Abstract
This study examined the relationship between loneliness, health, and mortality using a U.S. nationally representative sample of 2,101 adults aged 50 years and over from the 2002 to 2008 waves of the Health and Retirement Study. We estimated the effect of loneliness at one point on mortality over the subsequent six years, and investigated social relationships, health behaviors, and health outcomes as potential mechanisms through which loneliness affects mortality risk among older Americans. We operationalized health outcomes as depressive symptoms, self-rated health, and functional limitations, and we conceptualized the relationships between loneliness and each health outcome as reciprocal and dynamic. We found that feelings of loneliness were associated with increased mortality risk over a 6-year period, and that this effect was not explained by social relationships or health behaviors but was modestly explained by health outcomes. In cross-lagged panel models that tested the reciprocal prospective effects of loneliness and health, loneliness both affected and was affected by depressive symptoms and functional limitations over time, and had marginal effects on later self-rated health. These population-based data contribute to a growing literature indicating that loneliness is a risk factor for morbidity and mortality and point to potential mechanisms through which this process works.
Keywords: U.S.A., Loneliness, Mortality, Emotional Health, Functional Health, Self-Rated Health, Longitudinal Study, Cross-Lagged Path Model, elderly
Introduction
Loneliness is a prevalent and serious social and public health problem (Hawkley & Cacioppo, 2010). Research on loneliness, conducted mostly in Western countries, has shown that at any given time, twenty to forty percent of older adults report feeling lonely (De Jong Gierveld & Van Tilburg, 1999; Savikko et al., 2005; Theeke, 2009; Walker, 1993), and from five to seven percent report feeling intense or persistent loneliness (Steffick, 2000; Victor et al., 2005). Socially isolated individuals tend to feel lonely, but loneliness is not synonymous with being socially isolated. Loneliness can be thought of as perceived isolation and is more accurately defined as the distressing feeling that accompanies discrepancies between one’s desired and actual social relationships (Pinquart & Sorenson, 2003). Prospective studies have shown that feelings of loneliness predict depressive symptoms (Cacioppo et al., 2010), impaired sleep and daytime dysfunction (Hawkley et al., 2010a), reductions in physical activity (Hawkley et al., 2009), and impaired mental health and cognition (Wilson et al., 2007). At the biological level, loneliness is associated with increased vascular resistance (Cacioppo et al., 2002; Hawkley et al., 2003), increased systolic blood pressure (SBP) (Hawkley et al., 2010b), increased hypothalamic pituitary adrenocortical activity (Adam et al., 2006; Steptoe et al., 2004), under-expression of genes bearing anti-inflammatory glucocorticoid response elements (GREs), over-expression of genes bearing response elements for pro-inflammatory NF-κB/Rel transcription factors (Cole et al., 2007; Cole et al., 2011), and altered immunity (Kiecolt-Glaser et al., 1984; Pressman et al., 2005). Moreover, an increasing body of research shows that feelings of isolation and loneliness predict mortality (Patterson & Veenstra, 2010; Shiovitz-Ezra & Ayalon, 2010; Tilvis et al., 2011).
In this study, we specify a conceptual model that examines several mechanisms that might account for the effects of perceived isolation (i.e., loneliness) on mortality, and we test this model using a sample of U.S. older adults Our model posits that health—emotional, physical, and functional—is a proximal predictor of mortality and we therefore test for longitudinal effects of loneliness on health to determine whether health variables are plausible mediators of the loneliness effect on mortality. Previous research has tended to focus on the link between loneliness and specific diseases or health conditions, often in small, local samples. Most analyses have used cross-sectional data or examined changes in either loneliness or health, not their dynamic interactions. We add to this literature by (1) examining the link between loneliness and a number of general measures of health, (2) using a large, nationally-representative sample, and (3) modeling the dynamic interactions between loneliness and health over time.
Loneliness and Mortality
Our conceptual model posits that the influence of loneliness on mortality is attributable to the relationships between loneliness and social isolation, unhealthy behaviors, and poor health. Prospective epidemiological studies have shown that objectively indexed social isolation is a major risk factor for morbidity and mortality (House et al., 1988). Because feelings of loneliness are more prevalent and intense in socially isolated individuals, the mortality effects of loneliness may be explained, at least in part, by the higher likelihood of being more socially isolated among those feeling lonely. The effect of social isolation on health and mortality, in turn, has been attributed in part to the direct influence of friends and family on a person’s health behaviors (e.g., exercise, adequate and regular rest) which influence physiology and health (House et al., 1988). To the extent that socially isolated individuals are more likely to engage in poor health behaviors, health behaviors may help explain their increased mortality risk. Two lines of evidence suggest otherwise, however. First, health behaviors in epidemiological and field studies have failed to explain the health effects of social isolation in humans (Hawkley et al., 2010b; Seeman, 2000). Second, non-human social animals subjected to social isolation are also at increased risk for early morbidity and mortality (reviewed in Cacioppo & Hawkley, 2009), suggesting that the effects of isolation extend beyond the social control of health behaviors exerted by concerned friends and family.
Health behaviors may help explain loneliness differences in mortality risk, however. Our theoretical model of loneliness holds that loneliness activates implicit hypervigilance for social threat in the environment (Cacioppo & Hawkley, 2009). Chronic activation of social threat surveillance diminishes executive functioning, and heightened impulsivity influences the tendency of individuals to engage in health behaviors that require self-control. Consistent with this notion, among middle- and older-age U.S. adults, loneliness was associated with a lower likelihood of engaging in physical activity and a faster decline in levels of physical activity participation over a two-year follow-up period (Hawkley et al., 2009).
Our conceptual model further posits that loneliness differences in mortality may be more directly explained by health, where health outcomes are the more proximal predictors of mortality. We therefore introduce emotional, physical, and functional health as additional mechanisms that may explain the association between loneliness and heightened risk of mortality. In this study, the emotional health outcome to be examined is depressive symptoms, the physical health outcome is self-rated health, and the functional health outcome is functional limitations. Justification for these outcomes as plausible mediators of loneliness differences in mortality is based on evidence showing that loneliness predicts these outcomes (as will be discussed below) and that these outcomes predict mortality (Ariyo et al., 2000; Everson et al., 1998; Idler & Benyamini, 1997; Okun et al., 2010).
