Abstract
We systematically reviewed reports about determinants of HIV infection in injecting drug users from 2000 to 2009, classifying findings by type of environmental influence. We then modelled changes in risk environments in regions with severe HIV epidemics associated with injecting drug use. Of 94 studies identified, 25 intentionally examined risk environments. Modelling of HIV epidemics showed substantial heterogeneity in the number of HIV infections that are attributed to injecting drug use and unprotected sex. We estimate that, during 2010–15, HIV prevalence could be reduced by 41% in Odessa (Ukraine), 43% in Karachi (Pakistan), and 30% in Nairobi (Kenya) through a 60% reduction of the unmet need of programmes for opioid substitution, needle exchange, and antiretroviral therapy. Mitigation of patient transition to injecting drugs from non-injecting forms could avert a 98% increase in HIV infections in Karachi; whereas elimination of laws prohibiting opioid substitution with concomitant scale-up could prevent 14% of HIV infections in Nairobi. Optimisation of effectiveness and coverage of interventions is crucial for regions with rapidly growing epidemics. Delineation of environmental risk factors provides a crucial insight into HIV prevention. Evidence-informed, rights-based, combination interventions protecting IDUs’ access to HIV prevention and treatment could substantially curtail HIV epidemics.
Introduction
The estimated number of injecting drug users (IDUs) worldwide was 15.9 million (range 11.0–21.2 million) in 2007,1 of whom around 3 million were infected with HIV. HIV infection was reported in 120 (81%) of the 148 countries in which use of injecting drugs was documented. HIV prevalence in IDUs was 20–40% in five countries and more than 40% in nine.1 Extreme heterogeneity in HIV epidemics between, and sometimes within, countries, and the tendency for rapid HIV transmission between IDUs have been hallmarks of HIV epidemics associated with IDUs since the pandemic began.
Since sharing of syringes by IDUs was identified as a risk factor for HIV infection nearly 25 years ago, investigators have concentrated on circumstances in which sharing occurs (ie, who injects with syringes previously used by whom, the reasons for sharing, and locations where sharing takes place). Efforts have been made to differentiate risks for acquisition of HIV from injection with used syringes (ie, risk to self) versus loaning, renting, or selling of syringes (ie, risk to others); use of potentially contaminated syringes to measure or mix drug preparations (eg, frontloading or backloading); and the joint use of injection paraphernalia (eg, cookers, cotton, water, or ampoules).2 The role of personal and social networks as key influences of HIV risk behaviours in IDUs has been reported, consisting of studies of HIV serostatus of network members and subgroups of IDUs that can form transmission bridges (eg, male IDUs who have unprotected sex with other males, or IDUs who are sex workers).3 Although we mainly discuss HIV transmission risks within populations of IDUs, transmission from IDUs to people who do not inject drugs is a major concern in some countries with established HIV epidemics related to injecting drug use.4–6
Increased appreciation of the social determinants of health has given rise to interest in the mapping of social, structural, and environmental factors that shape risk of HIV acquisition.7 Increasingly, epidemiological and social science research7–12 promulgates the idea that individual HIV risk practices are shaped by social context and environment, and hence that HIV risk is socially produced.7,13 The conceptual framework of risk environment guides research measurement and interpretation on the social basis of drug-related harm, and encourages a focus on interactions between risk factors exogenous to the individual,7 rather than endogenous factors (eg, age, sex, race, or genetic composition), risk practices (eg, joint use of needles and syringes, or unprotected sex), or pathogenic characteristics (eg, HIV subtype, or drug resistance).
Figure 1 shows how physical, social, economic, and political environments are posited to interact with microenvironmental and macroenvironmental factors to confer risk or protection for HIV infection in injecting drug users,11,13 and panel 1 lists these environmental risk factors. Macroenvironmental influences include drug-trafficking patterns (physical), gender inequities (social), criminal justice expenditures (economic), or policies and laws for harm-reduction programmes (political).13 Microenvironmental influences include injection locations (physical), relationship dynamics (social), survival sex trade (economic), and coverage of harm reduction programmes (political). All these factors are constantly interacting, and often overlap with synergistic effects on HIV incidence.
Figure 1: HIV risk factors in injecting drug users.
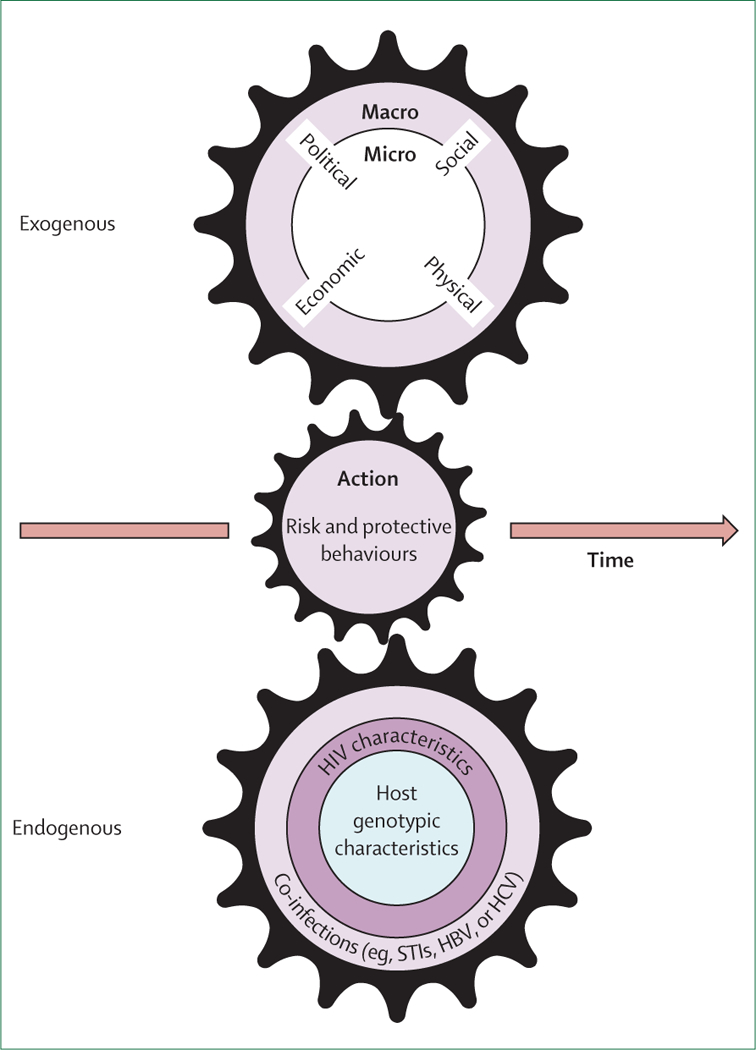
The HIV risk environment is a product of action produced by the continuing, interlocking, and synergistic effects of exogenous and endogenous factors over time. Developed from Glass and McAtee.14 STI=sexually transmitted infection. HBV=hepatitis B virus. HCV=hepatitis C virus.
Key messages
Understanding of the risks of HIV infection in injecting drug users (IDUs) should go beyond the individual and assess structural and environmental influences that shape risk practices and vulnerability to infection.
Over the past decade, only a quarter of epidemiological studies explicitly aimed to study risk factors operating in the HIV risk environment in IDUs.
Over the past decade, fewer than a third of studies that examined risk factors for HIV infection in IDUs were done in countries with high HIV burdens in IDUs.
Sexual transmission among IDUs and from IDUs to people who do not inject drugs can be a major factor in epidemics; in injectors, risk of HIV infection attributable to unprotected sex was nearly 5% during 2010–15 in Karachi, Pakistan, and Nairobi, Kenya, but was 15–45% in Odessa, Ukraine.
Reduction of the unmet need of opioid substitution, needle and syringe programmes, and antiretroviral therapy by 60% during 2010–15 could prevent 41% of incident HIV infections in Odessa, 43% in Karachi, and 30% in Nairobi.
Local HIV epidemics are sensitive to different types and amounts of structural changes: mitigation of the expected transition of non-injecting drug use to injecting drug use by 8–12% in Karachi could prevent 65–98% of incident HIV infections; elimination of laws prohibiting opioid substitution in Nairobi and scaling up of services to 80% coverage could prevent 14% of incident HIV infections in IDUs.
Extreme heterogeneity in global and local HIV epidemics in IDUs necessitates implementation of a tailored combination of interventions that addresses population determinants of HIV transmission, informed by a comprehensive analysis of local risks operating at many degrees of influence. Structural HIV prevention interventions are a crucial element of a combined prevention approach.
In regions with rapidly growing epidemics (eg, Nairobi), rapid optimisation of effective and widespread opioid substitution and needle and syringe programmes is crucial. Interventions that protect access to HIV prevention and treatment for IDUs can have substantial effect on local HIV epidemic trajectories.
Search strategy and selection criteria
We searched BIOSIS (ISI-CE BIOSIS previews), PubMed, and Embase for publications written in English, French, Spanish, Ukrainian, or Russian between 2000 and 2009. Our search had three required components: “HIV”, “HIV infections”, “HIV”, “AIDS”, “human immunodeficiency virus”, “acquired immunodeficiency syndrome”, or “acquired immune deficiency syndrome”; “substance abuse, intravenous”, “IDU”, “IDUs”, “injecting drug”, “intravenous drug”, “intravenous substance”, “injecting substance”, or “injecting drug use”; and “risk factor”, “correlate”, or “determinant”. We searched reference lists from retrieved manuscripts. Abstracts were examined to assess eligibility for inclusion, and we excluded studies in which HIV infection was not an outcome, multivariate analyses of risk factors were not done, or data for injecting drug users were not reported separately from those for users of non-injecting drugs. We excluded commentaries, editorials, and reviews. To obtain data for modelling scenarios, the same keywords were used with “Kenya”, “Pakistan”, and “Ukraine”. We also hand-searched published work from the UNAIDS data archive, peer-reviewed abstracts from conference proceedings, and national AIDS programme data.
Panel 1: Risk factors for HIV-1 infection in injecting drug users
Microenvironmental
Physical
Social
Economic
Cost of living and of health treatments*
Cost of syringes*
Cost of condoms*
Scarcity of income generation and employment19,34,39,52,55,56,62,78,79
Political
Macroenvironmental
Physical
Social
Economic
Scarcity of health service revenue or spending*
Correction expenditures*75
Growth of informal economies*
Uncertain economic transition*
Political
Policy and laws governing syringe access and exchange, and enforcement status89
Policy and laws governing drug treatment*
Policy and laws governing free highly active antiretroviral therapy coverage*
Public health policy governing sex work and enforcement status*
Laws governing possession of drugs and drug paraphernalia, and enforcement status85,93
Immigration policies and laws*
Laws governing protection of human and health rights*
Data from the risk environment framework (2000–09).13 *Environmental factors and domains identified in social science research and or descriptions of models of HIV risk environments that do not appear in the published work we reviewed.3,7–9,11
Panel 2: Voices from Odessa, Ukraine: personal accounts of the risk environment
Police
“There are plenty of problems with police. If they stop you with clean syringes, you get hassled; they will plant drugs in the syringes unless you pay them. They plant drugs in your pocket if they need information. There are many occasions when drug users are beaten by police just because they did not want to take the blame for someone, so they are forced to do it. Some people even get arrested only because they were buying syringes in a pharmacy. They [the police] have no bounds.”
Incarceration
“Many of us who have been released from prison have a big problem with documents (passports). While in prison, the documents were lost or expired and one needs money to be able to restore them. And we do not have money. Even if you have a place to live, you need to get registered (to access services), but without documents and money, it’s not possible. To get a job is totally unreal. Nobody wants to give a job to former prisoners or drug users. They send us away using all possible ways. Maybe some of us wanted to live clean, but out of desperation, we start selling and using drugs and end up in prison again. It’s a vicious circle.”
Medical care
“People are scared of drug users, even more so when we are HIV-positive. If you are admitted to hospital and a doctor finds out that you are a hopeless drug user (and he finds out about it very fast), he treats you with disgust. Their entire approach to you amounts to: ‘You are a drug user, you will not live long anyway, so what difference does it make what you die from?’ Not all of us are HIV-positive, but some doctors ‘diagnose’ us with HIV anyway. And to receive HIV medicines, you need to be registered (ie, have a registered address).”
Drug treatment
“And the main thing...there is practically no place where one could get free drug treatment. That’s a daydream. You need to go there with your own medicine and also give a bribe to the doctor. One has to pay for everything, for a psychologist’s help or rehabilitation. And, in the end, we do not have any place where we find understanding and help.”
