Abstract
Dermatophytic infection of the skin and its appendages is a common occurrence. Though usually straightforward, treatment of dermatophytosis becomes notably challenging in certain population groups – pregnant women, children, and elderly. Treatment with topical azoles/allylamines alone is effective in limited cutaneous disease in all three groups. Terbinafine is the preferred oral agent in elderly population for treatment of extensive cutaneous disease and onychomycosis due to its lack of cardiac complications and lower propensity for drug interactions. If required, additional physical/mechanical modalities can be employed for symptomatic onychomycosis. Data for systemic therapy in children mainly pertains to the treatment of tinea capitis. At present, very little data exists regarding the safety of systemic antifungals in pregnancy and there is an effort to restrict treatment to topical therapies because of their negligible systemic absorption.
Keywords: Children, dermatophytosis, elderly, pregnancy
Introduction
Superficial fungal infections account for nearly 25% of the global skin mycoses, making dermatophytic infections one of the most common types of infective diseases worldwide.[1] Dermatophytosis refers to a superficial mycotic infection caused by either of the three groups of keratinophilic fungi, namely, Trichophyton (infects skin, nails, hair), Microsporum (skin and hair), and Epidermophyton (skin and nails).[2] These comprise the most common agents responsible for superficial cutaneous fungal infections.[3,4]
There is a rising prevalence of dermatophytosis, especially in tropical countries, with a concomitant increase in the number of difficult to treat cases.[1,5] A recent review suggests that T. rubrum and T. mentagrophytes complex are the most frequent agents affecting skin and nail, whereas T. tonsurans, T. violaceum, and M. canis are the predominant pathogens responsible for tinea capitis.[6]
Various treatment options are available used either as monotherapy, combination therapy, or sequential therapy. Specific patient groups, such as pregnant women, children, and elderly, frequently require modified treatment algorithms due to their increased propensity for unacceptable adverse effects. This review will cover the treatment regimens for common dermatophytosis: cutaneous tinea (facei, corporis, cruris, manuum, pedis), onychomycosis, and tinea of the terminal hair bearing area (capitis/barbae) in these special patient groups.
Treatment of Dermatophytes Infections
General measures
Loose-fitting cotton or synthetic clothing which wick moisture away from skin surface are advisable. In addition, patients should be discouraged from sharing garments and towels.[4,5] Undergarments, socks, and caps should be regularly washed and dried in the sun and ironed.
Patients with tinea cruris may be assessed for associated conditions that may contribute to occlusion and thus persistence/recurrence viz. excessive sweating or obesity. Here, encouraging patients to change clothing more frequently, use absorbent powders and deodorants (decrease perspiration), and lose weight, if required, may be advisable.
In case of tinea pedis, imidazole or tolnaftate powders may be used prophylactically, and where other family members are affected, simultaneous treatment should be done.[4,7] The importance of avoiding occlusive footwear and use of slippers in public washrooms in curbing new or re-infection should be emphasized. Maceration or malodor warrant a search for secondary bacterial infection and should be treated with either a topical or systemic antibacterial agent.[8] At the community level, frequent washing of swimming baths and dressing room floors will help to limit the inter-individual spread in these high-risk areas.[4]
Elderly
Treatment of tinea in elderly patients must be individualized. Apart from the site and extent of involvement, other factors need to be taken into account: the presence of comorbidities and possibility of drug interactions. However, a healthy elderly patient may be treated in the same manner as a young adult.[9]
For elderly patients with a single skin lesion and multiple comorbidities/on polypharmacy, topical therapy alone can be administered. Situations where systemic therapy is indicated includes; (a) tinea involving two or more areas simultaneously, for example, tinea corporis with tinea cruris, (b) tinea corporis with extensive involvement where topical therapy may be impractical, (c) tinea pedis particularly moccasin or vesicular type, and (d) repeated failure of treatments with different topical agents.[5,10,11]
Various topical creams have been used for the treatment of cutaneous tinea. Rotta et al. in a meta-analysis found butenafine and terbinafine to be superior to clotrimazole, oxiconazole, and sertaconazole.[12] A Cochrane review observed topical 1% terbinafine and 1% naftifine to be efficacious with few adverse effects. Topical azoles (viz. clotrimazole, bifonazole, sulconazole, miconazole, sertaconazole, eberconazole, econazole, oxiconazole, luliconazole) were also found to have similar mycological and clinical cure rates, although only single studies were available for these. Also reviewed were the head-to-head trials of various topical azoles versus allylamines, in which cure rates were similarly comparable. Despite slight differences among the different classes of topicals in achieving cure, certain preparations are more appealing in elderly, attributable to the requirement of fewer daily applications as well as shorter treatment duration. For example, studies comparing once daily versus twice daily application of eberconazole, terbinafine, oxiconazole, and naftifine did not find any difference in cure rates.[14]
The use of topical antifungal and steroid combination in the initial treatment phase particularly in inflammatory lesions is common, however, evidence regarding the benefits of this combination over topical antifungal monotherapy is low and unconvincing.[13,14] Such combination therapy may prove to be counterproductive in settings where prescription of drugs is unregulated with over the counter easy availability of such formulations. A recent study also showed the efficacy of once daily topical naftifine 2% gel as monotherapy in moccasin tinea pedis.[15]
Systemic therapy used commonly includes oral itraconazole and terbinafine. Other effective options include griseofulvin and fluconazole.[5] Efficacy of these systemic agents has been established in several randomized controlled trials (RCTs).[16,17,18,19] A comparative trial of ultramicronized griseofulvin and itraconazole reported a significantly better outcome with 2 weeks of itraconazole therapy.[16] Fluconazole 150 mg per week was compared with griseofulvin 500 mg daily for 4–6 weeks, in tinea corporis or tinea cruris, in a double-blind trial by Faergemann et al. They reported mycological cure rates of 78% and 80% with fluconazole and griseofulvin, respectively.[17] Similarly, a study conducted by Cole et al. in 50 patients with tinea corporis, found terbinafine to have cure rate of 87% in contrast to 73% with griseofulvin.[18]
However, fluconazole and itraconazole are both CYP3A4 inhibitors, and hence are capable of multiple drug interactions. Itraconazole has been reported to have precipitated rhabdomyolysis in a patient on long-term statins.[20] Case reports of acute systolic failure in previously healthy persons attributable to itraconazole as well as cardiac arrest on co-administration with amiodarone suggest cautious use of this agent in elderly.[21,22] Because a large proportion of the elderly population would be on multiple drug therapy for various comorbidities, topical therapy alone or if required oral terbinafine should be preferred in this age group.
