Abstract
Hypertension has long been a worldwide health concern. Our aim was to investigate the prevalence, awareness, treatment, and control rates of hypertension and analyze the factors related to hypertension among adult residents of the coastal areas of Tianjin, China. This was a cross-sectional study. Adults aged 35 to 75 years were selected for the study using cluster random sampling methods. Detailed information was collected via face-to-face surveys and medical checkups. We assessed the rates of hypertension in the total population and sub-populations and used multivariable logistic regression to identify the factors associated with the prevalence and the control of hypertension. In total, 6305 participants aged 55.22 ± 10.37 years were included in this study. Approximately 49.8% (95% confidence interval [CI]: 48.5%–51.1%) of the population had hypertension; the prevalence increased with age and body mass index (all P < .001). Multivariable logistic regression showed that the odds ratio of hypertension was 5.93 times more in participants aged 65 to 75 years than in those aged 35 to 44 (95% CI: 4.85–7.26, P < .001). The odds ratio of hypertension was 3.63 times more in obese participants than in those of normal weight (95% CI: 3.08–4.28, P < .001). Additionally, the awareness, treatment, control, and control under-treatment rates of hypertension were 89.7%, 83.6%, 54.4%, and 60.5%, respectively. Factors associated with having controlled hypertension included sex, body mass index, and dyslipidemia (all P < .01). Our study identified that in the coastal area of Tianjin, China, about half have hypertension, also the region has high rates of hypertension awareness, treatment and control, and more than half of hypertension patients receiving treatment have controlled hypertension.
Keywords: awareness, control, hypertension, prevalence, treatment
1. Introduction
Hypertension is one of the most important modifiable cardiovascular and cerebrovascular risk factors, contributing to half of the coronary heart disease burden and almost two-thirds of the cerebrovascular disease burden.[1] Owing to widespread use of antihypertensive medications, global mean blood pressure (BP) has remained constant or decreased slightly over the past 4 decades. By contrast, the prevalence of hypertension has increased, especially in low- and middle-income countries.[2] In China, with its rapid economic development and the remarkable improvement of living standards in recent years, the number of hypertensive patients has been increasing. According to the China Report on Cardiovascular Health and Disease in 2020, >245 million Chinese adults have been diagnosed as hypertensive, and the number with high-normal BP has reached 435 million.[3]
Although hypertension is a preventable disease with increasing prevalence, the proportions of hypertension awareness, treatment, and BP control are low, particularly in low- and middle-income countries.[2] In the 2019 Lao STEP survey, only 39.9% of the population indicated that they had ever had their BP measured by a healthcare worker, and 81.8% of the population with hypertension were not on medication.[4] In national population-based surveys in China, despite modest improvements in hypertension awareness, treatment, and control since 2004, rates remained low; in 2018, 38.3% (36.3%–40.4%) of the sample were aware of their diagnosis, 34.6% (32.6%–36.7%) were taking prescribed antihypertensive medications, and only 12.0% (10.6%–13.4%) had achieved control.[5]
The status of hypertension varies widely with different geographic, demographic, and socioeconomic factors.[6] In China, recent studies have shown that the prevalence of hypertension was the highest in the northeast region (53.6%),[6] followed by the eastern region (49.8%)[7] and the central region (43.6%),[8] with the lowest rates in the southwestern region (38.4%).[9] BP level, hypertension category, and hypertension prevalence, awareness, treatment, and control were observed to be unequally distributed among the subgroups and by geographical region.[10] However, in municipalities such as Tianjin, especially in coastal areas, there is currently limited data on the prevalence, awareness, treatment, and control of hypertension. From 2007, the local government initiated the basic public health services project to provide medical and health services for residents in chronic disease management including hypertension.[11] In order to provide better services for the population covered by the basic public health project, understanding the prevalence and the management of chronic diseases in the area is essential before the implementation of these initiatives yearly. For areas with distinct population characteristics, understanding the prevalence, the awareness, and the management of hypertension and its related factors is vital for hypertension prevention and control. This study aimed to estimate up-to-date prevalence, awareness, treatment, and control of hypertension, as well as their influencing factors, among adults in a coastal district of Tianjin, China, to provide useful information to guide targeted prevention and control strategies for hypertension and cardiovascular disease.
2. Methods
2.1. Subjects
From May 2022 to December 2022, relying on the National Basic Public Health Service Project, a cardiovascular disease-related screening and survey project was conducted among residents over 35 years old in the coastal area of Tianjin, China. In this study, a cluster random sampling method was used to randomly select 4 of the 21 towns (streets) in the coastal area of Tianjin, China, and take all permanent residents as investigation samples. The survey subjects were residents who had lived at the project site for more than half a year within the year before the survey, and who voluntarily participated and signed a written informed consent. This study was permitted by the Ethics Committee of the National Center for Cardiovascular Disease (approval number: 2014-574, approval date: July 2014).
2.2. Information collection
The survey methods and contents were carried out according to the requirements of the project manual. The investigators were uniformly trained; the survey included questionnaires, physical checkups, and laboratory tests. The questionnaire included demographic characteristics, such as age, ethnic group, education, marital status, annual income, health insurance, history of the disease, and lifestyle factors including smoking and drinking. Physical checkups included BP, height, weight, and waist circumference. Laboratory tests included fasting blood glucose (FBG) and fasting blood lipids.
