Abstract
AIM: To present a critical discussion of the efficacy of the faecal pyruvate kinase isoenzyme type M2 (faecal M2-PK) test for colorectal cancer (CRC) screening based on the currently available studies.
METHODS: A literature search in PubMed and Embase was conducted using the following search terms: fecal Tumor M2-PK, faecal Tumour M2-PK, fecal M2-PK, faecal M2-PK, fecal pyruvate kinase, faecal pyruvate kinase, pyruvate kinase stool and M2-PK stool.
RESULTS: Stool samples from 704 patients with CRC and from 11 412 healthy subjects have been investigated for faecal M2-PK concentrations in seventeen independent studies. The mean faecal M2-PK sensitivity was 80.3%; the specificity was 95.2%. Four studies compared faecal M2-PK head-to-head with guaiac-based faecal occult blood test (gFOBT). Faecal M2-PK demonstrated a sensitivity of 81.1%, whereas the gFOBT detected only 36.9% of the CRCs. Eight independent studies investigated the sensitivity of faecal M2-PK for adenoma (n = 554), with the following sensitivities: adenoma < 1 cm in diameter: 25%; adenoma > 1 cm: 44%; adenoma of unspecified diameter: 51%. In a direct comparison with gFOBT of adenoma > 1 cm in diameter, 47% tested positive with the faecal M2-PK test, whereas the gFOBT detected only 27%.
CONCLUSION: We recommend faecal M2-PK as a routine test for CRC screening. Faecal M2-PK closes a gap in clinical practice because it detects bleeding and non-bleeding tumors and adenoma with high sensitivity and specificity.
Keywords: Faecal pyruvate kinase isoenzyme type M2, Colorectal cancer screening, Colorectal cancer, Stool, Faecal occult blood, Adenoma, Polyps
INTRODUCTION
Colorectal cancer (CRC) is the most frequent malignant disease in Europe according to an estimation of cancer incidence and mortality by the International Agency for Research on Cancer in Lyon, France[1]. In 2008, 436 000 persons were diagnosed with CRC, followed by breast cancer with 421 000 cases, lung cancer with 391 000 cases and prostate cancer with 382 000 cases. Approximately 212 000 patients died due to CRC that year, which makes it the second most common death from cancer (after lung cancer with approximately 342 000 deaths in 2008)[1]. Worldwide, in the developed countries about 1.167 million new cases of CRC and about 603 000 deaths due to CRC were estimated for 2007[2].
However, due to the long process of carcinogenesis in CRC (adenoma-carcinoma sequence), CRC has an overall good prognosis when diagnosed at an early stage. For that reason different CRC screening programs have been developed and are offered in various European countries.
The gold standard for early detection of colorectal neoplasia is colonoscopy. A great advantage of colonoscopy is that adenomas, the potential precursors of carcinogenesis, can be simultaneously detected and removed. However, the acceptance of screening colonoscopy among patients is low. For example, in Germany only 2.7% of insured people exercise their right to a colonoscopy even though it is reimbursed for people over 55 years old[3]. The most common in-vitro diagnostic method for CRC screening is the detection of occult blood in the stool using the guaiac-based faecal occult blood test (gFOBT). This test is based on the peroxidase activity of haemoglobin, which induces an oxidation and blue colouration of guaiac in the presence of hydrogen peroxide. Red meat and a number of vegetables may result in false positive results whereas vitamin C may result in false negative staining. Therefore, dietary restriction is recommended for three days prior to and during testing. A widespread criticism of gFOBT is its low sensitivity for adenomas and carcinomas (13%-50%)[4-8]. The immunological faecal occult blood tests (iFOBTs) specifically quantify human haemoglobin with antibodies. Comparative evaluations of immunochemical faecal occult blood tests from different manufacturers have revealed great variations in their respective sensitivities for colorectal adenoma detection[9,10].
The faecal pyruvate kinase isoenzyme type M2 (faecal M2-PK) test recognises a key enzyme controlling the metabolism of cells with a high proliferation rate, such as tumour cells, and thereby detects specific alterations in intestinal cells, such as polyps and CRC, as well as high-risk patients with acute or chronic inflammatory bowel diseases (IBD) (i.e., ulcerative colitis, Crohn’s disease).
M2-PK is a special isoenzyme of pyruvate kinase, a key enzyme within glycolysis which catalyzes the ATP-producing conversion of phosphoenolpyruvate (PEP) to pyruvate. Depending upon the metabolic functions of the tissues, different isoenzymes of pyruvate kinase are expressed. During tumour formation the tissue-specific isoenzymes disappear and the pyruvate kinase isoenzyme type M2 is expressed[11]. In contrast to all other pyruvate kinase isoenzymes (type L, M1 and R) which consist of four subunits, the M2 pyruvate kinase isoenzyme may occur in a highly active tetrameric form as well as in a dimeric form with low activity. The dimeric form is nearly inactive and favours the channelling of glucose carbons into synthetic processes, such as nucleic acid, amino acid and fatty acid synthesis. The tetrameric form is highly active and favours the energy-regenerating conversion of PEP to pyruvate and lactate (the Warburg effect). In tumour cells, M2-PK is mainly found to be in the dimeric form and has therefore been termed “Tumour M2-PK”. The dimerisation of M2-PK is induced by interaction with different oncoproteins, including pp60v-src-kinase, oncogenic fibroblast growth factor1 and human papilloma virus 16 E7[11].
The dimeric form of M2-PK is released from tumours into the blood and can be quantified by a sandwich enzyme-linked immunosorbent assay (ELISA; ScheBo Biotech AG, Giessen, Germany). About 40 studies have been published on M2-PK concentrations in blood since 1997. These demonstrate a significant increase in M2-PK and correlation with staging for the following tumours: melanoma, thyroid, breast, lung, kidney, oesophageal, gastric, pancreatic, colorectal, ovarian, cervical and renal cell cancer[12-19]. The long-term determination of M2-PK in EDTA-plasma is used as a tool for follow-up studies to monitor failure, relapse or success during therapy. In CRC and adenoma M2-PK is also released into the patients’ faeces. A sandwich ELISA and a lateral flow rapid test (for doctor’s office, point-of-care and laboratory use), both based upon two monoclonal antibodies which specifically recognise the dimeric form of M2-PK, are commercially available for the quantification of M2-PK in stool. The potential of the faecal M2-PK test for CRC screening has been evaluated in at least 17 different independent international studies. The objectives of this review were to obtain an overview of the currently available studies with faecal M2-PK and to present a critical discussion of the efficacy of the faecal M2-PK test for CRC screening.
