Abstract
Alcohol use is a major risk factor for burden of mortality and morbidity. Alcoholic liver disease (ALD) and alcohol use disorders (AUDs) are important disease outcomes caused by alcohol use. We will describe the global mortality and burden of disease in disability-adjusted life years for ALD and AUDs, based on data from the comparative risk assessment of the World Health Organization for 2016. AUDs have a limited impact on mortality in this assessment, since alcohol poisonings are almost the only disease category directly attributable to AUDs; most other alcohol-related deaths are indirect, and the cause which directly led to the death, such as liver cirrhosis, is the one recorded on the death certificate. Burden of disease for AUDs is thus mainly due to disability resulting from alcohol use. In contrast to AUDs, ALD is one of the major lethal outcomes of alcohol use, and burden of disease is mainly due to (premature) years of life lost. Many of the negative outcomes attributable to both AUDs and ALD are due to their interactions with other factors, most notably economic wealth. To avoid alcohol-attributable morbidity and mortality, measures should be taken to reduce the AUDs and ALD burden globally, especially among the poor.
Keywords: alcohol, burden of disease, mortality, alcohol use disorders, alcoholic liver disease, poverty, disability-adjusted life years, interaction
1. Introduction
Alcohol use is a major risk factor for mortality and morbidity, playing a role in more than 200 diseases and injury outcomes [1,2]. However, for most regions, it can be shown that a few of the larger disease and injury categories capture more than 90% of alcohol-attributable mortality and burden of disease (the latter usually measured in disability-adjusted life-years DALYs [3]), namely alcohol use disorders (AUDs), cancer, cardiovascular disease, liver disease, and injury [4,5]. This contribution will focus on two of these major contributors to alcohol-attributable burden of disease: AUDs and alcoholic liver disease (ALD). Contrary to the other major contributors of alcohol-attributable disease, these two categories are fully alcohol attributable: there would be neither AUDs nor ALD without alcohol use [1]. Together, these two categories make up about a quarter of all alcohol-attributable mortality (26.3%) and one-third of alcohol-attributable burden of disease as measured in DALYs (31.5%; data based on [4]).
AUDs rank among the most prevalent mental disorders globally [6]. Individuals with an AUD have impaired control over their alcohol consumption and exhibit a chronic, heavy, and often escalating pattern of alcohol use despite significant detrimental consequences to their overall health, the lives of their family members and friends, and to society in general [7]; for definitions see DSM-5 [8], ICD-10 [9], or ICD-11 [10]. AUDs are very closely associated with a pattern of heavy alcohol use over time, and it has been suggested that this specific type of drinking behaviour should be part of the definition of AUDs [11,12,13].
ALD (for a definition and short overview see [14]) is the most prevalent type of chronic liver disease worldwide [15]. The International Classification of Diseases (ICD-10) recognizes several forms of ALD [14,16,17], which are usually considered as stages, that range from relatively mild and reversible alcoholic hepatic steatosis (fatty liver) and alcoholic hepatitis, to alcoholic fibrosis and sclerosis of the liver, and further to severe and irreversible stages, such as alcoholic liver cirrhosis and alcoholic hepatic failure (for a brief summary of the pathogenesis, see [18,19,20]). In some classifications, alcohol-attributable liver cancers have been listed as part of ALD as well [20,21], but we will not include this category in our calculations. Alcohol use and liver disease have an exponentially increasing dose-response relationship [22,23]. An additional impact may result from a daily heavy drinking pattern with some studies showing that the same overall amount of alcohol intake but with a non-daily drinking pattern is associated with less harm (“liver holidays” [24,25]).
AUDs and ALD are associated due to their shared etiology—alcohol use. A recent analysis of all French hospital patients between 2008 and 2012 showed that women with AUDs had 13 to 20-fold elevated risks for liver diseases (for liver cirrhosis: Hazard Ratio (HR): 19.3; 95% Confidence interval (CI): 19.1–19.5; for liver cancer: HR: 13.2; 95% CI: 12.8–13.7), and men with AUDs had 16-fold higher risks for liver cirrhosis (HR: 16.0; 95% CI: 15.9–16.1) and liver cancer (HR: 16.1; 95% CI: 15.9–16.4; [26]).
2. Materials and Methods
2.1. Definitions of Outcomes
For prevalence, we defined AUDs as being composed of alcohol dependence and harmful use of alcohol (ICD-10 [27]; or as alcohol use disorders as defined in the DSM–see above). For AUDs-attributable burden of mortality and disease, as per the usual standard of both the Global Burden of Disease study and the WHO, the following conditions were included, most notably fetal alcohol syndrome and alcohol poisoning: F10–F10.9, G31.2, G72.1, P04.3, Q86.0, R78.0, X45–X45.9, X65–X65.9, Y15–Y15.9 (GBD and WHO [4,28,29].
