Abstract
Osteoarthritis afflicts millions of individuals across the world resulting in impaired quality of life and increased health costs. To understand this disease, physicians have been studying risk factors, such as genetic predisposition, aging, obesity, and joint malalignment; however have been unable to conclusively determine the direct etiology. Current treatment options are short-term or ineffective and fail to address pathophysiological and biochemical mechanisms involved with cartilage degeneration and the induction of pain in arthritic joints. OA pain involves a complex integration of sensory, affective, and cognitive processes that integrate a variety of abnormal cellular mechanisms at both peripheral and central (spinal and supraspinal) levels of the nervous system Through studies examined by investigators, the role of growth factors and cytokines has increasingly become more relevant in examining their effects on articular cartilage homeostasis and the development of osteoarthritis and osteoarthritis-associated pain. Catabolic factors involved in both cartilage degradation in vitro and nociceptive stimulation include IL-1, IL-6, TNF-α, PGE2, FGF-2 and PKCδ, and pharmacologic inhibitors to these mediators, as well as compounds such as RSV and LfcinB, may potentially be used as biological treatments in the future. This review explores several biochemical mediators involved in OA and pain, and provides a framework for the understanding of potential biologic therapies in the treatment of degenerative joint disease in the future.
Keywords: Osteoarthritis, cartilage, biochemical mediators, osteoarthritic pain
Introduction
Osteoarthritis (OA), a debilitating degenerative joint disease predominantly found in elderly individuals, is the principal source of physical disability resulting in increased health care costs and impaired quality of life in the United States [1]. The disease imparts a profound economic impact on today's society, with healthcare costs exceeding $60 billion per year and OA aggregate costs increasing to $185.5 billion per year based on 2007 data [2, 3]. By the year 2030, an estimated 25% of the adult population in the United States will be afflicted with OA resulting in some form of disability [4, 5]. While several risk factors have been associated with OA, including genetic predisposition [6], aging [4], obesity [7], and joint malalignment [8], the pathogenesis of OA remains largely unknown [4–6, 9–11].
Current non-arthroplasty treatment options for OA are short-term or ineffective, and fail to adequately address the underlying pathophysiological and biochemical mechanisms involved with cartilage degeneration and the induction of pain in arthritic joints. Investigations have been undertaken to focus on understanding many of these processes, with the goal of developing novel biological therapies that may slow and/or reverse cartilage degradation and provide pain relief. Here, we will review several biochemical mediators involved in OA, with an emphasis on factors mediating cartilage breakdown and the induction of pain in degenerative conditions.
Pathophysiology of Osteoarthritis
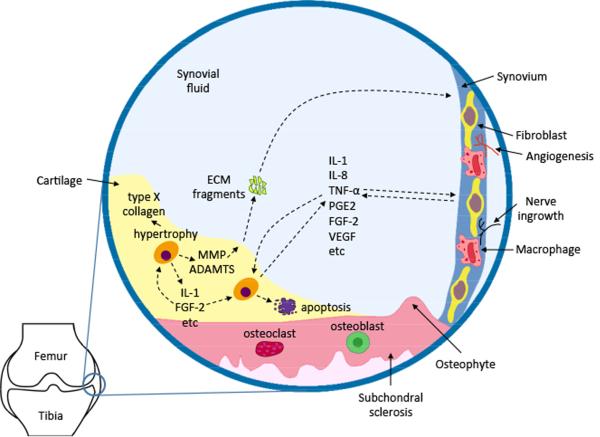
Under normal conditions, articular chondrocytes maintain a dynamic equilibrium between synthesis and degradation of extracellular matrix (ECM) components, including collagen type II and aggrecan, the most abundant proteoglycan (PG) in articular cartilage [11, 12]. In osteoarthritic states, however, a disruption of matrix equilibrium leads to progressive loss of cartilage tissue, clonal expansion of chondrocytes in the depleted regions, induction of oxidative states in a stressful cellular environment, and eventually, apoptosis of cells [9, 13]. With progression, there is usually an increase in both degradation and synthesis of ECM molecules within the joint, with an overall shift toward catabolism over anabolism. Chondrocyte metabolism is unbalanced due to excessive production of inflammatory cytokines and matrix-degrading enzymes, in conjunction with a downregulation of anabolic signaling, eventually leading to the destruction of ECM and subsequent cartilage degradation. Oxidative stress elicited by reactive oxygen species (ROS) further disturbs cartilage homeostasis and promotes catabolism via induction of cell death, breakdown of matrix components [14], upregulation of latent matrix-degrading enzyme production [15], inhibition of matrix synthesis, and oxidation of intracellular and extracellular molecules [11, 16]. Clinically, degradation of the ECM results in the gradual impairment of articular cartilage, often accompanied by pain and physical disability. Such cartilaginous changes also elicit profound pathological remodeling in the subchondral bone, typically in the form of sclerosis and osteophyte formation (Figure 1).
Figure 1.
Complex cellular interplay in synovial joint. In osteoarthritic state, aberrantly activated chondrocytes produce ECM-degrading proteases (MMPs, aggrecanases), pro-inflammatory cytokines (eg. IL-1), and catabolic growth factors (eg. FGF-2). These proteins can be secreted into synovial fluid, and subsequently act upon synoviocytes. Fragments derived from ECM degradation (eg. Fn-f) are also present in the synovial fluid as catabolic inducers. In OA, a subpopulation of chondrocytes undergoes hypertrophic changes, as manifested by their expression of type X collagen. Chondrocytes may also upregulate apoptosis, resulting in diminished local cellularity. In response to cartilage loss, pathological remodeling of subchondral bone gives rise to sclerosis and osteophyte formation. Synoviocytes (fibroblasts and macrophages) also actively synthesize proteases and cytokines which can negatively effect on the articular cartilage and synovium. Pathophysiological changes in synoviocytes pave the way for angiogenesis and innervations, which may account for OA pain [adapted from S. B. Abramson & M. Attur, Arthritis Res Ther 2009;11(3):227].
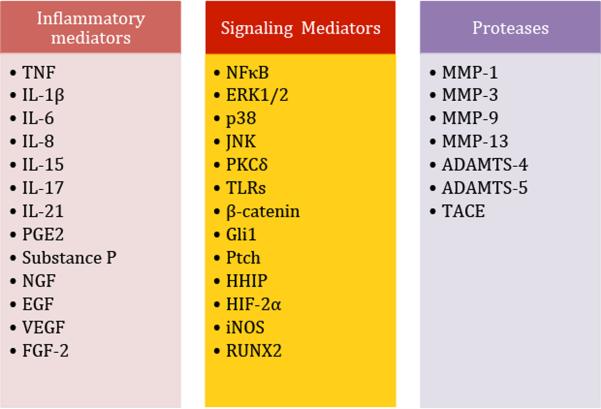
A series of catabolic and anabolic mediators have been found to play key roles in articular cartilage homeostasis and the development of OA (Figure 2). Many of the specific signaling cascades underlying the effects induced by catabolic and anabolic growth factors and cytokines remain inadequately characterized, but recent efforts have begun to further our understanding. Upregulation of catabolic processes and/or downregulation of anabolic processes leads to disruption of matrix equilibrium and subsequent cartilage degradation [14, 16–18]. The goal of biologic therapies is to impede joint destruction via inhibition of catabolic activity and/or upregulation of anabolic activity, thereby slowing or preventing the progression of OA. Previously, Ellman and colleagues presented a concise review of the literature on important factors involved in cartilage homeostasis [19]. Here, we focus on specific mediators that not only stimulate the induction of cartilage degradation, but also participate in nociceptive sensitization.
Figure 2.
Notable mediators in OA.