“We do not have enough organisations offering needle exchange, even though these programmes can help us from getting HIV. We really need more of them.”
“After I was arrested, I was experiencing drug withdrawal but I was not given any medical help. I made multiple emergency requests, but the police told me that my death will not distress anyone as they were impudently laughing in my face. We really hope that you will not remain indifferent to our problems.”
So far, the empirical basis for models of HIV risk environments has come from qualitative and social science research.11 Despite increased methodological interest in the development of social epidemiological and modelling approaches to the study of HIV determinants,8,9 little work has been done to assess the extent to which published epidemiology studies of HIV risk and injecting drug use map to the conceptual framework of risk environment.
Systematic review and modelling
We systematically reviewed epidemiological research about risk factors for HIV acquisition in IDUs during the past 10 years. We assessed the extent to which existing evidence and epidemiological studies are congruent with a risk environment approach for delineation of risk factors of HIV acquisition, to improve our understanding of social determinants of HIV and its prevention.
We also provide mathematical modelling projections for two cities with serious HIV epidemics in IDUs (Odessa, Ukraine and Karachi, Pakistan) and one city with an emerging drug-related epidemic (Nairobi, Kenya). These models allow us to assess the heterogeneity, influence of the environment, and potential effect of interventions for different environmental factors, in isolation and in combination in epidemics.
Six independent reviewers extracted data from the papers identified in the search strategy and entered them into a coding form that registered information about type of endogenous and exogenous risk factors, correlates of HIV transmission, magnitudes of association, study design, and location. We recorded study design features (sample size, location, years of data collection, and if prospective, cross-sectional, or ecological design), and whether data were from low and middle-income countries or high-income countries, what type of environmental influence (eg, macroenvironmental or microenvironmental, or physical, social, economic, or political) the study was designed to measure, and whether potential pathways were explored through interactions or stratified analyses. A randomly selected 10% were verified by a second reviewer. Coded data were mapped to the various types of environmental influence according to the risk environment framework described by Rhodes and Simic13 (panel 1). Data for the required modelling variables (tables 1–3, panel 2, and webappendix pp 13–33) were abstracted by native speakers; a randomly selected 10% of documents were independently selected by a second reviewer who verified accuracy.
Table 1:
Key parameter estimates for injecting drug users in Odessa, Ukraine
| Estimate (range) | Source | |
|---|---|---|
| Population size | 17100 (8900–21 360) | Local report for USAID94 |
| Male (%) | ||
| 2005 | 66.2% | Balakireva (2005)95 |
| 2007 | 78% | Balakireva (2007)96 |
| 2008 | 75.8% | Pohorila et al (2008)97 |
| Mean duration of injecting drug use (years) | ||
| 2005 | 9 (1–37) | Balakireva (2005)95 |
| 2007 | 13 (1–46) | Balakireva (2007)96 |
| 2008 | 10 (1–40) | Pohorila et al (2008)97 |
| Ever used non-sterile injecting equipment (%) | ||
| 2005 | 17.9% | Balakireva (2005)95 |
| Past month, 2007 | 27.1% | Balakireva (2007)96 |
| Past month, 2008 | 14.8% | Pohorila et al (2008)97 |
| Men who have ever had sex with men (%) | 2.4% | Balakireva (2005)98 |
| Estimate of HIV-1 prevalence (%) | ||
| 2008 | 368% | Pohorila et al (2008)97 |
| 2009 | 53% | Booth et al (2009)99 |
| Years of rapid epidemic spread | 1990–2000 | Rhodes et al (1999)100 |
Data are number (range) unless otherwise stated. Estimates and range are the mode and limits of the distribution of value allowed in the model analysis (see webappendix pp 7–9). Values are the principal parameters used in the mathematical models. USAID=United States Agency for International Development.
Table 3:
Key parameter estimates for injecting drug users in Nairobi, Kenya
| Estimate (range) | Source | |
|---|---|---|
| Population size | 3000–5000 | Estimate made on the basis that 60% of injecting drug users (3 500) were contacted by outreach workers by June, 2009; UNODC Regional Office for Eastern Africa110 |
| Group (%) | Nairobi Outreach Services Trust UNODC Report on Contacts 2009110 | |
| Sex (female) | 7% | |
| Female sex worker | 12% | |
| Sex (male) | 66% | |
| Men who have sex only with men | 7% | |
| Men buying sex | 8% | |
| Mean number of injections with non-sterile equipment per week | 3.6 (1–6) | Range is 95% confidence interval. Shared needle and syringe use in Nairobi110 |
| Baseline coverage of opioid substitution therapy, 2010 | 0% | UNODC Regional Office for Eastern Africa109 |
| Baseline coverage of needle-exchange programmes, 2010 | 0% | UNODC Regional Office for Eastern Africa109 |
| Injecting drug users receiving antiretroviral therapy, 2010 | <1% | UNODC Regional Office for Eastern Africa109 |
| Estimate of HIV-1 prevalence, 2010 (%) | 33–50%* | Minimum value is the self-reported HIV-1 test result reported in the Nairobi Outreach Services Trust UNODC Report on Contacts, and is an average of January, to October, 2000;110 maximum value is the reported HIV-1 prevalence in injecting drug users in Mombasa in 2004111 |
UNODC=United Nations Office on Drugs and Crime.
49.5% of injecting drug users were HIV-1 positive in Kenya in 2004.111 UNODC project data from June, 2009 (updated on a monthly basis), suggested that 30% of injecting drug users were HIV-1 positive.
We modelled potential HIV epidemic trajectories in Odessa, Ukraine (table 1, panel 2), Karachi, Pakistan (table 2), and Nairobi, Kenya (table 3). For Odessa and Karachi, we used a deterministic compartmental modelling approach (for details of the model see webappendix pp 1–12). As with previous studies,112–114 our model was of HIV transmission in an IDU population through shared use of injecting equipment and sexual contact. Transmission of HIV to the IDU population from people who do not inject drugs was assumed to be small, and was not included in the model. The modelled population consisted of IDUs who might or might not have reused non-sterile injecting equipment or been sexually active, and who were men, women, bisexual men (men who have sex with men and women), or homosexual men (men who have sex only with men [MSM]) (figure 2). Reductions in shared syringe use can arise either through increased access to sterile injecting equipment (eg, needle and syringe programmes) or through opioid substitution therapy. Our model did not assume any direct interaction between the effects of needle exchange and opioid substitution. If antiretroviral therapy was available, individuals started when their CD4-cell count reached 350 cells per μL of peripheral blood.115
Table 2:
Key parameter estimates for injecting drug users in Karachi, Pakistan
| Estimate (range) | Source | |
|---|---|---|
| Population size | 9000 (7200–10 400) | National AIDS Control Programme101 |
| Men (%) | 97.5% (95–100%) | Estimate is mean value reported in Karachi;102–104 minimum and maximum values are from reports for any city in Pakistan |
| Ever used non-sterile injecting equipment (%) | 83% (18–94%) | Estimate is percentage of injecting drug users who reported ever use of non-sterile equipment in Karachi;105 minimum value is percentage of those that reported use of used syringes at most-recent injection in Karachi;106 maximum value is highest report for ever use in any city in Pakistan from review of the published work50,107,108 |
| Men who have sex with men (%) | 14% (11–50%) | Estimate is percentage of male injecting drug users in Karachi who reported sex with men in the past month;106 minimum and maximum values are from reports for any city in Pakistan101 |
| Injecting drug users receiving opioid substitution therapy, 2009 (%) | 0% | Mathers et al108 |
| Injecting drug users in needle and syringe exchange programmes, 2008 (%) |
53.3% (10.6–53.3%) | Estimate is percentage of injecting drug users in Karachi who reported having obtained syringes from a drop-in programme;101 across Pakistan in 2008, needle and syringe programme coverage was estimated at nine syringes exchanged per injecting drug user109 |
| Injecting drug users receiving antiretroviral therapy, 2009 (%) | 0.38% (0.36–0.43%) | Mathers et al109 |
| HIV prevalence estimate, 2008 (%) | 23.1% (19.0–27.2%) | National AIDS Control Programme101 |
| Years of rapid epidemic spread | 2003–04 | Bokhari et al106 |
Data are number (range) unless otherwise stated. Estimates and range are the mode and limits of the distribution of value allowed in the model analysis (see webappendix pp 7–9).
Figure 2: Routes of HIV transmission among populations of IDUs.
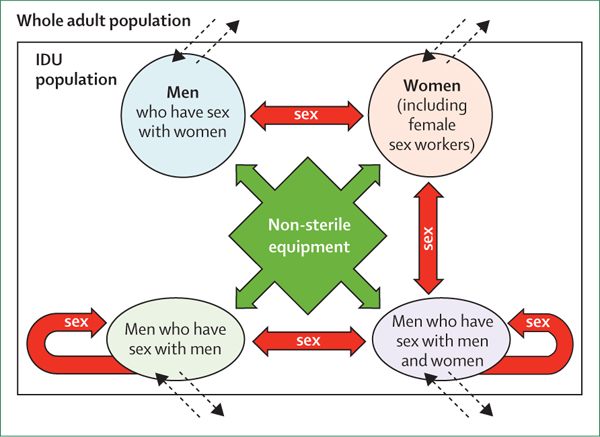
Population subgroups and risk of HIV infection from shared use of injection equipment (green arrows) and sex (red arrows) are shown. Dashed arrows show entry and exit to the injecting drug user population (ie, start or stop of drug injections). IDU=injecting drug users.
Models were analysed in a Bayesian framework, in which previous information was assembled as distributions around every model variable. Subsequent distribution of fitting sets of model variables was constructed to generate estimates for the course of the epidemic with and without intervention scale-up.
For Nairobi, because of the low availability of HIV prevalence estimates and IDU behavioural data, a different model was developed on the basis of an extension of UNAIDS’s modes of transmission modelling exercise. This method captured patterns of HIV transmission within and between different population subgroups in Nairobi, consisting of IDUs (subdivided into men and women, men that buy sex, MSM, and female sex workers), sex workers, and those forming casual sexual partnerships.116,117 Transmission to IDUs from sex partners who were not IDUs was captured in this model.
Determinant outcomes
We identified 2722 studies with the search strategy, retained 146 after reviewing titles, keywords, and abstracts; and reduced this number to 94 after review of the full manuscripts. 24 (26%) of these reports were designed to study some aspect of the HIV risk environment, and 81 (86%) identified at least one microenvironmental or macroenvironmental determinant (panel 1 and webappendix pp 35). Variables were classified as exogenous or endogenous and mapped to the risk environment framework. 37 (39%) reports were prospective or panel studies. Only 35 (37%) were done in low-income or middle-income countries, and 27 (29%) were done in countries where average HIV prevalence in IDUs was 20% or more.
The number of microenvironmental HIV determinants reported substantially exceeded macroenvironmental ones. Most studies of both macroenvironmental and microenvironmental determinants identified social or physical HIV determinants. Microsocial determinants were most frequently reported, including relationship and network dynamics, sexuality and sexual orientation, amount of education, and policing practices. The most frequently recorded microphysical variables included the locations where drugs were injected, homelessness, incarceration, and spatial inequities (eg, differential risk of HIV infection by city or neighbourhood). For macrophysical determinants, several studies reported population mobility as a risk factor for HIV infection,40,41,53,84 whereas none measured changes in distribution or drug-trafficking routes. Almost all studies reported macrosocial inequities related to gender or race and ethnicity, as opposed to measurements of social processes such as stigmatisation, or geopolitical forces such as exposure to war or conflict (panel 1).