ALD is defined as being composed of the alcohol-attributable portion of the following ICD-10 codes: B18–B18.9, I85–I85.9, I98.2, K70–K70.9, K71.3–K71.51, K71.7, K72.1–K74.69, K74.9, K75.8–K76.0, K76.6–K76.7, K76.9 (again as per the standard definition of both the Global Burden of Disease study and the WHO [4,28,29]). The designation of “alcohol-attributable” was defined as a counterfactual to a scenario in which no alcohol was involved: in other words, all causes of death and disease with one of the above-noted ICD codes were defined as ALD if they occurred in a situation where alcohol use had been involved [30,31]. Similar definitions have been used before [15,32].
2.2. Data Sources
For both prevalence and attributable burden, we relied on data from the WHO Global Status Report on Alcohol and Health [4], as slightly updated by Shield and colleagues [5]. As both authors undertook the burden calculations and were authors for the Global Status Report and subsequent publications, we report not only previously published data, but also our own calculations based on the underlying data.
3. Results
3.1. Alcohol Use Disorders
Before we report on AUDs, we would like to provide some background numbers on alcohol use for the year 2016, as the prevalence of alcohol use—in particular, heavy use—and AUDs is highly correlated [4]. In 2016, more than half (57%, or 3.1 billion people) of the global population aged 15 years and older had not drunk alcohol in the previous 12 months, while some 2.3 billion people in this age group were current drinkers. Alcohol is consumed by more than half of the population in the Americas, Europe, and in the Western Pacific region, which includes China [4]. Worldwide, alcohol use has increased over the past three decades, and is expected to continue to do so, both in its prevalence and level of use [33].
AUDs are among the most prevalent mental disorders globally, affecting 8.6% (95% CI: 8.1–9.1%) of men and 1.7% (95% CI: 1.6–1.9%) of women in 2016 (total prevalence 5.1%; 95% CI: 4.9–5.4%; see [4,6,7] for details). Although the prevalence of AUDs in men is still about five times greater than in women, in some countries—such as the US—there are signs that this gender gap is narrowing over time [34]. The prevalence of AUDs was highest in high-income countries (8.4%, 95% CI 8.0–8.9%) and upper-middle-income countries (5.4%, 95% CI 5.0–6.0%; for details on the country level, see Figure 1).
Figure 1.
Prevalence (in %) of alcohol use disorders in adults (15 years and older) in 2016. Based on [4].
By definition, all health harms caused by AUDs were initially caused by alcohol use. In those aged 15 years or older, these harms amounted to about 145,000 AUDs deaths in 2016 (145,600; no 95% CI is available as the Global Health Estimates do not estimate CIs for cause of death or disease burden; [5,35]). A significant gender disparity exists for AUDs, due to the higher level and more detrimental patterns of drinking in men. For men, 121,600 AUDs deaths were reported while for women, a total of 24,000 was recorded.
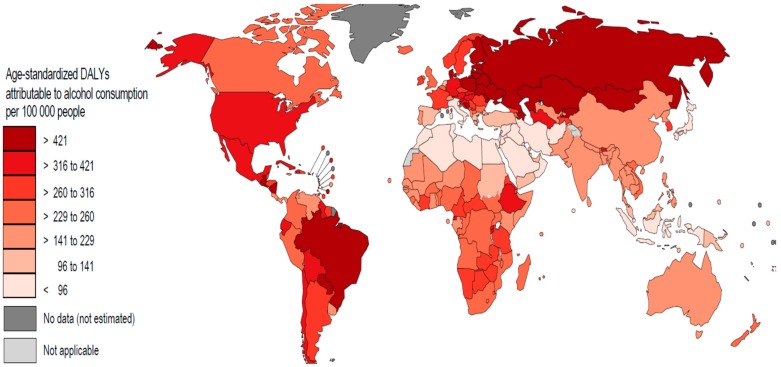
Burden of disease figures for AUDs were proportionally higher than those for mortality. In 2016, about 21.5 million years of life were lost due to ALD (21,455,000 DALYs). Once again, men were markedly more affected than women (men: 16,614,000 DALYs; women: 4,841,000 DALYs). The majority of these years of life lost were due to disability rather than to early death. Figure 2 shows the regional distribution.
Figure 2.
Age-standardized burden of disease (DALYs) of alcohol use disorders per 100,000 people in 2016. Based on [5].