Osteoarthritis and Pain
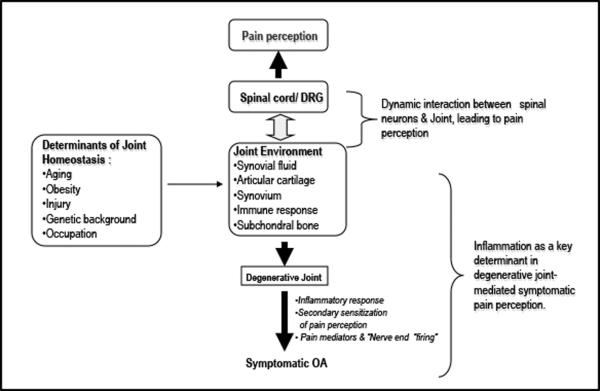
Clinically, pain is the most prominent and disabling symptom of OA. Arthritic pain is associated with inferior functional outcomes and reduced quality of life compared with a range of other chronic conditions [20]. OA pain involves a complex integration of sensory, affective, and cognitive processes that integrate a variety of abnormal cellular mechanisms at both peripheral (joints) and central (spinal and supraspinal) levels of the nervous system [10, 21–22] (Figure 3). Acute, adaptive pain, such as that following injury or surgery, serves a protective function and generally disappears after the injury heals [21]. In contrast, maladaptive chronic pain that persists beyond normal healing time or for more than 3–6 months may be considered pathologic as a symptom of ongoing disease. As OA-associated pain continues, severity and functional disability worsen due to a lack of effective preventative measures [5]. Research efforts have recently focused on the pain pathways involved in OA, as a better understanding of these molecular mechanisms may allow for the development of new therapeutic strategies to improve function and rein in the associated increase in healthcare costs [23–24].
Figure 3.
Pathophysiological status of each component in synovial joint is linked to joint degeneration and related pain perception. Local homeostasis inside the joint can be perturbed by various factors, such as aging, injury, and genetic predisposition. Low grade chronic inflammation in the joint not only contributes to accelerated cartilage damage and synovitis, but also renders the joint susceptible to peripheral sensitization and, in some cases, central sensitization.
Nociceptors are located throughout the joint in tissues peripheral to cartilage, including the joint capsule, ligaments, periosteum and subchondral bone [1, 25]. Joint cartilage and synovial injury influences peripheral afferent and dorsal root ganglion (DRG) neurons and sensitizes symptomatic pain perception through the dynamic interactions between neuropathic pathways and OA tissues [26]. Nociceptive input from the joint is processed via different spinal cord pathways, and inflammation may potentially reduce the threshold for nociceptive stimulus. These triggers are transmitted through the DRG, where they then travel up the spinothalamic tract to cortical centers for processing. The relative contribution of these processes into peripheral and central pathways appears to be strongly segmented, with intra-articular anesthetic studies in hip and knee OA suggestive of a peripheral drive to pain in approximately 60% to 80% of patients, depending on the affected joint [6, 27]. In some individuals, however, central mechanisms such as dysfunction of descending inhibitory control or altered cortical processing of noxious information, may play a greater role [28]. Therefore, research and pharmacotherapy for OA pain need to investigate two broad classes: central sensitization and peripheral sensitization, both leading to one final outcome: pain in a patient with OA.
Current “central” targets of pharmacotherapy for OA pain are numerous and include opioids, kinins, cannabinoids, and their respective receptors, in addition to adrenergic receptors, glutamate receptors, specific ion channels, and neurotrophins. The literature is replete with data on the alteration of pain pathways via inhibition of central processes [27]. By contrast, the peripheral processes linking pain with OA are lesser-known, and a better understanding of causative pro-inflammatory signaling that links OA with pain may allow clinicians to develop localized therapeutic regimens to treat OA symptoms via intraarticular injections [29]. Currently, there is a lack of a `gold standard' to relieve pain caused by OA, prompting recent research to focus more on understanding the pathophysiological mechanisms leading to joint degeneration and pain symptoms, with the aim of developing more long-term solutions via prevention and/or reversal of OA in the future [5, 14–15, 19, 30–34]. While much of this research is pre-translational, the potential for an injection of a particular mediator to induce anabolic, anti-catabolic, anti-inflammatory, and anti-pain effects in an arthritic joint via peripheral application is promising. Here, we will focus on select pro-inflammatory cytokines and mediators known to play a peripheral role in both cartilage degradation and pain processing, and briefly discuss two mediators with exciting therapeutic potential in the treatment of OA in the future, resveratrol (RSV) [35] and bovine lactoferricin (LfcinB) [36].
Catabolic & Pain Mediators in Osteoarthritis
Numerous mediators contribute to both degradative and nociceptive pathways associated with the progression of OA. Inflammatory stimuli initiate a cascade of events, including the release of cytokines by chondrocytes, leading to complex biochemical and mechanical interplay with other biological mediators to induce OA and promote pain [27, 37]. Particular mediators then stimulate hyperalgesia by a number of direct and indirect actions, including the sensitization of primary afferent fibers for mechanical stimuli. Examples include pro-inflammatory members from the interleukin family (IL-1, IL-6, and IL-17), tumor necrosis factor-α (TNF-α), and prostaglandin E2 (PGE2) (Figure 2). Each of these mediators not only stimulates the production of cartilage-degrading proteases to induce ECM degradation, but also contributes to OA-associated pain pathways. While many of the specific mechanisms involved in nociceptive sensitization by peripheral mediators remain largely unknown, the available literature demonstrates that these factors may be potential targets for novel biological therapies that may be used for prevention of OA and pain in the future [10, 13, 21, 37].
Interleukin-1
One of the most well-studied cytokines involved in OA, IL-1, has been shown to play a prominent role in both cartilage degradation and stimulation of nociceptive pathways [38–39]. IL-1 demonstrates potent bioactivities in inhibiting ECM synthesis and promoting cartilage breakdown, represses the expression of essential ECM components (ie. aggrecan and collagen type II) in chondrocytes [40–42], and induces a spectrum of proteolytic enzymes such as collagenases (MMP-1 and MMP-13) and ADAMTS-4, in both chondrocytes and synovial fibroblasts. Aside from these direct effects, IL-1β also induces a variety of other cytokines, including IL-6, IL-8, and leukemia inducing factor (LIF), which interact to induce additive or synergistic effects in the catabolic cascade. IL-1β has also been shown to activate nociceptors directly via intracellular kinase activation, and may also induce indirect nociceptive sensitization via the production of kinins and prostanoids [43]. This relationship is relevant to clinicians, as studies have demonstrated the possibility of associating patient cytokine levels with subjective outcome, pain perception, and radiographic findings of knee OA patients [44].
The significance of IL-1 in OA was further corroborated by in vivo studies and pharmaceutical efforts using IL-1 receptor antagonist (IL-1ra) as a potential therapeutic factor to prevent cartilage degeneration. As an inhibitory molecule of IL-1β, IL-1ra not only showed efficacy in OA animal models, but also improved clinical outcomes [45]. Both gene delivery and IL-1ra intra-articular injection models have been shown to impede OA progression, indicating anti-IL-1 therapy may be a viable option in OA disease modification [45–46].
IL-6
IL-6, another familiar pro-inflammatory cytokine with known involvement in cartilage degradation, has also been associated with hyperalgesia and hypersensitivity in joint tissues [47]. IL-6 plays an important role in the pathogenesis of rheumatoid arthritis, and its concentration is elevated in the serum and synovial fluid of arthritic patients [48–49]. Interestingly, primary afferent neurons also respond to IL-6 [50], suggesting a role of IL-6 in pain propagation in arthritic states. Indeed, more studies are warranted to elucidate the potential role of IL-6 in pain pathways associated with OA.
TNF-α
In addition to its potent catabolic effects in the pathophysiology of OA, TNF-α activates sensory neurons directly via the receptors TNFR1 and TNFR2, and initiates a cascade of inflammatory reactions via the production of IL-1, IL-6 and IL-8 [43, 51]. Direct TNF-α application in the periphery induces neuropathic pain, and this pain may be blocked by anti-inflammatory medications such as ibuprofen and celecoxib [52]. Anti-TNF-α treatment with a TNF antibody produces a prolonged reduction of pain symptoms in OA [53], and neutralization of TNF-α in mice rescues both mechanical hyperalgesia (testing of withdrawal responses in behavioral experiments) and the inflammatory process [54]. Taken together, TNF-α induces an analgesic effect, at least in part, via both neuronal and inflammatory stimulation. Antagonists to TNF-α, such as etanercept or infliximab, may serve as a potential therapeutic strategy to decrease OA pain clinically [27]. Further well-designed and controlled studies will help substantiate these promising preliminary data on TNF inhibitors in OA.
