Asthma is one of the most common chronic conditions affecting both children and adults, yet much remains to be learned of its etiology. This paper evolved from the extensive literature review undertaken as part of a proposal for a longitudinal birth cohort study to examine risk factors for the development of allergy and asthma in early childhood.
Although genetic predisposition is clearly evident, gene-by-environment interaction probably explains much of the international variation in prevalence rates for allergy and asthma. Environmental factors such as infections and exposure to endotoxins may be protective or may act as risk factors, depending in part on the timing of exposure in infancy and childhood. Some prenatal risk factors, including maternal smoking, have been firmly established, but diet and nutrition, stress, use of antibiotics and mode of delivery may also affect the early development of allergy and asthma. Later in childhood, putative risk factors include exposure to allergens, breastfeeding (which may initially protect and then increase the risk of sensitization), family size and structure, and sex and gender. In adulthood, recurrence of childhood asthma may be just as common as new-onset asthma, which may have an occupational basis. A better understanding of these risk factors may eventually lead to opportunities for primary prevention of asthma.
Methods
This paper arose from an extensive literature review undertaken in developing the Canadian Healthy Infant Longitudinal Development (CHILD) study, a multicentre national observational study that is currently in progress. The study, which will eventually recruit 5000 pregnant women, has the aim of determining the environmental, host, genetic and psychosocial risk factors for development of allergy and asthma in children. Although not a systematic review, the examination of epidemiologic risk factors in the development of asthma presented here began in 2004 with a search of MEDLINE, using the Medical Subject Heading (MeSH) terms “asthma,” “longitudinal” and “cohort study.” One of us (P.S.) reviewed the abstracts of all studies identified in the search, excluding those without at least one objective outcome measure and those in which the primary outcome measure was not asthma. Studies examining the same outcome measure were tabulated but not combined, since most did not consider exactly the same outcome at the same age. We then performed specific searches to fill gaps in the information gathered via the original search, specifically nutrition, sex and gender effects, and novel environmental exposures. The review was updated in July 2008.
Although the present article includes some references to adult asthma, its primary focus is the epidemiology of and risk factors for this condition in children. A more extensive summary of the literature review for the Canadian Healthy Infant Longitudinal Development study has been published elsewhere.1
Epidemiology of asthma: an overview
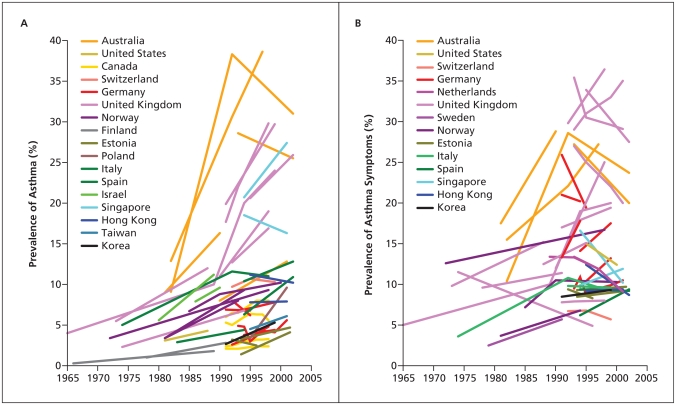
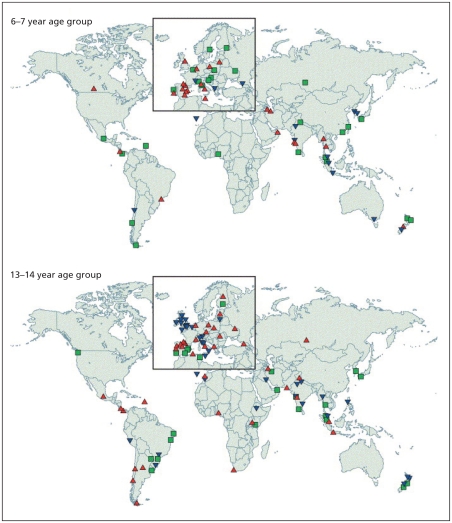
The recent substantial increase in the reported prevalence of asthma worldwide (Figure 1) has led to numerous studies of the prevalence and characteristics of this condition.2 Foremost among these are 2 major international initiatives that have collected data using validated questionnaires, one among children, the International Study of Asthma and Allergies in Childhood,3 and the other among young adults, the European Community Respiratory Health Survey.4 Follow-up investigations for both of these studies5,6 have examined temporal trends within and across populations. During a mean of 7 years following phase I of the International Study of Asthma and Allergies in Childhood, which in most participating countries was conducted between 1991 and 1993, the prevalence of asthma was stable or decreased in some areas of the world but increased substantially in many other areas, especially among children 13–14 years of age (Figure 2).5
Figure 1.
Changes in prevalence of diagnosed asthma (A) and asthma symptoms (B) over time among children and young adults. Reproduced, with permission, from Eder W, Ege MJ, von Mutius E. The asthma epidemic. N Engl J Med 2006;355:2226–35. Copyright 2006 Massachusetts Medical Society.2
Figure 2.
Annual changes in worldwide prevalence of asthma symptoms among children 6–7 years old and 13–14 years old, over a mean of 7 years following phase I of the International Study of Asthma and Allergies in Childhood (which in most participating countries was conducted between 1991 and 1993). Blue triangles identify locations where prevalence was reduced by at least 1 standard error (SE) per year, green squares identify locations where there was little change in prevalence (i.e., change of less than 1 SE per year) and red triangles identify locations where prevalence increased by at least 1 SE per year. Reproduced from The Lancet, Vol. 368, Asher MI, Montefort S, Bjorksten B, et al.; ISAAC Phase Three Study Group. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Pages 733–43, copyright 2006, with permission from Elsevier.5
Cross-sectional population-based studies such as these are highly dependent on recognition of symptoms, so they do not necessarily reflect the true heterogeneity of asthma. However, a wide variation in prevalence rates has been documented: studies of both children and adults have revealed low prevalence rates (2%–4%) in Asian countries (especially China and India) and high rates (15%–20%) in the United Kingdom, Canada, Australia, New Zealand and other developed countries.3–6
Observations of migrating populations7 and of Germany after reunification8 have strongly supported the role of local environmental factors, including allergens but likely many lifestyle factors as well, in determining the degree of expression of asthma within genetically similar populations. A recent analysis of data from the International Study of Asthma and Allergies in Childhood, comparing data from Vancouver, Canada, with data from centres in China, showed significant differences in prevalence rates between children of similar genetic ancestry living in different environments, with evidence for an effect of duration of residence in the new environment.9 Prevalence rates for asthma among children 13–14 years old were lowest for Chinese children born and studied in China, intermediate for Chinese children who had migrated during their lifetime to Canada and highest for Chinese children who had been born in Canada. In addition, the prevalence rate for the third of these groups was still lower than among non-Chinese children in the same environment. Together, these results strongly suggested gene-by-environment interactions.
Local and national studies have also provided insights into the epidemiology of exacerbations of asthma. For example, epidemics of asthma exacerbations in Barcelona, Spain, were eventually linked to exposure to atmospheric soybean dust released during cargo handling at the local port.10 The highly predictable annual epidemic of asthma exacerbations in school-age children in the northern hemisphere every September, peaking some 17 days after the return to school, appears to be predominantly driven by seasonal rhinovirus infection, probably compounded by other risk factors for asthma exacerbations, including reduction in use of asthma controller therapy over the summer months, exposure to seasonal allergens and possibly the stress of returning to school.11,12
Complementing these cross-sectional studies are longitudinal epidemiologic studies in a variety of populations and countries, which have allowed examination of risk factors predicting the development, persistence, remission or relapse of childhood asthma. One such population-based birth cohort study in Dunedin, New Zealand, which had a high retention rate, examined outcomes of childhood asthma at age 26 years.13 Female sex, airway hyperresponsiveness in mid and later childhood, and sensitization to house dust mites were all significantly and independently related to the likelihood of persistence of childhood asthma to early adulthood. Early age of onset of wheezing symptoms was predictive of relapse after remission, as were airway hyperresponsiveness and allergy to house dust mites. That study and others have clearly demonstrated the tracking of characteristics of asthma from childhood to adulthood, including severity and impairment of lung function.
Etiology of and risk factors for asthma
Asthma comprises a range of heterogeneous phenotypes that differ in presentation, etiology and pathophysiology. The risk factors for each recognized phenotype of asthma include genetic, environmental and host factors. Although a family history of asthma is common, it is neither sufficient nor necessary for the development of asthma.14
The substantial increases in the incidence of asthma over the past few decades and the geographic variation in both base prevalence rates and the magnitude of the increases support the thesis that environmental changes play a large role in the current asthma epidemic. Furthermore, environmental triggers may affect asthma differently at different times of a person’s life, and the relevant risk factors may change over time.
Short-term studies of risk factors may suggest a lower likelihood of asthma, whereas the same factors may be associated with greater risk if follow-up is more prolonged. This pattern may relate to overlap between different wheezing phenotypes in early childhood, only some of which persist as asthma in later childhood and adulthood. Because of this phenomenon, we examine here the risk factors for persistent asthma at different ages, specifically the prenatal period, infancy, childhood and, briefly, adulthood.
Genetics
Family and twin studies have indicated that genetics plays an important role in the development of asthma and allergy,15 likely through several genes of moderate effect (i.e., genes associated with relative risks in the range of 1.2–2).16,17
Genome-wide linkage studies and case–control studies have identified 18 genomic regions and more than 100 genes associated with allergy and asthma in 11 different populations. In particular, there are consistently replicated regions on the long arms of chromosomes 2, 5, 6, 12 and 13. Association studies of unrelated individuals have also identified more than 100 genes associated with allergy and asthma, 79 of which have been replicated in at least one further study.18 A recent genome-wide association study19 identified a new gene, ORMDL3, that exhibited a highly significantly association with asthma (p < 10−12) (for single nucleotide polymorphism rs8067378, odds ratio 1.84, 95% confidence interval 1.43–2.42) a finding that has now been replicated in several populations.20,21
Extensive heterogeneity in the genetic basis of asthma, and in gene-by-environment interactions, is likely. Failure to identify and precisely quantify environmental exposures and their timing may account for some of the difficulty that researchers have had in replicating genetic associations.
Prenatal risk factors
Risk factors in the prenatal period are multifactorial. Assessment is complicated by the variety of wheezing conditions that may occur in infancy and childhood, only some of which evolve to classical asthma.
