Abstract
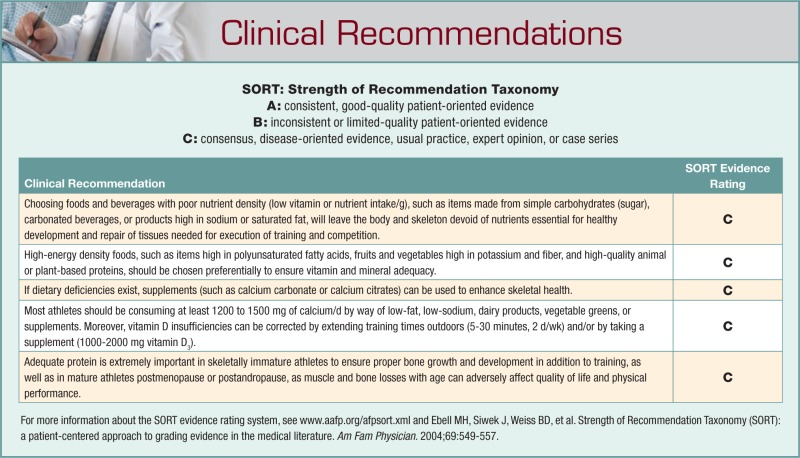
Nutrition, in sufficient amount and substance, is crucial for healthy growth and development of the skeleton and surrounding tissues, especially in physically active populations. Inadequate nutrition has been linked to maladies such as the female athlete triad, as well as poor training or competitive performance and increased risk of injury. Dietary choices favoring items high in quality protein of animal or plant origin, polyunsaturated fatty acids, fruits and vegetables high in potassium and fiber, and dairy products or other beverages fortified with calcium and vitamin D are essential to athletes to ensure adequate vitamin and mineral availability to the skeleton, which in turn can affect peak physical performance.
Keywords: bone, nutrition, dietary supplements, macronutrients, micronutrients, vitamins, osteopenia, bone mineral density, bone biomechanics
The skeleton is a dynamic tissue with structural and metabolic roles. Structurally, the skeleton protects vital organs against damaging mechanical forces, provides levers to transmit force from one area of the body to another, and has attachment sites for muscle-driven motion. Metabolically, the skeleton comprises numerous blood cell types and is the largest calcium reservoir of the body. This functional duality of bone is maintained as a dynamic homeostasis by intrinsic and extrinsic factors including diet, mechanical loading, hormonal status, and genetics. Disruption in any of these factors can have deleterious consequences.
Adequate nutrition, in amount and composition, is essential for skeletal health in all individuals, and the importance of meeting daily dietary requirements is amplified in those individuals who are physically active, such as athletes. Collective intake of vitamins, minerals, trace elements, and macronutrients must be considered to develop effective nutritional strategies to preserve bone structural integrity and strength, which can influence health and peak physical performance.
Diet plays an important role on skeletal tissue in athletic and physically active populations. Human and animal studies emphasize specific dietary and mechanical factors, their interrelations, and how they promote healthy bone growth and prevent bone loss. These factors determine bone mass, structure, quality, and rate of turnover.
Macronutrients and Bone
Diets are primarily comprised of macronutrients—protein, fat, and carbohydrates. In many instances, how these macronutrients affect bone health reflects their ability to alter calcium metabolism and, subsequently, skeletal homeostasis. Theories are presented about interrelations among selected macronutrients, calcium metabolism, and bone health.
Protein and Bone Health
Historically, conflicting evidence has characterized protein as being both detrimental and beneficial to bone health, depending on the amount of protein ingested (high-protein vs low-protein diets) and the source of protein (animal vs vegetable).30 Dietary protein represents a key nutrient in skeletal health as it affects bone in several ways: (1) it constitutes a large component of the organic structural matrix of bone, (2) it regulates serum concentrations of insulin-like growth factor (IGF)-1, and (3) it can affect calcium metabolism (calcium excretion and absorption).7,30,84
Early research suggested that high-protein diets were detrimental to skeletal health, as hypercalciuria occurred in a majority of studies after individuals consumed diets high in protein.3,12,32,61,103 Ostensibly, the consumption of animal proteins in particular could result in a substantial increase in metabolic acid production, which would necessitate the dissolution of bone mineral to neutralize the incursion of acid. It was theorized that, over time, this process would accelerate loss of bone mineral mass and increase the risk of skeletal fracture.7
An increase in calcium excretion, however, does not necessarily equate to calcium loss, negative calcium balance, and reduced bone mass. Calcium absorption must also be considered. For example, Kerstetter et al45 reported that eating a high protein diet (2.1 g of protein per 1 kg body mass) increased urinary calcium excretion, but also significantly increased intestinal calcium absorption. They hypothesized that increased absorption, and not skeletal mineral dissolution, was the main source of the elevated calcium excretion observed after ingesting high amounts of protein. Others supported that theory by arguing that the metabolic acid load, induced by consuming large amounts of protein, could be managed by the highly efficient mechanisms of hydrogen ion removal via the lung and kidney, as well as renal bicarbonate retention, without having to resort to the skeletal tissue, barring kidney or lung failure.7
Similarly, many studies have reported that high-protein diets were linked to the increased production of IGF-1, a key osteotrophic growth factor,30,84 increased bone mineral content, decreased risk of fracture, and increased fracture repair after injury.13,27,67 Higher-protein diets are also recommended for adolescent and child athletes undergoing strenuous training, as protein requirements are larger because of the process of bone modeling and growth, as well as the intensity of physical activity. Inadequate protein consumption in this group can attenuate the skeleton’s anabolic response to mechanical loading and may be detrimental to bone structure and strength.105
Diets lower in protein (0.7-0.8 g/kg) can be associated with elevated serum levels of parathyroid hormone (PTH), secondary to reduced intestinal calcium absorption, even with adequate calcium supplementation.44,45 A threshold effect was apparent, as protein levels below 0.9 g/kg were associated with disrupted mineral homeostasis.47 General agreement exists that diets moderate in protein (1.0-1.5 g/kg) are associated with normal calcium metabolism, which presumably does not alter skeletal homeostasis.46 Collectively, these data suggest that adequate protein is essential for developing and maintaining healthy skeletal tissue. Moreover, maintenance of adequate bone strength for high-performance activities is tightly linked to maintenance of adequate muscle mass and function, which is dependent on adequate intake of high-quality protein.30,98
In addition to quantity of protein, dietary protein source has also been a topic of controversy relative to bone health. The notable claim that animal proteins generate more acid and, therefore, are more calciuritic than vegetable proteins has recently been questioned. This hypothesis proposes that the sulfur content (from sulfur-containing amino acids) of animal proteins is greater than that of vegetable proteins and hence, the production of sulfuric acid from the metabolism of animal proteins would also be greater.7,62 However, Bonjour7 argues that this line of reasoning falters when considering a basic chemical analysis of the sulfur content of different proteins. The potential acid formation as sulfate was calculated, based on amino acid composition, for animal and vegetable proteins62: 82, 69, and 68 mEq/100 g protein for oatmeal, whole wheat, and white rice, respectively; and 73, 59, and 55 mEq/100 g protein in pork, beef, and milk, respectively. Bonjour’s research, numerous clinical trials,46,85 and a controlled feeding study that reported no change in urinary calcium excretion when soy protein was replaced with meat protein in postmenopausal women81 suggest that intestinal calcium absorption as determined by overall volume of protein intake is a much stronger determinant of urine calcium excretion than protein source, whether it be from plant or animal origins.7
Dietary Fat and Bone Health
In addition to protein, dietary fat in relation to bone health has also been investigated (mainly in terms of fatty acid composition). Many early nutritional studies were conducted to better understand the relation between saturated fat consumption and bone health. The relation between fat consumption and calcium absorption in a growing animal model was examined to determine whether fat favored or hindered calcium absorption in the gut.21,40,42,88 French21 used young male albino rats on diets with varying percentages of saturated fat (5%, 14%, 28%, and 45%) to substantiate claims that poor calcium absorption resulted from the formation of indigestible calcium-saturated fatty acid complexes within the intestine. Absorption of calcium decreased moderately and consistently with increasing fat content (5%-28%), with a considerable decline in intestinal calcium absorption in the 45% fat diet. Whether the decrease in calcium absorption led to decrements in skeletal strength was not reported.