Children
Cutaneous tinea is relatively less common than tinea capitis in the pediatric age group. An Indian study found cutaneous tinea occurring in only 3.1% of children in the age group of 0–10 years.[23] In a review by Seebacher et al. it was observed that the prevalence of tinea corporis in school going children of Ethiopia was 1.4% in comparison with tinea capitis which accounted for 88.8% of all dermatophytic infections.[24]
However, in recent years, the frequency of tinea in children including infants is noted to be increasing in India (unpublished data). The treatment of cutaneous tinea in children is generally limited to use of topical antifungals. Rapid turnover of skin in this age group may be contributing to relatively better clinical response to topical therapy alone compared to adult patients. Most clinical experience with oral griseofulvin and terbinafine use in children has been in the setting of tinea capitis and onychomycosis, and these agents may be used in extensive or refractory cutaneous tinea.[25] Several studies have demonstrated efficacy and safety of terbinafine use in children. A multicenter study including 132 children aged 1–10 years reported it to be well tolerated with no clinically relevant derangement of liver functions.[26]
A study on itraconazole systemic therapy using 5 mg/kg/day for a duration of 1 week in tinea corporis and cruris and 2 weeks in tinea pedis and manuum found it to be effective and safe.[27] A review of itraconazole use in infants with superficial dermatophytosis (5 mg/kg/day) and systemic mycoses (10 mg/kg/day) found it to be safe and effective, with few serious adverse effects which make it the second-line systemic therapy in the pediatric age group.[28]
In India, oral formulation for pediatric use is available for fluconazole as 50 mg/ml oral suspension and for itraconazole as oral solution (10 mg/ml) formulation. In the USA, terbinafine is available in a granule formulation (for sprinkling on food) and is licensed for children >4 years of age. A liquid formulation of itraconazole, griseofulv in syrup, and fluconazole suspension are available for use in the pediatric age group in the UK.[29]
Pregnant women
Topical azoles are minimally or not absorbed systemically, and therefore can be prescribed at any stage of pregnancy.[30]
The US Food and Drug Administration (FDA) has eliminated the pregnancy categories for drugs with effect from June 2015, and a staggered switchover to Pregnancy and Lactation Labeling Rule (PLLR) by 2020 is planned. At the time of writing this article, drugs discussed here would not have adopted the new labeling format, therefore, we have reviewed drug safety in pregnancy as per the FDA pregnancy categories.
The FDA categories for several topical antifungals – clotrimazole, terbinafine, ciclopirox, naftifine, oxiconazole is B. Econazole, miconazole, ketoconazole, selenium sulfide have been categorized as C and therefore should be avoided.[31,32]
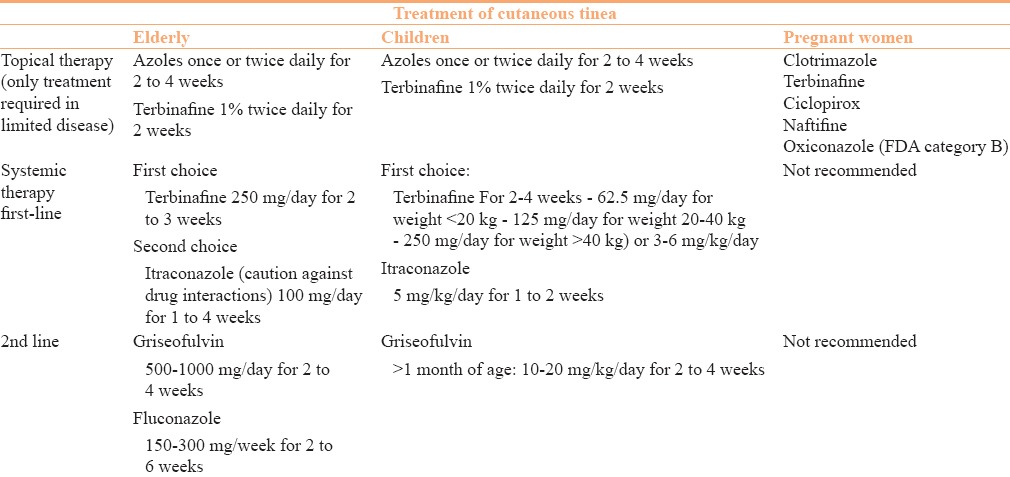
The FDA pregnancy category for oral fluconazole, itraconazole, and griseofulvin is C, and therefore should preferably be avoided throughout the duration of pregnancy. Terbinafine is the only oral antifungal to have been categorized as pregnancy category B, however, data on its use in pregnancy is not present. Although classified as category B, whether terbinafine crosses the placental barrier is unknown and should be deferred. It is also actively secreted in breast milk and therefore should not be used in breastfeeding mothers.[30] The treatment of cutaneous tinea in elderly, children, and pregnant patients is summarized in Table 1.[4,8,33]
Table 1.
