Abstract
Context
Whether recent declines in ischemic heart disease and its risk factors have been accompanied by declines in heart failure (HF) hospitalization and mortality is not known.
Objective
To examine changes in HF hospitalization rate and 1-year mortality rate in the U.S., nationally and by state/territory.
Design, Setting, and Participants
55,097,390 fee-for-service Medicare beneficiaries hospitalized between 1998 and 2008 in acute care hospitals in the U.S. and Puerto Rico admitted with a principal discharge diagnosis code for HF.
Main Outcome Measures
Changes in patient demographics and comorbidities, HF hospitalization rates, and 1-year mortality rates.
Results
The HF hospitalization rate adjusted for age, sex, and race declined from 2,845 per 100,000 person-years in 1998 to 2,007 per 100,000 person-years in 2008 (p<0.001), a relative decline of 29.5%. Age-adjusted HF-hospitalization rates declined over the study period for all race-sex categories. Black men had the lowest rate of decline (4,142 to 3,201 per 100,000 person-years) among all race-sex categories which persisted after adjusting for age (incidence rate ratio=0.81, 95% confidence interval [CI] 0.79 to 0.84). HF hospitalization rates declined significantly faster than the national mean in 16 states, and significantly slower in 3 states. Risk-adjusted 1-year mortality fell from 31.7% in 1999 to 29.6% in 2008 (p<0.001), a relative decline of 6.6%. 1-year mortality rates declined significantly in 4 states, but increased in 5 states.
Conclusions
The overall HF hospitalization rate declined substantially from 1998 to 2008, but at a lower rate for black men. The overall 1-year mortality rate declined slightly over the past decade, but remains high. Changes in HF hospitalization and 1-year mortality rates were uneven across states.
Keywords: heart failure, hospitalization, mortality, epidemiology
Background
Heart failure (HF) imposes one of the highest disease burdens of any medical condition in the United States, with an estimated 5.8 million Americans suffering from HF in 2006.1 The risk of developing HF increases with advancing age2 and as a result HF ranks as the most frequent cause of hospitalization and rehospitalization among older Americans.3, 4 HF is also one of the most resource intensive conditions with direct and indirect costs in the U.S. estimated at $39.2 billion in 2010.5
As the U.S. population grows older, the HF hospitalization rate would be expected to rise. But several other factors may counterbalance this demographic trend. Recent declines in the incidence of ischemic heart disease,6, 7 a common precursor for HF, may have led to declines in HF hospitalizations. Hypertension is an important cause of HF;8 rates of blood pressure control have also improved over time.9, 10 Higher use of secondary prevention therapies11–13 may have led to fewer recurrent HF hospitalizations. Secular trends in thresholds for hospital admission may also play a role, as clinicians substitute outpatient instead of inpatient care when feasible. 14
How HF hospitalization rates have changed in recent times is unknown, particularly on a national scale. Surveillance studies have produced clinically-validated information on trends in HF incidence; the Framingham Heart Study 15 found no change in HF incidence over the past 50 years for men, and a decline of about one-third for women; HF incidence in Olmstead County, Minnesota was stable from 1979–2000.16 Administrative data provide an alternative for assessing HF hospitalization trends on a national scale, given that surveillance studies may have limited generalizability to national trends. The availability of a complete sample of Medicare fee-for-service claims provides sufficient numbers to precisely estimate changes in HF hospitalization rates across demographic subgroups. A complete national sample can also accurately estimate trends across geographic regions to identify specific locations for targeted interventions. Accordingly, we analyzed a 100% sample of Medicare beneficiaries to identify trends in HF hospitalization rate from 1998 to 2008, nationally and by state/territory. Because changes in survival after HF hospitalization may have changed the denominator of HF patients at risk for recurrent hospitalization, we also examine trends in 1-year mortality after HF hospitalization, nationally and by state/territory.
Methods
Data Sources
We used inpatient National Claims History files from the Centers for Medicare and Medicaid Services (CMS) to identify all fee-for-service Medicare beneficiaries who were hospitalized for HF from 1998 to 2008. These administrative claims included information on patient demographics (age, sex, race), admission and discharge dates, and principal and secondary diagnosis codes (as coded by the International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM]. HF hospitalizations were defined as admission to an acute-care hospital for a principal discharge diagnosis of HF according to the following ICD-9-CM codes: 402.01, 402.11, 402.91, 404.01, 404.11, 404.91, 428, 404.03, 404.13, and 404.93 and 428.xx. Corresponding Medicare denominator files from 1998 to 2008 were obtained that contained information on a patient’s eligibility and enrollment in Medicare. Dates of death were ascertained through the corresponding vital status file from CMS, which includes both inhospital and out-of-hospital deaths. Beneficiaries under the age of 65 years or who were hospitalized for HF or resided outside of the 50 U.S. states, the District of Columbia and Puerto Rico were excluded from the analysis.
The unit of observation was a single beneficiary in a single year. The initial sample consisted of 479,198,670 observations in the denominator file (i.e. >40 million Medicare beneficiaries each year over 11 years). We then excluded observations with age<65 years (n=93,403,663), observations enrolled in managed care programs over an entire calendar year (n=69,398,888), or observations with home residence outside of the 50 continental states, the District of Columbia, or Puerto Rico (n=1,482,403). The final sample included 320,618,412 observations over the study period age 65 years or older, who had at least one month in Medicare fee-for-service, living in the targeted 52 states/territories/district. This represented 55,097,390 unique individual beneficiaries who contributed a total of 312,636,599 person-years of observation from 1998 to 2008.
Patient characteristics and comorbidities
Clinical characteristics of HF patients were examined across years, and stratified according to demographic factors of age (65–74, 75–84, 85 years or older), sex, and race (white, black, other). Race was determined using the Medicare denominator file which used patient-reported data from the Social Security Administration.17 Comorbidities examined were identical to those used by the CMS HF 30-day mortality measure for profiling hospitals.18 Clinical comorbidities were identified from secondary diagnosis codes that did not represent potential complications from the initial HF hospitalization, as well as principal and secondary diagnosis codes of all hospitalizations for any cause up to 1 year before the initial HF hospitalization. For conciseness, patient characteristics were reported in two-year intervals over the study period. Length of stay was calculated based on admission and discharge dates.
Primary outcomes
We calculated the HF hospitalization rate separately for each year by dividing the number of HF hospitalizations by the corresponding person-years of fee-for-service (FFS) Medicare beneficiaries for that year. Because FFS Medicare beneficiaries were enrolled throughout the year, some beneficiaries were in FFS for the entire year while others were in FFS for a few months. We tabulated the total beneficiary-months at risk (subsequently converted to beneficiary-years) for a given year to use as the denominator, with the total number HF hospitalizations for a given year as the numerator. Since beneficiaries can be hospitalized multiple times for HF in a given year, we also calculated the number of unique beneficiaries who were hospitalized with HF in a given year per 100,000 denominator population.
