Abstract
Melatonin is produced by the pineal gland and plays a role in regulating circadian rhythm. It influences the physiologic processes, such as the activation of the immune system and the antioxidant function. Melatonin has been reported in the samples of patients with periodontitis. Therefore, the role of melatonin in periodontal diseases must be appraised. Using the strategy of electronic search of various databases, we included studies, published until December 2021, measuring the expression of melatonin in patient samples and evaluating the effect of periodontal therapy on melatonin expression. This review also included studies evaluating the effect of melatonin supplementation on periodontal parameters. In total, 15 articles fulfilled the study inclusion criteria. The results revealed that melatonin is negatively correlated with the severity of periodontal diseases, and melatonin supplementation reduces the levels of periodontal inflammatory parameters. Hence, melatonin has a role in periodontal diseases, but additional studies are warranted to substantiate its use as a biomarker and host modulatory agent.
Keywords: Antioxidant, biomarker, host modulation, melatonin, periodontitis
INTRODUCTION
Periodontal diseases are chronic inflammatory diseases of the tissues supporting and surrounding the teeth. The prominent causative gram-negative bacteria in the dental plaque trigger the disease process by inducing an excessive host immune response. While counteracting the bacterial attack, this excessive host response leads to the destruction of periodontal tissues by secreting high levels of inflammatory cytokines, pro-osteoclastogenic factors, and matrix metalloproteinases.[1,2] The disease process can lead to the generation of free radicals such as reactive oxygen and nitrogen species during periodontal diseases.[3,4] This increased free radical production further decreases the antioxidant defense. This imbalance between the pro-oxidant and antioxidant systems may further result in oxidative attack and extensive deterioration of periodontal structures.[5,6]
Melatonin is a hormone synthesized and secreted by the pineal gland. This hormone plays a role in physiologic processes such as circadian rhythm control, immune system activation, and body temperature regulation.[7,8] Melatonin also has an antioxidant function as it serves as a direct free radical scavenger, stimulates antioxidative enzyme production and increases its efficiency.[9]
Melatonin levels are significantly decreased in the saliva, serum, and gingival crevicular fluid (GCF) of periodontitis patients compared with healthy controls.[10,11,12,13] The antioxidant function of melatonin suggests that this hormone is involved in the pathogenic processes of periodontal diseases.[9] Thus, the role of melatonin in periodontal diseases needs to be assessed.
This structured review evaluates the role of melatonin in periodontal diseases by addressing the following questions:
What are the levels of melatonin in periodontal health and disease? Is there a change in melatonin levels with increasing severity of the disease?
What is the effect of periodontal therapy on melatonin levels?
Which samples are used to assess melatonin levels?
What is the role of melatonin in periodontal therapy?
MATERIALS AND METHODS
Search strategy
To address the aforementioned questions, a comprehensive literature search of the following databases was performed using the keywords melatonin and periodontal diseases. We searched for papers published until December 2021. No limits and language restrictions were applied during the electronic search to obtain all the relevant articles pertaining to the review topic. In addition, a manual search for articles was conducted.
The search strategy is represented in Figure 1.
Figure 1.
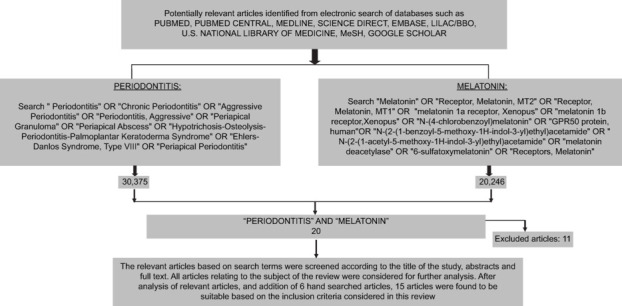
Selection flow chart depicting the selected articles
Databases
PUBMED
PUBMED CENTRAL
MEDLINE
SCIENCE DIRECT
EMBASE
LILAC
U.S. NATIONAL LIBRARY OF MEDICINE
MeSH
GOOGLE SCHOLAR.
Inclusion criteria
Studies associating melatonin levels and different types of periodontal diseases or disease severity were included. Clinical trials assessing melatonin levels and the influence of melatonin on periodontal therapy were also included.
Exclusion criteria
In vitro studies (both human and animal) and case reports were excluded.
