Abstract
Purpose
WEE1 is a crucial kinase involved in the regulation of G2/M checkpoint within the cell cycle. This article aims to comprehensively review the existing knowledge on the implication of WEE1 as a therapeutic target in tumor progression and drug resistance. Furthermore, we summarize the current predictive biomarkers employed to treat cancer with WEE1 inhibitors.
Methods
A systematic review of the literature was conducted to analyze the association between WEE1 inhibition and cancer progression, including tumor advancement and drug resistance. Special attention was paid to the identification and utilization of predictive biomarkers related to therapeutic response to WEE1 inhibitors.
Results
The review highlights the intricate involvement of WEE1 in tumor progression and drug resistance. It synthesizes the current knowledge on predictive biomarkers employed in WEE1 inhibitor treatments, offering insights into their prognostic significance. Notably, the article elucidates the potential for precision medicine by understanding these biomarkers in the context of tumor treatment outcomes.
Conclusion
WEE1 plays a pivotal role in tumor progression and is a promising therapeutic target. Distinguishing patients that would benefit from WEE1 inhibition will be a major direction of future research.
Keywords: Biomarkers, Cancer therapy, WEE1 inhibition
Introduction
The emergence of molecular signature-based targeted therapy has revolutionized the field of antitumor treatment (Lee et al. 2018). In particular, the investigation of the DNA damage and repair pathway has garnered significant attention in recent years. Notably, numerous clinical trials have provided evidence that WEE1 inhibitors exhibit encouraging efficacy. Furthermore, when combined with other therapies, WEE1 inhibition can lead to synergistic anti-tumor effects in several cancer types with limited treatment alternatives, such as recurrent uterine serous cancer with TP53 mutation (Liu et al. 2021), high-grade serous ovarian cancer with platinum resistance (Leijen et al. 2016b; Lheureux et al. 2021), and unresectable pancreatic cancer (Cuneo et al. 2019). Despite these encouraging advances, the beneficiaries of WEE1 inhibition remain uncertain. In other words, development of predictive biomarkers and identification of the appropriate population that would respond to WEE1 inhibitors are imperative. To this end, this article aims to provide a comprehensive review of the existing literature on the association the role of WEE1 as a therapeutic target in tumor progression and drug resistance. We also summarize the current progress on the predictive biomarkers employed in the treatment of tumors targeting WEE1.
The mechanism of action of WEE1 inhibitors
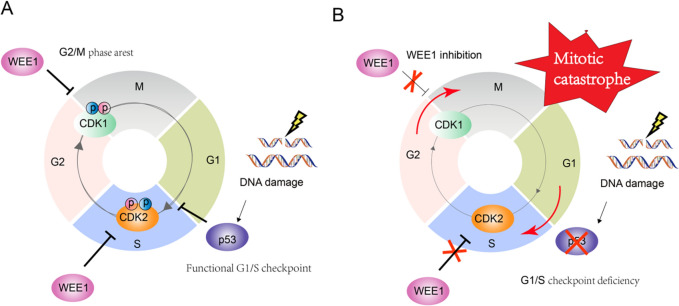
Cell cycle regulation plays a vital role in maintaining DNA integrity (Campos and Clemente-Blanco 2020), which, to a great extent, depends on the cell cycle checkpoints, namely the G1/S and G2/M checkpoints (Poon 2016). The p53 protein (encoded by the TP53 gene) plays a crucial role in DNA damage response by suppressing the G1/S cell cycle checkpoint (Jackson and Bartek 2009). The other pivotal checkpoint is the G2/M checkpoint, which is primarily regulated by WEE1 kinase (Smith et al. 2020). In the event of additional DNA damage during replication or failure to repair the initial damage, the WEE1 kinase hinders the progression of cell cycle into M phase by phosphorylating and inhibiting the activity of cyclin-dependent kinases CDK1/2 (Russell and Nurse 1987). This results in effective extension in the duration of DNA repair (Fig. 1A).
Fig. 1.
Cell cycle checkpoint regulation mechanism. A Cell cycle regulation in cells with intact cell cycle checkpoint function when DNA damage occurs; B Cell cycle regulation after G1/S checkpoint deficiency combined with WEE1 inhibition
Unfortunately, in the context of human cancers, TP53 is the most frequently mutated tumor suppressor across various cancer types, with high-grade serous ovarian cancer exhibiting the highest mutation rate (Zehir et al. 2017). Despite the notorious role of TP53 mutations in cancer, pharmacological intervention specifically targeting p53 mutations has been limited, with only a few targeted drugs, such as PRIMA-1 and PRIMA-1Met (APR-246), being tested in early clinical trials. In TP53-mutant tumor cells, the WEE1 checkpoint encounters heightened pressure and thus presents a potential target for therapeutic intervention (Smith et al. 2020). Inhibition of WEE1 facilitates or even expedites mitotic progression, leading to an increase in genomic instability (Matheson et al. 2016), which ultimately result in mitotic catastrophe (Matheson et al. 2016) (Fig. 1B). Besides, WEE1 also regulates CDK2 during the S phase to stabilize the replication machinery (Beck et al. 2012; Li et al. 2020a). Hence, the coordination of diverse cellular division events by WEE1 undeniably establishes its significance as a potential target for clinical utilization in the treatment of tumors (Fig. 1B).
WEE1 and cancer
WEE1 expression in tumors
Recent studies have demonstrated that up-regulation of WEE1 is prevalent in various types of tumors (Beck et al. 2012), particularly in those exhibiting loss of p53 function (De Witt Hamer et al. 2011; Lau and Pardee 1982). For instance, a comprehensive comparison of 34 cancer-versus-normal data sets, revealed increased expression of WEE1 mRNA in 77% of the samples (Mir et al. 2010). Similarly, heightened expression or increased activity of WEE1 was observed in glioma (Mueller et al. 2014; Music et al. 2016), liver cancer models (Masaki et al. 2000, 2003), medulloblastoma (Harris et al. 2014), seminoma (Mir et al. 2010), breast cancer, and osteosarcoma (PosthumaDeBoer et al. 2011; Wang et al. 2011). Collectively, these aforementioned studies suggest that WEE1 level is elevated in human cancer and thus has the potential to serve as a molecular marker for tumors.