Although 16 studies reported microeconomic influences as determinants of HIV infection, they exclusively reported associations with survival sex (ie, sex for basic necessities) and the sex trade with measures of income generation or employment, as opposed to costs associated with interventions for prevention (eg, needles, syringes, or condoms) or health care. For micropolitical determinants, nine studies reported coverage of drug treatment, sterile syringes, or HIV testing and counselling as independently associated with HIV infection, whereas no programme-wide policies related to syringe access or housing. Far fewer studies reported macroenvironmental influences related to economics, such as criminal justice expenditures,75 or policies, such as those governing syringe access89 or possession of drugs or drug paraphernalia.85,93
Modelling of HIV epidemics
Case 1: Odessa, Ukraine
Ukraine is the most HIV-affected country in Europe and Central Asia, with around 440 000 people aged 15–49 years infected with the virus (HIV frequency of 1.63%).118 In some cities, the frequency of HIV infection in IDUs rose from nearly zero in 1994 to more than 50% in 2 years, and as many as 820 400 people might be infected by 2014.119,120
Odessa is among the cities bearing the brunt of the HIV epidemic in Ukraine, with the first cases registered in 1987, and outbreaks documented in 1995.121 As in the rest of country, the epidemic was chiefly attributed to heterosexual transmission. However, by 1997, IDUs accounted for nearly 85% of all cases of HIV infection. Unprotected sex and injecting practices, including drawing of drug solutions from common containers, shared syringe use, and unprotected sex with concurrent casual or sex-trade partners, continued to fuel the epidemic.95,97 Young IDUs are more likely to engage in risky behaviours; 38% of all people infected with HIV in Odessa are 21–30 years old.122 Growing use of stimulants, especially in young people, leads to increased engagement in high-risk sexual and injecting behaviours; and drug-treatment programmes fail to reach stimulant users because they mainly target users of opiates.97
High rates of corruption, pervasive poverty, and marginalisation of drug users are epidemic macroenvironmental forces, as explained through the voices of people who inject drugs (panel 2). Since 2004, government spending directed at increased access to antiretroviral therapy, harm reduction, and buprenorphine maintenance has substantially increased,118 but remains suboptimal109 (table 1). Although 12–13% of the prison population injects drugs, there are no needle and syringe programmes or opioid substitution treatments available to prisoners.
Figure 3 shows the rapid spread of HIV in Odessa in the late 1990s, which has since stabilised at 50% prevalence. Few measures of the early rate of HIV spread and the small sample sizes of available prevalence estimates implied that a wide range of alternative epidemic trajectories were supported by the data, leaving substantial uncertainty in model projections. If we assume there will be no further change in risk in IDUs in Odessa, we predict there will be 6200 (95% credible interval 4500–6500) new HIV infections in IDUs between 2010 and 2015 (figure 3). New HIV infections from injecting drug use are mostly (40–80%) attributed to exposure to contaminated injection equipment, but another substantial route of transmission is unprotected sex between IDUs (15–45%).
Figure 3: Model projections for the HIV epidemic in IDUs in Odessa, Ukraine.
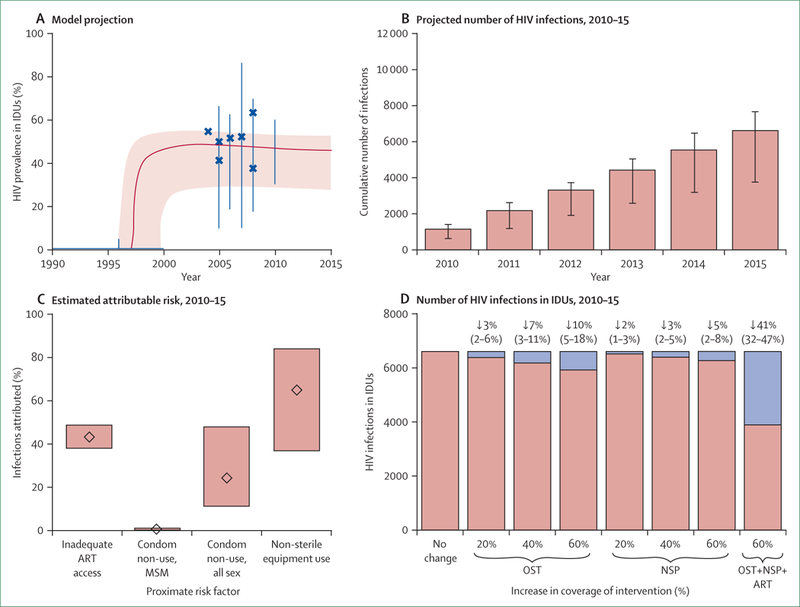
(A) HIV prevalence in IDUs, 1990–2015. Blue crosses show prevalence estimates from data; solid black lines show limits placed on HIV prevalence; pink area shows envelope of posterior model fits; and the thick red line shows the epidemic projection for the best-fitting model (for details of model and fitting procedure see webappendix pp 1–40). (B) Projected number of HIV infections every year for 2010–15 in the IDU population, assuming no further changes in patterns of risk (bars show best-fit estimate and vertical lines show 90% credible interval). (C) Estimates of the attributable risk of selected proximate risk factors for the IDU population. Estimates are the proportion of infections that would be averted in the absence of the risk factor, which is estimated as the proportion of projected infections that would be averted if that risk were absent from 2010–15; width of bar shows 95% credible interval and diamond shows median. Attributable risks do not sum to 100%. (D) Projected change in the number of HIV infections in Odessa (2010–15) and assuming increased coverage of OST, NSP, and ART by 20%, 40%, or 60%. Numbers (95% credible interval) are percentages of infections averted (shown in blue). Access to OST and NSP are assumed to reduce the rate of overall exposure to non-sterile injecting equipment by half, and present levels of access to interventions (table 1) are taken into account. IDUs=injecting drug users. ART=antiretroviral therapy. MSM=men who have sex only with men. OST=opioid substitution therapy. NSP=needle and syringe programme.
Suboptimal access to clinically indicated antiretroviral therapy (CD4-cell count ≤350 cells per μL) causes 40–47% of infections. Many HIV infections in IDUs could be averted through timely and widespread interventions that reduce the frequency with which IDUs use non-sterile equipment. A 60% reduction in the unmet need of opioid substitution services could avert 10% (5–18%) of new infections, and a similar reduction in unmet need ofneedle and syringe programmes could avert 5% (2–8%) (figure 3). However, even in these optimistic scenarios, many infections would still arise because of the residual risk from contaminated injection equipment and unprotected sex. Therefore, a scale-up of these programmes should proceed alongside equitable scale-up of antiretroviral therapy and support for behavioural changes and condom promotion in this setting. 41% (32–47%) of infections could be averted if coverage of opioid substitution therapy and needle-exchange programmes were scaled to reduce unmet need by 60%, and if 60% of IDUs were initiated promptly on antiretroviral therapy when indicated.
Elimination of police beatings in Odessa, Ukraine
Removal of an environmental risk factor can have a substantial effect on incidence of HIV infection. Our reviews41,51,75 and other studies (see papers 48, 49, 60, 62–64, and 66 in webappendix pp 38–39) suggest that policing practices can directly affect the risk of HIV acquisition by affecting where, when, with whom, and the context within which drugs are injected (eg, IDUs rushing injections or injecting in shooting galleries to avoid arrest). Police can also have an indirect effect on HIV risk, via pressuring or displacing IDUs away from needle and syringe programmes or drug-treatment settings.123 Problematic policing practices include arresting of drug users for carrying of sterile or used syringes, harassments at needle and syringe programmes or drug-treatment clinics, soliciting of bribes to avoid arrest, or in extreme cases, sexual abuse or violence. These actions can increase the chance of IDUs injecting with contaminated equipment. 24% of IDUs in Odessa report ever being beaten by police (table 1 and panel 2),99 and these people are more likely to report shared syringe use, use of preloaded syringes, and frontloading or backloading of syringes, among other risk behaviours.124 We suggest that elimination of police beatings would remove the excess in risk behaviour, across the population, that stems from some individuals ever having been beaten. The effect of this assumed change in risk behaviour on HIV incidence in Odessa was estimated with the model (see webappendix p 10).
Our model projects that a substantial number of new HIV infections could be prevented in Odessa by 2015 through elimination of police beatings (figure 4). In two other Ukrainian cities, Makeevka and Kiev, where beatings are less associated with increased risk behaviour (Booth R, unpublished data), we estimate 2–9% of infections could be averted. The influence of police beatings and other practices on HIV incidence probably varies by location and operates through several direct and indirect causal pathways, making precise quantitative estimates impossible to generate without additional data. Additional studies with quantitative and qualitative methods are needed to elucidate the magnitude and direction of these associations, and intervening variables and the interplay between them. We will then be able to assess the effect of elimination of these human rights violations on HIV incidence in IDU populations.
Figure 4: Estimated number of HIV infections averted by structural changes.
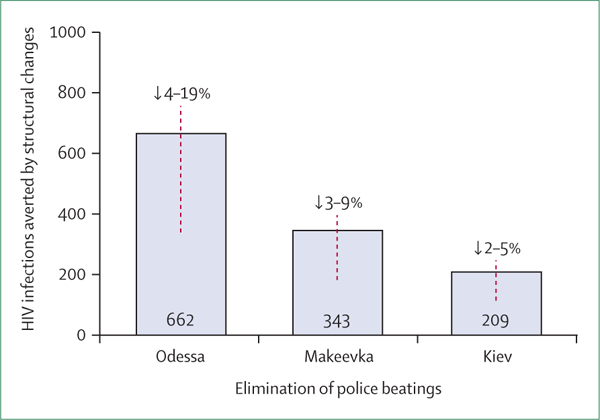
Projected number (95% credible interval of percentage reduction) of infections that could be averted after elimination of police beatings in Odessa, Makeevka, and Kiev. Estimations made on the basis of reported correlations between exposure to non-sterile injecting equipment and experience of beatings in the three Ukrainian cities (see webappendix p 10).99
Case 2: Karachi, Pakistan
Pakistan has had a thriving heroin consumption market for decades, and is neighbour to Afghanistan, the world’s largest producer of opium. In the 1980s and 1990s, national surveys107 suggested that the number of drug users increased yearly by 12%, with most people who used drugs taking heroin by inhalation or smoking. In the past 10 years, however, changes in drug trafficking and distribution prompted transitions from smoking of heroin to injection of heroin, liquid opiates, and other pharmaceuticals, these being readily available over-the-counter at chemist shops. By 2000, there were an estimated 500 000 people who used drugs nationwide,108 of whom 15–30% were IDUs.107 Although non-therapeutic drug use, prostitution, adultery, and homosexuality are illegal in Pakistan, all are widespread.125
HIV prevalence in Pakistan’s population of 91 million aged 15–49 years is low at 0.1% (~96 000 people). However, HIV outbreaks in IDUs occurred in Larkana in mid-2003,107 and in Sargodha, where HIV prevalence in IDUs rose from 9% in 2005–06, to 51% in 2007.50 HIV prevalence was 23% in Karachi, Pakistan’s most populous city in 2003,101 where there were 9000 IDUs in 2006,107 and was 19.6% in nearby Sukkur and 18.3% in Hyderabad. As in other cities, most IDUs in Karachi are male; 2–3%107 of female sex workers inject drugs, and 20–25% of these workers report having sex with IDUs.107 About half of male IDUs in Karachi are married;101 47% reported having sex with female sex workers,105 and 9–14%101,105 reported having sex with a male sex worker or hijra (transsexual) in the past month—two-thirds never use condoms.105
Challenges to prevention include the tendency for IDUs to use professional injectors (hit doctors), inject together in groups with common syringes or ampoules (79.5% of all injection drug users),105 and mix their blood with drug preparations before passing it on in an effort to potentiate the high. Furthermore, in the previous year, 16% of IDUs in Karachi reported visiting other cities in Pakistan,101 and 28% reported selling their blood.106
Needle and syringe programmes are present in Karachi and in many major cities in Pakistan,107 some of which provide mobile services, but coverage is grossly insufficient.109 Detoxification and residential rehabilitation are the predominant strategies for drug treatment. Although buprenorphine maintenance therapy has been piloted in a few cities,109 opioid substitution remains unavailable. In 2009, less than 1% of IDUs with HIV infection were receiving antiretroviral therapy.109 Although Pakistan’s epidemic is concentrated, it could be increasingly difficult to contain if reported rates of highrisk behaviours continue, or if high rates of transition to injection happen as a result of macroenvironmental changes in drug markets (ie, reduced availability or purity and increased price of heroin), in the absence of effective prevention scale-up.
In Karachi, the HIV epidemic spread in the late 1990s, although the earliest prevalence measurement in 1995 suggested little evidence of HIV penetration in IDUs. However, by 2003, estimated HIV prevalence in this group was 23% (figure 5), which rose to 30.1% in 2006, and decreased to 23.1% in 2008.101 We estimate that HIV incidence will stabilise, with 2400 (95% credible interval 1300–4400) new HIV infections in IDUs in 2010–15.
Figure 5: Model projections for the HIV epidemic in IDUs in Karachi, Pakistan.
