Abstract
Severe acute respiratory syndrome coronavirus (SARS-CoV) is a recently identified human coronavirus. The extremely high homology of the viral genomic sequences between the viruses isolated from human (huSARS-CoV) and those of palm civet origin (pcSARS-CoV) suggested possible palm civet-to-human transmission. Genetic analysis revealed that the spike (S) protein of pcSARS-CoV and huSARS-CoV was subjected to the strongest positive selection pressure during transmission, and there were six amino acid residues within the receptor-binding domain of the S protein being potentially important for SARS progression and tropism. Using the single-round infection assay, we found that a two-amino acid substitution (N479K/T487S) of a huSARS-CoV for those of pcSARS-CoV almost abolished its infection of human cells expressing the SARS-CoV receptor ACE2 but no effect upon the infection of mouse ACE2 cells. Although single substitution of these two residues had no effects on the infectivity of huSARS-CoV, these recombinant S proteins bound to human ACE2 with different levels of reduced affinity, and the two-amino acid-substituted S protein showed extremely low affinity. On the contrary, substitution of these two amino acid residues of pcSARS-CoV for those of huSRAS-CoV made pcSARS-CoV capable of infecting human ACE2-expressing cells. These results suggest that amino acid residues at position 479 and 487 of the S protein are important determinants for SARS-CoV tropism and animal-to-human transmission.
A novel coronavirus was identified as the etiological agent of human severe acute respiratory syndrome (SARS)1 and thus designated SARS coronavirus (SARS-CoV) (1, 2, 3, 4). The nucleotide sequence of human SARS-CoV (huSARS-CoV) differs in a great deal from all other known coronaviruses, and it is unlikely that huSARS-CoV is derived from these known coronaviruses (5, 6). An animal SARS-CoV was later isolated from Himalayan palm civets (Paguma larvata) and a raccoon dog (Nyctereutes procyonoides) at a live animal market of Shenzhen, Guangdong Province, China, and found to share the nucleotide sequence with the human SARS-CoV by 99.8% (7). Subsequent molecular epidemiological analysis indicates that SARS-CoV from palm civet (pcSARS-CoV) and huSARS-CoV are derived from a common ancestor (7, 8, 9). Single nucleotide variation(s) in the spike (S) protein, especially mutations that cause radical amino acid residue changes, have been found to be critical for disease progression (8, 9). This may reflect how the virus acquired the human cell tropism and its subsequent adaptation to human host (10).
One of the major differences between SARS-CoV and other previously defined coronavirus groups is reflected by the fact that its S protein is not capable of utilizing any previously identified coronavirus receptors for the viral entry process (11, 12, 13, 14, 15, 16, 17, 18). Recently, it has been demonstrated that the SARS-CoV S protein binds to the human angiotensin-converting enzyme 2 (ACE2) and then initiates the membrane fusion (16, 17). The S protein can be divided into two structurally distinct domains S1 and S2, and these two domains are responsible for receptor binding and membrane fusion, respectively (17, 19, 20). An 193-amino acid fragment, corresponding to amino acid residues 318–510 of the S1 domain has been shown to bind to the human ACE2 and efficiently block the S protein-mediated infection (17, 20, 21, 22), which may be due to the steric hindrance to the receptor-binding domain (RBD) of the S protein. Substitution of the acidic amino acid residues for alanine within the RBD has been found to interfere with the interaction of S protein to human ACE2 (20). Phylogenetic and molecular epidemiological studies suggest that the S protein has been under the strongest positive selection during the early phases of animal-to-human or human-to-human transmission (8, 9). These studies have also revealed several nonsynonymous amino acid residue variations within the RBD of the S protein, probably important for the receptor binding (9).
In this study, we examined the effects of 6 nonsynonymous amino acid residue variations upon SARS-CoV infection. We found that amino acid residues at positions 479 and 487 were essential for human ACE2-mediated huSARS-CoV infection. These results suggest that the entry barrier from palm civet to human would be compromised if these two amino acid residues in the pcSARS-CoV S protein are substituted for those of huSARS-CoV, individually or in combination. In addition, these findings mandate the imposition of stricter control of handling palm civets and other animals such as rodents to carefully monitor the evolution of animal SARS-CoV.
MATERIALS AND METHODS
Sequence Collection—The S gene sequences of all SARS-CoV strains, their origins, nomenclatures, GenBank™ accession numbers, and other related information were described elsewhere (9). The following abbreviations were depicted as: PC, palm civet; HP, human patient; 03 and 04, for SARS cases in 2002/2003 and 2003/2004, respectively.
Plasmids—Mutant S genes were generated by site-directed mutagenesis in the context of expression plasmid pTSh (17, 23, 24), which contains the humanized BJ01 S gene using a QuikChange kit (Stratagene). To construct a series of the C-terminal Fc-S (amino acids 14–520) genes, we amplified the coding sequences between the N-terminal 14 and 520 residues of the S protein from the full-length S gene and the corresponding mutant S genes with primers: forward 5′-CGCGGATCCATGGATGCAATGAAGA-3′, reverse for 5′-CCGGAATTCGATCAGGTCGGTGC-3′. Then the PCR products were digested with BamHI and XbaI and ligated to a modified pUR vector, which contains the signal sequence of Tpa and the Fc fragemt of human IgG1. All plasmids were confirmed by sequencing. The mouse ACE2 gene was amplified from a mouse kidney cDNA library using three pairs of overlapping primers: forward-1, 5′-GGATCCACCATGTCCAGCTCCTCCTGGCTCC-3′; reverse-1, 5′-GGGCAGGGAGGCATCCAGTGGGGC-3′; forward-2, 5′-GCCCCACTGGATGCCTCCCTGCCC-3′; reverse-2, 5′-CATCCATATTCCTTGCTCCTACCAC-3′; forward-3, 5′-GTGGTAGGAGCAAGGAATATGGATG-3′; and reverse-3, 5′-CTAAAAGGAAGTCTGAGCATCATCGTCGAC-3′. The genes were then subcloned into the retrovirus vector pBabe-puro (gift from Dr. Littman, New York University).