3.2. Alcoholic Liver Disease
Alcohol consumption caused almost half of the deaths attributed to chronic liver disease [5,36]. In the age group of 15 years and up, nearly 50% of the 1,254,000 liver disease deaths in 2016 were estimated to be alcohol-attributable (588,100; 95% CI: 531,700–683,400; 46.9% of all liver disease, 95% CI: 42.4–54.5%) [5]. This proportion is similar to previous estimates [15,32]. By gender, significantly more alcohol-attributable liver deaths were reported in men (416,700, 95% CI: 379,900–514,800) than in women (171,400, 95% CI: 134,500–189,700).
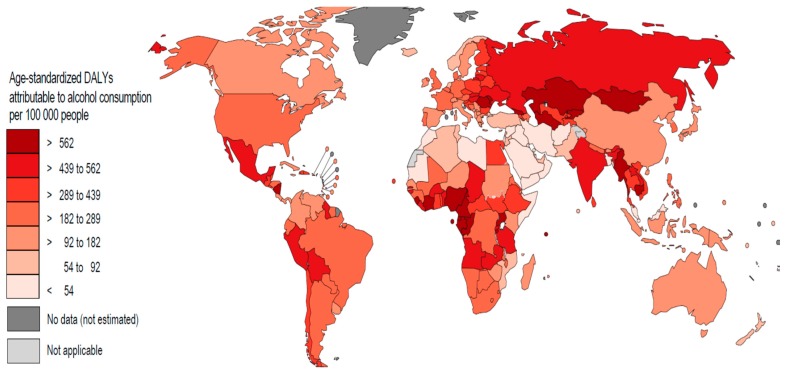
Burden of disease figures are similarly high. In 2016, about 21.5 million years of life were lost due to ALD (21,476,000 DALYs; 95% CI: 19,448,000–24,811,000); again, men were markedly more affected than women (men: 15,568,000 DALYs; 95% CI: 14,230,000–19,125,000; women: 5,909,000 DALYs; 95% CI: 4,653,000–6,423,000). The overwhelming majority of these years of life lost were due to premature deaths rather than disability.
The map in Figure 3 below shows age-standardized DALY rates per 100,000 for ALD for each WHO Member State. As expected, the lowest rates reported are seen in Southeast Asia and the Middle East, in the belt of the Muslim countries. The highest rates are found in Eastern European, West African, and Central Asian countries; the latter are relatively high in world rankings of alcohol consumption but are not necessarily among the top 20 [33].
Figure 3.
Age-standardized burden of disease (DALYs) attributable to alcohol use per 100,000 people in 2016). Based on [5].
A possible explanation for this would be that in these countries liver diseases are generally more prevalent—and are not necessarily caused by alcohol consumption, but rather by hepatitis B [37] and hepatitis C [38]. In those with existing liver disease, even a relatively small amount of alcohol can lead to serious complications or even be lethal, as shown in the significantly more exponential dose-response relationships for mortality compared to morbidity [22]. The role of alcohol use in the progression of hepatitis C was investigated in the earlier-mentioned representative cohort study of 97,347 French patients (see [26] above) with hepatitis C (the majority of the data was collected before the introduction of new methods to cure hepatitis C were available): the majority of liver complications, defined as either decompensated cirrhosis, primary liver cancer, liver transplants or liver deaths was alcohol-attributable ([39]; see also [40,41]).
Worldwide, chronic liver disease has increased significantly in overall mortality rates in the past decade (since 2010), both in terms of absolute deaths and in its ranking among major causes of death [42]. Because the alcohol-attributable share of these deaths has increased in tandem with the overall increase in chronic liver disease mortality (own calculations based on WHO, 2018), the increasing importance—from a health policy perspective—of liver disease applies especially to ALD.
4. Discussion
AUDs and ALD have both contributed markedly to alcohol-attributable burden of disease, with the higher contributor being ALD, especially with respect to mortality. To interpret these results, the following points and limitations should be considered:
The definition of AUDs, and its operationalization, are both controversial, as each is based on relatively unspecific criteria (e.g., [43]), is culture-specific, and can therefore not be easily compared [44,45]. They do not necessarily coincide perfectly with heavy drinking levels and can therefore not be linked to harm [11,12] or with biological research [7,13]. While alternatives do exist to estimate AUDs [46], these are not commonly used and we therefore did not use them.