The role of WEE1 in tumor progression
Inhibiting WEE1 effectively impeded the proliferation and migration of colorectal cancer liver metastases endothelial cells (CLMECs), leading to impaired vascular endothelial formation (Webster et al. 2017). Furthermore, WEE1 expression was closely associated with tumor-free survival rate, tumor burden, and the incidence of ulcer in melanoma (Magnussen et al. 2012), while WEE1 repression significantly reduced melanoma metastasis (DiSano et al. 2019). Additionally, the study by Magnussen et al. revealed a gradual increase in WEE1 expression during the process of carcinogenesis, with the highest expression observed in patients who had developed tumor metastasis (Magnussen et al. 2012). Furthermore, inhibiting WEE1 expression in glioma cells resulted in cell death (Sancar et al. 2004). These findings collectively suggest that WEE1 may promote tumor progression.
The role of WEE1 in drug resistance
DNA repair mechanisms are considered as a significant contributor to resistance against DNA damage therapies (Dibitetto et al. 2022). WEE1 suppression could overcome resistance to EGFR-TKIs inhibitors and enhance the efficacy of cisplatin and gemcitabine (Liu et al. 2019). Additionally, Li et al. (2020b) demonstrated the significant impact of the DGKA-c-Jun-WEE1 signaling axis on platinum sensitivity in platinum-resistant ovarian cancer cells. A study involving 287 patients with advanced high-grade serous ovarian cancer observed higher expression of WEE1 in samples that recurred after initial chemotherapy compared to pre-chemotherapy samples, as well as a significant association between high WEE1 expression and poor prognosis in post-chemotherapy patients (Slipicevic et al. 2014). Furthermore, high-throughput screening of related kinases in ovarian cancer cells revealed that WEE1 kinase potentially regulated resistance to CHK1 inhibitors (Carrassa et al. 2012). Besides, WEE1 inhibition effectively reversed resistance to BRAF inhibitors (Haarberg et al. 2013; Sharma et al. 2013) and AURKA inhibitor (MLN8237) in HPV- HNSCC (head and neck squamous cell carcinoma (Lee et al. 2019). These findings indicate that WEE1 kinase may mediate the resistance to traditional chemotherapy and targeted therapy, making it a potential biomarker and therapeutic target for post-treatment resistance.
Clinical development of WEE1 inhibitors
Despite considerable effort to develop small molecule inhibitors targeting WEE1 kinase, the available options are currently limited. Hitherto, a total of 79 clinical trials involving five WEE1 inhibitors have been reported by ClinicalTrials.gov (Table 1). Among these inhibitors, adavosertib (AZD1775) is the first-in-class potent inhibitor of WEE1 and has been involved in 61 trials. Following AZD1775, ZN-c3 has been studied in 12 trials, Debio-0123 in 4 trials, and SY-4835 and IMP7068 in only 1 trial each (Table 1). A sum of 28 clinical trials have been completed, with 9 trials dedicated to singular treatment and 19 trials investigating the efficacy of combination treatments.
Table 1.
Small molecule inhibitors of Wee1 under clinical trials
| Inhibitor | Properties | WEE1 IC50 (nM)* |
Chemical structure* | Sponsor | Phases | Completed (n)/total (n) |
|---|---|---|---|---|---|---|
| adavosertib | A first-in-class, potent, and ATP-competitive specific small-molecule Wee1 inhibitor | 5.2 |  |
AstraZeneca | II | 28/61 |
| ZN-c3 | A novel, selective, and orally active bioavailable Wee1 protein kinase inhibitor | 3.9 |  |
Zentalis Pharmaceuticals Inc | II | 0/12 |
| Debio-0123 | An oral, potent, and highly selective Wee1 inhibitor | Nd |  |
Almac Discovery Ltd | I | 0/4 |
| IMP7068 | A potent, highly selective Wee1 inhibitor | Nd |  |
Impact Therapeutics Inc | I | 0/1 |
| SY-4835 | A new type of highly active and selective Wee1 small molecular inhibitor | Nd | Nd | Shouyao Holdings | I | 0/1 |
*Nd not disclosed
The trials employing AZD1775 have yielded encouraging outcomes in prolonging progression-free survival of colorectal cancer patients with RAS/TP53 mutations (Seligmann et al. 2021). Furthermore, a clinical trial conducted on human glioblastoma showed that AZD1775 successfully penetrated the blood–brain barrier, with great potential as a standalone therapeutic intervention for this disease (Sanai et al. 2018). In addition, AZD1775 has been extensively investigated as a means to enhance the efficacy of DNA damaging chemotherapy or radiation. For example, for refractory high-grade serous ovarian cancer, the combination of AZD1775 with gemcitabine has exhibited more significant therapeutic effect compared to gemcitabine alone (Lheureux et al. 2021). Similarly, the combination of AZD1775 with gemcitabine plus radiotherapy has been shown to improve survival in locally advanced pancreatic cancer (Cuneo et al. 2019). Furthermore, patients with platinum-sensitive TP53-mutant ovarian cancer benefited from the combination of AZD1775 with paclitaxel and carboplatin (Oza et al. 2020). These clinical trials offer important evidence advocating AZD1775 either as a monotherapy or in conjunction with other chemotherapeutic agents.
However, its application has been limited due to the associated toxicities. The most frequently observed toxicities included myelosuppression (such as anemia, neutropenia, and thrombocytopenia) and diarrhea (Do et al. 2015). In a separate investigation afflicted with advanced solid tumors, patients received the most prevalent drug-related adverse events (AEs) being diarrhea and fatigue when AZD1775 was administered as a sole monotherapy dose, while 19% of patients experienced severe treatment-related AEs, including fatigue, nausea, vomiting, diarrhea, anemia, neutropenia, and thrombocytopenia in conjunction of AZD1775 with various chemotherapeutic agents (gemcitabine, carboplatin, or cisplatin) (Leijen et al. 2016a). In the meantime, the safety, tolerability, and antitumor efficacy of combining AZD1775 with cisplatin and docetaxel in advanced HNSCC has been demonstrated (Méndez et al. 2018), suggesting that more investigations are needed to better balance the efficacy and toxicity of AZD1775.
ZN-c3 is another selective inhibitor of WEE1 kinase with significant anti-proliferative efficacy in various cancer cell lines. It is currently under evaluation in several clinical trials of different cancers, including ovarian cancer, solid tumors, and osteosarcoma (Clinicaltrials.gov). Notably, ZN-c3 possesses the advantage of a high maximum tolerated dose, enabling it to achieve the similar growth/proliferation inhibition at significantly lower doses compared to AZD1775. Although ZN-c3 exhibits greater specificity compared to AZD1775, its inhibitory activity has been observed on multiple kinases, and common side effects such as fatigue, vomiting, diarrhea, and nausea have been consistently reported in several studies (Li et al. 2021; Tolcher et al. 2021). Nevertheless, ZN-c3 has demonstrated its efficacy as a standalone treatment for cancer cells, displaying high tolerance and satisfactory safety profiles.
