Abstract
The inhalation of reactive gases and vapors can lead to severe damage of the airways and lung, compromising the function of the respiratory system. Exposures to oxidizing, electrophilic, acidic, or basic gases frequently occur in occupational and ambient environments. Corrosive gases and vapors such as chlorine, phosgene, and chloropicrin were used as warfare agents and in terrorist acts. Chemical airway exposures are detected by the olfactory, gustatory, and nociceptive sensory systems that initiate protective physiological and behavioral responses. This review focuses on the role of airway nociceptive sensory neurons in chemical sensing and discusses the recent discovery of neuronal receptors for reactive chemicals. Using physiological, imaging, and genetic approaches, Transient Receptor Potential (TRP) ion channels in sensory neurons were shown to respond to a wide range of noxious chemical stimuli, initiating pain, respiratory depression, cough, glandular secretions, and other protective responses. TRPA1, a TRP ion channel expressed in chemosensory C-fibers, is activated by almost all oxidizing and electrophilic chemicals, including chlorine, acrolein, tear gas agents, and methyl isocyanate, the highly noxious chemical released in the Bhopal disaster. Chemicals likely activate TRPA1 through covalent protein modification. Animal studies using TRPA1 antagonists or TRPA1-deficient mice confirmed the role of TRPA1 in chemically induced respiratory reflexes, pain, and inflammation in vivo. New research shows that sensory neurons are not merely passive sensors of chemical exposures. Sensory channels such as TRPA1 are essential for maintenance of airway inflammation in asthma and may contribute to the progression of airway injury following high-level chemical exposures.
Keywords: chemosensation TRPA1 channel, irritants, airway obstruction, chemical injury
Toxic inhalation hazards (TIHs) are noxious gases and vapors that are harmful and often deadly when inhaled. Specific sensory receptors in the airways sense the presence of these chemicals and initiate conscious, involuntary, autonomic, inflammatory, and other responses to them (1). Some inhaled toxicants have their primary actions in tissues outside of the lungs or hinder oxygen from reaching the alveolar sacs. Usually the only noticeable sensations by these toxicants are their smell and taste, or they are not detected at all and are only recognizable by the signs and symptoms of their toxicity (2). Most TIHs are reactive chemical gases and vapors that can severely change the structures of the proteins, lipids, DNA, and other biomolecules, resulting in a loss of protein function, DNA mutations, and necrosis of airway epithelial cells (3, 4). The body defends itself against these “reactive-TIHs” with the tissue barriers presented by hair, skin, and mucous membranes, as well as by extracellular fibers, fluids, membrane, cytosolic components, and glandular secretions containing high concentrations of antioxidants, buffers, and other compounds that sequester and neutralize reactive chemicals. These include uric acid, glutathione, ascorbic acid, carotenes, lipoic acid, tocopherol, ubiquinol, ammonia, carbonic acid, phosphate, and enzymes. In certain incidences these enzymes produce more toxic metabolites (5–7). In severe exposures these protective chemicals are saturated and the reactive chemicals react with lung tissues, damaging lung and its delicate alveolar sacs (8). The airways have specialized mechanisms to protect alveoli from damage. The peripheral sensory neurons of the airways express specific acid-sensitive ion channel (ASIC) and TRP cation channels that are directly activated by reactive chemicals. The activation of these ion channels triggers signaling to the brain to perceive pain and to initiate involuntary, autonomic and motor reflexes of the glands and muscles of the airways and lungs (9–14). The activated channels also induce the sensory neuronal peripheral endings to release proinflammatory factors near the site of contact with the reactive TIH (15).
At trace levels, the reactive TIHs are perceived as pungent and irritating, and induce sneezing, coughing, mucus secretion, upper airway inflammation, and tearing. At higher levels, these sensory neuron–mediated sensations and responses progress to incapacitating pain, uncontrollable coughing, profuse lacrimation, and resistance to airflow by bronchospasm, mucus hypersecretion, and upper and lower airway inflammation (pneumonitis) (10, 16–21). These responses neutralize, hinder, and expel toxic materials, limiting damage to the delicate alveolar sacs. However, continued exposures can lead to exaggerated responses that compromise respiratory function (20, 22). Reactive TIHs can compound pre-existing conditions. For example, they are notorious for triggering attacks in individuals with asthma (irritant-induced asthma) (23). The continual respiratory responses might be involved in the development of chronic airway diseases, including bronchitis and occupational asthma, and reactive airway dysfunction syndrome (20–22, 24–29). Exaggerated sensory neuronal responses may contribute to the pulmonary edema and adult respiratory distress syndrome (ARDS) seen with high concentration exposure of TIHs (30, 31). Therefore, not only must the airways be able to immediately detect the presence of reactive TIHs and initiate the appropriate responses to prevent exposure to the alveolar sacs, they must also deactivate this in a controlled manner to allow for normal breathing and blood flow to occur once the threat has disappeared.
Injury and inflammation alter sensory neurons to become hyperactive or hypersensitive to noxious stimuli. This phenomenon has been thoroughly characterized in pain conditions such as migraine and chronic inflammatory or neuropathic pain. It would seem likely that similar mechanisms occur in the airway sensory innervation (32–34). The necrotic and damaged cells of the airway epithelium release signaling molecules, such as DNA, ATP, adenosine, uric acid, other small molecules, peptides, peptidase products, lipids, and lipid-oxidation products. These molecules act as warning signals to the nearby tissues, and initiate and modulate inflammatory responses by the surrounding cells, especially the front line immune cells (4). These signaling molecules, cytokines, and other inflammatory mediators released during an airway injury modulate the sensitivity and expression of sensory neuronal TIH receptors (35, 36) (see Table 2 for TRPA1 modulators). This could result in chronic or hypersensitive neurogenic inflammatory responses in the lungs and airways and possibly lead to chronic inflammatory lung diseases or hypersensitivity conditions (37).
TABLE 2.
TOXIC INHALATION HAZARDS ACTIVATING THE SENSORY NEURONAL ION CHANNEL TRPA1.
| Type of Chemical | Toxicant | Sensory Neuron | Ex Vivo, In Vivo Experiments | Trpa1−/− Antag | Ref. No. |
|---|---|---|---|---|---|
| Allergen | Ovalbumin | MeCh Resistence | Both | (97) | |
| Corrosive gas | Ammonium chloride | DRG | Pain | Trpa1−/− | (93) |
| Electrophile | Oximes | AP18 | (104) | ||
| Electrophile | Trans-2-pentenal | TG | Trpa1−/− | (105) | |
| Electrophile | Toluene diisocyanate | TG | Plethysmography | Trpa1−/− | (106) |
| Electrophile | Methyl isocyanate | DRG | Trpa1−/− | (86) | |
| Electrophile | Hexamethylene diisocyanate | DRG | Pain | Both | (86) |
| Electrophile | Benzyl bromide | DRG | (86) | ||
| Electrophile | Bromoacetone | DRG | Pain | Trpa1−/− | (86) |
| Electrophile | Crotonaldehyde | JG | Bronchus | Both | (95) |
| Electrophile | Acrolein | JG, TG | Bronchus, pain, heat | Both | (95, 107) |
| Electrophile | Allylisothiocyanate | DRG, TG | Pain, artery | Both | (108) |
| Electrophile | Methylvinylketone | (109) | |||
| Electrophile | Methacrolein | (109) | |||
| Electrophile tear gas | Chloroacetophenone | DRG | Pain | Both | (85, 86) |
| Electrophile tear gas | Chlorobenzalmalononitrile | DRG | Pain | Both | (85, 86) |
| Electrophile tear gas | Dibenzoxazepine | DRG | Pain | Both | (85, 86) |
| Electrophile fumigant | Chloropicrin | (86) | |||
| Electrophile air pollutant | Cigarette smoke extract | JG | Bronchus | Both | (95) |
| Aldehyde | Acetaldehyde | TG | Pain | Camphor | (110) |
| Aldehyde | Formalin | DRG | Pain | HC | (101) |
| Halide amine | Iodoacetamide | (88) | |||
| Oxidant | Ozone | Vagal gang | Lung | Trpa1−/− | (111) |
| Oxidant | Chlorine | DRG/TG | Plethysmography | Trpa1−/− | (84) |
| Oxidant | Hydrogen peroxide | DRG/TG | Plethys/pain | Trpa1−/− | (84, 112, 113) |
| Modulator | Substance P | Scratching | (114) | ||
| Modulator | Nitric oxide | DRG | Pain, heat | Trpa1−/− | (115, 116) |
| Modulator | GDGF and BDGF | DRG | (117) | ||
| Modulator | Bradykinin | Vagal/nodose | Esophy nerve | Trpa1−/− | (11, 96, 107) |
| Modulator | Ca2+ intracellular | (12, 13, 118) | |||
| Modulator | Enzyme/PAR2 | DRG | (14) | ||
| Modulator | NGF | TG | (119) | ||
| Modulator | Artemin | DRG | (120) |
Definition of abbreviations: BDGF = brain-derived growth factor; DRG = dorsal root ganglia; GDGF = glioma-derived growth factor; JG = jugular ganglia; TG = trigeminal ganglia.