MATERIALS AND METHODS
Search procedure for studies
In order to find the most relevant studies about faecal M2-PK and CRC screening, a literature search in PubMed and Embase was conducted using the following search terms: fecal tumor M2-PK, faecal tumour M2-PK, fecal M2-PK, faecal M2-PK, fecal pyruvate kinase, faecal pyruvate kinase, pyruvate kinase stool, M2-PK stool. In June 2011 this search revealed 34 publications dealing with faecal M2-PK[7,8,10,18,20-49] (Table 1). The ScheBo faecal M2-PK test was used in 33 publications, whereas one publication used another antibody combination and was therefore excluded. The following were also omitted from the meta-analysis: seven publications which summarized results from previous papers as reviews; three author-replies to questions about an existing published paper; one publication written in Bulgarian; two publications which investigated neither sensitivity nor specificity; seven publications that only referred to IBD (which was outside the scope of our review) (Table 1). The remaining 13 publications were included in the meta-analysis[7,8,10,30,31,33,35,37,41,44-46,49]. In addition, three posters from conferences[50-52] and a German doctoral thesis[53] known to the authors have been added to the list of relevant studies (Table 1). Hence, 17 published studies in total have been incorporated into the meta-analysis (Tables 1 and 2). For our meta-analysis the sensitivities for CRC and adenoma, positivity rates, as well as the specificities published within the individual papers were summarized in individual tables, together with the number of cases which underlie the calculated sensitivities and specificities. mean ± SD was calculated for the sensitivities and specificities of the combined data from the different studies using the Statistics package of SigmaPlot Version 11.0. The sensitivities for CRC and adenoma in all studies are based upon colonoscopy results. Calculated specificities are either based on colonoscopy results or are authors’ estimates derived from published prevalence data of CRC and adenoma in screening populations. In the absence of colonoscopies or estimated specificities, only the percentages of test-negative individuals were included in the tables.
Table 1.
Results of the literature search
| Results | Reference |
| All papers dealing with faecal M2-PK found in a literature search of Pubmed and Embase | [7, 8, 10,18, 20-49] |
| Additional published studies known to the authors | [50-53] |
| Excluded papers - reasons for exclusion | |
| Unique combination of antibodies | [47] |
| Reviews | [18, 24, 26, 28, 34, 38, 42] |
| Author replies or comments | [27, 32, 40] |
| Paper in Bulgarian language | [29] |
| No sensitivities or specificities calculated | [21, 48] |
| Studies referred to IBD | [20, 22, 23, 25, 36, 39, 43] |
| Included papers | |
| Studies found in Pubmed and Embase | [7, 8, 10, 30, 31, 33, 35, 37, 41, 44-46, 49] |
| Published studies known to the authors | [50-53] |
IBD: Inflammatory bowel diseases; faecal M2-PK: Faecal pyruvate kinase isoenzyme type M2
Table 2.
Overview of included studies
| Reference | Country of study | Conflict of interest regarding faecal M2-PK |
| Shastri et al[7], 2006 | Germany | None declared |
| Koss et al[8], 2008 | United Kingdom | None declared |
| Möslein et al[10], 2010 | Germany | None declared |
| Haug et al[30], 2008 | Germany | None declared |
| Shastri et al[31], 2008 | Germany | Coauthor Stein: Conference speaker for ScheBo Biotech AG |
| Haug et al[33], 2007 | Germany | None declared |
| Mulder et al[35], 2007 | The Netherlands | None declared |
| Ewald et al[37], 2007 | Germany | None declared |
| Tonus et al[41], 2006 | Germany | Non declared |
| Vogel et al[44], 2005 | Germany | Tests performed by ScheBo Biotech AG |
| Naumann et al[45], 2004 | Germany | None declared |
| Hardt et al[46], 2004 | Germany | None declared |
| Tonus et al[49], 2009 | Germany | None declared |
| Kloer et al[50], 2005 | Germany | None declared |
| McLoughlin et al[51], 2005 | Ireland | None declared |
| Bellutti et al[52], 2005 | Germany | None declared |
| Schmidt et al[53], 2009 | Germany | None declared |
Faecal M2-PK: Faecal pyruvate kinase isoenzyme type M2.
Faecal M2-PK test
In all seventeen studies included in our meta-analysis, the M2-PK stool test from ScheBo Biotech AG in Giessen, Germany was used. This test is a sandwich ELISA based on two monoclonal antibodies which specifically recognise the dimeric form of M2-PK.
In accordance with the manufacturer’s protocol all studies included a cut-off value of 4 U/mL. One study also included a lower cut-off value (3.33 U/mL[8]) and another also incorporated additional higher cut off values (5 U/mL and 6 U/mL[45]) to calculate the resultant sensitivities and specificities. To ensure comparability only those results obtained with the cut-off value of 4 U/mL are included in the meta-analysis.
RESULTS
Sensitivity of faecal M2-PK for colorectal carcinoma
Sensitivity of the faecal M2-PK test for CRC was investigated and calculated in twelve independent studies (Table 3 and Figure 1), which found sensitivities of faecal M2-PK for detection of CRC between 68% and 97%. The mean sensitivity of all twelve studies is 80.3% ± 7.1%. These twelve studies measured faecal M2-PK concentrations in a total of 704 stool samples of patients with CRC, whereby 559 tested positive. Five studies considered the tumor node metastases and/or Dukes classification and showed a close correlation between the sensitivity of the faecal M2-PK test and staging (Table 4). The mean sensitivities ranged from 59% for T1 to 90% for T4 and from 60% for Dukes A to 91% for Dukes D. gFOBT studies from various countries showed much lower sensitivities for CRC which ranged between 13% and 50%[4-6]. The higher sensitivity of faecal M2-PK compared to gFOBT was confirmed in four studies which measured faecal M2-PK and gFOBT head-to-head in the same patients (Table 5). Combining all four studies, 155 samples from patients with CRC were tested for faecal M2-PK and gFOBT. M2-PK correctly detected 81.1% whereas the gFOBT detected only 36.9%.
Table 3.
