Abstract
Acute respiratory distress syndrome (ARDS) is an acute respiratory illness characterised by bilateral chest radiographical opacities with severe hypoxaemia due to non-cardiogenic pulmonary oedema. The COVID-19 pandemic has caused an increase in ARDS and highlighted challenges associated with this syndrome, including its unacceptably high mortality and the lack of effective pharmacotherapy. In this Seminar, we summarise current knowledge regarding ARDS epidemiology and risk factors, differential diagnosis, and evidence-based clinical management of both mechanical ventilation and supportive care, and discuss areas of controversy and ongoing research. Although the Seminar focuses on ARDS due to any cause, we also consider commonalities and distinctions of COVID-19-associated ARDS compared with ARDS from other causes.
Introduction
Acute respiratory distress syndrome (ARDS) is the acute onset of hypoxaemia and bilateral pulmonary oedema due to excessive alveolocapillary permeability. Although ARDS has a codified clinical definition, known as the Berlin definition (panel 1 ) with stages that estimate mortality risk,1 there is no single test to identify or exclude the diagnosis. The heterogeneity of ARDS, evident in its causes, manifestations, and response to therapy,2, 3 challenges clinicians and scientists to provide impeccable supportive care and discover new therapies. This Seminar summarises current knowledge regarding ARDS epidemiology and risk factors, differential diagnosis, and clinical management, and highlights controversial topics and ongoing research. This Seminar also includes a section on the COVID-19 pandemic and ARDS.
Panel 1. The Berlin definition of ARDS and observed mortality1.
-
•
Acute onset (within 7 days of new or worsening respiratory symptoms)
-
•
Bilateral radiographical opacities that are not fully explained by effusion, atelectasis, or masses
-
•
Arterial hypoxaemia defined by thresholds:
-
•
Identified risk factor for ARDS (if no clear risk factor, exclude heart failure as a cause)
-
•
Not exclusively due to cardiac causes
ARDS=acute respiratory distress syndrome. CPAP=continuous positive pressure ventilation. FiO2=fraction of inspired oxygen. PaO2=partial pressure of oxygen. PEEP=positive end-expiratory pressure.
Epidemiology and outcomes
ARDS is more common than initially believed. In 2016, a study of patients in 459 intensive care units (ICUs) from 50 countries reported that 10% of ICU patients and 23% of mechanically ventilated patients fulfilled criteria for ARDS.4 Although the survey was done during the winter viral season and included ARDS that resolved rapidly,5 the hospital mortality of 35–45% closely resembled that described by the large datasets used to validate the Berlin definition.1, 4 Even patients whose ARDS resolved rapidly had a mortality rate of 31%.6 Given that many patients with diffuse lung injury supported with high-flow nasal cannula (HFNC) do not meet the ARDS Berlin definition, which requires positive pressure ventilation,1 the incidence of ARDS is probably even higher. The COVID-19 pandemic has highlighted this limitation, as many patients are treated without mechanical ventilation.7, 8 Men might be slightly more likely to develop ARDS, although outcome is largely similar between sexes.9 Women—and patients of shorter stature—are less likely to receive lung protective ventilator tidal volumes.10 For patients with severe persistent ARDS, women had higher mortality than men.11 Black patients might have a reduced risk of developing ARDS,9 and Black and Hispanic patients with ARDS had a higher mortality in at least one study, which seemed to be mediated by increased severity of illness.12 Tobacco use, alcohol use, hypoalbuminaemia, chemotherapy within the previous 6 months, and ambient air pollutant exposure4, 13, 14, 15, 16 can increase ARDS risk, whereas, in some studies, patients with diabetes were less likely to develop ARDS.17, 18
Mortality for ARDS remains sobering; observational studies consistently report greater than 30% hospital mortality,4 with one large trial of moderate to severe ARDS reporting 43% in-hospital mortality at 90 days.19 The proportion of ARDS mortality that is attributable to the syndrome itself (as opposed to risk factors and comorbidities) has been challenging to determine, but was estimated for sepsis-associated ARDS at 27–37%.20 The cause of death is more commonly sepsis and multiple organ failure than respiratory failure.21 Although most ARDS survivors recover normal or near-normal pulmonary function, many remain burdened by functional limitations related to muscle weakness, deconditioning, or psychological sequelae of severe illness.22, 23 Cognitive impairment is also distressingly common, affecting almost half of survivors at 2 years.24, 25
Causes and risk factors
Since its initial description,26 ARDS has been recognised as a clinical condition that develops in the setting of various causes or risk factors (panel 2 ). The most common risk factors are pneumonia and non-pulmonary sepsis, followed by aspiration of gastric contents.4, 27 Trauma and blood product transfusion are less common ARDS risk factors in the modern era as ventilator, fluid, and transfusion management has evolved,4, 28 whereas new causes such as e-cigarette or vaping product use-associated lung injury (EVALI) have emerged.29, 30 Bacterial and viral pneumonias frequently cause ARDS, with sporadic spikes in global ARDS incidence due to pandemic influenza31 and emerging viruses including SARS-CoV-232, 33 and the coronaviruses responsible for SARS34 and MERS.35, 36 Identification of a specific cause for ARDS remains a crucial therapeutic goal to improve outcomes associated with ARDS.37 Although genetic susceptibility to ARDS is suggested by the variability with which clinical risk factors predict ARDS development and by the replicated association of numerous genetic variants with ARDS risk,38, 39 the attributable risk of any singular genetic polymorphism to ARDS risk or outcome seems small.
Panel 2. Classic precipitants of ARDS.
Common precipitants
-
•
Pneumonia (bacterial and viral are the most common, whereas fungal, mycobacterial, and parasitic pneumonia are less common)
-
•
Non-pulmonary sepsis
-
•
Aspiration of gastric contents
-
•
Non-cardiogenic shock
-
•
Pancreatitis
-
•
Severe trauma or high-risk surgery (eg, esophagectomy)
-
•
Drug overdose
-
•
Ischaemia-reperfusion injury
Less common precipitants
-
•
Smoke inhalation
-
•
Drowning
-
•
Vape or e-cigarette use
-
•
Multiple transfusion of blood products
Diagnoses not typically classified as ARDS
-
•
Vasculitis
-
•
Diffuse alveolar haemorrhage
-
•
Drug-induced pneumonitis
-
•
Organising pneumonia
-
•
Hypersensitivity pneumonitis
-
•
Acute eosinophilic pneumonia
-
•
Acute exacerbation of interstitial lung disease
-
•
Acute chest syndrome (ie, sickle cell disease)
-
•
Alveolar proteinosis
-
•
Malignancy
ARDS=acute respiratory distress syndrome.
Diagnostic considerations
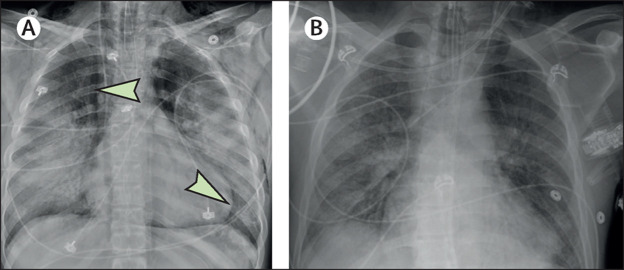
No single diagnostic test confirms or refutes a diagnosis of ARDS. Furthermore, it must be emphasised that ARDS is a syndrome rather than a specific pathologic entity and is currently identified by purely clinical criteria. As elaborated by the Berlin definition,1 ARDS diagnosis requires that new or worsening respiratory distress and bilateral chest radiographical abnormalities be present for 7 days or fewer, that heart failure cannot fully explain the hypoxaemia and radiographical infiltrates, and that the impaired oxygenation be clinically significant. By comparison with previous definitions,40 the Berlin definition provided more specific guidance on chest radiograph patterns consistent with ARDS—bilateral opacities consistent with pulmonary oedema (figure 1 ) that can be patchy or asymmetric1—and those that are inconsistent with ARDS, including isolated pleural effusions, atelectasis, or tumours.1
Figure 1.
Chest radiographs
(A) Vaping-associated lung injury with pneumomediastinum (arrows). (B) SARS-CoV-2 infection.
Imaging
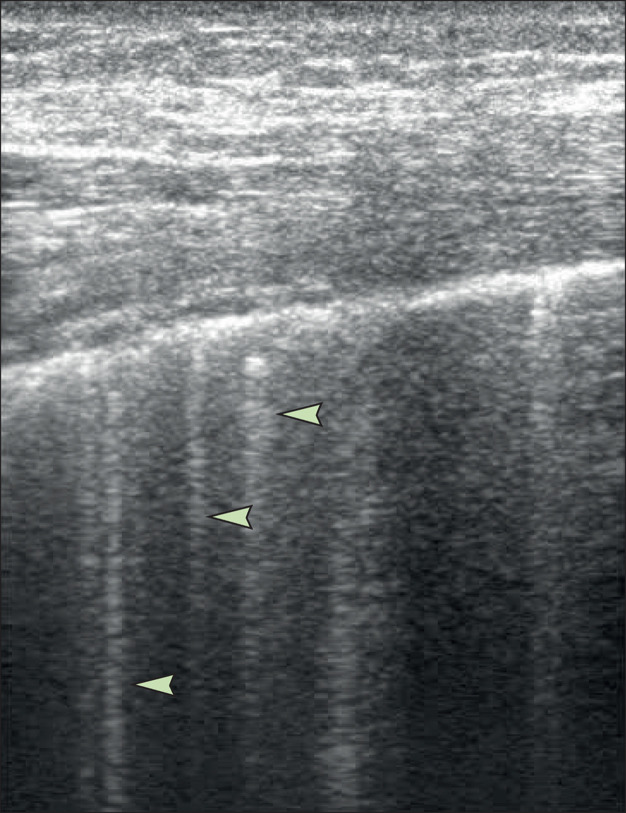
CT can fulfil the radiographical ARDS criterion, replacing or adding to chest radiograph,1 and can quantify lung oedema and potential recruitability of lung parenchyma.41 Chest CT can identify abnormalities that mimic ARDS on a radiograph, including pleural effusions, severe obesity with atelectasis, or nodules and masses, and can suggest interstitial lung disease.42, 43 CT can be challenging to obtain for severely hypoxaemic patients and those receiving high dose vasoactive medications, continuous renal replacement therapy, or other ICU interventions. CT exposes patients to ionising radiation, which restricts its repeatability, and is expensive. Lung ultrasonography can identify alveolar flooding using bilateral B line patterns, defined as three or more discrete vertical lines arising from the pleura in an intercostal space, representing hyperechoic reverberation artifacts44 (figure 2 ). Ultrasonography is portable, inexpensive, free from radiation, can be repeated as needed, and monitors lung recruitment45 and resolution of alveolar processes. Lung ultrasound has been proposed as an alternative to chest radiography for resource-limited settings in the Kigali modification to the Berlin definition of ARDS.46 However, sonographic B lines from hydrostatic pulmonary oedema are indistinguishable from those in ARDS. Combining cardiac and lung ultrasonography can suggest a cardiogenic process,47 although heart failure and ARDS can coexist.48 Ultrasound visualises primarily subpleural lung zones and can yield poor-quality images in the presence of extensive overlying soft tissue (as seen with obesity) or subcutaneous oedema.
Figure 2.
Lung ultrasound image showing B lines
B lines (arrows) are the vertical lines in the lower half of the image. Diffuse B lines (≥3 per region in multiple fields) are consistent with pulmonary oedema or acute respiratory distress syndrome.
Determining the inciting cause
Although some ARDS precipitants can be self-limited and others do not have specific treatment, prompt recognition, and treatment of reversible insults such as infection, hypersensitivity, or autoinflammation is essential. Clinical history provides crucial information about the duration of symptoms, an infectious prodrome or travel history, exposures, behaviours, or localising symptoms that might guide imaging or serological testing. Understanding the patient's comorbidities is essential to consider risks for infectious and sterile (eg, blunt trauma, pancreatitis, postoperative) processes.
The initial diagnostic approach for a patient with suspected ARDS focuses upon determining whether the patient has pneumonia or another infection because pneumonia and sepsis are the most common underlying diagnoses. Blood cultures should be drawn for all patients without an obvious sterile insult, and consideration should be given to obtaining sputum, tracheal aspirate, or bronchoalveolar lavage samples if safe to do so. The value of bronchoscopy, with sensitivity only 58% in one prospective study,49 is likely to be superior to sputum, especially for fungal causes (eg, Pneumocystis jirovecii), Legionella, or atypical pathogens (eg, Nocardia or Actinomyces bacteria). Bronchoalveolar lavage can also prompt consideration of alternative diagnoses to ARDS (panel 2) using a differential cell count and fluid cytology to identify eosinophilic pneumonia, alveolar proteinosis, or diffuse alveolar haemorrhage, or suggest hypersensitivity pneumonitis.43 In EVALI, bronchoalveolar lavage analysis detected vitamin E acetate in the majority of cases and never among healthy controls, implicating this chemical in the syndrome.50 With the advent of molecular testing, bronchoalveolar lavage or nasopharyngeal swab with PCR can detect numerous viral pathogens, which might prompt pathogen-specific treatment or isolation precautions51, 52 and reduce exposure to potentially unnecessary antibiotics.
