Abstract
Our recent work has provided the first evidence that MDSCs promote chronic colonic inflammation and colitis-associated carcinogenesis. Our findings not only reveal a novel function of MDSCs in connecting inflammation to cancer, but also provide a rationale for developing effective therapeutic strategies to subvert inflammation- and tumor-induced immunosuppression.
Keywords: colorectal cancer, inflammation, colitis-associated tumorigenesis, CXCR2, myeloid-derived suppressor cells
Colorectal cancer (CRC) includes hereditary, sporadic, and colitis-associated CRC. Epidemiologic and experimental evidence strongly support the concept that chronic inflammation contributes to tumor initiation, progression, and metastasis. Indeed, ulcerative colitis, the most common form of inflammatory bowel disease (IBD), is associated with an increased risk for the development of CRC.1 Since chronic inflammation is involved in immunosuppression,2 one potential mechanistic explanation for the contribution of chronic inflammation to cancer is that it promotes tumor development via induction of immunosuppression, a protumorigenic environment by virtue of immune tolerance to tumor cells. This notion is supported by the results of our recent mouse model study of IBD-associated carcinomas in which myeloid-derived suppressor cells (MDSCs), recruited by chronic inflammation, promoted colitis-associated tumorigenesis and disease progression via suppression of anticancer CD8+ T-cell cytotoxicity.
MDSCs are a heterogenous population of immature myeloid cells. In healthy individuals, immature myeloid cells differentiate into mature myeloid cells including macrophages, DCs, and granulocytes. However, this normal physiological process is interrupted in cancer patients. For example, the levels of MDSC in the blood are positively correlated with clinical cancer stage and metastatic tumor burden in mice and humans with colon cancers.4,5 MDSCs have been shown to contribute to cancer immune evasion via suppressing T-cell activation, proliferation, trafficking, and viability, inhibiting natural killer (NK) cells, and promoting activation and expansion of Foxp3 positive regulatory T (Treg) cells.6 Although significant evidence demonstrates that MDSCs play key roles in tumor-induced immunosuppression, it remains unclear how MDSCs are recruited from the circulatory system to the colonic mucosa during chronic inflammation and tumorigenesis. Our recent work provides the first evidence showing that a chemokine receptor, C-X-C family receptor 2 (CXCR2) is required for infiltration of MDSCs from the circulatory system to inflamed colonic mucosa and colitis-associated tumors in mice treated with the carcinogen azoxymethane/dextran sulfate sodium (AOM/DSS).3 We found that almost all circulatory MDSCs expressed cell-surface CXCR2 in our model. Since CXCR2 was previously only thought to mediate neutrophil migration to inflammatory sites, our findings uncover a previously unrecognized role for CXCR2 in recruiting MDSCs from the circulatory system into inflamed colonic mucosa and colitis-associated tumors. Moreover, additional research is needed to determine whether CXCR2 antagonists suppress chronic inflammation, colitis-associated carcinogenesis, and adenoma growth by inhibiting infiltration of MDSCs. Most importantly, it is essential to evaluate whether our results are clinically relevant by examining the correlation between CXCR2-expressing MDSCs, CXCR2 ligands, prostaglandin E2 (PGE2) levels, and clinical outcomes of patients with CRC.
Previous studies have shown that several pro-inflammatory mediators such as IL-1β, IL-6, and PGE2 induce MDSC accumulation and activation,7 suggesting that chronic inflammation might promote tumor initiation and progression by induction of immune suppression via MDSCs. However, so far, there has been no direct evidence demonstrating that MDSCs play a key role in connecting chronic inflammation to carcinogenesis. Our group was the first to report that colonic MDSCs recruited by chronic inflammation accelerate colitis-associated tumor formation and progression.3 Moreover, our results showed that PGE2 signaling induced expression of CXCR2 ligands in intestinal mucosa and tumors in vivo. These findings prompted us to postulate that PGE2 might induce an infiltration of MDSCs into colonic mucosa and neoplasms growths through the induction of CXCR2 ligands. Our laboratory is currently testing this hypothesis.
Among prostaglandins, PGE2 is the most abundant prostaglandin found in various types of human malignancies and is often associated with a poor prognosis.8 Research by our group and others has revealed that pro-inflammatory PGE2 is a key inflammatory mediator and plays a predominant role in various hallmarks of cancer progression among most types of malignancy including in CRC.8 PGE2 is produced from arachidonic acid by the action of cyclooxygenase enzymes (namely, COX-1 and COX-2) and prostaglandin E2 synthases. COX-1 is constitutively expressed in most tissues and was thought to be a housekeeping enzyme responsible for maintaining basal prostanoid levels important for tissue homeostasis and platelet function. By contrast, COX-2 is an immediate-early response gene that is normally absent from most cells but is highly induced at sites of inflammation and tumors, particularly in IBD and CRC.9 Currently, the best agents for targeting the COX-2 enzyme are nonsteroidal anti-inflammatory drugs (NSAIDs). Both epidemiologic and clinical evidence has demonstrated that NSAIDs have beneficial effects on reducing the risk of developing CRC.10 NSAIDs (except aspirin) can increase the risk for cardiovascular complications. Our findings concerning the PGE2-driven role of MDSCs in colorectal cancer might provide another potential mechanistic explanation for the well-characterized antitumor effects of NSAIDs.
