Abstract
Ovarian cancer (OC) is the seventh most commonly diagnosed cancer among women in the world and the tenth most common in China. Epithelial OC is the most predominant pathologic subtype, with five major histotypes that differ in origination, pathogenesis, molecular alterations, risk factors, and prognosis. Genetic susceptibility is manifested by rare inherited mutations with high to moderate penetrance. Genome-wide association studies have additionally identified 29 common susceptibility alleles for OC, including 14 subtype-specific alleles. Several reproductive and hormonal factors may lower risk, including parity, oral contraceptive use, and lactation, while others such as older age at menopause and hormone replacement therapy confer increased risks. These associations differ by histotype, especially for mucinous OC, likely reflecting differences in etiology. Endometrioid and clear cell OC share a similar, unique pattern of associations with increased risks among women with endometriosis and decreased risks associated with tubal ligation. OC risks associated with other gynecological conditions and procedures, such as hysterectomy, pelvic inflammatory disease, and polycystic ovarian syndrome, are less clear. Other possible risk factors include environmental and lifestyle factors such as asbestos and talc powder exposures, and cigarette smoking. The epidemiology provides clues on etiology, primary prevention, early detection, and possibly even therapeutic strategies.
Keywords: Ovarian cancer, epidemiology, risk factors, histology, reproductive history
Introduction
Ovarian cancer (OC) accounts for an estimated 239,000 new cases and 152,000 deaths worldwide annually1. The highest rates (11.4 per 100,000 and 6.0 per 100,000, respectively) are seen in Eastern and Central Europe. Although China has a relatively low incidence rate (4.1 per 100,000), the large population translates to an estimated 52,100 new cases and 22,500 related deaths in 20152. In comparison, 21,290 cases and 14,180 related deaths are estimated to occur in the USA during the same year3.
A woman’s lifetime risk of developing OC is 1 in 75, and her chance of dying of the disease is 1 in 1004. The disease typically presents at late stage when the 5-year relative survival rate is only 29%. Few cases (15%) are diagnosed with localized tumor (stage 1) when the 5-year survival rate is 92%4. Strikingly, the overall 5-year relative survival rate generally ranges between 30%–40% across the globe and has seen only very modest increases (2%–4%) since 19955.
Despite the public health significance, the etiology of this lethal disease is not completely understood. This review is divided into five sections: pathologic classification, descriptive epidemiology, genetic epidemiology, risk and preventive factors, and summary and conclusions.
Pathologic classification of OC
Nearly all benign and malignant ovarian tumors originate from one of three cell types: epithelial cells, stromal cells, and germ cells. In developed countries, more than 90% of malignant ovarian tumors are epithelial in origin, 5%–6% of tumors constitute sex cord-stromal tumors (e.g., granulosa cell tumors, thecomas, etc.), and 2%–3% are germ cell tumors (e.g., teratomas, dysgerminomas, etc.)6. The pathology and classification of ovarian tumors are described in detail by Chen et al.7. Most epidemiologic research, including the present review, focuses on epithelial OC.
Epithelial OC reflects a heterogeneous disease with histologic subtypes (histotypes) that differ in their cellular origin, pathogenesis, molecular alterations, gene expression, and prognosis8-11. Malignant OC, also known as carcinomas, are comprised of five main histotypes: high-grade serous (HGSOC; 70%), endometrioid (ENOC; 10%), clear cell (CCOC; 10%), mucinous (MOC; 3%), and low-grade serous (LGSOC; <5%)8,9. Within each of these categories, although most often among serous and mucinous, are tumors of uncertain malignant behavior known as borderline or low malignant potential (LMP) tumors that contain microscopic features of malignancy without frank invasion into surrounding stroma12.
The cellular origin and pathogenesis of OC is not well understood and, interestingly, most tumors appear to originate from other gynecological tissues and involve the ovary secondarily. Morphological and genetic studies have given rise to several hypothesis of origination, particularly for high-grade serous tumors that lack a clear progression model13,14. Compelling data suggest high and low grade serous neoplasms originate from fallopian tube epithelium, CCOC and ENOC from endometriotic cysts associated with endometriosis, and MOC from transitional cell nests at the tubal-mesothelial junction15,16. HGSOC and LGSOC are both thought to arise from tubal epithelium although through separate pathways. Atypical lesions within the fimbriated end of the fallopian tube (serous tubal intraepithelial carcinomas) display similar morphology and TP53 signatures as HGSOC tumors suggesting the neoplastic process may originate at these tubal lesions and shed onto the ovary where they aggressively progress17-19. LGSOC tumors present along a continuum that delineates a clear progression from benign serous cystadenoma to borderline serous tumor and then low-grade carcinoma. The epithelial inclusion glands presumed to derive the cystadenoma, although located in the ovary, are phenotypically tubal suggesting they formed from transplanted tubal epithelium20. Similar to low-grade serous tumors, mucinous, endometrioid, and clear cell carcinomas are thought to progress from borderline tumors in a stepwise manner and are designated as Type I tumors21. HGSOC has an aggressive phenotype and lacks a clear precursor and is considered Type II. Type I and Type II tumors display different, often mutually exclusive mutational profiles. Type I tumors are associated with mutations inBRAF andKRAS oncogenes in serous and mucinous tumors, andPTEN in endometroid tumors, all of which are not characteristic of HGSOC tumors which predominantly (~50%–80%) have p53 mutations21. Moreover, some risk and preventive factors vary by the major histotypes. Epidemiological studies of OC are increasingly investigating etiologic factors by histopathologic and molecular subtypes22-30, an integrative approach termed “molecular pathological epidemiology”31. These studies have shown that many risk factors associate differentially with the main histotypes and we present these results throughout this review.
Descriptive epidemiology
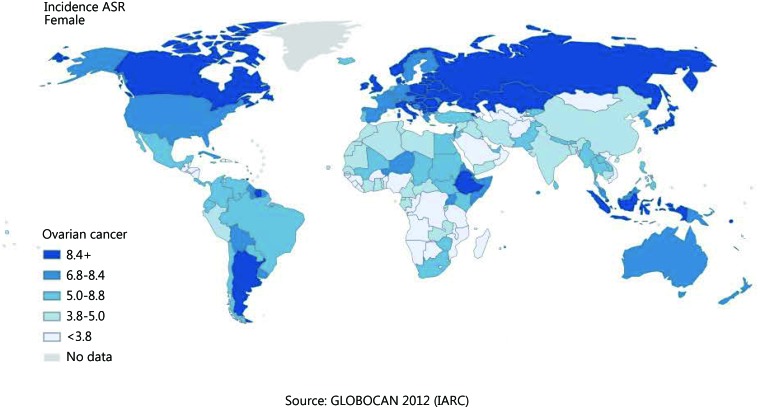
OC incidence exhibits wide geographic variation ( Figure 1 )32. The highest age-adjusted incidence rates are observed in developed parts of the world, including North America and Central and Eastern Europe, with rates generally exceeding 8 per 100,000. Rates are intermediate in South America (5.8 per 100,000), and lowest in Asia and Africa (≤3 per 100,000). Migration from countries with low rates to those with high rates results in greater risk33,34 underscoring the importance of non-genetic risk factors. Within the United States, racial differences in incidence and mortality mimic the observed international variation with rates highest among Whites, intermediate for Hispanics, and lowest among Blacks, and Asians4. Variation within large countries such as China also mimics international variation with incidence and mortality higher within developed, urban regions versus less developed, rural regions35.
1.
Ovarian cancer incidence exhibits wide geographic variation.
In most developed countries, largely including North America and Europe, OC incidence and mortality has gradually declined since the 1990s4,36-40. Conversely, historically less developed countries with recent economic growth and lifestyle changes have seen increases in incidence and mortality rates. In China, the increase is apparent only among rural women rather than those in more developed, urban regions2,41.
Genetic epidemiology
One of the most significant risk factors for OC is a family history of the disease42. First-degree relatives of probands have a 3- to 7-fold increased risk, especially if multiple relatives are affected, and at an early age of onset43-47. Rare high penetrant mutations in theBRCA1 andBRCA2 genes greatly increase lifetime risk48 and account for the majority of hereditary cases and 10%–15% of all cases49-57. Data from the Breast Cancer Linkage Consortium suggest the risk of OC through age 70 years is up to 44% inBRCA1 families58 and approaches 27% inBRCA2 families59. Hereditary non-polyposis colorectal cancer syndrome (HNPCC)60 may account for at least 2% of cases and confer up to a 20% lifetime risk48,61-64. Women with mutations in DNA repair genes, such asBRIP1,RAD51C, andRAD51D have estimated lifetime risks of 5.8%, 5.2%, and 12%, respectively65,66. Deleterious mutations in BRCA1/2 and other double-strand DNA break repair genes are more strongly associated with HGSOC susceptibility although they do occur in other tumor subtypes65-67. HNPCC associated OC typically presents as endometrioid or clear cell tumors rather than the common serous subtype68,69.
Collectively, known syndromes account for 36% of OC familial relative risk70. Genome-wide association studies71-80 have discovered 22 susceptibility alleles for invasive OC with weak to moderate effects in European populations ( Table 1 ). Eighteen of these risk loci are associated with all and/or serous OC, five are associated with MOC risk, one is associated with ENOC, and one is associated with CCOC, exemplifying the genetic heterogeneity by histotype. In addition, a large-scale pooled analysis of genome-wide association studies of ovarian, breast, and prostate cancers identified five novel loci81. The identified common risk alleles account for approximately 4% of the polygenic risk in the European population and, taken together with high risk alleles, explain 40% of the heritability82. Chen et al.83 conducted a genome-wide association study of 4,464 Han Chinese women that identified two novel loci (9q22.33 and 10p11.21) and evidence that four loci previously reported in European populations (3q25, 17q12, 17q21, and 19p13.11) may also influence risk.
1.
Common, low penetrance alleles associated with epithelial OC susceptibility
| Cytoband | SNP | BP (gene) | MAF | Histotype | OR (95% CI) | P | Consortia/studya | Referenceb |
| All=all histotypes; Serous=high and low grade serous histotypes; Mucinous=borderline/LMP and invasive mucinous histotypes; Low-grade serous=borderline/LMP serous histotypes.a Ovarian Cancer Association Consortium (OCAC) of case-control studies in European women; Consortium of Investigators of Modifiers of BRCA1/2 (CIMBA) European population; Breast Cancer Association Consortium (BCAC) European population; Prostate Cancer Association Group to Investigate Cancer Associated Alterations in the Genome (PRACTICAL) European population; Chinese GWAS of six studies: Tianjin Ovarian Cancer Study (TOCS), Chinese Academy of Medical Sciences Cancer Hospital (CAMSCH), Beijing University of Chemical Technology (BUCT), Nanjing Ovarian Cancer Study (NOCS), Shanghai Ovarian Cancer Study (SOCS), and Guangzhou Ovarian Cancer Study (GOCS).b First genome-wide significant SNP results reported and referenced. Loci may have been identified or replicated in other GWAS.c MAF in affected subjects reported.d Pleiotropic variant associated with ovarian, breast, and prostate cancers.e Pleiotropic variant associated with ovarian and breast cancers.f OR are reported from OCAC (not CIMBA) study since no meta-analysis OR were reported.g OR and MAFs are reported from Stage 1 OC cases whileP-values are from meta-analysis of all stages, all phases. | ||||||||
| 1p36 | rs56318008 | 22470407 (WNT4) | 0.15 | All | 1.11 (1.07–1.16) | 7.6E-09 | OCAC + CIMBA | Kuchenbaecker, 2015f |
| 1p34.3 | rs58722170 | 38096421 (RSPO1) | 0.23 | Serous | 1.12 (1.08–1.18) | 2.7E-12 | OCAC + CIMBA | Kuchenbaecker, 2015f |
| 2q13 | rs17041869 | 111896243 (BCL2L11) | 0.88 | Alld | 0.94 (0.93–0.96) | 5.1E-09 | OCAC + BCAC + PRACTICAL | Kar, 2016 |
| rs752590 | 113972945 | 0.21 | Mucinous | 1.34 (1.21–1.49) | 3.3E-08 | OCAC | Kelemen, 2015 | |
| 2q31.1 | rs711830 | 177037311 (HOXD3) | 0.32 | Mucinous | 1.30 (1.20–1.40) | 7.5E-12 | OCAC | Kelemen, 2015 |
| rs2072590 | 177042633 (HAGLR) | 0.32 | Serous | 1.20 (1.14–1.25) | 3.8E-14 | OCAC | Goode, 2010 | |
| 3q25 | rs7651446 | 156406997 (TIPARP) | 0.05 | All | 1.44 (1.35–1.53) | 1.5E-28 | OCAC | Pharoah, 2013 |
| 4q26 | rs17329882 | 119949960 (SYNPO2) | 0.24 | All | 1.09 (1.06–1.13) | 1.4E-08 | OCAC + CIMBA | Kuchenbaecker, 2015f |
| 4q32.3 | rs4691139 | 165908721 | 0.48 | All | 1.20 (1.17–1.38) | 3.4E-08 | CIMBA | Couch, 2013 |
| 5p15.33 | rs10069690 | 1279790 (TERT) | 0.26 | Serous | 1.15 (1.11–1.20) | 1.3E-11 | OCAC | Bojesen, 2013 |
| 6p22.1 | rs6456822 | 28480635 (GPX6) | 0.31 | Serous | 0.91 (0.87–0.94) | 3.0E-08 | OCAC + CIMBA | Kuchenbaecker, 2015f |
| 8q21.13 | rs11782652 | 82653644 (CHMP4C) | 0.07 | Serous | 1.24 (1.16–1.33) | 7.0E-10 | OCAC | Pharoah, 2013 |
| 8q24.21 | rs10088218 | 129543949 (LINC00824) | 0.13 | Serous | 0.76 (0.70–0.81) | 8.0E-15 | OCAC | Goode, 2010 |
| 9p22 | rs3814113 | 16915874 | 0.27c | Serous | 0.77 (0.73–0.81) | 4.1E-21 | OCAC | Song, 2009 |
| 9q22.33 | rs1413299 | 101761241 (COL15A1) | 0.48c | All | 1.53 (1.25–1.86) | 1.88E-08 | Chinese GWAS | Chen, 2014g |
| 9q31 | rs200182588 | 106856690 (SMC2-AS1) | 0.56 | Alle | 0.95 (0.94–0.97) | 8.9E-09 | OCAC + BCAC | Kar, 2016 |
| 9q34.2 | rs635634 | 136155000 | 0.85 | All | 1.11 (1.07–1.16) | 4.4E-09 | OCAC + CIMBA | Kuchenbaecker, 2015f |
| 10p11.21 | rs1192691 | 37169295 | 0.38c | All | 0.71 (0.60–0.83) | 2.62E-08 | Chinese GWAS | Chen, 2014g |
| 10p12 | rs1243180 | 21915619 (MLLT10) | 0.31 | All | 1.10 (1.06–1.13) | 1.8E-08 | OCAC | Pharoah, 2013 |
| 11q12 | rs7937840 | 61893972 (INCENP) | 0.26 | Alld | 1.05(1.03–1.06) | 5.0E-09 | OCAC + BCAC + PRACTICAL | Kar, 2016 |
| 15q26 | rs8037137 | 91506637 (RCCD1) | 0.86 | Alle | 1.07 (1.05–1.10) | 9.1E-10 | BCAC + OCAC | Kar, 2016 |
| 17q11.2 | rs143663961 | 29181220 (ATAD5) | 0.95 | All | 0.91 (0.88–0.94) | 2.6E-09 | OCAC + CIMBA | Kuchenbaecker, 2015f |
| 17q12 | rs7405776 | 36093022 (HNF1B) | 0.38 | Serous | 1.13 (1.09–1.17) | 3.1E-10 | OCAC | Shen, 2013 |
| rs11651755 | 36099840 (HNF1B) | 0.49 | Clear cell | 0.77 (0.70–0.84) | 1.6E-08 | OCAC | Shen, 2013 | |
| 17q21.31 | rs2960000 | 43534353 (PLEKHM1) | 0.18 | Serous | 1.16 (1.12–1.20) | 3.3E-10 | OCAC | Permuth-Wey, 2013 |
| 17q21.32 | rs9303542 | 46411500 (SKAP1) | 0.27 | All | 1.12 (1.08–1.16) | 6.0E-11 | OCAC | Pharoah, 2013 |
| 19p13.11 | rs2363956 | 17394124 (ANKLE1) | 0.51c | Serous | 1.16 (1.11–1.21) | 3.8E-11 | OCAC | Bolton, 2011 |
| rs1469713 | 19528806 (GATAD2A) | 0.64 | Alld | 0.96 (0.95–0.97) | 3.4E-10 | OCAC + BCAC + PRACTICAL | Kar, 2016 | |
| 19q13.2 | rs688187 | 39732752 | 0.32 | Mucinous | 0.67 (0.60–0.75) | 6.8E-13 | OCAC | Kelemen, 2015 |
Risk factors and preventive factors
Hormonal and reproductive risk factors
Epidemiological research has clearly implicated hormonal and reproductive factors in the pathogenesis of OC. Two predominant hypotheses have emerged to fit the data84. The ‘incessant ovulation’ hypothesis posits that the number of ovulatory cycles increases the rate of cellular division associated with the repair of the surface epithelium after each ovulation, thereby increasing spontaneous mutations85. The correlation between increasing numbers of lifetime ovulations and higher risk86-89 are consistent with this hypothesis. The ‘gonadotropin hypothesis’ attributes the impact to gonadotropins, such as luteinizing hormone and follicle-stimulating hormone90. Both of these proposed mechanisms provide a framework to interpret the epidemiologic data on both endogenous correlates of reproductive hormone exposure and exogenous sources of hormones. A more detailed review is available by Riman et al.91.
Age at menarche and age at menopause
According to the incessant ovulation hypothesis, early age at menarche and late age at menopause increases risk by increasing the number of ovulatory cycles. Conversely, according to the gonadotropin hypothesis, a late age at menopause delays the surge of post-menopausal gonadotropin hormones, possibly reducing risk. Results of studies that have examined the age at onset of menses are not terribly consistent92-102. One study among Chinese women reported lower risk with late age at menarche (after age 18)103, while another study observed a slight increased risk with late age at menarche104. Additional research has failed to clarify the literature85,93,105-112 although a meta-analysis yielded an overall inverse association with age at menarche (RR=0.85, 95% CI: 0.75–0.97)113. Data on age at natural menopause and OC risk are also inconsistent. Case-control studies have reported odds ratios ranging from 1.4 to 4.6 in the highest category of age at menopause92,93,95,99,103,104,108. In the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort, age at menopause (>52vs. ≤45 years) was associated with an increased risk (HR=1.57, 95% CI: 1.16–2.13); however after women diagnosed with OC within the first two years of follow-up were excluded the risk was slightly attenuated and marginally statistically significant (HR=1.40, 95% CI: 0.98–2.00)109. The authors speculated that older women in the sub-clinical stage of OC may mistake bleeding for menses. Other case-control studies98,100,106,107,114-116 and several cohort studies101,105 found no association. The inconsistent findings with ages at menarche and menopause may reflect differences in definitions, recall and misclassification bias, or differences in analysis117. The etiologic heterogeneity of tumor subtypes may also contribute to differential findings. A report from the Nurses’ Health Study (NHS) and NHS II found that age at natural menopause was associated with an increased risk of endometrioid tumors (RR=1.13, 95% CI: 1.04–1.22), but not serous invasive or mucinous tumors29. Studies conducted among populations with different distributions of age at menarche99,111,118 and age at menopause119 indicate differences in the genetic heritability of these factors across ancestral groups120-122. Regardless, the available evidence suggests that any magnitude of effect is likely small.
