Abstract
Background
This study prospectively examined the natural clinical course of six anxiety disorders over 7 years of follow-up in individuals with personality disorders (PDs) and/or major depressive disorder. Rates of remission, relapse, new episode onset and chronicity of anxiety disorders were examined for specific associations with PDs.
Method
Participants were 499 patients with anxiety disorders in the Collaborative Longitudinal Personality Disorders Study, who were assessed with structured interviews for psychiatric disorders at yearly intervals throughout 7 years of follow-up. These data were used to determine probabilities of changes in disorder status for social phobia (SP), generalized anxiety disorder (GAD), obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), panic disorder and panic disorder with agoraphobia.
Results
Estimated remission rates for anxiety disorders in this study group ranged from 73% to 94%. For those patients who remitted from an anxiety disorder, relapse rates ranged from 34% to 67%. Rates for new episode onsets of anxiety disorders ranged from 3% to 17%. Specific PDs demonstrated associations with remission, relapse, new episode onsets and chronicity of anxiety disorders. Associations were identified between schizotypal PD with course of SP, PTSD and GAD; avoidant PD with course of SP and OCD; obsessive-compulsive PD with course of GAD, OCD, and agoraphobia; and borderline PD with course of OCD, GAD and panic with agoraphobia.
Conclusions
Findings suggest that specific PD diagnoses have negative prognostic significance for the course of anxiety disorders underscoring the importance of assessing and considering PD diagnoses in patients with anxiety disorders.
Keywords: Chronicity, anxiety disorders, personality disorders, relapse, remission
Introduction
Anxiety disorders are prevalent diagnoses and are associated with substantial life impairments (Roy-Byrne & Cowley, 1994; Bruce et al. 2005; Grant et al. 2005; Boden et al. 2007; Weisberg, 2009; Yates, 2009). Prospective studies on the course of anxiety disorders suggest a chronic burden, with low rates of recovery that appear to be worsened by certain co-morbid psychiatric conditions (Bowen et al. 2000; Yonkers et al. 2003; Bruce et al. 2005). Factors that moderate the course of anxiety disorders, thereby reducing the probability of remission or increasing the likelihood for relapse, are an important focus for research. One such factor is the presence of a co-morbid personality disorder (PD).
Research has identified increased clinical severity and decreased psychosocial functioning in patients with anxiety disorder when PDs are co-morbid (Skodol et al. 1995; Ozkan & Altindag, 2005). In community mental health settings in four urban communities, PDs were associated with anxiety disorders and contributed independently to global functioning impairment (Newton-Howes et al. 2010). However, research has not consistently identified negative outcomes in anxiety disorders co-morbid with PDs. Although a prior study reported that co-occurring PDs moderated poorer outcome for panic disorder (Roy-Byrne & Cowley, 1994), a recent study found greater improvements in psychodynamic treatment of patients with panic disorder and cluster C PD co-morbidity (Milrod et al. 2007). In addition, it is unclear which specific PD diagnoses are associated with the prospective course of specific anxiety disorders.
Few studies have examined the association between PDs and anxiety course prospectively. Individuals who met diagnostic criteria for at least one PD by early adulthood had an elevated risk for anxiety disorder onset by middle adulthood, even when controlling for a history of Axis I disorders (Johnson et al. 2006). In a 6-year follow-up of 284 Norwegian outpatients using DSM-III-R diagnoses, borderline PD (BPD) predicted any anxiety disorder at follow-up, obsessive-compulsive PD (OCPD) predicted panic disorder at follow-up and avoidant PD (AVPD) predicted social phobia (SP) at follow-up (Alnæs & Torgersen, 1999). However, these diagnoses were based on one follow-up evaluation and did not examine remissions and relapse of anxiety disorders. Only one study has examined the effect of PD co-morbidity on the prospective, naturalistic course of anxiety disorders. A 5-year follow-up of 514 participants in the Harvard/Brown Anxiety Research Program (HARP) found that DSM-III-R PDs decreased rates of remission for generalized anxiety disorder (GAD) and SP, but not panic disorder (Massion et al. 2002). Specifically, dependent and AVPDs decreased remission rates for GAD, and AVPD decreased remission rates for SP. However, this study had several limitations. Only three anxiety disorders were assessed and the rates of specific PDs in the overall sample were low enough to preclude analysis of some PDs as course predictors [i.e. <1% schizotypal PD (STPD), 3–7% BPD, 5–9% OCPD]. The analysis examined remissions but did not look at relapse, chronicity or new episodes of anxiety disorders. Although the findings suggest that the presence of a PD impairs anxiety disorder outcome, the lack of power for specific PDs leaves questions unanswered. In particular, given prior findings in HARP that co-morbid PDs are associated with course of anxiety disorders, it is important to determine whether the presence of any specific PD diagnoses, relative to other PD diagnoses, are associated with the course of anxiety disorders in a clinical group with high rates of PD diagnoses.
The Collaborative Longitudinal Personality Disorders Study (CLPS) is a prospective, naturalistic study designed to assess the course and outcome of patients with PDs and a comparison group of patients with current major depressive disorder (MDD) but no PD (Gunderson et al. 2000; McGlashan et al. 2000; Skodol et al. 2005). Patients were not excluded based on presence of an anxiety disorder. Annual assessments were made for six anxiety disorders: SP; GAD; OCD; post-traumatic stress disorders (PTSD); panic disorder with and without agoraphobia. Importantly, status of each anxiety disorder was followed throughout the study, allowing for remission and relapse analysis. Previously published CLPS diagnostic co-occurrence at baseline or lifetime frequencies (22.9% for SP, 21.4% for GAD, 15.6% for OCD, 29.6% for PTSD and 26.1% for panic disorder) indicate that many individuals with PDs also have anxiety disorders (McGlashan et al. 2000).
