Abstract
Background
Interferon-γ is of key importance in the immune response to Cryptococcus neoformans. Mortality related to cryptococcal meningitis (CM) remains high, and novel treatment strategies are needed. We performed an RCT to determine whether addition of IFNγ to standard therapy increased the rate of clearance of cryptococcal infection in HIV-associated CM.
Methods
Patients were randomized to: (1) Amphotericin-B 1mg/kg/day plus 5-FC 100mg/kg/day for 2-weeks (Standard therapy), (2) Standard therapy plus IFNγ1b 100μg days 1 and 3 (IFNγ 2-doses), or (3) Standard therapy plus IFNγ1b 100μg days 1, 3, 5, 8, 10 and 12 (IFNγ 6-doses). Primary outcome was rate of clearance of cryptococcus from the CSF (early fungicidal activity, EFA) calculated from serial quantitative cultures, previously shown to be independently associated with survival.
Results
Rate of fungal clearance was significantly faster in IFNγ containing groups than with standard treatment. Mean EFA (logCFU/ml/day) was −0.49 with standard treatment, −0.64 with IFNγ 2-doses, and −0.64 with IFNγ 6-doses. Difference in EFA was −0.15 (95%CI −0.02- −0.27, p=0.02) between standard treatment and IFNγ 2-doses, and −0.15 (95%CI-0.05- −0.26, p=0.006) between standard treatment and IFNγ 6-doses. Mortality was 16% (14/88) at 2 weeks and 31% (27/87) at 10 weeks, with no significant difference between groups. All treatments were well tolerated.
Conclusions
Addition of short-course IFNγ to standard treatment significantly increased the rate of clearance of cryptococcal infection from the CSF, and was not associated with any increase in adverse events. Two doses of IFNγ are as effective as 6 doses.
Introduction
Cytokine therapy may potentially be of benefit in many infectious diseases, but currently has limited clinical application. Interferon gamma (IFNγ) plays a key role in the host response to intra-cellular pathogens, where it is instrumental in directing the immune system towards protective Th1 type immunity. One such pathogen is Cryptococcus neoformans, which is a frequent cause of severe meningoencephalitis in HIV-infected patients [1, 2]. Cryptococcal meningitis (CM) is the commonest cause of adult meningitis in Southern Africa, accounting for 63% of all microbiologically confirmed cases in the largest published series [3]. Despite optimal therapy with amphotericin B based treatment, acute mortality remains between 24 and 37% [4-6]. There is an urgent need to improve outcomes, but drug treatment options are extremely limited, with few novel anti-fungal agents on the horizon.
Immunotherapy with IFNγ has been investigated as a potential adjunctive agent for the treatment of CM [7]. Animal model data supports a central role for IFN-γ in defence against cryptococcal infection [8-13], and IFN-γ has been shown to potentiate the effect of amphotericin B both in vitro and in vivo [14, 15]. There is also direct in-vivo evidence for the importance of IFN-γ for clearance of cryptococcal infection in HIV-infected patients [16], and adjunctive IFN-γ (given in addition to amphotericin B and flucytosine) has been shown to be well tolerated, with no adverse effect on CD4 count or viral load [7]. However, no trial sufficiently powered to investigate the efficacy of adjunctive IFN-γ in the treatment of CM has previously been performed.
We performed an open label randomized controlled trial, using the statistically powerful and clinically validated surrogate endpoint of early fungicidal activity (EFA) [17], to determine whether the addition of exogenous IFN-γ to optimal anti-fungal therapy increased the rate of clearance of cryptococcal infection from the CSF of patients with HIV-associated CM. In view of data suggesting that the beneficial effects of IFN-γ occur very early in the treatment course [16], we compared two short course IFN-γ regimens (either 2 weeks or 3 days) with standard therapy.
Materials and Methods
The study was performed at GF Jooste Hospital, a public-sector adult referral hospital in Cape Town, South Africa, and approved by the Research Ethics Committee of the University of Cape Town, the Medicines Control Council of South Africa and the London-Surrey Borders Research Ethics Committee on behalf of St. George’s University of London. The study was conducted in accordance with the principles of the Helsinki Declaration and prospectively registered on the International Standard Randomised Controlled Trial Register (ISRCTN 72024361).
