Abstract
Adoptive cell transfer (ACT) melanoma immunotherapy typically employs acutely activated effector CD8+ T cells for their ability to rapidly recognize and clear antigen. We have previously observed that effector CD8+ T cells are highly susceptible to melanoma-induced suppression, whereas memory CD8+ T cells are not. Although memory T cells have been presumed to be potentially advantageous for ACT, the kinetics of local and systemic T cell responses after effector and memory ACT have not been compared. B16F10 melanoma cells stably transfected to express very low levels of the lymphocytic choriomeningitis virus (LCMV) peptide GP33 (B16GP33) were inoculated into syngeneic C57BL/6 mice. Equal numbers of bona fide naïve, effector, or memory phenotype GP33-specific CD8+ T cells were adoptively transferred into mice 1 day after B16GP33 inoculation. The efficacy of ACT immunotherapy was kinetically assessed using serial tumor measurements and flow cytometric analyses of local and systemic CD8+ T cell responses. Control of B16GP33 tumor growth, persistence of adoptively transferred CD8+ cells, intratumoral infiltration of CD8+ T cells, and systemic CD8+ T cell responsiveness to GP33 were strongest after ACT of memory CD8+ T cells. Following surgical tumor resection and melanoma tumor challenge, only mice receiving memory T cell-based ACT immunotherapy exhibited durable tumor-specific immunity. These findings demonstrate how the use of non-expanded memory CD8+ T cells may enhance ACT immunotherapeutic efficacy.
Keywords: Immunotherapy, Melanoma, T cell, Memory, Effector, Adoptive transfer
Introduction
Adoptive cell transfer (ACT) is an immunotherapeutic strategy that takes advantage of tumor antigen-specific CD8+ T cells within tumor-infiltrating lymphocyte (TIL) populations. Preclinical and clinical studies have proven the principle of ACT immunotherapy, in which TIL is isolated from tumors, stimulated to undergo massive in vitro proliferation, and infused into patients in hopes of causing immunological tumor regression [1–3]. ACT protocols typically depend on pre-transfer lymphodepletion to maximize the engraftment and persistence of ex vivo-expanded T cell populations [4–6]. Although clinical trials of melanoma ACT have demonstrated favorable response rates and cases of profound and durable disease regression, suboptimal response rates and the complexity and risks of pre-transfer lymphodepletion have tempered widespread implementation of this promising strategy.
CD8+ T cells pass through various states of differentiation determined by their temporal relation to antigen encounter [7–10]. Antigenic stimulation drives naïve CD8+ T cells to differentiate into effector CD8+ T cells capable of rapid proliferation and antigen clearance. Effector T cells are highly susceptible to apoptosis, but a subset of memory precursor effector T cells persist and eventually differentiate into memory CD8+ T cells capable of long-term proliferative renewal. In response to later antigen encounters, memory T cells quickly activate and expand [11, 12].
Because of their ability to undergo large-scale proliferative expansion and their effectiveness in recognizing and clearing antigen, effector T cells have been a mainstay of ACT. However, effector T cells are terminally differentiated cells with a finite life expectancy and no capacity for self-renewal. It has been well recognized that ACT efficacy can be enhanced with the use of less differentiated subtypes of T cells, including memory T cells [13–19]. However, the specific consequences of effector versus memory T cell transfer on the intratumoral and systemic immunological milieu and on endogenous tumor-directed T cell responses have not been clearly dissected. We have previously demonstrated that in vivo exposure to melanoma impairs the transition of resting to effector T cells and enhances the apoptotic contraction of acutely activated T cells CD8+ T cells [20, 21]; in contrast, the capacity of memory T cells for homeostatic proliferation and antigen-driven reactivation are unaltered by in vivo exposure to melanoma [22].
Based on these findings, we sought to compare the local and systemic immunological consequences of effector versus naïve versus memory CD8+ T cell-based ACT using a murine model of non-lymphodepletion adoptive melanoma immunotherapy. We employed a lymphocytic choriomeningitis virus (LCMV) infection model to generate bona fide resting naïve, activated effector, and resting memory CD8+ T cells, and used a recombinant B16F10 melanoma tumor model expressing low levels of the LCMV peptide GP33 previously optimized in our laboratory. In order to directly compare the in vivo efficacy of these various states of T cell activation and differentiation, we adoptively transferred unmodified GP33-specific naïve, effector, and memory CD8+ T cells without peptide or cytokine stimulation in order to preserve their activation status at the moment of in vivo antigen encounter. We report that, whereas effector and memory CD8+ T cells are comparable in their ability to inhibit melanoma tumor growth in vitro and promote endogenous melanoma-specific T cell responses in vivo, memory CD8+ T cells are more effective than effector CD8+ T cells at mediating ACT immunotherapy and that this enhanced efficacy is associated with a stronger induction of TIL, greater durability and persistence and survival of adoptively transferred T cells, the generation of a more potent systemic tumor-specific CD8+ T cell response, and a potential for promoting durable tumor immunity.
Materials and methods
Mice
Seven- to eight-week-old female Ly5.2+/C57BL/6 and Ly5.1+/B6.SJL mice were purchased from Taconic (Hudson, NY) and maintained in sterile housing. All mouse work was conducted with the approval of the University of Wisconsin and William S. Middleton Memorial VA Hospital Animal Care and Use Committees.
Tumor cell lines and virus
Tumor inoculations and viral infections were performed as previously described [20, 21]. A poorly immunogenic B16F10 melanoma cell line arising in C57BL/6 mice was cultured in RPMI-1640 medium (Mediatech, Herndon, VA) with 10 % fetal bovine serum, 2 mM l-glutamine, 100 μg/mL streptomycin, and 100 U/mL penicillin (Life Technologies, Inc., Grand Island, NY). B16F10 cells were transfected with a plasmid encoding GP33, a class I MHC-restricted LCMV surface glycoprotein. The plasmid also encoded G418 resistance, and poorly immunogenic clones with low levels of GP33 expression were selected [21]. Tumors were established in C57BL/6 mice with subcutaneous injections of 106 B16F10 or B16GP33 cells suspended in serum-free RPMI-1640 media. Viral infection was performed by inoculating C57BL/6 mice with intraperitoneal injections of 2 × 105 PFU of Armstrong strain of LCMV.
Adoptive cell transfer
Adoptive cell transfer was performed as previously described [21, 22]. Naïve CD8+ GP33-specific T cells were derived from splenocytes harvested from Ly5.1+ P14 TCR transgenic mice (C57BL/6 background with TCR specificity for GP33). Effector CD8+ GP33-specific T cells were derived from splenocytes harvested from congenic Ly5.1+ B6.SJL mice 8 days after LCMV infection. Memory CD8+ GP33-specific T cells were derived from splenocytes harvested from Ly5.1+ B6.SJL mice 50–80 days after LCMV infection. In order to enhance the yield of CD8+ GP33-specific memory T cells, 103 CD8+ GP33-specific T cells from resting Ly5.1+ P14 TCR transgenic mice were adoptively transferred into Ly5.1+ B6.SJL mice 1 day prior to LCMV infection. Magnetic bead separation columns (Miltenyi, Auburn, CA) were used to enrich splenocytes for CD8 expression. CD62L− effector memory T cells were separated from CD62L+ central memory T cells using CD62L magnetic bead separation columns (Miltenyi, Auburn, CA). CD8+ GP33-specific T cell populations were characterized and quantified by flow cytometry. Adoptive immunotherapy was performed by adoptively transferring 105 CD8+ GP33-specific T cells or serum-free media into tumor-bearing mice 1 or 7 days after B16GP33 tumor inoculation. Recipients of adoptive immunotherapy were Ly5.2+ C57BL/6 mice; in this way, exogenous donor-derived Ly5.1+ CD8+ T cells could be distinguished from endogenous Ly5.2+ CD8+ T cells after immunotherapy.