Prenatal tobacco smoke
Prenatal maternal smoking has been consistently associated with early childhood wheezing,22–25 and there is a dose–response relation between exposure and decreased airway calibre in early life.26,27 Prenatal maternal smoking is also associated with increased risks of food allergy,24 cytokine responses in the cord blood28,29 and concentrations of nitric oxide in exhaled air in newborns.30 Studies have shown a clear prenatal effect of smoking; this effect is increased when combined with postnatal smoke exposure.
Diet and nutrition
Observational studies examining prenatal nutrient levels or dietary interventions and the subsequent development of atopic disease have focused on foods with anti-inflammatory properties (e.g., omega-3 fatty acids) and antioxidants such as vitamin E and zinc. Several studies have demonstrated that higher intake of fish or fish oil during pregnancy is associated with lower risk of atopic disease (specifically eczema and atopic wheeze) up to age 6 years.31–33 Similarly, higher prenatal vitamin E and zinc levels have been associated with lower risk of development of wheeze up to age 5 years.34–36 However, no protective effect against the development of atopic disease in infants has been shown for maternal diets that excluded certain foods (e.g., cow’s milk, eggs) during pregnancy.37–40 The authors of 2 recent studies41,42 reported an inverse relation of maternal vitamin D levels with wheeze in early life, but no relation with atopy or symptoms in later life.
Stress
A number of animal models have suggested that prenatal maternal stress acts through regulation of the offspring’s hypothalamic–pituitary–adrenal axis to decrease cortisol levels, which may affect the development of an allergic phenotype. Although there is a correlation between caregiver stress early in the infant’s life and higher levels of immunoglobulin E in the infant43–45 and early wheezing,46 no studies to date have shown an association with asthma.47,48
Antibiotic use
The association between prenatal antibiotic treatment and subsequent development of atopic disease has been examined in 2 ways: with treatment as a dichotomous predictor (i.e., any antibiotic use) and by number of courses of antibiotics during pregnancy. Longitudinal cohort studies examining any antibiotic use showed a greater risk of persistent wheeze and asthma in early childhood49,50 and a dose–response relation between number of antibiotic courses and risk of wheeze or asthma.49,51
Mode of delivery
Development of atopy was 2 to 3 times more likely among infants delivered by emergency cesarean section,29,52–56 although no such association occurred with elective cesarean section.29,52,53,56–59 Potential reasons for these findings include maternal stress and differences in the infant’s gut microflora associated with different modes of delivery.
Risk factors in childhood
Phenotypes of asthma
Although some 50% of preschool children have wheezing, only 10%–15% have a diagnosis of “true” asthma by the time they reach school age.13,60 Commonly described phenotypes in early infancy and childhood are transient wheezing, nonatopic wheezing, late-onset wheezing and persistent wheezing.61 Only transient wheezing in early infancy has been well characterized, with decreased airflow rates on pulmonary function testing at birth,56,60,62 onset of wheezing within the first year and resolution by mid-childhood with no lasting effects on pulmonary function.
The other 3 phenotypes have been described primarily by age of onset in cohort studies, and their genesis in early infancy is largely unknown. The majority of children with persistent wheezing (in whom asthma will subsequently be diagnosed) experience their first symptoms before age 3. By 3 years, they have abnormal lung function that persists to adulthood,13,60,61 and by adolescence, most have atopy. Of children with nonatopic and late-onset wheezing, some experience remission, whereas others experience persistent symptoms and atopy.63
Distinguishing among these different phenotypes in early childhood is critical to understanding the role of risk factors and their timing in early infancy.
Breastfeeding
The influence of breastfeeding on the risk of childhood atopy and asthma remains controversial. The following represents observational data accumulated to date. Some studies have shown protection,64–66 whereas others have reported higher rates of allergy and asthma among breastfed children.67,68 A meta-analysis69 and several individual studies66,70 showed that exclusive breastfeeding for at least 3 months was associated with lower rates of asthma between 2 and 5 years of age, with the greatest effect occurring among those with a parental history of atopy. One of the difficulties in interpreting these data lies in differentiating viral-associated wheeze in childhood from development of atopic asthma. In a longitudinal birth cohort study, breastfeeding was associated with a higher risk of atopic asthma in later childhood, with the greatest in fluence occurring among those with a maternal history of atopy.67,68,71
The influence of avoiding nutritional allergens during breastfeeding is also controversial. In some studies, exclusion of milk, eggs and fish from the maternal diet was associated with decreased atopic dermatitis in infancy,72,73 but other studies found no association.40,74,75 Studies following children to 4 years of age have demonstrated no effect of maternal dietary restriction during lactation on the subsequent development of atopic diseases, including asthma.76
Lung function
Decreased airway calibre in infancy has been reported as a risk factor for transient wheezing,60 perhaps related to prenatal and postnatal exposure to environmental tobacco smoke.26,27 Furthermore, the presence of airways with decreased calibre has been associated with increased bronchial responsiveness and increased symptoms of wheeze.26 Several studies have suggested an association between reduced airway function in the first few weeks of life and asthma in later life.62,77 The magnitude of the effect of this risk factor in isolation (i.e., without concomitant allergy) is unclear; perhaps individuals with smaller airways require less stimulus (i.e., airway inflammation) before symptoms become apparent.
Children with wheezing (and diagnosed asthma) persisting to adulthood have a fixed decrement in lung function as early as age 7 or 9 years.13,78 Recent studies of preschool children have documented abnormal lung function in children with persistent wheezing as young as age 3 years.61 However, some infants in whom persistent wheezing develops have normal lung function shortly after birth, which suggests a critical period of exposures within the first few years of life, before the development of these persistent abnormalities in expiratory flows.60,79 In contrast, infants who exhibit early transient wheezing have decreased airflow shortly after birth.60,80 Maternal smoking with in utero nicotine exposure has been correlated with this type of lung dysfunction,26,27,60 but the effects of other exposures have been less well studied.
Family structure
Family size and the number and order of siblings may affect the risk of development of asthma. The hygiene hypothesis posits that exposure of an infant to a substantial number of infections and many types of bacteria stimulates the developing immune system toward nonasthmatic phenotypes.81,82 This may be exemplified in the real world by large family size, whereby later-born children in large families would be expected to be at lower risk of asthma than first-born children, because of exposure to their older siblings’ infections.
Although this theory has been supported by some studies of allergy prevalence,83,84 it has been partially refuted by recent studies of asthma prevalence suggesting that although large family size (more than 4 children) is associated with a decreased risk of asthma, birth order is not involved.85,86 Furthermore, doubt has been cast on simplistic renditions of this hypothesis, in that infections per se cannot explain some epidemiologic patterns (e.g., prevalence rates for allergy and asthma are high in some South American countries, where exposures to infection are higher than in some countries with lower rates of asthma3). In addition, not only allergic but also autoimmune and other chronic inflammatory diseases are increasing,87 a trend that is difficult to explain by the hygiene hypothesis alone, since allergic and autoimmune diseases are associated with competing immunologic phenotypes.
Socio-economic status
Children of parents with lower socio-economic status have greater morbidity from asthma,88–92 but findings with respect to the prevalence of asthma are mixed.93–97 Such results may depend both on how socio-economic status is measured and on the specific outcome examined. Some studies have reported associations of lower socio-economic status with greater airway obstruction and symptoms but not with a diagnosis of asthma.91,92 Whether socio-economic status is as relevant to the incidence of allergy and asthma as it is to the expression, severity and management of these diseases re mains unclear. Parental stress has also been prospectively associated with wheezing in infancy,46 and family difficulties have been linked to asthma.48,98 Children whose caregivers report high levels of stress and who have difficulties parenting are at greatest risk for asthma.99
Antibiotics and infections
The use of antibiotics has been associated with early wheezing and asthma in several studies,47,100,101 One suggested mechanism for this association is immunologic stimulation through changes in the bowel flora, but Kummeling and associates100 found no coincident increase in eczema or atopy, despite increased wheezing rates, which would argue against this mechanism. Greater antibiotic use might also represent a surrogate marker for a higher numbers of infections (perhaps viral) in early life.
Viral infections of the lower respiratory tract affect early childhood wheezing. Whether lower respiratory tract infection promotes sensitization to aeroallergens causing persistent asthma is controversial: childhood viral infections might be pathogenic in some children but protective in others.102–106 Infants of mothers with allergy or asthma have a relatively persistent maturational defect in Th1 cytokine synthesis in the first year of life, which may play a role in the development of persistent or severe viral infections.107 Severe viral infection of the lower respiratory tract in genetically susceptible infants who are already sensitized to inhalant allergens may lead to deviation toward Th2 responses promoting asthma. It is unclear whether these effects of lower respiratory tract infection are virus-specific (e.g., respiratory syncytial virus, rhinovirus) or whether synergistic exposures to allergens can induce asthma even in individuals who are not genetically susceptible. Interactions of genes with environmental exposures (including allergens, air pollution, environmental tobacco smoke and diet) modulate the host response to infections.108,109 It remains controversial whether the occurrence or timing of childhood infection is pathogenic or protective for the development and long-term outcome of asthma and allergy and of nonallergic wheeze phenotypes. This controversy relates in part to small sample size, cross-sectional analysis, lack of precise case definition and incomplete microbial assessment in studies of this phenomenon.110,111
Respiratory infections in early childhood are associated with early wheezing,109 but it is unclear whether infection alone has a role in the development of persistent asthma. Repeated lower respiratory tract infection may affect infants who are already at risk for asthma because of family history or atopy.63,112 Severe infection with certain viruses such as respiratory syncytial virus106 and rhinovirus113 may play a role in persistent wheezing, although other studies have suggested no effect.114 Considered as a proxy for viral infections, daycare attendance is associated with greater incidence of early wheeze but lower incidence of persistent wheeze.115
Allergic sensitization
Total serum immunoglobulin E level, a surrogate for allergen sensitivity, has been associated with the incidence of asthma.116 High levels of immunoglobulin E at birth were associated with greater incidence of both atopy117–119 and aeroallergen sensitivity but not necessarily asthma. However, sensitization to aeroallergens, particularly house dust mite, cat and cockroach allergens, is well documented as being associated with asthma.
Immune responses in the developing infant and young child may affect the development of asthma. For example, impairment in interferon γ production at 3 months was associated with a greater risk of wheeze.115 Immaturity in neonatal immune responses may promote the persistence of the Th2 immune phenotype and development of atopy,120 but an association with persistent asthma is as yet unproven. More recent work has focused on the role of the innate immune system in handling and presentation of antigens and suggests that polymorphisms in Toll-like receptors121,122 may play a greater role than previously recognized in the development of the skewed immune responses associated with persistent asthma.