Cell Lines—HEK-293T cells (ATCC) were used to prepare pseudotyped viruses. HeLa-F5 cells with a long terminal repeat insertion were generated by our laboratory (17) expressed human ACE2 stably. Huh-7 cells were used in virus infection and S protein binding assays. Mouse ACE2 (mACE2) gene was transduced into HeLa or NIH/3T3 cells by retroviral vector pBabe-puro containing mouse ACE2 gene and selected in culture medium containing 5 μg/ml puromycin to establish the mACE2-expressing cell lines. The expression of mACE2 protein was confirmed in these stable cell lines HeLa-mACE2 and 3T3-mACE2. All cells were cultured in Dulbecco's modified Eagle's medium supplemented with 10% fetal bovine serum.
Preparation of HIV-1 Pseudotyped Viruses—HIV-luc/SARS-pseudotyped viruses were generated as described previously (23, 24). Briefly, 10 μg of pNL.4.3.Luc.E–R– (HIV-luc) (25) and 10 μg of S gene or its mutant-expressing plasmids were co-transfected into 2 × 106 293T cells by the standard calcium phosphate precipitation method (26). The medium was replaced 12 h after transfection. The cell culture supernatant was collected 48 h after transfection, and the cell debris was removed by passing through a 0.45-μm filter (Millipore). The supernatant was further purified by ultracentrifugation through a 20% sucrose cushion at 50,000 × g for 90 min and assayed for p24 using a Vironostika HIV-1 Antigen MicroELISA Kit (Biomerieux) (23, 27). The purified viruses were stored and used as HIV-1-pseudotyped virus stocks. 0.5 μg of p24 purified pseudotyped viruses were lysed in PBS buffer containing 1% CHAPSO (Sigma), and lysate was separated on an SDS-10% polyacrylamide gel and transferred to a nitrocellulose membrane (Amersham Pharmacia). After blocking, the nitrocellulose membrane was incubated with the rabbit anti-Spike protein sera diluted 1:200 in PBS-T (24). The alkaline phosphatase-labeled goat anti rabbit immunoglobulin G (IgG) (Santa Cruz Biotechnology, 1:1000 dilution) was used as the secondary antibody in the detection.
Infection Assay with HIV-luc/SARS-pseudotyped Virus—HIV-luc/SARS-pseudotyped viruses equivalent to 1, 5, or 10 ng of HIV-1 p24 were used to infect target cells in a 96-well plates at a density of 8 × 103 cells/well. The medium was replaced 12 h post infection, and the cells were allowed to culture for additional 36 h. The cells were then washed and lysed with 30 μl of cell lysis buffer (Promega). Twenty microliters of lysates were assayed using a Luciferase Assay System (Promega), and the luciferase activity was determined in a Wallac Multilabel 1420 Counter (PerkinElmer Life Sciences).
Expression and Purification of Fc-S-(14–520) Fusion Protein—Plasmids expressing wild-type S protein and its mutants of BJ01 as fusion proteins with the C terminus of the human Fc fragment were transfected into 293T cells by the standard calcium phosphate precipitation method. The cell culture supernatant was collected 48 h post transfection, and the soluble Fc-S fusion proteins were purified with protein A-Sepharose beads (Invitrogen). The purity of the proteins were determined to be higher than 95% by SDS-PAGE followed by Coomassie Blue staining and further confirmed by Western blot using an anti-humanFc-alkaline phosphatase antibody (Sigma).
Binding Assay and Flow Cytometry—HeLa-F5 cells were harvested and resuspended in PBS containing 2 nm to 1 μm soluble wild-type S protein and its mutant proteins. The mixtures were allowed to incubate at 4 °C for 1 h and then washed with PBS. Cells were recovered by a brief centrifugation and resuspended in 100 μl of PBS containing 10 μg/ml an fluorescein isothiocyanate-conjugated anti-human IgG-Fc antibody (Sigma), incubated at 4 °C for 1 h, and washed twice with PBS. The binding of the S proteins to the cells were determined by a FACScan flow cytometer (MoFlo cytometer DAKO Cytomation, Denmark).
Real-time PCR—The PRIMEREXPRESS software (version 2.0, Applied Biosystems) was used to design real-time RT-PCR primers with a Tm value of between 59 and 60 °C and an amplification product of 101 bp. For standardization of the amount of mRNA, expression of β-actin in each sample was quantified. All PCR reactions were performed under the following conditions: one cycle at 50 °C for 2 min, one cycle at 95 °C for 10 min, then 45 cycles at 95 °C for 15 s and 60 °C for 1 min. Real-time detection of the emission intensity of SYBR Green was performed with an ABI prism 7000 sequence detector (Perkin-Elmer Applied Biosystems). We used an equivalent amount of cDNA sample, which was derived from 40 ng of total RNA, for each PCR reaction. Quantitative RT-PCR was performed three times, CT values were determined using the AUTOANALYSE features of the Sequence Detection System software. The cDNA of HeLa cells was used as a negative control. The value of the ACE2 expression was divided by that of the β-actin in each sample. The primers were as follows: human ACE2 and mouse ACE2 forward, 5′-TGAAAAAGTGGTGGGAGATGAAG-3′; human ACE2 reverse, 5′-AAACATGGAACAGAGATGCGG-3′; mouse ACE2 reverse, 5′-GAAACATGGAACAGAGATGCAGG-3′; β-actin forward, 5′-GCTCCATCCTGGCCTCG-3′; and β-actin reverse, 5′-CTAGAAGCATTTGCGGTGGAC-3′.