Prostanoids and PGE2
During pro-inflammatory states in articular cartilage, numerous prostanoid cyclooxygenase (COX) enzyme products are produced and released, including PGE2, PGD2, PGF2a, thromboxane, and PGI2 [27]. These factors serve as the premise for blocking the major synthetic enzymes COX-1 and COX-2 with either selective or non-selective COX-inhibitor medications (ie. NSAIDs, dexamethasone, or selective COX-2 inhibitors) [55]. COX activation has been shown to enhance production of matrix metalloproteinase-3, inhibit PG and collagen synthesis, and stimulate chondrocyte apoptosis.
Of these mediators, PGE2 is considered to be the major contributor to inflammatory pain in arthritic conditions. PGE2 exerts its effects via a variety of E prostanoid (EP) receptors (EP1, EP2, EP3, EP4), which are present in both peripheral sensory neurons and the spinal cord [27]. Activation of these receptors induces a variety of effects, ranging from calcium influx to cAMP activation or inhibition. Peripherally, sensitization of nociceptors by PGE2 is caused by the cAMP-mediated enhancement of sodium currents after ion channel phosphorylation [56]. However, in the spinal cord, PGE2 acts via different receptors than peripherally, suggesting further complexity in the prostanoid regulation of pain [57]. Several studies [58–59] have analyzed chondrocytes derived from tissue obtained during joint replacement surgery to understand the pathway of PGE2 synthesis. IL-1β has shown to stimulate and produce high levels of PGE2 that may induce pain and the degeneration with OA. Biochemically, IL-1β is noted to enhance the expression of COX-2 and microsomal prostaglandin E synthase-1 (mPGES-1) at the mRNA and protein levels [59]. It has been shown that increased production of PGE2 is concurrently accompanied by increases in mPGES-1 and COX-2 derived from OA chondrocytes stimulated with as IL-1β [59].
Previously in our laboratory, we have studied the role of PGE2 in human adult articular cartilage homeostasis and its relation to possible pain pathways [60]. PGE2 utilizes the EP2 and EP4 receptors to induce its downstream catabolic effects, and PGE2 may mediate pain pathways in articular cartilage via its stimulatory effect on the pain-associated factors IL-6 [47] and inducible nitric oxide synthase (iNOS) [58]. Further, when combined with the catabolic cytokine IL-1, PGE2 synergistically upregulates both IL-6 and iNOS mRNA levels in vitro [60]. Similar synergistic results were found with iNOS expression as well. Therefore, the EP2/4 receptor may be an important signaling initiator of the PGE2-signaling cascade and a potential target for therapeutic strategies aimed at preventing progression of arthritic disease and pain in the future.
As opposed to PGE2 EP receptor blockade, an alternative route of PGE2 inhibition is via the blockade of PGE synthase (PGES), a major route of conversion of prostaglandin H2 to PGE2 [27]. Two isoforms of the enzyme have been identified, membrane or microsomal associated (mPGES-1) and cytosolic (cPGES/p23), which are respectively linked with COX-2 and COX-1 dependent PGE2 production [61]. Both isoforms are upregulated by inflammatory mediators, and gene deletion studies in mice indicate an important role for mPGES in acute and chronic inflammation and inflammatory pain, revealing a potential target for pain treatment in OA [27,62].
FGF-2 and PKCδ
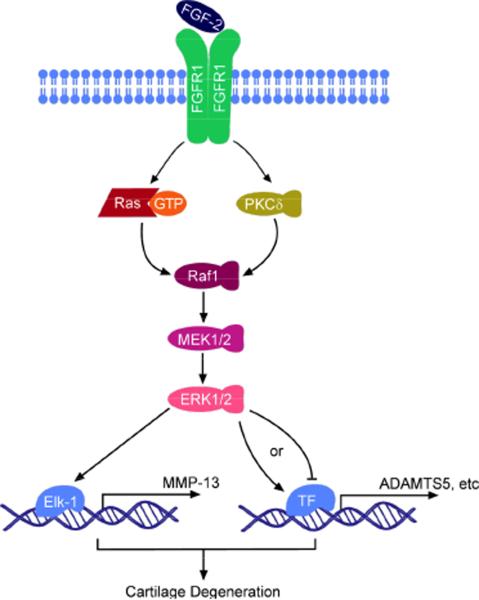
A consecutive line of evidence from our laboratory has demonstrated a potent catabolic and anti-anabolic role of FGF-2 in human cartilage homeostasis [63]. FGF-2 is released in supraphysiological amounts during loading and/or injury of the cartilage matrix and activates multiple transduction signal pathways (MAPKs), such as ERK, p38, and JNK [33]. These kinases in turn phosphorylate a set of transcription factors to regulate gene expression and modify cellular function, resulting in a decrease in PG synthesis and antagonism against anabolic growth factors, such as insulin-like growth factor 1 (IGF-1) and bone morphogenetic protein (BMP-7) in articular cartilage [33]. FGF-2 potently stimulates MMP-13 expression, which is the major type II collagen-degrading enzyme [33]. The FGFR1-Ras/PKCδ-Raf-MEK1/2-ERK1/2 signaling pathway is activated after FGF-2 stimulation, which mediates upregulation of matrix-degrading enzyme expression (ADAMTS-5 and MMP-13), as well as downregulation of aggrecan expression (Figure 4). Correspondingly, PKCδ inhibition significantly impairs these detrimental effects mediated by FGF-2 [19, 34, 63–64].
Figure 4.
Schematic model of FGF-2 signaling in articular chondrocytes. FGF-2 binds to FGFR1, which in turn activates both Ras and PKCδ. The signaling inputs then converge on the Raf1-MEK1/2-ERK1/2 axis. Activated ERK1/2 elicits transcription or repression of target genes mediated by a subset of transcription factors, including Elk-1 [adapted from D. Yan & H. J. Im et al., J Cell Biochem 2012].
It is worth noting that controversy over the role of FGF-2 in joint homeostasis does exist. Anabolic activity of FGF-2 in articular cartilage has been reported [19]. For example, unlike in human articular cartilage, intraarticular administration of FGF-2 demonstrates protective effects on cartilage in a murine OA animal model [63]. Such an apparent discrepancy can be explained by our recent finding that human and murine articular cartilage bear distinct FGFR expression profiles, where FGF-2 appeared to differentially regulate the expression of FGFR subtypes between human and murine cartilage. Further, despite the successful regeneration of cartilage in the murine model, FGF-2 fails to relieve symptomatic joint pain in vivo as determined by behavioral tests, perhaps due to FGF-2-promoted angiogenesis and inflammation in murine synovium [63]. These findings suggest that there are fundamental differences in cellular responses between human and murine tissues that eventually determine biological outcomes of FGF-2, possibly due to the complex interplay of FGFRs and their downstream signaling cascades. Our data pertaining to FGF-2 in human cartilage should add caution to the use of this particular growth factor for biological therapy in the future.
