Abstract
Background:
Transforming growth factor-β (TGF-β) is a major inducer of epithelial–mesenchymal transition (EMT) in different cell types. TGF-β-mediated EMT is thought to contribute to tumour cell spread and metastasis. Sialyl Lewis antigens synthesised by fucosyltransferase (FUT) 3 and FUT6 are highly expressed in patients with metastatic colorectal cancer (CRC) and are utilised as tumour markers for cancer detection and evaluation of treatment efficacy. However, the role of FUT3 and FUT6 in augmenting the malignant potential of CRC induced by TGF-β is unclear.
Methods:
Colorectal cancer cell lines were transfected with siRNAs for FUT3/6 and were examined by cell proliferation, invasion and migration assays. The expression and phosphorylation status of TGF-β downstream molecules were analysed by western blot. Fucosylation of TGF-β receptor (TβR) was examined by lectin blot analysis.
Results:
Inhibition of FUT3/6 expression by siRNAs suppressed the fucosylation of type I TβR and phosphorylation of the downstream molecules, thereby inhibiting the invasion and migration of CRC cells by EMT.
Conclusion:
Fucosyltransferase 3/6 has an essential role in cancer cell adhesion to endothelial cells by upregulation of sialyl Lewis antigens and also by enhancement of cancer cell migration through TGF-β-mediated EMT.
Keywords: colorectal cancer, fucosyltransferase, TGF-β, EMT
The overall survival rate for patients with colorectal cancer (CRC) has been improving due to recent advances in chemotherapy, such as the use of molecular-targeting therapy. However, patients with metastatic CRC still face a dismal prognosis. More than 1 million individuals develop CRC every year and the disease-specific mortality rate is nearly 33% in the developed world due to disease progression (Cunningham et al, 2010).
In order to improve survival of patients with metastatic CRC, early detection or prediction of metastasis is required. Several biomarkers have been introduced to increase treatment efficacy. The most important development in biomarkers for metastatic CRC has been the validation of KRAS mutation status as a predictor of non-responsiveness to epidermal growth factor receptor (EGFR)-targeted therapy (Karapetis et al, 2008). In the adjuvant setting, prognostic and predictive molecular markers (microsatellite instability and 18q imbalance) could potentially be used to discriminate between molecular phenotypes in stage II disease (clinically heterogeneous), thereby contributing to the risk-benefit assessment of adjuvant treatment (Jen et al, 1994; Ogunbiyi et al, 1998; Watanabe et al, 2001; Popat and Houlston, 2005; Popat et al, 2005). However, complex pathways contribute to progression of the disease and, in general, single markers might not be entirely useful for prediction of efficacy and outcome. With high-throughput genome-wide screening, predictive and prognostic molecular signatures are increasingly being sought but, as yet, none have been validated for clinical use.
Recent studies have suggested that the involvement of sialyltransferase and fucosyltransferases (FUTs) on cancer progression such as cancer cell metastasis and invasion are mediated by modification of the cell surface by these enzymes to attachment of glycosyl residues (Park et al, 2012). For one of the typical examples, it has been shown that silaylation and fucosylation of the EGFR have significant role in regulating its signal (Wang et al, 2006; Matsumoto et al, 2008; Liu et al, 2011).
Among several glycosylation enzymes, we focused on the biological characteristics of metastatic CRC, especially with respect to fucosylated antigens, such as sialyl Lewis x (sLeX) and sialyl Lewis a antigen (sLea, CA19-9), which are found in the sera and tumour tissues of CRC patients (Hakomori and Kannagi, 1983; Narimatsu et al, 1998). Fucosylated antigens are used as tumour markers for cancer detection and evaluation of treatment efficacy. For example, CA19-9 is frequently elevated in patients with CRC (∼60%) and has been identified as highly useful tumour marker for the disease (Koprowski et al, 1981). It has also been shown that elevated CA19-9 levels are associated with a lower postoperative survival rate among CRC patients (Filella et al, 1992; Kouri et al, 1992; Petrioli et al, 2012). Similar to CA19-9, elevation of sLex expression has also been shown to signify a poor prognosis in patients with CRC (Grabowski et al, 2000; Nakagoe et al, 2002).
For the synthesis of CA19-9, fucosyltransferase 3 (FUT3) adds L-fucose in an α(1,4) linkage to sialylated precursors (Tsuchida et al, 2003; Miyazaki et al, 2004). Conversely, for synthesis of sLex, fucosyltransferase 6 (FUT6) and perhaps FUT3 also add L-fucose in a α(1,3) linkage to sialylated precursors (Weston et al, 1992). It has been reported that enhanced activity of FUTs is associated with increased metastatic potential of CRC cells (Hiller et al, 2000; Kannagi et al, 2004; Muinelo-Romay et al, 2011), suggesting that fucosylation and L-fucose may have an important role in disease progression (Hakomori and Kannagi, 1983). In fact, these observations led us to investigate the ability of L-fucose-bound liposomes to target CA19-9-producing pancreatic cancer cells (Yoshida et al, 2012). Although it has been shown that suppression of FUTs inhibits E-selectin-mediated adhesion to endothelial cells and liver metastasis of a CRC cell line (Weston et al, 1999; Kanoh et al, 2003), the precise mechanisms underlying the potentiation of cancer cell malignancy by FUTs remain unknown.
Transforming growth factor-β (TGF-β) is a regulator of cell cycle progression and is considered a critical factor involved in the late stages of tumourigenesis (Leivonen and Kahari, 2007). Transforming growth factor-β is frequently overexpressed in metastatic colon cancer, and circulating levels of this cytokine may be an indicator of liver metastasis (Picon et al, 1998; Tsushima et al, 2001; Calon et al, 2012). A previous study demonstrated the antimetastatic role of Smad4 in a preclinical model of liver metastasis (Zhang et al, 2010). However, the mechanisms by which TGF-β promote liver metastasis are unknown.
Transforming growth factor-β is a major inducer of epithelial–mesenchymal transition (EMT) in different cell systems, including colon and hepatic cells (Kaimori et al, 2007; Caja et al, 2011; Grandclement et al, 2011; Katsuno et al, 2013). Transforming growth factor-β-mediated EMT allows epithelial cells to acquire a fibroblastic morphology, losing their polarity and expression of E-cadherin as well as other cell–cell adhesion molecules, with a concomitant increase in the expression of mesenchymal markers (van Zijl et al, 2009; Calon et al, 2012). The newly acquired phenotype of tumour cells that have undergone EMT is thought to contribute to tumour cell spread and metastasis.