Open lung biopsy is not commonly done during ARDS because there are risks and a lack of useful information in most cases.53 Transbronchial biopsy through a flexible bronchoscope is possible but still poses risks of bleeding and pneumothorax, and diagnostic yield might be only 35%.54, 55 Consideration for biopsy increases as physicians question whether the patient has an alternative to ARDS, particularly a disease that might be treatable.55
Underlying biology
Many different mechanisms contribute to the syndrome clinicians recognise as ARDS and, in different individuals, the role played by any one process can vary considerably. Pulmonary oedema occurs when fluid is filtered from the circulation into the lung extravascular spaces faster than it can be removed. In ARDS, pulmonary oedema arises primarily from a defect in alveolocapillary permeability, rather than primarily due to hydrostatic pressure. In this section, we discuss the key principles of ARDS pathogenesis; two detailed reviews56, 57 should be used for greater detail.
Endothelial permeability
Healthy lung vasculature has several safety features to prevent lung flooding across a range of vascular hydrostatic pressures. Fluid filtered from the pulmonary microvasculature into the interstitium is largely reabsorbed into the circulation due to low alveolar epithelial permeability, a protein osmotic gradient between vessel and interstitium, a hydrostatic pressure gradient from peripheral to central vessels, lymphatic flow, and pleural and mediastinal sinks when hydrostatic pressure is excessive.58, 59, 60, 61 However, when the vascular barrier becomes highly permeable to protein and solutes, the protein osmotic gradient is lost and the interstitium is easily flooded.
Healthy pulmonary endothelium largely inhibits inflammation and coagulation, whereas activated endothelium does the opposite.62 Stimuli as varied as hypoxia, cytokines, chemokines, thrombin, primed leukocytes, lipopolysaccharide, and damage-associated molecular patterns (DAMPs) can shift the endothelium towards a dysregulated, leaky state that attracts inflammatory cells.63, 64 Disruption of bonds between adjacent endothelial cells65 and cytoskeletal changes66 cause cells to pull away from one another and allows endothelial gap formation. Apoptosis also contributes to a dysfunctional vascular barrier.67, 68, 69 The activated endothelium recruits activated neutrophils that release their nuclear contents to form, with activated platelets, neutrophil extracellular traps.70 As pulmonary endothelium is disrupted, typically vascular-sequestered coagulation factors interact with tissue factor expressed by alveolar epithelial cells and alveolar macrophages, triggering activation of the extrinsic coagulation cascade.71
Alveolar epithelial injury, permeability, and dysfunction
An intact alveolar epithelium is a robust defence against alveolar flooding; not only is it relatively impermeable, but its active sodium and chloride transport helps drive oedema resolution.64, 72 In ARDS, both epithelial barrier function and fluid clearance are weakened or inactive.73 Epithelial injury can be incited directly by microbial pathogens, acid injury (eg, aspiration of gastric contents), hyperoxia, or mechanical stretch (eg, by the ventilator).74, 75, 76 Some of these insults cause epithelial apoptosis or necrosis, whereas others disrupt intercellular junctions, which increase epithelial permeability.75, 77, 78 Circulating factors (eg, DAMPs or cell-free haemoglobin) and microbial products, toxins, and circulating immune cells and inflammatory mediators can damage the epithelium.56, 57, 79
Dysregulated lung inflammation
Accumulation of white blood cells, particularly neutrophils, in the lung and alveolar space is clinically and pathologically significant in ARDS.26, 80 Neutrophils from people with ARDS are activated and functionally distinct: they have enhanced chemotaxis, enhanced metabolic activity, delayed apoptosis, and a novel transcriptional signature.81, 82, 83 Activated neutrophils and platelets interact in the injured lung to form neutrophil extracellular traps, complexes of filamentous chromatin fibres and neutrophil-derived proteins,70 which could help sequester pathogens but also confer lung injury.84 Alveolar macrophages exert both proinflammatory and anti-inflammatory responses and contribute to epithelial permeability.85, 86 In addition to dysregulated innate immunity, adaptive immunity also seems to play a major role in lung host defence and in the resolution of injury. Regulatory T cells were shown to have a crucial role in lung injury resolution in research done in animals and are detectable in bronchoalveolar fluid from humans with ARDS.87
Mechanical stress
Biomechanical forces also contribute to lung injury and ARDS. Rescue of patients with severe hypoxaemia has always relied upon mechanical ventilation; therefore, the concept that the ventilator could both rescue and harm patients is not new. Recognition that positive-end expiratory pressure (PEEP) could be lifesaving was emphasised in the original description of ARDS by Ashbaugh and colleagues26 in 1967, and subsequent research showed that the combination of large tidal volumes and zero PEEP induced haemorrhagic pulmonary oedema.88, 89, 90 Lung injury due to excessive mechanical strain or stress is sometimes termed ventilator-induced lung injury (VILI), and ventilation strategies that reduce VILI have been a major advancement in the care for patients with ARDS. A clinical trial of a tidal volume and pressure-limited ventilation strategy reduced mortality compared with ventilation with larger tidal volumes and more permissive airway pressures.91 A so-called low-stretch ventilation strategy with specific limits on ventilator set tidal volume and lung end-inspiratory (plateau) pressure was associated with reductions in plasma and bronchoalveolar lavage concentrations of inflammatory markers such as interleukin (IL-)1, IL-6, IL-8, and tumour necrosis factor α.92, 93 Research done in experimental models suggests that lung-derived circulating mediators can amplify lung injury and epithelial permeability, and some have proposed VILI as a mechanism by which lung injury propagates injury in distant organs (eg, the kidney or brain), leading to multiorgan system failure via biotrauma.94, 95 Although debate remains as to how to identify the optimal ventilation strategy for each individual patient, a general practice of avoiding overdistension and minimising cyclic atelectasis by appropriate use of PEEP form our current recommendations.96, 97
Initial management
Standard ventilator management
Mechanical ventilation does not cure ARDS; however, it does allow time for the body to recover from the disease that led to respiratory failure, providing adequate oxygenation and removing carbon dioxide without inducing VILI or other side-effects. In this section, we will discuss the standard approach to mechanical ventilation of ARDS (panel 3 ), and also discuss the associated challenges and controversies.
Panel 3. Key ventilator parameters for acute respiratory distress syndrome ventilation in a volume assist control mode.
Ventilator settings
-
•
Tidal volume: size of a breath (mL) scaled to predicted bodyweight, as normal lung volume is generally determined by height
-
•
Respiratory rate: breaths per minute
-
•
Minute ventilation: total volume of gas breathed in 1 min; tidal volume multiplied by respiratory rate
-
•
PEEP: a ventilator setting to maintain positive pressure in the lungs even when expiration has ended, resulting in an increased mean airway pressure and possibly recruited (ie, more aerated) lung parenchyma, measured in cm H2O
-
•
FiO2: the proportion of oxygen in inspired air (1·0=100% FiO2)
Ventilator measurements
-
•
Airway peak inspiratory pressure: peak pressure generated by delivering a ventilator breath, composed of resistive and elastic elements
-
•
Airway plateau pressure: pressure during an end-inspiratory hold (volume cycled mode) while the patient is passive; patient respiratory effort can cause inaccurate measurements
-
•
Airway driving pressure: difference between plateau pressure and set PEEP
FiO2=fraction of inspired oxygen. PEEP=positive end-expiratory pressure.
Tidal volume and plateau pressure: lung-protective ventilation
The recommended size of the ventilated breath, or tidal volume, has changed as we have learned more about ARDS and shifted from targeting a normal partial pressure of carbon dioxide (PCO2) to controlling lung distension.98, 99 Following the hypothesis that lung rest could be beneficial,100 and that permissive hypercapnia101 could be more appropriate than high-volume, high-pressure ventilation to treat an inflamed lung with its reduced volume of aeration, the value of low-stretch lung ventilation was established in 2000 in the ARMA trial,91 which reported a survival advantage with tidal volumes of 6 cc/kg predicted bodyweight compared with 12 cc/kg predicted bodyweight. This trial also set a plateau pressure limit of 30 cm H2O, with further tidal volume reductions as needed to keep plateau pressure below this goal. This concept is now widely accepted, and a lung-protective strategy targeting a tidal volume of less than 6 ml/kg predicted bodyweight and plateau pressure of less than 30 cm H2O has become standard practice in ARDS management.97, 102
In the original ARMA trial,91 target pH was in the range of 7·30–7·45, with target partial pressure of oxygen (PaO2) of 55–80 mm Hg or oxygen saturation (SpO2) of 88–95%. A randomised controlled trial, published in 2020, compared targeting a conservative oxygenation goal (SpO2 88–92%) to a liberal oxygenation goal (SpO2 ≥96%) in patients with ARDS,103 with the hypothesis suggested by previous studies104 that the conservative goal might prevent hyperoxic lung injury. However, 90-day mortality was higher in the conservative oxygenation group than the liberal oxygen goal group, and the trial was stopped early by the data safety monitoring committee. In the absence of subsequent data, we recommend that SpO2 goals should be 93% or higher.
Positive end-expiratory pressure
PEEP is the pressure that maintains some degree of inflation during the end-expiratory pause. Higher PEEP increases mean airway pressure, which usually improves oxygenation. Maintaining inflation during exhalation also decreases the stress of alveoli collapsing and reinflating during the respiratory cycle, termed atelectrauma.105 The most commonly used method for PEEP selection is to apply an algorithm matching PEEP to the fraction of inspired oxygen (FiO2) that the patient requires.91 This approach was tested in clinical trials by the ARDS network (ARDSNet) in the USA and is relatively simple to apply:91 the higher the fraction of oxygen required, the more PEEP is applied. Three large trials106, 107, 108 tested the hypothesis that a higher PEEP protocol would improve survival compared with the traditional ARDSNet PEEP protocol. For all three trials, no substantial differences in clinical outcomes were observed, suggesting that a high PEEP strategy was not superior for all patients with ARDS. Another trial applying an aggressive high PEEP strategy plus high-pressure recruitment manoeuvres found a statistically significant increase in mortality in the intervention arm; this approach is not recommended.109 Increasing PEEP can decrease venous return and lower preload, decrease left ventricular afterload, and potentially decrease myocardial oxygen demand.110 The effect on pulmonary vascular resistance (PVR) is unpredictable, as vascular compression by higher PEEP might increase PVR, yet PEEP-induced changes in aeration and oxygenation might decrease hypoxic vasoconstriction, lowering PVR. Similarly, the effect of PEEP on cardiac output depends on ventricular function, preload, and afterload.110
Prone position
Starting from the observation that oxygenation improved in patients in the prone position,111 physiological studies identified several mechanisms underlying this improvement, including decreasing the differential distribution of ventilation between ventral and caudal lung regions and shifting the density distribution of oedematous lung.112, 113 A series of randomised trials114, 115, 116 paralleled the evolution of pathophysiological understanding;117 although none of these trials individually showed a survival benefit to prone positioning, post-hoc analysis suggested potential benefit for the most severely hypoxaemic patients when prone position was combined with low stretch ventilation and applied for longer periods (16 h).118 Based on these findings, a prospective study examined prone ventilation for 17 h per day for patients with moderate or severe ARDS and showed a statistically significant survival benefit.119 Prone position should be strongly considered for patients meeting criteria (PaO2/FiO2 ratio persistently <150) and without contraindications. Careful attention must be applied during the proning procedure to avoid disruption of vascular access catheters and endotracheal tubes and, while the patient is proned, to avoid pressure-related complications. During the COVID-19 pandemic, prone positioning has also been used successfully in awake, non-intubated patients with acute hypoxaemic respiratory failure.120, 121
Neuromuscular blockade
When oxygen consumption and associated carbon dioxide production increase, total ventilation must increase to maintain constant arterial PaCO2 and pH. Hence, controlling oxygen consumption might have a possible benefit, especially in the early phase of ARDS.122 Several approaches are possible such as reducing body temperature,123 sedation,124 and neuromuscular blockade.125 Neuromuscular blockade also has the potential benefit of reducing ventilator dyssynchrony, which could lead to inadvertently high tidal volumes and transpulmonary pressures. In 2010, a large randomised study identified an adjusted mortality advantage with neuromuscular blockade (cisatracurium) compared with placebo in patients with moderate or severe ARDS (PaO2/FiO2 ratio <150 mm Hg), all of whom were deeply sedated.126 However, concern about neuromuscular blockade and deep sedation worsening critical illness polyneuromyopathy or longer term functional outcomes led to variable use of cisatracurium.102, 127, 128 A subsequent trial failed to show survival benefits in patients with moderate or severe ARDS who were randomly assigned to receive cisatracurium with deep sedation for 48 h compared with light sedation if tolerated, and goal-oriented sedation if not tolerated.129, 130 The control group showed that some cases of ARDS were difficult to manage even with deep sedation, prompting providers to use neuromuscular blockade in roughly 15% of patients in this group during the first 2 days.129 Importantly, in both of these trials, protocolised duration of neuromuscular blockade was intentionally short (≤48 h), and there was no difference in the incidence of ICU-acquired weakness observed with neuromuscular blockade. Although neuromuscular blockade is thus not mandated for all patients with moderate or severe ARDS, short duration neuromuscular blockade use is safe and could enable improved gas exchange and ventilator synchrony. Our recommendation is to use neuromuscular blockade for patients in whom providers are otherwise unable to reach ventilation synchrony within lung protective targets, for patients with severe hypoxaemia despite deep sedation, and in individualised cases when plateau pressures are high or difficult to accurately measure. Once initiated, we recommend that clinicians consider daily whether neuromuscular blockade remains helpful and consider discontinuation at the earliest opportunity.