Loneliness and Emotional, Physical, and Functional Health
Loneliness feels bad, as is evident by lower levels of well-being (Cacioppo et al., 2008) and higher levels of depressive symptoms (Nolen-Hoeksema & Ahrens, 2002) in lonelier individuals. Beyond cross-sectional associations between loneliness and depressive symptoms, loneliness leads to increases in depressive symptoms in longitudinal U.S. studies (Cacioppo et al., 2010; Hagerty & Williams, 1999; Wei et al., 2005). Accordingly, we expect that loneliness will predict increases in depressive symptoms over time in our sample, and that this predictive role is necessary if depressive symptoms are to be considered plausible mechanisms through which loneliness affects mortality.
Loneliness is associated with poor physical health, and this relationship is effectively captured in the inverse association between loneliness and self-rated health (Segrin & Domschke, 2011; Stephens et al., 2011). Moreover, loneliness and increases in loneliness over time predict decrements in self-rated health (Nummela et al., 2011). We expect that loneliness will predict decreases in self-rated health over time in our sample, and that this predictive role is necessary if self-rated health is to be considered a plausible mechanism through which loneliness affects mortality.
Finally, we examine whether loneliness is related to functional limitations and increases in functional limitations over time. Physical activity is important in maintaining higher levels of physical functioning (Keysor, 2003; Lee & Park, 2006; Netuveli et al., 2008), and because lonely individuals are less likely to engage in physical activity than their non-lonely counterparts (Hawkley et al., 2009), they are more likely to experience the onset or worsening of limitations. Prior cross-sectional research has shown an association between loneliness and functional limitations (Greenfield & Russell, 2011; Prieto-Flores et al., 2011), but a plausible role for functional limitations in explaining loneliness differences in mortality would gain support if loneliness predicts increases in functional limitations while controlling for concurrent effects of functional limitations on loneliness.
Our analyses allow reciprocal relationships between loneliness and each health outcome, thus providing more rigorous assessments than previous studies of the causal directions between these variables. We hypothesize that loneliness negatively affects each later health outcome, even after accounting for the potential effects of poor health on later feelings of loneliness. All models linking loneliness and health take into account sociodemographic characteristics of the individual, including age, gender, race/ethnicity, education, and household income and assets, as well as measures of social isolation or, conversely, social relationships (marital status, the presence of relatives, and separately, friends in the neighborhood), and health behaviors (sleep quality, physical exercise, smoking history and current smoking).
Methods
Data mainly come from the 2002, 2004, 2006 waves of the Health and Retirement Study (HRS) although mortality data in 2008 were also used. The HRS is a U.S. nationally representative, longitudinal study of older Americans composed of five birth cohorts that entered the study in different calendar years and the data are publicly available. The HRS began in 1992–93 as two separate samples: the original HRS focusing on 1931–41 birth cohorts and the Assets and Health Dynamics among the Oldest Old focusing on 1890–1923 birth cohorts. In 1998 the two samples were merged and two new samples, Cohort of Depression Age (1924–30 cohorts) and War Babies (1942–47 cohorts), were added, and in 2004, another new sample, Early Baby Boomers (1948–53 cohorts), was added, making the sample representative of those born in 1953 or before, approximately aged over 50 in 2004. Once they have entered the study, respondents were re-interviewed every two years. The spouses were also interviewed irrespective of their age. The sample for each cohort was derived from the same stratified, multistage area probability design in which blacks, Hispanics, and Floridians were over sampled. The HRS now includes over 30,000 respondents. The initial cohort response rates ranged from 70 percent to slightly over 80 percent; re-interview rates for all cohorts at each wave have been between 92 and 95 percent (Health and Retirement Study, 2011).
Since its inception in 1992, the HRS has focused on the health, economics, and demographics of aging and the retirement process. The 2002 wave of HRS included a module on loneliness and 2,190 respondents were randomly selected to answer the questions in this module. Among them 2,101 respondents were aged 50 years and above and they constituted our analytical sample. In 2004, 1,937 were re-interviewed. In 2006, 1,815 were re-interviewed (including some who were not interviewed in 2004). Between 2002 and 2008, 303 respondents died. Loneliness questions were asked again of 1,756 respondents in 2004 primarily during in-person interviews, and were asked again of 1,620 respondents in 2006 in self-administered questionnaires that were left with the respondents upon the completion of an in-person core interview. Note that not all of the 2002 loneliness module respondents were selected to answer questions on loneliness in both 2004 and 2006.
Loneliness
In each wave, HRS asked how often the respondent feels (i) lack of companionship, (ii) left out, and (iii) isolated from others. This three-item loneliness scale was adapted from the standard measure of loneliness, the Revised UCLA Loneliness Scale, and it has been shown to have good internal consistency and both concurrent and discriminant validity (Hughes et al., 2004). The three-point response scale for each item ranges from “hardly ever or never” to “often.” A loneliness scale was created by summing scores on the three items. It ranges from 3 to 9 with higher values indicating a greater degree of loneliness; Cronbach’s alpha is .73 for 2002, .77 for 2004, and .81 for 2006.
Mortality
The study assesses mortality between 2002 and 2008. Mortality was determined through matching to the National Death Index or from contacts with household members through 2008. HRS tracking studies indicated a 98.8% validation of deaths (Health and Retirement Study, 2011). Month and year of death were released in a tracking file. Survival time was the number of months from date of 2002 interview to date of death. Of the 303 respondents who died, 9 had missing date of death and we used multiple imputation methods to assign survival time for these cases (Rubin, 1987).