In this study, we focused on FUTs that were responsible for CA19-9 synthesis and investigated the involvement of signal transduction pathways related to cancer cell metastasis through EMT. Herein, we demonstrated that FUT3 and FUT6 could activate TGF-β receptors (TβRs) through fucosylation and enhanced TGF-β signalling, resulting in CRC cell migration and invasion possibly through EMT. Thus, these results suggest that FUT3 and FUT6 potentiates cancer cell adhesion to endothelial cells by upregulation of sialyl Lewis antigens and also by enhancement of cancer cell metastasis by EMT through TGF-β-mediated EMT.
Materials and methods
Cell lines
Colo205, Ls174T, HT29 and HCT15 cells were purchased from American Type Culture Collection (ATCC, Manassas, VA, USA). Ls180 cells were obtained from Japanese Collection of Research Bioresources Cell Bank (Osaka, Japan). Colo205 and HCT15 were cultured in RPMI 1640 (Life Technologies, Carlsbad, CA, USA) supplemented with 10% fetal bovine serum (FBS), L-glutamine and 1% penicillin–streptomycin. Ls174T and Ls180 were cultured in DMEM (Life Technologies) supplemented with 10% FBS, L-glutamine and 1% penicillin–streptomycin. HT29 cells were cultured in McCoy's 5 A medium (Life Technologies) supplemented with 10% FBS, L-glutamine and 1% penicillin–streptomycin.
Small interfering RNA and transfection
Small interfering RNA oligonucleotides were synthesised in a purified and annealed duplex form. The sequences targeting the human FUT gene are as follows: random; sense, 5′-CCUUAUACCUAACGACAGACCCUUU-3′, antisense, 5′-AAAGGGUCUGUCGUUAGGUAUAAGG-3′, FUT3; sense, 5′-CCGCACUGCUAUUUCAGCUGCUGGU-3′, antisense, 5′-ACCAGCAGCUGAAAUAGCAGUGCGG-3′, FUT6; sense, 5′-GCUGUCUGACCACGCUGCUGUUUCA-3′, antisense, 5′-UGAAACAGCAGCGUGGUCAGACAGC-3′. Small interfering RNA transfection experiments were carried out using TransMessenger transfection reagent (Qiagen, Hamburg, Germany) with 100 nM siRNA according to the manufacturer's instructions (Qiagen). Forty hours after siRNA transfection, cells were analysed for FUT mRNA expression and used in the experiments described below.
Wound healing assay and cell migration assay
Cells were harvested 48 h after transfection and then wound healing and cell migration assays were conducted using CytoSelect Wound Healing and Cell Migration assay kits (Cell Biolabs Inc., San Diego, CA, USA), respectively, according to the manufacturer's instructions. In brief, the wound healing assay was performed using a 24-well plate with CytoSelect Wound Healing Inserts. Cell suspensions containing 5 × 105 cells were added to the wells and incubated overnight. After removing the inserts, the cells were incubated for varying time periods as indicated and the wound healing surface area was calculated. Cell invasion was measured with a CytoSelect Cell Migration assay kit (Cell Biolabs Inc.). Cells were starved overnight in serum-free medium and resuspended at a concentration of 2.5 × 105 cells per ml in serum-free medium containing 0.1% BSA. Cell suspension (0.2 ml) was added to the top of each well, and 10 mg ml−1 fibronectin solution was added to the bottom well of the chamber as a chemoattractant. Forty-eight hours later, the cells remaining in the top chamber were carefully removed from the upper surface of the filters using a cotton swab. Cells that migrated to the lower surface of the filter were fixed with methanol and stained with methylene blue. Cell migration was quantitated by counting five random fields per filter at × 40 magnification. Data are presented as the mean number of cells per high-power field based on triplicate measurements from two independent experiments.
Western blotting and immunoprecipitation
Cells were solubilised in 1% Triton X-100 lysis buffer (20 mM Tris-HCl, pH 7.4, 10 mM EGTA, 10 mM MgCl2, 1 mM Na3VO4, 20 mM NaF, 2 μg ml−1 aprotinin, 5 μg ml−1 leupeptin and 0.1 mM phenylmethylsulfonyl fluoride), and then centrifuged at 15 000 g for 15 min. The supernatants were collected and protein concentrations were determined using a BCA protein assay kit (Thermo Scientific Inc., Rockford, IL, USA). Equal amounts of protein were run on 4–20% SDS–PAGE under reducing conditions and then transferred to PVDF membranes (Millipore Corp., Billerica, MA, USA). The blots were probed with anti-FUT3, anti-FUT6 antibodies (Abcam, Cambridge, MA, USA), anti-pSmad2, anti-pHSP27, anti-p-p38, anti-Snail, anti-ZEB1 and anti-E-cadherin antibodies (Cell Signaling, Beverly, MA, USA). Immunoreactive bands were visualised using an ECL kit (GE Healthcare Science, Pittsburgh, PA, USA). These membranes were stripped using stripping buffer (Thermo Scientific Inc.) and reprobed with an antibody against the corresponding proteins Smad2, HSP27 and p38 (Cell Signaling) to confirm equal loading. For the immunoprecipitation assay, cell lysates (∼1 mg of protein) prepared as described above, were incubated with anti-TβR-I or TβR-II antibody (Cell Signaling) overnight at 4 °C with gentle rocking. The immunoprecipitate was washed five times with lysis buffer and lectin blotting was performed as described below. The blots were quantified using LAS-4000UV mini and MultiGauge software (Fujifilm, Tokyo, Japan). Western blotting and immunoprecipitation studies for the indicated antibodies were performed three times to confirm the results.
Lectin blotting analysis
Whole-cell lysate or immunoprecipitate was subjected to 4–20% SDS–PAGE and transferred to PVDF membranes. The membranes were blocked with 5% BSA in Tris-buffered saline with 0.05% Tween-20 (TBST) overnight at 4 °C and then incubated with 0.5 μg ml−1 biotinylated Aleuria aurantia lectin (AAL; J-Oil Mills, Tokyo, Japan), which preferentially recognises Fucα1,3GlcNAc and Fucα1,6GlcNAc, in TBST for 1 h at room temperature. After washing with TBST four times, the membrane was incubated with HRP-conjugated streptavidin for 30 min, and lectin-reactive proteins were then detected using an ECL kit (GE Healthcare Science). The blots were quantified using LAS-4000UV mini and MultiGauge software (Fujifilm). Western blot and immunoprecipitation studies for the indicated antibodies were performed three times for confirmation of results.