The purpose of this study was to examine: (1) rates of remission, relapse and new onsets of anxiety disorders in a study group with high rates of PD diagnoses; (2) the prospective effects of a set of predictors; four PD diagnoses, MDD, gender, age and number of Axis I disorders, on the probability of remission, relapse and new onsets of anxiety disorders; (3) the prospective effects of the set of predictors on the chronicity of the anxiety disorders over 7 years of follow- up. This study represents the only naturalistic prospective assessment of DSM-IV PDs on remission, relapse, new episode onsets and chronicity of multiple anxiety disorders. It also extends prior findings on DSM-III-R PDs by examining the course of anxiety disorders in a study group with high rates of PD diagnosis.
Methods
Participants
Participants were drawn from the CLPS, a multi-site, prospective naturalistic longitudinal study. Recruitment sought a diverse, clinically representative study group from in- and out-patient clinical programs affiliated with four recruitment sites (Brown, Columbia, Harvard, and Yale). CLPS enrolled 668 participants aged 18–45 years with at least one of four PDs (STPD, BPD, AVPD and OCPD), or with current MDD without any PD. Details of the CLPS methods and study group characteristics, including specific co-occurrence patterns among Axis I and Axis II diagnoses, have been reported (Gunderson et al. 2000; McGlashan et al. 2000; Skodol et al. 2005). The co-occurrence patterns echo those reported for other clinical samples (Becker et al. 2000), increasing confidence in the generalizability of this study group to other clinical groups.
The current report includes 499 participants who met criteria for current anxiety disorder at baseline, or who had new episode onsets during the 7 years of follow-up and who had at least 12 months of follow-up data available. Mean age was 32.5 (S.D. = 8.1) years. Of the participants, 65% were female and 35% male, 76% were Caucasian and 24% minorities (13% African American, 8% Hispanic American and 2% ‘other’). Baseline anxiety disorder diagnoses in this study group were 29% SP, 31% GAD, 21% OCD, 33% PTSD, 13% panic disorder, 17% panic disorder with agoraphobia and 3% agoraphobia without panic disorder. There were 58%, 25%, 8% and 4% who had one, two, three and four anxiety disorder diagnosis at baseline, respectively. Altogether, 48% had a baseline diagnosis of MDD, 26% had no other Axis I diagnosis at baseline in addition to the anxiety disorder and 46%, 21%, and 6% had one, two or three other diagnoses, respectively. PD diagnosis rates at baseline were 17% STPD, 56% AVPD, 43% OCPD and 40% BPD; 12% had no PD diagnosis.
Procedures
All participants provided written informed consent following a full description of study procedures. Each collaborating site’s Institutional Review Board approved the study protocol. Interviewers were experienced research-clinicians with masters or doctoral degrees in mental health disciplines who underwent extensive standardized training to achieve reliability in diagnostic measures. Investigators at each site supervised interviewers within and across sites to maintain reliability and prevent temporal drift.
Assessment protocol
At baseline, interviewers administered the Structured Clinical Interview for DSM-IV Axis I Disorders – Patient Version (SCID-I/P; First et al. 1996) to assess Axis I psychiatric disorders and the Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV; Zanarini et al. 1996) to assess all PDs. Participants were re-interviewed at 6 and 12 months and yearly thereafter for 7 years following baseline. The course of anxiety disorders was assessed using the Longitudinal Interval Follow-up Evaluation (LIFE; Keller et al. 1987). To maximize the reliability of the course of Axis I disorders, these follow-up interviews were not blind and were conducted by the interviewer from the previous interval whenever possible.
Measures
The SCID-I/P (First et al. 1996), a diagnostic interview to assess current and lifetime psychiatric disorders, was administered at baseline. κ coefficients for inter-rater reliability for disorders ranged from 0.57 to 1.0; κ coefficients for specific anxiety disorders were as follows: 0.65 (for panic disorder), 0.63 (for SP), 0.57 (for OCD), 0.63 (for GAD) and 0.88 (for PTSD) (Zanarini et al. 2000).
The DIPD-IV (Zanarini et al. 1996), a semi-structured diagnostic interview to assess DSM-IV Axis II PDs, was given at baseline. Each PD criterion is assessed with one or more questions rated on a 3-point scale (0 = not present; 1 = present but of uncertain clinical significance; 2 = present and clinically significant). The DIPD-IV requires that criteria be pervasive for at least 2 years and characteristic of most of the person’s adult life. Inter-rater reliability (based on 84 pairs of raters independently rating 27 videotaped assessments) κ coefficients for PD diagnoses ranged from 0.58 to 1.0 (Zanarini et al. 2000). Test–retest reliability κ coefficients (based on two direct interviews of 52 participants, performed 7–10 days apart with the second interview blind to the first interview) ranged from 0.69 (BPD) to 0.74 (OCPD).
The LIFE (Keller et al. 1987) is a semi-structured interview rating system for assessing the longitudinal course of mental disorders. The LIFE has served as the primary measure for major longitudinal studies of psychopathology (Yonkers et al. 2003; Bruce et al. 2005; Grilo et al. 2005, 2007) and has good-to-excellent reliability (Warshaw et al. 2001). The LIFE developers and official training staff at the Brown site trained and certified interviewers across sites and provided on-going training and consultation for the interview and ratings. These methods have been shown to maintain long-term reliability and prevent drift (Warshaw et al. 2001).
As in the National Institute of Mental Health – Collaborative Depression Study (NIMH-CDS) and HARP studies (Keller et al. 1982a, b; Bruce et al. 2005), the LIFE measured the weekly presence and severity of psychopathology. The severity of psychopathology is quantified by weekly ‘ psychiatric status ratings ’ (PSRs) for each Axis I disorder present. For the current study a 3-point scale was used: PSR = 1, no symptoms; PSR = 2, moderate symptoms, but less than full diagnostic criteria; PSR = 3, symptoms meeting full diagnostic criteria. Remission from anxiety disorders was defined as eight consecutive weeks with PSR ratings <2 (minimal or no symptoms). Relapse was defined as four consecutive weeks with PSR ratings of 3. These definitions parallel those used in other major longitudinal studies of psychopathology (Keller et al. 1982a, b; Bruce et al. 2005). Relapse of GAD was examined using a four consecutive week definition and a DSM-IV 26 consecutive week (6 month) diagnostic definition. For individuals with a history of meeting full criteria and time duration for GAD, emergence of >4 weeks of clinically significant symptoms after remission may represent a meaningful and distressing syndromal recurrence (Kessler et al. 2005; Ruscio et al. 2005; Angst et al. 2006). Therefore, both definitions provide relevant insight into the course of GAD.