Conversely, the remaining three WEE1 inhibitors, namely Debio-0123, SY-4835, and IMP7068, are still under clinical evaluation. Thus, the efficacy and potential toxicity of these inhibitors have yet to be definitively established.
Predictive biomarkers
Despite the considerable therapeutic potential of WEE1 inhibition as standalone treatment or in combination therapies, biomarkers that accurately predict its susceptibility and resistance remains to be identified. Next, we summarize the potential biomarkers of WEE1 inhibitory treatment described so far (Fig. 2).
Fig. 2.

Biomarkers of sensitivity to WEE1 inhibition therapy
Biomarkers of sensitivity to WEE1 inhibition therapy
TP53 mutation
The correlation between TP53 mutation status and the sensitivity to AZD1775 have been extensively established (Bauman and Chung 2014; Bridges et al. 2011; Diab et al. 2019; Hirai et al. 2009; Ku et al. 2017; Yang et al. 2020). In addition, AZD1775 selectively sensitized p53-deficient cancer cells to radiotherapy, gemcitabine, carboplatin and cisplatin, compared with the isogenic wild-type line (Bridges et al. 2011; Hirai et al. 2009). Consistently, cells with dysfunctional p53 exhibited heightened sensitivity to WEE1 inhibition when combined with conventional chemotherapy and ionizing radiation (Barbosa et al. 2019; Wang et al. 2001; Yin et al. 2018). These investigations propose that TP53 mutation or dysfunction may serve as a bona fide biomarker for AZD1775 sensitivity.
High basal WEE1 expression
Gastric cancer cells exhibiting high expression of WEE1 displayed increased susceptibility to WEE1 inhibitory therapy (Kim et al. 2016), indicating that the efficacy of WEE1 inhibition may be dependent on the expression level of WEE1 kinase. Another study of 663 advanced non-small cell lung cancer patients showed that WEE1 rs3910384 genotype was markedly correlated with prognosis following platinum-based chemotherapy as well as the combined efficacy of platinum and gemcitabine (Liu et al. 2015). Furthermore, co-administration of AZD1775 and cisplatin demonstrated a synergistic effect in a patient-derived xenograft (PDX) model characterized by elevated basal expression of PAXIP1 and WEE1 (Jhuraney et al. 2016). These findings indicate that the basal level of WEE1 kinase may play a part in the responsiveness to WEE1 inhibition therapy.
RAS mutations
The particular status of KRAS mutation is critical to the response of non-small cell lung cancer (NSCLC) cells to sorafenib, a multi-target tyrosine kinase inhibitor. High-throughput screening utilizing a siRNA library targeting 719 human kinases identified WEE1 as a modulator of sorafenib response, while AZD1775 was observed to augment the susceptibility of KRAS mutated NSCLC cells towards sorafenib (Caiola et al. 2018). In addition, the concurrent inhibition of mTOR and WEE1 has been demonstrated to elicit robust synergistic cytotoxic effects in NSCLC cell lines harboring KRAS mutations. This combination therapy was also found to impede the growth of human tumor xenografts and induce tumor regression in a murine model of lung adenocarcinoma (Hai et al. 2017). Similarly, a notable observation was made regarding the combined effect of mTOR inhibitor and WEE1 inhibitor in both mutant neuroblastoma NRAS- and mutant KRAS-positive acute myelogenous leukemia (AML) cell lines and primary patient samples. It is worth mentioning that these findings have been shown to be applicable to other malignancies expressing mutant RAS, such as mutant NRAS-positive melanoma, and mutant KRAS-positive colorectal cancer, pancreatic cancer, and lung cancer (Weisberg et al. 2015). Moreover, combination of AZD1775 and cisplatin significantly prolonged overall survival in a genetically engineered mouse model of mutant KRAS with concomitant loss of LKB1. Of note, LKB1 is among the frequently mutated genes in NSCLC and commonly co-occurs with KRAS mutations (Richer et al. 2017). These findings suggest that WEE1 inhibitors exhibit promising anti-tumor potential when used in conjunction with other small molecule inhibitors in the context of RAS mutations.
BRCA mutations
A previous Phase I Study (NCT01748825) evaluated the single-agent activity of AZD1775 in patients with BRCA mutations. Notably, two patients with BRCA mutations, one with head and neck cancer and one with ovarian cancer, exhibited partial response (Do et al. 2015). Chen et al. demonstrate, using various in vitro and in vivo model systems, that triple-negative breast cancers (TNBCs) with either BRCA1/2 mutations or cyclin E overexpression exhibit heightened susceptibility to AZD-1775 when administered in conjunction with MK-4837 (a PARP inhibitor). The combined treatment of these two agents led to synergistic eradication of TNBC cells, which was attributed to the induction of replicative stress, downregulation of DNA repair mechanisms, failure in cytokinesis, and ultimately increased apoptosis (Chen et al. 2021). These findings highlight the potential clinical application of using BRCA mutations as biomarkers to select patients that may benefit from therapies involving AZD1775.
Cyclin E overexpression
Recently, cyclin E levels have been shown to correlate with the efficacy of AZD1775 in breast cancer models (Chen et al. 2018). Chen et al. conducted a study wherein they found that overexpression of cyclin E is more prevalent in TNBCs exhibiting high rates of recurrence and these cells more susceptible to inhibition of wee1 kinase. Furthermore, they also discovered that the overexpression of Cyclin E induces the activation of DNA replication stress pathways in a CDK2-dependent manner, consequently augmenting the activity of Wee1 kinase (Chen et al. 2018). Their study suggests that Cyclin E overexpression may serve as a biomarker of sensitivity to WEE1 inhibitors.
Epigenetic modifications
Interestingly, small cell lung cancers with alterations in the MYC family exhibited increased sensitivity to combined treatment of Olaparib and AZD1775 (Lallo et al. 2018). Conversely, AZD1775 enhanced gemcitabine sensitivity despite the presence of elevated c-MYC expression in medulloblastoma (Moreira et al. 2020). Our previous study indicated that tumor cells exhibiting elevated basal levels of DNMT1 and FOXM1 displayed heightened sensitivity to AZD1775 (Guo et al. 2022). In addition, the latest research reports that sirtuin 1 (SIRT1) deficiency induces WEE1 hyperacetylation and activation, rendering cancer cells resistant to WEE1 inhibition (Zhu et al. 2023). These findings imply that epigenetic alterations may play a role in the responsiveness of WEE1 inhibitory therapy.