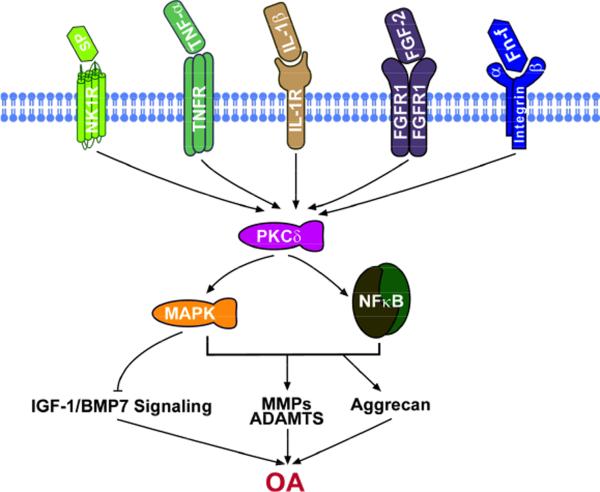
Multiple studies have implicated PKCδ as the rate-limiting factor in which PKCδ is situated at the convergent point of multiple signaling inputs, including FGF-2, substance P (SP), TNF-α, IL-1, and fibronectin fragment (Fn-f). PKCδ activation can lead to NFκB activation in addition to MAPK activation, and these pathways work in concert to inhibit anabolic signaling and stimulate ECM degeneration (Figure 5). Recently, PKCδ has also been shown to play a nociceptive role as a regulator of both peripheral knee joint tissues (cartilage, synovium, meniscus, subchondral bone) and spinal glial activity. Utilizing an established in vivo model for OA, research has shown glial activity may be controlled by the PKCδ axis which integrates key nociceptive signals that promote central knee OA pain [34]. While many of these concepts are novel and pre-translational in nature, they provide deeper insights into the feasibility of utilizing downstream FGF-2 pathway-specific inhibitors in prevention and/or treatment of degenerative joint diseases and OA-associated pain. Future focuses may be toward elucidating pharmacological interventions that have a high translational potential and may establish the potential efficacy of a PKCδ peptide inhibitor in the treatment of symptomatic OA.
Figure 5.
PKCδ functions as the signaling node of multiple pathways. Input from each illustrated ligand-receptor complex triggers PKCδ activation. PKCδ in turn activates MAP kinases (ERK1/2, p38, and JNK) and NFκB, leading to inhibition of anabolic signaling (eg. IGF-1 and BMP7), suppression of PG production, and upregulation of catabolic proteases.
Potential Biological Treatments: The Future
In addition to the development of pharmacologic inhibitors of key catabolic mediators discussed above, recent research has elucidated several compounds that may also play a key role in the future treatment of symptomatic OA. Two of these compounds, resveratrol (RSV) and bovine lactoferricin (LfcinB), have been extensively studied in our laboratory and show considerable promise as an additional potential biological treatment strategy for OA in the coming years.
Resveratrol
The phytoestrogen resveratrol (trans-3,4',5-trihydroxystilbene; RSV) is a natural polyphenol compound found in peanuts, cranberries, and the skin of red grapes, and is thought to be one of the compounds responsible for the health benefits of moderate red wine consumption [65–66]. The anti-inflammatory, anti-oxidant, cardioprotective, and anti-tumor properties of RSV have been well-documented in a variety of tissues [66–74], with recent studies beginning to analyze the effects of RSV on cartilage homeostasis. Elmali et al first reported a significant protective effect of RSV injections on articular cartilage degradation in rabbit models for OA and RA via histological analysis in vivo [75–76]. In human articular chondrocytes, Shakibaei [77] and Czaki [78] elucidated both anti-apoptotic and anti-inflammatory regulatory mechanisms mediated by RSV.
In our laboratory, we have demonstrated potent anabolic and anti-catabolic potential of RSV in bovine spine nucleus pulposus IVD tissue [32] and human adult articular chondrocytes [35] via inhibition of matrix-degrading enzyme expression at the transcriptional and translational level. Further, combination therapy of RSV with BMP-7 induces synergistic effects on PG accumulation, and RSV reverses the catabolic effects of FGF-2 and IL-1 on matrix-degrading enzyme expression, PG accumulation, and the expression of factors (iNOS, IL-1, IL-6) associated with oxidative stress and inflammatory states [32]. Future studies are needed to assess the role of RSV in nociceptive stimulation with OA, as well as its role in-vivo before its use in a clinical setting, but these findings reveal considerable promise for use of RSV as a unique biological therapy for treatment of cartilage degenerative diseases.
Lactoferricin
Bovine lactoferricin (LfcinB) is a 25-amino acid cationic peptide with an amphipathic, anti-parallel β-sheet structure that is obtained by acid-pepsin hydrolysis of the N-terminal region of lactoferrin (Lf) found in cow's milk [79–80]. Similar to RSV, the anti-inflammatory, anti-viral, anti-bacterial, anti-oxidant, anti-pain, and anti-cancer properties of LfcinB have been reported in a variety of tissues [81–82]. The natural anti-oxidative effect of LfcinB has also been reported, suggesting a possible chondroprotective biological role in articular cartilage [83], and recent studies have attempted to unravel the role of LfcinB in musculoskeletal disease. In a mouse collagen-induced and septic arthritis model, periarticular injection of human Lf substantially suppresses local inflammation [84]. Further, in a rat adjuvant arthritis model, oral administration of bovine Lf suppresses the development of arthritis and hyperalgesia in the adjuvant-injected paw, suggesting Lf has preventative and therapeutic effects on the adjuvant-induced inflammation and pain [85].
In our laboratory, LfcinB was found to exert potent anabolic and anti-catabolic effects in bovine nucleus pulposus matrix homeostasis in the IVD [36]. Further, we found similar anabolic and anti-catabolic effects of LfcinB in human articular cartilage (Im et al, unpublished data). LfcinB reverses the catabolic effects of FGF-2 and IL-1 on matrix-degrading enzyme production, PG accumulation, and expression of factors associated with oxidative stress and inflammation, suggesting the promise of LfcinB as an anti-catabolic and anti-inflammatory molecule in human articular cartilage. To date, the anti-pain potential of LfcinB has yet to be studied, and caution must be advised as further studies are warranted to determine, among other things, possible detrimental effects of the use of LfcinB (and RSV) in vivo.
Conclusion
In summary, the literature reveals important roles of growth factors and cytokines in articular cartilage homeostasis and the development of OA and OA-associated pain. Upregulation of catabolic processes and/or downregulation of anabolic processes leads to disruption of equilibrium with subsequent cartilage degradation and OA, and several of these pathways are known to induce pain in OA as well. Currently, many of the underlying pathways remain unknown, but recent efforts have begun to increase our understanding. Catabolic factors involved in both cartilage degradation in vitro and nociceptive stimulation include IL-1, IL-6, TNF-α, PGE2, FGF-2 and PKCδ, and pharmacologic inhibitors to these mediators, as well as compounds such as RSV and LfcinB, may potentially be used as biological treatments in the future.
Despite a tremendous research effort in recent years to elucidate these processes, however, biologic therapy for OA remains experimental in nature, and several unknowns exist. Given the wide array of interactions of growth factors that are necessary for maintenance of cartilage homeostasis in vivo, it is unlikely that any single growth factor will lead to complete cartilage repair or affect the arthritic joint clinically, and rather a combination approach will be required [86]. Further, appropriate dosing, scaffolds, and routes of administration must be determined before biological factors play a beneficial role clinically. Nevertheless, this paper reviews several of the most well-studied biochemical mediators involved in OA and pain, and provides a framework for the understanding of potential biologic therapies in the treatment of degenerative joint disease in the future.