To calculate 1-year mortality, we identified all HF hospitalizations that occurred in a given year of interest; if a patient had more than one HF hospitalization in a given year, one HF hospitalization was selected at random. The admission date of the HF hospitalization represented the “time zero” for the mortality analysis; that is, we examined the proportion of patients who died within 1-year of the HF admission. As a result, the 1-year mortality rate represented the likelihood of death within 1 year among HF patients hospitalized in a given calendar year. We assessed trends in 1-year mortality starting from 1999 rather than 1998 in order to have a full year of comorbidity data available for all beneficiaries. We conducted sensitivity analyses comparing age-sex-race mortality models with age-sex-race-comorbidity models to assess the potential influence of changing comorbidity coding patterns on trends in risk-adjusted mortality.
Statistical analysis
To evaluate the statistical significance of changes across years in patient characteristics, HF hospitalization rate and mortality rate we used the Mantel-Haenszel chi-squared test of linear association for categorical variables, and the Cuzick non-parametric test for continuous variables. The Cuzick test is an extension of the non-parametric Wilcoxon ranksum test to evaluate trends in a measured variable across more than two ordered groups.19 For assessing trends in the overall age-sex-race-adjusted HF hospitalization rate, we calculated the number of HF hospitalizations and total person-years in each state for 18 demographic combinations representing three age categories (65–74, 75–84, and 85 or older), two sex categories, and three race categories (white, black, other).
Because of the natural clustering of observations within states, we used a 2-stage (patient-level and state-level) hierarchical generalized linear modeling (HGLM) approach for evaluating HF hospitalization rate and 1-year mortality rate as a function of patient characteristics and a random state-specific effect. This strategy accounts for within-state correlation of the observed outcomes. Details of the derivation, validation and performance of an HGLM approach compared with a medical record model of HF have been published, and such an approach is employed by CMS for public reporting of hospital-specific HF mortality.20 Hierarchical Poisson regression models with the 50 states, Puerto Rico and Washington D.C. as random intercepts were used to estimate annual changes in the age-sex-race-adjusted HF hospitalization rate, and hierarchical logistic regression models were used to estimate annual changes in the age-sex-race-comorbidity-adjusted 1-year mortality rate. Analysis of trends for the incidence and mortality models incorporated dummy variables representing each year in order to evaluate yearly changes in hospitalization or mortality rates. The baseline year served as the reference for each subsequent year; we report the point estimate and 95% confidence intervals (CI) for each year representing the change from the baseline year’s HF hospitalization (change in incident rate ratio) or mortality rate (change in odds ratio of 1-year mortality). HF hospitalization rates and 1-year mortality rates were examined separately for each race-sex categories (e.g. white male, black female, etc.) using age-adjusted models adjusted for HF hospitalization rate, and age- comorbidities-adjusted models for mortality rates.
Risk-adjusted HF hospitalization and mortality rates were calculated for each year that represented what the rate would have been if the mix of patients were identical to the initial year (i.e. 1998 for HF hospitalization, 1999 for 1-year mortality) using dummy indicator variables for each year from the above regression models. The coefficients of these dummy indicator variables in the Poisson regression model for HF hospitalization represented changes in incidence risk ratio (IRR) for a given year compared with 1998. Similarly, the coefficient of these indicator variables in the logistic regression model for 1-year mortality represents changes in the relative odds ratio (OR) compared with 1999; these odds ratios were converted into relative risk ratios using the method of Zhang and Yu21 before calculating risk-adjusted 1-year mortality rates.
State analyses
We calculated risk-standardized HF hospitalization and 1-year mortality rates separately for each of the 50 states, the District of Columbia, and Puerto Rico using an approach analogous to prior work estimating risk-standardized HF mortality rates across hospitals.20 All Medicare FFS beneficiaries were sampled if they met the study inclusion criteria. In order to categorize hospitals, we produced hospital-specific probabilities of particular events. This was accomplished using a bootstrapping procedure that sampled states with replacement. For example, to determine whether the change in HF hospitalization rate for a specific state/district/territory was significantly different (p<0.05) than the mean change for the nation we sampled the 52 state/district/territories with replacement for the baseline (1998) and final years (2008), and fit a HGLM using all patients within each sampled state. This process was repeated 2,000 times with replacement in order to estimate state-specific point-estimates and 95% confidence intervals of the change in state-specific HF hospitalization rate from 1998 and 2008; states were then classified as significantly higher or lower than the national mean change in HF hospitalization rate. We estimated the probability that a particular state had a HF hospitalization rate higher than the mean national rate based on the proportion of bootstrapped estimates exceeding the national mean. We used the same approach for the 1-year mortality rate, except that the baseline year was 1999 and the final year was 2008, and we reported the number of states that were higher, no different, or lower than zero change over the study period because 1-year mortality changed only slightly over the study period.
Analyses were conducted using SAS version 9.2 (SAS Institute Inc, Cary, North Carolina) and HLM Version 6 (Scientific Software International, Lincolnwood, Illinois). Significance level was p<0.05 using two-sided tests. Maps of HF hospitalization and 1-year mortality rates were created using ArcView 10 (ESRI, Redlands, California). Institutional Review Board review and approval was obtained through the Yale University Human Investigation Committee. Medicare data was protected through a data use agreement with CMS.
Results
Hospitalization
Patient characteristics of the HF cohort are reported in Table 1. The mean age increased from 79.0 years to 79.9 years (p-for-trend<0.001) over the study period. There was a decrease in the proportion of female patients (58.9% to 55.7%, p<0.001) and increased in the proportion of black patients (11.3% to 11.7%, p<0.001). Several comorbidities were more commonly coded over time, including hypertension (47.9% to 60.9%, p<0.001), history of pneumonia (14.5% to 22.6%, p<0.001) and renal failure (8.0% to 20.0%, p<0.001). Mean length of stay decreased from 6.8 days in 1999/2000 to 6.4 days in 2007/2008 (p<0.001).
Table 1.