Treatment options for cutaneous tinea in elderly, children, and pregnant women
Treatment of Onychomycosis
General measures for all patients
T. rubrum has been reported to be present on carpets and public changing room floors. Therefore, emphasis on wearing wide protective footwear is imperative. Moreover, wearing absorbent socks and application of antifungal (miconazole/clotrimazole) or absorbent powders in shoes and on feet may help prevent recurrence. Patients should be encouraged to regularly trim nails to minimize trauma and avoid sharing nail clippers.[7,33]
Ideally, old mouldy footwear should be discarded. Because this may be impractical, patients can be advised to put naphthalene mothballs in shoes and enclose them tightly in a plastic bag for 3 days followed by airing to remove the naphthalene odor. This should kill the fungal arthroconidia in the footwear. Continued application of antifungal powders in these shoes would be helpful in ensuring that infectious fungal elements are removed. Because onychomycosis is contagious, it is advisable to treat all affected family members simultaneously to prevent reinfection.[7]
Furthermore, with an increase in the popularity of nail salons, there is a need to educate patients of the need for sterile techniques, as frequent manicures and pedicures in unhygienic conditions may predispose to paronychial and dermatophytic nail infections.[7]
Elderly
There is a higher prevalence of onychomycosis in the elderly with almost 20% of those aged above 60 years and 50% over 70 years reported to be affected.[7] This may be due to the inherent changes in the nail unit which occur with age due to impaired blood circulation, altered biomechanics, recurrent trauma, reduced immunity, and diabetes.[35] Apart from polypharmacy and comorbidities, impaired wound healing and peripheral vascular compromise are important factors that complicate the treatment of onychomycosis in elderly.
Baran et al. have suggested that, in the elderly, treatment should be topical antifungals with or without chemical (40% urea) or mechanical nail avulsion. Although this is preferred, for patients who are distressed by the disease, weekly fluconazole 300 mg or terbinafine 250 mg twice daily in a pulse form for 1 week every month can be given.[9] A randomized double-blind trial comparing continuous (250 mg/day for 12 weeks) and pulsed terbinafine (500 mg/day for a week per month for 3 cycles) in toenail onychomycosis found both regimens to be equally efficacious.[35]
Gupta et al. conducted a randomized, single blind trial on 101 elderly patients comparing pulse itraconazole and daily continuous terbinafine in the treatment of toenail dermatophytic onychomycosis and found the mycologic cure rate to be 64% with terbinafine and 62.7% with itraconazole. Approximately, 87% of their study population had diseases other than onychomycosis and were on an average of 1–2 oral medications. They reported only mild and transient adverse effects with the antifungal treatment with none of the patients requiring drug discontinuation.[36]
Recent British Association of Dermatologists’ guidelines suggest the use of amorolfine 5% lacquer local application once or twice a week for 6–12 months, followed by gentle nail filing to remove as much of the diseased nail as possible.[7] Ciclopirox nail lacquer application once daily up to 24 weeks for fingernails and 48 weeks for toenails is another option. Cure rates with ciclopirox are usually lower in comparison with amorolfine. However, no head-to-head trials have been done between the two.[7,37,38]
Newer topicals that have received FDA approval for onychomycosis are tavabarole 5% and efinaconazole 10%. Recent data have shown cure rates of 17.9% and 19.7%, respectively, with these drugs alone.[39] Tavabarole requires once daily application for 48 weeks and has minimal local adverse effects. Efinaconazole has a lower affinity to keratin, deeper nail bed penetration, and a higher potency against T. mentagrophytes compared with ciclopirox and amorolfine. Similar to tavabarole, once daily application for efinaconazole for 48 weeks is recommended.[40]
Two laser systems have received FDA approval [(Pinpointe® (NuvoLase Inc., CA, USA) and Genesis Plus® (Cutera Inc., CA, USA)] for temporary aesthetic improvement in onychomycosis by increasing the clear nail. Theoretically, lasers have fungicidal effects although in practice the results are variable.[41,42] A study conducted among 20 patients treated with long-pulsed 1064-nm Nd:YAG laser at 1 week intervals (four sessions) showed encouraging results, with reduction in discoloration, onycholysis, opacification, and jagged proximal edge.[43] Another trial using fractional carbon dioxide laser and topical amorolfine daily showed complete cure in 50% and clinical improvement in 92%.[44] The major disadvantage with laser therapy is the prohibitive cost which makes this option inaccessible to a large proportion of people. However, a recent review by Gupta et al. suggests that lasers in onychomycosis transiently increase the clear nail amount, thus fulfilling the FDA approved aesthetic endpoints. Comparison of mycological or complete cure (mycological plus clinical) rates with standard therapies for onychomycosis remains to be determined and requires high quality clinical trials.[42]
Photodynamic therapy (PDT) is becoming increasingly popular as an alternative and safe adjunct to treatment of onychomycosis. The principle is photosensitizer-induced reactive oxygen species production within the microorganisms resulting in cell death. Various photosensitizers have been used – 5-aminolevulinic acid, methyl-aminolevulinic acid (MAL), methylene blue, hypercin, rose Bengal, and photogem. An RCT compared methylene blue PDT with weekly fluconazole (total duration of 6 months), and found significantly better results in the PDT group.[45] However, a recent, multicenter trial failed to show significant difference between 40% urea only arm and 40% urea plus MAL-PDT arm. They attributed this to the unexpected response of onychomycosis with topical urea alone.[46]
Keeping in mind the newer options, topical therapy can be optimized for better response with the addition of either of these newer modalities.
