Abstract
Objective
HIV-infected patients in Africa are vulnerable to severe recurrent infection with Streptococcus pneumoniae, but no effective preventive strategy has been developed. We set out to determine which factors influence in-hospital mortality and long-term survival of Malawians with invasive pneumococcal disease.
Design, setting and patients
Acute clinical features, inpatient mortality and long-term survival were described among consecutively admitted hospital patients with S. pneumoniae in the blood or cerebrospinal fluid. Factors associated with inpatient mortality were determined, and patients surviving to discharge were followed to determine their long-term outcome.
Results
A total of 217 patients with pneumococcal disease were studied over an 18-month period. Among these, 158 out of 167 consenting to testing (95%) were HIV positive. Inpatient mortality was 65% for pneumococcal meningitis (n = 64), 20% for pneumococcaemic pneumonia (n = 92), 26% for patients with pneumococcaemia without localizing signs (n = 43), and 76% in patients with probable meningitis (n = 17). Lowered consciousness level, hypotension, and age exceeding 55 years at presentation were associated with inpatient death, but not long-term outcome in survivors. Hospital survivors were followed for a median of 414 days; 39% died in the community during the study period. Outpatient death was associated with multilobar chest signs, oral candidiasis, and severe anaemia as an inpatient.
Conclusion
Most patients with pneumococcal disease in Malawi have HIV co-infection. They have severe disease with a high mortality rate. At discharge, all HIV-infected adults have a poor prognosis but patients with multilobar chest signs or anaemia are at particular risk.
Keywords: Adult, Africa, bacteraemia, HIV-1, Malawi, meningitis, pneumonia, prognosis, Streptococcus pneumoniae
Introduction
It has been known for a decade that Streptococcus pneumoniae is an important pathogen in HIV-infected adults in Africa [1], causing a high incidence of bloodstream and recurrent infections [2]. HIV-infected patients in the United States have also been shown to have an increased incidence of bloodstream [3,4] and recurrent pneumococcal infections, with these infections exhibiting a wider spectrum of associated clinical features [5], including infection in atypical sites [6], compared with immunocompetent adults [7]. A decreased incidence of pneumonia and pneumococcal infections has recently accompanied the increased use of highly active antiretroviral therapy (HAART) in the United States [8]. HAART is currently unavailable in most of Africa, however, as a result of both the cost of the drugs and problems associated with drug delivery. Furthermore, the available 23-valent pneumococcal polysaccharide vaccine has been shown to be ineffective in HIV-infected adults in a vaccine trial in Uganda [9]. Antibiotic prophylaxis against bacterial infections is not widely used in HIV-infected adults because of issues of cost, drug delivery, high baseline levels of antibiotic resistance, and the risk of increasing drug resistance [10]. An increased understanding of the presentation and prognosis of pneumococcal disease in HIV-infected African adults may help in planning alternative approaches aimed at decreasing the disease burden.
Malawi is an underdeveloped country in sub-Saharan Africa, with an estimated seroprevalence of HIV of 35% among urban-dwelling adults [11]. We showed that in Blantyre, Malawi, S. pneumoniae was the most common cause of bacterial meningitis [12], and was a major cause of bacteraemia [13] among adult inpatients.
We now report both the acute mortality and long-term survival of HIV-infected Malawian patients admitted to hospital with invasive S. pneumoniae disease presenting as pneumococcal meningitis, bacteraemic pneumonia and bacteraemia without a detectable clinical focus. None of these patients was treated with antiretroviral therapy or antibiotic prophylaxis.
Materials and methods
Study site
The Queen Elizabeth Central Hospital, Blantyre, Malawi is a large government teaching hospital that serves the southern region of Malawi. Approximately 395 000 outpatients are seen in the emergency department each year, and 9800 adults are admitted from there to the non-fee-paying medical wards. Since the advent of the HIV pandemic, the numbers of admissions have increased fourfold [14], with the number of cases presenting with meningitis increasing eightfold [15]. The seroprevalence of HIV among medical inpatients in a sample of 758 patients in 2000 was 75% (D. Lewis, personal communication).
Patient recruitment and case definitions
All adults admitted to the medical wards during an 18-month period (October 1997 to March 1999) with a temperature greater than 37.5°C had samples collected for blood culture at the time of admission, along with clinical details on a standard proforma. In addition, patients with clinical features consistent with meningitis (two of the following: fever, headache, neck stiffness, altered consciousness) were recommended to have diagnostic lumbar puncture. If S. pneumoniae was identified in any of these samples, patients were recruited with informed consent to an observational study of clinical features and disease outcome.
Patients were defined as having pneumococcal meningitis if S. pneumoniae was identified in the cerebrospinal fluid (CSF) or if the CSF contained more than 50 neutrophils per millilitre in a patient with pneumococcaemia. Patients were defined as having bacteraemic pneumonia if they had chest signs on clinical examination and pneumococcaemia. These two categories of patients were distinguished from those with bacteraemia with no focal symptoms or signs. Patients with clinical meningitis and pneumococcaemia but normal CSF were also included in this ‘bacteraemic’ group.
Patient investigation and treatment
Patients were pre-counselled before HIV testing according to local guidelines, and were tested if consent was obtained (if the patient was unconscious, consent was sought from the accompanying relative or guardian). When possible, patients were offered an erect postero-anterior chest radiograph (no portable chest X-rays were taken), and simple haematological measurements were carried out. All patients suspected by the attending physician of having tuberculosis submitted three sputum samples for smear examination.