Supportive care
Although appropriate ventilator management is of paramount importance in ARDS, adherence to evidence-based supportive care is also crucial. In the setting of increased alveolar-capillary permeability, elevated hydrostatic pressure in the pulmonary vasculature leads to more rapid alveolar flooding than in patients with an intact alveolar-capillary barrier;131 at the same time, adequate tissue perfusion is crucial for patients with multisystem organ failure, which describes many patients with ARDS. Optimal fluid management in patients with ARDS and concomitant vasopressor-dependent shock remains controversial, with ongoing studies (eg, NCT03434028 and NCT04569942) addressing this issue. However, for patients with ARDS who either never or no longer require vasopressors, the Fluid and Catheter Treatment Trial48 (FACTT) showed that a fluid-conservative management strategy increased the number of ventilator-free days as compared with a fluid-liberal strategy, without increasing acute kidney injury or need for dialysis. Although the treatment algorithm used in FACTT was relatively complex, in practice, a strategy of diuresis targeted at a net even to negative daily fluid balance is feasible and likely to recapitulate the benefits of the FACTT protocol.132 No specific caloric goal or supplementation has been proven superior for ARDS in large trials.133, 134 Management of pain, agitation or sedation, and delirium, along with immobility and sleep (PADIS), is important, and sedation practices can strongly affect patient outcomes.128, 135 International critical care guidelines support a goal-directed approach to PADIS that seeks light sedation,136 and daily spontaneous breathing trials to test patients' readiness to liberate from mechanical ventilation.137 For patients with ARDS, spontaneous breathing trials should not begin until patients have reached an appropriately low threshold of support on the ARDSNet ventilator grid, typically with a FiO2 of 0·5 or less and PEEP less than or equal to 8 cm H2O.
Pharmacotherapy
By stark contrast with ventilator and fluid management of ARDS, where clearly beneficial interventions have been identified through rigorous randomised trials, decades of clinical trials of pharmacotherapies for ARDS have failed to identify any consistently effective drugs. Most of the biological pathways thought to be dysregulated in ARDS have been targeted in clinical trials (table 1 ), including inflammation, epithelial injury, endothelial injury, and disordered coagulation, but no drugs targeting these pathways have proven consistently effective.157 In 2020, vitamin D was proposed to have potentially beneficial immunomodulatory effects; however, in a randomised controlled trial of 1360 critically ill patients at high risk for ARDS or death, high dose vitamin D had no benefit on mortality or other outcomes.158 Similarly, a clinical trial published in 2020 randomly allocated 301 patients with moderate to severe ARDS to receive either placebo or intravenous interferon-β-1a, thought to improve pulmonary endothelial barrier function, but found no benefit.144
Table 1.
Selected pharmacotherapies found to be ineffective for ARDS in human clinical trials
| Potential mechanisms | Key studies | Comments | |
|---|---|---|---|
| Activated protein C | Anticoagulant, anti-inflammatory | Liu et al138 | .. |
| Anti-endotoxin antibodies | Bind endotoxin and thereby reduce inflammatory response | Bigatello et al139 | .. |
| Aspirin | Anti-inflammatory via antiplatelet effects | Kor et al140 | Did not reduce ARDS development in patients at high risk |
| β-agonists | Improved alveolar fluid clearance | Matthay et al,141 Gao Smith et al142 | .. |
| Ibuprofen | Anti-inflammatory, via inhibition of cyclooxygenase | Bernard et al143 | Did not reduce ARDS development in sepsis |
| Interferon β-1a | Improve pulmonary endothelial barrier function | Ranieri et al144 | .. |
| Keratinocyte growth factor | Promote epithelial repair | McAuley et al145 | .. |
| Ketoconazole | Anti-inflammatory | The ARDS Network146 | .. |
| Lisofylline | Anti-inflammatory | The ARDS Network147 | .. |
| Neutrophil elastase inhibitor (eg, sivelestat) | Anti-inflammatory | Zeiher et al,148 Iwata et al149 | .. |
| Nitric oxide (inhaled) | Pulmonary vasodilatation, improve V/Q mismatch | Gebistorf et al150 | Improved oxygenation; increased acute kidney injury |
| Omega-3 fatty acids | Anti-inflammatory | Rice et al134 | .. |
| Procysteine and N-acetylcysteine | Reduction in oxidant injury via restoring glutathione | Bernard et al151 | .. |
| Prostaglandin E1 | Pulmonary vasodilatation, improve V/Q mismatch | Fuller et al,152 Vincent et al153 | .. |
| Statins (eg, simvastatin, rosuvastatin) | Anti-inflammatory; endothelial stabilisation | McAuley et al,154 Truwit et al155 | .. |
| Surfactant | Promote epithelial repair, reduce atelectrauma | Spragg et al156 | Effective in neonatal respiratory distress syndrome |
ARDS=acute respiratory distress syndrome. V/Q=ventilation–perfusion.
Despite this discouraging track record, some phase 2 studies have identified potentially promising drugs. The CITRIS-ALI trial159 investigated high dose vitamin C versus placebo in 167 patients with early sepsis and ARDS; although no difference was observed in the primary outcome of modified sequential organ failure assessment score at 96 h, patients treated with vitamin C had a significant reduction in 28-day all-cause mortality, compared with placebo (30% vs 46%, p=0·03). Vitamin C is also being studied in sepsis and might have beneficial effects on systemic inflammation, coagulopathy, alveolar fluid clearance, and formation of neutrophil extracellular traps.160, 161, 162 Other potentially promising drugs in early phase clinical trials for ARDS include allogeneic mesenchymal stromal cells, carbon monoxide, sevoflurane, DNAse, and granulocyte-macrophage colony-stimulating factor.163, 164 The increasing interest in the use of enrichment strategies, either prognostic (enrolling patients at high risk for ARDS-related poor clinical outcomes) or predictive (enrolling patients with a biological phenotype well matched to the drug's mechanism) approaches, might improve the success rate of future studies.165, 166
Rescue therapies
Despite maximal supportive therapy with optimal ventilator and fluid management, some patients with ARDS will continue to worsen, with development of severe and refractory hypoxaemia, hypercapnia or acidosis, elevated plateau pressures, or a combination. In these patients, clinicians can consider so-called rescue therapies—ie, adjunctive therapies for ARDS whose benefits have not been conclusively shown for all patients but could show benefit in individualised circumstances (table 2 ).174 These therapies can include extracorporeal life support, alternative ventilator modalities or settings, or select pharmacotherapies. It is important to emphasise that these therapies should be considered primarily for patients with severe and refractory ARDS and should not be considered for routine management of typical ARDS patients (table 2).
Table 2.
Rescue therapies for ARDS
| Proposed mechanism | Clinical settings for use | Potential risks | Key studies | |
|---|---|---|---|---|
| ECMO | Allow ultraprotective ventilation; rescue oxygenation | Severe and persistent hypoxaemia; severe and persistent acidosis; refractory elevated inspiratory plateau pressure; first 7 days of mechanical ventilation with reversible cause | Bleeding, vascular access complications, thrombocytopenia, stroke; only available at referral centres | Peek et al,167 Combes et al168 |
| Higher PEEP strategies | Recruit collapsed alveolar units, thereby improving compliance and oxygenation | Refractory hypoxaemia | Decreased preload leading to hypotension; barotrauma | Mercat et al,106 Meade et al,107 Brower et al108 |
| Recruitment manoeuvre | Recruit collapsed alveolar units, thereby improving compliance and oxygenation | Refractory hypoxaemia, particularly in patients who seem PEEP responsive | Decreased preload leading to hypotension; barotrauma | Brower et al,108 Cavalcanti et al109 |
| Inhaled pulmonary vasodilators | Improve V/Q matching, reduce pulmonary vascular pressures | Refractory hypoxaemia | Associated with acute kidney injury; development of tachyphylaxis | Gebistorf et al150 |
| Corticosteroids | Decrease inflammation | Refractory hypoxaemia | Immunosuppression, critical illness myopathy or neuropathy; increased duration of viral shedding in influenza or SARS-CoV-1; conflicting data on benefits; late administration associated with harm | Lewis et al,157 Villar et al,169 Steinberg et al,170 Bernard et al171 |
| CRRT | Additional fluid removal and acid clearance; theoretical cytokine clearance | Refractory acidosis in setting of plateau pressure limitation | Risks of vascular access, bleeding | .. |
Several developments in rescue therapies merit additional discussion. Extracorporeal life support (one form of which is extracorporeal membrane oxygenation [ECMO]) uses cardiopulmonary bypass technology to pass the patient's blood through an oxygenator, which increases blood oxygen content without injurious ventilator pressures or volumes. The CESAR trial,167 published in 2009, reported that a higher proportion of patients with severe ARDS were alive and disability-free when randomly allocated to being transferred to centres that provided extracorporeal life support, as compared with staying at the referring hospital. Most but not all transferred patients received extracorporeal life support.167 In 2018, Combes and colleagues168 reported the results of the EOLIA trial, which randomly assigned 249 patients with early and very severe ARDS to immediate venovenous ECMO or continued supportive care; notably, 28% of patients in the control arm crossed over to ECMO because they had refractory hypoxaemia.168 Although patients randomly assigned to ECMO had an 11% absolute risk reduction for 60-day mortality compared with the control group (35% vs 46%, p=0·09), this outcome did not meet the predetermined criteria for statistical significance, and the trial was stopped early because of futility. Importantly, although conclusive benefit was not shown, ECMO appeared to be safe by comparison with conventional treatment, although with higher incidences of thrombocytopenia and bleeding requiring transfusion. The benefit of ECMO could partly be attributed to the reduced plateau pressures required by the ECMO protocol, the resulting lower tidal volumes, or both.168 These data suggest that ECMO should be strongly considered in patients with very severe ARDS who are early in the course of disease (mechanical ventilation ≤7 days) and with potentially reversible respiratory failure. There is substantial global and local variation in decision making about in whom to initiate ECMO, how long to maintain ECMO, and when to withdraw care in patients on ECMO.175, 176 These decisions are highly personalised to local resources, the patient's condition and comorbidities, and patient and surrogate wishes, and a multidisciplinary process for such complex decisions is recommended.176
Corticosteroids have been considered as a potentially effective therapy for ARDS since the syndrome's original description26 in 1967 and have persisted in the discussion of rescue therapies. Despite the intuitive appeal of an anti-inflammatory therapy for ARDS and numerous clinical trials of corticosteroids over the past several decades, results have been conflicting, and the topic remains controversial (figure 3 ). A 2019 Cochrane systematic review on corticosteroids in ARDS concluded, albeit with low-certainty evidence, that corticosteroids might improve the number of ventilator-free days up to day 28 in ARDS; however, the review was unable to draw firm conclusions about mortality or other outcomes.177 Villar and colleagues169 reported results of a randomised (but not placebo-controlled or masked) clinical trial comparing dexamethasone to standard care for patients with moderate to severe ARDS; patients in the dexamethasone group had 4·8 more ventilator-free days compared with untreated patients, and a 15% absolute risk reduction in 60-day mortality (21% vs 36%).169 However, there were several methodological issues with this trial, including lack of complete masking, high use of corticosteroids before enrolment, slow accrual and premature termination, and greater reintubation rate in the dexamethasone group. Importantly, corticosteroids might be harmful in influenza pneumonia, in which steroids have been reported to delay viral clearance, and when administered late in persistent ARDS (>14 days after diagnosis).170, 178, 179 In the 2019 EVALI outbreak, corticosteroids were reported to be beneficial, although the natural history of EVALI remains unclear, and many patients improved in the absence of corticosteroid treatment.180 In patients with acute respiratory failure requiring mechanical ventilation due to SARS-CoV-2 (most of whom presumably had ARDS), the RECOVERY trial181 reported that dexamethasone increased survival. These data emphasise the importance of identifying the specific cause of ARDS, since the underlying cause can dictate treatment response. Further research is needed to identify which patients with ARDS are most likely to benefit from corticosteroids and which patients could be harmed.
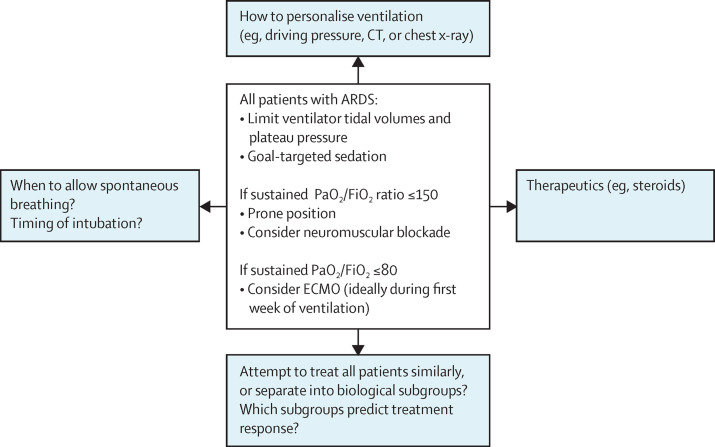
Figure 3.