Health Outcomes
Depressive symptoms, self-rated health, and functional limitations were measured in 2002, 2004, and 2006. (1) Depressive symptoms. HRS includes a short version of the Center for Epidemiological Studies Depression Scale (CES-D) designed for telephone interviews with older respondents (Turvey et al., 1999). Each item asked whether the respondent experienced a specific symptom in the past week (e.g., “I felt that everything I did was an effort”). Depression is conceptually related to but distinct from loneliness (Cacioppo et al., 2010). To reduce the overlap in measurement of the two concepts, we deleted the item in the CES-D that states “I felt lonely” from our depressive symptoms scale. We also deleted the item “sleep was restless” because quality of sleep was used as a separate covariate in our multivariate analysis. The number of depressive symptoms is a count of the affirmative responses from the remaining six items, with two items tapping positive affect reverse coded. (2) Self-rated health. Each respondent was asked to rate his or her physical health on a five-point scale from poor to excellent, providing a subjective assessment of his or her health status. (3) Functional limitations. The number of functional limitations was calculated by summing responses to twelve items assessing whether the respondent has any difficulty with specific forms of ambulation, such as walking a block and climbing a flight of stairs, or muscle movements, such as moving a large chair or picking up a dime. For the 371 respondents who indicated that they do not do certain activities, we used multiple imputation method to impute their values.
Covariates
Our measures of social relationships include marital status, presence of relatives living nearby, and presence of friends living nearby. (1) Marital status. We compared respondents who are currently married with those who are separated, divorced, widowed, or never married. (2) Relatives living nearby. This variable was coded 1 if the answer is yes to the question: “Besides the people living here with you, do you have any relative in your neighborhood?” and 0 if the answer is no. (3) Friends living nearby. It was coded 1 if the answer is yes to the question: “Do you have any good friends living in your neighborhood?” and 0 if the answer is no.
Measures of health behaviors include sleep quality, physical exercise, current and past smoking. (1) Sleep quality. Respondents were asked how often they (i) “have trouble falling asleep,” (ii) “have trouble with waking up during the night,” (iii) “have trouble with waking up too early and not being able to fall asleep again,” and (iv) “feel really rested when you wake up in the morning.” The three-point response options to each item range from “most of the time” to “rarely or never.” With the first three items reverse coded, the sleep quality scale is the sum of responses to the four items. It ranges from 4 to 12 with higher scores indicating poorer sleep quality; Cronbach’s alpha is .65 in 2002. (2) Physical exercise. This measure was coded 1 if the answer is yes to the question whether on average over the last 12 months the respondent has participated in vigorous physical activity or exercise three times a week or more, and 0 if the answer is no. (3) Smoking. Respondents were asked whether they ever smoked cigarettes in their life time and for those who answered yes, whether they smoke cigarettes now. Based on this information, we grouped respondents into three categories: never smoked, past smoker, and current smoker. Multiple imputation was used to assign past smoking status for the 13 respondents who were missing on this information.
Sociodemographics include age, gender, race/ethnicity, education, household income and household assets. Age was measured in years. We distinguish three race/ethnicity categories: black, Hispanic, and white/others. Education was measured with the years of schooling completed. We use the total household income and household assets with missing data imputed by the HRS staff. Household income and household assets were log transformed to adjust for positive skew.
Statistical Procedures
We weighted descriptive statistics by the sampling weight. The multivariate analyses were not weighted as research has shown that including variables related to sample selection in the regression produces unbiased coefficients without weights (Winship & Radbill, 1994). First, we conducted survival analysis to examine the effect of loneliness in 2002 on mortality between 2002 and 2008. Parametric hazard models with Weibull distribution were used to estimate the hazard ratios and 95% confidence intervals. The parametric models produced more efficient estimates than semiparametric (Cox) hazard models (Cleves et al., 2008), and the Weibull distribution was the most efficient and parsimonious functional form for our sample data based on the Akaike Information Criterion. Preliminary analyses using Cox models showed essentially the same patterns. A series of four hierarchical Weibull hazard models was estimated using Stata Version 11. The first model included loneliness and sociodemographic covariates in 2002, the next three models sequentially added social relationships, health behaviors, and health variables in 2002. We added predictors in blocks of conceptually related variables because we were interested in identifying whether one or more variables within each block were uniquely and independently predictive of mortality. These additive models allowed us to examine the extent to which the effect of loneliness on mortality risk is explained by social relationships, health behaviors, and emotional, physical, and functional health. We performed Sobel tests with bootstrapping to test the significance of the indirect effects and to determine whether the effect of loneliness was significantly reduced with the addition of each block of explanatory variables (Preacher & Hayes, 2008). Because the assumption that indirect effects calculated by the product of coefficients method (αβ) and those calculated by the difference in coefficients method (τ-τ′) were not always identical in survival analysis (Tein & MacKinnon, 2003), we report results from both methods.
Next, we used cross-lagged path analysis to examine the relationships between loneliness and each health outcome. The survival analysis indicates whether loneliness affects mortality risk and the degree to which this effect is reduced when we hold constant measures of health status, possible mechanisms through which loneliness affects mortality. However, because loneliness and health status were measured at the same time, the causal directions between them cannot be established. For this reason we turned next to cross-lagged panel models and estimated autoregressive and cross-lagged paths, which allowed us to address reciprocal influences of loneliness and health simultaneously (Curran, 2000). These models were estimated with MPlus Version 5 (Muthén & Muthén, 1998–2007). Missing data were not imputed; rather, available data from all 2,101 respondents were used in analyses. All models were estimated using Full Information Maximum Likelihood estimation with robust standard errors. The FIML method uses all information of the observed data, including mean and variance for the missing portions of a variable, given the observed portion(s) of other variables. FIML produces consistent and efficient estimates when the data are “missing at random” (MAR) and produces less biased estimates than other methods when the data deviate from MAR (Wothke, 1998). The degree of model fit was assessed with the chi-square goodness of fit statistic and the root-mean-square error of approximation (RMSEA). MacCallum and colleagues (1996) characterized a model with an RMSEA of .08 or less as an adequate fit; Hu & Bentler (1999) characterized a model with an RMSEA of .05 or less as a good fit and .10 or more as a poor fit.