All patients were treated according to local guidelines. Patients with a clinical diagnosis of meningitis were treated with intravenous benzyl penicillin (2.4 g every 6 h) and chloramphenicol (1 g every 6 h) for a minimum of 5 days; treatment was given orally when patients were fully conscious and eating. All patients with pneumococcal meningitis were given 3 weeks of antibiotic therapy (local policy). Patients with pneumonia were treated with oral amoxycillin unless they had clinical features of severe disease – at least one of the following: respiratory rate greater than 40 per minute, systolic blood pressure less than 90 mmHg, cyanosis, confusion or multilobar disease. In severe cases, combinations of intravenous benzyl penicillin (1.2 g every 6 h) and erythromycin (500 mg every 6 h) or gentamicin (240 mg once a day) were used at the discretion of the attending physician.
Laboratory testing
HIV testing
Blood samples were tested using two rapid tests (Uni-gold HIV and Serocard, Trinity Biotech, Dublin, Ireland).
Blood cultures
Blood culture was performed using 5 ml of venous blood inoculated into a single aerobic culture bottle containing 50 ml of supplemented brain heart infusion broth containing (E&O Laboratories, UK) and transferred immediately to the laboratory for manual processing.
Cerebrospinal fluid analysis
CSF samples were routinely analysed for total cell count and differential white cell count. Gram stains were performed if the white cell count was greater than or equal to 10/mm3, and India ink staining was carried out on all except the grossly turbid samples. All samples were cultured onto sheep blood agar for 48 h in the presence of carbon dioxide (candle extinction jar), with additional broth cultures for samples with an increased white cell count. Mycobacterial and viral cultures were not performed.
Description of pneumococcal isolates
Organisms were identified using colony morphology and optochin sensitivity. Antibiotic sensitivities were tested by disc diffusion. Penicillin susceptibility was assessed with a screening technique using a 1 µg oxacillin disc. Minimum inhibitory concentrations were not performed for any isolate. Serogrouping was carried out using the Quellung reaction observed with a set of diagnostic antisera (Statens Seruminstitut, Copenhagen, Denmark).
Outpatient follow-up
Patients participating in the follow-up study were provided with transport home from hospital and a monthly outpatient appointment. Patients failing to attend the regular follow-up clinic were visited at home. Details of intercurrent illness were recorded, and treatment prescribed as appropriate. If patients died, details of the terminal illness and date of death were recorded. No blood samples were taken on home visits, but samples were taken from patients feeling unwell at outpatient clinics. In addition, a series of blood culture samples from patients who were well was also collected at the clinic to determine if patients continued to have asymptomatic bacteraemia.
Data handling and statistical analysis
All patient data were stored in a database (MS Access 97, Microsoft Corp, USA), and statistical analyses were carried out using Stata version 6 (Statacorp, USA).
First, comparisons were made between patients with meningitis, bacteraemic pneumonia and bacteraemia. Details of the presenting history and examination findings at presentation as well as inpatient and long-term outcome were compared between these groups. Second, comparisons were made between patients who survived and those who died as inpatients. Finally, patients who died as outpatients were compared with those in whom outpatient follow-up was complete to one year. Continuous variables were compared using the Kruskall–Wallis test and categorical variables using the χ2 test. Multiple logistic regression was used to determine risk factors for inpatient death with comparative risk expressed as odds ratios (OR). Cox’s proportional hazard ratios (HR) were used to compare outpatient survival between groups.
Ethical review
This study was reviewed and approved by the Health Sciences Research Committee of Malawi. All subjects or their relatives gave written informed consent to participation in this study.
Results
Patients
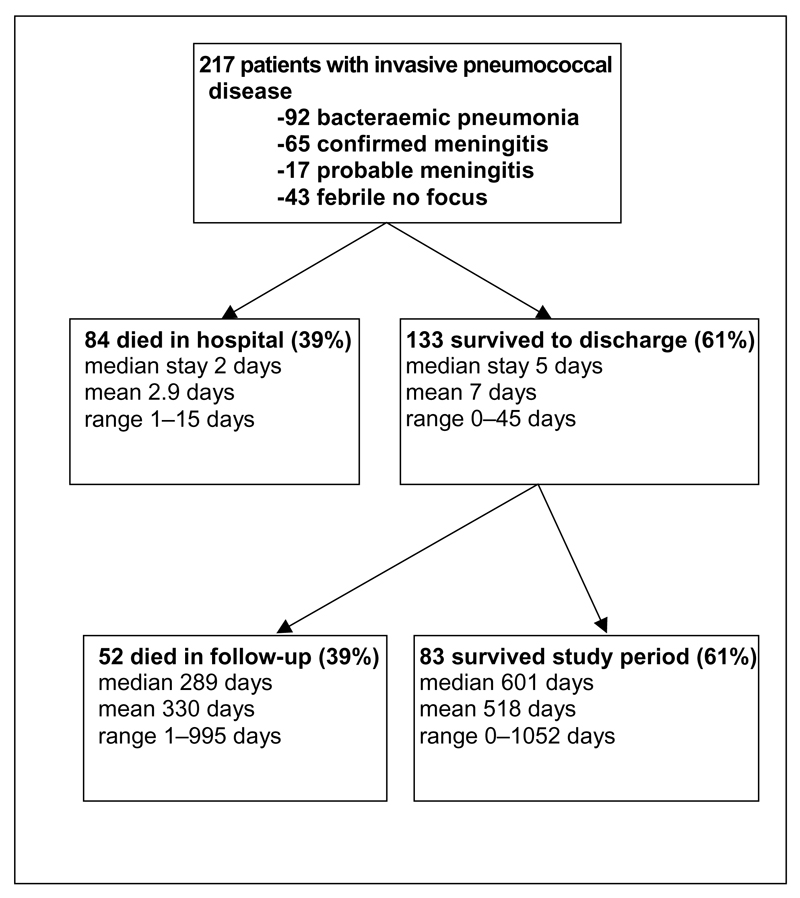
A total of 217 patients with invasive pneumococcal disease were recruited to the observational study (see Fig. 1). A total of 84 patients (39%) died during their hospital admission. Of the remaining 133, 52 died in follow-up, bringing the total mortality during the study to 136 (63%). A total of 82 patients had taken antibiotics prescribed by a pharmacy before admission (52% of 157 patients were able to give a full drug history).
