Abstract
Diagnosis, treatment, response monitoring, and outcome of pediatric acute myeloid leukemia (AML) have made enormous progress during the past decades. Because AML is a rare type of childhood cancer, with an incidence of approximately seven occurrences per 1 million children annually, national and international collaborative efforts have evolved. This overview describes these efforts and includes a summary of the history and contributions of each of the main collaborative pediatric AML groups worldwide. The focus is on translational and clinical research, which includes past, current, and future clinical trials. Separate sections concern acute promyelocytic leukemia, myeloid leukemia of Down syndrome, and relapsed AML. A plethora of novel antileukemic agents that have emerged, including new classes of drugs, are summarized as well. Finally, an important aspect of the treatment of pediatric AML—supportive care—and late effects are discussed. The future is bright, with a wide range of emerging innovative therapies and with more and more international collaboration that ultimately aim to cure all children with AML, with fewer adverse effects and without late effects.
INTRODUCTION
Outcomes for children with acute myeloid leukemia (AML) have improved significantly over the past 30 years. During this time, multiple international cooperative groups have contributed to an evolving treatment strategy that consists of four to five courses of intensive myelosuppressive chemotherapy; stem-cell transplantation (SCT) is reserved for a subgroup of patients.1–3 Pediatric AML therapy challenges patients, families, and care providers because of a high incidence of severe and dose-limiting short- and long-term toxicities. Given that AML in children is relatively rare, with an incidence of approximately seven occurrences per 1 million children annually, multicenter clinical trials are required for continued progress to define new therapies and new approaches to ameliorate adverse effects. Achievements in pediatric oncology stem from a willingness to collaborate and coordinate research efforts. Starting in the 1980s and 1990s, several (inter-) national study groups formed with the common goal of improving outcomes among children with cancer through cooperative research.
Collaboration has evolved to encompass different approaches by different cooperative groups. The diversity in approaches allows cooperative groups to ask scientific questions in parallel, which provides multiple opportunities for innovation and validation. A brief history of each major cooperative group is summarized in Table 1, and major recent findings as published in literature are summarized in Table 2.4–16 As cooperative groups do more to integrate their efforts, it is important to examine and understand how each has grown, adapted, and evolved to find common ground in their interpretation of local and global data sets. This review summarizes important achievements in the field of pediatric AML and the lessons learned through both parallel and integrated international efforts.
Table 1.
Summary of the Major International Cooperative Groups
| Group | Year Established | No. of Institutions | Annual Accrual Estimate, No. of Patients | Comment |
|---|---|---|---|---|
| AIEOP | 1975 | 55 in Italy; 31 that care for children with AML | 55-60 | Over the years, AIEOP has been able to conduct prospective studies of autologous and allogeneic transplantations, one of which was randomized and made significant contributions to the field. |
| BFM-AML | 1976 | 69 | 110 | Initially, centers from the former West Germany participated in three studies. Since study AML-BFM 93 occurred, the centers of the former German Democratic Republic, all Austrian centers, and several Swiss centers joined the group; more centers from the Czech Republic and Slovakia also recently joined. Maintenance therapy and cranial irradiation have long been the standard of care, but this is now changing. Today, cranial irradiation is replaced by intensified intrathecal therapy in children without CNS involvement. |
| BSPHO | 1996 | 7 | 15 | Until 2003, BSPHO collaborated with approximately 20 sites in France and Portugal within the EORTC Children's Leukemia Group. Subsequently, BSPHO collaborated with DCOG on the DB AML-01 trial and now participates in the NOPHO-DBH consortium. |
| COG | 2001 | > 200 | 260 | To add to the de novo AML experience, COG recently completed a phase III trial in ML-DS and a phase III trial in APL. Though these represented rare diseases, COG sites enrolled 108 patients with APL in 3.6 years and 205 children with ML-DS in 5.5 years. |
| DCOG | 1972 | 6 | 25 | DCOG has collaborated with many other groups and currently joins the NOPHO-DBH consortium. The care of complex pediatric oncology care in the Netherlands will be concentrated to a single center (Princess Máxima Center for Pediatric Oncology), which thus permits the DCOG to implement standards of care and initiatives in toxicity research for all patients. |
| JPLSG | 2003 | 149 | 150 | Approximately 90% of the children with AML in Japan are treated at JPLSG sites. Because the national health care system prohibits off-label use of drugs, newagent studies focus on obtaining approval for marketing authorization so that novel therapies can be used in children. However, lack of legislation to encourage pharmaceutical companies for pediatric drug development is a major obstacle for newagent studies in Japan. |
| NCRI CCL SG | 2010 | 20 | 50 | Greater than 95% of children (< 16 years old) with AML are treated at one of 20 national centers in the United Kingdom and the Republic of Ireland. Funding of clinical trials is competitive and by application to a consortium of national charities, which favor randomized studies. Historically, the United Kingdom has treated children and adults within a combined AML trial. However, the next pediatric AML trial, MyeChild 01, will be an international United Kingdom, France, and Republic of Ireland collaboration. |
| NOPHO | 1982 | 22 | 45 | From 2008, all centers in Hong Kong participated in the AML2004 trial, and, in 2010, DCOG and BSPHO initiated a trial that was based on NOPHO-AML 2004. The cooperation with DCOG, BSPHO, and Hong Kong has resulted in the opening of a new de novo AML treatment study, NOPHO-DBH AML-2012, in 2013. |
| SFCE | 2000 | 28 | 38 | In France, until the end of the 80s, children with AML were treated according to adult AML protocols. At the beginning of 2000, LAME and EORTC groups joined the French academic society for pediatric cancer, SFCE. SFCE will join the MyeChild 01 study with the NCRI. |
| SJCRH | 1962 | 8 | 40 | St Jude Children's Research Hospital, funded by the American Lebanese Syrian Associated Charities, has conducted two randomized, multi-institutional trials since 2002. Investigators have also shown that antibacterial prophylaxis dramatically reduced the incidence of bacterial infection, decreased length of hospital stays, and could be safely administered by caregivers in the outpatient setting. |
Abbreviations: AIEOP, The Italian Association for Pediatric Hematology and Oncology; AML, acute myeloid leukemia; APL, acute promyeolytic leukemia; BFM-AML, The Berlin-Frankfurt-Münster AML Group; BSPHO, The Belgian Society of Paediatric Haematology and Oncology; COG, Children's Oncology Group; DBH, Dutch-Belgium-Hong Kong; DCOG, The Dutch Childhood Oncology Group; DDR, German Democratic Republic; EORTC, European Organisation for Research and Treatment of Cancer; I-BFM-SG, The International BFM Study Group; JPLSG, The Japanese Pediatric Leukemia/Lymphoma Study Group; LAME, Leucemie Aique Myeloide Enfant; ML-DS, myeloid leukemia of Down syndrome; NCRI CCL SG, The Leukaemia Subgroup of the National Cancer Research Institute Children's Cancer and Leukaemia Study Group; NOPHO, The Nordic Society of Pediatric Hematology and Oncology; SFCE , Société Française de lutte contre les Cancers et leucémies de l'Enfant et de l'adolescent; SJCRH, St Jude Children's Research Hospital.
Table 2.
Outcomes of Pediatric AML in Recent Collaborative Group Studies
| Study Group and Source | Study Acronym and Inclusion Time | No. of Patients | No. (%) of Patients Treated With SCT | Median ± SD EFS (%) | Median ± SD OS (%) | Relapse (%) | Source |
|---|---|---|---|---|---|---|---|
| AIEOP | AML2002/01 (2002-2011) | 482 | Allo-SCT: 141 (29) | 8-year: 55 ± 3 | 8-year: 68 ± 2 | 24 | Pession et al 201311 |
| Auto-SCT: 102 (21) | |||||||
| BFM-AML SG | AML-BFM 2004 (2004-2010) | 521 | 42 (8) | 5-year: 55 ± 2 | 5-year: 74 ± 2 | 29 | Creutzig et al 20136 |
| COG | AAML03P1 (2003-2005) | 340 | 73 (21) | 3-year: 53 ± 6 | 3-year: 66 ± 5 | 33 ± 6 | Cooper et al 20125 |
| AAML0531 (2006-2010) | 1,022 (ages 0-29 years) | NA | 3-year: 53 v ≥ 47 | 3-year: 69 v 65 | 33 v 41 | Gamis et al 20149 | |
| Japan | AML99 (2000-2002) | 240 | Allo-SCT: 41 (17) | 5-year: 62 ± 7 | 5-year: 76 ± 5 | 32 | Tsukimoto et al 200915 |
| Auto-SCT: 5 (2) | |||||||
| JPLSG | AML-05 (2006-2010) | 443 | 54 (12) | 3-year: 54 ± 2 | 3-year: 73 ± 2 | 30 | Tomizawa et al, Leukemia 201314 and Int J Hematol 201313 |
| MRC | MRC AML12 (1995-2002) | 564 | 64 (11) | 10-year: 54 | 10-year: 63 | 35 | Gibson et al 201110 |
| EORTC-CLG | EORTC 58,921 (1993-2002) | 177 | Allo-SCT: 39 (27) | 7-year: 49 ± 4 | 7-year: 62 ± 4 | Entz-Werle et al 20058 | |
| NOPHO | NOPHO AML 2004 (2004-2009) | 151 | 22 (15) | 3-year: 57 ± 5 | 3-year: 69 ± 5 | 30 | Abrahamsson et al 20114, Hasle et al 201216 |
| PPLLSG | PPLLSG AML-98 (1998-2002) | 104 | Allo-SCT: 14 (13) | 5-year: 47 ± 5 | 5-year: 50 ± 5 | 24 | Dluzniewska et al 20057 |
| Auto-SCT: 8 (8) | |||||||
| SJCRH | AML02 (2002-2008) | 216 | 59 (25) | 3-year: 63 ± 4 | 3-year: 71 ± 4 | 21 | Rubnitz et al 201012 |
Abbreviations: AIEOP, Italian Association for Pediatric Hematology and Oncology; Allo, allogeneic; AML, acute myeloid leukemia; Auto, autologous; BFM SG, Berlin-Frankfurt-Munster Study Group; CLG, Children's Leukemia Group; COG, Children's Oncology Group; EFS, event-free survival; EORTC, European Organisation for Research and Treatment of Cancer; Japan, Japanese Childhood AML cooperative study; JPLSG, The Japanese Pediatric Leukemia/Lymphoma Study Group; MRC, Medical Research Council; NA, not available; NOPHO, Nordic Society for Pediatric Hematology and Oncology; OS, overall survival; PPLLSG, Polish Pediatric Leukemia/Lymphoma Study Group; SD, standard deviation; SCT, stem-cell transplantation; SJCRH, St Jude Children's Research Hospital.