Exposure to environmental tobacco smoke
Postnatal exposure to environmental tobacco smoke, especially from maternal smoking, has been consistently associated with respiratory symptoms of wheezing.22,26,56 Exposure to environmental tobacco smoke also consistently worsens asthma symptoms and is a risk factor for severe asthma.123,124
Exposure to animals
Although several studies have demonstrated a lower risk of development of atopy and asthma with exposure to farm animals in early life, the findings of studies of the influence of exposure to domestic cats and dogs have been inconsistent.125,126 In some studies, exposure to cats was associated with a greater risk of allergic sensitization,127 whereas other studies showed a lower risk.128,129 Exposure to dogs may be protective not only against the development of specific sensitization to dog allergen127,128 but also against other sensitization (e.g., to house dust mites) and asthma. Other studies of exposure to dogs have suggested that protection against wheezing may be mediated by high levels of endotoxin.130
Gene-by-environment interactions
The effects of gene-by-environment interactions in asthma are complex. In some cases the genes code for enzymes that detoxify inhaled agents (e.g., glutathione transferase genes and environmental pollution), whereas in other cases, the exposures may have a more direct effect on gene expression via epigenetic mechanisms, such as DNA methylation or histone modification. Epigenetic modification of DNA is believed to be responsible for the phenotypic differences that develop over time between monozygotic twins.131 It has been suggested that it is principally through epigenetic modification of DNA that lifestyle and chemical exposures affect susceptibility to diseases.132 Nutrition and diet (e.g., folic acid, vitamin B12), smoking, exposure to microbial products, maternal stress and maternal care are potential factors influencing fetal genetic expression, and a further window for epigenetic modification in early life may allow environmental factors to modify a child’s genome with the potential to cause or prolong allergy and asthma. Further work is needed to verify and understand these risks.
Sex and gender
Sex affects the development of asthma in a time-dependent manner. Until age 13–14 years, the incidence and prevalence of asthma are greater among boys than among girls.133–142 Studies through puberty139,143–155 have shown a greater incidence of asthma among adolescent and young adult females133–135,156,157 and a greater proportion of males with remission of asthma.136–140 Before age 12, boys have more severe asthma than girls,142 with higher rates of admission to hospital.158–165 In contrast, adult females have more severe asthma than males, with more hospital admissions,161,166,167 slower improvement,120 longer hospital stays161 and higher rates of readmission.168 Most authors have attributed these changes in prevalence and severity to events of puberty,140,141 although mechanisms for differences between the sexes have not been established.
In childhood, airway hyperresponsiveness is more common and more severe among males;169 however, airway hyperresponsiveness increases in females during adolescence,170,171 such that by adulthood it is both more common and more severe among adult women.154,155,172–174 Similar findings have been reported from studies of atopy, which is more common in males before age 13;175 during adolescence, the rate of new-onset atopy is higher among females,176,177 so that by young adulthood the prevalence of atopy is almost equal.
The influence of some environmental risk factors such as allergens may be modified by sex. In one study of adults, 18% of women with asthma, but only 2.3% of men with asthma, had normal results on common tests related to atopy (negative skin prick tests, immunoglobulin E < 100 IU/mL and eosinophilia < 5%),178 which suggested different disease mechanisms between the sexes. Interactions have been found between maternal and paternal history of atopy, breastfeeding and sex of the child in terms of the risk of asthma and atopy.71 Finally, the influence of obesity on the development of asthma is greater among women than among men and has not been shown to be influenced by caloric intake or physical activity.179,180 Some have suggested that the relation between obesity and asthma may be causal, given the consistency, temporal association and dose–response relationships reported in the epidemiologic literature, but the mechanisms remain to be elucidated.181
Adult-onset asthma
Asthma in adults may have persisted from childhood, may have occurred as a relapse of earlier childhood asthma (whether or not recalled by the individual) or may be true adult-onset asthma with no symptoms in earlier life.182–184 New-onset asthma in adulthood may have environmental (especially occupational) causes with or without allergen sensitization.185–187 Although adult asthma may develop in relation to specific drug treatments (e.g., β-blockers, nonsteroidal anti-inflammatory drugs) or, in women, the use of hormone replacement therapy,188 occupational exposure to sensitizing agents or irritants is more common.
Occupational asthma
Asthma related to workplace exposures has been documented in many occupational settings. Commonly associated occupations and exposures include car painting (isocyanates), hairdressing (various chemicals), domestic and commercial cleaning (cleaning solutions), health care professions (latex) and baking (flour dust), among many others.189
The relation between exposure to substances in the work-place and new-onset adult asthma was explored among 6837 participants with no previously reported asthma symptoms in phase I of the European Community Respiratory Health Study.187 Exposure to substances known to cause occupational asthma was associated with a higher risk of asthma overall (relative risk [RR] 1.6, 95% confidence interval [CI] 1.1–2.3) and of asthma defined by airway hyperresponsiveness (RR 2.4, 95% CI 1.3–4.6). Of common occupations, nursing was associated with the highest risk of occupational asthma (RR 2.2, 95% CI 1.3–4.0, p = 0.007), whereas exposure to an acute inhalation event, such as fire, mixing of cleaning agents or a chemical spill, was associated with an even higher risk (RR 3.3, 95% CI 1.0–11.1, p = 0.05). The population attributable risk of occupational exposure for adult asthma in that study ranged from 10% to 25%.
Other risk factors for adult asthma
Smoking tobacco190 or marijuana191,192 may give rise to symptoms suggesting asthma, although symptoms of cough and sputum production, suggesting chronic bronchitis, are more common. As in childhood, the differential diagnosis should include other forms of airway inflammation and other causes of intermittent dyspnea and wheezing, such as cardiac failure. However, new-onset asthma can occur at any age, without prior illness or concomitant disease. Atopy as a risk factor for asthma is less common with increasing age,193 but occasionally it is the dominant trigger. Air pollution may affect adult asthma, but more often it is a factor worsening pre-existing asthma rather than a cause of incident asthma.194–196
Conclusions
Many cross-sectional studies have confirmed increases in the incidence and prevalence of asthma over the past 2 to 3 decades, but much remains unknown as to the fundamental immunologic, genetic and environmental mechanisms underlying the development of this condition and its increased expression, especially in the developed world. Nonetheless, some risk factors have now been clearly and consistently identified. For instance, avoidance of maternal smoking in pregnancy and in the early postpartum period can be strongly encouraged, as can avoidance of known occupational sensitizers. In contrast, previous advice to avoid animals and to breastfeed as long as possible to reduce the risks of asthma has been challenged by more recent studies. It is likely that detailed studies of gene-by-environment interactions and of epigenetics will eventually untangle the inconsistencies among the many putative exposures and outcomes. Although there are indications that the increase in asthma has reached a plateau, at least in countries with the highest prevalence rates, much of the epidemiology and many of the risk factors for asthma remain to be adequately explained. Reduction in risk, and perhaps even true primary prevention of asthma, remains elusive but is a key goal of asthma management.
Key points
The prevalence of asthma varies widely around the world, probably because of gene-by-environment interactions.
Prenatal risk factors for asthma may include maternal smoking, diet and nutrition, stress, use of antibiotics and delivery by cesarean section.
Childhood risk factors for asthma may include allergic sensitization, environmental tobacco smoke, exposure to animals, breastfeeding, decreased lung function in infancy, family size and structure, socio-economic status, antibiotics and infections, and sex and gender.
Occupational exposures constitute a common risk factor for adult asthma.
This article is the first in a 7-part case study series that was developed as a knowledge translation initiative of the Canadian Thoracic Society Asthma Committee. The series aims to educate and inform primary care providers and nonrespiratory specialists about the diagnosis and management of asthma. The key messages presented in the cases are not clinical practice guidelines but are based on a review of the most recent scientific evidence available. Financial support for the publication of this series has been provided, in part, by the Canadian Thoracic Society.
Acknowledgement
The authors thank Dr. Peter Paré, iCapture Centre, University of British Columbia, for his invaluable assistance in editing and contributing to the genetics sections of this manuscript.
Footnotes
This article has been peer reviewed.
Competing interests: Piush Mandhane has received speaker’s honoraria from Merck Canada and the Edmonton Thoracic Society. None declared for Padmaja Subbarao and Malcolm Sears.
Contributors: All authors contributed to the development and editing of the publication, and all approved the final version submitted for publication.
Funding: The Canadian Thoracic Society has received funding to facilitate the knowledge translation activities of the CTS Asthma Committee from AstraZeneca Canada, GlaxoSmithKline Inc., Merck Frosst Canada and Novartis Pharmaceuticals. None of the sponsors played a role in the collection, review, analysis or interpretation of the scientific literature or in any decisions regarding the key messages presented in the case studies.