Similar results have been reported in human populations. Corwin et al14 reported a negative association between saturated fat intake and hip bone mineral density (BMD) in both men and women using NHANES III (Third National Health and Nutrition Examination Survey) data (n = 14 850). After adjusting for age, sex, weight, height, race, total energy and calcium intake, smoking, and weightbearing exercise, the greatest effects were seen in men under the age of 50 years in the femoral neck, where individuals in the highest quintile of saturated fat consumption had a mean femoral neck BMD that was 4.3% less than the individuals in the lowest quintile of consumption.
Simple Carbohydrates and Bone Health
With diets high in refined sugar, the monosaccharide glucose and the disaccharide sucrose are the simple carbohydrate models that have been extensively studied. Results of many earlier studies examining glucose consumption and calcium excretion agreed that upon ingestion of glucose, calciuria was exaggerated.18,53 Lemann et al53 used healthy male subjects to investigate how glucose consumption affected urinary calcium excretion, and whether mineral loss was due to an increased glomerular filtration rate (GFR) or reduced net renal tubular reabsorption in the kidney. Despite a decrease in GFR upon standing from a recumbent position, urine excretion of calcium increased significantly for individuals administered an oral glucose solution. Glucose ingestion may (directly or indirectly) have an alteration of renal cell metabolism in the region of the distal tubule of the kidney, affecting net calcium reabsorption.
Other theories about how glucose could affect calcium metabolism have also been suggested. Ericsson et al20 reported exaggerated urinary calcium loss in young adult humans after consumption of a glucose solution. Lactic acids, formed by osteoclast metabolism of glucose molecules, may have potentially dissolved calcium and magnesium salts from adjacent bone surfaces, resulting in greater than normal calcium excretion in the urine. Alternatively, glucose in high concentrations could have a direct inhibitory effect on osteoblast proliferation and differentiation in vitro.89
In addition to implicating glucose/sucrose directly for altering renal cell metabolism, others suggest that inhibition of calcium reabsorption is mediated by the insulin response to diet. In human and animal models, an insulin spike preceded peak calcium clearance and demonstrated strong, positive correlations between serum insulin levels and urinary calcium excretion. More specifically, hypercalciuria induced by glucose could be 80% inhibited with the administration of mannoheptulose, a drug that suppresses insulin secretion.35,99 Potentially, the effect of insulin may be direct, affecting renal calcium transport by means of a calcium ATPase (an enzyme that catalyzes adenosine triphosphate [ATP] into adenosine diphosphate [ADP]) pump located on the basal-lateral membrane of the renal cell wall.49 Because insulin can inhibit calcium ATPase in adipocytes,76 a similar effect may be experienced in renal cells leading to a calciuritic response to hyperinsulinemia.
Refined carbohydrates affect bone growth and mechanical strength. Tjaderhane and Larmas91 studied growing male and female Wistar rats to test skeletal mechanical integrity in groups fed a control or high-sucrose diet. The breaking strengths of the tibiae and femurs were significantly lower in the sucrose-fed group in both sexes when compared to controls, and skeletal degradation was more prominent in females, independent of body weight.
Their data were augmented by studies54,83,104 quantifying the effect of diets high in both saturated fat and sucrose (HFS) on bone mechanics and mineralization. Li et al54 found that cortical bone exposed to an HFS diet had significantly lower maximal load and failure energies as well as decreased tensile stress at the proportional limit when compared to control samples after 10 weeks. Similar decrements in mechanical strength and bone quality were documented in the axial skeleton (vertebrae), in growing and skeletally mature animal models, and over short- and long-term studies.54,83,104 Cancellous bone, such as vertebrae, was more adversely affected than cortical bone, such as tibia, likely because of its proximity to vasculature and its accelerated rate of bone turnover.83
Consumption of carbonated beverages, such as soft drinks, is associated with significant decreases in bone mineral density in both males and females.100-102 Potential negative effects of carbonated soft drinks on bone have been linked primarily with the caffeine23 and sugar content75,92 found in these drinks. Changes in bones due to the consumption of soft drinks may be due to the concomitant decreased consumption of milk and other fluids.31 For example, a study conducted by Ogur et al75 on growing male and female Sprague-Dawley rats found that water consumption was decreased 6-fold in rats fed cola beverages, supporting claims that reduced consumption of nutrient-dense fluids may contribute to the negative effects observed in children and adolescents habitually consuming soft drinks.100,101 Moreover, these authors found that consuming cola beverages was associated with substantial increases in triglycerides, very low-density lipoproteins, and body mass, in concert with decreases in triiodothyronine (T3), thyroxine (T4), and blood iron levels.75 Femoral BMD was lower in the cola-fed groups versus controls. These data suggest a decrease in lean tissue, concomitant with an increase in fat mass in the cola-fed subjects. Moreover, cola consumption can enhance the loss of 2 micronutrients (calcium and iron) crucial to health and performance that are already likely to be low in the diets of athletes, especially young ones.63
More recently, a study was conducted to investigate the effects of feeding different sugar-sweetened beverages on bone mass and strength in growing rats.92 Rats were randomly assigned to consume either deionized, distilled water (ddH2O; control) or a ddH2O containing 13% w/v (weight/volume) glucose, sucrose, fructose, or high-fructose corn syrup (HFCS)-55 for 8 weeks. Tsanzi et al92 reported the 13% glucose solution had the most profound negative effects on the rats versus the fructose-sweetened beverage, which did not differ significantly from controls. Glucose consumption led to polydipsia, which led to a significant reduction in food and associated mineral ingestion, despite increased caloric intake. As a result, calcium and phosphorus intake was decreased, and calcium excretion was increased. Bone mineral density, bone mineral content (BMC), and total phosphorus content of whole femurs and tibiae were significantly lower in rats fed a 13% glucose solution versus fructose solution. Moreover, rats consuming the fructose solution had higher calcium intake, lower calcium excretion, and higher calcium retention versus the glucose-fed group,92 supporting previous findings reported in a human study by Milne and Nielson65 that found that bone alkaline phosphatase, a marker of bone formation, was increased with high fructose intake. Thus glucose, rather than fructose, exerts more deleterious effects on mineral balance and bone.