Parity and infertility
The association between pregnancy and OC risk has been studied extensively. Pregnancy causes anovulation and suppresses secretion of pituitary gonadotropins and is thus consistent with both the ‘incessant ovulation’ and the ‘gonadotropin’ hypotheses. Indeed, parous women have a 30%-60% lower risk than nulliparous women85,92,99,103-107,115,117,123-126 and each additional full-term pregnancy lowers risk by approximately 15%98,105,127. Studies in African American128 and Asian129,130 populations have yielded similar results. The protective effect associated with parity is evident across the main histotypes although perhaps slightly weaker for serous carcinomas, with roughly 20% lower risk in parous women, versus other subtypes, particularly clear cell and endometrioid that show 50%–70% reductions in risk28-30,131,132. Comparable to the breast cancer literature, case-control studies with hospital controls have reported elevated risk with late age at first birth (>30 years of age)92,97,98,106,108,123,133-136, but not among studies with population controls96,98,137. Recent data also suggests that OC risk does not vary by the time interval between the first and last birth138.
It is unclear whether spontaneous or induced abortions impact OC risk. About half of the published studies found that an increased number of incomplete pregnancies may slightly decrease risk85,92,97,98,104,105,139-141 while others have reported risk to be increased107,126, or not affected96,99,100,102,106,115,123,125,142. Induced abortions have been associated with lower risk in several studies105,140,141, but not others96,108,139. With regard to spontaneous abortions, positive100,123,139, inverse102, and null associations103,125,140 with risk have been reported. Interpretation of this literature is difficult because of the recognized potential for recall bias Should be 'abortions' here not pregnancies but better to end at recall bias.143.
Infertility is a term that is used to describe a heterogeneous group of biologically distinct conditions ranging from genital tract infections and tubal disturbances to medical conditions such as endometriosis and polycystic ovarian syndrome (PCOS)144,145. Infertility appears to be a risk factor in most studies92,98,102,106,115,123,125,126,136,144, but not all105,146. The inconsistent results may reflect the failure to examine the various types of infertility separately. It is yet to be determined whether nulliparity and low parityper se, rather than difficulty becoming pregnant due to female infertility, is the relevant factor. Infertility seems to pose the greatest risk among women who remain nulliparous, while periods of temporary infertility among parous women are of little concern92,98,102,106,125. For example, in a large Canadian case-control study in which most nulliparous women were so by choice, infertility was not associated with risk among parous women but there was a trend towards elevated risk among a small group of infertile nulliparous women (OR=2.5, 95% CI: 0.6–4.1)102. A particular challenge is trying to distinguish an influence of infertility from an adverse effect of fertility drug exposure. Although some studies report that women with a prior history of fertility drug use who remain nulliparous are at an elevated risk for ovarian tumors, particularly tumors of LMP98,147, the results are not consistent144-146,148-150. Early detection bias may explain the discrepant findings, as early-stage cancers may be over-diagnosed in infertile women due to the close medical surveillance151. Further muddying of the water is caused by factors that may influence both infertility and OC risk such as a personal history of endometriosis152-154, PCOS155, and BRCA1 mutations156.
Lactation
Lactation suppresses secretion of pituitary gonadotropins and leads to anovulation, particularly in the initial months after delivery157. Both the incessant ovulation and gonadotropin hypotheses would predict lactation reduces the risk of OC. In fact, most studies indicate a slight protective effect from breastfeeding, with odds ratios approximating 0.6–0.798,99,102,124-126,158-161, although some have not96,100,115. Few studies have explored the association by tumor subtype, with one report of the greatest risk reduction for endometrioid tumors162 while another observed the strongest reduction among mucinous cancers30. A recent meta-analysis indicates a significant protective effect (summary RR=0.68, 95% CI: 0.61–0.76) for breastfeeding that increased with longer duration (summary RR=0.85, 0.73, and 0.64 for <6 months, 6–12 months, and >12 months of total breastfeeding duration)163. Thus, lactation protects against epithelial OC, especially for long-term duration.
Benign gynecologic conditions and gynecologic surgery
Several gynecologic conditions have been examined as risk factors for OC, including PCOS, endometriosis, and pelvic inflammatory disease (PID). PCOS is a multi-factorial disease often characterized by obesity, hirsutism, infertility, and menstrual abnormalities. Due to unopposed endogenous estrogen and/or elevated androgens, women with PCOS have an increased risk for endometrial cancer. The association between PCOS and OC risk was investigated using data from the Cancer and Steroid Hormone Study, a population-based case-control study155. Among 476 histologically confirmed epithelial OC cases and 4,081 controls, 7 cases (1.5%) and 24 controls (0.06%) reported a history of PCOS (OR=2.5, 95% CI: 1.1–5.9)155. The limited data was insufficient for a consensus statement that PCOS is a risk factor164. Larger studies that adjust for potential confounders are clearly needed.
Endometriosis is one of the most common gynecological disorders, affecting 10%–15% of women in reproductive years165. Despite being considered a benign condition, endometriosis has been linked with OC in the medical literature since 1925. Sayasneh and colleagues165 conducted a systematic review of eight studies; seven reported an increased risk of OC, with effect sizes ranging from 1.3 to 1.9. The strongest associations with endometriosis are evident among endometrioid and clear cell histologies30,165,166, consistent with molecular data that supports endometrial epithelium as the origin of these subtypes8. In addition, Pearce and colleagues167 identified an increased risk of low-grade serous OC (OR=2.11, 95% CI: 1.39–3.20) among women with endometriosis as well as for endometrioid (OR=2.04, 95% CI: 1.67–2.48) and clear cell cancers (OR=3.05, 95% CI: 2.43–3.84). The authors speculated that the processes of endometriosis and endosalpingiosis may result from a similar underlying host susceptibility to implantation of exfoliated Müllerian epithelial cells from both the endometrium and fallopian tube. The association between endometriosis and endometrioid and clear cell ovarian carcinomas may represent shared risk factors165, genetic susceptibility168, and/or pathogenesis169 rather than a causal association.
PID causes inflammation of the endometrium, fallopian tubes, and ovaries. Studies evaluating the association between PID and OC risk have yielded inconsistent results103,170-172. Lin and colleagues173 evaluated this association in a large nationwide cohort from Chinese Taiwan that included 67,936 women with PID (42 of whom later developed OC) and 135,872 women without a history of PID (48 of whom developed OC). A history of PID was a significant risk factor (adjusted HR=1.92, 95% CI: 1.27–2.92), especially among subjects diagnosed with PID before the age of 35 and women who had at least 5 episodes of PID. Other studies found no association171,172. In the Danish MALOVA (MALignant OVArian tumor) case-control study of 2,300 women, PID history was associated with increased risk of ovarian borderline tumors but not with invasive OC174. Rasmussen et al.175 further evaluated borderline ovarian tumors in a cohort of over 1.3 million Danish women and found that history of PID was associated with an 85% increased risk of serous borderline tumors but not those of the mucinous subtype. In previous studies of PID and OC risk, some only considered invasive tumors103,108,173 whereas others included both invasive and borderline tumors172 perhaps contributing to the inconsistent findings. There is no evidence that risk associated with PID history varies by histotype of invasive ovarian carcinomas172,174.
Several gynecologic procedures appear to influence the risk for OC. It is well established that among high risk women, bilateral prophylactic oophorectomy decreases risk by at least 90%176. Numerous studies have identified a reduced risk associated with either a hysterectomy or tubal ligation ranging from 30%–40%92,102,177-183 with the highest risk reductions observed among endometrioid and clear cell histotypes30,181,184-187. Furthermore, the risk reduction from these procedures appears to last for at least 10–15 years, which argues against screening bias (due to selective removal of subclinical ovarian tumors)116,178,188,189. Although it is unknown how these procedures reduce the risk of OC, it has been proposed that through retrograde menstruation (i.e. menstrual fluid flows backwards into the fallopian tubes instead of leaving the body through the vagina) endometrial tissue implants on peritoneal and ovarian surfaces (endometriosis) and becomes invasive, developing into endometrioid or clear cell ovarian carcinomas13,190. Indeed, this hypothesis is supported by epidemiological studies that show the strongest associations with tubal ligation and endometriosis for ENOC and CCOC.
Oral contraceptives and other forms of contraception
The epidemiological literature over the past several decades has consistently reported that use of oral contraceptives is inversely associated with the risk of OC. The protective effect increases with longer duration of use98,102,191-195 with about a 20% decreased risk for each 5 years of use that persists decades after use has ceased115,124,193,196-200. Moreover, the risk reduction does not appear to be specific to any particular oral contraceptive formulation195,201 or OC histotype, although oral contraceptive use appears less effective for mucinous cancers in some studies23,27,28,30,118,131,200. Oral contraceptive use corresponds to the prevention of approximately 30,000 OC cases every year and has already prevented an estimated 200,000 OC cases and 100,000 deaths over the last 50 years200. Progestin-only contraceptives have been less studied, mostly due to the low prevalence of use, but the available data suggest they may also lower risk of OC124,193,202.
Relatively few studies have examined methods of contraception other than oral contraceptives. The use of an intrauterine device (IUD) has been associated with reduced OC risk in several studies182,203,204 while the NHS cohort observed increased risks205, however, there was a low prevalence of IUD use in that population which occurred prior to the newer IUD formulations. Similar to oral contraceptives, any protective effect associated with IUD use may be dependent upon duration of use. Huang and colleagues203 evaluated IUD use and OC risk in the Shanghai Women’s Health Study cohort and found long-term IUD use of at least 20 years was associated with a 38% reduction in risk. IUD use is the most common contraceptive method in China with a prevalence rate of about 50% among women of reproductive age206. The authors propose that the high prevalence of long-term IUD use and the associated strong protective effect may contribute to the low incidence of OC observed in China203. Vasectomy has been evaluated in association with OC risk and findings have been inconclusive205, although Ness and colleagues182 reported that vasectomy may confer a small reduction in risk (adjusted OR=0.77, 95% CI: 0.61–0.99), perhaps due to reduced exposure to sperm. Given that contraceptive methods are modifiable, further research to replicate these findings is needed. Additionally, research is needed to elucidate how different types of contraception influence OC risk, especially by histotype.
Hormone replacement therapy (HRT)
Unlike oral contraceptive use that has a well-established benefit on OC risk, the association with HRT is less clear. HRT reduces the secretion of gonadotropins and should therefore decrease risk, but the reduced levels are still higher than pre-menopausal women207. Conversely, postmenopausal HRT may enhance estrogen-induced proliferation of ovarian cells and therefore increase risk208. Initial studies on the topic have focused on unopposed estrogen therapy (ET) among postmenopausal women. Several case-control98,209,210, cohort211 and meta-analysis212,213 studies have found no association with duration of use, although two have observed either a significant or suggestive trend in increased risk23,214. More recent studies indicate that OC risk is increased in ever users of HRT215-218 and larger increases are seen for longer durations of use219-223. For example, in the NHS cohort both current and past HRT users of five or more years had a significantly higher risk than never users (RR=1.41, 95% CI: 1.07–1.86 and RR=1.52, 95% CI: 1.01–2.27, respectively), but no association with risk was seen for users of less than five years for either current or past users (RR=1.01, 95% CI: 0.70–1.44 and RR=0.88, 95% CI: 0.64–1.19, respectively)219. The authors concluded that the elevated risk appeared to be driven largely by duration rather than by status of use. Conversely, a collaborative re-analysis of 52 epidemiological studies found OC risk was increased in current HRT users, even those with less than 5 years of use224. Furthermore, risk decreased over time after cessation of use, although a small excess in risk was still observed even 10 years after stopping long duration HRT.
Combined estrogen and progestin use and OC risk have only recently been evaluated in studies with sufficient statistical power. It has been hypothesized that progestin promotes apoptosis while estrogen promotes proliferation of ovarian epithelial cells225 thus the effects of unopposed ET are thought to be more detrimental to the ovaries than estrogen plus progestin (EPT)225. Most studies that investigated EPT use and OC risk have found no association or a weak protective association118,215,216,218,219,222,225-227. A few prospective studies215,221,228 and meta-analysis217 have reported a small increased risk for EPT users compared to ET only users. For example, a recent meta-analysis of 14 population-based studies concluded that ET is associated with a 22% increased risk of OC per 5-year increment of use; however, the risk among women who used EPT was attenuated to only a 10% increase216. The authors suggest that the addition of progestin mitigates the effect of estrogen, because the increased risk among EPT users was statistically significantly lower than the risk among ET users (P=0.004)216. However, several prospective cohort studies observed similar increased risks for both ET and EPT users224,228. The basis for the inconsistent literature is not readily apparent.
Some studies have indicated that any HRT-associated risk is limited to specific histologic subtypes. For example, in the NHS the increased risk was slightly stronger for endometrioid tumors and was not present for mucinous tumors, consistent with other studies29,30,131,210,229. Endometrioid tumors are histologically similar to endometrial tissue230 and ET use increases the risk of endometrial cancer208, enhancing plausibility.
The available data indicates that HRT is a risk factor for OC. The magnitude may be moderate, but women should be counseled about the potential dangers of long-term use, particularly for unopposed ET. Although large-scale reductions in hormone therapy have occurred since reports of negative health effects from the Heart and Estrogen/Progestin Replacement Study (HERS) and the Women’s Health Initiative (WHI)231, approximately 12% of women over 40 still take HRT for menopausal symptoms232,233 totaling some 6 million women in the USA and UK alone224. Given the prevalence of HRT and that many women take HRT several years before the peak age-specific incidence of OC, even a small change in risk may have a significant impact on OC rates at the population level.
Obesity
In postmenopausal women the predominant source of circulating estrogens is aromatization of androgens in adipose tissue84,234. The compelling role of obesity in the pathogenesis of hormone-related cancers, such as endometrial and post-menopausal breast cancers235, has prompted research on the potential association with OC236. One measure of great interest is body mass index (BMI), calculated as weight in kilograms divided by height in meters squared. A 2007 meta-analysis of 28 population studies reported an increased risk of OC for overweight women (BMI of 25–29.9 kg/m2) and obese women (BMI ≥ 30 kg/m2) compared with normal weight (BMI of 18.5–24.9 kg/m2), pooled RR=1.2 and 1.3, respectively237. In a 2008 analysis of 12 prospective cohort studies, an increased risk was seen among pre-menopausal obese women compared to normal weight women (RR=1.72; 95% CI: 1.02–2.89); however, this increased risk was not apparent among post-menopausal women (RR=1.07; 95% CI: 0.87–1.33)238. A more recent analysis of 12 case-control studies by the Ovarian Cancer Association Consortium (OCAC) also found that the positive association with BMI was stronger among pre-menopausal women239. Conversely, the EPIC cohort study observed the strongest risk associations for measures of adiposity (BMI and weight) among post-menopausal women240. In the NHS, greater hip circumference, a measure of fat distribution, was a risk factor among post-menopausal women, but waist-to-hip ratio, waist circumference and BMI were not241.
Several studies have evaluated obesity and OC risk stratified by HRT use239-244. The results for BMI did not differ by HRT use in the OCAC analysis, NHS, or EPIC study. In contrast, three studies observed an increased risk only for obese women that have never used HRT [RR 1.8 (95% CI: 1.2–2.8)242 and RR=1.10 (95% CI: 1.07–1.13)244] and for never HRT users with greater weight gain since age 18 (RR=1.8; 95% CI: 1.0–3.0 for ≥40 lbs.vs. stable weight), a larger waist circumference (RR=1.8; 95% CI: 1.1.–3.0 for ≥35vs. <35 inches) and a larger waist-to-height ratio (RR=1.8; 95% CI: 1.1.–3.1 for ≥35vs. <35 inches)243.
The risk associated with obesity may be specific to non-serous and low-grade serous subtypes. Two large-scale pooled analyses, one performed by OCAC239 and another by the Collaborative Group on Epidemiological Studies of Ovarian Cancer244, observed the strongest risk increases for borderline serous tumors (OR/RR=1.24 and 1.29 per 5 kg/m2, respectively) and somewhat lower increases for clear cell (OR/RR=1.06 and 1.05 per 5 kg/m2), mucinous (OR/RR=1.19 and 1.15 per 5 kg/m2), and endometrioid (OR/RR=1.17 and 1.08 per 5 kg/m2) tumors. Overall, serous tumors were not associated with an increased risk in either study, however, the OCAC analysis included stratification by tumor grade and found an increased risk for low-grade serous tumors only (OR=1.13 per 5 kg/m2). OCAC confirmed these findings in a later Mendelian randomization study where genetically predicted BMI was associated with an increased risk for non-high-grade serous subtypes only (OR=1.29; 95% CI: 1.03–1.61 per 5 BMI units) and the strongest increase was observed for low-grade serous tumors (OR=1.93; 95% CI: 1.33–2.81)245. An increased risk for OC has been observed between waist-to-hip ratio and risk of mucinous tumors (HR per 0.05 unit increment=1.19; 95% CI: 1.02–1.38), but not with serous, endometrioid, or clear cell tumors240. The large prospective NIH-AARP Diet and Health Study reported obese women had elevated risk of endometrioid OC (RR=1.64; 95% CI: 1.00–2.70), but not for serous131. Similarly, in the NHS, obesity was associated with increased endometrioid risk29; however, in a systematic review only the pooled analysis and one case-control study found BMI to be associated with an increased risk of endometrioid OC237.
In summary, elevated BMI appears to increase risk of OC. Since adiposity is a modifiable risk factor for OC, other cancers and other chronic diseases, weight control is prudent.
Diet and nutrition
Despite numerous analytical epidemiological studies, whether diet affects risk of OC is largely unresolved. The notable exception is intake of vegetables, for which the evidence that higher intakes are associated with lower risk is emerging246 and to a certain extent also for consumption of whole grain foods and low-fat milk. Associations with specific fats and oils, fish and meats and certain milk products are inconsistent and no firm conclusions can be made. Recently, the EPIC cohort study and Netherlands Cohort Study performed a nutrient-wide association analysis evaluating 28 foods/food groups and 29 nutrients by dietary questionnaires from 430,476 women including 1,522 incident OC cases. Meta-analysis of the two cohort studies found that women with a high intake of saturated fats had elevated risks (HR=1.21, 95% CI: 1.04–1.41). Studies on meat consumption are not consistent247-249. A large prospective study found that women in the highest intake quartile of dietary nitrate had an increased risk of OC (HR=1.31, 95% CI: 1.01–1.68, andP=0.02). Similarly, the association between coffee and tea intake is inconclusive104,108,250-256.
Although the majority of vitamin D is produced in the skin from UV-B exposure257, it is also partly obtained from our diet or dietary supplements. Vitamin D is converted to 25-hydroxyvitamin [25(OH)D] in the liver and metabolized to the active form in the kidney. 1, 25-dihydroxyvitamin D [1, 25(OH)2D3] is involved in bone metabolism, modulation of the immune response, and regulation of cell proliferation and differentiation257,258. Experimental studies have shown that 1, 25(OH)2D3 inhibits cell proliferation in OC cell lines and induces apoptosis259. However, epidemiological evidence that vitamin D status influences OC risk is inconsistent. One systemic review concluded that there is no strong evidence that vitamin D decreases risk260 and a meta-analysis of ten longitudinal studies261 as well as other cohort studies262 reached a similar conclusion. In the meta-analysis the protective effect was evident in seven of the ten studies and the pooled estimate was a 17% reduced risk with increasing 25(OH)D levels; however, the pooled estimate was not statistically significant (RR = 0.83, 95% CI: 0.63–1.08)261. To address the conflicting findings from observational studies, a recent Mendelian randomization study263 of almost 32,000 European women was conducted and found single nucleotide polymorphisms (SNPs) associated with circulating vitamin D levels were associated with an increased risk of OC (OR=1.27; 95% CI: 1.06–1.54). The beneficial effect of vitamin D may be more pronounced among overweight or obese women259,264 perhaps reflecting differential bioavailability of circulating 25(OH)D levels259.