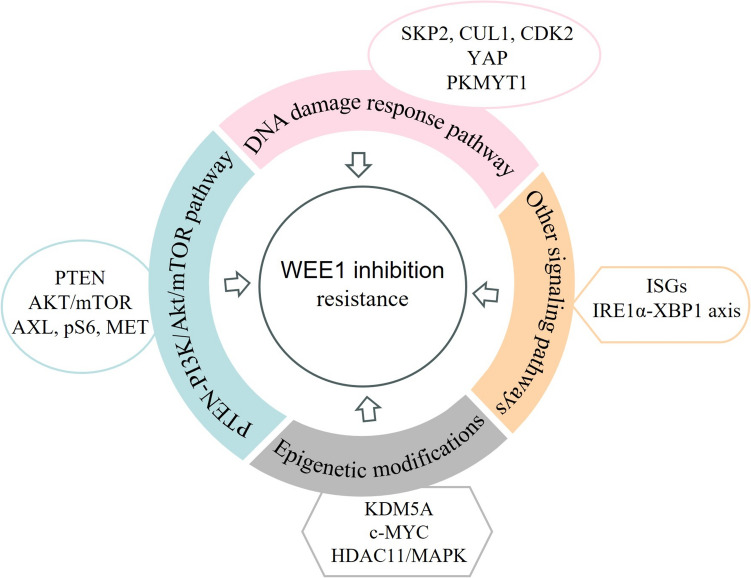
Biomarkers associated with resistance to WEE1 inhibition
Despite numerous studies demonstrating the considerable effectiveness of WEE1 inhibition therapy in combating tumors, the emergence of primary and secondary resistance remains an inevitable challenge. Therefore, a summary of biomarkers predicting resistance to WEE1 inhibitors will help formulate treatment strategies to avoid it (Fig. 3).
Fig. 3.
Biomarkers of resistance to WEE1 inhibition therapy
Biomarkers in the PTEN-PI3K/Akt/mTOR signaling pathway
It has been recently reported that breast cancer cells with high PTEN expression can regain their activity after discontinuation of AZD1775 treatment (Brunner et al. 2020). This suggests that the presence of high levels of PTEN may contribute to resistance against WEE1 inhibitors. Furthermore, a high-throughput proteomic analysis revealed the overexpression of AKT/mTOR pathway molecules and phosphorylated S6 ribosomal protein in small cell lung cancer and ovarian cancer models that exhibit primary resistance to AZD1775 (Li et al. 2020a; Sen et al. 2017). Similarly, our previous high-throughput Reverse Phase Protein Array (RPPA) observed a compensatory up-regulation of the mTOR pathway following AZD1775 treatment during early stages of ovarian cancer. Combination of WEE1 and mTOR dual inhibition demonstrated synergistic effects in both ovarian cancer cell lines and PDX models (Li et al. 2020a). These findings suggest that activation of the PTEN-PI3K/Akt/mTOR signaling pathway may play a crucial role in conferring resistance to WEE1 inhibition therapy.
Biomarkers in DNA damage response pathway
In a comprehensive investigation involving ovarian cancer, chronic myeloid leukemia, and breast cancer, the surviving cells following WEE1 inhibitor treatment were subjected to sequencing analysis. The results revealed that G1/S regulatory genes (SKP2, CUL1, CDK2) were significantly enriched in the surviving cells, where inhibiting these genes effectively mitigated the formation of DNA damage (Heijink et al. 2015). Additionally, another study in ovarian cancer showed that the resistance to AZD1775 therapy was mediated by YAP through the E2F1 DNA damage response axis (Oku et al. 2018). Notably, independent studies consistently demonstrated a correlation between high expression of PKMYT1 and reduced sensitivity to AZD1775 (Ghelli Luserna Di Rorà et al. 2018; Lewis et al. 2019). These findings propose that the resistance to WEE1 repression may be attributed to adaptive responses within the DNA damage response pathway.
Biomarkers in epigenetic modifications
It was recently shown that the survival of AZD1775-resistant acute leukemia cell lines relied on the activity of MYC and HDAC, which was in part due to the increased KDM5A activity (Garcia et al. 2020), thus corroborating preclinical studies that advocate for the combined utilization of WEE1 and HDAC inhibitors (Qi et al. 2015; Tanaka et al. 2017; Zhou et al. 2015). Similarly, research by Zhou et al. also found that the WEE1 inhibitor PD0166285 can arise the expression of HDAC11 which was negatively correlated with survival of AML patients. Mechanistically, HDAC11 can reduce the anti-tumor effect of PD0166285 through an effect on p53 stability and the changes in phosphorylation levels of MAPK pathways (Zhou et al. 2023). The above studies suggest that epigenetic modifications, such as HDACs, are involved in mediating resistance to WEE1 inhibitor treatment, and targeting these molecules can effectively reverse WEE1 treatment resistance.
Biomarkers in other signaling pathways
Furthermore, our recent study revealed that ovarian and colorectal cancer cells sensitive to AZD1775 monotherapy exhibited an up-regulation of interferon signaling gene groups in a responsive manner (Guo et al. 2022). This finding was further confirmed through RNA-seq analysis of murine AZD1775-resistant ovarian cancer cells (Guo et al. 2022), suggesting that adaptive immune signaling may play a role in the development of resistance to AZD1775. In keeping with this, we also demonstrated that refractory ovarian cells can enhance the ability to adapt to AZD1775 treatment by activating the IRE1α-XBP1 axis of the unfolded protein response pathway (Xiao et al. 2022). Our study suggests that immune and unfolded protein response may be involved in WEE1 therapeutic resistance.
Conclusion
WEE1 inhibition has exhibited significant potential in tumor treatment. Preclinical investigations have paved the way for the advancement of clinical trials involving WEE1 inhibitors. The refinement of predictive biomarkers would help identifying populations that would benefit from WEE1 inhibitor therapy. Understanding the prognostic significance of these biomarkers in relation to tumor treatment outcomes and patient prognosis is key to the development of appropriate treatment strategy. Despite these important progress, further investigation is warranted to identify additional biomarkers that can inform the development of treatment strategies.
Author contributions
ZW and WL drafted the manuscript. FL performed the literature collection and classification. RX performed the manuscript review and editing. All authors read and approved the final manuscript.