Acknowledgments
This work was supported by NIH NIAMS R01 grants from AR053220, AR062136 (to HJI) and R01AR049069 (to AJvW).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Buckwalter JA, Saltzman C, Brown T. The impact of osteoarthritis: implications for research. Clin Orthop Relat Res. 2004 Oct.(no. 427):S6–15. doi: 10.1097/01.blo.0000143938.30681.9d. doi:10.1097/01.blo.0000143938.30681.9d. [DOI] [PubMed] [Google Scholar]
- [2].Kotlarz H, Gunnarsson CL, Fang H, Rizzo JA. Insurer and out-of-pocket costs of osteoarthritis in the US: evidence from national survey data. Arthritis Rheum. 2009 Dec.vol. 60(no. 12):3546–3553. doi: 10.1002/art.24984. doi:10.1002/art.24984. [DOI] [PubMed] [Google Scholar]
- [3].Pereira D, Peleteiro B, Araújo J, Branco J, Santos RA, Ramos E. The effect of osteoarthritis definition on prevalence and incidence estimates: a systematic review. Osteoarthritis and Cartilage. 2011 Nov.vol. 19(no. 11):1270–1285. doi: 10.1016/j.joca.2011.08.009. doi:10.1016/j.joca.2011.08.009. [DOI] [PubMed] [Google Scholar]
- [4].Issa SN, Sharma L. Epidemiology of osteoarthritis: an update. Curr Rheumatol Rep. 2006 Feb.vol. 8(no. 1):7–15. doi: 10.1007/s11926-006-0019-1. doi:10.1007/s11926-006-0019-1. [DOI] [PubMed] [Google Scholar]
- [5].Buckwalter JA, Saltzman C, Brown T. The Impact of Osteoarthritis. Clin Orthop Relat Res. 2004 Oct.vol. 427:S6–S15. doi: 10.1097/01.blo.0000143938.30681.9d. doi:10.1097/01.blo.0000143938.30681.9d. [DOI] [PubMed] [Google Scholar]
- [6].Valdes AM, Spector TD. Genetic epidemiology of hip and knee osteoarthritis. Nature Publishing Group. 2010 Nov.vol. 7(no. 1):23–32. doi: 10.1038/nrrheum.2010.191. doi:10.1038/nrrheum.2010.191. [DOI] [PubMed] [Google Scholar]
- [7].Richette P, Poitou C, Garnero P, Vicaut E, Bouillot JL, Lacorte JM, Basdevant A, Clement K, Bardin T, Chevalier X. Benefits of massive weight loss on symptoms, systemic inflammation and cartilage turnover in obese patients with knee osteoarthritis. Annals of the Rheumatic Diseases. 2010 Dec.vol. 70(no. 1):139–144. doi: 10.1136/ard.2010.134015. doi:10.1136/ard.2010.134015. [DOI] [PubMed] [Google Scholar]
- [8].Tanamas S, Hanna FS, Cicuttini FM, Wluka AE, Berry P, Urquhart DM. Does knee malalignment increase the risk of development and progression of knee osteoarthritis? A systematic review. Arthritis & ?Rheumatism. 2009;61(4):459–467. doi: 10.1002/art.24336. doi:10.1002/art.24336. [DOI] [PubMed] [Google Scholar]
- [9].Lane NE, Brandt K, Hawker G, Peeva E, Schreyer, Tsuji W, Hochberg MC. OARSI-FDA initiative: defining the disease state of osteoarthritis. Presented at the Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society; 2011. pp. 478–482. doi:10.1016/j.joca.2010.09.013. [DOI] [PubMed] [Google Scholar]
- [10].Dieppe PA, Lohmander LS. Pathogenesis and management of pain in osteoarthritis. Lancet. 2005 Feb.vol. 365(no. 9463):965–973. doi: 10.1016/S0140-6736(05)71086-2. doi:10.1016/S0140-6736(05)71086-2. [DOI] [PubMed] [Google Scholar]
- [11].Sandell L, Aigner T. Articular cartilage and changes in arthritis. An introduction: cell biology of osteoarthritis. Arthritis Res. 2001 doi: 10.1186/ar148. doi:10.1186/ar148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Nakata K, Ono K, Miyazaki J, Olsen BR, Muragaki Y, Adachi E, Yamamura K, et al. Osteoarthritis associated with mild chondrodysplasia in transgenic mice expressing alpha 1(IX) collagen chains with a central deletion. Proceedings of the National Academy of Sciences of the United States of America. 1993;90(7):2870–2874. doi: 10.1073/pnas.90.7.2870. doi:10.1073/pnas.90.7.2870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Bauer DC, Hunter DJ, Abramson SB, Attur M, Corr M, Felson D, Heinegård D, Jordan JM, Kepler TB, Lane NE, Saxne T, Tyree B, Kraus VB. Classification of osteoarthritis biomarkers: a proposed approach. Osteoarthritis and Cartilage. 2006 Aug.vol. 14(no. 8):723–727. doi: 10.1016/j.joca.2006.04.001. doi:10.1016/j.joca.2006.04.001. [DOI] [PubMed] [Google Scholar]
- [14].Im H-J, Li X, Muddasani P, Kim G-H, Davis F, Rangan J, Forsyth CB, Ellman M, Thonar EJ. Basic fibroblast growth factor accelerates matrix degradation via a neuro-endocrine pathway in human adult articular chondrocytes. J. Cell. Physiol. 2008;vol. 215(no. 2):452–463. doi: 10.1002/jcp.21317. doi:10.1002/jcp.21317. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [15].P Im HJ, Muddasani P, Natarajan V, Schmid TM, Block JA, Davis F, van Wijnen AJ, et al. Basic Fibroblast Growth Factor Stimulates Matrix Metalloproteinase-13 via the Molecular Cross-talk between the Mitogen-activated Protein Kinases and Protein Kinase C Pathways in Human Adult Articular Chondrocytes. Journal of Biological Chemistry. 2007;282(15):11110–11121. doi: 10.1074/jbc.M609040200. doi:10.1074/jbc.M609040200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Goldring MB, Berenbaum F. The regulation of chondrocyte function by proinflammatory mediators: prostaglandins and nitric oxide. Clinical Orthopaedics and Related Research®. 2004;(427 Suppl):S37–46. doi: 10.1097/01.blo.0000144484.69656.e4. doi:10.1097/01.blo.0000144484.69656.e4. [DOI] [PubMed] [Google Scholar]
- [17].Loeser RF. Molecular mechanisms of cartilage destruction in osteoarthritis. J Musculoskelet Neuronal Interact. 2008 Sep.vol. 8(no. 4):303–306. [PubMed] [Google Scholar]
- [18].Sundman EA, Cole BJ, Fortier LA. Growth Factor and Catabolic Cytokine Concentrations Are Influenced by the Cellular Composition of Platelet-Rich Plasma. The American Journal of Sports Medicine. 2011 Aug. doi: 10.1177/0363546511417792. doi:10.1177/0363546511417792. [DOI] [PubMed] [Google Scholar]
- [19].Ellman MB, An HS, Muddasani P, Im H-J. Biological impact of the fibroblast growth factor family on articular cartilage and intervertebral disc homeostasis. Gene. 2008 Aug.vol. 420(no. 1):82–89. doi: 10.1016/j.gene.2008.04.019. doi:10.1016/j.gene.2008.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Hunter DJ, McDougall JJ, Keefe FJ. The Symptoms of Osteoarthritis and the Genesis of Pain. Rheumatic Disease Clinics of North America. 2008 Aug.vol. 34(no. 3):623–643. doi: 10.1016/j.rdc.2008.05.004. doi:10.1016/j.rdc.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Lee YC, Nassikas NJ, Clauw DJ. The role of the central nervous system in the generation and maintenance of chronic pain in rheumatoid arthritis, osteoarthritis and fibromyalgia. Arthritis Res. Ther. 2011;vol. 13(no. 2):211. doi: 10.1186/ar3306. doi:10.1186/ar3306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Li X, Kim JS, Wijnen AJ, Im HJ. Osteoarthritic tissues modulate functional properties of sensory neurons associated with symptomatic OA pain. Molecular Biology Reports. 2011;38(8):5335–5339. doi: 10.1007/s11033-011-0684-7. doi:10.1007/s11033-011-0684-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Imamura M, Imamura ST, Kaziyama HHS, Targino RA, Hsing WT, De Souza LPM, Cutait MM, Fregni F, Camanho GL. Impact of nervous system hyperalgesia on pain, disability, and quality of life in patients with knee osteoarthritis: A controlled analysis. Arthritis Rheum. 2008 Oct.vol. 59(no. 10):1424–1431. doi: 10.1002/art.24120. doi:10.1002/art.24120. [DOI] [PubMed] [Google Scholar]
