Abstract
Background
Up to the end of January, 2022, South Africa has had four recognisable COVID-19 pandemic waves, each predominantly dominated by one variant of concern: the ancestral strain with an Asp614Gly mutation during the first wave, the beta variant (B.1.351) during the second wave, the delta variant (B.1.617.2) during the third wave, and lastly, the omicron variant (B.1.1.529) during the fourth wave. We aimed to assess the clinical disease severity of patients admitted to hospital with SARS-CoV-2 infection during the omicron wave and compare the findings with those of the preceding three pandemic waves in South Africa.
Methods
We defined the start and end of each pandemic wave as the crossing of the threshold of weekly incidence of 30 laboratory-confirmed SARS-CoV-2 cases per 100 000 population. Hospital admission data were collected through an active national COVID-19-specific surveillance programme. We compared disease severity across waves by post-imputation random effect multivariable logistic regression models. Severe disease was defined as one or more of the following: acute respiratory distress, receipt of supplemental oxygen or mechanical ventilation, admission to intensive care, or death.
Findings
We analysed 335 219 laboratory-confirmed SARS-CoV-2 hospital admissions with a known outcome, constituting 10·4% of 3 216 179 cases recorded during the four waves. During the omicron wave, 52 038 (8·3%) of 629 617 cases were admitted to hospital, compared with 71 411 (12·9%) of 553 530 in the Asp614Gly wave, 91 843 (12·6%) of 726 772 in the beta wave, and 131 083 (10·0%) of 1 306 260 in the delta wave (p<0·0001). During the omicron wave, 15 421 (33·6%) of 45 927 patients admitted to hospital had severe disease, compared with 36 837 (52·3%) of 70 424 in the Asp614Gly wave, 57 247 (63·4%) of 90 310 in the beta wave, and 81 040 (63·0%) of 128 558 in the delta wave (p<0·0001). The in-hospital case-fatality ratio during the omicron wave was 10·7%, compared with 21·5% during the Asp614Gly wave, 28·8% during the beta wave, and 26·4% during the delta wave (p<0·0001). Compared with those admitted to hospital during the omicron wave, patients admitted during the other three waves had more severe clinical presentations (adjusted odds ratio 2·07 [95% CI 2·01–2·13] in the Asp614Gly wave, 3·59 [3·49–3·70] in the beta wave, and 3·47 [3·38–3·57] in the delta wave).
Interpretation
The trend of increasing cases and admissions across South Africa's first three waves shifted in the omicron wave, with a higher and quicker peak but fewer patients admitted to hospital, less clinically severe illness, and a lower case-fatality ratio compared with the preceding three waves. Omicron marked a change in the SARS-CoV-2 epidemic curve, clinical profile, and deaths in South Africa. Extrapolations to other populations should factor in differing vaccination and previous infection levels.
Funding
National Institute for Communicable Diseases.
Introduction
The fifth SARS-CoV-2 variant of concern, omicron (B.1.1.529), was first publicly announced in South Africa on Nov 25, 2021.1 Within days, omicron led to a resurgence of SARS-CoV-2 cases in South Africa and several other countries.2
Genomic sequencing revealed that, in South Africa, 1353 (86%) of 1579 sequenced SARS-CoV-2 samples in November, 2021, and 1361 (99%) of 1377 of those in December, 2021, were omicron.3 The proportion of real-time RT-PCR (rtPCR)-positive tests with S gene target failure, a marker of omicron,4 was 2% (11 of 458) in October, 95% (10 536 of 11 037) in November, and 98% (19 174 of 19 638) in December.5 Phylogenetic surveillance showed that, in South Africa, the predominant variants (>90% of viral sequences) were the ancestral strain with an Asp614Gly mutation during the first wave (June to August, 2020), the beta variant (B.1.351) during the second wave (November, 2020 to February, 2021), and the delta variant (B.1.617.2) during the third wave (May to September, 2021).3
Research in context.
Evidence before this study
The omicron (B.1.1.529) variant of SARS-CoV-2 drove increases in COVID-19 cases and hospitalisations in South Africa between November, 2021, and January, 2022, and has been identified in at least 175 countries across the globe. Previous variants have been found to be more transmissible and to cause more severe disease compared with the SARS-CoV-2 ancestral strain. Early indications suggested that omicron was highly transmissible and associated with some immune escape. In South Africa, just before the omicron-dominated fourth wave, 35% of the adult population was fully vaccinated, and community-based surveys showed seroprevalence levels of 73%. Considering the early data on transmissibility, immune escape, and high level of so-called hybrid immunity in South Africa, data on the severity of the omicron variant would be important for guiding public health action. We searched PubMed and medRxiv using the terms “SARS-CoV-2”, “omicron”, and “severity”, and we included publications from Jan 1, 2020, to Jan 20, 2022, without language restrictions. Studies from South Africa, Denmark, and the UK suggested significantly reduced odds of hospitalisation and severe disease for individuals infected with omicron compared with those infected with the delta (B.1.617.2) variant, but these studies included early data in the first 4–6 weeks of the omicron wave. Tissue-based studies showed that omicron infects the cells of the bronchus more efficiently but alveolar cells of the lungs less efficiently than the delta variant.
Added value of this study
We analysed data from the DATCOV national active hospital surveillance system for COVID-19 hospitalisations, comparing disease severity between the first pandemic wave dominated by an Asp614Gly mutation of the ancestral strain, the second wave dominated by the beta (B.1.351) variant, the third wave dominated by the delta variant, and the fourth wave dominated by the omicron variant. Our study revealed that during the omicron-dominated fourth wave, a lower proportion of individuals were admitted to hospital compared with the other three waves, and that among patients admitted to hospital, a lower proportion required invasive ventilation or treatment in intensive care, had severe disease, or died in hospital compared with the preceding three waves. After adjusting for age, sex, race, comorbidities, health sector, and province, we found approximately a two-to-three-times higher risk of severe disease in the first three waves compared with the omicron-dominated fourth wave. Our analysis did not include individual-level data on lineage, vaccination status, or previous infections.
Implications of all the available evidence
The reasons for the lower admission rates and less severe infections in patients admitted to hospital during the omicron-dominated fourth wave were likely to be due to both a less virulent virus and high immunity from previous infections or vaccination. This analysis adds to the available evidence of decreased disease severity during the omicron-dominated wave, with use of data from South Africa's large national surveillance system, comparing all admissions reported in each full wave period across all four waves of COVID-19. The country's well developed surveillance systems for variant identification and monitoring hospitalisation were essential to rapidly investigate the effect of omicron, and they continue to be important for pandemic preparedness for new SARS-CoV-2 variants.