Funding
This study has received support from the National Natural Science Foundation of China (82060472, 82303671), and the Fundamental Research Funds for the Central Universities (2042023kf0084).
Data availability
All data generated or analyzed during this study are included in this published article.
Declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical statement
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zizhuo Wang and Wenting Li contributed equally to this work.
References
- Barbosa RSS, Dantonio PM, Guimarães T, de Oliveira MB, Fook Alves VL, Sandes AF, et al. Sequential combination of bortezomib and WEE1 inhibitor, MK-1775, induced apoptosis in multiple myeloma cell lines. Biochem Biophys Res Commun. 2019;519(3):597–604. doi: 10.1016/j.bbrc.2019.08.163. [DOI] [PubMed] [Google Scholar]
- Bauman JE, Chung CH. CHK it out! Blocking WEE kinase routs TP53 mutant cancer. Clin Cancer Res. 2014;20(16):4173–4175. doi: 10.1158/1078-0432.Ccr-14-0720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck H, Nähse-Kumpf V, Larsen MS, O'Hanlon KA, Patzke S, Holmberg C, et al. Cyclin-dependent kinase suppression by WEE1 kinase protects the genome through control of replication initiation and nucleotide consumption. Mol Cell Biol. 2012;32(20):4226–4236. doi: 10.1128/mcb.00412-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridges KA, Hirai H, Buser CA, Brooks C, Liu H, Buchholz TA, et al. MK-1775, a novel Wee1 kinase inhibitor, radiosensitizes p53-defective human tumor cells. Clin Cancer Res. 2011;17(17):5638–5648. doi: 10.1158/1078-0432.CCR-11-0650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunner A, SuryoRahmanto A, Johansson H, Franco M, Viiliäinen J, Gazi M, et al. PTEN and DNA-PK determine sensitivity and recovery in response to WEE1 inhibition in human breast cancer. Elife. 2020 doi: 10.7554/eLife.57894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caiola E, Frapolli R, Tomanelli M, Valerio R, Iezzi A, Garassino MC, et al. Wee1 inhibitor MK1775 sensitizes KRAS mutated NSCLC cells to sorafenib. Sci Rep. 2018;8(1):948. doi: 10.1038/s41598-017-18900-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos A, Clemente-Blanco A. Cell cycle and dna repair regulation in the damage response: protein phosphatases take over the reins. Int J Mol Sci. 2020 doi: 10.3390/ijms21020446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrassa L, Chilà R, Lupi M, Ricci F, Celenza C, Mazzoletti M, et al. Combined inhibition of Chk1 and Wee1: in vitro synergistic effect translates to tumor growth inhibition in vivo. Cell Cycle. 2012;11(13):2507–2517. doi: 10.4161/cc.20899. [DOI] [PubMed] [Google Scholar]
- Chen X, Low KH, Alexander A, Jiang Y, Karakas C, Hess KR, Carey JPW, Bui TN, Vijayaraghavan S, Evans KW, Yi M, Ellis DC, Cheung KL, Ellis IO, Fu S, Meric-Bernstam F, Hunt KK, Keyomarsi K. Cyclin E Overexpression Sensitizes Triple-Negative Breast Cancer to Wee1 Kinase Inhibition. Clin Cancer Res. 2018;24(24):6594–6610. doi: 10.1158/1078-0432.CCR-18-1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Yang D, Carey JPW, Karakas C, Albarracin C, Sahin AA, et al. Targeting replicative stress and DNA repair by combining PARP and Wee1 kinase inhibitors is synergistic in triple negative breast cancers with cyclin E or BRCA1 alteration. Cancers. 2021 doi: 10.3390/cancers13071656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuneo KC, Morgan MA, Sahai V, Schipper MJ, Parsels LA, Parsels JD, et al. Dose escalation trial of the Wee1 inhibitor adavosertib (AZD1775) in combination with gemcitabine and radiation for patients with locally advanced pancreatic cancer. J Clin Oncol. 2019;37(29):2643–2650. doi: 10.1200/jco.19.00730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Witt Hamer PC, Mir SE, Noske D, Van Noorden CJ, Würdinger T. WEE1 kinase targeting combined with DNA-damaging cancer therapy catalyzes mitotic catastrophe. Clin Cancer Res. 2011;17(13):4200–4207. doi: 10.1158/1078-0432.Ccr-10-2537. [DOI] [PubMed] [Google Scholar]
- Diab A, Kao M, Kehrli K, Kim HY, Sidorova J, Mendez E. Multiple defects sensitize p53-deficient head and neck cancer cells to the WEE1 kinase inhibition. Mol Cancer Res. 2019;17(5):1115–1128. doi: 10.1158/1541-7786.Mcr-18-0860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dibitetto D, Marshall S, Sanchi A, Liptay M, Badar J, Lopes M, et al. DNA-PKcs promotes fork reversal and chemoresistance. Mol Cell. 2022;82(20):3932–3942 e3936. doi: 10.1016/j.molcel.2022.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiSano JA, Huffnagle I, Gowda R, Spiegelman VS, Robertson GP, Pameijer CR. Loss of miR-155 upregulates WEE1 in metastatic melanoma. Melanoma Res. 2019;29(2):216–219. doi: 10.1097/cmr.0000000000000545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Do K, Wilsker D, Ji J, Zlott J, Freshwater T, Kinders RJ, et al. Phase I study of single-agent AZD1775 (MK-1775), a Wee1 kinase inhibitor, in patients with refractory solid tumors. J Clin Oncol. 2015;33(30):3409–3415. doi: 10.1200/JCO.2014.60.4009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia TB, Uluisik RC, van Linden AA, Jones KL, Venkataraman S, Vibhakar R, Porter CC. Increased HDAC activity and c-MYC expression mediate acquired resistance to WEE1 inhibition in acute leukemia. Front Oncol. 2020;10:296. doi: 10.3389/fonc.2020.00296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GhelliLusernaDiRorà A, Beeharry N, Imbrogno E, Ferrari A, Robustelli V, Righi S, et al. Targeting WEE1 to enhance conventional therapies for acute lymphoblastic leukemia. J Hematol Oncol. 