RESULTS
Six Putative Key Amino Acid Residues within the S Protein RBD Were Identified Based on the Correlation between Nonsynonymous Variations and the SARS-CoV Progression and Tropism—We analyzed the phylogenetic relationship between the amino acid sequence variations within the RBD of S protein from 105 SARS-CoV isolates and the epidemiology of these viruses (9). The amino acid sequences of all the huSARS-CoVs of the 2002–2003 pandemic (HP03) were almost identical in the RBD except amino acid residue 344 of several early SARS cases (GZ01/GZ02, ZS-A, ZS-B, and ZS-C) and amino acid residue 353 of some late SARS cases (Singapore isolates). Thus, we used GZ02, BJ01, and TOR2 as the HP03 representatives of the early, middle, and late phases of the 2002/2003 epidemic, respectively (8). We also compared the amino acid sequences of four pcSARS-CoV strains isolated from the Shenzhen market in 2003 (PC03) (7, 8, 9), ten pcSARS-CoV strains from the Guangzhou market in 2004 (PC04) (9), and three huSARS-CoV strains from the 2003–2004 outbreak (HP04) (9) (Fig. 1 ). Notably, there were six nonsynonymous variations located in the RBD region occurring either in pcSARS-CoV or early phase huSARS-CoVs, and they were amino acid residues at position 344, 360, 472, 479, 480, and 487 (Fig. 1). These variations can be categorized into three groups. The first group included those at residues 344, 360 and 487, which were identical in all isolates except HP03 (K344/F360/T487 in HP03 while R344/S360/S487 in others). The second group contained the variations at residues 472 and 480. These variations occurred at different times of virus isolation but not from different hosts, i.e. residues Pro-472 and Gly-480 in HP04 and PC04 and residues Leu-472 and Asp-480 in HP03 and PC03. The third group included residue 479, the one with the greatest diversity represented by lysine, arginine, or asparagine in pcSARS-CoV but only asparagine in huSARS-CoV. The amino acid sequence analyses indicated that PC03, PC04, and HP04 had greater similarity to each other than to the HP03, and that HP04 appeared nearly identical to the PC04. This result is in accordance with a previous report (9). The three-dimensional structure of the S protein has been successfully simulated (Protein Data Bank code 1T7G) (28) and predicted to have these six amino acids exposed at the surface of the S1 domain (9, 28).
Fig. 1.
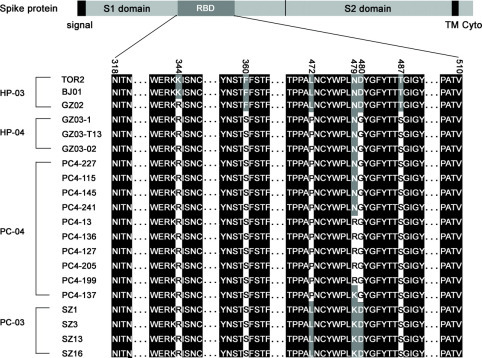
Sequence homology and diversity of the receptor-binding domain (RBD, amino acids 318–510) of the spike gene in palm civet and human SARS-CoV. The sequences of all HP03 are identical in RBD except several earliest cases (GZ01/GZ02, ZS-A, ZS-B, and ZS-C) at position 344 and some late cases (Singapore isolates) at residue 353. Thus, GZ02, BJ01, or TOR2 was used to represent general HP03. In the diagram, PC represents palm civet and HP represents human patient. Both of them were suffixed with “03”or“04” to indicate the time when they were isolated. The positions with variation were indicated at the top (344, 360, 472, 479, 480, and 487).
Combinatorial Substitution of Two Key Residues (N479K/T487S) in the S Protein RBD of huSARS-CoV Greatly Interferes with the Human-ACE2-mediated Pseudotyped Virus Entry—To determine the relationship between the variations of these amino acids and the SARS-CoV infectivity, we substituted each of these six amino acid residues of the huSARS-CoV S protein for those of pcSARS-CoV S protein. HIV-luc and plasmids expressing wild-type S protein (BJ01) or its mutants of huSARS-CoV were co-transfected into 293T cells to prepare HIV-luc/SARS-pseudotyped viruses. The pseudotyped viruses in the supernatant were normalized by the p24 protein, and the viruses equivalent to 10 ng of p24 were used to infect the human ACE2-expressing cells: HeLa-F5 (17, 23, 24, 29, 30). To ensure that these substitutions did not alter the subcellular localization of the S protein, we determined the cell surface expression of S proteins using the convalescent SARS patients' serum followed by the FACS analysis. The results showed that these substitutions did not affect the expression of S proteins (data not shown). We then performed the single-round infection assay using the pseudotyped viruses. The results showed that none of the single substitutions had any effects on huSARS-CoV infection of HeLa-F5 cells expressing the human ACE2 (Fig. 2A).
Fig. 2.