Published sensitivities of the faecal pyruvate kinase isoenzyme type M2 test for colorectal cancer
| Reference | n (%) |
| Hardt et al[46], 2004 | 60 (73) |
| Naumann et al[45], 2004 | 27 (85.2) |
| Kloer et al[50], 2005 | 147 (79.6) |
| McLoughlin et al[51], 2005 | 35 (97) |
| Vogel et al[44], 2005 | 22 (77) |
| Shastri et al[7], 2006 | 74 (81.1) |
| Tonus et al[41], 2006 | 54 (78) |
| Haug et al[33], 2007 | 65 (68) |
| Mulder et al[35], 2007 | 52 (85) |
| Koss et al[8], 2008 | 32 (81) |
| Shastri et al[31], 2008 | 55 (78.2) |
| Schmidt et al[53], 2009 | 81 (80.3) |
| Sum | 704 |
| mean ± SD | 80.3 ± 7.1 |
n: Number of colorectal cancer samples; %: Sensitivity.
Figure 1.
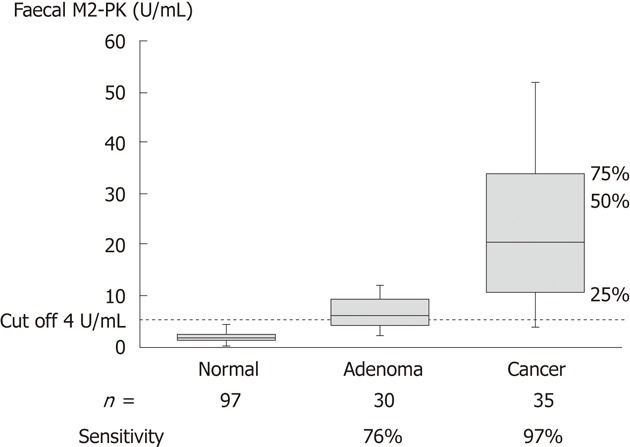
Faecal pyruvate kinase isoenzyme type M2 in healthy controls, patients with colorectal adenoma and colorectal cancer[51]. Faecal M2-PK: Faecal pyruvate kinase isoenzyme type M2.
Table 4.
Correlation of faecal pyruvate kinase isoenzyme type M2 sensitivity with tumor node metastasis and Dukes classification n (%)
| Reference |
Tumor node metastasis classificatoin |
Dukes classification |
||||||
| T1 | T2 | T3 | T4 | Dukes A | Dukes B | Dukes C | Dukes D | |
| Kloer et al[50], 2005 | 9 (55.5) | 18 (61.1) | 49 (81.6) | 12 (83.3) | 23 (52.2) | 24 (76.0) | 26 (80.8) | 17 (82.4) |
| Tonus et al[41], 2006 | 5 (60) | 11 (64) | 25 (89) | 4 (100) | 5 (60.0) | 17 (76.0) | 9 (89) | 10 (90.0) |
| Haug et al[33], 2007 | 6 (67) | 16 (44) | 34 (71) | 4 (100) | 12 (67.0) | 18 (61.0) | 12 (67.0) | 6 (100.0) |
| Schmidt et al[53], 2009 | 8 (57) | 20 (84) | 42 (79) | 11 (91) | ||||
| Hardt et al[46], 2004 | 7 (57) | 11 (64) | 33 (78) | 9 (78) | ||||
| Sum | 35 | 76 | 183 | 40 | 40 | 59 | 47 | 33 |
| mean ± SD | 59 ± 5 | 63 ± 14 | 80 ± 7 | 90 ± 10 | 60 ± 7 | 71 ± 9 | 79 ± 11 | 91 ± 9 |
n: Number of samples tested; %: Sensitivity.
Table 5.
Head-to-head comparison of the sensitivity for colorectal cancer of faecal pyruvate kinase isoenzyme type M2 and guaiac-based faecal occult blood test n (%)
| Reference | CRC M2-PK | CRC gFOBT |
| Naumann et al[45], 2004 | 27 (85.2) | 27 (62.9) |
| Vogel et al[44], 2005 | 22 (77) | 22 (27) |
| Shastri et al[7], 2006 | 74 (81.1) | 74 (36.5) |
| Koss et al[8], 2008 | 32 (81) | 32 (21) |
| Sum | 155 | 155 |
| mean ± SD | 81.1 ± 3.3 | 36.9 ± 18.5 |
n: Number of samples tested; %: Sensitivity; CRC: Colorectal cancer; gFOBT: Guaiac-based faecal occult blood test; M2-PK: Pyruvate kinase isoenzyme type M2.
Sensitivity of faecal M2-PK for adenoma
More than 90% of colorectal carcinomas evolve from adenoma via the adenoma-carcinoma sequence within 10 to 15 years. Therefore, the early detection and removal of adenoma is an important aspect in the prevention of CRC. The sensitivity of faecal M2-PK for adenoma was investigated in eight studies and ranged between 20% and 76%, whereby a clear dependency with the diameter of the adenoma is described (Table 6). In total, 339 adenomas with a diameter < 1 cm and 117 adenomas with a diameter > 1 cm were investigated. Twenty-five percent of the adenomas < 1 cm in diameter tested positive with the faecal M2-PK test and 44% of the adenomas > 1 cm were correctly detected. Three studies included a total of 98 stool samples from patients with adenoma of unclassified diameter. Faecal M2-PK concentrations above the cut-off were found in 51% of the samples. In direct comparisons of faecal M2-PK with gFOBT, 25% of patients with polyps < 1 cm tested positive with the M2-PK test whereas only 9% were identified by the gFOBT (Table 7). Fourty-seven percent of adenomas > 1 cm in diameter tested positive with the M2-PK test whereas the gFOBT detected only 27% (Table 7). One study with adenomas of unclassified diameter revealed a sensitivity of 48% for M2-PK in comparison to 9% for gFOBT. Möslein et al[10] combined adenomas > 1 cm in diameter and CRC to form a group with 55 cases of “advanced neoplasia”. The resultant sensitivity of faecal M2-PK for advanced neoplasia was 27.3% whereas the sensitivity of gFOBT was only 9.1%. This study also included a head-to-head comparison of four iFOBTs from different manufacturers using the same 55 samples of patients with advanced neoplasia. With sensitivities of 7.3%, 8.5%, 18.9% and 20%, respectively, all four iFOBTs were less sensitive than faecal M2-PK.