PROGNOSTIC FACTORS AND RISK-GROUP STRATIFICATION
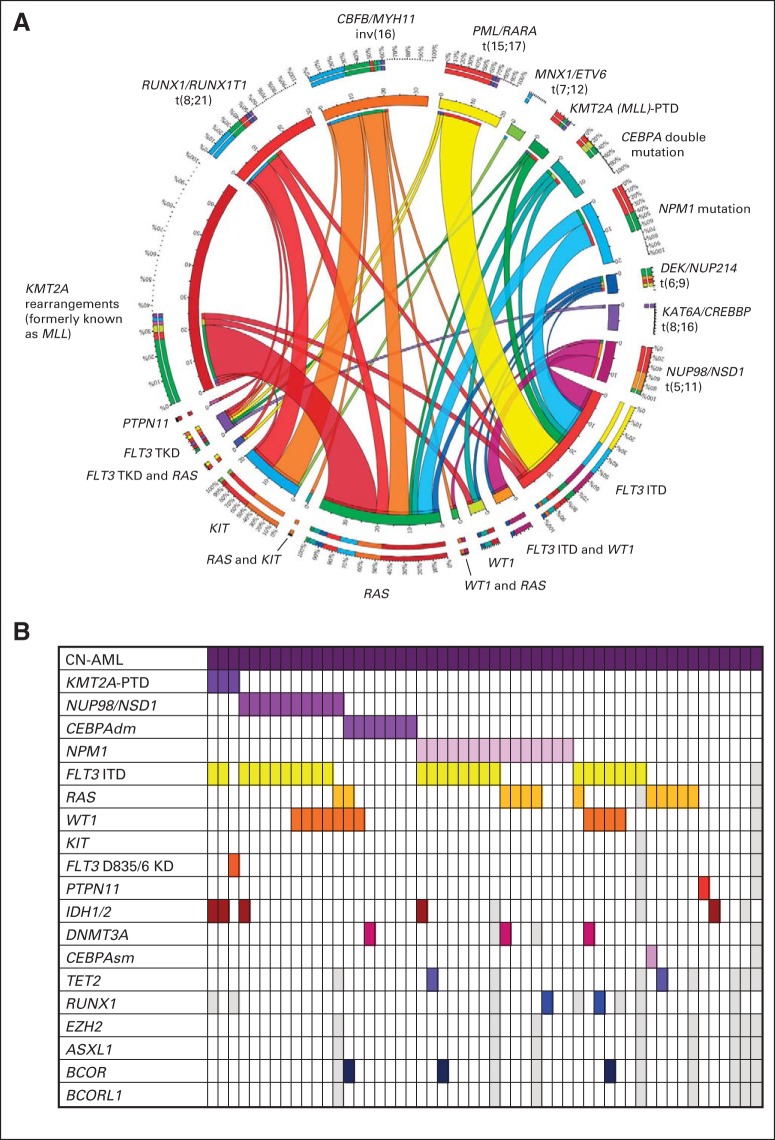
There is general agreement across groups about the definition of high-risk (HR) AML. Groups differ in the use of low, standard, and intermediate risks to designate all other types of AML. For the purposes of this review, disease in all patients with non-HR AML will be called standard-risk (SR) AML. Novel data from the genomic era show that only a limited number of gene mutations are required for AML pathogenesis compared with solid tumors,17 but their spectrum may be broader than the class I (proliferative) and class II (blocking) mutations postulated by Kelly and Gilliland18 as required in AML pathogenesis. Figure 1 summarizes many of the novel insertion and deletion events recently identified through next-generation sequencing approaches as well as the well-known large translocation events. As a result of efforts in sequencing and cytogenetics, new molecular subsets have been identified through independent and combined data analysis across cooperative groups. Intergroup validation of disease markers is key to building confidence in the true prognostic impact of the marker. This section will not review all genetic events in AML but will focus on those identified across different groups.
Fig 1.
(A) Distribution of genetic abnormalities in pediatric acute myeloid leukemia (AML). Collaborating type I and type II mutations in pediatric AML. The circos plot depicts the frequency of the type II mutations and co-occurrence of type I mutations in patients with de novo pediatric AML. The length of the arch corresponds with the frequency of the type II mutation, and the width of the ribbon corresponds with the percentage of patients who have a specific type I mutation or combination of type I mutations. (B) Overview of co-occurring mutations in pediatric cytogenetically normal (CN) AML (N = 53). Each column represents a single occurrence. A colored field means that the occurrence is positive for a mutation or translocation in the corresponding gene(s). A white field indicates that the occurrence tested negative for a mutation or translocation in the corresponding gene(s). A gray field indicates an occurrence that could not be tested for mutations in the corresponding gene. dm, double mutations; ITD, internal tandem duplication; PTD, partial tandem duplication; sm, small mutations.
The core-binding factor (CBF) mutations—inversion16(p13;1q22), t(16;16)(p13;q22), and t(8;21)(q22;q22)—are recognized by all study groups as markers of SR AML. A recent North American and European collaboration confirmed that mutations in the nucleophosmin1 gene (NPM1)19,20 and CEBPα gene also predict a favorable prognosis.21–23 Including CBF, NPM1, and CEBPα mutations, the consensus SR group now comprises roughly 30% to 40% of patients with childhood AML, which is considerably larger than in adult AML.24
Among the common markers of HR disease are the FLT3 mutations, a family that includes internal tandem duplications (FLT3/ITD) and point mutations in the kinase domain (FLT3/KD). FLT3/ITDs occur in approximately 10% to 20% of pediatric AML occurrences, and there is a wealth of data on their significance as a poor prognostic marker.25,26 Approximately 10% of FLT3 mutations are either gained or lost at relapse, which suggests that FLT3 mutations can be late subclonal events, and they are not always the driver of prognosis and response.27,28 However, the reports of secondary resistance mutations after treatment with FLT3 inhibitors suggests that these are indeed driver mutations.29 The prognostic significance and biologic role of FLT3/KD mutations is less clear.30
Although FLT3/ITD, monosomy 7, and monosomy 5 are longstanding traditional markers of HR disease, the prognostic impact of KMT2A (previously known as MLL) rearrangements (which occur in 20% to 24% of all patients with childhood AML) has only recently been clearly defined. KMT2A is notoriously promiscuous and has more than 120 translocation partners described.31,32 A recent large, retrospective effort from 11 international groups included data from greater than 750 pediatric patients with KMT2A-rearranged AML and showed that the translocation partner predicts clinical outcome. AML with t(1;11)(q21;q23) was rare but did exceptionally well, whereas disease with t(6;11)(q27;q23), t(10;11)(p12;q23), or t(10;11)(p11.2;q23) had a dismal outcome.31
Repetitive rearrangements that involve NUP98 have been identified in European and North American cohorts. The cryptic translocation NUP98/NSD1 occurs in 15% of patients with cytogenetically normal AML and is associated with a high frequency of FLT3 mutations and a dismal outcome.33,34 In a collaborative effort, North American and European groups also identified NUP98/JARID1A in acute megakaryoblastic leukemias (AMKL).35 This differs from the well-known t(1;22)(p13;q13) translocation, which results in the RBM15/MLK1 fusion product that is mainly present in infants with AMKL.36,37 The recently describedCBFA2T3/GLIS2 fusion transcript, found both in non–Down syndrome AMKL and in other AML subtypes, confers a poor outcome in North American and European cohorts.38,39 As a consequence of these findings, a large international cooperative effort has been established for genome-wide analysis of AMKL.
Infants with AML can also be characterized by a translocation t(7:12)(q36;p13), which is a recurrent translocation involving the MNX1/ETV6 gene in AML. This abnormality is associated with poor outcome.40 Recently, other ETV6 abnormalities in both European and North American cohorts were reported at scientific meetings, but these data are not published yet.
The t(6;9)(p22;q34) and the t(8;16)(p11;p13) translocations predict a poor prognosis across cooperative groups. A fusion between the DEK and NUP234 genes results from t(6;9)(p22;q34) translocation. This abnormality occurs in older children and has a poor clinical outcome, which may improve with SCT.41,42 The t(8;16)(p11;p13) translocation may have an age-dependent impact on prognosis and fuses KAT6A to the CREBBP gene. In very young children (28% of patients are diagnosed in the first month of life), this translocation is associated with spontaneous remission and warrants a watch-and-wait strategy before initiation of chemotherapy. Older children require intensive chemotherapy.43
Despite these findings, there is not always consistency across groups. NPM1 mutations may occur concurrent with FLT3/ITD. The Medical Research Council (MRC) results suggest that the NPM1 mutation with FLT3/ITD predicts a poor prognosis.44,45 Others have shown that the presence of an NPM1 mutation may abrogate the negative effects of FLT3/ITD.19,46 Mutations in WT1 have yielded variable outcome reports from Europe (poor prognosis) and North America (no prognostic impact).47,48 In Europe, rare structural abnormalities in EVI1 failed to demonstrate prognostic significance.49,50 However, in a Japanese series, EVI1 gene expression was related to outcome, especially in patients with KMT2A/AF9 rearrangements.51 Although chromosome 7 abnormalities have long been considered a poor prognostic marker, Hasle et al52 performed a large retrospective study that demonstrated that monosomy 7 has a worse outcome than del7q.
RAS pathway mutations are present in approximately 20% of pediatric patients with AML and mainly occur in KMT2A-rearranged cases, and AML with inv(16) and NPM1-mutated AML.53,54 NRAS mutations (8%) and KRAS mutations (13%) are the most common RAS pathway mutations.53,55 To date, RAS mutations are not associated with a prognostic influence or response to therapy in either North American or European cohorts. However, this should not preclude the study of MEK inhibitors for RAS pathway–mutated AML.56,57
RESPONSE ASSESSMENT AND RISK ASSIGNMENT
Minimal residual disease (MRD), as defined by multidimensional flow cytometry after induction chemotherapy in AML,58,59 is prognostic in childhood AML and predicts relapse risk.60–62 Most groups use a combination of genetic abnormalities and response as detected with multidimensional flow cytometry to allocate patients to HR treatment, which includes the need for SCT. Monitoring of MRD by molecular markers (eg, fusion genes, mutations) is currently being standardized in Europe by several cooperating reference laboratories. These methods may allow enhanced MRD detection and early identification of a molecular relapse.38,62,63
PROSPECTIVE COLLABORATIVE CLINICAL TRIALS AND STANDARD THERAPEUTIC APPROACH
Several cooperative groups have recently published single-arm or randomized clinical trials in childhood AML, as summarized in Table 2. Collaboration among cooperative groups has led to rapid accrual to randomized trials, and the coordinated efforts of multiple cooperative group studies permits a validation and comparison of results so that the best therapies may be assimilated into future trial designs. As we begin to apply targeted therapies to patients in increasingly smaller subsets of molecularly defined disease, coordination of research questions across cooperative groups becomes even more critical. In this section, the collective work to define a standard therapeutic approach to childhood AML is discussed.
Induction Treatment: Randomized
Type of anthracycline.
A Berlin-Frankfurt-Munster Acute Myeloid Leukemia (BFM-AML) study demonstrated a trend toward improved early treatment response with idarubicin (IDA) compared with daunorubicin (DNR), but overall survival (OS) was similar in both arms.64 In a subsequent study, this group compared liposomal DNR (DNX) and IDA and observed decreased treatment-related mortality with DNX, despite a dose increase from 60 to 80 mg/m2 per dose. OS was similar in both arms, but event-free survival (EFS) was significantly better within patients who were t(8;21) positive and treated with DNX.6 MRC AML12 compared mitoxantrone (Mitox) to DNR during induction. Mitox resulted in improved disease-free survival (DFS) but no difference in EFS and OS.10 The European Organisation for Research and Treatment of Cancer (EORTC) and Leucemie Aique Myeloide Enfant (LAME) reported enhanced DFS with Mitox and IDA compared with DNR.65
Cumulative dose of anthracyclines at induction.
In adults with AML, higher doses of DNR are associated with improved survival.66,67 The BFM-AML Study Group currently employs a high dose of DNX (three doses at 80 mg/m2) without undue toxicity.6 However, the risk of cardiac toxicity at increasing cumulative doses of DNX in children is still largely unknown. In general, children are at higher risk for anthracycline-induced cardiotoxicity at lower threshold doses than adults.68 MRC AML15 results suggest that consolidation with high-dose cytarabine and no anthracyclines is effective.69Thus, it may be possible to reduce cumulative anthracycline doses by intensifying anthracyclines in induction and omitting them from consolidation.
Cytarabine and additional drugs.
In adult AML, it seems that high-dose cytarabine at induction improves outcome.70,71 In children, several international trials have studied high-dose cytarabine with variable results.12,72,73 However, in each, other differences in treatment approach prevent a firm conclusion about the benefit of high-dose versus low-dose cytarabine. Nonetheless, there is no doubt about the usefulness of cytarabine combined with an anthracycline.
The addition of a third drug is not as clear. A recent, retrospective, large cohort study in pediatric patients with AML positive for t(8;21)(q22:q22) showed that a higher cumulative dose of etoposide was associated with better outcome, but this finding has not been published yet. Moreover, several recent, large, randomized trials in adults and children demonstrated the benefit of added gemtuzumab ozogamicin to conventional chemotherapy at induction treatment.9,74–76 In contrast, study MRC AML15 did not show superiority of the addition of etoposide to DNR and cytarabine in adults.69 Several groups continue to address these questions in randomized studies.
Consolidation Chemotherapy
Number of courses.
It needs to be stressed that many questions about consolidation are dependent on the quality of remission from induction chemotherapy, which makes it difficult to draw conclusions that can be generalized. Many study groups now routinely apply five courses of chemotherapy in total, with three consolidation courses. However, there is no high-level evidence to support this approach. In fact, study MRC AML15 showed primarily in adults that four courses (two each of induction and consolidation) are equally effective as five.69 The Japanese group reported that a reduction of the number of consolidation courses could be done without affecting outcome, but the group still administered at least five cycles of consolidation therapy.15,77 For patients with inv(16), both the MRC trials and the BFM-AML studies have shown excellent outcomes with four courses of chemotherapy.73,78 Indeed, in adults, Burnett et al69 reported that patients who had been treated with IDA-FLAG (fludarabine, cytarabine, and granulocyte colony-stimulating factor [G-CSF]) twice for induction only—without any consolidation—had outcomes similar to those treated with conventional ADE (cytarabine, DNR, and etopside) and consolidation.