Characteristics of patients hospitalized with heart failure, 1999–2008
| 1999–2000 | 2001–2002 | 2003–2004 | 2005–2006 | 2007–2008 | |
|---|---|---|---|---|---|
| Number of HF hosp | 1017410 | 1026363 | 1048103 | 953706 | 820727 |
| Age (mean, SD) | 79.0 (7.7) | 79.1 (7.8) | 79.3 (7.8) | 79.6 (7.9) | 79.9 (8.0) |
| Female | 598993 (58.9) | 599416 (58.4) | 601251 (57.4) | 536431 (56.2) | 457174 (55.7) |
| White | 860860 (84.6) | 864831 (84.3) | 880764 (84.0) | 798581 (83.7) | 688680 (83.9) |
| Black | 114804 (11.3) | 119665 (11.7) | 123185 (11.8) | 113358 (11.9) | 95707 (11.7) |
| Other race | 41746 (4.1) | 41867 (4.1) | 44154 (4.2) | 41767 (4.4) | 36340 (4.4) |
| Comorbidities | |||||
| Cardiovascular conditions and risk factors | |||||
| Coronary artery disease | 564365 (55.5) | 583036 (56.8) | 602460 (57.5) | 541162 (56.7) | 454815 (55.4) |
| Prior heart failure | 309219 (30.4) | 322255 (31.4) | 334472 (31.9) | 306133 (32.1) | 264651 (32.2) |
| Prior myocardial infarction | 73613 (7.2) | 76880 (7.5) | 75265 (7.2) | 63452 (6.7) | 55166 (6.7) |
| Unstable angina | 63460 (6.2) | 57987 (5.6) | 48696 (4.6) | 35535 (3.7) | 26455 (3.2) |
| Peripheral vascular disease | 72217 (7.1) | 77437 (7.5) | 80431 (7.7) | 72063 (7.6) | 63020 (7.7) |
| Stroke | 16627 (1.6) | 16275 (1.6) | 15581 (1.5) | 14134 (1.5) | 12354 (1.5) |
| Cerebrovascular disease other than stroke | 50941 (5.0) | 48807 (4.8) | 44433 (4.2) | 35473 (3.7) | 29676 (3.6) |
| Hypertension | 487460 (47.9) | 532256 (51.9) | 564108 (53.8) | 502223 (52.7) | 499978 (60.9) |
| Diabetes mellitus | 373151 (36.7) | 397640 (38.7) | 408184 (38.9) | 366621 (38.4) | 307059 (37.4) |
| Geriatric conditions | |||||
| Dementia | 94031 (9.2) | 102191 (10.0) | 109615 (10.5) | 102154 (10.7) | 91619 (11.2) |
| Functional disability | 24392 (2.4) | 24045 (2.3) | 22636 (2.2) | 18106 (1.9) | 17606 (2.1) |
| Malnutrition | 31327 (3.1) | 31241 (3.0) | 35052 (3.3) | 36011 (3.8) | 40134 (4.9) |
| Other Medical conditions | |||||
| Chronic obstructive pulmonary disease | 331241 (32.6) | 353538 (34.4) | 376219 (35.9) | 352487 (37.0) | 286107 (34.9) |
| Pneumonia | 147932 (14.5) | 158486 (15.4) | 168679 (16.1) | 180319 (18.9) | 185769 (22.6) |
| Respiratory Failure | 46759 (4.6) | 49056 (4.8) | 52755 (5.0) | 56480 (5.9) | 66693 (8.1) |
| Liver disease | 10806 (1.1) | 11397 (1.1) | 12522 (1.2) | 11772 (1.2) | 10246 (1.2) |
| Renal Failure | 80998 (8.0) | 96269 (9.4) | 116556 (11.1) | 146920 (15.4) | 164497 (20.0) |
| Other Non-medical conditions | |||||
| Major psychiatric disorder | 21094 (2.1) | 21732 (2.1) | 21237 (2.0) | 17252 (1.8) | 16861 (2.1) |
| Depression | 59387 (5.8) | 68443 (6.7) | 74062 (7.1) | 62283 (6.5) | 51582 (6.3) |
| Trauma in past year | 47445 (4.7) | 52321 (5.1) | 58493 (5.6) | 54851 (5.8) | 49036 (6.0) |
| Mean length of stay, days (SD) | 6.8 (5.8) | 6.8 (5.6) | 6.6 (5.4) | 6.5 (5.2) | 6.4 (5.2) |
Abbreviations: HF, heart failure; SD, standard deviation. Other race includes Asian, Hispanic, North American Native, or other not specified. Comparison across years of patient characteristics using Mantel-Haenszel chi-squared test for linear association for categorical variables and Cuzick test for continuous variables using 2-sided test. All p-values <0.001.
The number of Medicare fee-for-service beneficiary-years decreased from 35,981,165 in 1998 to 27,297,535 in 2008. (Table 2) From 1998 to 2008, the overall unadjusted HF hospitalization rate fell from 2,845 to 1,957 per 100,000, a relative decline of 31.2%. The number of unique Medicare beneficiaries enrollees hospitalized at least once for HF in a given year fell from 2,014 per 100,000 to 1,462 per 100,000 over the study period. Decreases in the unadjusted HF hospitalization rates were observed across all age, sex and race categories. (Table 2) Black men had the lowest decline in unadjusted HF hospitalization rate (4,142 to 3,201 per 100,000, −22.7%) among all race-sex categories.
Table 2.
HF hospitalization rates, 1998–2008
| 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Person-years | 35981165 | 26161068 | 26442259 | 27209640 | 27990835 | 28455841 | 28733294 | 28773892 | 28070387 | 27520683 | 27297535 |
| HF hospitalization rate per 100,000 | 2845 | 2656 | 2612 | 2542 | 2468 | 2496 | 2459 | 2333 | 2223 | 2116 | 1957 |
| # unique HF patients per 100,000 | 2014 | 1935 | 1933 | 1886 | 1833 | 1851 | 1815 | 1724 | 1631 | 1533 | 1462 |
| Observed HF hospitalization rate per 100,000 beneficiaries | |||||||||||
| Age 65 to 74 | 1783 | 1614 | 1564 | 1514 | 1468 | 1462 | 1416 | 1328 | 1229 | 1145 | 1026 |
| Age 75 to 84 | 3582 | 3264 | 3203 | 3121 | 3027 | 3065 | 3027 | 2859 | 2717 | 2586 | 2403 |
| Age 85 and higher | 5746 | 5453 | 5406 | 5297 | 5152 | 5272 | 5255 | 5081 | 4935 | 4757 | 4519 |
| Male | 2944 | 2718 | 2624 | 2565 | 2509 | 2546 | 2536 | 2437 | 2324 | 2212 | 2055 |
| Female | 2778 | 2613 | 2603 | 2527 | 2439 | 2461 | 2402 | 2258 | 2149 | 2046 | 1883 |
| White | 2749 | 2555 | 2508 | 2435 | 2361 | 2390 | 2356 | 2228 | 2121 | 2024 | 1878 |
| White male | 2882 | 2650 | 2558 | 2493 | 2434 | 2472 | 2465 | 2358 | 2251 | 2146 | 2000 |
| White female | 2658 | 2490 | 2474 | 2395 | 2310 | 2330 | 2277 | 2132 | 2026 | 1933 | 1786 |
| Black | 4311 | 4124 | 4005 | 3969 | 3888 | 3940 | 3885 | 3787 | 3669 | 3503 | 3209 |
| Black male | 4142 | 3939 | 3727 | 3749 | 3701 | 3766 | 3772 | 3758 | 3635 | 3451 | 3201 |
| Black female | 4410 | 4235 | 4172 | 4103 | 4004 | 4049 | 3955 | 3805 | 3691 | 3537 | 3215 |
| Other race | 2187 | 2177 | 2215 | 2129 | 2067 | 2053 | 1980 | 1887 | 1753 | 1627 | 1470 |
| Other male | 2260 | 2212 | 2192 | 2096 | 2090 | 2073 | 2017 | 1939 | 1781 | 1672 | 1492 |
| Other female | 2138 | 2154 | 2231 | 2154 | 2049 | 2038 | 1953 | 1848 | 1731 | 1593 | 1454 |
| Risk-adjusted HF hospitalization rate per 100,000 beneficiaries | 2845 | 2752 | 2697 | 2622 | 2542 | 2566 | 2525 | 2392 | 2272 | 2163 | 2007 |
Abbreviations: HF, heart failure; SD, standard deviation. P<0.001 across years for all subgroups using a continuous time variable from a Poisson regression model. Other race includes Asian, Hispanic, North American Native, or other not specified. Risk-adjusted rates relative to 1998
The overall risk-adjusted HF hospitalization rate fell from 2,845 per 100,000 to 2,007 (95% CI 1974 to 2041) per 100,000, a relative decline of 29.5%. (p for trend<0.001). In age-adjusted analyses stratified by race-sex categories, the HF hospitalization rate declined in 2008 compared with 1998 for white men (incidence rate ratio [IRR] = 0.73, 95%CI .0.71 to 0.74), white women (IRR=0.0.72, 95%CI 0.70 to 0.74), black men (IRR=0.81, 95%CI 0.79 to 0.84), black women (IRR= 0.76, 95%CI 0.74 to 0.78), other-race men (IRR= 0.64, 95%CI 0.61 to 0.67) and other-race women (IRR=0.67, 95%CI 0.63 to 0.70). (eFigure 1) Black men had the lowest rate of decline in age-adjusted HF hospitalization from 1998 to 2008 among all race-sex groups.