BP was measured using electronic sphygmomanometers (Omron HEM-7430, Omron Corporation, Kyoto, Japan). After 5 minutes of sitting, the BP of the right upper arm was measured twice, and the average BP was recorded. If the difference between the 2 systolic BP (SBP) measurements was >10 mm Hg (1 mm Hg = 0.133 kPa), a third measurement was performed, and the average BP value of the 3 readings was used. Height and weight were measured using an electronic height and weight meter. The screening subjects took off their shoes, hats, and coats, and stood during the measurement with their waist and back straight, their arms naturally hanging down, and their eyes in front of them. Height measurements were made in centimeters and were accurate to 0.1 cm. Weight measurements were in kilograms and were accurate to 0.1 kg. Waist circumference was measured at the midpoint of the line between the lower margin of the rib arch and the anterior superior iliac ridge, and measurements were accurate to 0.5 cm.
Laboratory tests were carried out according to the manual of instrument and reagent operation. Fasting venous blood samples (>8 h) were collected from an antecubital vein into tubes containing EDTA, and total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), and FBG concentrations were measured on the same day of the checkups. Serum TC, TG, and FBG levels were determined by enzymatic methods. HDL-C and LDL-C levels were measured using a homogeneous assay (HUMAN, Wiesbaden, Germany).
2.3. Definitions
In this study, hypertension was diagnosed and determined according to the National Clinical Practice Guidelines on the Management of Hypertension (2020 Edition).[12] In short, the diagnosis was determined according to the outpatient BP combined with disease history. Hypertension was defined as having any 1 or more of the following conditions: average SBP of 140 mm Hg or higher or average diastolic BP (DBP) of 90 mm Hg or higher; currently receiving antihypertensive medications or reporting that they had received antihypertensive treatments.
Awareness referred to a self-reported hypertension history or self-reported use of antihypertensive drugs among patients with hypertension. Treatment of hypertension referred to the use of antihypertensive medication among participants with hypertension. Among patients with hypertension, control of hypertension referred to an average SBP < 140 mm Hg and an average DBP < 90 mm Hg among patients with hypertension; control under treatment referred to an average SBP < 140 mm Hg and average DBP < 90 mm Hg after using antihypertensive medication.[12,13]
Body mass index (BMI) was calculated by dividing the weight in kilograms by the height in meters squared. Current smoking was defined as smoking at least 1 cigarette every day. Current drinking was defined as drinking alcohol almost every day or occasionally, including those who had been abstinent for <1 year. Diabetes referred to the use of hypoglycemic medication or a measured FBG level ≥ 7.0 mmol/L or non-FBG level ≥ 11.1 mmol/L.[14] Dyslipidemia referred to either TG ≥ 2.26 mmol/L, TC ≥ 6.22 mmol/L, LDL-C ≥ 4.14 mmol/L, HDL-C < 1.04 mmol/L, or self-reported use of lipid-lowering drugs.[15]
2.4. Statistical analysis
Continuous variables were expressed as mean ± SD and were compared using the t test. Categorical variables were reported as numbers and proportions. Proportions were compared using the Pearson chi-square test or trend chi-square tests. Tests of 2 sides and P < .05 were statistically significant. To analyze the association between individual characteristics and prevalence as well as control under treatment of hypertension, multivariable logistic regression models were built using hypertension prevalence and control under treatment as dependent variables (No = 0, Yes = 1). In the regression model analyzing the prevalence of hypertension, the variable screening method was backward conditional, the probability of a variable entering the equation was 0.05, excluding 0.10, and the other parameters were as per system defaults. In the regression model of hypertension control, the entry method was used for the relevant variables. Multivariable logistic regression was used to estimate adjusted odds ratio (ORs) and 95% confidence interval (CI). Data analysis and processing were completed by professional statistical analysts using SPSS software version 26.00 (Armonk: IBM Corp).
3. Results
3.1. Population characteristics and prevalence of hypertension
In total, 6305 participants (2660 men and 3645 women) aged 55.22 ± 10.37 years (55.36 ± 10.68 years for men and 55.12 ± 10.14 years for women) were included in this study. The characteristics of the study participants according to hypertension status are shown in Table 1. Overall, 49.8% (95% CI: 48.5%–51.1%) of the population had hypertension, including 55.8% of men and 45.5% of women, the prevalence of hypertension in men was higher than that in women (P < .001). The prevalence of hypertension increased with age, and an increasing trend was observed (P < .001). Also, the prevalence of hypertension increased with BMI (P < .001), and the prevalence was 24.0% in the low-BMI group (BMI < 18.5kg/m2) and 69.7% in the obesity group (BMI ≥ 28kg/m2). A higher prevalence of hypertension was also found among those with a lower education level (P < .001). Additionally, the prevalence of hypertension was higher in population who currently smoke or drink or have diabetes or dyslipidemia (all P < .001) (Table 1).
Table 1.