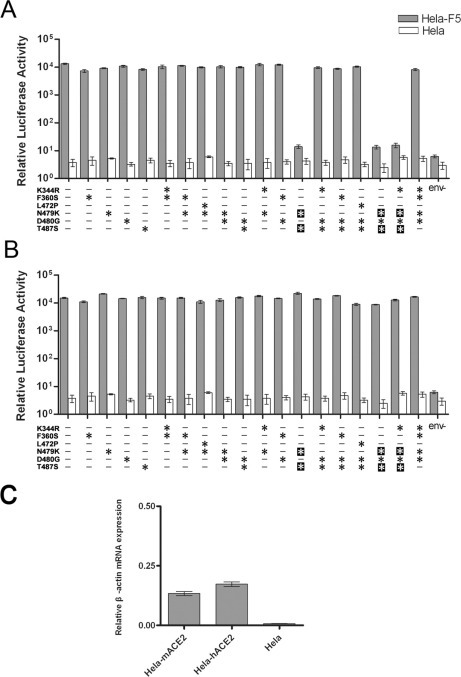
The infectivity of pseudotyped viruses bearing a panel of huSARS-CoV S proteins with individual or combinatorial substitution of K344R, F360S, N479K, D480G, and T487S. These mutated S genes were constructed based on the S gene of BJ01 isolate. The substituted positions are marked with asterisks. All pseudotyped virus' stocks were normalized by HIV core antigen p24, and 10 ng/well was used for infection assay. Luciferase activity was determined 48 h after infection, and they were displayed as means ± S.D. of four parallel wells. Three independent experiments were done to confirm the results. A, the infectivity of various pseudotyped viruses to HeLa-F5 cells and HeLa cells. Pseudotyped virus bearing BJ01 S protein was used as positive control (first column). env-, pseudotyped virus without envelope protein. B, the infectivity of these pseudotyped viruses to HeLa-mACE2 cells and HeLa cells. C, relative human and mouse ACE2 mRNA expression examined using quantitative RT-PCR. The amount of mRNA expression of human ACE2 or mouse ACE2 was divided by that of β-actin in each sample to normalize the value. Quantitative RT-PCR was performed three times. The cDNA of HeLa cells was used as a negative control.
We then made a number of two-amino acid residue substitutions and multiple amino acid residue substitutions of huSARS-CoV S protein for those of pcSARS-CoV S protein and determined their effects on huSARS-CoV infection. The results showed that all except the two-amino acid substitution at positions 479 and 487 (N479K/T487S) had no significant effect on huSARS-CoV infection, whereas N479K/T487S substitution almost completely inhibited the viral infection (Fig. 2A). Similar results were obtained when only 1 or 5 ng of p24 equivalent viruses were used in the infection, suggesting that the inhibition by the N479K/T487S substitution was not caused by the possible overdose of viruses. No pseudotyped virus bearing S protein variant showed infectivity to HeLa cells. The mouse ACE2 protein has been shown to mediate the SARS-CoV entry (22). Thus, we cloned the mouse ACE2 gene and stably expressed it in HeLa cells (HeLa-mACE2) as a target cell control. As expected, the results showed that none of the single or double amino acid substitutions had any effects on huSARS-CoV infection of these mouse cells (Fig. 2B). The different effects of the N479K/T487S double substitution on huSARS-CoV infection of HeLa-F5 and HeLa-mACE2 cells was not due to different levels of ACE2 expression between these two types of cells, because the real-time RT-PCR results showed that the ACE2 expression was comparable in these cells (Fig. 2C).
The Greatly Reduced Infectivity Mediated with the N479K/T487S-substituted huSARS-CoV S Protein Is Correlated with Its Decreased Binding Affinity to the Human ACE2—To determine whether the inhibitory effects of the N479K/T487S double substitution on huSARS-CoV infection studied by the single-round infection assay (17, 23, 24, 29) resulted from the inability of the N479K/T487S S protein to bind to human ACE2, we expressed five soluble fragments containing either the single or the double substitutions of the huSARS-CoV S protein, i.e. SN479K, ST487S, and SN479K/T487S. We also expressed the wild-type SBJ01 and another single substitution SF360S as controls. We fused these proteins with the human Fc fragment to facilitate protein purification. These proteins were expressed at an expected molecular mass of 97 kDa and a comparable level in mammalian cells, as assessed by SDS-PAGE and Western blot using an anti-human-Fc-alkaline phosphatase antibody (Fig. 3A ). To compare the binding ability of these S proteins to human ACE2, HeLa-F5 cells were incubated with these proteins, and the binding affinity was analyzed through FACS. The binding affinity of S protein at 100 nm was SBJ01 ≈ SF360S > ST487S > SN479K >> SN479K/T487S (Fig. 3B). The binding kinetics of the corresponding S proteins was established with a series of S protein concentrations ranging from 2 nm to 1 μm (Fig. 3C), and the relative affinity appeared similarly to the results above (Fig. 3B). The binding kinetics of SF360S was nearly identical to that of SBJ01. ST487S had a significantly lower affinity than SBJ01 in the low concentration range but appeared to be almost similar to the level of SBJ01 at a high S protein concentration (0.5 μm). The affinity of SN479K remained much lower than that of ST487S at all concentrations tested and had no detectable binding when the S protein concentration was below 60 nm.SN479K/T487S showed undetectable binding ability even when the S protein concentration reached 1 μm.
Fig. 3.
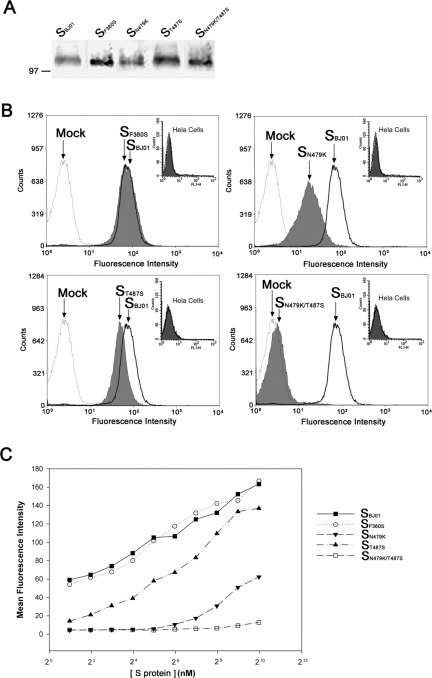
The binding affinity of selected mutants of huSARS-CoV S proteins to human ACE2.A, Western blotting analysis of mutated S fragments (13–510) fused with human Fc. Proteins were submitted to run 10% SDS-PAGE and blotted with anti-human-Fc-alkaline phosphatase antibody. B, FACS analysis of S fragments binding to HeLa-F5 cells and HeLa cells (top right corner). Cells were incubated with 100 nm S fragments, and the binding affinity of S proteins was detected through FACS analysis using fluorescein isothiocyanate-conjugated anti-human IgG-Fc antibody (solid line, BJ01; gray, mutated S fragments; and dotted line, mock). C, binding affinity curves of various S fragments. The mean fluorescence intensity in the y-axis was determined by a series of FACS analyses in which HeLa F5 cells were incubated with serially diluted S fragments (▪, SBJ01; ○, SF360S; ▾, SN479K; ▴, ST487S; and □, SN479K/T487S) from 1 μm to 2 nm.