Areas of consensus and controversy in ARDS management
Central box shows the areas of consensus. Blue boxes show areas of controversy and new directions. ARDS=acute respiratory distress syndrome. ECMO=extracorporeal membrane oxygenation. FiO2=fraction of inspired oxygen. PaO2=partial pressure of oxygen.
Controversies and new research in ARDS
Personalising mechanical ventilation
The best method to select a patient's PEEP remains controversial. Randomised controlled trials to adjust PEEP based on the patient's oxygenation182 or radiographical focality183 have not shown a consistent benefit. One suggestion has been to use driving pressure (ie, plateau pressure minus PEEP) as an alternative target to optimise ventilatory parameters. In re-analysis of multiple randomised trials of ventilator strategies, driving pressure retained the strongest association with mortality compared with either tidal volume or plateau pressure,184 suggesting that driving pressure minimisation might be beneficial. However, although randomised trials have shown benefit to a tidal volume pressure and plateau pressure-limited approach, no such evidence base exists for driving pressure. An approach to maintain a consistent, low driving pressure (12 cm H2O) while doing recruitment manoeuvres and stepwise PEEP de-escalation to select the optimal PEEP resulted in excess mortality compared with traditional PEEP–FiO2 selection.109 Despite a favourable pilot study,185 use of oesophageal manometry to estimate pleural pressure and personalise PEEP to maintain a positive transpulmonary pressure did not reduce mortality or time on the ventilator.186
Spontaneous breathing during ARDS
Another topic of controversy in ARDS is deciding when patients should be permitted to set their own breathing pattern, tidal volumes, and respiratory flows. The putative advantages of spontaneous breathing in ARDS—either through ventilator modes that give the patient control of breath size and frequency or through non-invasive ventilatory support—include potentially improved distribution of ventilation matched to perfusion in dorsal-dependent lung regions,187 reduced need for sedation, avoidance of complications of endotracheal intubation, and prevention of diaphragm atrophy.188 Countering these possible benefits are potential disadvantages including dyspnoea and anxiety, increased oxygen consumption and carbon dioxide generation, ventilator asynchrony, and pendelluft,189 a term describing movement of air from one region of the lung to another, which is not effective gas exchange.189 Furthermore, there is concern that negative intrathoracic pressure generates large swings in transpulmonary pressure, which can incite pulmonary oedema, sometimes termed patient self-inflicted lung injury.188, 190
Non-invasive ventilation191 and HFNC192 have been proposed as alternatives even in well established ARDS. Some studies have reported that patients with ARDS who were unsuccessfully treated with non-invasive ventilation, and subsequently required intubation, had worse outcomes.193, 194 It is possible that some of these patients developed negative transpulmonary pressures during non-invasive ventilation causing patient self-inflicted lung injury. The same reasoning might apply to HFNC.195 However, HFNC reduced mortality when applied early in patients with acute hypoxaemic respiratory failure, many of whom probably had early ARDS.196 No large-scale trial has specifically addressed the optimal timing of intubation in ARDS.
Heterogeneity in ARDS
ARDS is by definition a syndromic diagnosis rather than a distinct pathological entity; therefore, patients with ARDS have great heterogeneity in their clinical, physiological, radiological, and biological phenotypes. Since the earliest consensus definition of ARDS,40 this heterogeneity has been recognised as a potential barrier to effective therapy, but ARDS researchers and clinicians have lacked consensus on the usefulness of and optimal approach to further subdividing the syndrome.40
Clinically apparent subphenotypes of ARDS have been shown to differ physiologically and biologically.197 In theory, extrapulmonary ARDS (eg, non-pulmonary sepsis) should first affect endothelial permeability, leading to prevalent diffuse oedema, whereas pulmonary ARDS should first affect the alveolar epithelium. Experimental data fit this model,198 and patients with direct (ie, pulmonary) lung injury have lower severity of illness, fewer organ failures, more evidence of lung epithelial injury and lower concentrations of plasma biomarkers of endothelial injury, compared with patients with indirect (ie, extrapulmonary) lung injury.199, 200 However, after the first few days of ARDS, and indeed often in clinical practice, it is difficult to differentiate between pulmonary and extrapulmonary ARDS, and evidence that these phenotypes should alter treatment is insufficient.
In another example of clinically apparent heterogeneity, the LIVE trial183 tested the value of personalising therapy according to radiological assessment of diffuse versus focal lung injury as compared with a conventional generalised approach.183 The overall trial showed no difference in outcomes between the personalised and standard care groups; however, when the 20% of patients in the personalised group whose radiological phenotype was misclassified were excluded, the personalised strategy seemed beneficial. These results highlight the potential value, and challenges, of a targeted approach to ARDS trials and management.201
Investigators have applied unsupervised data-driven analytical approaches to ask whether there are unobserved subphenotypes within ARDS. Latent class analysis of clinical and protein biomarker data from five randomised trial cohorts of patients with ARDS identified two distinct and consistent subphenotypes in all five cohorts.2, 202, 203, 204 One subphenotype, representing about 30% of patients with ARDS, has higher plasma concentrations of inflammatory cytokines, lower plasma concentrations of the coagulation factor protein C and bicarbonate, a higher prevalence of shock, and consistently worse clinical outcomes than patients with the subphenotype characterised by lower inflammatory markers.205 In secondary analyses of completed clinical trials, these two subphenotypes seemed to respond differently to PEEP, fluid management strategy, and simvastatin, although prospective confirmation of these findings is needed. Similarly, cluster analysis of plasma protein biomarker data identified two distinct ARDS subphenotypes, termed reactive and uninflamed.206 The reactive subphenotype had worse clinical outcomes and different expression of 29% of genes measured in whole blood using an array-based analysis.207 How ARDS subphenotypes identified with these two different approaches correspond to each other, or to transcriptomic-based subphenotypes of sepsis,208 remains unknown. Prospective validation of subphenotype identification and differential treatment responses will be required before clinical care should be affected.
ARDS due to COVID-19
By May, 2021, there were over 160 million cases of confirmed COVID-19 worldwide, with over 3·3 million reported deaths.209 This global pandemic has increased interest in ARDS due to SARS-CoV-2, as many clinical centres have become overwhelmed with patients with severe ARDS. Early reports highlighted unique features of COVID-19-associated ARDS,210 although subsequent data suggested that it shares many physiological aspects with classic ARDS, including heterogeneity.211 Similarly, early reports suggested a high prevalence of venous thrombosis and coagulopathy in COVID-19-associated ARDS,212 and it will be important to compare these data with other causes of ARDS in which endothelial dysfunction and disordered coagulation are important factors.213
Remdesivir, a novel antiviral therapy that has shown in-vitro efficacy against coronaviruses, can shorten time to clinical improvement for patients hospitalised with severe COVID-19 disease and has received Emergency Use Authorisation by the US Food and Drug Administration for use in this setting; however, data on its efficacy are conflicting and WHO has recommended against its use.52 The RECOVERY trial,181 a large pragmatic randomised open-label study in the UK, reported that dexamethasone 6 mg daily for 10 days was associated with a lower 28-day mortality for hospitalised patients with COVID-19, with the largest effect seen in patients receiving mechanical ventilation.181 Meta-analysis of seven randomised trials testing different steroid regimens that included over 1700 patients detected a summary odds ratio for death of 0·66 (95% CI 0·53–0·82, p<0·001) with similar estimates of effect for dexamethasone or hydrocortisone.214 Hydroxychloroquine is not effective.215 Numerous potential therapies are being urgently explored, including anticoagulation, immune modulatory approaches (eg, IL-6 receptor blockade), repurposed drugs (eg, azithromycin), convalescent plasma, and monoclonal antibodies. Although some of these therapies might ultimately prove beneficial, they all have potential to cause serious adverse events (eg, bleeding complications and immunosuppression). While awaiting more data, a prudent strategy for treatment of patients with COVID-19-associated ARDS is to adhere to the fundamental principles of initial care for ARDS (panel 4 ), including lung-protective ventilation, to treat with dexamethasone and consider remdesivir on the basis of published clinical trials, and to attempt to enrol patients in randomised controlled trials of novel therapies whenever feasible rather than applying untested therapies that could equally harm or benefit patients.
Panel 4. Fundamental elements of initial intensive care unit care for patients with ARDS.
-
•
Lung protective ventilation strategy: goal tidal volume ≤6 mL/kg, plateau pressure ≤30 cm H2O, PEEP relative to FiO2 set according to ARDS Network grids or local practice,91 generally PEEP ≥5 cm H2O
-
•
Assiduous search for and treatment of underlying cause of ARDS
-
•
Sedation and analgesia only as needed to promote comfort, ventilator synchrony
-
•
Fluid conservative strategy including aggressive diuresis if needed to reach net negative fluid status, once shock has resolved (off vasopressors)
-
•
Stress ulcer prophylaxis, deep venous thrombosis prophylaxis with subcutaneous heparin or low-molecular weight heparin, unless otherwise contraindicated
-
•
Daily spontaneous breathing trials to assess for ventilator liberation beginning when the patient can tolerate FiO2 ≤0·5 and PEEP ≤8 cm H2O
-
•
For patients with moderate to severe ARDS (PaO2/FiO2 ratio <150 mm Hg), consider:
-
•Neuromuscular blockade, with goal duration <48 h
-
•Prone positioning for at least 17 h per day
-
•
ARDS=acute respiratory distress syndrome. FiO2=fraction of inspired oxygen. PaO2=partial pressure of oxygen. PEEP=positive end-expiratory pressure.
Conclusions
More than 50 years after its original definition, ARDS remains common and clinical outcomes remain sobering. Nowadays, ARDS is particularly relevant because of the global ARDS pandemic due to SARS-CoV-2 affecting millions worldwide. Substantial progress has been made over the past five decades in understanding the epidemiology and biology of this heterogeneous syndrome, and in developing an evidence-based approach to supportive care, premised on a low tidal volume and plateau pressure-limited ventilation strategy and an assiduous search for and treatment of the underlying cause of ARDS. Key future directions for ARDS include identification of which elements of treatment apply broadly to any patient meeting the syndrome's diagnostic criteria and which elements should be personalised to specific aspects of physiology and biology that could identify a more treatment-responsive subgroup.
Search strategy and selection criteria
We searched PubMed from database inception to Dec 14, 2020, using the search terms "Acute Respiratory Distress Syndrome", "ARDS", "acute lung injury", "positive end expiratory pressure", "COVID-19", "SARS-CoV-2", "prone position", and "neuromuscular blockade". The search was limited to studies of humans. Returned lists of articles were then screened manually by reading abstracts to exclude neonatal lung injury and neonatal respiratory distress syndrome. Comprehensive reviews that have been published within the past 3 years were also read in full, and their reference lists were reviewed. Remaining manuscripts were read in full and their references reviewed when appropriate.
Acknowledgments
Acknowledgments
The authors would like to thank Prof Lorraine Ware (Vanderbilt University School of Medicine, Nashville, TN, USA) for her review of a draft version of this article.
Contributors
All authors contributed equally to the research and writing of this Seminar.
Declaration of interests
NJM reports grants from National Institutes of Health (NIH)–National Heart, Lung, and Blood Institute, and support to do clinical trials from Quantum Leap Healthcare Collaborative and BioMarck, outside the submitted work. CSC reports grants from NIH, during the writing of this Seminar, grants and personal fees from Roche–Genentech and Bayer, personal fees from Quark Pharmaceuticals, Prometic, Gen1e Life Sciences, and Vasomune, and grants from Quantum Leap Healthcare Collaborative, outside the submitted work. LG declares no competing interests.
Footnotes
CPAP delivered by non-invasive or invasive ventilation.
PEEP delivered by invasive mechanical ventilation.