Immunofluorescence
Cells were rinsed twice with PBS, fixed in paraformaldehyde (PFA) 4% for 10 min at RT, dried, washed with PBS and blocked for 1 h in 0.1% BSA in PBS. Filters were then incubated first with Ab (diluted in blocking solution) for 1 h, washed five times in PBS containing 0.05% Tween, treated with similarly prepared dilutions of secondary antibodies for 30 min and washed again as above. Tetramethylrhodamine isothiocyanate-conjugated secondary antibodies against rabbit IgG (Jackson ImmunoResearch Laboratories, West Grove, PA, USA) were diluted 1 : 1000. Confocal analysis was performed using a Leica TCS-NT confocal microscope and the expression level of E-cadherin was quantified by NIH Image.
Statistics
Results are presented as the mean (± s.d.) for each sample. Differences between the two groups were examined by unpaired t-test and paired t-test. If two groups could not be considered to be of equal variance, t-test with Welch's correction was performed.
Additional materials and methods are available in Supplementary Information Online.
Results
Both FUT3 and FUT6 are essential for activation of Smad signalling upon TGF-β stimulation
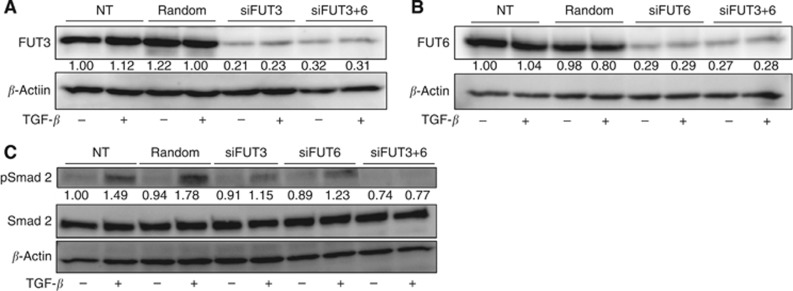
To elucidate the mechanism by which cell growth and invasion is regulated by FUT3 and FUT6, we focused on TGF-β signalling, as TGF-β has been reported to have an important role in EMT, which triggers cancer cell metastasis. In light of previous reports, we chose Colo205 cells for the following examination, as Colo205 cells have been reported to carry no TβR mutations, and Ls174T cells that express high CA19-9 carry mutant TβR (Ilyas et al, 1999; Pasche et al, 2005). Furthermore, Colo205 cells express high levels of FUT3/6 and they secrete CA19-9 and sLex (Supplementary Figure 1A–C). We first examined the protein expression level of FUT3 and FUT6 upon TGF-β stimulation in cells transfected with random siRNA, siRNA for FUT3 (siFUT3), and/or siRNA for FUT6 (siFUT6) (Figure 1A and B; Supplementary Figure 2), and found that the expression level of FUT3 or FUT6 was not changed by TGF-β stimulation even in the presence or absence of siRNA. Although, as shown in Figure 1C, activation of Smad2 was suppressed in cells transfected with siFUT3 or siFUT6 but not in random siRNA-transfected cells. In the presence of both siFUT3 and siFUT6, phosphorylation of Smad2 was further inhibited upon TGF-β stimulation (Figure 1C). When other FUTs were suppressed by each siRNA, Smad2 phosphorylation status was not affected upon TGF-β stimulation, indicating that FUT3 and/or FUT6 were required for TGF-β signalling in CRC cell lines (Supplementary Figure 3).
Figure 1.
Suppression of FUT3 and FUT6 inhibits Smad2 phosphorylation upon TGF-β stimulation. (A and B) Western blot analysis for FUT3 (A) and FUT6 (B). Lysate from Colo205 cells transfected with indicated siRNAs was electrophoresed and immunoblotted with FUT3 and FUT6 antibodies. The same membranes were reprobed with β-actin to verify equal amounts of protein. (C) FUT3 and FUT6 were required for phosphorylation of Smad2. Colo205 cells transfected with random, siRNA for FUT3 (siFUT3), siRNA for FUT6 (siFUT6) or siRNA for FUT3 and 6 (siFUT3+6) were treated with TGF-β for 6 h, then probed with pSmad2. Western blots for β-actin and Smad2 represent equally loaded amounts of protein. The experiments were repeated three times to confirm the results.
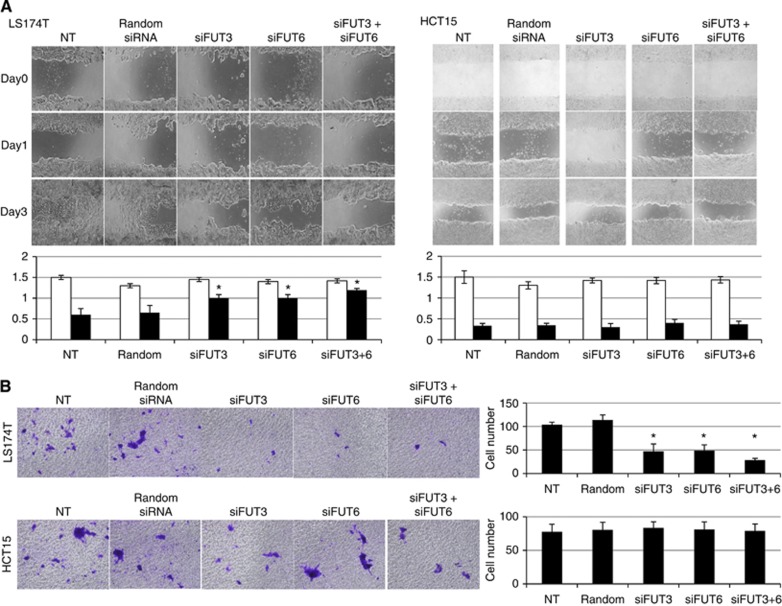
Suppression of FUT3 and FUT6 resulted in inhibition of wound healing and cell invasion
In order to investigate the effect of FUT3 and/or FUT6 on cell invasion and migration, we performed wound healing and invasion assays. With regard to FUT3 and FUT6 expressions, we chose two cell lines that expressed high and low levels of FUT3/6 regardless of TβR status (Supplementary Figure 1). In cells that express high levels of FUT3/6, CA19-9 and sLex were also highly expressed, but this was not the case in the cells expressing low levels of FUT3/6 (Supplementary Figure 1). As shown in Figure 2A, the migration area of parental (non-treated, NT) or random siRNA transfected-Ls174T cells, which expressed high levels of FUT3/6, was decreased from 1.5±0.15 mm2 to 0.6±0.15 mm2 in NT and from 1.3±0.08 mm2 to 0.65±0.17 mm2 in random siRNA after 2 days, respectively. In contrast, the migration area of cells transfected with siRNA for FUT3 and/or FUT6 (siFUT3 0.45 mm2 reduction, siFUT6 0.4 mm2 reduction and siFUT3+6 0.23 mm2 reduction) was significantly lower compared with NT or random siRNA-transfected-cells. However, in cells expressing low levels of FUT3/6 (HCT15 cells), suppression of cell migration induced by siRNA transfection for FUT3 and/or FUT6 was not observed (Figure 2). Furthermore, the invasion assay revealed that the number of invaded cells was inhibited by siFUT3 and/or siFUT6 in Ls174T cells but not in HCT15 cells (Figure 2B), suggesting that FUT3 and/or FUT6 have an important role in cell migration and invasion in CA19-9-producing cells.