Risk-standardized HF hospitalization rates in 1998 and 2008 varied significantly by state. (Figures 1A and 1B). In 2008, the risk-standardized HF hospitalization rate was lowest in Vermont (1,149 per 100,000) and highest in Wyoming (2,931 per 100,000). Oregon had the largest relative decline in risk-standardized HF hospitalization rate between 1998 and 2008, while Wyoming did not have a significantly different change. (Figure 2A) The decline in risk-standardized HF hospitalization rate was significantly higher than the change in the national rate in sixteen states, and significantly lower in three states (Wyoming, Rhode Island, and Connecticut). The change in a state’s risk-standardized HF hospitalization rates was not associated with whether it started with a low or high baseline rate; in linear regression models, the 1998 rate was not significantly associated with the subsequent change in HF hospitalization rate between 1998 and 2008 (p=0.06) and explained little of the variance (r-squared=0.05).
Figure 1.
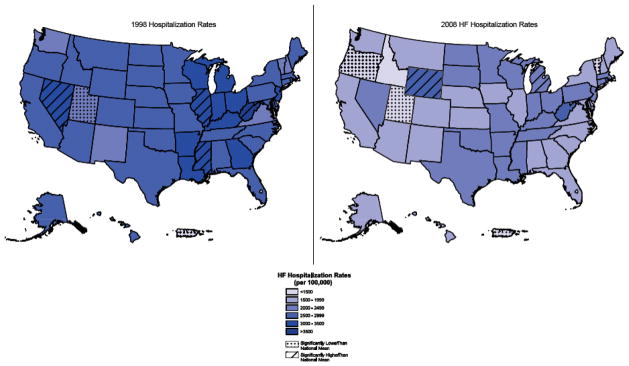
Risk-standardized HF hospitalization rate by state, (A) 1998 and (B) 2008
State-specific HF hospitalizations rates per 100,000 for 1998 and 2008.
States categorized as having HF hospitalization rate significantly higher or lower than the national mean (2-sided p<0.05) based on bootstrapped 95% confidence intervals.
Figure 2.
Change in risk-standardized (A) HF hospitalization rate and (B) 1-year mortality rate from 1998 to 2008, by state.
Point estimates represented by diamonds with 95% confidence intervals. The vertical line represents the overall national decline (for HF hospitalization rate or no change (for 1-year mortality). Probability represents the likelihood that the change in a state’s HF hospitalization rate exceeds that of the overall national rate (−838 per 100,000), or that the change in a state’s mortality rate exceeded zero, based on bootstrap analysis.
1-year Mortality
The unadjusted 1-year mortality rate for HF hospitalization was 31.7% in 1999 and 32.0% in 2008. During this time period enrollees aged 65 to 74 years and aged 75 to 84 years had decreases in unadjusted 1-year mortality (23.8% to 22.0%, p-for-trend <0.001, and 31.1% to 30.3% respectively, p for trend<0.001), while enrollees aged 85 year and older had a slight increase in 1-year mortality (42.3% to 42.7%, p<0.001). Unadjusted 1-year mortality rose for slightly for women (30.4% to 31.1%, p<0.001) but declined for men (33.6% to 33.1%, p<0.001). White beneficiaries had slightly higher unadjusted mortality rates (32.6% to 33.0%, p<0.001) while black beneficiaries had slightly lower mortality rates (26.6% to 26.2% p<0.001; beneficiaries of other race had a higher unadjusted 1-year mortality rate (27.9% to 28.7%, p<0.001). (Table 3)
Table 3.
1-year mortality rates after HF hospitalization, 1999–2008
| 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | |
|---|---|---|---|---|---|---|---|---|---|---|
| # HF hospitalizations | 506234 | 511176 | 513158 | 513205 | 526617 | 521486 | 495929 | 457777 | 421764 | 398963 |
| Overall | 31.7 | 31.4 | 31.9 | 31.2 | 31.1 | 30.6 | 30.7 | 30.7 | 31.7 | 32.0 |
| Age 65 to 74 | 23.8 | 23.4 | 23.4 | 22.5 | 22.4 | 21.7 | 21.4 | 20.9 | 21.7 | 22.0 |
| Age 75 to 84 | 31.1 | 30.5 | 31.1 | 30.5 | 30.1 | 29.6 | 29.3 | 29.1 | 30.1 | 30.3 |
| Age 85 and higher | 42.3 | 42.4 | 42.9 | 42.4 | 42.6 | 41.9 | 42.4 | 42.2 | 43.0 | 42.7 |
| Male | 33.6 | 33.4 | 33.9 | 33.0 | 32.7 | 32.0 | 31.5 | 31.5 | 32.5 | 33.1 |
| Female | 30.4 | 30.1 | 30.4 | 29.8 | 29.9 | 29.6 | 30.1 | 30.0 | 31.1 | 31.1 |
| White | 32.6 | 32.2 | 32.7 | 32.1 | 32.0 | 31.5 | 31.6 | 31.6 | 32.6 | 33.0 |
| White male | 34.5 | 34.1 | 34.8 | 33.9 | 33.5 | 32.8 | 32.2 | 32.3 | 33.3 | 34.1 |
| White female | 31.3 | 30.8 | 31.2 | 30.7 | 30.9 | 30.6 | 31 | 31 | 32 | 32.1 |
| Black | 26.6 | 26.3 | 26.6 | 25.7 | 25.8 | 25.5 | 25.6 | 25.4 | 26.5 | 26.2 |
| Black male | 27.9 | 27.8 | 28.1 | 27.1 | 27.3 | 26.7 | 26.3 | 26.4 | 26.9 | 26.9 |
| Black female | 25.8 | 25.5 | 25.8 | 25 | 25 | 24.7 | 25.2 | 24.9 | 26.2 | 25.8 |
| Other | 27.9 | 29.0 | 28.5 | 28.1 | 28.3 | 27.3 | 27.8 | 27.7 | 28.0 | 28.7 |
| Other male | 29.6 | 30.5 | 29.6 | 29.7 | 29.7 | 28.9 | 28.8 | 28.3 | 28.9 | 29 |
| Other female | 26.8 | 27.9 | 27.8 | 26.9 | 27.2 | 26.1 | 27.1 | 27.2 | 27.3 | 28.5 |
| Risk-adjusted 1 year mortality | 31.7 | 31.4 | 31.8 | 30.9 | 30.7 | 29.8 | 29.4 | 28.2 | 29.6 | 29.6 |
Abbreviations: HF, heart failure. Comparison across years using Cuzick 2-sided test with p <0.001 for all subgroups. Other race includes Asian, Hispanic, North American Native, or other not specified. Risk-adjusted rates relative to 1999
Risk-adjusted 1-year mortality (age-sex-race-comorbidity adjusted) fell from 31.7% to 29.6% between 1999 and 2008 (p-for-trend <0.001). Age-sex-race-adjusted models estimated a decline in 1-year mortality from 31.7% in 1999 to 30.6% in 2008. In age- and comorbidity-adjusted analyses stratified by race-sex categories, 1-year mortality in 2008 was lower compared with 1999 for white men (odds ratio [OR]=0.90, 95%CI 0.89 to 0.92), white women (OR=0.91, 95%CI 0.90 to 0.92), black men (OR=0.91, 95%CI 0.87 to 0.95), black women (OR=0.89, 95%CI 0.85 to 0.92) and other-race men (OR=0.89, 95%CI 0.83 to 0.95) with a non-significant trend for other-race women (OR=0.96, 95%CI 0.90 to 1.02). (eFigure 1) The mortality model C-statistic was 0.67 with an adjusted r-squared of 0.11.