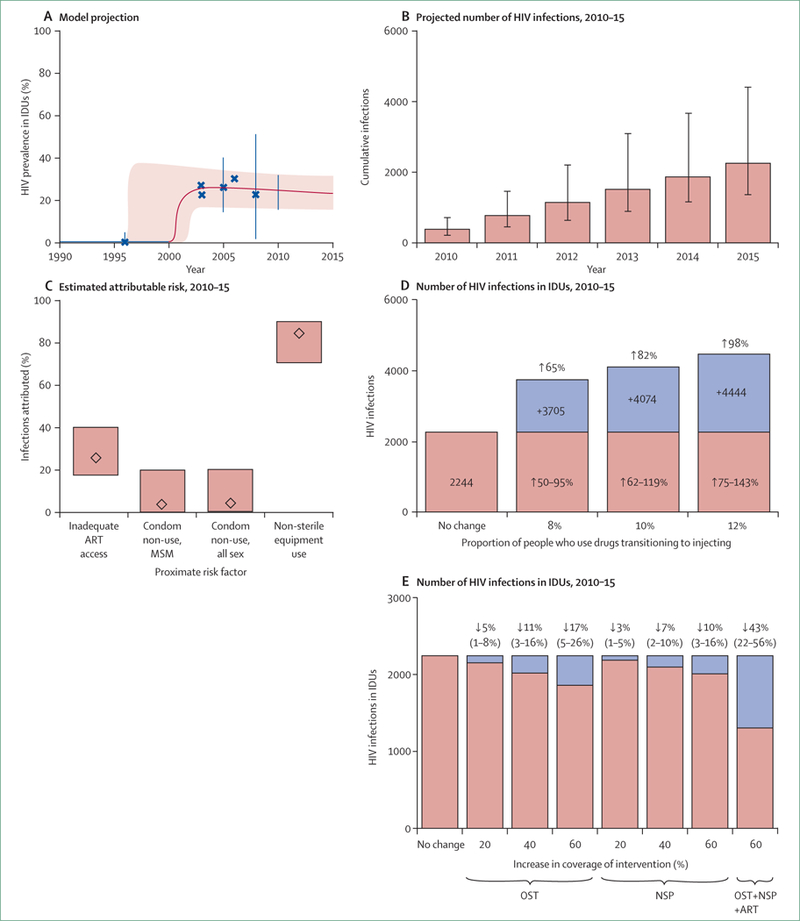
(A) HIV prevalence in IDUs, 1990–2015. Blue crosses show prevalence estimates from data; solid black lines show limits placed on HIV prevalence; pink area shows envelope of posterior model fits; and the thick red line shows the epidemic projection for the best-fitting model (for details of model and fitting procedure see webappendix pp 1–40). (B) Projected number of HIV infections every year for 2010–15 in the IDU population, assuming no further changes in patterns of risk (bars show best-fit estimate and vertical lines show 95% credible interval). (C) Estimates of the attributable risk of selected proximate risk factors for the IDU population. Estimates are the proportion of infections that would be averted in the absence of the risk factor, which is estimated as the proportion of projected infections that would be averted if that risk were absent from 2010–15; width of bar shows 95% credible interval and diamond shows median. Attributable risks do not sum to 100%. (D) Projected number of infections in the IDU population during 2010–15, assuming that 8%, 10%, or 12% of people who use non-injecting drugs transition to injecting drugs in 2010. (for the model structure and variables see webappendix pp 1–40). (E) Projected change in the number of HIV infections in Karachi (2010–15) and assuming increased coverage of OST, NSP, and ART by 20%, 40%, or 60%. Numbers (95% credible interval) are percentages of infections averted (shown in blue). Access to OST and NSPs are assumed to reduce the rate of overall exposure to non-sterile injecting equipment by half, and present levels of access to interventions (table 2) are taken into account. IDUs=injecting drug users. ART=antiretroviral therapy. MSM=men who have sex only with men. OST=opioid substitution therapy. NSP=needle and syringe programme.
Modelling provides most support for rapidly growing epidemics beginning after 2000, because of the high degree of shared use of injection equipment.105,106 Although a quarter of male IDUs have sex with female sex workers,101 the low HIV prevalence in female sex workers in Karachi and the relative frequency and probability of transmission through sex and injection behaviours suggest that little transmission is attributable to this route. Furthermore, only about 4.6% of HIV infections are attributed to unprotected sex with other IDUs (figure 5). However, the proportion of HIV infections attributable to inadequate antiretroviral therapy coverage is substantial (19–40% if antiretroviral therapy is started at CD4-cell count ≤350 cells per μL), but is marginally lower than that reported in Odessa because of the higher proportion of cases of incident HIV caused by injection behaviour in Karachi.
Non-injecting drug users might increasingly transition to injecting in the coming years, and, because of the large numbers of these people in Karachi,50 the spread of the epidemic could accelerate. If 10% of non-injecting drug users started injecting in 2010, the number of new HIV infections could increase by 82% by 2015 (~4000 extra infections) compared with the most conservative scenario that assumes no transitions (figure 5). If 12% of non-injecting drug users started injecting, the increase in new infections in IDUs in Karachi would be close to 98% (4400 extra infections). Because of the virtual absence of opioid substitution in Pakistan, implementation and scale-up of this therapy could have a substantial effect on reduction of shared syringe use by lessening of the frequency of injections or the number of active IDUs. If 60% of IDUs in Karachi were to be given opioid substitution, the number of new HIV infections could decrease by up to 28% in 2010–15. Thus, actions to limit the quantity of drug users who transition to injecting and a substantial scale-up of opioid substitution therapies are two priority interventions for Pakistan.
Case 3: Nairobi, Kenya
Kenya is in eastern Africa, borders the Indian Ocean between Somalia and Tanzania, and has a population of 39 million, 42% of whom are younger than 15 years of age. 1.5–2 million adults and children had HIV in 2007, of whom 1.4–1.8 million were aged 15 years and older.126 Only a quarter of Kenyans with HIV infection know their serostatus.117 Urbanisation is happening at an estimated 4% annual rate of change (2005–10 estimate), and the capital city, Nairobi, has an estimated population of 3.04 million. Recreational drugs taken in Kenya include bhangi (herbal cannabis), heroin, khat (a plant with amphetamine-like properties), flunitrazepam, diazepam, glue, and alcohol.127 Estimates of the number of people who take heroin vary from 12 201,117 to 18 000,127 up to 24 500.116 Overall, less than 10% of heroin users are thought to have injected.117 However, one study128 reported that 44.9% of Nairobi heroin users had injected and 52.5% of 101 present injectors were HIV positive, compared with 13.5% of 181 non-injecting heroin users.128 Hepatitis C prevalence was 61.4% in the presently injecting group compared with 3.8% in those not injecting. In 2005, although only 0.3% of the adult male population were injecting drugs, an estimated 4.8% of new HIV infections happened through this route.116 Although 73% of Nairobi injectors knew about the risks of HIV transmission in 2005, 28% had used a needle after someone else, and 43% had passed their own needle to another person in the past 6 months.129 By 2008, injection-drug use accounted for 3.8% of incident HIV infections in Kenya (5.8% in Nairobi).117
Kenya’s national AIDS strategic plan for 2010–13 referred to development of policies and legislation for the provision of needle and syringe programmes and opioid substitution therapy for the first time. Needle and syringe programmes are not permitted by law in Kenya,109 but some non-governmental organisations in Nairobi and Mombasa reportedly provide education about harm reduction. There are very few opioid substitution services in private clinics in Kenya, and substitution therapy is not permitted in public clinics because of rigid interpretation of a law regulating opiate pain medications. Treatment that is not reliant on non-opioid substitution for drug dependence is available in government hospitals and is provided by non-governmental organisations.129 The number of people receiving antiretroviral therapy in Kenya rose from 29 000 in 2004,126 to 242 881 in 2008,130 but less than 1% of IDUs who were HIV positive were receiving therapy in 2008.109
The HIV epidemic in IDUs in Nairobi will grow substantially; 4000 (95% CI credible interval 2600–5400) new HIV infections are expected from 2010 to 2015, 95% as a direct result of exposure to contaminated injecting equipment and 5% from sexual transmission (figure 6). In the model, the much higher rate of non-sterile equipment use in Nairobi than Odessa or Karachi leads to a lower proportion of risk of HIV infection for injection drug use via unprotected sex there, despite the much higher prevalence of HIV infection in sexual partners. The high rate of non-sterile equipment use could also undermine the effect of needle and syringe and opioid substitution programmes (figure 6). Scale-up of needle and syringe programmes to reach 40% of the population might reduce HIV prevalence by as little as 4%, assuming that such a programme halves the frequency of injections with nonsterile equipment.
Figure 6: Model projections of the HIV epidemic in IDUs in Nairobi, Kenya.
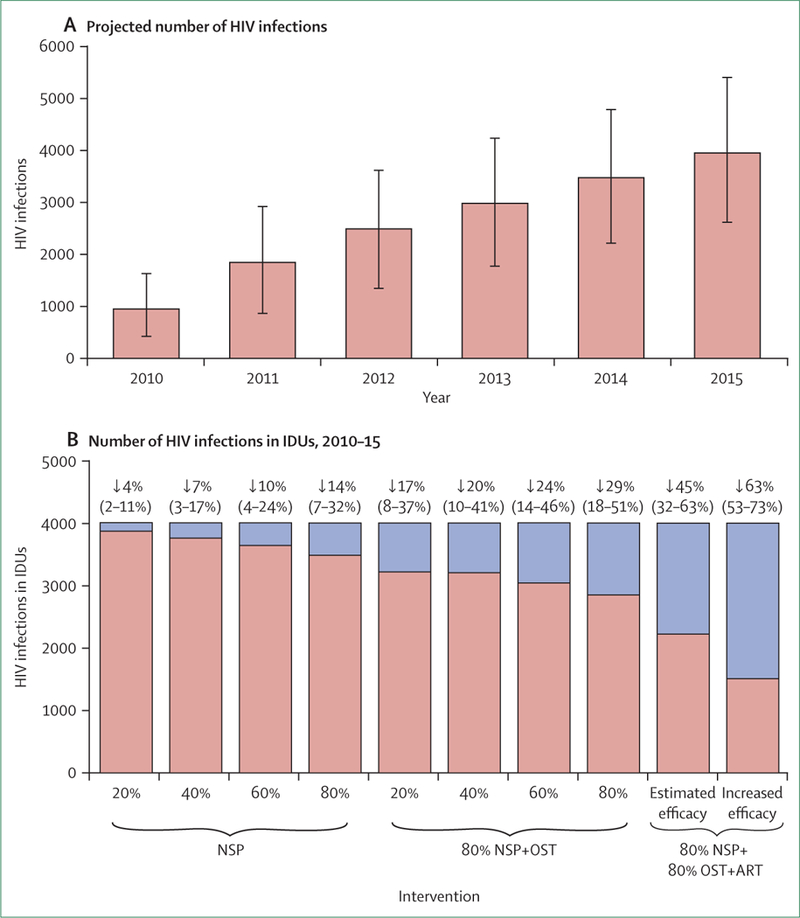
(A) Expected number of HIV infections (with 95% uncertainty interval) in IDUs in Nairobi, 2010–15. (B) Estimated effect of interventions on the total number of infections in IDUs, 2010–15. Red parts of the bars are proportion of infections averted relative to a no-intervention scenario. Interventions are 20%, 40%, 60%, or 80% coverage of NSPs; 80% coverage of NSPs plus 20%, 40%, 60%, or 80% coverage of OST; 80% coverage of NSPs and OST plus 80% coverage of antiretroviral therapy (initiated at CD4 count of 350 cells per μL) to those in need; and 80% coverage of NSTs and OST at a higher effectiveness (70%) and ART. IDUs=injecting drug users. NSP=needle and syringe programme. OST=opioid substitution therapy. ART=antiretroviral therapy.
However, a combination of interventions at high coverage would have a far greater effect; 80% coverage of both opioid substitution and needle and syringe programmes could avert around 1100 (26%) infections by 2015. Elimination of laws prohibiting opioid substitution and scaling up services to 80% of IDUs could reduce the number of incident HIV infections by 14%. If increased coverage of antiretroviral therapy is added to opioid substitution and needle and syringe programmes, with rapid initiation when CD4-cell counts are lower than 350 cells per μL, about 1800 (45%) infections could be averted. However, the high rate of reported risk behaviour in the population implies that, even with all these interventions at full coverage, there could still be more than 2000 new infections in IDUs during 2010–15. Thus, to further reduce the effect of this epidemic, sustaining of high-coverage, high-effectiveness needle and syringe programmes and opioid substitution interventions will be crucial. With an effectiveness rate of 70% (rather than 50% assumed elsewhere, see webappendix p 11), and with 80% of the population accessing needle and syringe and opioid substitution programmes, our model suggests that almost 2500 (~67%) new infections could be prevented.