Data analyses
Statistical analyses were conducted with SAS version 9.1.3 (SAS Institute Inc., USA). For each anxiety disorder, we used standard survival analysis methods to obtain rates of remission, relapse and new episode onsets on weekly PSR ratings over the 7 years of follow-up. Anxiety disorders examined in the analyses were SP, GAD, OCD, PTSD and panic disorder with and without agoraphobia. Although assessed, agoraphobia without panic disorder was excluded from remission and relapse analyses due to small sample size at baseline (n = 12). Cox (1972) proportional hazards regression analyses were used to examine possible predictors of remission, relapse and new episodes (individuals who did not report a current anxiety disorder episode at baseline). In these analyses, we simultaneously considered the following variables: age; gender; total number of Axis I disorders; presence of MDD, STPD, AVPD, OCPD and BPD diagnoses at baseline. Analyses considered only the first relapse in instances with multiple relapses. Linear regression analyses examined the chronicity of anxiety disorder episodes. Chronicity was determined by calculating the proportion of weeks of follow-up that were spent in episode (PSR 2 or PSR 3) for individuals with anxiety disorders at baseline and for those with new episode onsets after baseline. The same aforementioned variables were used in the chronicity analyses. For all tests, two-tailed tests with α = 0.05 were considered statistically significant.
Results
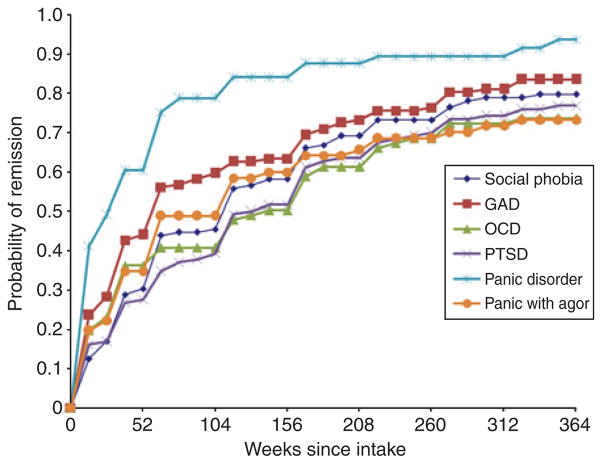
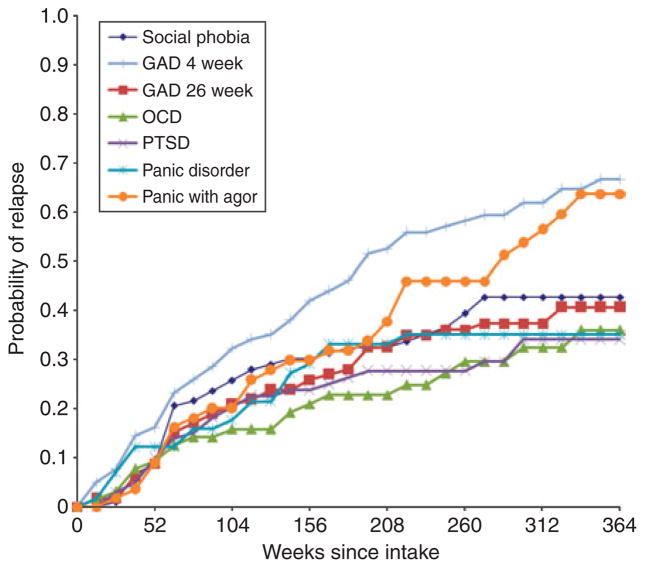
Figure 1 displays the survival curve for probability of remission from each anxiety disorder and Fig. 2 displays the survival curve for probability of relapse of each anxiety disorder. Results from the proportional hazard regressions appear in Table 1 for remission, Table 2 for relapse and Table 3 for new onsets of each anxiety disorder.
Fig. 1.
Remission survival curves for anxiety disorders over 7 years (364 weeks) of follow-up. GAD, generalized anxiety disorder; OCD, obsessive-compulsive disorder; PTSD, post-traumatic stress disorder; agor, agoraphobia.
Fig. 2.
Relapse survival curves for anxiety disorders over 7 years (364 weeks) of follow-up. GAD, generalized anxiety disorder; OCD, obsessive-compulsive disorder; PTSD, post-traumatic stress disorder; agor, agoraphobia.
Table 1.