The risk-standardized 1-year mortality rates in 1998 and 2008 varied substantially by state. (Figures 3A and 3B) In 2008, the 1-year risk-standardized mortality rate ranged from a low of 29.1% in Maine to a high of 35.2% in Arizona. Washington D.C. had the largest relative decline (from 32.0% to 30.3%) while South Dakota had the largest relative increase (from 30.2% to 33.0%) (Figure 2B) There were 4 states with a statistically significant decline in 1-year risk-standardized mortality between 1998 and 2008, and 5 states with a statistically significant increase. The change in a state’s risk-standardized 1-year mortality rate was not associated with whether it started with a low or high baseline rate; the 1999 rate was not significantly associated with subsequent change in mortality rate from 1999 to 2008 (p>0.99) and explained little of the variance (r-squared=0.01)
Figure 3.

Risk-standardized 1-year mortality rate by region, (A) 1999 and (B) 2008
State-specific 1-year mortality rate after HF hospitalizations for 1999 and 2008.
States categorized as having 1-year mortality rate significantly higher or lower than the national mean (2-sided p<0.05) based on bootstrapped 95% confidence intervals
Discussion
To our knowledge, this is the largest study to date examining trends in HF hospitalization rates across the U.S. We found a relative 29.5% decline in the risk-adjusted HF hospitalization rate from 1998 to 2008 that was primarily the result of fewer unique individuals hospitalized for HF. The decline in HF hospitalizations is even more remarkable given that small trend towards improved survival after HF hospitalization would allow for potentially more repeat hospitalizations for HF in a given year. In absolute terms, this implies that if the 2008 Medicare fee-for-service population of 27.3 million had a HF hospitalization rate of 1998, an additional 229,000 HF hospitalizations (95% CI 219,000 to 238,000) would have been expected that did not occur. With a mean HF hospitalization cost of $18,000 in 2008,22 this decline represents a savings on the order of $4.1 billion in fee-for-service Medicare.
Throughout this time there were changes in risk factors and clinical practice patterns that may explain the decline in HF hospitalizations. The HF hospitalization rate may have fallen due to fewer incident HF cases. Risk factors for developing HF have decreased in recent years. For example, coronary artery disease, accounting for over 60% of HF cases,23 has decreased as demonstrated by studies reporting a fall in acute myocardial infarction (AMI) rates over the past decade.6, 7 In addition, the risk of developing HF after MI has declined over time24, 25 which may reflect improvements in myocardial salvage. Hypertension is another important cause of HF,8, 26 and blood pressure control has improved modestly over time,9, 10 which may have contributed to a decline in incident HF. Second, changes in secondary prevention may reduce HF exacerbations leading to hospitalization—HF treatments such as beta-blockers, angiotensin converting enzyme-inhibitors, and angiotensin receptor blockers are known to reduce recurrent HF episodes, and use of many of these medications has increased over time.12, 27 Device therapy has also become more common for HF patients, which may have led to fewer repeat HF episodes.28 Third, our findings may reflect changing clinical practice patterns favoring outpatient rather than inpatient management of HF. A study by Ezekowitz et al observed that hospitalizations represented a smaller proportion of HF cases (39% to 30%) from 2000–2006 in Alberta, Canada with a corresponding increase towards outpatient and emergency department care.14 However, shifts away from inpatient to outpatient care of HF would be expected to affect HF hospitalization rates to a limited extent, as clinical discretion to avoid hospitalization would presumably exist only for HF cases of milder severity. While many of these factors may have contributed towards a decline in HF hospitalizations, our study is unable to determine causality.
Our finding of a substantial decline in HF hospitalizations is in contrast with studies from earlier time periods. In the Framingham Heart Study, the incidence of HF was generally stable between 1970 and 1999.15 A study of subjects living in Olmsted County, Minnesota also suggested that HF incidence was unchanged from 1979–2000.16 In the National Hospital Discharge Survey, Fang et al found an increase in HF hospitalizations between 1979 and 2004 for patients aged 65 years and older.29 Our results may differ from these earlier studies because HF hospitalizations may have started to decline only recently. A study by Curtis et al used a 5% sample of Medicare inpatient and outpatient claims, and reported a decline in HF incidence from 32.3 to 29.1 per 1,000 between 1994 and 2003;30 this dataset selected 5 out of 100 Medicare fee-for-service beneficiaries based on the last two digits of a unique patient identifier. Studies from Sweden, Scotland, Australia, and New Zealand have also reported that HF hospitalization rates started to decline in the 1990s.31–34
Differences in HF case ascertainment may also explain contrasts in HF trends across prior studies. For example, a study from southeast London reported that HF incidence (identified from both hospital and clinic visits) was unchanged between 1995–7 and 2004–5;35 data on HF hospitalization were not reported separately. The study by Ezekowitz et al reported that the HF incidence rate would have fallen more slowly if outpatient and emergency department visits were included in addition to hospitalizations.14 While our study only examined hospitalized HF cases, documenting a decline in HF hospitalizations over time is an important finding in its own right, as it suggests that overall HF incidence or its severity has decreased, or that the medical system is more effectively triaging a number of HF patients for outpatient or emergency department care.