Implications
Comment
Our systematic review of the published work from the past decade, and modelling scenarios of local HIV epidemics in three diverse cities emphasises the important role of the risk environment in vulnerability to HIV infection in people who inject drugs. Although the published work suggested that physical, social, economic, and political environments can be microenvironmental or macroenvironmental, and are independently associated with HIV infection in injectors, only a quarter of studies were designed to assess environmental influences. Even fewer tried to measure macroenvironmental influences, or economic or political determinants. Fewer than a third of studies were done in countries with the greatest burden of HIV infection in IDUs, suggesting that research has not kept pace with the rapid evolution of HIV epidemics in people who inject drugs.
Research of the HIV risk environment
Heuristics of the HIV risk environment (figure 1 and panel 1) provide a loose theoretical framework for empirical efforts to improve the evidence-base on the social relations of HIV transmission.11,13 Undertaking of epidemiological studies that explicitly delineate social-determinant causal pathways for HIV infection to inform social and structural approaches to HIV prevention is daunting.131 Although our review shows that epidemiological studies rarely explicitly embrace investigations of social determinants, they nonetheless identify environmental risk factors as important. We contend that future epidemiological studies of HIV in IDUs should make use of the methods and findings of qualitative and social science research in their efforts to systematically delineate how microenvironmental and macroenvironmental influences combine to increase or reduce HIV risk. We advocate for fully integrated mixed-method approaches that triangulate findings from qualitative and quantitative methodologies.
Findings from our review present challenges for future research. Investigations should shift from binary epidemiological models of straightforward cause and effect to multifaceted models that emphasise HIV infection as an outcome of many contributing factors interacting at once.11 Social determinants are often complex and indirect in their effects with intervening factors (panel 2), and are a substantial challenge to delineation of causal relationships. For example, policing practices can affect the extent to which IDUs engage in protective behaviours in many ways, from reducing their ability to avoid use of contaminated injection equipment or access to needle and syringe programmes, to increasing the likelihood of injection in locations with a high prevalence of HIV (eg, shooting galleries or prison).
Theoretical models of HIV risk environments need to shift from heuristics that list factors (panel 1) to those that model interactions, processes, and pathways (figure 1). Furthermore, an emphasis on protective factors such as resilience, social cohesion, and solidarity is needed for individuals, communities, and populations. Because present epidemiological studies mainly focus on determinants of risk behaviour, rather than HIV infection, there is a need to understand the links between downstream or proximate factors and upstream or more distal influences on behaviour. Interventions on the basis of observational studies that are too narrow or superficial in scope tend not to address social contexts that shape behaviour, and therefore might be unable to create enabling environments that preserve and promote the protective resilience that can prevent the emergence of HIV epidemics.
A few studies were exceptions to the rule, and can serve as models for future studies. In an ecological study of 96 metropolitan areas in the USA, Friedman and colleagues75 reported that three measures of legal repressiveness (arrests for possession of cocaine or heroin, police staff per capita, and costs for corrections) were independently associated with population HIV prevalence. Innovative use of administrative data allowed the investigators to change the unit of analysis from the individual to the community, allowing simultaneous study of the effect of macrosocial and macroeconomic influences on HIV prevalence. Wood and colleagues30 prospectively examined the effects of reduction of plasma HIV-1 viral load in a community on HIV incidence in IDUs. In this study, undetectable rates of HIV-1 viral load in the community were a marker of antiretroviral therapy coverage, which permitted causal inferences to be made about the effect of policies of universal access to antiretroviral therapy on risk of HIV acquisition for the individual.
Review limitations
Other eligible reports could have been selected with different keywords, and we might not have included all studies that explored the effect of risk environments on high-risk behaviours. Because we explicitly focused on the epidemiology of HIV risk environments, our review did not include empirical or theoretical social science studies on the social, economic, and structural determinants of HIV and health inequality. A well-established body of published work from social science exists on the political economy of HIV and drug-related health.11
The environmental risk determinants summarised in panel 1 are inevitably restricted in scope to those factors that epidemiological research has previously operationalised and found significant. Epidemiological research and subsequent reviews should build on social science to hypothesise and test other social, political, and economic influences that indirectly affect the risk of HIV acquisition through many, presently not delineated, pathways.
Another limitation is that models of risk environment draw distinctions between microenvironmental and macroenvironmental factors, and forms of risk environment (physical, social, economic, political). Analytically, these definitions are often somewhat overlapping of each other in practice. Police practices can be classified as a microenvironmental effect in some studies, affecting social environment, or a macroenvironmental effect of law enforcement, policy, and other cultural practices.
Modelling of the HIV risk environment
Our modelling scenarios confirmed the importance of structural change on the projected HIV epidemic trajectories in Odessa, Karachi, and Nairobi in the next 5 years. Since coverage of antiretroviral therapy for IDUs in these cities is very low (<1%), the benefits of providing optimal therapy for those with CD4-cell counts lower than 350 cells per μL are compelling, and could avert 40–50% of incident HIV infections in Odessa and Karachi. Implementation of widespread coverage of antiretroviral therapy to IDUs when clinically indicated to avert immediate HIV-related deaths is a clinical and moral imperative. Our results and other findings30,132 suggest that antiretroviral therapy can contribute to subsequent reductions in HIV transmission. However, the resources needed to meet such targets, including voluntary HIV testing, efficient linkage and retention in care, CD4 diagnostics, adherence counselling, and resistance monitoring are substantial.
Our results support the well-established role of sterile syringe provision and opioid substitution as cornerstones of HIV prevention in IDUs. However, modelling results suggest that epidemic context alters their potential effect. Our findings from Odessa, Karachi, and Nairobi strongly advocate simultaneous combination of opioid substitution, needle and syringe programmes, and antiretroviral therapy scale up wherever possible, since their effects are synergistic.132 An important outcome from the Nairobi models is that, in an epidemic in which the force of infection is great (eg, an outbreak), the approximate 50% effectiveness of needle and syringe programmes and opioid substitution (see webappendix p 11) restricts effect as much as does coverage. This finding implies that investment in strategies to optimise intervention effectiveness is needed as coverage increases. Straightforward incremental scale-up will not achieve intended direct and indirect effects if interventions are not tailored, intensified, and otherwise adapted to address local epidemic dynamics.
Data from our review of the published work19,27,56,57,65,80,82 and our modelling suggest that opioid substitution scale-up should be an intervention priority. Methadone and buprenorphine maintenance have been added to WHO’s essential drug list, but have yet to be implemented widely in Kenya, Ukraine, and Pakistan, with potentially disastrous results. Access to therapeutic opioid medications is regulated by specific provisions in UN conventions, and these treaties recognise them as indispensable for medical care.134 Despite this benefit, treatment for dependency with opiates is not available in Kenya, where the amount of morphine available for palliative care was 0.14 mg per head in 2004—less than 2.5% of the global mean of 5.9 mg per head.135 One hospice physician stated “Physicians are afraid of morphine...Doctors [in Kenya] are so used to patients dying in pain...they think that this is how you must die. They are suspicious if you don’t die this way—[and feel] that you died prematurely.”136 These reports suggest a substantial disconnect between drug-control authorities and the health-care system.137 Similar to many other lowincome and middle-income countries, national drug control authorities in Kenya have concentrated more on control of illicit use than on facilitation of legitimate medical use.138 WHO’s guidelines for assessment of national opioid control policies adopted in 2000 are anchored in a four-pillar approach aimed at achievement of a balance so drug control does not interfere with medical availability of opioid analgesics for pain relief and opioid substitution.139 Our model suggests that legislative changes to permit opioid substitution in IDUs in Nairobi could prevent up to 14% of new HIV infections in the next 5 years, assuming 80% coverage.
Apart from the need for enhanced HIV and drug addiction prevention and treatment programmes and policies in Karachi, HIV epidemic projections advocate prevention of the transition from use of non-injection drugs to injection drugs. In Pakistan, where the number of people who smoke or inhale heroin is substantial,107 macroenvironmental changes in drug trafficking routes that change the availability, purity, or price of heroin can lead to increased transitions from non-injecting to injecting drug use, as was reported after the terrorist attacks of Sept 11, 2001.140
Our modelling scenarios suggest that an 8–12% increase in transition from non-injection drug use to injection drug use, even in the short-term, could lead to around a 65–98% rise in HIV incidence in Karachi in the next 5 years. Such effects are potentiated in the absence of opioid substitution, which could otherwise have a substantial benefit via reduction of the frequency and duration of injections. These findings suggest the need to invest in interventions to prevent transitions to injection and monitoring of perceived changes in local drug markets that might serve as harbingers of changes in injection behaviours.
Modelling limitations
Our modelling analysis allowed a direct quantification of the uncertainty in projections, leveraging substantial information from a wide range of sources. We showed patterns and trends in common with previous work,112–114 and the explosive HIV epidemics occurring in Vancouver, Canada and Kathmandu, Nepal despite the existence of needle and syringe programmes.141,142 Estimates of HIV prevalence in IDUs are a good source of epidemiological information, allowing model projections for Odessa and Karachi to be based on direct observational data.
However, our modelling results are limited by the need to make detailed assumptions about forms of behaviour that are highly stigmatised in a hard-to-reach population. Some of the most important model variables, such as IDU population size and the frequency with which IDUs were exposed to potentially contaminated syringes were imprecisely estimated. Reporting of highly stigmatised behaviours can be unreliable. If individuals under-report injecting behaviour, investigators can overestimate the rate of spread of infection or degree of epidemic saturation. If injecting behaviour is under-reported compared with sexual behaviour, the model could overestimate the contribution of sex in epidemics. There tend to be few estimates of HIV prevalence at the start of the epidemic, so the time and speed of initial spread cannot be known precisely. This uncertainty leads to substantial doubt about model projections for future courses of local HIV epidemics, especially because the link between risk behaviours and HIV acquisition is complex, and warrants caution in interpretation of our findings.114
Our models used a straightforward representation of opioid substitution and needle and syringe programmes; the effects of opioid substitution on non-HIV mortality and individuals moving in and out of programmes were not captured here, although they are addressed elsewhere in this Series.133 The deterministic framework used in our models constrained characterisation of the network of contacts between IDUs, and might have influenced our results. If a more complex network topology were represented, for example with distinction of isolated pockets of high-risk behaviour within the IDU population, then the modelled spread of infection might have been more gradual in Karachi, compared with the explosive spread suggested by our model, and therefore the predicted effect of interventions would be reduced. The Nairobi model assumed a homogeneous IDU population that, although not unreasonable on the basis of available reports from outreach groups, could have led to overestimation of the potential for epidemic growth in this population.
Survey data capturing intersecting types of risk in IDU populations and links between IDUs and other at-risk groups, and improved measurement of HIV prevalence, will be most valuable for development of our understanding of epidemics, and modelling and assessment of the effects of interventions.
Conclusion
Many types of environmental influence are important determinants of HIV risk and vulnerability. The modelling scenarios we present support the importance of simultaneously scaling up the coverage of HIV prevention programmes in IDUs (ie, opioid substitution therapy, needle and syringe programmes, or antiretroviral therapy) to produce the best outcomes with their synergistic potential. Adequate coverage of these interventions could not only avert thousands of HIV infections, but also substantially reduce local HIV epidemics through protection of the rights of IDUs to HIV prevention and treatment.
Our findings support the need to shift the focus for change from individuals to their social and political contexts, shifting responsibility for harm to include the social and political–economic institutions that have a role in harm production.11 Through revelation of the social, political, and economic dimensions of HIV transmission, a risk environment approach allows epidemiology to contribute to strategies for reduction of adverse health outcomes driven by health inequities and social suffering. Creation of enabling environments for HIV prevention is synonymous with the promotion of health and human rights.