Participants and Procedures
Between July 2007 and May 2010 sequential HIV-positive adults (age ≥ 21 years) with a first episode of cryptococcal meningitis, diagnosed by CSF India ink or cryptococcal antigen testing (titres ≥ 1:1024, Meridian Cryptococcal Latex Agglutination System, Meridian Bioscience) were screened for enrollment. Exclusion criteria were an alanine aminotransferase concentration more than five times the upper limit of normal (> 200 IU/ml), a neutrophil count < 500 × 106 cells/L, a platelet count < 50,000 × 106 cells/L, pregnancy or lactation, previous serious reaction to study drugs or concomitant medication contraindicated with study drugs. Patients already receiving ART were also excluded. Written informed consent was obtained from each participant, or from the next of kin for patients with altered mental status, prior to randomization. Randomisation was stratified by Glasgow Coma Score (GCS) of 15 or <15. Patients were assigned to one of three intervention groups by means of random computer generated lists in block sizes of 8, using numbers in two sets of sealed envelopes (GCS of 15 or <15) prepared by independent persons. Study clinicians opened envelopes in sequence from the appropriate set as patients were enrolled.
The three intervention arms were: (1) Amphotericin B deoxycholate (Fungizone, Bristol-Myers Squibb) 1mg/kg/day by intravenous infusion over 4 hours plus oral flucytosine (Valeant pharmaceuticals) 25mg/kg 4 times per day for 2 weeks (“Standard therapy”), (2) Standard therapy plus Interferon-γ1b (Immukin, Boehringer Ingelheim) 100μg by sub-cutaneous injection on days 1 and 3 (“IFNγ 2-doses”), and (3) Standard therapy plus Interferon-γ1b (Immukin, Boehringer Ingelheim) 100μg by sub-cutaneous injection on days 1, 3, 5, 8, 10 and 12 (“IFNγ 6-doses”).
Unless contraindicated all patients received 1L 0.9% (normal) saline with 20mmol KCl prior to amphotericin B to minimise nephrotoxicity, and were routinely given oral potassium and magnesium supplementation. Amphotericin B was discontinued if the serum creatinine increased to >220μmol/L despite adequate hydration, and patients were switched to fluconazole 400mg/day. When necessary, flucytosine doses were adjusted for reduced renal function, reduced by 50% for grade 3 neutropaenia or thrombocytopaenia, and discontinued for grade 4 neutropaenia or thrombocytopaenia. After 2 weeks all patients received fluconazole (Diflucan, Pfizer) 400mg daily for 8 weeks and 200mg daily thereafter, unless they were taking rifampicin, in which case doses were increased by 50%. Anti-retroviral therapy with stavudine, lamivudine and either efavirenz or nevirapine was initiated between 2 and 4 weeks after starting antifungal therapy, unless contra-indicated, in accordance with South African national guidelines [18, 19], and patients were followed-up for one-year post enrolment with particular attention paid to any clinical presentations related to cryptococcal immune reconstitution inflammatory syndrome (IRIS).
Evaluations and Outcomes
Lumbar punctures (LPs) with opening pressure measurements and quantitative CSF cultures were performed on treatment days 1, 3, 7 and 14. Patients with a markedly elevated opening pressure (>30 cm H20) or symptoms of raised intra-cranial pressure had more frequent LPs in accordance with current guidelines [20], and quantitative cultures were also performed on these samples. CSF samples were analysed to determine the cell count and differential, protein and glucose levels. CSF IFN-γ concentrations were determined using the Luminex multianalyte system (Luminex) and cytokine kits (Bio-Rad), as described elsewhere [16]. Quantitative cryptococcal cultures (QCCs) were plated in serial ten-fold dilution, as previously described [17], and the dilution with the least colonies, but at least 30 colony forming units (CFUs) per 200 μl, was used to calculate CFU/ml. QCC results were verified by laboratory personnel blinded to treatment group. Cryptococcal clearance rates were calculated using a summary statistic for each patient, defined as the decrease in log CFU/ml/day using the slope of the linear regression of log CFU/ml against time for each patient, as previously described [17]. All data points were analyzed except sterile cultures in the second week if these values lessened the slope, as sterility would have been achieved before that day’s LP and this value would therefore underestimate the true slope [17]. All participants had baseline blood tests including hematology, renal and liver function, CD4+ cell counts, and HIV viral load. During the initial 2 weeks patients underwent alternate day renal function and electrolyte assessment and twice weekly haematologic and liver function tests to monitor adverse events. Clinical and laboratory adverse events were graded using the NIH DAIDS Toxicity Table [21]. The primary outcome measure was mean rate of decrease in CSF cryptococcal CFU, also called early fungicidal activity (EFA), for each treatment arm. Secondary outcome measures were mortality at 2 and 10 weeks, serious adverse events and laboratory toxicities.