Fig. 1.
Patient group studied. This flow chart shows the total number of patients followed in the study and their diagnoses. The numbers of patients dying as inpatients or during follow-up are also shown.
Prevalence of known risk factors for invasive pneumococcal disease
The most common risk factors for invasive pneumococcal disease in this cohort were HIV infection and a previous history of lung disease. A total of 167 of the 217 patients (77%) consented to HIV testing, of whom 158 (95% of those tested) were HIV positive. Patients from whom consent was not obtained were more often suffering from meningitis (OR 2.2, P = 0.02) or were women (OR 2.1, P = 0.03). As a group, those refusing consent had a mortality rate of 72% compared with 29% in the group with known HIV status (χ2 30, P < 0.001). A total of 41 patients had a previous history of lung disease, of whom 24 presented with pneumonia (χ2 7.5, P = 0.02).
There were equal numbers of men and women in the study, and although the mean age of the men exceeded that of the women (men 35.9 years, women 30.5 years; t = −4.03, P = 0.0001), the mortality in men and women was the same. A total of 25 patients were more than 55 years old. Less than 15% of the cohort reported ever having smoked a cigarette. Only eight patients regularly drank alcohol, and none described themselves as alcohol dependent. None of the patients had a history of liver or kidney disease, immunosuppressive medication, solid or haematological tumours, stroke or ischaemic heart disease.
Clinical features and acute outcome
Clinical features of the cohort are compared in Table 1 according to the clinical definitions described above. A total of 52 patients (26% of the group) had a chest X-ray; 48 of these were patients who survived to discharge and four died in hospital (37% of patients surviving to discharge had a chest X-ray, but only 6% of those who died; χ2 23.7, P < 0.001). The number of chest X-rays taken was limited by local facilities, and the ability of the patients to reach the X-ray department. Of the 52 films taken, five were reported to be normal, seven showed lobar pneumonia, 21 showed multilobar consolidation, and 19 showed abnormalities not typical of acute pneumococcal pneumonia. The latter group included predominantly bilateral basal infiltration (16), but also bilateral apical cavitation (one), mycetoma (one), and pleural effusion later shown to be empyema (one).
Table 1.
Patients compared by diagnostic group.
| Clinical Features | Pneumonia | Meningitis | Bacteraemia | P valuea |
|---|---|---|---|---|
| Number in group (n = 200) | 92 | 65 | 43 | |
| Demographics | ||||
| Age (mean) | 33.9 | 32.1 | 31.5 | 0.7 |
| Sex, female : male (% male) | 39 : 53 (58) | 36 : 29 (45) | 23 : 20 (47) | 0.2 |
| Features of acute presentation with a difference between highlighted group and other groups, n (%) | ||||
| Cough | 88 (97) | 26 (40) | 25 (58) | <0.001 |
| Chills | 43 (47) | 9 (14) | 8 (19) | <0.001 |
| Dyspnoea | 65 (71) | 21 (32) | 8 (19) | <0.001 |
| Confusion | 5 (5) | 38 (58) | 1 (2) | <0.001 |
| Previous treatment | ||||
| Traditional medicine | 30 (38) | 9 (14) | 10 (23) | 0.03 |
| Pharmacy outpatient antibiotics | 42 (53) | 24 (53) | 16 (57) | 0.9 |
| Features of AIDS – excess in highlighted group | ||||
| Previous pneumonia | 16 (17) | 6 (9) | 1 (2) | 0.03 |
| Wasting | 64 (70) | 26 (40) | 19 (44) | <0.001 |
| Prolonged fever | 34 (37) | 11 (17) | 11 (26) | 0.02 |
| Persistent cough | 14 (15) | 1 (2) | 2 (5) | 0.006 |
| Lymph nodes | 14 (15) | 1 (2) | 2 (5) | 0.006 |
| Features on examination – excess in highlighted group | ||||
| Multilobar signs | 34 (36) | 7 (11) | 0 (0) | <0.001 |
| Herpes labialis, n (%) | 9 (10) | 17 (26) | 3 (7) | 0.005 |
| Reduced Glasgow coma score | 3 (3) | 38 (58) | 0 (0) | <0.001 |
| Hospital stay | ||||
| Inpatient mortality, n (%) | 18 (20) | 42 (65) | 11 (26) | <0.001 |
| Days in hospital (survived) mean (SD) | 6.6 (6.3) | 10 (4.7) | 4.4 (2.6) | 0.0001 |
| Days in hospital (died) mean (SD) | 5.1 (3.7) | 2.1 (1.7) | 3.3 (4.0) | 0.004 |
Continuous variables were compared using the Kruskal–Wallis test and categorical variables using χ2. In this table, basic demographic features are compared between patient groups, and the features of history and examination at presentation that distinguished one group from another are highlighted. In addition, differences in treatment before admission, features of AIDS and overall outcome are compared.