Our study reveals a decline in the denominator of fee-for-service Medicare patients in our study over 11 years, consistent with rising enrollment for Medicare managed care programs.36, 37 However, Medicare managed care patients are likely healthier than their fee-for-service counterparts,38 a phenomenon that makes the observed decline in HF hospitalization rates in the fee-for-service population even more dramatic, considering the latter group would be expected to be composed of sicker patients. While the decline in risk-adjusted 1-year mortality rate of an absolute 2.1 percentage points between 1999 and 2008 was statistically significant, we must be cautious in its interpretation. First, risk-adjusted 1-year mortality appeared to have a nadir in 2006, and thus more recent mortality trends may not be as favorable. In addition, we note that the absolute number of lives saved over time was modest. If the 2008 Medicare fee-for-service HF population had the 1-year mortality rate of 1998, this represents only an additional 8,378 HF patients alive at 1 year. While any improvements in HF survival are to be welcomed, reductions in 1-year mortality over the past decade were modest on an absolute scale. Lastly, not all states had equal decreases in 1-year mortality; in fact, 5 states had significant increases in 1-year mortality over the study period, indicating a need for better treatment strategies in these areas.
Our study found that some comorbidities appeared to have increased over time in patients hospitalized for HF. Although some of this increase may have represented changes in coding patterns by hospitals, clinical data from the National Health and Nutrition Examination Survey suggests that the prevalence of comorbidities has increased over time in HF patients, including hypertension and renal dysfunction.39 We conducted sensitivity analyses examining how adding comorbidities would affect the mortality models. Age-sex-race-adjusted models estimated a decline in 1-year mortality from 31.7% in 1999 to 30.6% in 2008, whereas additional adjustment for comorbidities resulted in a decline to 29.6% in 2008. This suggests that secular changes in comorbidity coding would be expected to have limited influence on the change in mortality rates.
The decline in 1-year mortality for HF hospitalizations is consistent with reports of improved survival in both Framingham and Olmstead County cohorts.15, 16 In a prior study of the Medicare beneficiaries, risk-adjusted 1-year mortality decreased between 1994 and 2002.30 These trends are also consistent with our earlier study reporting 30-day mortality from 1993–2006 (a decrease from 12.6% to 10.8%).40 A recent study from the Veteran’s Administration (VA) of patients 80 years and older reported that 1-year mortality decreased from 49% to 27% over 1998–2008.41 While our study did not find such a dramatic change, this may be due to differences in the respective patient populations— VA patients were nearly entirely male and the risk profile of HF patients who seek care at the VA versus non-VA hospitals may have changed over time. While our study was unable to identify the causes of improved survival after HF hospitalization we speculate that improvements in clinical care (pharmacologic, device, risk factor management) that lead to decreased HF hospitalizations decreased mortality as well.
While the HF hospitalization rate has decreased nationally, our results demonstrate this has occurred unevenly across race-sex categories, especially for black men who had the lowest rate of decline. Similarly, 1-year mortality declined for all race-sex categories except for non-white non-black women. Administrative data is unable to identify the reasons for these disparities, but demonstrates important areas for future investigation into differences in clinical presentation and treatment patterns.
Limitations
Our study was limited to the Medicare population, and trends in HF hospitalization and mortality may differ in younger patients with different types of insurance. We were unable to determine whether the observed changes were due to changes by hospitals in medical coding; however, substantial up-coding or down-coding would likely result in changes to the coefficients of the CMS HF mortality model, yet these coefficients remained stable from 2005 to 2008.42, 43 We were unable to determine whether certain subcategories of HF may have differed, i.e. systolic versus diastolic HF, and ischemic versus non-ischemic HF. Our study focused on HF hospitalizations and was not able to assess changes in HF care in outpatient clinics or emergency departments, and as such may underestimate overall HF incidence rates.44 HF diagnosis and presence of comorbidities were based on the presence of administrative codes and not clinically confirmed; however administrative codes have been shown to be highly specific for cardiovascular diagnoses and risk factors. 45
Conclusion
From 1998 to 2008, the overall risk-adjusted HF hospitalization rate declined from 2,845 to 2,007 per 100,000 fee-for-service Medicare beneficiaries. This decline was principally due to fewer individual patients hospitalized with HF, rather than reducing the frequency of HF hospitalizations. However, black men had the lowest rate of decline for HF hospitalization among race-sex groups. Risk-adjusted 1-year mortality with HF hospitalization was 31.7% in 1999 and 29.6% in 2008. Substantial geographic variation existed for both HF hospitalization and 1-year mortality rates, representing marked differences in outcomes that are not explained insurance status.
Supplementary Material
eFigure 1. Change in (A) HF hospitalization rate and (B) 1-year mortality rate from baseline year (vertical line), by race-sex category.
Acknowledgments
This work was supported by an Agency for Healthcare Research and Quality (AHRQ) Career Development Award (1K08HS018781-01) for Dr. Chen, and a National Heart Lung Blood Institute (NHLBI) Cardiovascular Outcomes Center Award (1U01HL105270-01) for Drs. Krumholz, Normand and Wang. Funding from AHRQ and NHLBI contributed to: the design and conduct of the study; management, analysis, and interpretation of the data; and preparation of the manuscript.
Drs. Chen and Krumholz had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis
Dr. Chen—has participated sufficiently in the work to take public responsibility for the whole content, and has made substantial contributions to the intellectual content of the paper for: conception and design, analysis and interpretation of data, drafting of the manuscript, and supervision.
Dr. Krumholz—has participated sufficiently in the work to take public responsibility for the whole content, and has made substantial contributions to the intellectual content of the paper for: conception and design, acquisition of data, analysis and interpretation of data, drafting of the manuscript, obtaining funding, and supervision.
Dr. Normand —has participated sufficiently in the work to take public responsibility for part of the content, and has made substantial contributions to the intellectual content of the paper for: analysis and interpretation of data, critical revision of the manuscript for important intellectual content, and supervision.
Dr. Wang —has participated sufficiently in the work to take public responsibility for part of the content, and has made substantial contributions to the intellectual content of the paper for: analysis and interpretation of data, critical revision of the manuscript for important intellectual content, and statistical analysis.
We appreciate the assistance of Brian Merry for his construction of the Figures. Mr. Merry is an employee of the Yale-New Haven Hospital Center for Outcomes Research and Evaluation.
Contributor Information
Jersey Chen, Section of Cardiovascular Medicine, Department of Internal Medicine, Yale University School of Medicine, New Haven, Connecticut.
Sharon-Lise T. Normand, Department of Health Care Policy, Harvard Medical School and Department of Biostatistics, Harvard School of Public Health, Boston, Massachusetts.
Yun Wang, Section of Cardiovascular Medicine, Department of Internal Medicine, Yale University School of Medicine, New Haven, Connecticut. Center for Outcomes Research and Evaluation, Yale-New Haven Hospital, New Haven, Connecticut Robert Wood Johnson Clinical Scholars Program, Department of Medicine; and the Section of Health Policy and Administration, School of Public Health, Yale University School of Medicine, New Haven, Connecticut.