Figure 2.
Suppression of either FUT3 and/or FUT6 by siRNA resulted in inhibition of cell migration and cell invasion. (A) Wound healing assay for CRC cell lines transfected with siFUT3 and/or siFUT6. Representative photographs for the indicated conditions (upper panel). Wound field surface area was calculated according to the manufacturer's instructions. Lower panel shows the average wound field surface area based on randomly chosen wells. *P<0.05 (NT or random vs. FUT3, FUT6, FUT3+6). (B) Cell invasion assay for CRC cell lines transfected with siFUT3 and/or siFUT6. Left panel shows representative photographs for the indicated conditions. Right panel shows the number of invaded cells that were transfected with the indicated siRNA. These results were confirmed by 3 independent experiments. *P<0.05 (NT or random vs FUT3, FUT6, FUT3+6).
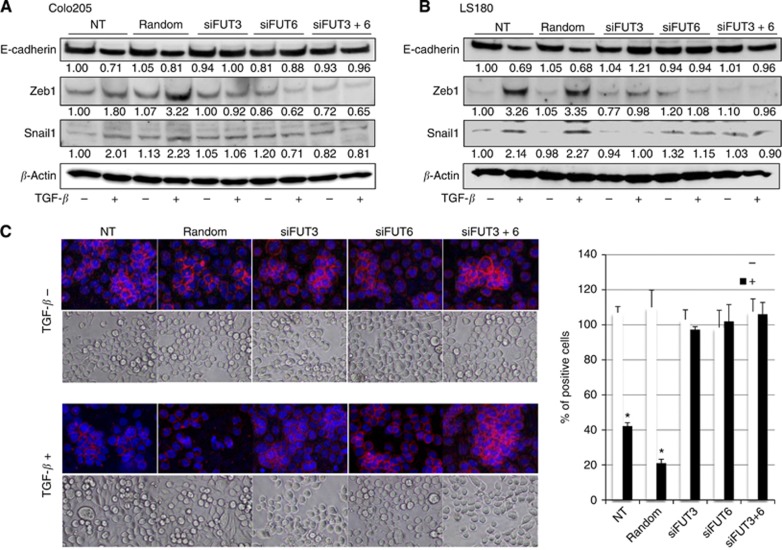
Inhibition of TGF-β-induced EMT in CRC cells by FUT3 and/or FUT6 siRNA
We next examined whether EMT of CRC cells induced by TGF-β stimulation could be affected by siRNA for FUT3 and/or FUT6 using Colo205 and LS180 cells, which have been reported to carry no TβR mutations. The expression of E-cadherin and the number of epithelial cells were reduced in parental and random siRNA-transfected cells upon TGF-β stimulation (Figure 3A–C). In contrast, zinc finger E-box binding (ZEB) transcription factor ZEB1 and snail expression were induced upon TFG-β stimulation in random siRNA-transfected cells but not in siFUT3- and/or siFUT6-transfected cells. However, these effects were not observed in cells transfected with siFUT3 and/or siFUT6, indicating that both FUT3 and/or FUT6 are required for TGF-β-induced cell signalling and EMT. These observations were confirmed in three independent experiments.
Figure 3.
Suppression of FUT3 and/or FUT6 inhibits TGF-β-induced EMT. (A and B) Suppression of EMT by siFUT3 and/or siFUT6. Colo205 (A) and LS180 (B) cells were treated with TGF-β for 3 days after transduction with random siRNA, siFUT3 and/or siFUT6, then probed with Zeb1, Snail and E-cadherin. Western blot for β-actin was used to control for equal protein loading. The relative mean density is presented as the ratio to no treatment (NT). (C) Representative images of Colo205 cells and immunohistochemical staining for E-cadherin with or without TGF-β. Cells were treated with TGF-β for 3 days after transduction with random siRNA, siFUT3, and/or siFUT6, then probed with E-cadherin and visualised by TRITC. The expression of E-cadherin was quantified and presented as the ratio to no treatment (right panel). The results were confirmed by three independent experiments.
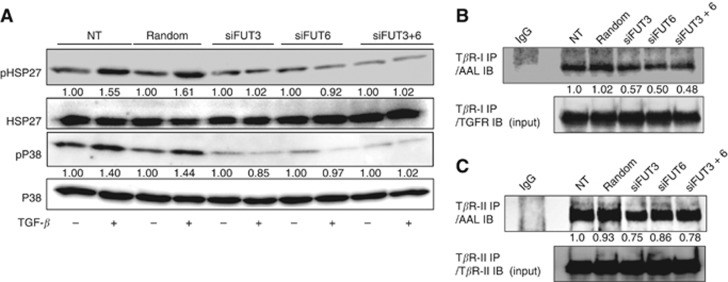
We performed a protein array analysis to identify molecules related to cancer cell metastasis that were downregulated by siFUT3 or siFUT6 using protein array (data not shown). In Colo205 cells transfected with siRNA for FUT3 or FUT6, phosphorylation of HSP27 and p38delta was found to be downregulated compared with mock-transfected cells (data not shown). Hsp27 and p38delta have been reported to have important roles in cancer metastasis (Hedges et al, 1999; Wang et al, 2002; Shin et al, 2005; Tan et al, 2010; Zhu et al, 2010; Kwon et al, 2011). We verified the phosphorylation status of Hsp27 and p38delta using serum-starved cell lysates. As shown in Figure 4A, siRNA for FUT3 and/or FUT6 suppressed phosphorylation of both molecules, but phosphorylation was not affected in random siRNA-transfected or parental cells upon TGF-β stimulation, suggesting that FUT3 and/or FUT6 are required for HSP27 and p38delta activation in TGF-β signalling.
Figure 4.