Of specific interest to athletes, these results have implications about the consumption of sports drinks. According to the aforementioned study, the authors suggested that the glucose/fructose ratio found in HFCS is important. For example, soft drinks use HFCS-55, a compilation of 55% fructose, 42% glucose, and 3% complex saccharides.33 This sweetener (HFCS-55) did not negatively affect the rat skeleton at any of the tested sites in the study conducted by Tsanzi et al.92 However, sports drinks (eg, Gatorade or Powerade), often consumed by athletes to replenish energy and electrolytes, commonly use HFCS-42, which contains 42% fructose and 58% glucose.33 As the glucose/fructose ratio is greater in sports drinks, it has been suggested that these beverages may potentially exert larger negative effects on the skeleton than drinks comprised of a higher proportion of fructose. Indeed, sports drink consumption has been linked with significant erosion of tooth tissue in vitro.78 Hence it may be worthwhile to promote the consumption of fluids without glucose, such as bottled or tap water, milk or soy-based solutions, or fluids containing greater proportions of fructose to glucose, such as orange juice, or sports drinks fortified with calcium to prevent losses in BMD in this population.
Fats and Carbohydrates Beneficial to Bone Health
Some evidence notwithstanding, it is important to recall that not all fats and carbohydrates are detrimental to skeletal health. On the contrary, optimal quantities of polyunsaturated fatty acids (PUFAs), such as omega-3 fatty acid chains, may inhibit the activities of osteoclasts and enhance the activities of osteoblasts in animals, thus appearing to impede bone resorption and promote bone formation.87,93 Moreover, in a recent controlled feeding study using human participants, diets high in plant-derived PUFAs were associated with decreased markers of bone resorption after 6 weeks.24 Self-reported omega-3 intake correlated with femoral neck BMD in 247 older men and women. Individuals reporting higher consumption of omega-3 fatty acids had significantly higher hip BMD than subjects reporting lower intake (<1.27 g/d).82
Complex carbohydrates, such as in fruits and vegetables, can augment skeletal growth by increasing calcium absorption and neutralizing metabolic acid loads with their substantial potassium content.71 Many fruits and vegetables contain nondigestible carbohydrates, such as inulin-type fructans, which cannot be digested by mammalian enzymes.17 As these molecules cannot be broken down in the small intestine, they travel to the colon where they ferment to produce numerous organic acids, essentially lowering the luminal pH of the large intestine. The reduction in pH alters calcium speciation, which increases calcium solubility in the lumen, largely amplifying calcium bioavailability and enhancing passive transport into the body.16 Inulins have also been reported to indirectly enhance epithelial cell growth, thus increasing absorptive area within the large and small intestine.79
Large increases in calcium absorption have been noted with the addition of dietary inulins in young adults (58% increase in calcium absorption in response to 40 g/d of inulin after 24 d)15 as well as in postmenopausal women (42% increase after consuming 8 g/d of inulins for 3 months).48 It is unclear whether the increases in calcium absorption will impact bone metabolism, but 1 clinical trial investigating this question in adolescent males found that after 1 year of inulin supplementation (8 g/d), total body BMC and BMD were higher in the inulin-supplemented group versus controls.1
Micronutrients and Bone
Dietary calcium and vitamin D are key factors in promoting bone health and preventing bone loss. Although a detailed review of how these micronutrients interact and affect bone growth and development is beyond the scope of this review,51,66,95,97 suggested requirements for athletic and physically active populations are provided.
Athletes and physically active individuals are exposed to physiologic demands substantially greater than those of sedentary individuals. As such, the need for vitamins and minerals may increase with intense physical training because of increased losses due to sweat, decreased nutrient absorption, and increased need associated with tissue maintenance and repair.51
Calcium is especially important, as benefits of adequate intake include not only the skeleton, but also muscle contraction, heartbeat regulation, nerve impulse transmission, regulation of blood pressure and immune function, and other critically important physiologic processes.51 Current daily adequate intake recommendations for calcium vary by sex and age. Optimal calcium intake is 1200 mg/d for young adults, 1000 mg/d for women ages 25 to 50 years, and 1500 mg/d for postmenopausal women not on hormone replacement therapy.51 Adequate calcium consumption is critically important for female athletes in weight-control sports such as figure skating, wrestling, dancing, boxing, gymnastics, or distance running, as these athletes commonly exhibit inadequate dietary intake of calories and nutrients, subsequently developing oligomenorrhea or amenorrhea.95 As such, optimal intake is listed as 1500 mg/d for this subgroup.2
Dairy products and other high calcium content foods are preferred calcium sources as opposed to commercial calcium supplements,69,74 largely because of calcium bioavailability as well as the nutrient density of these sources. Primary sources of calcium are cheese, milk, and yogurt, but dairy products are not the only source of dietary calcium. Kale and turnip greens, broccoli, tofu, and calcium-fortified foods such as orange juice are all examples of food that contribute to overall dietary calcium intake.51
Selected foods or supplements can contribute to increased calcium utilization and incorporation into the skeleton. For example, both phosphorus and vitamin D are effective in enhancing calcium uptake. Phosphorus intake is a critical factor for promoting the incorporation of absorbed calcium in bone, but excessive phosphorus can be detrimental to bone metabolism. As such, a calcium-to-phosphorus ratio of 2:1 is recommended for healthy bone production.43 Conversely, consumption of excess amounts of sodium can enhance calcium excretion in the urine, as calcium and sodium compete for reabsorption in the renal tubules. Nordin et al72 reported that for every 2300 mg of sodium excreted by the kidney, approximately 40 to 60 mg of calcium are also lost.