Use of high-dose cytarabine as single-agent compared with combination chemotherapy.
The use of single-agent high-dose cytarabine in consolidation has been addressed in only one randomized study. In adult patients, high-dose cytarabine was equally effective in consolidation to MidAC/MACE (Mitox and cytarabine/amsacrine, cytarabine, and etopside) but required less supportive care. Only in the minority of patients with adverse cytogenetics did MidAC/MACE consolidation seem superior.69
Maintenance Treatment
Two studies assessed maintenance chemotherapy in pediatric AML, but neither demonstrate a benefit.79,80 In fact, both studies suggested a lower salvage rate from relapse if maintenance therapy had been applied. Other modalities for maintenance therapy concern more immunotherapy-like approaches. An example is interleukin-2, which failed to show a benefit in DFS.81 The BFM-AML group has applied conventional 1-year maintenance chemotherapy for decades, and overall results are similar to other groups that do not use maintenance. AML-BFM 2012 will randomly assign patients to receive maintenance to assess benefit and the possibility that certain molecular subsets may benefit. Maintenance post-SCT is another area in which more clinical research can be performed. Children's Oncology Group (COG) is evaluating the potential benefit of maintenance with an FLT3 inhibitor to prevent relapse.
CNS Prophylaxis and Treatment
Unlike the established approach in acute lymphocytic leukemia (ALL), there are little clinical data to support an optimal approach to CNS prophylaxis in patients with AML. In general, CNS relapse does occur, either isolated or as part of a combined relapse that usually involves the bone marrow. The International BFM Study Group (I-BFM-SG) study, Relapsed AML 2001/01, demonstrated that nearly 10% of patients had CNS involvement at relapse.82 When CNS prophylaxis is not used, CNS involvement at relapse may be as high as 20%, which suggests the benefit of prophylaxis.83 Moreover, the incidence of AML cells in the CSF in children with newly diagnosed AML has been reported to be as high as 30%,84 which also favors some sort of CNS-directed treatment at initial diagnosis. Most if not all pediatric study groups are administering prophylactic intrathecal chemotherapy and have moved away from cranial radiation. A St Jude study demonstrated that, even when CNS leukemia is present at initial diagnosis, systemic and intrathecal chemotherapies are sufficient.85 However, there have been no randomized studies to define the optimal intrathecal chemotherapy. Clinical observations reported by the St Jude group suggest that triple-intrathecal chemotherapy may provide benefit over single-agent cytarabine.86 With improved systemic control of AML, the prophylaxis and treatment of CNS disease becomes a more and more important area of clinical research.
SCT
Consensus on the role of SCT in first complete remission (CR) for children with AML has led to much debate.87,88 Historical comparisons of outcomes are difficult because of differences in intensity of chemotherapy before SCT. Although a meta-analysis provides evidence of the antileukemic efficacy of the transplantation procedure,89 the benefit needs to be balanced against procedure-related mortality and OS benefit.90 Recently, several authors have readdressed the issue of SCT in CR1.90,91 It is clear that that transplantation-related mortality has decreased and that the difference between related and unrelated donors is no longer evident.91 A recent paper from St Jude once more provided evidence for the graft-versus-leukemia effect that is more evident in AML than in ALL.92 In both Europe and North America, there is broad support for SCT in patients in high–relapse-prone molecular subsets and in those who have positive residual disease after induction. The benefit for SCT in specific molecular subsets of AML is not known, however. Moreover, most study groups advocate SCT in second CR, although the concept has never been challenged formally.80,82,93,94
PLANNED AND ONGOING CLINICAL TRIALS
In Table 3, the planned and ongoing clinical trials from the various collaborative groups are summarized. Of interest, several European groups have developed collaborative studies to increase accrual and permit randomized comparisons. The I-BFM-SG is working toward a pan-European backbone for all patients in an effort to standardize approaches and to permit intergroup comparisons and clinical studies in small subgroups. In its last three trials, COG has adopted an approach close to that of the MRC.
Table 3.
Overview of Ongoing or Pending Clinical Trials in Newly Diagnosed AML, Including Main Study Questions and Primary End Points
| Group | Years of Accrual | Sample Size, No. of Patients | Age Range, Years | Primary Design and Objective(s) | Primary End Point(s) | Secondary Objectives |
|---|---|---|---|---|---|---|
| AIEOP | 2015-2018 | 250 | 018 | FLADx versus ICE as second induction course for reducing end of induction MRD; FLAMSA in place of autologous SCT in patients with intermediate-risk disease as third consolidation | End of induction BM MRD < 0.1%; LFS | To validate the new stratification criteria (SR, IR, HR); to reduce anthracycline dosage in SR patients; to compare MRD using MDF versus PCR |
| BFM-AML | 2014-2019 | 500 | 0 to < 19 | Random assignment to clofarabine, cytarabine, and DNX versus ADxE in induction I; random assignment to maintenance therapy | EFS of randomly assigned patients; EFS from second random assignment | To implement a molecular and MRD-based risk classification; to assess safety of novel therapies in combination with chemotherapy; o identify early molecular relapse by MRD monitoring in peripheral blood |
| COG | 2010-2016 | 1,050-1,250 | 0 to < 30 | Random assignment: standard MRC-based therapy with or without bortezomib; a nonrandomized stratification of patients positive for FLT3-ITD to chemotherapy plus sorafenib | EFS; OS To assess MRD response with intensification of induction II for patients positive by MRD at the end of induction I; to assess OS, DFS, RR with sorafenib in patients with FLT3-ITD and with best donor allogeneic SCT | |
| JPLSG | 2014-2018 | 300 | 0 to < 19 | Random assignment of high-dose cytarabine induction versus standard-dose cytarabine induction | EFS; MDF BM MRD after initial induction | To improve overall outcome; to achieve similar or decreased early mortality and death in CR1; to improve outcome of molecular subgroups; to compare WT1 transcript MRD versus MDF MRD |
| NCRI-UK and SFCE MyeChild 01 | 2015-2020 | Up to 700 | 0 to < 18 | Random assignment (R1) of mitoxantrone versus DNX in induction; random assignment (R2) of a single dose of GO 3 mg/m2 versus the maximum tolerated number of doses (max 3, as identified by a dose-finding study) combined with induction; random assignment (R3) of HD cytarabine versus FLA in consolidation for patients with SR disease; random assignment (R4) of MAC versus RIC for patients with HR disease undergoing HSCT | R1/2: EFS; R3: RFS; R4: RFS, incidence at day 100 post-transplantation of grade 3-5 toxicity | To compare the predictive value of flow and molecular MRD monitoring for relapse risk |
| NOPHO-DBH AML-2012 | 2013-2019 | 300-350 | 0 to < 19 | Random assignment of DNX versus mitoxantrone in induction I; random assignment of FLADx versus ADxE in induction II | MRD in BM on day 22, course I; MRD in BM on day 22 from start of course II | To estimate survival by MRD-based stratification; to assess early mortality and death in CR1; to compare qPCR for fusion gene transcripts versus MDF in assessment of MRD |
| SJCRH | 2008-2016 | 240 | 0 to < 21 | Random assignment of cytarabine, daunorubicin, and etoposide versus clofarabine and cytarabine in induction | MRD by MDF on day 22 of induction I | To estimate EFS of chemotherapy versus chemotherapy followed by natural killer cell transplantation |
Abbreviations: ADxE, cytarabine, liposomal daunorubicin, and etoposide; AIEOP, Italian Association for Pediatric Hematology and Oncology; BFM, Berlin-Frankfurt-Munster; BM, bone marrow; CIR, cumulative incidence of relapse; COG, Children's Oncology Group; CR1, first complete remission; DBH, Dutch-Belgium-Hong Kong; DFS, disease-free survival; DNX, liposomal daunorubicin; ECM, HD cytarabine, etoposide, and mitoxantrone; EFS, event-free survival; FLA, fludarabine and cytarabine; FLADx, fludarabine, cytarabine, and liposomal daunorubicin; FLAMSA, fludarabine, cytarabine, and amsacrine; GO, gemtuzumab ozogamicin; HD, high dose; HR, high risk; HSCT, hematopoietic stem cell transplantation; ICE, idarubicin, cytarabine, and etoposide; IR, intermediate risk; JPLSG, Japanese Pediatric Leukemia/Lymphoma Study Group; LFS, leukemia-free survival; MAC, myeloablative conditioning; MDF, multidimensional flow cytometry; MRC, Medical Research Council; MRD, minimal residual disease; NCI CTCAE, National Cancer Institute Common Terminology Criteria for Adverse Events; NCRI-UK, National Cancer Research Institute-United Kingdom; RIC, reduced intensity conditioning; NOPHO, Nordic Society for Pediatric Hematology and Oncology; OS, overall survival; (q)PCR, (quantitative) polymerase chain reaction; R, response; RFS, relapse-free survival; RR, relapse rate; SCT, stem-cell transplantation; SFCE, Société Française de lutte contre les Cancers et leucémies de l'Enfant et de l'adolescent; SJCRH, St Jude Children's Research Hospital; SR, standard risk; WT1, Wilms tumor 1.
SEPARATE TREATMENT PROTOCOLS FOR SPECIFIC SUBGROUPS OF PEDIATRIC AML
Acute Promyelocytic Leukemia
The GIMEMA-AIEOP AIDA0493 trial treated all children with acute promyelocytic leukemia (APL) with all-trans-retinoic acid (ATRA) and IDA in induction, and patients were randomly assigned to no maintenance, maintenance with chemotherapy and ATRA, or ATRA alone. The OS at 10 years was 89%, which set a new benchmark for pediatric AML95 and helped define ATRA as standard in induction. INT0129, the first North America Intergroup trial in APL, demonstrated an 81% complete response rate in children who received ATRA alone for induction and a DFS of 48% for patients who received ATRA in induction and/or maintenance, versus 0% for patients who received chemotherapy with no ATRA.96 The International Consortium on Childhood APL Study 01 (ICC APL01) is studying ATRA at induction, consolidation, and maintenance. ICC APL01 has recently been closed for enrollment of patients with SR disease. With the demonstration that single-agent arsenic trioxide (ATO) had significant activity in relapsed97 and newly diagnosed APL,98 the Italian-German adult cooperative group initiated a randomized trial in adult patients with SR APL of ATO-ATRA versus ATRA, IDA, Mitox, methotrexate, and mercaptopurine. The 2-year EFS in the ATO-ATRA group was 97% compared with 86% in the ATRA chemotherapy combination group (P = .02 for superiority).99 COG investigators recently reported at scientific meetings the favorable safety and tolerability of ATO in combination with conventional chemotherapy, but data are still unpublished. COG and ICC-APL (under the umbrella of I-BFM-SG) are planning similar but not identical trials in children. It is expected that, with the introduction of ATRA and ATO, APL will be curable in a vast majority of patients without the need to apply chemotherapy. These trials should not only independently confirm the promising results from the adult trials but also analyze the safety and toxicities of this combination in children.
Myeloid Leukemia of Down Syndrome
Myeloid Leukemia of Down syndrome (ML-DS) is a unique disease entity and is characterized by individual mutations in the GATA1 transcription factor in the leukemic clone. Patients with ML-DS require dose-reduced treatment protocols without SCT.100,101 In fact, improvements in EFS and OS have been observed with therapy reductions in several independent cooperative group studies.100,102,103 Recent collaborative efforts are directed toward identification of risk groups by making use of GATA1 MRD and other genomic markers. In children with ML-DS, the current dose-adapted protocol of an I-BFM-SG study aims to provide an OS of greater than 85%. A total of 150 children should be enrolled by the end of 2015. In parallel, the protocol recommendations have been applied to children in greater than 20 countries in Europe, Asia, and South America. The promising experiences supported the ongoing development of an international prospective clinical trial that is based on an MRD-guided stratification. COG recently completed an analysis of the AAML0431 study. With a 25% reduction in total anthracycline dose and a reduction in the number of intrathecal treatments from seven to two, the 3-year DFS rate was 93.5% in patients with SR disease (age < 4 years and MRD negative at the end of induction 1), and it was 70.6% in patients who were MRD positive at the end of induction 1. These results compare favorably to the predecessor Children's Cancer Group study despite the dose reduction.101 At relapse, ML-DS loses the chemosensitive phenotype, which remains poorly understood to date.104
TREATMENT FOR RELAPSED AML
Treatment outcome at relapse is dependent on cytogenetics and the interval between diagnosis and relapse.82,105 These factors are not independent from each other; patients classified as good risk tend to experience relapse later than patients classified as poor risk in their initial treatment period. Several reports showed the poor outcome of relapsed AML in general, despite intensive reinduction and SCT.80,105–110 The current concept of treatment is intensive reinduction with one or two courses followed by SCT once in CR or in aplasia.80 The I-BFM-SG study Relapsed AML 2001/01 was developed in 1999 to study the optimal remission reinduction regimen for relapsed AML. At that time, several groups used high cumulative doses of anthracyclines at initial diagnosis, and it was not clear whether anthracyclines would be beneficial in reinduction at relapse. Therefore, the study randomly assigned patients to FLAG or FLAG plus DNX. The study showed that early treatment response improved when DNX was added to conventional chemotherapy.82 OS did not improve for the total group of patients, but the study was not powered to demonstrate that. Of interest, OS improved significantly for the subgroup of patients with CBF AML. Relapsed AML 2001/01 also showed the prognostic significance of early treatment response in pediatric patients with relapsed AML.111 Although the I-BFM-SG has chosen to run large, randomized studies of pediatric AML, relapsed AML in COG is considered an indication for studies with experimental agents. It would be beneficial, however, if consensus could be reached on a transatlantic platform for reinduction to which novel agents could be added to expedite recruitment. However, DNX, the favorite anthracycline in relapsed AML in Europe, is not registered in North America, which hampers this approach.