Supplementary Material
Acknowledgments
This report was funded by the US National Institute on Drug Abuse grant DA027772-S1, the US Office of AIDS Research, and The Wellcome Trust (UK). RB was supported by a US NIH grant (RO1DA17620). We thank Christy Anderson, Richard Armenta, Annick Borquez, Philippe Bourgois, David Celentano, Jessica Cubeta, Penny Coppernoll-Blach, Anna Dovbah, Faran Emmanuel, Samuel R Friedman, Micah Gell-Redman, Eleanor Gouws, Mauro Guarinieri, Peter Hartsock, Brian Houle, Francisco I Bastos, Natalia Kitsenko, Robert Malow, Bradley Mathers, Lisovska Oksana, Jane Marie Ongo’lo, Samiran Panda, Natalia Rehtina, Diana Rossi, Richard Rothenberg, Tatyana Saliuk, Oleg Semeryk, Ani Shakarishvili, Alexandra Thomas, Emily To, Lucas Wiessing, Daniel Wolfe, and Carl Latkin.
Footnotes
Steering committee
This article is part of The Lancet Series on HIV in people who use drugs, which was developed and coordinated by Chris Beyrer (Center for Public Health and Human Rights, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA); Steff anie Strathdee (University of California, San Diego, CA, USA); Adeeba Kamarulzaman (University of Malaya, Kuala Lumpur, Malaysia); and Kasia Malinowska-Sempruch (Open Society Institute, Drug Policy Program, Warsaw, Poland).
Conflicts of interest
We declare that we have no conflicts of interest.
Contributor Information
Steffanie A Strathdee, Department of Medicine, University of California, San Diego, Division of Global Public Health, CA, USA.
Timothy B Hallett, Imperial College, London,London, UK.
Natalia Bobrova, University College London, UK.
Tim Rhodes, London School of Hygiene and Tropical Medicine, University of London, UK.
Robert Booth, University of Colorado Denver, CO, USA.
Reychad Abdool, United Nations Office on Drugs and Crime, Regional Office for Eastern Africa, Kenya.
Catherine A Hankins, Joint United Nations Programme on HIV/AIDS, Geneva, Switzerland.
References
- 1.Mathers BM, Degenhardt L, Phillips B, et al. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Lancet 2008; 372: 1733–45. [DOI] [PubMed] [Google Scholar]
- 2.Santibanez SS, Garfein RS, Swartzendruber A, Purcell DW, Paxton LA, Greenberg AE. Update and overview of practical epidemiologic aspects of HIV/AIDS among injection drug users in the United States. J Urban Health 2006; 83: 86–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Latkin CA, Forman V, Knowlton A, Sherman S. Norms, social networks, and HIV-related risk behaviors among urban disadvantaged drug users. Soc Sci Med 2003; 56: 465–76. [DOI] [PubMed] [Google Scholar]
- 4.Des Jarlais DC, Arasteh K, Perlis T, et al. Convergence of HIV seroprevalence among injecting and non-injecting drug users in New York City. AIDS 2007; 21: 231–35. [DOI] [PubMed] [Google Scholar]
- 5.Booth RE, Kwiatkowski CF, Brewster JT, Sinitsyna L, Dvoryak S. Predictors of HIV sero-status among drug injectors at three Ukraine sites. AIDS 2006; 20: 2217–23. [DOI] [PubMed] [Google Scholar]
- 6.Panda S, Chatterjee A, Bhattacharya SK, et al. Transmission of HIV from injecting drug users to their wives in India. Int J STD AIDS 2000; 11: 468–73. [DOI] [PubMed] [Google Scholar]
- 7.Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Soc Sci Med 2005; 61: 1026–44. [DOI] [PubMed] [Google Scholar]
- 8.Poundstone KE, Strathdee SA, Celentano DD. The social epidemiology of human immunodeficiency virus/acquired immunodeficiency syndrome. Epidemiol Rev 2004; 26: 22–35. [DOI] [PubMed] [Google Scholar]
- 9.Galea S, Nandi A, Vlahov D. The social epidemiology of substance use. Epidemiol Rev 2004; 26: 36–52. [DOI] [PubMed] [Google Scholar]
- 10.Blankenship KM, Friedman SR, Dworkin S, Mantell JE. Structural interventions: Concepts, challenges and opportunities for research. J Urban Health 2006; 83: 59–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rhodes T Risk environments and drug harms: a social science for harm reduction approach. Int J Drug Policy 2009; 20: 193–201. [DOI] [PubMed] [Google Scholar]
- 12.Rothenberg R, Baldwin J, Trotter R, Muth S. The risk environment for HIV transmission: results from the Atlanta and Flagstaff network studies. J Urban Health 2001; 78: 419–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rhodes T, Simic M. Transition and the HIV risk environment. BMJ 2005; 331: 220–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med 2006; 62: 1650–71. [DOI] [PubMed] [Google Scholar]
- 15.Strathdee SA, Galai N, Safaiean M, et al. Sex differences in risk factors for HIV seroconversion among injection drug users: a 10-year perspective. Arch Intern Med 2001; 161: 1281–88. [DOI] [PubMed] [Google Scholar]
- 16.Panda S, Kumar MS, Lokabiraman S, et al. Risk factors for HIV infection in injection drug users and evidence for onward transmission of HIV to their sexual partners in Chennai, India. J Acquir Immune Defic Syndr 2005; 39: 9–15. [DOI] [PubMed] [Google Scholar]
- 17.Wylie JL, Shah L, Jolly AM. Demographic, risk behaviour and personal network variables associated with prevalent hepatitis C, hepatitis B, and HIV infection in injection drug users in Winnipeg, Canada. BMC Public Health 2006; 6: 229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zamani S, Kihara M, Gouya MM, et al. Prevalence of and factors associated with HIV-1 infection among drug users visiting treatment centers in Tehran, Iran. AIDS 2005; 19: 709–16. [DOI] [PubMed] [Google Scholar]
- 19.March JC, Oviedo-Joekes E, Romero M. Factors associated with reported hepatitis C and HIV among injecting drug users in ten European cities. Enferm Infecc Microbiol Clin 2007; 25: 91–97 [DOI] [PubMed] [Google Scholar]
- 20.Hu DJ, Subbarao S, Vanichseni S, et al. Higher viral loads and other risk factors associated with HIV-1 seroconversion during a period of high incidence among injection drug users in Bangkok. J Acquir Immune Defic Syndr 2002; 30: 240–47 [DOI] [PubMed] [Google Scholar]
- 21.Buavirat A, Page-Shafer K, van Griensven GJ, et al. Risk of prevalent HIV infection associated with incarceration among injecting drug users in Bangkok, Thailand: case-control study. BMJ 2003; 326: 308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zamani S, Kihara M, Gouya MM, et al. High prevalence of HIV infection associated with incarceration among community-based injecting drug users in Tehran, Iran. J Acquir Immune Defic Syndr 2006; 42: 342–46. [DOI] [PubMed] [Google Scholar]
- 23.Kheirandish P, Seyedalinaghi SA, Hosseini M, et al. Prevalence and correlates of HIV infection among male injection drug users in detention, Tehran, Iran. J Acquir Immune Defic Syndr 2009; 53: 273–75. [DOI] [PubMed] [Google Scholar]
- 24.Nelson KE, Galai N, Safaeian M, Strathdee SA, Celentano DD, Vlahov D. Temporal trends in the incidence of human immunodeficiency virus infection and risk behavior among injection drug users in Baltimore, Maryland, 1988; 156: 641–53. [DOI] [PubMed] [Google Scholar]
- 25.Reyes JC, Robles RR, Colon HM, et al. Homelessness and HIV risk behaviors among drug injectors in Puerto Rico. J Urban Health 2005; 82: 446–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Azim T, Chowdhury EI, Reza M, et al. Prevalence of infections, HIV risk behaviors and factors associated with HIV infection among male injecting drug users attending a needle/syringe exchange program in Dhaka, Bangladesh. Subst Use Misuse 2008; 43: 2124–44. [DOI] [PubMed] [Google Scholar]
- 27.Tyndall MW, Currie S, Spittal P, et al. Intensive injection cocaine use as the primary risk factor in the Vancouver HIV-1 epidemic. AIDS 2003; 17: 887–93. [DOI] [PubMed] [Google Scholar]
- 28.Zhang Y, Shan H, Trizzino J, et al. HIV incidence, retention rate, and baseline predictors of HIV incidence and retention in a prospective cohort study of injection drug users in Xinjiang, China. IntJ Infect Dis 2007; 11: 318–23. [DOI] [PubMed] [Google Scholar]
- 29.Estebanez PE, Russell NK, Aguilar MD, Beland F, Zunzunegui MV. Women, drugs and HIV/AIDS: results of a multicentre European study. Int J Epidemiol 2000; 29: 734–43. [DOI] [PubMed] [Google Scholar]
- 30.Wood E, Kerr T, Marshall BD, et al. Longitudinal community plasma HIV-1 RNA concentrations and incidence of HIV-1 among injecting drug users: prospective cohort study. BMJ 2009; 338: b1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boileau C, Bruneau J, Al-Nachawati H, Lamothe F, Vincelette J. A prognostic model for HIV seroconversion among injection drug users as a tool for stratification in clinical trials. J Acquir Immune Defic Syndr 2005; 39: 489–95. [DOI] [PubMed] [Google Scholar]
- 32.Barrio G, De La Fuente L, Toro C, et al. Prevalence of HIV infection among young adult injecting and non-injecting heroin users in Spain in the era of harm reduction programmes: gender differences and other related factors. Epidemiol Infect 2007; 135: 592–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Beyrer C, Jittiwutikarn J, Teokul W, et al. Drug use, increasing incarceration rates, and prison-associated HIV risks in Thailand. AIDS Behav 2003; 7: 153–61. [DOI] [PubMed] [Google Scholar]
- 34.Choopanya K, Des Jarlais DC, Vanichseni S, et al. Incarceration and risk for HIV infection among injection drug users in Bangkok. J Acquir Immune Defic Syndr 2002; 29: 86–94. [DOI] [PubMed] [Google Scholar]
- 35.Estebanez P, Russell NK, Aguilar MD, Cifuentes I, Zunzunegui MV, McPherson K. Determinants of HIV prevalence amongst female IDU in Madrid. Eur J Epidemiol 2001; 17: 573–80. [DOI] [PubMed] [Google Scholar]
- 36.Hacker MA, Friedman SR, Telles PR, et al. The role of “long-term” and “new” injectors in a declining HIV/AIDS epidemic in Rio de Janeiro, Brazil. Subst Use Misuse 2005; 40: 99–123. [DOI] [PubMed] [Google Scholar]
- 37.Koshkina EA, Kirghanova VV, Rhodes T, Platt L. HIV and HCV risk factors among injecting drug users in Moscow. Narcologija 2005; 5: 16–20. [Google Scholar]
- 38.Stark K, Herrmann U, Ehrhardt S, Bienzle U. A syringe exchange programme in prison as prevention strategy against HIV infection and hepatitis B and C in Berlin, Germany. Epidemiol Infect 2006; 134: 814–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vanichseni S, Kitayaporn D, Mastro TD, et al. Continued high HIV-1 incidence in a vaccine trial preparatory cohort of injection drug users in Bangkok, Thailand. AIDS 2001; 15: 397–405. [DOI] [PubMed] [Google Scholar]
- 40.Spittal PM, Craib KJ, Teegee M, et al. The Cedar project: prevalence and correlates of HIV infection among young Aboriginal people who use drugs in two Canadian cities. Int J Circumpolar Health 2007; 66: 226–40. [PubMed] [Google Scholar]
- 41.Strathdee SA, Lozada R, Ojeda VD, et al. Differential effects of migration and deportation on HIV infection among male and female injection drug users in Tijuana, Mexico. PLoS One 2008; 3: e2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Booth RE, Mikulich-Gilbertson SK, Brewster JT, Salomonsen-Sautel S, Semerik O. Predictors of self-reported HIV infection among drug injectors in Ukraine. J Acquir Immune Defic Syndr 2004; 35: 82–88. [DOI] [PubMed] [Google Scholar]
