Abstract
Objective: To explore the effect of acupuncture combined with Shenqi Yigan Decoction on liver function and T cell subsets in patients with Hepatitis B virus-induced liver fibrosis. Methods: All of the 90 patients with HBV-induced liver fibrosis were divided into two groups with the control group (n=45) treated with the conventional treatment, and the observation group (n=45) treated with acupuncture and Shenqi Yigan decoction based on the observation group. The seroconversion rate of hepatitis Be antigen (HBeAg), the liver function, the serum indexes of liver fibrosis of hyaluronic acid (HA), laminin (LN), type III procollagen (PC III), type IV collagen (IV-C), the T cell subsets and the inflammatory factors were compared between the two groups. Results: After 2 and 4 months of treatment, the HBeAg seroconversion rate of patients in the observation group was higher than that of the control group, but the difference was not significant (P>0.05). And the HBeAg seroconversion rate of patients in the observation group was significantly higher than that of the control group after 6 months treatment (P<0.05). After treatment, the serum levels of the liver function index of aspartate aminotransferase (AST), alanine aminotransferase (ALT), total bilirubin (Tbil), the liver fibrosis index of HA, LN, PC III, and the inflammatory factor of type IV collagen (IV-C), C-reactive protein (CRP) and tumor necrosis factor-α (TNF-α) in the two groups were lower than those before treatment, in addition, the levels of there index were lower in the observation group (all P<0.05). After treatment, the proportion of CD3+, CD4+ T lymphocyte subsets and CD4+/CD8+ in peripheral blood of the two groups were increased, and the proportion of CD8+ was decreased. The change range of the observation group was larger than that of the observation group (all P<0.01). The proportion of patients with liver fibrosis grade F1 in the observation group after treatment was significantly higher than that before treatment, and the proportion of patients with liver fibrosis grade F2 to F3 was significantly lower than that before treatment. There was a significant difference in liver fibrosis grade between the two groups after treatment (P<0.05). Conclusion: The combined treatment of acupuncture and Shenqi Yigan decoction can significantly improve the liver function of patients with HBV-induced liver fibrosis, delay the progress of liver fibrosis, improve the cellular immune function and reduce the inflammatory reaction.
Keywords: Hepatitis B virus-induced liver fibrosis, acupuncture, Shenqi Yigan Decoction, liver function, T cell subsets
Introduction
Hepatitis B virus (HBV) is a global infectious disease with liver injury as the main clinical manifestation. As the disease progresses, it can lead to liver fibrosis, liver cirrhosis and even the liver cancer [1]. Among which, the liver fibrosis is caused by abnormal proliferation of connective tissue in the liver caused by long-term infection of HBV, leading to diffuse precipitation of extracellular matrix in the liver [2]. Liver fibrosis can aggravate the inflammatory response through a variety of cytokines, further leading to the changes in the microenvironment in the liver, and then leading to the occurrence of liver cirrhosis [3]. After HBV infection, the CD4+ T lymphocytes are prone to apoptosis, the proportion of CD4+ cells is decreased, the proportion of CD8 cells is increased, and the CD4/CD8 reflecting the immune function of the body is also decreased. As the function of T lymphocytes is exhausted and the function of secreting cytokines decreases, it can induce continuous proliferation of HBV, aggravate the inflammatory response, induce the liver fibrosis, and eventually cause the liver cirrhosis [4]. Therefore, improving the T lymphocyte subsets and delaying the progression of liver fibrosis have important clinical significance for the prevention of liver cirrhosis and even liver cancer.
According to traditional Chinese medicine, the main cause of HBV-induced liver fibrosis is liver blood stasis, which can be reversed as long as the state of liver blood stasis is improved [5]. Shenqi Yigan decoction is a classic prescription for promoting blood circulation and removing blood stasis. It is also a common prescription for a variety of liver diseases caused by liver blood stasis, such as liver fibrosis, liver cirrhosis and so on. Studies have found that the decoction of the Shenqi Yigan decoction has obvious protective effect on liver function of patients with liver fibrosis, and it can delay the progression of liver fibrosis [6]. But its effect on immune function of patients with liver fibrosis has not reached a consensus. Acupuncture and moxibustion are the quintessence of traditional Chinese medicine, which have the function of dredging the channel and regulating yin and yang. Studies have pointed out that acupuncture can increase the activity of antioxidant enzymes in the liver of fatigue rats by regulating glutathione, and then reducing the injury of free radicals [7]. It can also inhibit the production of free fatty acids in the liver, reduce the content of cholesterol, and improve the liver injury caused by CCl4. However, the application of acupuncture in patients with liver fibrosis is very rare. In this study, a combined treatment of acupuncture and medicine was used to explore the effects of acupuncture combined with Shenqi Yigan Decoction on liver function and T cell subsets in patients with HBV-induced liver fibrosis.