REFERENCES
- 1.Subbarao P, Becker A, Brook JR, et al. CHILD Study Investigators. Epidemiology of asthma: risk factors for development. Expert Rev Clin Immunol. 2009;5:77–95. doi: 10.1586/1744666X.5.1.77. [DOI] [PubMed] [Google Scholar]
- 2.Eder W, Ege MJ, von Mutius E. The asthma epidemic. N Engl J Med. 2006;355:2226–35. doi: 10.1056/NEJMra054308. [DOI] [PubMed] [Google Scholar]
- 3.International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. Lancet. 1998;351:1225–32. [PubMed] [Google Scholar]
- 4.Janson C, Anto J, Burney P, et al. The European Community Respiratory Health Survey: What are the main results so far? European Community Respiratory Health Survey II. Eur Respir J. 2001;18:598–611. doi: 10.1183/09031936.01.00205801. [DOI] [PubMed] [Google Scholar]
- 5.Asher MI, Montefort S, Bjorksten B, et al. ISAAC Phase Three Study Group. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006;368:733–43. doi: 10.1016/S0140-6736(06)69283-0. [DOI] [PubMed] [Google Scholar]
- 6.Zock JP, Heinrich J, Jarvis D, et al. Distribution and determinants of house dust mite allergens in Europe: the European Community Respiratory Health Survey II. J Allergy Clin Immunol. 2006;118:682–90. doi: 10.1016/j.jaci.2006.04.060. [DOI] [PubMed] [Google Scholar]
- 7.Cohen RT, Canino GJ, Bird HR, et al. Area of residence, birthplace, and asthma in Puerto Rican children. Chest. 2007;131:1331–8. doi: 10.1378/chest.06-1917. [DOI] [PubMed] [Google Scholar]
- 8.von Mutius E, Martinez FD, Fritzsch C, et al. Prevalence of asthma and atopy in two areas of West and East Germany. Am J Respir Crit Care Med. 1994;149:358–64. doi: 10.1164/ajrccm.149.2.8306030. [DOI] [PubMed] [Google Scholar]
- 9.Wang HY, Wong GW, Chen YZ, et al. Prevalence of asthma among Chinese adolescents living in Canada and in China. CMAJ. 2008;179:1133–42. doi: 10.1503/cmaj.071797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anto JM, Sunyer J, Rodriguez-Roisin R, et al. Community outbreaks of asthma associated with inhalation of soybean dust. Toxicoepidemiological Committee. N Engl J Med. 1989;320:1097–102. doi: 10.1056/NEJM198904273201701. [DOI] [PubMed] [Google Scholar]
- 11.Johnston NW, Sears MR. Asthma exacerbations. 1: Epidemiology. Thorax. 2006;61:722–8. doi: 10.1136/thx.2005.045161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sears MR, Johnston NW. Understanding the September asthma epidemic. J Allergy Clin Immunol. 2007;120:526–9. doi: 10.1016/j.jaci.2007.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sears MR, Greene JM, Willan AR, et al. A longitudinal, population-based, cohort study of childhood asthma followed to adulthood. N Engl J Med. 2003;349:1414–22. doi: 10.1056/NEJMoa022363. [DOI] [PubMed] [Google Scholar]
- 14.Burke W, Fesinmeyer M, Reed K, et al. Family history as a predictor of asthma risk. Am J Prev Med. 2003;24:160–9. doi: 10.1016/s0749-3797(02)00589-5. [DOI] [PubMed] [Google Scholar]
- 15.Willemsen G, van Beijsterveldt TCEM, van Baal CGCM, et al. Heritability of self-reported asthma and allergy: a study in adult Dutch twins, siblings and parents. Twin Res Hum Genet. 2008;11:132–42. doi: 10.1375/twin.11.2.132. [DOI] [PubMed] [Google Scholar]
- 16.Holberg CJ, Elston RC, Halonen M, et al. Segregation analysis of physician-diagnosed asthma in Hispanic and non-Hispanic white families. A recessive component? Am J Respir Crit Care Med. 1996;154:144–50. doi: 10.1164/ajrccm.154.1.8680670. [DOI] [PubMed] [Google Scholar]
- 17.Lawrence S, Beasley R, Doull I, et al. Genetic analysis of atopy and asthma as quantitative traits and ordered polychotomies. Ann Hum Genet. 1994;58:359–68. doi: 10.1111/j.1469-1809.1994.tb00732.x. [DOI] [PubMed] [Google Scholar]
- 18.Ober C, Hoffjan S. Asthma genetics 2006: the long and winding road to gene discovery. Genes Immun. 2006;7:95–100. doi: 10.1038/sj.gene.6364284. [DOI] [PubMed] [Google Scholar]
- 19.Moffatt MF, Kabesch M, Liang L, et al. Genetic variants regulating ORMDL3 expression contribute to the risk of childhood asthma. Nature. 2007;448:470–3. doi: 10.1038/nature06014. [DOI] [PubMed] [Google Scholar]
- 20.Galanter J, Choudhry S, Eng C, et al. ORMDL3 gene is associated with asthma in three ethnically diverse populations. Am J Respir Crit Care Med. 2008;177:1194–200. doi: 10.1164/rccm.200711-1644OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tavendale R, Macgregor DF, Mukhopadhyay, et al. A polymorphism controlling ORMDL3 expression is associated with asthma that is poorly controlled by current medications. J Allergy Clin Immunol. 2008;121:860–3. doi: 10.1016/j.jaci.2008.01.015. [DOI] [PubMed] [Google Scholar]
- 22.Stein RT, Holberg CJ, Sherrill D, et al. Influence of parental smoking on respiratory symptoms during the first decade of life: the Tucson Children’s Respiratory Study. Am J Epidemiol. 1999;149:1030–7. doi: 10.1093/oxfordjournals.aje.a009748. [DOI] [PubMed] [Google Scholar]
- 23.Lewis S, Richards D, Bynner J, et al. Prospective study of risk factors for early and persistent wheezing in childhood. Eur Respir J. 1995;8:349–56. doi: 10.1183/09031936.95.08030349. [DOI] [PubMed] [Google Scholar]
- 24.Lau S, Nickel R, Niggemann B, et al. The development of childhood asthma: lessons from the German Multicentre Allergy Study (MAS) Paediatr Respir Rev. 2002;3:265–72. doi: 10.1016/s1526-0542(02)00189-6. [DOI] [PubMed] [Google Scholar]
- 25.Tariq SM, Hakim EA, Matthews SM, et al. Influence of smoking on asthmatic symptoms and allergen sensitisation in early childhood. Postgrad Med J. 2000;76:694–9. doi: 10.1136/pmj.76.901.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dezateux C, Stocks J, Dundas I, et al. Impaired airway function and wheezing in infancy: the influence of maternal smoking and a genetic predisposition to asthma. Am J Respir Crit Care Med. 1999;159:403–10. doi: 10.1164/ajrccm.159.2.9712029. [DOI] [PubMed] [Google Scholar]
- 27.Lødrup Carlsen KC. The Environment and Childhood Asthma (ECA) Study in Oslo: ECA-1 and ECA-2. Pediatr Allergy Immunol. 2002;13(Suppl 15):29–31. doi: 10.1034/j.1399-3038.13.s.15.2.x. [DOI] [PubMed] [Google Scholar]
- 28.Devereux G, Barker RN, Seaton A. Antenatal determinants of neonatal immune responses to allergens. Clin Exp Allergy. 2002;32:43–50. doi: 10.1046/j.0022-0477.2001.01267.x. [DOI] [PubMed] [Google Scholar]
- 29.Macaubas C, de Klerk NH, Holt BJ, et al. Association between antenatal cytokine production and the development of atopy and asthma at age 6 years. Lancet. 2003;362:1192–7. doi: 10.1016/s0140-6736(03)14542-4. [DOI] [PubMed] [Google Scholar]
- 30.Frey U, Kuehni C, Roiha H, et al. Maternal atopic disease modifies effects of pre-natal risk factors on exhaled nitric oxide in infants. Am J Respir Crit Care Med. 2004;170:260–5. doi: 10.1164/rccm.200307-1002OC. [DOI] [PubMed] [Google Scholar]
- 31.Willers SM, Devereux G, Craig LC, et al. Maternal food consumption during pregnancy and asthma, respiratory and atopic symptoms in 5-year-old children. Thorax. 2007;62:773–9. doi: 10.1136/thx.2006.074187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Romieu I, Torrent M, Garcia-Esteban R, et al. Maternal fish intake during pregnancy and atopy and asthma in infancy. Clin Exp Allergy. 2007;37:518–25. doi: 10.1111/j.1365-2222.2007.02685.x. [DOI] [PubMed] [Google Scholar]
- 33.Mihrshahi S, Ampon R, Webb K, et al. The association between infant feeding practices and subsequent atopy among children with a family history of asthma. Clin Exp Allergy. 2007;37:671–9. doi: 10.1111/j.1365-2222.2007.02696.x. [DOI] [PubMed] [Google Scholar]
- 34.Litonjua AA, Rifas-Shiman SL, Ly NP, et al. Maternal antioxidant intake in pregnancy and wheezing illnesses in children at 2 y of age. Am J Clin Nutr. 2006;84:903–11. doi: 10.1093/ajcn/84.4.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Devereux G, Turner SW, Craig LC, et al. Low maternal vitamin E intake during pregnancy is associated with asthma in 5-year-old children. Am J Respir Crit Care Med. 2006;174:499–507. doi: 10.1164/rccm.200512-1946OC. [DOI] [PubMed] [Google Scholar]
- 36.Martindale S, McNeill G, Devereux G, et al. Antioxidant intake in pregnancy in relation to wheeze and eczema in the first two years of life. Am J Respir Crit Care Med. 2005;171:121–8. doi: 10.1164/rccm.200402-220OC. [DOI] [PubMed] [Google Scholar]
- 37.Kramer MS, Kakuma R. Maternal dietary antigen avoidance during pregnancy or lactation, or both, for preventing or treating atopic disease in the child [review] Cochrane Database Syst Rev. 2006;(3):CD000133. doi: 10.1002/14651858.CD000133.pub2. [DOI] [PubMed] [Google Scholar]
- 38.Fälth-Magnusson K, Kjellman NI. Development of atopic disease in babies whose mothers were receiving exclusion diet during pregnancy — a randomized study. J Allergy Clin Immunol. 1987;80:868–75. doi: 10.1016/s0091-6749(87)80279-8. [DOI] [PubMed] [Google Scholar]
- 39.Falth-Magnusson K, Kjellman NI. Allergy prevention by maternal elimination diet during late pregnancy — a 5-year follow-up of a randomized study. J Allergy Clin Immunol. 1992;89:709–13. doi: 10.1016/0091-6749(92)90378-f. [DOI] [PubMed] [Google Scholar]