Risk for remission of anxiety disorders
| Predictor | Social phobia
|
GAD
|
OCD
|
PTSD
|
Panic without agoraphobia
|
Panic with agoraphobia
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Risk ratio | p | Risk ratio | p | Risk ratio | p | Risk ratio | p | Risk ratio | p | Risk ratio | p | |
| Age | 0.984 | 0.18 | 1.002 | 0.90 | 0.986 | 0.36 | 0.968* | 0.03 | 0.981 | 0.28 | 0.975 | 0.18 |
| Gender | 0.912 | 0.66 | 1.091 | 0.67 | 1.051 | 0.86 | 0.801 | 0.42 | 0.756 | 0.42 | 1.502 | 0.24 |
| Axis I | 1.254 | 0.14 | 0.986 | 0.92 | 1.060 | 0.73 | 0.833 | 0.20 | 0.942 | 0.78 | 0.895 | 0.58 |
| MDD | 0.922 | 0.76 | 0.998 | 0.99 | 0.839 | 0.59 | 0.726 | 0.20 | 1.319 | 0.44 | 0.892 | 0.74 |
| STPD | 0.980 | 0.94 | 0.675 | 0.18 | 0.683 | 0.24 | 0.564* | 0.05 | 0.760 | 0.51 | 0.769 | 0.42 |
| AVPD | 0.482* | 0.002 | 0.927 | 0.69 | 1.237 | 0.44 | 0.803 | 0.28 | 0.905 | 0.75 | 1.124 | 0.69 |
| OCPD | 0.806 | 0.30 | 0.967 | 0.86 | 0.719 | 0.20 | 0.688 | 0.09 | 0.679 | 0.26 | 1.095 | 0.75 |
| BPD | 0.916 | 0.69 | 0.920 | 0.69 | 1.015 | 0.95 | 1.051 | 0.83 | 0.880 | 0.68 | 0.627 | 0.14 |
GAD, Generalized anxiety disorder; OCD, obsessive-compulsive disorder; PTSD, post-traumatic stress disorder; MDD, major depressive disorder; STPD, schizotypal personality disorder; AVPD, avoidant personality disorder; OCPD, obsessivecompulsive personality disorder; BPD, borderline personality disorder.
p≤0.05.
Table 2.
Risk for relapse of anxiety disorders
| Predictor | Social phobia
|
GAD 4 weeks
|
GAD 26 weeks
|
OCD
|
PTSD
|
Panic without agoraphobia
|
Panic with agoraphobia
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Risk ratio | p | Risk ratio | p | Risk ratio | p | Risk ratio | p | Risk ratio | p | Risk ratio | p | Risk ratio | p | |
| Age | 0.982 | 0.39 | 0.984 | 0.29 | 0.986 | 0.48 | 0.985 | 0.65 | 1.014 | 0.59 | 0.979 | 0.56 | 1.038 | 0.14 |
| Gender | 1.486 | 0.27 | 1.518 | 0.14 | 1.128 | 0.74 | 0.799 | 0.65 | 0.676 | 0.40 | 1.268 | 0.73 | 3.131* | 0.03 |
| Axis I | 1.031 | 0.89 | 1.461* | 0.05 | 1.574 | 0.08 | 0.520 | 0.11 | 1.036 | 0.90 | 0.640 | 0.19 | 2.116* | 0.03 |
| MDD | 1.037 | 0.93 | 1.139 | 0.66 | 1.112 | 0.79 | 1.682 | 0.42 | 1.229 | 0.69 | 0.910 | 0.87 | 0.414 | 0.08 |
| STPD | 2.469* | 0.03 | 1.089 | 0.85 | 1.309 | 0.60 | 0.799 | 0.75 | 1.079 | 0.88 | 0.174 | 0.10 | 1.100 | 0.84 |
| AVPD | 1.073 | 0.87 | 1.155 | 0.59 | 1.454 | 0.30 | 0.952 | 0.93 | 1.127 | 0.76 | 2.389 | 0.10 | 0.354* | 0.05 |
| OCPD | 1.083 | 0.83 | 1.784* | 0.03 | 1.317 | 0.44 | 1.148 | 0.79 | 0.332* | 0.05 | 0.701 | 0.57 | 0.668 | 0.31 |
| BPD | 0.773 | 0.48 | 1.207 | 0.51 | 0.692 | 0.36 | 3.557* | 0.01 | 1.535 | 0.34 | 3.144 | 0.06 | 1.144 | 0.75 |
GAD, Generalized anxiety disorder; OCD, obsessive-compulsive disorder; PTSD, post-traumatic stress disorder; MDD, major depressive disorder; STPD, schizotypal personality disorder; AVPD, avoidant personality disorder; OCPD, obsessive-compulsive personality disorder; BPD, borderline personality disorder.
p≤0.05.
Table 3.
New episode onsets of anxiety disorders
| Predictor | Social phobia
|
GADa
|
OCD
|
PTSD
|
Panic without agoraphobia
|
Panic with agoraphobia
|
Agoraphobia
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Risk ratio | p | Risk ratio | p | Risk ratio | p | Risk ratio | p | Risk ratio | p | Risk ratio | p | Risk ratio | p | |
| Age | 0.974 | 0.15 | 1.025 | 0.09 | 0.985 | 0.48 | 1.048* | 0.02 | 1.010 | 0.64 | 1.020 | 0.53 | 1.047 | 0.07 |
| Gender | 0.783 | 0.46 | 0.976 | 0.92 | 1.354 | 0.43 | 1.842 | 0.10 | 1.198 | 0.64 | 3.515 | 0.10 | 2.085 | 0.13 |
| Axis I | 1.409 | 0.09 | 1.292 | 0.11 | 1.157 | 0.55 | 1.082 | 0.73 | 1.310 | 0.25 | 0.763 | 0.47 | 1.299 | 0.33 |
| MDD | 1.125 | 0.75 | 0.835 | 0.52 | 0.803 | 0.60 | 0.957 | 0.91 | 1.229 | 0.63 | 1.864 | 0.34 | 1.368 | 0.52 |
| STPD | 1.080 | 0.85 | 1.041 | 0.90 | 1.967 | 0.12 | 0.750 | 0.59 | 0.582 | 0.38 | 1.237 | 0.78 | 1.035 | 0.95 |
| AVPD | 3.667* | 0.0001 | 1.218 | 0.40 | 2.039* | 0.05 | 1.215 | 0.56 | 1.183 | 0.63 | 1.706 | 0.31 | 2.240 | 0.07 |
| OCPD | 0.779 | 0.42 | 2.209* | 0.001 | 1.958* | 0.05 | 0.879 | 0.71 | 0.546 | 0.13 | 0.683 | 0.52 | 2.667* | 0.02 |
| BPD | 1.064 | 0.85 | 2.162* | 0.001 | 1.209 | 0.60 | 1.724 | 0.11 | 1.416 | 0.33 | 3.043* | 0.04 | 1.492 | 0.34 |
GAD, Generalized anxiety disorder; OCD, obsessive-compulsive disorder; PTSD, post-traumatic stress disorder; MDD, major depressive disorder; STPD, schizotypal personality disorder; AVPD, avoidant personality disorder; OCPD, obsessive-compulsive personality disorder; BPD, borderline personality disorder.