Substitution of Amino Acid Residues Lys-479 and Ser-487 in the Typical pcSARS-CoV S Protein RBD to Asn-479 and Thr-487, Individually or in Combination, Enhanced the Human-ACE2-mediated Pseudotyped Virus Entry—To further determine the roles of these two amino acid substitution at positions 479 and 487 in SARS-CoV infection and transmission, we substituted these two amino acids of SZ3 S protein for those of huSARS-CoV S protein and determined their effects on infection to human ACE2-expressing cells. Two single individual amino acid substitutions were included. SZ3 and BJ01 S proteins were used as controls. Similarly, we performed the single-round infection in HeLa-F5 cells with these S protein-pseudotyped viruses and S protein incorporation in the virions were determined (Fig. 4A). The infection results showed that, compared with the wild-type SZ3, the two single amino acid substitutions and the double amino acid substitution greatly increased pcSARS-CoV infection, although less efficiently than the case mediated by the BJ01 S protein (Fig. 4B).
Fig. 4.
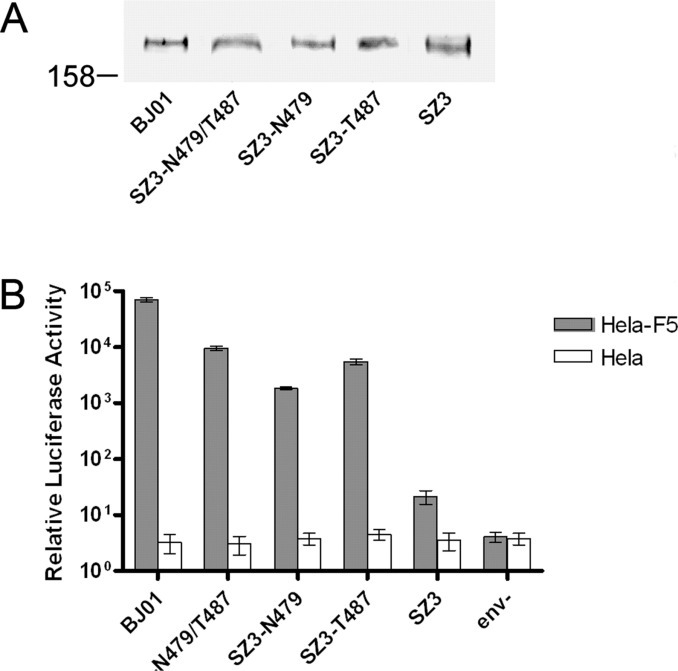
The infectivity of pseudotyped viruses bearing SZ3 S proteins and its variants.A, Western blotting analysis of S protein incorporated in pseudotyped virus. S protein variants associated with HIV particles were detected by Western blotting using rabbit anti-Spike protein serum. B, the infectivity of various pseudotyped viruses to HeLa-F5 cells and HeLa cells. All pseudotyped virus stocks were normalized by HIV core antigen p24, and 10 ng/well was used for the infection assay. Luciferase activity was determined 48 h after infection, and they were displayed as means ± S.D. of four parallel wells. Three independent experiments were done to confirm the results. Pseudotyped virus bearing BJ01 S protein was used as positive control (first column).
DISCUSSION
Two years after the emergence of SARS, the origin of SARS-CoV is still a research conundrum. Although molecular epidemiological and phylogenetic studies indicated that SARS-CoV is a virus of animal origin and SARS is a zoonotic disease (7, 8, 9), the mechanism by which the SARS-CoV evolved in its hosts, animal and human, as well as transmitted from animal (e.g. palm civet) to human, is still unknown.
It is clear that the S gene experienced the strongest positive selection among all genes of SARS-CoV to adapt to its hosts, and the majority of the nonsynonymous variations in the S gene are located within the S1 domain (9). Of these variations, this study indicated that 6 residues in the ACE2 RBD are particularly interesting due to the possibility of being responsible for the entry barrier between pcSARS-CoV and huSARS-CoV. The biological implication of these variations is the significant difference in antibody neutralization of various kinds of pseudotyped lentiviruses expressing S proteins of different hosts, or different epidemic phases (31). These observations have logically led to the hypothesis that the mutations in the RBD are essential for the zoonotic tropism.
In this study, the effects of the RBD variations on SARS-CoV infectivity in human cells were investigated employing the HIV/SARS-pseudotyped viruses (17, 23, 24, 29). The N479K/T487S double substitutions dramatically reduced the infectivity of pseudotyped virus to only 0.1% of BJ01, whereas any single substitutions or double substitutions with or of the other 4 residues had no obvious effects (Fig. 2). These results inferred that any variation in one of the two substitutions is essential for receptor binding and viral entry into the human ACE2-expressing cells. This loss-of-function observation was substantiated with a gain-of-function experiment by substituting amino acid residues Lys-479 and Ser-487 in the typical pcSARS-CoV S protein RBD to Asn-479 and Thr-487, individually or in combination. The results showed that, compared with the wild-type SZ3, both the two single amino acid substitutions and the double amino acid substitution greatly enhanced the human ACE2-mediated pseudotyped virus entry of the pcSARS-CoV infection, although less efficiently than the case mediated by the BJ01 S protein (Fig. 4B). Thus we clearly demonstrated that a typical pcSARS-CoV (SZ3) S protein with limited variations of critical amino acid residues (K479N and/or S487T) in the RBD acquired the ability to utilizing human ACE2 as a receptor with high efficiency.