Children
Onychomycosis is relatively uncommon in the pediatric age group, approximate worldwide prevalence being <0 5%.[47] It is theorized that children have a lower likelihood of developing onychomycosis due to faster nail growth, lower surface area of nail unit, and lower exposure to environments containing pathogens.[48] However, similar to adults, distal lateral and subungal onychomycosis (DLSO) is the most common clinical presentation, toenails are more often affected, and dominant pathogen implicated is T. rubrum followed by T. mentagrophytes.[7] Children with onychomycosis must be evaluated for concomitant tinea pedis and capitis. Close family members should also be examined for onychomycosis.[7,9]
At present, there are no FDA-approved medications for onychomycosis in the pediatric age group and several off-label options have been tried. Although there are no clinical trials demonstrating efficacy of topical antifungals in children, initial therapy with topical antifungals may prove successful due to the faster nail growth rate in this age group.[48]
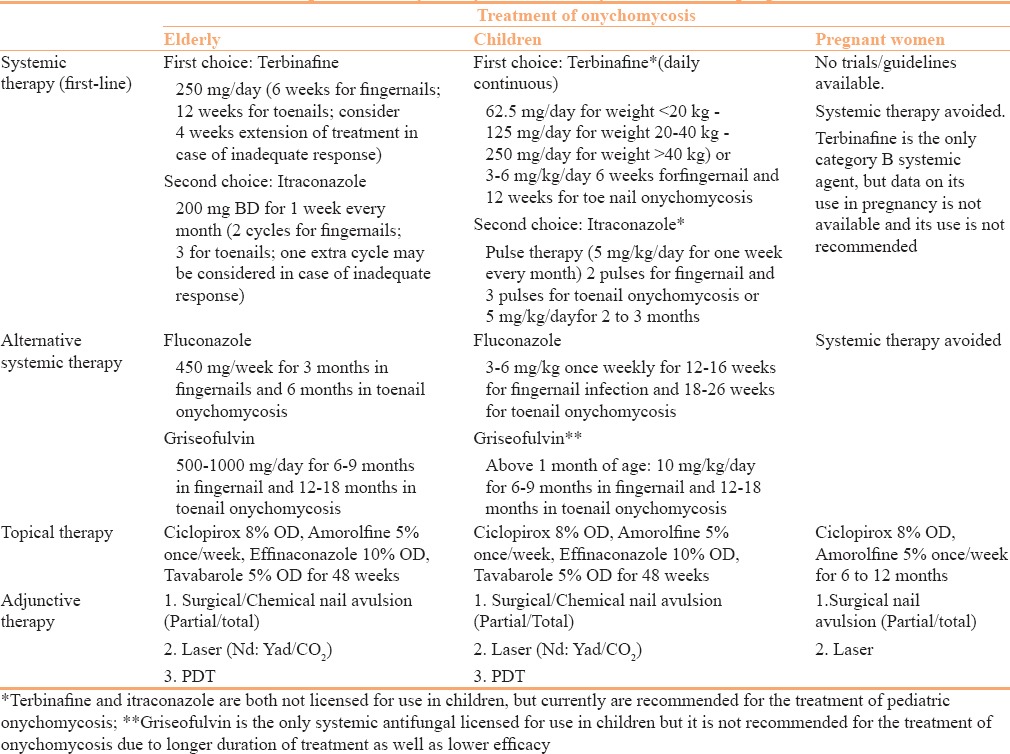
There are several studies demonstrating the safety and efficacy of systemic treatment in children. A systematic review by Gupta et al. found that treatment with systemic antifungals alone resulted in 70.8% cure rate and combined systemic plus topical therapy resulted in a 80.0% cure rate. A majority of the studies reviewed reported the use of terbinafine or itraconazole.[49] There are several other studies demonstrating safety, higher cure rates, and faster response to systemic therapies in pediatric populations.[50,51] The British Association of Dermatologists currently recommends the use of three drugs for systemic use in children with onychomycosis – terbinafine, itraconazole, and fluconazole.[7] Details have been tabulated in Table 2.[7,8,31,32,33] Griseofulvin, although licensed for use in children, is not recommended as a first-line systemic agent for pediatric onychomycosis due to prolonged treatment required and lower efficacy.[7]
Table 2.
