Abstract
Background
CBFA2T3-GLIS2 is a fusion gene found in 17% of non-Down syndrome acute megakaryoblastic leukemia (non-DS AMKL, FAB M7) and in 8% of pediatric cytogenetically normal acute myeloid leukemia (CN-AML, in association with several French-American-British (FAB) subtypes). Children with AML harboring this aberration have a poor outcome, regardless of the FAB subtype. This fusion gene drives a peculiar expression pattern and leads to overexpression of some of Hedgehog-related genes. GLI-similar protein 2 (GLIS2) is closely related to the GLI family, the final effectors of classic Hedgehog pathway. These observations lend compelling support to the application of GLI inhibitors in the treatment of AML with the aberration CBFA2T3-GLIS2. GANT61 is, nowadays, the most potent inhibitor of GLI family proteins.
Methods
We exposed to GANT61 AML cell lines and primary cells positive and negative for CBFA2T3-GLIS2 and analyzed the effect on cellular viability, induction of apoptosis, cell cycle, and expression profile.
Results
As compared to AML cells without GLIS2 fusion, GANT61 exposure resulted in higher sensitivity of both cell lines and primary AML cells carrying CBFA2T3-GLIS2 to undergo apoptosis and G1 cell cycle arrest. Remarkably, gene expression studies demonstrated downregulation of GLIS2-specific signature genes in both treated cell lines and primary cells, in comparison with untreated cells. Moreover, chromatin immunoprecipitation analysis revealed direct regulation by GLIS2 chimeric protein of DNMT1 and DNMT3B, two genes implicated in important epigenetic functions.
Conclusions
Our findings indicate that the GLI inhibitor GANT61 may be used to specifically target the CBFA2T3-GLIS2 fusion gene in pediatric AML.
Electronic supplementary material
The online version of this article (doi:10.1186/s13045-017-0396-0) contains supplementary material, which is available to authorized users.
Keywords: Acute myeloid leukemia, Acute megakaryoblastic leukemia, CBFA2T3-GLIS2, GANT61, Hedgehog pathway
Findings
Pediatric acute myeloid leukemia (AML) carrying CBFA2T3-GLIS2 fusion gene deserves particular interest, being associated with a grim prognosis in all the reports published so far [1–3]. The incidence of this aberration is 17 and 8% in pediatric non-Down syndrome acute megakaryoblastic and in pediatric cytogenetically normal AML, respectively [1–3]. The expression profile of CBFA2T3-GLIS2 is associated with upregulation of both Hedgehog (HH) and bone morphogenic protein (BMP) signaling [1, 4].
The protein GLIS2 shares a highly homologous zinc finger domain with members of the GLI proteins, the final effectors of classic Hedgehog pathway. GANT61 is a GLI inhibitor showing a potent effect on the inhibition of transcription activity of GLI proteins, blocking their binding to DNA [5–8]. Considering the high homology of the DNA-binding domain between GLIS2 and GLI family proteins, we hypothesized that GANT61 might be used to specifically target the CBFA2T3-GLIS2 fusion gene in pediatric AML.
In the present study, we investigated the in vitro effects of GANT61 on AML cell lines and primary cells from AML patients harboring the CBFA2T3-GLIS2 fusion gene.
The materials and methods are detailed in Additional file 1. Molecular analysis of CBFA2T3-GLIS2 fusion gene is reported in Additional file 2: Figure S1. Genetic features of control AML cell lines without GLIS2 fusion are reported in Additional file 3: Table S1.
Our results showed that AML cell lines with CBFA2T3-GLIS2 fusion gene have a higher sensitivity to GANT61 than other AML cell lines without this genetic aberration (Fig. 1a). Similar results were obtained on primary leukemia cells isolated from AML patients, being the IC50 of the GLIS2-positive leukemia and negative primary cells 13.6 and 41.6 μM, respectively (Fig. 1b).
Fig. 1.