We also demonstrated that these double substitutions interfered with the interaction between S protein and human ACE2, because the huSARS-CoV SN479K/T487S protein displayed no detectable binding affinity to human ACE2 at the concentration up to 1 μm. Although the individual single mutations of these two residues had no significant decrease in the viral entry, their binding affinity toward ACE2 was significantly reduced (Fig. 3C). Particularly, the SN479K protein demonstrated extremely low binding affinity, whereas the ST487S protein still had moderate binding capability, although significantly lower than that of SBJ01. The phenotypic discrepancies between the entry of pseudotyped virus and the S protein-ACE2 binding affinity may be due to the difference in the sensitivities of the tests on one hand and the distinction in intrinsic mechanisms of the two processes on the other hand. For the latter, the binding of the virions to the susceptible cells is multivalent, and the entry of the pseudotyped virus is a complex stepwise process, whereas the monomeric or oligomeric soluble S protein is likely to bind to the human ACE2 with lower affinity. Similar phenomena were observed in herpes simplex 1 virus (32).
It is particularly interesting to consider these biochemical data with the molecular epidemiological data known so far (7, 8, 9). The SK497/S487 protein naturally exists in all isolates of PC03 and one isolate of PC04. Although most isolates of PC04 had the SR479/S487 protein, they should have similar phenotypes like other viruses from palm civets that carry the SK479/S487 protein, due to the similar biochemical properties of the two basic amino acids, Lys and Arg. Considering that these double amino acid-substituted viruses had extremely low viral entry ability and receptor binding affinity specifically toward ACE2-expressing human cells, it is not surprising that workers who handled or had close contact with PC03 showed no SARS-like syndrome, although they may have positive antiserum against SARS-CoV (7). These results strongly suggest that the coexistence of Lys/Arg-479 and Ser-487 functions as the entry barrier for animal-to-human transmission of the SARS-CoV.
The maintenance of this entry barrier requires the conservation of both Lys-479 and Ser-487. Proved by our results, once one substitution at positions 479 or 487 occurred in animal SARS-CoV, the virus could greatly increase its affinity toward the human receptor ACE2 and even cross the species barrier to cause animal-to-human transmission. All the viral isolates of HP04 had a genome very close to that of PC04; in particular, they all had the SN479/S487 protein as did the four PC04 isolates (9).
Unlike Asn-479, Thr-487 did not exist in any other natural SARS-CoV isolates except HP03. In fact, all the virus isolates of HP03, from the earliest strains that have been detected so far, had the same SN479/T487 protein. Because of the high human ACE2 binding affinity of the SBJ01 protein and all HP03 isolates exclusively containing the Thr-487 residue, we propose that the S487T amino acid switch may reflect the virus adaptation to human host and that the presence of the SN479/T487 protein is essential for causing the pandemic, i.e. the successful transition from animal-to-human transmission to human-to-human transmission.
Our data support the claim that it is not difficult to overcome the entry barrier between animal and human and that palm civet may serve as a favorable incubator. Proper identification of the 479 and 487 critical residues are not only significant in biochemical studies of ligand-receptor binding but are also important for monitoring public health. The existence of SN479/S487 in both HP04 and PC04 reveals a dangerous signal. It manifests that some isolates in palm civet have already evolved to acquire the ability to cross the entry barrier between palm civets and humans. Consistent with this, it is significant to emphasize that the inhibition of the pseudotyped virus infection caused by the N479K/T487S double substitution of huSARS-CoV S protein was human-specific, because the decrease of infectivity could be observed only in human ACE2-expressing cells and not in cells expressing mouse ACE2 (Fig. 2). Although one early study has showed that the mouse ACE2 is a relative poor receptor (7), our data showed that the high level and sustained expression of mouse ACE2 was capable of supporting SARS-CoV-pseudotyped virus entry. These results are in accordance with the finding from the animal model study that mouse can be efficiently infected by huSARS-CoV (33). We believe that the potential intermediate host position of rodents for SARS-CoV should be carefully studied as a reasonable extrapolation of these experimental findings.
Acknowledgments
We thank Tung-Tian Sun, Hui Zhang, and Johnny He for critical reading of the manuscript. We also acknowledge Yiming Shao, Lin Yuan, Jindong Zhao, Weixing Zhao, Liying Du, and Xiaolei Yin for their great help in pseudotyped virus p24 quantification, real-time PCR, and flow cytometry analyses. We also acknowledge that a similar article has been published (34) during our revision of this report.
Footnotes
The abbreviations used are: SARS, severe acute respiratory syndrome; SARS-CoV SARS coronavirus; pcSARS-CoV, SARS-CoV-like virus from palm civet; huSARS-CoV, human SARS-CoV; S protein, spike protein; ACE2, angiotensin-converting enzyme 2; RBD, receptor-binding domain; HP03, isolates from human patients of the 2002/2003 epidemic; HP04, isolates from human patients of the 2003/2004 outbreak; PC03, isolates from palm civets of Shenzhen market in 2003; PC04, isolates from palm civets of Guangzhou market in 2004. FACS, fluorescence-activated cell sorting; HIV-1, human immunodeficiency virus, type 1; PBS, phosphate-buffered saline; CHAPSO, 3-[(3-cholamidopropyl)dimethylammonio]-2-hydroxy-1-propanesulfonic acid; RT, reverse transcription.