MTT assay
CD8+ GP33-specific T cells were co-cultured with B16F10 or B16GP33 melanoma cells at multiple effector/target ratios with IL-2 (10 ng/mL) for 24 h in 48-well plates. B16F10 or B16GP33 melanoma cell proliferative activity was quantified using the Celltiter 96 non-radioactive MTT assay kit (Promega, Madison, WI) following manufacturer’s instructions.
Flow cytometry
Flow cytometric characterization of lymphocytes was performed using methods as previously described [19–22]. Prior to adoptive transfer, harvested splenocytes were stained with APC-labeled MHC class I (Db) tetramers loaded with GP33, PErCP-labeled anti-CD8, PE-labeled anti-CD62L, PECy7-labeled anti-CD127, and FITC-labeled anti-KLRG1 antibodies and analyzed by flow cytometry. On day 4 or 14 after B16GP33 tumor inoculation, tumors were explanted and homogenized, and single-cell suspensions of tumor-infiltrating lymphocytes were isolated using Histopaque (Sigma-Aldrich, St. Louis, MO). Tumor-infiltrating lymphocytes were stained with APC-labeled MHC class I (Db) tetramers loaded with GP33 peptide, PerCP-labeled anti-CD8, PE-labeled anti-Ly5.1, and FITC-labeled anti-CD44 and analyzed by flow cytometry. Also on day 14 after B16GP33 tumor inoculation, splenocytes (106 cells/well) were stimulated with media alone or with GP33 peptide (0.1 μg/mL) with brefeldin A and human recombinant IL-2 (10 U/well) and incubated in flat-bottomed 96-well plates at 37 °C for 5 h. After staining with FITC-labeled anti-CD8 antibody, the Cytofix/Cytoperm kit (BD Biosciences-Pharmingen, San Diego, CA) was used to permeabilize and stain the cells with APC-labeled anti-IFNγ antibody. Stained cells were quantified on a FACSCalibur flow cytometer (BD Biosciences-Pharmingen, San Diego, CA) and analyzed using FlowJo software (Tree Star, Inc., Ashland, OR). Unless otherwise specified, all reagents and antibodies were purchased from BD Biosciences.
Hematoxylin and eosin staining
Mice were killed on day 18 after tumor injection. Tumors were resected and prepared for staining. Deparaffinized slides were prepared in xylene and rehydrated through a graded alcohol series to dH20. Slides were stained in filtered and modified Harris hematoxylin for 4 min, washed with running tap water, and then differentiated in 1 % acid alcohol. The slides were washed with tap water, soaked with 1 % ammonia water for 30 s, washed with water, acclimated in 95 % ETOH, and then stained with 1 % alcoholic eosin solution for 1 min. Slides were dehydrated through two changes of 95 % followed by 100 % ETOH, cleared in xylene, and mounted with Cytoseal.
Statistical analysis
IBM SPSS statistical software version 19 (Armonk, NY) was used to analyze experimental data. A repeated-measures analysis of variance (ANOVA) with pair-wise comparisons performed using Fisher’s protected least significant difference tests was used to compare experimental groups. All reported p values are two-sided, and significance was defined as p < 0.05. Error bars in graphical representations of data represent standard errors of the mean.
Results
Memory CD8+ T cell-based ACT is more effective than naïve or effector CD8+ T cell-based ACT at inhibiting in vivo melanoma growth
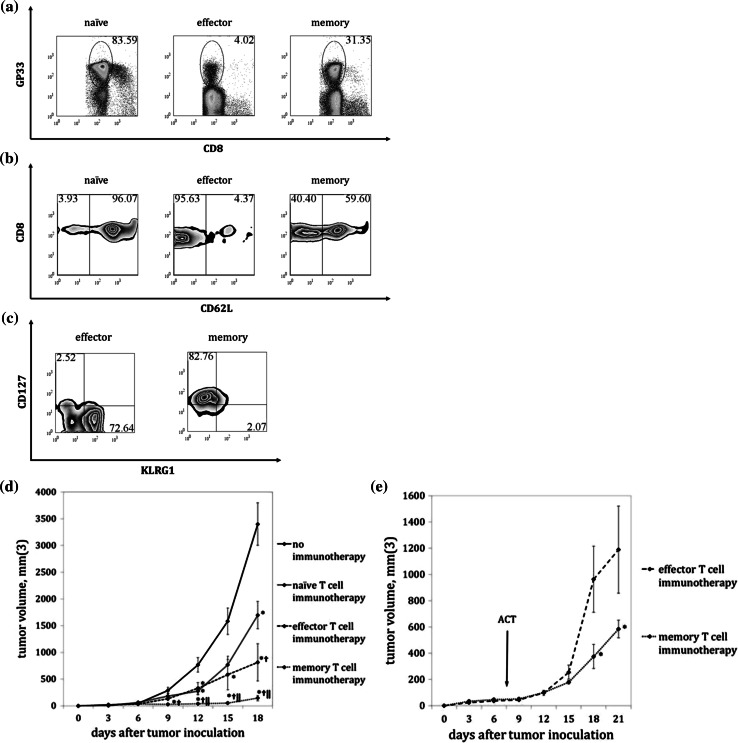
To identify differences in immunotherapeutic efficacy between various states of CD8+ T cell differentiation, C57BL/6 mice were inoculated with subcutaneous B16GP33 melanoma tumors and intravenously injected with 105 GP33-specific CD8+ T cells in various states of differentiation 1 day later. As shown in Fig. 1a–c, GP33-specific CD8+ T cells harvested from uninfected P14 TCR transgenic mice, B6.SJL mice at 8 days after LCMV infection, and B6.SJL mice at >60 days after LCMV infection were predominantly of naïve, effector, and memory phenotype, respectively, as assessed by CD44, CD62L, KLRG, and CD127 expression. Control mice did not receive ACT. Exponential tumor growth was observed in control mice, and minimal tumor inhibition was observed in mice treated with naïve T cell ACT. Significant inhibition of tumor growth was observed in mice that received effector T cell ACT, but significantly greater inhibition was seen in mice that received equivalent numbers of memory T cells (Fig. 1d). Similar findings were observed when mice were treated with effector or memory T cell ACT 7 days after tumor inoculation (Fig. 1e).
Fig. 1.