- 40.Lilja G, Dannaeus A, Falth-Magnusson K, et al. Immune response of the atopic woman and foetus: effects of high- and low-dose food allergen intake during late pregnancy. Clin Allergy. 1988;18:131–42. doi: 10.1111/j.1365-2222.1988.tb02852.x. [DOI] [PubMed] [Google Scholar]
- 41.Camargo CA, Jr, Rifas-Shiman SL, Litonjua AA, et al. Maternal intake of vitamin D during pregnancy and risk of recurrent wheeze in children at 3 y of age. Am J Clin Nutr. 2007;85:788–95. doi: 10.1093/ajcn/85.3.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Devereux G, Litonjua AA, Turner SW, et al. Maternal vitamin D intake during pregnancy and early childhood wheezing. Am J Clin Nutr. 2007;85:853–9. doi: 10.1093/ajcn/85.3.853. [DOI] [PubMed] [Google Scholar]
- 43.Wright RJ, Finn P, Contreras JP, et al. Chronic caregiver stress and IgE expression, allergen-induced proliferation, and cytokine profiles in a birth cohort predisposed to atopy. J Allergy Clin Immunol. 2004;113:1051–7. doi: 10.1016/j.jaci.2004.03.032. [DOI] [PubMed] [Google Scholar]
- 44.Wright RJ, Cohen RT, Cohen S. The impact of stress on the development and expression of atopy. Curr Opin Allergy Clin Immunol. 2005;5:23–9. doi: 10.1097/00130832-200502000-00006. [DOI] [PubMed] [Google Scholar]
- 45.Lin YC, Wen HJ, Lee YL, et al. Are maternal psychosocial factors associated with cord immunoglobulin E in addition to family atopic history and mother immunoglobulin E? Clin Exp Allergy. 2004;34:548–54. doi: 10.1111/j.1365-2222.2004.1928.x. [DOI] [PubMed] [Google Scholar]
- 46.Wright RJ, Cohen S, Carey V, et al. Parental stress as a predictor of wheezing in infancy: a prospective birth-cohort study. Am J Respir Crit Care Med. 2002;165:358–65. doi: 10.1164/ajrccm.165.3.2102016. [DOI] [PubMed] [Google Scholar]
- 47.Kozyrskyj AL, Ernst P, Becker AB. Increased risk of childhood asthma from antibiotic use in early life. Chest. 2007;131:1753–9. doi: 10.1378/chest.06-3008. [DOI] [PubMed] [Google Scholar]
- 48.Mrazek DA, Klinnert M, Mrazek PJ, et al. Prediction of early-onset asthma in genetically at-risk children. Pediatr Pulmonol. 1999;27:85–94. doi: 10.1002/(sici)1099-0496(199902)27:2<85::aid-ppul4>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 49.Jedrychowski W, Galas A, Whyatt R, et al. The prenatal use of antibiotics and the development of allergic disease in one year old infants. A preliminary study. Int J Occup Med Environ Health. 2006;19:70–6. doi: 10.2478/v10001-006-0010-0. [DOI] [PubMed] [Google Scholar]
- 50.Benn CS, Thorsen P, Jensen JS, et al. Maternal vaginal microflora during pregnancy and the risk of asthma hospitalization and use of antiasthma medication in early childhood. J Allergy Clin Immunol. 2002;110:72–7. doi: 10.1067/mai.2002.125833. [DOI] [PubMed] [Google Scholar]
- 51.McKeever TM, Lewis SA, Smith C, et al. The importance of prenatal exposures on the development of allergic disease: a birth cohort study using the West Midlands General Practice Database. Am J Respir Crit Care Med. 2002;166:827–32. doi: 10.1164/rccm.200202-158OC. [DOI] [PubMed] [Google Scholar]
- 52.Nafstad P, Magnus P, Jaakkola JJ. Risk of childhood asthma and allergic rhinitis in relation to pregnancy complications. J Allergy Clin Immunol. 2000;106:867–73. doi: 10.1067/mai.2000.110558. [DOI] [PubMed] [Google Scholar]
- 53.Annesi-Maesano I, Moreau D, Strachan D. In utero and perinatal complications preceding asthma. Allergy. 2001;56:491–7. doi: 10.1034/j.1398-9995.2001.056006491.x. [DOI] [PubMed] [Google Scholar]
- 54.Lewis S, Butland B, Strachan D, et al. Study of the aetiology of wheezing illness at age 16 in two national British birth cohorts. Thorax. 1996;51:670–6. doi: 10.1136/thx.51.7.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nafstad P, Samuelsen SO, Irgens LM, et al. Pregnancy complications and the risk of asthma among Norwegians born between 1967 and 1993. Eur J Epidemiol. 2003;18:755–61. doi: 10.1023/a:1025395405101. [DOI] [PubMed] [Google Scholar]
- 56.Stick SM, Burton PR, Gurrin L, et al. Effects of maternal smoking during pregnancy and a family history of asthma on respiratory function in newborn infants. Lancet. 1996;348:1060–4. doi: 10.1016/s0140-6736(96)04446-7. [DOI] [PubMed] [Google Scholar]
- 57.Kero J, Gissler M, Gronlund MM, et al. Mode of delivery and asthma — is there a connection? Pediatr Res. 2002;52:6–11. doi: 10.1203/00006450-200207000-00004. [DOI] [PubMed] [Google Scholar]
- 58.Xu B, Pekkanen J, Hartikainen AL, et al. Caesarean section and risk of asthma and allergy in adulthood. J Allergy Clin Immunol. 2001;107:732–3. doi: 10.1067/mai.2001.113048. [DOI] [PubMed] [Google Scholar]
- 59.Bager P, Melbye M, Rostgaard K, et al. Mode of delivery and risk of allergic rhinitis and asthma. J Allergy Clin Immunol. 2003;111:51–6. doi: 10.1067/mai.2003.34. [DOI] [PubMed] [Google Scholar]
- 60.Martinez FD, Wright AL, Taussig LM, et al. Asthma and wheezing in the first six years of life. The Group Health Medical Associates. N Engl J Med. 1995;332:133–8. doi: 10.1056/NEJM199501193320301. [DOI] [PubMed] [Google Scholar]
- 61.Lowe LA, Simpson A, Woodcock A, et al. Wheeze phenotypes and lung function in preschool children. Am J Respir Crit Care Med. 2005;171:231–7. doi: 10.1164/rccm.200406-695OC. [DOI] [PubMed] [Google Scholar]
- 62.Young S, Arnott J, O’Keeffe PT, et al. The association between early life lung function and wheezing during the first 2 yrs of life. Eur Respir J. 2000;15:151–7. doi: 10.1183/09031936.00.15115100. [DOI] [PubMed] [Google Scholar]
- 63.Illi S, von Mutius E, Lau S, et al. Perennial allergen sensitisation early in life and chronic asthma in children: a birth cohort study. Lancet. 2006;368:763–70. doi: 10.1016/S0140-6736(06)69286-6. [DOI] [PubMed] [Google Scholar]
- 64.Bergmann RL, Diepgen TL, Kuss O, et al. Breastfeeding duration is a risk factor for atopic eczema. Clin Exp Allergy. 2002;32:205–9. doi: 10.1046/j.1365-2222.2002.01274.x. [DOI] [PubMed] [Google Scholar]
- 65.Dell S, To T. Breastfeeding and asthma in young children: findings from a population-based study. Arch Pediatr Adolesc Med. 2001;155:1261–5. doi: 10.1001/archpedi.155.11.1261. [DOI] [PubMed] [Google Scholar]
- 66.Oddy WH. Breastfeeding and asthma in children: findings from a West Australian study. Breastfeed Rev. 2000;8:5–11. [PubMed] [Google Scholar]
- 67.Sears MR, Greene JM, Willan AR, et al. Long-term relation between breastfeeding and development of atopy and asthma in children and young adults: a longitudinal study. Lancet. 2002;360:901–7. doi: 10.1016/S0140-6736(02)11025-7. [DOI] [PubMed] [Google Scholar]
- 68.Wright AL, Holberg CJ, Taussig LM, et al. Maternal asthma status alters relation of infant feeding to asthma in childhood. Adv Exp Med Biol. 2000;478:131–7. doi: 10.1007/0-306-46830-1_11. [DOI] [PubMed] [Google Scholar]
- 69.Gdalevich M, Mimouni D, Mimouni M. Breast-feeding and the risk of bronchial asthma in childhood: a systematic review with meta-analysis of prospective studies. J Pediatr. 2001;139:261–6. doi: 10.1067/mpd.2001.117006. [DOI] [PubMed] [Google Scholar]
- 70.Kull I, Almqvist C, Lilja G, et al. Breast-feeding reduces the risk of asthma during the first 4 years of life. J Allergy Clin Immunol. 2004;114:755–60. doi: 10.1016/j.jaci.2004.07.036. [DOI] [PubMed] [Google Scholar]
- 71.Mandhane PJ, Greene JM, Cowan JO, et al. Sex differences in factors associated with childhood- and adolescent-onset wheeze. Am J Respir Crit Care Med. 2005;172:45–54. doi: 10.1164/rccm.200412-1738OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Businco L, Marchetti F, Pellegrini G, et al. Predictive value of cord blood IgE levels in ‘at-risk’ newborn babies and influence of type of feeding. Clin Allergy. 1983;13:503–8. doi: 10.1111/j.1365-2222.1983.tb02631.x. [DOI] [PubMed] [Google Scholar]
- 73.Lovegrove JA, Hampton SM, Morgan JB. The immunological and long-term atopic outcome of infants born to women following a milk-free diet during late pregnancy and lactation: a pilot study. Br J Nutr. 1994;71:223–38. doi: 10.1079/bjn19940129. [DOI] [PubMed] [Google Scholar]
- 74.Sigurs N, Hattevig G, Kjellman B. Maternal avoidance of eggs, cow’s milk, and fish during lactation: effect on allergic manifestations, skin-prick tests, and specific IgE antibodies in children at age 4 years. Pediatrics. 1992;89:735–9. [PubMed] [Google Scholar]
- 75.Hattevig G, Sigurs N, Kjellman B. Effects of maternal dietary avoidance during lactation on allergy in children at 10 years of age. Acta Paediatr. 1999;88:7–12. [PubMed] [Google Scholar]
- 76.Muraro A, Dreborg S, Halken S, et al. Dietary prevention of allergic diseases in infants and small children. Part III: Critical review of published peer-reviewed observational and interventional studies and final recommendations. Pediatr Allergy Immunol. 2004;15:291–307. doi: 10.1111/j.1399-3038.2004.00127.x. [DOI] [PubMed] [Google Scholar]
- 77.Haland G, Carlsen KC, Sandvik L, et al. Reduced lung function at birth and the risk of asthma at 10 years of age. N Engl J Med. 2006;355:1682–9. doi: 10.1056/NEJMoa052885. [DOI] [PubMed] [Google Scholar]