Treatment options for onychomycosis in elderly, children, and pregnant women
Pregnant women
It is generally advisable to avoid the use of systemic therapy in pregnancy.[9] Throughout pregnancy, use of topical monotherapy is preferred. Topical ciclopirox (FDA pregnancy category B) and amorolfine (not FDA approved) are considered safe throughout pregnancy, and thus may be used in those with superficial white onychomycosis (SWO), onychomycosis due to molds, and DLSO involving less than 50% of the nail area without matricidal involvement.[30,52]
Mechanical modalities, namely cutting, abrading, filing, and nail avulsion are adjunctive options for refractory disease.[53] Because topical treatment alone may lead to treatment failure, surgery in the form of nail plate avulsion may be considered in those with painful onychomycosis. Partial nail avulsion is preferred over total to avoid disfigurement and the risk of distal embedding following nail regrowth.[41]
A recent review noted the safety of carbon dioxide and Nd:Yag lasers in pregnancy.[54] Lasers, including fractional carbon dioxide and long pulsed Nd:Yag, have been described as effective adjuncts in the treatment of onychomycosis as mentioned above and may be used to provide relief in case it is available and patient can afford the treatment.[43,44]
Treatment of Tinea Capitis
General measures
Hairbrushes and combs have been shown to carry viable spores and should be cleaned thoroughly with a disinfectant. Household bleach or sodium hypochlorite (2% aqueous solution) is suitable for this purpose. To prevent the transmission of spores, 2–4 times weekly use of 1% selenium sulphide, 1% or 2% zinc pyrithione, 2.5% povidone–iodine, and 2% ketoconazole shampoos have been shown to be effective.[8,29]
Because tinea capitis caused by T. tonsurans is known to be highly infectious, screening of family members is recommended with treatment of those who are found to harbor occult disease as failure to do so results in higher recurrence rates.[29]
Mycological evidence of an animal species warrants a search for infection in pets or cattle and other animals the patient may have had contact with. Treatment of infected animals by veterinarians with griseofulvin is both effective and economical.[4]
Corticosteroids have been used in inflammatory tinea capitis (e.g., kerion) with the aim to reduce scarring. However, in comparison with oral antifungal treatment alone no definite long-term advantage has been shown and therefore are no longer recommended.[29]
Elderly
It is well-known that tinea capitis is an affliction of the young, nevertheless several studies have shown that tinea capitis in adults is not a particularly rare entity. A recent review by Khosravi et al. revealed a wide variation in prevalence of adult tinea capitis, ranging from 2.6% in Italy to as high as 63% in Taiwan.[55]
A higher prevalence among post-menopausal women and immunosuppressed individuals has been reported.[55,56] In recent epidemic-like situation of dermatophytes infection in India, a significant proportion of adult patients are being noted to have tinea capitis as a result of extension of facial tinea or from lesions on upper parts of the body (unpublished data). The most common etiological agent reported is Trichophyton species. Treatment with oral terbinafine, itraconazole, and griseofulvin has been used with good efficacy. Terbinafine 250 mg daily for 2–4 weeks may be preferred over itraconazole and griseofulvin in patients on multiple drugs.
Topical antifungals should be used to prevent spread but cannot supplant systemic treatment.[4,29]
Children
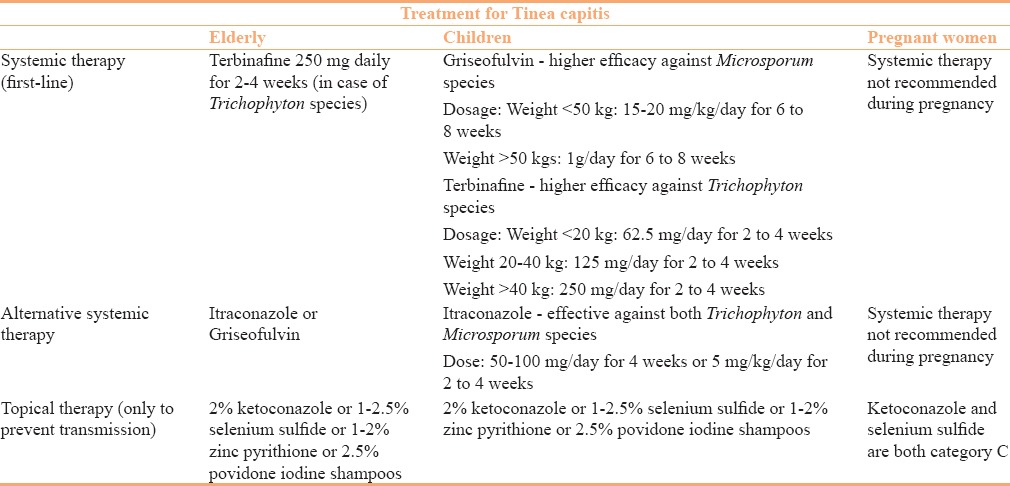
Current recommendations dictate that treatment protocols should cover the most likely pathogen based on local epidemiology or fungal culture.[29] The recommended systemic agents and their doses have been tabulated in Table 3.[8,29,31,32]
Table 3.
Treatment options for tinea capitis in elderly, children, and pregnant women
In cases not responding to both first and second-line drugs, noncompliance must be ruled out following which treatment with fluconazole or voriconazole may be tried. The recommended treatment is mycological cure. Therefore, repeat mycology (potassium hydroxide microscopy and fungal culture) must be done before discontinuation of therapy.[29]
Pregnant women
There are no studies or guidelines available for the management of tinea capitis in pregnancy. Considering the fact that tinea capitis is not an emergency, systemic antifungals should be deferred till after delivery/lactation and topical therapy alone along with symptomatic treatment may be administered initially.
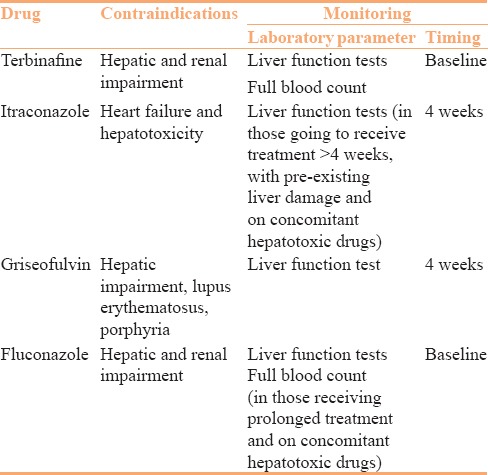
Table 4 mentions the monitoring required for systemic antifungals when given for prolonged period of time.
Table 4.