Statistical analysis
Data were analyzed using Stata, version 11.0 (StataCorp). Variables were compared across groups using Kruskal-Wallis, χ2, or Fisher’s Exact tests as appropriate. An a priori decision was made to use linear regression analysis to compare early fungicidal activity by treatment group (using the standard treatment arm as a comparator), with adjustment for baseline fungal burden and CSF IFN-γ concentration, which were found to be associated with rate of clearance in previous studies [16, 17], and CD4 cell count, giving summary differences with 95% confidence intervals. Statistical significance was defined as p ≤ 0.05.
In an earlier trial, addition of 5FC to AmB was associated with a 74% increase in EFA [17], and standard deviations (SD) for EFA in differing treatment groups ranged from 0.13 to 0.19. Using a SD of 0.18, 27 patients per arm gave 90% power to detect a 30% or greater improvement in early fungicidal activity in either of the experimental arms compared to the standard, at a 5% two-sided significance level. An initial sample size of 120 patients (40 per arm) was set to ensure at least 27 patients per arm with complete data; however, following per-protocol interim analysis in conjunction with the data safety monitoring board at 60 patients, the sample size was reduced to 90 patients as statistically significant differences in the primary endpoint were already present between treatment groups, and retention and data completeness were high.
Role of the funding source
The funding source had no involvement in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. All study drugs were obtained at full cost price from their respective manufacturers.
Results
Ninety patients were randomized, but 2 were subsequently found to meet exclusion criteria (1 previous episode of CM, 1 thrombocytopaenia – figure 1) and were excluded from analyses. Baseline clinical and laboratory characteristics were similar across groups (table 1). At the time of screening 64 patients (71%) were known to be HIV positive, diagnosed a median of 7 months prior to presentation with CM. All enrolled patients were HIV-infected. Overall, the median CD4 cell count was 27 (IQR 14-52) cells/μL, and 37% of patients had abnormal mental status, defined as seizures or GCS < 15 prior to enrolment.
Figure 1.
CONSORT diagram.
Table 1.
Baseline clinical and laboratory characteristics. Results are median (IQR) unless indicated.
| All patients | Control (AmB/5FC) |
AmB/5FC IFNγ 2 doses |
AmB/5FC IFNγ 6 doses |
P value* | |
|---|---|---|---|---|---|
| n | 90 | 31 | 29 | 30 | |
| Age (yrs) | 32 (28-38) | 33 (29-39) | 31 (28-37) | 32 (28-40) | 0.77 |
| Sex (% Male) | 44% (40) | 52% (16) | 38% (11) | 43% (13) | 0.56 |
| Weight (Kg) | 53 (48-59) | 53 (48-59) | 54 (46-60) | 51 (49-57) | 0.93 |
| Duration of symptoms (days) |
14 (7-21) | 14 (7-21) | 14 (7-14) | 12 (7-21) | 0.92 |
| Concurrent TB treatment (%) |
36% (32) | 39% (12) | 34% (10) | 33% (10) | 0.90 |
| Abnormal mental status (%) |
37% (33) | 29% (9) | 41% (12) | 40% (12) | 0.55 |
| Baseline CD4 count (×106/ml) |
27 (14-51) | 36 (18-63) | 22 (11-51) | 22 (14-46) | 0.34 |
| Viral load (copies/ml) |
120,000 (28,000- 300,000) |
120,000 (40,000- 235,000) |
97,000 (13,000- 280,000) |
130,000 (28,000- 450,000) |
0.48 |
| CSF OP (cmH20) | 26 (15-38) | 28 (15-40) | 26 (16-34) | 26 (15-38) | 0.82 |
| CSF Nϕ count (×106/L) |
0 (0-1) | 0 (0-2) | 0 (0-0) | 0 (0-3) | 0.23 |
| CSF Lϕ count (×106/L) |
14 (0-72) | 25 (4-122) | 3 (0-57) | 25 (1-67) | 0.09 |
| CSF protein (g/dL) | 0.97 (0.55- 1.54) |
1.09 (0.65- 1.36) |
0.79 (0.42- 1.68) |
0.97 (0.55- 1.25) |
0.72 |
| CSF glucose (mmol/L) |
2.1 (1.3-2.5) | 2.0 (1.4-2.7) | 2.0 (1.6-2.4) | 2.25 (1.1-2.6) | 0.84 |
| India Ink +ve (%) | 92% (83) | 90% (28) | 97% (28) | 90% (27) | 0.57 |
| Baseline fungal burden (CFU/ml CSF) |
240,000 (36,500- 745,000) |
240,000 (16,000- 535,000) |
517,500 (67,000- 1,895,000) |
90,750 (10,100- 650,000) |
0.06 |
| CSF interferon-γ conc. (pg/ml) |
52.1 (20-86) | 56.2 (20-74) | 32.2 (14-86) | 64.4 (20-92) | 0.46 |
| Hb (g/dL) | 11.5 (9.8- 12.6) |
12.0 (9.9- 12.6) |
11.0 (9.5- 12.4) |
11.7 (9.8- 13.3) |
0.40 |
| Creatinine (μmol/L) | 72 (62-80) | 73 (66-80) | 69 (61-74) | 76 (61-89) | 0.29 |
P-values calculated using the Kruskal-Wallis, χ2 or Fisher’s Exact tests as appropriate.