Table 6.
Sensitivity of faecal pyruvate kinase isoenzyme type M2 for adenoma n (%)
| Reference | Adenoma without diameter | Adenoma < 1 cm ø | Adenoma > 1 cm ø |
| Naumann et al[45], 2004 | 11 (27.3) | 13 (61.5) | |
| McLoughlin et al[51], 2005 | 30 (76) | ||
| Vogel et al[44], 2005 | 21 (48) | ||
| Shastri et al[7], 2006 | 21 (28.6) | 10 (20.0) | |
| Mulder et al[35], 2007 | 47 (28) | ||
| Koss et al[8], 2008 | 5 (20) | 5 (60) | |
| Shastri et al[31], 2008 | 48 (29.2) | 21 (57.1) | |
| Haug et al[30], 2008 | 254 (22.1) | 68 (23.5) | |
| Sum | 98 | 339 | 117 |
| mean ± SD | 51 ± 24 | 25 ± 4 | 44 ± 21 |
n: Number of samples tested; %: Sensitivity;ø: Diameter.
Table 7.
Head-to-head comparison of sensitivity for adenoma of faecal pyruvate kinase isoenzyme type M2 and guaiac-based faecal occult blood test n (%)
| Reference | Adenoma < 1 cm ø M2-PK | Adenoma < 1 cm ø gFOBT | Adenoma > 1 cm ø M2-PK | Adenoma > 1 cm ø gFOBT | Adenoma w/o ø M2-PK | Adenoma w/o ø gFOBT |
| Naumann et al[45], 2004 | 11 (27.3) | 11 (18.2) | 13 (61.5) | 13 (30.8) | ||
| Vogel et al[44], 2005 | 21 (48) | 21 (9) | ||||
| Shastri et al[7], 2006 | 21 (28.6) | 21 (9.5) | 10 (20.0) | 10 (30.0) | ||
| Koss et al[8], 2008 | 5 (20.0) | 5 (0.0) | 5 (60.0) | 5 (20.0) | ||
| Sum | 37 | 37 | 28 | 28 | 21 | 21 |
| mean ± SD | 25 ± 5 | 9 ± 9 | 47 ± 24 | 27 ± 6 |
n: Number of samples tested; %: Sensitivity; w/o ø: Without measurement of diameter; ø: Diameter; gFOBT: Guaiac-based faecal occult blood test; M2-PK: Pyruvate kinase isoenzyme type M2.
Specificity of faecal M2-PK for colorectal carcinoma
The specificity of an in-vitro diagnostic test reflects the proportion of correctly identified negatives. Consequently, the composition of the control group has a profound effect on the specificity. By its very definition, screening is used in a population to detect a disease in individuals without signs or symptoms of that disease. Therefore, symptoms in the gastrointestinal tract, such as pain, visible blood in the stool or known inflammation are not appropriate for inclusion into the control group of a CRC screening study. In total, seventeen publications calculated specificities for the M2-PK stool test. Nine of these studies included patients from hospitals (clinical settings instead of screening settings) with positive gFOBTs and with inflammation and/or other symptoms in the gastrointestinal tract into the control group and hence these studies have been discounted from our evaluation of the specificity of faecal M2-PK[7,30,31,35,44-46,50,53]. Eight studies, comprising 11 412 samples in total, had control groups which conformed to the correct composition for screening studies (Table 8, Figures 2 and 3). Ninty one point five percent tested negative which means that about 9% of those tested had a faecal M2-PK value above the cut-off value of 4 U/mL. Colonoscopies were performed in four studies[8,10,51,41] (Table 8) and revealed specificities of 98% (n = 97), 93% (n = 42), 100% (n = 13) and 89.5% (n = 796). In study 49 with 4854 participants, the authors calculated an estimated specificity of 93.4% based on a prevalence of CRC of 2%. Based on a prevalence of 0.5% for CRC and 18% for advanced adenoma, the authors of study 52 with 2787 participants calculated an estimated specificity for colorectal neoplasia of 97.4%. The screening in study 49 with 4854 participants describes a continuous increase in the percentage of faecal M2-PK positive volunteers with age from 30 years old upwards (Figure 3).
Table 8.
Measurements of faecal pyruvate kinase isoenzyme type M2 in stool samples of healthy individuals
| Reference | No. of healthy participants | Test-negative participants (%) | Colonoscopy (yes/no) | Specificity (%) |
| Belluti et al[52], 2005 | 2787 | 91.6 | No | 97.4 (e) |
| McLoughlin et al[51], 2005 | 97 | 98 | Yes | 98 |
| Tonus et al[41], 2006 | 42 | 93 | Yes | 93 |
| Ewald et al[37], 2007 | 1906 | 90.4 | No | |
| Haug et al[33], 2007 | 917 | 78.6 | No | |
| Koss et al[8], 2008 | 13 | 100.0 | Yes | 100.0 |
| Tonus et al[49], 2009 | 4854 | 91.2 | No | 93.4 (e) |
| Möslein et al[10], 2010 | 796 | 89.5 | Yes | 89.5 |
| Sum | 11 412 | |||
| mean ± SD | 91.5 ± 6.4 | 95.2 ± 3.9 |
e: Estimated specificities calculated by authors based on the sensitivity of faecal pyruvate kinase isoenzyme type M2 for colorectal cancer (CRC) and advanced neoplasia, and the prevalence of CRC and advanced adenoma.
Figure 2.
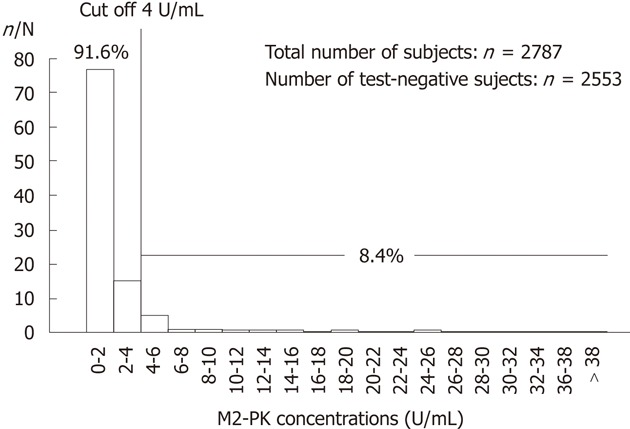
Distribution of faecal pyruvate kinase isoenzyme type M2 concentrations in a screening collective of 2787 participants aged from 45 to 65 years[52]. n: Number of test negative; N: Total number of subjects; M2-PK: Pyruvate kinase isoenzyme type M2.