Meningitis
A total of 65 patients had a diagnosis of pneumococcal meningitis (29 men and 36 women), of whom 42 died (65%) as inpatients within a median period of 2 days (range 1–9 days). Ten patients with pneumococcal meningitis also had clinical signs of chest infection, one had a knee effusion and one had otitis media. In addition, 17 patients with clinical features of meningitis or decreased consciousness level and subsequent pneumococcal bacteraemia (six men and 11 women) did not have CSF examined because they either died very quickly, refused lumbar puncture, or had a failed procedure. Of these patients, 13 (76%) died within a median period of 2 days (range 1–7 days). These cases were termed ‘probable meningitis’, but could not be included in further analysis because of the lack of a definitive diagnosis.
Pneumonia
A total of 92 patients had bacteraemia, together with a clinical diagnosis of pneumonia made on examination (53 men and 39 women). A total of 18 of these patients (20%) died as inpatients within a median period of 4.5 days (range 1–14 days). There was no difference in acute mortality in patients with right and left-sided unilateral disease (40 and 16 patients, respectively), but multilobar chest signs (34 patients) were accompanied by a poor prognosis in outpatient follow-up compared with patients with unilateral signs (OR 6.6, CI 2.3–19.0; P = 0.001). Fourteen patients had serial sputum samples examined for acid-fast bacilli while an inpatient. Of these, one had positive Ziehl–Neilson slides on all three samples.
Bacteraemia
A total of 43 patients (20 men and 23 women) had pneumococcal bacteraemia in the absence of signs of pneumonia – one of these had both S. pneumoniae and Salmonella enteritidis on blood culture. Three patients in this group had clinical meningitis – two had normal CSF and one Cryptococcus neoformans infection. Lumbar puncture was not indicated in the other patients. Chest X-rays were taken of eight patients in this group, and were reported as showing a potential focus of infection in six patients. Eleven patients (26%) in this group died within a median period of 2 days (range 1–15 days).
Comparison of inpatient outcome by clinical group
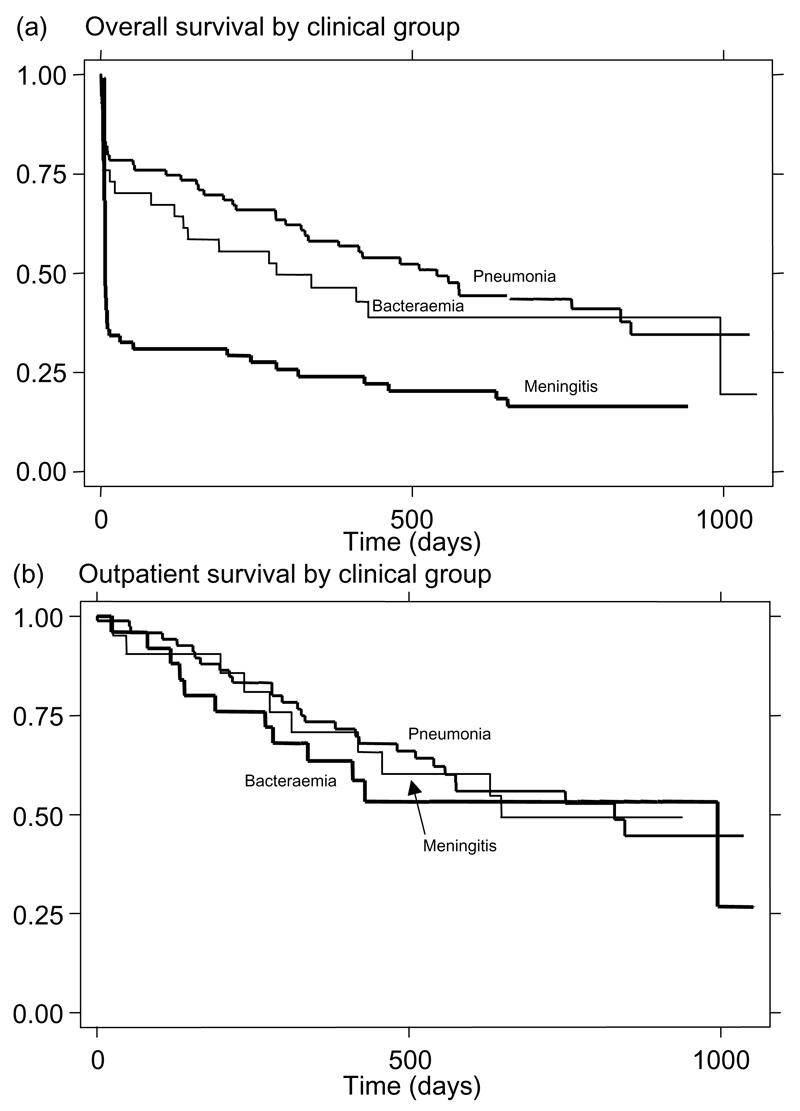
The survival of patients by inpatient presentation is shown in Fig. 2a. There was no significant difference between the mean ages of patients, or their sex distribution, between the diagnostic groups (see Table 1). There was a significant difference between the inpatient mortality of patients with confirmed meningitis compared with pneumonia (OR 7.5, CI 3.6–15.5; P < 0.0001) or bacteraemia (OR 5.3, CI 2.3–12.5; P < 0.0001), but not between patients with bacteraemia and those with pneumonia (OR 1.4, CI 0.6–3.3; P = 0.4).
Fig. 2.
Kaplan–Meier survival estimates by clinical group. (a) Overall patient survival is plotted for the whole group divided according to the diagnosis of pneumonia, confirmed meningitis or bacteraemia. There is a significant difference in mortality rates (P < 0.0001), which is caused by inpatient mortality. (b) Outpatient survival is plotted in the same manner and shows no significant difference in mortality rates after leaving hospital by clinical group (P = 0.55). Patients dying as inpatients do not appear in (b).