Contraindications and monitoring
Conclusion
Treatment of dermatophytosis in special population groups such as pregnant women, children, and elderly needs a cautious approach. Topical azoles and allylamines are preferred for treatment in pregnancy as well as in both extremes of age. Ample evidence of safety is available for oral antifungals, terbinafine, and itraconazole in both elderly and children. However, in cases where systemic treatment is required, terbinafine is preferred, except in pregnancy and lactation where all oral agents are best avoided. In recalcitrant/recurrent dermatophytosis, a longer duration with or without an increase in the dose of terbinafine may be tried. However, if antifungal drug susceptibility pattern is supportive, itraconazole may be preferred as a systemic agent. Although current evidence for this recommendation does not exist, combination of an oral agent and a topical formulation with different mechanisms of action can be tried in such cases e.g., oral allylamine with a topical azole. This approach may be helpful in cases of cutaneous infection that persists despite 4 weeks of standard treatment. Nonpharmacological measures are equally important for effective management, prevention of spread to others and tackling recurrent/chronic disease and effort must be made to educate patients regarding precautions required. In the future, development of newer drugs or topical drug formulations with a “depot” effect may help reduce the duration of treatment required as well as recurrences.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Havlickova B, Czaika VA, Friedrich M. Epidemiological trends in skin mycoses worldwide. Mycoses. 2008;51:2–15. doi: 10.1111/j.1439-0507.2008.01606.x. [DOI] [PubMed] [Google Scholar]
- 2.Weitzman I, Summerbell RC. The dermatophytes. Clin Microbiol Rev. 1995;8:240–59. doi: 10.1128/cmr.8.2.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nenoff P, Krüger C, Ginter-Hanselmayer G, Tietz HJ. Mycology - an update. Part 1: Dermatomycoses: Causative agents, epidemiology and pathogenesis. J Dtsch Dermatol Ges. 2014;12:188–209. doi: 10.1111/ddg.12245. [DOI] [PubMed] [Google Scholar]
- 4.Hay RL, Ashbee RH. Fungal Infections. In: Griffiths CEM, editor. Rook's Textbook of Dermatology. 9th ed. New Delhi: Wiley-Blackwell; 2016. pp. 32.1–55. [Google Scholar]
- 5.Sahoo AK, Mahajan R. Management of tineacorporis, tineacruris, and tineapedis: A comprehensive review. Indian Dermatol Online J. 2016;7:77–86. doi: 10.4103/2229-5178.178099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhan P, Liu W. The Changing Face of Dermatophytic Infections Worldwide. Mycopathologia. 2017;182:77–86. doi: 10.1007/s11046-016-0082-8. [DOI] [PubMed] [Google Scholar]
- 7.Ameen M, Lear JT, Madan V, Mohd Mustapa MF, Richardson M. British Association of Dermatologists’ guidelines for the management of onychomycosis 2014. Br J Dermatol. 2014;17:937–58. doi: 10.1111/bjd.13358. [DOI] [PubMed] [Google Scholar]
- 8.Schieke SM, Garg A. Superficial Fungal Infection. In: Goldsmith LA, editor. Fitzpatrick's Dermatology in General Medicine. 8th ed. Palantino: McGraw-Hill; 2012. pp. 2277–96. [Google Scholar]
- 9.Baran R, Hay RJ, Garduno JI. Review of antifungal therapy, part II: Treatment rationale, including specific patient populations. J Dermatolog Treat. 2008;19:168–75. doi: 10.1080/09546630701657187. [DOI] [PubMed] [Google Scholar]
- 10.Weinstein A, Berman B. Topical treatment of common superficial tinea infections. Am Fam Physician. 2002;65:2095–102. [PubMed] [Google Scholar]
- 11.Ely JW, Rosenfeld S, Seabury Stone M. Diagnosis and management of tinea infections. Am Fam Physician. 2014;90:702–10. [PubMed] [Google Scholar]
- 12.Rotta I, Ziegelmann PK, Otuki MF, Riveros BS, Bernardo NL, Correr CJ. Efficacy of topical antifungals in the treatment of dermatophytosis: A mixed-treatment comparison meta-analysis involving 14 treatments. JAMA Dermatol. 2013;149:341–9. doi: 10.1001/jamadermatol.2013.1721. [DOI] [PubMed] [Google Scholar]
- 13.El-Gohary M, van Zuuren EJ, Fedorowicz Z, Burgess H, Doney L, Stuart B, et al. Topical antifungal treatments for tineacruris and tineacorporis. Cochrane Database Syst Rev. 2014;4:CD009992. doi: 10.1002/14651858.CD009992.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Van Zuuren EJ, Fedorowicz Z, El-Gohary M. Evidence-based topical treatments for tineacruris and tineacorporis: A summary of a Cochrane systematic review. Br J Dermatol. 2015;172:616–41. doi: 10.1111/bjd.13441. [DOI] [PubMed] [Google Scholar]
- 15.Stein Gold LF, Vlahovic T, Verma A, Olayinka B, Fleischer AB., Jr Naftifine Hydrochloride Gel 2%: An Effective Topical Treatment for Moccasin-Type Tinea Pedis. J Drugs Dermatol. 2015;14:1138–44. [PubMed] [Google Scholar]