If calcium supplements are needed to augment dietary intake, there are several types of calcium supplements (calcium salts), each with distinct absorption rates: calcium carbonate (36%-42% absorbed), calcium acetate and calcium lactate (28%-36% absorbed), calcium citrate (27%-33% absorbed), and calcium gluconate (24%-30% absorbed).25 Conversely, others suggest that calcium citrate and calcium carbonate should be considered equal in regard to potential calcium absorption and benefit to the skeleton.29 As with any form of calcium, taking smaller doses at regular intervals throughout the day, as well as taking supplements with meals, can enhance mineral absorption.4
Calcium inadequacy should be a major concern for all individuals, especially athletes, as deficiencies in calcium are most often coincident with deficiencies in total energy consumption, protein intake, and vitamin D status—all of which can negatively affect bone health and physical performance.77
Vitamin D, a central factor in skeletal health, has a surprisingly high prevalence of insufficiency and deficiency worldwide, including athletic populations.11,26,97 Similar to calcium, the benefits of adequate vitamin D intake reach beyond the skeleton. Vitamin D deficiency increases the risk of autoimmune diseases and nonskeletal chronic diseases and can also have a profound effect on human immunity, inflammation, and muscle function (particularly in the elderly). Vitamin D is largely produced in skin exposed to ultraviolet light B radiation with subsequent hydroxylation in the liver and kidney, but can also be obtained in the diet from a limited number of sources including fatty fish (eg, cod liver oil or wild salmon), fortified milk/dairy products, and fortified cereal.97
Poor vitamin D status can compromise an athlete’s overall health and ability to perform by affecting bone health, innate and exercise-related immunity, and inflammation.97 Nonetheless, there is no evidence to suggest that vitamin D requirements for athletes are greater than in the general population. Athletes at risk of poor vitamin D status include those with low vitamin D intake or limited sun exposure. The latter includes athletes who only practice indoors or those who practice outdoors in the early mornings or late afternoons, as well as those diligently applying sunscreen, wearing athletic clothing with sun-protection factors, or having dark-pigmented skin.97 Additionally, as vitamin D is a fat-soluble compound stored within fatty deposits in the body, athletes with very low body fat might be at increased risk for vitamin D insufficiency resulting from limited endogenous storage potential and/or bioavailability.97
The current daily adequate intakes in Canada and the United States are 200 IU/d for children and adults up to 50 years of age, 400 IU/d for adults aged 51 to 70, and 600 IU/d for adults over 71 years of age.97 Most vitamin D experts agree, however, that the current recommended values are insufficient for optimal health and are petitioning governments to reevaluate the current evidence, which suggests at least 1000 to 4000 IU/d of vitamin D3 to ensure adequate protective health effects.28,36,94 Recommendations to help achieve adequate vitamin D status (serum 25-hydroxyvitamin D3 of at least 75-80 nmol/L) include regular safe sun exposure (2 times/wk, between the hours of 10 am and 3 pm on the arms and legs for 5-30 minutes, depending on season, latitude, and skin pigmentation) or dietary supplementation with 1000 to 2000 IU of vitamin D3/d.97
Special Nutritional Concerns: Female Athlete Triad
The female athlete triad is characterized by low energy availability (due to inadequate dietary intake, excessive physical training, or both), menstrual irregularities, and subsequent loss of bone mass. Energy availability can be defined as “dietary energy intake minus exercise energy expenditure”57 and is considered the primary nutritional concern for today’s female athlete. Low energy availability, especially in the form of fat,22,57 has been reported to affect reproductive function adversely in both short-term55,56,58,59 and long-term studies,10,96 disrupting luteinizing hormone pulsatility and negatively affecting ovarian function, and thus estrogen production.
Females participating in a number of competitive sports, as well as noncompeting physically active females, are at risk of developing one or more of the comorbidities associated with the triad, which includes low bone mass. Low energy availability and disrupted menstrual status impair bone turnover, essentially uncoupling the formation and resorption processes in favor of resorption.57 Bone density is commonly low in athletes experiencing amenorrhea or oligomenorrhea.22,57 In a randomized clinical trial, the rate of bone resorption increased and the rate of bone formation decreased in as little as 5 days after energy availability was reduced below 30 kcal/kg fat-free mass (FFM)/d (healthy, adequately nourished, sedentary young adult women achieve energy balance at an average of 45 kcal/kg FFM/d).39,55,58,59 By comparison, whereas eumenorrheic athletes have been found to restrict their energy availability by approximately 30% (>30 kcal/kg FFM/d), amenorrheic athletes have been found to restrict theirs by 44% to 67% (15-25 kcal/kg FFM/d).50,90 Maintaining healthy bone mass is critical for a number of reasons: (1) low bone density is an etiological factor in stress fractures in athletes68 and (2) low bone mass is the best predictor of postmenopausal fractures.38
As a preventative measure, some researchers suggest screening prior to participation in sports, to identify high-risk individuals. Overall, a comprehensive assessment including diet and exercise history, physical examination, mental health (ie, body image) screening, and bone density testing is recommended to discern symptoms of the triad. Moreover, if a component of the triad is subsequently diagnosed, the athlete should be treated by a team of health professionals, including physician, dietician, and psychologist, as well as active participation from the athlete’s coach, physical trainers, exercise physiologists, teammates, and parents.22,70
Menopause: Nutritional Supplements
For athletes or for women taking part in regular physical activity during perimenopause or postmenopause, recent research has found that taking nutritional supplements in addition to exercise can attenuate bone loss and potentially augment bone mass in this at-risk population. Calcium and vitamin D take on an increasingly critical role in the maintenance of skeletal integrity in this population. A recent randomized trial conducted for the Women’s Health Initiative (WHI) found that calcium and vitamin D supplementation resulted in considerably less bone loss at the hip in postmenopausal women compared with placebo.41 A review by Rizzoli et al80 also found that vitamin D and calcium, when taken together, are effective in preventing bone loss52,86 and preventing fracture. Combined supplementation of vitamin D with calcium reduced risk of hip fracture by 25% and risk of nonvertebral fracture by 23%.8 Efficacy for antiresorptive therapies is based on combining treatment with calcium and vitamin D supplementation. As such, women on antiresorptive therapy should also be combining their treatment with calcium and vitamin D for optimal results.6,19,64
Use of dietary supplements in postmenopausal women is encouraged, especially over the age of 65 years or if previously diagnosed with osteopenia or a vitamin deficiency, as dietary intake of calcium and vitamin D generally falls in this population. Endogenous production of vitamin D decreases because of a combination of decreasing sunlight exposure and age-related declines in the ability of the dermis to manufacture vitamin D precursors.34,60 Intestinal absorption and renal reabsorption of calcium also decrease with increasing age.73 Thus, daily oral doses of 700 to 800 IU of vitamin D and 1000 to 1200 mg of calcium may be a cost-effective way to attenuate bone loss and prevent fracture in postmenopausal women.80
Another fat-soluble vitamin, vitamin K, can also exert a protective effect on the postmenopausal skeleton. In a recent randomized control trial, subjects taking a vitamin K supplement of 200 µg/d (ie, obtainable from consuming approximately 50 g of green, leafy vegetables) in combination with vitamin D and calcium reported a significant increase in ultradistal BMD and BMC.5 These results were substantiated by a study of 155 postmenopausal women given a vitamin K supplement in addition to calcium and vitamin D. Participants consuming vitamin K showed a 35% reduction in bone loss at the femoral neck after 36 months of supplementation.9
In the interest of maintaining musculoskeletal tissues to enhance performance in elderly athletes, a recent randomized controlled trial performed on 29 early postmenopausal women suggested that ingesting a protein-containing nutrient supplement (10 g of whey protein, 31 g of carbohydrate, 5 µg of vitamin D, and 250 mg of calcium) after a 24-week strength training program enhanced muscle mass and strength by 6% to 12%, lean body mass, and femoral neck BMD by 1% to 3% (likely in response to elevated levels of osteocalcin) versus controls.37 Although the specific nutritional component to incur the positive benefits observed in this study was not elucidated, the authors reasoned that the promotion of adequate nutrition is essential, and that these effects would likely be enhanced further if applied over several years, presumably resulting in a perceptible difference in health and physical function.