ACT of memory CD8+ T cells results in optimal control of melanoma tumor growth. Naïve, effector, and memory Ly5.1+ CD8+ GP33-specific T cells are harvested and characterized by flow cytometry for: a TCR specificity for GP33 by staining with MHC tetramer loaded with GP33 peptide (gated on CD8+ lymphocytes) b CD62L expression, and c CD127 and KLRG1 expression (gated on CD8+ GP33-specific cells). d Serial B16GP33 tumor measurements in mice treated with no immunotherapy or ACT of 105 CD8+ GP33-specific naïve, effector, or memory T cells one day after tumor inoculation demonstrated maximal inhibition of tumor growth after memory T cell ACT. e Memory T cells remained more effective than effector T cells when ACT is performed 7 days after tumor inoculation. These experiments are performed 3–4 times with similar results, with four mice per group (*p < 0.05 vs. no immunotherapy; † p < 0.05 vs. naïve T cell immunotherapy; ‖ p < 0.05 vs. effector T cell immunotherapy)
Memory CD8+ T cell subsets are similarly effective at inhibiting melanoma growth in vivo
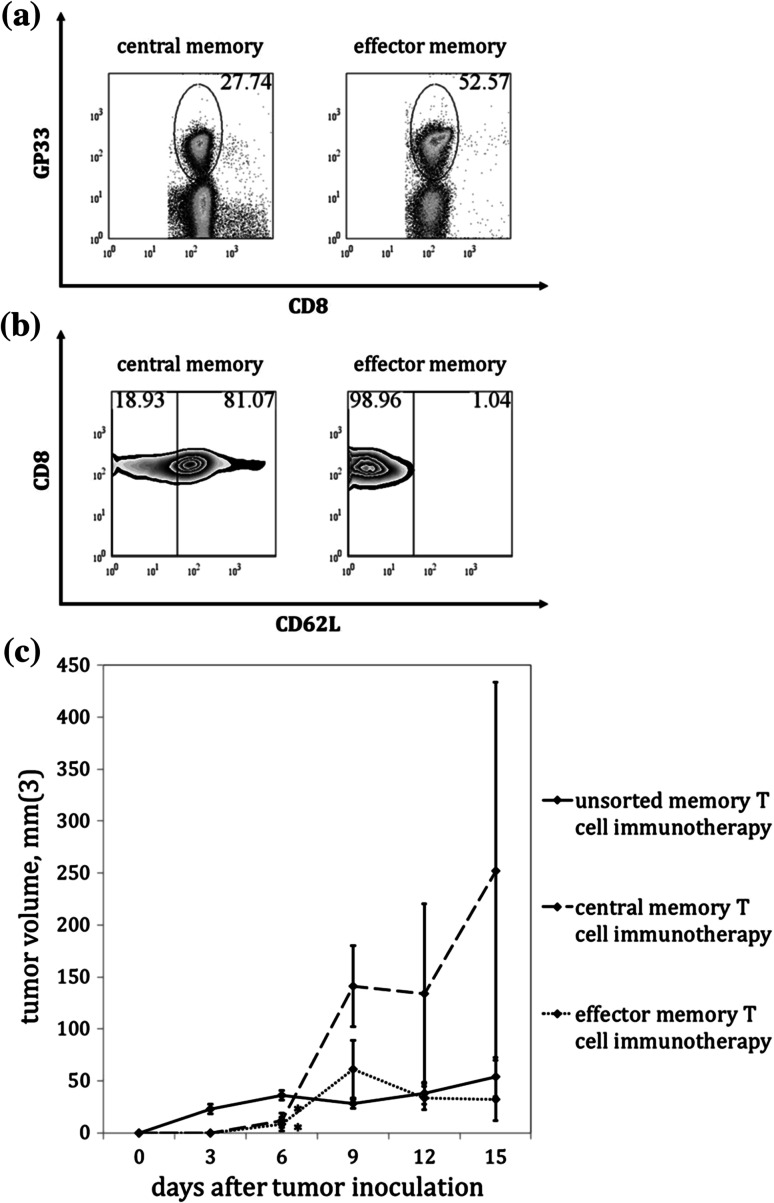
To determine whether memory T cell subsets have differential efficacy in inhibiting melanoma growth, GP33-specific CD8+ memory T cells were separated by column separation based on CD62L expression into effector memory (CD62L−) and central memory (CD62L+) subsets (Figs. 2a,b) and 105 GP33-specific CD8+ T cells were adoptively transferred into C57BL/6 mice 1 day after B16GP33 melanoma tumor inoculation. As shown in Fig. 2c, adoptive transfer of 105 GP33-specific CD8+ effector memory T cells (TEM) appeared to result in a somewhat stronger inhibition of tumor growth than adoptive transfer of 105 GP33-specific CD8+ central memory T cells (TCM), but these differences were not statistically significant.
Fig. 2.
Memory T cell subsets are comparable in their ability to inhibit melanoma tumor growth. Memory CD8+ GP33-specific T cells are separated into central memory (CD62L+) and effector memory (CD62L−) subsets by magnetic bead column separation and then characterized by FACS analysis based on: a TCR specificity for GP33 (gated on CD8+ lymphocytes) and b CD62L expression (gated on CD8+ GP33-specific cells). c Serial B16GP33 tumor measurements in mice treated with ACT of 105 CD8+ GP33-specific unsorted, central, or effector memory T cells demonstrated no statistically significant differences in tumor control. This experiment is performed three times with similar results, with four mice per group (*p < 0.05 vs. unsorted memory T cell immunotherapy)
Memory CD8+ T cells are not more potent than effector CD8+ T cells at inhibiting melanoma growth in vitro
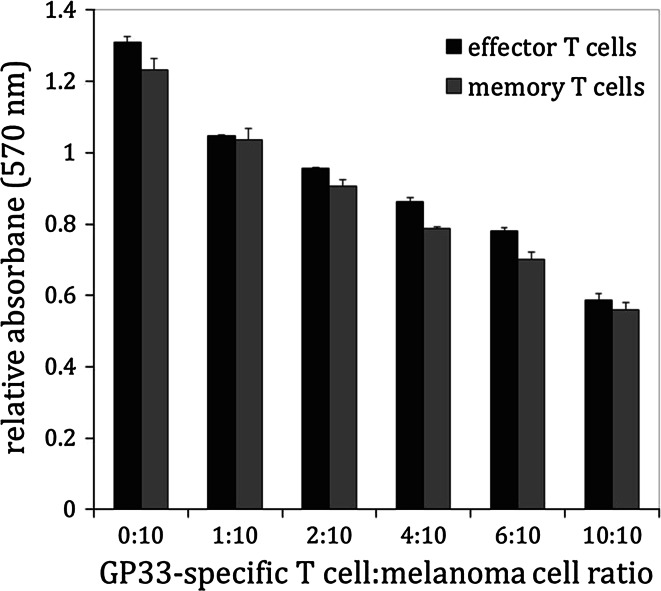
To determine whether memory CD8+ T cells are intrinsically more cytostatic or cytotoxic than effector CD8+ T cells, B16GP33 melanoma cells were co-cultured with effector or memory CD8+ GP33-specific T cells at various ratios for 24 h. In the last 4 h of co-culture, melanoma cells were pulsed with MTT and cellular proliferation was measured by standard colorimetric assay. Figure 3 shows that the inhibitory effects of effector and memory CD8+ T cells on B16GP33 melanoma tumor growth were similar, suggesting that there were no substantial differences in their intrinsic ability to arrest target cell proliferation.
Fig. 3.