The mutations identified in omicron suggested that it would probably be highly transmissible, with immune escape, but provided no indication on whether it would have a different clinical severity profile compared with previous variants.1 Clinical severity of COVID-19 is influenced by several factors besides virulence of the viral variant, including age, sex, race, comorbidities, vaccination status, immunity from previous SARS-CoV-2 infection, and early therapy or prophylaxis.
The South African COVID-19 vaccination programme began with health-care workers in February, 2021. It subsequently expanded to adults older than 60 years in May, 2021, and then subsequently to other age groups until adolescents aged 12–17 years were included in mid-October, 2021. As a result, vaccination coverage was low during the delta wave but by Nov 17, 2021, before the omicron wave started, 35% of South Africa's adult population were fully vaccinated with either two doses of BNT162b2 (tozinameran; Pfizer-BioNtech) or one dose of Ad26.CoV2.S (Janssen).6 A third dose of BNT162b2 and a second dose of Ad26.CoV2.S only became available at the tail end of the omicron wave in January, 2022. Additionally, a substantial number of people had been infected with SARS-CoV-2 during each wave. SARS-CoV-2 seroprevalence was 47% (95% CI 46–49) in blood donors in South Africa after the second wave7 and 73% (72–74) in a community-based survey in Gauteng province after the third wave.8 Early treatment with remdesivir or monoclonal antibodies is not widely available and is infrequently used in South Africa.
In this study, we aimed to assess the clinical severity of COVID-19 in patients admitted to hospital with laboratory-confirmed SARS-CoV-2 infection during the omicron wave and whether it differed from the Asp614Gly mutation, beta variant, and delta variant waves in South Africa.
Methods
Study design and data collection
We collated data on rtPCR and antigen-positive SARS-CoV-2 cases daily from laboratory reports,9 while data on COVID-19 hospital admissions were collected through DATCOV, an active surveillance programme established specifically for COVID-19.10 We did secondary data analysis using data from the DATCOV national hospital surveillance database from March 5, 2020, to Jan 22, 2022. DATCOV surveillance collects data on all individuals with a positive SARS-CoV-2 rtPCR test or antigen test, with a confirmed duration of stay in hospital of 1 full day or longer, regardless of reason for admission. This included patients who had COVID-19 symptoms, were admitted for isolation, acquired nosocomial COVID-19 infection, or tested positive incidentally when admitted for other reasons. Incidental positive SARS-CoV-2 tests have been noted to occur mainly during the initial period, when cases are rising, of all four waves in South Africa. Some of the patients admitted during a COVID-19 wave might have been admitted in the preceding waves; these repeat admissions (more than 90 days after the first positive SARS-CoV-2 test) were included in the analysis. We calculated incidence risks using mid-year population figures for 2020 from Statistics South Africa.11
We defined severe COVID-19 disease as one or more of the following: development of acute respiratory distress syndrome, receipt of oxygen or invasive mechanical ventilation, treatment in high-care or intensive-care units (ICUs), or death, using a modified definition based on the recommendations from the WHO Clinical Platform External Clinical Advisory Group.12
The Human Research Ethics Committee (Medical) at the University of the Witwatersrand (Johannesburg, South Africa) approved the project protocol as part of a national surveillance programme (M160667). Because COVID-19 is a notifiable disease, individual patient consent was waived.
Definition of COVID-19 pandemic waves in South Africa
Each COVID-19 wave was defined as the period starting in the week in which the country surpassed a weekly incidence risk of 30 cases per 100 000 individuals and ending in the following week in which the weekly incidence dropped below that value.13, 14 The omicron-dominated wave crossed the weekly incidence risk threshold in the last week of November, 2021. The start of each of these four wave periods selected also correlated with most cases being due to the Asp614Gly mutation, beta variant, delta variant, and omicron variant, respectively.3 The full wave periods were included for all four waves: wave 1 lasted from week 24 to week 34, 2020 (June 7 to Aug 22; 76 days); wave 2 lasted from week 47, 2020, to week 5, 2021 (Nov 15, 2020, to Feb 6, 2021; 83 days); wave 3 lasted from week 19 to week 37, 2021 (May 9 to Sept 18; 132 days); and wave 4 lasted from week 47, 2021, to week 3, 2022 (Nov 21, 2021, to Jan 22, 2022; 62 days).
Statistical analysis
Analysis of disease severity was restricted to patients admitted to hospital who had already accumulated outcomes; all patients still in hospital or transferred to other hospitals without final outcomes were excluded because they remained at risk of developing severe outcomes, including death. We used descriptive statistics to describe the trends in cases, hospital admissions, severe disease, and death over the equivalent periods of the Asp614Gly (first), beta (second), delta (third), and omicron (fourth) waves. Bivariate comparisons between wave periods used the Wilcoxon rank-sum (Mann-Whitney) test to compare continuous variables (length of stay), and the Pearson χ2 test to compare categorical variables (disease severity, need of oxygen, need of intensive care, and death).
We used post-imputation random effect (on admission facility) multivariable logistic regression models to compare severe disease between waves. To account for incomplete or missing data on selected variables, we used multivariate imputation by chained equation and generated ten complete imputed datasets that were used for subsequent analyses. Variables analysed with multivariate imputation by chained equation included race and comorbidities, where up to a third of the data were missing. Complete or near-complete variables included in the imputation process were age, sex, province of hospitalisation, health sector (ie, public or private), disease severity, and in-hospital outcome (ie, discharged alive or died).