Summary
Adequate nutritional status is critical to the development and maintenance of a healthy skeleton—the apparatus upon which physical activities and exercise are performed. Appropriate dietary choices enhance overall health and augment peak physical performance in athletes of all ages. Nutritional adequacy is a necessity for skeletal and overall health, and provides a strong foundation upon which to train, grow, and develop physically.
Footnotes
No potential conflict of interest declared.
References
- 1. Abrams SA, Griffin IJ, Hawthorne KM, et al. A combination of prebiotic short- and long-chain inulin-type fructans enhances calcium absorption and bone mineralization in young adolescents. Am J Clin Nutr. 2005;82(2):471-476 [DOI] [PubMed] [Google Scholar]
- 2. American Academy of Pediatrics, Committee on Sports Medicine and Fitness Medical concerns in the female athlete. Pediatrics. 2000;106(3):610-613 [PubMed] [Google Scholar]
- 3. Bengoa JM, Sitrin MD, Wood RJ, Rosenberg IH. Amino acid-induced hypercalciuria in patients on total parenteral nutrition. Am J Clin Nutr. 1983;38(2):264-269 [DOI] [PubMed] [Google Scholar]
- 4. Blanchard J, Aeschlimann JM. Calcium absorption in man: some dosing recommendations. J Pharmacokinet Biopharm. 1989;17(6):631-644 [DOI] [PubMed] [Google Scholar]
- 5. Bolton-Smith C, McMurdo ME, Paterson CR, et al. Two-year randomized controlled trial of vitamin K1 (phylloquinone) and vitamin D3 plus calcium on the bone health of older women. J Bone Miner Res. 2007;22(4):509-519 [DOI] [PubMed] [Google Scholar]
- 6. Bone HG, Hosking D, Devogelaer JP, et al. Ten years’ experience with alendronate for osteoporosis in postmenopausal women. N Engl J Med. 2004;350(12):1189-1199 [DOI] [PubMed] [Google Scholar]
- 7. Bonjour JP. Dietary protein: an essential nutrient for bone health. J Am Coll Nutr. 2005;24(6 Suppl):526S-536S [DOI] [PubMed] [Google Scholar]
- 8. Boonen S, Lips P, Bouillon R, Bischoff-Ferrari HA, Vanderschueren D, Haentjens P. Need for additional calcium to reduce the risk of hip fracture with vitamin d supplementation: evidence from a comparative metaanalysis of randomized controlled trials. J Clin Endocrinol Metab. 2007;92(4):1415-1423 [DOI] [PubMed] [Google Scholar]
- 9. Braam LA, Knapen MH, Geusens P, et al. Vitamin K1 supplementation retards bone loss in postmenopausal women between 50 and 60 years of age. Calcif Tissue Int. 2003;73:21-26 [DOI] [PubMed] [Google Scholar]
- 10. Bullen BA, Skrinar GS, Beitins IZ, von Mering G, Turnbull BA, McArthur JW. Induction of menstrual disorders by strenuous exercise in untrained women. N Engl J Med. 1985;312(21):1349-1353 [DOI] [PubMed] [Google Scholar]
- 11. Chen TC, Chimeh F, Lu Z, et al. Factors that influence the cutaneous synthesis and dietary sources of vitamin D. Arch Biochem Biophys. 2007;460(2):213-217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chu JY, Margen S, Costa FM. Studies in calcium metabolism, II: effects of low calcium and variable protein intake on human calcium metabolism. Am J Clin Nutr. 1975;28(9):1028-1035 [DOI] [PubMed] [Google Scholar]
- 13. Cooper C, Atkinson EJ, Hensrud DD, et al. Dietary protein intake and bone mass in women. Calcif Tissue Int. 1996;58(5):320-325 [DOI] [PubMed] [Google Scholar]
- 14. Corwin RL, Hartman TJ, Maczuga SA, Graubard BI. Dietary saturated fat intake is inversely associated with bone density in humans: analysis of NHANES III. J Nutr. 2006;136(1):159-165 [DOI] [PubMed] [Google Scholar]
- 15. Coudray C, Bellanger J, Castiglia-Delavaud C, Remesy C, Vermorel M, Rayssignuier Y. Effect of soluble or partly soluble dietary fibres supplementation on absorption and balance of calcium, magnesium, iron and zinc in healthy young men. Eur J Clin Nutr. 1997;51:375-380 [DOI] [PubMed] [Google Scholar]
- 16. Coxam V. Current data with inulin-type fructans and calcium, targeting bone health in adults. J Nutr. 2007;137(11 Suppl):2527S-2533S [DOI] [PubMed] [Google Scholar]
- 17. Cummings JH, Macfarlane GT, Englyst HN. Prebiotic digestion and fermentation. Am J Clin Nutr. 2001;73(2 Suppl):415S-420S [DOI] [PubMed] [Google Scholar]
- 18. DeFronzo RA, Cooke CR, Andres R, Faloona GR, Davis PJ. The effect of insulin on renal handling of sodium, potassium, calcium, and phosphate in man. J Clin Invest. 1975;55(4):845-855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Delmas PD, Ensrud KE, Adachi JD, et al. Efficacy of raloxifene on vertebral fracture risk reduction in postmenopausal women with osteoporosis: four-year results from a randomized clinical trial. J Clin Endocrinol Metab. 2002;87(8):3609-3617 [DOI] [PubMed] [Google Scholar]
- 20. Ericsson Y, Angmar-Mansson B, Flores M. Urinary mineral ion loss after sugar ingestion. Bone Miner. 1990;9(3):233-237 [DOI] [PubMed] [Google Scholar]
- 21. French CE. The interrelation of calcium and fat utilization in the growing albino rat. J Nutr. 1942;23:375-384 [Google Scholar]
- 22. Gabel KA. Special nutritional concerns for the female athlete. Curr Sports Med Rep. 2006;5(4):187-191 [DOI] [PubMed] [Google Scholar]
- 23. Garcia-Contreras F, Paniagua R, Avila-Diaz M, et al. Cola beverage consumption induces bone mineralization reduction in ovariectomized rats. Arch Med Res. 2000;31(4):360-365 [DOI] [PubMed] [Google Scholar]