References
- 1.Ksiazek T.G., Erdman D., Goldsmith C.S., Zaki S.R., Peret T., Emery S., Tong S., Urbani C., Comer J.A., Lim W., Rollin P.E., Dowell S.F., Ling A.E., Humphrey C.D., Shieh W.J., Guarner J., Paddock C.D., Rota P., Fields B., DeRisi J., Yang J.Y., Cox N., Hughes J.M., LeDuc J.W., Bellini W.J., Anderson L.J. N. Engl. J. Med. 2003;348:1953–1966. doi: 10.1056/NEJMoa030781. [DOI] [PubMed] [Google Scholar]
- 2.Drosten C., Gunther S., Preiser W., van der W.S., Brodt H.R., Becker S., Rabenau H., Panning M., Kolesnikova L., Fouchier R.A., Berger A., Burguiere A.M., Cinatl J., Eickmann M., Escriou N., Grywna K., Kramme S., Manuguerra J.C., Muller S., Rickerts V., Sturmer M., Vieth S., Klenk H.D., Osterhaus A.D., Schmitz H., Doerr H.W. N. Engl. J. Med. 2003;348:1967–1976. doi: 10.1056/NEJMoa030747. [DOI] [PubMed] [Google Scholar]
- 3.Fouchier R.A., Kuiken T., Schutten M., van Amerongen G., van Doornum G.J., van den Hoogen B.G., Peiris M., Lim W., Stohr K., Osterhaus A.D. Nature. 2003;423:240. doi: 10.1038/423240a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peiris J.S., Lai S.T., Poon L.L., Guan Y., Yam L.Y., Lim W., Nicholls J., Yee W.K., Yan W.W., Cheung M.T., Cheng V.C., Chan K.H., Tsang D.N., Yung R.W., Ng T.K., Yuen K.Y. Lancet. 2003;361:1319–1325. doi: 10.1016/S0140-6736(03)13077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rota P.A., Oberste M.S., Monroe S.S., Nix W.A., Campagnoli R., Icenogle J.P., Penaranda S., Bankamp B., Maher K., Chen M.H., Tong S., Tamin A., Lowe L., Frace M., DeRisi J.L., Chen Q., Wang D., Erdman D.D., Peret T.C., Burns C., Ksiazek T.G., Rollin P.E., Sanchez A., Liffick S., Holloway B., Limor J., McCaustland K., Olsen-Rasmussen M., Fouchier R., Gunther S., Osterhaus A.D., Drosten C., Pallansch M.A., Anderson L.J., Bellini W.J. Science. 2003;300:1394–1399. doi: 10.1126/science.1085952. [DOI] [PubMed] [Google Scholar]
- 6.Marra M.A., Jones S.J., Astell C.R., Holt R.A., Brooks-Wilson A., Butterfield Y.S., Khattra J., Asano J.K., Barber S.A., Chan S.Y., Cloutier A., Coughlin S.M., Freeman D., Girn N., Griffith O.L., Leach S.R., Mayo M., McDonald H., Montgomery S.B., Pandoh P.K., Petrescu A.S., Robertson A.G., Schein J.E., Siddiqui A., Smailus D.E., Stott J.M., Yang G.S., Plummer F., Andonov A., Artsob H., Bastien N., Bernard K., Booth T.F., Bowness D., Czub M., Drebot M., Fernando L., Flick R., Garbutt M., Gray M., Grolla A., Jones S., Feldmann H., Meyers A., Kabani A., Li Y., Normand S., Stroher U., Tipples G.A., Tyler S., Vogrig R., Ward D., Watson B., Brunham R.C., Krajden M., Petric M., Skowronski D.M., Upton C., Roper R.L. Science. 2003;300:1399–1404. doi: 10.1126/science.1085953. [DOI] [PubMed] [Google Scholar]
- 7.Guan Y., Zheng B.J., He Y.Q., Liu X.L., Zhuang Z.X., Cheung C.L., Luo S.W., Li P.H., Zhang L.J., Guan Y.J., Butt K.M., Wong K.L., Chan K.W., Lim W., Shortridge K.F., Yuen K.Y., Peiris J.S., Poon L.L. Science. 2003;302:276–278. doi: 10.1126/science.1087139. [DOI] [PubMed] [Google Scholar]
- 8.Chinese SARS Molecular Epidemiology Consortium Science. 2004;303:1666–1669. doi: 10.1126/science.1092002. [DOI] [PubMed] [Google Scholar]
- 9.Song H.D., Tu C.C., Zhang G.W., Wang S.Y., Zheng K., Lei L.C., Chen Q.X., Gao Y.W., Zhou H.Q., Xiang H., Zheng H.J., Chern S.W., Cheng F., Pan C.M., Xuan H., Chen S.J., Luo H.M., Zhou D.H., Liu Y.F., He J.F., Qin P.Z., Li L.H., Ren Y.Q., Liang W.J., Yu Y.D., Anderson L., Wang M., Xu R.H., Wu X.W., Zheng H.Y., Chen J.D., Liang G., Gao Y., Liao M., Fang L., Jiang L.Y., Li H., Chen F., Di B., He L.J., Lin J.Y., Tong S., Kong X., Du L., Hao P., Tang H., Bernini A., Yu X.J., Spiga O., Guo Z.M., Pan H.Y., He W.Z., Manuguerra J.C., Fontanet A., Danchin A., Niccolai N., Li Y.X., Wu C.I., Zhao G.P. Proc. Natl. Acad. Sci. U. S. A. 2005;102:2430–2435. doi: 10.1073/pnas.0409608102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schickli J.H., Thackray L.B., Sawicki S.G., Holmes K.V. J. Virol. 2004;78:9073–9083. doi: 10.1128/JVI.78.17.9073-9083.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Delmas B., Gelfi J., L'Haridon R., Vogel L.K., Sjostrom H., Noren O., Laude H. Nature. 1992;357:417–420. doi: 10.1038/357417a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yeager C.L., Ashmun R.A., Williams R.K., Cardellichio C.B., Shapiro L.H., Look A.T., Holmes K.V. Nature. 1992;357:420–422. doi: 10.1038/357420a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dveksler G.S., Dieffenbach C.W., Cardellichio C.B., McCuaig K., Pensiero M.N., Jiang G.S., Beauchemin N., Holmes K.V. J. Virol. 1993;67:1–8. doi: 10.1128/jvi.67.1.1-8.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holmes K.V., Dveksler G., Gagneten S., Yeager C., Lin S.H., Beauchemin N., Look A.T., Ashmun R., Dieffenbach C. Adv. Exp. Med. Biol. 1993;342:261–266. doi: 10.1007/978-1-4615-2996-5_40. [DOI] [PubMed] [Google Scholar]