- 16.Bourlond A, Lachapelle JM, Aussems J, Boyden B, Campaert H, Conincx S, et al. Double-blind comparison of itraconazole with griseofulvin in the treatment of tineacorporis and tineacruris. Int J Dermatol. 1989;28:410–2. doi: 10.1111/j.1365-4362.1989.tb02491.x. [DOI] [PubMed] [Google Scholar]
- 17.Faergemann J, Mörk NJ, Haglund A, Odegård T. A multicentre (double-blind) comparative study to assess the safety and efficacy of fluconazole and griseofulvin in the treatment of tineacorporis and tineacruris. Br J Dermatol. 1997;136:575–7. [PubMed] [Google Scholar]
- 18.Cole GW, Stricklin G. A comparison of a new oral antifungal, terbinafine, with griseofulvin as therapy for tineacorporis. Arch Dermatol. 1989;125:1537–9. [PubMed] [Google Scholar]
- 19.Panagiotidou D, Kousidou T, Chaidemenos G, Karakatsanis G, Kalogeropoulou A, Teknetzis A, et al. A comparison of itraconazole and griseofulvin in the treatment of tineacorporis and tineacruris: A double-blind study. J Int Med Res. 1992;20:392–400. doi: 10.1177/030006059202000504. [DOI] [PubMed] [Google Scholar]
- 20.Dybro AM, Damkier P, Rasmussen TB, Hellfritzsch M. Statin-associated rhabdomyolysis triggered by drug-drug interaction with itraconazole. BMJ Case Rep. 2016;7:2016. doi: 10.1136/bcr-2016-216457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paul V, Rawal H. Cardiotoxicity with Itraconazole. BMJ Case Rep. 2017;10:2017. doi: 10.1136/bcr-2017-219376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tsimogianni AM, Andrianakis I, Betrosian A, Douzinas E. Cardiac arrest provoked by itraconazole and amiodarone interaction: A case report. J Med Case Rep. 2011;5:333. doi: 10.1186/1752-1947-5-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maulingkar SV, Pinto MJ, Rodrigues S. A clinico-mycological study of dermatophytoses in Goa, India. Mycopathologia. 2014;178:297–301. doi: 10.1007/s11046-014-9806-9. [DOI] [PubMed] [Google Scholar]
- 24.Seebacher C, Bouchara JP, Mignon B. Updates on the epidemiology of dermatophyte infections. Mycopathologia. 2008;166:335–52. doi: 10.1007/s11046-008-9100-9. [DOI] [PubMed] [Google Scholar]
- 25.Elewski BE. Cutaneous mycoses in children. Br J Dermatol. 1996;134:37–8. doi: 10.1111/j.1365-2133.1996.tb15651.x. [DOI] [PubMed] [Google Scholar]
- 26.Filho ST, Cucé LC, Foss NT, Marques SA, Santamaria JR. Efficacy, safety and tolerability of terbinafine for Tineacapitis in children: Brazilian multicentric study with daily oral tablets for 1, 2 and 4 weeks. J Eur Acad Dermatol Venereol. 1998;11:141–6. [PubMed] [Google Scholar]
- 27.Gupta AK, Nolting S, de Prost Y, Delescluse J, Degreef H, Theissen U, et al. The use of itraconazole to treat cutaneous fungal infections in children. Dermatology. 1999;199:248–52. doi: 10.1159/000018256. [DOI] [PubMed] [Google Scholar]
- 28.Chen S, Sun KY, Feng XW, Ran X Lama J, Ran YP. Efficacy and safety of itraconazole use in infants. World J Pediatr. 2016;12:399–407. doi: 10.1007/s12519-016-0034-x. [DOI] [PubMed] [Google Scholar]
- 29.Fuller LC, Barton RC, MohdMustapa MF, Proudfoot LE, Punjabi SP, Higgins EM. British Association of Dermatologists’ guidelines for the management of tineacapitis 2014. Br J Dermatol. 2014;171:454–63. doi: 10.1111/bjd.13196. [DOI] [PubMed] [Google Scholar]
- 30.Pilmis B, Jullien V, Sobel J, Lecuit M, Lortholary O, Charlier C. Antifungal drugs during pregnancy: An updated review. J Antimicrob Chemother. 2015;70:14–22. doi: 10.1093/jac/dku355. [DOI] [PubMed] [Google Scholar]
- 31.Murase JE, Heller MM, Butler DC. Safety of dermatologic medications in pregnancy and lactation: Part I. Pregnancy. J Am Acad Dermatol. 2014;70:401–15. doi: 10.1016/j.jaad.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 32.Patel VM, Schwartz RA, Lambert WC. Topical Antiviral and Antifungal Medications in Pregnancy: A Review of Safety Profiles. J Eur Acad Dermatol Venereol. 2017:27. doi: 10.1111/jdv.14297. [DOI] [PubMed] [Google Scholar]
- 33.Gupta AK, Foley KA, Versteeg SG. New Antifungal Agents and New Formulations Against Dermatophytes. Mycopathologia. 2017;182:127–41. doi: 10.1007/s11046-016-0045-0. [DOI] [PubMed] [Google Scholar]
- 34.Murdan S. Nail disorders in older people, and aspects of their pharmaceutical treatment. Int J Pharm. 2016;512:405–11. doi: 10.1016/j.ijpharm.2016.05.022. [DOI] [PubMed] [Google Scholar]
- 35.Yadav P, Singal A, Pandhi D, Das S. Comparative efficacy of continuous and pulse dose terbinafine regimes in toenail dermatophytosis: A randomized double-blind trial. Indian J Dermatol Venereol Leprol. 2015;81:363–9. doi: 10.4103/0378-6323.158634. [DOI] [PubMed] [Google Scholar]