Age, sex, race, presence of a comorbidity (including hypertension, diabetes, chronic cardiac disease, chronic kidney disease, asthma or chronic pulmonary disease, cancer, HIV, or tuberculosis), type of health sector (private or public), and province of hospitalisation were included in the model to assess the relationship between each wave period and disease severity in patients with a positive SARS-CoV-2 test who were admitted to hospital. The presence of obesity, while important, was excluded from the analysis due to poor data completeness for this variable. The statistical analysis was implemented using Stata, version 15. We followed STROBE guideline recommendations.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
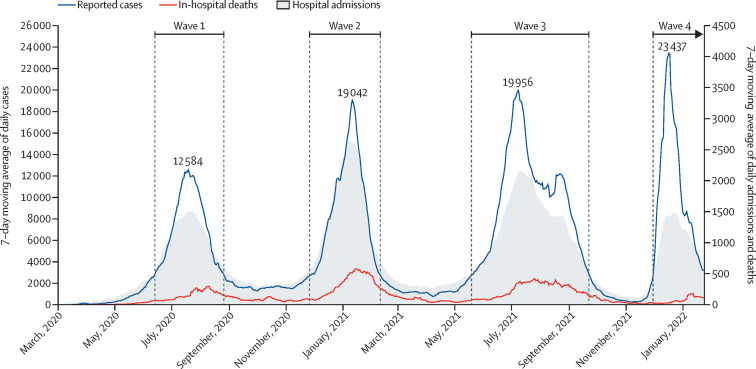
To date, South Africa has had four distinct waves of SARS-CoV-2 infections, with approximately 3-month periods of low transmission between each wave (figure 1 ). The 7-day moving average of daily cases had a peak that was higher in each successive peak of the four waves. Although the wave duration increased across the first three waves, it declined in the fourth wave. The number of SARS-CoV-2 positive cases identified during each wave was 553 530 in the Asp614Gly wave, 726 772 in the beta wave, 1 306 260 in the delta wave, and 629 617 in the omicron wave (table 1 ). Unlike the pattern observed in the preceding waves, the rise in cases during the omicron wave was not accompanied by a concomitant rise in hospital admissions (figure 1); instead, the peak in admissions was lower and of shorter duration than those of the preceding waves. The proportion of cases admitted to hospital was higher in the first three waves than in the omicron wave (p<0·0001; table 1).
Figure 1.
7-day moving average of SARS-CoV-2 cases, COVID-19 hospital admissions, and in-hospital deaths in South Africa, March 5, 2020, to Jan 22, 2022
Table 1.
Summary of SARS-CoV-2 cases, COVID-19 admissions, and in-hospital deaths for four SARS-CoV-2 pandemic waves in South Africa
| SARS-CoV-2 positive cases | Incidence of SARS-CoV-2 positive cases, per 100 000 individuals | Cases admitted to hospital | p value | Proportion of admitted cases with an outcome who died in hospital | p value | |
|---|---|---|---|---|---|---|
| All ages | ||||||
| Asp614Gly | 553 530 | 928·4 | 71 411 (12·9%) | <0.0001 | 15 144 (21·5%) | <0·0001 |
| Beta | 726 772 | 1219·0 | 91 843 (12·6%) | <0·0001 | 26 032 (28·8%) | <0·0001 |
| Delta | 1 306 260 | 2190·9 | 131 083 (10·0%) | <0·0001 | 33 947 (26·4%) | <0·0001 |
| Omicron | 629 617 | 1056·0 | 52 038 (8·3%) | .. | 4907 (10·7%) | .. |
| Age <5 years | ||||||
| Asp614Gly | 6280 | 109·3 | 812 (12·9%) | <0·0001 | 41 (5·1%) | <0·0001 |
| Beta | 8522 | 148·4 | 1284 (15·1%) | <0·0001 | 56 (4·5%) | <0·0001 |
| Delta | 19 019 | 331·1 | 2797 (14·7%) | <0·0001 | 109 (4·0%) | <0·0001 |
| Omicron | 14 050 | 244·6 | 3568 (25·4%) | .. | 67 (2·1%) | .. |
| Age 5–19 years | ||||||
| Asp614Gly | 41 829 | 260·1 | 1550 (3·7%) | <0·0001 | 59 (3·9%) | <0·0001 |
| Beta | 56 873 | 353·6 | 1517 (2·7%) | <0·0001 | 70 (4·8%) | <0·0001 |
| Delta | 188 689 | 1173·3 | 4359 (2·3%) | <0·0001 | 121 (2·9%) | 0·0024 |
| Omicron | 68 778 | 427·7 | 3899 (5·7%) | .. | 62 (1·8%) | .. |
| Age 20–39 years | ||||||
| Asp614Gly | 223 169 | 1078·9 | 15 039 (6·7%) | <0·0001 | 1051 (7·1%) | <0·0001 |
| Beta | 271 440 | 1312·3 | 15 658 (5·8%) | <0·0001 | 1581 (10·3%) | <0·0001 |
| Delta | 483 252 | 2336·3 | 24 241 (5·0%) | <0·0001 | 2193 (9·3%) | <0·0001 |
| Omicron | 273 902 | 1324·2 | 17 027 (6·2%) | .. | 649 (4·3%) | .. |
| Age 40–59 years | ||||||
| Asp614Gly | 208 211 | 1781·7 | 29 504 (14·2%) | <0·0001 | 4933 (16·9%) | <0·0001 |
| Beta | 258 981 | 2216·1 | 35 958 (13·9%) | <0·0001 | 8182 (23·1%) | <0·0001 |
| Delta | 437 093 | 3740·3 | 48 909 (11·2%) | <0·0001 | 11 097 (23·1%) | <0·0001 |
| Omicron | 188 486 | 1612·9 | 12 259 (6·5%) | .. | 1199 (11·2%) | .. |
| Age ≥60 years | ||||||
| Asp614Gly | 74 041 | 1364·4 | 24 506 (33·1%) | <0·0001 | 9266 (37·5%) | <0·0001 |
| Beta | 130 956 | 2413·3 | 37 426 (28·6%) | <0·0001 | 16 469 (43·9%) | <0·0001 |
| Delta | 178 207 | 3284·0 | 50 777 (28·5%) | <0·0001 | 20 872 (40·9%) | <0·0001 |