Figure 3.
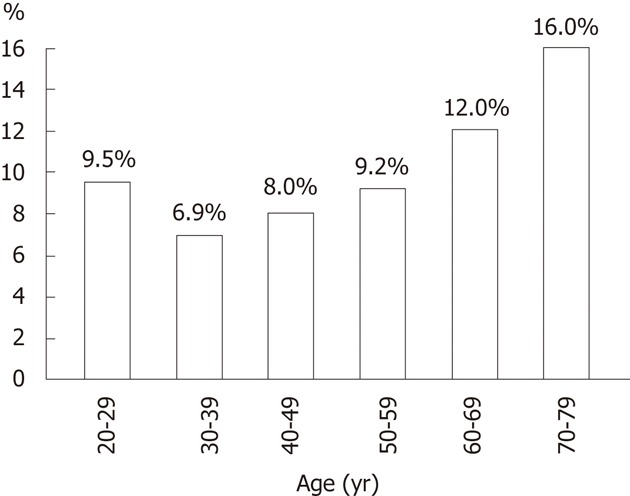
Percentage of faecal pyruvate kinase isoenzyme type M2-positive volunteers by age group (from Tonus et al[49]).
DISCUSSION
With a sensitivity of about 80% for CRC and 44% for adenoma > 1 cm, faecal M2-PK outclasses the gFOBT which has sensitivity between 13% and 50% for CRC (Tables 3-7, and literature[4-6]). The superiority of faecal M2-PK may be due to the fact that M2-PK is a metabolic biomarker which is characteristic for the metabolic state of tumour cells and their precursors, whereas detection of bowel cancer using the gFOBT is restricted to bleeding tumours and adenoma. Therefore, faecal M2-PK has the advantage that it detects both bleeding as well as non-bleeding tumours and adenoma and will close a gap in clinical practice. Conversely, faecal M2-PK does not have false positive results due to various non-cancerous sources of bleeding, e.g., haemorrhoids and fissures. Screening studies involving a total of more than 11 000 healthy subjects have demonstrated a mean specificity of 95.2% for the detection of CRC/advanced neoplasia with faecal M2-PK. The specificities were 100%, 98%, 93% and 89.5%, respectively, in studies which incorporated colonoscopies; 97.4% and 93.4% in studies with estimated specificities; and 90.4% and 78.6 % in studies without colonoscopies (Table 8). This demonstrates that specificities were higher in studies with confirmatory colonoscopies in comparison to studies without colonoscopies. Whilst gFOBT specificities ≥ 94% are reported in the literature[5,6], the authors of a meta-analysis of over 440 000 subjects from six independent studies concluded that more than 80% of the positive gFOBT results are actually false positives[54]. In most studies the calculated specificities are based on the results of colonoscopy. Colonoscopy is the gold standard for early detection of CRC and polyps and has the advantage that polyps, the potential precursors of carcinogenesis, can be simultaneously detected and removed. However, recent studies have revealed that colonoscopies may have false negative results, e.g., due to suboptimal bowel preparation. For example, a systematic review which summarized six studies totaling 465 patients who had undergone two colonoscopies on the same day revealed a pooled miss rate of 22% for polyps of any size[55].
IBD may also be a cause of increased faecal M2-PK levels and hence detection of previously undiagnosed patients by faecal M2-PK is another advantage of the test, whereas those patients with known IBD are subject to their own endoscopic monitoring program and are not categorized as suitable for inclusion in a non-invasive CRC screening program.
The cost of one faecal M2-PK ELISA test is about 15-25 US$. In comparison, based on 2004 data from privately insured beneficiaries, costs were estimated to be about 557 US$ (range: 150-1112 US$) for a colonoscopy, 174 US$ (range: 54-392 US$) for a flexible sigmoidoscopy and 7 US$ (range: 2-16 US$) for a guaiac faecal occult blood test[56].
In conclusion, faecal M2-PK, either as an ELISA or as a lateral flow rapid test, is a cost-effective and easy-to-perform routine test. In contrast to the gFOBT, only one small stool sample (from a single stool passage), which may be collected with a convenient stool sample device, is necessary and no dietary restrictions are needed. Faecal M2-PK is an appropriately sensitive tool to pre-select those patients who require colonoscopy for further diagnostic confirmation or exclusion of CRC. Based on the current data we recommend the use of faecal M2-PK as a routine in-vitro diagnostic test for CRC screening.
COMMENTS
Background
Colorectal cancer (CRC) is the most frequent malignant disease worldwide. The gold standard for early detection of colorectal neoplasia is colonoscopy. However, the acceptance of screening colonoscopy by potential screenees is low. Faecal pyruvate kinase isoenzyme type M2 (faecal M2-PK) is an in-vitro diagnostic test which recognizes a specific metabolic characteristic of proliferating cells in 4 mg stool samples. The simplicity of sample collection can encourage participation in CRC screening programs.
Research frontiers
The sensitivity and specificity of faecal M2-PK for CRC screening has been investigated in numerous publications. Here the paper presents a critical discussion of the efficacy of faecal M2-PK for CRC screening based on the accumulated data from currently available studies.
Innovations and breakthroughs
The most established in-vitro diagnostic test for CRC screening is the guaiac-based faecal occult blood test (gFOBT). In contrast to the FOBTs, faecal M2-PK detects bleeding and non-bleeding tumors. With a sensitivity of about 80% for CRC and 44% for adenoma > 1 cm, faecal M2-PK outclasses the gFOBT which has a sensitivity between 13% and 50% for CRC.
Applications
This meta-analysis summarizes the results of 17 published studies evaluating the faecal M2-PK test for CRC screening. The data will help to critically assess the efficiency of the faecal M2-PK test in comparison to other in-vitro diagnostic tests for CRC screening.
Peer review
This is a meta-analysis about screening CRC with fecal MK-pyruvate kinase.