This table displays the various toxic inhalation hazards found to activate the sensory neuron ion channel, TRPA1. The first column is for the chemistry of the toxicant, the next is the toxicant identified to be a TRPA1 agonist, followed by sensory neurons studied, how the effect of the toxicant on this channel was examined in vivo and ex vivo, and whether TRPA1 was involvement in the responses with an antagonist to TRPA1 or mutant mice lacking a functional trpa1 gene. The last column provides a reference for the study that made these findings.
Currently, the therapy for acute exposures to reactive TIHs is their removal by dilution, washing, and chemical neutralization, the treatment of pain and inflammation with anti-inflammatory medications and analgesics, and stabilization of the airways with bronchodilators (38). Morbidity from high-level exposures to reactive TIHs can occur after the initial structural damage. Sensory neuron–mediated inflammation may have role in pulmonary edema, pneumonitis, and other complications of ARDS implicated in fatalities from high-level exposures (30). Occupational asthma can develop from reactive TIH exposure in workplace settings, and this is usually treated by counteracting the symptoms of airway inflammation and smooth muscle constriction. Antagonists blocking TIH receptors and or modulators of these receptors may provide novel therapeutics to alleviate the irritation and inflammation resulting from acute exposures. This may in turn abate the inflammation and pulmonary edema caused by high-level exposures and treat the chronic lung and airway diseases associated with reactive chemical inhalation.
INTRODUCTION OF TOXIC INHALATION HAZARDS
Noxious gases and other inhalation toxins are widely used and produced in the modern industrial world. The ease and low cost of manufacturing of these chemicals, plus their high toxicity and relatively short half-life, make them very beneficial as fumigants, nematicides, fungicides, disinfectants, and sanitizers in agriculture, pest control, disinfection, cleaning, and water purification industries. Many TIHs are important reactants in metallurgy and in the organic synthesis of plastics, pharmaceuticals, semiconductors, and other materials. Copious amounts of chlorine gas and other TIHs are used for bleaching and chemical synthesis, and large quantities of ammonia and nitric acid are used for fertilizer production (2, 39). TIHs are created as by-products of water purification, metal smelting, and combustion, as well as by the interaction of combustion by-products with ultraviolet light and oxygen in the air or water (40). This includes oxides and other toxins produced in welding and numerous other air pollutants from industry, automobiles, smelters, forest fires, cigarette smoke, and volcanoes (2).Workers in industrial, custodial, agricultural, and other occupations with low but frequent exposures to reactive TIHs, as well as welders, smokers, and people in areas of frequent air pollution, often suffer from the chronic airway and lung diseases (41–43).
To maintain a supply for their use, large volumes of TIHs are transported and stored, sometimes near large population centers. Unfortunately, accidental leaks from industrial facilities and transportation vehicles do occur. The resulting high-concentration exposures to TIH have caused immediate large-scale evacuations, fatalities, and severe injuries of the lungs and other tissues in the survivors (44). The most infamous accident involving TIHs was the tragedy of Bhopal, India, where thousands of residents died from exposure to methyl isocyanate (45). High exposures of TIHs were used in chemical warfare, especially in World War I, and have since been outlawed by international treaties. Unfortunately, rogue military regimes and terrorists have used gaseous warfare agents to attack and indiscriminately kill and injure civilian populations (46, 47).
Expectantly, state, federal, and international law and agencies tightly regulate the use, storage, transportation, emissions, and disposal of TIHs, and the exposure levels allowed in the environment and the workplace. The executive agencies of the United States concerned with these regulations have classified and described the various TIHs. This information is accessible through the Material Safety Data Sheets, the websites of the individual agencies, and the National Library of Medicine Toxicological Data Network (ToxNet) website (http://toxnet.nlm.nih.gov).
The occupational health database, Haz-Map (http://hazmap.nlm.nih.gov), within ToxNet has classified about 220 chemicals as “Toxic Gases and Vapors” (this group is not all the TIH; for instance, the database has ∼450 chemicals that can induce pneumonitis). In Table 1, these “Toxic Gases and Vapors” are loosely categorized by their chemistry and the mechanism of their toxicity (2). Category one includes chemicals that target the cholinergic systems (acetylcholine antagonists and acetylcholine esterase inhibitors). Category 2 includes chemicals that deplete or hinder oxygen from reaching the alveoli and thereby asphyxiate (simple asphyxiates). Category 3 included chemicals that target metal ions in vital enzymes, cytochrome c oxidase, hemoglobin, and other metalloproteins (cyanides, aliphatic nitriles, metalloid hydrides, and carbon monoxide). The cyanide anion is a nucleophile that readily forms nitriles. This reaction is readily reversible in biological systems for most aliphatic nitriles, thereby producing cyanide, but less reversible for aromatic nitriles (48, 49). Category 4 includes chemicals that induce severe blistering, including blistering and damage to the airways (arsines and mustard gases). Some of these vesicants are only detectable by their odor and the blistering effects do not occur until hours after exposure. Category 5 includes chemicals that react indiscriminately with most biological molecules. These can be further categorized by the type of chemical reactant (acids, corrosive gases, oxidants, reducers, electrophiles, and nucleophiles) and the type of chemical (isocyanate, halogen). Some chemicals belong to multiple subcategories, and members of a category may differ in their chemical properties but react in a manner similar to other members of the category. For example, often acid halides will produce an alkylation of a protein and a strong acid, both contributing to the toxicity. Members of the reactive chemical subcategories usually induce similar symptoms (irritation, pneumonitis, and pulmonary edema). Only a few sensory neuron ion channels are responsible for detecting most of the TIHs and initiating many of their symptoms. TIHs activate these channels by forming chemical reactions with them. Therefore, TIHs that form similar chemical reactions will activate the same channel and have similar symptoms, even if the chemical structures are different.
TABLE 1.