Search results
The systematic search in all electronic databases based on the relevance of the title and abstract to the topic of interest returned 26 articles. The search was completed by checking the reference terms and the key words given in the relevant articles. A manual search was also conducted. Full text for the relevant articles fulfilling the inclusion criteria was retrieved. After assessing the full text, 15 articles relevant to this review and satisfying the inclusion criteria were subjected to data extraction.
Data extraction
Data were extracted by two independent review authors. In case of any disagreement on the inclusion of certain articles, a discussion was conducted to resolve it. When a study did not report raw data but included precise graphical representations, the data were extracted. The articles were classified based on the levels of evidence given by the Centre for Evidence-Based Medicine (available online at http://www.cebm.net/).
RESULTS
In total, 15 articles were selected according to the inclusion and exclusion criteria. Table 1 presents the general information regarding the articles. Table 2 presents the level of evidence of the selected articles.
Table 1:
General information of selected articles
| Author | Study design | Results |
|---|---|---|
| Cutando A et al. 2006[10] | Cross sectional study | There is a significant correlation between Community Periodontal Index (CPI) and Salivary/Plasma melatonin ratios. As the degree of periodontal disease increased, the salivary melatonin level decreased. |
| Srinath R et al 2010[13] | Cross sectional study | Salivary and GCF melatonin levels (mean: 2.17 pg/ml and 1.54 pg/ml respectively) were found to be reduced to lowest concentrations in chronic periodontitis. |
| Mhaske n et al 2010[14] |
Cross sectional study | A negative association between the salivary melatonin levels and periodontal severity was seen. |
| Bertl K et al 2013[15] | Longitudinal study | Periodontal therapy resulted in a statistically significant increase of the salivary melatonin levels. |
| Almughrabi OM et al 2013[16] | Cross sectional study | Progressive decreases in the salivary and GCF melatonin levels are seen from health to periodontitis groups. |
| Bertl K et al 2013[15] | Longitudinal study | Significant negative correlation was seen between change in melatonin levels and bleeding on probing after treatment (P=0.02) |
| Hagh L et al 2013[17] | Longitudinal study | The non-surgical treatment significantly increased salivary melatonin levels in severe and moderate periodontitis and gingivitis groups. |
| Hagh L et al 2014[18] | Cross- sectional study | Healthy subjects had a significantly higher salivary melatonin level compared to patients with gingivitis and there is a significant difference between salivary melatonin levels in patients with gingivitis and periodontitis. |
| Balaji TM et al. 2015[19] | Cross- sectional study | There was no significant difference in plasma (P=0.933) and salivary (P=0.266) levels of melatonin in the two groups. |
| Ghallab NA et al 2016[20] | Cross- sectional study | GCF-MDA levels were significantly higher in the GAgP group compared to CP, and higher in CP group compared to the C group. |
| Lodhi K et al 2016[21] | Cross-sectional study | The melatonin levels were positively significant related to gingival index and probing depth. |
| Bazyar H et al 2018[23] | Randomized Controlled Trial | The mean serum levels of melatonin were significantly increased post-intervention (4.52±1.78 and 5.03±1.68 pg/mL, respectively; P=0.005). |
Table 2:
Level of evidence of selected articles based on the oxford centre for evidence-based medicine – levels of evidence criteria {AVAILABLE ON http://www.cebm.net/}
| Author | Study design | Level of evidence |
|---|---|---|
| Cutando A et al. 2006[11] | Cross sectional study | 3b |
| Gomez-Moreno G. et al. 2007[12] | Cross sectional study | 3b |
| Srinath R et al. 2010[13] | Cross sectional study | 3b |
| Mhaske N et al. 2010[14] | Cross sectional study | 3b |
| Bertl K et al. 2012[15] | Longitudinal study | 2b |
| Almughrabi OM et al. 2013[16] | Cross sectional study | 3b |
| Bertl K et al. 2013[17] | Longitudinal study | 2b |
| Hagh L et al. 2013[18] | Longitudinal study | 2b |
| Hagh L et al. 2014[19] | Cross- sectional study | 3b |
| Balaji TM et al. 2015[20] | Cross- sectional study | 3b |
| Ghallab NA et al. 2016[21] | Cross- sectional study | 3b |
| Lodhi K et al. 2016[22] | Cross- sectional study | 3b |
| El-Sharkawy H et al. 2018[23] | Randomized controlled trial | 1b |
| Bazyar H et al. 2018[24] | Randomized controlled trial | 1b |
| Tinto M et al. 2018[25] | Randomized controlled trial | 1b |
Melatonin levels in periodontal disease