- 24. Griel AE, Kris-Etherton PM, Hilpert KF, Zhao G, West SG, Corwin RL. An increase in dietary n-3 fatty acids decreases a marker of bone resorption in humans. Nutr J. 2007;6:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gropper SS, Smith JL, Groff JL. Advanced Nutrition and Human Metabolism. 4th ed. Belmont, CA: Wadsworth Thompson Learning; 2004 [Google Scholar]
- 26. Hanley DA, Davison KS. Vitamin D insufficiency in North America. J Nutr. 2005;135(2):332-337 [DOI] [PubMed] [Google Scholar]
- 27. Hannan MT, Tucker KL, Dawson-Hughes B, Cupples LA, Felson DT, Kiel DP. Effect of dietary protein on bone loss in elderly men and women: the Framingham Osteoporosis Study. J Bone Miner Res. 2000;15(12):2504-2512 [DOI] [PubMed] [Google Scholar]
- 28. Heaney RP. The Vitamin D requirement in health and disease. J Steroid Biochem Mol Biol. 2005;97(1-2):13-19 [DOI] [PubMed] [Google Scholar]
- 29. Heaney RP, Dowell MS, Bierman J, Hale CA, Bendich A. Absorbability and cost effectiveness in calcium supplementation. J Am Coll Nutr. 2001;20(3):239-246 [DOI] [PubMed] [Google Scholar]
- 30. Heaney RP, Layman DK. Amount and type of protein influences bone health. Am J Clin Nutr. 2008;87(5):1567S-1570S [DOI] [PubMed] [Google Scholar]
- 31. Heaney RP, Rafferty K. Carbonated beverages and urinary calcium excretion. Am J Clin Nutr. 2001;74(3):343-347 [DOI] [PubMed] [Google Scholar]
- 32. Hegsted M, Schuette SA, Zemel MB, Linkswiler HM. Urinary calcium and calcium balance in young men as affected by level of protein and phosphorus intake. J Nutr. 1981;111(3):553-562 [DOI] [PubMed] [Google Scholar]
- 33. Hein G, White J, Storey M, Lineback D. Highs and lows of high fructose corn syrup. Nutr Today. 2005;40:253-256 [Google Scholar]
- 34. Holick MF, Matsuoka LY, Wortsman J. Age, vitamin D, and solar ultraviolet. Lancet. 1989;2(8671):1104-1105 [DOI] [PubMed] [Google Scholar]
- 35. Holl MG, Allen LH. Sucrose ingestion, insulin response and mineral metabolism in humans. J Nutr. 1987;117(7):1229-1233 [DOI] [PubMed] [Google Scholar]
- 36. Hollis BW. Circulating 25-hydroxyvitamin D levels indicative of vitamin D sufficiency: implications for establishing a new effective dietary intake recommendation for vitamin D. J Nutr. 2005;135(2):317-322 [DOI] [PubMed] [Google Scholar]
- 37. Holm L, Olesen JL, Matsumoto K, et al. Protein-containing nutrient supplementation following strength training enhances the effect on muscle mass, strength, and bone formation in postmenopausal women. J Appl Physiol. 2008;105(1):274-281 [DOI] [PubMed] [Google Scholar]
- 38. Hui SL, Slemenda CW, Johnston CC., Jr. Baseline measurement of bone mass predicts fracture in white women. Ann Intern Med. 1989;111(5):355-361 [DOI] [PubMed] [Google Scholar]
- 39. Ihle R, Loucks AB. Dose-response relationships between energy availability and bone turnover in young exercising women. J Bone Miner Res. 2004;19(8):1231-1240 [DOI] [PubMed] [Google Scholar]
- 40. Irving L. The relation of solubility to the absorption of calcium salts from the intestine. J Biol Chem. 1926;68:518 [Google Scholar]
- 41. Jackson RD, LaCroix AZ, Gass M, et al. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med. 2006;354(7):669-683 [DOI] [PubMed] [Google Scholar]
- 42. Jones J. The influence of fat on calcium and phosphorus metabolism. J Nutr. 1940;20:367 [Google Scholar]
- 43. Kass-Wolff JH. Calcium in women: healthy bones and much more. J Obstet Gynecol Neonatal Nurs. 2004;33(1):21-33 [DOI] [PubMed] [Google Scholar]
- 44. Kerstetter JE, Caseria DM, Mitnick ME, et al. Increased circulating concentrations of parathyroid hormone in healthy, young women consuming a protein-restricted diet. Am J Clin Nutr. 1997;66(5):1188-1196 [DOI] [PubMed] [Google Scholar]
- 45. Kerstetter JE, O’Brien KO, Insogna KL. Dietary protein affects intestinal calcium absorption. Am J Clin Nutr. 1998;68(4):859-865 [DOI] [PubMed] [Google Scholar]
- 46. Kerstetter JE, O’Brien KO, Insogna KL. Dietary protein, calcium metabolism, and skeletal homeostasis revisited. Am J Clin Nutr. 2003;78(3 Suppl):584S-592S [DOI] [PubMed] [Google Scholar]
- 47. Kerstetter JE, Svastisalee CM, Caseria DM, Mitnick ME, Insogna KL. A threshold for low-protein-diet-induced elevations in parathyroid hormone. Am J Clin Nutr. 2000;72(1):168-173 [DOI] [PubMed] [Google Scholar]
- 48. Kim YY, Lee EY, Cho YH, et al. The effect of chicory fructan fiber on calcium absorption and bone metabolism in Korean postmenopausal women. Nutr Sci. 2004;7:151-157 [Google Scholar]
- 49. Kinne-Saffran E, Kinne R. Localization of a calcium-stimulated ATPase in the basal-lateral plasma membranes of the proximal tubule of rat kidney cortex. J Membr Biol. 1974;17:263-274 [DOI] [PubMed] [Google Scholar]
- 50. Kopp-Woodroffe SA, Manore MM, Dueck CA, Skinner JS, Matt KS. Energy and nutrient status of amenorrheic athletes participating in a diet and exercise training intervention program. Int J Sport Nutr. 1999;9(1):70-88 [DOI] [PubMed] [Google Scholar]
- 51. Kunstel K. Calcium requirements for the athlete. Curr Sports Med Rep. 2005;4(4):203-206 [DOI] [PubMed] [Google Scholar]
- 52. Lanham-New SA. Importance of calcium, vitamin D and vitamin K for osteoporosis prevention and treatment. Proc Nutr Soc. 2008;67(2):163-176 [DOI] [PubMed] [Google Scholar]
- 53. Lemann J, Jr, Lennon EJ, Piering WR, Prien EL, Jr, Ricanati ES. Evidence that glucose ingestion inhibits net renal tubular reabsorption of calcium and magnesium in man. J Lab Clin Med. 1970;75(4):578-585 [PubMed] [Google Scholar]