The reported deaths resulting from AUDs only include deaths where either AUDs or alcohol poisoning was listed as the cause of death on the death certificate (see above). Similar to other mental disorders, addictive disorders such as AUDs have been associated with considerable excess mortality [47,48,49,50], even though most of these disorders do not appear in large numbers in cause-of-death statistics. The underlying cause of death in the WHO Global Health Estimates [42] is defined as the disease or injury that initiated the train of morbid events which led directly to the death, or the circumstances of the accident or violence that produced the injury. For AUDs, the cause of death would therefore be attributed to injuries such as suicides, or other chronic disorders such as ischemic heart disease or ALD [1,50,51]. However, to avoid double counting, these deaths are not counted as AUDs mortality.
The last limitation of the estimation of AUDs prevalence and harm in this study is the reliance on the Global Health Estimates, which do not provide confidence intervals [35]. There is obviously uncertainty inherent in the estimates of AUDs and attributable harm which we could not capture.
The burden for ALD is clearly larger than for AUDs in terms of DALYs and particularly for mortality (but see previous point). ALD is the single most important health harm caused by alcohol use [4,5]. The estimation methodology used is consistent with the definition of ALD (i.e., without alcohol use, these cases of ALD deaths or disease would not have existed). However, in contrast to other causes of death, ALD deaths were not estimated based on death certificates (in the countries where such certificates exist), or based on specific verbal autopsies [52,53], but were indirectly estimated via attributable fractions (see Materials and Methods above). The reason for this is the high stigmatization of all disorders which have the terms ‘alcohol’ or ‘alcoholic’ in their names (for general considerations, see [54]). Alcohol’s involvement in a death may be missed by those certifying or reporting the death (the latter in verbal autopsies), or may be deliberately not mentioned to protect the reputation of the deceased (see [55], for further conclusions). A landmark study of death recording practices in 12 cities in 10 countries found that the number of deaths assigned to the ICD category ‘liver cirrhosis with mention of alcoholism’ rose by 135% after taking into account additional information obtained from hospital records and interviews with attending physicians and family members. The majority of the new cases were previously coded in categories like cirrhosis without any mention of alcohol [56]. Underestimation of ALD and other 100% alcohol-attributable disease categories has persisted to this day (e.g., [57]; see short overview of a recent study in [58]).
Finally, while there was uncertainty reported around the ALD estimates, it may be underestimated as it did not include any uncertainty for the cause of death or burden of disease (i.e., only for exposure and risk relations) [59].
Overall, AUDs and ALD have been shown to have a profound impact on the global burden of disease. Both disease categories are particularly tightly linked to heavy drinking occasions. In North America, both disease conditions have been contributing to decreasing life expectancies, especially in lower socioeconomic strata (US: [60,61,62]; Canada: [63,64,65,66]). For this region, disorders attributable to heavy alcohol consumption can, in effect, be used as an indicator for major increases in disease burden.
5. Conclusions
Policies to reduce the above-described burden of alcohol-attributable disease should be initiated [67]. While effective and cost-effective policies already do exist to reduce alcohol-attributable burden [67,68,69], two additional considerations should be focused on: first, each measure must be examined to ensure it does not widen the gap between socioeconomic strata and, second, the measures should target heavy drinking occasions. Thus, in addition to the raising taxes on alcohol, restricting its availability, and banning its advertisement, the current “best buys” for alcohol control—measures such as minimum pricing per unit—should be considered, as they have shown to have a strong effect on the drinking behaviour of heavy drinkers in lower socioeconomic strata [70].
Acknowledgments
This contribution is based on validated data for alcohol exposure up to and including 2016, as carried out by the WHO Headquarters and the WHO regional offices. We would like to than Astrid Otto for referencing and copy-editing.
Author Contributions
Both authors contributed equally to conceptualization, methodology, formal analysis, investigation, data curation, writing, and visualization.