We estimated separate cross-lagged path models for loneliness and each health outcome. All models include sociodemographic characteristics, measures of social relationships, and health behaviors as covariates. Our theoretical models assume that prospective relationships between variables are stable over time. These assumptions were modeled by applying equality constraints to the autoregressive and cross-lagged paths, thereby imposing “stationarity” on the relationships among variables in the model. We also assumed that the 2-year prospective effects of covariates on loneliness, depressive symptoms, self-rated health, and functional limitations did not differ from one time point to another. Therefore equality constraints were applied to each of these covariates over the two 2-year intervals. Correlations between variables and residuals at a given time were also estimated.
Results
Descriptive Statistics
Weighted descriptive statistics of the variables are presented in Table 1. The average score of the loneliness scale was quite similar in 2002 and 2004, but increased between 2004 and 2006 (t = 9.56, p < .001). The latter increase may be in part due to the change in data collection method from in-person interviews in 2004 to self-administered questionnaires in 2006. There were no significant changes in the average number of depressive symptoms over the 4-year period. Self-rated health had deteriorated from 2002 to 2006 (t = −3.85, p < .001) and the number of functional limitations had increased (t = 4.95, p < .001). Intraclass correlation, which indicates within-subject stability, was .51 for depressive symptoms, .67 for self-rated health, and .76 for functional limitations.
Table 1.
Descriptive statistics of the HRS sample
| Variables | Year 2002 | Year 2004 | Year 2006 | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Mean/% | SD | Mean/% | SD | N | Mean/% | SD | N | |
| Loneliness (3–9) | 3.84 | 1.33 | 3.80 | 1.32 | 1,675 | 4.29 | 1.53 | 1,540 |
| Depressive symptoms (0–6) | .95 | 1.43 | .89 | 1.44 | 1,902 | .90 | 1.42 | 1,765 |
| Self-rated health (1–5) | 3.35 | 1.08 | 3.28 | 1.08 | 1,936 | 3.21 | 1.07 | 1,813 |
| Functional limitations (0–12) | 2.58 | 2.71 | 2.74 | 2.85 | 1,937 | 3.09 | 3.03 | 1,815 |
| Married % | 76.4 | |||||||
| Relatives living nearby % | 31.8 | |||||||
| Friends living nearby % | 70.3 | |||||||
| Sleep quality poor (4–12) | 6.41 | 2.00 | ||||||
| Physical exercise % | 45.7 | |||||||
| Past smoker % | 44.3 | |||||||
| Current smoker % | 13.5 | |||||||
| Age (50–98) | 67.08 | 9.16 | ||||||
| Female % | 59.6 | |||||||
| Black % | 7.6 | |||||||
| Hispanic % | 5.1 | |||||||
| Education (0–17) | 12.67 | 2.83 | ||||||
| Household income (log) (0–15) | 10.57 | 1.09 | ||||||
| Household assets (log) (0–17) | 11.71 | 2.73 | ||||||
Note: N=2,101 in Year 2002. The numbers are weighted.
Loneliness and Mortality
Table 2 presents results from the analysis of mortality between 2002 and 2008. Net of sociodemographic characteristics, feeling lonely in 2002 was associated with increased mortality risk over the subsequent six years (OR = 1.14, 95% CI = 1.06, 1.23) (Table 2, Model I). When social relationships were added in Model II, the change in the coefficient for loneliness was not statistically significant and none of the social relationship measures were associated with mortality risk. A test of mediation using the product of coefficients method showed that neither the total indirect effect nor the indirect effect through each of the social relationship variable was statistically significant. When health behaviors were added in Model III, the coefficient for loneliness did not decrease significantly, although physical exercise and past and current smoking were all associated with mortality in the expected direction. A test of mediation using the product of coefficients method showed that neither the total indirect effect nor the indirect effect through each of the health behavior variables was statistically significant.
Table 2.
Hazard ratios of the Weibull models of mortality from 2002 to 2008
| Variables | Model I | Model II | Model III | Model IV | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Hazard ratio | 95% CI | Hazard ratio | 95% CI | Hazard ratio | 95% CI | Hazard Ratio | 95% CI | |
| Loneliness in 2002 | 1.14*** | [1.06, 1.23] | 1.13** | [1.05, 1.22] | 1.12** | [1.03, 1.21] | 1.07+ | [.99, 1.17] |
| Married | .91 | [.69, 1.21] | .93 | [.70, 1.23] | .87 | [.65, 1.15] | ||
| Relatives living nearby | .92 | [.72, 1.17] | .92 | [.72, 1.17] | .93 | [.72, 1.19] | ||
| Friends living nearby | .86 | [.66, 1.11] | .95 | [.73, 1.24] | .91 | [.70, 1.19] | ||
| Sleep quality poor | 1.02 | [.96, 1.08] | .94+ | [.89, 1.00] | ||||
| Physical exercise | .60*** | [.47, .78] | .79+ | [.61, 1.04] | ||||
| Past smokera | 1.37* | [1.06, 1.78] | 1.30+ | [1.00, 1.69] | ||||
| Current smokera | 1.57* | [1.06, 2.32] | 1.46+ | [.98, 2.17] | ||||
| Depressive symptoms in 2002 | .98 | [.89, 1.07] | ||||||
| Self-rated health in 2002 | .65*** | [.57, .75] | ||||||
| Functional limitations in 2002 | 1.08** | [1.02, 1.13] | ||||||
| Age | 1.09*** | [1.08, 1.10] | 1.09*** | [1.07, 1.10] | 1.09*** | [1.07, 1.10] | 1.08*** | [1.07, 1.10] |
| Female | .49*** | [.39, .62] | .48*** | [.38, .61] | .50*** | [.39, .65] | .50*** | [.38, .64] |
| Blacka | .90 | [.62, 1.30] | .90 | [.62, 1.32] | .90 | [.62, 1.31] | .78 | [.54, 1.13] |
| Hispanica | 1.09 | [.69, 1.73] | 1.09 | [.69, 1.74] | 1.06 | [.67, 1.69] | 1.02 | [.64, 1.61] |
| Education | 1.02 | [.98, 1.06] | 1.02 | [.98, 1.06] | 1.02 | [.98, 1.07] | 1.05* | [1.01, 1.09] |
| Household income (log) | .81*** | [.73, .89] | .82*** | [.74, .91] | .83*** | [.74, .92] | .86** | [.77, .96] |
| Household assets (log) | .95** | [.91, .99] | .95* | [.92, .99] | .96* | [.92, 1.00] | .97 | [.93, 1.01] |
| Chi-square | 273.76 | 276.19 | 300.77 | 378.87 | ||||
| df | 8 | 11 | 15 | 18 | ||||
Note: N=2,101. Results are unweighted. Sobel test of the change in coefficient of loneliness from Model I to Model II is −.005 with bias corrected 90% CI=[−.021, .012], total mediated effect through social relationship variables is .005 with 90% CI=[−.004, .018]; the change in coefficient of loneliness from Model II to Model III is −.012 with 90% CI=[−.030, .007], total mediated effect through health behavior variables is .014 with 90% CI=[−.002, .035]; the change in coefficient of loneliness from Model III to Model IV is −.041 with 90% CI=[−.076, −.001], total mediated effect through health variables is .051 with 90% CI=[.016, .082].