- [24].Im H-J, Kim J-S, Li X, Kotwal N, Sumner DR, van Wijnen AJ, Davis FJ, Yan D, Levine B, Henry JL, Desevré J, Kroin JS. Alteration of sensory neurons and spinal response to an experimental osteoarthritis pain model. Arthritis Rheum. 2010 Jun.vol. 62(no. 10):2995–3005. doi: 10.1002/art.27608. doi:10.1002/art.27608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Felson DT. The sources of pain in knee osteoarthritis. Curr Opin Rheumatol. 2005 Sep.vol. 17(no. 5):624–628. doi: 10.1097/01.bor.0000172800.49120.97. doi:10.1097/01.bor.0000172800.49120.97. [DOI] [PubMed] [Google Scholar]
- [26].Li X, Kim J-S, Wijnen AJ, Im H-J. Osteoarthritic tissues modulate functional properties of sensory neurons associated with symptomatic OA pain. Mol Biol Rep. 2011 Feb.vol. 38(no. 8):5335–5339. doi: 10.1007/s11033-011-0684-7. doi:10.1007/s11033-011-0684-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Read S. Future targets to control osteoarthritis pain. Arthritis Res. Ther. 2007 doi: 10.1186/ar2178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Kosek E, Ordeberg G. Lack of pressure pain modulation by heterotopic noxious conditioning stimulation in patients with painful osteoarthritis before, but not following, surgical pain relief. Pain. 2000 Oct.vol. 88(no. 1):69–78. doi: 10.1016/S0304-3959(00)00310-9. doi:10.1016/S0304-3959(00)00310-9. [DOI] [PubMed] [Google Scholar]
- [29].Hunter DJ, McDougall JJ, Keefe FJ. The symptoms of osteoarthritis and the genesis of pain. Medical Clinics of NA. 2009 Jan.vol. 93(no. 1):83–100. xi. doi: 10.1016/j.mcna.2008.08.008. doi:10.1016/j.mcna.2008.08.008. [DOI] [PubMed] [Google Scholar]
- [30].Loeser R, Yammani R, Carlson C. Articular chondrocytes express the receptor for advanced glycation end products: potential role in osteoarthritis. Arthritis & …. 2005 doi: 10.1002/art.21199. doi:10.1002/art.21199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Chubinskaya S, Pacione C, Im H. Basic fibroblast growth factor inhibits the anabolic activity of insulin- like growth factor 1 and osteogenic protein 1 in adult human articular chondrocytes. Arthritis & …. 2005 doi: 10.1002/art.21472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Li X, Phillips FM, An HS, Ellman M, Thonar EJ, Wu W, Park D, et al. The action of resveratrol, a phytoestrogen found in grapes, on the intervertebral disc. Spine. 2008;33(24):2586–2595. doi: 10.1097/BRS.0b013e3181883883. doi:10.1097/BRS.0b013e3181883883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Im HJ, Muddasani P, Natarajan V, Schmid TM, Block JA, Davis F, van Wijnen AJ, Loeser RF. Basic Fibroblast Growth Factor Stimulates Matrix Metalloproteinase-13 via the Molecular Cross-talk between the Mitogen-activated Protein Kinases and Protein Kinase C Pathways in Human Adult Articular Chondrocytes. Journal of Biological Chemistry. 2007 Feb.vol. 282(no. 15):11110–11121. doi: 10.1074/jbc.M609040200. doi:10.1074/jbc.M609040200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Ellman M, Kim J, An H, Kroin J. The pathophysiological role of the PKCδ pathway in the intervertebral disc: In vitro, ex vivo and in vivo studies. Arthritis & …. 2011 doi:10.1002/art.34337. [Google Scholar]
- [35].Im H-J, Li X, Chen D, Yan D, Kim J, Ellman MB, Stein GS, Cole B, KC R, Cs-Szabo G, van Wijnen AJ. Biological effects of the plant-derived polyphenol resveratrol in human articular cartilage and chondrosarcoma cells. J. Cell. Physiol. 2012 doi: 10.1002/jcp.24049. pp. n/a-n/a. doi:10.1002/jcp.24049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Kim J, Ellman M, An H, Yan D. Lactoferricin mediates anabolic and anti- catabolic effects in the intervertebral disc. Journal of Cellular …. 2012 doi: 10.1002/jcp.22867. doi:10.1002/jcp.22867. [DOI] [PubMed] [Google Scholar]
- [37].Schaible HG, Ebersberger A, A., Natura G. Update on peripheral mechanisms of pain: beyond prostaglandins and cytokines. Arthritis research & therapy. 2011;13(2):210. doi: 10.1186/ar3305. doi:10.1186/ar3305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Benito MJ, Veale DJ, FitzGerald O, van den Berg WB, Bresnihan B. Synovial tissue inflammation in early and late osteoarthritis. Annals of the Rheumatic Diseases. 2005 Sep.vol. 64(no. 9):1263–1267. doi: 10.1136/ard.2004.025270. doi:10.1136/ard.2004.025270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Youssef PP, Triantafillou S, Parker A, Coleman M, Roberts-Thomson PJ, Ahern MJ, Smith MD. Variability in cytokine and cell adhesion molecule staining in arthroscopic synovial biopsies: quantification using color video image analysis. J. Rheumatol. 1997 Dec.vol. 24(no. 12):2291–2298. [PubMed] [Google Scholar]
- [40].Goldring MB, Birkhead J, Sandell LJ, Kimura T, Krane SM. Interleukin 1 suppresses expression of cartilage-specific types II and IX collagens and increases types I and III collagens in human chondrocytes. J. Clin. Invest. 1988 Dec.vol. 82(no. 6):2026–2037. doi: 10.1172/JCI113823. doi:10.1172/JCI113823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Lefebvre V, Peeters-Joris C, Vaes G. Modulation by interleukin 1 and tumor necrosis factor alpha of production of collagenase, tissue inhibitor of metalloproteinases and collagen types in differentiated and dedifferentiated articular chondrocytes. Biochim. Biophys. Acta. 1990 May;vol. 1052(no. 3):366–378. doi: 10.1016/0167-4889(90)90145-4. doi:10.1172/JCI113823. [DOI] [PubMed] [Google Scholar]
- [42].Richardson DW, Dodge GR. Effects of interleukin-1β and tumor necrosis factor-α on expression of matrix-related genes by cultured equine articular chondrocytes. American Journal of Veterinary Research. 2000 Jun.vol. 61(no. 6):624–630. doi: 10.2460/ajvr.2000.61.624. doi:10.2460/ajvr.2000.61.624. [DOI] [PubMed] [Google Scholar]
- [43].Sommer C. Recent findings on how proinflammatory cytokines cause pain: peripheral mechanisms in inflammatory and neuropathic hyperalgesia. Neuroscience letters. 2004 doi: 10.1016/j.neulet.2003.12.007. doi:10.1016/j.neulet.2003.12.007. [DOI] [PubMed] [Google Scholar]