TOXIC INHALATION HAZARDS AND THEIR MECHANISMS OF INJURY
| Sensory Recognition |
Toxicity |
|||||||
|---|---|---|---|---|---|---|---|---|
| Toxic Gas or Vapor | No. of TIHs | Irritate | Odor | Receptor | Pneu monitis | Edema | Signs and Symptoms | Mechanism of Toxicity |
| Cholinergic toxins | 7 | No | None to fruity | M1 and M2 | No | No | Miosis (BZ opposite) | Parasympathetic |
| Simple asphyxiants | 15 | No | No | Carotid | No | No | Suffocation | Asphyxia |
| Target Fe cations | ||||||||
| Carbon monoxide | 1 | No | No | No | No | Lassitude | Binds to O2 site on hemegloblin | |
| Cyanide salts, halo-, HCN | 12 | Some | Bitter almond | Pain, lassitude | Electron transport | |||
| Aliphatic nitriles | 34 | Yes | Varies | Yes | Yes | Pain, lassitude | Electron transport | |
| Metalloid hydrides | 8 | Yes | Varies | Yes | Yes | Pain, edema, tremors | Heme, CYP, and other sites, reducers | |
| Vesicants | ||||||||
| Mustard gases (Nucleophile/ Electrophile) | 3 | No | Fish, garlic, musty | Yes | Yes | Late onset blistering | Perhaps onium ions | |
| Arsines-chemical weapons | 5 | Yes | Agreeable to nausea | Yes | Yes | Pain, vomit, blisters | ||
| Electrophiles | ||||||||
| Chloroformates and similar acid halides | 36 | Yes | Pungent | AISC TRPV1 | Yes | Yes | Pain, | Alkylation of biomolecules |
| Phosgenes | 3 | Only Oxime | Cut hay, fruity, pungent | Yes | Yes | Pain for oxime, respiratory distress | Alkylation of biomolecules | |
| Aromatic nitriles | 13 | Yes | Varies | TRPA1 | Pain | Alkylation of biomolecules | ||
| Isocyanates and O- and Cl− alkenes | 17 | Yes | Pungent | TRPA1 | Yes | Yes | Pain | Alkylation of biomolecules |
| Oxidizers | ||||||||
| Oxides, halides, halogens | 16 | Yes | Pungent | TRPA1 | Yes | Yes | Pain | Alkylation of biomolecules |
| Chlorosilanes | 11 | Yes | Pungent | Yes | Yes | Pain | Alkylation of biomolecules | |
| Nitroxides | 5 | Yes | Pungent | TRPA1 | Yes | Yes | Pain | Alkylation of biomolecules |
| Reducers | ||||||||
| Hydrazines | 3 | Yes | Fish NH4 | Yes | Hemolytic | |||
| Hydrogen sulfide and thiols (weak nucleophiles) | 4 | Yes | Rotten eggs | Yes | Yes | Vomiting | Asphyxiant | |
| Corrosive gases | 12 | Yes | Pungent | TRPA1 | React w/biomolecules | |||
| Acids/acids in H2O | 18 | Yes | Acrid | AISC TRPV1 | Yes | Yes | React w/biomolecules | |
Definition of abbreviation: TIH = toxic inhalation hazard.
The rows of the table are a loose subjugation of those chemicals considered “Toxic Gases and Vapors” by the Haz-Map (http://hazmap.nlm.nih.gov) website based on their toxicity and chemistry. The first column identifies the toxicants group, the second is the number of the almost 250 chemicals grouped into this classification, next are sensations induced (respiratory irritation and odor), followed by a column of sensory receptor proteins/systems activated by these toxicants, and the last columns are the toxic effects and symptoms.
MECHANISMS
Olfactory and Gustatory Chemoreceptors
The major sensations induced by exogenous chemicals are smell, detected by olfactory neurons; taste, detected by the taste receptor cells in the taste buds; and pungency/irritation/pain that are mediated by peripheral sensory neurons (50). Most TIHs are associated with an odor and many elicit a taste sensation, such as the sour taste of acids and the bitter taste of cyanide. In addition to being an important aspect of consciously identifying TIHs, odors and tastes may have a role in initiating peripheral physiological responses. This is probably a more important mechanism in animals with more sophisticated olfactory systems than humans, such as rodents and certain insects (51). The odors of the volatile organic sulfur compounds and some other TIHs are innately repulsive and nauseating (52). However, this repulsive sensation can desensitize with continued exposure, and toxic exposures have occurred without victims becoming aware of the presence of the sulfide compound (53). Certain TIHs have an agreeable smell and elicit no acute noxious sensations, so their avoidance behavior has to be learned. For example, the faint and agreeable odor of certain nerve gases is the only physiological mechanism to recognize them until the hypercholinergic effects occur (54). Carbon monoxide, some simple asphyxiates, and the chemical weapon quinuclidinyl benzilate (BZ) are odorless and can go undetected until victims show effects from their toxicity (2).
The chemoreceptors for odors are specific ligand-gated G protein–coupled receptors (GPCRs) on olfactory neurons that stimulate adenylate cyclase to synthesize cAMP via a G protein called Golf. Insects also express ion channel odorant receptors (55). The receptor for bitter-tasting chemicals is the GPCR TAS2Rn, which is coupled with the G protein gustducin. Interestingly, these receptors are also expressed in the motile cilia of the airway epithelium. The α-subunit of gustducin facilitates the activity of cAMP phosphodiesterase by binding inhibitory subunits and thereby decreasing intracellular cAMP levels, while the β-subunit activates PLC β2 and subsequently increases intracellular Ca2+. The rise in Ca2+ gates the monovalent TRP ion channel TRPM5. This produces a bitter taste sensation mediated by the taste buds and increases the activity of cilia to expel mucous-bound-toxin up and out of the lung (56–58).
The acidity-invoked sour sensation is not completely understood at the receptor level. It is likely due to H+ and H3O+ cations activating specific ion channels. Different acid receptor proteins have been proposed, including members of the ASICs (a sub-family of the amiloride-sensitive Na+ channels), hyperpolarization-activated cyclic nucleotide–gated K+ channels (HCNs), 2-pore domain K+ leak conductance channels, and the TRP ion channel TRPP3 and its partner PKD1L3 (59). It is possible that ASIC channels are directly activated by low pH, while TRPP3 and PKD1L3 are primed by acidity, and subsequently activated by return to physiological pH (60, 61).
Sensory Neuron Chemoreceptors
Most TIHs (80–90% of theTIHs in Haz-Map) are reactive chemicals and produce similar sensations of a pungent “burning” irritation and pain by activating chemoreceptor sensory neurons. The airway mucosal epithelium is densely innervated with projections from the peripheral nerves of the somatic sensory system, including two nerve fiber types involved in chemical nociception (62). These fibers are anatomically distinguishable from each other by their diameter and degree of myelination. A-δ fibers have a slightly larger diameter and are encased in thin myelin sheaths, while the C-fiber neurons are unmyelinated with smaller diameters. Activation of A-δ fibers nerves produces a fast, sharp pain sensation, while the slow velocity C-fiber activation induces a slow “burning” pain. In the respiratory system, these fibers correspond through the trigeminal or vagus nerve with brainstem nuclei to coordinate sensations. This results in reflexes and responses to deter further inhalation, expel toxicants by coughing and sneezing, dilute and neutralize reactive toxins by parasympathetic glandular secretions, and alter breathing patterns and other brain-mediated airway responses to reactive TIHs (10, 16–21). In rodents, TIHs activation of sensory neurons induces a decrease in respiratory rate by increasing the pause between individual breaths. This is used as a common model to measure and determine respiratory irritation by TIHs (16, 18, 63).
Reactive TIHs also induce peripheral endings of C-fiber neurons to secrete peptides and other molecules at and near the site of contact, such as Substance P (SP) and calcitonin gene-related peptide (CGRP). SP preferentially binds to the tachykinin receptor NK1 receptors, while CGRP binds to calcitonin receptor–like receptor (CRLR) coupled with the receptor activity modifying protein (RAMP1 or 3). NK1 receptors are GPCRs coupled to the Gq subunit, which actives PLC and increases intracellular Ca2+. CGRP receptors (CRLR+RAMP) are coupled to the Gs subunit, which activates adenylate cyclase, increasing intracellular cAMP. These peptide receptors show partially overlapping expression patterns. In certain instances their actions are synergistic, while in other instances they counteract each other (34, 64, 65). Extensive studies on SP and CGRP have shown that they are predominantly proinflammatory factors that increase bronchoconstriction, immune cell infiltration, vasodilation, mast cell degranulation, plasma extravasation, and other local inflammatory responses (34). The acute pneumonitis from certain reactive TIHs most likely has a neurogenic inflammatory component. Possibly, the pulmonary edema resulting from reactive TIH exposure also has a sensory neuronal component. Substance P and CGRP have been proposed to be involved in the pathology of allergic asthma (66, 67). Occupational asthma and reactive airway dysfunction syndrome may also have a neurogenic inflammatory component (68).
Acid Sensing: ASICs
Acidic TIHs stimulate both A-δ and C-fiber sensory neurons. This results in acidic TIH induction of a sharp, immediate pungent pain and reflex-like breath withdrawal as well as burning pain, pneumonitis, coughing, mucus secretion, and other responses (69–71). C-fibers appear to have at least two distinct electrophysiological currents sensitive to acidic pH, suggesting at least two distinct ion channel populations responding to acidic stimuli. An influx of Na+ occurs at pH levels slightly below the homeostatic level that rapidly inactivates and a mixed Ca2+/Na+ influx occurs at more acidic conditions. Various combinations of splice-variants of the three members of the ASIC (ASIC1a, ASIC1b, ASIC2a, ASIC2b, and ASIC3) family of ion channels appear to be responsible for the first currents. These channels are expressed in both A-δ and C-fiber sensory neurons and show similar electrophysiological properties in heterologous expression systems, with conducting Na+ currents induced between pH 6 and 7 that rapidly inactivate. Different combinations of subunits and splice variants of the three ASIC genes may explain the observed differences in kinetics and pH sensitivity in native neurons (59).