Predictors of inpatient death
Three important features were predictive of inpatient death in the whole group (see Table 2). These were confusion on admission (OR 5.8, CI 2.9–11.3; P < 0.0001), age greater than 55 years (OR 3.8, CI 1.7–8.7; P = 0.001) and hypotension (systolic blood pressure less than 90 mmHg; OR 4.8, CI 1.1–21.6; P = 0.04). The OR for confusion corrected for age and hypotension was 16.1 (CI 5.1–51.1; P < 0.0001). The likelihood of survival and the presenting level of consciousness were significantly correlated. Among patients presenting with a normal Glasgow Coma Score (GCS), the mortality was 30%, compared with 50% with a GCS of between 9 and 14, and was 74% in those with a GCS of less than 9 (χ2 26; P < 0.001).
Table 2.
Factors associated with inpatient mortality are not associated with poorer long-term outcome
| Inpatient mortality |
Long-term outcome |
|||||
|---|---|---|---|---|---|---|
| Feature | OR | CI | P | HR | CI | P |
| Features associated with increased inpatient mortality | ||||||
| Confusion | 5.7 | 2.9–11.3 | < 0.001 | 0.91 | 0.41–2.0 | 0.82 |
| Diastolic BP/mmHg | 0.95 | 0.93–0.98 | 0.004 | 0.99 | 0.97–1.1 | 0.36 |
| Age > 55 years | 3.8 | 1.7–8.7 | 0.001 | 1.8 | 0.56–5.8 | 0.3 |
| Features associated with increased long-term mortality rate | ||||||
| Oral candida | 0.25 | 0.1–0.6 | 0.001 | 1.8 | 1.1–3.3 | 0.03 |
| Multilobar disease | 1.0 | 0.5–2.0 | 0.96 | 2.1 | 1.17–3.8 | 0.01 |
| Anaemia | 1.2 | 0.3–5.5 | 0.8 | 3.9 | 1.5–10.1 | 0.005 |
BP, Blood pressure.
In the table, the three features confirmed by regression analysis to be most associated with inpatient mortality are presented together with their associated odds ratio (OR) and the confidence interval (CI) and P value. The same features were then examined for any predictive value on long-term outcome and the associated hazard ratio (HR) and CI and P value are presented in the right-hand panel. In the lower panel, the reverse process was carried out, that is, features associated with a poor long-term prognosis were examined for their predictive value on inpatient mortality. It can be seen that factors associated with poor acute outcome are different from those predicting poor longer-term survival.
Subgroup analyses showed that among the bacteraemia patients who had no clinical signs by definition, age exceeding 55 years was strongly associated with a poor outcome (OR 17, CI 3.1–93.5; P = 0.001). Among patients with pneumonia, hypotension at presentation was strongly associated with inpatient death (OR 10.4, CI 1.8–60.6, P = 0.009). Meningitis patients had a mortality rate of 67% overall, and an OR of 6.7 (CI 3.5–12.8; P < 0.001) for inpatient death compared with other patients in the group. This difference remained significant even after correction for confusion (OR 4.3, CI 2.0–9.4; P < 0.001).
Patient long-term survival
A total of 133 patients were discharged from hospital. These patients had a median stay in hospital of 5 days, and were followed for up to 1052 days (median 414 days). Patient attendance at clinic was poor, and the bulk of follow-up was carried out actively in the community. Late in the study, patients were increasingly likely to be ill and to return to their rural homes from the city, making follow-up more difficult. A total of 51 patients (39%) died during the follow-up period, with a median survival of 330 days.
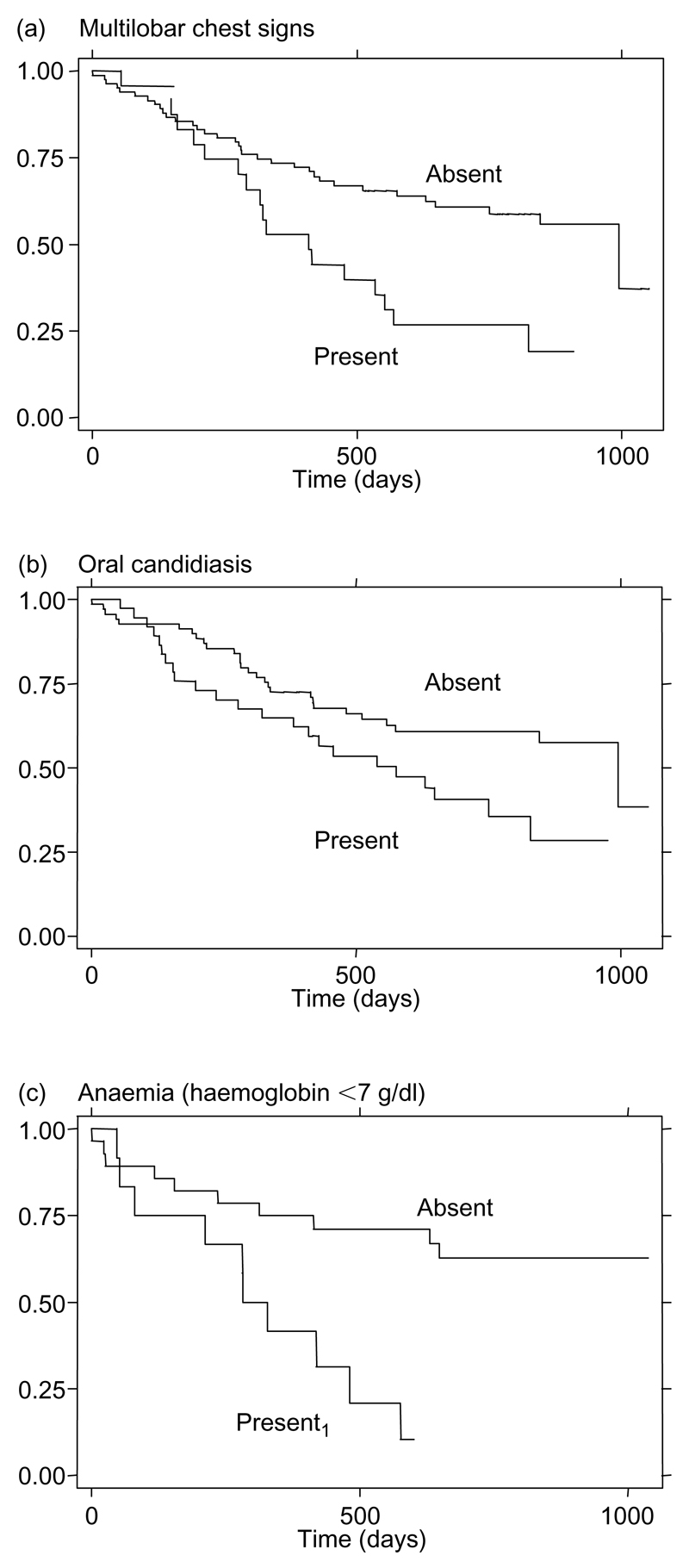
The survival curves by clinical diagnostic groups for patients discharged from hospital are shown in Fig. 1b. Despite the significantly different inpatient mortality rate between the groups with meningitis, bacteraemia and pneumonia, respectively (above), outpatient mortality did not differ between groups (37, 37 and 40%, respectively; χ2 0.68, P = 0.96). Outpatient mortality was also not related to age, shock at presentation or low GCS – all of which were associated with high inpatient mortality rates (see Table 2). Increased out-patient mortality (see Fig. 3) was associated with multilobar chest signs (HR 2.1, CI 1.2–3.8; P = 0.01), oral candida (HR 1.8, CI 1.1–3.3; P = 0.03), and anaemia (HR 3.9, CI 1.5–10; P = 0.005), although haematological data were only available for 53 out of 133 patients followed-up.