The melatonin concentration was estimated in 13 studies. Nine studies compared melatonin levels in healthy and chronic periodontitis patients.[13,14,15,16,17,18,19,20,21] Five studies compared melatonin levels in healthy people and patients with chronic periodontitis and gingivitis.[13,16,17,18,21] Four studies estimated melatonin levels in periodontitis patients, but the type of periodontitis was not specified.[11,12,22,23] Three studies reported melatonin levels in patients with aggressive periodontitis.[15,16,20] Bertl K et al.[15] included patients with aggressive periodontitis in the study but did not mention any specific group for the aggressive periodontitis patients and specific estimation of melatonin levels for that group. Melatonin levels negatively correlated with the severity of periodontal disease and periodontal parameters and indices in all included studies, except one study,[21] which reported an increase in salivary melatonin levels with increased severity of periodontal diseases, contrary to other reports.[21]
Effect of periodontal therapy on melatonin levels
Four studies evaluating the effects of non-surgical therapy on melatonin levels reported that periodontitis treatment increased melatonin levels in patients.[15,17,22,23] An improvement in clinical parameters negatively correlated with the increase in melatonin levels. In this regard, Bazyar H et al.[23] investigated the effect of non-surgical therapy, along with melatonin supplementation, in an intervention group and a placebo group. In that study, the mean serum melatonin levels were significantly higher in the intervention group than in the placebo group.
Samples used for assessment
Saliva samples are most commonly used for estimating melatonin levels.[11,12,16,17,18,19,21] GCF samples were used in four studies,[11,13,16,19] while serum samples were used in two studies for analyzing melatonin levels.[15,23] Plasma samples were used for estimating melatonin levels in three studies.[11,12,19] Balaji TM et al. used gingival samples for assessing melatonin levels.[19]
Influence of melatonin on periodontal therapy
Three studies reported the influence of melatonin on periodontal therapy.[23,24,25] These clinical trials reported a significant reduction in inflammatory and periodontal parameters in the intervention groups compared with the control groups. El-Sharkawy H et al. and Bazyar H et al. included patients with systemic diseases (primary insomnia and type II diabetes, respectively)[23,24] and suggested that melatonin can be used as a non-surgical and reliable adjunctive therapy for the management of periodontitis.
DISCUSSION
Melatonin in periodontal health and disease
Periodontal tissue destruction is a result of the abnormal response against specific bacterial groups. Activation of oxidative stress and the redox-sensitive gene transcription factors such as nuclear factor kappa B, along with the production of proinflammatory cytokines, causes further periodontal tissue destruction. This host response is characterized by high levels of inflammation and excessive production of proteolytic enzymes and reactive oxygen species (ROS).[26] These oxidation-related changes and increased ROS production with the generation of free radicals cause delayed migration of neutrophils into the tissues, thereby leading to further destruction and metabolic changes.[4,27,28]
Melatonin has a protective role and exhibits a negative association with the severity of periodontal diseases, which can be attributed to its antioxidant and immunomodulatory properties. Melatonin has the unique property of “cascade reaction” wherein it serves as a potent antioxidant and free radical scavenger along with its metabolites, thereby stimulating antioxidant enzymes.[29,30] Along with its antioxidant properties, melatonin reduces the synthesis of proinflammatory cytokines and adhesion molecules, thereby reducing periodontal tissue destruction.[31]
Melatonin secretion peaks between 24:00 h and 02:00 h and is the lowest between 12:00 h and 14:00 h. Melatonin secretion also reduces with ageing.[7] Melatonin was found in all the samples assessed, with saliva samples being the most common. The GCG revealed a 60% reduction in melatonin levels compared with serum melatonin levels.[13,32] Salivary melatonin levels do not reflect the absolute serum concentrations as only the free melatonin fraction diffuses passively into the saliva.[33] Moreover, 24%–33% of plasma melatonin passes into the mouth via salivary glands, while the remaining 70% is bound to albumin and remains in circulation.[34] TM Balaji et al. found melatonin levels in gingival tissue samples, which could be attributable to the release of melatonin from gingival mast cells or its diffusion into the gingiva from systemic circulation.[19,35] These observations should be further validated to elucidate the mechanism of melatonin synthesis and its presence in gingival tissues.