Baseline characteristics of the study population and prevalence of hypertension.
| Without hypertension (n = 3164) | Hypertension (n = 3141) | Total (n = 6305) | χ2/χ2trend/t | P | |
|---|---|---|---|---|---|
| Sex, n (%) | 64.814 | <.001 | |||
| Male | 1177 (44.2) | 1483 (55.8) | 2660 (42.2) | ||
| Female | 1987 (54.5) | 1658 (45.5) | 3645 (57.8) | ||
| Age, yr | 51.45 ± 10.19 | 59.02 ± 9.08 | 55.22 ± 10.37 | −31.126 | <.001 |
| Age groups, n (%) | 808.631 | <.001 | |||
| <45 | 1110 (77.8) | 318 (22.2) | 1426 (22.6) | ||
| 45–55 | 954 (56.7) | 728 (43.3) | 1682 (26.7) | ||
| 55–65 | 749 (37.9) | 1227 (62.1) | 1976 (31.3) | ||
| ≥65 | 351 (28.7) | 870 (71.3) | 1221 (19.4) | ||
| BMI, kg/m2 | 24.35 ± 3.08 | 26.14 ± 3.35 | 25.24 ± 3.34 | −21.988 | <.001 |
| BMI groups, n (%) | 416.441 | <.001 | |||
| <18.5 | 57 (76.0) | 18 (24.0) | 75 (1.2) | ||
| 18.5–23.9 | 1510 (64.3) | 840 (35.7) | 2350 (37.3) | ||
| 24.0–27.9 | 1230 (46.1) | 1437 (53.9) | 2667 (42.3) | ||
| ≥28 | 367 (30.3) | 846 (69.7) | 1213 (19.2) | ||
| Current smoking, n (%) | 983 | 65.197 | <.001 | ||
| No | 2787 (52.4) | 2535 (47.6) | 5322 (84.4) | ||
| Yes | 377 (38.4) | 606 (61.6) | 983 (15.6) | ||
| Current drinking, n (%) | 96.386 | <.001 | |||
| No | 2939 (52.4) | 2675 (47.6) | 5614 (89.0) | ||
| Yes | 225 (32.6) | 466 (67.4) | 691 (11.0) | ||
| Diabetes, n (%) | 436.64 | <.001 | |||
| No | 2728 (57.8) | 1991 (42.2) | 4718 (74.8) | ||
| Yes | 436 (27.5) | 1150 (72.5) | 1586 (25.2) | ||
| Dyslipidemia, n (%) | 280.013 | <.001 | |||
| No | 2620 (56.5) | 2017 (43.5) | 4637 (73.5) | ||
| Yes | 544 (32.6) | 1124 (67.4) | 1668 (26.5) | ||
| Farmer, n (%) | 0.006 | .940 | |||
| No | 3121 (50.2) | 3099 (49.8) | 6220 (98.7) | ||
| Yes | 43 (1.4) | 42 (1.3) | 85 (1.3) | ||
| Education level, n (%) | 278.137 | <.001 | |||
| <High school | 1085 (43.0) | 1436 (57.0) | 2521 (40.0) | ||
| High school | 1064 (46.0) | 1251 (54.0) | 2315 (36.7) | ||
| College or above | 1015 (69.1) | 454 (30.9) | 1469 (23.3) | ||
| Employment status, n (%) | 252.617 | <.001 | |||
| Employed | 2233 (58.2) | 1603 (41.8) | 3836 (60.8) | ||
| Retired | 931 (37.7) | 1538 (62.3) | 2469 (39.2) | ||
| SBP, mm Hg | 119.68 ± 9.67 | 136.82 ± 15.00 | 128.22 ± 15.24 | −53.882 | <.001 |
| DBP, mm Hg | 74.87 ± 6.87 | 82.58 ± 9.96 | 78.71 ± 9.38 | −35.753 | <.001 |
| HR, times/min | 71.41 ± 7.25 | 73.04 ± 9.07 | 72.22 ± 8.25 | −7.886 | <.001 |
| TC, mmol/L | 4.87 ± 1.13 | 5.06 ± 1.26 | 4.96 ± 1.20 | −6.176 | <.001 |
| LDL-C, mmol/L | 2.74 ± 0.89 | 2.92 ± 1.01 | 2.82 ± 0.95 | −7.384 | <.001 |
| HDL-C, mmol/L | 1.37 ± 0.34 | 1.31 ± 0.34 | 1.34 ± 0.34 | 7.788 | <.001 |
| TG, mmol/L | 1.57 ± 0.79 | 1.82 ± 0.91 | 1.69 ± 0.86 | −11.564 | <.001 |
| FPG, mmol/L | 5.71 ± 1.38 | 6.42 ± 1.74 | 6.06 ± 1.61 | −18.032 | <.001 |
| Waist circumference, cm | 83.27 ± 8.63 | 88.86 ± 9.27 | 86.06 ± 9.38 | −24.764 | <.001 |
Continuous variables are presented as mean ± SD. Categorical variables are presented as frequency (%). Age groups and BMI groups were analyzed using trend chi-square.
BMI = body mass index, SBP = systolic blood pressure, DBP= diastolic blood pressure, HR= heart rate, TC= total cholesterol, LDL-C= low-density lipoprotein cholesterol, HDL-C= high-density lipoprotein cholesterol, TG= triglyceride, FPG= fasting plasma glucose.