2018;11(1):99. doi: 10.1186/s13045-018-0641-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo E, Xiao R, Wu Y, Lu F, Liu C, Yang B, et al. WEE1 inhibition induces anti-tumor immunity by activating ERV and the dsRNA pathway. J Exp Med. 2022 doi: 10.1084/jem.20210789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haarberg HE, Paraiso KH, Wood E, Rebecca VW, Sondak VK, Koomen JM, Smalley KS. Inhibition of Wee1, AKT, and CDK4 underlies the efficacy of the HSP90 inhibitor XL888 in an in vivo model of NRAS-mutant melanoma. Mol Cancer Ther. 2013;12(6):901–912. doi: 10.1158/1535-7163.Mct-12-1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hai J, Liu S, Bufe L, Do K, Chen T, Wang X, et al. Synergy of WEE1 and mTOR inhibition in mutant KRAS-driven lung cancers. Clin Cancer Res. 2017;23(22):6993–7005. doi: 10.1158/1078-0432.CCR-17-1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PS, Venkataraman S, Alimova I, Birks DK, Balakrishnan I, Cristiano B, et al. Integrated genomic analysis identifies the mitotic checkpoint kinase WEE1 as a novel therapeutic target in medulloblastoma. Mol Cancer. 2014;13:72. doi: 10.1186/1476-4598-13-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heijink AM, Blomen VA, Bisteau X, Degener F, Matsushita FY, Kaldis P, et al. A haploid genetic screen identifies the G1/S regulatory machinery as a determinant of Wee1 inhibitor sensitivity. Proc Natl Acad Sci USA. 2015;112(49):15160–15165. doi: 10.1073/pnas.1505283112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirai H, Iwasawa Y, Okada M, Arai T, Nishibata T, Kobayashi M, et al. Small-molecule inhibition of Wee1 kinase by MK-1775 selectively sensitizes p53-deficient tumor cells to DNA-damaging agents. Mol Cancer Ther. 2009;8(11):2992–3000. doi: 10.1158/1535-7163.MCT-09-0463. [DOI] [PubMed] [Google Scholar]
- Jackson SP, Bartek J. The DNA-damage response in human biology and disease. Nature. 2009;461(7267):1071–1078. doi: 10.1038/nature08467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jhuraney A, Woods NT, Wright G, Rix L, Kinose F, Kroeger JL, et al. PAXIP1 potentiates the combination of WEE1 inhibitor AZD1775 and platinum agents in lung cancer. Mol Cancer Ther. 2016;15(7):1669–1681. doi: 10.1158/1535-7163.Mct-15-0182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HY, Cho Y, Kang H, Yim YS, Kim SJ, Song J, Chun KH. Targeting the WEE1 kinase as a molecular targeted therapy for gastric cancer. Oncotarget. 2016;7(31):49902–49916. doi: 10.18632/oncotarget.10231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ku BM, Bae YH, Koh J, Sun JM, Lee SH, Ahn JS, et al. Mutational status of TP53 defines the efficacy of Wee1 inhibitor AZD1775 in KRAS-mutant non-small cell lung cancer. Oncotarget. 2017;8(40):67526–67537. doi: 10.18632/oncotarget.18728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lallo A, Frese KK, Morrow CJ, Sloane R, Gulati S, Schenk MW, et al. The combination of the PARP inhibitor olaparib and the WEE1 inhibitor AZD1775 as a new therapeutic option for small cell lung cancer. Clin Cancer Res. 2018;24(20):5153–5164. doi: 10.1158/1078-0432.Ccr-17-2805. [DOI] [PubMed] [Google Scholar]
- Lau CC, Pardee AB. Mechanism by which caffeine potentiates lethality of nitrogen mustard. Proc Natl Acad Sci USA. 1982;79(9):2942–2946. doi: 10.1073/pnas.79.9.2942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee YT, Tan YJ, Oon CE. Molecular targeted therapy: treating cancer with specificity. Eur J Pharmacol. 2018;834:188–196. doi: 10.1016/j.ejphar.2018.07.034. [DOI] [PubMed] [Google Scholar]
- Lee JW, Parameswaran J, Sandoval-Schaefer T, Eoh KJ, Yang DH, Zhu F, et al. Combined aurora kinase A (AURKA) and WEE1 inhibition demonstrates synergistic antitumor effect in squamous cell carcinoma of the head and neck. Clin Cancer Res. 2019;25(11):3430–3442. doi: 10.1158/1078-0432.Ccr-18-0440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leijen S, van Geel RM, Pavlick AC, Tibes R, Rosen L, Razak AR, et al. Phase I study evaluating WEE1 inhibitor AZD1775 as monotherapy and in combination with gemcitabine, cisplatin, or carboplatin in patients with advanced solid tumors. J Clin Oncol. 2016;34(36):4371–4380. doi: 10.1200/JCO.2016.67.5991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leijen S, van Geel RM, Sonke GS, de Jong D, Rosenberg EH, Marchetti S, et al. Phase II study of WEE1 inhibitor AZD1775 plus carboplatin in patients with TP53-mutated ovarian cancer refractory or resistant to first-line therapy within 3 months. J Clin Oncol. 2016;34(36):4354–4361. doi: 10.1200/jco.2016.67.5942. [DOI] [PubMed] [Google Scholar]
- Lewis CW, Bukhari AB, Xiao EJ, Choi WS, Smith JD, Homola E, et al. Upregulation of Myt1 promotes acquired resistance of cancer cells to Wee1 inhibition. Cancer Res. 2019;79(23):5971–5985. doi: 10.1158/0008-5472.Can-19-1961. [DOI] [PubMed] [Google Scholar]
- Lheureux S, Cristea MC, Bruce JP, Garg S, Cabanero M, Mantia-Smaldone G, et al. Adavosertib plus gemcitabine for platinum-resistant or platinum-refractory recurrent ovarian cancer: a double-blind, randomised, placebo-controlled, phase 2 trial. Lancet. 2021;397(10271):281–292. doi: 10.1016/s0140-6736(20)32554-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F, Guo E, Huang J, Lu F, Yang B, Xiao R, et al. mTOR inhibition overcomes primary and acquired resistance to Wee1 inhibition by augmenting replication stress in epithelial ovarian cancers. Am J Cancer Res. 2020;10(3):908–924. [PMC free article] [PubMed] [Google Scholar]