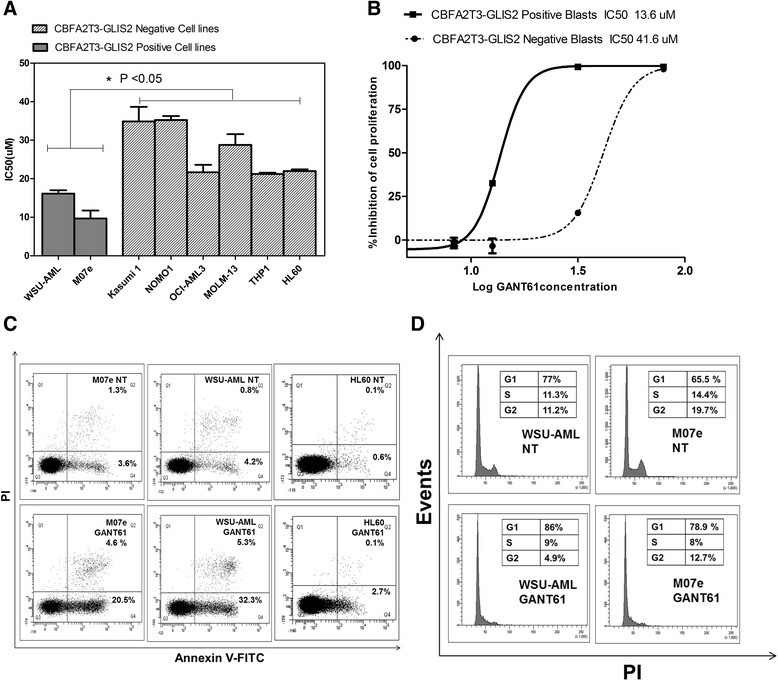
a IC50 of CBFA2T3-GLIS2 and negative cell lines 72 h after GANT61 exposure. b Dose-response curves after 72 h of GANT61 treatment of primary cells derived from patients with acute myeloid leukemia (AML) either positive or negative for CBFA2T3-GLIS2 fusion gene. *p < 0.05 c Flow cytometric analysis of Annexin V FITC/PI-stained AML cell lines treated for 24 h with 20 μM of GANT61. The percentages of early apoptotic cells (Annexin V FITC+/PI−, lower right quadrant) and late apoptotic/necrotic cells (Annexin V FITC+/PI+, upper right quadrant) are indicated. NT sample treated with vehicle alone (DMSO). d Cell cycle analysis. Flow cytometric analysis of PI-stained AML cell lines carrying the CBFA2T3-GLIS2 fusion gene after 48 h of treatment with GANT61. NT sample treated with vehicle alone (DMSO)
Treatment with GANT61 induced an increase of about 30% of apoptotic cells (Fig. 1c) and block of cell cycle in G0/G1 phase only in M07e and WSU-AML lines positive to CBFA2T3-GLIS2 (Fig. 1d and Additional file 4: Figure S2).
We further analyzed the expression profile of cell lines and primary cells following GANT61 treatment. Through qPCR, we demonstrated that GANT61 treatment led to a significant reduction of the expression of BMP2 and GLIS2 (Fig. 2a, b). In order to fully characterize the effect of GANT61 treatment on whole transcriptome profile of CBFA2T3-GLIS2-positive cells, gene expression was assessed by microarray analysis. After GANT61 treatment, the expression of target genes of CBFA2T3-GLIS2, such as CRISP3, GATA3, H2AFY, or NCAM1(CD56) was significantly downregulated (p < 0.05) (Fig. 2c). Moreover additional genes were downregulated by the treatment with GANT61 (p < 0.05), as for example, genes involved in cell cycle control, such as CDC25A, CDC7, CDCA2, and CCNA2. The expression of these genes is required for progression through cell cycle, and their expression is aberrant in AML, as well as in other malignancies [9, 10]. In our model, the expression of these genes is downregulated following GANT61 treatment, this partly explaining the cell cycle arrest observed in AML cell lines with GLIS2 fusion after GANT61 treatment (Fig. 1d). Genes involved in cell proliferation (KIF14, MELK, MCM10, NUF2) and epigenetic regulators namely DNMT1 and DNMT3B were also present. Considering the particular interest of these DNA methyltransferase genes, we performed chromatin immunoprecipitation (ChIP) analysis using a CBFA2T3-specific antibody on WSU-AML and M07e cell lines. Our findings showed that CBFA2T3-GLIS2 fusion protein directly binds to the proximal promoter of DNMT1 and DNMT3B, positively regulating their expression (Fig. 2d). Overexpression of DNMT genes could lead to DNA hypermethylation and could be involved in the leukemogenesis process.
Fig. 2.