Introduction of siFUT3 and/or siFUT6 resulted in inhibition of HSP27 and p38 activation through suppression of TβR-I fucosylation. (A) Phosphorylation of HSP27 and p38 was inhibited by downregulation of FUT3 and/or FUT6. Colo205 cells transfected with random, siFUT3, siFUT6 or siFUT3+6 were treated with TGF-β under the conditions described in the text, harvested and used for western blotting. (B and C) Colo205 cells transfected with random, siFUT3, siFUT6 or siFUT3+siFUT6 were solubilised and immunoprecipitated with TβR-I (B) and TβR-II (C) antibodies. TβR-I and TβR-II-bound proteins were probed with biotinylated-AAL. The relative mean density is presented as the ratio to no treatment (NT). The results were confirmed by three independent experiments.
Downregulation of TβR fucosylation by FUT3 and/or FUT6 siRNA
We next investigated the requirement for FUT3 and/or FUT6 in TβR fucosylation using lectin blot analysis. In a preliminary experiment, we found that TGF-β stimulation itself did not affect fucosylation of TβR (Supplementary Figure 4). However, siFUT3 and/or siFUT6 decreased the fucosylation status of type I TβR (TβR-I) by 50% compared with NT or random siRNA treatment. In contrast, the fucosylation status of type II TβR (TβR-II) was inhibited to a lesser extent by siFUT3 and/or siFUT6, indicating that activation of Smads and downstream signalling were dependent on fucosylation of TβR-I and minimally on TβR-II in CRC cell lines (Figure 4B and C). Furthermore, when fucosylated-TβRs were detected by CA19-9 or sLex directly by each of the specific antibodies, reduction of each expression was observed (Supplementary Figure 5), indicating that TβR-bound CA19-9 and sLex might exist and regulate its signal transduction pathway directly. But further study should be required for future work.
The results of the study indicated that colorectal adenocarcinoma cells actively take up L-fucose, which accelerates their metastatic potential, and produce CA19-9. Therefore, L-fucose-bound nanoparticles, which we previously developed, might be suitable as a new therapeutic strategy, especially for treating patients with CRC expressing FUT3 or FUT6 (Yoshida et al, 2012).
Discussion
The present study demonstrates that FUT3 and FUT6 activate TGF-β signalling through fucosylation of TβR-I in CA19-9 and/or sLex-producing CRC cells, leading to augmentation of their malignant potential.
It has been shown that enhanced activity of FUT3/6 induces sLea (CA19-9) and sLex expression, respectively, and potentiates the malignant potential of metastatic CRC (Kannagi et al, 2004). These glycans induced by FUT promote extravasation of cancer cells via interacting with E-selectin on endothelial cells (Weston et al, 1999; Hiller et al, 2000; Kanoh et al, 2003; Kannagi et al, 2004), but the molecular mechanisms remain unclear. In this study, we revealed that activation of HSP27 and p38, which mediate cell motility and migration, was downregulated by inhibition of TβR-I fucosylation induced by siFUT3 and siFUT6, resulting in the suppression of EMT.
Transforming growth factor-β has an important role in EMT by combining both Smad- and non-Smad-dependent signalling pathways (Katsuno et al, 2013). In Smad-dependent signalling, Smads and Snail (EMT transcription factor) bind to regulatory promoter sequences of the gene encoding E-cadherin, leading to TGF-β-induced suppression of its expression (Vincent et al, 2009). Thus, the inhibition of E-cadherin expression induced by siFUT3/6 is considered to be mediated by the inactivation of the Smad pathway.
In relation to the Smad-independent pathway, p38 has been reported to have an important role in TGF-β-induced EMT (Yu et al, 2002; Kolosova et al, 2011; Moustakas and Heldin, 2012). Although the downstream pathway of p38 in TGF-β-induced EMT is not fully understood, previous reports have indicated that a relationship exists between p38 and HSP27 (Hedges et al, 1999; Wang et al, 2002). Our results suggest that inhibition of FUT3 and FUT6 resulted in downregulation of HSP27 phosphorylation, possibly through inactivation of p38 induced by the suppression of TGF-β signalling. The expression of p38 in patients with cholangeal cell carcinoma has been shown to be correlated with sensitivity to chemotherapeutic agents as well as disease prognosis (Tan et al, 2010). Furthermore, it has also been reported that HSP27 is associated with the metastatic potential of cancer cells (Zhu et al, 2010). These findings indicate that p38 and HSP27 are key molecules for cancer cell migration and metastasis in TGF-β signalling.
It has been demonstrated that FUT8 catalyses the transfer of a fucosyl moiety from GDP-fucose to the innermost GlcNAc residue of hybrid and complex N-linked oligosaccharides in glycoproteins via α(1,6)-linkage to form core-fucosylation. Knockdown of FUT8 by siRNA has been shown to inhibit EMT by suppressing the TGF-β signalling pathway due to inhibition of core-fucosylation of TGFβ-RII in renal tubular cells (Lin et al, 2011). Furthermore, in FUT8-knockout mice, the growth of mouse embryonic fibroblasts was suppressed by inhibition of EGF receptor activation because of downregulation of core-fucosylation of the receptor (Wang et al, 2006). Whereas, FUT3 or FUT6 adds α-1,3/1,4-fucose to GlcNAc residues in type 1 and type 2 precursors (de Vries et al, 2001). Our results obtained from CRC cells, based on lectin blot analysis, indicated that FUT3 and FUT6 regulate TGFβ-Rs via glycosylation sites aside from the core-fucosylation induced by FUT8. Nevertheless, further investigation will be necessary to clarify the sites within TβRs that are fucosylated by FUT3 and FUT6, and the mechanism of crosstalk in growth factor signalling induced by other FUTs such as FUT1, 8.
Overexpression of FUT3 and FUT6 might be predictive of a poor prognosis in patients with CRC not only because of the increased interaction between E-selectin and endothelial cells through sLea/sLex but also via activation of TGF-β signalling through EMT, leading to enhanced metastatic potential. It should be noted that EGF/bFGF signalling augments EMT by inducing sLea/sLex expression (Sakuma et al, 2012). In our preliminary examination, we observed that 80% of stage IV patients were positive for both FUT3 and FUT6 expressions (data not shown), although we could not show a significant correlation between the metastatic stage and FUT3/6 expression due to the small size of the study. Future investigation may be necessary to reliably determine whether such a correlation exists.