References
- 1.Ranieri VM, Rubenfeld GD, Thompson BT, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307:2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 2.Calfee CS, Delucchi KL, Sinha P, et al. Acute respiratory distress syndrome subphenotypes and differential response to simvastatin: secondary analysis of a randomised controlled trial. Lancet Respir Med. 2018;6:691–698. doi: 10.1016/S2213-2600(18)30177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Calfee CS, Delucchi K, Parsons PE, Thompson BT, Ware LB, Matthay MA. Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials. Lancet Respir Med. 2014;2:611–620. doi: 10.1016/S2213-2600(14)70097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bellani G, Laffey JG, Pham T, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315:788–800. doi: 10.1001/jama.2016.0291. [DOI] [PubMed] [Google Scholar]
- 5.Villar J, Schultz MJ, Kacmarek RM. The LUNG SAFE: a biased presentation of the prevalence of ARDS! Crit Care. 2016;20:108. doi: 10.1186/s13054-016-1273-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Madotto F, Pham T, Bellani G, et al. Resolved versus confirmed ARDS after 24 h: insights from the LUNG SAFE study. Intensive Care Med. 2018;44:564–577. doi: 10.1007/s00134-018-5152-6. [DOI] [PubMed] [Google Scholar]
- 7.Gershengorn HB, Hu Y, Chen J-T, et al. The impact of high-flow nasal cannula use on patient mortality and the availability of mechanical ventilators in COVID-19. Ann Am Thorac Soc. 2020;18:623–631. doi: 10.1513/AnnalsATS.202007-803OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alqahtani JS, Mendes RG, Aldhahir A, et al. Global current practices of ventilatory support management in COVID-19 patients: an international survey. J Multidiscip Healthc. 2020;13:1635–1648. doi: 10.2147/JMDH.S279031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lemos-Filho LB, Mikkelsen ME, Martin GS, et al. Sex, race, and the development of acute lung injury. Chest. 2013;143:901–909. doi: 10.1378/chest.12-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Han S, Martin GS, Maloney JP, et al. Short women with severe sepsis-related acute lung injury receive lung protective ventilation less frequently: an observational cohort study. Crit Care. 2011;15:R262. doi: 10.1186/cc10524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McNicholas BA, Madotto F, Pham T, et al. Demographics, management and outcome of females and males with acute respiratory distress syndrome in the LUNG SAFE prospective cohort study. Eur Respir J. 2019;54 doi: 10.1183/13993003.00609-2019. [DOI] [PubMed] [Google Scholar]
- 12.Erickson SE, Shlipak MG, Martin GS, et al. Racial and ethnic disparities in mortality from acute lung injury. Crit Care Med. 2009;37:1–6. doi: 10.1097/CCM.0b013e31819292ea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trillo-Alvarez C, Cartin-Ceba R, Kor DJ, et al. Acute lung injury prediction score: derivation and validation in a population-based sample. Eur Respir J. 2011;37:604–609. doi: 10.1183/09031936.00036810. [DOI] [PubMed] [Google Scholar]
- 14.Calfee CS, Matthay MA, Kangelaris KN, et al. Cigarette smoke exposure and the acute respiratory distress syndrome. Crit Care Med. 2015;43:1790–1797. doi: 10.1097/CCM.0000000000001089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moss M, Burnham EL. Chronic alcohol abuse, acute respiratory distress syndrome, and multiple organ dysfunction. Crit Care Med. 2003;31(suppl):S207–S212. doi: 10.1097/01.CCM.0000057845.77458.25. [DOI] [PubMed] [Google Scholar]
- 16.Reilly JP, Zhao Z, Shashaty MGS, et al. Low to moderate air pollutant exposure and acute respiratory distress syndrome after severe trauma. Am J Respir Crit Care Med. 2019;199:62–70. doi: 10.1164/rccm.201803-0435OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moss M, Guidot DM, Steinberg KP, et al. Diabetic patients have a decreased incidence of acute respiratory distress syndrome. Crit Care Med. 2000;28:2187–2192. doi: 10.1097/00003246-200007000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Boyle AJ, Madotto F, Laffey JG, et al. Identifying associations between diabetes and acute respiratory distress syndrome in patients with acute hypoxemic respiratory failure: an analysis of the LUNG SAFE database. Crit Care. 2018;22:268. doi: 10.1186/s13054-018-2158-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moss M, Huang DT, Brower RG, et al. Early neuromuscular blockade in the acute respiratory distress syndrome. N Engl J Med. 2019;380:1997–2008. doi: 10.1056/NEJMoa1901686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Auriemma CL, Zhuo H, Delucchi K, et al. Acute respiratory distress syndrome-attributable mortality in critically ill patients with sepsis. Intensive Care Med. 2020;46:1222–1231. doi: 10.1007/s00134-020-06010-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stapleton RD, Wang BM, Hudson LD, Rubenfeld GD, Caldwell ES, Steinberg KP. Causes and timing of death in patients with ARDS. Chest. 2005;128:525–532. doi: 10.1378/chest.128.2.525. [DOI] [PubMed] [Google Scholar]
- 22.Herridge MS, Tansey CM, Matté A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364:1293–1304. doi: 10.1056/NEJMoa1011802. [DOI] [PubMed] [Google Scholar]
- 23.Cheung AM, Tansey CM, Tomlinson G, et al. Two-year outcomes, health care use, and costs of survivors of acute respiratory distress syndrome. Am J Respir Crit Care Med. 2006;174:538–544. doi: 10.1164/rccm.200505-693OC. [DOI] [PubMed] [Google Scholar]
- 24.Mikkelsen ME, Christie JD, Lanken PN, et al. The Adult Respiratory Distress Syndrome Cognitive Outcomes Study: long-term neuropsychological function in survivors of acute lung injury. Am J Respir Crit Care Med. 2012;185:1307–1315. doi: 10.1164/rccm.201111-2025OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hopkins RO, Weaver LK, Collingridge D, Parkinson RB, Chan KJ, Orme JF., Jr Two-year cognitive, emotional, and quality-of-life outcomes in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2005;171:340–347. doi: 10.1164/rccm.200406-763OC. [DOI] [PubMed] [Google Scholar]
- 26.Ashbaugh DG, Bigelow DB, Petty TL, Levine BE. Acute respiratory distress in adults. Lancet. 1967;2:319–323. [Google Scholar]
- 27.Laffey JG, Madotto F, Bellani G, et al. Geo-economic variations in epidemiology, patterns of care, and outcomes in patients with acute respiratory distress syndrome: insights from the LUNG SAFE prospective cohort study. Lancet Respir Med. 2017;5:627–638. doi: 10.1016/S2213-2600(17)30213-8. [DOI] [PubMed] [Google Scholar]
- 28.Pepe PE, Potkin RT, Reus DH, Hudson LD, Carrico CJ. Clinical predictors of the adult respiratory distress syndrome. Am J Surg. 1982;144:124–130. doi: 10.1016/0002-9610(82)90612-2. [DOI] [PubMed] [Google Scholar]
- 29.Krishnasamy VP, Hallowell BD, Ko JY, et al. Characteristics of a nationwide outbreak of e-cigarette, or vaping, product use-associated lung injury—United States, August 2019–January 2020. MMWR Morb Mortal Wkly Rep. 2020;69:90–94. doi: 10.15585/mmwr.mm6903e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Layden JE, Ghinai I, Pray I, et al. Pulmonary illness related to e-cigarette use in Illinois and Wisconsin—final report. N Engl J Med. 2019;382:903–916. doi: 10.1056/NEJMoa1911614. [DOI] [PubMed] [Google Scholar]
- 31.Chowell G, Bertozzi SM, Colchero MA, et al. Severe respiratory disease concurrent with the circulation of H1N1 influenza. N Engl J Med. 2009;361:674–679. doi: 10.1056/NEJMoa0904023. [DOI] [PubMed] [Google Scholar]
- 32.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 34.Peiris JSM, Yuen KY, Osterhaus ADME, Stöhr K. The severe acute respiratory syndrome. N Engl J Med. 2003;349:2431–2441. doi: 10.1056/NEJMra032498. [DOI] [PubMed] [Google Scholar]
- 35.Memish ZA, Zumla AI, Al-Hakeem RF, Al-Rabeeah AA, Stephens GM. Family cluster of Middle East respiratory syndrome coronavirus infections. N Engl J Med. 2013;368:2487–2494. doi: 10.1056/NEJMoa1303729. [DOI] [PubMed] [Google Scholar]
- 36.Cauchemez S, Fraser C, Van Kerkhove MD, et al. Middle East respiratory syndrome coronavirus: quantification of the extent of the epidemic, surveillance biases, and transmissibility. Lancet Infect Dis. 2014;14:50–56. doi: 10.1016/S1473-3099(13)70304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Papazian L, Calfee CS, Chiumello D, et al. Diagnostic workup for ARDS patients. Intensive Care Med. 2016;42:674–685. doi: 10.1007/s00134-016-4324-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guillen-Guio B, Lorenzo-Salazar JM, Ma SF, et al. Sepsis-associated acute respiratory distress syndrome in individuals of European ancestry: a genome-wide association study. Lancet Respir Med. 2020;8:258–266. doi: 10.1016/S2213-2600(19)30368-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reilly JP, Christie JD, Meyer NJ. Fifty years of research in ARDS. Genomic contributions and opportunities. Am J Respir Crit Care Med. 2017;196:1113–1121. doi: 10.1164/rccm.201702-0405CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bernard GR, Artigas A, Brigham KL, et al. The American–European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149:818–824. doi: 10.1164/ajrccm.149.3.7509706. [DOI] [PubMed] [Google Scholar]
- 41.Cressoni M, Cadringher P, Chiurazzi C, et al. Lung inhomogeneity in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2014;189:149–158. doi: 10.1164/rccm.201308-1567OC. [DOI] [PubMed] [Google Scholar]
- 42.Putman RK, Hunninghake GM, Dieffenbach PB, et al. Interstitial lung abnormalities are associated with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195:138–141. doi: 10.1164/rccm.201604-0818LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schwarz MI, Albert RK. “Imitators” of the ARDS: implications for diagnosis and treatment. Chest. 2004;125:1530–1535. doi: 10.1378/chest.125.4.1530. [DOI] [PubMed] [Google Scholar]
- 44.Volpicelli G, Elbarbary M, Blaivas M, et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38:577–591. doi: 10.1007/s00134-012-2513-4. [DOI] [PubMed] [Google Scholar]
- 45.Bouhemad B, Brisson H, Le-Guen M, Arbelot C, Lu Q, Rouby J-J. Bedside ultrasound assessment of positive end-expiratory pressure-induced lung recruitment. Am J Respir Crit Care Med. 2011;183:341–347. doi: 10.1164/rccm.201003-0369OC. [DOI] [PubMed] [Google Scholar]
- 46.Riviello ED, Kiviri W, Twagirumugabe T, et al. Hospital incidence and outcomes of the acute respiratory distress syndrome using the Kigali modification of the Berlin definition. Am J Respir Crit Care Med. 2016;193:52–59. doi: 10.1164/rccm.201503-0584OC. [DOI] [PubMed] [Google Scholar]
- 47.Sekiguchi H, Schenck LA, Horie R, et al. Critical care ultrasonography differentiates ARDS, pulmonary edema, and other causes in the early course of acute hypoxemic respiratory failure. Chest. 2015;148:912–918. doi: 10.1378/chest.15-0341. [DOI] [PubMed] [Google Scholar]
- 48.Wiedemann HP, Wheeler AP, Bernard GR, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354:2564–2575. doi: 10.1056/NEJMoa062200. [DOI] [PubMed] [Google Scholar]
- 49.Meduri GU, Reddy RC, Stanley T, El-Zeky F. Pneumonia in acute respiratory distress syndrome. A prospective evaluation of bilateral bronchoscopic sampling. Am J Respir Crit Care Med. 1998;158:870–875. doi: 10.1164/ajrccm.158.3.9706112. [DOI] [PubMed] [Google Scholar]
- 50.Blount BC, Karwowski MP, Shields PG, et al. Vitamin E acetate in bronchoalveolar-lavage fluid associated with EVALI. N Engl J Med. 2020;382:697–705. doi: 10.1056/NEJMoa1916433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Siegel JD, Rhinehart E, Jackson M, et al. 2007 guideline for isolation precautions: preventing transmission of infectious agents in healthcare settings. Am J Infect Control. 2007;35:S65–164. doi: 10.1016/j.ajic.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of COVID-19—preliminary report. Reply. N Engl J Med. 2020;383:994. doi: 10.1056/NEJMc2022236. [DOI] [PubMed] [Google Scholar]
- 53.Libby LJ, Gelbman BD, Altorki NK, Christos PJ, Libby DM. Surgical lung biopsy in adult respiratory distress syndrome: a meta-analysis. Ann Thorac Surg. 2014;98:1254–1260. doi: 10.1016/j.athoracsur.2014.05.029. [DOI] [PubMed] [Google Scholar]
- 54.Bulpa PA, Dive AM, Mertens L, et al. Combined bronchoalveolar lavage and transbronchial lung biopsy: safety and yield in ventilated patients. Eur Respir J. 2003;21:489–494. doi: 10.1183/09031936.03.00298303. [DOI] [PubMed] [Google Scholar]
- 55.Palakshappa JA, Meyer NJ. Which patients with ARDS benefit from lung biopsy? Chest. 2015;148:1073–1082. doi: 10.1378/chest.15-0076. [DOI] [PubMed] [Google Scholar]