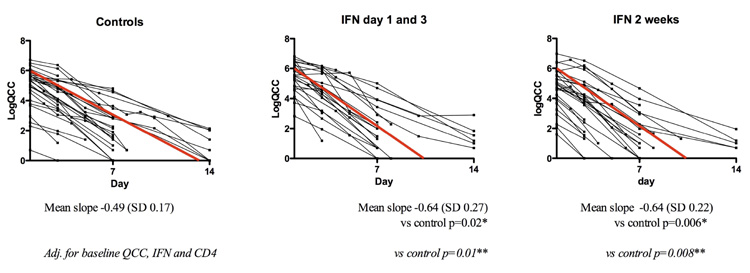
Early Fungicidal Activity
The rate of fungal clearance was more rapid in the two IFN-γ containing arms than in the standard treatment arm (figure 2). The mean (SD) EFA was −0.49 (0.17) with standard treatment, −0.64 (0.27) with IFNγ 2-doses, and −0.64 (0.22) with IFNγ 6-doses. The difference in EFA was −0.15 logCFU/ml/day (95% CI −0.02 to −0.27, p=0.02) between standard treatment and IFNγ 2-doses, and −0.15 logCFU/ml/day (95% CI −0.05 to −0.26, p=0.006) between standard treatment and IFNγ 6-doses. Adjusting for baseline fungal burden, baseline CSF IFNγ concentration and baseline CD4 count did not alter the strength of association between treatment group and EFA (p=0.01 control vs IFNγ 2-doses, and p=0.008 control vs IFNγ 6-doses). Further adjusting for additional factors including age, sex, weight, CSF lymphocyte count and concurrent TB treatment did not significantly change the relationship between treatment group and EFA.
Figure 2.
Early fungicidal activity (EFA) by treatment group. The figure shows the individual patient slopes over the initial 14 days of treatment. The red line is a graphic representation of the mean slope in each treatment group. Mean slope (standard deviation) is given below each plot, with a p-value for both unadjusted and adjusted (for baseline CD4 cell count, CSF IFN γ and fungal burden) comparisons with control.
Mortality
The mortality at 2 weeks was 19% (6 of 31) in the control group, 15% (4 of 27) in the IFNγ 2-doses group and 13% (4 of 30) in the IFNγ 6-doses, with no significant difference between groups (see table 2). At 10 weeks the mortality was 32% (10 of 31), 33% (9 of 27) and 27% (8 of 30) in the control, IFNγ 2-doses, and IFNγ 6-doses groups respectively. The factors associated with mortality at 10 weeks in bivariate analysis were high baseline fungal burden (p=0.02), abnormal mental status (p=0.03), and low body-weight at admission (p=0.002). Most deaths in the first 2 weeks were due to cryptococcal meningitis (13 of 14), while the majority of those occurring between weeks 2 and 10 were due to other AIDS related opportunistic infections (10 of 13, see table 3).
Table 2.
Outcomes$
| All patients |
Control (AmB/5FC) |
AmB/5FC IFNγ 2 doses |
AmB/5FC IFNγ 6 doses |
P value* | |
|---|---|---|---|---|---|
| n | 90 | 31 | 27 | 30 | |
| Mean slope (log10 CFU/ml/d) |
−0.59 | −0.49 | −0.64 | −0.64 | 0.02/0.006 |
| Median slope (log10 CFU/ml/d) |
−0.56 | −0.48 | −0.57 | −0.62 | 0.04/0.01 |
| 2 week mortality (%) |
16% (14) | 19% (6) | 15% (4) | 13% (4) | 0.82 |
| 10 wk mortality (%) |
31% (27) | 32% (10) | 33% (9) | 27% (8) | 0.84 |
P-values calculated using linear regression modeling (mean slope, vs control), Rank-Sum testing (median slopes, vs control) or χ2 tests (mortality)
Two patients were excluded from the analysis as they were found to have exclusion criteria following enrollment (one previous episode of CM, on severe thrombocytopaenia).