Effector and memory CD8+ T cells are similar in their ability to inhibit melanoma proliferation in vitro. 2 × 105 B16F10 or B16GP33 melanoma cells are co-cultured with CD8+ GP33-specific effector or memory T cells at various effector/target ratios for 24 h. MTT assays measuring the viability of adherent melanoma cells demonstrated comparable dose-dependent inhibition of B16GP33 melanoma cell viability; non-specific inhibition of parental B16F10 melanoma cells (which do not express GP33) is not observed. This experiment is performed four times with similar results, with four wells per group
Memory CD8+ T cell-based ACT promotes more potent intratumoral CD8+ T cell infiltration than effector CD8+ T cell-based ACT
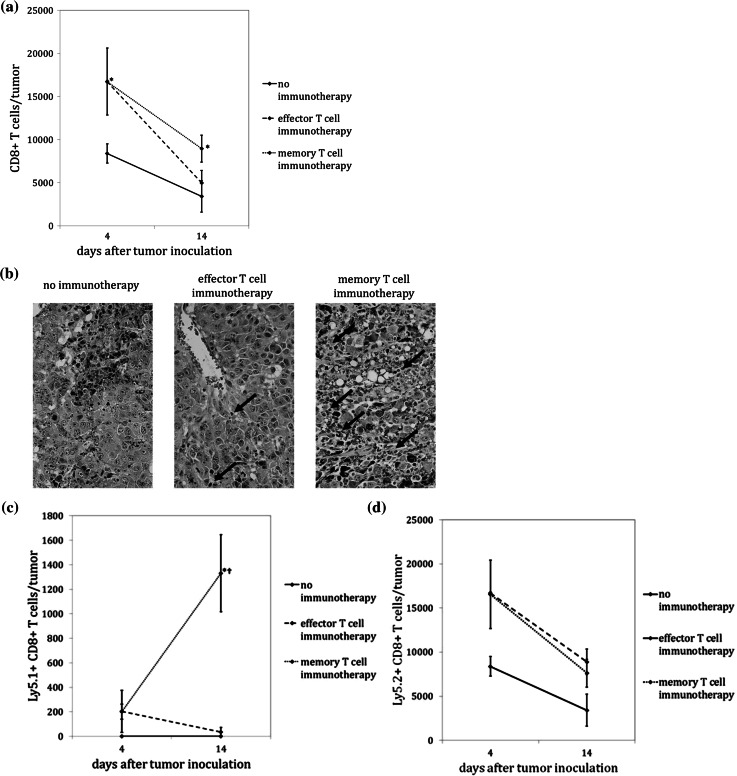
To determine whether potency of memory T cell ACT was due to enhanced intratumoral T cell infiltration, B16GP33 melanoma-bearing C57BL/6 mice received adoptive transfer of 105 effector or memory CD8+ T cells 1 day after tumor injection and were euthanized on days 4 and 14. Tumors were explanted and homogenized into single-cell suspensions from which lymphocyte populations were characterized by flow cytometry. As shown in Fig. 4a, significantly higher intratumoral populations of total (donor-derived plus endogenous) CD8+ T cells were observed on day 4 in mice that had received ACT immunotherapy, with no differences observed between effector and memory T cells. The numbers of intratumoral CD8+ T cells decreased by day 14 in all groups, but significantly higher numbers were present in mice that had received memory T cell ACT. As depicted in Fig. 4b, hematoxylin and eosin microscopic examination of paraffinized tumor sections collected on day 18 also appeared to demonstrate more potent TIL populations following memory CD8+ T cell ACT. Figure 4c shows that, whereas CD8+ T cells derived from Ly5.1+ donor mice declined from day 4 to day 14 after effector T cell ACT, donor-derived CD8+ T cells increased in number after memory T cell ACT. As demonstrated in Fig. 4d, the increase in TIL seen after memory T cell ACT was due to differences in donor-derived T cells, as no differences in endogenously derived Ly5.2+ TIL were observed between the two immunotherapy groups at the two time points.
Fig. 4.
Memory T cell ACT results in a stronger local T cell response. As before, no immunotherapy or ACT of 105 Ly5.1+/CD8 + GP33-specific effector or memory T cells is performed on day one after B16GP33 tumor inoculation in Ly5.2+/C57BL/6 mice. a FACS analysis after tumor inoculation showed higher CD8+ T cell infiltration on day 4 after tumor inoculation in mice receiving ACT, and higher CD8+ T cell infiltration on day 14 in mice receiving memory T cell ACT. b Representative hematoxylin and eosin-stained sections of tumors resected on day 18 also demonstrated higher numbers of infiltrating lymphocytes after memory T cell ACT. c In contrast to effector T cell ACT, exogenously derived Ly5.1+/CD8+ T cell infiltration increased over time after memory T cell ACT. d No significant differences in endogenously derived Ly5.2+/CD8+ T cell infiltration is observed between effector and memory T cell ACT. These experiments are performed three times with similar results with four mice per group (*p < 0.05 vs. no immunotherapy; † p < 0.05 vs. effector T cell immunotherapy)
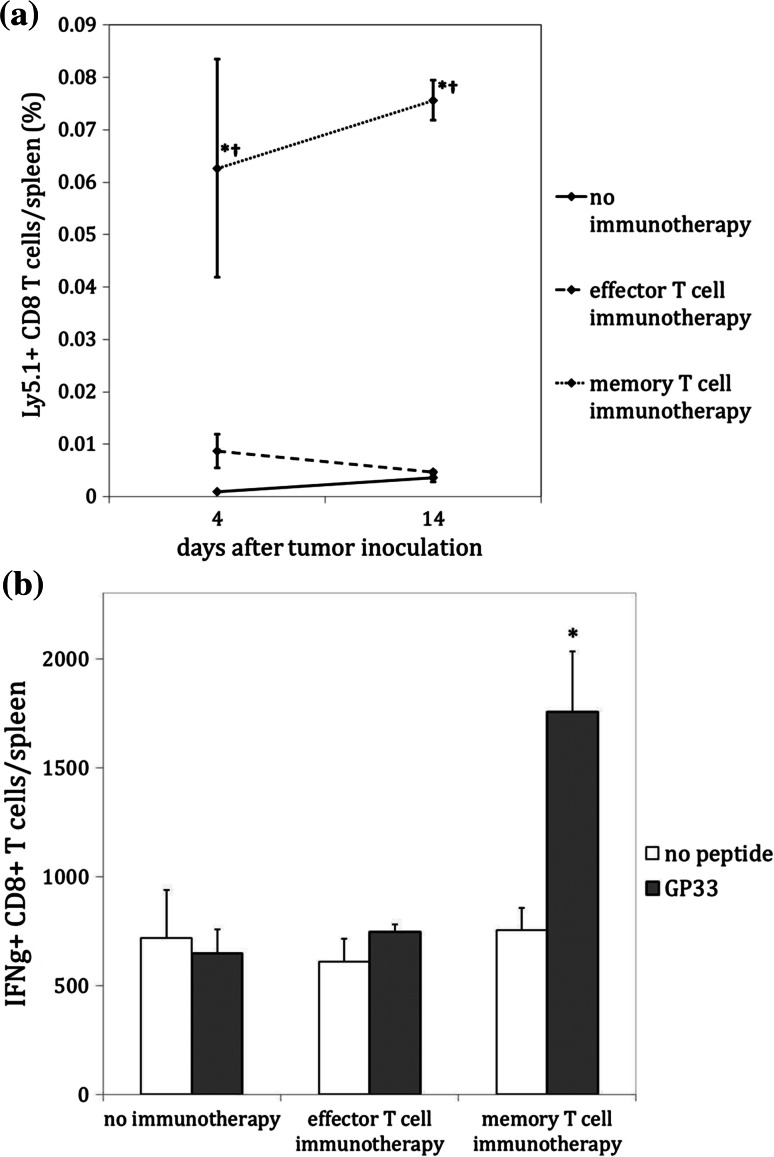
Memory CD8+ T cell-based ACT results in systemic CD8+ T cell responsiveness against tumor antigen
To compare the survival and persistence of circulating donor-derived CD8+ T cells following ACT immunotherapy, spleens were harvested from mice killed on days 4 and 14. Significantly more donor-derived Ly5.1+ CD8+ T cells were observed within the spleens of mice following memory T cell ACT as compared to effector T cell ACT (Fig. 5a). To determine whether effector or memory T cell-based ACT could promote systemic T cell responsiveness to tumor antigen, splenocytes harvested on day 4 were stimulated for 5 h with or without GP33 peptide in the presence of IL-2 and brefeldin A. GP33-specific CD8+ T cells were identified by flow cytometry based on intracellular levels of IFNγ expression. As shown in Fig. 5b, circulating GP33-specific CD8+ T cells were only detected in mice that had been treated with memory T cell-based ACT.
Fig. 5.