- 56.Matthay MA, Zemans RL, Zimmerman GA, et al. Acute respiratory distress syndrome. Nat Rev Dis Primers. 2019;5:18. doi: 10.1038/s41572-019-0069-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Matthay MA, Ware LB, Zimmerman GA. The acute respiratory distress syndrome. J Clin Invest. 2012;122:2731–2740. doi: 10.1172/JCI60331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Matthay MA, Wiener-Kronish JP. Intact epithelial barrier function is critical for the resolution of alveolar edema in humans. Am Rev Respir Dis. 1990;142:1250–1257. doi: 10.1164/ajrccm/142.6_Pt_1.1250. [DOI] [PubMed] [Google Scholar]
- 59.Erdmann AJ, 3rd, Vaughan TR, Jr, Brigham KL, Woolverton WC, Staub NC. Effect of increased vascular pressure on lung fluid balance in unanesthetized sheep. Circ Res. 1975;37:271–284. doi: 10.1161/01.res.37.3.271. [DOI] [PubMed] [Google Scholar]
- 60.Staub NC. Pulmonary edema. Physiol Rev. 1974;54:678–811. doi: 10.1152/physrev.1974.54.3.678. [DOI] [PubMed] [Google Scholar]
- 61.Hastings RH, Folkesson HG, Matthay MA. Mechanisms of alveolar protein clearance in the intact lung. Am J Physiol Lung Cell Mol Physiol. 2004;286:L679–L689. doi: 10.1152/ajplung.00205.2003. [DOI] [PubMed] [Google Scholar]
- 62.Zimmerman GA, Albertine KH, Carveth HJ, et al. Endothelial activation in ARDS. Chest. 1999;116(suppl):18–24S. doi: 10.1378/chest.116.suppl_1.18s. [DOI] [PubMed] [Google Scholar]
- 63.Millar FR, Summers C, Griffiths MJ, Toshner MR, Proudfoot AG. The pulmonary endothelium in acute respiratory distress syndrome: insights and therapeutic opportunities. Thorax. 2016;71:462–473. doi: 10.1136/thoraxjnl-2015-207461. [DOI] [PubMed] [Google Scholar]
- 64.Sun S, Sursal T, Adibnia Y, et al. Mitochondrial DAMPs increase endothelial permeability through neutrophil dependent and independent pathways. PloS one. 2013;8 doi: 10.1371/journal.pone.0059989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.London NR, Zhu W, Bozza FA, et al. Targeting Robo4-dependent Slit signaling to survive the cytokine storm in sepsis and influenza. Sci Transl Med. 2010;2 doi: 10.1126/scitranslmed.3000678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dudek SM, Garcia JG. Cytoskeletal regulation of pulmonary vascular permeability. J Appl Physiol (1985) 2001;91:1487–1500. doi: 10.1152/jappl.2001.91.4.1487. [DOI] [PubMed] [Google Scholar]
- 67.Abadie Y, Bregeon F, Papazian L, et al. Decreased VEGF concentration in lung tissue and vascular injury during ARDS. Eur Respir J. 2005;25:139–146. doi: 10.1183/09031936.04.00065504. [DOI] [PubMed] [Google Scholar]
- 68.Fujita M, Kuwano K, Kunitake R, et al. Endothelial cell apoptosis in lipopolysaccharide-induced lung injury in mice. Int Arch Allergy Immunol. 1998;117:202–208. doi: 10.1159/000024011. [DOI] [PubMed] [Google Scholar]
- 69.Gill SE, Rohan M, Mehta S. Role of pulmonary microvascular endothelial cell apoptosis in murine sepsis-induced lung injury in vivo. Respir Res. 2015;16:109. doi: 10.1186/s12931-015-0266-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Caudrillier A, Kessenbrock K, Gilliss BM, et al. Platelets induce neutrophil extracellular traps in transfusion-related acute lung injury. J Clin Invest. 2012;122:2661–2671. doi: 10.1172/JCI61303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bastarache JA, Wang L, Geiser T, et al. The alveolar epithelium can initiate the extrinsic coagulation cascade through expression of tissue factor. Thorax. 2007;62:608–616. doi: 10.1136/thx.2006.063305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cohen DS, Matthay MA, Cogan MG, Murray JF. Pulmonary edema associated with salt water near-drowning: new insights. Am Rev Respir Dis. 1992;146:794–796. doi: 10.1164/ajrccm/146.3.794. [DOI] [PubMed] [Google Scholar]
- 73.Ware LB, Matthay MA. Alveolar fluid clearance is impaired in the majority of patients with acute lung injury and the acute respiratory distress syndrome. Am J Respir Crit Care Med. 2001;163:1376–1383. doi: 10.1164/ajrccm.163.6.2004035. [DOI] [PubMed] [Google Scholar]
- 74.Wiener-Kronish JP, Albertine KH, Matthay MA. Differential responses of the endothelial and epithelial barriers of the lung in sheep to Escherichia coli endotoxin. J Clin Invest. 1991;88:864–875. doi: 10.1172/JCI115388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Short KR, Kasper J, van der Aa S, et al. Influenza virus damages the alveolar barrier by disrupting epithelial cell tight junctions. Eur Respir J. 2016;47:954–966. doi: 10.1183/13993003.01282-2015. [DOI] [PubMed] [Google Scholar]
- 76.Hook JL, Islam MN, Parker D, Prince AS, Bhattacharya S, Bhattacharya J. Disruption of staphylococcal aggregation protects against lethal lung injury. J Clin Invest. 2018;128:1074–1086. doi: 10.1172/JCI95823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Albertine KH, Soulier MF, Wang Z, et al. Fas and fas ligand are up-regulated in pulmonary edema fluid and lung tissue of patients with acute lung injury and the acute respiratory distress syndrome. Am J Pathol. 2002;161:1783–1796. doi: 10.1016/S0002-9440(10)64455-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bachofen M, Weibel ER. Structural alterations of lung parenchyma in the adult respiratory distress syndrome. Clin Chest Med. 1982;3:35–56. [PubMed] [Google Scholar]
- 79.Kerchberger VE, Huang Y, Koyama T, et al. Clinical and genetic contributors to new-onset atrial fibrillation in critically ill adults. Crit Care Med. 2019;48:22–30. doi: 10.1097/CCM.0000000000004034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Katzenstein AL, Bloor CM, Leibow AA. Diffuse alveolar damage—the role of oxygen, shock, and related factors. A review. Am J Pathol. 1976;85:209–228. [PMC free article] [PubMed] [Google Scholar]
- 81.Zimmerman GA, Renzetti AD, Hill HR. Functional and metabolic activity of granulocytes from patients with adult respiratory distress syndrome. Evidence for activated neutrophils in the pulmonary circulation. Am Rev Respir Dis. 1983;127:290–300. doi: 10.1164/arrd.1983.127.3.290. [DOI] [PubMed] [Google Scholar]
- 82.Juss JK, House D, Amour A, et al. Acute respiratory distress syndrome neutrophils have a distinct phenotype and are resistant to phosphoinositide 3-kinase inhibition. Am J Respir Crit Care Med. 2016;194:961–973. doi: 10.1164/rccm.201509-1818OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Juss J, Herre J, Begg M, et al. Genome-wide transcription profiling in neutrophils in acute respiratory distress syndrome. Lancet. 2015;385(suppl 1):S55. doi: 10.1016/S0140-6736(15)60370-1. [DOI] [PubMed] [Google Scholar]
- 84.Lefrançais E, Mallavia B, Zhuo H, Calfee CS, Looney MR. Maladaptive role of neutrophil extracellular traps in pathogen-induced lung injury. JCI Insight. 2018;3 doi: 10.1172/jci.insight.98178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Frank JA, Wray CM, McAuley DF, Schwendener R, Matthay MA. Alveolar macrophages contribute to alveolar barrier dysfunction in ventilator-induced lung injury. Am J Physiol Lung Cell Mol Physiol. 2006;291:L1191–L1198. doi: 10.1152/ajplung.00055.2006. [DOI] [PubMed] [Google Scholar]
- 86.Aggarwal NR, King LS, D'Alessio FR. Diverse macrophage populations mediate acute lung inflammation and resolution. Am J Physiol Lung Cell Mol Physiol. 2014;306:L709–L725. doi: 10.1152/ajplung.00341.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.D'Alessio FR, Tsushima K, Aggarwal NR, et al. CD4+CD25+Foxp3+ Tregs resolve experimental lung injury in mice and are present in humans with acute lung injury. J Clin Invest. 2009;119:2898–2913. doi: 10.1172/JCI36498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dreyfuss D, Saumon G. Role of tidal volume, FRC, and end-inspiratory volume in the development of pulmonary edema following mechanical ventilation. Am Rev Respir Dis. 1993;148:1194–1203. doi: 10.1164/ajrccm/148.5.1194. [DOI] [PubMed] [Google Scholar]
- 89.Webb HH, Tierney DF. Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressures. Protection by positive end-expiratory pressure. Am Rev Respir Dis. 1974;110:556–565. doi: 10.1164/arrd.1974.110.5.556. [DOI] [PubMed] [Google Scholar]
- 90.Dreyfuss D, Soler P, Basset G, Saumon G. High inflation pressure pulmonary edema. Respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. Am Rev Respir Dis. 1988;137:1159–1164. doi: 10.1164/ajrccm/137.5.1159. [DOI] [PubMed] [Google Scholar]
- 91.Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 92.Parsons PE, Eisner MD, Thompson BT, et al. Lower tidal volume ventilation and plasma cytokine markers of inflammation in patients with acute lung injury. Crit Care Med. 2005;33:1–6. doi: 10.1097/01.ccm.0000149854.61192.dc. [DOI] [PubMed] [Google Scholar]
- 93.Ranieri VM, Suter PM, Tortorella C, et al. Effect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress syndrome: a randomized controlled trial. JAMA. 1999;282:54–61. doi: 10.1001/jama.282.1.54. [DOI] [PubMed] [Google Scholar]
- 94.dos Santos CC, Okutani D, Hu P, et al. Differential gene profiling in acute lung injury identifies injury-specific gene expression. Crit Care Med. 2008;36:855–865. doi: 10.1097/CCM.0B013E3181659333. [DOI] [PubMed] [Google Scholar]
- 95.dos Santos CC, Slutsky AS. Mechanotransduction, ventilator-induced lung injury and multiple organ dysfunction syndrome. Intensive Care Med. 2000;26:638–642. doi: 10.1007/s001340051217. [DOI] [PubMed] [Google Scholar]
- 96.Gattinoni L, Tonetti T, Cressoni M, et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med. 2016;42:1567–1575. doi: 10.1007/s00134-016-4505-2. [DOI] [PubMed] [Google Scholar]
- 97.Fan E, Del Sorbo L, Goligher EC, et al. An official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice Guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195:1253–1263. doi: 10.1164/rccm.201703-0548ST. [DOI] [PubMed] [Google Scholar]
- 98.Pontoppidan H, Geffin B, Lowenstein E. Acute respiratory failure in the adult. 1. N Engl J Med. 1972;287:690–698. doi: 10.1056/NEJM197210052871404. [DOI] [PubMed] [Google Scholar]
- 99.Ricard JD. Are we really reducing tidal volume—and should we? Am J Respir Crit Care Med. 2003;167:1297–1298. doi: 10.1164/rccm.2303003. [DOI] [PubMed] [Google Scholar]
- 100.Gattinoni L, Agostoni A, Pesenti A, et al. Treatment of acute respiratory failure with low-frequency positive-pressure ventilation and extracorporeal removal of CO2. Lancet. 1980;2:292–294. doi: 10.1016/s0140-6736(80)90237-8. [DOI] [PubMed] [Google Scholar]
- 101.Hickling KG, Henderson SJ, Jackson R. Low mortality associated with low volume pressure limited ventilation with permissive hypercapnia in severe adult respiratory distress syndrome. Intensive Care Med. 1990;16:372–377. doi: 10.1007/BF01735174. [DOI] [PubMed] [Google Scholar]
- 102.Bellani G, Laffey JG, Pham T, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315:788–800. doi: 10.1001/jama.2016.0291. [DOI] [PubMed] [Google Scholar]
- 103.Barrot L, Asfar P, Mauny F, et al. Liberal or conservative oxygen therapy for acute respiratory distress syndrome. N Engl J Med. 2020;382:999–1008. doi: 10.1056/NEJMoa1916431. [DOI] [PubMed] [Google Scholar]
- 104.Chu DK, Kim LH, Young PJ, et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet. 2018;391:1693–1705. doi: 10.1016/S0140-6736(18)30479-3. [DOI] [PubMed] [Google Scholar]
- 105.Lachmann B. Open up the lung and keep the lung open. Intensive Care Med. 1992;18:319–321. doi: 10.1007/BF01694358. [DOI] [PubMed] [Google Scholar]
- 106.Mercat A, Richard JC, Vielle B, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299:646–655. doi: 10.1001/jama.299.6.646. [DOI] [PubMed] [Google Scholar]
- 107.Meade MO, Cook DJ, Guyatt GH, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299:637–645. doi: 10.1001/jama.299.6.637. [DOI] [PubMed] [Google Scholar]
- 108.Brower RG, Lanken PN, MacIntyre N, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351:327–336. doi: 10.1056/NEJMoa032193. [DOI] [PubMed] [Google Scholar]
- 109.Cavalcanti AB, Suzumura ÉA, Laranjeira LN, et al. Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2017;318:1335–1345. doi: 10.1001/jama.2017.14171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Alviar CL, Miller PE, McAreavey D, et al. Positive pressure ventilation in the cardiac intensive care unit. J Am Coll Cardiol. 2018;72:1532–1553. doi: 10.1016/j.jacc.2018.06.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Piehl MA, Brown RS. Use of extreme position changes in acute respiratory failure. Crit Care Med. 1976;4:13–14. doi: 10.1097/00003246-197601000-00003. [DOI] [PubMed] [Google Scholar]
- 112.Pelosi P, D'Andrea L, Vitale G, Pesenti A, Gattinoni L. Vertical gradient of regional lung inflation in adult respiratory distress syndrome. Am J Respir Crit Care Med. 1994;149:8–13. doi: 10.1164/ajrccm.149.1.8111603. [DOI] [PubMed] [Google Scholar]