NEW AGENT STUDIES
Drug development is typically achieved through collaborative study groups or consortia, such as Innovative Therapies for Children with Cancer, Therapeutic Advances in Childhood Leukemia, I-BFM-SG, and COG. With the exception of gemtuzumab ozogamicin in Europe, however, no new drugs were licensed for AML in the recent past. A more detailed summary of potential new agents was recently published elsewhere.112,113 Table 4 summarizes some of the major classes and findings.9,29, 108,114–135
Table 4.
Novel Drugs and Treatment Modalities Relevant in Pediatric AML
| Drug by Modality | Comments |
|---|---|
| Chemotherapy | |
| Clofarabine | Safely combined with conventional chemotherapy in relapse, but no randomized assessment of efficacy.107,114 In Europe, clofarabine replaced fludarabine in the FLAG-DNX course in a phase II study. The BFM-AML group will randomize clofarabine/cytarabine versus a conventional ADxE block in their current study. |
| Vosaroxin | A quinolone antibiotic with topoisomerase II inhibitory properties was recently evaluated in a randomized trial.134 A pediatric investigational plan is in place, and pediatric studies plan to commence early in 2016. |
| CPX-351 (liposomal cytarabine:daunrubicin) | In a randomized, phase II study in adults, this yielded higher response rates than a conventional 3 + 7 reinduction regimen.115 A pediatric phase I study is ongoing (NCTB01943682) and phase II expansion through COG is planned. |
| Immunotherapy | |
| GO | GO has activity in pediatric AML in a phase I study,117 a phase II study,118 and a randomized phase 3 study.9 I-BFM-SG Relapsed AML 2010/01 will randomize the best arm of AML 2001/01 against the same regimen plus GO in relapsed AML. In 2010, the FDA label for GO was voluntarily withdrawn. |
| SGN33A | SGN33A is a conjugated monoclonal antibody that links the antibody to an average of two molecules of a pyrrolobenzodiazepine dimer, a highly potent DNA crosslinker; a phase I study in adults is ongoing. |
| BITE antibodies | BITE antibodies directed against CD33 in AML are awaiting clinical testing.119 |
| CAR T cells | Potential target antigens in AML are CD33, CD123, and anti-Lewis-Y. Because of expression on hematopoietic stem cells, therapies will possibly be myeloablative. Phase I studies are open in adults with AML (NCT01864902 and NCT01716364). |
| Tyrosine kinase inhibitors | |
| FLT3 inhibitors (sorafenib, quizartinib, crenolanib) | Röllig et al119a presented data from a randomized study in young adults that showed a benefit in the sorafenib arm. Novel, more potent, and more selective FLT3 inhibitors like quizartinib are in development and include compounds that may retain their activity in case of secondary resistance mutations,29 such as crenolanib.120 |
| KIT inhibitor (dasatinib) | KIT mutations occur in at least 20% of CBF-AML and may be targetable with a tyrosine kinase inhibitor.121–124 ITCC completed a phase I study of dasatinib in acute leukemias, which included a number of patients with AML; however, none of these were KIT mutated.135 A trial in adults with core binding factor mutations is planned (NCT00850382). |
| Trametinib | Single agent activity is modest,125 but the frequency of RAS pathway mutations provides compelling reason to study MEK inhibition in NRAS- and KRAS-mutated AML. |
| Polo-kinase inhibitor (volasertib) | A randomized, phase II trial in adults unfit for intensive chemotherapy showed a higher response rate than low-dose cytarabine.126 A pediatric dose-finding study is underway. |
| Aurora-kinase inhibitor (barasertib) | Early clinical development in adults is underway in adults.127 |
| Proteasome inhibitors | |
| Bortezomib, carfilzomib | In a phase II study of bortezomib in combination with chemotherapy in children with relapsed or refractory AML, COG reported a 51% response rate.108 A randomized hase III trial in children with de novo AML is underway (NCT01371981). The second-generation proteasome inhibitor carfilzomib, approved by the FDA for multiple myeloma, is now under evaluation in pediatric leukemia (NCT02303821).128 |
| Epigenetic agents | |
| Methyltransferase inhibitors (azacitidine, decitabine) | Ongoing trials of hypomethylating agents include a dose-finding study of the sequential combination of decitabine and cytarabine (NCT01853228) as well as a study of azacitidine in patients with AML in CR1 with rising MRD. Two trials (NCT00943553, NCT016270410) are evaluating decitabine priming prior to ADE induction chemotherapy in adults and children with newly diagnosed AML. In children, the combination showed acceptable tolerability, although data are unpublished. Another study performed in the TACL consortium seems to safely combine azacitidine with chemotherapy (NCT01861002). |
| Histone deacetylases (vorinostat, panobinostat) | Panobinostat is investigated in the TACL consortium in a phase I study (NCT01321346). The role of these compounds in pediatric AML needs to be better defined, although preclinical data with panobinostat are compelling.129 |
| DOT1L inhibitor (EPZ-5676) | Inhibition of the DOT1L hisone methyltransferase was suggested as a strategy to treat AML.130 Clinical studies in adults have thus far only reported modest responses despite sufficient inhibition of H3K79 methylation.131 A pediatric dose-finding study is ongoing in North America. |
| BET protein inhibitors (JQ1, OTX015) | Inhibition of BET proteins with compounds such as JQ1 or OTX015 may provide a new treatment strategy in AML, although clinical results are not yet available.132 |
| Other | |
| Nuclear export inhibitor (KPT-330) | This nuclear export inhibitor is currently being tested in pediatric leukemias (NCT02091245). |
| Pegylated recombinant arginase (BCT-100) | BCT-100 is a pegylated recombinant arginase, which leads to arginine depletion and AML cell death.133 |
Abbrevaitions: ADxE, cytarabine, liposomal daunorubicin, and etoposide; AML, acute myeloid leukemia; BITE, bi-specific T-cell engager antibodies; BFM, Berlin-Frankfurt-Münster; CAR, chimeric antigen receptor; CBF, core-binding factor; COG, Children's Oncology Group; CR1, first complete response; DNX, daunorubicin; DOT1L, disruption of telopmeric silencing-1 like; FDA, Food and Drug Administration; FLAG, fludarabine, cytarabine, and granulocyte colony-stimulating factor; GO, gemtuzumab ozogamicin; MRD, minimal residual disease; TACL, Therapeutic Advances in Childhood Leukemia.
SUPPORTIVE CARE
Without doubt, the advancements in supportive care have contributed significantly to the improvement in outcome for pediatric patients with AML, given the requirement for intensive chemotherapy that is needed to treat AML. Series in the past showed relatively high mortality related to leukemia and treatment complications.136,137 Patients with AML are at particular risk of viridans group streptococcal and Gram-negative bacteremia and invasive fungal infections. Candida and Aspergillus are prominent causes of fungal infection, although other fungi, such as Scedosporium, Fusarium, and Mucor, are emerging. In terms of infection prevention, approaches evaluated include prophylactic antimicrobial agents, prophylactic G-CSF, and nonpharmacologic approaches.138–140 Major questions relate to the risk-benefit ratio for antimicrobial prophylaxis to prevent invasive bacterial and fungal infection. In terms of antibacterial prophylaxis, it is unknown whether the risks of prophylaxis, which include Clostridium difficile infection, invasive fungal infection, and promotion of antibacterial resistance, are outweighed by the benefits. However, a Cochrane review that summarizes the available data provides evidence for a reduction in mortality.140,141 The best agents to use for antifungal prophylaxis are also unknown but include fluconazole; extended-spectrum triazoles, such as voriconazole and posaconazole; echinocandins, such as micafungin and caspofungin; and amphotericin products.139,142 To address these knowledge deficits, COG is conducting three randomized, controlled trials in patients with AML. One study compares levofloxacin prophylaxis versus no levofloxacin prophylaxis in intensively treated patients with leukemia and evaluates the evolution of resistant pathogens during exposure to levofloxacin. A second randomized trial compares fluconazole prophylaxis versus caspofungin prophylaxis during each cycle of neutropenia in patients with newly diagnosed or relapsed AML. The third study is a double-blind, randomized trial to evaluate if chlorhexidine bathing can reduce central line–associated bloodstream infection. Although prophylactic G-CSF reduces infection rate and infection-related mortality, widespread use has not been promoted, because it does not influence OS.143 Moreover, a placebo-controlled trial in adults did not show survival benefit despite quicker neutrophil recovery.144 G-CSF may even result in a higher relapse incidence in patients with AML that expresses the isoform IV of the G-CSF receptor.145
Another major supportive care issue faced by patients with AML is hyperleukocytosis, and approximately 20% of children and adolescents with AML have an initial WBC count greater than 100 × 109/L at diagnosis. Pulmonary leukostasis, CNS ischemia and hemorrhage, and early deaths are common in these patients. Patients with hyperleukocytosis should receive aggressive hydration; administration of rasburicase; optimization of coagulation, which includes the use of fresh frozen plasma and platelet transfusion; and urgent administration of chemotherapy. The role of leukopheresis is controversial in improving outcomes and does not seem to improve survival.146 Creation and dissemination of clinical practice guidelines to manage supportive care for patients with AML should be a priority. Recent international collaborations have been focused on developing guidelines for the management of pediatric fever and neutropenia147and for mucositis prevention.148
THE FUTURE OF INTERNATIONAL COOPERATIVE GROUP COLLABORATION
In the 1980s and 1990s, institutions across the globe organized into cooperative groups to better serve the clinical and scientific challenges in childhood cancer. Though initially these groups functioned independently, the interest and imperative for larger international networks of investigators has grown in response to the requirement for increasingly large and complex trial designs. Prospective clinical trials, with randomized questions when possible, remain the foundation for progress in improved outcomes for children with AML. As molecular aberrations define smaller and smaller subsets of childhood AML that require a targeted or a risk-adapted approach, the need for intergroup trials has been amplified. More and more countries and institutions are joining cooperative groups in Europe and North America. Inclusion of countries across the globe is growing. Challenges remain in defining standards for risk stratification, indications for bone marrow transplantation, patient-appropriate dose reductions, and optimal therapy for targetable molecular lesions as well as for optimal supportive care guidelines. The fate of children with AML who live in countries with fewer resources also must not be forgotten. Through cooperative and integrated efforts, the international research community can address these challenges.
Acknowledgment
We thank all study groups and their past, present, and future representatives that participate in collaborative projects and clinical trials, the importance of which cannot be underestimated but is not taken for granted. In addition, we thank all clinicians, statisticians, scientists, cytogeneticists and other laboratory personnel, and data managers for their efforts. We also thank J.D.E. de Rooij, C.M. Zwaan, M. Fornerod, and M.M. van den Heuvel-Eibrink at Erasmus MC, Rotterdam, and J. Cloos at Vrije Universiteit Medical Center, Amsterdam, for generation of figures and genetic aberration data for figures that was based on collaborative BFM-AML and Dutch Childhood Oncology Group studies. We were also supported by the Sophia Foundation, Dutch Cancer Society, and Foundation KiKa scientific grants (for generation of figures and figure data on genetic aberrations).