Memory T cell ACT results in a stronger systemic T cell response. In the same experiments described in Fig. 4, splenocytes are also harvested and analyzed by flow cytometry. a On days 4 and 14, significantly higher numbers of exogenously derived Ly5.1+/CD8+ T cells are measured in the spleens of mice treated with memory T cell ACT (*p < 0.05 vs. no immunotherapy; † p < 0.05 vs. effector T cell immunotherapy). b Splenocyte reactivity to GP33 on day 14 (as indicated by GP33 peptide-stimulated intracellular levels of IFNγ) is only observed in mice treated with memory T cell ACT. This experiment is performed three times with similar results with three mice per group (*p < 0.05 vs. no peptide)
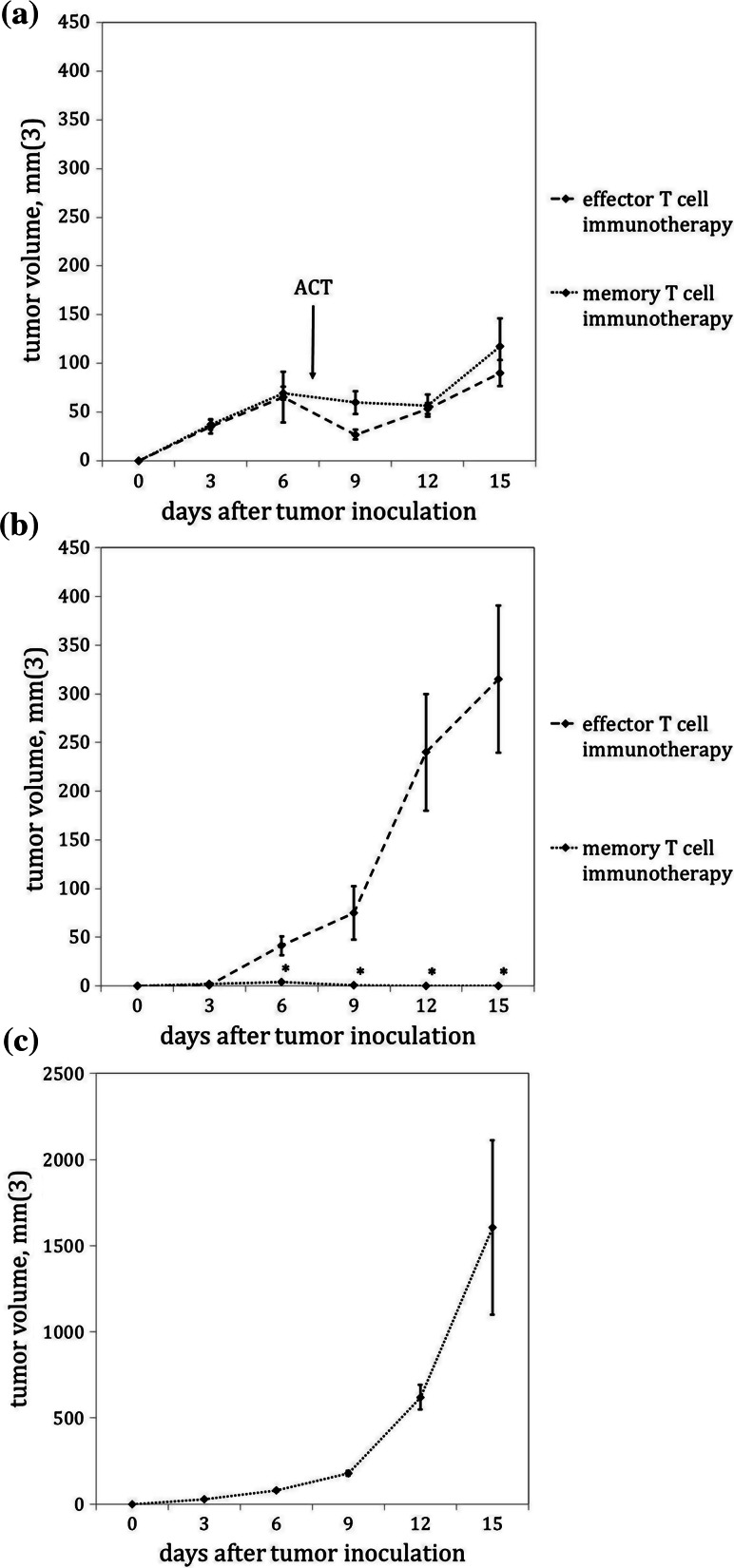
Memory CD8+ T cell-based ACT can promote long-lived tumor immunity
One theoretical immunotherapeutic advantage of using memory T cells for ACT is their ability to persist indefinitely and sustain tumor immunity. To test this possibility, mice received 5 × 105 GP33-specific CD8+ effector or memory T cells ACT on day 7 after B16GP33 melanoma inoculation, after which tumors were resected on day 15. Effector and memory T cell ACT were similar in their ability to transiently arrest the growth of established tumors (Fig. 6a). On day 25, mice were challenged with contralateral subcutaneous inoculation with B16GP33 melanoma. As shown in Fig. 6b, whereas challenge tumors grew exponentially in mice that had received effector T cell ACT, mice that had received memory T cell ACT were immune to B16GP33. This immunity appeared to be antigen specific, as subsequent challenge with parental B16F10 melanoma cells resulted in typical exponential tumor growth (Fig. 6c).
Fig. 6.
Neoadjuvant memory T cell ACT promotes durable tumor antigen-specific immunity. Ly5.2+/C57BL/6 mice are inoculated with 106 B16GP33 cells and then treated with ACT of 5 × 105 Ly5.1+/CD8+ GP33-specific effector or memory T cells on day 7. B16GP33 tumors are then surgically resected on day 15. a Effector and memory T cell ACT both resulted in inhibition of established B16GP33 tumors. b Whereas contralateral challenge B16GP33 tumors inoculated on day 25 grew exponentially in mice that had received effector T cell ACT, no growth of challenge B16GP33 tumors is seen in mice that had received memory T cells. c In contrast, parental B16F10 melanoma tumors that did not express GP33 grew exponentially in B16GP33-immune mice. These experiments are performed two times with similar results with four mice per group (*p < 0.05 between groups)
Discussion
The remarkable successes of checkpoint inhibitors like anti-CTLA-4 and anti-PD-1 monoclonal antibodies [23–29] have tempered enthusiasm for other T cell-based modalities of cancer immunotherapy, including ACT. One theoretical advantage that ACT could have over checkpoint inhibition would be in its antigenic specificity and the consequent avoidance of generalized autoimmune complications [30, 31]. Despite its promise, ACT immunotherapy would need to overcome the hurdles of treatment complexity involved with TIL isolation and expansion and pre-transfer lymphodepletion. We and others hypothesize that the clinical benefit of ACT immunotherapy can be magnified with the use of memory CD8+ T cells in place of effector CD8+ T cells. Our laboratory has previously found that in vivo exposure to melanoma drives effector CD8+ T cells toward accentuated apoptotic contraction, whereas the survival and function of memory CD8+ T cells is uniquely resistant to melanoma-induced suppression [20–22].
We observed that adoptive transfer of memory T cells was much more potent than the adoptive transfer of equal numbers of tumor antigen-specific effector T cells. Interestingly, memory T cells were not more effective at inhibiting melanoma cell growth than effector T cells in an in vitro co-culture setting, suggesting that there is no difference in their intrinsic cytotoxic or cytostatic activity. Rather, the presence of stronger TIL populations following memory T cell-based ACT suggests that this enhanced in vivo efficacy may be due to the induction of a more potent local antitumor immune response. Memory T cells are comprised of two subsets (TEM and TCM) according to their expression levels of CD62L [32]. It has been proposed that TCM may represent an optimal cell type for use in ACT [33, 34]. Despite the improved ability of TEM to traffic into peripheral tissues, we observed no clear differential inhibition of in vivo melanoma growth with CD62− TEM as compared to CD62L+ TCM.