- 113.Gattinoni L, Pelosi P, Vitale G, Pesenti A, D'Andrea L, Mascheroni D. Body position changes redistribute lung computed-tomographic density in patients with acute respiratory failure. Anesthesiology. 1991;74:15–23. doi: 10.1097/00000542-199101000-00004. [DOI] [PubMed] [Google Scholar]
- 114.Gattinoni L, Caironi P, Cressoni M, et al. Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med. 2006;354:1775–1786. doi: 10.1056/NEJMoa052052. [DOI] [PubMed] [Google Scholar]
- 115.Taccone P, Pesenti A, Latini R, et al. Prone positioning in patients with moderate and severe acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2009;302:1977–1984. doi: 10.1001/jama.2009.1614. [DOI] [PubMed] [Google Scholar]
- 116.Guerin C, Gaillard S, Lemasson S, et al. Effects of systematic prone positioning in hypoxemic acute respiratory failure: a randomized controlled trial. JAMA. 2004;292:2379–2387. doi: 10.1001/jama.292.19.2379. [DOI] [PubMed] [Google Scholar]
- 117.Gattinoni L, Taccone P, Carlesso E, Marini JJ. Prone position in acute respiratory distress syndrome. Rationale, indications, and limits. Am J Respir Crit Care Med. 2013;188:1286–1293. doi: 10.1164/rccm.201308-1532CI. [DOI] [PubMed] [Google Scholar]
- 118.Sud S, Friedrich JO, Adhikari NKJ, et al. Effect of prone positioning during mechanical ventilation on mortality among patients with acute respiratory distress syndrome: a systematic review and meta-analysis. CMAJ. 2014;186:E381–E390. doi: 10.1503/cmaj.140081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Guérin C, Reignier J, Richard JC, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 120.Coppo A, Bellani G, Winterton D, et al. Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. Lancet Respir Med. 2020;8:765–774. doi: 10.1016/S2213-2600(20)30268-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Thompson AE, Ranard BL, Wei Y, Jelic S. Prone positioning in awake, nonintubated patients with COVID-19 hypoxemic respiratory failure. JAMA Intern Med. 2020;180 doi: 10.1001/jamainternmed.2020.3030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Suzuki S, Hotchkiss JR, Takahashi T, Olson D, Adams AB, Marini JJ. Effect of core body temperature on ventilator-induced lung injury. Crit Care Med. 2004;32:144–149. doi: 10.1097/01.CCM.0000098857.14923.44. [DOI] [PubMed] [Google Scholar]
- 123.Manthous CA, Hall JB, Olson D, et al. Effect of cooling on oxygen consumption in febrile critically ill patients. Am J Respir Crit Care Med. 1995;151:10–14. doi: 10.1164/ajrccm.151.1.7812538. [DOI] [PubMed] [Google Scholar]
- 124.Kress JP, O'Connor MF, Pohlman AS, et al. Sedation of critically ill patients during mechanical ventilation. A comparison of propofol and midazolam. Am J Respir Crit Care Med. 1996;153:1012–1018. doi: 10.1164/ajrccm.153.3.8630539. [DOI] [PubMed] [Google Scholar]
- 125.Marik PE, Kaufman D. The effects of neuromuscular paralysis on systemic and splanchnic oxygen utilization in mechanically ventilated patients. Chest. 1996;109:1038–1042. doi: 10.1378/chest.109.4.1038. [DOI] [PubMed] [Google Scholar]
- 126.Papazian L, Forel JM, Gacouin A, et al. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med. 2010;363:1107–1116. doi: 10.1056/NEJMoa1005372. [DOI] [PubMed] [Google Scholar]
- 127.Alhurani RE, Oeckler RA, Franco PM, Jenkins SM, Gajic O, Pannu SR. Refractory hypoxemia and use of rescue strategies. A US National Survey of Adult Intensivists. Ann Am Thorac Soc. 2016;13:1105–1114. doi: 10.1513/AnnalsATS.201508-560OC. [DOI] [PubMed] [Google Scholar]
- 128.Shehabi Y, Bellomo R, Reade MC, et al. Early intensive care sedation predicts long-term mortality in ventilated critically ill patients. Am J Respir Crit Care Med. 2012;186:724–731. doi: 10.1164/rccm.201203-0522OC. [DOI] [PubMed] [Google Scholar]
- 129.Moss M, Huang DT, Brower RG, et al. Early neuromuscular blockade in the acute respiratory distress syndrome. N Engl J Med. 2019;380:1997–2008. doi: 10.1056/NEJMoa1901686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ely EW, Truman B, Shintani A, et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS) JAMA. 2003;289:2983–2991. doi: 10.1001/jama.289.22.2983. [DOI] [PubMed] [Google Scholar]
- 131.Staub NC. Pulmonary edema: physiologic approaches to management. Chest. 1978;74:559–564. doi: 10.1378/chest.74.5.559. [DOI] [PubMed] [Google Scholar]
- 132.Calfee CS, Matthay MA. Non-ventilatory management of acute lung injury and the acute respiratory distress syndrome. Chest. 2007;131:913–920. doi: 10.1378/chest.06-1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Rice TW, Wheeler AP, Thompson BT, et al. Initial trophic vs full enteral feeding in patients with acute lung injury: the EDEN randomized trial. JAMA. 2012;307:795–803. doi: 10.1001/jama.2012.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Rice TW, Wheeler AP, Thompson BT, deBoisblanc BP, Steingrub J, Rock P. Enteral omega-3 fatty acid, gamma-linolenic acid, and antioxidant supplementation in acute lung injury. JAMA. 2011;306:1574–1581. doi: 10.1001/jama.2011.1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Shehabi Y, Bellomo R, Kadiman S, et al. Sedation intensity in the first 48 hours of mechanical ventilation and 180-day mortality: a multinational prospective longitudinal cohort study. Crit Care Med. 2018;46:850–859. doi: 10.1097/CCM.0000000000003071. [DOI] [PubMed] [Google Scholar]
- 136.Devlin JW, Skrobik Y, Gélinas C, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46:1532–1548. doi: 10.1097/CCM.0000000000003259. [DOI] [PubMed] [Google Scholar]
- 137.Girard TD, Alhazzani W, Kress JP, et al. An official American Thoracic Society/American College of Chest Physicians clinical practice guideline: liberation from mechanical ventilation in critically ill adults. Rehabilitation protocols, ventilator liberation protocols, and cuff leak tests. Am J Respir Crit Care Med. 2017;195:120–133. doi: 10.1164/rccm.201610-2075ST. [DOI] [PubMed] [Google Scholar]
- 138.Liu KD, Levitt J, Zhuo H, et al. Randomized clinical trial of activated protein C for the treatment of acute lung injury. Am J Respir Crit Care Med. 2008;178:618–623. doi: 10.1164/rccm.200803-419OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Bigatello LM, Greene RE, Sprung CL, et al. HA-1A in septic patients with ARDS: results from the pivotal trial. Intensive Care Med. 1994;20:328–334. doi: 10.1007/BF01720904. [DOI] [PubMed] [Google Scholar]
- 140.Kor DJ, Carter RE, Park PK, et al. Effect of aspirin on development of ARDS in at-risk patients presenting to the emergency department: the LIPS-A randomized clinical trial. JAMA. 2016;315:2406–2414. doi: 10.1001/jama.2016.6330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Matthay MA, Brower RG, Carson S, et al. Randomized, placebo-controlled clinical trial of an aerosolized β2-agonist for treatment of acute lung injury. Am J Respir Crit Care Med. 2011;184:561–568. doi: 10.1164/rccm.201012-2090OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Gao Smith F, Perkins GD, Gates S, et al. Effect of intravenous β-2 agonist treatment on clinical outcomes in acute respiratory distress syndrome (BALTI-2): a multicentre, randomised controlled trial. Lancet. 2012;379:229–235. doi: 10.1016/S0140-6736(11)61623-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Bernard GR, Wheeler AP, Russell JA, et al. The effects of ibuprofen on the physiology and survival of patients with sepsis. N Engl J Med. 1997;336:912–918. doi: 10.1056/NEJM199703273361303. [DOI] [PubMed] [Google Scholar]
- 144.Ranieri VM, Pettilä V, Karvonen MK, et al. Effect of intravenous interferon β-1a on death and days free from mechanical ventilation among patients with moderate to severe acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2020;323:725–733. doi: 10.1001/jama.2019.22525. [DOI] [PubMed] [Google Scholar]
- 145.McAuley DF, Cross LM, Hamid U, et al. Keratinocyte growth factor for the treatment of the acute respiratory distress syndrome (KARE): a randomised, double-blind, placebo-controlled phase 2 trial. Lancet Respir Med. 2017;5:484–491. doi: 10.1016/S2213-2600(17)30171-6. [DOI] [PubMed] [Google Scholar]
- 146.The ARDS Network Ketoconazole for early treatment of acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2000;283:1995–2002. doi: 10.1001/jama.283.15.1995. [DOI] [PubMed] [Google Scholar]
- 147.The Acute Respiratory Distress Syndrome Network Randomized, placebo-controlled trial of lisofylline for early treatment of acute lung injury and acute respiratory distress syndrome. Crit Care Med. 2002;30:1–6. doi: 10.1097/00003246-200201000-00001. [DOI] [PubMed] [Google Scholar]
- 148.Zeiher BG, Artigas A, Vincent JL, et al. Neutrophil elastase inhibition in acute lung injury: results of the STRIVE study. Crit Care Med. 2004;32:1695–1702. doi: 10.1097/01.ccm.0000133332.48386.85. [DOI] [PubMed] [Google Scholar]
- 149.Iwata K, Doi A, Ohji G, et al. Effect of neutrophil elastase inhibitor (sivelestat sodium) in the treatment of acute lung injury (ALI) and acute respiratory distress syndrome (ARDS): a systematic review and meta-analysis. Intern Med. 2010;49:2423–2432. doi: 10.2169/internalmedicine.49.4010. [DOI] [PubMed] [Google Scholar]
- 150.Gebistorf F, Karam O, Wetterslev J, Afshari A. Inhaled nitric oxide for acute respiratory distress syndrome (ARDS) in children and adults. Cochrane Database Syst Rev. 2016;2016 doi: 10.1002/14651858.CD002787.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Bernard GR, Wheeler AP, Arons MM, et al. A trial of antioxidants N-acetylcysteine and procysteine in ARDS. Chest. 1997;112:164–172. doi: 10.1378/chest.112.1.164. [DOI] [PubMed] [Google Scholar]
- 152.Fuller BM, Mohr NM, Skrupky L, Fowler S, Kollef MH, Carpenter CR. The use of inhaled prostaglandins in patients with ARDS: a systematic review and meta-analysis. Chest. 2015;147:1510–1522. doi: 10.1378/chest.14-3161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Vincent JL, Brase R, Santman F, et al. A multi-centre, double-blind, placebo-controlled study of liposomal prostaglandin E1 (TLC C-53) in patients with acute respiratory distress syndrome. Intensive Care Med. 2001;27:1578–1583. doi: 10.1007/s001340101077. [DOI] [PubMed] [Google Scholar]
- 154.McAuley DF, Laffey JG, O'Kane CM, et al. Simvastatin in the acute respiratory distress syndrome. N Engl J Med. 2014;371:1695–1703. doi: 10.1056/NEJMoa1403285. [DOI] [PubMed] [Google Scholar]
- 155.Truwit JD, Bernard GR, Steingrub J, et al. Rosuvastatin for sepsis-associated acute respiratory distress syndrome. N Engl J Med. 2014;370:2191–2200. doi: 10.1056/NEJMoa1401520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Spragg RG, Lewis JF, Walmrath HD, et al. Effect of recombinant surfactant protein C-based surfactant on the acute respiratory distress syndrome. N Engl J Med. 2004;351:884–892. doi: 10.1056/NEJMoa033181. [DOI] [PubMed] [Google Scholar]
- 157.Lewis SR, Pritchard MW, Thomas CM, Smith AF. Pharmacological agents for adults with acute respiratory distress syndrome. Cochrane Database Syst Rev. 2019;7 doi: 10.1002/14651858.CD004477.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Ginde AA, Brower RG, Caterino JM, et al. Early high-dose vitamin D3 for critically ill, vitamin D-deficient patients. N Engl J Med. 2019;381:2529–2540. doi: 10.1056/NEJMoa1911124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Fowler AA, 3rd, Truwit JD, Hite RD, et al. Effect of vitamin C infusion on organ failure and biomarkers of inflammation and vascular injury in patients with sepsis and severe acute respiratory failure: the CITRIS-ALI randomized clinical trial. JAMA. 2019;322:1261–1270. doi: 10.1001/jama.2019.11825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Mohammed BM, Fisher BJ, Kraskauskas D, et al. Vitamin C: a novel regulator of neutrophil extracellular trap formation. Nutrients. 2013;5:3131–3151. doi: 10.3390/nu5083131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Fowler AA, 3rd, Syed AA, Knowlson S, et al. Phase I safety trial of intravenous ascorbic acid in patients with severe sepsis. J Transl Med. 2014;12:32. doi: 10.1186/1479-5876-12-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Fisher BJ, Seropian IM, Kraskauskas D, et al. Ascorbic acid attenuates lipopolysaccharide-induced acute lung injury. Crit Care Med. 2011;39:1454–1460. doi: 10.1097/CCM.0b013e3182120cb8. [DOI] [PubMed] [Google Scholar]
- 163.Matthay MA, Calfee CS, Zhuo H, et al. Treatment with allogeneic mesenchymal stromal cells for moderate to severe acute respiratory distress syndrome (START study): a randomised phase 2a safety trial. Lancet Respir Med. 2019;7:154–162. doi: 10.1016/S2213-2600(18)30418-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Matthay MA, McAuley DF, Ware LB. Clinical trials in acute respiratory distress syndrome: challenges and opportunities. Lancet Respir Med. 2017;5:524–534. doi: 10.1016/S2213-2600(17)30188-1. [DOI] [PubMed] [Google Scholar]