Of all the studies included in this review, only one exhibited a contradictory result where the salivary melatonin levels increased from healthy to gingivitis to periodontitis groups.[21] The authors suggest that this increase was due to an increase in signals owing to the increased severity of periodontal inflammation in the oral cavity, thereby causing an increased protective response.[21,36,37]
Melatonin as a host modulatory agent in periodontal therapy
Various studies have evaluated melatonin as a host modulatory agent for periodontal therapy. El-Sharkawy H et al., Bazyar H et al., and Tinto M et al. presented the benefits of melatonin supplementation on periodontal parameters and reduction of inflammatory markers, thereby offering evidence supporting the benefits of melatonin use as adjunctive therapy for non-surgical periodontal treatment.[23,24,25]
Melatonin also possesses antimicrobial properties against certain groups of bacteria and viruses.[38,39] Zhou W et al.[40] evaluated the effects of melatonin against Porphyromonas gingivalis and found that melatonin could inhibit biofilm formation, in addition to acting on the lipopolysaccharide, thereby decreasing the viability of P. gingivalis.
Melatonin has immunomodulatory, antioxidant, and anti-inflammatory properties and has been shown to promote osteoblast proliferation, thereby enhancing bone formation.[41,42,43] The use of calcium aluminum scaffolds containing melatonin and platelet-rich plasma had a proliferative effect on human osteoblasts, thereby offering avenues in guided tissue regeneration applications.[44]
Reports have suggested the use of melatonin for implant therapy. In vitro studies have evaluated the use of melatonin in implant sites and its use along with growth factors around implants to improve the osteogenic effects of bone grafts and osseointegration of implants.[45,46,47] Clinical trials have also reported that using melatonin for osseointegration of dental implants is beneficial.[48] These investigations warrant further studies to validate the role of melatonin in periodontal and implant therapy.
CONCLUSIONS
This structured review shows that melatonin plays a role in periodontal disease, and the conclusions are as follows:
Melatonin levels negatively correlated with the severity of periodontal disease and periodontal parameters and indices in all the included studies, except one.
Melatonin levels increased following non-surgical periodontal therapy.
Saliva was the most commonly assessed sample for melatonin levels. Other samples included GCF, serum, plasma, and gingival tissue samples.
Melatonin supplementation had a beneficial effect on periodontal parameters, and it reduced the level of proinflammatory markers.
Evidence shows that melatonin can be used as a marker for periodontitis and a host modulation agent in periodontal therapy. However, additional interventional and longitudinal studies are needed to verify its suitability as a marker or treatment modality.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Brook I. Microbiology and management of periodontal infections. Gen Dent. 2003;51:424–8. [PubMed] [Google Scholar]
- 2.Holtfreter B, Kocher T, Hoffmann T, Desvarieux M, Micheelis W. Prevalence of periodontal disease and treatment demands based on a German dental survey (DMS IV) J Clin Periodontol. 2010;37:211–9. doi: 10.1111/j.1600-051X.2009.01517.x. [DOI] [PubMed] [Google Scholar]
- 3.Gustafsson A, Åsman B. Increased release of free oxygen radicals from peripheral neutrophils in adult periodontitis after Feγ‐receptor stimulation. J Clin Periodontol. 1996;23:38–44. doi: 10.1111/j.1600-051x.1996.tb00502.x. [DOI] [PubMed] [Google Scholar]