Acid-Sensing Ion Channels: TRPV1
At lower pH (∼5) the nonspecific cation channel TRPV1 is activated in sensory neurons (72). While the various heteromeric combinations of ASIC-mediated acid-sensitive channels are ubiquitous in both chemosensory fiber types, the splice-variant and subtype distribution of ASICs have some specificity. TRPV1-like acid-sensitive currents are primarily observed in unmyelinated C-fiber neurons (59). These currents correlate with TRPV1 expression and the currents are not observed in the sensory neurons of mice devoid of TRPV1. While TRPV1 is activated at relatively low pH, inflammatory mediators and injury signals can augment the sensitivity of TRPV1 to acidity, and acidity can in turn hypersensitize TRPV1 (73). While it is unlikely that the pH in the lung would drop low enough to activate TRPV1 during inhalation of a TIH, repeated inhalation or underlying inflammation may facilitate TRPV1 to become hypersensitive and therefore triggered by an exposure to a gaseous acid (73–80). For instance, TRPV1 is sensitized by the potent proinflammatory signal, bradykinin (81).
TRPV1 is well established to have a crucial role in the nociception of heat. It is the site of action for the active ingredient in chili peppers, capsaicin. There are symptom similarities between high-level exposures to capsaicin as pepper spray (OC tear gas) and exposures to reactive chemical TIHs. However, studies of TRPV1 gene–deleted mice still show normal irritant responses to TIHs mediated by sensory neurons (82).
Most C fibers express either TRPV1 (80–90%) or the cold activated ion channel, TRPM8 (8%). TRPM8 is sensitive to cool temperatures and is at least partially responsible for the sensation elicited by cool temperatures and by menthol and related compounds. Similar to TRPP3 and TRPM5, these proteins belong to the Transient Receptor Potential (TRP) superfamily of cation channels. TRP proteins are believed to form tetrameric cation channels in a manner similar to the voltage-gated K+ channels, with six transmembrane spans and an ion selectivity filter-pore between the fifth and the sixth span. Both the amino and carboxyl terminal spans are cytosolic. Most TRP channels conduct and are regulated by calcium ions. Predictably, their physiological functions often correlate with the dynamic roles that calcium performs in cells, organisms, and disease, especially in sensing and signaling (83).
Oxidant and Electrophile Sensing: TRPA1
TRPA1, a nonspecific cation channel expressed in 30–40% of the TRPV1-expressing C-fiber neurons, is directly activated by volatile reactive organic electrophiles or oxidative agents (∼40% TIHs on Haz-Map site shown in Table 1) (84). This has been demonstrated in vitro and in vivo in numerous publications using TRPA1-gene deleted mice or treatments with TRPA1-antagonists. Table 2 provides a relatively inclusive list of all the TIHs and related chemicals found thus far to activate TRPA1. However, TRPA1's role in the airway responses to many of these reactive chemical TIHs has yet to be characterized. The most potent and specific TRPA1 agonists characterized so far are the CS-, CR-, and CN-tear gases (riot control agents) (85, 86). These agents appear to target TRPA1 to induce their intended effects of incapacitating pain, glandular secretions, coughing, acute neurogenic inflammation, and other symptoms associated with exposures to reactive chemical TIHs.
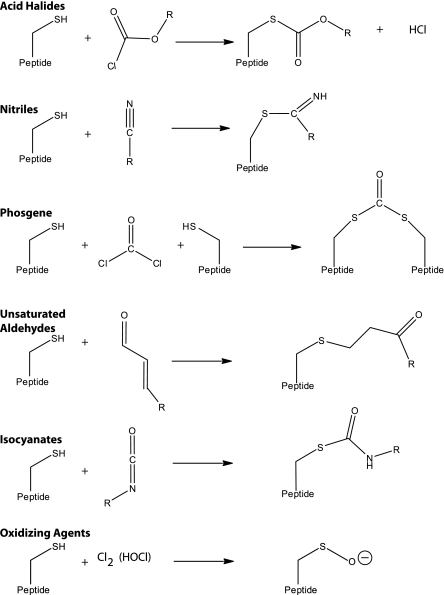
Just before the first putative transmembrane span of TRPA1 a short protein moiety is located containing three cysteine residues and a lysine residue. These amino acid residues form a “binding site” for the protein modifying TIHs. It is believed that covalent modification of these residues leads to activation of the channel, although additional residues have been shown to also be involved (87–89). Figure 1 shows the likely modification of cysteine residues by certain types of TIH molecules that are electrophiles or oxidants. As mentioned, some of these reactive organic molecules have yet to be examined for activity on TRPA1 (90–92). Most likely, if the molecule can form covalent bonds with the cysteine residues of glutathione, then it will also react with the cysteines in the “covalent modification binding site” and thereby activate TRPA1 and the C-type sensory neuron. Interestingly, ammonia also activates TRPA1, probably through alkalinization of the cytosolic spans (93).
Figure 1.
Chemical structure drawings representing the possible interaction of a cysteine at the TRPA1 “covalent modification binding site” and a toxic inhalation hazard chemical. Each of the reactions shown is with a chemical known to activate TRPA1 or that induces symptoms and effects similar to TRPA1 agonists. These chemicals tend to be electrophiles and oxidants.
Similar to many TRP channels, TRPA1 conducts both divalent and monovalent cations. TRPA1-carried cations depolarize the membrane, thereby activating voltage-gated Na+ and Ca2+ channels to propagate action potentials and consequentially signal the spinal and brainstem nerves to initiate reflexes and autonomic and other protective responses of the airways and the lungs (94). In TRPA1-deficient (Trpa1−/−) mice or mice treated with a TRPA1-antagonist, pain, neurogenic inflammation, bronchial constriction, and respiratory depression in response to reactive chemicals are absent or abated (see Table 2, second to last row). Activation of TRPA1 also results in the secretion of proinflammatory factors such as Substance P and CGRP (95). Neuronal peptide release is thought to be triggered by the influx of Ca2+ into the airway nerve ending, either directly through TRPA1 or by TRPA1-triggered voltage-gated Ca2+ channels. However, other mechanisms may be involved. About half of TRPA1's amino acid sequence is dedicated to a span of about 17 ankyrin repeat domains on the amino terminal span that may interact with signaling complexes and the vesicle release machinery.
Some of the necrotic cell–derived factors and mediators released as a consequence of chemical injury and inflammation modulate the sensitivity and activity of TRPA1 (see Table 2). Hyperactive or hypersensitive TRPA1 channels may contribute to chronic bronchitis, occupational asthma, and other inflammatory lung diseases associated with exposures to reactive TIHs (96). TRPA1 is crucially involved in allergenic respiratory sensitivity to ovalbumin, an inducer of allergic asthma in animal models (97). These findings show that airway sensory neurons actively modulate the local immune response to allergens.
Phosgene, Ozone, and Nitrogen Dioxide
The relatively hydrophobic reactive chemicals, phosgene, ozone, and nitrogen dioxide, do not readily diffuse through the mucus and epithelium to reach underlying sensory nerve endings (2). Therefore, they are usually not detected by sensory neurons and do not trigger defensive responses, thereby permitting the toxicants to penetrate more deeply into the lungs to the delicate alveolar sacs. The inability of the chemosensory system to detect these hydrophobic TIHs may compound the damage these chemicals inflict in the respiratory system. An additional factor to their toxicity is that hydrophobic TIHs do not readily interact with the aqueous compounds in the airway fluids that sequester and neutralize reactive chemicals.