- 54. Li KC, Zernicke RF, Barnard RJ, Li AF. Effects of a high fat-sucrose diet on cortical bone morphology and biomechanics. Calcif Tissue Int. 1990;47(5):308-313 [DOI] [PubMed] [Google Scholar]
- 55. Loucks AB. The response of luteinizing hormone pulsatility to 5 days of low energy availability disappears by 14 years of gynecological age. J Clin Endocrinol Metab. 2006;91(8):3158-3164 [DOI] [PubMed] [Google Scholar]
- 56. Loucks AB, Heath EM. Dietary restriction reduces luteinizing hormone (LH) pulse frequency during waking hours and increases LH pulse amplitude during sleep in young menstruating women. J Clin Endocrinol Metab. 1994;78(4):910-915 [DOI] [PubMed] [Google Scholar]
- 57. Loucks AB, Stachenfeld NS, DiPietro L. The female athlete triad: do female athletes need to take special care to avoid low energy availability? Med Sci Sports Exerc. 2006;38(10):1694-1700 [DOI] [PubMed] [Google Scholar]
- 58. Loucks AB, Thuma JR. Luteinizing hormone pulsatility is disrupted at a threshold of energy availability in regularly menstruating women. J Clin Endocrinol Metab. 2003;88(1):297-311 [DOI] [PubMed] [Google Scholar]
- 59. Loucks AB, Verdun M, Heath EM. Low energy availability, not stress of exercise, alters LH pulsatility in exercising women. J Appl Physiol. 1998;84(1):37-46 [DOI] [PubMed] [Google Scholar]
- 60. MacLaughlin J, Holick MF. Aging decreases the capacity of human skin to produce vitamin D3. J Clin Invest. 1985;76(4):1536-1538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Margen S, Chu JY, Kaufmann NA, Calloway DH. Studies in calcium metabolism, I: the calciuretic effect of dietary protein. Am J Clin Nutr. 1974;27(6):584-589 [DOI] [PubMed] [Google Scholar]
- 62. Massey LK. Dietary animal and plant protein and human bone health: a whole foods approach. J Nutr. 2003;133(3):862S-865S [DOI] [PubMed] [Google Scholar]
- 63. Maughan R. Nutrition and the young athlete. Medicina Sportiva. 2000;4:E51-E58 [Google Scholar]
- 64. Meunier PJ, Roux C, Seeman E, et al. The effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosis. N Engl J Med. 2004;350(5):459-468 [DOI] [PubMed] [Google Scholar]
- 65. Milne DB, Nielsen FH. The interaction between dietary fructose and magnesium adversely affects macromineral homeostasis in men. J Am Coll Nutr. 2000;19(1):31-37 [DOI] [PubMed] [Google Scholar]
- 66. Morgan KT. Nutritional determinants of bone health. J Nutr Elder. 2008;27(1-2):3-27 [DOI] [PubMed] [Google Scholar]
- 67. Munger RG, Cerhan JR, Chiu BC. Prospective study of dietary protein intake and risk of hip fracture in postmenopausal women. Am J Clin Nutr. 1999;69(1):147-152 [DOI] [PubMed] [Google Scholar]
- 68. Myburgh KH, Hutchins J, Fataar AB, Hough SF, Noakes TD. Low bone density is an etiologic factor for stress fractures in athletes. Ann Intern Med. 1990;113(10):754-759 [DOI] [PubMed] [Google Scholar]
- 69. National Institutes of Health Consensus Development Conference Statement: Osteoporosis Prevention, Diagnosis, and Therapy. Bethesda, MD: National Institutes of Health; 2000:27-29 [Google Scholar]
- 70. Nattiv A, Loucks AB, Manore MM, Sanborn CF, Sundgot-Borgen J, Warren MP. American College of Sports Medicine position stand: the female athlete triad. Med Sci Sports Exerc. 2007;39(10):1867-1882 [DOI] [PubMed] [Google Scholar]
- 71. New SA, Robins SP, Campbell MK, et al. Dietary influences on bone mass and bone metabolism: further evidence of a positive link between fruit and vegetable consumption and bone health? Am J Clin Nutr. 2000;71(1):142-151 [DOI] [PubMed] [Google Scholar]
- 72. Nordin BE, Need AG, Morris HA, Horowitz M. The nature and significance of the relationship between urinary sodium and urinary calcium in women. J Nutr. 1993;123(9):1615-1622 [DOI] [PubMed] [Google Scholar]
- 73. North American Menopause Society The role of calcium in peri- and postmenopausal women: 2006 position statement of the North American Menopause Society. Menopause. 2006;3:862-877 [DOI] [PubMed] [Google Scholar]
- 74. Nutrition and Your Health: Dietary Guidelines for Americans. Washington, DC: US Department of Agriculture and US Department of Health and Human Services; 2000 [Google Scholar]
- 75. Ogur R, Uysal B, Ogur T, et al. Evaluation of the effect of cola drinks on bone mineral density and associated factors. Basic Clin Pharmacol Toxicol. 2007;100(5):334-338 [DOI] [PubMed] [Google Scholar]
- 76. Pershadsingh HA, McDonald JM. Direct addition of insulin inhibits a high affinity Ca2+-ATPase in isolated adipocyte plasma membranes. Nature, 1979;281(5731):495-497 [DOI] [PubMed] [Google Scholar]
- 77. Petrie HJ, Stover EA, Horswill CA. Nutritional concerns for the child and adolescent competitor. Nutrition. 2004;20(7-8):620-631 [DOI] [PubMed] [Google Scholar]
- 78. Ramalingam L, Messer LB, Reynolds EC. Adding casein phosphopeptide-amorphous calcium phosphate to sports drinks to eliminate in vitro erosion. Pediatr Dent. 2005;27(1):61-67 [PubMed] [Google Scholar]
- 79. Raschka L, Daniel H. Mechanisms underlying the effects of inulin-type fructans on calcium absorption in the large intestine of rats. Bone. 2005;37(5):728-735 [DOI] [PubMed] [Google Scholar]
- 80. Rizzoli R, Boonen S, Brandi ML, Burlet N, Delmas P, Reginster JY. The role of calcium and vitamin D in the management of osteoporosis. Bone. 2008;42(2):246-249 [DOI] [PubMed] [Google Scholar]