We previously demonstrated that L-fucose-mediated cell targeting is a promising new therapeutic strategy for CA19-9-producing pancreatic adenocarcinoma (Yoshida et al, 2012). Thus, fucose-targeting therapy could be effective for increasing survival in patients with metastatic CRC.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on British Journal of Cancer website (http://www.nature.com/bjc)
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Material
References
- Caja L, Bertran E, Campbell J, Fausto N, Fabregat I. The transforming growth factor-beta (TGF-beta) mediates acquisition of a mesenchymal stem cell-like phenotype in human liver cells. J Cell Physiol. 2011;226 (5:1214–1223. doi: 10.1002/jcp.22439. [DOI] [PubMed] [Google Scholar]
- Calon A, Espinet E, Palomo-Ponce S, Tauriello DV, Iglesias M, Cespedes MV, Sevillano M, Nadal C, Jung P, Zhang XH, Byrom D, Riera A, Rossell D, Mangues R, Massague J, Sancho E, Batlle E. Dependency of colorectal cancer on a TGF-beta-driven Program in stromal cells for metastasis initiation. Cancer cell. 2012;22 (5:571–584. doi: 10.1016/j.ccr.2012.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham D, Atkin W, Lenz HJ, Lynch HT, Minsky B, Nordlinger B, Starling N. Colorectal cancer. Lancet. 2010;375 (9719:1030–1047. doi: 10.1016/S0140-6736(10)60353-4. [DOI] [PubMed] [Google Scholar]
- de Vries T, Knegtel RM, Holmes EH, Macher BA. Fucosyltransferases: structure/function studies. Glycobiology. 2001;11 (10:119R–128R. doi: 10.1093/glycob/11.10.119r. [DOI] [PubMed] [Google Scholar]
- Filella X, Molina R, Grau JJ, Pique JM, Garcia-Valdecasas JC, Astudillo E, Biete A, Bordas JM, Novell A, Campo E, et al. Prognostic value of CA 19.9 levels in colorectal cancer. Annals of surgery. 1992;216 (1:55–59. doi: 10.1097/00000658-199207000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabowski P, Mann B, Mansmann U, Lovin N, Foss HD, Berger G, Scherubl H, Riecken EO, Buhr HJ, Hanski C. Expression of SIALYL-Le(x) antigen defined by MAb AM-3 is an independent prognostic marker in colorectal carcinoma patients. Int J Cancer. 2000;88 (2:281–286. [PubMed] [Google Scholar]
- Grandclement C, Pallandre JR, Valmary Degano S, Viel E, Bouard A, Balland J, Remy-Martin JP, Simon B, Rouleau A, Boireau W, Klagsbrun M, Ferrand C, Borg C. Neuropilin-2 expression promotes TGF-beta1-mediated epithelial to mesenchymal transition in colorectal cancer cells. PLoS One. 2011;6 (7:e20444. doi: 10.1371/journal.pone.0020444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakomori S, Kannagi R. Glycosphingolipids as tumor-associated and differentiation markers. J Natl Cancer Inst. 1983;71 (2:231–251. [PubMed] [Google Scholar]
- Hedges JC, Dechert MA, Yamboliev IA, Martin JL, Hickey E, Weber LA, Gerthoffer WT. A role for p38(MAPK)/HSP27 pathway in smooth muscle cell migration. J Biol Chem. 1999;274 (34:24211–24219. doi: 10.1074/jbc.274.34.24211. [DOI] [PubMed] [Google Scholar]
- Hiller KM, Mayben JP, Bendt KM, Manousos GA, Senger K, Cameron HS, Weston BW. Transfection of alpha(1,3)fucosyltransferase antisense sequences impairs the proliferative and tumorigenic ability of human colon carcinoma cells. Mol Carcinog. 2000;27 (4:280–288. [PubMed] [Google Scholar]
- Ilyas M, Efstathiou JA, Straub J, Kim HC, Bodmer WF. Transforming growth factor beta stimulation of colorectal cancer cell lines: type II receptor bypass and changes in adhesion molecule expression. Proc Natl Acad Sci USA. 1999;96 (6:3087–3091. doi: 10.1073/pnas.96.6.3087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jen J, Kim H, Piantadosi S, Liu ZF, Levitt RC, Sistonen P, Kinzler KW, Vogelstein B, Hamilton SR. Allelic loss of chromosome 18q and prognosis in colorectal cancer. N Engl J Med. 1994;331 (4:213–221. doi: 10.1056/NEJM199407283310401. [DOI] [PubMed] [Google Scholar]
- Kaimori A, Potter J, Kaimori JY, Wang C, Mezey E, Koteish A. Transforming growth factor-beta1 induces an epithelial-to-mesenchymal transition state in mouse hepatocytes in vitro. J Biol Chem. 2007;282 (30:22089–22101. doi: 10.1074/jbc.M700998200. [DOI] [PubMed] [Google Scholar]
- Kannagi R, Izawa M, Koike T, Miyazaki K, Kimura N. Carbohydrate-mediated cell adhesion in cancer metastasis and angiogenesis. Cancer Sci. 2004;95 (5:377–384. doi: 10.1111/j.1349-7006.2004.tb03219.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanoh A, Ota M, Narimatsu H, Irimura T. Expression levels of FUT6 gene transfected into human colon carcinoma cells switch two sialyl-Lewis X-related carbohydrate antigens with distinct properties in cell adhesion. Biochem Biophys Res Commun. 2003;303 (3:896–901. doi: 10.1016/s0006-291x(03)00420-0. [DOI] [PubMed] [Google Scholar]
- Karapetis CS, Khambata-Ford S, Jonker DJ, O'Callaghan CJ, Tu D, Tebbutt NC, Simes RJ, Chalchal H, Shapiro JD, Robitaille S, Price TJ, Shepherd L, Au HJ, Langer C, Moore MJ, Zalcberg JR. K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med. 2008;359 (17:1757–1765. doi: 10.1056/NEJMoa0804385. [DOI] [PubMed] [Google Scholar]
- Katsuno Y, Lamouille S, Derynck R. TGF-beta signaling and epithelial-mesenchymal transition in cancer progression. Curr Opin Oncol. 2013;25 (1:76–84. doi: 10.1097/CCO.0b013e32835b6371. [DOI] [PubMed] [Google Scholar]