Footnotes
Supported by a PHRC grant from INCa and grants from SFCE and other associations (for ELAM02 and MyeChild01); by the nongovernmental and nonprofit German Cancer Aid (Deutsche Krebshilfe e.V.) for AML-BFM studies; by a grant from Demeures et Chateaux for EORTC 58921; by a grant for Clinical Cancer Research and a grant-in-aid for Cancer Research from the Ministry of Health, Labor, and Welfare of Japan for JPLSG studies; by Awards No. U10-CA180886, U10-CA180899, U10-CA098543, and U10-CA098413from the National Cancer Institute, National Institutes of Health, for COG; and by the Leukemia Research Foundation of Delaware for members of the international AML community to participate in the 2014 COG meeting.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Authors' disclosures of potential conflicts of interest are found in the article online at www.jco.org. Author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Disclosures provided by the authors are available with this article at www.jco.org.
AUTHOR CONTRIBUTIONS
Conception and design: C. Michel Zwaan, Edward A. Kolb, Dirk Reinhardt, Henrik Hasle, Franco Locatelli, Marry M. van den Heuvel, Gertjan J.L. Kaspers
Provision of study materials or patients: All authors
Collection and assembly of data: Edward A. Kolb, Jonas Abrahamsson, Souichi Adachi, Eveline S.J.M. De Bont, Barbara De Moerloose, Michael Dworzak, Brenda E.S. Gibson, Henrik Hasle, Guy Leverger, Christine Ragu, Raul C. Ribeiro, Carmelo Rizzari, Jeffrey E. Rubnitz, Owen P. Smith, Lillian Sung, Daisuke Tomizawa, Ursula Creutzig, Gertjan J.L. Kaspers
Data analysis and interpretation: C. Michel Zwaan, Jonas Abrahamsson, Souichi Adachi, Richard Aplenc, Eveline S.J.M. De Bont, Brenda E.S. Gibson, Guy Leverger, Christine Ragu, Raul C. Ribeiro, Jeffrey E. Rubnitz, Owen P. Smith, Lillian Sung, Ursula Creutzig, Gertjan J.L. Kaspers
Manuscript writing: All authors
Final approval of manuscript: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Collaborative Efforts Driving Progress in Pediatric Acute Myeloid Leukemia
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jco.ascopubs.org/site/ifc.
C. Michel Zwaan
Consulting or Advisory Role: Bristol-Myers Squibb (Inst), Novartis (Inst), Celgene (Inst), Pfizer (Inst), Sunesis Phamaceuticals, Daiichi-Sankyo Development
Travel, Accommodations, Expenses: Pfizer
Edward A. Kolb
No relationship to disclose
Dirk Reinhardt
Consulting or Advisory Role: Boehringer Ingelheim, Celgene (Inst), Sunesis Pharmaceuticals
Travel, Accommodations, Expenses: Grifols
Jonas Abrahamsson
No relationship to disclose
Souichi Adachi
No relationship to disclose
Richard Aplenc
Honoraria: Sigma Tau Pharmaceuticals
Travel, Accommodations, Expenses: Sigma Tau Pharmaceuticals
Eveline S.J.M. De Bont
No relationship to disclose
Barbara De Moerloose
Travel, Accommodations, Expenses: Jazz Pharmaceuticals, EUSA Pharma
Michael Dworzak
No relationship to disclose
Brenda E.S. Gibson
Honoraria: Janssen Pharmaceuticals
Consulting or Advisory Role: Janssen Pharmaceuticals
Henrik Hasle
Consulting or Advisory Role: Celgene
Guy Leverger
No relationship to disclose
Franco Locatelli
No relationship to disclose
Christine Ragu
No relationship to disclose
Raul C. Ribeiro
No relationship to disclose
Carmelo Rizzari
Honoraria: Jazz Pharmaceuticals, EUSA Pharma
Consulting or Advisory Role: Jazz Pharmaceuticals, EUSA Pharma
Travel, Accommodations, Expenses: Jazz Pharmaceuticals
Jeffrey E. Rubnitz
No relationship to disclose
Owen P. Smith
No relationship to disclose
Lillian Sung
No relationship to disclose
Daisuke Tomizawa
Honoraria: Chugai Pharmaceutical, Teijin Pharma, Otsuka, Kyowa Hakko Kirin, Sanofi
Marry M. van den Heuvel
No relationship to disclose
Ursula Creutzig
No relationship to disclose
Gertjan J.L. Kaspers
Consulting or Advisory Role: Boehringer Ingelheim, Celgene
REFERENCES
- 1.Creutzig U, Van Den Heuvel-Eibrink MM, Gibson B, et al. Diagnosis and management of acute myeloid leukemia in children and adolescents: Recommendations from an international expert panel. Blood. 2012;120:3167–3205. doi: 10.1182/blood-2012-03-362608. [DOI] [PubMed] [Google Scholar]
- 2.Kaspers GJL. Pediatric acute myeloid leukemia. Expert Rev Anticancer Ther. 2012;12:405–413. doi: 10.1586/era.12.1. [DOI] [PubMed] [Google Scholar]
- 3.Pui C-H, Carroll WL, Meshinchi S, et al. Biology, risk stratification, and therapy of pediatric acute leukemias: An update. J Clin Oncol. 2011;29:551–565. doi: 10.1200/JCO.2010.30.7405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abrahamsson J, Forestier E, Heldrup J, et al. Response-guided induction therapy in pediatric acute myeloid leukemia with excellent remission rate. J Clin Oncol. 2011;29:310–315. doi: 10.1200/JCO.2010.30.6829. [DOI] [PubMed] [Google Scholar]
- 5.Cooper TM, Franklin J, Gerbing RB, et al. AAML03P1, a pilot study of the safety of gemtuzumab ozogamicin in combination with chemotherapy for newly diagnosed childhood acute myeloid leukemia: A report from the Children's Oncology Group. Cancer. 2012;118:761–769. doi: 10.1002/cncr.26190. [DOI] [PubMed] [Google Scholar]
- 6.Creutzig U, Zimmermann M, Bourquin JP, et al. Randomized trial comparing liposomal daunorubicin with idarubicin as induction for pediatric acute myeloid leukemia: Results from study AML-BFM 2004. Blood. 2013;122:37–43. doi: 10.1182/blood-2013-02-484097. [DOI] [PubMed] [Google Scholar]
- 7.Dluzniewska A, Balwierz W, Armata J, et al. Twenty years of Polish experience with three consecutive protocols for treatment of childhood acute myelogenous leukemia. Leukemia. 2005;19:2117–2124. doi: 10.1038/sj.leu.2403892. [DOI] [PubMed] [Google Scholar]
- 8.Entz-Werle N, Suciu S, van der Werfften BJ, et al. Results of 58872 and 58921 trials in acute myeloblastic leukemia and relative value of chemotherapy vs allogeneic bone marrow transplantation in first complete remission: The EORTC Children Leukemia Group report. Leukemia. 2005;19:2072–2081. doi: 10.1038/sj.leu.2403932. [DOI] [PubMed] [Google Scholar]
- 9.Gamis AS, Alonzo TA, Meshinchi S, et al. Gemtuzumab ozogamicin in children and adolescents with de novo acute myeloid leukemia improves event-free survival by reducing relapse risk: Results from the randomized phase III Children's Oncology Group Trial AAML0531. J Clin Oncol. 2014;32:3021–3032. doi: 10.1200/JCO.2014.55.3628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gibson BES, Webb DKH, Howman AJ, et al. Results of a randomized trial in children with acute myeloid leukemia: Medical Research Council AML12 trial. Br J Haematol. 2011;155:366–376. doi: 10.1111/j.1365-2141.2011.08851.x. [DOI] [PubMed] [Google Scholar]
- 11.Pession A, Masetti R, Rizzari C, et al. Results of the AIEOP AML 2002/01 multicenter prospective trial for the treatment of children with acute myeloid leukemia. Blood. 2013;122:170–178. doi: 10.1182/blood-2013-03-491621. [DOI] [PubMed] [Google Scholar]
- 12.Rubnitz JE, Inaba H, Dahl G, et al. Minimal residual disease-directed therapy for childhood acute myeloid leukemia: Results of the AML02 multicentre trial. Lancet Oncol. 2010;11:543–552. doi: 10.1016/S1470-2045(10)70090-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tomizawa D, Tawa A, Watanabe T, et al. Appropriate dose reduction in induction therapy is essential for the treatment of infants with acute myeloid leukemia: A report from the Japanese pediatric leukemia/lymphoma study group. Int J Hematol. 2013;98:578–588. doi: 10.1007/s12185-013-1429-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tomizawa D, Tawa A, Watanabe T, et al. Excess treatment reduction including anthracyclines results in higher incidence of relapse in core binding factor acute myeloid leukemia in children. Leukemia. 2013;27:2413–2416. doi: 10.1038/leu.2013.153. [DOI] [PubMed] [Google Scholar]
- 15.Tsukimoto I, Tawa A, Horibe K, et al. Risk-stratified therapy and the intensive use of cytarabine improves the outcome in childhood acute myeloid leukemia: The AML99 trial from the Japanese childhood AML cooperative study group. J Clin Oncol. 2009;27:4007–4013. doi: 10.1200/JCO.2008.18.7948. [DOI] [PubMed] [Google Scholar]
- 16.Hasle H, Abrahamsson J, Forestier E, et al. Gemtuzumab ozogamicin as postconsolidation therapy does not prevent relapse in children with AML: Results from NOPHO-AML 2004. Blood. 2012;120:978–984. doi: 10.1182/blood-2012-03-416701. [DOI] [PubMed] [Google Scholar]
- 17.Vogelstein B, Papadopoulos N, Velculescu VE, et al. Cancer genome landscapes. Science. 2013;339:1546–1558. doi: 10.1126/science.1235122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kelly LM, Gilliland DG. Genetics of myeloid leukemias. Annu Rev Genomics Hum Genet. 2002;3:179–198. doi: 10.1146/annurev.genom.3.032802.115046. [DOI] [PubMed] [Google Scholar]
- 19.Hollink IHIM, Zwaan CM, Zimmermann M, et al. Favorable prognostic impact of NPM1 gene mutations in childhood acute myeloid leukemia, with emphasis on cytogenetically normal AML. Leukemia. 2009;23:262–270. doi: 10.1038/leu.2008.313. [DOI] [PubMed] [Google Scholar]
- 20.Brown P, Mcintyre E, Rau R, et al. The incidence and clinical significance of nucleophosmin mutations in childhood AML. Hematology. 2008:979–985. doi: 10.1182/blood-2007-02-076604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ho PA, Alonzo TA, Gerbing RB, et al. Prevalence and prognostic implications of CEBPA mutations in pediatric acute myeloid leukemia (AML): A report from the Children's Oncology Group. Blood. 2009;113:6558–6566. doi: 10.1182/blood-2008-10-184747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hollink IH, van den Heuvel-Eibrink MM, Arentsen-Peters ST, et al. Characterization of CEBPA mutations and promoter hypermethylation in pediatric acute myeloid leukemia. Haematologica. 2011;96:384–392. doi: 10.3324/haematol.2010.031336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Matsuo H, Kajihara M, Tomizawa D, et al. Prognostic implications of CEBPA mutations in pediatric acute myeloid leukemia: A report from the Japanese Pediatric Leukemia/Lymphoma Study Group. Blood Cancer J. 2014;4:e226. doi: 10.1038/bcj.2014.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mrózek K, Bloomfield CD. Chromosome aberrations, gene mutations, and expression changes, and prognosis in adult acute myeloid leukemia. Hematology Am Soc Hematol Educ Program. 2006:169–177. doi: 10.1182/asheducation-2006.1.169. [DOI] [PubMed] [Google Scholar]
- 25.Zwaan CM, Meshinchi S, Radich JP, et al. FLT3 internal tandem duplication in 234 children with acute myeloid leukemia: Prognostic significance and relation to cellular drug resistance. Blood. 2003;102:2387–2394. doi: 10.1182/blood-2002-12-3627. [DOI] [PubMed] [Google Scholar]
- 26.Meshinchi S, Alonzo TA, Stirewalt DL, et al. Clinical implications of FLT3 mutations in pediatric AML. Blood. 2006;108:3654–3661. doi: 10.1182/blood-2006-03-009233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cloos J, Goemans BF, Hess CJ, et al. Stability and prognostic influence of FLT3 mutations in paired initial and relapsed AML samples. Leukemia. 2006;20:1217–1220. doi: 10.1038/sj.leu.2404246. [DOI] [PubMed] [Google Scholar]
- 28.Bachas C, Schuurhuis GJ, Hollink IHIM, et al. High-frequency type I/II mutational shifts between diagnosis and relapse are associated with outcome in pediatric AML: Implications for personalized medicine. Blood. 2010;116:2752–2758. doi: 10.1182/blood-2010-03-276519. [DOI] [PubMed] [Google Scholar]