HEALTH EFFECTS OF TIHS AND COUNTERMEASURES
The TIHs can be loosely grouped into those that are reactive chemicals and those that are not. The major sensations to “nonreactive TIHs” are smell and taste or a lack of any sensation. The sense of smell is important to recognize the danger, so the appropriate protective measures can be made. In addition to having an odor/taste associated with them, most of the “reactive TIHs” activate specific receptors on the somatosensory peripheral nerves of the airways. The receptors for the “reactive TIHs” may become hyperactive, hypersensitive, or overexpressed. As summarized above, these receptors are cation channels that stimulate the sensory nerves to initiate a variety of physiological responses, including local neurogenic inflammation and reflex-mediated responses, such as bronchospasms, mucus hypersection, coughing, and central sensations such as pain. Therefore, hyperactive or hypersensitive channels may cause continuous or hypersensitive inflammation, airway resistance, coughing, and pain, and possibly contribute to chronic inflammatory lung diseases. Targeting these ion channels may not only alleviate the acute effects from exposure to a reactive TIH, but also have a role in therapy for the lung diseases and syndromes associated with reactive TIHs.
The sensory neuronal receptors for the “reactive TIHs” have been identified. Slight acidity activates ASIC Na+ channels, while stronger acidity activates TRPV1 Ca2+/Na+ conducting channels. The ASIC channel antagonist, amiloride, might be effective in treating people exposed to acidic TIHs, and more specific antagonists have been developed (98). In the last few years, the pharmaceutical industry has produced several potent TRPV1 antagonists with hopes of treating aliments such as chronic cough, chronic pain, and arthritis. However, the role of TRPV1 in heat sensitivity and its apparent function in the regulation of body core temperature caused potentially detrimental side effects (99, 100). Topical and acute applications, such as an aerosol spray of TRPV1 antagonists, may minimize these side effects, while being efficacious in treating airway irritation and inflammation. TIHs that are electrophils and oxidants activate the Ca2+/Na+ channel TRPA1. Antagonists to TRPA1 have been discovered, but are in the early phases of research and development and are currently not ready for clinical use (101–103). Rodents treated with these antagonists have shown reduced nociception and inflammatory peptide release in response to reactive TIHs (see Table 2).
Inflammatory mediators resulting from tissue injury, immune challenge, or other sources can modulate TRPA1, TRPV1, and other sensory neuron ion channels. Current therapies for reactive TIH-induced airway irritation and inflammation target these mediators, and include methyl xanthines as well as steroidal and nonsteroidal antiinflammatory drugs. Perhaps part of these medications' therapeutic effect is to diminish the modulation and facilitation of reactive TIH receptors.
Activation of TRPA1, TRPV1, AISCs, and other C-fiber ion channels can induce the release of proinflammatory peptides, such as SP and CGRP. These peptides mediate many of the sensory neuron inflammatory effects and may have a role in the asthmatic-like symptoms seen with frequent low-level exposures to TIHs. CGRP antagonists are used in treating migraine headeaches and may also prove beneficial to decrease neurogenic inflammation in the airways.
In summary, most toxic gases and vapors are detected by olfactory neurons and taste receptor cells. Those that are reactive chemicals are detected by the peripheral sensory neurons by activating TRPV1, TRPA1, or ASIC ion channels (TIH receptors). The activation of these channels induces neurogenic inflammatory and brain-mediated responses of the airways. These responses compromise breathing and can lead to disease states if they persist. The TIH receptors and the sensory neurons may be hypersensitized, leading to disorders of hypersensitive or chronic airway inflammation and cough. The channels may have a role in the pulmonary edema and other aspects of ARDS seen with high-level exposures to reactive TIHs. Therefore, targeting these channels may provide novel treatments to alleviate TIH-induced irritation, airway inflammation, disorders of chronic airway inflammation, cough, and perhaps even the ARDS seen with high-level exposure.
The research is supported by the CounterACT Program, National Institutes Of Health Office of the Director, and the National Institute of Environmental Health Sciences, Grant Numbers ES015056, ES017218, and ES015056 (to S.-E.J.).
Supported by a grants from the American Asthma Foundation Research Program (Grant 07-0212).
Conflict of Interest Statement: B.F.B. has a patent through Yale University on a method for preventing or alleviating the noxious effects resulting from toxicant exposure. S.-E.J. served as a consultant for Hydra Biosciences, Cambridge, MA ($5,001–$10,000) and served on their Advisory Board ($1,001–$5,000). He receives royalties from the University of California, San Francisco, for the Trpa1-/- mouse strain ($1,001–$5,000) and from Hydra Biosciences, Cambridge, MA for license negotiations.
References
- 1.Taylor-Clark T, Undem BJ. Transduction mechanisms in airway sensory nerves. J Appl Physiol 2006;101:950–959. [DOI] [PubMed] [Google Scholar]
- 2.Brown JA. Information on hazardous chemicals and occupational diseases.2009.
- 3.Guidotti TL. An international registry for toxic inhalation and pulmonary edema: notes from work in progress. Int Arch Occup Environ Health 1996;68:380–386. [DOI] [PubMed] [Google Scholar]
- 4.Bianchi ME. DAMPs, PAMPs and alarmins: all we need to know about danger. J Leukoc Biol 2007;81:1–5. [DOI] [PubMed] [Google Scholar]
- 5.Lin CY, Wheelock AM, Morin D, Baldwin RM, Lee MG, Taff A, Plopper C, Buckpitt A, Rohde A. Toxicity and metabolism of methylnaphthalenes: comparison with naphthalene and 1-nitronaphthalene. Toxicology 2009;260:16–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cruzan G, Bus J, Banton M, Gingell R, Carlson G. Mouse specific lung tumors from CYP2F2-mediated cytotoxic metabolism: an endpoint/toxic response where data from multiple chemicals converge to support a mode of action. Regul Toxicol Pharmacol 2009;55:205–218. [DOI] [PubMed] [Google Scholar]
- 7.Lanosa MJ, Willis DN, Jordt S, Morris JB. Role of metabolic activation and the trpa1 receptor in the sensory irritation response to styrene and naphthalene. Toxicol Sci 2010;115:589–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lang JD, McArdle PJ, O'Reilly PJ, Matalon S. Oxidant-antioxidant balance in acute lung injury. Chest 2002;122:314S–320S. [DOI] [PubMed] [Google Scholar]
- 9.Lee LY, Gu Q. Role of TRPV1 in inflammation-induced airway hypersensitivity. Curr Opin Pharmacol 2009;9:243–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bessac BF, Jordt SE. Breathtaking trp channels: TRPA1 and TRPV1 in airway chemosensation and reflex control. Physiology (Bethesda) 2008;23:360–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bandell M, Story GM, Hwang SW, Viswanath V, Eid SR, Petrus MJ, Earley TJ, Patapoutian A. Noxious cold ion channel TRPA1 is activated by pungent compounds and bradykinin. Neuron 2004;41:849–857. [DOI] [PubMed] [Google Scholar]
- 12.Doerner JF, Gisselmann G, Hatt H, Wetzel CH. Transient receptor potential channel a1 is directly gated by calcium ions. J Biol Chem 2007;282:13180–13189. [DOI] [PubMed] [Google Scholar]