Fig. 3.
Outpatient risk factors. Kaplan–Meier plots showing survival among patients with multilobar chest signs (a) or oral candida (b) compared with the survival of the rest of the group. (c) All patients with a recorded haemoglobin result (n = 53) were divided according to whether or not they had anaemia (Hb < 7 g/dl at presentation, n = 16) or not (haemoglobin > 7 g/dl, n = 37). There was a significantly increased mortality rate in patients with multilobar disease compared with the rest of the group [hazard ratios (HR) 2.1, 95% confidence intervals (CI) 1.2–3.8; P = 0.01]. There was also increased mortality in the group with oral candida compared with those without oral candida (HR 1.8, CI 1.1–3.3; P = 0.03), and among patients with anaemia compared with those without anaemia (HR 3.9, CI 1.5–10.1; P = 0.005).
Isolates of Streptococcus pneumoniae: source, antibiotic resistance and serogroups
All isolates in this study were obtained from normally sterile sites in symptomatic patients. Early in the study, 130 blood cultures were taken from asymptomatic clinic attendees to establish if patients had asymptomatic bacteraemia. None grew S. pneumoniae. During this time, recurrent invasive pneumococcal disease was diagnosed by blood culture in four symptomatic patients during the study, along with one case each of Acinetobacter, Citrobacter and non-typhoidal salmonella.
A total of 145 isolates (145/173; 84%) from blood cultures and 55 isolates (55/63; 87%) from CSF culture were found to be fully sensitive to penicillin. There was no increase in inpatient, outpatient or overall mortality in the patients from whom the resistant isolates were obtained compared with patients with penicillin-sensitive isolates. Antibiotic sensitivity was also determined for erythromycin (99%), chloramphenicol (76%), tetracycline (50%), and co-trimoxazole (6%). No significant difference was found in the antibiotic sensitivity of blood and CSF isolates.
A total of 119 pneumococcal isolates were serogrouped in our laboratory using diagnostic antisera (Pneumotest, Statens Seruminstitut, Denmark); 73% were found to be in the serogroups covered by the 23-valent pneumococcal polysaccharide vaccine.
Discussion
We have described clinical features and outcome in a cohort of 217 consecutive patients with invasive pneumococcal disease in a resource-deprived environment in which the majority of patients are HIV infected. A total of 39% of patients died of their acute illness, and only 38% of the cohort remained alive at the end of the 18-month study period. Pneumococcal disease is a very different illness in Africa from that experienced in most western hospitals.
Three modes of presentation were observed – meningitis, with an inpatient mortality rate of 65%, and pneumonia and bacteraemia, with inpatient mortality rates of 20 and 26%, respectively. Despite the difference in disease severity at presentation, survivors of these groups had equal long-term survivals.
The factors associated with inpatient death were confusion or lowered coma score, age greater than 55 years and hypotension. The median time to death was 2 days from admission to hospital. These data suggest that the patients who died in this series might not have been saved with altered medical therapy [16], but rather with a change in health-seeking behaviour or healthcare delivery, resulting in earlier admission to hospital. Over 50% of patients in this series had been treated in community pharmacies before admission, however, and many patients had approached both traditional healers and dispensary physicians before being admitted (Table 1). There is evidence, therefore, that healthcare provision, rather than health-seeking behaviour, must be improved to alter the mortality rate of this disease. In our hospital, less than 2.5% of patients presenting to the emergency department are admitted to medical wards (9800/395 000, 2.4%), as bed occupancy is already between 100 and 200%.