- 29.Smith CC, Wang Q, Chin C, et al. Validation of ITD mutations in FLT3 as a therapeutic target in human acute myeloid leukemia. Nature. 2012;485:260–263. doi: 10.1038/nature11016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meshinchi S, Stirewalt DL, Alonzo Ta, et al. Structural and numerical variation of FLT3/ITD in pediatric AML: Brief report. Blood. 2012:4930–4933. doi: 10.1182/blood-2008-01-117770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Balgobind BV, Raimondi SC, Harbott J, et al. Novel prognostic subgroups in childhood 11q23/MLL-rearranged acute myeloid leukemia: Results of an international retrospective study. Cancer. 2009;114:2489–2496. doi: 10.1182/blood-2009-04-215152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meyer C, Hofmann J, Burmeister T, et al. The MLL recombinome of acute leukemias in 2013. Leukemia. 2013;27:2165–2176. doi: 10.1038/leu.2013.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hollink IH, van den Heuvel-Eibrink MM, Arentsen-Peters ST, et al. NUP98/NSD1 characterizes a novel poor prognostic group in acute myeloid leukemia with a distinct HOX gene expression pattern. 2011;118:3645–3656. doi: 10.1182/blood-2011-04-346643. [DOI] [PubMed] [Google Scholar]
- 34.Ostronoff F, Othus M, Gerbing RB, et al. NUP98/NSD1 and FLT3/ITD coexpression is more prevalent in younger AML patients and leads to induction failure: A COG and SWOG report. Blood. 2015;124:2400–2408. doi: 10.1182/blood-2014-04-570929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.de Rooij JD, Hollink IH, Arentsen-Peters ST, et al. NUP98/JARID1A is a novel recurrent abnormality in pediatric acute megakaryoblastic leukemia with a distinct HOX gene expression pattern. Leukemia. 2013;27:2280–2288. doi: 10.1038/leu.2013.87. [DOI] [PubMed] [Google Scholar]
- 36.Reinhardt D, Diekamp S, Langebrake C, et al. Acute megakaryoblastic leukemia in children and adolescents, excluding Down's syndrome: Improved outcome with intensified induction treatment. Leukemia. 2005;19:1495–1496. doi: 10.1038/sj.leu.2403815. [DOI] [PubMed] [Google Scholar]
- 37.O'Brien MM, Cao X, Pounds S, et al. Prognostic features in acute megakaryoblastic leukemia in children without Down syndrome: A report from the AML02 multicenter trial and the Children's Oncology Group Study POG 9421. Leukemia. 2012:731–734. doi: 10.1038/leu.2012.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Masetti R, Pigazzi M, Togni M, et al. CBFA2T3-GLIS2 fusion transcript is a novel common feature in pediatric, cytogenetically normal AML, not restricted to FAB M7 subtype. Blood. 2013;121:3469–3472. doi: 10.1182/blood-2012-11-469825. [DOI] [PubMed] [Google Scholar]
- 39.Gruber TA, Gedman AL, Zhang J, et al. An inv(16)(p13.3q24.3) –encoded CBFA2T3-GLIS2 fusion protein defines an aggressive subtype of pediatric acute megakaryoblastic leukemia. Cancer Cell. 2012;22:683–697. doi: 10.1016/j.ccr.2012.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Von Bergh ARM, Van Drunen E, Van Wering ER, et al. High incidence of t(7;12)(q36;p13) in infant AML but not in infant ALL, with a dismal outcome and ectopic expression of HLXB9. Genes Chromosomes Cancer. 2006;45:731–739. doi: 10.1002/gcc.20335. [DOI] [PubMed] [Google Scholar]
- 41.Sandahl JD, Coenen EA, Forestier E, et al. T(6;9)(p22;q34)/DEK-NUP214-rearranged pediatric myeloid leukemia: An international study of 62 patients. Haematologica. 2014;99:865–872. doi: 10.3324/haematol.2013.098517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tarlock K, Alonzo TA, Moraleda PP, et al. Acute myeloid leukemia (AML) with t(6;9)(p23;q34) is associated with poor outcome in childhood AML regardless of FLT3-ITD status: A report from the Children's Oncology Group. Br J Haematol. 2014;166:254–259. doi: 10.1111/bjh.12852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Coenen EA, Zwaan CM, Reinhardt D, et al. Pediatric acute myeloid leukemia with t(8;16)(p11;p13), a distinct clinical and biological entity: A collaborative study by the International Berlin-Frankfurt-Munster AML study group. Blood. 2013;122:2704–2713. doi: 10.1182/blood-2013-02-485524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Linch DC, Hills RK, Burnett AK, et al. Impact of FLT3 ITD mutant allele level on relapse risk in intermediate-risk acute myeloid leukemia Impact of FLT3 ITD mutant allele level on relapse risk in intermediate-risk acute myeloid leukemia. Blood. 2014;124:273–276. doi: 10.1182/blood-2014-02-554667. [DOI] [PubMed] [Google Scholar]
- 45.Walter RB, Othus M, Burnett AK, et al. Resistance prediction in AML: Analysis of 4,601 patients from MRC/NCRI, HOVON/SAKK, SWOG, and MD Anderson Cancer Center. Leukemia. 2015;29:312–320. doi: 10.1038/leu.2014.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pratcorona M, Brunet S, Nomdedéu J, et al. Favorable outcome of patients with acute myeloid leukemia harboring a low-allelic burden FLT3-ITD mutation and concomitant NPM1 mutation: Relevance to post-remission therapy. Blood. 2013;121:2734–2738. doi: 10.1182/blood-2012-06-431122. [DOI] [PubMed] [Google Scholar]
- 47.Hollink IH, Van den Heuvel-Eibrink MM, Zimmermann M, et al. Clinical relevance of Wilms tumor 1 gene mutations in childhood acute myeloid leukemia. Blood. 2009;113:5951–5960. doi: 10.1182/blood-2008-09-177949. [DOI] [PubMed] [Google Scholar]
- 48.Ho PA, Alonzo TA, Gerbing RB, et al. Prevalence and prognostic implications of WT1 mutations in pediatric acute myeloid leukemia (AML): A report from the Children's Oncology Group. Blood. 2010;116:702–710. doi: 10.1182/blood-2010-02-268953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Balgobind BV, Lugthart S, Hollink IH, et al. EVI1 overexpression in distinct subtypes of pediatric acute myeloid leukemia. Leukemia. 2010;24:942–949. doi: 10.1038/leu.2010.47. [DOI] [PubMed] [Google Scholar]
- 50.Ho PA, Alonzo TA, Gerbing RB, et al. High EVI1 Expression is associated with MLL rearrangements and predicts decreased survival in pediatric acute myeloid leukemia: A report from the Children's Oncology Group. Br J Haematol. 2013;162:670–677. doi: 10.1111/bjh.12444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Matsuo H, Kajihara M, Tomizawa D, et al. EVI1 overexpression is a poor prognostic factor in pediatric patients with mixed lineage leukemia-AF9 rearranged acute myeloid leukemia. Haematologica. 2014;99:e225–e227. doi: 10.3324/haematol.2014.107128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hasle H, Alonzo TA, Auvrignon A, et al. Monosomy 7 and deletion 7q in children and adolescents with acute myeloid leukemia: An international retrospective study. Blood. 2007;109:4641–4647. doi: 10.1182/blood-2006-10-051342. [DOI] [PubMed] [Google Scholar]
- 53.Balgobind BV, Hollink IH, Arentsen-Peters ST, et al. Integrative analysis of type-I and type-II aberrations underscores the genetic heterogeneity of pediatric acute myeloid leukemia. Haematologica. 2011;96:1478–1487. doi: 10.3324/haematol.2010.038976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Berman JN, Gerbing RB, Alonzo TA, et al. Prevalence and clinical implications of NRAS mutations in childhood AML: A report from the Children's Oncology Group. Leukemia. 2011;25:1039–1042. doi: 10.1038/leu.2011.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Meshinchi S, Stirewalt D. Activating mutations of RTK/ras signal transduction pathway in pediatric acute myeloid leukemia. Blood. 2003;102:1474–1479. doi: 10.1182/blood-2003-01-0137. [DOI] [PubMed] [Google Scholar]
- 56.Burgess MR, Hwang E, Firestone AJ, et al. Preclinical efficacy of MEK inhibition in Nras-mutant AML. Blood. 2014;124:3947–3955. doi: 10.1182/blood-2014-05-574582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kampen KR, Ter Elst A, Mahmud H, et al. Insights in dynamic kinome reprogramming as a consequence of MEK inhibition in MLL-rearranged AML. Leukemia. 2013;28:589–599. doi: 10.1038/leu.2013.342. [DOI] [PubMed] [Google Scholar]
- 58.Meshinchi S, Thomson B, Finn LS, et al. Comparison of multidimensional flow cytometry with standard morphology for evaluation of early marrow response in pediatric acute lymphoblastic leukemia. J Pediatr Hematol. 2001;23:585–590. doi: 10.1097/00043426-200112000-00007. [DOI] [PubMed] [Google Scholar]
- 59.van der Velden VH, van der Sluijs-Geling A, Gibson BE, et al. Clinical significance of flowcytometric minimal residual disease detection in pediatric acute myeloid leukemia patients treated according to the DCOG ANLL97/MRC AML12 protocol. Leukemia. 2010;24:1599–1606. doi: 10.1038/leu.2010.153. [DOI] [PubMed] [Google Scholar]
- 60.Sievers EL, Lange BJ, Alonzo TA, et al. Immunophenotypic evidence of leukemia after induction therapy predicts relapse: Results from a prospective Children's Cancer Group study of 252 patients with acute myeloid leukemia. Blood. 2003;101:3398–3406. doi: 10.1182/blood-2002-10-3064. [DOI] [PubMed] [Google Scholar]
- 61.Loken MR, Alonzo TA, Pardo L, et al. Residual disease detected by multidimensional flow cytometry signifies high relapse risk in patients with de novo acute myeloid leukemia: A report from Children's Oncology Group. Blood. 2012;120:1581–1588. doi: 10.1182/blood-2012-02-408336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Inaba H, Coustan-Smith E, Cao X, et al. Comparative analysis of different approaches to measure treatment response in acute myeloid leukemia. J Clin Oncol. 2012;30:3625–3632. doi: 10.1200/JCO.2011.41.5323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ommen HB, Schnittger S, Jovanovic JV, et al. Strikingly different molecular relapse kinetics in NPM1c, PML-RARA, RUNX1-RUNX1T1, and CBFB-MYH11 acute myeloid leukemias. Blood. 2010;115:198–205. doi: 10.1182/blood-2009-04-212530. [DOI] [PubMed] [Google Scholar]
- 64.Creutzig U, Zimmermann M, Ritter J, et al. Treatment strategies and long-term results in pediatric patients treated in four consecutive AML-BFM trials. Leukemia. 2005;19:2030–2042. doi: 10.1038/sj.leu.2403920. [DOI] [PubMed] [Google Scholar]
- 65.Mandelli F, Vignetti M, Suciu S, et al. Daunorubicin versus mitoxantrone versus idarubicin as induction and consolidation chemotherapy for adults with acute myeloid leukemia: The EORTC and GIMEMA groups study AML-10. J Clin Oncol. 2009;27:5397–5403. doi: 10.1200/JCO.2008.20.6490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Löwenberg B, Ossenkoppele GJ, van Putten W, et al. High-dose daunorubicin in older patients with acute myeloid leukemia. N Engl J Med. 2009;361:1235–1248. doi: 10.1056/NEJMoa0901409. [DOI] [PubMed] [Google Scholar]
- 67.Lee JH, Joo YD, Kim H, et al. A randomized trial comparing standard versus high-dose daunorubicin induction in patients with acute myeloid leukemia. Blood. 2011;118:3832–3841. doi: 10.1182/blood-2011-06-361410. [DOI] [PubMed] [Google Scholar]
- 68.Armenian SH, Hudson MM, Mulder RL, et al. Recommendations for cardiomyopathy surveillance for survivors of childhood cancer: A report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Lancet Oncol. 2015;16:e123–e136. doi: 10.1016/S1470-2045(14)70409-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Burnett AK, Russell NH, Hills RK, et al. Optimization of chemotherapy for younger patients with acute myeloid leukemia: Results of the medical research council AML15 trial. J Clin Oncol. 2013;31:3360–3368. doi: 10.1200/JCO.2012.47.4874. [DOI] [PubMed] [Google Scholar]