- 36.Gupta AK, Konnikov N, Lynde CW. Single-blind, randomized, prospective study on terbinafine and itraconazole for treatment of dermatophyte toenail onychomycosis in the elderly. J Am Acad Dermatol. 2001;44:479–84. doi: 10.1067/mjd.2001.110874. [DOI] [PubMed] [Google Scholar]
- 37.Shemer A, Nathansohn N, Trau H, Amichai B, Grunwald MH. Ciclopirox nail lacquer for the treatment of onychomycosis: An open non-comparative study. J Dermatol. 2010;37:137–9. doi: 10.1111/j.1346-8138.2009.00773.x. [DOI] [PubMed] [Google Scholar]
- 38.Crawford F, Hollis S. Topical treatments for fungal infections of the skin and nails of the foot. Cochrane Database Syst Rev. 2007;3:CD001434. doi: 10.1002/14651858.CD001434.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Elewski BE, Vlahovic TC, Korotzer A. Topical treatment for Onychomycosis: Is it More Effective than the Clinical Data Suggests? J Clin Aesthet Dermatol. 2016;9:34–9. [PMC free article] [PubMed] [Google Scholar]
- 40.Saunders J, Maki K, Koski R, Nybo SE. Tavaborole, Efinaconazole, and Luliconazole: Three New Antimycotic Agents for the Treatment of Dermatophytic Fungi. J Pharm Pract. 2016 doi: 10.1177/0897190016660487. pii: 0897190016660487 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 41.Grover C, Khurana A. An update on treatment of onychomycosis. Mycoses. 2012;55:541–51. doi: 10.1111/j.1439-0507.2012.02199.x. [DOI] [PubMed] [Google Scholar]
- 42.Gupta AK, Versteeg SG. A critical review of improvement rates for laser therapy used to treat toenail onychomycosis. J Eur Acad Dermatol Venereol. 2017;31:1111–8. doi: 10.1111/jdv.14212. [DOI] [PubMed] [Google Scholar]
- 43.Piccolo D, Kostaki D, Del Duca E, Cannarozzo G, Sannino M, Nisticò S. Long-Pulsed 1064-nm Nd:YAG Laser for the Treatment of Onychomycosis. Photomed Laser Surg. 2017;35:213–6. doi: 10.1089/pho.2016.4153. [DOI] [PubMed] [Google Scholar]
- 44.Lim EH, Kim HR, Park YO, Lee Y, Seo YJ, Kim CD, et al. Toenail onychomycosis treated with a fractional carbon-dioxide laser and topical antifungal cream. J Am Acad Dermatol. 2014;70:918–23. doi: 10.1016/j.jaad.2014.01.893. [DOI] [PubMed] [Google Scholar]
- 45.Figueiredo Souza LW, Souza SV, Botelho AC. Randomized controlled trial comparing photodynamic therapy based on methylene blue dye and fluconazole for toenail onychomycosis. Dermatol Ther. 2014;27:43–7. doi: 10.1111/dth.12042. [DOI] [PubMed] [Google Scholar]
- 46.Gilaberte Y, Robres MP, Frías MP, García-Doval I, Rezusta A, Aspiroz C. Methyl aminolevulinate photodynamic therapy for onychomycosis: A multicentre, randomized, controlled clinical trial. J Eur Acad Dermatol Venereol. 2017;31:347–54. doi: 10.1111/jdv.13842. [DOI] [PubMed] [Google Scholar]
- 47.Piraccini BM, Starace M, Bruni F. Onychomycosis in children. Expert Rev Dermatol. 2012;7:569–78. [Google Scholar]
- 48.Feldstein S, Totri C, Friedlander SF. Antifungal therapy for onychomycosis in children. Clin Dermatol. 2015;33:333–9. doi: 10.1016/j.clindermatol.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 49.Gupta AK, Paquet M. Systemic antifungals to treat onychomycosis in children: A systematic review. Pediatr Dermatol. 2013;30:294–302. doi: 10.1111/pde.12048. [DOI] [PubMed] [Google Scholar]
- 50.Huang PH, Paller AS. Itraconazole pulse therapy for dermatophyte onychomycosis in children. Arch Pediatr Adolesc Med. 2000;154:614–8. doi: 10.1001/archpedi.154.6.614. [DOI] [PubMed] [Google Scholar]
- 51.Jones TC. Overview of the use of terbinafine (Lamisil) in children. Br J Dermatol. 1995;132:683–9. doi: 10.1111/j.1365-2133.1995.tb00711.x. [DOI] [PubMed] [Google Scholar]
- 52.Iorizzo M, Piraccini BM, Tosti A. Today's treatments options for onychomycosis. J Dtsch Dermatol Ges. 2010;8:875–9. doi: 10.1111/j.1610-0387.2010.07499.x. [DOI] [PubMed] [Google Scholar]
- 53.Hay RJ, Baran R. Baran & Dawber's diseases of the nails and their management. 1st ed. Pondicherry: Wiley-Blackwell; 2012. Fungal (Onychomycosis) and Other Infections Involving the Nail Apparatus; pp. 211–56. [Google Scholar]
- 54.Trivedi MK, Kroumpouzos G, Murase JE. A review of the safety of cosmetic procedures during pregnancy and lactation. Int J Womens Dermatol. 2017;3:6–10. doi: 10.1016/j.ijwd.2017.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Khosravi AR, Shokri H, Vahedi G. Factors in Etiology and Predisposition of Adult Tinea Capitis and Review of Published Literature. Mycopathologia. 2016;181:371–8. doi: 10.1007/s11046-016-0004-9. [DOI] [PubMed] [Google Scholar]
- 56.El-Khalawany M, Shaaban D, Hassan H, Abdalsalam F, Eassa B, Abdel Kader A, et al. A multicenter clinicomycological study evaluating the spectrum of adult tinea capitis in Egypt. Acta Dermatovenerol Alp Pannonica Adriat. 2013;2s:77–82. [PubMed] [Google Scholar]