- 165.US Food and Drug Administration Enrichment strategies for clinical trials to support approval of human drugs and biological products. March, 2019. https://www.fda.gov/media/121320/download
- 166.Shankar-Hari M, Calfee CS. Lack of clinical benefit of interferon β-1a among patients with severe acute respiratory distress syndrome: time to overhaul drug trials in ARDS? JAMA. 2020;323:713–715. doi: 10.1001/jama.2019.22524. [DOI] [PubMed] [Google Scholar]
- 167.Peek GJ, Mugford M, Tiruvoipati R, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet. 2009;374:1351–1363. doi: 10.1016/S0140-6736(09)61069-2. [DOI] [PubMed] [Google Scholar]
- 168.Combes A, Hajage D, Capellier G, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378:1965–1975. doi: 10.1056/NEJMoa1800385. [DOI] [PubMed] [Google Scholar]
- 169.Villar J, Ferrando C, Martínez D, et al. Dexamethasone treatment for the acute respiratory distress syndrome: a multicentre, randomised controlled trial. Lancet Respir Med. 2020;8:267–276. doi: 10.1016/S2213-2600(19)30417-5. [DOI] [PubMed] [Google Scholar]
- 170.Steinberg KP, Hudson LD, Goodman RB, et al. Efficacy and safety of corticosteroids for persistent acute respiratory distress syndrome. N Engl J Med. 2006;354:1671–1684. doi: 10.1056/NEJMoa051693. [DOI] [PubMed] [Google Scholar]
- 171.Bernard GR, Luce JM, Sprung CL, et al. High-dose corticosteroids in patients with the adult respiratory distress syndrome. N Engl J Med. 1987;317:1565–1570. doi: 10.1056/NEJM198712173172504. [DOI] [PubMed] [Google Scholar]
- 172.Ferguson ND, Cook DJ, Guyatt GH, et al. High-frequency oscillation in early acute respiratory distress syndrome. N Engl J Med. 2013;368:795–805. doi: 10.1056/NEJMoa1215554. [DOI] [PubMed] [Google Scholar]
- 173.Young D, Lamb SE, Shah S, et al. High-frequency oscillation for acute respiratory distress syndrome. N Engl J Med. 2013;368:806–813. doi: 10.1056/NEJMoa1215716. [DOI] [PubMed] [Google Scholar]
- 174.Fielding-Singh V, Matthay MA, Calfee CS. Beyond low tidal volume ventilation: treatment adjuncts for severe respiratory failure in acute respiratory distress syndrome. Crit Care Med. 2018;46:1820–1831. doi: 10.1097/CCM.0000000000003406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Combes A, Schmidt M, Hodgson CL, et al. Extracorporeal life support for adults with acute respiratory distress syndrome. Intensive Care Med. 2020;46:2464–2476. doi: 10.1007/s00134-020-06290-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Abrams D, Pham T, Burns KEA, et al. Practice patterns and ethical considerations in the management of venovenous extracorporeal membrane oxygenation patients: an international survey. Crit Care Med. 2019;47:1346–1355. doi: 10.1097/CCM.0000000000003910. [DOI] [PubMed] [Google Scholar]
- 177.Lewis SR, Pritchard MW, Thomas CM, Smith AF. Pharmacological agents for adults with acute respiratory distress syndrome. Cochrane Database Syst Rev. 2019;7 doi: 10.1002/14651858.CD004477.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Brun-Buisson C, Richard J-CM, Mercat A, Thiébaut ACM, Brochard L. Early corticosteroids in severe influenza A/H1N1 pneumonia and acute respiratory distress syndrome. Am J Respir Crit Care Med. 2011;183:1200–1206. doi: 10.1164/rccm.201101-0135OC. [DOI] [PubMed] [Google Scholar]
- 179.Ruan S-Y, Lin H-H, Huang C-T, Kuo P-H, Wu H-D, Yu C-J. Exploring the heterogeneity of effects of corticosteroids on acute respiratory distress syndrome: a systematic review and meta-analysis. Crit Care. 2014;18:R63. doi: 10.1186/cc13819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Siegel DA, Jatlaoui TC, Koumans EH, et al. Interim guidance for health care providers evaluating and caring for patients with suspected e-cigarette, or vaping, product use associated lung injury—United States, October 2019. MMWR Morb Mortal Wkly Rep. 2019;68:919–927. doi: 10.15585/mmwr.mm6841e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Horby P, Lim WS, Emberson, et al. Dexamethasone in hospitalised patients with COVID-19. N Engl J Med. 2021;384:693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Briel M, Meade M, Mercat A, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 2010;303:865–873. doi: 10.1001/jama.2010.218. [DOI] [PubMed] [Google Scholar]
- 183.Constantin J-M, Jabaudon M, Lefrant J-Y, et al. Personalised mechanical ventilation tailored to lung morphology versus low positive end-expiratory pressure for patients with acute respiratory distress syndrome in France (the LIVE study): a multicentre, single-blind, randomised controlled trial. Lancet Respir Med. 2019;7:870–880. doi: 10.1016/S2213-2600(19)30138-9. [DOI] [PubMed] [Google Scholar]
- 184.Amato MBP, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372:747–755. doi: 10.1056/NEJMsa1410639. [DOI] [PubMed] [Google Scholar]
- 185.Talmor D, Sarge T, Malhotra A, et al. Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med. 2008;359:2095–2104. doi: 10.1056/NEJMoa0708638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Beitler JR, Sarge T, Banner-Goodspeed VM, et al. Effect of titrating positive end-expiratory pressure (PEEP) with an esophageal pressure-guided strategy vs an empirical high PEEP-FiO2 strategy on death and days free from mechanical ventilation among patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2019;321:846–857. doi: 10.1001/jama.2019.0555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Putensen C, Mutz NJ, Putensen-Himmer G, Zinserling J. Spontaneous breathing during ventilatory support improves ventilation-perfusion distributions in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 1999;159:1241–1248. doi: 10.1164/ajrccm.159.4.9806077. [DOI] [PubMed] [Google Scholar]
- 188.Yoshida T, Fujino Y, Amato MB, Kavanagh BP. Fifty years of research in ARDS. Spontaneous breathing during mechanical ventilation. Risks, mechanisms, and management. Am J Respir Crit Care Med. 2017;195:985–992. doi: 10.1164/rccm.201604-0748CP. [DOI] [PubMed] [Google Scholar]
- 189.Yoshida T, Torsani V, Gomes S, et al. Spontaneous effort causes occult pendelluft during mechanical ventilation. Am J Respir Crit Care Med. 2013;188:1420–1427. doi: 10.1164/rccm.201303-0539OC. [DOI] [PubMed] [Google Scholar]
- 190.Yoshida T, Roldan R, Beraldo MA, et al. Spontaneous effort during mechanical ventilation: maximal injury with less positive end-expiratory pressure. Crit Care Med. 2016;44:e678–e688. doi: 10.1097/CCM.0000000000001649. [DOI] [PubMed] [Google Scholar]
- 191.Antonelli M, Conti G, Rocco M, et al. A comparison of noninvasive positive-pressure ventilation and conventional mechanical ventilation in patients with acute respiratory failure. N Engl J Med. 1998;339:429–435. doi: 10.1056/NEJM199808133390703. [DOI] [PubMed] [Google Scholar]
- 192.Rello J, Pérez M, Roca O, et al. High-flow nasal therapy in adults with severe acute respiratory infection: a cohort study in patients with 2009 influenza A/H1N1v. J Crit Care. 2012;27:434–439. doi: 10.1016/j.jcrc.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 193.Bellani G, Laffey JG, Pham T, et al. Noninvasive ventilation of patients with acute respiratory distress syndrome. Insights from the LUNG SAFE study. Am J Respir Crit Care Med. 2017;195:67–77. doi: 10.1164/rccm.201606-1306OC. [DOI] [PubMed] [Google Scholar]
- 194.Kangelaris KN, Ware LB, Wang CY, et al. Timing of intubation and clinical outcomes in adults with acute respiratory distress syndrome. Crit Care Med. 2016;44:120–129. doi: 10.1097/CCM.0000000000001359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Mauri T, Turrini C, Eronia N, et al. Physiologic effects of high-flow nasal cannula in acute hypoxemic respiratory failure. Am J Respir Crit Care Med. 2017;195:1207–1215. doi: 10.1164/rccm.201605-0916OC. [DOI] [PubMed] [Google Scholar]
- 196.Frat J-P, Thille AW, Mercat A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372:2185–2196. doi: 10.1056/NEJMoa1503326. [DOI] [PubMed] [Google Scholar]
- 197.Gattinoni L, Pelosi P, Suter PM, Pedoto A, Vercesi P, Lissoni A. Acute respiratory distress syndrome caused by pulmonary and extrapulmonary disease. Different syndromes? Am J Respir Crit Care Med. 1998;158:3–11. doi: 10.1164/ajrccm.158.1.9708031. [DOI] [PubMed] [Google Scholar]
- 198.Shaver CM, Bastarache JA. Clinical and biological heterogeneity in acute respiratory distress syndrome: direct versus indirect lung injury. Clin Chest Med. 2014;35:639–653. doi: 10.1016/j.ccm.2014.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Calfee CS, Janz DR, Bernard GR, et al. Distinct molecular phenotypes of direct vs indirect ARDS in single-center and multicenter studies. Chest. 2015;147:1539–1548. doi: 10.1378/chest.14-2454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Luo L, Shaver CM, Zhao Z, et al. Clinical predictors of hospital mortality differ between direct and indirect ARDS. Chest. 2017;151:755–763. doi: 10.1016/j.chest.2016.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Hendrickson CM, Calfee CS. A new frontier in ARDS trials: phenotyping before randomisation. Lancet Respir Med. 2019;7:830–831. doi: 10.1016/S2213-2600(19)30175-4. [DOI] [PubMed] [Google Scholar]
- 202.Calfee CS, Delucchi K, Parsons PE, Thompson BT, Ware LB, Matthay MA. Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials. Lancet Respir Med. 2014;2:611–620. doi: 10.1016/S2213-2600(14)70097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Famous KR, Delucchi K, Ware LB, et al. Acute respiratory distress syndrome subphenotypes respond differently to randomized fluid management strategy. Am J Respir Crit Care Med. 2017;195:331–338. doi: 10.1164/rccm.201603-0645OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Sinha P, Delucchi KL, Thompson BT, McAuley DF, Matthay MA, Calfee CS. Latent class analysis of ARDS subphenotypes: a secondary analysis of the statins for acutely injured lungs from sepsis (SAILS) study. Intensive Care Med. 2018;44:1859–1869. doi: 10.1007/s00134-018-5378-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Reilly JP, Calfee CS, Christie JD. Acute respiratory distress syndrome phenotypes. Semin Respir Crit Care Med. 2019;40:19–30. doi: 10.1055/s-0039-1684049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Bos LD, Schouten LR, van Vught LA, et al. Identification and validation of distinct biological phenotypes in patients with acute respiratory distress syndrome by cluster analysis. Thorax. 2017;72:876–883. doi: 10.1136/thoraxjnl-2016-209719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Bos LDJ, Scicluna BP, Ong DSY, Cremer O, van der Poll T, Schultz MJ. Understanding heterogeneity in biologic phenotypes of acute respiratory distress syndrome by leukocyte expression profiles. Am J Respir Crit Care Med. 2019;200:42–50. doi: 10.1164/rccm.201809-1808OC. [DOI] [PubMed] [Google Scholar]
- 208.Davenport EE, Burnham KL, Radhakrishnan J, et al. Genomic landscape of the individual host response and outcomes in sepsis: a prospective cohort study. Lancet Respir Med. 2016;4:259–271. doi: 10.1016/S2213-2600(16)00046-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Gattinoni L, Coppola S, Cressoni M, Busana M, Rossi S, Chiumello D. COVID-19 does not lead to a “typical” acute respiratory distress syndrome. Am J Respir Crit Care Med. 2020;201:1299–1300. doi: 10.1164/rccm.202003-0817LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Ziehr DR, Alladina J, Petri CR, et al. Respiratory pathophysiology of mechanically ventilated patients with COVID-19: a cohort study. Am J Respir Crit Care Med. 2020;201:1560–1564. doi: 10.1164/rccm.202004-1163LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Klok FA, Kruip MJHA, van der Meer NJM, et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: an updated analysis. Thromb Res. 2020;191:148–150. doi: 10.1016/j.thromres.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Mangalmurti NS, Reilly JP, Cines DB, Hunter CA, Meyer NJ, Vaughan AE. COVID-19-associated acute respiratory distress syndrome clarified: a vascular endotype? Am J Respir Crit Care Med. 2020;202:750–753. doi: 10.1164/rccm.202006-2598LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Sterne JAC, Murthy S, Diaz JV, et al. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. JAMA. 2020;324:1330–1341. doi: 10.1001/jama.2020.17023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Garcia JG, Liu F, Verin AD, et al. Sphingosine 1-phosphate promotes endothelial cell barrier integrity by Edg-dependent cytoskeletal rearrangement. J Clin Invest. 2001;108:689–701. doi: 10.1172/JCI12450. [DOI] [PMC free article] [PubMed] [Google Scholar]