- Kolosova I, Nethery D, Kern JA. Role of Smad2/3 and p38 MAP kinase in TGF-beta1-induced epithelial-mesenchymal transition of pulmonary epithelial cells. J Cell Physiol. 2011;226 (5:1248–1254. doi: 10.1002/jcp.22448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koprowski H, Herlyn M, Steplewski Z, Sears HF. Specific antigen in serum of patients with colon carcinoma. Science. 1981;212 (4490:53–55. doi: 10.1126/science.6163212. [DOI] [PubMed] [Google Scholar]
- Kouri M, Pyrhonen S, Kuusela P. Elevated CA19-9 as the most significant prognostic factor in advanced colorectal carcinoma. J Surg Oncol. 1992;49 (2:78–85. doi: 10.1002/jso.2930490204. [DOI] [PubMed] [Google Scholar]
- Kwon SM, Kim SA, Fujii S, Maeda H, Ahn SG, Yoon JH. Transforming growth factor beta1 promotes migration of human periodontal ligament cells through heat shock protein 27 phosphorylation. Biol Pharm Bull. 2011;34 (4:486–489. doi: 10.1248/bpb.34.486. [DOI] [PubMed] [Google Scholar]
- Leivonen SK, Kahari VM. Transforming growth factor-beta signaling in cancer invasion and metastasis. Int J Cancer. 2007;121 (10:2119–2124. doi: 10.1002/ijc.23113. [DOI] [PubMed] [Google Scholar]
- Lin H, Wang D, Wu T, Dong C, Shen N, Sun Y, Xie H, Wang N, Shan L. Blocking core fucosylation of TGF-beta1 receptors downregulates their functions and attenuates the epithelial-mesenchymal transition of renal tubular cells. Am J Physiol Renal Physiol. 2011;300 (4:F1017–F1025. doi: 10.1152/ajprenal.00426.2010. [DOI] [PubMed] [Google Scholar]
- Liu YC, Yen HY, Chen CY, Chen CH, Cheng PF, Juan YH, Chen CH, Khoo KH, Yu CJ, Yang PC, Hsu TL, Wong CH. Sialylation and fucosylation of epidermal growth factor receptor suppress its dimerization and activation in lung cancer cells. Proc Natl Acad Sci USA. 2011;108 (28:11332–11337. doi: 10.1073/pnas.1107385108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsumoto K, Yokote H, Arao T, Maegawa M, Tanaka K, Fujita Y, Shimizu C, Hanafusa T, Fujiwara Y, Nishio K. N-Glycan fucosylation of epidermal growth factor receptor modulates receptor activity and sensitivity to epidermal growth factor receptor tyrosine kinase inhibitor. Cancer Sci. 2008;99 (8:1611–1617. doi: 10.1111/j.1349-7006.2008.00847.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyazaki K, Ohmori K, Izawa M, Koike T, Kumamoto K, Furukawa K, Ando T, Kiso M, Yamaji T, Hashimoto Y, Suzuki A, Yoshida A, Takeuchi M, Kannagi R. Loss of disialyl Lewis(a), the ligand for lymphocyte inhibitory receptor sialic acid-binding immunoglobulin-like lectin-7 (Siglec-7) associated with increased sialyl Lewis(a) expression on human colon cancers. Cancer Res. 2004;64 (13:4498–4505. doi: 10.1158/0008-5472.CAN-03-3614. [DOI] [PubMed] [Google Scholar]
- Moustakas A, Heldin CH. Induction of epithelial-mesenchymal transition by transforming growth factor beta. Sem Cancer Biol. 2012;22 (5-6:446–454. doi: 10.1016/j.semcancer.2012.04.002. [DOI] [PubMed] [Google Scholar]
- Muinelo-Romay L, Villar-Portela S, Cuevas Alvarez E, Gil-Martin E, Fernandez-Briera A. alpha(1,6)Fucosyltransferase expression is an independent prognostic factor for disease-free survival in colorectal carcinoma. Hum Pathol. 2011;42 (11:1740–1750. doi: 10.1016/j.humpath.2011.01.021. [DOI] [PubMed] [Google Scholar]
- Nakagoe T, Fukushima K, Tanaka K, Sawai T, Tsuji T, Jibiki M, Nanashima A, Yamaguchi H, Yasutake T, Ayabe H, Arisawa K. Evaluation of sialyl Lewis(a), sialyl Lewis(x), and sialyl Tn antigens expression levels as predictors of recurrence after curative surgery in node-negative colorectal cancer patients. J Exp Clin Cancer Res. 2002;21 (1:107–113. [PubMed] [Google Scholar]
- Narimatsu H, Iwasaki H, Nakayama F, Ikehara Y, Kudo T, Nishihara S, Sugano K, Okura H, Fujita S, Hirohashi S. Lewis and secretor gene dosages affect CA19-9 and DU-PAN-2 serum levels in normal individuals and colorectal cancer patients. Cancer Res. 1998;58 (3:512–518. [PubMed] [Google Scholar]
- Ogunbiyi OA, Goodfellow PJ, Herfarth K, Gagliardi G, Swanson PE, Birnbaum EH, Read TE, Fleshman JW, Kodner IJ, Moley JF. Confirmation that chromosome 18q allelic loss in colon cancer is a prognostic indicator. J Clin Oncol. 1998;16 (2:427–433. doi: 10.1200/JCO.1998.16.2.427. [DOI] [PubMed] [Google Scholar]
- Park JJ, Yi JY, Jin YB, Lee YJ, Lee JS, Lee YS, Ko YG, Lee M. Sialylation of epidermal growth factor receptor regulates receptor activity and chemosensitivity to gefitinib in colon cancer cells. Biochem Pharmacol. 2012;83 (7:849–857. doi: 10.1016/j.bcp.2012.01.007. [DOI] [PubMed] [Google Scholar]
- Pasche B, Knobloch TJ, Bian Y, Liu J, Phukan S, Rosman D, Kaklamani V, Baddi L, Siddiqui FS, Frankel W, Prior TW, Schuller DE, Agrawal A, Lang J, Dolan ME, Vokes EE, Lane WS, Huang CC, Caldes T, Di Cristofano A, Hampel H, Nilsson I, von Heijne G, Fodde R, Murty VV, de la Chapelle A, Weghorst CM. Somatic acquisition and signaling of TGFBR1*6A in cancer. JAMA. 2005;294 (13:1634–1646. doi: 10.1001/jama.294.13.1634. [DOI] [PubMed] [Google Scholar]
- Petrioli R, Licchetta A, Roviello G, Pascucci A, Francini E, Bargagli G, Conca R, Miano ST, Marzocca G, Francini G. CEA and CA19.9 as early predictors of progression in advanced/metastatic colorectal cancer patients receiving oxaliplatin-based chemotherapy and bevacizumab. Cancer Invest. 2012;30 (1:65–71. doi: 10.3109/07357907.2011.629380. [DOI] [PubMed] [Google Scholar]
- Picon A, Gold LI, Wang J, Cohen A, Friedman E. A subset of metastatic human colon cancers expresses elevated levels of transforming growth factor beta1. Cancer Epidemiol Biomarkers Prev. 1998;7 (6:497–504. [PubMed] [Google Scholar]