Funding
This research was in part funded by the contributions of the World Health Organization to the WHO Collaborating Centre, and by from the Canadian Institutes of Health Research (CIHR) for the Ontario CRISM Node Team grant (#SMN-139150).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Rehm J., Gmel Sr G.E., Gmel G., Hasan O.S., Imtiaz S., Popova S., Probst C., Roerecke M., Room R., Samokhvalov A.V. The relationship between different dimensions of alcohol use and the burden of disease—An update. Addiction. 2017;112:968–1001. doi: 10.1111/add.13757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rehm J., Imtiaz S. A narrative review of alcohol consumption as a risk factor for global burden of disease. Subst. Abus. Treat. Prev. Policy. 2016;11:37. doi: 10.1186/s13011-016-0081-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murray C.J.L. Quantifying the burden of disease: The technical basis for disability-adjusted life years. Bull. World Health Organ. 1994;72:429–445. [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization Global Status Report on Alcohol and Health 2018. [(accessed on 28 October 2019)]; Available online: https://www.who.int/substance_abuse/publications/global_alcohol_report/en/
- 5.Shield K.D., Manthey J., Rylett M., Probst C., Wettlaufer A., Rehm J. National, Regional, and Global Burdens of Disease from 2000 to 2016 Attributable to Alcohol Use. Lancet Public Health. doi: 10.1016/S2468-2667(19)30231-2. (in press) [DOI] [PubMed] [Google Scholar]
- 6.Rehm J., Shield K.D. Global Burden of Disease and the Impact of Mental and Addictive Disorders. Curr. Psychiatry Rep. 2019;21:10. doi: 10.1007/s11920-019-0997-0. [DOI] [PubMed] [Google Scholar]
- 7.Carvalho A.F., Heilig M., Perez A., Probst C., Rehm J. Alcohol use disorders. Lancet. 2019;394:781–792. doi: 10.1016/S0140-6736(19)31775-1. [DOI] [PubMed] [Google Scholar]
- 8.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; Philadelphia, PA, USA: 2013. [Google Scholar]
- 9.World Health Organization The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. F10–F19 Mental and Behavioural Disorders due to Psychoactive Substance Use. [(accessed on 27 November 2019)]; Available online: https://www.who.int/substance_abuse/terminology/ICD10ClinicalDiagnosis.pdf.
- 10.World Health Organization ICD-11 for Mortality and Morbidity Statistics. [(accessed on 27 November 2019)]; Available online: https://icd.who.int/browse11/l-m/en.
- 11.Rehm J., Marmet S., Anderson P., Gual A., Kraus L., Nutt D.J., Room R., Samokhvalov A.V., Scafato E., Trapencieris M. Defining substance use disorders: Do we really need more than heavy use? Alcohol Alcohol. 2013;48:633–640. doi: 10.1093/alcalc/agt127. [DOI] [PubMed] [Google Scholar]
- 12.Rehm J., Anderson P., Gual A., Kraus L., Marmet S., Nutt D.J., Room R., Samokhvalov A.V., Scafato E., Shield K.D., et al. The tangible common denominator of substance use disorders: A reply to commentaries to Rehm et al. (2013a) Alcohol Alcohol. 2014;49:118–122. doi: 10.1093/alcalc/agt171. [DOI] [PubMed] [Google Scholar]
- 13.Rehm J., Heilig M., Gual A. ICD-11 for Alcohol Use Disorders: Not a Convincing Answer to the Challenges. Alcohol. Clin. Exp. Res. 2019;43 doi: 10.1111/acer.14182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seitz H.K., Bataller R., Cortez-Pinto H., Gao B., Gual A., Lackner C., Mathurin P., Mueller S., Szabo G., Tsukamoto H. Alcoholic liver disease. Nat. Rev. Dis. Primers. 2018;4:16. doi: 10.1038/s41572-018-0014-7. [DOI] [PubMed] [Google Scholar]
- 15.Rehm J., Samokhvalov A.V., Shield K.D. Global burden of alcoholic liver diseases. J. Hepatol. 2013;59:160–168. doi: 10.1016/j.jhep.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 16.O’Shea R.S., Dasarathy S., McCullough A.J., Practice Guideline Committee of the American Association for the Study of Liver Diseases. Practice Parameters Committee of the American College of Gastroenterology Alcoholic liver disease. Hepatology. 2010;51:307–328. doi: 10.1002/hep.23258. [DOI] [PubMed] [Google Scholar]
- 17.European Association for the Study of the Liver EASL Clinical Practice Guidelines: Management of alcohol-related liver disease. J. Hepatol. 2018;69:154–181. doi: 10.1016/j.jhep.2018.03.018. [DOI] [PubMed] [Google Scholar]