A complementary approach has been to examine SNPs in the vitamin D receptor, which mediates the biological activity of the active form of vitamin D and interacts with other cell-signaling pathways258,265,266. The vitamin D receptor polymorphism FokI is among the most extensively studied and several studies have observed an increased OC risk among carriers267,268. Associations with other common vitamin D receptor variants, BsmI, ApaI, and TaqI, and OC risk remain controversial269. Prescott and colleagues270 investigated all vitamin D receptor variants genotyped as part of a GWAS stratified by predicted 25(OD)D scores (highvs. low) derived from known determinants of serum 25(OH)D270. There was evidence that OC risk was increased for minor allele carriers of rs731236 (OR=1.31) and rs7975232 (OR=1.83) among women with high predicted 25(OH)D but these findings require replication.
Exercise and physical activity
The general health benefits of exercise are well established and a specific effect on OC might be expected, at least indirectly, through the resulting reduction of adipose tissue (and therefore estrogen levels), lower ovulation frequency, and reduced chronic inflammation271. To date, 29 epidemiological studies have investigated physical activity and OC risk, including fourteen prospective cohort studies272-285, two historical cohort studies286,287, ten population-based case-control studies252,288-296 and three hospital-based case-control studies297-299. Results are not entirely consistent, but a 2007 meta-analysis estimated a nearly 20% lower risk for the most active women compared to the least active (pooled relative risk=0.81, 95% CI: 0.72–0.92)292. Most studies that measured physical activity across the lifespan reported consistent null findings278,279,282,290,292 or risk reductions252,289,291,297 in each age period. Similarly, prolonged sedentary behavior278, high levels of total sitting duration283,285,300, and chronic recreational physical inactivity295 have all been noted to increase risk. The benefit of physical activity does not appear to vary by histological type285,295 but there are insufficient data to draw firm conclusions291,294. Although further research can refine the picture, when considering the additional benefits of exercise on weight control, bone density, and heart disease, the promotion of regular activity should be encouraged.
Other lifestyle and environmental factors
Cigarette smoking
The majority of early reports concluded that smoking was not a risk factor125,253,301,302. Results from more contemporary studies suggest this is most likely because analyses were not conducted separately for histologic subtypes. Indeed, smoking appears to increase the risk for mucinous OC in a dose-response manner, but not other subtypes22,26,30,303. In 2012, a meta-analysis of 51 epidemiological studies concluded that current smokers have a 50% increase in invasive mucinous OC risk and an over two-fold increase in borderline mucinous OC risk (summary RR=2.25, 95% CI: 1.64–3.08) compared to never smokers, but no increased risk of serous (0.96, 95% CI: 0.87–1.06) or clear cell (0.80, 95% CI: 0.63–1.01) cancers and lower risk of endometrioid cancers (0.82, 95% CI: 0.71–0.95)304. In another meta-analysis, the risk of mucinous cancer increased in a dose-response relationship with amount smoked, but returned to that of never smokers within 20–30 years of stopping smoking305. Histologically, mucinous ovarian tumors resemble mucinous gastrointestinal cancers, some of which (pancreatic gastric, and colorectal cancers) have also been associated with smoking305,306. Collectively, these findings suggest that risk of OC is one more reason to avoid cigarette smoking.
Alcohol consumption
Alcohol consumption increases circulating concentrations of androgens, estrogens, and other sex hormones in serum and urine and has been linked to increased risk of breast cancer307,308. Studies of alcohol use and OC are inconsistent, with null associations99,125,252,253,309-312, evidence for increased risk104,313,314 and decreased risk315-317. There have been efforts to resolve the observed inconsistency by quantifying risk by the type of alcohol consumed (wine, beer, or alcohol)314,315,318, histologic subtype of the tumor314,315,317, or by other potential modifiers such as dietary fiber intake319. In a large population-based case-control study320, consumption of beer (not liquor or wine) during early adulthood (20–30 years of age) was associated with a moderately increased risk of invasive OC, with the association limited to serous tumors (OR=1.52, 95% CI: 1.01–2.30), though results for other histological subtypes were based on sparse data. This risk was associated with regular consumption (1 or more drinks per day), and there was no evidence of a dose response relationship. Data from the Netherlands Cohort Study on Diet and Cancer found no risk association with alcohol consumption in the form of wine, beer, or liquor321. A pooled analysis of 10 cohort studies that included over 500,000 women and 2,001 incident OC cases also observed no risk association with total alcohol intake (pooled multivariate RR=1.12, 95% CI: 0.86–1.44 comparing > 30 to 0 g of alcohol per day) or alcohol intake from wine, beer, or spirits322. There was no association (OR=1.13, 95% CI: 0.92–1.38) between wine consumption and OC risk in a recent meta-analysis of 10 studies (3 cohort and 7 case-control studies) with 135,871 women, including 65,578 wine drinkers323. Based on these data, it seems reasonable to conclude that if alcohol intake does influence risk of OC, the magnitude is small and possibly limited to particular histologic subtypes.
Asbestos and talcum powder
Both human324,325 and animal studies326 have found asbestos fibers in the ovaries. However, a link between asbestos exposure and OC has not been firmly established, partly due to small numbers of exposed women and disease misclassification (i.e. peritoneal mesothelioma, an asbestos-related disease, is often misdiagnosed as OC on death certificates). A systematic review and meta-analysis of fourteen cohort and two case-control studies327 noted a statistically significant 75% excess risk of OC in women who had been exposed to asbestos (effect size=1.75, 95% CI: 1.45–2.10). However, the association was attenuated (effect size=1.29, 95% CI: 0.97–1.73) among studies that examined cancer incidence based upon pathologically confirmed cases327. Despite the lack of consistency, the International Agency for Research on Cancer (IARC) has declared that evidence is ‘sufficient’ in humans that exposure to asbestos causes OC328.
Similar to asbestos, talcum powder is a silicate that has been studied extensively in relation to cancer risk with inconsistent results. While mechanistic, pathology, and animal studies do not support evidence for the carcinogenicity of talc on the ovarian epithelium329, epidemiological studies have indicated an association with talc use and increased OC risk. In 2006, a meta-analysis of 21 studies330 reported an approximately 35% increase in risk with genital exposure to talc and an earlier meta-analysis had similar findings331. However, more recent studies have continued to report conflicting results. In 2014, the Women’s Health Initiative reported a null association among a cohort of 61,576 post-menopausal women. Cramer and colleagues332 conducted a retrospective case-control study that observed increased risk among talc users similar to those previously reported (OR=1.3, 95% CI: 1.16–1.52), particularly among serous and endometrioid cancers. The study also found that risk was greatest among pre-menopausal women and in post-menopausal women who used hormonal therapy, suggesting estrogen plays a role in the association. In addition, genetic studies suggest that women with certain variants in glutathionine S-transferase M1 (GSTM1) and/or glutathionine S-transferase T1 (GSTT1) may have a higher risk of OC associated with talc use333. Based on the available evidence, in 2006 the IARC classified genital talc use as possibly carcinogenic to humans334.
Drug use
Epidemiological evidence linking PID and endometriosis to increased OC risk suggests inflammation plays an important role in ovarian carcinogenesis. In addition, animal andin vitro studies suggest aspirin inhibits the growth of OC335-337. Several prospective338,339 and case-control340-344 studies have observed an inverse association between aspirin and nonsteroidal anti-inflammatory drugs (NSAIDS) and OC incidence, though other studies have reported no association345,346. Prizment and colleagues339 investigated these drugs using data from a prospective cohort of approximately 20,000 women from the Iowa Women’s Health Study. Compared to women who reported no use of aspirin, the relative risks of OC for those who used aspirin < 2, 2–5 times, and ≥ 6 times per week were 0.83, 0.77, and 0.61, respectively (P=0.04) but no association was observed between NSAID use and risk. Conversely, in the NHS I and II338 regular use of NSAIDS was protective (HR=0.81, 95% CI: 0.64–1.01) but aspirin use was not (HR=1.11, 95% CI: 0.92–1.33). No dose-response relationship with increased frequency or duration of use was observed, and results did not differ when stratifying by tumor histology338. A recent pooled analysis of 12 case-control studies in the OCAC340 found aspirin use was associated with a reduced risk of OC (OR=0.91, 95% CI: 0.84–0.99), especially among daily users of low-dose (<100 mg) aspirin (OR=0.66, 95% CI: 0.53–0.83). Thus, the same aspirin regimen prescribed to protect against cardiovascular events and other cancers (e.g. colorectal cancer) could reduce the risk of OC by 20%–34%340.
A growing body of evidence supports a role for the anti-diabetic agent, metformin, in the prevention and treatment of multiple cancers347. A case-control study including 1,611 incident OC cases was performed using the UK-based General Practice Research Database348. Long-term use (≥ 30 prescriptions) of metformin (and not sulfonylureas or insulin) was associated with a trend towards reduced risk (OR=0.61, 95% CI: 0.30–1.25), but the results were not statistically significant. Additional studies have observed decreased incidence and mortality among metformin treated groups349. Given the absence of good screening tests, the potential for use of metformin as a chemopreventive agent merits further exploration.
Conclusions
OC is a leading cause of cancer incidence and mortality worldwide. This review describes the magnitude of the problem and summarizes epidemiological studies that have identified genetic, environmental, and lifestyle factors that may increase and decrease risk of this lethal disease. These factors have likely impacted the diverse patterns and trends of OC incidence and mortality seen across the globe. Increased and earlier use of oral contraceptives has very likely contributed to the declining trends observed in most developed countries while reduced parity and changes in diet and physical activity could play a role in the increasing trends observed in several countries with economic growth.
Most risk factors show substantial heterogeneity across the five histologic subtypes indicating different etiologies, particularly between mucinous and non-mucinous subtypes ( Table 2 ). The fact that risk factor associations support accepted models of pathogenesis for the individual histotypes give weight to causality, although such inference is limited. Mendelian randomization studies, which exclude explanations such as bias, confounding and reverse causality, have inferred a likely causal effect of BMI on risk of non-HGS OC and of vitamin D on risk of invasive and HGS OC. Additional epidemiological studies of instrumental variables and incorporating tumor histopathology are needed to refine effect estimates for histotypes and enhance causal inference.
2.
Summary of the five major epithelial OC histotypes
| Item | All invasive | High-grade serousa (HGSOC) | Low-grade serous (LGSOC) | Mucinous (MOC) | Endometrioid (ENOC) | Clear cell (CCOC) |
| Weak: ≤25%, Moderate: 25%–50%, Strong: ≥50%, NA=not available, NE=not estimated.a Given that the majority of serous tumors are high-grade, risk associations for overall serous subtype are reported when no data is available by grade. | ||||||
| Precursor lesion | NA | Serous tubal intraepithelial carcinoma (STIC) | Borderline serous tumor | Cystadenoma, borderline mucinous tumor | Atypical endometriosis | Atypical endometriosis |
| Somatic mutations | NA | BRCA1/2, TP53 | BRAF, KRAS | KRAS | PTEN, CTNNB1, ARID1A, PIK3CA | ARID1A, PIK3CA |
| Established risk factor | ||||||
| Age at menarche | Null-weak protection | Null | NE | Null | Null | Weak protection |
| Age at menopause | Moderate increase | Null | NE | Null | Weak risk | Moderate risk |
| Parity | Weak-moderate protection | Weak protection | NE | Weak protection | Moderate protection | Moderate-strong protection |
| Lactation | Weak-moderate protection | Weak protection | NE | Moderate protection | Moderate protection | Null-weak protection |
| Endometriosis | Moderate-strong risk | Null | Strong risk | Null | Strong risk | Strong risk |
| Tubal ligation | Moderate protection | Null-weak protection | Null | Null-weak protection | Strong protection | Strong protection |
| Oral contraceptives | Moderate protection | Moderate protection | NE | Null-weak protection | Moderate protection | Moderate protection |
| Hormone therapy | Moderate risk | Moderate-strong risk | NE | Null | Moderate-strong risk | Null-weak protection |
| Body mass index | Weak risk | Null | Weak risk | Weak risk | Weak risk | Weak risk |
| Smoking | Null | Null | NE | Moderate-strong risk | Null-weak protection | Null-weak protection |
Although many of the risk factors cannot be modified, reflecting the contribution of genetics and unavoidable exposures, a number of others can be altered. Increasing parity and oral contraceptive use lower risk of OC. The same is probably true, but to a weaker degree, of lactation, regular physical activity and avoidance of cigarettes. An individual’s risk is in part a result of the cumulative effect of exposures. Several risk prediction models for OC have been developed to estimate absolute risk based on one’s risk factor profile350-353. The EPIC study350 modeled factors of menopausal status, hormone therapy use, oral contraceptive use, parity, oophorectomy, and BMI and estimated 5- year absolute risks of OC for women aged 68 years varied from 0.10% to 0.24% (lowest 10th percentilevs. highest 10th percentile) depending on the factors. Cumulatively, risk factors accounted for a relative risk of 1.8 for women with the average reported age at menopause (50 years old), average duration of hormone therapy use (2 years), and overweight BMI (25 kg/m2). This cumulative relative risk increases to 3.5 for obese (BMI=30 kg/m2) women with later age of menopause (60 years old) and longer hormone therapy use (5 years). Preventive factors accounted for a cumulative relative risk of 0.47 for women with average parity (2 full-term pregnancies) and oral contraceptive use (5 years) with stronger protection conferred with higher parity and duration of use (RR=0.33, 4 full term pregnancies and 10 years of use). Notably, modifiable factors can mitigate relative risk of unavoidable exposures such as later age of menopause. For example, reducing BMI from 30 to 24 kg/m2, utilizing oral contraceptives for 5 years, and forgoing hormone therapy use, the relative risk of a woman who reaches menopause at 60 is mitigated from 3.5 to 0.99.
It is important to emphasize that the established risk factors aside from highly penetrant gene mutations confer neither large increases in risk nor account for all the variability in the incidence of this disease. Thus, additional causes of OC are yet to be identified. Additional research is needed to better understand the heterogeneous etiology of this deadly disease, with a view to better prevention and early detection strategies.
References
- 1.Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. Lyon, France: International Agency for Research on Cancer, 2013[2016-09-09]. http://globocan.iarc.fr.
- 2.Chen WQ, Zheng RS, Baade PD, Zhang SW, Zeng HM, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–32. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 3.American Cancer Society. Cancer Facts & Figures 2015. Atlanta: American Cancer Society, 2015.