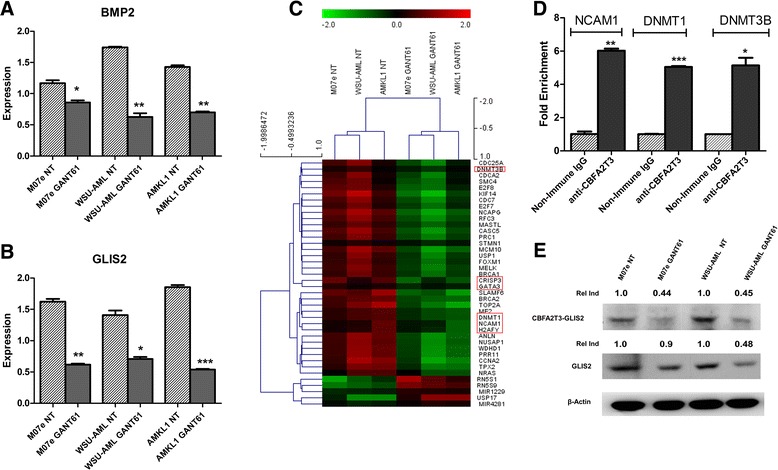
Quantitative PCR of selected mediators of GLIS2 pathway a BMP2 and b GLIS2 after 48 h treatment with GANT61. *p < 0.05; **p < 0.01; ***p < 0.001. c Hierarchical clustering of genes differentially expressed between untreated and treated AML leukemia blast cells and cell lines, with a p value <0.05. d ChIP analysis, performed on WSU-AML cell line showed around five-fold enrichment of chimeric protein on DNMT1, DNMT3B, and NCAM1 promoters. e Western blot analysis showing the decrease of GLIS2 protein and CBFA2T3-GLIS chimeric protein in samples treated with GANT61. Thirty micrograms of protein were blotted to each lane. Antibody to β-actin served as a loading control. The Relative Induction (Rel Ind) is the amount of protein present in treated samples relative to untreated cells after normalizing to β-actin density
Since in the classic Hedgehog signaling pathway, several target genes involved in feedback mechanisms (HHIP, PTCH1, GLI1) have been described; we hypothesized that CBFA2T3-GLIS2 chimeric protein could regulate wild-type GLIS2 protein with the same feedback mechanism. Western blotting analysis confirmed the presence of chimeric protein and showed also the presence of wild-type GLIS2. These results may point to the role of the fusion protein in regulating wild-type GLIS2. Following GANT61 treatment, the expression of both proteins was decreased with respect to untreated samples, suggesting that GANT61 treatment targeted both CBFA2T3-GLIS2 fusion protein and also wild-type GLIS2 expression (Fig. 2e). Moreover, other AML cell lines not carrying the CBFA2T3-GLIS2 fusion gene did not show expression of GLIS2 (data not shown).
On the other hand, western blotting analysis showed that expression of GLI1 and GLI2 did not decrease following GANT61 treatment (Additional file 5: Figure S3).
Another study demonstrated a high sensitivity of this subgroup of AML with GLIS2 fusion to Aurora A kinase (AURKA) inhibitors [4]. We therefore investigated the effect of GANT61 and AURKA inhibitor MK-0457 in M07e and WSU-AML cell lines carrying the CBFA2T3-GLIS2 fusion gene. Cell lines were incubated for 48 h with either single drugs or a combination of the two drugs at a constant ratio of 1:10 (GANT61:MK-0457). The combined treatment showed a higher cytotoxic effect when compared to each single drug, and the two inhibitors displayed a synergistic effect on cell growth, as indicated by the CI value (Additional file 6: Figure S4).
This work provides preliminary data from preclinical in vitro and ex vivo studies targeting pediatric AML with CBFA2T3-GLIS2 fusion gene. Although further investigation will be required to confirm these results, our experience with GANT61 represents a preliminary background for further evaluating in vivo the inhibition of GLIS2-mediated transcription in AML harboring the CBFA2T3-GLIS2 fusion gene.
Acknowledgements
The authors would like to thank Dr. Tanja Gruber from St. Jude Children’s Research Hospital, Memphis, for kindly providing the WSU-AML cell line.
Funding
This work was partly supported by the grants from Fondazione Veronesi (Young Investigator Grant, to R. Masetti), AIRC (Associazione Italiana Ricerca sul Cancro, My First AIRC grant to R. Masetti), AIRC (Associazione Italiana Ricerca sul Cancro, Special Grant “5xmille”-9962 to F. Locatelli), Ministero della Salute (RF-2010-2316606 to F. Locatelli; Ricerca Corrente to F. Locatelli) and Ministero dell’Istruzione, Università e Ricerca (Grant Progetto di Rilevante Interesse Nazionale, PRIN 2010, to F. Locatelli), Cariparo-Fondazione città della Speranza to M. Pigazzi and G. Basso, and PRAT-Università degli Studi di Padova to M. Pigazzi.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Authors’ contributions
MR and SNB designed the work, performed the data analysis, and wrote the manuscript; AA contributed to write the manuscript; SNB, AA, FC, AL, JB, SS, MF, and MP performed the laboratory work for this study; MD and VI performed the statistical and bioinformatics analyses; AMM, GB, FL, and AP supervised the work and contributed to the critical revision; AP, designed and supervised the research. All authors read and approved the final version of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The samples analyzed have been obtained from patients enrolled in the Associazione Italiana Ematologia Oncologia Pediatrica 2002/01 clinical trial, which was approved by the institutional review board of the Sant’Orsola-Malpighi Hospital, Bologna, Italy. The patients gave informed consent in accordance with the Declaration of Helsinki.