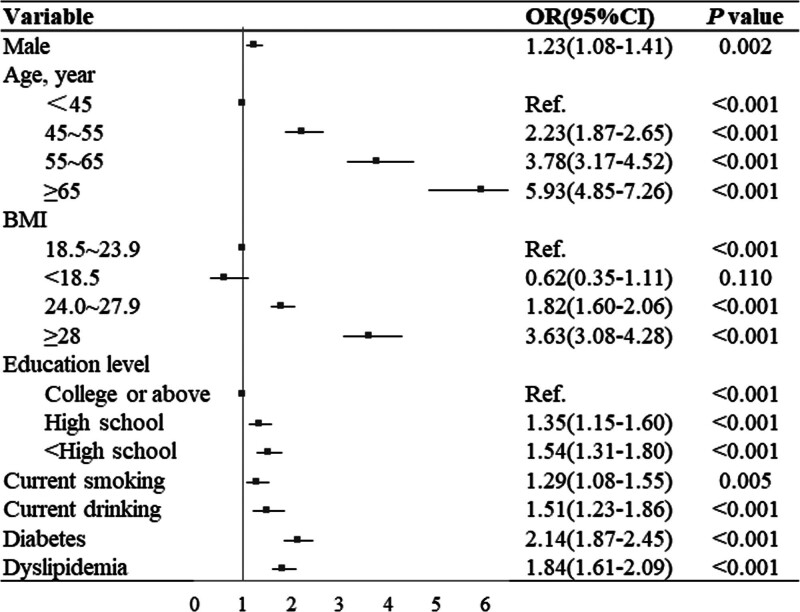
3.2. Factors associated with prevalence of hypertension
ORs and 95% CIs for the associations between sex, age, BMI, educational level, current smoking, current drinking, diabetes, dyslipidemia, and the prevalence of hypertension as determined using multivariable logistic regression models are shown in Figure 1. The OR for hypertension was 5.93 times more in participants aged 65 to 75 years than in those aged 35 to 44 (95% CI: 4.85–7.26, P < .001), and 3.63 times more in participants in the obesity group than those in the normal weight group (95% CI: 3.08–4.28, P < .001). Furthermore, male sex (OR = 1.23, 95% CI: 1.08–1.41, P = .002), lower education level (OR = 1.54, 95% CI: 1.31–1.80, P < .001), current smoking (OR = 1.29, 95% CI: 1.08–1.55, P = .005), current drinking (OR = 1.51, 95% CI: 1.23–1.86, P < .001), diabetes (OR = 2.41, 95% CI: 1.87–2.45, P < .001), and dyslipidemia (OR = 1.84, 95% CI: 1.61–2.09, P < .001) were each significantly associated with the prevalence of hypertension.
Figure 1.
Multivariable logistic regression showing factors associated with prevalence of hypertension. BMI = body mass index, CI = confidence interval, OR = odds ratio, Ref. = Reference.
3.3. Awareness, treatment, and control of hypertension
As indicated in Table 2, among patients with hypertension, the rates of awareness, treatment, and control are 89.7%, 83.6%, and 54.4%. Among those receiving treatment, 60.5% had their hypertension controlled. The proportion of hypertension awareness and treatment was associated with age and an increased trend with age was observed (χ2trend for awareness = 18.579 and χ2trend for treatment = 22.105, both P < .001). The proportions of hypertension awareness and treatment were 91.4% and 86.0%, respectively, in the participants aged 65 to 75 years. Additionally, the proportions of hypertension awareness and treatment were higher in patients with diabetes or dyslipidemia (both P < .01), whereas the control of hypertension was lower in those patients (both P < .01). Participants with normal weight had a higher proportion of hypertension control (P < .01).
Table 2.
The related factors of awareness, treatment, and control of hypertension in the study population.
| N (%) | Awareness (n = 2816) | P | N (%) | Treatment (n = 2627) | P | N (%) | Control (n = 1708) | P | |
|---|---|---|---|---|---|---|---|---|---|
| χ 2 | χ 2 | χ 2 | |||||||
| Sex | 0.408 | .523 | 0.875 | .350 | 3.594 | .058 | |||
| Female | 1481 (89.3) | 1377 (83.1) | 928 (56.0) | ||||||
| Male | 1335 (90.0) | 1250 (84.3) | 780 (52.6) | ||||||
| Age, yr | 18.579 | <.001 | 22.105 | <.001 | 0.802 | .370 | |||
| <45 | 254 (80.4) | 226 (71.5) | 152 (48.1) | ||||||
| 45–55 | 657 (90.3) | 614 (84.3) | 447 (61.4) | ||||||
| 55–65 | 1110 (90.5) | 1039 (84.7) | 648 (52.8) | ||||||
| ≥65 | 795 (91.4) | 748 (85.98) | 461 (53.0) | ||||||
| BMI, kg/m2 | 1.964 | .161 | 4.55 | .033 | 10.503 | .001 | |||
| <18.5 | 14 (77.8) | 11 (61.1) | 9 (50.0) | ||||||
| 18.5–23.9 | 743 (88.5) | 688 (81.9) | 494 (58.8) | ||||||
| 24.0–27.9 | 1297 (90.3) | 1210 (84.2) | 777 (54.1) | ||||||
| ≥28 | 762 (90.1) | 718 (84.9 | 428 (50.6) | ||||||
| Educational level | 0.013 | .909 | 0.013 | .908 | 1.345 | .246 | |||
| Junior high school and below | 1291 (89.9) | 1205 (83.9) | 769 (53.6) | ||||||
| High school | 1113 (89.0) | 1040 (83.1) | 681 (54.4) | ||||||
| College or above | 412 (90.8) | 382 (84.1) | 258 (56.8) | ||||||
| Current smoking | 4.139 | .042 | 2.212 | .137 | 0.053 | .818 | |||
| No | 2259 (89.1) | 2108 (83.2) | 1381 (54.5) | ||||||
| Yes | 557 (91.9) | 519 (85.6) | 327 (53.9) | ||||||
| Current drinking | 1.834 | .176 | 2.333 | .127 | 4.651 | .031 | |||
| No | 2390 (89.3) | 2226 (83.2) | 1478 (55.2) | ||||||
| Yes | 426 (91.4) | 401 (86.0) | 232 (49.8) | ||||||
| Diabetes | 9.990 | .002 | 10.385 | .001 | 5.432 | .020 | |||
| No | 1759 (88.3) | 1633 (82.0) | 1114 (56.0) | ||||||
| Yes | 1057 (91.9) | 994 (86.4) | 594 (51.7) | ||||||
| Dyslipidemia | 10.331 | .001 | 14.567 | <.001 | 10.424 | .001 | |||
| No | 1782 (88.3) | 1649 (81.8) | 1140 (56.5) | ||||||
| Yes | 1034 (92.0) | 978 (87.0) | 568 (50.5) |
BMI = body mass index.