- 13.Wang YY, Chang RB, Waters HN, McKemy DD, Liman ER. The nociceptor ion channel TRPA1 is potentiated and inactivated by permeating calcium ions. J Biol Chem 2008;283:32691–32703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dai Y, Wang S, Tominaga M, Yamamoto S, Fukuoka T, Higashi T, Kobayashi K, Obata K, Yamanaka H, Noguchi K. Sensitization of TRPA1 by PAR2 contributes to the sensation of inflammatory pain. J Clin Invest 2007;117:1979–1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Castranova V, Frazer DG, Manley LK, Dey RD. Pulmonary alterations associated with inhalation of occupational and environmental irritants. Int Immunopharmacol 2002;2:163–172. [DOI] [PubMed] [Google Scholar]
- 16.Alarie Y. Irritating properties of airborne materials to the upper respiratory tract. Arch Environ Health 1966;13:433–449. [DOI] [PubMed] [Google Scholar]
- 17.Hu H, Fine J, Epstein P, Kelsey K, Reynolds P, Walker B. Tear gas–harassing agent or toxic chemical weapon? JAMA 1989;262:660–663. [DOI] [PubMed] [Google Scholar]
- 18.Kuwabara Y, Alexeeff GV, Broadwin R, Salmon AG. Evaluation and application of the RD50 for determining acceptable exposure levels of airborne sensory irritants for the general public. Environ Health Perspect 2007;115:1609–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lundberg JM, Saria A. Capsaicin-induced desensitization of airway mucosa to cigarette smoke, mechanical and chemical irritants. Nature 1983;302:251–253. [DOI] [PubMed] [Google Scholar]
- 20.McLoud TC. Occupational lung disease. Radiol Clin North Am 1991;29:931–941. [PubMed] [Google Scholar]
- 21.Nowak D. Chemosensory irritation and the lung. Int Arch Occup Environ Health 2002;75:326–331. [DOI] [PubMed] [Google Scholar]
- 22.Springer J, Groneberg DA, Dinh QT, Quarcoo D, Hamelmann E, Braun-Dullaeus RC, Geppetti P, Anker SD, Fischer A. Neurokinin-1 receptor activation induces reactive oxygen species and epithelial damage in allergic airway inflammation. Clin Exp Allergy 2007;37:1788–1797. [DOI] [PubMed] [Google Scholar]
- 23.Francis HC, Prys-Picard CO, Fishwick D, Stenton C, Burge PS, Bradshaw LM, Ayres JG, Campbell SM, Niven RM. Defining and investigating occupational asthma: a consensus approach. Occup Environ Med 2007;64:361–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leikauf GD. Hazardous air pollutants and asthma. Environ Health Perspect 2002;110:505–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weisel CP. Assessing exposure to air toxics relative to asthma. Environ Health Perspect 2002;110:527–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brooks SM, Weiss MA, Bernstein IL. Reactive airways dysfunction syndrome (RADS): persistent asthma syndrome after high level irritant exposures. Chest 1985;88:376–384. [DOI] [PubMed] [Google Scholar]
- 27.Medina-Ramon M, Zock JP, Kogevinas M, Sunyer J, Torralba Y, Borrell A, Burgos F, Anto JM. Asthma, chronic bronchitis, and exposure to irritant agents in occupational domestic cleaning: a nested case-control study. Occup Environ Med 2005;62:598–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prezant DJ, Levin S, Kelly KJ, Aldrich TK. Upper and lower respiratory diseases after occupational and environmental disasters. Mt Sinai J Med 2008;75:89–100. [DOI] [PubMed] [Google Scholar]
- 29.Shakeri MS, Dick FD, Ayres JG. Which agents cause reactive airways dysfunction syndrome (RADS)? A systematic review. Occup Med (Lond) 2008;58:205–211. [DOI] [PubMed] [Google Scholar]
- 30.Lin S, Walker J, Xu L, Gozal D, Yu J. Behaviours of pulmonary sensory receptors during development of acute lung injury in the rabbit. Exp Physiol 2007;92:749–755. [DOI] [PubMed] [Google Scholar]
- 31.Dhara VR, Dhara R. The union carbide disaster in Bhopal: a review of health effects. Arch Environ Health 2002;57:391–404. [DOI] [PubMed] [Google Scholar]
- 32.Miller RJ, Jung H, Bhangoo SK, White FA. Cytokine and chemokine regulation of sensory neuron function. Handb Exp Pharmacol 2009;194:417–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Benemei S, Nicoletti P, Capone JG, De Cesaris F, Geppetti P. Migraine. Handb Exp Pharmacol 2009;194:75–89. [DOI] [PubMed] [Google Scholar]
- 34.Benemei S, Nicoletti P, Capone JG, Geppetti P. CGRP receptors in the control of pain and inflammation. Curr Opin Pharmacol 2009;9:9–14. [DOI] [PubMed] [Google Scholar]
- 35.Duan B, Wu LJ, Yu YQ, Ding Y, Jing L, Xu L, Chen J, Xu TL. Upregulation of acid-sensing ion channel ASIC1a in spinal dorsal horn neurons contributes to inflammatory pain hypersensitivity. J Neurosci 2007;27:11139–11148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Adcock JJ. TRPV1 receptors in sensitisation of cough and pain reflexes. Pulm Pharmacol Ther 2009;22:65–70. [DOI] [PubMed] [Google Scholar]
- 37.Pisi G, Olivieri D, Chetta A. The airway neurogenic inflammation: clinical and pharmacological implications. Inflamm Allergy Drug Targets 2009;8:176–181. [DOI] [PubMed] [Google Scholar]
- 38.Warden CR. Respiratory agents: irritant gases, riot control agents, incapacitants, and caustics. Crit Care Clin 2005;21:719–737. (vi.). [DOI] [PubMed] [Google Scholar]
- 39.Evans RB. Chlorine: state of the art. Lung 2005;183:151–167. [DOI] [PubMed] [Google Scholar]
- 40.Dotson A, Westerhoff P, Krasner SW. Nitrogen enriched dissolved organic matter (dom) isolates and their affinity to form emerging disinfection by-products. Water Sci Technol 2009;60:135–143. [DOI] [PubMed] [Google Scholar]
- 41.Greskevitch M, Kullman G, Bang KM, Mazurek JM. Respiratory disease in agricultural workers: mortality and morbidity statistics. J Agromedicine 2007;12:5–10. [DOI] [PubMed] [Google Scholar]
- 42.Lillienberg L, Zock JP, Kromhout H, Plana E, Jarvis D, Toren K, Kogevinas M. A population-based study on welding exposures at work and respiratory symptoms. Ann Occup Hyg 2008;52:107–115. [DOI] [PubMed] [Google Scholar]
- 43.Rushton L. Occupational causes of chronic obstructive pulmonary disease. Rev Environ Health 2007;22:195–212. [DOI] [PubMed] [Google Scholar]
- 44.Centers for Disease Control and Prevention (CDC). Public health consequences from hazardous substances acutely released during rail transit–South Carolina, 2005; selected states, 1999–2004. MMWR Morb Mortal Wkly Rep 2005;54:64–67. [PubMed] [Google Scholar]
- 45.Mehta PS, Mehta AS, Mehta SJ, Makhijani AB. Bhopal tragedy's health effects: a review of methyl isocyanate toxicity. JAMA 1990;264:2781–2787. [PubMed] [Google Scholar]
- 46.Balali-Mood M, Hefazi M. Comparison of early and late toxic effects of sulfur mustard in Iranian veterans. Basic Clin Pharmacol Toxicol 2006;99:273–282. [DOI] [PubMed] [Google Scholar]
- 47.Ala'Aldeen DAA. Death clouds: Saddam Hussein's chemical war against the Kurds 5/1/1991. (Accessed May 24, 2010.) Available from: http://www.dlawer.net/?q=node/79
- 48.Farooqui MY, Mumtaz MM. Toxicology of methacrylonitrile. Toxicology 1991;65:239–250. [DOI] [PubMed] [Google Scholar]
- 49.Kaplita PV, Smith RP. Pathways for the bioactivation of aliphatic nitriles to free cyanide in mice. Toxicol Appl Pharmacol 1986;84:533–540. [DOI] [PubMed] [Google Scholar]
- 50.Buck LB. The molecular architecture of odor and pheromone sensing in mammals. Cell 2000;100:611–618. [DOI] [PubMed] [Google Scholar]
- 51.Kaupp UB. Olfactory signalling in vertebrates and insects: differences and commonalities. Nat Rev Neurosci 2010;11:188–200. [DOI] [PubMed] [Google Scholar]
- 52.Bentley R, Chasteen TG. Environmental VOSCs–formation and degradation of dimethyl sulfide, methanethiol and related materials. Chemosphere 2004;55:291–317. [DOI] [PubMed] [Google Scholar]