Abbreviations
- AML
Acute myeloid leukemia
- AURKA
Aurora A kinase
- BMP
Bone morphogenic protein
- ChIP
Chromatin immunoprecipitation
- FAB
French-American-British
- GLIS2
GLI-similar protein 2
- HH
Hedgehog
- PI
Propidium iodide
- WST1
4-[3-(4 lodophenyl)-2-(4-nitrophenyl)-2H-5-tetrazolio]-1,3-benzene disulfonate)
Additional files
Materials and methods. (DOCX 22 kb)
A) Molecular analysis of CBFA2T3-GLIS2 fusion gene. 1.M07e, 2.WSU-AML, 3.KASUMI1, 4.NOMO1, 5.OCI-AML3, 6.MOLM13, 7.THP1, 8.HL60, 9.Negative Control. B) Sequencing of CBFA2T3-GLIS2 fusion gene in M07e and in C) WSU-AML. (TIF 6759 kb)
Genetic features of control AML cell lines. * Data provided by DSMZ and by literature. (XLSX 11 kb)
Cell cycle analysis. Flow cytometric analysis of PI-stained AML cell lines negative to CBFA2T3-GLIS2 fusion gene after 48 h of treatment with GANT61. NT: sample treated with vehicle alone (DMSO). (TIF 183 kb)
Western blotting analysis of GLI1/2 protein in cell lines either positive or negative for GLIS2 fusion gene treated with GANT61. NT, untreated cells. One representative of three independent experiments is shown. (TIF 205 kb)
Cytotoxic effect of either GANT61, or MK-0457 or of GANT61 in association with MK-0457 on A) M07e and in B) WSU-AML cell lines. (TIF 369 kb)
References
- 1.Gruber TA, et al. An Inv(16)(p13.3q24.3)-encoded CBFA2T3-GLIS2 fusion protein defines an aggressive subtype of pediatric acute megakaryoblastic leukemia. Cancer Cell. 2012;22(5):683–697. doi: 10.1016/j.ccr.2012.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Masetti R, et al. CBFA2T3-GLIS2 fusion transcript is a novel common feature in pediatric, cytogenetically normal AML, not restricted to FAB M7 subtype. Blood. 2013;121(17):3469–3472. doi: 10.1182/blood-2012-11-469825. [DOI] [PubMed] [Google Scholar]
- 3.De Rooij JD, et al. Recurrent abnormalities can be used for risk group stratification in pediatric AMKL: a retrospective intergroup study. Blood. 2016;127(26):3424–3430. doi: 10.1182/blood-2016-01-695551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thiollier C, et al. Characterization of novel genomic alterations and therapeutic approaches using acute megakaryoblastic leukemia xenograft models. J Exp Med. 2012;209(11):2017–2031. doi: 10.1084/jem.20121343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wellbrock J, et al. Expression of hedgehog pathway mediator GLI represents a negative prognostic marker in human acute myeloid leukemia and its inhibition exerts antileukemic effects. Clin Cancer Res. 2015;21(10):2388–2398. doi: 10.1158/1078-0432.CCR-14-1059. [DOI] [PubMed] [Google Scholar]
- 6.Lauth M, et al. Inhibition of GLI-mediated transcription and tumor cell growth by small-molecule antagonists. Proc Natl Acad Sci USA. 2007;104(20):8455–8460. doi: 10.1073/pnas.0609699104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.An D, et al. Gli inhibitor GANT61 causes apoptosis in myeloid leukemia cells and acts in synergy with rapamycin. Leuk Res. 2012;36(6):742–748. doi: 10.1016/j.leukres.2012.02.012. [DOI] [PubMed] [Google Scholar]
- 8.Agyeman A, et al. Mode and specificity of binding of the small molecule GANT61 to GLI determines inhibition of GLI-DNA binding. Oncotarget. 2014;5(12):4492–4503. doi: 10.18632/oncotarget.2046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bertoli S, et al. CDC25A governs proliferation and differentiation of FLT3-ITD acute myeloid leukemia. Oncotarget. 2015;6(35):38061–38078. doi: 10.18632/oncotarget.5706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ji P, et al. DNA damage response involves modulation of Ku70 and Rb functions by cyclin A1 in leukemia cells. Int J Cancer. 2007;121(4):706–713. doi: 10.1002/ijc.22634. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.