- 4.Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Waldron W, et al. SEER Cancer Statistics Review, 1975–2008, National Cancer Institute. Bethesa, MD, http://seer.cancer.gov/csr/1975_2008/, based on November 2010 SEER data submission, posted to the SEER web site, 2011. (请核对文献类型及格式)
- 5.Allemani C, Weir HK, Carreira H, Harewood R, Spika D, Wang XS, et al. Global surveillance of cancer survival 1995-2009: analysis of individual data for 25676887 patients from 279 population-based registries in 67 countries (CONCORD-2) Lancet. 2015;385:977–1010. doi: 10.1016/S0140-6736(14)62038-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sankaranarayanan R, Ferlay J. Worldwide burden of gynaecological cancer: the size of the problem. Best Pract Res Clin Obstet Gynaecol. 2006;20:207–25. doi: 10.1016/j.bpobgyn.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 7.Chen VW, Ruiz B, Killeen JL, Coté TR, Wu XC, Correa CN, et al. Pathology and classification of ovarian tumors. Cancer. 2003;97:2631–42. doi: 10.1002/cncr.11345. [DOI] [PubMed] [Google Scholar]
- 8.McCluggage WG. Morphological subtypes of ovarian carcinoma: a review with emphasis on new developments and pathogenesis. Pathology. 2011;43:420–32. doi: 10.1097/PAT.0b013e328348a6e7. [DOI] [PubMed] [Google Scholar]
- 9.Prat J. Ovarian carcinomas: five distinct diseases with different origins, genetic alterations, and clinicopathological features. Virchows Arch. 2012;460:237–49. doi: 10.1007/s00428-012-1203-5. [DOI] [PubMed] [Google Scholar]
- 10.The Cancer Genome Atlas Research Network. Integrated genomic analyses of ovarian carcinoma. Nature. 2011;474:609–15. doi: 10.1038/nature10166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marquez RT, Baggerly KA, Patterson AP, Liu JS, Broaddus R, Frumovitz M, et al. Patterns of gene expression in different histotypes of epithelial ovarian cancer correlate with those in normal fallopian tube, endometrium, and colon. Clin Cancer Res. 2005;11:6116–26. doi: 10.1158/1078-0432.CCR-04-2509. [DOI] [PubMed] [Google Scholar]
- 12.Song T, Lee YY, Choi CH, Kim TJ, Lee JW, Bae DS, et al. Histologic distribution of borderline ovarian tumors worldwide: a systematic review. J Gynecol Oncol. 2013;24:44–51. doi: 10.3802/jgo.2013.24.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kurman RJ, Shih IM. The origin and pathogenesis of epithelial ovarian cancer: a proposed unifying theory. Am J Surg Pathol. 2010;34:433–43. doi: 10.1097/PAS.0b013e3181cf3d79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vang R, Shih IM, Kurman RJ. Fallopian tube precursors of ovarian low- and high-grade serous neoplasms. Histopathology. 2013;62:44–58. doi: 10.1111/his.12046. [DOI] [PubMed] [Google Scholar]
- 15.Veras E, Mao TL, Ayhan A, Ueda S, Lai H, Hayran M, et al. Cystic and adenofibromatous clear cell carcinomas of the ovary: distinctive tumors that differ in their pathogenesis and behavior: a clinicopathologic analysis of 122 cases. Am J Surg Pathol. 2009;33:844–53. doi: 10.1097/PAS.0b013e31819c4271. [DOI] [PubMed] [Google Scholar]
- 16.Seidman JD, Khedmati F. Exploring the histogenesis of ovarian mucinous and transitional cell (Brenner) neoplasms and their relationship with Walthard cell nests: a study of 120 tumors. Arch Pathol Labor Med. 2008;132:1753–60. doi: 10.5858/132.11.1753. [DOI] [PubMed] [Google Scholar]
- 17.Piek JMJ, van Diest PJ, Zweemer RP, Jansen JW, Poort-Keesom RJJ, Menko FH, et al. Dysplastic changes in prophylactically removed Fallopian tubes of women predisposed to developing ovarian cancer. J Pathol. 2001;195:451–6. doi: 10.1002/path.1000. [DOI] [PubMed] [Google Scholar]
- 18.Kindelberger DW, Lee Y, Miron A, Hirsch MS, Feltmate C, Medeiros F, et al. Intraepithelial carcinoma of the fimbria and pelvic serous carcinoma: Evidence for a causal relationship. Am J Surg Pathol. 2007;31:161–9. doi: 10.1097/01.pas.0000213335.40358.47. [DOI] [PubMed] [Google Scholar]
- 19.Kuhn E, Kurman RJ, Vang R, Sehdev AS, Han GM, Soslow R, et al. TP53 mutations in serous tubal intraepithelial carcinoma and concurrent pelvic high-grade serous carcinoma-evidence supporting the clonal relationship of the two lesions. J Pathol. 2012;226:421–6. doi: 10.1002/path.3023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li J, Abushahin N, Pang SJ, Xiang L, Chambers SK, Fadare O, et al. Tubal origin of 'ovarian' low-grade serous carcinoma. Mod Pathol. 2011;24:1488–99. doi: 10.1038/modpathol.2011.106. [DOI] [PubMed] [Google Scholar]
- 21.Shih IM, Kurman RJ. Ovarian tumorigenesis: a proposed model based on morphological and molecular genetic analysis. Ame J Pathol. 2004;164:1511–8. doi: 10.1016/s0002-9440(10)63708-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marchbanks PA, Wilson H, Bastos E, Cramer DW, Schildkraut JM, Peterson HB. Cigarette smoking and epithelial ovarian cancer by histologic type. Obstet Gynecol. 2000;95:255–60. doi: 10.1016/s0029-7844(99)00531-1. [DOI] [PubMed] [Google Scholar]
- 23.Risch HA, Marrett LD, Jain M, Howe GR. Differences in risk factors for epithelial ovarian cancer by histologic type: Results of a case-control study. Am J Epidemiol. 1996;144:363–72. doi: 10.1093/oxfordjournals.aje.a008937. [DOI] [PubMed] [Google Scholar]
- 24.Chiaffarino F, Parazzini F, Bosetti C, Franceschi S, Talamini R, Canzonieri V, et al. Risk factors for ovarian cancer histotypes. Eur J Cancer. 2007;43:1208–13. doi: 10.1016/j.ejca.2007.01.035. [DOI] [PubMed] [Google Scholar]
- 25.Eltabbakh GH, Natarajan N, Piver MS, Mettlin CJ. Epidemiologic differences between women with borderline ovarian tumors and women with epithelial ovarian cancer. Gynecol Oncol. 1999;74:103–7. doi: 10.1006/gyno.1999.5459. [DOI] [PubMed] [Google Scholar]
- 26.Kurian AW, Balise RR, McGuire V, Whittemore AS. Histologic types of epithelial ovarian cancer: have they different risk factors? Gynecol Oncol. 2005;96:520–30. doi: 10.1016/j.ygyno.2004.10.037. [DOI] [PubMed] [Google Scholar]
- 27.Parazzini F, Chiaffarino F, Negri E, Surace M, Benzi G, Franceschi S, et al. Risk factors for different histological types of ovarian cancer. Int J Gynecol Cancer. 2004;14:431–6. doi: 10.1111/j.1048-891x.2004.14302.x. [DOI] [PubMed] [Google Scholar]
- 28.Tung KH, Goodman MT, Wu AH, McDuffie K, Wilkens LR, Kolonel LN, et al. Reproductive factors and epithelial ovarian cancer risk by histologic type: a multiethnic case-control study. Am J Epidemiol. 2003;158:629–38. doi: 10.1093/aje/kwg177. [DOI] [PubMed] [Google Scholar]
- 29.Gates MA, Rosner BA, Hecht JL, Tworoger SS. Risk factors for epithelial ovarian cancer by histologic subtype. Am J Epidemiol. 2010;171:45–53. doi: 10.1093/aje/kwp314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wentzensen N, Poole EM, Trabert B, White E, Arslan AA, Patel AV, et al. Ovarian cancer risk factors by histologic subtype: an analysis from the ovarian cancer cohort consortium. J Clin Oncol. 2016;34:2888–98. doi: 10.1200/JCO.2016.66.8178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ogino S, Nishihara R, Vander Weele TJ, Wang M, Nishi A, Lochhead P, et al. The role of molecular pathological epidemiology in the study of neoplastic and non-neoplastic diseases in the era of precision medicine. Epidemiology. 2016;27:602–11. doi: 10.1097/EDE.0000000000000471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ferlay JSH, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008 v 1.2: Cancer Incidence, Mortality, and Prevalence Worldwide: IARC CancerBase No. 10. Lyon, France: International Agency for Research on Cancer, 2008[2011-12-18]. http://globocan.iarc.fr. (未找到本条文献信息, 请核对)
- 33.Herrinton LJ, Stanford JL, Schwartz SM, Weiss NS. Ovarian cancer incidence among Asian migrants to the United States and their descendants. J Natl Cancer Inst. 1994;86:1336–9. doi: 10.1093/jnci/86.17.1336. [DOI] [PubMed] [Google Scholar]
- 34.Kliewer EV, Smith KR. Ovarian cancer mortality among immigrants in Australia and Canada. Cancer Epidemiol Biomarkers Prev. 1995;4:453–8. [PubMed] [Google Scholar]
- 35.Wei KR, Li YM, Zheng RS, Zhang SW, Liang ZH, Cen HS, et al. Ovary cancer incidence and mortality in China, 2011. Chin J Cancer Res. 2015;27:38–43. doi: 10.3978/j.issn.1000-9604.2015.01.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bray F, Loos AH, Tognazzo S, La Vecchia C. Ovarian cancer in Europe: Cross-sectional trends in incidence and mortality in 28 countries, 1953-2000. Int J Cancer. 2005;113:977–90. doi: 10.1002/ijc.20649. [DOI] [PubMed] [Google Scholar]
- 37.Coleman MP, Estève J, Damiecki P, Arslan A, Renard H. Trends in cancer incidence and mortality. IARC Sci Publ. 1993:1–806. doi: 10.3109/9780415874984-2. [DOI] [PubMed] [Google Scholar]
- 38.Howe HL, Wu XC, Ries LA, Cokkinides V, Ahmed F, Jemal A, et al. Annual report to the nation on the status of cancer, 1975-2003, featuring cancer among U. S. Hispanic/Latino populations. Cancer. 2006;107:1711–42. doi: 10.1002/cncr.22193. [DOI] [PubMed] [Google Scholar]
- 39.Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Waldron W, et al. SEER Cancer Statistics Review, 1975–2008, National Cancer Institute. Bethesa, MD, http://seer.cancer.gov/csr/1975_2008/, based on November 2010 SEER data submission, posted to the SEER web site, 2011. (请核对本条文献格式)(本条文献与第4、65条文献重复, 请核对)
- 40.Malvezzi M, Carioli G, Rodriguez T, Negri E, La Vecchia C. Global trends and predictions in ovarian cancer mortality. Ann Oncol. 2016;27:2017–25. doi: 10.1093/annonc/mdw306. [DOI] [PubMed] [Google Scholar]
- 41.Teng ZM, Han RQ, Huang XY, Zhou JY, Yang J, Luo PF, et al. Increase of incidence and mortality of ovarian cancer during 2003-2012 in Jiangsu Province, China. Front Public Health. 2016;4:146. doi: 10.3389/fpubh.2016.00146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nguyen HN, Averette HE, Janicek M. Ovarian carcinoma: A review of the significance of familial risk factors and the role of prophylactic oophorectomy in cancer prevention. Cancer. 1994;74:545–55. doi: 10.1002/1097-0142(19940715)74:2<545::aid-cncr2820740204>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 43.Parazzini F, Negri E, La Vecchia C, Restelli C, Franceschi S. Family history of reproductive cancers and ovarian cancer risk: an Italian case-control study. Am J Epidemiol. 1992;135:35–40. doi: 10.1093/oxfordjournals.aje.a116199. [DOI] [PubMed] [Google Scholar]
- 44.Stratton JF, Pharoah P, Smith SK, Easton D, Ponder BAJ. A systematic review and meta-analysis of family history and risk of ovarian cancer. Br J Obstet Gynaecol. 1998;105:493–9. doi: 10.1111/j.1471-0528.1998.tb10148.x. [DOI] [PubMed] [Google Scholar]
- 45.Sutcliffe S, Pharoah PDP, Easton DF, Ponder BAJ. Ovarian and breast cancer risks to women in families with two or more cases of ovarian cancer. Int J Cancer. 2000;87:110–7. doi: 10.1002/1097-0215(20000701)87:1<110::aid-ijc16>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 46.Ziogas A, Gildea M, Cohen P, Bringman D, Taylor TH, Seminara D, et al. Cancer risk estimates for family members of a population-based family registry for breast and ovarian cancer. Cancer Epidemiol Biomarkers Prev. 2000;9:103–11. [PubMed] [Google Scholar]
- 47.Negri E, Pelucchi C, Franceschi S, Montella M, Conti E, Dal Maso L, et al. Family history of cancer and risk of ovarian cancer. Eur J Cancer. 2003;39:505–10. doi: 10.1016/s0959-8049(02)00743-8. [DOI] [PubMed] [Google Scholar]
- 48.Lynch HT, Casey MJ, Snyder CL, Bewtra C, Lynch JF, Butts M, et al. Hereditary ovarian carcinoma: heterogeneity, molecular genetics, pathology, and management. Mol Oncol. 2009;3:97–137. doi: 10.1016/j.molonc.2009.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Malander S, Ridderheim M, Måsbäck A, Loman N, Kristoffersson U, Olsson H, et al. One in 10 ovarian cancer patients carry germ line BRCA1 or BRCA2 mutations: results of a prospective study in Southern Sweden. Eur J Cancer. 2004;40:422–8. doi: 10.1016/j.ejca.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 50.Menkiszak J, Gronwald J, Górski B, Jakubowska A, Huzarski T, Byrski T, et al. Hereditary ovarian cancer in Poland. Int J Cancer. 2003;106:942–5. doi: 10.1002/ijc.11338. [DOI] [PubMed] [Google Scholar]
- 51.Pal T, Permuth-Wey J, Betts JA, Krischer JP, Fiorica J, Arango H, et al. BRCA1 and BRCA2 mutations account for a large proportion of ovarian carcinoma cases. Cancer. 2005;104:2807–16. doi: 10.1002/cncr.21536. [DOI] [PubMed] [Google Scholar]
- 52.Risch HA, McLaughlin JR, Cole DEC, Rosen B, Bradley L, Kwan E, et al. Prevalence and penetrance of germline BRCA1 and BRCA2 mutations in a population series of 649 women with ovarian cancer. Am J Hum Genet. 2001;68:700–10. doi: 10.1086/318787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stratton JF, Gayther SA, Russell P, Dearden J, Gore M, Blake P, et al. Contribution of BRCA1 mutations to ovarian cancer. N Engl J Med. 1997;336:1125–30. doi: 10.1056/NEJM199704173361602. [DOI] [PubMed] [Google Scholar]
- 54.Takahashi H, Behbakht K, McGovern PE, Chiu HC, Couch FJ, Weber BL, et al. Mutation analysis of the BRCA1 gene in ovarian cancers. Cancer Res. 1995;55:2998–3002. [PubMed] [Google Scholar]
- 55.Anton-Culver H, Cohen PF, Gildea ME, Ziogas A. Characteristics of BRCA1 mutations in a population-based case series of breast and ovarian cancer. Eur J Cancer. 2000;36:1200–8. doi: 10.1016/s0959-8049(00)00110-6. [DOI] [PubMed] [Google Scholar]
- 56.Bjørge T, Lie AK, Hovig E, Gislefoss RE, Hansen S, Jellum E, et al. BRCA1 mutations in ovarian cancer and borderline tumours in Norway: a nested case-control study. Br J Cancer. 2004;91:1829–34. doi: 10.1038/sj.bjc.6602199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Van Der Looij M, Szabo C, Besznyak I, Liszka G, Csokay B, Pulay T, et al. Prevalence of founder BRCA1 and BRCA2 mutations among breast and ovarian cancer patients in Hungary. Int J Cancer. 2000;86:737–40. doi: 10.1002/(sici)1097-0215(20000601)86:5<737::aid-ijc21>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 58.Ford D, Easton DF, Bishop DT, Narod SA, Goldgar DE. Risks of cancer in BRCA1-mutation carriers. Lancet. 1994;343:692–5. doi: 10.1016/s0140-6736(94)91578-4. [DOI] [PubMed] [Google Scholar]
- 59.Antoniou A, Pharoah PDP, Narod S, Risch HA, Eyfjord JE, Hopper JL, et al. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet. 2003;72:1117–30. doi: 10.1086/375033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lynch HT, Smyrk T. Hereditary nonpolyposis colorectal cancer (Lynch syndrome): An updated review. Cancer. 1996;78:1149–67. doi: 10.1002/(SICI)1097-0142(19960915)78:6<1149::AID-CNCR1>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 61.Aarnio M, Mecklin JP, Aaltonen LA, Nyström-Lahti M, Järvinen HJ. Life-time risk of different cancers in hereditary non-polyposis colorectal cancer (HNPCC) syndrome. Int J Cancer. 1995;64:430–3. doi: 10.1002/ijc.2910640613. [DOI] [PubMed] [Google Scholar]
- 62.Aarnio M, Sankila R, Pukkala E, Salovaara R, Aaltonen LA, de la Chapelle A, et al. Cancer risk in mutation carriers of DNA-mismatch-repair genes. Int J Cancer. 1999;81:214–8. doi: 10.1002/(sici)1097-0215(19990412)81:2<214::aid-ijc8>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 63.Prat J, Ribé A, Gallardo A. Hereditary ovarian cancer. Hum Pathol. 2005;36:861–70. doi: 10.1016/j.humpath.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 64.Bonadona V, Bonaïti B, Olschwang S, Grandjouan S, Huiart L, Longy M, et al. Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome. JAMA. 2011;305:2304–10. doi: 10.1001/jama.2011.743. [DOI] [PubMed] [Google Scholar]
- 65.Song HL, Dicks E, Ramus SJ, Tyrer JP, Intermaggio MP, Hayward J, et al. Contribution of germline mutations in the RAD51B, RAD51C, and RAD51D genes to ovarian cancer in the population. J Clin Oncol. 2015;33:2901–7. doi: 10.1200/JCO.2015.61.2408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ramus SJ, Song HL, Dicks E, Tyrer JP, Rosenthal AN, Intermaggio MP, et al. Germline mutations in the BRIP1, BARD1, PALB2, and NBN genes in women with ovarian cancer. J Natl Cancer Inst. 2015;107:djv214. doi: 10.1093/jnci/djv214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lakhani SR, Manek S, Penault-Llorca F, Flanagan A, Arnout L, Merrett S, et al. Pathology of ovarian cancers in BRCA1 and BRCA2 carriers. Clin Cancer Res. 2004;10:2473–81. doi: 10.1158/1078-0432.ccr-1029-3. [DOI] [PubMed] [Google Scholar]
- 68.Ketabi Z, Bartuma K, Bernstein I, Malander S, Grönberg H, Björck E, et al. Ovarian cancer linked to Lynch syndrome typically presents as early-onset, non-serous epithelial tumors. Gynecol Oncol. 2011;121:462–5. doi: 10.1016/j.ygyno.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 69.Pal T, Akbari MR, Sun P, Fulp J, Thompson Z, Coppola D, et al. Frequency of mutations in mismatch repair genes in a population-based study of women with ovarian cancer. Br J Cancer. 2012;107:1783–90. doi: 10.1038/bjc.2012.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bahcall OG. iCOGS collection provides a collaborative model. Nat Genet. 2013;45:343. doi: 10.1038/ng.2592. [DOI] [PubMed] [Google Scholar]