| Omicron | 84 401 | 1555·4 | 15 285 (18·1%) | .. | 2008 (22·2%) | .. |
Data are n or n (%). The p values are comparing the omicron wave with the Asp614Gly, beta, and delta waves. The predominant SARS-CoV-2 variants in each of the four COVID-19 waves in South Africa were, in order: Asp614Gly mutation (June 7 to Aug 22, 2020), beta variant (B.1.351; Nov 15, 2020, to Feb 6, 2021), delta variant (B.1.617·2; May 9 to Sept 18, 2021), and omicron variant (B.1.1.529; Nov 21, 2021, to Jan 22, 2022). All ages: population 59 622 350, 25·0% fully vaccinated. * Age <5 years: population 5 743 450; 0% fully vaccinated. Age 5–19 years: population 16 082 084, 1·5% fully vaccinated. * Age 20–39 years: population 20 684 164, 22·9% fully vaccinated.* Age 40–59 years: population 11 686 162, 46·0% fully vaccinated.* Age ≥60 years: population 5 426 490, 57·8% fully vaccinated.* *Vaccination coverage data for the omicron wave is from Nov 14, 2021.6
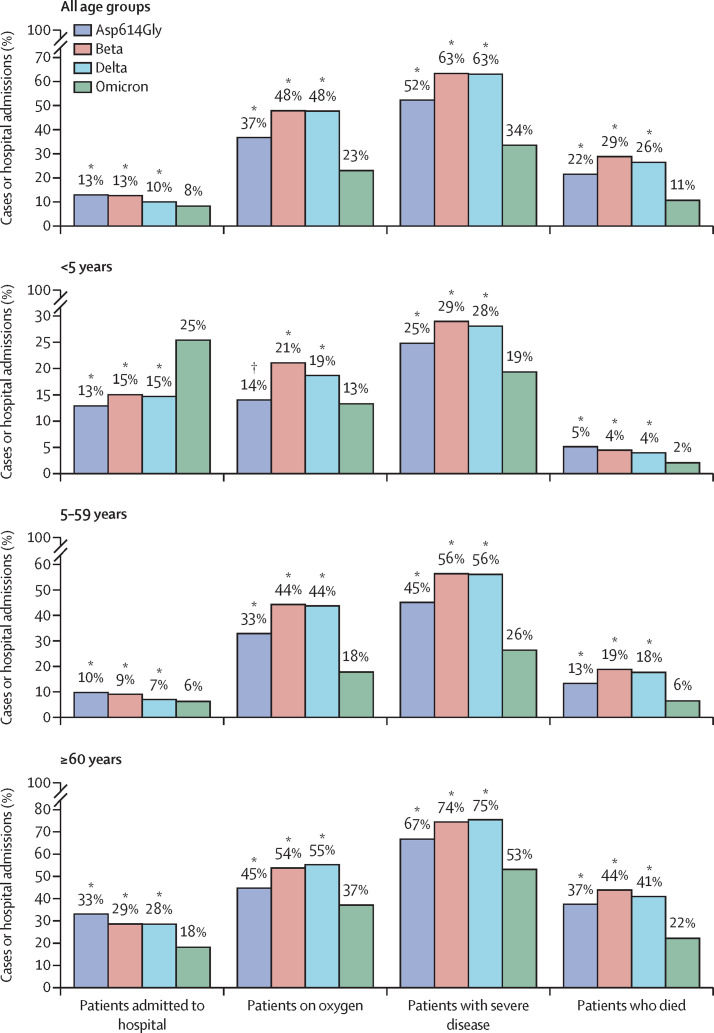
We analysed 335 219 laboratory-confirmed SARS-CoV-2-positive hospital admissions with a known outcome, constituting 10·4% of 3 216 179 cases recorded during the four waves. For the omicron wave, clinical outcomes were known for 45 927 (88·3%) of 52 038 patients positive for SARS-CoV-2 who were admitted to hospital as of Jan 22, 2022; the remainder were still in hospital and did not yet have a documented in-hospital outcome. Outcomes were unknown for 987 (1·4%) of 71 411 patients admitted to hospital in the Asp614Gly wave, 1533 (1·7%) of 91 843 in the beta wave, and 2525 (1·9%) of 131 083 in the delta wave. In patients with known clinical outcomes, 36 837 (52·3%) of 70 424 in the Asp614Gly wave, 57 247 (63·4%) of 90 310 in the beta wave, and 81 040 (63·0%) of 128 558 in the delta wave met the criteria for severe disease, compared with 15 421 (33·6%) of 45 927 in the omicron wave (p<0·0001; table 2 ). The proportion of patients requiring supplemental oxygen was lower during the omicron wave than during the other three waves (p<0·0001; table 2, figure 2 ). Median length of hospital stay was also lower in the omicron wave than in the other three waves (p<0·0001; table 2). The in-hospital case-fatality ratio during the omicron wave was 10·7%, compared with 21·5% during the Asp614Gly wave, 28·8% during the beta wave, and 26·4% during the delta wave (p<0·0001; table 1).
Table 2.
Indicators of disease severity among SARS-CoV-2 positive cases admitted in each of four SARS-CoV-2 pandemic waves in South Africa
| Cases admitted to hospital with known outcome | Median length of stay, days | p value | Proportion of admitted cases who received supplemental oxygen | p value | Proportion of admitted cases who were treated in ICU | p value | Proportion of admitted cases who had severe disease | p value | |
|---|---|---|---|---|---|---|---|---|---|
| All ages | |||||||||
| Asp614Gly | 70 424 | 6 (3–11) | <0·0001 | 25 890 (36·8%) | <0·0001 | 11 125 (15·8%) | <0·0001 | 36 837 (52·3%) | <0·0001 |
| Beta | 90 310 | 6 (3–10) | <0·0001 | 43 235 (47·9%) | <0·0001 | 11 597 (12·8%) | <0·0001 | 57 247 (63·4%) | <0·0001 |
| Delta | 128 558 | 6 (3–11) | <0·0001 | 61 318 (47·7%) | <0·0001 | 18 812 (14·6%) | <0·0001 | 81 040 (63·0%) | <0·0001 |
| Omicron | 45 927 | 4 (2–8) | .. | 10 565 (23·0%) | .. | 2872 (6·3%) | .. | 15 421 (33·6%) | .. |
| Age <5 years | |||||||||
| Asp614Gly | 798 | 4 (2–8) | <0·0001 | 112 (14·0%) | 0·64 | 73 (9·1%) | <0·0001 | 198 (24·8%) | 0·0010 |
| Beta | 1249 | 4 (2–8) | <0·0001 | 263 (21·1%) | <0·0001 | 97 (7·8%) | <0·0001 | 362 (29·0%) | <0·0001 |
| Delta | 2732 | 3 (2–6) | <0·0001 | 509 (18·6%) | <0·0001 | 184 (6·7%) | <0·0001 | 767 (28·1%) | <0·0001 |
| Omicron | 3242 | 3 (2–5) | .. | 432 (13·3%) | .. | 127 (3·9%) | .. | 627 (19·3%) | .. |
| Age 5–19 years | |||||||||
| Asp614Gly | 1529 | 5 (2–9) | <0·0001 | 200 (13·1%) | 0·034 | 108 (7·1%) | <0·0001 | 318 (20·8%) | 0·0010 |
| Beta | 1471 | 4 (2–9) | <0·0001 | 308 (20·9%) | <0·0001 | 80 (5·4%) | 0·0010 | 427 (29·0%) | <0·0001 |
| Delta | 4212 | 5 (2–9) | <0·0001 | 768 (18·2%) | <0·0001 | 206 (4·9%) | 0·0010 | 1056 (25·1%) | <0·0001 |
| Omicron | 3503 | 3 (2–5) | .. | 384 (11·0%) | .. | 118 (3·4%) | .. | 593 (16·9%) | .. |