Materials and methods
Baseline data
All of 90 patients with HBV-induced liver fibrosis treated in Affiliated Hospital of North Sichuan Medical College from February 2018 to January 2020 were divided into two groups of observation group (n=45) and control group (n=45). The baseline data of the two groups are shown in the part of results.
Inclusion criteria: (1) The age of the patients are from 35 to 75 years old. (2) Patients who meet the diagnostic criteria of HBV-induced liver fibrosis of Guidelines for the prevention and treatment of chronic hepatitis B (2015 edition) [8]. (3) Patients have the syndrome of blood stasis obstructing collaterals according to traditional Chinese medicine differentiation. (4) Patients who have not received anti-liver fibrosis treatment before enrollment. (5) Patients who have signed the informed consent form.
Exclusion criteria: (1) Patients were complicated with other liver diseases, such as liver cirrhosis, liver ascites, liver cancer, hepatitis C, etc. (2) Patients with liver fibrosis that caused by other reasons. (3) Patients were contraindicated to acupuncture, such as coagulation disorders or intolerance to acupuncture treatment. (4) Patients with allergic constitution or allergic to some traditional Chinese medicine in Shenqi Yigan decoction. (5) Patients with malignant tumor or accompanied by severe mental illness. (6) Patients were complicated with substantial diseases of important organs such as heart and kidney. (7) Female patients who were pregnant or breastfeeding. This study has been approved by the Medical Ethics Committee of Affiliated Hospital of North Sichuan Medical College.
Methods
The control group was given conventional treatment of oral adminstration of Entecavir dispersible tablets (Origin: Shandong Lukang Pharmaceutical Co., Ltd, China, with the specification of 1.0 mg calculated by C12H15N5O3) with 1.0 mg/time, 1 time/d, and oral adminstration of Diammonium Glycyrrhizinate Enteric-coated Capsules (Origin: Chiatai Tianqing Pharmaceutical Group Co., Ltd., China, with the specification of 50 mg) with 150 mg/times, 3 times/d for 6 months. The observation group added acupuncture combined with Shenqi Yigan decoction, using disposable sterile acupuncture needle (Origin: Shenzhen Yinuo Medical Apparatus and Instruments Co., Ltd., China, with the specification of 0.35 mm×40 mm) to acupuncture bilateral Zusanli with the depth of 1.2 Cun, Taichong point (0.8 Cun) and Sanyinjiao (0.8 Cun). The reinforcing method was performed after needling sensation (Zusanli, Sanyinjiao) and induce qi with essence (Taichong acupoint) were used, and the needle was retained for 30 min, 1 time/d. The prescription of Shenqi Yigan Decoction: Astragalus Root 25 g, Honeysuckle 25 g, Radix Salviae Miltiorrhizae 20 g, Isatis Root 18 g, Pseudostellaria Root 18 g, Magnolia officinalis 12 g, Tangerine peel 12 g, Schisandra 9 g, Gardenia 9 g, Rhubarb 6 g, Licorice 6 g, 1 dose/d, decocted in water, once in the morning and once in the evening, for 6 continuous treatment of 6 months.
Outcome measures
Main outcomes
(1) About 5 mL of venous blood was drawn from patients before and after treatment. After it collected, the serum was collected by centrifugation for 10 min with 3000 r/min. Automatic biochemical analyzer (American Beckman Coulter Company. Model: AU5800. Origin: USA) was used to detect the level of liver function indexes, including serum Aspartate aminotransferase (AST), Alanine aminotransferase (ALT) and total bilirubin (TBil). The serum indexes of liver fibrosis were detected by enzyme-linked immunosorbent assay (ELISA), including hyaluronic acid (HA), laminin (LN), type III procollagen (PC III) and type IV collagen (IV-C). The ELISA kits were purchased from Shanghai Enzymatic Biotechnology Co., Ltd., China. All operations were carried out in strict accordance with the instructions of the kit.
