prevention: emerging examples, entrenched barriers, and new thinking. Lancet. 2015, 385(9985):2400–2409. [DOI] [PubMed] [Google Scholar]
- 59.Cawley J: Does Anything Work to Reduce Obesity? (Yes, Modestly). J Health Polit Policy Law 2016, 41(3):463–472. [DOI] [PubMed] [Google Scholar]
- 60.Richardson MB, Williams MS, Fontaine KR, Allison DB: The development of scientific evidence for health policies for obesity: why and how? Int J Obes. 2017, 41(6):840–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Freudenberg N, Franzosa E, Sohler N, Li R, Devlin H, Albu J: The State of Evaluation Research on Food Policies to Reduce Obesity and Diabetes Among Adults in the United States, 2000–2011. Prev Chronic Dis. 2015, 12:E182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yanovski SZ, Yanovski JA: Toward Precision Approaches for the Prevention and Treatment of Obesity. JAMA. 2018, 319(3):223–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.