- 53.Knight LD, Presnell SE. Death by sewer gas: case report of a double fatality and review of the literature. Am J Forensic Med Pathol 2005;26:181–185. [PubMed] [Google Scholar]
- 54.Yanagisawa N, Morita H, Nakajima T. Sarin experiences in Japan: acute toxicity and long-term effects. J Neurol Sci 2006;249:76–85. [DOI] [PubMed] [Google Scholar]
- 55.Sato K, Touhara K. Insect olfaction: receptors, signal transduction, and behavior. Results Probl Cell Differ 2009;47:121–138. [DOI] [PubMed] [Google Scholar]
- 56.Andres-Barquin PJ, Conte C. Molecular basis of bitter taste: the T2R family of G protein-coupled receptors. Cell Biochem Biophys 2004;41:99–112. [DOI] [PubMed] [Google Scholar]
- 57.Behrens M, Meyerhof W. Mammalian bitter taste perception. Results Probl Cell Differ 2009;47:203–220. [DOI] [PubMed] [Google Scholar]
- 58.Shah AS, Ben-Shahar Y, Moninger TO, Kline JN, Welsh MJ. Motile cilia of human airway epithelia are chemosensory. Science 2009;325:1131–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Holzer P. Acid-sensitive ion channels and receptors. Handb Exp Pharmacol 2009;194:283–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Huque T, Cowart BJ, Dankulich-Nagrudny L, Pribitkin EA, Bayley DL, Spielman AI, Feldman RS, Mackler SA, Brand JG. Sour ageusia in two individuals implicates ion channels of the ASIC and PKD families in human sour taste perception at the anterior tongue. PLoS One 2009;4:e7347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Inada H, Kawabata F, Ishimaru Y, Fushiki T, Matsunami H, Tominaga M. Off-response property of an acid-activated cation channel complex PKD113-PKD2l1. EMBO Rep 2008;9:690–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Belvisi MG. Sensory nerves and airway inflammation: role of A delta and C-fibres. Pulm Pharmacol Ther 2003;16:1–7. [DOI] [PubMed] [Google Scholar]
- 63.Morris JB, Wilkie WS, Shusterman DJ. Acute respiratory responses of the mouse to chlorine. Toxicol Sci 2005;83:380–387. [DOI] [PubMed] [Google Scholar]
- 64.Birklein F, Schmelz M. Neuropeptides, neurogenic inflammation and complex regional pain syndrome (CRPS). Neurosci Lett 2008;437:199–202. [DOI] [PubMed] [Google Scholar]
- 65.Groneberg DA, Quarcoo D, Frossard N, Fischer A. Neurogenic mechanisms in bronchial inflammatory diseases. Allergy 2004;59:1139–1152. [DOI] [PubMed] [Google Scholar]
- 66.Bozic CR, Lu B, Hopken UE, Gerard C, Gerard NP. Neurogenic amplification of immune complex inflammation. Science 1996;273:1722–1725. [DOI] [PubMed] [Google Scholar]
- 67.Aoki-Nagase T, Nagase T, Oh-Hashi Y, Shindo T, Kurihara Y, Yamaguchi Y, Yamamoto H, Tomita T, Ohga E, Nagai R, et al. Attenuation of antigen-induced airway hyperresponsiveness in CGRP-deficient mice. Am J Physiol Lung Cell Mol Physiol 2002;283:L963–L970. [DOI] [PubMed] [Google Scholar]
- 68.Meggs WJ. RADS and RUDS–the toxic induction of asthma and rhinitis. J Toxicol Clin Toxicol 1994;32:487–501. [DOI] [PubMed] [Google Scholar]
- 69.Caravati EM. Acute hydrofluoric acid exposure. Am J Emerg Med 1988;6:143–150. [DOI] [PubMed] [Google Scholar]
- 70.Lopes FD, Alvarenga GS, Quiles R, Dorna MB, Vieira JE, Dolhnikoff M, Martins MA. Pulmonary responses to tracheal or esophageal acidification in guinea pigs with airway inflammation. J Appl Physiol 2002;93:842–847. [DOI] [PubMed] [Google Scholar]
- 71.Stanek J, Symanowicz PT, Olsen JE, Gianutsos G, Morris JB. Sensory-nerve-mediated nasal vasodilatory response to inspired acetaldehyde and acetic acid vapors. Inhal Toxicol 2001;13:807–822. [DOI] [PubMed] [Google Scholar]
- 72.Tominaga M, Caterina MJ, Malmberg AB, Rosen TA, Gilbert H, Skinner K, Raumann BE, Basbaum AI, Julius D. The cloned capsaicin receptor integrates multiple pain-producing stimuli. Neuron 1998;21:531–543. [DOI] [PubMed] [Google Scholar]
- 73.Jordt SE, Tominaga M, Julius D. Acid potentiation of the capsaicin receptor determined by a key extracellular site. Proc Natl Acad Sci USA 2000;97:8134–8139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bhattacharya A, Scott BP, Nasser N, Ao H, Maher MP, Dubin AE, Swanson DM, Shankley NP, Wickenden AD, Chaplan SR. Pharmacology and antitussive efficacy of 4-(3-trifluoromethyl-pyridin-2-yl)-piperazine-1-carboxylic acid (5-trifluoromethyl-pyridin-2-yl)-amide (JNJ17203212), a transient receptor potential vanilloid 1 antagonist in guinea pigs. J Pharmacol Exp Ther 2007;323:665–674. [DOI] [PubMed] [Google Scholar]
- 75.Gu Q, Lee LY. Characterization of acid signaling in rat vagal pulmonary sensory neurons. Am J Physiol Lung Cell Mol Physiol 2006;291:L58–L65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Jia Y, McLeod RL, Wang X, Parra LE, Egan RW, Hey JA. Anandamide induces cough in conscious guinea-pigs through VR1 receptors. Br J Pharmacol 2002;137:831–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kollarik M, Undem BJ. Mechanisms of acid-induced activation of airway afferent nerve fibres in guinea-pig. J Physiol 2002;543:591–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kollarik M, Undem BJ. Activation of bronchopulmonary vagal afferent nerves with bradykinin, acid and vanilloid receptor agonists in wild-type and TRPV1−/− mice. J Physiol 2004;555:115–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Leung SY, Niimi A, Williams AS, Nath P, Blanc FX, Dinh QT, Chung KF. Inhibition of citric acid- and capsaicin-induced cough by novel TRPV-1 antagonist, V112220, in guinea-pig. Cough 2007;3:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Trevisani M, Milan A, Gatti R, Zanasi A, Harrison S, Fontana G, Morice AH, Geppetti P. Antitussive activity of iodo-resiniferatoxin in guinea pigs. Thorax 2004;59:769–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chuang HH, Prescott ED, Kong H, Shields S, Jordt SE, Basbaum AI, Chao MV, Julius D. Bradykinin and nerve growth factor release the capsaicin receptor from ptdIns(4,5)P2-mediated inhibition. Nature 2001;411:957–962. [DOI] [PubMed] [Google Scholar]
- 82.Symanowicz PT, Gianutsos G, Morris JB. Lack of role for the vanilloid receptor in response to several inspired irritant air pollutants in the c57bl/6j mouse. Neurosci Lett 2004;362:150–153. [DOI] [PubMed] [Google Scholar]
- 83.Latorre R, Zaelzer C, Brauchi S. Structure-functional intimacies of transient receptor potential channels. Q Rev Biophys 2009;42:201–246. [DOI] [PubMed] [Google Scholar]
- 84.Bessac BF, Sivula M, von Hehn CA, Escalera J, Cohn L, Jordt SE. TRPA1 is a major oxidant sensor in murine airway sensory neurons. J Clin Invest 2008;118:1899–1910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Brone B, Peeters PJ, Marrannes R, Mercken M, Nuydens R, Meert T, Gijsen HJ. Tear gasses CN, CR, and CS are potent activators of the human TRPA1 receptor. Toxicol Appl Pharmacol 2008;231:150–156. [DOI] [PubMed] [Google Scholar]
- 86.Bessac BF, Sivula M, von Hehn CA, Caceres AI, Escalera J, Jordt SE. Transient receptor potential ankyrin 1 antagonists block the noxious effects of toxic industrial isocyanates and tear gases. FASEB J 2009;23:1102–1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hinman A, Chuang HH, Bautista DM, Julius D. TRP channel activation by reversible covalent modification. Proc Natl Acad Sci USA 2006;103:19564–19568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Macpherson LJ, Dubin AE, Evans MJ, Marr F, Schultz PG, Cravatt BF, Patapoutian A. Noxious compounds activate TRPA1 ion channels through covalent modification of cysteines. Nature 2007;445:541–545. [DOI] [PubMed] [Google Scholar]