Whereas effector T cell ACT was incapable of inducing measurable systemic T cell responsiveness to tumor antigen, CD8+ T cell reactivity to the melanoma antigen GP33 was observed among splenocytes following memory T cell ACT. When effector or memory T cell-based ACT was administered in a neoadjuvant manner prior to curative tumor resection, melanoma challenge experiments verified that only memory T cell-based ACT was capable of inducing durable tumor immunity. Notably, antigen-specific immunity was observed at late time points when donor-derived Ly5.1+ CD8+ T cells were no longer detectable in the spleen (data not shown). This suggests that the adoptive transfer of tumor-specific memory T cells eventually promoted the generation of endogenously derived tumor-directed T cell responses that were not seen after effector T cell ACT.
Taken together, these observations suggest that the adoptive transfer of tumor-specific memory T cells may cooperate with endogenous tumor-specific immune responses in a way that generates more potent influx of TIL, greater inhibition of tumor growth, tumor-specific responsiveness among circulating T cell populations, and tumor-specific immunity. Clinical immunohistochemical studies in colorectal adenocarcinoma, renal cell carcinoma, hepatocellular carcinoma, esophageal squamous cell carcinoma, and ovarian carcinoma reinforce the likelihood that tumoral infiltration by memory T cells may represent an optimal immune response to tumors [35–39]; indeed, an analysis of resected colorectal adenocarcinoma tumors found that the intratumoral presence of memory T cell infiltrates was a powerfully favorable prognostic predictor that outperformed traditional markers of disease biology such as tumor depth or presence of nodal metastases [40].
Previous studies have also compared the potential efficacy of effector and memory T cells as mediators of adoptive immunotherapy. A comprehensive body of work from the Surgery Branch of the National Cancer Institute has shown that ACT efficacy can be maximized with the use of less differentiated T cell subsets [13–19]. It has been reported that the use of T cell populations derived from naïve, resting T cells resulted in the strongest immunotherapeutic effect. However, the current study differs from this work in methodology and intent. To replicate protocols used in human ACT immunotherapy, the previous studies characterized tumor-infiltrating T cells as resting, effector, or memory phenotype based on flow cytometric characteristics. These cell populations then underwent potent in vitro activation and expansion protocols using stimulation with tumor lysates and IL-2, after which they were used for adoptive transfer [14–16]. As a result, it is likely that the initial differentiation state of these cell populations did not remain intact through this period of aggressive activation and expansion. In contrast, we wished to examine the local and systemic immunological consequences of direct in vivo encounter between these various T cell differentiation states and melanoma; the avoidance of post-isolation, pre-transfer T cell stimulation in our experimental protocol allowed us to precisely control the phenotype of tumor-specific T cells at the moment of antigen encounter in vivo.
Although our observations suggest that memory T cells may represent an optimal vehicle for ACT immunotherapy, a number of obstacles would need to be cleared in order for memory T cell-based immunotherapy to become a reality. The most obvious hurdle is that of identifying a source of memory T cells. Several analyses of TIL populations within explanted tumor specimens have verified the presence (and prognostic benefit) of memory T cells within intratumoral infiltrates [34–40]. However, it is unlikely that current methods of TIL isolation will produce quantities of memory T cells sufficient for use in ACT immunotherapy. Interestingly, several recent investigations have highlighted the possibility that in vitro stimulation of effector T cells with specific cytokines and inhibitors of glucose metabolism may promote memory T cell differentiation [41–50]. Our laboratory is presently investigating the possibility of using cytokine therapy to maximize the yield of CD8+ memory TIL either as a preconditioning regimen administered prior to tumor explantation or as a conditioning regimen to promote the expansion of isolated memory CD8+ T cells in vitro. We are also undertaking studies to determine the quantity of memory CD8+ T cells needed to produce levels of tumor inhibition comparable to those seen with the use of traditional effector CD8+ T cells.
Acknowledgments
This work was funded by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Biomedical Science Research and Development Service, CDA-2 and Merit Review Award (1I01BX001619-01A1) (Cho), by the generous support of Ronald and Patricia A Kissinger (Cho), University of Wisconsin Cellular and Molecular Pathology Training Program and National Institutes of Health (NIH) Grant T32 GM081061 (Contreras), and NIH Grant AI48785 (Suresh). The content is solely the responsibility of the authors and does not represent the views of the Department of Veterans Affairs or the United States Government or the National Institutes of Health.
Abbreviations
- ACT
Adoptive cell transfer
- LCMV
Lymphocytic choriomeningitis virus
Compliance with ethical standards
Conflict of interest
All authors have declared that there are no financial conflicts of interest with regard to this work.
References
- 1.Rosenberg SA, Yannelli JR, Yang JC, Topalian SL, Schwartzentruber DJ, Weber JS, Parkinson DR, Seipp CA, Einhorn JH, White DE. Treatment of patients with metastatic melanoma with autologous tumor-infiltrating lymphocytes and interleukin 2. J Natl Cancer Inst. 1994;86:1159–1166. doi: 10.1093/jnci/86.15.1159. [DOI] [PubMed] [Google Scholar]
- 2.Rosenberg SA, Dudley ME. Adoptive cell therapy for the treatment of patients with metastatic melanoma. Curr Opin Immunol. 2009;21:233–240. doi: 10.1016/j.coi.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosenberg SA, Yang JC, Sherry RM, Kammula UW, Hughes MS, Phan GQ, Citrin DE, Restifo NP, Robbins PF, Wunderlich JR, Morton KE, Laurencot CM, Steinberg SM, White DE, Dudley ME. Durable complete responses in heavily pretreated patients with metastatic melanoma using T-cell transfer immunotherapy. Clin Cancer Res. 2011;17:4550–4557. doi: 10.1158/1078-0432.CCR-11-0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dudley ME, Wunderlich JR, Yang JC, Sherry RM, Topalian SL, Restifo NP, Royal RE, Kammula U, White DE, Mavroukakis SA, Rogers LJ, Gracia GJ, Jones SA, Mangiameli DP, Pelletier MM, Gea-Banacloche J, Robinson MR, Berman DM, Filie AC, Abati A, Rosenberg SA. Adoptive cell transfer therapy following non-myeloablative but lymphodepleting chemotherapy for the treatment of patients with refractory metastatic melanoma. J Clin Oncol. 2005;23:2346–2357. doi: 10.1200/JCO.2005.00.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klebanoff CA, Khong HT, Antony PA, Palmer DC, Restifo NP. Sinks, suppressors and antigen presenters: how lymphodepletion enhances T cell-mediated tumor immunotherapy. Trends Immunol. 2005;26:111–117. doi: 10.1016/j.it.2004.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yee C. The use of endogenous T cells for adoptive transfer. Immunol Rev. 2014;257:250–263. doi: 10.1111/imr.12134. [DOI] [PubMed] [Google Scholar]