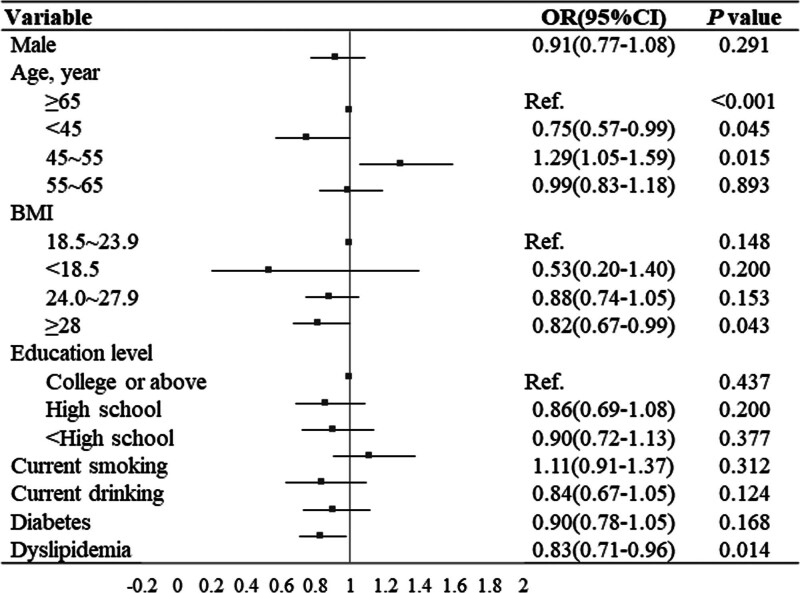
3.4. The factors associated with control under treatment for hypertension
Using a multivariate logistic model, we identified significant determinants that were associated with the control of hypertension under treatment. As shown in Figure 2, control of hypertension was associated with sex, BMI and dyslipidemia (P < .05). Among those treated, participants aged 45 to 55 had a 29% higher rate of control of hypertension than did those aged 65 and over (OR = 1.29, 95% CI: 1.05–1.59, P < .05), while participants with obesity had 18% lower control of hypertension than did those with normal weight (OR = 0.82, 95% CI: 0.67–0.99, P < .05), and participants with dyslipidemia had 17% lower control of hypertension than did those without dyslipidemia (OR = 0.83, 95% CI: 0.71–0.96, P < .05).
Figure 2.
Multivariate logistic regression analysis of the factors associated with control of hypertension under treatment. BMI = body mass index, CI = confidence interval, OR = odds ratio, Ref. = Reference.
4. Discussion
This study presents the latest reliable information about the epidemiological situation of hypertension in coastal areas of Tianjin, China. The findings of our study indicate that the mean SBP and DBP were 128.22 ± 15.24 mm Hg, 78.71 ± 9.38 mm Hg, respectively, and 49.8% (95% CI: 48.5%–51.1%) adults in coastal areas of Tianjin were hypertensive. In those with hypertension, 89.7% were aware of their diagnosis of hypertension, 83.6% had received treatment, and 54.4% had BP under control. Of patients treated, about 60.5% had their hypertension effectively controlled.
Hypertension is the leading cause of cardiovascular disease and premature death worldwide.[2] Compared with our results, 1 study conducted in Beijing Province, a geographical location similar to Tianjin, showed lower prevalence of hypertension (35.5%). In another study conducted in Inner Mongolia, the largest province in northern China, the prevalence of hypertension was notably higher at 55.7%.[13] Similarly, in a cross-sectional survey conducted in rural Northeast China, which included 10,926 representative participants aged ≥ 40 years, the prevalence of hypertension was higher than found in our study (53.6%).[6] The explanations for this regional heterogeneity may include differences in regional characteristics, population structure, and socioeconomic level.[16] Previous data have shown that hypertension is listed first in prevalence among 5 chronic diseases in Tianjin,[17] and the prevalence of hypertension in the coastal area is at a high level.[16,18] Compared with previous studies conducted in this area,[17,19] our data indicate that the prevalence of hypertension in 2022 is much higher than that in 2018 (39.8%)[20] and in 2015 (32.7%).[21] Variations in the levels of risk factors for hypertension, such as high sodium intake, low potassium intake, obesity, alcohol consumption, physical inactivity, and unhealthy diet, may explain some of this increase.[4]
Our study found that the factors influencing the prevalence of hypertension were male sex, increasing age, overweight/obesity, current smoking, current drinking, diabetes, and dyslipidemia. This was partly consistent with many other previous studies.[22–29] Our study also showed that highly educated people had a lower rate of hypertension than those with lower education levels. The same conclusion was found in a study conducted among urban adults in southwestern China.[9] Also, we found that in our cohort the prevalence rate of prehypertension was greater in men than in women (55.8% vs 45.5%), consistent with several other studies.[5,29] In terms of age groups, we found hypertension rates of 22.2%, 43.3%, 62.1%, and 71.3% in the age groups of 35 to 44,45 to 54, 55 to 64, and 65 to 74 years, respectively. These rates were higher than those in some regional surveys reported in northern, northwest, and southern China in recent years, such as Inner Mongolia[13] (32.6%, 50.6%, 64.2%, and 73.4% in the age groups of 35–44, 45–54, 55–64, and 64–75 years, respectively), Xinjiang[30] (32.5%, 39.8%, 47.2%, and 53.6% in the age groups of 35–44, 45–54, 55–64, and ≥65 years, respectively), the Shenzhen region[31] (14.0%, 28.5%, 42.3%, and 55.6% in the age groups of 35–44, 45–54, 55–64, and ≥65 years, respectively), and the Guangxi Zhuang Autonomous Region[32] (6.75%, 20.04%, 35.46%, and 50.13% in the age groups of 35–44, 45–54, 55–64, and 65–74 years, respectively). This difference may result from different lifestyles and dietary habits. The results of 1 meta-analysis showed that despite a decrease in salt intake since the 2000s, sodium intake in northern China remains among the highest in the world, and the North–South divide in sodium intake persists.[33] Previous studies have suggested that the explanation for the particularly high prevalence could be that residents living in the coastal regions consume significantly more salt than those in inland areas, which could affect BP.[34] Furthermore, we found that higher education level was associated with less hypertension, and hypertension in subjects educated to the level of college degree or above was 30% lower than that in people with a junior high school education or below. Therefore, future methods for hypertension prevention should aim for targeted populations such as older or obese people, the less-educated, those who smoke and drink, or those with diabetes and dyslipidemia.