- Li J, Pan C, Boese AC, Kang J, Umano AD, Magliocca KR, et al. DGKA provides platinum resistance in ovarian cancer through activation of c-JUN-WEE1 signaling. Clin Cancer Res. 2020;26(14):3843–3855. doi: 10.1158/1078-0432.Ccr-19-3790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Boren B, Huang PQ, Bunker KD, Doñate F, Samatar AA. Abstract 1965: Discovery of ZN-c3, a potent Wee-1 inhibitor with a differentiated pharmacologic and kinase selectivity profile. Cancer Res. 2021;81(13):1965. doi: 10.1158/1538-7445.AM2021-1965. [DOI] [Google Scholar]
- Liu D, Wu C, Jiao Y, Hou L, Lu D, Zheng H, et al. WEE1 kinase polymorphism as a predictive biomarker for efficacy of platinum-gemcitabine doublet chemotherapy in advanced non-small cell lung cancer patients. Sci Rep. 2015;5:11114. doi: 10.1038/srep11114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu D, Cao Z, Xu W, Lin G, Zhou X, Ding X, et al. Enhancement of chemosensitivity by WEE1 inhibition in EGFR-TKIs resistant non-small cell lung cancer. Biomed Pharmacother. 2019;117:109185. doi: 10.1016/j.biopha.2019.109185. [DOI] [PubMed] [Google Scholar]
- Liu JF, Xiong N, Campos SM, Wright AA, Krasner C, Schumer S, et al. Phase II study of the WEE1 inhibitor adavosertib in recurrent uterine serous carcinoma. J Clin Oncol. 2021;39(14):1531–1539. doi: 10.1200/jco.20.03167. [DOI] [PubMed] [Google Scholar]
- Magnussen GI, Holm R, Emilsen E, Rosnes AK, Slipicevic A, Flørenes VA. High expression of Wee1 is associated with poor disease-free survival in malignant melanoma: potential for targeted therapy. PLoS One. 2012;7(6):e38254. doi: 10.1371/journal.pone.0038254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masaki T, Shiratori Y, Rengifo W, Igarashi K, Matsumoto K, Nishioka M, et al. Hepatocellular carcinoma cell cycle: study of Long–Evans cinnamon rats. Hepatology. 2000;32(4 Pt 1):711–720. doi: 10.1053/jhep.2000.17705. [DOI] [PubMed] [Google Scholar]
- Masaki T, Shiratori Y, Rengifo W, Igarashi K, Yamagata M, Kurokohchi K, et al. Cyclins and cyclin-dependent kinases: comparative study of hepatocellular carcinoma versus cirrhosis. Hepatology. 2003;37(3):534–543. doi: 10.1053/jhep.2003.50112. [DOI] [PubMed] [Google Scholar]
- Matheson CJ, Backos DS, Reigan P. Targeting WEE1 kinase in cancer. Trends Pharmacol Sci. 2016;37(10):872–881. doi: 10.1016/j.tips.2016.06.006. [DOI] [PubMed] [Google Scholar]
- Méndez E, Rodriguez CP, Kao MC, Raju S, Diab A, Harbison RA, et al. A phase I clinical trial of AZD1775 in combination with neoadjuvant weekly docetaxel and cisplatin before definitive therapy in head and neck squamous cell carcinoma. Clin Cancer Res. 2018;24(12):2740–2748. doi: 10.1158/1078-0432.Ccr-17-3796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mir SE, De Witt Hamer PC, Krawczyk PM, Balaj L, Claes A, Niers JM, et al. In silico analysis of kinase expression identifies WEE1 as a gatekeeper against mitotic catastrophe in glioblastoma. Cancer Cell. 2010;18(3):244–257. doi: 10.1016/j.ccr.2010.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreira DC, Venkataraman S, Subramanian A, Desisto J, Balakrishnan I, Prince E, et al. Targeting MYC-driven replication stress in medulloblastoma with AZD1775 and gemcitabine. J Neurooncol. 2020;147(3):531–545. doi: 10.1007/s11060-020-03457-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller S, Hashizume R, Yang X, Kolkowitz I, Olow AK, Phillips J, et al. Targeting Wee1 for the treatment of pediatric high-grade gliomas. Neuro Oncol. 2014;16(3):352–360. doi: 10.1093/neuonc/not220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Music D, Dahlrot RH, Hermansen SK, Hjelmborg J, de Stricker K, Hansen S, Kristensen BW. Expression and prognostic value of the WEE1 kinase in gliomas. J Neurooncol. 2016;127(2):381–389. doi: 10.1007/s11060-015-2050-4. [DOI] [PubMed] [Google Scholar]
- Oku Y, Nishiya N, Tazawa T, Kobayashi T, Umezawa N, Sugawara Y, Uehara Y. Augmentation of the therapeutic efficacy of WEE1 kinase inhibitor AZD1775 by inhibiting the YAP-E2F1-DNA damage response pathway axis. FEBS Open Bio. 2018;8(6):1001–1012. doi: 10.1002/2211-5463.12440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oza AM, Estevez-Diz M, Grischke EM, Hall M, Marmé F, Provencher D, et al. A biomarker-enriched, randomized phase II trial of adavosertib (AZD1775) plus paclitaxel and carboplatin for women with platinum-sensitive TP53-mutant ovarian cancer. Clin Cancer Res. 2020;26(18):4767–4776. doi: 10.1158/1078-0432.Ccr-20-0219. [DOI] [PubMed] [Google Scholar]
- Poon RY. Cell cycle control: a system of interlinking oscillators. Methods Mol Biol. 2016;1342:3–19. doi: 10.1007/978-1-4939-2957-3_1. [DOI] [PubMed] [Google Scholar]
- PosthumaDeBoer J, Würdinger T, Graat HC, van Beusechem VW, Helder MN, van Royen BJ, Kaspers GJ. WEE1 inhibition sensitizes osteosarcoma to radiotherapy. BMC Cancer. 2011;11:156. doi: 10.1186/1471-2407-11-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi W, Zhang W, Edwards H, Chu R, Madlambayan GJ, Taub JW, et al. Synergistic anti-leukemic interactions between panobinostat and MK-1775 in acute myeloid leukemia ex vivo. Cancer Biol Ther. 2015;16(12):1784–1793. doi: 10.1080/15384047.2015.1095406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richer AL, Cala JM, O'Brien K, Carson VM, Inge LJ, Whitsett TG. WEE1 kinase inhibitor AZD1775 has preclinical efficacy in LKB1-deficient non-small cell lung cancer. Cancer Res. 2017;77(17):4663–4672. doi: 10.1158/0008-5472.CAN-16-3565. [DOI] [PubMed] [Google Scholar]
- Russell P, Nurse P. Negative regulation of mitosis by wee1+, a gene encoding a protein kinase homolog. Cell. 1987;49(4):559–567. doi: 10.1016/0092-8674(87)90458-2. [DOI] [PubMed] [Google Scholar]