Footnotes
Peer reviewers: Dr. Cuneyt Kayaalp, MD, Professor, Department of General Surgery, Staff Surgeon of Gastrointestinal Surgery, Turgut Ozal Medical Center, Inonu University, Malatya 44315, Turkey; Dr. Jose Perea, Department of Surgery, 12 De Octubre University Hospital, Rosas De Aravaca, 82A, 28023 Madrid, Spain
S- Editor Cheng JX L- Editor Logan S E- Editor Xiong L
.
References
- 1.Ferlay J, Parkin DM, Steliarova-Foucher E. Estimates of cancer incidence and mortality in Europe in 2008. Eur J Cancer. 2010;46:765–781. doi: 10.1016/j.ejca.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 2.Garcia M, Jemal A, Ward EM, Center MM, Hao Y, Siegel RL, Thun MJ. Global cancer facts and figures 2007. Atlanta, GA: American Cancer Society; 2007. [Google Scholar]
- 3.Altenhof L. Wissenschaftliche Begleitung der Früherkennungs-Koloskopie 6. Jahresberich. 2008 Available from: http://www.berliner-gastroenterologen.de/uploads/media/6.Jahresbericht_ZI_01.pdf. [Google Scholar]
- 4.Allison JE, Tekawa IS, Ransom LJ, Adrain AL. A comparison of fecal occult-blood tests for colorectal-cancer screening. N Engl J Med. 1996;334:155–159. doi: 10.1056/NEJM199601183340304. [DOI] [PubMed] [Google Scholar]
- 5.Imperiale TF, Ransohoff DF, Itzkowitz SH, Turnbull BA, Ross ME. Fecal DNA versus fecal occult blood for colorectal-cancer screening in an average-risk population. N Engl J Med. 2004;351:2704–2714. doi: 10.1056/NEJMoa033403. [DOI] [PubMed] [Google Scholar]
- 6.Lieberman DA, Weiss DG. One-time screening for colorectal cancer with combined fecal occult-blood testing and examination of the distal colon. N Engl J Med. 2001;345:555–560. doi: 10.1056/NEJMoa010328. [DOI] [PubMed] [Google Scholar]
- 7.Shastri YM, Naumann M, Oremek GM, Hanisch E, Rösch W, Mössner J, Caspary WF, Stein JM. Prospective multicenter evaluation of fecal tumor pyruvate kinase type M2 (M2-PK) as a screening biomarker for colorectal neoplasia. Int J Cancer. 2006;119:2651–2656. doi: 10.1002/ijc.22243. [DOI] [PubMed] [Google Scholar]
- 8.Koss K, Maxton D, Jankowski JA. Faecal dimeric M2 pyruvate kinase in colorectal cancer and polyps correlates with tumour staging and surgical intervention. Colorectal Dis. 2008;10:244–248. doi: 10.1111/j.1463-1318.2007.01334.x. [DOI] [PubMed] [Google Scholar]
- 9.Hundt S, Haug U, Brenner H. Comparative evaluation of immunochemical fecal occult blood tests for colorectal adenoma detection. Ann Intern Med. 2009;150:162–169. doi: 10.7326/0003-4819-150-3-200902030-00005. [DOI] [PubMed] [Google Scholar]
- 10.Möslein G, Schneider C, Theilmeier A, Erckenbrecht H, Normann S, Hoffmann B, Tilmann-Schmidt D, Horstmann O, Graeven U, Poremba C. [Analysis of the statistical value of various commercially available stool tests - a comparison of one stool sample in correlation to colonoscopy] Dtsch Med Wochenschr. 2010;135:557–562. doi: 10.1055/s-0030-1247866. [DOI] [PubMed] [Google Scholar]
- 11.Mazurek S. Pyruvate kinase type M2: a key regulator of the metabolic budget system in tumor cells. Int J Biochem Cell Biol. 2011;43:969–980. doi: 10.1016/j.biocel.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 12.Wechsel HW, Petri E, Bichler KH, Feil G. Marker for renal cell carcinoma (RCC): the dimeric form of pyruvate kinase type M2 (Tu M2-PK) Anticancer Res. 1999;19:2583–2590. [PubMed] [Google Scholar]
- 13.Lüftner D, Mesterharm J, Akrivakis C, Geppert R, Petrides PE, Wernecke KD, Possinger K. Tumor type M2 pyruvate kinase expression in advanced breast cancer. Anticancer Res. 2000;20:5077–5082. [PubMed] [Google Scholar]
- 14.Schneider J, Morr H, Velcovsky HG, Weisse G, Eigenbrodt E. Quantitative detection of tumor M2-pyruvate kinase in plasma of patients with lung cancer in comparison to other lung diseases. Cancer Detect Prev. 2000;24:531–535. [PubMed] [Google Scholar]
- 15.Kaura B, Bagga R, Patel FD. Evaluation of the Pyruvate Kinase isoenzyme tumor (Tu M2-PK) as a tumor marker for cervical carcinoma. J Obstet Gynaecol Res. 2004;30:193–196. doi: 10.1111/j.1447-0756.2004.00187.x. [DOI] [PubMed] [Google Scholar]
- 16.Ugurel S, Bell N, Sucker A, Zimpfer A, Rittgen W, Schadendorf D. Tumor type M2 pyruvate kinase (TuM2-PK) as a novel plasma tumor marker in melanoma. Int J Cancer. 2005;117:825–830. doi: 10.1002/ijc.21073. [DOI] [PubMed] [Google Scholar]
- 17.Ahmed AS, Dew T, Lawton FG, Papadopoulos AJ, Devaja O, Raju KS, Sherwood RA. M2-PK as a novel marker in ovarian cancer. A prospective cohort study. Eur J Gynaecol Oncol. 2007;28:83–88. [PubMed] [Google Scholar]
- 18.Kumar Y, Tapuria N, Kirmani N, Davidson BR. Tumour M2-pyruvate kinase: a gastrointestinal cancer marker. Eur J Gastroenterol Hepatol. 2007;19:265–276. doi: 10.1097/MEG.0b013e3280102f78. [DOI] [PubMed] [Google Scholar]
- 19.Nisman B, Yutkin V, Nechushtan H, Gofrit ON, Peretz T, Gronowitz S, Pode D. Circulating tumor M2 pyruvate kinase and thymidine kinase 1 are potential predictors for disease recurrence in renal cell carcinoma after nephrectomy. Urology. 2010;76:513.e1–513.e6. doi: 10.1016/j.urology.2010.04.034. [DOI] [PubMed] [Google Scholar]