- 7.Murali-Krishna K, Altman JD, Suresh M, Sourdive DJ, Zajac AJ, Miller JD, Slansky J, Ahmed R. Counting antigen-specific CD8 T cells: a reevaluation of bystander activation during viral infection. Immunity. 1998;8:177–187. doi: 10.1016/S1074-7613(00)80470-7. [DOI] [PubMed] [Google Scholar]
- 8.Kaech SM, Wherry EJ, Ahmed R. Effector and memory T-cell differentiation: implications for vaccine development. Nat Rev Immunol. 2002;2:251–262. doi: 10.1038/nri778. [DOI] [PubMed] [Google Scholar]
- 9.Wherry EJ, Teichgräber V, Becker TC, Masopust D, Kaech SM, Antia R, von Andrian UH, Ahmed R. Lineage relationship and protective immunity of memory CD8 T cell subsets. Nat Immunol. 2003;4:225–234. doi: 10.1038/ni889. [DOI] [PubMed] [Google Scholar]
- 10.Sarkar S, Teichgräber V, Kalia V, Polley A, Masopust D, Harrington LE, Ahmed R, Wherry EJ. Strength of stimulus and clonal competition impact the rate of memory CD8 T cell differentiation. J Immunol. 2007;179:6704–6714. doi: 10.4049/jimmunol.179.10.6704. [DOI] [PubMed] [Google Scholar]
- 11.Joshi NS, Cui W, Chandele A, Lee HK, Urso DR, Hagman J, Gapin L, Kaech SM. Inflammation directs memory precursor and short-lived effector CD8(+) T cell fates via the graded expression of T-bet transcription factor. Immunity. 2007;27:281–295. doi: 10.1016/j.immuni.2007.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zimmermann C, Prevost-Blondel A, Blaser C, Pircher H. Kinetics of the response of naïve and memory CD8 T cells to antigen: similarities and differences. Eur J Immunol. 1999;29:284–290. doi: 10.1002/(SICI)1521-4141(199901)29:01<284::AID-IMMU284>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 13.Gattinoni L, Klebanoff CA, Palmer DC, Wrzesinski C, Kerstann K, Yu Z, Finkelstein SE, Theoret MR, Rosenberg SA, Restifo NP. Acquisition of full effector function in vitro paradoxically impairs the in vivo antitumor efficacy of adoptively transferred CD8+ T cells. J Clin Invest. 2005;115:1616–1626. doi: 10.1172/JCI24480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klebanoff CA, Gattinoni L, Tradbi-Parizi P, Kerstann K, Cardones AR, Finkelstein SE, Palmer DC, Antony PA, Hwang ST, Rosenberg SA, Waldmann TA, Restifo NP. Central memory self/tumor-reactive CD8+ T cells confer superior antitumor immunity compared with effector memory T cells. Proc Natl Acad Sci USA. 2005;102:9571–9576. doi: 10.1073/pnas.0503726102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hinrichs CS, Borman ZA, Cassard L, Gattinoni L, Spolski R, Yu Z, Sanchez-Perez L, Muranski P, Kern SJ, Logun C, Palmer DC, Ji Y, Reger RN, Leonard WJ, Danner RL, Rosenberg SA, Restifo NP. Adoptively transferred effector cells derived from naïve rather than central memory CD8+ T cells mediated superior antitumor immunity. Proc Natl Acad Sci USA. 2009;106:17469–17474. doi: 10.1073/pnas.0907448106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hinrichs CS, Borman ZA, Gattinoni L, Yu Z, Burns WR, Huang J, Klebanoff CA, Johnson LA, Kerkar SP, Yang S, Muranski P, Palmer DC, Scott CD, Morgan RA, Robbins PF, Rosenberg SA, Restifo NP. Human effector CD8+ T cells derived from naïve rather than memory subsets possess superior traits for adoptive immunotherapy. Blood. 2011;117:808–814. doi: 10.1182/blood-2010-05-286286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klebanoff CA, Gattinoni L, Palmer DC, Muranski P, Ji Y, Hinrichs CS, Borman ZA, Kerkar SP, Scott CD, Finkelstein SE, Rosenberg SA, Restifo NP. Determinants of successful CD8+ T-cell adoptive immunotherapy for large established tumors in mice. Clin Cancer Res. 2011;17:5343–5352. doi: 10.1158/1078-0432.CCR-11-0503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Klebanoff CA, Gattinoni L, Restifo NP. Sorting through subsets: which T-cell populations mediate highly effective adoptive immunotherapy? J Immunother. 2012;35:651–660. doi: 10.1097/CJI.0b013e31827806e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crompton JG, Sukumar M, Restifo NP. Uncoupling T-cell expansion from effector differentiation in cell-based immunotherapy. Immunol Rev. 2014;257:264–276. doi: 10.1111/imr.12135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Russ AJ, Wentworth L, Xu K, Seroogy CM, Rakhmilevich A, Sondel PM, Suresh M, Cho CS. Suppression of T-cell expansion by melanoma is exerted on resting cells. Ann Surg Oncol. 2011;18:3848–3857. doi: 10.1245/s10434-011-1667-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Russ AJ, Xu K, Wentworth L, Alam S, Meyers JV, Macklin MD, Rakhmilevich AL, Suresh M, Cho CS. Melanoma-induced suppression of tumor antigen-specific T cell expansion is comparable to suppression of global T cell expansion. Cell Immunol. 2011;271:104–109. doi: 10.1016/j.cellimm.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wentworth L, Meyers JV, Alam S, Russ AJ, Suresh M, Cho CS. Memory T cells are uniquely resistant to melanoma-induced suppression. Cancer Immunol Immunother. 2013;62:149–159. doi: 10.1007/s00262-012-1326-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mahvi DA, Meyers JV, Tatar AJ, Contreras A, Suresh M, Leverson GE, Sen S, Cho CS. CTLA-4 blockade plus adoptive T cell transfer promotes optimal melanoma immunity in mice. J Immunother. 2015;38:54–61. doi: 10.1097/CJI.0000000000000064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel JC, Akerley W, van den Eertwegh AJ, Lutzky J, Lorigan P, Vaubel JM, Linette GP, Hogg D, Ottensmeier CH, Lebbé C, Peschel C, Quirt I, Clark JI, Wolchok JD, Weber JS, Tian J, Yellin MJ, Nichol GM, Hoos A, Urba WJ. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–723. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prieto PA, Yang JC, Sherry RM, Hughes MS, Kammula US, White DE, Levy CL, Rosenberg SA, Phan GQ. CTLA-4 blockade with ipilimumab: long-term follow-up of 177 patients with metastatic melanoma. Clin Cancer Res. 2012;18:2039–2047. doi: 10.1158/1078-0432.CCR-11-1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Topalian SL, Sznol M, McDermott DF, Kluger HM, Carvajal RD, Sharfman WH, Brahmer JR, Lawrence DP, Atkins MB, Powderly JD, Leming PD, Lipson EJ, Puzanov I, Smith DC, Taube JM, Wigginton JM, Kollia GD, Gupta A, Pardoll DM, Sosman JA, Hodi FS. Survival, durable tumor remission, and long-term safety in patients with advanced melanoma receiving nivolumab. J Clin Oncol. 2014;32:1020–1030. doi: 10.1200/JCO.2013.53.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hamid O, Robert C, Daud A, Hodi FS, Hwu WJ, Kefford R, Wolchok JD, Hersey P, Joseph RW, Weber JS, Dronca R, Gangadhar TC, Patnaik A, Zarour H, Joshua AM, Gergich K, Elassaiss-Schaap J, Algazi A, Mateus C, Boasberg P, Tumeh PC, Chmielowski B, Ebbinghaus SW, Li XN, Kang SP, Ribas A. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med. 2013;369:134–144. doi: 10.1056/NEJMoa1305133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wolchok JD, Kluger H, Callahan MK, Postow MA, Rizvi NA, Lesokhin AM, Segal NH, Ariyan CE, Gordon RA, Reed K, Burke MM, Caldwell A, Kronenberg SA, Agunwamba BU, Zhang X, Lowy I, Inzunza HD, Feely W, Horak CE, Hong Q, Korman AJ, Wigginton JM, Gupta A, Sznol M. Nivolumab plus ipilimumab in advanced melanoma. N Engl J Med. 2013;369:122–133. doi: 10.1056/NEJMoa1302369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Couzin-Frankel J. Breakthrough of the year 2013: cancer immunotherapy. Science. 2013;342:1432–1433. doi: 10.1126/science.342.6165.1432. [DOI] [PubMed] [Google Scholar]