- 70.Bishop JF. Approaches to induction therapy with adult acute myeloid leukemia. Acta Haematol. 1998;99:133–137. doi: 10.1159/000040827. [DOI] [PubMed] [Google Scholar]
- 71.Weick BJK, Kopecky KJ, Appelbaum FR, et al. A randomized investigation of high-dose versus standard-dose cytosine arabinoside with daunorubicin in patients with previously untreated acute myeloid leukemia: A Southwest Oncology Group study. Blood. 1996;88:2841–2851. [PubMed] [Google Scholar]
- 72.Ravindranath Y, Chang M, Steuber CP, et al. Pediatric Oncology Group (POG) studies of acute myeloid leukemia (AML): A review of four consecutive childhood AML trials conducted between 1981 and 2000. Leukemia. 2005;19:2101–2116. doi: 10.1038/sj.leu.2403927. [DOI] [PubMed] [Google Scholar]
- 73.Creutzig U, Zimmermann M, Bourquin JP, et al. Second induction with high-dose cytarabine and mitoxantrone: Different impact on pediatric AML patients with t(8;21) and with inv(16) Blood. 2011;118:5409–5415. doi: 10.1182/blood-2011-07-364661. [DOI] [PubMed] [Google Scholar]
- 74.Burnett AK, Hills RK, Milligan D, et al. Identification of patients with acute myeloblastic leukemia who benefit from the addition of gemtuzumab ozogamicin: Results of the MRC AML15 Trial. J Clin Oncol. 2011;29:369–377. doi: 10.1200/JCO.2010.31.4310. [DOI] [PubMed] [Google Scholar]
- 75.Burnett AK, Russell NH, Hills RK, et al. Addition of gemtuzumab ozogamicin to induction chemotherapy improves survival in older patients with acute myeloid leukemia. J Clin Oncol. 2012;30:3924–3931. doi: 10.1200/JCO.2012.42.2964. [DOI] [PubMed] [Google Scholar]
- 76.Castaigne S, Pautas C, Terré C, et al. Effect of gemtuzumab ozogamicin on survival of adult patients with de-novo acute myeloid leukaemia (ALFA-0701): A randomized, open-label, phase 3 study. Lancet. 2012;379:1508–1516. doi: 10.1016/S0140-6736(12)60485-1. [DOI] [PubMed] [Google Scholar]
- 77.Tomizawa D, Tabuchi K, Kinoshita A, et al. Repetitive cycles of high-dose cytarabine are effective for childhood acute myeloid leukemia: long-term outcome of the children with AML Treated on two consecutive trials of Tokyo Children's Cancer Study Group. Pediatr Blood Cancer. 2007;49:127–132. doi: 10.1002/pbc.20944. [DOI] [PubMed] [Google Scholar]
- 78.Harrison CJ, Hills RK, Moorman AV, et al. Cytogenetics of childhood acute myeloid leukemia: United Kingdom Medical Research Council Treatment Trials AML 10 and 12. J Clin Oncol. 2010;28:2674–2681. doi: 10.1200/JCO.2009.24.8997. [DOI] [PubMed] [Google Scholar]
- 79.Perel Y, Auvrignon a, Leblanc T, et al. Treatment of childhood acute myeloblastic leukemia: Dose intensification improves outcome and maintenance therapy is of no benefit—Multicenter studies of the French LAME (Leucémie Aiguë Myéloblastique Enfant) Cooperative Group. Leukemia. 2005;19:2082–2089. doi: 10.1038/sj.leu.2403867. [DOI] [PubMed] [Google Scholar]
- 80.Kaspers G. How I treat pediatric relapsed acute myeloid leuaemia. Br J Haematol. 2014;166:636–645. doi: 10.1111/bjh.12947. [DOI] [PubMed] [Google Scholar]
- 81.Lange, Beverly J, Yang RK, Gan J, et al. Soluble Interleukin-2 receptor a activation in a Children's Oncology Group randomized trial of interleukin-2 therapy for pediatric acute myeloid leukemia. Pediatr Blood Cancer. 2011;57:398–405. doi: 10.1002/pbc.22966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kaspers GJL, Zimmermann M, Reinhardt D, et al. Improved outcome in pediatric relapsed acute myeloid leukemia: Results of a randomized trial on liposomal daunorubicin by the International BFM Study Group. J Clin Oncol. 2013;31:599–607. doi: 10.1200/JCO.2012.43.7384. [DOI] [PubMed] [Google Scholar]
- 83.Pui C-H, Schrappe M, Ribeiro RC, et al. Childhood and adolescent lymphoid and myeloid leukemia. Hematology Am Soc Hematol Educ Program. 2004:118–145. doi: 10.1182/asheducation-2004.1.118. [DOI] [PubMed] [Google Scholar]
- 84.Kaspers GJ, Creutzig U. Pediatric acute myeloid leukemia: International progress and future directions. Leukemia. 2005;19:2025–2029. doi: 10.1038/sj.leu.2403958. [DOI] [PubMed] [Google Scholar]
- 85.Abbott BL, Rubnitz JE, Tong X, et al. Clinical significance of central nervous system involvement at diagnosis of pediatric acute myeloid leukemia: A single institution's experience. Leukemia. 2003;17:2090–2096. doi: 10.1038/sj.leu.2403131. [DOI] [PubMed] [Google Scholar]
- 86.Pui CH, Howard SC. Current management and challenges of malignant disease in the CNS in pediatric leukemia. Lancet Oncol. 2008;9:257–268. doi: 10.1016/S1470-2045(08)70070-6. [DOI] [PubMed] [Google Scholar]
- 87.Creutzig U, Reinhardt D. Current controversies: Which patients with acute myeloid leukaemia should receive a bone marrow transplantation? A European view. Br J Haematol. 2002;118:365–377. doi: 10.1046/j.1365-2141.2002.03697.x. [DOI] [PubMed] [Google Scholar]
- 88.Chen AR, Alonzo TA, Woods WG, et al. Current controversies: Which patients with acute myeloid leukemia should receive a bone marrow transplantation? An American view. Br J Haematol. 2002;118:378–384. doi: 10.1046/j.1365-2141.2002.03701.x. [DOI] [PubMed] [Google Scholar]
- 89.Bleakley M, Lau L, Shaw PJ, et al. Acute myeloid leukemia bone marrow transplantation for pediatric AML in first remission: A systematic review and meta-analysis. Bone Marrow Transplant. 2002;29:843–852. doi: 10.1038/sj.bmt.1703528. [DOI] [PubMed] [Google Scholar]
- 90.Niewerth D, Creutzig U, Bierings MB, et al. A review on allogeneic stem cell transplantation for newly diagnosed pediatric acute myeloid leukemia. Blood. 2010;116:2205–2214. doi: 10.1182/blood-2010-01-261800. [DOI] [PubMed] [Google Scholar]
- 91.Hasle H. A critical review of which children with acute myeloid leukemia need stem cell procedures. Br J Haematol. 2014;166:23–33. doi: 10.1111/bjh.12900. [DOI] [PubMed] [Google Scholar]
- 92.Leung W, Pui CH, Coustan-Smith E, et al. Detectable minimal residual disease before hematopoietic cell transplantation is prognostic but does not preclude cure for children with very-high-risk leukemia. Blood. 2012;120:468–472. doi: 10.1182/blood-2012-02-409813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Goemans BF, Tamminga RY, Corbijn CM, et al. Outcome for children with relapsed acute myeloid leukemia in the Netherlands following initial treatment between 1980 and 1998: Survival after chemotherapy only? Haematologica. 2008;93:1418–1420. doi: 10.3324/haematol.12807. [DOI] [PubMed] [Google Scholar]
- 94.Beier R, Albert MH, Bader P, et al. Allo-SCT using BU, CY, and melphalan for children with AML in second CR. Bone Marrow Transplant. 2012:651–656. doi: 10.1038/bmt.2012.204. [DOI] [PubMed] [Google Scholar]
- 95.Testi AM, Biondi A, Lo Coco F, et al. GIMEMA-AIEOPAIDA protocol for the treatment of newly diagnosed acute promyelocytic leukemia (APL) in children. Blood. 2005;106:447–453. doi: 10.1182/blood-2004-05-1971. [DOI] [PubMed] [Google Scholar]
- 96.Gregory J, Kim H, Alonzo T, et al. Treatment of children with acute promyelocytic leukemia: Results of the first North American Intergroup Trial INT0129. Pediatr Blood Cancer. 2009;53:1005–1010. doi: 10.1002/pbc.22165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Soignet SL, Maslak P, Wang Z-G, et al. Complete remission after treatment of acute promyelocytic leukemia. N Engl J Med. 1998;339:1341–1348. doi: 10.1056/NEJM199811053391901. [DOI] [PubMed] [Google Scholar]
- 98.Mathews V, George B, Chendamarai E, et al. Single-agent arsenic trioxide in the treatment of newly diagnosed acute promyelocytic leukemia: Long-term follow-up data. J Clin Oncol. 2010;28:3866–3871. doi: 10.1200/JCO.2010.28.5031. [DOI] [PubMed] [Google Scholar]
- 99.Lo-Coco F, Avvisati G, Vignetti M, et al. Retinoic acid and arsenic trioxide for acute promyelocytic leukemia. N Engl J Med. 2013;369:111–121. doi: 10.1056/NEJMoa1300874. [DOI] [PubMed] [Google Scholar]
- 100.Zwaan CM, Reinhardt D, Hitzler J, et al. Acute leukemias in children with Down syndrome. Hematol Oncol Clin North Am. 2010;24:19–34. doi: 10.1016/j.hoc.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 101.Sorrell AD, Alonzo TA, Hilden JM, et al. Favorable survival maintained in children who have myeloid leukemia associated with Down syndrome using reduced-dose chemotherapy on Children's Oncology Group trial A2971: A report from the Children's Oncology Group. Cancer. 2012;118:4806–4814. doi: 10.1002/cncr.27484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kudo K, Kojima S, Tabuchi K, et al. Prospective study of a pirarubicin, intermediate-dose cytarabine, and etoposide regimen in children with Down syndrome and acute myeloid leukemia: The Japanese childhood AML cooperative study group. J Clin Oncol. 2007;25:5442–5447. doi: 10.1200/JCO.2007.12.3687. [DOI] [PubMed] [Google Scholar]
- 103.Creutzig U, Reinhardt D, Diekamp S, et al. AML patients with Down syndrome have a high cure rate with AML-BFM therapy with reduced dose intensity. Leukemia. 2005;19:1355–1360. doi: 10.1038/sj.leu.2403814. [DOI] [PubMed] [Google Scholar]
- 104.Taga T, Saito AM, Kudo K, et al. Clinical characteristics and outcome of refractory/relapsed myeloid leukemia in children with Down syndrome. Blood. 2012;120:1810–1815. doi: 10.1182/blood-2012-03-414755. [DOI] [PubMed] [Google Scholar]
- 105.Webb DK, Wheatley K, Harrison G, et al. Outcome for children with relapsed acute myeloid leukemia following initial therapy in the Medical Research Council (MRC) AML 10 trial: MRC Childhood Leukemia Working Party. Leukemia. 1999;13:25–31. doi: 10.1038/sj.leu.2401254. [DOI] [PubMed] [Google Scholar]
- 106.Sander A, Zimmermann M, Dworzak M, et al. Consequent and intensified relapse therapy improved survival in pediatric AML: Results of relapse treatment in 379 patients of three consecutive AML-BFM trials. Leukemia. 2010;24:1422–1428. doi: 10.1038/leu.2010.127. [DOI] [PubMed] [Google Scholar]
- 107.Cooper TM, Alonzo TA, Gerbing RB, et al. AAML0523: A report from the Children's Oncology Group on the efficacy of clofarabine in combination with cytarabine in pediatric patients with recurrent acute myeloid leukemia. Cancer. 2014;120:2482–2489. doi: 10.1002/cncr.28674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Horton TM, Perentesis JP, Gamis AS, et al. A Phase 2 study of bortezomib combined with either idarubicin/cytarabine or cytarabine/etoposide in children with relapsed, refractory or secondary acute myeloid leukemia: A report from the Children's Oncology Group. Pediatr Blood Cancer. 2014;61:1754–1760. doi: 10.1002/pbc.25117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Gorman M. Outcome for children treated for relapsed or refractory acute myelogenous leukemia (rAML): A Therapeutic Advances in Childhood Leukemia (TACL) consortium study. Pediatr Blood Cancer. 2010;55:421–429. doi: 10.1002/pbc.22612. [DOI] [PubMed] [Google Scholar]
- 110.Nakayama H, Tabuchi K, Tawa A, et al. Outcome of children with relapsed acute myeloid leukemia following initial therapy under the AML99 protocol. Int J Hematol. 2014;100:171–179. doi: 10.1007/s12185-014-1616-9. [DOI] [PubMed] [Google Scholar]