Reference categories are “Never smoked,” and “White or Others.”
p < .1,
p < .05,
p < .01,
p < .001
The next model (Model IV) added measures of health. The effect of loneliness became only marginally significant when depressive symptoms, self-rated health, and functional limitations were added jointly (OR = 1.07, 95% CI = .99, 1.17), and this attenuation was marginally significant at p < .1. Among these health measures, self-rated health and functional limitations each had a significant independent effect on mortality risk. A test of mediation using the product of coefficients method showed that the total indirect effect through all three health variables was significant (B = .05, 90% CI = .02, .08, p < .05), and the individual indirect effects of self-rated health (B = .04, 90% CI = .02, .06, p < .001) and functional limitations (B = .02, 90% CI = .01, .03, p < .01) were also significant.
Not surprisingly, mortality risk was higher for individuals who were older, male, and with lower household income and assets. Education was not associated with mortality risk in Model I when household income and assets were controlled for, but its effect on mortality risk became positive and significant once health measures were added in Model IV. This indicates a statistical suppression effect that reflects correlations between education and health. Specifically, education was associated with better health, but when income/assets and health advantages of education were held constant, education predicted greater risk of mortality.
Loneliness and Emotional, Physical, and Functional Health
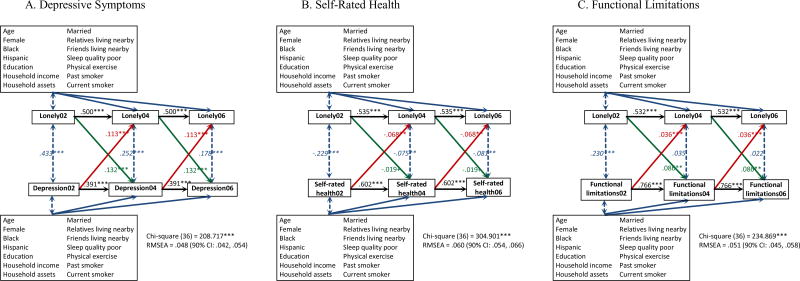
Figure 1 shows the cross-lagged relationships between loneliness and depressive symptoms, self-rated health, and functional limitations while controlling for sociodemographic covariates, social relations, and health behaviors. The results support stationary processes and in each case fit the data adequately. The RMSEA was .048 (90% CI = .042, .054) for depressive symptoms, .060 (90% CI = .054, .066) for self-rated health, and .051 (90% CI = .045, .058) for functional limitations. The 2-year cross-lagged effect of loneliness on depressive symptoms was significant (B = .132, p < .001), and the 2-year cross-lagged effect of depressive symptoms on loneliness was also significant (B = .113, p < .001). Thus these results provide evidence for a reciprocal relationship between loneliness and depressive symptoms. We also see a similar reciprocal relationship between loneliness and functional limitations. The 2-year cross-lagged effect of loneliness on functional limitations was significant (B = .086, p < .01), as was the 2-year cross-lagged effect of functional limitations on loneliness (B = .036, p < .001). The 2-year cross-lagged effect of loneliness on self-rated health was marginally significant (B = −.019, p < .10), and the 2-year cross-lagged effect of self-rated health on loneliness was significant (B = −.068, p < .01).
Figure 1.
Cross-lagged relationship between loneliness and health net of sociodemographic covariates, social relationships, and health behaviors. Italicized estimates are standardized covariances (i.e., correlations) and the remaining estimates are unstandardized coefficients. + p < .1, * p < .05, ** p < .01, *** p < .001.
Discussion
This study replicates and extends a growing body of prospective research showing that loneliness has adverse consequences for health and mortality. In a large, population-based national sample of older Americans, we replicated prior research by showing that feelings of loneliness are associated with increased mortality risk. Net of sociodemographic characteristics, social relationships, and health behaviors, older adults with the highest levels of loneliness were 1.96 times more likely to die within six years than those with the lowest levels of loneliness.
Several studies exist on the mechanisms that may explain the association between loneliness and mortality. Sugisawa et al. (1994) reported that the effect of loneliness on mortality over a 3-year period among older adults in Japan was fully explained by chronic diseases, functional status, and self-rated health. Patterson & Veenstra (2010) found that the relationship between loneliness and mortality fell to non-significance when social relationships and health behaviors were taken into account. Shiovitz-Ezra & Ayalon (2010) found that the effect of loneliness on mortality remained statistically significant after controlling for medical status, functional impairment, and depression. The apparent inconsistencies may be attributable to differences in the mechanisms that were investigated and the measures that were included. Shiovitz-Esra & Ayalon (2010), for instance, did not include health behaviors or social relationships in their analysis. In the present study, we included measures of each of these mechanisms. In addition, we used a time sensitive model for survival analysis while some previous studies used a simple “died-didn’t die” dichotomy (e.g., Patterson & Veenstra, 2010). Moreover, unlike other studies, we explicitly tested the significance of mediated (i.e., indirect) effects and the resulting change in the magnitude of the direct effect of loneliness. Our results showed that the three health outcomes combined to affect changes in the risk of dying later, and that taking the health variables into account resulted in a small decline in the association between loneliness and mortality. The results of the mediational analyses further indicated that functional status and self-rated health, but not depressive symptoms, constitute proximal mechanisms through which loneliness affects later mortality.