GAD onset using a 26-week definition for diagnosis.
p≤0.05.
Social phobia
Of the 135 subjects with SP at baseline, life-table analyses estimated that 79.7% had remitted by year 7. Subjects with AVPD at baseline were significantly less likely to remit from SP compared with those without AVPD [hazard ratio (HR) = 0.482, p = 0.0025]. For the 104 subjects with SP at baseline who remitted, 43% relapsed by year 7 of follow-up. Patients with STPD at baseline were more likely to have a SP relapse than those without STPD (HR = 2.469, p = 0.03). In total, 46 new episode onsets of SP occurred over 7 years of follow-up, five of which had a lifetime history of the disorder; the probability of new episode onset was 0.10. Patients with baseline AVPD were more likely to have a new episode onset of SP compared with those without AVPD (HR = 3.667, p = 0.0001). Regression analyses examining the chronicity of SP episodes show that the presence of AVPD versus no AVPD at baseline had a significantly greater effect relative to the other predictors on the proportion of weeks spent in episode of SP (β = 0.19, t = 3.11, p = 0.0022).
GAD
Of the 148 subjects with GAD at baseline, life-table analyses estimated that 83.5% had remitted by year 7. For the 118 subjects with GAD at baseline who remitted, 67% relapsed using a 4-week definition for GAD. Using a 26-week definition, 41% relapsed by year 7. Patients with OCPD at baseline were more likely to have a GAD relapse using a 4-week definition compared with those without OCPD (Table 2; HR = 1.784, p = 0.0328). A greater number of Axis I diagnoses were also associated with 4-week GAD relapse (HR = 1.461, p = 0.05). This did not hold for a 26-week definition of relapse. There were 77 new episode onsets (using a 26-week definition) of GAD by year 7; two of which had a lifetime history of the disorder. The probability of new episode onset was 0.17. Subjects with baseline OCPD were more likely than those without OCPD to have a new episode onset (HR = 2.209, p = 0.001). Patients diagnosed with BPD at intake were more likely to have a new episode onset of GAD than those without baseline BPD (HR = 2.162, p = 0.001). Regression analyses examining the chronicity of GAD episodes show that the presence of STPD versus no STPD at intake had a significantly greater effect than other predictors on the proportion of weeks spent in episode of GAD (β = 0.14, t = 2.26, p = 0.0247).
Obsessive-compulsive disorder
Of the 91 subjects with obsessive-compulsive disorder (OCD) at baseline, life-table analyses estimated that 73.6% remitted by year 7. Of the 64 subjects with OCD at baseline who remitted, 36% relapsed by year 7. Patients with BPD at intake were more likely than those without BPD to relapse in OCD (HR = 3.56, p = 0.014). There were 35 new episode onsets of OCD by year 7; four of which had a lifetime history of the disorder, with risk for new episode onset 0.07 over 7 years. Patients with OCPD or AVPD diagnosis at intake were more likely to have a new episode onset of OCD than those without these baseline diagnoses (OCPD HR = 1.958, p = 0.05 AVPD HR = 2.039, p = 0.05).
PTSD
Of the 142 subjects with PTSD at baseline, 76.8% had remitted by year 7. Subjects with STPD at baseline were significantly less likely to remit from PTSD compared with those without STPD (HR = 0.564, p = 0.05). Older patients were slightly less likely to remit from PTSD (HR = 0.968, p = 0.0337). Of the 102 subjects with PTSD at baseline who remitted, 34% had relapsed by year 7. Proportional hazard regression analyses indicate that subjects with OCPD at intake were less likely to have a PTSD relapse than those without OCPD at intake (HR = 0.332, p = 0.047). There were 39 new episode onsets of PTSD by 7 years of follow-up, 12 of which had a lifetime history of the disorder, with risk for new episode onset of 0.09. Older patients were slightly more likely to have a new episode onset of PTSD than younger patients (HR = 1.048, p = 0.0216).
Panic disorder without agoraphobia
Of the 63 subjects with panic without agoraphobia at baseline, 93.6% remitted by year 7. Of the 57 subjects with panic without agoraphobia at baseline who remitted, 35% relapsed by year 7. Having a BPD diagnosis at intake resulted in a HR of 3.14 for relapse of panic without agoraphobia and approached significance (p = 0.06). There were 34 new episode onsets of panic without agoraphobia by year 7, three of which had a lifetime history of the disorder, with the probability risk for new episode onset 0.07. Only AVPD approached significance in moderating weeks spent in episode (p = 0.058).
Panic disorder with agoraphobia
Of the 82 subjects with panic with agoraphobia diagnoses at baseline, 73.2% remitted by year 7. Of the 56 subjects with baseline panic with agoraphobia who remitted, 64% relapsed by year 7. Subjects with AVPD at intake were less likely to relapse in panic with agoraphobia than those without baseline AVPD (HR = 0.354, p = 0.047), Women were more likely to relapse (HR = 3.131, p = 0.0276) and the total number of Axis I disorders was associated with an increased relapse risk (HR = 2.116, p = 0.0261). There were 16 new episode onsets of panic with agoraphobia by year 7, with four cases having a lifetime history of the disorder; the probability of a new episode onset was 0.03. Subjects with BPD at baseline were significantly more likely than those without BPD to have a new episode onset of panic with agoraphobia (HR = 3.043, p = 0.04).