- 111.Creutzig U, Zimmermann M, Dworzak MN, et al. The prognostic significance of early treatment response in pediatric relapsed acute myeloid leukemia: Results of the international study Relapsed AML 2001/01. Haematologica. 2014;99:1472–1478. doi: 10.3324/haematol.2014.104182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Moore AS, Kearns PR, Knapper S, et al. Novel therapies for children with acute myeloid leukemia. Leukemia. 2013;27:1451–1460. doi: 10.1038/leu.2013.106. [DOI] [PubMed] [Google Scholar]
- 113.Tasian SK, Pollard JA, Aplenc R. Molecular therapeutic approaches for pediatric acute myeloid leukemia. Front Oncol. 2014;4:55. doi: 10.3389/fonc.2014.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Shukla N, Kobos R, Renaud T, et al. Phase II trial of clofarabine with topotecan, vinorelbine, and thiotepa in pediatric patients with relapsed or refractory acute leukemia. Pediatr Blood Cancer. 2014;61:431–435. doi: 10.1002/pbc.24789. [DOI] [PubMed] [Google Scholar]
- 115.Lancet JE, Cortes JE, Hogge DE, et al. Phase 2 trial of CPX-351, a fixed 5:1 molar ratio of cytarabine/daunorubicin, vs cytarabine/daunorubicin in older adults with untreated AML. Blood. 2014;123:3239–3246. doi: 10.1182/blood-2013-12-540971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Lancet JE, Roboz GJ, Cripe LD, et al. A phase 1b/2 study of vosaroxin in combination with cytarabine in patients with relapsed or refractory acute myeloid leukemia. Haematologica. 2014;100:231–237. doi: 10.3324/haematol.2014.114769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Zwaan CM, Reinhardt D, Corbacioglu S, et al. Gemtuzumab ozogamicin: First clinical experiences in children with relapsed/refractory acute myeloid leukemia treated on compassionate-use basis. Blood. 2003;101:3868–3871. doi: 10.1182/blood-2002-07-1947. [DOI] [PubMed] [Google Scholar]
- 118.Zwaan CM, Reinhardt D, Zimmerman M, et al. Salvage treatment for children with refractory first or second relapse of acute myeloid leukemia with gemtuzumab ozogamicin: Results of a phase II study. Br J Haematol. 2010;148:768–776. doi: 10.1111/j.1365-2141.2009.08011.x. [DOI] [PubMed] [Google Scholar]
- 119.Laszlo GS, Gudgeon CJ, Harrington KH, et al. Cellular determinants for preclinical activity of a novel CD33/CD3 bispecific T-cell engager (BiTE) antibody, AMG 330, against human AML. Blood. 2014;123:554–561. doi: 10.1182/blood-2013-09-527044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119a.Röllig C, Müller-Tidow C, Hüttmann A, et al. Sorafenib versus placebo in addition to standard therapy in younger patients with newly diagnosed acute myeloid leukemia: Results from 267 patients treated in the randomized placebo-controlled SALSoraml trial. Presented at the American Society of Hematology Annual Meeting; December 6-9, 2014; San Francisco, CA. (abstr 6) [Google Scholar]
- 120.Galanis A, Ma H, Rajkhowa T, et al. Crenolanib is a potent inhibitor of flt3 with activity against resistance-conferring point mutants. Blood. 2014;123:94–100. doi: 10.1182/blood-2013-10-529313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Goemans BF, Zwaan CM, Miller M, et al. Mutations in KIT and RAS are frequent events in pediatric core-binding factor acute myeloid leukemia. Leukemia. 2005;19:1536–1542. doi: 10.1038/sj.leu.2403870. [DOI] [PubMed] [Google Scholar]
- 122.Pollard JA, Alonzo TA, Gerbing RB, et al. Prevalence and prognostic significance of KIT mutations in pediatric patients with core binding factor AML enrolled on serial pediatric cooperative trials for de novo AML. Blood. 2010;115:2372–2379. doi: 10.1182/blood-2009-09-241075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Manara E, Bisio V, Masetti R, et al. Core-binding factor acute myeloid leukemia in pediatric patients enrolled in the AIEOP AML 2002/01 trial: Screening and prognostic impact of c-KIT mutations. Leukemia. 2014;28:1132–1134. doi: 10.1038/leu.2013.339. [DOI] [PubMed] [Google Scholar]
- 124.Shimada A, Taki T, Tabuchi K. KIT mutations, and not FLT3 internal tandem duplication, are strongly associated with a poor prognosis in pediatric acute myeloid leukemia with t(8;21): A study of the Japanese Childhood AML Cooperative Study Group. Blood. 2006;107:1806–1809. doi: 10.1182/blood-2005-08-3408. [DOI] [PubMed] [Google Scholar]
- 125.Jain N, Curran E, Iyengar NM, et al. Phase 2 study of the oral MEK inhibitor selumetinib in advanced acute myelogenous leukemia: A University of Chicago phase 2 consortium trial. Clin Cancer Res. 2014;20:490–498. doi: 10.1158/1078-0432.CCR-13-1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Döhner H, Lübbert M, Fiedler W, et al. Randomized, phase 2 trial comparing low-dose cytarabine with or without volasertib in AML patients not suitable for intensive induction therapy. Blood. 2014:1426–1434. doi: 10.1182/blood-2014-03-560557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kantarjian HM, Martinelli G, Jabbour EJ, et al. Stage I of a phase 2 study assessing the efficacy, safety, and tolerability of barasertib (AZD1152) versus low-dose cytosine arabinoside in elderly patients with acute myeloid leukemia. Cancer. 2013;119:2611–2619. doi: 10.1002/cncr.28113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Stewart AK, Rajkumar SV, Dimopoulos MA, et al. Carfilzomib, lenalidomide, and dexamethasone for relapsed multiple myeloma. N Engl J Med. 2015;372:142–152. doi: 10.1056/NEJMoa1411321. [DOI] [PubMed] [Google Scholar]
- 129.Stumpel D, Schneider P, Seslija L, et al. Connectivity mapping identifies HDAC inhibitors for the treatment of t(4;11)-positive infant acute lymphoblastic leukemia. Leukemia. 2012;26:682–692. doi: 10.1038/leu.2011.278. [DOI] [PubMed] [Google Scholar]
- 130.Daigle SR, Olhava EJ, Therkelsen CA, et al. Selective killing of mixed lineage leukemia cells by a potent small-molecule DOT1L inhibitor. Cancer Cell. 2014;20:53–65. doi: 10.1016/j.ccr.2011.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Stein EM, Tallman MS. Mixed lineage rearranged leukemia. Curr Opin Hematol. 2015;22:92–96. doi: 10.1097/MOH.0000000000000123. [DOI] [PubMed] [Google Scholar]
- 132.Zuber J, Shi J, Wang E, et al. RNAi screen identifies Brd4 as a therapeutic target in acute myeloid leukaemia. Nature. 2011;478:524–528. doi: 10.1038/nature10334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Mussai F, Egan S, Higginbotham-Jones J, et al. Arginine dependence of acute myeloid leukemia blast proliferation: A novel therapeutic target. Blood. 2015;125:2386–2397. doi: 10.1182/blood-2014-09-600643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Lancet JE. A phase 1b/2 study of vosaroxin in combination with cytarabine in patients with relapsed or refractory acute myeloid leukemia. Haematologica. 2015;100:231–237. doi: 10.3324/haematol.2014.114769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zwaan CM, Rizzari C, Mechinaud F, et al. Dasatinib in children and adolescents with relapsed or refractory leukemia: Results of the CA180-018 phase I dose-escalation study of the Innovative Therapies for Children with Cancer Consortium. J Clin Oncol. 2013;31:2460–2468. doi: 10.1200/JCO.2012.46.8280. [DOI] [PubMed] [Google Scholar]
- 136.Slats AM, Egeler RM, van der Does-van den Berg A, et al. Causes of death—other than progressive leukemia—in childhood acute lymphoblastic (ALL) and myeloid leukemia (AML): The Dutch Childhood Oncology Group experience. Leukemia. 2005;19:537–544. doi: 10.1038/sj.leu.2403665. [DOI] [PubMed] [Google Scholar]
- 137.Creutzig U, Zimmermann M, Reinhardt D, et al. Early deaths and treatment-related mortality in children undergoing therapy for acute myeloid leukemia: Analysis of the multicenter clinical trials AML-BFM 93 and AML-BFM 98. J Clin Oncol. 2004;22:4384–4393. doi: 10.1200/JCO.2004.01.191. [DOI] [PubMed] [Google Scholar]
- 138.Sung L, Aplenc R, Alonzo TA, et al. Effectiveness of supportive care measures to reduce infections in pediatric AML: A report from the Children's Oncology Group. Blood. 2013;121:3573–3577. doi: 10.1182/blood-2013-01-476614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Groll AH, Castagnola E, Cesaro S, et al. Fourth European Conference on Infections in Leukaemia (ECIL-4): Guidelines for diagnosis, prevention, and treatment of invasive fungal diseases in pediatric patients with cancer or allogeneic hemopoietic stem-cell transplantation. Lancet Oncol. 2014;15:e327–e340. doi: 10.1016/S1470-2045(14)70017-8. [DOI] [PubMed] [Google Scholar]
- 140.Van de Wetering MD, van Woensel JB, Lawrie TA. Prophylactic antibiotics for preventing Gram-positive infections associated with long-term central venous catheters in oncology patients. Cochrane Database Syst Rev. 2013;11:1–33. doi: 10.1002/14651858.CD003295.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Alexander S, Nieder M, Zerr DM, et al. Prevention of bacterial infection in pediatric oncology: What do we know, what can we learn? Pediatr Blood Cancer. 2012;59:16–20. doi: 10.1002/pbc.23416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Dvorak CC, Fisher BT, Sung L, et al. Antifungal prophylaxis in pediatric hematology/oncology: New choices and new data. Pediatr Blood Cancer. 2012;59:21–26. doi: 10.1002/pbc.23415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Sung L, Nathan PC, Alibhai SMH, et al. Meta-analysis: Effect of prophylactic hematopoietic colony-stimulating factors on mortality and outcomes of infection. Ann Intern Med. 2007;147:400–411. doi: 10.7326/0003-4819-147-6-200709180-00010. [DOI] [PubMed] [Google Scholar]
- 144.Wheatley K, Goldstone AH, Littlewood T, et al. Randomized placebo-controlled trial of granulocyte colony stimulating factor (G-CSF) as supportive care after induction chemotherapy in adult patients with acute myeloid leukaemia: A study of the United Kingdom Medical Research Council Adult Leukemia Working Party. Br J Haematol. 2009;146:54–63. doi: 10.1111/j.1365-2141.2009.07710.x. [DOI] [PubMed] [Google Scholar]
- 145.Ehlers S, Herbst C, Zimmermann M, et al. Granulocyte colony-stimulating factor (G-CSF) treatment of childhood acute myeloid leukemias that overexpress the differentiation-defective G-CSF receptor isoform IV is associated with a higher incidence of relapse. J Clin Oncol. 2010;28:2591–2597. doi: 10.1200/JCO.2009.25.9010. [DOI] [PubMed] [Google Scholar]
- 146.Oberoi S, Lehrnbecher T, Phillips B, et al. Leukapheresis and low-dose chemotherapy do not reduce early mortality in acute myeloid leukemia hyperleukocytosis: A systematic review and meta-analysis. Leuk Res. 2014;38:460–468. doi: 10.1016/j.leukres.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 147.Lehrnbecher T, Phillips R, Alexander S, et al. Guideline for the management of fever and neutropenia in children with cancer and/or undergoing hematopoietic stem-cell transplantation. J Clin Oncol. 2012;30:4427–4438. doi: 10.1200/JCO.2012.42.7161. [DOI] [PubMed] [Google Scholar]
- 148.Sung L, Robinson P, Treister N, et al. Guideline for the prevention of oral and oropharyngeal mucositis in children receiving treatment for cancer or undergoing haematopoietic stem cell transplantation. BMJ Support Palliat Care. doi: 10.1136/bmjspcare-2014-000804. doi: 10.1136/bmjspcare-2014-000804 [epub ahead of print on March 27, 2015] [DOI] [PMC free article] [PubMed] [Google Scholar]