- 78.Phelan PD, Robertson CF, Olinsky A. The Melbourne Asthma Study: 1964–1999. J Allergy Clin Immunol. 2002;109:189–94. doi: 10.1067/mai.2002.120951. [DOI] [PubMed] [Google Scholar]
- 79.Clarke JR, Reese A, Silverman M. Bronchial responsiveness and lung function in infants with lower respiratory tract illness over the first six months of life. Arch Dis Child. 1992;67:1454–8. doi: 10.1136/adc.67.12.1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Turner SW, Palmer LJ, Rye PJ, et al. The relationship between infant airway function, childhood airway responsiveness, and asthma. Am J Respir Crit Care Med. 2004;169:921–7. doi: 10.1164/rccm.200307-891OC. [DOI] [PubMed] [Google Scholar]
- 81.Schaub B, Lauener R, von Mutius E. The many faces of the hygiene hypothesis. J Allergy Clin Immunol. 2006;117:969–77. doi: 10.1016/j.jaci.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 82.Strachan DP. Hay fever, hygiene, and household size. BMJ. 1989;299:1259–60. doi: 10.1136/bmj.299.6710.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Matricardi PM, Franzinelli F, Franco A, et al. Sibship size, birth order, and atopy in 11,371 Italian young men. J Allergy Clin Immunol. 1998;101:439–44. doi: 10.1016/s0091-6749(98)70350-1. [DOI] [PubMed] [Google Scholar]
- 84.Kinra S, Davey SG, Jeffreys M, et al. Association between sibship size and allergic diseases in the Glasgow Alumni Study. Thorax. 2006;61:48–53. doi: 10.1136/thx.2004.034595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Goldberg S, Israeli E, Schwartz S, et al. Asthma prevalence, family size, and birth order. Chest. 2007;131:1747–52. doi: 10.1378/chest.06-2818. [DOI] [PubMed] [Google Scholar]
- 86.Bernsen RM, de Jongste JC, van der Wouden JC. Birth order and sibship size as independent risk factors for asthma, allergy, and eczema. Pediatr Allergy Immunol. 2003;14:464–9. doi: 10.1046/j.0905-6157.2003.00108.x. [DOI] [PubMed] [Google Scholar]
- 87.Bach JF. The effect of infections on susceptibility to autoimmune and allergic diseases. N Engl J Med. 2002;347:911–20. doi: 10.1056/NEJMra020100. [DOI] [PubMed] [Google Scholar]
- 88.Halfon N, Newacheck PW. Childhood asthma and poverty: differential impacts and utilization of health services. Pediatrics. 1993;91:56–61. [PubMed] [Google Scholar]
- 89.Goodman DC, Stukel TA, Chang CH. Trends in pediatric asthma hospitalization rates: regional and socioeconomic differences. Pediatrics. 1998;101:208–13. doi: 10.1542/peds.101.2.208. [DOI] [PubMed] [Google Scholar]
- 90.Claudio L, Tulton L, Doucette J, et al. Socioeconomic factors and asthma hospitalization rates in New York City. J Asthma. 1999;36:343–50. doi: 10.3109/02770909909068227. [DOI] [PubMed] [Google Scholar]
- 91.Erzen D, Carriere KC, Dik N, et al. Income level and asthma prevalence and care patterns. Am J Respir Crit Care Med. 1997;155:1060–5. doi: 10.1164/ajrccm.155.3.9116987. [DOI] [PubMed] [Google Scholar]
- 92.Strachan DP, Anderson HR, Limb ES, et al. A national survey of asthma prevalence, severity, and treatment in Great Britain. Arch Dis Child. 1994;70:174–8. doi: 10.1136/adc.70.3.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Litonjua AA, Carey VJ, Weiss ST, et al. Race, socioeconomic factors, and area of residence are associated with asthma prevalence. Pediatr Pulmonol. 1999;28:394–401. doi: 10.1002/(sici)1099-0496(199912)28:6<394::aid-ppul2>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 94.Miller JE. The effects of race/ethnicity and income on early childhood asthma prevalence and health care use. Am J Public Health. 2000;90:428–30. doi: 10.2105/ajph.90.3.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Peckham C, Butler N. A national study of asthma in childhood. J Epidemiol Community Health. 1978;32:79–85. doi: 10.1136/jech.32.2.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hamman RF, Halil T, Holland WW. Asthma in schoolchildren. Demographic associations and peak expiratory flow rates compared in children with bronchitis. Br J Prev Soc Med. 1975;29:228–38. doi: 10.1136/jech.29.4.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ernst P, Demissie K, Joseph L, et al. Socioeconomic status and indicators of asthma in children. Am J Respir Crit Care Med. 1995;152:570–5. doi: 10.1164/ajrccm.152.2.7633709. [DOI] [PubMed] [Google Scholar]
- 98.Klinnert MD, Nelson HS, Price MR, et al. Onset and persistence of childhood asthma: predictors from infancy. Pediatrics. 2001;108:E69. doi: 10.1542/peds.108.4.e69. [DOI] [PubMed] [Google Scholar]
- 99.Klinnert MD, Mrazek PJ, Mrazek DA. Early asthma onset: the interaction between family stressors and adaptive parenting. Psychiatry. 1994;57:51–61. doi: 10.1080/00332747.1994.11024668. [DOI] [PubMed] [Google Scholar]
- 100.Kummeling I, Stelma FF, Dagnelie PC, et al. Early life exposure to antibiotics and the subsequent development of eczema, wheeze, and allergic sensitization in the first 2 years of life: the KOALA Birth Cohort Study. Pediatrics. 2007;119:e225–31. doi: 10.1542/peds.2006-0896. [DOI] [PubMed] [Google Scholar]
- 101.Alm B, Erdes L, Mollborg P, et al. Neonatal antibiotic treatment is a risk factor for early wheezing. Pediatrics. 2008;121:697–702. doi: 10.1542/peds.2007-1232. [DOI] [PubMed] [Google Scholar]
- 102.Lemanske RF, Jr, Busse WW. Asthma: factors underlying inception, exacerbation, and disease progression. J Allergy Clin Immunol. 2006;117(2 Suppl Mini-Primer):S456–61. doi: 10.1016/j.jaci.2005.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Arruda LK, Sole D, Baena-Cagnani CE, et al. Risk factors for asthma and atopy. Curr Opin Allergy Clin Immunol. 2005;5:153–9. doi: 10.1097/01.all.0000162308.89857.6c. [DOI] [PubMed] [Google Scholar]
- 104.Martinez FD. Role of viral infections in the inception of asthma and allergies during childhood: Could they be protective? Thorax. 1994;49:1189–91. doi: 10.1136/thx.49.12.1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Stein RT, Sherrill D, Morgan WJ, et al. Respiratory syncytial virus in early life and risk of wheeze and allergy by age 13 years. Lancet. 1999;354:541–5. doi: 10.1016/S0140-6736(98)10321-5. [DOI] [PubMed] [Google Scholar]
- 106.Sigurs N, Gustafsson PM, Bjarnason R, et al. Severe respiratory syncytial virus bronchiolitis in infancy and asthma and allergy at age 13. Am J Respir Crit Care Med. 2005;171:137–41. doi: 10.1164/rccm.200406-730OC. [DOI] [PubMed] [Google Scholar]
- 107.Martinez FD, Holt PG. Role of microbial burden in aetiology of allergy and asthma. Lancet. 1999;354(Suppl 2):SII12–5. doi: 10.1016/s0140-6736(99)90437-3. [DOI] [PubMed] [Google Scholar]
- 108.Gern JE, Brooks GD, Meyer P, et al. Bidirectional interactions between viral respiratory illnesses and cytokine responses in the first year of life. J Allergy Clin Immunol. 2006;117:72–8. doi: 10.1016/j.jaci.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 109.Friedlander SL, Jackson DJ, Gangnon RE, et al. Viral infections, cytokine dysregulation and the origins of childhood asthma and allergic diseases. Pediatr Infect Dis J. 2005;24(Suppl):S170–6. doi: 10.1097/01.inf.0000187273.47390.01. [DOI] [PubMed] [Google Scholar]
- 110.Becker A, Watson W, Ferguson A, et al. The Canadian Asthma Primary Prevention Study: outcomes at 2 years of age. J Allergy Clin Immunol. 2004;113:650–6. doi: 10.1016/j.jaci.2004.01.754. [DOI] [PubMed] [Google Scholar]
- 111.Chan-Yeung M, Ferguson A, Watson W, et al. The Canadian Childhood Asthma Primary Prevention Study: outcomes at 7 years of age. J Allergy Clin Immunol. 2005;116:49–55. doi: 10.1016/j.jaci.2005.03.029. [DOI] [PubMed] [Google Scholar]
- 112.Oddy WH, de Klerk NH, Sly PD, et al. The effects of respiratory infections, atopy, and breastfeeding on childhood asthma. Eur Respir J. 2002;19:899–905. doi: 10.1183/09031936.02.00103602. [DOI] [PubMed] [Google Scholar]
- 113.Lemanske RF, Jr, Jackson DJ, Gangnon RE, et al. Rhinovirus illnesses during infancy predict subsequent childhood wheezing. J Allergy Clin Immunol. 2005;116:571–7. doi: 10.1016/j.jaci.2005.06.024. [DOI] [PubMed] [Google Scholar]
- 114.Joshi P, Shaw A, Kakakios A, et al. Interferon-gamma levels in nasopharyngeal secretions of infants with respiratory syncytial virus and other respiratory viral infections. Clin Exp Immunol. 2003;131:143–7. doi: 10.1046/j.1365-2249.2003.02039.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Celedón JC, Litonjua AA, Ryan L, et al. Day care attendance, respiratory tract illnesses, wheezing, asthma, and total serum IgE level in early childhood. Arch Pediatr Adolesc Med. 2002;156:241–5. doi: 10.1001/archpedi.156.3.241. [DOI] [PubMed] [Google Scholar]
- 116.Sears MR, Burrows B, Flannery EM, et al. Relation between airway responsiveness and serum IgE in children with asthma and in apparently normal children. N Engl J Med. 1991;325:1067–71. doi: 10.1056/NEJM199110103251504. [DOI] [PubMed] [Google Scholar]
- 117.Tariq SM, Arshad SH, Matthews SM, et al. Elevated cord serum IgE increases the risk of aeroallergen sensitization without increasing respiratory allergic symptoms in early childhood. Clin Exp Allergy. 1999;29:1042–8. doi: 10.1046/j.1365-2222.1999.00594.x. [DOI] [PubMed] [Google Scholar]