- 4.Kimura S, Yonemura T, Kaya H. Increased oxidative product formation by peripheral blood polymorphonuclear leukocytes in human periodontal diseases. J Periodontal Res. 1993;28:197–203. doi: 10.1111/j.1600-0765.1993.tb01069.x. [DOI] [PubMed] [Google Scholar]
- 5.Akalin FA, Toklu E, Renda N. Analysis of superoxide dismutase activity levels in gingiva and gingival crevicular fluid in patients with chronic periodontitis and periodontally healthy controls. J Clin Periodontol. 2005;32:238–43. doi: 10.1111/j.1600-051X.2005.00669.x. [DOI] [PubMed] [Google Scholar]
- 6.Sies H. Oxidative stress: Oxidants and antioxidants. Exp Physiol. 1997;82:291–5. doi: 10.1113/expphysiol.1997.sp004024. [DOI] [PubMed] [Google Scholar]
- 7.Reiter RJ. Pineal melatonin: Cell biology of its synthesis and of its physiological interactions. Endocr Rev. 1991;12:151–80. doi: 10.1210/edrv-12-2-151. [DOI] [PubMed] [Google Scholar]
- 8.Kumasaka S, Shimozuma M, Kawamoto T, Mishima K, Tokuyama R, Kamiya Y, et al. Possible involvement of melatonin in tooth development: Expression of melatonin 1a receptor in human and mouse tooth germs. Histochem Cell Biol. 2010;133:577–84. doi: 10.1007/s00418-010-0698-6. [DOI] [PubMed] [Google Scholar]
- 9.Reiter RJ, Tan DX, Mayo JC, Sainz RM, Leon J, Czarnocki Z. Melatonin as an antioxidant: Biochemical mechanisms and pathophysiological implications in humans. Acta Biochim Pol. 2003;50:1129–46. [PubMed] [Google Scholar]
- 10.Cutando A, Gómez-Moreno G, Villalba J, Ferrera MJ, Escames G, Acuña-Castroviejo D. Relationship between salivary melatonin levels and periodontal status in diabetic patients. J Pineal Res. 2003;35:239–44. doi: 10.1034/j.1600-079x.2003.00075.x. [DOI] [PubMed] [Google Scholar]
- 11.Cutando A, Galindo P, Gómez-Moreno G, Arana C, Bolaños J, Acuña-Castroviejo D, et al. Relationship between salivary melatonin and severity of periodontal disease. J Periodontol. 2006;77:1533–8. doi: 10.1902/jop.2006.050287. [DOI] [PubMed] [Google Scholar]
- 12.Gómez-Moreno G, Cutando-Soriano A, Arana C, Galindo P, Bolaños J, Acuña-Castroviejo D, et al. Melatonin expression in periodontal disease. J Periodontal Res. 2007;42:536–40. doi: 10.1111/j.1600-0765.2007.00978.x. [DOI] [PubMed] [Google Scholar]
- 13.Srinath R, Acharya AB, Thakur SL. Salivary and gingival crevicular fluid melatonin in periodontal health and disease. J Periodontol. 2010;81:277–83. doi: 10.1902/jop.2009.090327. [DOI] [PubMed] [Google Scholar]
- 14.Mhaske N, Marawar P, Sheker A, Mote N. Evaluation of melatonin levels in saliva in periodontal health and disease: A clinico-biochemical study. J Int Clin Dent Res Organ. 2010;2:119–25. [Google Scholar]
- 15.Bertl K, Schoiber A, Haririan H, Laky M, Steiner I, Rausch WD, et al. Non-surgical periodontal therapy influences salivary melatonin levels. Clin Oral Investig. 2013;17:1219–25. doi: 10.1007/s00784-012-0801-6. [DOI] [PubMed] [Google Scholar]
- 16.Almughrabi OM, Marzouk KM, Hasanato RM, Shafik SS. Melatonin levels in periodontal health and disease. J Periodontal Res. 2013;48:315–21. doi: 10.1111/jre.12010. [DOI] [PubMed] [Google Scholar]
- 17.Hagh LG, Yousefimanesh H, Mohammadi F, Ahangarpour A. Evaluation of nonsurgical treatment effects on salivary melatonin level in periodontal disease: A radioimmunoassay study. World J Dent. 2013;4:217–23. [Google Scholar]
- 18.Hagh L, Zakavi F, Daraeighadikolaei A, Ahangarpour A, Hajati S, Daraeighadikolaei A. Salivary melatonin and the severity of attachment loss: A case-control study. J Oral Dis. 2014;2014:1–4. [Google Scholar]
- 19.Balaji TM, Vasanthi HR, Rao SR. Gingival, plasma and salivary levels of melatonin in periodontally healthy individuals and chronic periodontitis patients: A pilot study. J Clin Diagn Res. 2015;9:ZC23–5. doi: 10.7860/JCDR/2015/11311.5652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghallab NA, Hamdy E, Shaker OG. Malondialdehyde, superoxide dismutase and melatonin levels in gingival crevicular fluid of aggressive and chronic periodontitis patients. Aust Dent J. 2016;61:53–61. doi: 10.1111/adj.12294. [DOI] [PubMed] [Google Scholar]