| Age 20–39 years | |||||||||
| Asp614Gly | 14 809 | 5 (2–10) | <0·0001 | 3330 (22·5%) | <0·0001 | 1293 (8·7%) | <0·0001 | 4672 (31·5%) | <0·0001 |
| Beta | 15 361 | 5 (3–9) | <0·0001 | 5290 (34·4%) | <0·0001 | 1177 (7·7%) | <0·0001 | 6547 (42·6%) | <0·0001 |
| Delta | 23 700 | 5 (3–9) | <0·0001 | 7641 (32·2%) | <0·0001 | 2059 (8·7%) | <0·0001 | 9718 (41·0%) | <0·0001 |
| Omicron | 15 259 | 3 (2–7) | .. | 2121 (13·9%) | .. | 502 (3·3%) | .. | 3202 (21·0%) | .. |
| Age 40–59 years | |||||||||
| Asp614Gly | 29 120 | 7 (4–11) | <0·0001 | 11 441 (39·3%) | <0·0001 | 4937 (17·0%) | <0·0001 | 15 515 (53·3%) | <0·0001 |
| Beta | 35 426 | 6 (4–10) | <0·0001 | 17 574 (49·6%) | <0·0001 | 5290 (14·9%) | <0·0001 | 22 508 (63·5%) | <0·0001 |
| Delta | 48 010 | 7 (4–11) | <0·0001 | 24 817 (51·7%) | <0·0001 | 8553 (17·8%) | <0·0001 | 31 854 (66·3%) | <0·0001 |
| Omicron | 10 703 | 5 (2–8) | .. | 2728 (25·5%) | .. | 723 (6·8%) | .. | 3975 (37·1%) | .. |
| Age ≥60 years | |||||||||
| Asp614Gly | 24 168 | 7 (3–13) | <0·0001 | 10 807 (44·7%) | <0·0001 | 4714 (19·5%) | <0·0001 | 16 134 (66·8%) | <0·0001 |
| Beta | 36 803 | 6 (3–11) | <0·0001 | 19 800 (53·8%) | <0·0001 | 4953 (13·5%) | <0·0001 | 27 403 (74·5%) | <0·0001 |
| Delta | 49 904 | 7 (4–12) | <0·0001 | 27 583 (55·3%) | <0·0001 | 7810 (15·7%) | <0·0001 | 37 645 (75·4%) | <0·0001 |
| Omicron | 13 220 | 5 (3–9) | .. | 4900 (37·1%) | .. | 1402 (10·6%) | .. | 7024 (53·1%) | .. |
Data are n, median (IQR), or n (%). The p values are comparing the omicron wave with the Asp614Gly, beta, and delta waves. The predominant SARS-CoV-2 variants in each of the four COVID-19 waves in South Africa were, in order: Asp614Gly mutation (June 7 to Aug 22, 2020), beta variant (B.1.351; Nov 15, 2020, to Feb 6, 2021), delta variant (B.1.617·2; May 9 to Sept 18, 2021), and omicron variant (B.1.1.529; Nov 21, 2021, to Jan 22, 2022). All ages: population 59 622 350, 25·0% fully vaccinated. Age <5 years: population 5 743 450; 0% fully vaccinated. Age 5–19 years: population 16 082 084, 1·5% fully vaccinated. Age 20–39 years: population 20 684 164, 22·9% fully vaccinated. Age 40–59 years: population 11 686 162, 46·0% fully vaccinated. Age ≥60 years: population 5 426 490, 57·8% fully vaccinated. ICU=intensive care unit.
Figure 2.
Proportion of cases admitted, admissions who received supplementary oxygen, patients with severe disease, and in-hospital deaths, for individuals of all ages, those younger than 5 years, those aged 6–59 years, and those aged 60 years or older
Proportions presented for each COVID-19 wave in South Africa: Asp614Gly (June 7, to Aug 22, 2020), beta (B.1.351; Nov 15, 2020, to Feb 6, 2021), delta (B.1.617.2; May 9, to Sept 18, 2021), and omicron (B.1.1.529; Nov 21, 2021, to Jan 22, 2022). *p<0·001; †p>0·05 comparing omicron wave to the Asp614Gly, beta, and delta waves.
Children and adolescents (individuals younger than 20 years) constituted 14·3% (7467 of 52 038) of total hospital admissions in the omicron wave, compared with 3·3% (2362 of 71 411) in the Asp614Gly wave, 3·0% (2801 of 91 843) in the beta wave, and 5·5% (7156 of 131 083) in the delta wave. In children younger than 5 years, 3568 (25·4%) of 14 050 laboratory-confirmed cases were admitted to hospital during the omicron wave compared with 2797 (14·7%) of 19 019 during the delta wave, but the number of children younger than 5 years who were admitted to hospital was similar in both waves and was higher than that during the Asp614Gly and beta waves (table 1). The proportion of children younger than 5 years admitted to hospital who had severe disease was lower in the omicron wave than in the other three waves (p<0·001; table 2).
On multivariable analysis, compared with those admitted to hospital in the omicron wave, patients were more likely to have severe disease if they were admitted to hospital in the Asp614Gly wave (adjusted odds ratio 2·07, 95% CI 2·01–2·13), beta wave (3·59, 3·49–3·70), and delta wave (3·47, 3·38–3·57; table 3 ). Other factors associated with severe disease in this patient population were older age, being male, being Indian (compared with being White), presence of a comorbidity, and the province of hospital admission.
Table 3.