Agoraphobia without panic disorder
There were 26 new episode onsets of agoraphobia without panic during the 7-year follow-up, one of which had a lifetime history for the disorder. The probability of a new episode onset was 0.05. Those with OCPD at baseline were significantly more likely than those without OCPD to have a new episode onset of agoraphobia without panic (HR = 2.667, p = 0.016). Older age had a small but significant effect on the proportion of weeks spent in episode (β = 0.02, t = 2.49, p = 0.02).
Discussion
This study provides the first examination of the naturalistic, 7-year course of six anxiety disorders in a clinical group with a high rate of PDs. Remission estimates in this study group indicate that by year 7, between 73% and 94% of individuals had anxiety disorders remit and between 34% and 67% of those individuals had anxiety disorders relapse. When compared with findings from the HARP study (37–82% remission and 39–56% relapse; Bruce et al. 2005), these high rates of remission and relapse suggest that anxiety disorders are remitting and relapsing more frequently in a clinical group with a high rate of PD diagnoses. Our findings highlight the complex and variable course of anxiety disorders, characterized by frequent remissions and relapses over time as well as the occurrence of new onsets of anxiety disorders in patient groups with high rates of PDs. Our findings also highlight the negative prognostic significance of PDs on the course of anxiety disorders. These findings underscore the importance of considering both anxiety disorders and PDs by researchers and clinicians who work with either patient group.
The high rates of PD diagnoses in this study group allowed examination of specific PD associations with the course of specific anxiety disorders while controlling for the effects of age, gender, number of Axis I disorders and the other study PD diagnoses. OCPD was associated with increased risk for new onset of OCD, GAD and agoraphobia episodes, increased risk of GAD relapse and decreased risk of PTSD relapse over and above other factors. AVPD was associated with decreased likelihood of SP remission, increased likelihood of new SP and OCD episode onset and greater chronicity in SP episodes. AVPD was also associated with decreased risk for relapse of panic disorder with agoraphobia. BPD was associated with increased risk of new episode onsets for GAD and panic disorder with agoraphobia, as well as an increased risk of relapse of OCD. STPD was associated with decreased remission rates in PTSD, increased risk for relapse of SP and greater chronicity in GAD episodes.
Several of these findings replicate associations identified in prior studies conducted over shorter duration or without continuous follow-up. This study replicates findings that AVPD is predominately associated with the course of SP (Massion et al. 2002) and corroborates speculation that these two disorders share a common dimension (Ralevski et al. 2005; Reich, 2009). Prior research reviewed by Reich (2000) also associated cluster A PDs, such as STPD, with SP, although this finding has been dismissed by the authors as an erroneous assignment of paranoid fears to social anxiety. However, the present findings that STPD increases risk for SP in a carefully diagnosed clinical group suggest that either the prior findings may have been accurate or, alternatively, that the criteria for SP are constructed in a manner that makes it difficult to ascertain the differences in pathological mechanisms underlying the symptomatic expression. We replicated findings associating BPD with increased risk for new onsets of anxiety disorder episodes (Alnæs & Torgersen, 1999), specifically panic disorder and GAD. The BPD and STPD associations with GAD in this study group replicate the findings from a large epidemiological survey (Grant et al. 2009). Our finding associating BPD with increased risk of OCD relapse is consistent with prior findings that individuals with a BPD diagnosis and self-mutilation exhibited significantly greater OCD symptomatology (McKay et al. 2000). The present finding that PDs were not associated with remission from panic disorder also replicates prior research (Massion et al. 2002). Contrary to prior findings, we did not identify OCPD as a risk factor for new onsets or chronicity of panic disorder (Alnæs & Torgersen, 1999), although it was associated with new onsets of OCD (Maina et al. 2008) and with relapse of GAD (Grant et al. 2009). Consistent with theoretical assertions in OCPD regarding control of worry, individuals with OCPD may have increased vulnerability for worry when they find their perfectionistic motives are unattainable or their rigid standards are unmet.
These findings have several clinical and research implications. Treatment planning for individuals with co-occurring PDs and anxiety disorders may need to take into account these findings when considering the course of symptoms. In particular, individuals who present for treatment with PD diagnoses and who have a history of a co-occurring anxiety disorder (BPD with OCD, or AVPD with SP) may warrant additional treatment focus on preventing the recurrence of symptoms associated with anxiety disorder. Further research is needed to examine whether existing treatments for anxiety disorders are equally effective in samples with co-occurring PDs. In addition, the associations in course between disorders may be mechanistically explained by personality traits, which underlie both disorders. Future directions should consider whether maladaptive personality traits increase vulnerability for course of anxiety disorders.
Several potential limitations should be considered when interpreting our findings. One limitation is the absence of a comparison group with no PD for each anxiety disorder. However, this study group did contain a MDD with no PD comparison group, a diagnosis that is frequently co-morbid with anxiety disorders. This MDD control group expands the potential variance in ways that serve to strengthen the analytic approach in lieu of a purified contrast group. In addition, the study was a naturalistic study of treatment- seeking individuals, yielding greater variability among participants than a controlled treatment protocol and thereby increasing the generalizability of these findings to patients with PDs. However, these findings may not generalize to non-treatment-seeking individuals or to individuals who are treatment seeking but do not express interest in participating in research. In addition, although the LIFE methodology is well validated and reliable, it is potentially vulnerable to bias or participant difficulties in recall of symptoms. Weekly assessment of symptoms may result in different associations than were identified in the current study.