- 20.Turner D, Leach ST, Mack D, Uusoue K, McLernon R, Hyams J, Leleiko N, Walters TD, Crandall W, Markowitz J, et al. Faecal calprotectin, lactoferrin, M2-pyruvate kinase and S100A12 in severe ulcerative colitis: a prospective multicentre comparison of predicting outcomes and monitoring response. Gut. 2010;59:1207–1212. doi: 10.1136/gut.2010.211755. [DOI] [PubMed] [Google Scholar]
- 21.Joshi S, Lewis SJ, Creanor S, Ayling RM. Age-related faecal calprotectin, lactoferrin and tumour M2-PK concentrations in healthy volunteers. Ann Clin Biochem. 2010;47:259–263. doi: 10.1258/acb.2009.009061. [DOI] [PubMed] [Google Scholar]
- 22.Jeffery J, Lewis SJ, Ayling RM. Fecal dimeric M2-pyruvate kinase (tumor M2-PK) in the differential diagnosis of functional and organic bowel disorders. Inflamm Bowel Dis. 2009;15:1630–1634. doi: 10.1002/ibd.20946. [DOI] [PubMed] [Google Scholar]
- 23.Johnson MW, Maestranzi S, Duffy AM, Dewar DH, Ciclitira PJ, Sherwood RA, Nicholls JR. Faecal M2-pyruvate kinase: a novel, noninvasive marker of ileal pouch inflammation. Eur J Gastroenterol Hepatol. 2009;21:544–550. doi: 10.1097/MEG.0b013e3283040cb3. [DOI] [PubMed] [Google Scholar]
- 24.Loitsch SM, Shastri Y, Stein J. Stool test for colorectal cancer screening--it’s time to move! Clin Lab. 2008;54:473–484. [PubMed] [Google Scholar]
- 25.Shastri YM, Povse N, Schröder O, Stein J. Comparison of a novel fecal marker--fecal tumor pyruvate kinase type M2 (M2-PK) with fecal calprotectin in patients with inflammatory bowel disease: a prospective study. Clin Lab. 2008;54:389–390. [PubMed] [Google Scholar]
- 26.Vogt W. [Prevention of colon cancer--update 2008] Praxis (Bern 1994) 2008;97:1077–1083. doi: 10.1024/1661-8157.97.20.1077. [DOI] [PubMed] [Google Scholar]
- 27.Shastri YM, Stein JM. Faecal tumour pyruvate kinase M2: not a good marker for the detection of colorectal adenomas. Br J Cancer. 2008;99:1366; author reply 1367. doi: 10.1038/sj.bjc.6604656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hardt PD, Ewald N. Tumor M2 pyruvate kinase: a tumor marker and its clinical application in gastrointestinal malignancy. Expert Rev Mol Diagn. 2008;8:579–585. doi: 10.1586/14737159.8.5.579. [DOI] [PubMed] [Google Scholar]
- 29.Ivanova A, Iarŭmov N, Toshev S, Adzharov D, Krŭstev Z, Angelov K, Sokolov M, Gribnev P. [Pilot study on M2-PK-- a new non-invasive parameter for early diagnosis of colorectal carcinoma] Khirurgiia (Sofiia) 2007:6: 5–7. [PubMed] [Google Scholar]
- 30.Haug U, Hundt S, Brenner H. Sensitivity and specificity of faecal tumour M2 pyruvate kinase for detection of colorectal adenomas in a large screening study. Br J Cancer. 2008;99:133–135. doi: 10.1038/sj.bjc.6604427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shastri YM, Loitsch S, Hoepffner N, Povse N, Hanisch E, Rösch W, Mössner J, Stein JM. Comparison of an established simple office-based immunological FOBT with fecal tumor pyruvate kinase type M2 (M2-PK) for colorectal cancer screening: prospective multicenter study. Am J Gastroenterol. 2008;103:1496–1504. doi: 10.1111/j.1572-0241.2008.01824.x. [DOI] [PubMed] [Google Scholar]
- 32.Shastri YM, Stein JM. New faecal tests for colorectal cancer screening: is tumour pyruvate kinase M2 one of the options? Br J Cancer. 2007;97:1595–1596; author reply 1597. doi: 10.1038/sj.bjc.6604039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Haug U, Rothenbacher D, Wente MN, Seiler CM, Stegmaier C, Brenner H. Tumour M2-PK as a stool marker for colorectal cancer: comparative analysis in a large sample of unselected older adults vs colorectal cancer patients. Br J Cancer. 2007;96:1329–1334. doi: 10.1038/sj.bjc.6603712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vollmer H. [Intestinal cancer precautions. Stool test for tumor M2 pyruvate kinase] Med Monatsschr Pharm. 2007;30:351–352. [PubMed] [Google Scholar]
- 35.Mulder SA, van Leerdam ME, van Vuuren AJ, Francke J, van Toorenenbergen AW, Kuipers EJ, Ouwendijk RJ. Tumor pyruvate kinase isoenzyme type M2 and immunochemical fecal occult blood test: performance in screening for colorectal cancer. Eur J Gastroenterol Hepatol. 2007;19:878–882. doi: 10.1097/MEG.0b013e3282cfa49c. [DOI] [PubMed] [Google Scholar]
- 36.Czub E, Herzig KH, Szaflarska-Popawska A, Kiehne K, Socha P, Woś H, Kamińska B, Błaszczyński M, Cichy W, Bała G, et al. Fecal pyruvate kinase: a potential new marker for intestinal inflammation in children with inflammatory bowel disease. Scand J Gastroenterol. 2007;42:1147–1150. doi: 10.1080/00365520701320513. [DOI] [PubMed] [Google Scholar]
- 37.Ewald N, Schaller M, Bayer M, Akinci A, Bretzel RG, Kloer HU, Hardt PD. Fecal pyruvate kinase-M2 (tumor M2-PK) measurement: a new screening concept for colorectal cancer. Anticancer Res. 2007;27:1949–1952. [PubMed] [Google Scholar]
- 38.Hathurusinghe HR, Goonetilleke KS, Siriwardena AK. Current status of tumor M2 pyruvate kinase (tumor M2-PK) as a biomarker of gastrointestinal malignancy. Ann Surg Oncol. 2007;14:2714–2720. doi: 10.1245/s10434-007-9481-x. [DOI] [PubMed] [Google Scholar]