- 43.Mehrabadi A, Paterson K, Pearce M, et al. Gender differences in HIV and hepatitis C related vulnerabilities among aboriginal young people who use street drugs in two Canadian cities. Women Health 2008; 48: 235–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.De La Fuente L, Bravo MJ, Toro C, et al. Injecting and HIV prevalence among young heroin users in three Spanish cities and their association with the delayed implementation of harm reduction programmes. J Epidemiol Community Health 2006; 60: 537–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maas B, Fairbairn N, Kerr T, Li K, Montaner JS, Wood E. Neighborhood and HIV infection among IDU: place of residence independently predicts HIV infection among a cohort of injection drug users. Health Place 2007; 13: 432–39. [DOI] [PubMed] [Google Scholar]
- 46.Zhang L, Zhu J, Rui B, et al. High HIV risk among Uigur minority ethnic drug users in northwestern China. Trop Med Int Health 2008; 13: 814–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wood E, Lloyd-Smith E, Li K, et al. Frequent needle exchange use and HIV incidence in Vancouver, Canada. Am J Med 2007; 120: 172–79. [DOI] [PubMed] [Google Scholar]
- 48.Neaigus A, Zhao M, Gyarmathy VA, Cisek L, Friedman SR, Baxter RC. Greater drug injecting risk for HIV, HBV, and HCV infection in a city where syringe exchange and pharmacy syringe distribution are illegal. J Urban Health 2008; 85: 309–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rhodes T, Lowndes C, Judd A, et al. Explosive spread and high prevalence of HIV infection among injecting drug users in Togliatti City, Russia. AIDS 2002; 16: F25–31. [DOI] [PubMed] [Google Scholar]
- 50.Emmanuel F, Archibald C, Razaque A, Sandstrom P. Factors associated with an explosive HIV epidemic among injecting drug users in Sargodha, Pakistan. J Acquir Immune Defic Syndr 2009; 51: 85–90. [DOI] [PubMed] [Google Scholar]
- 51.Strathdee SA, Lozada R, Pollini RA, et al. Individual, social, and environmental influences associated with HIV infection among injection drug users in Tijuana, Mexico. J Acquir Immune Defic Syndr 2008; 47: 369–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Williams ML, McCurdy SA, Bowen AM, et al. HIV seroprevalence in a sample of Tanzanian intravenous drug users. AIDS Educ Prev 2009; 21: 474–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shafer KP, Hahn JA, Lum PJ, Ochoa K, Graves A, Moss A. Prevalence and correlates of HIV infection among young injection drug users in San Francisco. J Acquir Immune Defic Syndr 2002; 31: 422–31. [DOI] [PubMed] [Google Scholar]
- 54.Hien NT, Giang LT, Binh PN, Deville W, Van Ameijden EJC, Wolffers I. Risk factors of HIV infection and needle sharing among injecting drug users in Ho Chi Minh City, Vietnam. J Subst Abuse 2001; 13: 45–58. [DOI] [PubMed] [Google Scholar]
- 55.Vertefeuille J, Strathdee SA, Huettner S, Brown M, Vlahov D. Factors associated with HIV seroprevalence among participants enrolling at a needle exchange program. J Drug Issues 2002; 32: 1125–38. [Google Scholar]
- 56.Rhodes T, Platt L, Maximova S, et al. Prevalence of HIV, hepatitis C and syphilis among injecting drug users in Russia: a multi-city study. Addiction 2006; 101: 252–66. [DOI] [PubMed] [Google Scholar]
- 57.Platt L, Bobrova N, Rhodes T, et al. High HIV prevalence among injecting drug users in Estonia: implications for understanding the risk environment. AIDS 2006; 20: 2120–23. [DOI] [PubMed] [Google Scholar]
- 58.Welp EA, Lodder AC, Langendam MW, Coutinho RA, van Ameijden EJ. HIV prevalence and risk behaviour in young drug users in Amsterdam. AIDS 2002; 16: 1279–84. [DOI] [PubMed] [Google Scholar]
- 59.Hankins C, Alary M, Parent R, Blanchette C, Claessens C, the SurvUDI Working Group. Continuing HIV transmission among injection drug users in Eastern Central Canada: the SurvUDI Study, 1995 to 2000. J Acquir Immune Defic Syndr 2002; 30: 514–21. [DOI] [PubMed] [Google Scholar]
- 60.Tuan NA, Fylkesnes K, Thang BD, et al. Human immunodeficiency virus (HIV) infection patterns and risk behaviours in different population groups and provinces in Viet Nam. Bull World Health Organ 2007; 85: 35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Liu W, Chen J, Rodolph M, et al. HIV prevalence among injection drug users in rural Guangxi China. Addiction 2006; 101: 1493–98. [DOI] [PubMed] [Google Scholar]
- 62.Rondinelli AJ, Ouellet LJ, Strathdee SA, et al. Young adult injection drug users in the United States continue to practice HIV risk behaviors. Drug Alcohol Depend 2009; 104: 167–74. [DOI] [PubMed] [Google Scholar]
- 63.Beyrer C, Patel Z, Stachowiak JA, et al. Characterization of the emerging HIV type 1 and HCV epidemics among injecting drug users in Dushanbe, Tajikistan. AIDS Res Hum Retroviruses 2009; 25: 853–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kral AH, Bluthenthal RN, Lorvick J, Gee L, Bacchetti P, Edlin BR. Sexual transmission of HIV-1 among injection drug users in San Francisco, USA: risk-factor analysis. Lancet 2001; 357: 1397–401. [DOI] [PubMed] [Google Scholar]
- 65.Stachowiak JA, Tishkova FK, Strathdee SA, et al. Marked ethnic differences in HIV prevalence and risk behaviors among injection drug users in Dushanbe, Tajikistan, 2004. Drug Alcohol Depend 2006; 82 (suppl 1): S7–14. [DOI] [PubMed] [Google Scholar]
- 66.O’Connell JM, Kerr T, Li K, et al. Requiring help injecting independently predicts incident HIV infection among injection drug users. J Acquir Immune Defic Syndr 2005; 40: 83–88. [DOI] [PubMed] [Google Scholar]
- 67.Spittal PM, Craib KJ, Wood E, et al. Risk factors for elevated HIV incidence rates among female injection drug users in Vancouver. CMAJ 2002; 166: 894–99. [PMC free article] [PubMed] [Google Scholar]
- 68.Diaz T, Vlahov D, Greenberg B, Cuevas Y, Garfein R. Sexual orientation and HIV infection prevalence among young Latino injection drug users in Harlem. J Womens Health Gend Based Med 2001; 10: 371–80. [DOI] [PubMed] [Google Scholar]
- 69.Salmon AM, Van Beek I, Amin J, Grulich A, Maher L. High HIV testing and low HIV prevalence among injecting drug users attending the Sydney Medically Supervised Injecting Centre. Aust N Z J Public Health 2009; 33: 280–83. [DOI] [PubMed] [Google Scholar]
- 70.Chitwood DD, Comerford M, Sanchez J. Prevalence and risk factors for HIV among sniffers, short-term injectors, and long-term injectors of heroin. J Psychoactive Drugs 2003; 35: 445–53. [DOI] [PubMed] [Google Scholar]
- 71.Doherty MC, Garfein RS, Monterroso E, Brown D, Vlahov D. Correlates of HIV infection among young adult short-term injection drug users. AIDS 2000; 14: 717–26. [DOI] [PubMed] [Google Scholar]
- 72.Kral AH, Lorvick J, Gee L, et al. Trends in human immunodeficiency virus seroincidence among street-recruited injection drug users in San Francisco, 1987–1998. Am J Epidemiol 2003; 157: 915–22. [DOI] [PubMed] [Google Scholar]
- 73.Maslow CB, Friedman SR, Perlis TE, Rockwell R, Des Jarlais DC. Changes in HIV seroprevalence and related behaviors among male injection drug users who do and do not have sex with men: New York City, 1990–1999. Am J Public Health 2002; 92: 382–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ouellet LJ, Thorpe LE, Huo D, et al. Prevalence and incidence of HIV among out-of-treatment injecting drug users, Chicago 1994–1996. J Acquir Immune Defic Syndr 2000; 25: 443–50. [DOI] [PubMed] [Google Scholar]
- 75.Friedman SR, Cooper HL, Tempalski B, et al. Relationships of deterrence and law enforcement to drug-related harms among drug injectors in US metropolitan areas. AIDS 2006; 20: 93–99. [DOI] [PubMed] [Google Scholar]
- 76.Zhang Y, Shan H, Trizzino J, et al. Demographic characteristics and risk behaviors associated with HIV positive injecting drug users in Xinjiang, China. J Infect 2007; 54: 285–90. [DOI] [PubMed] [Google Scholar]
- 77.Des Jarlais DC, Kling R, Hammett TM, et al. Reducing HIV infection among new injecting drug users in the China–Vietnam Cross Border Project. AIDS 2007; 21 (suppl 8): S109–14. [DOI] [PubMed] [Google Scholar]
- 78.Sanchez JL, Todd CS, Bautista CT, et al. High HIV prevalence and risk factors among injection drug users in Tashkent, Uzbekistan, 2003–2004. Drug Alcohol Depend 2006; 82 (suppl 1): S15–22. [DOI] [PubMed] [Google Scholar]
- 79.Niccolai LM, Toussova OV, Verevochkin SV, Barbour R, Heimer R, Kozlov AP. High HIV prevalence, suboptimal HIV testing, and low knowledge of HIV-positive serostatusamong injection drug users in St Petersburg, Russia. AIDS Behav 2008; published online Oct 9. DOI: 10.1007/s10461-008-9469-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Platt L, Rhodes T, Hickman M, et al. Changes in HIV prevalence and risk among new injecting drug users in a Russian city of high HIV prevalence. J Acquir Immune Defic Syndr 2008; 47: 623–31. [DOI] [PubMed] [Google Scholar]
- 81.Vorobjov S, Uuskula A, Abel-Ollo K, Talu A, Ruutel K, Des Jarlais DC. Comparison of injecting drug users who obtain syringes from pharmacies and syringe exchange programs in Tallinn, Estonia. Harm Reduct J 2009; 6: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Van Den Berg C, Smit C, Van Brussel G, Coutinho R, Prins M, Amsterdam Cohort. Full participation in harm reduction programmes is associated with decreased risk for human immunodeficiency virus and hepatitis C virus: evidence from the Amsterdam Cohort Studies among drug users. Addiction 2007; 102: 1454–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Suntharasamai P, Martin M, Vanichseni S, et al. Factors associated with incarceration and incident human immunodeficiency virus (HIV) infection among injection drug users participating in an HIV vaccine trial in Bangkok, Thailand, 1999–2003. Addiction 2009; 104: 235–42. [DOI] [PubMed] [Google Scholar]
- 84.Tran TMT, Nguyen HT, Yatsuya H, Hamajima N, Nishimura A, Ito K. HIV prevalence and factors associated with HIV infection among male injection drug users under 30: a cross-sectional study in Long An, Vietnam. BMC Public Health 2006; 6: 248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Friedman SR, Perlis T, Des Jarlais DC. Laws prohibiting over-the-counter syringe sales to injection drug users: relations to population density, HIV prevalence, and HIV incidence. Am J Public Health 2001; 91: 791–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mesquita F, Kral A, Reingold A, et al. Trends of HIV infection among injection drug users in Brazil in the 1990s: the impact of changes in patterns of drug use. J Acquir Immune Defic Syndr 2001; 28: 298–302. [DOI] [PubMed] [Google Scholar]
- 87.Israilov B Results of epidemiological surveillance of HIV in the Kyrgyz Republic. Epidemiol Infect Dis 2008; 4: 8–10. [Google Scholar]
- 88.Miller CL, Kerr T, Frankish JC, et al. Binge drug use independently predicts HIV seroconversion among injection drug users: implications for public health strategies. Subst Use Misuse 2006; 41: 199–210. [DOI] [PubMed] [Google Scholar]
- 89.Des Jarlais DC, Arasteh K, Hagan H, McKnight C, Perlman DC, Friedman SR. Persistence and change in disparities in HIV infection among injection drug users in New York City after large-scale syringe exchange programs. Am J Public Health 2009; 99 (suppl 2): S445–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ruan Y, Qin G, Yin L, et al. Incidence of HIV, hepatitis C and hepatitis B viruses among injection drug users in southwestern China: a 3-year follow-up study. AIDS 2007; 21 (suppl 8): S39–46. [DOI] [PubMed] [Google Scholar]
- 91.Spittal P, Bruneau J, Craib K, et al. Surviving the sex trade: a comparison of HIV risk behaviours among street-involved women in two Canadian cities who inject drugs. AIDS Care 2003; 15: 187–95. [DOI] [PubMed] [Google Scholar]