- Popat S, Houlston RS. A systematic review and meta-analysis of the relationship between chromosome 18q genotype, DCC status and colorectal cancer prognosis. Eur J Cancer. 2005;41 (14:2060–2070. doi: 10.1016/j.ejca.2005.04.039. [DOI] [PubMed] [Google Scholar]
- Popat S, Hubner R, Houlston RS. Systematic review of microsatellite instability and colorectal cancer prognosis. J Clin Oncol. 2005;23 (3:609–618. doi: 10.1200/JCO.2005.01.086. [DOI] [PubMed] [Google Scholar]
- Sakuma K, Aoki M, Kannagi R. Transcription factors c-Myc and CDX2 mediate E-selectin ligand expression in colon cancer cells undergoing EGF/bFGF-induced epithelial-mesenchymal transition. Proc Natl Acad Sci USA. 2012;109 (20:7776–7781. doi: 10.1073/pnas.1111135109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin KD, Lee MY, Shin DS, Lee S, Son KH, Koh S, Paik YK, Kwon BM, Han DC. Blocking tumor cell migration and invasion with biphenyl isoxazole derivative KRIBB3, a synthetic molecule that inhibits Hsp27 phosphorylation. J Biol Chem. 2005;280 (50:41439–41448. doi: 10.1074/jbc.M507209200. [DOI] [PubMed] [Google Scholar]
- Tan FL, Ooi A, Huang D, Wong JC, Qian CN, Chao C, Ooi L, Tan YM, Chung A, Cheow PC, Zhang Z, Petillo D, Yang XJ, Teh BT. p38delta/MAPK13 as a diagnostic marker for cholangiocarcinoma and its involvement in cell motility and invasion. Int J Cancer. 2010;126 (10:2353–2361. doi: 10.1002/ijc.24944. [DOI] [PubMed] [Google Scholar]
- Tsuchida A, Okajima T, Furukawa K, Ando T, Ishida H, Yoshida A, Nakamura Y, Kannagi R, Kiso M, Furukawa K. Synthesis of disialyl Lewis a (Le(a)) structure in colon cancer cell lines by a sialyltransferase, ST6GalNAc VI, responsible for the synthesis of alpha-series gangliosides. J Biol Chem. 2003;278 (25:22787–22794. doi: 10.1074/jbc.M211034200. [DOI] [PubMed] [Google Scholar]
- Tsushima H, Ito N, Tamura S, Matsuda Y, Inada M, Yabuuchi I, Imai Y, Nagashima R, Misawa H, Takeda H, Matsuzawa Y, Kawata S. Circulating transforming growth factor beta 1 as a predictor of liver metastasis after resection in colorectal cancer. Clin Cancer Res. 2001;7 (5:1258–1262. [PubMed] [Google Scholar]
- van Zijl F, Mair M, Csiszar A, Schneller D, Zulehner G, Huber H, Eferl R, Beug H, Dolznig H, Mikulits W. Hepatic tumor-stroma crosstalk guides epithelial to mesenchymal transition at the tumor edge. Oncogene. 2009;28 (45:4022–4033. doi: 10.1038/onc.2009.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent T, Neve EP, Johnson JR, Kukalev A, Rojo F, Albanell J, Pietras K, Virtanen I, Philipson L, Leopold PL, Crystal RG, de Herreros AG, Moustakas A, Pettersson RF, Fuxe J. A SNAIL1-SMAD3/4 transcriptional repressor complex promotes TGF-beta mediated epithelial-mesenchymal transition. Nature Cell Biol. 2009;11 (8:943–950. doi: 10.1038/ncb1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Ma R, Flavell RA, Choi ME. Requirement of mitogen-activated protein kinase kinase 3 (MKK3) for activation of p38alpha and p38delta MAPK isoforms by TGF-beta 1 in murine mesangial cells. J Biol Chem. 2002;277 (49:47257–47262. doi: 10.1074/jbc.M208573200. [DOI] [PubMed] [Google Scholar]
- Wang X, Gu J, Ihara H, Miyoshi E, Honke K, Taniguchi N. Core fucosylation regulates epidermal growth factor receptor-mediated intracellular signaling. J Biol Chem. 2006;281 (5:2572–2577. doi: 10.1074/jbc.M510893200. [DOI] [PubMed] [Google Scholar]
- Watanabe T, Wu TT, Catalano PJ, Ueki T, Satriano R, Haller DG, Benson AB, 3rd, Hamilton SR. Molecular predictors of survival after adjuvant chemotherapy for colon cancer. N Engl J Med. 2001;344 (16:1196–1206. doi: 10.1056/NEJM200104193441603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weston BW, Hiller KM, Mayben JP, Manousos GA, Bendt KM, Liu R, Cusack JC., Jr Expression of human alpha(1,3)fucosyltransferase antisense sequences inhibits selectin-mediated adhesion and liver metastasis of colon carcinoma cells. Cancer Res. 1999;59 (9:2127–2135. [PubMed] [Google Scholar]
- Weston BW, Smith PL, Kelly RJ, Lowe JB. Molecular cloning of a fourth member of a human alpha (1,3)fucosyltransferase gene family. Multiple homologous sequences that determine expression of the Lewis x, sialyl Lewis x, and difucosyl sialyl Lewis x epitopes. J Biol Chem. 1992;267 (34:24575–24584. [PubMed] [Google Scholar]
- Yoshida M, Takimoto R, Murase K, Sato Y, Hirakawa M, Tamura F, Sato T, Iyama S, Osuga T, Miyanishi K, Takada K, Hayashi T, Kobune M, Kato J. Targeting anticancer drug delivery to pancreatic cancer cells using a fucose-bound nanoparticle approach. Plos One. 2012;7 (7:e39545. doi: 10.1371/journal.pone.0039545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu L, Hebert MC, Zhang YE. TGF-beta receptor-activated p38 MAP kinase mediates Smad-independent TGF-beta responses. EMBO J. 2002;21 (14:3749–3759. doi: 10.1093/emboj/cdf366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang B, Halder SK, Kashikar ND, Cho YJ, Datta A, Gorden DL, Datta PK. Antimetastatic role of Smad4 signaling in colorectal cancer. Gastroenterology. 2010;138 (3:969–80 e1-3. doi: 10.1053/j.gastro.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Z, Xu X, Yu Y, Graham M, Prince ME, Carey TE, Sun D. Silencing heat shock protein 27 decreases metastatic behavior of human head and neck squamous cell cancer cells in vitro. Mol Pharm. 2010;7 (4:1283–1290. doi: 10.1021/mp100073s. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.