- 18.European Association for the Study of L. EASL clinical practical guidelines: Management of alcoholic liver disease. J. Hepatol. 2012;57:399–420. doi: 10.1016/j.jhep.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 19.Teschke R. Alcoholic Liver Disease: Alcohol Metabolism, Cascade of Molecular Mechanisms, Cellular Targets, and Clinical Aspects. Biomedicines. 2018;6:106. doi: 10.3390/biomedicines6040106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Teschke R. Alcoholic Liver Disease: Current Mechanistic Aspects with Focus on Their Clinical Relevance. Biomedicines. 2019;7:68. doi: 10.3390/biomedicines7030068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Teschke R. Hepatocellular carcinoma in alcoholic liver disease: Mechanistic considerations and clinical facts. Hepatoma. Res. 2019;5:40. doi: 10.20517/2394-5079.2019.0017. [DOI] [Google Scholar]
- 22.Rehm J., Taylor B., Mohapatra S., Irving H., Baliunas D., Patra J., Roerecke M. Alcohol as a risk factor for liver cirrhosis: A systematic review and meta-analysis. Drug Alcohol. Rev. 2010;29:437–445. doi: 10.1111/j.1465-3362.2009.00153.x. [DOI] [PubMed] [Google Scholar]
- 23.Roerecke M., Vafaei A., Hasan O.S.M., Chrystoja B.R., Cruz M., Lee R., Neuman M.G., Rehm J. Alcohol Consumption and Risk of Liver Cirrhosis: A Systematic Review and Meta-Analysis. Am. J. Gastroenterol. 2019;114:1574–1586. doi: 10.14309/ajg.0000000000000340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rehm J., Roerecke M. Patterns of drinking and liver cirrhosis-what do we know and where do we go? J. Hepatol. 2015;62:1000–1001. doi: 10.1016/j.jhep.2015.01.027. [DOI] [PubMed] [Google Scholar]
- 25.Marugame T., Yamamoto S., Yoshimi I., Sobue T., Inoue M., Tsugane S., Japan Public Health Center-based Prospective Study G. Patterns of alcohol drinking and all-cause mortality: Results from a large-scale population-based cohort study in Japan. Am. J. Epidemiol. 2007;165:1039–1046. doi: 10.1093/aje/kwk112. [DOI] [PubMed] [Google Scholar]
- 26.Schwarzinger M., Thiebaut S.P., Baillot S., Mallet V., Rehm J. Alcohol use disorders and associated chronic disease-a national retrospective cohort study from France. BMC Public Health. 2017;18:43. doi: 10.1186/s12889-017-4587-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization ICD-10 Version: 2016. [(accessed on 28 October 2019)]; Available online: https://icd.who.int/browse10/2016/en.
- 28.GBD 2017 Risk Factors Collaborators Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1923–1994. doi: 10.1016/S0140-6736(18)32225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Institute of Health Metrics and Evaluation (GHDx) Global Burden of Disease Study 2015 (GBD 2015) Life Expectancy, All-Cause and Cause-Specific Mortality 1980–2015. [(accessed on 28 October 2019)]; Available online: http://ghdx.healthdata.org/record/ihme-data/gbd-2017-cause-icd-code-mappings.
- 30.Murray C.J., Lopez A.D. On the comparable quantification of health risks: Lessons from the Global Burden of Disease Study. Epidemiology. 1999;10:594–605. doi: 10.1097/00001648-199909000-00029. [DOI] [PubMed] [Google Scholar]
- 31.Rehm J., Monteiro M., Room R., Gmel G., Jernigan D., Frick U., Graham K. Steps towards constructing a global comparative risk analysis for alcohol consumption: Determining indicators and empirical weights for patterns of drinking, deciding about theoretical minimum, and dealing with different consequences. Eur. Addict. Res. 2001;7:138–147. doi: 10.1159/000050731. [DOI] [PubMed] [Google Scholar]
- 32.Lopez A.D., Williams T.N., Levin A., Tonelli M., Singh J.A., Burney P.G., Rehm J., Volkow N.D., Koob G., Ferri C.P. Remembering the forgotten non-communicable diseases. BMC Med. 2014;12:200. doi: 10.1186/s12916-014-0200-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Manthey J., Shield K.D., Rylett M., Hasan O.S.M., Probst C., Rehm J. Global alcohol exposure between 1990 and 2017 and forecasts until 2030: A modelling study. Lancet. 2019;393:2493–2502. doi: 10.1016/S0140-6736(18)32744-2. [DOI] [PubMed] [Google Scholar]
- 34.Grant B.F., Chou S.P., Saha T.D., Pickering R.P., Kerridge B.T., Ruan W.J., Huang B., Jung J., Zhang H., Fan A., et al. Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001-2002 to 2012-2013: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74:911–923. doi: 10.1001/jamapsychiatry.2017.2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.World Health Organization Global Health Estimates (GHE) [(accessed on 28 October 2019)]; Available online: https://www.who.int/healthinfo/global_burden_disease/en/
- 36.Rehm J., Shield K.D., Frick U. Epidemiologie alkoholischer Lebererkrankungen. In: Seitz S.M.H.K., editor. Alkoholische Leber- und Krebserkrankungen. De Gruyter.; Berlin, Germany: 2019. pp. 25–40. [Google Scholar]
- 37.World Health Organization Fact Sheet: Hepatitis B. [(accessed on 28 October 2019)]; Available online: https://www.who.int/news-room/fact-sheets/detail/hepatitis-b.