The mortality rate during outpatient follow-up in this study was 31% per year. Patients were followed in the community for up to 1052 days (median 414 days). During this time, 39% of the cohort discharged from hospital died. This overall mortality rate is similar to that of larger studies, in which unselected HIV-infected patients were followed in a similar setting [9]. The design of this study does not allow the determination of whether pneumococcal infection is itself a poor prognostic factor in HIV-infected adults.
We found three main factors to be associated with poor outpatient outcome in this study: anaemia defined as haemoglobin less than 7 g/dl (OR 7), oral candidiasis (OR 3.4), and multilobar pulmonary disease (OR 4.6). None of these factors was associated with acute inpatient death. The association of severe anaemia with poor outcome in HIV-infected patients has been noted by other authors [17–19], and may be partly caused by Mycobacterium tuberculosis infection involving the bone marrow, as well as concurrent viral infections and nutritional deficiencies. Unfortunately, the haematology data in this study are limited, and no information about the causes of anaemia was obtained. Oral candidiasis is a feature of HIV disease progression, and as such the association with poor outcome is unsurprising. Multilobar chest signs may reflect the severity of pneumococcal disease, but could alternatively result from M. tuberculosis infection or pulmonary malignancy.
What strategies for improved care can be developed from these observations? First, all patients presenting with pneumococcal infection in areas of high HIV prevalence must be suspected of being co-infected with HIV, and are therefore likely to have a poor prognosis in the longer term. Second, the multilobar chest signs described as being associated with poor outcome among outpatients are suggestive of dual pathology, and especially of tuberculosis. A recent study of pneumonia patients in Kenya has demonstrated that tuberculosis is under-diagnosed among patients presenting as an emergency [20]. Sputum examination for acid-fast bacilli in all inpatients with chest signs may be justified but will create an extra burden on already strained resources [21,22]. Present practice is to examine sputum from patients with a history of cough of 3 weeks’ duration, hence the very low rate of sputum examination in this series. The observations in this study supported Scott et al. [23] in their suggestion that more patients should have sputum examination carried out during hospital admission.
The substantial difference in outcome observed between severely anaemic patients and those with a haemoglobin level above 7 g/dl (median survival 282 days compared with 648 days) is based on a small number of subjects (n = 53), but merits further investigation. Nutritional support and the treatment of other infections could potentially make an important difference, but these strategies are untried. It is more likely, however, that the prognosis for these patients would only improve with HAART.
The prevention of pneumococcal disease in Malawi remains an important goal. The 23-valent pneumococcal polysaccharide vaccine has been shown to be ineffective in primary prophylaxis in HIV-infected adults in Africa [9], but conjugate vaccine trials have yet to report, and secondary prophylaxis with either type of vaccine remains untried. Antibiotic prophylaxis with trimethoprim–sulphamethoxazole has been shown to reduce HIV-associated morbidity in West Africa [24], but no clear results of this kind have yet been reported from other sub-Saharan regions, including Blantyre, where there is a high rate of cotrimoxazole resistance in pneumococcal isolates [10,25].
Acknowledgments
Sponsorship: This work received financial support from the Wellcome Trust of Great Britain (Training Fellowship held by SG through the Liverpool Wellcome Trust Centre for Research in Clinical Tropical Medicine) and forms part of the Malawi-Liverpool-Wellcome Trust Programme of Research in Clinical Tropical Medicine.
References
- 1.Gilks CF, Brindle RJ, Otieno LS, et al. Life-threatening bacteraemia in HIV-1 seropositive adults admitted to hospital in Nairobi, Kenya. Lancet. 1990;336:545–549. doi: 10.1016/0140-6736(90)92096-z. [DOI] [PubMed] [Google Scholar]
- 2.Gilks CF, Ojoo SA, Ojoo JC, et al. Invasive pneumococcal disease in a cohort of predominantly HIV-1 infected female sex-workers in Nairobi, Kenya. Lancet. 1996;347:718–723. doi: 10.1016/s0140-6736(96)90076-8. [DOI] [PubMed] [Google Scholar]
- 3.Redd SC, Rutherford GW, Sande MA, et al. The role of human immunodeficiency virus in pneumococcal bacteraemia in San Francisco residents. J Infect Dis. 1990;162:1012–1017. doi: 10.1093/infdis/162.5.1012. [DOI] [PubMed] [Google Scholar]
- 4.Hibbs JR, Douglas JMJ, Judson FN, et al. Prevalence of human immunodeficiency virus infection, mortality rate, and serogroup distribution among patients with pneumococcal bacteremia at Denver General Hospital, 1984–1994. Clin Infect Dis. 1997;25:195–199. doi: 10.1086/514538. [DOI] [PubMed] [Google Scholar]