Age was associated with awareness, treatment, and control of hypertension. As shown in our survey, the awareness and treatment rates of hypertension increased with age.[25] This may be explained by the fact that as physical health gradually declines with age, more attention is paid to health. Middle-aged and elderly people are often able to take the initiative to undergo regular checkups, while young people are less likely to seek medical treatment voluntarily because of various factors, including social and psychological factors. Regular self-examination may contribute to improving the awareness and treatment of hypertension; however, the awareness and treatment of hypertension among young people should also be strengthened.[35]
In evaluating treatment conditions, there have typically been 2 methods with different denominators[6,18,19]: 1 based on self-reports of a hypertension diagnosis (awareness), and the other based on the entirety of those with hypertension as screened by the investigation. Correspondingly, the former is larger than the latter. However, these different methods have their own utility in hypertension management. Using the awareness of hypertension in estimating treatment rate focuses on the effectiveness of the method in use, but using all hypertension focuses on the public results of treatment. In this study, the awareness rate was 89.7%, and the hypertension treatment rate was about 83.6% in all hypertension. The proportion of untreated hypertension may be explained by the lack of knowledge of the disease and the ineffectiveness of some methods. As with treatment, the control rate also had 2 methods of estimation. One uses those treated as the denominator, also called treated-control rate, and evaluates the effectiveness of treatment,[36,37] whereas the other uses all subjects with hypertension as the denominator, which measures the controlled condition of hypertension[6,18]; in this study, these rates were 60.5% and 54.4%, respectively. Overall, the awareness, treatment, and control rates of hypertension in this study were much higher than global levels (45.6%, 36.9%, 13.8%) reported in 2016[38] and the results of the Chinese population in 2018 (38.3%, 34.6%, 12.0%)[39] and in 2014 to 2017 (44.7%, 30.1%, 7.2%).[25] This may be because the current survey area has a relatively developed economy, a higher level of education, better community medical equipment, and a higher level of hypertension diagnosis and treatment than the national average. Additionally, compared with results from the same period in Beijing (52.6%, 50.4%, 23.9%),[40] the awareness, treatment, and control of hypertension in the coastal areas of Tianjin were also better. Although the rates improved greatly compared with previous years and other regions,[18,20–23] the results nonetheless mean that nearly 10% of hypertension was underestimated in the participants, about 20% of hypertension was untreated, and approximately one-half of hypertension was uncontrolled. Health authorities should note that comprehensive methods should be included for hypertension management in the community population.
For control of hypertension, we found that participants aged 45 to 55 years have a 29% higher control of hypertension than those aged 65 and over. This means that early control of BP in hypertensive patients is more effective than control at an older age. Additionally, we also found that participants with obesity or dyslipidemia had 18% and 17% lower control of hypertension than those with normal weight or without dyslipidemia, respectively. This should remind health practitioners that obese individuals and subjects with underlying chronic diseases such as dyslipidemia and diabetes are at higher risk of uncontrolled hypertension and should thus be given close attention and careful monitoring.[25,41]
4.1. Limitations
This study has certain limitations: This study is a single-center survey and only represents results from selected regions. BP was measured only on the day of the survey instead of via results on 3 consecutive days. This is difficult to avoid in a field investigation. However, as with other published papers, the results nonetheless reveal some aspects of the prevalence, awareness, treatment, and control of hypertension. This study is only a cross-sectional survey, and there accordingly may have been some bias affecting the final results. Although ideally the treatment rate and the control rate should use the awareness and the treatment as denominators, for the purposes of comparison with national data and for public needs, all hypertensions were used as the denominators, which may have underestimated the real condition.
5. Conclusion
This study found that among populations aged 35 to 75 years in the coastal area of Tianjin, China, about half have hypertension, meaning that hypertension is highly prevalent in the area. However, the region has high rates of hypertension awareness, treatment, and control, and more than half of hypertension patients receiving treatment have controlled hypertension. Age, sex, diabetes, dyslipidemia, smoking, drinking, higher BMI, and education levels were closely related to prevalence, awareness, treatment, and control of hypertension. Further exploration of the factors associated with hypertension is needed to develop strategies that focus on controlling modifiable risk factors to improve the prevention of hypertension.