(2) About 2 mL of venous blood was drawn from patients before and after treatment for the detection of the ratio of CD3+, CD4+ and CD8+ T lymphocyte subsets in peripheral blood by flow cytometry (Beckman Coulter Company, USA: Gallios, Origin: USA). After the detection, the ratio of CD4+/CD8+ was calculated [9].
Secondary outcomes
The HBeAg seroconversion rate was compared between the two groups after 2 months, 4 months and 6 months of treatment. HBeAg seroconversion rate = the number of HBeAg seroconversion cases/total cases *100%.
The levels of serum C-reactive protein (CRP) and tumor necrosis factor-α (TNF-α) were detected by ELISA.
The grading of liver fibrosis was compared between the two groups before and after treatment. The grading criteria of liver fibrosis were as follows: F0: no liver fibrosis, F1: mild liver fibrosis, F2: moderate liver fibrosis, F3: severe liver fibrosis, F4: liver cirrhosis [10].
Statistical analysis
SPSS 20.0 was used for data statistics, the enumeration data was expressed in %, and χ2 test was used for comparison. The measurement data was expressed as mean ± standard deviation (x̅ ± sd), the paired t-test was used for comparison between the same group before and after treatment, and independent sample t-test was used for comparison between the two groups. P<0.05 indicates that the difference is statistically significant.
Results
Baseline data
There was no statistical difference in baseline data between the two groups (P>0.05), and comparisons can be made between the two groups. The details were shown in Table 1.
Table 1.
Comparison of general data in patients of the two groups (n, x̅ ± sd)
| Index | Observation group (n=45) | Control group (n=45) | χ2/t | P |
|---|---|---|---|---|
| Gender (n) | 0.401 | 0.527 | ||
| Male | 25 | 22 | ||
| Female | 20 | 23 | ||
| Age (years) | 58.5±5.3 | 57.6±6.5 | 0.720 | 0.474 |
| BMI (kg/m2) | 23.20±2.65 | 23.49±2.33 | 0.551 | 0.583 |
| Course of hepatitis B disease (years) | 13.95±3.20 | 14.41±3.51 | 0.650 | 0.518 |
| Liver fibrosis grading (n) | 1.113 | 0.291 | ||
| F1 | 26 | 21 | ||
| F2-F3 | 19 | 24 | ||
| AST (U/L) | 57.79±4.07 | 58.45±5.48 | 0.649 | 0.518 |
| ALT (U/L) | 65.59±6.50 | 66.05±5.48 | 0.363 | 0.718 |
| TBil (μmol/L) | 37.60±5.29 | 36.98±4.30 | 0.610 | 0.543 |
| HBeAg | 2.182 | 0.140 | ||
| Positive | 25 | 18 | ||
| Negative | 20 | 27 | ||
| HBV DNA (mEq/mL) | 0.94±0.10 | 0.90±0.23 | 1.070 | 0.288 |
Note: AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; TBil: total bilirubin; HBeAg: hepatitis Be antigen; HBV: hepatitis B virus.
Comparison of the HBeAg seroconversion rate between the two groups
The HBeAg seroconversion rate of patients in the observation group after 2 and 4 months treatment was higher than that of the control group, but there was no significant difference between the two groups (P>0.05). The HBeAg seroconversion rate of patients in the observation group was significantly higher than that of the control group after 6 months treatment (P<0.05). The details were shown in Table 2.
Table 2.
Comparison of HBeAg seroconversion rate between the two groups after treatment (n, %)
| Groups | Treatment for 2 months | Treatment for 4 months | Treatment for 6 months |
|---|---|---|---|
| Observation group (n=45) | 15 (33.33) | 29 (64.44) | 39 (86.67) |
| Control group (n=45) | 12 (26.67) | 22 (48.89) | 30 (66.67) |
| χ2 | 0.476 | 2.217 | 5.031 |
| P | 0.490 | 0.136 | 0.025 |
Note: HBeAg: hepatitis Be antigen.
Liver function
After treatment, the serum levels of AST, ALT and TBil in the two groups were lower than those before treatment, and the observation group were lower than the control group (all P<0.001). The details were shown in Table 3.
Table 3.