- 5.Frankel RE, Virata M, Hardalo C, Altice FL, Friedland G. Invasive pneumococcal disease: clinical features, serotypes, and antimicrobial resistance patterns in cases involving patients with and without human immunodeficiency virus infection. Clin Infect Dis. 1996;23:577–584. doi: 10.1093/clinids/23.3.577. [DOI] [PubMed] [Google Scholar]
- 6.Rodriguez BM, Musher DM, Hamill RJ, et al. Unusual manifestations of pneumococcal infection in human immunodeficiency virus-infected individuals: the past revisited. Clin Infect Dis. 1992;14:192–199. doi: 10.1093/clinids/14.1.192. [DOI] [PubMed] [Google Scholar]
- 7.Janoff EN, Breiman RF, Daley CL, Hopewell PC. Pneumococcal disease during HIV infection. Epidemiologic, clinical, and immunologic perspectives. Ann Intern Med. 1992;117:314–324. doi: 10.7326/0003-4819-117-4-314. [DOI] [PubMed] [Google Scholar]
- 8.Sullivan JH, Moore RD, Keruly JC, Chaisson RE. Effect of antiretroviral therapy on the incidence of bacterial pneumonia in patients with advanced HIV infection. Am J Resp Crit Care Med. 2000;162:64–67. doi: 10.1164/ajrccm.162.1.9904101. [DOI] [PubMed] [Google Scholar]
- 9.French N, Nakiyingi J, Carpenter LM, et al. 23-Valent pneumococcal polysaccharide vaccine in HIV-1-infected Ugandan adults: double-blind, randomised and placebo controlled trial. Lancet. 2000;355:2106–2111. doi: 10.1016/s0140-6736(00)02377-1. [DOI] [PubMed] [Google Scholar]
- 10.Feikin DR, Dowell SF, Nwanyanwu OC, et al. Increased carriage of trimethoprim/sulfamethoxazole-resistant Streptococcus pneumoniae in Malawian children after treatment for malaria with sulfadoxine/pyrimethamine. J Infect Dis. 2000;181:1501–1505. doi: 10.1086/315382. [DOI] [PubMed] [Google Scholar]
- 11.Taha ET, Dallabetta GA, Hoover DR, et al. Trends of HIV-1 and sexually transmitted diseases among pregnant and postpartum women in urban Malawi. AIDS. 1998;12:197–203. doi: 10.1097/00002030-199802000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Gordon SB, Walsh AL, Chaponda M, et al. Bacterial meningitis in malawian adults: pneumococcal disease is common, severe, and seasonal. Clin Infect Dis. 2000;31:53–57. doi: 10.1086/313910. [DOI] [PubMed] [Google Scholar]
- 13.Gordon MA, Walsh AL, Chaponda M, et al. Bacteraemia and mortality among adult medical admissions in Malawi – predominance of non-typhi salmonellae and Streptococcus pneumoniae. J Infect. 2001;42:44–49. doi: 10.1053/jinf.2000.0779. [DOI] [PubMed] [Google Scholar]
- 14.Brown KG. Analysis of admissions to the adult medical wards at Queen Elizabeth Central Hospital, Blantyre, Malawi. East Afr Med J. 1975;52:509–528. [PubMed] [Google Scholar]
- 15.Brown KG. Meningitis in Queen Elizabeth Central Hospital, Blantyre, Malawi. East African Med J. 1975;52:376–385. [PubMed] [Google Scholar]
- 16.Austrian R, Gold J. Pneumococcal bacteraemia with especial reference to bacteremic pneumococcal pneumonia. Ann Intern Med. 1964;60:759–776. doi: 10.7326/0003-4819-60-5-759. [DOI] [PubMed] [Google Scholar]
- 17.Moore RD. Human immunodeficiency virus infection, anemia, and survival. Clin Infect Dis. 1999;29:44–49. doi: 10.1086/520178. [DOI] [PubMed] [Google Scholar]
- 18.Antelman G, Msamanga GI, Spiegelman D, et al. Nutritional factors and infectious disease contribute to anemia among pregnant women with human immunodeficiency virus in Tanzania. J Nutr. 2000;130:1950–1957. doi: 10.1093/jn/130.8.1950. [DOI] [PubMed] [Google Scholar]
- 19.van den Broek NR, Letsky EA. Etiology of anemia in pregnancy in south Malawi. Am J Clin Nutr. 2000;72(Suppl):247S–256S. doi: 10.1093/ajcn/72.1.247S. [DOI] [PubMed] [Google Scholar]
- 20.Scott JA, Hall AJ, Muyodi C, et al. Aetiology, outcome, and risk factors for mortality among adults with acute pneumonia in Kenya. Lancet. 2000;355:1225–1230. doi: 10.1016/s0140-6736(00)02089-4. [DOI] [PubMed] [Google Scholar]
- 21.Harries A, Hargreaves N, Kemp J, Kwanjana J, Salaniponi F. Diagnosis of tuberculosis in Africa. Lancet. 2000;355:2256. doi: 10.1016/S0140-6736(05)72758-6. [DOI] [PubMed] [Google Scholar]
- 22.Harries AD. Tuberculosis in Africa: clinical presentation and management. Pharmacol Ther. 1997;73:1–50. doi: 10.1016/s0163-7258(96)00115-5. [DOI] [PubMed] [Google Scholar]
- 23.Scott JA, Hall AJ, Muyodi C, et al. Aetiology, outcome, and risk factors for mortality among adults with acute pneumonia in Kenya. Lancet. 2000;355:1225–1230. doi: 10.1016/s0140-6736(00)02089-4. [DOI] [PubMed] [Google Scholar]
- 24.Wiktor SZ, Sassan-Morokro M, Grant AD, et al. Efficacy of trimethoprim–sulphamethoxazole prophylaxis to decrease morbidity and mortality in HIV-1-infected patients with tuberculosis in Abidjan, Cote d’Ivoire: a randomised controlled trial. Lancet. 1999;353:1469–1475. doi: 10.1016/s0140-6736(99)03465-0. published erratum appears in Lancet 1999, 353:2078. [DOI] [PubMed] [Google Scholar]
- 25.Boeree MJ, Harries AD, Zijlstra EE, Taylor TE, Molyneux ME. Cotrimoxazole in HIV-1 infection. Lancet. 1999;354:334. doi: 10.1016/S0140-6736(05)75236-3. [DOI] [PubMed] [Google Scholar]