- 71.Shen H, Fridley BL, Song HL, Lawrenson K, Cunningham JM, Ramus SJ, et al. Epigenetic analysis leads to identification of HNF1B as a subtype-specific susceptibility gene for ovarian cancer. Nat Commun. 2013;4:1628. doi: 10.1038/ncomms2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Permuth-Wey J, Lawrenson K, Shen HC, Velkova A, Tyrer JP, Chen ZH, et al. Identification and molecular characterization of a new ovarian cancer susceptibility locus at 17q21.31. Nat Commun. 2013;4:1627. doi: 10.1038/ncomms2613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kuchenbaecker KB, Ramus SJ, Tyrer J, Lee A, Shen HC, Beesley J, et al. Identification of six new susceptibility loci for invasive epithelial ovarian cancer. Nat Genet. 2015;47:164–71. doi: 10.1038/ng.3185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bolton KL, Tyrer J, Song H, Ramus SJ, Notaridou M, Jones C, et al. Common variants at 19p13 are associated with susceptibility to ovarian cancer. Nat Genet. 2010;42:880–4. doi: 10.1038/ng.666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kelemen LE, Lawrenson K, Tyrer J, Li QY, Lee JM, Seo JH, et al. Genome-wide significant risk associations for mucinous ovarian carcinoma. Nat Genet. 2015;47:888–97. doi: 10.1038/ng.3336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Song HL, Ramus SJ, Tyrer J, Bolton KL, Gentry-Maharaj A, Wozniak E, et al. A genome-wide association study identifies a new ovarian cancer susceptibility locus on 9p22.2. Nat Genet. 2009;41:996–1000. doi: 10.1038/ng.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pharoah PDP, Tsai YY, Ramus SJ, Phelan CM, Goode EL, Lawrenson K, et al. GWAS meta-analysis and replication identifies three new susceptibility loci for ovarian cancer. Nat Genet. 2013;45:362–70. doi: 10.1038/ng.2564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bojesen SE, Pooley KA, Johnatty SE, Beesley J, Michailidou K, Tyrer JP, et al. Multiple independent variants at the TERT locus are associated with telomere length and risks of breast and ovarian cancer. Nat Genet. 2013;45:371–84. doi: 10.1038/ng.2566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Couch FJ, Wang XS, McGuffog L, Lee A, Olswold C, Kuchenbaecker KB, et al. Genome-wide association study in BRCA1 mutation carriers identifies novel loci associated with breast and ovarian cancer risk. PLoS Genet. 2013;9:e1003212. doi: 10.1371/journal.pgen.1003212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Goode EL, Chenevix-Trench G, Song HL, Ramus SJ, Notaridou M, Lawrenson K, et al. A genome-wide association study identifies susceptibility loci for ovarian cancer at 2q31 and 8q24. Nat Genet. 2010;42:874–9. doi: 10.1038/ng.668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kar SP, Beesley J, Amin Al Olama A, Michailidou K, Tyrer J, Kote-Jarai Z, et al. Genome-wide meta-analyses of breast, ovarian, and prostate cancer association studies identify multiple new susceptibility loci shared by at least two cancer types. Cancer Discov. 2016;6:1052–67. doi: 10.1158/2159-8290.CD-15-1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cuellar-Partida G, Lu Y, Dixon SC, Fasching PA, Hein A, Burghaus S, et al. Assessing the genetic architecture of epithelial ovarian cancer histological subtypes. Hum Genet. 2016;135:741–56. doi: 10.1007/s00439-016-1663-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chen KX, Ma HX, Li L, Zang RY, Wang C, Song FJ, et al. Genome-wide association study identifies new susceptibility loci for epithelial ovarian cancer in Han Chinese women. Nat Commun. 2014;5:4682. doi: 10.1038/ncomms5682. [DOI] [PubMed] [Google Scholar]
- 84.Risch HA. Hormonal etiology of epithelial ovarian cancer, with a hypothesis concerning the role of androgens and progesterone. J Natl Cancer Inst. 1998;90:1774–86. doi: 10.1093/jnci/90.23.1774. [DOI] [PubMed] [Google Scholar]
- 85.Casagrande JT, Louie EW, Pike MC, Roy S, Ross RK, Henderson BE. "Incessant ovulation" and ovarian cancer. Lancet. 1979;2:170–3. doi: 10.1016/s0140-6736(79)91435-1. [DOI] [PubMed] [Google Scholar]
- 86.Tung KH, Wilkens LR, Wu AH, McDuffie K, Nomura AM, Kolonel LN, et al. Effect of anovulation factors on pre- and postmenopausal ovarian cancer risk: revisiting the incessant ovulation hypothesis. Am J Epidemiol. 2005;161:321–9. doi: 10.1093/aje/kwi046. [DOI] [PubMed] [Google Scholar]
- 87.Moorman PG, Schildkraut JM, Calingaert B, Halabi S, Vine MF, Berchuck A. Ovulation and ovarian cancer: a comparison of two methods for calculating lifetime ovulatory cycles (United States) Cancer Causes Control. 2002;13:807–11. doi: 10.1023/a:1020678100977. [DOI] [PubMed] [Google Scholar]
- 88.Schildkraut JM, Moorman PG, Bland AE, Halabi S, Calingaert B, Whitaker R, et al. Cyclin E overexpression in epithelial ovarian cancer characterizes an etiologic subgroup. Cancer Epidemiol Biomarkers Prev. 2008;17:585–93. doi: 10.1158/1055-9965.EPI-07-0596. [DOI] [PubMed] [Google Scholar]
- 89.Terry KL, Titus-Ernstoff L, McKolanis JR, Welch WR, Finn OJ, Cramer DW. Incessant ovulation, mucin 1 immunity, and risk for ovarian cancer. Cancer Epidemiol Biomarkers Prev. 2007;16:30–5. doi: 10.1158/1055-9965.EPI-06-0688. [DOI] [PubMed] [Google Scholar]
- 90.Cramer DW, Welch WR. Determinants of ovarian cancer risk. II. Inferences regarding pathogenesis. J Natl Cancer Inst. 1983;71:717–21. [PubMed] [Google Scholar]
- 91.Riman T, Nilsson S, Persson IR. Review of epidemiological evidence for reproductive and hormonal factors in relation to the risk of epithelial ovarian malignancies. Acta Obstet Gynecol Scand. 2004;83:783–95. doi: 10.1111/j.0001-6349.2004.00550.x. [DOI] [PubMed] [Google Scholar]
- 92.Booth M, Beral V, Smith P. Risk factors for ovarian cancer: a case-control study. Br J Cancer. 1989;60:592–8. doi: 10.1038/bjc.1989.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Franceschi S, La Vecchia C, Booth M, Tzonou A, Negri E, Parazzini F, et al. Pooled analysis of 3 European case-control studies of ovarian cancer: II. Age at menarche and at menopause. Int J Cancer. 1991;49:57–60. doi: 10.1002/ijc.2910490111. [DOI] [PubMed] [Google Scholar]
- 94.Parazzini F, Franceschi S, La Vecchia C, Fasoli M. The epidemiology of ovarian cancer. Gynecol Oncol. 1991;43:9–23. doi: 10.1016/0090-8258(91)90003-n. [DOI] [PubMed] [Google Scholar]
- 95.Parazzini F, La Vecchia C, Negri E, Gentile A. Menstrual factors and the risk of epithelial ovarian cancer. J Clin Epidemiol. 1989;42:443–8. doi: 10.1016/0895-4356(89)90134-0. [DOI] [PubMed] [Google Scholar]
- 96.Purdie D, Green A, Bain C, Siskind V, Ward B, Hacker N, et al. Reproductive and other factors and risk of epithelial ovarian cancer: an Australian case-control study. Int J Cancer. 1995;62:678–84. doi: 10.1002/ijc.2910620606. [DOI] [PubMed] [Google Scholar]
- 97.Tavani A, Negri E, Franceschi S, Parazzini F, La Vecchia C. Risk factors for epithelial ovarian cancer in women under age 45. Eur J Cancer. 1993;29:1297–301. doi: 10.1016/0959-8049(93)90077-s. [DOI] [PubMed] [Google Scholar]
- 98.Whittemore AS, Harris R, Itnyre J. Characteristics relating to ovarian cancer risk: collaborative analysis of 12 US case-control studies. II. Invasive epithelial ovarian cancers in white women. Collaborative Ovarian Cancer Group. Am J Epidemiol. 1992;136:1184–203. doi: 10.1093/oxfordjournals.aje.a116427. [DOI] [PubMed] [Google Scholar]
- 99.Wu ML, Whittemore AS, Paffenbarger RS Jr, Sarles DL, Kampert JB, Grosser S, et al. Personal and environmental characteristics related to epithelial ovarian cancer. I. Reproductive and menstrual events and oral contraceptive use. Am J Epidemiol. 1988;128:1216–27. doi: 10.1093/oxfordjournals.aje.a115076. [DOI] [PubMed] [Google Scholar]
- 100.Wynder EL, Dodo H, Barber HRK. Epidemiology of cancer of the ovary. Cancer. 1969;23:352–70. doi: 10.1002/1097-0142(196902)23:2<352::aid-cncr2820230212>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 101.Hankinson SE, Colditz GA, Hunter DJ, Willett WC, Stampfer MJ, Rosner B, et al. A prospective study of reproductive factors and risk of epithelial ovarian cancer. Cancer. 1995;76:284–90. doi: 10.1002/1097-0142(19950715)76:2<284::aid-cncr2820760219>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 102.Risch HA, Marrett LD, Howe GR. Parity, contraception, infertility, and the risk of epithelial ovarian cancer. Am J Epidemiol. 1994;140:585–97. doi: 10.1093/oxfordjournals.aje.a117296. [DOI] [PubMed] [Google Scholar]
- 103.Shu XO, Brinton LA, Gao YT, Yuan JM. Population-based case-control study of ovarian cancer in Shanghai. Cancer Res. 1989;49:3670–4. [PubMed] [Google Scholar]
- 104.Tzonou A, Day NE, Trichopoulos D, Walker A, Saliaraki M, Papapostolou M, et al. The epidemiology of ovarian cancer in Greece: a case-control study. Eur J Cancer Clin Oncol. 1984;20:1045–52. doi: 10.1016/0277-5379(84)90107-x. [DOI] [PubMed] [Google Scholar]
- 105.Kvåle G, Heuch I, Nilssen S, Beral V. Reproductive factors and risk of ovarian cancer: a prospective study. Int J Cancer. 1988;42:246–51. doi: 10.1002/ijc.2910420217. [DOI] [PubMed] [Google Scholar]
- 106.McGowan L, Norris HJ, Hartge P, Hoover R, Lesher L. Risk factors in ovarian cancer. Eur J Gynaecol Oncol. 1988;9:195–9. [PubMed] [Google Scholar]
- 107.Newhouse ML, Pearson RM, Fullerton JM, Boesen EA, Shannon HS. A case control study of carcinoma of the ovary. Br J Prev Soc Med. 1977;31:148–53. doi: 10.1136/jech.31.3.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Polychronopoulou A, Tzonou A, Hsieh CC, Trichopoulos D, Kaprinis G, Rebelakos A, et al. Reproductive variables, tobacco, ethanol, coffee and somatometry as risk factors for ovarian cancer. Int J Cancer. 1993;55:402–7. doi: 10.1002/ijc.2910550312. [DOI] [PubMed] [Google Scholar]
- 109.Tsilidis KK, Allen NE, Key TJ, Dossus L, Lukanova A, Bakken K, et al. Oral contraceptive use and reproductive factors and risk of ovarian cancer in the European Prospective Investigation into Cancer and Nutrition. Br J Cancer. 2011;105:1436–42. doi: 10.1038/bjc.2011.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Moorman PG, Palmieri RT, Akushevich L, Berchuck A, Schildkraut JM. Ovarian cancer risk factors in African-American and white women. Am J Epidemiol. 2009;170:598–606. doi: 10.1093/aje/kwp176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Weiderpass E, Sandin S, Inoue M, Shimazu T, Iwasaki M, Sasazuki S, et al. Risk factors for epithelial ovarian cancer in Japan - results from the Japan Public Health Center-based Prospective Study cohort. Int J Oncol. 2012;40:21–30. doi: 10.3892/ijo.2011.1194. [DOI] [PubMed] [Google Scholar]
- 112.Shin A, Song YM, Yoo KY, Sung J. Menstrual factors and cancer risk among Korean women. Int J Epidemiol. 2011;40:1261–8. doi: 10.1093/ije/dyr121. [DOI] [PubMed] [Google Scholar]
- 113.Gong TT, Wu QJ, Vogtmann E, Lin B, Wang YL. Age at menarche and risk of ovarian cancer: A meta-analysis of epidemiological studies. Int J Cancer. 2013;132:2894–900. doi: 10.1002/ijc.27952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Annegers JF, Strom H, Decker DG, Dockerty MB, O'Fallon WM. Ovarian cancer. Incidence and case-control study. Cancer. 1979;43:723–9. doi: 10.1002/1097-0142(197902)43:2<723::aid-cncr2820430248>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 115.Cramer DW, Hutchison GB, Welch WR, Scully RE, Ryan KJ. Determinants of ovarian cancer risk. I. Reproductive experiences and family history. J Natl Cancer Inst. 1983;71:711–6. [PubMed] [Google Scholar]
- 116.Hartge P, Hoover R, McGowan L, Lesher L, Norris HJ. Menopause and ovarian cancer. Am J Epidemiol. 1988;127:990–8. doi: 10.1093/oxfordjournals.aje.a114902. [DOI] [PubMed] [Google Scholar]
- 117.La Vecchia C. Epidemiology of ovarian cancer: a summary review. Eur J Cancer Prev. 2001;10:125–9. doi: 10.1097/00008469-200104000-00002. [DOI] [PubMed] [Google Scholar]
- 118.Riman T, Dickman PW, Nilsson S, Correia N, Nordlinder H, Magnusson CM, et al. Risk factors for invasive epithelial ovarian cancer: results from a Swedish case-control study. Am J Epidemiol. 2002;156:363–73. doi: 10.1093/aje/kwf048. [DOI] [PubMed] [Google Scholar]
- 119.Schoenaker DAJM, Jackson CA, Rowlands JV, Mishra GD. Socioeconomic position, lifestyle factors and age at natural menopause: a systematic review and meta-analyses of studies across six continents. Int J Epidemiol. 2014;43:1542–62. doi: 10.1093/ije/dyu094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Shi J, Zhang B, Choi JY, Gao YT, Li H, Lu W, et al. Age at menarche and age at natural menopause in East Asian women: a genome-wide association study. Age. 2016;38:513–23. doi: 10.1007/s11357-016-9939-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Spencer KL, Malinowski J, Carty CL, Franceschini N, Fernández-Rhodes L, Young A, et al. Genetic variation and reproductive timing: African American women from the Population Architecture using Genomics and Epidemiology (PAGE) Study. PLoS One. 2013;8:e55258. doi: 10.1371/journal.pone.0055258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.He CY, Kraft P, Chen C, Buring JE, Paré G, Hankinson SE, et al. Genome-wide association studies identify loci associated with age at menarche and age at natural menopause. Nat Genet. 2009;41:724–8. doi: 10.1038/ng.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Joly DJ, Lilienfeld AM, Diamond EL, Bross ID. An epidemiologic study of the relationship of reproductive experience to cancer of the ovary. Am J Epidemiol. 1974;99:190–209. doi: 10.1093/oxfordjournals.aje.a121603. [DOI] [PubMed] [Google Scholar]
- 124.No authors listed. The reduction in risk of ovarian cancer associated with oral-contraceptive use. N Engl J Med. 1987;316:650–5. doi: 10.1056/NEJM198703123161102. [DOI] [PubMed] [Google Scholar]
- 125.Hartge P, Schiffman MH, Hoover R, McGowan L, Lesher L, Norris HJ. A case-control study of epithelial ovarian cancer. Am J Obstet Gynecol. 1989;161:10–6. doi: 10.1016/0002-9378(89)90221-4. [DOI] [PubMed] [Google Scholar]
- 126.Nasca PC, Greenwald P, Chorost S, Richart R, Caputo T. An epidemiologic case-control study of ovarian cancer and reproductive factors. Am J Epidemiol. 1984;119:705–13. doi: 10.1093/oxfordjournals.aje.a113791. [DOI] [PubMed] [Google Scholar]
- 127.Adami HO, Lambe M, Persson I, Ekbom A, Adami HO, Hsieh CC, et al. Parity, age at first childbirth, and risk of ovarian cancer. Lancet. 1994;344:1250–4. doi: 10.1016/s0140-6736(94)90749-8. [DOI] [PubMed] [Google Scholar]
- 128.Moorman PG, Alberg AJ, Bandera EV, Barnholtz-Sloan J, Bondy M, Cote ML, et al. Reproductive factors and ovarian cancer risk in African-American women. Ann Epidemiol. 2016;26:654–62. doi: 10.1016/j.annepidem.2016.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Chen Y, Wu PC, Lang JH, Ge WJ, Hartge P, Brinton LA. Risk factors for epithelial ovarian cancer in Beijing, China. Int J Epidemiol. 1992;21:23–9. doi: 10.1093/ije/21.1.23. [DOI] [PubMed] [Google Scholar]
- 130.Gay GMW, Lim JSP, Chay WY, Chow KY, Tan MH, Lim WY. Reproductive factors, adiposity, breastfeeding and their associations with ovarian cancer in an Asian cohort. Cancer Cause Control. 2015;26:1561–73. doi: 10.1007/s10552-015-0649-6. [DOI] [PubMed] [Google Scholar]
- 131.Yang HP, Trabert B, Murphy MA, Sherman ME, Sampson JN, Brinton LA, et al. Ovarian cancer risk factors by histologic subtypes in the NIH‐AARP diet and health study. Intl J Cancer. 2011;131:938–48. doi: 10.1002/ijc.26469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Fortner RT, Ose J, Merritt MA, Schock H, Tjønneland A, Hansen L, et al. Reproductive and hormone-related risk factors for epithelial ovarian cancer by histologic pathways, invasiveness and histologic subtypes: Results from the EPIC cohort. Int J Cancer. 2015;137:1196–208. doi: 10.1002/ijc.29471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.La Vecchia C, Decarli A, Franceschi S, Regallo M, Tognoni G. Age at first birth and the risk of epithelial ovarian cancer. J Natl Cancer Inst. 1984;73:663–6. [PubMed] [Google Scholar]
- 134.Negri E, Franceschi S, Tzonou A, Booth M, La Vecchia C, Parazzini F, et al. Pooled analysis of 3 European case-control studies: I. Reproductive factors and risk of epithelial ovarian cancer. Int J Cancer. 1991;49:50–6. doi: 10.1002/ijc.2910490110. [DOI] [PubMed] [Google Scholar]
- 135.Franceschi S, La Vecchia C, Helmrich SP, Mangioni C, Tognoni G. Risk factors for epithelial ovarian cancer in Italy. Am J Epidemiol. 1982;115:714–9. doi: 10.1093/oxfordjournals.aje.a113353. [DOI] [PubMed] [Google Scholar]
- 136.Hildreth NG, Kelsey JL, LiVolsi VA, Fischer DB, Holford TR, Mostow ED, et al. An epidemiologic study of epithelial carcinoma of the ovary. Am J Epidemiol. 1981;114:398–405. doi: 10.1093/oxfordjournals.aje.a113207. [DOI] [PubMed] [Google Scholar]
- 137.John EM, Whittemore AS, Harris R, Itnyre J. Characteristics relating to ovarian cancer risk: collaborative analysis of seven U. S. case-control studies. Epithelial ovarian cancer in black women. J Natl Cancer Inst. 1993;85:142–7. doi: 10.1093/jnci/85.2.142. [DOI] [PubMed] [Google Scholar]
- 138.Bevier M, Sundquist J, Hemminki K. Does the time interval between first and last birth influence the risk of endometrial and ovarian cancer? Eur J Cancer. 2011;47:586–91. doi: 10.1016/j.ejca.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 139.Chen MT, Cook LS, Daling JR, Weiss NS. Incomplete pregnancies and risk of ovarian cancer (Washington, United States) Cancer Causes Control. 1996;7:415–20. doi: 10.1007/BF00052667. [DOI] [PubMed] [Google Scholar]
- 140.Mori M, Harabuchi I, Miyake H, Casagrande JT, Henderson BE, Ross RK. Reproductive, genetic, and dietary risk factors for ovarian cancer. Am J Epidemiol. 1988;128:771–7. doi: 10.1093/oxfordjournals.aje.a115030. [DOI] [PubMed] [Google Scholar]
- 141.Negri E, Franceschi S, La Vecchia C, Parazzini F. Incomplete pregnancies and ovarian cancer risk. Gynecol Oncol. 1992;47:234–8. doi: 10.1016/0090-8258(92)90112-v. [DOI] [PubMed] [Google Scholar]
- 142.Dick ML, Siskind V, Purdie DM, Green AC. Incomplete pregnancy and risk of ovarian cancer: results from two Australian case-control studies and systematic review. Cancer Causes Control. 2009;20:1571–85. doi: 10.1007/s10552-009-9402-3. [DOI] [PubMed] [Google Scholar]