Comparison of liver function between the two groups before and after treatment (x̅ ± sd)
| Index | Time point | Observation group (n=45) | Control group (n=45) | t | P |
|---|---|---|---|---|---|
| AST (U/L) | Before treatment | 57.79±4.07 | 58.45±5.48 | 0.649 | 0.518 |
| After treatment | 37.59±4.85*** | 41.43±4.30*** | 3.560 | 0.000 | |
| ALT (U/L) | Before treatment | 65.59±6.50 | 66.05±5.48 | 0.363 | 0.718 |
| After treatment | 38.70±4.39*** | 42.40±4.95*** | 3.751 | 0.000 | |
| TBil (μmol/L) | Before treatment | 37.60±5.29 | 36.98±4.30 | 0.610 | 0.543 |
| After treatment | 27.04±4.95*** | 32.40±3.86*** | 5.728 | 0.000 |
Note: Compared with before treatment;
P<0.001.
AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; TBil: total bilirubin.
Indexes of liver fibrosis
After treatment, the levels of serum HA, LN, PC III and IV-C in the two groups were significantly lower than those before treatment, and the observation group were lower than the observation group (all P<0.05). The details were shown in Table 4.
Table 4.
Comparison of the levels of liver fibrosis indexes between the two groups before and after treatment (μg/L, x̅ ± sd)
| Index | Time point | Observation group (n=45) | Control group (n=45) | t | P |
|---|---|---|---|---|---|
| HA | Before treatment | 320.05±65.40 | 325.59±58.06 | 0.425 | 0.672 |
| After treatment | 221.06±49.96*** | 275.08±48.58*** | 5.200 | 0.000 | |
| LN | Before treatment | 171.27±19.95 | 169.89±18.47 | 0.341 | 0.734 |
| After treatment | 133.85±13.20*** | 140.04±12.48*** | 2.286 | 0.025 | |
| PC III | Before treatment | 50.05±6.50 | 49.96±5.38 | 0.072 | 0.943 |
| After treatment | 30.04±4.39*** | 37.04±4.96*** | 7.089 | 0.000 | |
| IV-C | Before treatment | 155.68±21.94 | 156.30±18.48 | 0.145 | 0.885 |
| After treatment | 121.28±17.09*** | 134.49±16.60*** | 3.719 | 0.000 |
Note: Compared with before treatment;
P<0.001.
HA: hyaluronic acid; LN: laminin; PC III: type III procollagen; IV-C: type IV collagen.
T lymphocyte subsets
After treatment, the ratio of CD3+, CD4+ and CD4+/CD8+ in peripheral blood of the two groups increased, while the ratio of CD8+ decreased. And the observation group changed more significantly (all P<0.01). The details were shown in Table 5 and Figure 1.
Table 5.
Comparison of the proportion of T lymphocyte subsets between the two groups before and after treatment (x̅ ± sd)
| Index | Time point | Observation group (n=45) | Control group (n=45) | t | P |
|---|---|---|---|---|---|
| CD3+ (%) | Before treatment | 48.80±4.40 | 49.13±4.38 | 0.357 | 0.722 |
| After treatment | 56.68±5.10*** | 52.20±4.95*** | 4.228 | 0.000 | |
| CD4+ (%) | Before treatment | 30.03±4.03 | 30.64±3.55 | 0.762 | 0.448 |
| After treatment | 36.06±4.87*** | 33.48±4.03*** | 2.738 | 0.007 | |
| CD8+ (%) | Before treatment | 32.05±3.33 | 32.43±3.74 | 0.509 | 0.612 |
| After treatment | 27.58±3.05*** | 29.95±3.88*** | 3.221 | 0.002 | |
| CD4+/CD8+ | Before treatment | 0.93±0.29 | 0.94±0.27 | 0.169 | 0.866 |
| After treatment | 1.28±0.22*** | 1.12±0.30*** | 2.885 | 0.005 |
Note: Compared with before treatment;
P<0.001.
Figure 1.