Acknowledgments
The authors wish to acknowledge all staff members involved in collecting the data.
Author contributions
Data curation: Fenghua Wang.
Formal analysis: Fenghua Wang.
Investigation: Fenghua Wang, Xiongguan Wang.
Methodology: Fenghua Wang, Maoti Wei, Ning Yang.
Project administration: Xiongguan Wang, Fenghua Wang.
Supervision: Ning Yang.
Writing – original draft: Fenghua Wang.
Writing – review & editing: Fenghua Wang, Maoti Wei.
Abbreviations:
- BMI
- body mass index
- BP
- blood pressure
- CI
- confidence interval
- DBP
- diastolic BP
- FBG
- fasting blood glucose
- HDL-C
- high-density lipoprotein cholesterol
- LDL-C
- low-density lipoprotein cholesterol
- OR
- odds ratio
- SBP
- systolic BP
- TC
- total cholesterol
- TG
- triglyceride
This study was supported by the Transfer Payments from Central Government for Local Health and Family Planning Service: Program of Early Screening and Comprehensive Intervention for High-risk Cardiovascular Diseases (Z135080000022).
The authors have no conflicts of interest to disclose.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
How to cite this article: Wang F, Wei M, Yang N, Wang X. Prevalence, awareness, treatment, control of hypertension among adults inhabited in the coastal area of Tianjin, China. Medicine 2024;103:26(e38676).
Contributor Information
Maoti Wei, Email: weimaoti@163.com.
Ning Yang, Email: yangningzxdl@sina.com.
Xiongguan Wang, Email: wangxg0304@sina.com.
References
- [1].Bureau of Disease Prevention and Control, National Health Commission of Peoples's Republic of China, National Center for Cardiovascular Disease. National guidelines for hypertension management in China (2019)[J]. 2020;48:10–46. [Google Scholar]
- [2].Mills KT, Stefanescu A, He J. The global epidemiology of hypertension[J]. Nat Rev Nephrol. 2020;16:223–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].The Writing Committee of the Report on Cardiovascular Health and Disease in China. Report on cardiovascular health and diseases in China 2021: an updated summary[J]. Chinese Circ J. 2021;36:553–78. [Google Scholar]
- [4].Pengpid S, Vonglokham M, Kounnavong S, et al. The prevalence, awareness, treatment, and control of hypertension among adults: the first cross-sectional national population-based survey in Laos[J]. Vasc Health Risk Manag. 2019;15:27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Zhang M, Shi Y, Zhou B, et al. Prevalence, awareness, treatment, and control of hypertension in China, 2004-18: findings from six rounds of a national survey[J]. BMJ (Clinical research ed.). 2023;380:e071952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Xing L, Liu S, Jing L, et al. Trends in prevalence, awareness, treatment, and control of hypertension in Rural Northeast China: 2008 to 2018[J]. Biomed Res Int. 2020;2020:1456720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Yan XF, Yang JW, Bai XK, et al. Awareness, treatment and control of hypertension in 640 000 adults in eastern China[J]. Chin J Epidemiol. 2020;41:68–73. [DOI] [PubMed] [Google Scholar]
- [8].Xing W, Wang S, Liu X, et al. Prevalence and management of hypertension in Central China: a cross-sectional survey[J]. J Int Med Res. 2023;51:3000605221148905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Huang XB, Zhang Y, Wang TD, et al. Prevalence, awareness, treatment, and control of hypertension in southwestern China[J]. Sci Rep. 2019;9:19098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Wang W, Zhang M, Xu CD, et al. Hypertension prevalence, awareness, treatment, and control and their associated socioeconomic factors in China: a spatial analysis of a national representative survey[J]. Biomed Environ Sci. 2021;34:937–51. [DOI] [PubMed] [Google Scholar]
- [11].Status of basic public health services in Tianjin (2022) [R/OL]. https://wsjk.tj.gov.cn/ZWGK3158/ZFXXGK5869/FDZDGKNR4356/tjxxn/202309/t20230927_6417334.html. [Google Scholar]
- [12].The National Essential Public Health Service Program Office for Management of Hypertension in Primary Health Care, National Center for Cardiovascular Diseases, National Committee on Hypertension Management in Primary Health Care. National clinical practice guidelines on the management of hypertension in primary health care in China (2020)[J]. Chin J Front Med Sci (Electric Version). 2021;13:26–37. [Google Scholar]
- [13].Xu X, Bao H, Tian Z, et al. Prevalence, awareness, treatment, and control of hypertension in Northern China: a cross-sectional study[J]. BMC Cardiovasc Disord. 2021;21:525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Chinese Diabetes Society, National Office for Primary Diabetes Care. National guideline for the prevention and control of diabetes in primary (2022)[J]. Chin J Intern Med. 2022;61:833–53. [Google Scholar]
- [15].Joint Committee Issued Chinese Guideline for the Management of Dyslipidemia in Adults. 2016 Chinese guideline for the management of dyslipidemia in adults[J]. Chin J Cardiol. 2016;44:833–53. [DOI] [PubMed] [Google Scholar]
- [16].Zhao S, Xin P, Li J, et al. Prevalence of hypertension and related influencing factors among adult residents of Tianjin in 2018[J]. Chin J Pre Contr Chron Dis. 2022;30:125–33. [Google Scholar]