- 118.Wickman M, Ahlstedt S, Lilja G, et al. Quantification of IgE antibodies simplifies the classification of allergic diseases in 4-year-old children. A report from the prospective birth cohort study – BAMSE. Pediatr Allergy Immunol. 2003;14:441–7. doi: 10.1046/j.0905-6157.2003.00079.x. [DOI] [PubMed] [Google Scholar]
- 119.Karmaus W, Arshad H, Mattes J. Does the sibling effect have its origin in utero? Investigating birth order, cord blood immunoglobulin E concentration, and allergic sensitization at age 4 years. Am J Epidemiol. 2001;154:909–15. doi: 10.1093/aje/154.10.909. [DOI] [PubMed] [Google Scholar]
- 120.Prescott SL, King B, Strong TL, et al. The value of perinatal immune responses in predicting allergic disease at 6 years of age. Allergy. 2003;58:1187–94. doi: 10.1034/j.1398-9995.2003.00263.x. [DOI] [PubMed] [Google Scholar]
- 121.Tulic MK, Fiset PO, Manoukian JJ, et al. Role of Toll-like receptor 4 in protection by bacterial lipopolysaccharide in the nasal mucosa of atopic children but not adults. Lancet. 2004;363:1689–97. doi: 10.1016/S0140-6736(04)16253-3. [DOI] [PubMed] [Google Scholar]
- 122.Lauener RP, Birchler T, Adamski J, et al. Expression of CD14 and Toll-like receptor 2 in farmers’ and non-farmers’ children. Lancet. 2002;360:465–6. doi: 10.1016/S0140-6736(02)09641-1. [DOI] [PubMed] [Google Scholar]
- 123.Lin RY, Rehman A. Clinical characteristics of adult asthmatics requiring intubation. J Med. 1995;26:261–77. [PubMed] [Google Scholar]
- 124.James AL, Palmer LJ, Kicic E, et al. Decline in lung function in the Busselton Health Study: the effects of asthma and cigarette smoking. Am J Respir Crit Care Med. 2005;171:109–14. doi: 10.1164/rccm.200402-230OC. [DOI] [PubMed] [Google Scholar]
- 125.Simpson A, Custovic A. Pets and the development of allergic sensitization. Curr Allergy Asthma Rep. 2005;5:212–20. doi: 10.1007/s11882-005-0040-x. [DOI] [PubMed] [Google Scholar]
- 126.Takkouche B, Gonzalez-Barcala FJ, Etminan M, et al. Exposure to furry pets and the risk of asthma and allergic rhinitis: a meta-analysis. Allergy. 2008;63:857–64. doi: 10.1111/j.1398-9995.2008.01732.x. [DOI] [PubMed] [Google Scholar]
- 127.Almqvist C, Egmar AC, Hedlin G, et al. Direct and indirect exposure to pets —risk of sensitization and asthma at 4 years in a birth cohort. Clin Exp Allergy. 2003;33:1190–7. doi: 10.1046/j.1365-2222.2003.01764.x. [DOI] [PubMed] [Google Scholar]
- 128.Huss K, Adkinson NF, Jr, Eggleston PA, et al. House dust mite and cockroach exposure are strong risk factors for positive allergy skin test responses in the Childhood Asthma Management Program. J Allergy Clin Immunol. 2001;107:48–54. doi: 10.1067/mai.2001.111146. [DOI] [PubMed] [Google Scholar]
- 129.Henriksen AH, Holmen TL, Bjermer L. Sensitization and exposure to pet allergens in asthmatics versus non-asthmatics with allergic rhinitis. Respir Med. 2001;95:122–9. doi: 10.1053/rmed.2000.1004. [DOI] [PubMed] [Google Scholar]
- 130.Campo P, Kalra HK, Levin L, et al. Influence of dog ownership and high endotoxin on wheezing and atopy during infancy. J Allergy Clin Immunol. 2006;118:1271–8. doi: 10.1016/j.jaci.2006.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Fraga MF, Ballestar E, Paz MF, et al. Epigenetic differences arise during the lifetime of monozygotic twins. Proc Natl Acad Sci U S A. 2005;102:10604–9. doi: 10.1073/pnas.0500398102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Qiu J. Epigenetics: unfinished symphony. Nature. 2006;441:143–5. doi: 10.1038/441143a. [DOI] [PubMed] [Google Scholar]
- 133.de Marco R, Locatelli F, Sunyer J, et al. Differences in incidence of reported asthma related to age in men and women. A retrospective analysis of the data of the European Respiratory Health Survey. Am J Respir Crit Care Med. 2000;162:68–74. doi: 10.1164/ajrccm.162.1.9907008. [DOI] [PubMed] [Google Scholar]
- 134.Crawford WA, Beedham CG. The changing demographic pattern in asthma related to sex and age. A study of 13,651 patients on sodium cromoglycate (Intal) Med J Aust. 1976;1:430–4. [PubMed] [Google Scholar]
- 135.Bjornson CL, Mitchell I. Gender differences in asthma in childhood and adolescence. J Gend Specif Med. 2000;3:57–61. [PubMed] [Google Scholar]
- 136.de Marco R, Locatelli F, Cerveri I, et al. Incidence and remission of asthma: a retrospective study on the natural history of asthma in Italy. J Allergy Clin Immunol. 2002;110:228–35. doi: 10.1067/mai.2002.125600. [DOI] [PubMed] [Google Scholar]
- 137.Sears MR. Growing up with asthma. BMJ. 1994;309:72–3. doi: 10.1136/bmj.309.6947.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Weiss ST, Sparrow D, O’Connor GT. The interrelationship among allergy, airways responsiveness, and asthma. J Asthma. 1993;30:329–49. doi: 10.3109/02770909309056738. [DOI] [PubMed] [Google Scholar]
- 139.Bronnimann S, Burrows B. A prospective study of the natural history of asthma. Remission and relapse rates. Chest. 1986;90:480–4. doi: 10.1378/chest.90.4.480. [DOI] [PubMed] [Google Scholar]
- 140.Nicolai T, Illi S, Tenborg J, et al. Puberty and prognosis of asthma and bronchial hyper-reactivity. Pediatr Allergy Immunol. 2001;12:142–8. doi: 10.1034/j.1399-3038.2001.0007.x. [DOI] [PubMed] [Google Scholar]
- 141.Zannolli R, Morgese G. Does puberty interfere with asthma? Med Hypotheses. 1997;48:27–32. doi: 10.1016/s0306-9877(97)90020-7. [DOI] [PubMed] [Google Scholar]
- 142.Meurer JR, George V, Subichin S, et al. Asthma severity among children hospitalized in 1990 and 1995. Arch Pediatr Adolesc Med. 2000;154:143–9. doi: 10.1001/archpedi.154.2.143. [DOI] [PubMed] [Google Scholar]
- 143.Williams H, McNicol KN. Prevalence, natural history, and relationship of wheezy bronchitis and asthma in children. An epidemiological study. BMJ. 1969;4:321–5. doi: 10.1136/bmj.4.5679.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Gerritsen J, Koëter GH, Postma DS, et al. Prognosis of asthma from childhood to adulthood. Am Rev Respir Dis. 1989;140:1325–30. doi: 10.1164/ajrccm/140.5.1325. [DOI] [PubMed] [Google Scholar]
- 145.Roche WR. Inflammatory and structural changes in the small airways in bronchial asthma. Am J Respir Crit Care Med. 1998;157:S191–4. doi: 10.1164/ajrccm.157.5.rsaa-5. [DOI] [PubMed] [Google Scholar]
- 146.Schwartz J, Weiss ST. Relationship of skin test reactivity to decrements in pulmonary function in children with asthma or frequent wheezing. Am J Respir Crit Care Med. 1995;152:2176–80. doi: 10.1164/ajrccm.152.6.8520794. [DOI] [PubMed] [Google Scholar]
- 147.Selroos O, Pietinalho A, Lofroos AB, et al. Effect of early vs late intervention with inhaled corticosteroids in asthma. Chest. 1995;108:1228–34. doi: 10.1378/chest.108.5.1228. [DOI] [PubMed] [Google Scholar]
- 148.Sherrill DL, Martinez FD, Lebowitz MD, et al. Longitudinal effects of passive smoking on pulmonary function in New Zealand children. Am Rev Respir Dis. 1992;145:1136–41. doi: 10.1164/ajrccm/145.5.1136. [DOI] [PubMed] [Google Scholar]
- 149.Sherrill D, Sears MR, Lebowitz MD, et al. The effects of airway hyperresponsiveness, wheezing, and atopy on longitudinal pulmonary function in children: a 6-year follow-up study. Pediatr Pulmonol. 1992;13:78–85. doi: 10.1002/ppul.1950130204. [DOI] [PubMed] [Google Scholar]
- 150.Oswald H, Phelan PD, Lanigan A, et al. Childhood asthma and lung function in mid-adult life. Pediatr Pulmonol. 1997;23:14–20. doi: 10.1002/(sici)1099-0496(199701)23:1<14::aid-ppul2>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 151.Kjellman B, Hesselmar B. Prognosis of asthma in children: a cohort study into adulthood. Acta Paediatr. 1994;83:854–61. doi: 10.1111/j.1651-2227.1994.tb13157.x. [DOI] [PubMed] [Google Scholar]
- 152.Sears MR, Herbison GP, Holdaway MD, et al. The relative risks of sensitivity to grass pollen, house dust mite and cat dander in the development of childhood asthma. Clin Exp Allergy. 1989;19:419–24. doi: 10.1111/j.1365-2222.1989.tb02408.x. [DOI] [PubMed] [Google Scholar]
- 153.Sears MR, Holdaway MD, Flannery EM, et al. Parental and neonatal risk factors for atopy, airway hyper-responsiveness, and asthma. Arch Dis Child. 1996;75:392–8. doi: 10.1136/adc.75.5.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Roorda RJ, Gerritsen J, van Aalderen WM, et al. Follow-up of asthma from childhood to adulthood: influence of potential childhood risk factors on the outcome of pulmonary function and bronchial responsiveness in adulthood. J Allergy Clin Immunol. 1994;93:575–84. doi: 10.1016/s0091-6749(94)70069-9. [DOI] [PubMed] [Google Scholar]
- 155.Godden DJ, Ross S, Abdalla M, et al. Outcome of wheeze in childhood. Symptoms and pulmonary function 25 years later. Am J Respir Crit Care Med. 1994;149:106–12. doi: 10.1164/ajrccm.149.1.8111567. [DOI] [PubMed] [Google Scholar]
- 156.Becklake MR, Kauffmann F. Gender differences in airway behaviour over the human life span. Thorax. 1999;54:1119–38. doi: 10.1136/thx.54.12.1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Dodge RR, Burrows B. The prevalence and incidence of asthma and asthma-like symptoms in a general population sample. Am Rev Respir Dis. 1980;122:567–75. doi: 10.1164/arrd.1980.122.4.567. [DOI] [PubMed] [Google Scholar]