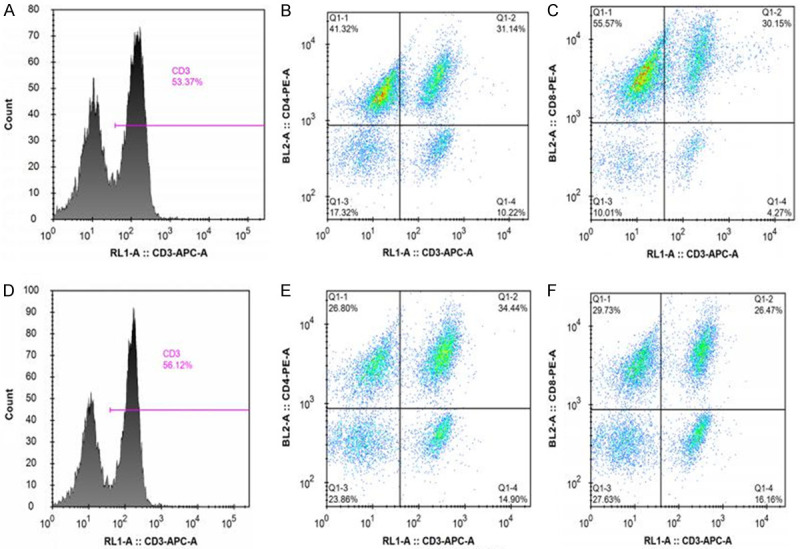
The expression of CD3+ (%), CD4+ (%), CD8+ (%) in the control group and observation group. A: Control group CD3+ (%); B: Control group CD4+ (%); C: Control group CD8+ (%); D: Observation group CD3+ (%); E: Observation group CD4+ (%); F: Observation group CD8+ (%).
Inflammatory factors
After treatment, the levels of serum CRP and TNF-α in both groups were significantly lower than those before treatment, and the observation group was lower than the control group (all P<0.05). The details were shown in Figure 2.
Figure 2.
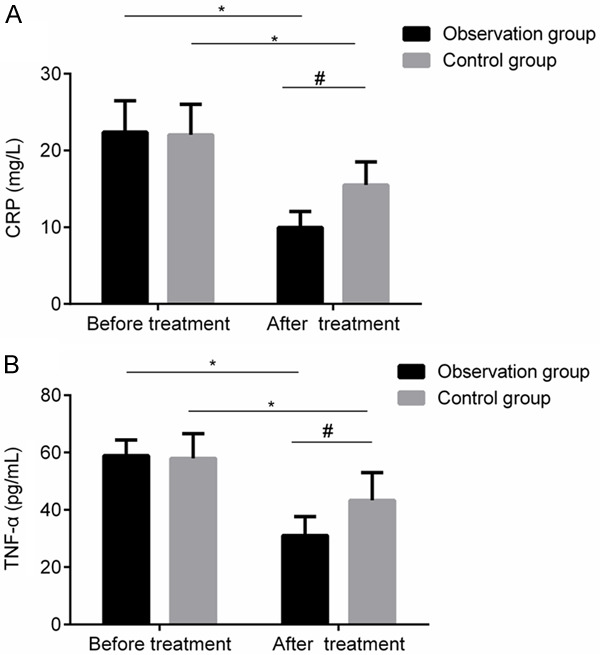
Comparison of serum inflammatory factors between the two groups before and after treatment. A: Serum CRP level; B: Serum TNF-α level. Compared with before treatment, *P< 0.05; compared with control group after treatment, #P<0.05. CRP: C-reactive protein; TNF-α: tumor necrosis factor-α.
Comparison of prognosis between the two groups
During the follow-up for 3 months after discharge, there was 1 case conversion of liver cirrhosis in the observation group and 3 cases conversion of cirrhosis in the control group. There was no significant difference in the proportion of patients of cirrhosis between the two groups (P>0.05); After treatment, the proportion of patients with liver fibrosis grade F1 in the observation group was significantly higher than that before treatment, while the proportion of patients with grade F2 to F3 was significantly lower than that before treatment, and there was a significant difference in liver fibrosis grade between the two groups after treatment (P<0.05). The details were shown in Table 6.
Table 6.
Changes of liver fibrosis grade in two groups before and after treatment (n, %)
| Groups | Time point | F1 | F2-F3 | F4 |
|---|---|---|---|---|
| Observation group (n=45) | Before treatment | 26 (57.78) | 19 (42.22) | 0 (0.00) |
| After treatment | 36 (80.00) | 8 (17.78) | 1 (2.22) | |
| χ2 | 7.094 | |||
| P | 0.029 | |||
| Control group (n=45) | Time point | 21 (46.67) | 24 (53.33) | 0 (0.00) |
| Before treatment | 25 (55.56) | 17 (37.78) | 3 (6.67) | |
| χ2 | 4.543 | |||
| P | 0.103 | |||
Note: Comparison between the two groups after treatment, χ2=6.224, P=0.045.