Harlan M. Krumholz, Section of Cardiovascular Medicine, Department of Internal Medicine, Yale University School of Medicine, New Haven, Connecticut. Center for Outcomes Research and Evaluation, Yale-New Haven Hospital, New Haven, Connecticut Robert Wood Johnson Clinical Scholars Program, Department of Medicine; and the Section of Health Policy and Administration, School of Public Health, Yale University School of Medicine, New Haven, Connecticut.
References
- 1.Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart Disease and Stroke Statistics--2010 Update: A Report From the American Heart Association. Circulation. 2010 Feb 23;121(7):e46–215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 2.Ho K, Pinsky J, Kannel W, Levy D. The epidemiology of heart failure: The Framingham Study. J Am Coll Cardiol. 1993;22:6–13. doi: 10.1016/0735-1097(93)90455-a. [DOI] [PubMed] [Google Scholar]
- 3.Wier LM, Levit K, Stranges E, et al. Exhibit 2.3 Most frequent principal diagnoses by age. Rockville, MD: Agency for Healthcare Research and Quality; [Accessed May 1, 2011]. 2010. HCUP Facts and Figures: Statistics on Hospital-based Care in the United States, 2008. Available at ( http://www.hcup-us.ahrq.gov/reports.jsp) [PubMed] [Google Scholar]
- 4.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among Patients in the Medicare Fee-for-Service Program. New England Journal of Medicine. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 5.Lloyd-Jones D, Adams RJ, et al. Writing Group M. Heart Disease and Stroke Statistics--2010 Update: A Report From the American Heart Association. Circulation. 2010 Feb 23;121(7):e46–215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 6.Chen J, Normand SL, Wang Y, Drye EE, Schreiner GC, Krumholz HM. Recent declines in hospitalizations for acute myocardial infarction for Medicare fee-for-service beneficiaries: progress and continuing challenges. Circulation. 2010 Mar 23;121(11):1322–1328. doi: 10.1161/CIRCULATIONAHA.109.862094. [DOI] [PubMed] [Google Scholar]
- 7.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010 Jun 10;362(23):2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 8.Levy D, Larson MG, Vasan RS, Kannel WB, Ho KKL. The Progression From Hypertension to Congestive Heart Failure. JAMA: The Journal of the American Medical Association. 1996 May 22;275(20):1557–1562. [PubMed] [Google Scholar]
- 9.Hajjar I, Kotchen JM, Kotchen TA. Hypertension: trends in prevalence, incidence, and control. Annu Rev Public Health. 2006;27:465–490. doi: 10.1146/annurev.publhealth.27.021405.102132. [DOI] [PubMed] [Google Scholar]
- 10.Wang TJ, Vasan RS. Epidemiology of Uncontrolled Hypertension in the United States. Circulation. 2005 Sep 13;112(11):1651–1662. doi: 10.1161/CIRCULATIONAHA.104.490599. [DOI] [PubMed] [Google Scholar]
- 11.Lee DS, Mamdani MM, Austin PC, et al. Trends in heart failure outcomes and pharmacotherapy: 1992 to 2000. Am J Med. 2004 May 1;116(9):581–589. doi: 10.1016/j.amjmed.2003.11.025. [DOI] [PubMed] [Google Scholar]
- 12.Fonarow GC, Albert NM, Curtis AB, et al. Improving evidence-based care for heart failure in outpatient cardiology practices: primary results of the Registry to Improve the Use of Evidence-Based Heart Failure Therapies in the Outpatient Setting (IMPROVE HF) Circulation. 2010 Aug 10;122(6):585–596. doi: 10.1161/CIRCULATIONAHA.109.934471. [DOI] [PubMed] [Google Scholar]
- 13.Fonarow GC, Heywood JT, Heidenreich PA, Lopatin M, Yancy CW. Temporal trends in clinical characteristics, treatments, and outcomes for heart failure hospitalizations, 2002 to 2004: findings from Acute Decompensated Heart Failure National Registry (ADHERE) Am Heart J. 2007 Jun;153(6):1021–1028. doi: 10.1016/j.ahj.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 14.Ezekowitz JA, Kaul P, Bakal JA, Quan H, McAlister FA. Trends in heart failure care: has the incident diagnosis of heart failure shifted from the hospital to the emergency department and outpatient clinics? Eur J Heart Fail. 2010 Feb;13(2):142–147. doi: 10.1093/eurjhf/hfq185. [DOI] [PubMed] [Google Scholar]
- 15.Levy D, Kenchaiah S, Larson MG, et al. Long-term trends in the incidence of and survival with heart failure. N Engl J Med. 2002 Oct 31;347(18):1397–1402. doi: 10.1056/NEJMoa020265. [DOI] [PubMed] [Google Scholar]
- 16.Roger VL, Weston SA, Redfield MM, et al. Trends in heart failure incidence and survival in a community-based population. JAMA. 2004 Jul 21;292(3):344–350. doi: 10.1001/jama.292.3.344. [DOI] [PubMed] [Google Scholar]
- 17.Eicheldinger C, Bonito A. More Accurate Racial and Ethnic Codes for Medicare Administrative Data. Health Care Financing Review. 2008 Spring;(3):27–42. [PMC free article] [PubMed] [Google Scholar]
- 18.Keenan PS, Normand S-LT, Lin Z, et al. An Administrative Claims Measure Suitable for Profiling Hospital Performance on the Basis of 30-Day All-Cause Readmission Rates Among Patients With Heart Failure/CLINICAL PERSPECTIVE. Circulation: Cardiovascular Quality and Outcomes. 2008 Sep 1;1(1):29–37. doi: 10.1161/CIRCOUTCOMES.108.802686. [DOI] [PubMed] [Google Scholar]
- 19.Cuzick J. A Wilcoxon-Type Test for Trend. Statistics in Medicine. 1985;4:87–89. doi: 10.1002/sim.4780040112. [DOI] [PubMed] [Google Scholar]
- 20.Krumholz HM, Wang Y, Mattera JA, et al. An Administrative Claims Model Suitable for Profiling Hospital Performance Based on 30-Day Mortality Rates Among Patients With Heart Failure. Circulation. 2006 Apr 4;113(13):1693–1701. doi: 10.1161/CIRCULATIONAHA.105.611194. [DOI] [PubMed] [Google Scholar]
- 21.Zhang J, Yu KF. What’s the Relative Risk? A Method of Correcting the Odds Ratio in Cohort Studies of Common Outcomes. JAMA: The Journal of the American Medical Association. 1998 Nov 18;280(19):1690–1691. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 22.Titler MG, Jensen GA, Dochterman JM, et al. Cost of hospital care for older adults with heart failure: medical, pharmaceutical, and nursing costs. Health Serv Res. 2008 Apr;43(2):635–655. doi: 10.1111/j.1475-6773.2007.00789.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Risk Factors for Congestive Heart Failure in US Men and Women: NHANES I Epidemiologic Follow-up Study. Arch Intern Med. 2001 Apr 9;161(7):996–1002. doi: 10.1001/archinte.161.7.996. [DOI] [PubMed] [Google Scholar]