- Sanai N, Li J, Boerner J, Stark K, Wu J, Kim S, et al. Phase 0 trial of AZD1775 in first-recurrence glioblastoma patients. Clin Cancer Res. 2018;24(16):3820–3828. doi: 10.1158/1078-0432.Ccr-17-3348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sancar A, Lindsey-Boltz LA, Unsal-Kaçmaz K, Linn S. Molecular mechanisms of mammalian DNA repair and the DNA damage checkpoints. Annu Rev Biochem. 2004;73:39–85. doi: 10.1146/annurev.biochem.73.011303.073723. [DOI] [PubMed] [Google Scholar]
- Seligmann JF, Fisher DJ, Brown LC, Adams RA, Graham J, Quirke P, et al. Inhibition of WEE1 Is effective in TP53- and RAS-mutant metastatic colorectal cancer: a randomized trial (FOCUS4-C) comparing adavosertib (AZD1775) with active monitoring. J Clin Oncol. 2021;39(33):3705–3715. doi: 10.1200/jco.21.01435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen T, Tong P, Diao L, Li L, Fan Y, Hoff J, et al. Targeting AXL and mTOR pathway overcomes primary and acquired resistance to WEE1 inhibition in small-cell lung cancer. Clin Cancer Res. 2017;23(20):6239–6253. doi: 10.1158/1078-0432.Ccr-17-1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma A, Madhunapantula SV, Gowda R, Berg A, Neves RI, Robertson GP. Identification of aurora kinase B and Wee1-like protein kinase as downstream targets of (V600E)B-RAF in melanoma. Am J Pathol. 2013;182(4):1151–1162. doi: 10.1016/j.ajpath.2012.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slipicevic A, Holth A, Hellesylt E, Tropé CG, Davidson B, Flørenes VA. Wee1 is a novel independent prognostic marker of poor survival in post-chemotherapy ovarian carcinoma effusions. Gynecol Oncol. 2014;135(1):118–124. doi: 10.1016/j.ygyno.2014.07.102. [DOI] [PubMed] [Google Scholar]
- Smith HL, Southgate H, Tweddle DA, Curtin NJ. DNA damage checkpoint kinases in cancer. Expert Rev Mol Med. 2020;22:e2. doi: 10.1017/erm.2020.3. [DOI] [PubMed] [Google Scholar]
- Tanaka N, Patel AA, Tang L, Silver NL, Lindemann A, Takahashi H, et al. Replication stress leading to apoptosis within the S-phase contributes to synergism between vorinostat and AZD1775 in HNSCC harboring high-risk TP53 mutation. Clin Cancer Res. 2017;23(21):6541–6554. doi: 10.1158/1078-0432.Ccr-17-0947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolcher A, Mamdani H, Chalasani P, Meric-Bernstam F, Gazdoiu M, Makris L, Pultar P, Voliotis D. Abstract CT016: Clinical activity of single-agent ZN-c3, an oral WEE1 inhibitor, in a phase 1 dose-escalation trial in patients with advanced solid tumors. Cancer Res. 2021;81(13 Suppl):CT016. doi: 10.1158/1538-7445.AM2021-CT016. [DOI] [Google Scholar]
- Wang Y, Li J, Booher RN, Kraker A, Lawrence T, Leopold WR, Sun Y. Radiosensitization of p53 mutant cells by PD0166285, a novel G(2) checkpoint abrogator. Cancer Res. 2001;61(22):8211–8217. [PubMed] [Google Scholar]
- Wang H, Huang M, Zhang DY, Zhang F. Global profiling of signaling networks: study of breast cancer stem cells and potential regulation. Oncologist. 2011;16(7):966–979. doi: 10.1634/theoncologist.2010-0230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster PJ, Littlejohns AT, Gaunt HJ, Young RS, Rode B, Ritchie JE, et al. Upregulated WEE1 protects endothelial cells of colorectal cancer liver metastases. Oncotarget. 2017;8(26):42288–42299. doi: 10.18632/oncotarget.15039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisberg E, Nonami A, Chen Z, Liu F, Zhang J, Sattler M, et al. Identification of Wee1 as a novel therapeutic target for mutant RAS-driven acute leukemia and other malignancies. Leukemia. 2015;29(1):27–37. doi: 10.1038/leu.2014.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao R, You L, Zhang L, Guo X, Guo E, Zhao F, et al. Inhibiting the IRE1α axis of the unfolded protein response enhances the antitumor effect of AZD1775 in TP53 mutant ovarian cancer. Adv Sci (Weinh) 2022;9(21):e2105469. doi: 10.1002/advs.202105469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L, Shen C, Pettit CJ, Li T, Hu AJ, Miller ED, et al. Wee1 kinase inhibitor AZD1775 effectively sensitizes esophageal cancer to radiotherapy. Clin Cancer Res. 2020;26(14):3740–3750. doi: 10.1158/1078-0432.Ccr-19-3373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin Y, Shen Q, Tao R, Chang W, Li R, Xie G, et al. Wee1 inhibition can suppress tumor proliferation and sensitize p53 mutant colonic cancer cells to the anticancer effect of irinotecan. Mol Med Rep. 2018;17(2):3344–3349. doi: 10.3892/mmr.2017.8230. [DOI] [PubMed] [Google Scholar]
- Zehir A, Benayed R, Shah RH, Syed A, Middha S, Kim HR, et al. Mutational landscape of metastatic cancer revealed from prospective clinical sequencing of 10,000 patients. Nat Med. 2017;23(6):703–713. doi: 10.1038/nm.4333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou L, Zhang Y, Chen S, Kmieciak M, Leng Y, Lin H, et al. A regimen combining the Wee1 inhibitor AZD1775 with HDAC inhibitors targets human acute myeloid leukemia cells harboring various genetic mutations. Leukemia. 2015;29(4):807–818. doi: 10.1038/leu.2014.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Z, Zhong L, Chu X, Wan P, Dan W, Shao X, et al. HDAC11 mediates the ubiquitin-dependent degradation of p53 and inhibits the anti-leukemia effect of PD0166285. Med Oncol. 2023;40(11):325. doi: 10.1007/s12032-023-02196-2. [DOI] [PubMed] [Google Scholar]
- Zhu X, Su Q, Xie H, Song L, Yang F, Zhang D, et al. SIRT1 deacetylates WEE1 and sensitizes cancer cells to WEE1 inhibition. Nat Chem Biol. 2023;19(5):585–595. doi: 10.1038/s41589-022-01240-y. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.