Discussion
According to the theory of traditional Chinese medicine, the occurrence of liver fibrosis is due to the invasion of damp-heat and evil toxins to the liver, the stasis of liver blood, the stagnation of QI due to the liver depression, the dampness due to spleen deficiency. Therefore, traditional Chinese medicine believes that promoting blood circulation and removing blood stasis should be the main treatment principle [11]. Shenqi Yigan decoction is a representative prescription for the treatment of liver cirrhosis. It can not only promote liver cell regeneration, but also inhibit the process of necrosis of liver cells and hepatitis [12]. In this prescription, Astragalus Root has the function of replenishing Qi to invigorate the splee, invigorating Qi and generate blood, and driving out evil spirits. Radix Salviae Miltiorrhizae has the functions of promoting blood circulation to dispel blood stasis and nourishing the blood and cooling blood. Isatis Root and Honeysuckle have the functions of clearing away heat and toxic material. Magnolia Bark compatibility with Tangerine Peel has the function of regulating qi-flowing for strengthening spleen, and eliminating dampness and eliminating phlegm. Chinese Magnoliavine Fruit has the function of astringenting for spontaneous sweating and tonifying qi and strengthening liver. Gardenia and Rhubarb has the function of normalizing gallbladder to cure jaundice. Licorice blends all medicines, tonifying spleen and replenishing Qi, clearing heat and detoxification. All kinds of medicines are used together to play the effects of promoting blood circulation and removing blood stasis, tonifying Qi, strengthening liver and spleen [6]. Acupuncture is the core of traditional Chinese medicine. This study is based on the meridian theory of traditional Chinese medicine to acupuncture points of the “foot three needles”. The “foot three needles” are all three Yin points, and these acupoints are closely related to the function of liver and spleen. Acupuncture the “foot three needles” is helpful to dredge the meridians and collaterals, replenishing Qi to invigorate the spleen [13]. The combination of acupuncture and medicine can enhance the function of activating blood circulation and removing blood stasis, dredging channels and collaterals, tonifying qi, strengthening liver and invigorating spleen.
The serum indexes of HA, LN, PC III and IV-C can effectively reflect the condition of liver injury and fibrosis, and they are commonly used as clinical indicators to reflect the liver fibrosis. Many studies have confirmed that the levels of the above four indexes for liver fibrosis in patients with liver injury were increased in varying degrees, and they were decreased with the recovery of the disease [14,15]. In this study, the liver function and the four indexes of liver fibrosis in the observation group were lower than those in the control group. There was no significant difference in the proportion of patients with liver cirrhosis between the two groups within 3 months after discharge. And the proportion of patients with liver fibrosis grade F1 in the observation group after treatment was significantly higher than that before treatment, and the proportion of patients with liver fibrosis F2-F3 grade was significantly lower than that before treatment. There were similar changes in the control group before and after treatment, but there was no statistical difference in the grade of liver fibrosis before and after treatment. It suggests that the combination of acupuncture and Shenqi Yigan decoction can not only improve the liver function of patients with HBV-induced liver fibrosis, but also effectively delay the progress of liver fibrosis, reduce the grade of liver fibrosis, and promote the transformation of liver fibrosis to mild. Zhou et al. also found that the addition of acupuncture on the basis of conventional treatment can improve the level of the four indexes of liver fibrosis in patients with liver fibrosis, it can be more beneficial to delay the progression of liver fibrosis [16]. This study has also found that there was no significant difference in the HBeAg seroconversion rate between the two groups 2 and 4 months after treatment. But the HBeAg seroconversion rate in the observation group was significantly higher than that in the control group after 6 months treatment, suggesting that the combination treatment of acupuncture and Shenqi Yigan decoction is more beneficial to promote the HBeAg seroconversion rate in patients with HBV-induced liver fibrosis. Yu et al. also found that Shenqi Yigan decoction adjuvant treatment can significantly increase the HBeAg seroconversion rate in patients with HBV-induced liver fibrosis [6].