- 30.Weber JS, Dummer R, de Pril V, Lebbé C, Hodi FS, MDX010-20 Investigators Patterns of onset and resolution of immune-related adverse events of special interest with ipilimumab: detailed safety analysis from a phase 3 trial in patients with advanced melanoma. Cancer. 2013;119:1675–1682. doi: 10.1002/cncr.27969. [DOI] [PubMed] [Google Scholar]
- 31.Fecher LA, Agarwala SS, Hodi FS, Weber JS. Ipilimumab and its toxicities: a multidisciplinary approach. Oncologist. 2013;18:733–743. doi: 10.1634/theoncologist.2012-0483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roberts AD, Ely KH, Woodland DL. Differential contributions of central and effector memory T cells to recall responses. J Exp Med. 2005;202:123–133. doi: 10.1084/jem.20050137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fiorenza S, Kenna TJ, Comerford I, McColl S, Steptoe RJ, Leggatt GR, Frazer IH. A combination of local inflammation and central memory T cells potentiates immunotherapy in the skin. J Immunol. 2012;189:5622–5631. doi: 10.4049/jimmunol.1200709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang S, Gattinoni L, Liu F, Ji Y, Yu Z, Restifo NP, Rosenberg SA, Morgan RA. In vitro generated anti-tumor T lymphocytes exhibit distinct subsets mimicking in vivo antigen experienced cells. Cancer Immunol Immunother. 2011;60:739–749. doi: 10.1007/s00262-011-0977-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pages F, Kirilovsky A, Mlecnik B, Asslaber M, Tosolini M, Bindea G, Lagorce C, Wind P, Marliot F, Bruneval P, Zatloukal K, Trajanoski Z, Berger A, Fridman WH, Galon J. In situ cytotoxic and memory T cells predict outcome in patients with early-stage colorectal cancer. J Clin Oncol. 2009;27:5944–5951. doi: 10.1200/JCO.2008.19.6147. [DOI] [PubMed] [Google Scholar]
- 36.Hotta K, Sho M, Fujimoto K, Shimada K, Yamato I, Anai S, Konishi N, Hirao Y, Nonomura K, Nakajima Y. Prognostic significance of CD45RO + memory T cells in renal cell carcinoma. Br J Cancer. 2011;105:1191–1196. doi: 10.1038/bjc.2011.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cariani E, Pilli M, Zerbini A, Rota C, Olivani A, Pelosi G, Schianchi C, Soliani P, Campanini N, Silini EM, Trenti T, Ferrari C, Missale G. Immunological and molecular correlates of disease recurrence after liver resection for hepatocellular carcinoma. PLoS One. 2012;7:e32493. doi: 10.1371/journal.pone.0032493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Enomoto K, Sho M, Wakatsuki K, Takayama T, Matsumoto S, Nakamura S, Akahori T, Tanaka T, Migita K, Ito M, Nakajima Y. Prognostic importance of tumor-infiltrating memory T cells in oesophageal squamous cell carcinoma. Clin Exp Immunol. 2012;168:186–191. doi: 10.1111/j.1365-2249.2012.04565.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Webb JR, Milne K, Watson K, Deleeuw RJ, Nelson BH. Tumor-infiltrating lymphocytes expressing the tissue resident memory marker CD103 are associated with increased survival in high-grade serous ovarian cancer. Clin Cancer Res. 2014;20:434–444. doi: 10.1158/1078-0432.CCR-13-1877. [DOI] [PubMed] [Google Scholar]
- 40.Galon J, Costes A, Sanchez-Cabo F, Kirilovsky A, Mlecnik B, Lagorce-Pagès C, Tosolini M, Camus M, Berger A, Wind P, Zinzindohoué F, Bruneval P, Cugnenc PH, Trajanoski Z, Fridman WH, Pagès F. Type, density and location of immune cells within human colorectal tumors predict clinical outcome. Science. 2006;313:1960–1964. doi: 10.1126/science.1129139. [DOI] [PubMed] [Google Scholar]
- 41.Klebanoff CA, Finkelstein SE, Surman DR, Lichtman MK, Gattinoni L, Theoret MR, Grewal N, Spiess PJ, Antony PA, Palmer DC, Tagaya Y, Rosenberg SA, Waldmann TA, Restifo NP. IL-15 enhances the in vivo antitumor activity of tumor-reactive CD8+ T cells. Proc Natl Acad Sci USA. 2004;101:1969–1974. doi: 10.1073/pnas.0307298101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Le HK, Graham L, Miller CH, Kmieciak M, Manjili MH, Bear HD. Incubation of antigen-sensitized T lymphocytes activated with bryostatin 1 + ionomycin in IL-7 + IL-15 increases yield of cells capable of inducing regression of melanoma metastases compared to culture in IL-2. Cancer Immunol Immunother. 2009;58:1565–1576. doi: 10.1007/s00262-009-0666-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Huarte E, Fisher J, Turk MJ, Mellinger D, Foster C, Wolf B, Meehan KR, Fadul CE, Ernstoff MS. Ex vivo expansion of tumor specific lymphocytes with IL-15 and IL-21 for adoptive immunotherapy in melanoma. Cancer Lett. 2009;285:80–88. doi: 10.1016/j.canlet.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cha E, Graham L, Manjili MH, Bear HD. IL-7 + IL-15 are superior to IL-2 for the ex vivo expansion of 4T1 mammary carcinoma-specific T cells with greater efficacy against tumors in vivo. Breast Cancer Res Treat. 2010;122:359–369. doi: 10.1007/s10549-009-0573-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yang S, Dudley ME, Rosenberg SA, Morgan RA. A simplified method for the clinical-scale generation of central memory-like CD8+ T cells after transduction with lentiviral vectors encoding antitumor antigen T-cell receptors. J Immunother. 2010;33:648–658. doi: 10.1097/CJI.0b013e3181e311cb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pouw N, Treffers-Westerlaken E, Kraan J, Wittink F, ten Hagen T, Verweij J, Debets R. Combination of IL-21 and IL-15 enhances tumor-specific cytotoxicity and cytokine production of TCR-transduced primary T cells. Cancer Immunol Immunother. 2010;59:921–931. doi: 10.1007/s00262-010-0818-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sukumar M, Liu J, Ji Y, Subramanian M, Crompton JG, Yu Z, Roychoudhuri R, Palmer DC, Muranski P, Karoly ED, Mohney RP, Klebanoff CA, Lal A, Finkel T, Restifo NP, Gattinoni L. Inhibiting glycolytic metabolism enhances CD8+ T cell memory and anti-tumor function. J Clin Invest. 2013;123:4479–4488. doi: 10.1172/JCI69589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kaiser AD, Gadiot J, Guislain A, Blank CU. Mimicking homeostatic proliferation in vitro generates T cells with high anti-tumor function in non-lymphopenic hosts. Cancer Immunol Immunother. 2013;62:503–515. doi: 10.1007/s00262-012-1350-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Litterman AJ, Zellmer DM, LaRue RS, Jameson SC, Largaespada DA. Antigen-specific culture of memory-like CD8 T cells for adoptive immunotherapy. Cancer Immunol Res. 2014;2:839–845. doi: 10.1158/2326-6066.CIR-14-0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zoon CK, Seitelman E, Keller S, Graham L, Blevins TL, Dumur CI, Bear HD. Expansion of melanoma-specific lymphocytes in alternative gamma chain cytokines: gene expression variances between T cells and T-cell subsets exposed to IL-2 versus IL-7/15. Cancer Gene Ther. 2014;21:441–447. doi: 10.1038/cgt.2014.48. [DOI] [PMC free article] [PubMed] [Google Scholar]