- 38.Messina J.P., Humphreys I., Flaxman A., Brown A., Cooke G.S., Pybus O.G., Barnes E. Global distribution and prevalence of hepatitis C virus genotypes. Hepatology. 2015;61:77–87. doi: 10.1002/hep.27259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schwarzinger M., Baillot S., Yazdanpanah Y., Rehm J., Mallet V. Alcohol use disorders and the burden of chronic hepatitis C in France, 2008-2013: A nationwide retrospective cohort study. J. Hepatol. 2017;67:454–461. doi: 10.1016/j.jhep.2017.03.031. [DOI] [PubMed] [Google Scholar]
- 40.Alavi M., Janjua N.Z., Chong M., Grebely J., Aspinall E.J., Innes H., Valerio H.M., Hajarizadeh B., Hayes P.C., Krajden M., et al. The contribution of alcohol use disorder to decompensated cirrhosis among people with hepatitis C: An international study. J. Hepatol. 2018;68:393–401. doi: 10.1016/j.jhep.2017.10.019. [DOI] [PubMed] [Google Scholar]
- 41.Schwarzinger M., Rehm J., Mallet V. “Who killed JR”: Chronic hepatitis C or alcohol use disorders? J. Hepatol. 2018;68:1098–1099. doi: 10.1016/j.jhep.2017.11.042. [DOI] [PubMed] [Google Scholar]
- 42.World Health Organization Disease Burden and Mortality Estimates: Cause-Specific Mortality. [(accessed on 28 October 2019)];2000–2016 Available online: http://www.who.int/healthinfo/global_burden_disease/estimates/en/
- 43.Martin C.S., Langenbucher J.W., Chung T., Sher K.J. Truth or consequences in the diagnosis of substance use disorders. Addiction. 2014;109:1773–1778. doi: 10.1111/add.12615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rehm J., Room R. Cultural specificity in alcohol use disorders. Lancet. 2015 doi: 10.1016/S0140-6736(15)00123-3. [DOI] [PubMed] [Google Scholar]
- 45.Rehm J., Room R. The cultural aspect: How to measure and interpret epidemiological data on alcohol-use disorders across cultures. Nord. Stud. Alcohol Drugs. 2017;34:330–341. doi: 10.1177/1455072517704795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rehm J. How should prevalence of alcohol use disorders be assessed globally? Int. J. Methods Psychiatr. Res. 2016;25:79–85. doi: 10.1002/mpr.1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Charlson F.J., Baxter A.J., Dua T., Degenhardt L., Whiteford H.A., Vos T. Excess Mortality from Mental, Neurological, and Substance Use Disorders in the Global Burden of Disease Study 2010. In: Patel V., Dua T., Laxminarayan R., Medina-Mora M.E., editors. Mental, Neurological, and Substance Use Disorders, Disease Control Priorities. Volume 4. The International Bank for Reconstruction and Development/The World Bank; Washington, DC, USA: 2016. pp. 41–65. [PubMed] [Google Scholar]
- 48.Rehm J., Dawson D., Frick U., Gmel G., Roerecke M., Shield K.D., Grant B. Burden of disease associated with alcohol use disorders in the United States. Alcohol Clin. Exp. Res. 2014;38:1068–1077. doi: 10.1111/acer.12331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Roerecke M., Rehm J. Alcohol use disorders and mortality: A systematic review and meta-analysis. Addiction. 2013;108:1562–1578. doi: 10.1111/add.12231. [DOI] [PubMed] [Google Scholar]
- 50.Harris E.C., Barraclough B. Excess mortality of mental disorder. Br. J. Psychiatry. 1998;173:11–53. doi: 10.1192/bjp.173.1.11. [DOI] [PubMed] [Google Scholar]
- 51.Roerecke M., Rehm J. Cause-specific mortality risk in alcohol use disorder treatment patients: A systematic review and meta-analysis. Int. J. Epidemiol. 2014;43:906–919. doi: 10.1093/ije/dyu018. [DOI] [PubMed] [Google Scholar]
- 52.Soleman N., Chandramohan D., Shibuya K. Verbal autopsy: Current practices and challenges. Bull. World Health Organ. 2006;84:239–245. doi: 10.2471/BLT.05.027003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Thomas L.M., D’Ambruoso L., Balabanova D. Verbal autopsy in health policy and systems: A literature review. BMJ Glob. Health. 2018;3:e000639. doi: 10.1136/bmjgh-2017-000639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schomerus G., Lucht M., Holzinger A., Matschinger H., Carta M.G., Angermeyer M.C. The stigma of alcohol dependence compared with other mental disorders: A review of population studies. Alcohol Alcohol. 2011;46:105–112. doi: 10.1093/alcalc/agq089. [DOI] [PubMed] [Google Scholar]