- 143.Riman T, Persson I, Nilsson S. Hormonal aspects of epithelial ovarian cancer: review of epidemiological evidence. Clin Endocrinol. 1998;49:695–707. doi: 10.1046/j.1365-2265.1998.00577.x. [DOI] [PubMed] [Google Scholar]
- 144.Mosgaard BJ, Lidegaard Ø, Kjaer SK, Schou G, Andersen AN. Infertility, fertility drugs, and invasive ovarian cancer: a case-control study. Fertil Steril. 1997;67:1005–12. doi: 10.1016/s0015-0282(97)81431-8. [DOI] [PubMed] [Google Scholar]
- 145.Modan B, Ron E, Lerner-Geva L, Blumstein T, Menczer J, Rabinovici J, et al. Cancer incidence in a cohort of infertile woman. Am J Epidemiol. 1998;147:1038–42. doi: 10.1093/oxfordjournals.aje.a009397. [DOI] [PubMed] [Google Scholar]
- 146.Franceschi S, La Vecchia C, Negri E, Guarneri S, Montella M, Conti E, et al. Fertility drugs and risk of epithelial ovarian cancer in Italy. Hum Reprod. 1994;9:1673–5. doi: 10.1093/oxfordjournals.humrep.a138771. [DOI] [PubMed] [Google Scholar]
- 147.Rossing MA, Daling JR, Weiss NS, Moore DE, Self SG. Ovarian tumors in a cohort of infertile women. N Engl J Med. 1994;331:771–6. doi: 10.1056/NEJM199409223311204. [DOI] [PubMed] [Google Scholar]
- 148.Ness RB, Cramer DW, Goodman MT, Kjaer SK, Mallin K, Mosgaard BJ, et al. Infertility, fertility drugs, and ovarian cancer: a pooled analysis of case-control studies. Am J Epidemiol. 2002;155:217–24. doi: 10.1093/aje/155.3.217. [DOI] [PubMed] [Google Scholar]
- 149.Potashnik G, Lerner-Geva L, Genkin L, Chetrit A, Lunenfeld E, Porath A. Fertility drugs and the risk of breast and ovarian cancers: results of a long-term follow-up study. Fertil Steril. 1999;71:853–9. doi: 10.1016/s0015-0282(99)00085-0. [DOI] [PubMed] [Google Scholar]
- 150.Venn A, Watson L, Lumley J, Giles G, King C, Healy D. Breast and ovarian cancer incidence after infertility and in vitro fertilisation. Lancet. 1995;346:995–1000. doi: 10.1016/s0140-6736(95)91687-3. [DOI] [PubMed] [Google Scholar]
- 151.Ayhan A, Salman MC, Celik H, Dursun P, Ozyuncu O, Gultekin M. Association between fertility drugs and gynecologic cancers, breast cancer, and childhood cancers. Acta Obstet Gynecol Scand. 2004;83:1104–11. doi: 10.1111/j.0001-6349.2004.00669.x. [DOI] [PubMed] [Google Scholar]
- 152.Brinton LA, Sakoda LC, Sherman ME, Frederiksen K, Kjaer SK, Graubard BI, et al. Relationship of benign gynecologic diseases to subsequent risk of ovarian and uterine tumors. Cancer Epidemiol Biomarkers Prev. 2005;14:2929–35. doi: 10.1158/1055-9965.EPI-05-0394. [DOI] [PubMed] [Google Scholar]
- 153.Edmondson RJ, Monaghan JM. The epidemiology of ovarian cancer. Int J Gynecol Cancer. 2001;11:423–9. doi: 10.1046/j.1525-1438.2001.01053.x. [DOI] [PubMed] [Google Scholar]
- 154.Vigano P, Somigliana E, Parazzini F, Vercellini P. Bias versus causality: interpreting recent evidence of association between endometriosis and ovarian cancer. Fertil Steril. 2007;88:588–93. doi: 10.1016/j.fertnstert.2006.11.180. [DOI] [PubMed] [Google Scholar]
- 155.Schildkraut JM, Schwingl PJ, Bastos E, Evanoff A, Hughes C. Epithelial ovarian cancer risk among women with polycystic ovary syndrome. Obstet Gynecol. 1996;88:554–9. doi: 10.1016/0029-7844(96)00226-8. [DOI] [PubMed] [Google Scholar]
- 156.Oktay K, Kim JY, Barad D, Babayev SN. Association of BRCA1 mutations with occult primary ovarian insufficiency: a possible explanation for the link between infertility and breast/ovarian cancer risks. J Clin Oncol. 2010;28:240–4. doi: 10.1200/JCO.2009.24.2057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Ovarian cancer. In: Schottenfeld D, Fraumeni JF, eds. Cancer Epidemiology and Prevention. New York: Oxford University Press; 1996. [Google Scholar]
- 158.Gwinn ML, Lee NC, Rhodes PH, Layde PM, Rubin GL. Pregnancy, breast feeding, and oral contraceptives and the risk of epithelial ovarian cancer. J Clin Epidemiol. 1990;43:559–68. doi: 10.1016/0895-4356(90)90160-q. [DOI] [PubMed] [Google Scholar]
- 159.Rosenblatt KA, Thomas DB, The WHO Collaborative Study of Neoplasia and Steroid Contraceptives. Lactation and the risk of epithelial ovarian cancer. Int J Epidemiol. 1993;22:192–7. doi: 10.1093/ije/22.2.192. [DOI] [PubMed] [Google Scholar]
- 160.Schneider AP II. Risk factor for ovarian cancer. N Engl J Med. 1987;317:508–9. doi: 10.1056/NEJM198708203170813. [DOI] [PubMed] [Google Scholar]
- 161.Jordan SJ, Siskind V, Green AC, Whiteman DC, Webb PM. Breastfeeding and risk of epithelial ovarian cancer. Cancer Causes Control. 2010;21:109–16. doi: 10.1007/s10552-009-9440-x. [DOI] [PubMed] [Google Scholar]
- 162.Jordan SJ, Cushing-Haugen KL, Wicklund KG, Doherty JA, Rossing MA. Breast-feeding and risk of epithelial ovarian cancer. Cancer Causes Control. 2012;23:919–27. doi: 10.1007/s10552-012-9963-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Li DP, Du C, Zhang ZM, Li GX, Yu ZF, Wang X, et al. Breastfeeding and ovarian cancer risk: a systematic review and meta-analysis of 40 epidemiological studies. Asian Pac J Cancer Prev. 2014;15:4829–37. doi: 10.7314/apjcp.2014.15.12.4829. [DOI] [PubMed] [Google Scholar]
- 164.Fauser BCJM, Tarlatzis BC, Rebar RW, Legro RS, Balen AH, Lobo R, et al. Consensus on women's health aspects of polycystic ovary syndrome (PCOS): the Amsterdam ESHRE/ASRM-Sponsored 3rd PCOS Consensus Workshop Group. Fertil Steril. 2012;97:28–38. doi: 10.1016/j.fertnstert.2011.09.024. [DOI] [PubMed] [Google Scholar]
- 165.Sayasneh A, Tsivos D, Crawford R. Endometriosis and ovarian cancer: a systematic review. ISRN Obstet Gynecol. 2011;2011:140310. doi: 10.5402/2011/140310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Merritt MA, De Pari M, Vitonis AF, Titus LJ, Cramer DW, Terry KL. Reproductive characteristics in relation to ovarian cancer risk by histologic pathways. Hum Reprod. 2013;28:1406–17. doi: 10.1093/humrep/des466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Pearce CL, Templeman C, Rossing MA, Lee A, Near AM, Webb PM, et al. Association between endometriosis and risk of histological subtypes of ovarian cancer: a pooled analysis of case-control studies. Lancet Oncol. 2012;13:385–94. doi: 10.1016/S1470-2045(11)70404-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Lu Y, Cuellar-Partida G, Painter JN, Nyholt DR, Morris AP, Fasching PA, et al. Shared genetics underlying epidemiological association between endometriosis and ovarian cancer. Hum Mol Genet. 2015;24:5955–64. doi: 10.1093/hmg/ddv306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Kori M, Gov E, Arga KY. Molecular signatures of ovarian diseases: Insights from network medicine perspective. Syst Biol Reprod Med. 2016;62:266–82. doi: 10.1080/19396368.2016.1197982. [DOI] [PubMed] [Google Scholar]
- 170.Risch HA, Howe GR. Pelvic inflammatory disease and the risk of epithelial ovarian cancer. Cancer Epidemiol Biomarkers Prev. 1995;4:447–51. [PubMed] [Google Scholar]
- 171.Parazzini F, La Vecchia C, Negri E, Moroni S, dal Pino D, Fedele L. Pelvic inflammatory disease and risk of ovarian cancer. Cancer Epidemiol Biomarkers Prev. 1996;5:667–9. [PubMed] [Google Scholar]
- 172.Merritt MA, Green AC, Nagle CM, Webb PM. Talcum powder, chronic pelvic inflammation and NSAIDs in relation to risk of epithelial ovarian cancer. Int J Cancer. 2008;122:170–6. doi: 10.1002/ijc.23017. [DOI] [PubMed] [Google Scholar]
- 173.Lin HW, Tu YY, Lin SY, Su WJ, Lin WL, Lin WZ, et al. Risk of ovarian cancer in women with pelvic inflammatory disease: a population-based study. Lancet Oncol. 2011;12:900–4. doi: 10.1016/S1470-2045(11)70165-6. [DOI] [PubMed] [Google Scholar]
- 174.Rasmussen CB, Faber MT, Jensen A, Høgdall E, Høgdall C, Blaakær J, et al. Pelvic inflammatory disease and risk of invasive ovarian cancer and ovarian borderline tumors. Cancer Causes Control. 2013;24:1459–64. doi: 10.1007/s10552-013-0216-y. [DOI] [PubMed] [Google Scholar]
- 175.Rasmussen CB, Jensen A, Albieri V, Andersen KK, Kjaer SK. Increased risk of borderline ovarian tumors in women with a history of pelvic inflammatory disease: A nationwide population-based cohort study. Gynecol Oncol. 2016;143:346–51. doi: 10.1016/j.ygyno.2016.08.318. [DOI] [PubMed] [Google Scholar]
- 176.Domchek SM, Rebbeck TR. Prophylactic oophorectomy in women at increased cancer risk. Curr Opin Obstet Gynecol. 2007;19:27–30. doi: 10.1097/GCO.0b013e32801195da. [DOI] [PubMed] [Google Scholar]
- 177.Green A, Purdie D, Bain C, Siskind V, Russell P, Quinn M, et al. Tubal sterilisation, hysterectomy and decreased risk of ovarian cancer. Int J Cancer. 1997;71:948–51. doi: 10.1002/(sici)1097-0215(19970611)71:6<948::aid-ijc6>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 178.Hankinson SE, Hunter DJ, Colditz GA, Willett WC, Stampfer MJ, Rosner B, et al. Tubal ligation, hysterectomy, and risk of ovarian cancer. A prospective study. JAMA. 1993;270:2813–8. [PubMed] [Google Scholar]
- 179.Kreiger N, Sloan M, Cotterchio M, Parsons P. Surgical procedures associated with risk of ovarian cancer. Int J Epidemiol. 1997;26:710–15. doi: 10.1093/ije/26.4.710. [DOI] [PubMed] [Google Scholar]
- 180.Miracle-McMahill HL, Calle EE, Kosinski AS, Rodriguez C, Wingo PA, Thun MJ, et al. Tubal ligation and fatal ovarian cancer in a large prospective cohort study. Am J Epidemiol. 1997;145:349–57. doi: 10.1093/oxfordjournals.aje.a009112. [DOI] [PubMed] [Google Scholar]
- 181.Rosenblatt KA, Thomas DB. Reduced risk of ovarian cancer in women with a tubal ligation or hysterectomy. The World Health Organization Collaborative Study of Neoplasia and Steroid Contraceptives. Cancer Epidemiol Biomarkers Prev. 1996;5:933–5. [PubMed] [Google Scholar]
- 182.Ness RB, Dodge RC, Edwards RP, Baker JA, Moysich KB. Contraception methods, beyond oral contraceptives and tubal ligation, and risk of ovarian cancer. Ann Epidemiol. 2011;21:188–96. doi: 10.1016/j.annepidem.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Cibula D, Widschwendter M, Májek O, Dusek L. Tubal ligation and the risk of ovarian cancer: review and meta-analysis. Hum Reprod Update. 2011;17:55–67. doi: 10.1093/humupd/dmq030. [DOI] [PubMed] [Google Scholar]
- 184.Rice MS, Murphy MA, Vitonis AF, Cramer DW, Titus LJ, Tworoger SS, et al. Tubal ligation, hysterectomy and epithelial ovarian cancer in the New England Case-Control Study. Int J Cancer. 2013;133:2415–21. doi: 10.1002/ijc.28249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Rice MS, Hankinson SE, Tworoger SS. Tubal ligation, hysterectomy, unilateral oophorectomy, and risk of ovarian cancer in the Nurses' Health Studies. Fertil Steril. 2014;102:192–198.e193. doi: 10.1016/j.fertnstert.2014.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Madsen C, Baandrup L, Dehlendorff C, Kjær SK. Tubal ligation and salpingectomy and the risk of epithelial ovarian cancer and borderline ovarian tumors: a nationwide case-control study. Acta Obstet Gynecol Scand. 2015;94:86–94. doi: 10.1111/aogs.12516. [DOI] [PubMed] [Google Scholar]
- 187.Gaitskell K, Green J, Pirie K, Reeves G, Beral V. Tubal ligation and ovarian cancer risk in a large cohort: Substantial variation by histological type. Int J Cancer. 2016;138:1076–84. doi: 10.1002/ijc.29856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Weiss NS, Harlow BL. Why does hysterectomy without bilateral oophorectomy influence the subsequent incidence of ovarian cancer? Am J Epidemiol. 1986;124:856–8. doi: 10.1093/oxfordjournals.aje.a114463. [DOI] [PubMed] [Google Scholar]
- 189.Chiaffarino F, Parazzini F, Decarli A, Franceschi S, Talamini R, Montella M, et al. Hysterectomy with or without unilateral oophorectomy and risk of ovarian cancer. Gynecol Oncol. 2005;97:318–22. doi: 10.1016/j.ygyno.2005.01.030. [DOI] [PubMed] [Google Scholar]
- 190.Bulun SE. Endometriosis. N Engl J Med. 2009;360:268–79. doi: 10.1056/NEJMra0804690. [DOI] [PubMed] [Google Scholar]
- 191.Franceschi S, Parazzini F, Negri E, Booth M, La Vecchia C, Beral V, et al. Pooled analysis of 3 European case-control studies of epithelial ovarian cancer: III. Oral contraceptive use. Int J Cancer. 1991;49:61–5. doi: 10.1002/ijc.2910490112. [DOI] [PubMed] [Google Scholar]
- 192.La Vecchia C, Franceschi S. Oral contraceptives and ovarian cancer. Eur J Cancer Prev. 1999;8:297–304. doi: 10.1097/00008469-199908000-00005. [DOI] [PubMed] [Google Scholar]
- 193.Rosenberg L, Palmer JR, Zauber AG, Warshauer ME, Lewis JL Jr, Strom BL, et al. A case-control study of oral contraceptive use and invasive epithelial ovarian cancer. Am J Epidemiol. 1994;139:654–61. doi: 10.1093/oxfordjournals.aje.a117055. [DOI] [PubMed] [Google Scholar]
- 194.Vessey M, Painter R. Oral contraceptive use and cancer. Findings in a large cohort study, 1968-2004. Br J Cancer. 2006;95:385–9. doi: 10.1038/sj.bjc.6603260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.La Vecchia C. Oral contraceptives and ovarian cancer: an update, 1998-2004. Eur J Cancer Prev. 2006;15:117–24. doi: 10.1097/01.cej.0000179274.24200.9d. [DOI] [PubMed] [Google Scholar]
- 196.No authors listed. Epithelial ovarian cancer and combined oral contraceptives. The WHO Collaborative Study of Neoplasia and Steroid Contraceptives. Int J Epidemiol. 1989;18:538–45. [PubMed] [Google Scholar]
- 197.Beral V, Hannaford P, Kay C. Oral contraceptive use and malignancies of the genital tract. Results from the Royal College of General Practitioners' Oral Contraception Study. Lancet. 1988;2:1331–5. doi: 10.1016/s0140-6736(88)90869-0. [DOI] [PubMed] [Google Scholar]
- 198.La Vecchia C, Altieri A, Franceschi S, Tavani A. Oral contraceptives and cancer: an update. Drug Saf. 2001;24:741–54. doi: 10.2165/00002018-200124100-00003. [DOI] [PubMed] [Google Scholar]
- 199.Rosenblatt KA, Thomas DB, Noonan EA, The WHO Collaborative Study of Neoplasia and Steroid Contraceptives. High-dose and low-dose combined oral contraceptives: protection against epithelial ovarian cancer and the length of the protective effect. Eur J Cancer. 1992;28:1872–6. doi: 10.1016/0959-8049(92)90026-x. [DOI] [PubMed] [Google Scholar]
- 200.Collaborative Group on Epidemiological Studies of Ovarian Cancer. Ovarian cancer and oral contraceptives: collaborative reanalysis of data from 45 epidemiological studies including 23257 women with ovarian cancer and 87303 controls. Lancet. 2008;371:303–14. doi: 10.1016/S0140-6736(08)60167-1. [DOI] [PubMed] [Google Scholar]
- 201.Ness RB, Grisso JA, Klapper J, Schlesselman JJ, Silberzweig S, Vergona R, et al. Risk of ovarian cancer in relation to estrogen and progestin dose and use characteristics of oral contraceptives. Am J Epidemiol. 2000;152:233–41. doi: 10.1093/aje/152.3.233. [DOI] [PubMed] [Google Scholar]
- 202.Liang AP, Levenson AG, Layde PM, Shelton JD, Hatcher RA, Potts M, et al. Risk of breast, uterine corpus, and ovarian cancer in women receiving medroxyprogesterone injections. JAMA. 1983;249:2909–12. [PubMed] [Google Scholar]
- 203.Huang ZZ, Gao YT, Wen WQ, Li HL, Zheng W, Shu XO, et al. Contraceptive methods and ovarian cancer risk among Chinese women: A report from the Shanghai Women's Health Study. Int J Cancer. 2015;137:607–14. doi: 10.1002/ijc.29412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Soini T, Hurskainen R, Grénman S, Mäenpä J, Paavonen J, Pukkala E. Cancer risk in women using the levonorgestrel-releasing intrauterine system in finland. Obstet Gynecol. 2014;124:292–9. doi: 10.1097/AOG.0000000000000356. [DOI] [PubMed] [Google Scholar]
- 205.Tworoger SS, Fairfield KM, Colditz GA, Rosner BA, Hankinson SE. Association of oral contraceptive use, other contraceptive methods, and infertility with ovarian cancer risk. Am J Epidemiol. 2007;166:894–901. doi: 10.1093/aje/kwm157. [DOI] [PubMed] [Google Scholar]
- 206.Wang CT. Trends in contraceptive use and determinants of choice in China: 1980-2010. Contraception. 2012;85:570–9. doi: 10.1016/j.contraception.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 207.Mathur RS, Landgrebe SC, Moody LO, Semmens JP, Williamson HO. The effect of estrogen treatment on plasma concentrations of steroid hormones, gonadotropins, prolactin and sex hormone-binding globulin in post-menopausal women. Maturitas. 1985;7:129–33. doi: 10.1016/0378-5122(85)90018-0. [DOI] [PubMed] [Google Scholar]
- 208.Fraser IS, Jansen RPS, Lobo RA. Estrogens and Progestogens in Clinical Practice. London: Churchill Livingstone. 1998 [Google Scholar]
- 209.Riman T, Dickman PW, Nilsson S, Correia N, Nordlinder H, Magnusson CM, et al. Hormone replacement therapy and the risk of invasive epithelial ovarian cancer in Swedish women. J Natl Cancer Inst. 2002;94:497–504. doi: 10.1093/jnci/94.7.497. [DOI] [PubMed] [Google Scholar]
- 210.Weiss NS, Lyon JL, Krishnamurthy S, Dietert SE, Liff JM, Daling JR. Noncontraceptive estrogen use and the occurrence of ovarian cancer. J Natl Cancer Inst. 1982;68:95–8. [PubMed] [Google Scholar]
- 211.Braem MG, Onland-Moret NC, van den Brandt PA, Goldbohm RA, Peeters PHM, Kruitwagen RFPM, et al. Reproductive and hormonal factors in association with ovarian cancer in the Netherlands cohort study. Am J Epidemiol. 2010;172:1181–9. doi: 10.1093/aje/kwq264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Coughlin SS, Giustozzi A, Smith SJ, Lee NC. A meta-analysis of estrogen replacement therapy and risk of epithelial ovarian cancer. J Clin Epidemiol. 2000;53:367–75. doi: 10.1016/s0895-4356(99)00179-1. [DOI] [PubMed] [Google Scholar]
- 213.Garg PP, Kerlikowske K, Subak L, Grady D. Hormone replacement therapy and the risk of epithelial ovarian carcinoma: a meta-analysis. Obstet Gynecol. 1998;92:472–9. doi: 10.1016/s0029-7844(98)00139-2. [DOI] [PubMed] [Google Scholar]