- [17].. Chun Yang. Study on the Utilization and Influence Factors of Community Health Service in Binhai New Area [D]. Mater’s dissertation of Tianjin Medical university; 2017. [Google Scholar]
- [18].. Tian SL. Study on the Relationship between Dietary Patterns and Hypertension of Dietary Survey Population in Tianjin[D]. Tianjin: Tianjin Medical University; 2018. [Google Scholar]
- [19].. Cui Jia. Analysis of the Causes of Death of Residents in Binhai New Area, Tianjin from 2013 to 2017[D]. Mater’s dissertation of Tianjin Medical university; 2019. [Google Scholar]
- [20].Zheng W, Wang X, Xue X, et al. Characteristics of hypertension in the last 16 years in high prevalence region of China and the attribute ratios for cardiovascular mortality[J]. BMC Public Health. 2023;23:114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Tian Ying. The study on the Risk Factors of Chronic Disease and Nutrition Intervention in Tianjin[D]. Mater’s dissertation of Tianjin Medical University; 2010. [Google Scholar]
- [22].Chen SY, Wu YH, Lin SW, et al. Prevalence and influencing factors of hypertension among young adults in urban coastal areas of Fujian province[J]. Chin J Hypertens. 2015;23:1080–3. [Google Scholar]
- [23].Xu ZX, Geng K, Pang WY, et al. Analysis of major chronic diseases and influencing factors among residents in Changping district of Beijing[J]. Chin J Public Health. 2008;24:1010–1. [Google Scholar]
- [24].Qi MJ, Hou G, Gao L, et al. Prevalence, awareness, treatment and control rate of hypertension in adults aged 35-75 years in Henan province. Chin J Hypertens. 2021;29:959–64. [Google Scholar]
- [25].Lu J, Lu Y, Wang X, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 17 million adults in a population-based screening study (China PEACE Million Persons Project)[J]. Lancet. 2017;390:2549–58. [DOI] [PubMed] [Google Scholar]
- [26].Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China hypertension survey, 2012-2015[J]. Circulation. 2018;137:2344–56. [DOI] [PubMed] [Google Scholar]
- [27].Xu J, Ding XB, Tang WG, et al. Analysis on the prevalence of hypertension and its risk factors among residents aged 35-75 years old in Chongqing[J]. J of Pub Health and Prev Med. 2020;31:31–5. [Google Scholar]
- [28].Zheng JY, Wu WX, Su YS, et al. Correlation between dyslipidemia and hypertension in adults[J]. Chin J Pre Contr Chron Dis. 2015;23:915–18. [Google Scholar]
- [29].Dong GH, Wang D, Liu MM, et al. Sex difference of the prevalence and risk factors associated with prehypertension among urban Chinese adults from 33 communities of China: the CHPSNE study[J]. J Hypertens. 2012;30:485–91. [DOI] [PubMed] [Google Scholar]
- [30].Heizhati M, Wang L, Yao X, et al. Prevalence, awareness, treatment and control of hypertension in various ethnic groups (Hui, Kazakh, Kyrgyz, Mongolian, Tajik) in Xinjiang, Northwest China[J]. Blood Press. 2020;29:276–84. [DOI] [PubMed] [Google Scholar]
- [31].Cai W, Wang Y, Peng K, et al. Prevalence of hypertension in Shenzhen, China: a population-based, cross-sectional study[J]. BMJ Open. 2022;12:e061606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Fan G, Jiang Z, Li J, Shi L, Gui C, Huang R. Prevalence, awareness, treatment and control of hypertension in Guangxi Zhuang Autonomous Region[J]. Sci Rep. 2022;12:900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Tan M, He FJ, Wang C, MacGregor GA. Twenty-four-hour urinary sodium and potassium excretion in China: a systematic review and meta-analysis[J]. J Am Heart Assoc. 2019;8:e012923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].He FJ, Tan M, Ma Y, MacGregor GA. Salt reduction to prevent hypertension and cardiovascular disease: JACC State-of-the-Art Review[J]. J Am Coll Cardiol. 2020;75:632–47. [DOI] [PubMed] [Google Scholar]
- [35].Han FL, Yang LH, Zhang HP, et al. Analysis of the prevalence of hypertension and its influencing factors in adult Chinese adults of different genders[J]. Chin J Hosp Stat. 2019;26:321–325 + 330. [Google Scholar]
- [36].Wei J, Mi Y, Li Y, et al. Factors associated with awareness, treatment and control of hypertension among 3579 hypertensive adults in China: data from the China Health and Nutrition Survey[J]. BMC Public Health. 2021;21:423–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AH A/AAPA/ABC/APCM/ AGS/APHA/ ASH/ ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines[J]. Hypertension. 2018;71:e13–e115. [DOI] [PubMed] [Google Scholar]
- [38].Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries[J]. Circulation. 2016;134:441–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Report on Nutrition and Chronic Diseases in China 2020[M]. Beijing: People’s Medical Publishing House, 2020:1–148. [Google Scholar]
- [40].You K, Zhang WX, Zhang SW, et al. Prevalence, awareness, treatment and control of hypertension in Shunyi district of Beijing and its influencing factors[J]. Chin J Pre Contr Chron Dis. 2022;30:209–13. [Google Scholar]
- [41].Zhang FL, Guo ZN, Xing YQ, Wu YH, Liu HY, Yang Y. Hypertension prevalence, awareness, treatment, and control in northeast China: a population-based cross-sectional survey[J]. J Hum Hypertens. 2017;32:54–65. [DOI] [PubMed] [Google Scholar]