- 39.Chung-Faye G, Hayee B, Maestranzi S, Donaldson N, Forgacs I, Sherwood R. Fecal M2-pyruvate kinase (M2-PK): a novel marker of intestinal inflammation. Inflamm Bowel Dis. 2007;13:1374–1378. doi: 10.1002/ibd.20214. [DOI] [PubMed] [Google Scholar]
- 40.Shastri YM, Stein J. Fecal tumor M2 pyruvate kinase is not a specific biomarker for colorectal cancer screening. World J Gastroenterol. 2007;13:2768–2769. doi: 10.3748/wjg.v13.i19.2768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tonus C, Neupert G, Sellinger M. Colorectal cancer screening by non-invasive metabolic biomarker fecal tumor M2-PK. World J Gastroenterol. 2006;12:7007–7011. doi: 10.3748/wjg.v12.i43.7007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ewald N, Toepler M, Akinci A, Kloer HU, Bretzel RG, Hardt PD. [Pyruvate kinase M2 (tumor M2-PK) as a screening tool for colorectal cancer (CRC). A review of current published data] Z Gastroenterol. 2005;43:1313–1317. doi: 10.1055/s-2005-858657. [DOI] [PubMed] [Google Scholar]
- 43.Walkowiak J, Banasiewicz T, Krokowicz P, Hansdorfer-Korzon R, Drews M, Herzig KH. Fecal pyruvate kinase (M2-PK): a new predictor for inflammation and severity of pouchitis. Scand J Gastroenterol. 2005;40:1493–1494. doi: 10.1080/00365520500319112. [DOI] [PubMed] [Google Scholar]
- 44.Vogel T, Driemel C, Hauser A, Hansmann A, Lange S, Jonas M, Möslein G. [Comparison of different stool tests for the detection of cancer of the colon] Dtsch Med Wochenschr. 2005;130:872–877. doi: 10.1055/s-2005-865100. [DOI] [PubMed] [Google Scholar]
- 45.Naumann M, Schaum B, Oremek GM, Hanisch E, Rösch W, Mössner J, Caspary WF, Stein J. [Faecal pyruvate kinase type M2--a valid screening parameter for colorectal cancer? Preliminary results from a multicenter comparative study] Dtsch Med Wochenschr. 2004;129:1806–1807. doi: 10.1055/s-2004-829033. [DOI] [PubMed] [Google Scholar]
- 46.Hardt PD, Mazurek S, Toepler M, Schlierbach P, Bretzel RG, Eigenbrodt E, Kloer HU. Faecal tumour M2 pyruvate kinase: a new, sensitive screening tool for colorectal cancer. Br J Cancer. 2004;91:980–984. doi: 10.1038/sj.bjc.6602033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hardt PD, Toepler M, Ngoumou B, Rupp J, Kloer HU. Fecal pyruvate kinase concentrations (ELISA based on a combination of clone 1 and clone 3 antibodies) for gastric cancer screening. Anticancer Res. 2003;23:855–857. [PubMed] [Google Scholar]
- 48.Hardt PD, Toepler M, Ngoumou B, Rupp J, Kloer HU. Measurement of fecal pyruvate kinase type M2 (tumor M2-PK) concentrations in patients with gastric cancer, colorectal cancer, colorectal adenomas and controls. Anticancer Res. 2003;23:851–853. [PubMed] [Google Scholar]
- 49.Tonus C, Neupert G, Witzel K. The faecal tumour M2-PK screening test for invasive and pre-invasive colorectal cancer: estimated specificity and results as a function of age for a study population of 4854 volunteers. Nowotwory J Oncol. 2009;59:32e–37e. [Google Scholar]
- 50.Kloer HU, Hardt PD Schlierbach P, Toepler M. The tumour metabolic marker M2-PK in stool: a new biomarker for colorectal cancer. ASCO Annual Meeting Proceedings. 2005 ASCO Annual Meeting; 2005 May 13-15; Orlando, FL. Alexandria, VA. In: Journal of Clinical Oncology; 2005. p. ASCO, 2005: 3598. [Google Scholar]
- 51.McLoughlin R, Shiel E, Sebastian S, Ryan B, O´Connor HJ, O´Morain C. Tumor M2-PK, a novel screening tool for colorectal cancer. Oct 2-5; Birmingham, UK. London. In: Poster Abstracts and Trade Exhibition Book. NCRI Cancer Conference;; 2005. p. Callisto, 2005: 202. [Google Scholar]
- 52.Bellutti M, Mönkemüller K, Malfertheiner R. Faecal Tumour M2-pyruvate kinase (M2-PK) as a potential screening parameter for colorectal adenoma and carcinoma: preliminary results. Nov 24-26; Magdeburg, Germany. Attiki, Greece. In: Anticancer Res. Abstract Eur Bridging Meeting;; 2005. pp. International Institute of Anticancer Research, 2007: 1949–1952. [Google Scholar]
- 53.Schmidt C. Wertigkeit der fäkalen Tumour M2 Pyruvate kinase (TuM2-PK) für die Detektion eines kolorektalen Karzinoms. In: Doctoral thesis of the Medical Faculty of the University of Würzburg; 2009. [Google Scholar]
- 54.Towler B, Irwig L, Glasziou P, Kewenter J, Weller D, Silagy C. A systematic review of the effects of screening for colorectal cancer using the faecal occult blood test, hemoccult. BMJ. 1998;317:559–565. doi: 10.1136/bmj.317.7158.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.van Rijn JC, Reitsma JB, Stoker J, Bossuyt PM, van Deventer SJ, Dekker E. Polyp miss rate determined by tandem colonoscopy: a systematic review. Am J Gastroenterol. 2006;10:343–350. doi: 10.1111/j.1572-0241.2006.00390.x. [DOI] [PubMed] [Google Scholar]
- 56.Campbell KP, Coates RJ, Chattopadhyay S. Evidence-statement: Colorectal Cancer (Screening) In: Campbell KP, Lanza A, Dixon R, Chattopadhyay S, Molinari N, et al., editors. A Purchasers Guide to Clinical Preventive Services: Moving Science into Coverage. Washington, DC: National Business Group on Health; 2006. pp. 195–200. [Google Scholar]