Mortality analysis showed that health outcomes assessed at the same time as loneliness helped explain the effect of loneliness on mortality, but did not permit evaluation of the causal direction between loneliness and health. Using cross-lagged models, we found that loneliness predicted increases in depressive symptoms, modest decreases in self-rated health and increases in functional limitations over two years even when the reciprocal effects of these health measures on loneliness were taken into account. These findings are consistent with a causal direction that implicates decrements in emotional and physical health as mechanisms through which loneliness leads to increases in mortality risk.
Possessing a richness of social attachments and friends protects against mortality (House et al., 1988), and generally signifies lower levels of loneliness (Hawkley et al., 2008; Pinquart & Sorenson, 2003). Ancillary analyses confirmed that respondents who were married and who had more friends living nearby were less lonely (not shown), but these objective characteristics of respondents’ social lives did not explain much of the effect of loneliness on mortality risk. This is consistent with Patterson and Veenstra (2010) which, in a much larger sample of more than 6,500 adults followed over a 34-year period, found only a modest effect of marital status and no effect of number of close friends and relatives on mortality risk independent of a significant effect of loneliness.
We posited that social relationships may influence mortality to the extent that family and friends exert social control by encouraging and supporting salubrious health behaviors. At the same time, we noted that health behaviors are insufficient to account for the mortality effects of the existence (or not) of social relationships in humans and are not plausible explanations for mortality effects in socially isolated non-human social animals. The effects of loneliness on self-control (Cacioppo & Hawkley, 2009), on the other hand, suggest that health behaviors may differ as a function of loneliness and help explain mortality differences. This reasoning did not find support, however. Although health behaviors influenced mortality as expected, health behaviors (physical exercise, smoking) did not explain loneliness differences in mortality.
The fact that loneliness continues to predict health outcomes when health behaviors are held constant suggests that loneliness alters physiology at a more fundamental level. The sizeable remaining effect of loneliness on mortality in our final model allows for additional explanatory mechanisms. Prior research indicates that loneliness increases vascular resistance (Hawkley et al., 2003), increases SBP (Hawkley et al., 2010b), alters hypothalamic pituitary adrenocortical activity (Adam et al., 2006), diminishes sleep salubrity (Hawkley et al., 2010a), alters gene transcription (Cole et al., 2007, 2011), and diminishes immunity (Pressman et al., 2005). Future research should include efforts to examine how these physiological processes contribute to the effect of loneliness on mortality.
This study used a 3-item composite index of loneliness which has been shown to have good validity and reliability (Hughes et al., 2004). This measure is an important improvement over previous studies on the loneliness-mortality relationship that measured loneliness with a single item asking respondents whether and/or how often they felt lonely. Specifically, our 3-item measure avoids use of the term “lonely” or “loneliness” and thus avoids much of the stigma associated with and consequent underestimation of loneliness. Nevertheless, the fact that mean loneliness levels were higher in 2006 than in 2002 and 2004, and that this difference corresponded to a change from an interview-based to a self-administered questionnaire leaves open the possibility that stigma may have resulted in an underestimation of loneliness in the interview-based data. Future waves of HRS, in which loneliness will continue to be assessed by self-administered questionnaire, will allow testing the degree to which the relationships reported in this study are robust to questionnaire format.
Furthermore, even though we analyzed the reciprocal associations of loneliness with depressive symptoms, self-rated health, and functional limitations, arguably other factors, such as sleep quality and physical activities, could be both cause and effect of loneliness and health. Future research needs to construct more complex models to gain a better understanding of the dynamics of these relationships.
Our study contributes to a growing literature indicating that loneliness is a risk factor for morbidity and mortality and it points to potential mechanisms through which this process works. Whether loneliness has similar health effects and operates through similar mechanisms in non-Western countries as was observed in the U.S. remains to be studied, and the importance of such research is highlighted by the fact that loneliness is as or more prevalent in non-Western countries as in the United States. In China, for example, a national survey conducted in 2000 found that 29.8% of older adults were lonely (Yang & Victor, 2008); in rural China, as many as 78.1% of the older adults were reportedly moderately or intensely lonely (Wang et al., 2011). The potential implications for health and longevity are great in a world characterized by societal unrest and threats to the integrity of people’s sense of interpersonal and collective connectedness.
Highlights.
Using longitudinal data, we examined the causal relationship between loneliness and emotional, physical, and functional health in the USA
We show that the effects of loneliness on mortality risk in old age are modestly explained by mediating health outcomes.
Loneliness both affects and is affected by depressive symptoms and functional limitations over time, and has marginal effects on later self-rated health.