- 21.Lodhi K, Saimbi CS, Khan MA, Nath C, Shukla R. Evaluation of melatonin levels in saliva in gingivitis and periodontitis cases: A pilot study. Contemp Clin Dent. 2016;7:519–23. doi: 10.4103/0976-237X.194115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bertl K, Schoiber A, Haririan H, Laky M, Andrukhov O, Womastek I, et al. The influence of non-surgical periodontal therapy on salivary melatonin levels: A pilot study. 2013 doi: 10.1007/s00784-012-0801-6. Available from: https://www.gbo.com/fileadmin/user_upload/Downloads/Scientific_Publications/Scientific_Publications_Preanalytics/TheInfluenceOfNonSurgical PeriodontalTherapyOnSalivaryMelatoninLevels.pdf . [DOI] [PubMed] [Google Scholar]
- 23.Bazyar H, Gholinezhad H, Moradi L, Salehi P, Abadi F, Ravanbakhsh M, et al. The effects of melatonin supplementation in adjunct with non-surgical periodontal therapy on periodontal status, serum melatonin and inflammatory markers in type 2 diabetes mellitus patients with chronic periodontitis: A double-blind, placebo-controlled trial. Inflammopharmacology. 2019;27:67–76. doi: 10.1007/s10787-018-0539-0. [DOI] [PubMed] [Google Scholar]
- 24.El-Sharkawy H, Elmeadawy S, Elshinnawi U, Anees M. Is dietary melatonin supplementation a viable adjunctive therapy for chronic periodontitis?-A randomized controlled clinical trial. J Periodontal Res. 2019;54:190–7. doi: 10.1111/jre.12619. [DOI] [PubMed] [Google Scholar]
- 25.Tinto M, Sartori M, Pizzi I, Verga A, Longoni S. Melatonin as host modulating agent supporting nonsurgical periodontal therapy in patients affected by untreated severe periodontitis: A preliminary randomized, triple-blind, placebo-controlled study. J Periodontal Res. 2020;55:61–7. doi: 10.1111/jre.12686. [DOI] [PubMed] [Google Scholar]
- 26.Chapple IL, Matthews JB. The role of reactive oxygen and antioxidant species in periodontal tissue destruction. Periodontol 2000. 2007;43:160–232. doi: 10.1111/j.1600-0757.2006.00178.x. [DOI] [PubMed] [Google Scholar]
- 27.Valko M, Leibfritz D, Moncol J, Cronin MT, Mazur M, Telser J. Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol. 2007;39:44–84. doi: 10.1016/j.biocel.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 28.Ozdem M. Melatonin: It’s antioxidant effects on periodontal disease. J Healthc Commun. 2018;3(1):17. [Google Scholar]
- 29.Arnao M.B., Hernández-Ruiz J. The physiological function of melatonin in plants. Plant Signal Behav. 2006;1:89–95. doi: 10.4161/psb.1.3.2640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kara A, Akman S, Ozkanlar S, Tozoglu U, Kalkan Y, Canakci CF, et al. Immune modulatory and antioxidant effects of melatonin in experimental periodontitis in rats. Free Radic Biol Med. 2013;55:21–6. doi: 10.1016/j.freeradbiomed.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 31.Reiter RJ. Interactions of the pineal hormone melatonin with oxygen-centered free radicals: A brief review. Braz J Med Biol Res. 1993;26:1141–55. [PubMed] [Google Scholar]
- 32.Cutando A, Gomez-Moreno G, Arana C, Castroviejo-Acuna D, Reiter JR. Melatonin: Potential functions in the oral cavity. J Periodontol. 2007;78:1094–102. doi: 10.1902/jop.2007.060396. [DOI] [PubMed] [Google Scholar]
- 33.Laakso ML, Porkka-Heiskanen T, Alila A, Stenberg D, Johansson G. Correlation between salivary and serum melatonin: Dependence on serum melatonin levels. J Pineal Res. 1990;9:39–50. doi: 10.1111/j.1600-079x.1990.tb00692.x. [DOI] [PubMed] [Google Scholar]
- 34.McIntyre IM, Norman TR, Burrows GD, Armstrong SM. Melatonin rhythm in human plasma and saliva. J Pineal Res. 1987;4:177–83. doi: 10.1111/j.1600-079x.1987.tb00854.x. [DOI] [PubMed] [Google Scholar]