HBV does not act directly on hepatocytes, but it can cause the damage to liver cell and continuous onsets of hepatitis by stimulating immune response disorders. The cellular immunity plays a decisive role in the process of immune response, and it can be reflected by the detection of T lymphocyte subsets [17]. In the process of liver injury and continuous onsets of hepatitis, the inflammatory factors such as CRP and TNF-α can activate a variety of immune cells, it can further enhance the inflammatory response and aggravate hepatocyte injury [18,19]. The effect of Astragalus Root on enhancing the immune function has been confirmed by modern pharmacological studies. And other studies have reported that Astragalus Root can reduce the deposition of immune complexes in the liver [20]. This study found that after treatment, the proportion of CD3+, CD4+ and CD4+/CD8+ in peripheral blood of the observation group were higher than those in the control group, while the proportion of CD8+ and the levels of serum CRP and TNF-α in the observation group were lower than those in the control group. It is suggested that the combined treatment of acupuncture and Shenqi Yigan decoction can more effectively improve the cellular immune function and reduce the inflammatory reaction in patients with HBV-induced liver fibrosis, which may be related to the immunomodulatory effect of Astragalus Root in Shenqi Yigan decoction. Modern pharmacological studies also confirmed that the main component of Astragalus Root of Astragaloside A has obvious anti-inflammatory and immunostimulatory activity [21]. Wang et al. reported that the immune function of patients was significantly improved after taking immunomodulatory traditional Chinese medicine [22].
However, the sample size of this study was limited and the follow-up time was short. The effect of this combinated treatment on patients with HBV-induced liver fibrosis is still needs to be confirmed by a large sample and multi-center clinical study. In addition, this study has not studied the specific mechanism of its treatment, which is also needs to be improved in the future study.
In conclusion, the this combinated treatment of acupuncture and Shenqi Yigan decoction can significantly improve the liver function of patients with HBV-induced liver fibrosis, delay the progress of liver fibrosis, improve the cellular immune fun Disclosure of conflict of interestction and reduce the inflammatory reaction. It is worthy of clinical promotion.
Disclosure of conflict of interest
None.
References
- 1.Seto WK, Lo YR, Pawlotsky JM, Yuen MF. Chronic hepatitis B virus infection. Lancet. 2018;392:2313–2324. doi: 10.1016/S0140-6736(18)31865-8. [DOI] [PubMed] [Google Scholar]
- 2.Xiao H, Shi M, Xie Y, Chi X. Comparison of diagnostic accuracy of magnetic resonance elastography and fibroscan for detecting liver fibrosis in chronic hepatitis b patients: a systematic review and meta-analysis. PLoS One. 2017;12:e0186660. doi: 10.1371/journal.pone.0186660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen D, Shimakawa Y, Ndow G, Sow A, Tamba S, Njie R, Lo G, Ghosh S, Toure-Kane C, Ka M, Mboup S, Okeke E, Toure S, Diop M, D’Alessandro U, Taylor-Robinson S, Mendy M, Zoulim F, Thursz MR, Lemoine M, Chemin I. Prevention of liver fibrosis and liver cancer linked to hepatitis b virus in africa: the prolifica study. Med Sci (Paris) 2019;35:431–439. doi: 10.1051/medsci/2019076. [DOI] [PubMed] [Google Scholar]
- 4.Liu X, He L, Han J, Wang L, Li M, Jiang Y, Wang X, Yang Z. Association of neutrophil-lymphocyte ratio and T lymphocytes with the pathogenesis and progression of HBV-associated primary liver cancer. PLoS One. 2017;12:e0170605. doi: 10.1371/journal.pone.0170605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Song Y, Zhao J, Wang S, Huang H, Hong J, Zuo J, Huo S. The efficacy of chinese patent medicine combined with entecavir for the treatment of chronic HBV-related liver fibrosis or cirrhosis: protocol for a systematic review and meta-analysis of randomized controlled trials or prospective cohort studies. Medicine (Baltimore) 2019;98:e15732. doi: 10.1097/MD.0000000000015732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yu S, Sun YF, Wang JJ. The effect and significance of shenqi yigan decoction on liver function and liver fibrosis indexes of patients with hepatitis b liver fibrosis before and after treatment. World Chin Med. 2019;14:2121–2124. [Google Scholar]