- 15.Tresnan D.B., Holmes K.V. Adv. Exp. Med. Biol. 1998;440:69–75. doi: 10.1007/978-1-4615-5331-1_9. [DOI] [PubMed] [Google Scholar]
- 16.Li W., Moore M.J., Vasilieva N., Sui J., Wong S.K., Berne M.A., Somasundaran M., Sullivan J.L., Luzuriaga K., Greenough T.C., Choe H., Farzan M. Nature. 2003;426:450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang P., Chen J., Zheng A., Nie Y., Shi X., Wang W., Wang G., Luo M., Liu H., Tan L., Song X., Wang Z., Yin X., Qu X., Wang X., Qing T., Ding M., Deng H. Biochem. Biophys. Res. Commun. 2004;315:439–444. doi: 10.1016/j.bbrc.2004.01.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jeffers S.A., Tusell S.M., Gillim-Ross L., Hemmila E.M., Achenbach J.E., Babcock G.J., Thomas W.D., Jr., Thackray L.B., Young M.D., Mason R.J., Ambrosino D.M., Wentworth D.E., Demartini J.C., Holmes K.V. Proc. Natl. Acad. Sci. U. S. A. 2004;101:15748–15753. doi: 10.1073/pnas.0403812101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bosch B.J., van der Z.R., de Haan C.A., Rottier P.J. J. Virol. 2003;77:8801–8811. doi: 10.1128/JVI.77.16.8801-8811.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xiao X., Chakraborti S., Dimitrov A.S., Gramatikoff K., Dimitrov D.S. Biochem. Biophys. Res. Commun. 2003;312:1159–1164. doi: 10.1016/j.bbrc.2003.11.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Babcock G.J., Esshaki D.J., Thomas W.D., Jr., Ambrosino D.M. J. Virol. 2004;78:4552–4560. doi: 10.1128/JVI.78.9.4552-4560.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong S.K., Li W., Moore M.J., Choe H., Farzan M. J. Biol. Chem. 2004;279:3197–3201. doi: 10.1074/jbc.C300520200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nie Y., Wang P., Shi X., Wang G., Chen J., Zheng A., Wang W., Wang Z., Qu X., Luo M., Tan L., Song X., Yin X., Chen J., Ding M., Deng H. Biochem. Biophys. Res. Commun. 2004;321:994–1000. doi: 10.1016/j.bbrc.2004.07.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang H., Wang G., Li J., Nie Y., Shi X., Lian G., Wang W., Yin X., Zhao Y., Qu X., Ding M., Deng H. J. Virol. 2004;78:6938–6945. doi: 10.1128/JVI.78.13.6938-6945.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Connor R.I., Chen B.K., Choe S., Landau N.R. Virology. 1995;206:935–944. doi: 10.1006/viro.1995.1016. [DOI] [PubMed] [Google Scholar]
- 26.Jordan M., Schallhorn A., Wurm F.M. Nucleic Acids Res. 1996;24:596–601. doi: 10.1093/nar/24.4.596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang Z., Nie Y., Wang P., Ding M., Deng H. Virology. 2004;330:332–341. doi: 10.1016/j.virol.2004.09.023. [DOI] [PubMed] [Google Scholar]
- 28.Bernini A., Spiga O., Ciutti A., Chiellini S., Bracci L., Yan X., Zheng B., Huang J., He M.L., Song H.D., Hao P., Zhao G., Niccolai N. Biochem. Biophys. Res. Commun. 2004;325:1210–1214. doi: 10.1016/j.bbrc.2004.10.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nie Y., Wang G., Shi X., Zhang H., Qiu Y., He Z., Wang W., Lian G., Yin X., Du L., Ren L., Wang J., He X., Li T., Deng H., Ding M. J. Infect. Dis. 2004;190:1119–1126. doi: 10.1086/423286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li W., Greenough T.C., Moore M.J., Vasilieva N., Somasundaran M., Sullivan J.L., Farzan M., Choe H. J. Virol. 2004;78:11429–11433. doi: 10.1128/JVI.78.20.11429-11433.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang Z.Y., Werner H.C., Kong W.P., Leung K., Traggiai E., Lanzavecchia A., Nabel G.J. Proc. Natl. Acad. Sci. U. S. A. 2005;102:797–801. doi: 10.1073/pnas.0409065102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dubin G., Basu S., Mallory D.L., Basu M., Tal-Singer R., Friedman H.M. J. Virol. 1994;68:2478–2485. doi: 10.1128/jvi.68.4.2478-2485.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Subbarao K., McAuliffe J., Vogel L., Fahle G., Fischer S., Tatti K., Packard M., Shieh W.J., Zaki S., Murphy B. J. Virol. 2004;78:3572–3577. doi: 10.1128/JVI.78.7.3572-3577.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li W., Zhang C., Sui J., Kuhn J.H., Moore M.J., Luo S., Wong S.K., Huang I.C., Xu K., Vasilieva N., Murakami A., He Y., Marasco W.A., Guan Y., Choe H., Farzan M. EMBO J. 2005;24:1634–1643. doi: 10.1038/sj.emboj.7600640. [DOI] [PMC free article] [PubMed] [Google Scholar]