The moderating influence of PDs on anxiety disorder course may represent differential stylistic approaches that use cognitive, affective and behavioral mechanisms to differentially mitigate dispositional anxiety, increasing risk for relapse, delaying remission and increasing chronicity for anxiety disorders and decreasing risk for relapse for other anxiety disorders. For example, a diagnosis of BPD may make individuals predisposed to OCD tendencies more vulnerable to mitigating increasing anxiety resulting from affective and interpersonal instability through compulsive or impulsive behaviors, such as self-harm. Alternatively, individuals with AVPD may establish a lifestyle in which they effectively avoid social, work and recreational situations, resulting in little opportunity to experience situations in which agoraphobic responses may occur, thus ‘protecting ’ against relapse of the panic disorder. AVPD and panic disorder with agoraphobia may have a synergistic, or pathoplastic, relationship such that the presence of personality trait tendencies and anxious predispositions interact to promote the presence of one or the other disorder. Future research will need to examine the prospective interactive effects of these disorders to determine the risk, protective and/or pathoplastic mechanisms underlying these findings. In particular, future studies will need to examine the concurrent course of PDs and anxiety disorders and consider whether alternative definitions of remission, relapse and chronicity, or whether an alternative construal of the disorders (e.g. changes within diagnostic categories in the DSM), affect findings. These data not only raise questions but also inform the boundaries of these classes of disorder relevant to the development of the DSM-V.
Footnotes
Declaration of Interest
Supported by NIMH grants MH 50837, 50838, 50839, 50840, 50850; MH016545; MH073708; MH080221. This publication has been reviewed and approved by the Publications Committee of the Collaborative Longitudinal Personality Disorders Study.
References
- Alnæs R, Torgersen S. A 6-year follow-up study of anxiety disorders in psychiatric outpatients: development and continuity with personality disorders and personality traits as predictors. Nordic Journal of Psychiatry. 1999;53:409–416. [Google Scholar]
- Angst J, Gamma A, Joseph Bienvenu O, Eaton WW, Ajdacic V, Eich D, Rossler W. Varying temporal criteria for generalized anxiety disorder: prevalence and clinical characteristics in a young age cohort. Psychological Medicine. 2006;36:1283–1292. doi: 10.1017/S0033291706007938. [DOI] [PubMed] [Google Scholar]
- Becker DF, Grilo CM, Edell WS, McGlashan TH. Comorbidity of borderline personality disorder with other personality disorders in hospitalized adolescents and adults. The American Journal of Psychiatry. 2000;157:2011–2016. doi: 10.1176/appi.ajp.157.12.2011. [DOI] [PubMed] [Google Scholar]
- Boden JM, Fergusson DM, Horwood LJ. Anxiety disorders and suicidal behaviours in adolescence and young adulthood: findings from a longitudinal study. Psychological Medicine. 2007;37:431–440. doi: 10.1017/S0033291706009147. [DOI] [PubMed] [Google Scholar]
- Bowen RC, Senthilselvan A, Barale A. Physical illness as an outcome of chronic anxiety disorders. Canadian Journal of Psychiatry. 2000;45:459–464. doi: 10.1177/070674370004500506. [DOI] [PubMed] [Google Scholar]
- Bruce SE, Yonkers KA, Otto MW, Eisen JL, Weisberg RB, Pagano M, Shea MT, Keller MB. Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: a 12-year prospective study. American Journal of Psychiatry. 2005;162:1179–1187. doi: 10.1176/appi.ajp.162.6.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox DR. Regression models and life tables. Journal of the Royal Statistical Society Series B (Methodological) 1972;34:187–220. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders – Patient Version (SCID-I/P) New York State Psychiatric Institute; New York: 1996. [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Saha TD, Smith SM, Pulay AJ, Pickering RP, Ruan WJ, Compton WM. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Molecular Psychiatry. 2009;14:1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Blanco C, Stinson FS, Chou SP, Goldstein RB, Dawson DA, Smith S, Saha TD, Huang B. The epidemiology of social anxiety disorder in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2005;66:1351–1361. doi: 10.4088/jcp.v66n1102. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Pagano ME, Skodol AE, Sanislow CA, McGlashan TH, Gunderson JG, Stout RL. Natural course of bulimia nervosa and of eating disorder not otherwise specified: 5-year prospective study of remissions, relapses, and the effects of personality disorder psychopathology. Journal of Clinical Psychiatry. 2007;68:738–746. doi: 10.4088/jcp.v68n0511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Sanislow CA, Shea MT, Skodol AE, Stout RL, Gunderson JG, Yen S, Bender DS, Pagano ME, Zanarini MC, Morey LC, McGlashan TH. Two-year prospective naturalistic study of remission from major depressive disorder as a function of personality disorder comorbidity. Journal of Consulting and Clinical Psychology. 2005;73:78–85. doi: 10.1037/0022-006X.73.1.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunderson JG, Shea MT, Skodol AE, McGlashan TH, Morey LC, Stout RL, Zanarini MC, Grilo CM, Oldham JM, Keller MB. The Collaborative Longitudinal Personality Disorders Study: development, aims, design, and sample characteristics. Journal of Personality Disorders. 2000;14:300–315. doi: 10.1521/pedi.2000.14.4.300. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, Brook JS. Personality disorders evident by early adulthood and risk for anxiety disorders during middle adulthood. Journal of Anxiety Disorders. 2006;20:408–426. doi: 10.1016/j.janxdis.2005.06.001. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The Longitudinal Interval Follow-up Evaluation. A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Keller MB, Shapiro RW, Lavori PW, Wolfe N. Recovery in major depressive disorder: analysis with the life table and regression models. Archives of General Psychiatry. 1982a;39:905–910. doi: 10.1001/archpsyc.1982.04290080025004. [DOI] [PubMed] [Google Scholar]