Factors associated with severe disease among patients admitted to hospital with a SARS-CoV-2-positive test in the four pandemic waves in South Africa
| Proportion with severe disease | Unadjusted odds ratio | Adjusted odds ratio | p value | |
|---|---|---|---|---|
| Age group, years | ||||
| <20 | 23·2 (22·6–23·8) | 1 (ref) | 1 (ref) | .. |
| 20–39 | 34·9 (34·6–35·3) | 1·98 (1·90–2·07) | 1·70 (1·63–1·78) | <0·0001 |
| 40–59 | 59·9 (59·6–60·2) | 5·99 (5·76–6·24) | 4·12 (3·95–4·30) | <0·0001 |
| ≥60 | 71·1 (70·8–71·3) | 10·33 (9·92–10·76) | 7·17 (6·86–7·48) | <0·0001 |
| Sex | ||||
| Female | 53·8 (53·6–54·1) | 1 (ref) | 1 (ref) | .. |
| Male | 60·5 (60·3–60·8) | 1·37 (1·35–1·39) | 1·32 (1·30–1·34) | <0·0001 |
| Race | ||||
| White | 68·3 (67·9–68·8) | 1 (ref) | 1 (ref) | .. |
| Mixed | 50·8 (50·1–51·5) | 1·68 (1·63–1·74) | 0·99 (0·96–1·02) | 0·45 |
| Black | 54·5 (54·2–54·7) | 1·26 (1·21–1·32) | 1·00 (0·96–1·05) | 0·87 |
| Indian | 64·1 (63·2–65·0) | 1·69 (1·61–1·77) | 1·17 (1·11–1·23) | <0·0001 |
| Other | 62·1 (58·4–65·8) | 1·32 (1·10–1·58) | 1·14 (0·94–1·39) | 0·19 |
| Comorbid condition | ||||
| No comorbidity | 50·5 (50·2–50·8) | 1 (ref) | 1 (ref) | .. |
| Comorbid condition | 62·2 (62·0–62·5) | 2·24 (2·19–2·28) | 1·51 (1·48–1·55) | <0·0001 |
| Health sector | ||||
| Private sector | 60·6 (60·3–60·8) | 1 (ref) | 1 (ref) | .. |
| Public sector | 53·3 (53·0–53·5) | 1·14 (0·89–1·47) | 0·80 (0·62–1·02) | 0·076 |
| Province | ||||
| Western Cape | 42·1 (41·7–42·5) | 1 (ref) | 1 (ref) | .. |
| Eastern Cape | 69·1 (68·6–69·7) | 4·01 (2·66–6·03) | 5·40 (3·59–8·14) | <0·0001 |
| Free State | 67·8 (67·1–68·5) | 3·62 (2·22–5·91) | 4·83 (2·97–7·85) | <0·0001 |
| Gauteng | 58·5 (58·2–58·7) | 1·89 (1·28–2·78) | 2·44 (1·66–3·61) | <0·0001 |
| KwaZulu-Natal | 56·4 (56·0–56·8) | 2·61 (1·75–3·88) | 3·36 (2·26–4·99) | <0·0001 |
| Limpopo | 65·6 (64·9–66·4) | 5·54 (3·36–9·14) | 6·96 (4·22–11·48) | <0·0001 |
| Mpumalanga | 66·5 (65·7–67·2) | 6·44 (3·75–11·04) | 8·37 (4·90–14·30) | <0·0001 |
| North West | 52·1 (51·4–52·8) | 2·14 (1·17–3·92) | 2·59 (1·42–4·71) | 0·0018 |
| Northern Cape | 66·5 (65·3–67·7) | 6·35 (3·15–12·77) | 8·00 (4·00–16·01) | <0·0001 |
| Wave period | ||||
| Omicron | 33·6 (33·1–34·0) | 1 (ref) | 1 (ref) | .. |
| Asp614Gly | 52·3 (51·9–52·7) | 2·67 (2·60–2·75) | 2·07 (2·01–2·13) | <0·0001 |
| Beta | 63·4 (63·1–63·7) | 4·61 (4·48–4·73) | 3·59 (3·49–3·70) | <0·0001 |
| Delta | 63·0 (62·8–63·3) | 4·21 (4·10–4·32) | 3·47 (3·38–3·57) | <0·0001 |
Data are % (95% CI) or odds ratio (95% CI). The predominant SARS-CoV-2 variants in each of the four COVID-19 waves in South Africa were, in order: Asp614Gly mutation (June 7 to Aug 22, 2020), beta variant (B.1.351; Nov 15, 2020, to Feb 6, 2021), delta variant (B.1.617.2; May 9 to Sept 18, 2021), and omicron variant (B.1.1.529; Nov 21, 2021, to Jan 22, 2022). Univariate and multivariable analysis implemented on the imputed dataset (n=335 219); we used a random effects multivariate logistic regression model controlling for clustering by facility.
Discussion
A lower proportion of SARS-CoV-2 cases were admitted to hospital during the omicron wave in South Africa, with those admitted having shorter hospital stays and less severe illness, and fewer patients requiring oxygen or intensive care treatment compared with the Asp614Gly, beta, or delta waves. Both disease severity and in-hospital case-fatality ratio were at least two times higher in the three preceding waves than in the omicron wave. The change in disease severity was more marked in adults than in children.
The number of adults aged 20 years or older admitted to hospital with SARS-CoV-2 was substantially lower in the omicron wave than in preceding waves, leading to lower clinical burdens on health-care services. The patients admitted to hospital during the omicron wave placed less demand on oxygen supplies, ventilators, and ICU beds than patients admitted in the preceding waves. Early reports from other countries also suggest reduced severity among hospital admissions in the omicron wave.15, 16
The admission rate was higher in the largely unvaccinated age group of individuals younger than 20 years, especially in children younger than 5 years, in the omicron wave than in the first three waves. However, the children younger than 5 years admitted to hospital had less severe illness in the omicron wave than in the first three waves. Early reports from the UK also indicate an increased admission rate but decreased severity among children in the omicron wave.17 Possible reasons for the higher admission rate in children could be that higher transmissibility led to more infections in children, more incidental infection among children admitted to hospital for other reasons, or their lower rates of previous infection8 and vaccination.6 It is also possible that, among children, omicron might result in more symptomatic upper respiratory tract disease requiring hospital admission.
The lower admission rates and less severe infections in patients admitted to hospital during the omicron wave are most likely due to a combination of a less virulent variant and immunity from vaccination and previous infections, especially for the many vaccinated individuals who had a previous infection and thus have so-called hybrid immunity.18 Tissue-based studies showed that the omicron variant infects the cells of the bronchus more efficiently, but infects alveolar cells of the lungs less efficiently than the delta variant.19, 20 The lower virulence of omicron has also been shown in animal models, with mice developing less severe disease with omicron than with other variants.21, 22, 23 The lower virulence of omicron, which at least partly accounts for the reductions in the proportion of severe infections observed in the omicron waves in several countries, could be contributing to its higher infection rates because many individuals who are infectious remain clinically well and mobile, thereby continuing to spread the virus within their communities. The higher efficiency of upper airway infection with omicron might lead to children becoming symptomatic more often due to their smaller airways becoming more readily congested.
Reinfections with omicron in individuals who have had a previous infection are high.24 Although a previous infection might not prevent a symptomatic breakthrough infection, it might generate T-cell responses that provide protection from severe disease,25, 26 thereby contributing, at least partly, to the observed high infection rate but lower severity with omicron. South Africa had a particularly severe wave of delta variant infections, leading to a large increase in seroprevalence after the delta-driven third wave. If a previous infection with the delta variant specifically provides some T-cell immunity that protects against severe disease from omicron infection, this might be a contributor to the less severe infections observed in the omicron-driven fourth wave.