- 158.Kao CC, See LC, Yan DC, et al. Time trends and seasonal variations in hospital admissions for childhood asthma in Taiwan from 1990 to 1998. Asian Pac J Allergy Immunol. 2001;19:63–8. [PubMed] [Google Scholar]
- 159.Joseph CL, Havstad SL, Ownby DR, et al. Racial differences in emergency department use persist despite allergist visits and prescriptions filled for antiinflammatory medications. J Allergy Clin Immunol. 1998;101:484–90. doi: 10.1016/S0091-6749(98)70355-0. [DOI] [PubMed] [Google Scholar]
- 160.Schaubel D, Johansen H, Mao Y, et al. Risk of preschool asthma: incidence, hospitalization, recurrence, and readmission probability. J Asthma. 1996;33:97–103. doi: 10.3109/02770909609054537. [DOI] [PubMed] [Google Scholar]
- 161.Skobeloff EM, Spivey WH, St Clair SS, et al. The influence of age and sex on asthma admissions. JAMA. 1992;268:3437–40. [PubMed] [Google Scholar]
- 162.To T, Dick P, Feldman W, et al. A cohort study on childhood asthma admissions and readmissions. Pediatrics. 1996;98:191–5. [PubMed] [Google Scholar]
- 163.Von Behren J, Kreutzer R, Smith D. Asthma hospitalization trends in California, 1983–1996. J Asthma. 1999;36:575–82. doi: 10.3109/02770909909087294. [DOI] [PubMed] [Google Scholar]
- 164.Wilkins K, Mao Y. Trends in rates of admission to hospital and death from asthma among children and young adults in Canada during the 1980s. CMAJ. 1993;148:185–90. [PMC free article] [PubMed] [Google Scholar]
- 165.Hyndman SJ, Williams DR, Merrill SL, et al. Rates of admission to hospital for asthma. BMJ. 1994;308:1596–600. doi: 10.1136/bmj.308.6944.1596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Trawick DR, Holm C, Wirth J. Influence of gender on rates of hospitalization, hospital course, and hypercapnea in high-risk patients admitted for asthma: a 10-year retrospective study at Yale-New Haven Hospital. Chest. 2001;119:115–9. doi: 10.1378/chest.119.1.115. [DOI] [PubMed] [Google Scholar]
- 167.Chen Y, Stewart P, Johansen H, et al. Sex difference in hospitalization due to asthma in relation to age. J Clin Epidemiol. 2003;56:180–7. doi: 10.1016/s0895-4356(02)00593-0. [DOI] [PubMed] [Google Scholar]
- 168.Chen Y, Dales R, Stewart P, et al. Hospital readmissions for asthma in children and young adults in Canada. Pediatr Pulmonol. 2003;36:22–6. doi: 10.1002/ppul.10307. [DOI] [PubMed] [Google Scholar]
- 169.Le Souëf PN, Sears MR, Sherrill D. The effect of size and age of subject on airway responsiveness in children. Am J Respir Crit Care Med. 1995;152:576–9. doi: 10.1164/ajrccm.152.2.7633710. [DOI] [PubMed] [Google Scholar]
- 170.Ernst P, Ghezzo H, Becklake MR. Risk factors for bronchial hyperresponsiveness in late childhood and early adolescence. Eur Respir J. 2002;20:635–9. doi: 10.1183/09031936.02.00962002. [DOI] [PubMed] [Google Scholar]
- 171.Gustafsson PM, Kjellman B. Asthma from childhood to adulthood: course and outcome of lung function. Respir Med. 2000;94:466–74. doi: 10.1053/rmed.1999.0763. [DOI] [PubMed] [Google Scholar]
- 172.Tashkin DP, Altose MD, Bleecker ER, et al. The Lung Health Study: airway responsiveness to inhaled methacholine in smokers with mild to moderate airflow limitation. The Lung Health Study Research Group. Am Rev Respir Dis. 1992;145:301–10. doi: 10.1164/ajrccm/145.2_Pt_1.301. [DOI] [PubMed] [Google Scholar]
- 173.Kanner RE, Connett JE, Altose MD, et al. Gender difference in airway hyperresponsiveness in smokers with mild COPD. The Lung Health Study. Am J Respir Crit Care Med. 1994;150:956–61. doi: 10.1164/ajrccm.150.4.7921469. [DOI] [PubMed] [Google Scholar]
- 174.Leynaert B, Bousquet J, Henry C, et al. Is bronchial hyperresponsiveness more frequent in women than in men? A population-based study. Am J Respir Crit Care Med. 1997;156:1413–20. doi: 10.1164/ajrccm.156.5.9701060. [DOI] [PubMed] [Google Scholar]
- 175.Sears MR, Burrows B, Flannery EM, et al. Atopy in childhood. I. Gender and allergen related risks for development of hay fever and asthma. Clin Exp Allergy. 1993;23:941–8. doi: 10.1111/j.1365-2222.1993.tb00279.x. [DOI] [PubMed] [Google Scholar]
- 176.Barbee RA, Kaltenborn W, Lebowitz MD, et al. Longitudinal changes in allergen skin test reactivity in a community population sample. J Allergy Clin Immunol. 1987;79:16–24. doi: 10.1016/s0091-6749(87)80010-6. [DOI] [PubMed] [Google Scholar]
- 177.Cline MG, Burrows B. Distribution of allergy in a population sample residing in Tucson, Arizona. Thorax. 1989;44:425–31. doi: 10.1136/thx.44.5.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Oryszczyn MP, Bouzigon E, Maccario J, et al. Interrelationships of quantitative asthma-related phenotypes in the Epidemiological Study on the Genetics and Environment of Asthma, Bronchial Hyperresponsiveness, and Atopy. J Allergy Clin Immunol. 2007;119:57–63. doi: 10.1016/j.jaci.2006.09.026. [DOI] [PubMed] [Google Scholar]
- 179.Camargo CA, Jr, Weiss ST, Zhang S, et al. Prospective study of body mass index, weight change, and risk of adult-onset asthma in women. Arch Intern Med. 1999;159:2582–8. doi: 10.1001/archinte.159.21.2582. [DOI] [PubMed] [Google Scholar]
- 180.Hancox RJ, Milne BJ, Poulton R, et al. Sex differences in the relation between body mass index and asthma and atopy in a birth cohort. Am J Respir Crit Care Med. 2005;171:440–5. doi: 10.1164/rccm.200405-623OC. [DOI] [PubMed] [Google Scholar]
- 181.Weiss ST. Obesity: insight into the origins of asthma. Nat Immunol. 2005;6:537–9. doi: 10.1038/ni0605-537. [DOI] [PubMed] [Google Scholar]
- 182.Bauer BA, Reed CE, Yunginger JW, et al. Incidence and outcomes of asthma in the elderly. A population-based study in Rochester, Minnesota. Chest. 1997;111:303–10. doi: 10.1378/chest.111.2.303. [DOI] [PubMed] [Google Scholar]
- 183.Butland BK, Strachan DP. Asthma onset and relapse in adult life: the British 1958 birth cohort study. Ann Allergy Asthma Immunol. 2007;98:337–43. doi: 10.1016/S1081-1206(10)60879-4. [DOI] [PubMed] [Google Scholar]
- 184.Wenzel SE. Asthma: defining of the persistent adult phenotypes. Lancet. 2006;368:804–13. doi: 10.1016/S0140-6736(06)69290-8. [DOI] [PubMed] [Google Scholar]
- 185.Eagan TM, Gulsvik A, Eide GE, et al. Occupational airborne exposure and the incidence of respiratory symptoms and asthma. Am J Respir Crit Care Med. 2002;166:933–8. doi: 10.1164/rccm.200203-238OC. [DOI] [PubMed] [Google Scholar]
- 186.Le Moual N, Kennedy SM, Kauffmann F. Occupational exposures and asthma in 14,000 adults from the general population. Am J Epidemiol. 2004;160:1108–16. doi: 10.1093/aje/kwh316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Kogevinas M, Zock JP, Jarvis D, et al. Exposure to substances in the workplace and new-onset asthma: an international prospective population-based study (ECRHS-II) Lancet. 2007;370:336–41. doi: 10.1016/S0140-6736(07)61164-7. [DOI] [PubMed] [Google Scholar]
- 188.Troisi RJ, Speizer FE, Willett WC, et al. Menopause, postmenopausal estrogen preparations, and the risk of adult-onset asthma. A prospective cohort study. Am J Respir Crit Care Med. 1995;152:1183–8. doi: 10.1164/ajrccm.152.4.7551368. [DOI] [PubMed] [Google Scholar]
- 189.Bakerly ND, Moore VC, Vellore AD, et al. Fifteen-year trends in occupational asthma: data from the Shield surveillance scheme. Occup Med (Lond) 2008;58:169–74. doi: 10.1093/occmed/kqn007. [DOI] [PubMed] [Google Scholar]
- 190.Gilliland FD, Islam T, Berhane K, et al. Regular smoking and asthma incidence in adolescents. Am J Respir Crit Care Med. 2006;174:1094–100. doi: 10.1164/rccm.200605-722OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Tetrault JM, Crothers K, Moore BA, et al. Effects of marijuana smoking on pulmonary function and respiratory complications: a systematic review. Arch Intern Med. 2007;167:221–8. doi: 10.1001/archinte.167.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Taylor DR, Fergusson DM, Milne BJ, et al. A longitudinal study of the effects of tobacco and cannabis exposure on lung function in young adults. Addiction. 2002;97:1055–61. doi: 10.1046/j.1360-0443.2002.00169.x. [DOI] [PubMed] [Google Scholar]
- 193.Jaakkola MS, Ieromnimon A, Jaakkola JJ. Are atopy and specific IgE to mites and molds important for adult asthma? J Allergy Clin Immunol. 2006;117:642–8. doi: 10.1016/j.jaci.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 194.McCreanor J, Cullinan P, Nieuwenhuijsen MJ, et al. Respiratory effects of exposure to diesel traffic in persons with asthma. N Engl J Med. 2007;357:2348–58. doi: 10.1056/NEJMoa071535. [DOI] [PubMed] [Google Scholar]
- 195.Chen CH, Xirasagar S, Lin HC. Seasonality in adult asthma admissions, air pollutant levels, and climate: a population-based study. J Asthma. 2006;43:287–92. doi: 10.1080/02770900600622935. [DOI] [PubMed] [Google Scholar]
- 196.Johnston FH, Webby RJ, Pilotto LS, et al. Vegetation fires, particulate air pollution and asthma: a panel study in the Australian monsoon tropics. Int J Environ Health Res. 2006;16:391–404. doi: 10.1080/09603120601093642. [DOI] [PubMed] [Google Scholar]