- 89.Xiao B, Dubin AE, Bursulaya B, Viswanath V, Jegla TJ, Patapoutian A. Identification of transmembrane domain 5 as a critical molecular determinant of menthol sensitivity in mammalian TRPA1 channels. J Neurosci 2008;28:9640–9651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Cai J, Bhatnagar A, Pierce WM Jr. Protein modification by acrolein: formation and stability of cysteine adducts. Chem Res Toxicol 2009;22:708–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Pearson PG, Slatter JG, Rashed MS, Han DH, Grillo MP, Baillie TA. S-(N-methylcarbamoyl)glutathione: A reactive S-linked metabolite of methyl isocyanate. Biochem Biophys Res Commun 1990;166:245–250. [DOI] [PubMed] [Google Scholar]
- 92.van Iersel ML, Ploemen JP, Lo Bello M, Federici G, van Bladeren PJ. Interactions of alpha, beta-unsaturated aldehydes and ketones with human glutathione S-transferase P1–1. Chem Biol Interact 1997;108:67–78. [DOI] [PubMed] [Google Scholar]
- 93.Fujita F, Uchida K, Moriyama T, Shima A, Shibasaki K, Inada H, Sokabe T, Tominaga M. Intracellular alkalization causes pain sensation through activation of TRPA1 in mice. J Clin Invest 2008;118:4049–4057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Birrell MA, Belvisi MG, Grace M, Sadofsky L, Faruqi S, Hele DJ, Maher SA, Freund-Michel V, Morice AH. TRPA1 agonists evoke coughing in guinea pig and human volunteers. Am J Respir Crit Care Med 2009;180:1042–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Andre E, Campi B, Materazzi S, Trevisani M, Amadesi S, Massi D, Creminon C, Vaksman N, Nassini R, Civelli M, et al. Cigarette smoke-induced neurogenic inflammation is mediated by alpha,beta-unsaturated aldehydes and the TRPA1 receptor in rodents. J Clin Invest 2008;118:2574–2582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yu S, Ouyang A. TRPA1 in bradykinin-induced mechanical hypersensitivity of vagal C fibers in guinea pig esophagus. Am J Physiol Gastrointest Liver Physiol 2009;296:G255–G265. [DOI] [PubMed] [Google Scholar]
- 97.Caceres AI, Brackmann M, Elia MD, Bessac BF, del Camino D, D'Amours M, Witek JS, Fanger CM, Chong JA, Hayward NJ, et al. A sensory neuronal ion channel essential for airway inflammation and hyperreactivity in asthma. Proc Natl Acad Sci USA 2009;106:9099–9104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Chen X, Qiu L, Li M, Durrnagel S, Orser BA, Xiong ZG, Macdonald JF. Diarylamidines: high potency inhibitors of acid-sensing ion channels. Neuropharmacology 2010;58:1045–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Takemura M, Quarcoo D, Niimi A, Dinh QT, Geppetti P, Fischer A, Chung KF, Groneberg DA. Is TRPV1 a useful target in respiratory diseases? Pulm Pharmacol Ther 2008;21:833–839. [DOI] [PubMed] [Google Scholar]
- 100.Gavva NR. Body-temperature maintenance as the predominant function of the vanilloid receptor TRPV1. Trends Pharmacol Sci 2008;29:550–557. [DOI] [PubMed] [Google Scholar]
- 101.McNamara CR, Mandel-Brehm J, Bautista DM, Siemens J, Deranian KL, Zhao M, Hayward NJ, Chong JA, Julius D, Moran MM, et al. TRPA1 mediates formalin-induced pain. Proc Natl Acad Sci USA 2007;104:13525–13530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Defalco J, Steiger D, Gustafson A, Emerling DE, Kelly MG, Duncton MA. Oxime derivatives related to ap18: Agonists and antagonists of the TRPA1 receptor. Bioorg Med Chem Lett 2010;20:276–279. [DOI] [PubMed] [Google Scholar]
- 103.Petrus M, Peier AM, Bandell M, Hwang SW, Huynh T, Olney N, Jegla T, Patapoutian A. A role of TRPA1 in mechanical hyperalgesia is revealed by pharmacological inhibition. Mol Pain 2007;3:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Defalco J, Steiger D, Gustafson A, Emerling DE, Kelly MG, Duncton MA. Oxime derivatives related to AP18: agonists and antagonists of the TRPA1 receptor. Bioorg Med Chem Lett 2010;20:276–279. [DOI] [PubMed] [Google Scholar]
- 105.Inoue T, Bryant BP. Multiple cation channels mediate increases in intracellular calcium induced by the volatile irritant, trans-2-pentenal in rat trigeminal neurons. Cell Mol Neurobiol 2010;30:35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Taylor-Clark TE, Kiros F, Carr MJ, McAlexander MA. Transient receptor potential ankyrin 1 mediates toluene diisocyanate-evoked respiratory irritation. Am J Respir Cell Mol Biol 2009;40:756–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bautista DM, Jordt SE, Nikai T, Tsuruda PR, Read AJ, Poblete J, Yamoah EN, Basbaum AI, Julius D. TRPA1 mediates the inflammatory actions of environmental irritants and proalgesic agents. Cell 2006;124:1269–1282. [DOI] [PubMed] [Google Scholar]
- 108.Jordt SE, Bautista DM, Chuang HH, McKemy DD, Zygmunt PM, Hogestatt ED, Meng ID, Julius D. Mustard oils and cannabinoids excite sensory nerve fibres through the TRP channel ANKTM1. Nature 2004;427:260–265. [DOI] [PubMed] [Google Scholar]
- 109.Escalera J, von Hehn CA, Bessac BF, Sivula M, Jordt SE. TRPA1 mediates the noxious effects of natural sesquiterpene deterrents. J Biol Chem 2008;283:24136–24144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Bang S, Kim KY, Yoo S, Kim YG, Hwang SW. Transient receptor potential a1 mediates acetaldehyde-evoked pain sensation. Eur J Neurosci 2007;26:2516–2523. [DOI] [PubMed] [Google Scholar]
- 111.Taylor-Clark TE, Undem BJ. Ozone activates airway nerves via the selective stimulation of TRPA1 ion channels. J Physiol 2010;588:423–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sawada Y, Hosokawa H, Matsumura K, Kobayashi S. Activation of transient receptor potential ankyrin 1 by hydrogen peroxide. Eur J Neurosci 2008;27:1131–1142. [DOI] [PubMed] [Google Scholar]
- 113.Andersson DA, Gentry C, Moss S, Bevan S. Transient receptor potential a1 is a sensory receptor for multiple products of oxidative stress. J Neurosci 2008;28:2485–2494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Naono-Nakayama R, Sunakawa N, Ikeda T, Nishimori T. Differential effects of substance P or hemokinin-1 on transient receptor potential channels, TRPV1, TRPA1 and TRPM8, in the rat. Neuropeptides 2010;44:57–61. [DOI] [PubMed] [Google Scholar]
- 115.Miyamoto T, Dubin AE, Petrus MJ, Patapoutian A. TRPV1 and TRPA1 mediate peripheral nitric oxide-induced nociception in mice. PLoS One 2009;4:e7596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Takahashi N, Mizuno Y, Kozai D, Yamamoto S, Kiyonaka S, Shibata T, Uchida K, Mori Y. Molecular characterization of TRPA1 channel activation by cysteine-reactive inflammatory mediators. Channels (Austin) 2008;2:287–298. [DOI] [PubMed] [Google Scholar]
- 117.Ciobanu C, Reid G, Babes A. Acute and chronic effects of neurotrophic factors BDNF and GDNF on responses mediated by thermo-sensitive TRP channels in cultured rat dorsal root ganglion neurons. Brain Res 2009;1284:54–67. [DOI] [PubMed] [Google Scholar]
- 118.Zurborg S, Yurgionas B, Jira JA, Caspani O, Heppenstall PA. Direct activation of the ion channel TRPA1 by Ca2+. Nat Neurosci 2007;10:277–279. [DOI] [PubMed] [Google Scholar]
- 119.Diogenes A, Akopian AN, Hargreaves KM. NGF up-regulates TRPA1: implications for orofacial pain. J Dent Res 2007;86:550–555. [DOI] [PubMed] [Google Scholar]
- 120.Elitt CM, McIlwrath SL, Lawson JJ, Malin SA, Molliver DC, Cornuet PK, Koerber HR, Davis BM, Albers KM. Artemin overexpression in skin enhances expression of TRPV1 and TRPA1 in cutaneous sensory neurons and leads to behavioral sensitivity to heat and cold. J Neurosci 2006;26:8578–8587. [DOI] [PMC free article] [PubMed] [Google Scholar]