- 214.Kaufman DW, Kelly JP, Welch WR, Rosenberg L, Stolley PD, Warshauer ME, et al. Noncontraceptive estrogen use and epithelial ovarian cancer. Am J Epidemiol. 1989;130:1142–51. doi: 10.1093/oxfordjournals.aje.a115441. [DOI] [PubMed] [Google Scholar]
- 215.Beral V. Ovarian cancer and hormone replacement therapy in the Million Women Study. Lancet. 2007;369:1703–10. doi: 10.1016/S0140-6736(07)60534-0. [DOI] [PubMed] [Google Scholar]
- 216.Pearce CL, Chung K, Pike MC, Wu AH. Increased ovarian cancer risk associated with menopausal estrogen therapy is reduced by adding a progestin. Cancer. 2009;115:531–9. doi: 10.1002/cncr.23956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Greiser CM, Greiser EM, Dören M. Menopausal hormone therapy and risk of ovarian cancer: systematic review and meta-analysis. Hum Reprod Update. 2007;13:453–63. doi: 10.1093/humupd/dmm012. [DOI] [PubMed] [Google Scholar]
- 218.Zhou B, Sun QM, Cong RH, Gu HJ, Tang NP, Yang L, et al. Hormone replacement therapy and ovarian cancer risk: a meta-analysis. GynecolOncol. 2008;108:641–51. doi: 10.1016/j.ygyno.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 219.Danforth KN, Tworoger SS, Hecht JL, Rosner BA, Colditz GA, Hankinson SE. A prospective study of postmenopausal hormone use and ovarian cancer risk. Br J Cancer. 2007;96:151–6. doi: 10.1038/sj.bjc.6603527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Folsom AR, Anderson JP, Ross JA. Estrogen replacement therapy and ovarian cancer. Epidemiology. 2004;15:100–4. doi: 10.1097/01.ede.0000091606.31903.8e. [DOI] [PubMed] [Google Scholar]
- 221.Lacey JV Jr, Brinton LA, Leitzmann MF, Mouw T, Hollenbeck A, Schatzkin A, et al. Menopausal hormone therapy and ovarian cancer risk in the National Institutes of Health-AARP Diet and Health Study Cohort. J Natl Cancer Inst. 2006;98:1397–405. doi: 10.1093/jnci/djj375. [DOI] [PubMed] [Google Scholar]
- 222.Lacey JV Jr, Mink PJ, Lubin JH, Sherman ME, Troisi R, Hartge P, et al. Menopausal hormone replacement therapy and risk of ovarian cancer. JAMA. 2002;288:334–41. doi: 10.1001/jama.288.3.334. [DOI] [PubMed] [Google Scholar]
- 223.Rodriguez C, Patel AV, Calle EE, Jacob EJ, Thun MJ. Estrogen replacement therapy and ovarian cancer mortality in a large prospective study of US women. JAMA. 2001;285:1460–5. doi: 10.1001/jama.285.11.1460. [DOI] [PubMed] [Google Scholar]
- 224.Collaborative Group on Epidemiological Studies of Ovarian Cancer. Menopausal hormone use and ovarian cancer risk: individual participant meta-analysis of 52 epidemiological studies. Lancet. 2015;385:1835–42. doi: 10.1016/S0140-6736(14)61687-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Hildebrand JS, Gapstur SM, Feigelson HS, Teras LR, Thun MJ, Patel AV. Postmenopausal hormone use and incident ovarian cancer: associations differ by regimen. Int J Cancer. 2010;127:2928–35. doi: 10.1002/ijc.25515. [DOI] [PubMed] [Google Scholar]
- 226.Rossing MA, Cushing-Haugen KL, Wicklund KG, Doherty JA, Weiss NS. Menopausal hormone therapy and risk of epithelial ovarian cancer. Cancer Epidemiol Biomarkers Prev. 2007;16:2548–56. doi: 10.1158/1055-9965.EPI-07-0550. [DOI] [PubMed] [Google Scholar]
- 227.Tsilidis KK, Allen NE, Key TJ, Dossus L, Kaaks R, Bakken K, et al. Menopausal hormone therapy and risk of ovarian cancer in the European prospective investigation into cancer and nutrition. Cancer Causes Control. 2011;22:1075–84. doi: 10.1007/s10552-011-9782-z. [DOI] [PubMed] [Google Scholar]
- 228.Mørch LS, Løkkegaard E, Andreasen AH, Krüger-Kjaer S, Lidegaard O. Hormone therapy and ovarian cancer. JAMA. 2009;302:298–305. doi: 10.1001/jama.2009.1052. [DOI] [PubMed] [Google Scholar]
- 229.Risch HA. Estrogen replacement therapy and risk of epithelial ovarian cancer. Gynecol Oncol. 1996;63:254–7. doi: 10.1006/gyno.1996.0315. [DOI] [PubMed] [Google Scholar]
- 230.Robbins Basic Pathology. Philadelphia, PA: Saunders/Elsevier; 2007. [Google Scholar]
- 231.Chlebowski RT, Hendrix SL, Langer RD, Stefanick ML, Gass M, Lane D, et al. Influence of estrogen plus progestin on breast, cancer and mammography in healthy postmenopausal women: The Women's Health Initiative Randomized trial. JAMA. 2003;289:3243–53. doi: 10.1001/jama.289.24.3243. [DOI] [PubMed] [Google Scholar]
- 232.Coombs NJ, Cronin KA, Taylor RJ, Freedman AN, Boyages J. The impact of changes in hormone therapy on breast cancer incidence in the US population. Cancer Cause Control. 2010;21:83–90. doi: 10.1007/s10552-009-9437-5. [DOI] [PubMed] [Google Scholar]
- 233.Ness J, Aronow WS. Prevalence and causes of persistent use of hormone replacement therapy among postmenopausal women: a follow-up study. Am J Ther. 2006;13:109–12. doi: 10.1097/00045391-200603000-00004. [DOI] [PubMed] [Google Scholar]
- 234.Rodriguez C, Calle EE, Fakhrabadi-Shokoohi D, Jacobs EJ, Thun MJ. Body mass index, height, and the risk of ovarian cancer mortality in a prospective cohort of postmenopausal women. Cancer Epidemiol Biomarkers Prev. 2002;11:822–8. [PubMed] [Google Scholar]
- 235.Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer. 2004;4:579–91. doi: 10.1038/nrc1408. [DOI] [PubMed] [Google Scholar]
- 236.Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371:569–78. doi: 10.1016/S0140-6736(08)60269-X. [DOI] [PubMed] [Google Scholar]
- 237.Olsen CM, Green AC, Whiteman DC, Sadeghi S, Kolahdooz F, Webb PM. Obesity and the risk of epithelial ovarian cancer: a systematic review and meta-analysis. Eur J Cancer. 2007;43:690–709. doi: 10.1016/j.ejca.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 238.Schouten LJ, Rivera C, Hunter DJ, Spiegelman D, Adami HO, Arslan A, et al. Height, body mass index, and ovarian cancer: a pooled analysis of 12 cohort studies. Cancer Epidemiol Biomarkers Prev. 2008;17:902–12. doi: 10.1158/1055-9965.EPI-07-2524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Olsen CM, Nagle CM, Whiteman DC, Ness R, Pearce CL, Pike MC, et al. Obesity and risk of ovarian cancer subtypes: evidence from the Ovarian Cancer Association Consortium. Endocr Relat Cancer. 2013;20:251–62. doi: 10.1530/ERC-12-0395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Lahmann PH, Cust AE, Friedenreich CM, Schulz M, Lukanova A, Kaaks R, et al. Anthropometric measures and epithelial ovarian cancer risk in the European Prospective Investigation into Cancer and Nutrition. Int J Cancer. 2010;126:2404–15. doi: 10.1002/ijc.24952. [DOI] [PubMed] [Google Scholar]
- 241.Kotsopoulos J, Baer HJ, Tworoger SS. Anthropometric measures and risk of epithelial ovarian cancer: results from the nurses' health study. Obesity. 2009;18:1625–31. doi: 10.1038/oby.2009.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Leitzmann MF, Koebnick C, Danforth KN, Brinton LA, Moore SC, Hollenbeck AR, et al. Body mass index and risk of ovarian cancer. Cancer. 2009;115:812–22. doi: 10.1002/cncr.24086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Canchola AJ, Chang ET, Bernstein L, Largent JA, Reynolds P, Deapen D, et al. Body size and the risk of ovarian cancer by hormone therapy use in the California Teachers Study cohort. Cancer Causes Control. 2010;21:2241–8. doi: 10.1007/s10552-010-9647-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Collaborative Group on Epidemiological Studies of Ovarian Cancer. Ovarian cancer and body size: individual participant meta-analysis including 25, 157 women with ovarian cancer from 47 epidemiological studies. PLoS Med. 2012;9:e1001200. doi: 10.1371/journal.pmed.1001200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Dixon SC, Nagle CM, Thrift AP, Pharoah PDP, Pearce CL, Zheng W, et al. Adult body mass index and risk of ovarian cancer by subtype: a Mendelian randomization study. Int J Epidemiol. 2016;45:884–95. doi: 10.1093/ije/dyw158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Schulz M, Lahmann PH, Riboli E, Boeing H. Dietary determinants of epithelial ovarian cancer: a review of the epidemiologic literature. Nutr Cancer. 2004;50:120–40. doi: 10.1207/s15327914nc5002_2. [DOI] [PubMed] [Google Scholar]
- 247.Kolahdooz F, van der Pols JC, Bain CJ, Marks GC, Hughes MC, Whiteman DC, et al. Meat, fish, and ovarian cancer risk: results from 2 Australian case-control studies, a systematic review, and meta-analysis. Am J Clin Nutr. 2010;91:1752–63. doi: 10.3945/ajcn.2009.28415. [DOI] [PubMed] [Google Scholar]
- 248.Wallin A, Orsini N, Wolk A. Red and processed meat consumption and risk of ovarian cancer: a dose-response meta-analysis of prospective studies. Br J Cancer. 2011;104:1196–201. doi: 10.1038/bjc.2011.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Gilsing AMJ, Weijenberg MP, Goldbohm RA, van den Brandt PA, Schouten LJ. Consumption of dietary fat and meat and risk of ovarian cancer in the Netherlands Cohort Study. Am J Clin Nutr. 2011;93:118–26. doi: 10.3945/ajcn.2010.29888. [DOI] [PubMed] [Google Scholar]
- 250.Oppeneer SJ, Robien K. Tea consumption and epithelial ovarian cancer risk: a systematic review of observational studies. Nutr Cancer. 2011;63:817–26. doi: 10.1080/01635581.2011.594210. [DOI] [PubMed] [Google Scholar]
- 251.Larsson SC, Wolk A. Coffee consumption is not associated with ovarian cancer incidence. Cancer Epidemiol Biomarkers Prev. 2005;14:2273–4. doi: 10.1158/1055-9965.EPI-05-0280. [DOI] [PubMed] [Google Scholar]
- 252.Riman T, Dickman PW, Nilsson S, Nordlinder H, Magnusson CM, Persson IR. Some life-style factors and the risk of invasive epithelial ovarian cancer in Swedish women. Eur J Epidemiol. 2004;19:1011–9. doi: 10.1007/s10654-004-1633-8. [DOI] [PubMed] [Google Scholar]
- 253.Whittemore AS, Wu ML, Paffenbarger RS Jr, Sarles DL, Kampert JB, Grosser S, et al. Personal and environmental characteristics related to epithelial ovarian cancer. II. Exposures to talcum powder, tobacco, alcohol, and coffee. Am J Epidemiol. 1988;128:1228–40. doi: 10.1093/oxfordjournals.aje.a115077. [DOI] [PubMed] [Google Scholar]
- 254.Arab L. Epidemiologic evidence on coffee and cancer. Nutr Cancer. 2010;62:271–83. doi: 10.1080/01635580903407122. [DOI] [PubMed] [Google Scholar]
- 255.Baker JA, Boakye K, McCann SE, Beehler GP, Rodabaugh KJ, Villella JA, et al. Consumption of black tea or coffee and risk of ovarian cancer. Int J Gynecol Cancer. 2007;17:50–4. doi: 10.1111/j.1525-1438.2006.00773.x. [DOI] [PubMed] [Google Scholar]
- 256.Nagle CM, Olsen CM, Bain CJ, Whiteman DC, Green AC, Webb PM. Tea consumption and risk of ovarian cancer. Cancer Causes Control. 2010;21:1485–91. doi: 10.1007/s10552-010-9577-7. [DOI] [PubMed] [Google Scholar]
- 257.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 258.Deeb KK, Trump DL, Johnson CS. Vitamin D signalling pathways in cancer: potential for anticancer therapeutics: Nat Rev. Cancer. 2007;7:684–700. doi: 10.1038/nrc2196. [DOI] [PubMed] [Google Scholar]
- 259.Zheng W, Danforth KN, Tworoger SS, Goodman MT, Arslan AA, Patel AV, et al. Circulating 25-hydroxyvitamin D and risk of epithelial ovarian cancer: Cohort consortium vitamin D pooling project of rarer cancers. Am J Epidemiol. 2010;172:70–80. doi: 10.1093/aje/kwq118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Cook LS, Neilson HK, Lorenzetti DL, Lee RC. A systematic literature review of vitamin D and ovarian cancer. AmJ Obstet Gynecol. 2010;203:70.e71–8. doi: 10.1016/j.ajog.2010.01.062. [DOI] [PubMed] [Google Scholar]
- 261.Yin L, Grandi N, Raum E, Haug U, Arndt V, Brenner H. Meta-analysis: Circulating vitamin D and ovarian cancer risk. Gynecolc Oncol. 2011;121:369–75. doi: 10.1016/j.ygyno.2011.01.023. [DOI] [PubMed] [Google Scholar]
- 262.Prescott J, Bertrand KA, Poole EM, Rosner BA, Tworoger SS. Surrogates of long-term vitamin d exposure and ovarian cancer risk in two prospective cohort studies. Cancers. 2013;5:1577–600. doi: 10.3390/cancers5041577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Ong JS, Cuellar-Partida G, Lu Y, Australian Ovarian Cancer Study, Fasching PA, Hein A, et al. Association of vitamin D levels and risk of ovarian cancer: a Mendelian randomization study. Int J Epidemiol. 2016;45:1619–30. doi: 10.1093/ije/dyw207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Tworoger SS, Lee IM, Buring JE, Rosner B, Hollis BW, Hankinson SE. Plasma 25-hydroxyvitamin D and 1, 25-dihydroxyvitamin D and risk of incident ovarian cancer. Cancer Epidemiol Biomarkers Prev. 2007;16:783–8. doi: 10.1158/1055-9965.EPI-06-0981. [DOI] [PubMed] [Google Scholar]
- 265.Uitterlinden AG, Fang Y, van Meurs JBJ, Pols HA, van Leeuwen JPTM. Genetics and biology of vitamin D receptor polymorphisms. Gene. 2004;338:143–56. doi: 10.1016/j.gene.2004.05.014. [DOI] [PubMed] [Google Scholar]
- 266.Xu YQ, He BS, Pan YQ, Deng QW, Sun HL, Li R, et al. Systematic review and meta-analysis on vitamin D receptor polymorphisms and cancer risk. Tumour Biol. 2014;35:4153–69. doi: 10.1007/s13277-013-1544-y. [DOI] [PubMed] [Google Scholar]
- 267.Li S, Xu H, Li SC, Qi XQ, Sun WJ. Vitamin D receptor rs2228570 polymorphism and susceptibly to ovarian cancer: a meta-analysis. Tumour Biol. 2014;35:1319–22. doi: 10.1007/s13277-013-1175-3. [DOI] [PubMed] [Google Scholar]
- 268.Xu H, Li S, Qiu JQ, Gao XL, Zhang P, Yang YX. The VDR gene FokI polymorphism and ovarian cancer risk. Tumour Biol. 2013;34:3309–16. doi: 10.1007/s13277-013-0826-8. [DOI] [PubMed] [Google Scholar]
- 269.Song GG, Lee YH. Vitamin D receptor FokI, BsmI, ApaI, and TaqI polymorphisms and susceptibility to ovarian cancer: a meta-analysis. Immunol Investig. 2013;42:661–72. doi: 10.3109/08820139.2013.822881. [DOI] [PubMed] [Google Scholar]
- 270.Prescott J, Bertrand KA, Reid BM, Permuth-Wey J, De Vivo I, Cramer DW, et al. Evidence of differential effects of vitamin d receptor variants on epithelial ovarian cancer risk by predicted vitamin d status. Front Oncol. 2014;4:286. doi: 10.3389/fonc.2014.00286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.McTiernan A. Mechanisms linking physical activity with cancer. Nat Rev Cancer. 2008;8:205–11. doi: 10.1038/nrc2325. [DOI] [PubMed] [Google Scholar]
- 272.Chionh F, Baglietto L, Krishnan K, English DR, MacInnis RJ, Gertig DM, et al. Physical activity, body size and composition, and risk of ovarian cancer. Cancer Causes Control. 2010;21:2183–94. doi: 10.1007/s10552-010-9638-y. [DOI] [PubMed] [Google Scholar]
- 273.Bertone ER, Willett WC, Rosner BA, Hunter DJ, Fuchs CS, Speizer FE, et al. Prospective study of recreational physical activity and ovarian cancer. J Natl Cancer Inst. 2001;93:942–8. doi: 10.1093/jnci/93.12.942. [DOI] [PubMed] [Google Scholar]
- 274.Anderson JP, Ross JA, Folsom AR. Anthropometric variables, physical activity, and incidence of ovarian cancer: The Iowa Women's Health Study. Cancer. 2004;100:1515–21. doi: 10.1002/cncr.20146. [DOI] [PubMed] [Google Scholar]
- 275.Hannan LM, Leitzmann MF, Lacey JV Jr, Colbert LH, Albanes D, Schatzkin A, et al. Physical activity and risk of ovarian cancer: a prospective cohort study in the United States. Cancer Epidemiol Biomarkers Prev. 2004;13:765–70. [PubMed] [Google Scholar]
- 276.Schnohr P, Grønbæk M, Petersen L, Ole Hein H, Ia Sørensen T. Physical activity in leisure-time and risk of cancer: 14-year follow-up of 28, 000 Danish men and women. Scand J Public Health. 2005;33:244–9. doi: 10.1080/14034940510005752. [DOI] [PubMed] [Google Scholar]
- 277.Biesma RG, Schouten LJ, Dirx MJM, Goldbohm RA, van den Brandt PA. Physical activity and risk of ovarian cancer: results from the Netherlands Cohort Study (The Netherlands) Cancer Causes Control. 2006;17:109–15. doi: 10.1007/s10552-005-0422-3. [DOI] [PubMed] [Google Scholar]
- 278.Patel AV, Rodriguez C, Pavluck AL, Thun MJ, Calle EE. Recreational physical activity and sedentary behavior in relation to ovarian cancer risk in a large cohort of US women. Am J Epidemiol. 2006;163:709–16. doi: 10.1093/aje/kwj098. [DOI] [PubMed] [Google Scholar]
- 279.Weiderpass E, Margolis KL, Sandin S, Braaten T, Kumle M, Adami HO, et al. Prospective study of physical activity in different periods of life and the risk of ovarian cancer. Int J Cancer. 2006;118:3153–60. doi: 10.1002/ijc.21800. [DOI] [PubMed] [Google Scholar]
- 280.Lahmann PH, Friedenreich C, Schulz M, Cust AE, Lukanova A, Kaaks R, et al. Physical activity and ovarian cancer risk: the European Prospective Investigation into Cancer and Nutrition. Cancer Epidemiol Biomarkers Prev. 2009;18:351–4. doi: 10.1158/1055-9965.EPI-08-0958. [DOI] [PubMed] [Google Scholar]
- 281.Leitzmann MF, Koebnick C, Moore SC, Danforth KN, Brinton LA, Hollenbeck AR, et al. Prospective study of physical activity and the risk of ovarian cancer. Cancer Causes Control. 2009;20:765–73. doi: 10.1007/s10552-008-9291-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Huang TY, Eliassen AH, Hankinson SE, Okereke OI, Kubzansky LD, Wang ML, et al. A prospective study of leisure-time physical activity and risk of incident epithelial ovarian cancer: Impact by menopausal status. Int J Cancer. 2016;138:843–52. doi: 10.1002/ijc.29834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Patel AV, Hildebrand JS, Campbell PT, Teras LR, Craft LL, McCullough ML, et al. Leisure-time spent sitting and site-specific cancer incidence in a large U. S. cohort. Cancer Epidemiol Biomarkers Prev. 2015;24:1350–9. doi: 10.1158/1055-9965.EPI-15-0237. [DOI] [PubMed] [Google Scholar]
- 284.Xiao Q, Yang HP, Wentzensen N, Hollenbeck A, Matthews CE. Physical activity in different periods of life, sedentary behavior, and the risk of ovarian cancer in the NIH-AARP diet and health study. Cancer Epidemiol Biomarkers Prev. 2013;22:2000–8. doi: 10.1158/1055-9965.EPI-13-0154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Hildebrand JS, Gapstur SM, Gaudet MM, Campbell PT, Patel AV. Moderate-to-vigorous physical activity and leisure-time sitting in relation to ovarian cancer risk in a large prospective US cohort. Cancer Causes Control. 2015;26:1691–7. doi: 10.1007/s10552-015-0656-7. [DOI] [PubMed] [Google Scholar]