Although SARS-CoV-2 vaccine effectiveness in preventing symptomatic infection has been affected by virus variants,27 vaccines remain effective in reducing the risk of severe disease,28 including against omicron.29 Because vaccination coverage was higher before the omicron wave in individuals older than 60 years (58%), it might have made an important contribution to the lower severity of omicron infections, especially in that age group. However, vaccination cannot fully account for the markedly lower numbers of severe infection in individuals aged 20–39 years during the omicron wave, as fewer than a quarter of this age group was vaccinated at the time. Additionally, since vaccinations started only in mid-2021 in South Africa, a substantial number of vaccinated individuals have hybrid immunity, which retains higher omicron neutralisation than vaccination alone.30
One of the limitations of this study is that clinical outcomes were not known for 11% of patients in the omicron wave because it ended at the time of analysis and some patients were still in hospital. As clinical outcomes have varied little over the course of the omicron wave, we do not anticipate that these results will change substantially when the outstanding clinical outcomes are added. Additionally, testing strategies for determining cases have changed over time, although most testing during the waves has focused on testing individuals with COVID-19 symptoms and those with exposure to SARS-CoV-2. Testing rates across all age groups were lower in the first wave than in subsequent ones, but they have remained constant from the second to the fourth waves. Although the criteria for hospital admission with COVID-19 might have changed over time, the changes have been minimal over the past 6 months when both delta and omicron waves occurred.
Additionally, this study has some data limitations. First, disease severity relies on clinical parameters such as oxygen and ventilation treatment and not laboratory parameters, although oxygen is usually initiated on the basis of an objectively measured oxygen saturation level. Second, the incompleteness of reporting in DATCOV and missing values in some patient data might have caused us to underestimate severity, but the completeness of reporting is unlikely to have changed substantially over the four waves. Furthermore, the surveillance system does not collect data on all comorbidities, neurological conditions, and liver disease, and data on obesity are incomplete. Third, although the dataset did not have individual-level data on infecting lineage for cases included in this analysis, each of the four waves included in this study had a predominant variant that allowed for wave period to be used as a proxy for dominant variant. During the fourth wave, genomic sequencing, as well as S-gene target failure, showed that over 95% of circulating viruses were omicron variant. Fourth, the surveillance system has incomplete data on reason for hospital admission and, among the 40% of patients for whom data were available, 30% were admitted to hospital with an incidental SARS-CoV-2-positive test. This is unlikely to be different across waves, as testing and admission criteria were similar. Finally, DATCOV contains incomplete data on previous SARS-CoV-2 infections and vaccination status, which limits exploration at individual patient level of their potential roles in the lower disease severity observed. Infection and reinfection are substantially underascertained due to the high proportion of asymptomatic infections and challenges in testing, especially in the large number of young people in South Africa. Data on COVID-19 hospital admissions are collected at the health service level by clinicians and nurses and contain limited information on self-reported vaccination status; vaccination data are collected in a different system and linkage of the two data systems is still underway. This limitation has highlighted the need for the creators of the different surveillance datasets to ensure compatibility and potential for integration.
The trend of increasing cases and admissions across South Africa's first three waves shifted in the omicron fourth wave. The omicron wave was characterised by a higher and quicker peak but fewer patients admitted to hospital, less clinically severe illness, and a lower case-fatality ratio. Omicron marked a change in the SARS-CoV-2 epidemic curve, clinical profile, and deaths in South Africa. Early reports from several other countries also indicate less severe disease with omicron, despite the differences in population structure, comorbidity prevalence, prevalence of previous infections, and vaccination coverage. Since each of the five variants of concern have evolved independently of each other, it remains speculative in the absence of data as to whether the next variant will follow the trend of greater severity seen progressively with the first three waves or follow the low severity observed with omicron. Data from a well developed surveillance system for variant identification and hospital admissions are essential as part of pandemic preparedness to rapidly investigate the impact of new SARS-CoV-2 variants and viruses causing future pandemics.
Data sharing
The dataset analysed for the manuscript is available upon reasonable request. The data dictionary is available at request to the corresponding author.
Declaration of interests
CC reports grants from Sanofi Pasteur, the US Centers for Disease Control and Prevention (CDC), PATH, South African Medical Research Council (SAMRC), the Bill & Melinda Gates Foundation, and the Wellcome Trust, outside the submitted work. MJG reports grants from SAMRC and the Bill & Melinda Gates Foundation, outside the submitted work. AvG reports grants from CDC (Atlanta), African Society for Laboratory Medicine–Africa CDC (from the Bill & Melinda Gates Foundation), SAMRC, AFRO, the Fleming Fund, and the Wellcome Trust; and other support from WHO, during the conduct of the study. NW reports grants from the Bill & Melinda Gates Foundation and Sanofi, outside the submitted work. All other authors declare no competing interests.
Acknowledgments
Acknowledgments
DATCOV, as a national surveillance system, is funded by the National Institute for Communicable Diseases (NICD) and the South African National Government. No additional funding was obtained towards the completion of this analysis and the development of this manuscript. We acknowledge the NICD team responsible for reporting test, case, and hospitalisation data. We thank the National Department of Health for implementation support and access to vaccination rates (in particular Tania Van der Merwe), the NICD for support and oversight, and the Network for Genomics Surveillance in South Africa for sequence frequencies. Our gratitude to the laboratories, clinicians, and data teams in all public and private sector hospitals throughout the country reporting cases and hospitalisation data, who are acknowledged and listed as the DATCOV author group.