Acknowledgments
This research was supported by Grants R01-AG036433e01, R01- AG034052, and R37-AG030481 from the National Institute on Aging. An earlier draft was presented at the Annual Meeting of the Population Association of America, Washington, DC, March 31–April 2, 2011. We thank Phil Schumm for his assistance on data analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adam EK, Hawkley LC, Kudielka BM, Cacioppo JT. Day-to-day dynamics of experience: Cortisol associations in a population-based sample of older adults. Proceedings of the National Academy of Science of the United States of America. 2006;103:17058–17063. doi: 10.1073/pnas.0605053103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ariyo AA, Haan M, Tangen CM, Rutledge JC, Cushman M, Dobs A, Furberg CD. Depressive symptoms and risks of coronary heart disease and mortality in elderly Americans. Circulation. 2000;102:1773–1779. doi: 10.1161/01.cir.102.15.1773. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC. Perceived social isolation and cognition. Trends in Cognitive Sciences. 2009;13(10):447–454. doi: 10.1016/j.tics.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Crawford LE, Ernst JM, Burleson MH, Kowalewski RB, et al. Loneliness and health: Potential mechanisms. Psychosomatic Medicine. 2002;64(3):407–417. doi: 10.1097/00006842-200205000-00005. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Kalil A, Hughes ME, Waite L, Thisted RA. Happiness and the invisible threads of social connection: The Chicago Health, Aging, and Social Relations Study. In: Eid M, Larsen R, editors. The Science of Well-Being. New York: Guilford; 2008. pp. 195–219. [Google Scholar]
- Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-Year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology and Aging. 2010;25(2):453–463. doi: 10.1037/a0017216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleves M, Gould W, Gutierrez R, Marchenko Y. An introduction to survival analysis using Stata. College Station, TX: Stata Press; 2008. [Google Scholar]
- Cole SW, Hawkley LC, Arevalo JM, Sung CY, Rose RM, Cacioppo JT. Social regulation of gene expression in human leukocytes: Clucocorticoid resistance in the leukocyte transcriptome. Genome Biology. 2007;8:R189.1–R189.13. doi: 10.1186/gb-2007-8-9-r189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole SW, Hawkley LC, Arevalo JM, Cacioppo JT. Transcript origin analysis identifies antigen presenting cells as primary targets of socially regulated leukocyte gene expression. Proceedings of the National Academy of Sciences. 2011;108:3080–3085. doi: 10.1073/pnas.1014218108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran PJ. A latent curve framework for the study of developmental trajectories in adolescent substance use. In: Rose JS, Chassin L, Presson CC, Sherman SJ, editors. Multivariate applications in substance use research: New methods for new questions. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. pp. 1–4. [Google Scholar]
- De Jong Gierveld J, Van Tilburg T. Living arrangements of older adults in the Netherlands and Italy: Coresidence values and behaviour and their consequences for loneliness. Journal of Cross-Cultural Gerontology. 1999;14(1):1–24. doi: 10.1023/a:1006600825693. [DOI] [PubMed] [Google Scholar]
- Everson SA, Roberts RE, Goldberg DE, Kaplan GA. Depressive symptoms and increased risk of stroke mortality over a 29-year period. Archives of Internal Medicine. 1998;158:1133–1138. doi: 10.1001/archinte.158.10.1133. [DOI] [PubMed] [Google Scholar]
- Greenfield EA, Russell D. Identifying living arrangements that heighten risk for loneliness in later life: Evidence from the U.S. National Social Life, Health, and Aging Project. Journal of Applied Gerontology. 2011;30:524–534. [Google Scholar]
- Hagerty BM, Williams AR. The effect of sense of belonging, social support, conflict, and loneliness on depression. Nursing Research. 1999;48(4):215–219. doi: 10.1097/00006199-199907000-00004. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Berntson GG, Burleson MH, Cacioppo JT. Loneliness in everyday life: Cardiovascular activity, psychosocial context, and health behaviors. Journal of Personality & Social Psychology. 2003;85(1):105–120. doi: 10.1037/0022-3514.85.1.105. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Cacioppo JT. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine. 2010;40:218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Hughes ME, Waite LJ, Masi CM, Thisted RA, Cacioppo JT. From social structural factors to perceptions of relationship quality and loneliness: The Chicago Health, Aging, and Social Relations Study. Journal of Gerontology Social Sciences. 2008;63(6):S375–S384. doi: 10.1093/geronb/63.6.s375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Preacher JT, Cacioppo JT. Loneliness impairs daytime functioning but not sleep duration. Health Psychology. 2010a;29(2):124–129. doi: 10.1037/a0018646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Thisted RA, Cacioppo JT. Loneliness predicts reduced physical activity: Cross-sectional and longitudinal analyses. Health Psychology. 2009;28:354–363. doi: 10.1037/a0014400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Thisted RA, Masi CM, Cacioppo JT. Loneliness predicts increased blood pressure: Five-year cross-lagged analyses in middle-aged and older adults. Psychology & Aging. 2010b;25:132–141. doi: 10.1037/a0017805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health and Retirement Study. Sample sizes and response rates (2002 and beyond) 2011 Retrieved September 19, 2011 ( http://hrsonline.isr.umich.edu/sitedocs/sampleresponse.pdf)
- House J, Landis KR, Umberson D. Social relationships and health. Science. 1988;241:540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A Short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Keysor JJ. Does late-life physical activity or exercise prevent or minimize disablement?: A critical review of the scientific evidence. American Journal of Preventive Medicine. 2003;25(3):129–136. doi: 10.1016/s0749-3797(03)00176-4. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Garner W, Speicher C, Penn GM, Holliday J, Glaser R. Psychosocial modifiers of immunocompetence in medical students. Psychosomatic Medicine. 1984;46:7–14. doi: 10.1097/00006842-198401000-00003. [DOI] [PubMed] [Google Scholar]
- Lee Y, Park K-h. Health practices that predict recovery from functional limitations in older adults. American Journal of Preventive Medicine. 2006;31(1):25–31. doi: 10.1016/j.amepre.2006.03.018. [DOI] [PubMed] [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;1(2):130–149. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Los Angeles, CA: Muthén and Muthén; 1998–2007. [Google Scholar]