- 35.Maldonado MD, Mora-Santos M, Naji L, Carrascosa-Salmoral MP, Naranjo MC, Calvo JR. Evidence of melatonin synthesis and release by mast cells. Possible modulatory role on inflammation. Pharmacol Res. 2010;62:282–7. doi: 10.1016/j.phrs.2009.11.014. [DOI] [PubMed] [Google Scholar]
- 36.Giordano M, Palermo MS. Melatonin-induced enhancement of antibody-dependent cellular cytotoxicity. J Pineal Res. 1991;10:117–21. doi: 10.1111/j.1600-079x.1991.tb00827.x. [DOI] [PubMed] [Google Scholar]
- 37.Morrey KM, McLachlan JA, Serkin CD, Bakouche O. Activation of human monocytes by the pineal hormone melatonin. J Immunol. 1994;153:2671–80. [PubMed] [Google Scholar]
- 38.Tekbas OF, Ogur R, Korkmaz A, Kilic A, Reiter RJ. Melatonin as an antibiotic: New insights into the actions of this ubiquitous molecule. J Pineal Res. 2008;44:222–6. doi: 10.1111/j.1600-079X.2007.00516.x. [DOI] [PubMed] [Google Scholar]
- 39.Boga JA, Coto-Montes A, Rosales-Corral SA, Tan DX, Reiter RJ. Beneficial actions of melatonin in the management of viral infections: A new use for this “molecular handyman”? Rev Med Virol. 2012;22:323–38. doi: 10.1002/rmv.1714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhou W, Zhang X, Zhu CL, He ZY, Liang JP, Song ZC. Melatonin receptor agonists as the “perioceutics” agents for periodontal disease through modulation of porphyromonas gingivalis virulence and inflammatory response. PLoS One. 2016;11:e0166442.. doi: 10.1371/journal.pone.0166442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cobo-Vázquez C, Fernández-Tresguerres I, Ortega-Aranegui R, López-Quiles J. Effects of local melatonin application on post-extraction sockets after third molar surgery. A pilot study. Med Oral Patol Oral Cir Bucal. 2014;19:e628–33.. doi: 10.4317/medoral.19851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Roth JA, Kim BG, Lin WL, Cho MI. Melatonin promotes osteoblast differentiation and bone formation. J Biol Chem. 1999;274:22041–7. doi: 10.1074/jbc.274.31.22041. [DOI] [PubMed] [Google Scholar]
- 43.Luchetti F, Canonico B, Bartolini D, Arcangeletti M, Ciffolilli S, Murdolo G, et al. Melatonin regulates mesenchymal stem cell differentiation: A review. J Pineal Res. 2014;56:382–97. doi: 10.1111/jpi.12133. [DOI] [PubMed] [Google Scholar]
- 44.Clafshenkel WP, Rutkowski JL, Palchesko RN, Romeo JD, McGowan KA, Gawalt ES, et al. A novel calcium aluminateemelatonin scaffold enhances bone regeneration within a calvarial defect. J Pineal Res. 2012;53:206–18. doi: 10.1111/j.1600-079X.2012.00989.x. [DOI] [PubMed] [Google Scholar]
- 45.Muñoz F, López-Peña M, Miño N, Gómez-Moreno G, Guardia J, Cutando A. Topical application of melatonin and growth hormone accelerates bone healing around dental implants in dogs. Clin Implant Dent Relat Res. 2012;14:226–35. doi: 10.1111/j.1708-8208.2009.00242.x. [DOI] [PubMed] [Google Scholar]
- 46.Takechi M, Tatehara S, Satomura K, Fujisawa K, Nagayama M. Effect of FGF-2 and melatonin on implant bone healing: A histomorphometric study. J Mater Sci Mater Med. 2008;19:2949–52. doi: 10.1007/s10856-008-3416-3. [DOI] [PubMed] [Google Scholar]
- 47.Calvo‐Guirado JL, Aguilar Salvatierra A, Gargallo‐Albiol J, Delgado‐Ruiz RA, Maté Sanchez JE, Satorres‐Nieto M. Zirconia with laser‐modified microgrooved surface vs. titanium implants covered with melatonin stimulates bone formation. Experimental study in tibia rabbits. Clin Oral Implants Res. 2015;26:1421–9. doi: 10.1111/clr.12472. [DOI] [PubMed] [Google Scholar]
- 48.El-Gammal MY, Salem AS, Anees MM, Tawfik MA. Clinical and radiographic evaluation of immediate loaded dental implants with local application of melatonin: A preliminary randomized controlled clinical trial. J Oral Implantol. 2016;42:119–25. doi: 10.1563/aaid-joi-D-14-00277. [DOI] [PubMed] [Google Scholar]