- 81. Roughead ZK, Hunt JR, Johnson LK, Badger TM, Lykken GI. Controlled substitution of soy protein for meat protein: effects on calcium retention, bone, and cardiovascular health indices in postmenopausal women. J Clin Endocrinol Metab. 2005;90(1):181-189 [DOI] [PubMed] [Google Scholar]
- 82. Rousseau JH, Kleppinger A, Kenny AM. Self-reported dietary intake of omega-3 fatty acids and association with bone and lower extremity function. J Am Geriatr Soc. 2008. August 22 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 83. Salem GJ, Zernicke RF, Barnard RJ. Diet-related changes in mechanical properties of rat vertebrae. Am J Physiol. 1992;262(2 Pt 2):R318-R321 [DOI] [PubMed] [Google Scholar]
- 84. Schurch MA, Rizzoli R, Slosman D, Vadas L, Vergnaud P, Bonjour JP. Protein supplements increase serum insulin-like growth factor-I levels and attenuate proximal femur bone loss in patients with recent hip fracture: a randomized, double-blind, placebo-controlled trial. Ann Intern Med. 1998;128(10):801-809 [DOI] [PubMed] [Google Scholar]
- 85. Shapses SA, Robins SP, Schwartz EI, Chowdhury H. Short-term changes in calcium but not protein intake alter the rate of bone resorption in healthy subjects as assessed by urinary pyridinium cross-link excretion. J Nutr. 1995;125(11):2814-2821 [DOI] [PubMed] [Google Scholar]
- 86. Shea B, Wells G, Cranney A, et al. Meta-analyses of therapies for postmenopausal osteoporosis, VII: meta-analysis of calcium supplementation for the prevention of postmenopausal osteoporosis. Endocr Rev. 2002;23(4):552-559 [DOI] [PubMed] [Google Scholar]
- 87. Sun D, Krishnan A, Zaman K, Lawrence R, Bhattacharya A, Fernandes G. Dietary n-3 fatty acids decrease osteoclastogenesis and loss of bone mass in ovariectomized mice. J Bone Miner Res. 2003;18(7):1206-1216 [DOI] [PubMed] [Google Scholar]
- 88. Tadayyon B, Lutwak L. Interrelationship of triglycerides with calcium, magnesium and phosphorus in the rat. J Nutr. 1969;97(2):246-254 [DOI] [PubMed] [Google Scholar]
- 89. Terada M, Inaba M, Yano Y, et al. Growth-inhibitory effect of a high glucose concentration on osteoblast-like cells. Bone. 1998;22:17-23 [DOI] [PubMed] [Google Scholar]
- 90. Thong FS, McLean C, Graham TE. Plasma leptin in female athletes: relationship with body fat, reproductive, nutritional, and endocrine factors. J Appl Physiol. 2000;88(6):2037-2044 [DOI] [PubMed] [Google Scholar]
- 91. Tjaderhane L, Larmas M. A high sucrose diet decreases the mechanical strength of bones in growing rats. J Nutr. 1998;128(10):1807-1810 [DOI] [PubMed] [Google Scholar]
- 92. Tsanzi E, Light HR, Tou JC. The effect of feeding different sugar-sweetened beverages to growing female Sprague-Dawley rats on bone mass and strength. Bone. 2008;42(5):960-968 [DOI] [PubMed] [Google Scholar]
- 93. Watkins BA, Li Y, Lippman HE, Feng S. Modulatory effect of omega-3 polyunsaturated fatty acids on osteoblast function and bone metabolism. Prostaglandins Leukot Essent Fatty Acids. 2003;68(6):387-398 [DOI] [PubMed] [Google Scholar]
- 94. Whiting SJ, Calvo MS. Dietary recommendations to meet both endocrine and autocrine needs of Vitamin D. J Steroid Biochem Mol Biol. 2005;97(1-2):7-12 [DOI] [PubMed] [Google Scholar]
- 95. Williams MH. Dietary supplements and sports performance: minerals. J Int Soc Sports Nutr. 2005;2:43-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Williams NI, Helmreich DL, Parfitt DB, Caston-Balderrama A, Cameron JL. Evidence for a causal role of low energy availability in the induction of menstrual cycle disturbances during strenuous exercise training. J Clin Endocrinol Metab. 2001;86(11):5184-5193 [DOI] [PubMed] [Google Scholar]
- 97. Willis KS, Peterson NJ, Larson-Meyer DE. Should we be concerned about the vitamin D status of athletes? Int J Sport Nutr Exerc Metab. 2008;18(2):204-224 [DOI] [PubMed] [Google Scholar]
- 98. Wolfe RR. The underappreciated role of muscle in health and disease. Am J Clin Nutr. 2006;84(3):475-482 [DOI] [PubMed] [Google Scholar]
- 99. Wood RJ, Allen LH. Evidence for insulin involvement in arginine- and glucose-induced hypercalciuria in the rat. J Nutr. 1983;113(8):1561-1567 [DOI] [PubMed] [Google Scholar]
- 100. Wyshak G. Teenaged girls, carbonated beverage consumption, and bone fractures. Arch Pediatr Adolesc Med. 2000;154(6):610-613 [DOI] [PubMed] [Google Scholar]
- 101. Wyshak G, Frisch RE. Carbonated beverages, dietary calcium, the dietary calcium/phosphorus ratio, and bone fractures in girls and boys. J Adolesc Health. 1994;15(3):210-215 [DOI] [PubMed] [Google Scholar]
- 102. Wyshak G, Frisch RE, Albright TE, Albright NL, Schiff I, Witschi J. Nonalcoholic carbonated beverage consumption and bone fractures among women former college athletes. J Orthop Res. 1989;7(1):91-99 [DOI] [PubMed] [Google Scholar]
- 103. Zemel MB. Calcium utilization: effect of varying level and source of dietary protein. Am J Clin Nutr. 1988;48(3 Suppl):880-883 [DOI] [PubMed] [Google Scholar]
- 104. Zernicke RF, Salem GJ, Barnard RJ, Schramm E. Long-term, high-fat-sucrose diet alters rat femoral neck and vertebral morphology, bone mineral content, and mechanical properties. Bone. 1995;16(1):25-31 [DOI] [PubMed] [Google Scholar]
- 105. Zernicke RF, Salem GJ, Barnard RJ, Woodward JS, Jr, Meduski JW, Meduski JD. Adaptations of immature trabecular bone to exercise and augmented dietary protein. Med Sci Sports Exerc. 1995;27(11):1486-1493 [PubMed] [Google Scholar]