- Netuveli G, Wiggins RD, Montgomery SM, Hildon Z, Blane D. Mental health and resilience at older ages: Bouncing back after adversity in the British Household Panel Survey. Journal of Epidemiology and Community Health. 2008;62(11):987–991. doi: 10.1136/jech.2007.069138. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Ahrens C. Age differences and similarities in the correlates of depressive symptoms. Psychology and Aging. 2002;17:116–124. doi: 10.1037//0882-7974.17.1.116. [DOI] [PubMed] [Google Scholar]
- Nummela O, Seppänen M, Uutela A. The effect of loneliness and change in loneliness on self-rated health (SRH): A longitudinal study among aging people. Archives of Gerontology and Geriatrics. 2011;53:163–167. doi: 10.1016/j.archger.2010.10.023. [DOI] [PubMed] [Google Scholar]
- Okun MA, August KJ, Rook KS, Newsom JT. Does volunteering moderate the relation between functional limitations and mortality? Social Science & Medicine. 2010;71:1662–1668. doi: 10.1016/j.socscimed.2010.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson AC, Veenstra G. Loneliness and risk of mortality: A longitudinal investigation in Alameda County, California. Social Science & Medicine. 2010;71(1):181–186. doi: 10.1016/j.socscimed.2010.03.024. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sorenson S. Risk factors for loneliness in adulthood and old age: A meta-analysis. In: Shohov SP, editor. Advances in Psychology Research. Hauppauge, NY: Nova Science; 2003. pp. 111–143. [Google Scholar]
- Preacher K, Hayes A. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Pressman SD, Cohen S, Miller GE, Barkin A, Rabin BS, Treanor JJ. Loneliness, social network size, and immune response to influenza vaccination in college freshmen. Health Psychology. 2005;24(3):297–306. doi: 10.1037/0278-6133.24.3.297. [DOI] [PubMed] [Google Scholar]
- Prieto-Flores M, Forjaz MJ, Fernandez-Mayoralas G, Rojo-Perez F, Martinez-Martin P. Factors associated with loneliness of noninstitutionalized and institutionalized older adults. Journal of Aging & Health. 2011;23:177–194. doi: 10.1177/0898264310382658. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley & Sons; 1987. [Google Scholar]
- Savikko N, Routasalo P, Tilvis RS, Strandberg TE, Pitkälä KH. Predictors and subjective causes of loneliness in an aged population. Archives of Gerontology and Geriatrics. 2005;41(3):223–233. doi: 10.1016/j.archger.2005.03.002. [DOI] [PubMed] [Google Scholar]
- Segrin C, Domschke T. Social support, loneliness, recuperative processes, and their direct and indirect effects on health. Health Communication. 2011;26:221–232. doi: 10.1080/10410236.2010.546771. [DOI] [PubMed] [Google Scholar]
- Seeman T. Health-promoting effects of friends and family on health outcomes in older adults. American Journal of Health Promotion. 2000;14:362–370. doi: 10.4278/0890-1171-14.6.362. [DOI] [PubMed] [Google Scholar]
- Shiovitz-Ezra S, Ayalon L. Situational versus chronic loneliness as risk factors for all-cause mortality. International Psychogeriatrics. 2010;22(3):455–462. doi: 10.1017/S1041610209991426. [DOI] [PubMed] [Google Scholar]
- Steffick DE. Documentation on affective functioning measures in the Health and Retirement Study. Ann Arbor: University of Michigan, Survey Research Center; 2000. [Google Scholar]
- Steptoe A, Owen N, Kunz-Ebrecht SR, Brydon L. Loneliness and neuroendocrine, cardiovascular, and inflammatory stress responses in middle-aged men and women. Psychoneuroendocrinology. 2004;29:593–611. doi: 10.1016/S0306-4530(03)00086-6. [DOI] [PubMed] [Google Scholar]
- Stephens C, Alpass F, Towers A, Stevenson B. The effects of types of social networks, perceived social support, and loneliness on the health of older people: Accounting for the social context. Journal of Aging & Health. 2011;23:887–911. doi: 10.1177/0898264311400189. [DOI] [PubMed] [Google Scholar]
- Sugisawa H, Liang J, Liu X. Social networks, social support, and mortality among older people in Japan. Journal of Gerontology: Social Sciences. 1994;49(1):S3–S13. doi: 10.1093/geronj/49.1.s3. [DOI] [PubMed] [Google Scholar]
- Tein J-Y, MacKinnon DP. Estimating mediated effects with survival data. In: Yanai H, Rikkyo AO, Shigemasu K, Kano Y, Meulman JJ, editors. New Developments on Psychometrics. Tokyo, Japan: Springer-Verlag Tokyo Inc; 2003. pp. 405–412. [Google Scholar]
- Theeke LA. Predictors of loneliness in U.S. adults over age sixty-five. Archives of Psychiatric Nursing. 2009;23(5):387–396. doi: 10.1016/j.apnu.2008.11.002. [DOI] [PubMed] [Google Scholar]
- Tilvis RS, Laitala VV, Routasalo PE, Pitkälä KH. Suffering from loneliness indicates significant mortality risk of older people. Journal of Aging Research. 2011 doi: 10.4061/2011/534781. Article ID 534781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turvey CL, Wallace RB, Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. International Psychogeriatrics. 1999;11(2):139–148. doi: 10.1017/s1041610299005694. [DOI] [PubMed] [Google Scholar]
- Victor CR, Scambler SJ, Bowling ANN, Bond J. The prevalence of, and risk factors for, loneliness in later life: A survey of older people in Great Britain. Ageing & Society. 2005;25(6):357–375. [Google Scholar]
- Walker A. Age and Attitudes: Main Results from a Eurobarometer Survey. Commission of the European Communities; 1993. [Google Scholar]
- Wang G, Zhang X, Wang K, Li Y, Shen Q, Ge X, Hang W. Loneliness among the rural older people in Anhui, China: Prevalence and associated factors. International Journal of Geriatric Psychiatry. 2011;26:1162–1168. doi: 10.1002/gps.2656. [DOI] [PubMed] [Google Scholar]
- Wei M, Russell DW, Zakalik RA. Adult attachment, social self-efficacy, self-disclosure, loneliness, and subsequent depression for freshman college students: A longitudinal study. Journal of Counseling Psychology. 2005;52(4):602–614. [Google Scholar]
- Wilson RS, Krueger KR, Arnold SE, Schneider JA, Kelly JF, Barnes LL, et al. Loneliness and risk of Alzheimer disease. Archives of General Psychiatry. 2007;64(2):234–240. doi: 10.1001/archpsyc.64.2.234. [DOI] [PubMed] [Google Scholar]
- Winship C, Radbill L. Sampling weights and regression analysis. Sociological Methods & Research. 1994;23(2):230–257. [Google Scholar]
- Wothke W. Longitudinal and multi-group modeling with missing data. In: Little TD, Schnabel KU, Baumert J, editors. Modeling longitudinal and multiple group data: Practical issues, applied approaches and specific examples. Mahwah, NJ: Lawrence Erlbaum Publishers; 1998. [Google Scholar]
- Yang K, Victor CR. The prevalence of and risk factors for loneliness among older adults in China. Ageing and Society. 2008;28:305–327. [Google Scholar]