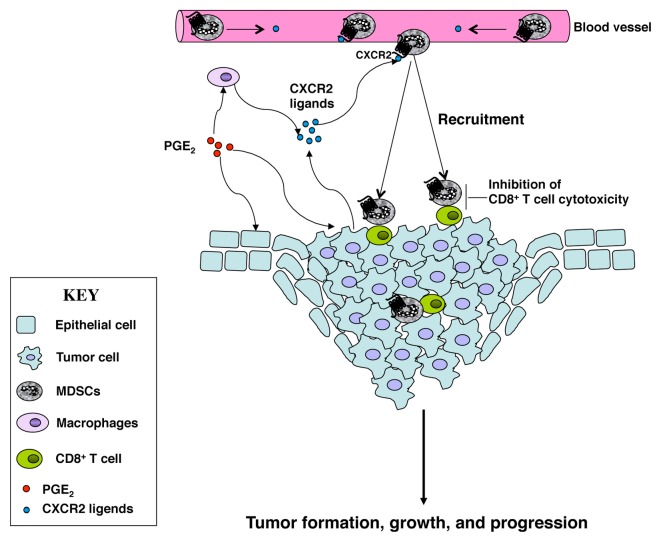
In summary, our recent work has demonstrated that CXCR2 is required for the recruitment of MDSCs into the inflamed colonic mucosa and tumors and that colonic MDSCs recruited by chronic inflammation contribute to colitis-associated tumor formation and progression via suppression of colonic CD8+ T-cell cytotoxicity. Moreover, our observation that PGE2 induction of CXCR2 ligands in colonic mucosa and tumors suggest that PGE2 might promote tumor formation and progression by recruiting MDSCs via a CXCR2-ligand-CXCR2 pathway (Fig. 1). These findings not only have extended our current knowledge of how chronic inflammation contributes to cancer, but also provided a rationale for the development of new therapeutic approaches to subvert tumor-induced immunosuppression via CXCR2 antagonists and its neutralizing antibodies.
Figure 1. A possible model for the role of PGE2 in the regulation of tumor-induced immunosuppression. Pro-inflammatory prostaglandin E2 (PGE)2 produced by tumor epithelial cells and tumor-associated stromal cells such as macrophages induces CXCR2 ligands, which in turn recruit CXCR2-expressing MDSCs into the tumor though the circulatory system. The recruited MDSCs promote tumor formation, growth, and progression primarily via suppressing CD8+ T-cell cytotoxicity against tumor cells.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- 1.Ekbom A, Helmick C, Zack M, Adami HO. Ulcerative colitis and colorectal cancer. A population-based study. N Engl J Med. 1990;323:1228–33. doi: 10.1056/NEJM199011013231802. [DOI] [PubMed] [Google Scholar]
- 2.Kanterman J, Sade-Feldman M, Baniyash M. New insights into chronic inflammation-induced immunosuppression. Semin Cancer Biol. 2012;22:307–18. doi: 10.1016/j.semcancer.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 3.Katoh H, Wang D, Daikoku T, Sun H, Dey SK, Dubois RN. CXCR2-expressing myeloid-derived suppressor cells are essential to promote colitis-associated tumorigenesis. Cancer Cell. 2013;24:631–44. doi: 10.1016/j.ccr.2013.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mandruzzato S, Solito S, Falisi E, Francescato S, Chiarion-Sileni V, Mocellin S, Zanon A, Rossi CR, Nitti D, Bronte V, et al. IL4Ralpha+ myeloid-derived suppressor cell expansion in cancer patients. J Immunol. 2009;182:6562–8. doi: 10.4049/jimmunol.0803831. [DOI] [PubMed] [Google Scholar]
- 5.Diaz-Montero CM, Salem ML, Nishimura MI, Garrett-Mayer E, Cole DJ, Montero AJ. Increased circulating myeloid-derived suppressor cells correlate with clinical cancer stage, metastatic tumor burden, and doxorubicin-cyclophosphamide chemotherapy. Cancer Immunol Immunother. 2009;58:49–59. doi: 10.1007/s00262-008-0523-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gabrilovich DI, Ostrand-Rosenberg S, Bronte V. Coordinated regulation of myeloid cells by tumours. Nat Rev Immunol. 2012;12:253–68. doi: 10.1038/nri3175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ostrand-Rosenberg S, Sinha P. Myeloid-derived suppressor cells: linking inflammation and cancer. J Immunol. 2009;182:4499–506. doi: 10.4049/jimmunol.0802740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang D, Dubois RN. Eicosanoids and cancer. Nat Rev Cancer. 2010;10:181–93. doi: 10.1038/nrc2809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang D, Dubois RN. The role of COX-2 in intestinal inflammation and colorectal cancer. Oncogene. 2010;29:781–8. doi: 10.1038/onc.2009.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang D, DuBois RN. The role of anti-inflammatory drugs in colorectal cancer. Annu Rev Med. 2013;64:131–44. doi: 10.1146/annurev-med-112211-154330. [DOI] [PubMed] [Google Scholar]