- 55.Lange S., Roerecke M., Rehm J. For most fully alcohol-attributable diagnoses in the ICD, the etiological specification should be removed. Adicciones. doi: 10.20882/adicciones.1376. (in press) [DOI] [PubMed] [Google Scholar]
- 56.Puffer R.R., Griffith G.W. Patterns of Urban Mortality: Report of the Inter-American Investigation of Mortality. Pan American Health Organization; Washington, DC, USA: 1967. [Google Scholar]
- 57.Tuusov J., Lang K., Vali M., Parna K., Tonisson M., Ringmets I., McKee M., Helander A., Leon D.A. Prevalence of alcohol-related pathologies at autopsy: Estonian Forensic Study of Alcohol and Premature Death. Addiction. 2014;109:2018–2026. doi: 10.1111/add.12695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rehm J., Hasan O.S.M., Imtiaz S., Neufeld M. Quantifying the contribution of alcohol to cardiomyopathy: A systematic review. Alcohol. 2017;61:9–15. doi: 10.1016/j.alcohol.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 59.Gmel G., Shield K.D., Frick H., Kehoe T., Gmel G., Rehm J. Estimating uncertainty of alcohol-attributable fractions for infectious and chronic diseases. BMC Med. Res. Methodol. 2011;11:48. doi: 10.1186/1471-2288-11-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Case A., Deaton A. Mortality and morbidity in the 21(st) century. Brook. Pap. Econ. Act. 2017;2017:397–476. doi: 10.1353/eca.2017.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rehm J., Probst C. Decreases of Life Expectancy Despite Decreases in Non-Communicable Disease Mortality: The Role of Substance Use and Socioeconomic Status. Eur. Addict. Res. 2018;24:53–59. doi: 10.1159/000488328. [DOI] [PubMed] [Google Scholar]
- 62.Woolf S.H., Schoomaker H. Life Expectancy and Mortality Rates in the United States, 1959-2017. JAMA. 2019;322:1996–2016. doi: 10.1001/jama.2019.16932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Statistics Canada The Daily: Changes in Life Expectancy by Selected Causes of Death. [(accessed on 29 October 2019)];2017 Available online: https://www150.statcan.gc.ca/n1/en/daily-quotidien/190530/dq190530d-eng.pdf?st=21plbOYt.
- 64.Probst C., Rehm J. Alcohol use, opioid overdose and socioeconomic status in Canada: A threat to life expectancy? CMAJ. 2018;190:E1294–E1295. doi: 10.1503/cmaj.180806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tjepkema M., Wilkins R., Long A. Cause-specific mortality by income adequacy in Canada: A 16-year follow-up study. Health Rep. 2013;24:14–22. [PubMed] [Google Scholar]
- 66.Alcohol Harm in Canada: Examining Hospitalizations Entirely Caused by Alcohol and Strategies to Reduce Alcohol Harm. [(accessed on 22 June 2017)]; Available online: https://secure.cihi.ca/estore/productFamily.htm?pf=PFC3445&lang=fr&media=
- 67.Babor T.F., Caetano R., Casswell S., Edwards G., Giesbrecht N., Graham K., Grube J., Gruenewald P., Hill L., Holder H., et al. Alcohol: No Ordinary Commodity. Research and Public Policy. 2nd ed. Oxford University Press; London, UK: 2010. [Google Scholar]
- 68.Chisholm D., Moro D., Bertram M., Pretorius C., Gmel G., Shield K., Rehm J. Are the “Best Buys” for Alcohol Control Still Valid? An Update on the Comparative Cost-Effectiveness of Alcohol Control Strategies at the Global Level. J. Stud. Alcohol Drugs. 2018;79:514–522. doi: 10.15288/jsad.2018.79.514. [DOI] [PubMed] [Google Scholar]
- 69.Anderson P., Chisholm D., Fuhr D.C. Effectiveness and cost-effectiveness of policies and programmes to reduce the harm caused by alcohol. Lancet. 2009;373:2234–2246. doi: 10.1016/S0140-6736(09)60744-3. [DOI] [PubMed] [Google Scholar]
- 70.O’Donnell A., Anderson P., Jane-Llopis E., Manthey J., Kaner E., Rehm J. Immediate impact of minimum unit pricing on alcohol purchases in Scotland: Controlled interrupted time series analysis for 2015-18. BMJ. 2019;366:l5274. doi: 10.1136/bmj.l5274. [DOI] [PMC free article] [PubMed] [Google Scholar]