- Keller MB, Shapiro RW, Lavori PW, Wolfe N. Relapse in major depressive disorder: analysis with the life table. Archives of General Psychiatry. 1982b;39:911–915. doi: 10.1001/archpsyc.1982.04290080031005. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Brandenburg N, Lane M, Roy-Byrne P, Stang PD, Stein DJ, Wittchen HU. Rethinking the duration requirement for generalized anxiety disorder: evidence from the National Comorbidity Survey Replication. Psychological Medicine. 2005;35:1073–1082. doi: 10.1017/s0033291705004538. [DOI] [PubMed] [Google Scholar]
- McGlashan TH, Grilo CM, Skodol AE, Gunderson JG, Shea MT, Morey LC, Zanarini MC, Stout RL. The Collaborative Longitudinal Personality Disorders Study: baseline Axis I/II and II/II diagnostic co-occurrence. Acta Psychiatrica Scandinavica. 2000;102:256–264. doi: 10.1034/j.1600-0447.2000.102004256.x. [DOI] [PubMed] [Google Scholar]
- McKay D, Kulchycky S, Danyko S. Borderline personality and obsessive-compulsive symptoms. Journal of Personality Disorders. 2000;14:57–63. doi: 10.1521/pedi.2000.14.1.57. [DOI] [PubMed] [Google Scholar]
- Maina G, Albert U, Salvi V, Pessina E, Bogetto F. Early-onset obsessive-compulsive disorder and personality disorders in adulthood. Psychiatry Research. 2008;158:217–225. doi: 10.1016/j.psychres.2006.08.003. [DOI] [PubMed] [Google Scholar]
- Massion AO, Dyck IR, Shea MT, Phillips KA, Warshaw MG, Keller MB. Personality disorders and time to remission in generalized anxiety disorder, social phobia, and panic disorder. Archives of General Psychiatry. 2002;59:434–440. doi: 10.1001/archpsyc.59.5.434. [DOI] [PubMed] [Google Scholar]
- Milrod BL, Leon AC, Barber JP, Markowitz JC, Graf E. Do comorbid personality disorders moderate panic-focused psychotherapy? An exploratory examination of the American Psychiatric Association practice guideline. Journal of Clinical Psychiatry. 2007;68:885–891. doi: 10.4088/jcp.v68n0610. [DOI] [PubMed] [Google Scholar]
- Newton-Howes G, Tyrer P, Anagnostakis K, Cooper S, Bowden-Jones O, Weaver T. The prevalence of personality disorder, its comorbidity with mental state disorders, and its clinical significance in community mental health teams. Social Psychiatry and Psychiatric Epidemiology. 2010;45:453–460. doi: 10.1007/s00127-009-0084-7. [DOI] [PubMed] [Google Scholar]
- Ozkan M, Altindag A. Comorbid personality disorders in subjects with panic disorder: do personality disorders increase clinical severity ? Comprehensive Psychiatry. 2005;46:20–26. doi: 10.1016/j.comppsych.2004.07.015. [DOI] [PubMed] [Google Scholar]
- Ralevski E, Sanislow CA, Grilo CM, Skodol AE, Gunderson JG, Tracie Shea M, Yen S, Bender DS, Zanarini MC, McGlashan TH. Avoidant personality disorder and social phobia: distinct enough to be separate disorders ? Acta Psychiatrica Scandinavica. 2005;112:208–214. doi: 10.1111/j.1600-0447.2005.00580.x. [DOI] [PubMed] [Google Scholar]
- Reich J. The relationship of social phobia to avoidant personality disorder: a proposal to reclassify avoidant personality disorder based on clinical empirical findings. European Psychiatry: Journal of the Association of European Psychiatrists. 2000;15:151–159. doi: 10.1016/s0924-9338(00)00240-6. [DOI] [PubMed] [Google Scholar]
- Reich J. Avoidant personality disorder and its relationship to social phobia. Current Psychiatry Reports. 2009;11:89–93. doi: 10.1007/s11920-009-0014-0. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne PP, Cowley DS. Course and outcome in panic disorder: a review of recent follow-up studies. Anxiety. 1994;1:151–160. doi: 10.1002/anxi.3070010402. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Lane M, Roy-Byrne P, Stang PE, Stein DJ, Wittchen HU, Kessler RC. Should excessive worry be required for a diagnosis of generalized anxiety disorder ? Results from the US National Comorbidity Survey Replication. Psychological Medicine. 2005;35:1761–1772. doi: 10.1017/S0033291705005908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skodol AE, Gunderson JG, Shea MT, McGlashan TH, Morey LC, Sanislow CA, Bender DS, Grilo CM, Zanarini MC, Yen S, Pagano ME, Stout RL. The Collaborative Longitudinal Personality Disorders Study (CLPS): overview and implications. Journal of Personality Disorders. 2005;19:487–504. doi: 10.1521/pedi.2005.19.5.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skodol AE, Oldham JM, Hyler SE, Stein DJ, Hollander E, Gallaher PE, Lopez AE. Patterns of anxiety and personality disorder comorbidity. Journal of Psychiatric Research. 1995;29:361–374. doi: 10.1016/0022-3956(95)00015-w. [DOI] [PubMed] [Google Scholar]
- Warshaw MG, Dyck I, Allsworth J, Stout RL, Keller MB. Maintaining reliability in a long-term psychiatric study: an ongoing inter-rater reliability monitoring program using the longitudinal interval follow-up evaluation. Journal of Psychiatric Research. 2001;35:297–305. doi: 10.1016/s0022-3956(01)00030-9. [DOI] [PubMed] [Google Scholar]
- Weisberg RB. Overview of generalized anxiety disorder: epidemiology, presentation, and course. Journal of Clinical Psychiatry. 2009;70 (Suppl 2):4–9. [PubMed] [Google Scholar]
- Yates WR. Phenomenology and epidemiology of panic disorder. Annals of Clinical Psychiatry: Official Journal of the American Academy of Clinical Psychiatrists. 2009;21:95–102. [PubMed] [Google Scholar]
- Yonkers KA, Bruce SE, Dyck IR, Keller MB. Chronicity, relapse, and illness – course of panic disorder, social phobia, and generalized anxiety disorder: findings in men and women from 8 years of follow-up. Depression and Anxiety. 2003;17:173–179. doi: 10.1002/da.10106. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Sickel AE, Yong L. Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV) McLean Hospital; Belmont, MA: 1996. [Google Scholar]
- Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaefer E, Morey LC, Grilo CM, Shea MT, McGlashan TH, Gunderson JG. The Collaborative Longitudinal Personality Disorders Study: reliability of axis I and II diagnoses. Journal of Personality Disorders. 2000;14:291–299. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]