- 7.Lim DW, Kim H, Park JY, Kim JE, Moon JY, Park SD, Park WH. Amomum cardamomum L. Ethyl acetate fraction protects against carbon tetrachloride-induced liver injury via an antioxidant mechanism in rats. BMC Complement Altern Med. 2016;16:155. doi: 10.1186/s12906-016-1121-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang GQ, Wang FS, Cheng J, Ren H, Zhuang H, Sun J, Li LJ, Li J, Meng QH, Zhao JM. Guidelines for the prevention and treatment of chronic hepatitis B (2015 edition) Chin J Exp Clin Infect Dis. 2015;19:1–18. [Google Scholar]
- 9.Louati N, Rekik T, Menif H, Gargouri J. Blood lymphocyte T subsets reference values in blood donors by flow cytometry. Tunis Med. 2019;97:327–334. [PubMed] [Google Scholar]
- 10.Mitsuka Y, Midorikawa Y, Abe H, Matsumoto N, Moriyama M, Haradome H, Sugitani M, Tsuji S, Takayama T. A prediction model for the grade of liver fibrosis using magnetic resonance elastography. BMC Gastroenterol. 2017;17:133. doi: 10.1186/s12876-017-0700-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gracia-Sancho J, Marrone G, Fernández-Iglesias A. Liver microcirculation and mechanisms of portal hypertension. Nat Rev Gastroenterol Hepatol. 2019;16:221–234. doi: 10.1038/s41575-018-0097-3. [DOI] [PubMed] [Google Scholar]
- 12.Shen GW, Li Q. Effect of Shenqi Yigan decoction on the expression of malondialdehyde, TNF-A and matrix metalloproteinase 1 in patients with hepatitis B liver cirrhosis. Clin Res Chin Med. 2016;8:18–20. [Google Scholar]
- 13.Wang S, Zhang B, Liao M, Zhuang X, Xu Z, Huang Y, Zhuang L. Vascular cognitive impairment with no dementia treated with auricular acupuncture and acupuncture: a randomized controlled trial. Zhongguo Zhen Jiu. 2016;36:571–576. doi: 10.13703/j.0255-2930.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 14.Enomoto H, Bando Y, Nakamura H, Nishiguchi S, Koga M. Liver fibrosis markers of nonalcoholic steatohepatitis. World J Gastroenterol. 2015;21:7427–7435. doi: 10.3748/wjg.v21.i24.7427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang D, Lin T, Wang S, Cheng L, Xie L, Lu Y, Chen M, Zhu L, Shi J. The liver fibrosis index is superior to the APRI and FIB-4 for predicting liver fibrosis in chronic hepatitis B patients in China. BMC Infect Dis. 2019;19:878. doi: 10.1186/s12879-019-4459-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou J, Liang Y, Lin XM, Ma RJ, Fang JQ. Acupuncture in treating liver fibrosis: a review with recommendation for future studies. Afr J Tradit Complement Altern Med. 2012;9:452–458. doi: 10.4314/ajtcam.v9i4.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tsai S, Clemente-Casares X, Zhou AC, Lei H, Ahn JJ, Chan YT, Choi O, Luck H, Woo M, Dunn SE, Engleman EG, Watts TH, Winer S, Winer DA. Insulin receptor-mediated stimulation boosts T cell immunity during inflammation and infection. Cell Metab. 2018;28:922–934. e924. doi: 10.1016/j.cmet.2018.08.003. [DOI] [PubMed] [Google Scholar]
- 18.Robinson MW, Harmon C, O’Farrelly C. Liver immunology and its role in inflammation and homeostasis. Cell Mol Immunol. 2016;13:267–276. doi: 10.1038/cmi.2016.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jiménez-Castro MB, Cornide-Petronio ME, Gracia-Sancho J, Peralta C. Inflammasome-mediated inflammation in liver ischemia-reperfusion injury. Cells. 2019;8:1131. doi: 10.3390/cells8101131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hong HD, Kim JC, Lim TG, Song YR, Cho CW, Jang M. Mixing ratio optimization for functional complex extracts of rhodiola crenulata, panax quinquefolius, and astragalus membranaceus using mixture design and verification of immune functional efficacy in animal models. J Funct Foods. 2018;40:447–454. doi: 10.1016/j.jff.2017.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Qi Y, Gao F, Hou L, Wan C. Anti-inflammatory and immunostimulatory activities of astragalosides. Am J Chin Med. 2017;45:1157–1167. doi: 10.1142/S0192415X1750063X. [DOI] [PubMed] [Google Scholar]
- 22.Wang Z, Cao D, Li C, Min L, Wang G. Mediator MED23 regulates inflammatory responses and liver fibrosis. PLoS Biol. 2019;17:e3000563. doi: 10.1371/journal.pbio.3000563. [DOI] [PMC free article] [PubMed] [Google Scholar]