- 286.Pukkala E, Poskiparta M, Apter D, Vihko V. Life-long physical activity and cancer risk among Finnish female teachers. Eur J Cancer Prev. 1993;2:369–76. doi: 10.1097/00008469-199309000-00002. [DOI] [PubMed] [Google Scholar]
- 287.Zheng W, Shu XO, Gao YT, McLaughlin JK, Chow WH, Blot WJ. Occupational physical activity and the incidence of cancer of the breast, corpus uteri, and ovary in Shanghai. Cancer. 1993;71:3620–4. doi: 10.1002/1097-0142(19930601)71:11<3620::aid-cncr2820711125>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 288.Moorman PG, Jones LW, Akushevich L, Schildkraut JM. Recreational physical activity and ovarian cancer risk and survival. Ann Epidemiol. 2011;21:178–87. doi: 10.1016/j.annepidem.2010.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Cottreau CM, Ness RB, Kriska AM. Physical activity and reduced risk of ovarian cancer. Obstet Gynecol. 2000;96:609–14. doi: 10.1016/s0029-7844(00)00972-8. [DOI] [PubMed] [Google Scholar]
- 290.Bertone ER, Newcomb PA, Willett WC, Stampfer MJ, Egan KM. Recreational physical activity and ovarian cancer in a population‐based case‐control study. Int J Cancer. 2002;99:431–6. doi: 10.1002/ijc.10365. [DOI] [PubMed] [Google Scholar]
- 291.Pan SY, Ugnat AM, Mao Y, The Canadian Cancer Registries Epidemiology Research Group. Physical activity and the risk of ovarian cancer: A case‐control study in Canada. Int J Cancer. 2005;117:300–7. doi: 10.1002/ijc.21157. [DOI] [PubMed] [Google Scholar]
- 292.Olsen CM, Bain CJ, Jordan SJ, Nagle CM, Green AC, Whiteman DC, et al. Recreational physical activity and epithelial ovarian cancer: a case-control study, systematic review, and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2007;16:2321–30. doi: 10.1158/1055-9965.EPI-07-0566. [DOI] [PubMed] [Google Scholar]
- 293.Carnide N, Kreiger N, Cotterchio M. Association between frequency and intensity of recreational physical activity and epithelial ovarian cancer risk by age period. Eur J Cancer Prev. 2009;18:322–30. doi: 10.1097/CEJ.0b013e32832bf3fa. [DOI] [PubMed] [Google Scholar]
- 294.Rossing MA, Cushing-Haugen KL, Wicklund KG, Doherty JA, Weiss NS. Recreational physical activity and risk of epithelial ovarian cancer. Cancer Causes Control. 2010;21:485–91. doi: 10.1007/s10552-009-9479-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Cannioto R, LaMonte MJ, Risch HA, Hong CC, Sucheston-Campbell LE, Eng KH, et al. Chronic recreational physical inactivity and epithelial ovarian cancer risk: evidence from the ovarian cancer association consortium. Cancer Epidemiol Biomarkers Prev. 2016;25:1114–24. doi: 10.1158/1055-9965.EPI-15-1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Abbott SE, Bandera EV, Qin B, Peres LC, Moorman PG, Barnholtz-Sloan J, et al. Recreational physical activity and ovarian cancer risk in African American women. Cancer Med. 2016;5:1319–27. doi: 10.1002/cam4.677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Tavani A, Gallus S, La Vecchia C, Dal Maso L, Negri E, Pelucchi C, et al. Physical activity and risk of ovarian cancer: an Italian case-control study. Int J Cancer. 2001;91:407–11. doi: 10.1002/1097-0215(200002)9999:9999<::aid-ijc1065>3.3.co;2-d. [DOI] [PubMed] [Google Scholar]
- 298.Dosemeci M, Hayes RB, Vetter R, Hoover RN, Tucker M, Engin K, et al. Occupational physical activity, socioeconomic status, and risks of 15 cancer sites in Turkey. Cancer Causes Control. 1993;4:313–21. doi: 10.1007/BF00051333. [DOI] [PubMed] [Google Scholar]
- 299.Zhang M, Lee AH, Binns CW. Physical activity and epithelial ovarian cancer risk: A case‐control study in China. Int J Cancer. 2003;105:838–43. doi: 10.1002/ijc.11165. [DOI] [PubMed] [Google Scholar]
- 300.Zhang M, Xie X, Lee AH, Binns CW. Sedentary behaviours and epithelial ovarian cancer risk. Cancer Causes Control. 2004;15:83–9. doi: 10.1023/B:CACO.0000016633.47025.2a. [DOI] [PubMed] [Google Scholar]
- 301.Franks AL, Lee NC, Kendrick JS, Rubin GL, Layde PM. Cigarette smoking and the risk of epithelial ovarian cancer. Am J Epidemiol. 1987;126:112–7. doi: 10.1093/oxfordjournals.aje.a114642. [DOI] [PubMed] [Google Scholar]
- 302.Smith EM, Sowers MF, Burns TL. Effects of smoking on the development of female reproductive cancers. J Natl Cancer Inst. 1984;73:371–6. doi: 10.1093/jnci/73.2.371. [DOI] [PubMed] [Google Scholar]
- 303.Modugno F, Ness RB, Cottreau CM. Cigarette smoking and the risk of mucinous and nonmucinous epithelial ovarian cancer. Epidemiology. 2002;13:467–71. doi: 10.1097/00001648-200207000-00016. [DOI] [PubMed] [Google Scholar]
- 304.Collaborative Group on Epidemiological Studies of Ovarian Cancer. Ovarian cancer and smoking: individual participant meta-analysis including 28114 women with ovarian cancer from 51 epidemiological studies. Lancet Oncol. 2012;13:946–56. doi: 10.1016/S1470-2045(12)70322-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Jordan SJ, Whiteman DC, Purdie DM, Green AC, Webb PM. Does smoking increase risk of ovarian cancer? A systematic review. Gynecol Oncol. 2006;103:1122–9. doi: 10.1016/j.ygyno.2006.08.012. [DOI] [PubMed] [Google Scholar]
- 306.Newcomb PA, Storer BE, Marcus PM. Cigarette smoking in relation to risk of large bowel cancer in women. Cancer Res. 1995;55:4906–9. [PubMed] [Google Scholar]
- 307.Rinaldi S, Peeters PHM, Bezemer ID, Dossus L, Biessy C, Sacerdote C, et al. Relationship of alcohol intake and sex steroid concentrations in blood in pre- and post-menopausal women: the European Prospective Investigation into Cancer and Nutrition. Cancer Cause Control. 2006;17:1033–43. doi: 10.1007/s10552-006-0041-7. [DOI] [PubMed] [Google Scholar]
- 308.Seitz HK, Pelucchi C, Bagnardi V, La Vecchia C. Epidemiology and pathophysiology of alcohol and breast cancer: update 2012. Alcohol Alcoholism. 2012;47:204–12. doi: 10.1093/alcalc/ags011. [DOI] [PubMed] [Google Scholar]
- 309.Gwinn ML, Webster LA, Lee NC, Layde PM, Rubin GL. Alcohol consumption and ovarian cancer risk. Am J Epidemiol. 1986;123:759–66. doi: 10.1093/oxfordjournals.aje.a114304. [DOI] [PubMed] [Google Scholar]
- 310.Adami HO, McLaughlin JK, Hsing AW, Wolk A, Ekbom A, Holmberg L, et al. Alcoholism and cancer risk: a population-based cohort study. Cancer Causes Control. 1992;3:419–25. doi: 10.1007/BF00051354. [DOI] [PubMed] [Google Scholar]
- 311.Rota M, Pasquali E, Scotti L, Pelucchi C, Tramacere I, Islami F, et al. Alcohol drinking and epithelial ovarian cancer risk. a systematic review and meta-analysis. Gynecol Oncol. 2012;125:758–63. doi: 10.1016/j.ygyno.2012.03.031. [DOI] [PubMed] [Google Scholar]
- 312.Yan-Hong H, Jing L, Hong L, Shan-Shan H, Yan L, Ju L. Association between alcohol consumption and the risk of ovarian cancer: a meta-analysis of prospective observational studies. BMC Public Health. 2015;15:223. doi: 10.1186/s12889-015-1355-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Larsson SC, Wolk A. Wine consumption and epithelial ovarian cancer. Cancer Epidemiol Biomarkers Prev. 2004;13:1823; author reply 1823–4. [PubMed] [Google Scholar]
- 314.Modugno F, Ness RB, Allen GO. Alcohol consumption and the risk of mucinous and nonmucinous epithelial ovarian cancer. Obstet Gynecol. 2003;102:1336–43. doi: 10.1016/j.obstetgynecol.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 315.Goodman MT, Tung KH. Alcohol consumption and the risk of borderline and invasive ovarian cancer. Obstet Gynecol. 2003;101:1221–8. doi: 10.1016/s0029-7844(03)00050-4. [DOI] [PubMed] [Google Scholar]
- 316.Kelemen LE, Sellers TA, Vierkant RA, Harnack L, Cerhan JR. Association of folate and alcohol with risk of ovarian cancer in a prospective study of postmenopausal women. Cancer Causes Control. 2004;15:1085–93. doi: 10.1007/s10552-004-1546-6. [DOI] [PubMed] [Google Scholar]
- 317.Webb PM, Purdie DM, Bain CJ, Green AC. Alcohol, wine, and risk of epithelial ovarian cancer. Cancer Epidemiol Biomarkers Prev. 2004;13:592–9. [PubMed] [Google Scholar]
- 318.Cook LS, Leung ACY, Swenerton K, Gallagher RP, Magliocco A, Steed H, et al. Adult lifetime alcohol consumption and invasive epithelial ovarian cancer risk in a population-based case-control study. Gynecol Oncol. 2016;140:277–84. doi: 10.1016/j.ygyno.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 319.Chhim AS, Fassier P, Latino-Martel P, Druesne-Pecollo N, Zelek L, Duverger L, et al. Prospective association between alcohol intake and hormone-dependent cancer risk: modulation by dietary fiber intake. Am J Clin Nutr. 2015;102:182–9. doi: 10.3945/ajcn.114.098418. [DOI] [PubMed] [Google Scholar]
- 320.Peterson NB, Trentham-Dietz A, Newcomb PA, Chen Z, Hampton JM, Willett WC, et al. Alcohol consumption and ovarian cancer risk in a population-based case-control study. Int J Cancer. 2006;119:2423–7. doi: 10.1002/ijc.22137. [DOI] [PubMed] [Google Scholar]
- 321.Schouten LJ, Zeegers MPA, Goldbohm RA, van den Brandt PA. Alcohol and ovarian cancer risk: results from the Netherlands Cohort Study. Cancer Causes Control. 2004;15:201–9. doi: 10.1023/B:CACO.0000019512.71560.2b. [DOI] [PubMed] [Google Scholar]
- 322.Genkinger JM, Hunter DJ, Spiegelman D, Anderson KE, Buring JE, Freudenheim JL, et al. Alcohol intake and ovarian cancer risk: a pooled analysis of 10 cohort studies. Br J Cancer. 2006;94:757–62. doi: 10.1038/sj.bjc.6603020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Kim HS, Kim JW, Shouten LJ, Larsson SC, Chung Hyun H, Kim YB, et al. Wine drinking and epithelial ovarian cancer risk: a meta-analysis. J Gynecol Oncol. 2010;21:112–8. doi: 10.3802/jgo.2010.21.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Heller DS, Gordon RE, Westhoff C, Gerber S. Asbestos exposure and ovarian fiber burden. Am J Ind Med. 1996;29:435–9. doi: 10.1002/(SICI)1097-0274(199605)29:5<435::AID-AJIM1>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 325.Langseth H, Johansen BV, Nesland JM, Kjaerheim K. Asbestos fibers in ovarian tissue from Norwegian pulp and paper workers. Int J Gynecol Cancer. 2007;17:44–9. doi: 10.1111/j.1525-1438.2006.00768.x. [DOI] [PubMed] [Google Scholar]
- 326.Roggli VL, Brody AR. Experimental Models of asbestos-related diseases. In: Rogglie VL, Greenberg SD, Pratt PC, eds. Pathology of Asbestos-Associated Diseases. Boston, MA: Little Brown & Company. 1992 [Google Scholar]
- 327.Reid A, de Klerk N, Musk AW. Does exposure to asbestos cause ovarian cancer? A systematic literature review and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2011;20:1287–95. doi: 10.1158/1055-9965.EPI-10-1302. [DOI] [PubMed] [Google Scholar]
- 328.International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Overall Evaluations of Carcinogenicity: An Updating of IARC Monographs Supplement 7. International Agency for Research on Cancer 1987. Lyon, France: International Agency for Research on Cancer; 1987. (未找到本条文献信息, 请核对)
- 329.Muscat JE, Huncharek MS. Perineal talc use and ovarian cancer: a critical review. Eur J Cancer Prev. 2008;17:139–46. doi: 10.1097/CEJ.0b013e32811080ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Langseth H, Hankinson SE, Siemiatycki J, Weiderpass E. Perineal use of talc and risk of ovarian cancer. J Epidemiol Commun Health. 2008;62:358–60. doi: 10.1136/jech.2006.047894. [DOI] [PubMed] [Google Scholar]
- 331.Huncharek M, Geschwind JF, Kupelnick B. Perineal application of cosmetic talc and risk of invasive epithelial ovarian cancer: a meta-analysis of 11, 933 subjects from sixteen observational studies. Anticancer Res. 2003;23:1955–60. [PubMed] [Google Scholar]
- 332.Cramer DW, Vitonis AF, Terry KL, Welch WR, Titus LJ. The association between talc use and ovarian cancer: a retrospective case-control study in two US States. Epidemiology. 2016;27:334–46. doi: 10.1097/EDE.0000000000000434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Gates MA, Tworoger SS, Terry KL, Titus-Ernstoff L, Rosner B, De Vivo I, et al. Talc use, variants of the GSTM1, GSTT1, and NAT2 genes, and risk of epithelial ovarian cancer. Cancer Epidemiol Biomarkers Prev. 2008;17:2436–44. doi: 10.1158/1055-9965.EPI-08-0399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Baan R, Straif K, Grosse Y, Secretan B, El Ghissassi F, Cogliano V. Carcinogenicity of carbon black, titanium dioxide, and talc. Lancet Oncol. 2006;7:295–6. doi: 10.1016/s1470-2045(06)70651-9. [DOI] [PubMed] [Google Scholar]
- 335.Li L, Mao XG, Qin XM, Zhou M, Xing H, Dong F, et al. Aspirin inhibits growth of ovarian cancer by upregulating caspase-3 and downregulating bcl-2. Oncol Lett. 2016;12:93–6. doi: 10.3892/ol.2016.4607. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 336.Huang Y, Lichtenberger LM, Taylor M, Bottsford-Miller JN, Haemmerle M, Wagner MJ, et al. Anti-tumor and anti-angiogenic effects of aspirin-PC in ovarian cancer. Mol Cancer Ther. 2016;15:2894–904. doi: 10.1158/1535-7163.MCT-16-0074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Cooke NM, Spillane CD, Sheils O, O'Leary J, Kenny D. Aspirin and P2Y12 inhibition attenuate platelet-induced ovarian cancer cell invasion. BMC Cancer. 2015;15:627. doi: 10.1186/s12885-015-1634-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Pinheiro SP, Tworoger SS, Cramer DW, Rosner BA, Hankinson SE. Use of nonsteroidal antiinflammatory agents and incidence of ovarian cancer in 2 large prospective cohorts. Am J Epidemiol. 2009;169:1378–87. doi: 10.1093/aje/kwp062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Prizment AE, Folsom AR, Anderson KE. Nonsteroidal anti-inflammatory drugs and risk for ovarian and endometrial cancers in the Iowa Women's Health Study. Cancer Epidemiol Biomarkers Prev. 2010;19:435–42. doi: 10.1158/1055-9965.EPI-09-0976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Trabert B, Ness RB, Lo-Ciganic WH, Murphy MA, Goode EL, Poole EM, et al. Aspirin, nonaspirin nonsteroidal anti-inflammatory drug, and acetaminophen use and risk of invasive epithelial ovarian cancer: a pooled analysis in the ovarian cancer association consortium. J Natl Cancer Inst. 2014;106:djt431. doi: 10.1093/jnci/djt431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Baandrup L, Kjaer SK, Olsen JH, Dehlendorff C, Friis S. Low-dose aspirin use and the risk of ovarian cancer in Denmark. Ann Oncol. 2015;26:787–92. doi: 10.1093/annonc/mdu578. [DOI] [PubMed] [Google Scholar]
- 342.Schildkraut JM, Moorman PG, Halabi S, Calingaert B, Marks JR, Berchuck A. Analgesic drug use and risk of ovarian cancer. Epidemiology. 2006;17:104–7. doi: 10.1097/01.ede.0000190538.55645.f8. [DOI] [PubMed] [Google Scholar]
- 343.Ammundsen HB, Faber MT, Jensen A, Høgdall E, Blaakaer J, Høgdall C, et al. Use of analgesic drugs and risk of ovarian cancer: results from a Danish case-control study. Acta Obstet Gynecol Scand. 2012;91:1094–102. doi: 10.1111/j.1600-0412.2012.01472.x. [DOI] [PubMed] [Google Scholar]
- 344.Peres LC, Camacho F, Abbott SE, Alberg AJ, Bandera EV, Barnholtz-Sloan J, et al. Analgesic medication use and risk of epithelial ovarian cancer in African American women. Br J Cancer. 2016;114:819–25. doi: 10.1038/bjc.2016.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Hannibal CG, Rossing MA, Wicklund KG, Cushing-Haugen KL. Analgesic drug use and risk of epithelial ovarian cancer. Am J Epidemiol. 2008;167:1430–7. doi: 10.1093/aje/kwn082. [DOI] [PubMed] [Google Scholar]
- 346.Ni XJ, Ma JJ, Zhao YC, Wang Y, Wang S. Meta-analysis on the association between non-steroidal anti-inflammatory drug use and ovarian cancer. Br J Clin Pharmacol. 2013;75:26–35. doi: 10.1111/j.1365-2125.2012.04290.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Li D. Metformin as an antitumor agent in cancer prevention and treatment. J Diabetes. 2011;3:320–7. doi: 10.1111/j.1753-0407.2011.00119.x. [DOI] [PubMed] [Google Scholar]
- 348.Bodmer M, Becker C, Meier C, Jick SS, Meier CR. Use of metformin and the risk of ovarian cancer: A case-control analysis. Gynecol Oncol. 2011;123:200–4. doi: 10.1016/j.ygyno.2011.06.038. [DOI] [PubMed] [Google Scholar]
- 349.Irie H, Banno K, Yanokura M, Iida M, Adachi M, Nakamura K, et al. Metformin: A candidate for the treatment of gynecological tumors based on drug repositioning. Oncol Lett. 2016;11:1287–93. doi: 10.3892/ol.2016.4075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Li K, Hüsing A, Fortner RT, Tjønneland A, Hansen L, Dossus L, et al. An epidemiologic risk prediction model for ovarian cancer in Europe: the EPIC study. Br J Cancer. 2015;112:1257–65. doi: 10.1038/bjc.2015.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Pfeiffer RM, Park Y, Kreimer AR, Lacey JV, Pee D, Greenlee RT, et al. Risk prediction for breast, endometrial, and ovarian cancer in white women aged 50 y or older: derivation and validation from population-based cohort studies. PLoS Med. 2013;10:e1001492. doi: 10.1371/journal.pmed.1001492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Rosner BA, Colditz GA, Webb PM, Hankinson SE. Mathematical models of ovarian cancer incidence. Epidemiology. 2005;16:508–15. doi: 10.1097/01.ede.0000164557.81694.63. [DOI] [PubMed] [Google Scholar]
- 353.Clyde MA, Palmieri Weber R, Iversen ES, Poole EM, Doherty JA, Goodman MT, et al. Risk prediction for epithelial ovarian cancer in 11 united states-based case-control studies: incorporation of epidemiologic risk factors and 17 confirmed genetic loci. Am J Epidemiol. 2016;184:579–89. doi: 10.1093/aje/kww091. [DOI] [PMC free article] [PubMed] [Google Scholar]