- [44].Orita S, Koshi T, Mitsuka T, Miyagi M, Inoue G, Arai G, Ishikawa T, Hanaoka E, Yamashita K, Yamashita M, Eguchi Y, Toyone T, Takahashi K, Ohtori S. Associations between proinflammatory cytokines in the synovial fluid and radiographic grading and pain-related scores in 47 consecutive patients with osteoarthritis of the knee. BMC Musculoskelet Disord. 2011 Jun.vol. 12(no. 1):144. doi: 10.1186/1471-2474-12-144. doi:10.1186/1471-2474-12-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Evans C, Gouze E, Gouze J, Robbins P. Gene therapeutic approaches–transfer in vivo. Advanced drug delivery …. 2006 doi: 10.1016/j.addr.2006.01.009. doi:10.1016/j.addr.2006.01.009. [DOI] [PubMed] [Google Scholar]
- [46].Caron JP, Fernandes JC, Martel-Pelletier J, Tardif G, Mineau F, Geng C, Pelletier JP. Chondroprotective effect of intraarticular injections of interleukin- 1 receptor antagonist in experimental osteoarthritis. Suppression of collagenase- 1 expression. Arthritis & Rheum. 1996 doi: 10.1002/art.1780390914. doi:10.1002/art.1780390914. [DOI] [PubMed] [Google Scholar]
- [47].Brenn D, Richter F, Schaible H. Sensitization of unmyelinated sensory fibers of the joint nerve to mechanical stimuli by interleukin- 6 in the rat: An inflammatory mechanism of joint pain. Arthritis Rheum. 2007 doi: 10.1002/art.22282. doi:10.1002/art.22282. [DOI] [PubMed] [Google Scholar]
- [48].Arvidson N, Gudbjörnsson B, Elfman L. Circadian rhythm of serum interleukin-6 in rheumatoid arthritis. Annals of the Rheumatic Diseases. 1994 doi: 10.1136/ard.53.8.521. doi:10.1136/ard.53.8.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Silacci P, Dayer JM, Desgeorges A, Peter R, Manueddu C, Guerne PA. Interleukin (IL)-6 and its soluble receptor induce TIMP-1 expression in synoviocytes and chondrocytes, and block IL-1-induced collagenolytic activity. The Journal of biological chemistry. 1998;273(22):13625–13629. doi: 10.1074/jbc.273.22.13625. [DOI] [PubMed] [Google Scholar]
- [50].Obreja O, Biasio W, Andratsch M, Lips KS, Rathee PK, Ludwig A, Rose-John S, Kress M. Fast modulation of heat-activated ionic current by proinflammatory interleukin 6 in rat sensory neurons. Brain. 2005 Jul.vol. 128(no. 7):1634–1641. doi: 10.1093/brain/awh490. doi:10.1093/brain/awh490. [DOI] [PubMed] [Google Scholar]
- [51].Aoki Y, Ohtori S, Ino H, Douya H, Ozawa T, Saito T, Moriya H, Takahashi K. Disc inflammation potentially promotes axonal regeneration of dorsal root ganglion neurons innervating lumbar intervertebral disc in rats. Spine. 2004 Dec.vol. 29(no. 23):2621–2626. doi: 10.1097/01.brs.0000146051.11574.b4. doi:10.1097/01.brs.0000146051.11574.b4. [DOI] [PubMed] [Google Scholar]
- [52].Schäfers M, Marziniak M, Sorkin L, Yaksh T. Cyclooxygenase inhibition in nerve-injury-and TNF-induced hyperalgesia in the rat. Exp Neurology. 2004 Jan. doi: 10.1016/j.expneurol.2003.09.015. doi:10.1016/j.expneurol.2003.09.015. [DOI] [PubMed] [Google Scholar]
- [53].Grunke M, Schulze-Koops H. Successful treatment of inflammatory knee osteoarthritis with tumour necrosis factor blockade. Annals of the Rheumatic Diseases. 2006 doi: 10.1136/ard.2006.053272. doi:10.1136/ard.2006.053272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Inglis JJ, Notley CA, Essex D, Wilson AW, Feldmann M, Anand P, Williams R. Collagen-induced arthritis as a model of hyperalgesia: functional and cellular analysis of the analgesic actions of tumor necrosis factor blockade. Arthritis & Rheumatism. 2007;56(12):4015–4023. doi: 10.1002/art.23063. doi:10.1002/art.23063. [DOI] [PubMed] [Google Scholar]
- [55].Yaksh TL, Dirig DM, Conway CM, Svensson C, Luo ZD, Isakson PC. The acute antihyperalgesic action of nonsteroidal, anti-inflammatory drugs and release of spinal prostaglandin E2 is mediated by the inhibition of constitutive spinal cyclooxygenase-2 (COX-2) but not COX-1. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2001;21(16):5847–5853. doi: 10.1523/JNEUROSCI.21-16-05847.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].England S, Bevan S, Docherty RJ. PGE2 modulates the tetrodotoxin-resistant sodium current in neonatal rat dorsal root ganglion neurones via the cyclic AMP-protein kinase A cascade. The Journal of physiology. 1996;495(Pt 2):429–440. doi: 10.1113/jphysiol.1996.sp021604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Bär KJ, Natura G, Telleria-Diaz A, Teschner P, Vogel R, Vasquez E, Schaible HG, et al. Changes in the effect of spinal prostaglandin E2 during inflammation: prostaglandin E (EP1–EP4) receptors in spinal nociceptive processing of input from the normal or inflamed knee joint. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2004;24(3):642–651. doi: 10.1523/JNEUROSCI.0882-03.2004. doi:10.1523/JNEUROSCI.0882-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Hardy MM, Seibert K, Manning PT, Currie MG, Woerner BM, Edwards D, Koki A, Tripp CS. Cyclooxygenase 2-dependent prostaglandin E2 modulates cartilage proteoglycan degradation in human osteoarthritis explants. Arthritis Rheum. 2002 Jul.vol. 46(no. 7):1789–1803. doi: 10.1002/art.10356. doi:10.1002/art.10356. [DOI] [PubMed] [Google Scholar]
- [59].Shimpo H, Sakai T, Kondo S, Mishima S, Yoda M, Hiraiwa H, Ishiguro N. Regulation of prostaglandin E2 synthesis in cells derived from chondrocytes of patients with osteoarthritis. J Orthop Sci. 2009 Oct.vol. 14(no. 5):611–617. doi: 10.1007/s00776-009-1370-7. doi:10.1007/s00776-009-1370-7. [DOI] [PubMed] [Google Scholar]
- [60].Li X, Ellman M, Muddasani P, Wang JH-C, Cs-Szabo G, van Wijnen AJ, Im H-J. Prostaglandin E2 and its cognate EP receptors control human adult articular cartilage homeostasis and are linked to the pathophysiology of osteoarthritis. Arthritis & Rheumatism. 2009;60(2):513–523. doi: 10.1002/art.24258. doi:10.1002/art.24258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Claveau D, Sirinyan M, Guay J, Gordon R, Chan C-C, Bureau Y, Riendeau D, et al. Microsomal prostaglandin E synthase-1 is a major terminal synthase that is selectively up-regulated during cyclooxygenase-2-dependent prostaglandin E2 production in the rat adjuvant-induced arthritis model. Journal of immunology (Baltimore, Md. : 1950) 2003;170(9):4738–4744. doi: 10.4049/jimmunol.170.9.4738. [DOI] [PubMed] [Google Scholar]
- [62].Trebino CE, Stock JL, Gibbons CP, Naiman BM, Wachtmann TS, Umland JP, Pandher K, et al. Impaired inflammatory and pain responses in mice lacking an inducible prostaglandin E synthase. Proceedings of the National Academy of Sciences of the United States of America. 2003;100(15):9044–9049. doi: 10.1073/pnas.1332766100. doi:10.1073/pnas.1332766100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Li X, Ellman MB, Kroin JS, Chen D, Yan D, Mikecz K, Ranjan Kc, et al. Species-specific biological effects of FGF-2 in articular cartilage: Implication for distinct roles within the FGF receptor family. Journal of Cellular Biochemistry. 2012;113(7):2532–2542. doi: 10.1002/jcb.24129. doi:10.1002/jcb.24129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Yan D, Chen D, Im HJ. Fibroblast growth factor-2 promotes catabolism via FGFR1-Ras-Raf-MEK1/2-ERK1/2 axis that coordinates with the PKCδ pathway in human articular chondrocytes. Journal of Cellular Biochemistry. 2012 doi: 10.1002/jcb.24160. doi:10.1002/jcb.24160. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [65].Wang Z, Huang Y, Zou J, Cao K, Xu Y, Wu JM. Effects of red wine and wine polyphenol resveratrol on platelet aggregation in vivo and in vitro. International journal of molecular medicine. 2002;9(1):77–79. [PubMed] [Google Scholar]