- 92.Yin L, Qin G, Qian HZ, et al. Continued spread of HIV among injecting drug users in southern Sichuan Province, China. Harm Reduct J 2007; 4: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lopez-Zetina J, Kerndt P, Ford W, Woerhle T, Weber M. Prevalence of HIV and hepatitis B and self-reported injection risk behavior during detention among street-recruited injection drug users in Los Angeles County, 1994–1996. Addiction 2001; 96: 589–95. [DOI] [PubMed] [Google Scholar]
- 94.Balakireva O, Semerik O, Guk A, et al. Situational analysis with HIV/AIDS epidemic in Odesa region, and analysis of couTER-reaction USAID, Kiev, Ukraine: Vydavnytstvo Raevskogo, 2006. [Google Scholar]
- 95.Balakireva O, Bochkova L, Galich JU, et al. Behavior monitoring of injection drug users as a component of second generation surveillance Kiev: International HIV/AIDS Alliance in Ukraine 2005. http://www.aidsalliance.org.ua/ru/library/our/monitoring_reports/pdf/idu.pdf (accessed Sept 9, 2009). [Google Scholar]
- 96.Balakireva O, Bondar T, Denisjuk A. Behavior monitoring of injection drug users as a component of second generation surveillance. Kiev: International HIV/AIDS Alliance in Ukraine; 2007. http://www.aidsalliance.org.ua/ru/library/our/monitoring_reports/pdf/report_IDU_rus.pdf (accessed Sept 9, 2009). [Google Scholar]
- 97.Pohorila NB, Dieva TS, Maksomov MY. Analytical report based on 2008 survey results: monitoring the behavior of injecting drug users. Kiev: SOCIS-CSPS and the ICF International HIV/AIDS Alliance in Ukraine; 2008; http://www.aidsalliance.org.ua/ru/library/our/monitoring_reports/pdf/IDU_report_2008_engl.pdf (accessed March 13, 2010). [Google Scholar]
- 98.Balakireva O Behavior monitoring of youth as a component of second generation surveillance. Kiev: International HIV/AIDS Alliance in Ukraine; 2005. http://www.aidsalliance.org.ua/ru/library/our/monitoring_reports/pdf/youth.pdf (accessed Sept 4, 2010). [Google Scholar]
- 99.Booth RE, Lehman WE, Dvoryak S, Brewster JT, Sinitsyna L. Interventions with injection drug users in Ukraine. Addiction 2009; 104: 1864–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rhodes T, Ball A, Stimson GV, et al. HIV infection associated with drug injecting in the newly independent states, eastern Europe: the social and economic context of epidemics. Addiction 1999; 94: 1323–36. [DOI] [PubMed] [Google Scholar]
- 101.National AIDS Control Programme. HIV second generation surveillance in Pakistan: national report round III. 2007–2008. Islamabad, Pakistan: National AIDS Control Programme, 2008. [Google Scholar]
- 102.Agha A, Parviz S, Younus M, Fatmi Z. Socio-economic and demographic factors associated with injecting drug use among drug users in Karachi, Pakistan. J Pak Med Assoc 2006; 56 (suppl 1): S55–60. [PubMed] [Google Scholar]
- 103.Khuwaja A, Ali N, Zafar A. Use of psychoactive drugs among patients visiting outpatient clinics in Karachi, Pakistan. Singapore Med J 2007; 48: 509–13. [PubMed] [Google Scholar]
- 104.Parviz S, Fatmi Z, Altaf A, et al. Background demographics and risk behaviors of injecting drug users in Karachi, Pakistan. Int J Infect Dis 2006; 10: 364–71. [DOI] [PubMed] [Google Scholar]
- 105.Altaf A, Shah SA, Zaidi NA, Memon A, Nadeem uR, Wray N High risk behaviors of injection drug users registered with harm reduction programme in Karachi, Pakistan. Harm Reduct J 2007; 4: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bokhari A, Nizamani NM, Jackson DJ, et al. HIV risk in Karachi and Lahore, Pakistan: an emerging epidemic in injecting and commercial sex networks. Int J STD AIDS 2007; l8: 486–92. [DOI] [PubMed] [Google Scholar]
- 107.Emmanuel F, Fatima M. Coverage to curb the emerging HIV epidemic among injecting drug users in Pakistan: delivering prevention services where most needed. Int J Drug Policy 2008; 19 (suppl 1): S59–64. [DOI] [PubMed] [Google Scholar]
- 108.United Nations Drug Control Programme Global Assessment Programme on Drug Abuse. Report on Pakistan. Vienna, Austria: UNODC, 2002. [Google Scholar]
- 109.Mathers BM, Degenhardt L, Ali H, et al. HIV prevention, treatment, and care services for people who inject drugs: a systematic review of global, regional, and national coverage. Lancet 2010; 375: 1014–28. [DOI] [PubMed] [Google Scholar]
- 110.UNODC. Nairobi outreach services trust UNODC report on contacts. Nairobi, Kenya: UNODC ROEA project database, 2009. [Google Scholar]
- 111.UNODC. A study on the linkages between drug abuse, injecting drug use and HIV/AIDS in Kenya: a rapid situation assessment. Nairobi, Kenya: UNODC ROEA project database, 2004. [Google Scholar]
- 112.Grassly NC, Lowndes CM, Rhodes T, Judd A, Garnett GP. Modelling emerging HIV epidemics: the role of injecting drug use and sexual transmission in the Russian Federation, China and India. Int J Drug Policy 2003; 14: 25–43. [Google Scholar]
- 113.Vickerman P, Kumaranayake L, Balakireva O, et al. The cost-effectiveness of expanding harm reduction activities for injecting drug users in Odessa, Ukraine. Sex Transm Dis 2006; 33 (10 suppl): S89–102. [DOI] [PubMed] [Google Scholar]
- 114.Blower SM, Hartel D, Dowlatabadi H, Anderson RM, May RM. Drugs, sex and HIV: a mathematical model for New York City. Philos Trans R Soc Lond B Biol Sci 1991; 331: 171–87. [DOI] [PubMed] [Google Scholar]
- 115.WHO. Rapid advice: antiretroviral therapy for HIV infection in adults and adolescents, 2009. http://www.who.int/hiv/pub/arv/advice/en/ (accessed Feb 2, 2010).
- 116.Gouws E, White PJ, Stover J, Brown T. Short term estimates of adult HIV incidence by mode of transmission: Kenya and Thailand as examples. Sex Transm Infect 2006; 82 (suppl 3): iii51–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Gelmon L, Kenya P, Oguya F, Cheluget B, Haile G. UNAIDS: Kenya HIV prevention response and modes of transmission (MoT) analysis, 2009. http://www.unaidsrstesa.org/files/u1/Kenya_MoT_Country_Synthesis_Report_22Mar09.pdf (accessed Sept 5, 2009). [Google Scholar]
- 118.Ministry of Health of Ukraine. National report on monitoring progress towards the UNGLASS (United National General Assembly Special Session) declaration of commitment on HIV/ AIDS. 2008. http://www.unaids.org/en/CountryResponses/Countries/ukraine.asp (accessed Jan 1, 2010). [Google Scholar]
- 119.World Bank, International HIV/AIDS Alliance in Ukraine . Socioeconomic impact of HIV/AIDS in Ukraine. Washington, DC, USA: Library of Congress, 2006. [Google Scholar]
- 120.WHO Regional Office for Europe. Sexually transmitted infections/HIV/AIDS: WHO/Europe survey on HIV/AIDS and antiretroviral therapy 2006 programme. Copenhagen, Denmark: World Health Organization, 2007. [Google Scholar]
- 121.Barnett T, Whiteside A, Khodakevich L, Kruglov Y, Steshenko V. The HIV/AIDS epidemic in Ukraine: its potential social and economic impact. Soc Sci Med 2000; 51: 1387–403. [DOI] [PubMed] [Google Scholar]
- 122.EHRN. Young people & injecting drug use in selected countries of Central and Eastern Europe. Vilnius, Lithuania: Eurasian Harm Reduction Network, 2009. [Google Scholar]
- 123.Burris S, Strathdee SA. To serve and protect? Toward a better relationship between drug control policy and public health. AIDS 2006; 20: 117–18. [DOI] [PubMed] [Google Scholar]
- 124.Booth RE, Dvoryak S, Anderson C, Brewster JT, Strathdee SA. Police brutality is independently associated with sharing injection equipment among injection drug users in Odessa, Ukraine. XVI Conference of the International AIDS Society; Vienna, Austria; July 18, 2010 (abstr 9260). [Google Scholar]
- 125.UNAIDS. Report on the global AIDS epidemic. 2008. http://www.unaids.org/en/KnowledgeCentre/HIVData/GlobalReport/2008/2008_Global_report.asp (accessed Aug 26, 2009). [Google Scholar]
- 126.Mayhew S, Collumbien M, Qureshi A, et al. Protecting the unprotected: mixed-method research on drug use, sex work and rights in Pakistan’s fight against HIV/AIDS. Sex Transm Infect 2009; 85: ii31–36. [DOI] [PubMed] [Google Scholar]
- 127.UNODC project KENI08. Prevention of HIV and AIDS in high-risk settings among vulnerable populations in Kenya. 2009. [Google Scholar]
- 128.Odek-Ogunde M, Lore W, Owiti FR. Risky behaviours among injecting drug users in Kenya. Proceedings of 14th International Conference on the Reduction of Drug Related Harm. Chiang Mai, Thailand; April 6–10, 2003. [Google Scholar]
- 129.Dewing S, Pluddemann A, Meyers B, Parry C. Review of injection drug use in six African countries: Egypt, Kenya, Mauritius, Nigeria, South Africa and Tanzania. Drugs Educ Prev Pol 2006; 13: 121–37 [Google Scholar]
- 130.WHO/UNAIDS/UNICEF. Scaling up priority HIV/AIDS interventions in the health sector: progress report. Geneva, Switzerland: World Health Organization, UNAIDS, United Nations International Children’s Fund, 2009. [Google Scholar]
- 131.Gupta GR, Parkhurst JO, Ogden JA, Aggleton P, Mahal A. Structural approaches to HIV prevention. Lancet 2008; 372: 764–75. [DOI] [PubMed] [Google Scholar]
- 132.Wolfe D, Carrieri MP, Shepard D. Treatment and care for injecting drug users with HIV infection: a review of barriers and ways forward. Lancet 2010; published online July 20. DOI: 10.1016/S0140-6736(10)60832-X. [DOI] [PubMed] [Google Scholar]
- 133.Degenhardt L, Mathers B, Vickerman P, Rhodes T, Latkin C, Hickman M. Prevention of HIV infection for people who inject drugs: why individual, structural, and combination approaches are needed. Lancet 2010; published online July 20. DOI: 10.1016/S0140-6736(10)60742-8. [DOI] [PubMed] [Google Scholar]
- 134.Jürgens R, Csete J, Amon JJ, Baral S, Beyrer C. People who use drugs, HIV, and human rights. Lancet 2010; published online July 20. DOI: 10.1016/S0140-6736(10)60830-6. [DOI] [PubMed] [Google Scholar]
- 135.Pain and Policy Studies Group. International narcotic control board demographic yearbook. Vienna, Austria: International Narcotics Control Board, 2007. [Google Scholar]
- 136.Human Rights Watch. Human Rights Watch interview with Dr Weru of Nairobi Hospice, Nairobi, Kenya, “Please, do not make us suffer any more...”. Access to Pain Treatment as a Human Right. New York: Human Rights Watch, 2009. [Google Scholar]
- 137.Harding R, Powell R, Kiyange F, Downing J, Mwangi-Powell F. Pain relieving drugs in 12 African PEPFAR countries: mapping current providers, identifying current challenges, and enabling expansion of pain control provision in the management of HIV/AIDS. King’s College, London; 2007 [Google Scholar]
- 138.Burris S, Corey SD. A blueprint for reforming access to opioid medications. 2009. http://ssrn.com/abstract=1356815 (accessed Sept 5, 2009).
- 139.WHO. Achieving balance in national opioids control policy: guidelines for assessment. 2000. http://www.painpolicy.wisc.edu/publicat/00whoabi/00whoabi.htm (accessed Sept 3, 2009).
- 140.Zafar T, ul Hasan S. A sociodemographic and behavioral profile of heroin users and the risk environment in Quetta, Pakistan. Int J Drug Policy 2002; 13: 121–25. [Google Scholar]
- 141.Strathdee SA, Patrick DM, Currie SL, et al. Needle exchange is not enough: lessons from the Vancouver injecting drug use study. AIDS 1997; 11: F59–65. [DOI] [PubMed] [Google Scholar]
- 142.Oelrichs RB, Shrestha IL, Anderson DA, Deacon NJ. The explosive human immunodeficiency virus type 1 epidemic among injecting drug users of Kathmandu, Nepal, is caused by a subtype C virus of restricted genetic diversity. J Virol 2000; 74: 1149–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