- 24.Shafazand M, Rosengren A, Lappas G, Swedberg K, Schaufelberger M. Decreasing trends in the incidence of heart failure after acute myocardial infarction from 1993–2004: a study of 175,216 patients with a first acute myocardial infarction in Sweden. Eur J Heart Fail. 2011 Feb;13(2):135–141. doi: 10.1093/eurjhf/hfq205. [DOI] [PubMed] [Google Scholar]
- 25.Hellermann JP, Goraya TY, Jacobsen SJ, et al. Incidence of heart failure after myocardial infarction: is it changing over time? Am J Epidemiol. 2003 Jun 15;157(12):1101–1107. doi: 10.1093/aje/kwg078. [DOI] [PubMed] [Google Scholar]
- 26.Dunlay SM, Weston SA, Jacobsen SJ, Roger VL. Risk factors for heart failure: a population-based case-control study. Am J Med. 2009 Nov;122(11):1023–1028. doi: 10.1016/j.amjmed.2009.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith NL, Chan JD, Rea TD, et al. Time trends in the use of [beta]-blockers and other pharmacotherapies in older adults with congestive heart failure. American Heart Journal. 2004;148(4):710–717. doi: 10.1016/j.ahj.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 28.McAlister F, Ezekowitz J, Hooton N, et al. Cardiac resynchronization therapy for patients with left ventricular systolic dysfunction: a systematic review. JAMA. 2007;297(22):2502–2514. doi: 10.1001/jama.297.22.2502. [DOI] [PubMed] [Google Scholar]
- 29.Fang J, Mensah GA, Croft JB, Keenan NL. Heart failure-related hospitalization in the U.S., 1979 to 2004. J Am Coll Cardiol. 2008 Aug 5;52(6):428–434. doi: 10.1016/j.jacc.2008.03.061. [DOI] [PubMed] [Google Scholar]
- 30.Curtis LH, Whellan DJ, Hammill BG, et al. Incidence and prevalence of heart failure in elderly persons, 1994–2003. Arch Intern Med. 2008 Feb 25;168(4):418–424. doi: 10.1001/archinternmed.2007.80. [DOI] [PubMed] [Google Scholar]
- 31.Schaufelberger M, Swedberg K, Koster M, Rosen M, Rosengren A. Decreasing one-year mortality and hospitalization rates for heart failure in Sweden; Data from the Swedish Hospital Discharge Registry 1988 to 2000. Eur Heart J. 2004 Feb;25(4):300–307. doi: 10.1016/j.ehj.2003.12.012. [DOI] [PubMed] [Google Scholar]
- 32.Jhund PS, Macintyre K, Simpson CR, et al. Long-term trends in first hospitalization for heart failure and subsequent survival between 1986 and 2003: a population study of 5.1 million people. Circulation. 2009 Feb 3;119(4):515–523. doi: 10.1161/CIRCULATIONAHA.108.812172. [DOI] [PubMed] [Google Scholar]
- 33.Teng TH, Finn J, Hobbs M, Hung J. Heart failure: incidence, case fatality, and hospitalization rates in Western Australia between 1990 and 2005. Circ Heart Fail. 2010 Mar;3(2):236–243. doi: 10.1161/CIRCHEARTFAILURE.109.879239. [DOI] [PubMed] [Google Scholar]
- 34.Wasywich CA, Gamble GD, Whalley GA, Doughty RN. Understanding changing patterns of survival and hospitalization for heart failure over two decades in New Zealand: utility of ‘days alive and out of hospital’ from epidemiological data. Eur J Heart Fail. 2010 May;12(5):462–468. doi: 10.1093/eurjhf/hfq027. [DOI] [PubMed] [Google Scholar]
- 35.Mehta PA, Dubrey SW, McIntyre HF, et al. Improving survival in the 6 months after diagnosis of heart failure in the past decade: population-based data from the UK. Heart. 2009 Nov;95(22):1851–1856. doi: 10.1136/hrt.2008.156034. [DOI] [PubMed] [Google Scholar]
- 36.Congressional Budget Office Testimony SoPRO. The Medicare Advantage program: Enrollment trends and budgetary effects. Washington D.C: Congressional Budget Office; [Accessed March 8, 2011]. 2007. Director before the Committee on Finance, United States Senate, April 11, 2007. Available at http://www.cbo.gov/ftpdocs/79xx/doc7994/04-11-MedicareAdvantage.pdf. [Google Scholar]
- 37.Medicare Payment Advisory Commission. Report to Congress: Medicare Payment Policy. Vol. 2008 Washington D.C: Medicare Payment Advisory Commission; Mar, 2008. [Google Scholar]
- 38.Morgan RO, Virnig BA, DeVito CA, Persily NA. The Medicare-HMO Revolving Door — The Healthy Go in and the Sick Go Out. New England Journal of Medicine. 1997;337(3):169–175. doi: 10.1056/NEJM199707173370306. [DOI] [PubMed] [Google Scholar]
- 39.Wong CY, Chaudhry SI, Desai MM, Krumholz HM. Trends in Comorbidity, Disability, and Polypharmacy in Heart Failure. The American Journal of Medicine. 2010;124(2):136–143. doi: 10.1016/j.amjmed.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA. 2010 Jun 2;303(21):2141–2147. doi: 10.1001/jama.2010.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shah RU, Tsai V, Klein L, Heidenreich PA. Characteristics and Outcomes of Very Elderly Patients Following First Hospitalization for Heart Failure. Circ Heart Fail. 2011 Apr 5; doi: 10.1161/CIRCHEARTFAILURE.110.959114. [DOI] [PubMed] [Google Scholar]
- 42.Bernheim SM, Wang Y, Bhat KR, et al. 2010 Measures Maintenance Technical Report: Acute Myocardial Infarction, Heart Failure, and Pneumonia 30-Day Risk-Standardized Mortality Measures. New Haven, CT: Yale-New Haven Health Services Corporation/Center for Outcomes Research & Evaluation; [Accessed March 11, 2011]. 2010. Available at: http://www.qualitynet.org. [Google Scholar]
- 43.Grosso LM, Schreiner GC, Wang Y, et al. 2009 Measures Maintenance Technical Report: Acute Myocardial Infarction, Heart Failure, and Pneumonia 30-Day Risk-Standardized Mortality Measures. New Haven, CT: Yale-New Haven Health Services Corporation/Center for Outcomes Research & Evaluation; [Accessed March 11, 2011]. 2009. Available at: http://www.qualitynet.org. [Google Scholar]
- 44.Ezekowitz JA, Kaul P. The epidemiology and management of elderly patients with myocardial infarction or heart failure. Heart Fail Rev. 2010 Sep;15(5):407–413. doi: 10.1007/s10741-010-9162-x. [DOI] [PubMed] [Google Scholar]
- 45.Birman-Deych E, Waterman AD, Yan Y, Nilasena DS, Radford MJ, Gage BF. Accuracy of ICD-9-CM codes for identifying cardiovascular and stroke risk factors. Med Care. 2005 May;43(5):480–485. doi: 10.1097/01.mlr.0000160417.39497.a9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Change in (A) HF hospitalization rate and (B) 1-year mortality rate from baseline year (vertical line), by race-sex category.