- [66].Leiro J, Alvarez E, Arranz JA, Laguna R, Uriarte E, Orallo F. Effects of cis-resveratrol on inflammatory murine macrophages: antioxidant activity and down-regulation of inflammatory genes. J. Leukoc. Biol. 2004 Jun.vol. 75(no. 6):1156–1165. doi: 10.1189/jlb.1103561. doi:10.1189/jlb.1103561. [DOI] [PubMed] [Google Scholar]
- [67].Haider UGB, Sorescu D, Griendling KK, Vollmar AM, Dirsch VM. Resveratrol increases serine15-phosphorylated but transcriptionally impaired p53 and induces a reversible DNA replication block in serum-activated vascular smooth muscle cells. Molecular pharmacology. 2003;63(4):925–932. doi: 10.1124/mol.63.4.925. doi:10.1124/mol.63.4.925. [DOI] [PubMed] [Google Scholar]
- [68].Bhat KP, Kosmeder JW, Pezzuto JM. Biological effects of resveratrol. Antioxid. Redox Signal. 2001 Dec.vol. 3(no. 6):1041–1064. doi: 10.1089/152308601317203567. doi:10.1089/152308601317203567. [DOI] [PubMed] [Google Scholar]
- [69].Bertelli AA, Ferrara F, Diana G, Fulgenzi A, Corsi M, Ponti W, Ferrero ME, et al. Resveratrol, a natural stilbene in grapes and wine, enhances intraphagocytosis in human promonocytes: a co-factor in antiinflammatory and anticancer chemopreventive activity. International journal of tissue reactions. 1999;21(4):93–104. [PubMed] [Google Scholar]
- [70].Frémont L. Biological effects of resveratrol. Life sciences. 2000;66(8):663–673. doi: 10.1016/s0024-3205(99)00410-5. doi:10.1016/S0024-3205(99)00410-5. [DOI] [PubMed] [Google Scholar]
- [71].Huang KS, Lin M, Cheng GF. Anti-inflammatory tetramers of resveratrol from the roots of Vitis amurensis and the conformations of the seven-membered ring in some oligostilbenes. Phytochemistry. 2001 Sep.vol. 58(no. 2):357–362. doi: 10.1016/s0031-9422(01)00224-2. doi:10.1016/S0031-9422(01)00224-2. [DOI] [PubMed] [Google Scholar]
- [72].Jang M, Cai L, Udeani GO, Slowing KV, Thomas CF, Beecher CW, Fong HH, Farnsworth NR, Kinghorn AD, Mehta RG, Moon RC, Pezzuto JM. Cancer chemopreventive activity of resveratrol, a natural product derived from grapes. Science. 1997 Jan.vol. 275(no. 5297):218–220. doi: 10.1126/science.275.5297.218. doi:10.1126/science.275.5297.218. [DOI] [PubMed] [Google Scholar]
- [73].Martinez J, J., Moreno JJ. Effect of resveratrol, a natural polyphenolic compound, on reactive oxygen species and prostaglandin production. Biochemical pharmacology. 2000;59(7):865–870. doi: 10.1016/s0006-2952(99)00380-9. doi:10.1016/S0006-2952(99)00380-9. [DOI] [PubMed] [Google Scholar]
- [74].Ignatowicz E, Baer-Dubowska W. Resveratrol, a natural chemopreventive agent against degenerative diseases. Pol J Pharmacol. 2001;53(6):557–569. [PubMed] [Google Scholar]
- [75].Elmali N, Esenkaya I, Harma A, Ertem K, Turkoz Y, Mizrak B. Effect of resveratrol in experimental osteoarthritis in rabbits. Inflamm. Res. 2005 Apr.vol. 54(no. 4):158–162. doi: 10.1007/s00011-004-1341-6. doi:10.1007/s00011-004-1341-6. [DOI] [PubMed] [Google Scholar]
- [76].Elmali N, Baysal O, Harma A, Esenkaya I, Mizrak B. Effects of resveratrol in inflammatory arthritis. Inflammation. 2007 Apr.vol. 30(no. 1):1–6. doi: 10.1007/s10753-006-9012-0. doi:10.1007/s10753-006-9012-0. [DOI] [PubMed] [Google Scholar]
- [77].Shakibaei M, Csaki C, Nebrich S, Mobasheri A. Resveratrol suppresses interleukin-1beta-induced inflammatory signaling and apoptosis in human articular chondrocytes: potential for use as a novel nutraceutical for the treatment of osteoarthritis. Biochemical pharmacology. 2008;76(11):1426–1439. doi: 10.1016/j.bcp.2008.05.029. doi:10.1016/j.bcp.2008.05.029. [DOI] [PubMed] [Google Scholar]
- [78].Csaki C, Keshishzadeh N, Fischer K, Shakibaei M. Regulation of inflammation signalling by resveratrol in human chondrocytes in vitro. Biochemical pharmacology. 2008;75(3):677–687. doi: 10.1016/j.bcp.2007.09.014. doi:10.1016/j.bcp.2007.09.014. [DOI] [PubMed] [Google Scholar]
- [79].Gitay-Goren H, Soker S, Vlodavsky I, Neufeld G. The binding of vascular endothelial growth factor to its receptors is dependent on cell surface-associated heparin-like molecules. J. Biol. Chem. 1992 Mar.vol. 267(no. 9):6093–6098. [PubMed] [Google Scholar]
- [80].Baker EN, Baker HM. A structural framework for understanding the multifunctional character of lactoferrin. Biochimie. 2009;91(1):3–10. doi: 10.1016/j.biochi.2008.05.006. doi:10.1016/j.biochi.2008.05.006. [DOI] [PubMed] [Google Scholar]
- [81].Mader JS, Richardson A, Salsman J, Top D, de Antueno R, Duncan R, Hoskin DW. Bovine lactoferricin causes apoptosis in Jurkat T-leukemia cells by sequential permeabilization of the cell membrane and targeting of mitochondria. Exp. Cell Res. 2007 Jul.vol. 313(no. 12):2634–2650. doi: 10.1016/j.yexcr.2007.05.015. doi:10.1016/j.yexcr.2007.05.015. [DOI] [PubMed] [Google Scholar]
- [82].Gifford JL, Hunter HN, Vogel HJ. Lactoferricin: a lactoferrin-derived peptide with antimicrobial, antiviral, antitumor and immunological properties. Cell. Mol. Life Sci. 2005 Nov.vol. 62(no. 22):2588–2598. doi: 10.1007/s00018-005-5373-z. doi:10.1007/s00018-005-5373-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Henrotin YE, Bruckner P, Pujol J-PL. The role of reactive oxygen species in homeostasis and degradation of cartilage. Osteoarthr. Cartil. 2003 Oct.vol. 11(no. 10):747–755. doi: 10.1016/s1063-4584(03)00150-x. doi:10.1016/S1063-4584(03)00150-X. [DOI] [PubMed] [Google Scholar]
- [84].Guillen C, McInnes IB, Vaughan D, Speekenbrink AB, Brock JH. The effects of local administration of lactoferrin on inflammation in murine autoimmune and infectious arthritis. Arthritis Rheum. 2000 Sep.vol. 43(no. 9):2073–2080. doi: 10.1002/1529-0131(200009)43:9<2073::AID-ANR19>3.0.CO;2-U. doi:10.1002/1529-0131(200009)43:9<2073∷AID-ANR19>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- [85].Hayashida K-I, Kaneko T, Takeuchi T, Shimizu H, Ando K, Harada E. Oral administration of lactoferrin inhibits inflammation and nociception in rat adjuvant-induced arthritis. J. Vet. Med. Sci. 2004 Feb.vol. 66(no. 2):149–154. doi: 10.1292/jvms.66.149. doi:10.1292/jvms.66.149. [DOI] [PubMed] [Google Scholar]
- [86].Fortier LA, Barker JU, Strauss EJ, McCarrel TM, Cole BJ. The Role of Growth Factors in Cartilage Repair. Clinical Orthopaedics and Related Research. 2011 doi: 10.1007/s11999-011-1857-3. doi:10.1007/s11999-011-1857-3. [DOI] [PMC free article] [PubMed] [Google Scholar]