Contributors
WJ, SSAK, and CM contributed to literature search. WJ, LB, CC, LO, and CM contributed to study design and refining methods of analysis. CM, WJ, SSAK, and RW contributed to data analysis and creation of tables and figures. WJ, SSAK, CC, and CM contributed to data interpretation and initial draft. WJ and SSAK drafted the initial manuscript and all other co-authors contributed scientific inputs equally towards the interpretation of the findings and the final draft of the manuscript. WJ, CM, RW, and LO verified the underlying data. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
References
- 1.Abdool Karim SS, Abdool Karim Q. Omicron SARS-CoV-2 variant: a new chapter in the COVID-19 pandemic. Lancet. 2021;398:2126–2128. doi: 10.1016/S0140-6736(21)02758-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Viana R, Moyo S, Amoako DG, et al. Rapid epidemic expansion of the SARS-CoV-2 omicron variant in southern Africa. Nature. 2022;603:679–686. doi: 10.1038/s41586-022-04411-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Network for Genomics Surveillance in South Africa SARS-CoV-2 genomic surveillance update. https://www.nicd.ac.za/wp-content/uploads/2022/01/Update-of-SA-sequencing-data-from-GISAID-14-Jan-2022_dash_v2-Read-Only.pdf
- 4.Scott L, Hsiao N, Moyo S, et al. Track omicron's spread with molecular data. Science. 2021;374:1454–1455. doi: 10.1126/science.abn4543. [DOI] [PubMed] [Google Scholar]
- 5.Wolter N, Jassat W, Walaza S, et al. Early assessment of the clinical severity of the SARS-CoV-2 omicron variant in South Africa: a data linkage study. Lancet. 2022;399:437–446. doi: 10.1016/S0140-6736(22)00017-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Department of Health Latest vaccine statistics. https://sacoronavirus.co.za/latest-vaccine-statistics/
- 7.South African National Blood Service Updated estimates of the prevalence of SARS-CoV-2 antibodies among blood donors in South Africa. 2021. https://sanbs.org.za/wp-content/uploads/2016/09/updated-estimates-of-the-prevalence-of-sars-cov-2-antibodies-among-blood-donors-in-south-africa.pdf
- 8.Madhi SA, Kwatra G, Myers JE, et al. Population immunity and COVID-19 severity with omicron variant in South Africa. N Engl J Med. 2022 doi: 10.1056/NEJMoa2119658. published online Feb 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.South Africa Department of Health COVID-19 South African online portal. https://sacoronavirus.co.za/
- 10.Jassat W, Cohen C, Kufa T, et al. National Institute for Communicable Diseases; Johannesburg: 2020. DATCOV: a sentinel surveillance programme for hospitalised individuals with COVID-19 in South Africa, 2020. [Google Scholar]
- 11.Statistics South Africa Mid-year population estimates, 2020. Statistical release PO302. 2021. http://www.statssa.gov.za/publications/P0302/P03022020.pdf
- 12.WHO . World Health Organization; Geneva: 2021. Living guidance for clinical management of COVID-19, 23 November 2021. [Google Scholar]
- 13.National Institute for Communicable Diseases Proposed definition of COVID-19 wave in South Africa. 2021. https://www.nicd.ac.za/wp-content/uploads/2021/11/Proposed-definition-of-COVID-19-wave-in-South-Africa.pdf
- 14.Jassat W, Mudara C, Ozougwu L, et al. Difference in mortality among individuals admitted to hospital with COVID-19 during the first and second waves in South Africa: a cohort study. Lancet Glob Health. 2021;9:e1216–e1225. doi: 10.1016/S2214-109X(21)00289-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nyberg T, Ferguson NM, Nash SG, et al. Comparative analysis of the risks of hospitalisation and death associated with SARS-CoV-2 omicron (B.1.1.529) and delta (B.1.617.2) variants in England. SSRN. 2022 doi: 10.2139/ssrn.4025932. published online Feb 4. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bager P, Wohlfahrt J, Bhatt S, et al. Reduced risk of hospitalisation associated with infection with SARS-CoV-2 omicron relative to delta: a Danish cohort study. SSRN. 2022 doi: 10.2139/ssrn.4008930. published online Jan 14. [DOI] [Google Scholar]
- 17.Public Health England SARS-CoV-2 variants of concern and variants under investigation in England. Technical briefing 34. 2022. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1046853/technical-briefing-34-14-january-2022.pdf
- 18.Dan JM, Mateus J, Kato Y, et al. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science. 2021;371 doi: 10.1126/science.abf4063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hui KPY, Ho JCW, Cheung MC, et al. SARS-CoV-2 omicron variant replication in human bronchus and lung ex vivo. Nature. 2022;603:715–720. doi: 10.1038/s41586-022-04479-6. [DOI] [PubMed] [Google Scholar]
- 20.Meng B, Abdullahi A, Ferreira I, et al. Altered TMPRSS2 usage by SARS-CoV-2 omicron impacts infectivity and fusogenicity. Nature. 2022;603:706–714. doi: 10.1038/s41586-022-04474-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bentley EG, Kirby A, Sharma P, et al. SARS-CoV-2 omicron-B.1.1.529 variant leads to less severe disease than Pango B and delta variants strains in a mouse model of severe COVID-19. bioRxiv. 2021 doi: 10.1101/2021.12.26.474085. published online Dec 30. (preprint). [DOI] [Google Scholar]
- 22.Halfmann PJ, Iida S, Iwatsuki-Horimoto K, et al. SARS-CoV-2 omicron virus causes attenuated disease in mice and hamsters. Nature. 2022;603:687–692. doi: 10.1038/s41586-022-04441-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ryan KA, Watson RJ, Bewley KR, et al. Convalescence from prototype SARS-CoV-2 protects Syrian hamsters from disease caused by the omicron variant. bioRxiv. 2021 doi: 10.1101/2021.12.24.474081. published online Dec 26. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pulliam JRC, van Schalkwyk C, Govender N, et al. Increased risk of SARS-CoV-2 reinfection associated with emergence of the omicron variant in South Africa. medRxiv. 2022 doi: 10.1101/2021.11.11.21266068. published online March 6. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Le Bert N, Tan AT, Kunasegaran K, et al. SARS-CoV-2-specific T cell immunity in cases of COVID-19 and SARS, and uninfected controls. Nature. 2020;584:457–462. doi: 10.1038/s41586-020-2550-z. [DOI] [PubMed] [Google Scholar]
- 26.Abu-Raddad LJ, Chemaitelly H, Bertollini R. Severity of SARS-CoV-2 reinfections as compared with primary infections. N Engl J Med. 2021;385:2487–2489. doi: 10.1056/NEJMc2108120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abdool Karim SS, de Oliveira T. New SARS-CoV-2 variants—clinical, public health, and vaccine implications. N Engl J Med. 2021;384:1866–1868. doi: 10.1056/NEJMc2100362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rosenberg ES, Dorabawila V, Easton D, et al. COVID-19 vaccine effectiveness in New York State. N Engl J Med. 2022;386:116–127. doi: 10.1056/NEJMoa2116063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Collie S, Champion J, Moultrie H, Bekker LG, Gray G. Effectiveness of BNT162b2 vaccine against omicron variant in South Africa. N Engl J Med. 2022;386:494–496. doi: 10.1056/NEJMc2119270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cele S, Jackson L, Khoury DS, et al. Omicron extensively but incompletely escapes Pfizer BNT162b2 neutralization. Nature. 2022;602:654–656. doi: 10.1038/s41586-021-04387-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset analysed for the manuscript is available upon reasonable request. The data dictionary is available at request to the corresponding author.