Table 3.
Safety data.
| All patients |
Control (AmB/5FC) |
AmB/5FC IFNγ 2 doses |
AmB/5FC P IFNγ 6 doses |
P value * |
|
|---|---|---|---|---|---|
| n | 90 | 31 | 27 $ | 30 | |
| Deaths (due to Cryptococcosis) |
16 | 6 | 6 | 4 | 0.65 |
| Deaths (Other causes) |
11 | 4 (HIV wasting syndrome, nosocomial pneumonia, 2 x sepsis) |
3 (nosocomial pneumonia/HIV encephalopathy, gastroenteritis) |
4 (2 x sepsis, TB, unknown) |
0.98 |
| Grade 4 clinical SAE |
23 | 9 (2 x diarrhoea and vomiting, 2 x seizures, 2 x pneumonia, cryptococcal IRIS, GI bleed, scalp laceration) |
8 (2 x vomiting, 2 x sepsis, persistent raised ICP, otitis externa, MRSA drip site/TB infection, cerebral infarct) |
6 (nevirapine toxicity, angioedema, persistent raised ICP, probable PCP, cryptococcal IRIS, TB) |
0.49 |
| Grade 3 |
Lab
SAEs |
||||
| Anaemia | 14 (16%) |
6 (19%) | 4 (15%) | 4 (13%) | 0.88 |
| Leukopaenia | 5 (6%) | 1 (3%) | 2 (8%) | 2 (7%) | 0.74 |
| Neutropaenia | 4 (5%) | 1 (3%) | 1 (4%) | 2 (7%) | 0.84 |
| Thrombocytopaenia | 4 (5%) | 1 (3%) | 1 (4%) | 2 (7%) | 0.84 |
| ALT | 0 | 0 | 0 | 0 | ---- |
| Creatinine | 18 (21%) |
7 (23%) | 5 (19%) | 6 (20%) | 1.00 |
| Potassium↓ | 2 (2%) | 0 | 1 (4%) | 1 (3%) | 0.54 |
| Magnesium↓ | 22 (25%) |
6 (19%) | 9 (35%) | 7 (23%) | 0.40 |
| Sodium↓ | 5 (6%) | 3 (10%) | 0 | 2 (7%) | 0.37 |
| Grade 4 |
Lab
SAEs |
||||
| Anaemia | 17 (18%) |
4 (13%) | 7 (27%) | 6 (20%) | 0.42 |
| Leukopaenia | 0 | 0 | 0 | 0 | ---- |
| Neutropaenia | 3 (3%) | 1 (3%) | 1 (4%) | 1 (3%) | 1.00 |
| Thrombocytopaenia | 1 (1%) | 1 (3%) | 0 | 0 | 1.00 |
| ALT | 0 | 0 | 0 | 0 | ---- |
| Creatinine* | 0 | 0 | 0 | 0 | ---- |
| Potassium↓ | 1 (1%) | 0 | 0 | 1 (3%) | 0.64 |
| Magnesium↓ | 5 (6%) | 1 (3%) | 2 (8%) | 2 (7%) | 0.74 |
| Sodium↓ | 2 (2%) | 0 | 1 (4%) | 1 (3%) | 0.54 |
| IRIS | |||||
| IRIS** | 9/65 (14%) |
2/23 (9%) | 2/18 (11%) | 5/24 (21%) | 0.55 |
| Time to IRIS (days) | 60 (24- 115) |
64 (12-115) | 24 (19-29) | 110 (60-116) | 0.32 |
P-values calculated using the Kruskal-Wallis or χ2 tests as appropriate.
One patient in this group absconded on day 2 of treatment, and although known to be alive at 2 and 10 weeks, has no reportable laboratory safety monitoring data, hence denominator is 26 for laboratory SAEs.
Expressed as percentage of patients who initiated ART.
Baseline CSF interferon-γ concentrations
Baseline CSF IFN-γ concentration was positively associated with CSF lymphocyte count (p=0.047) and CSF protein (p<0.001); and negatively associated with baseline log10 fungal burden (p=0.001). After adjustment for treatment group, baseline CSF IFN-γ concentration was positively associated with increasing EFA (p=0.02). There was no association between IFN-γ concentration and CD4 cell count, abnormal mental status, or CSF opening pressure (p=0.3, 0.4 and 0.9 respectively).
Safety
All treatment arms were tolerated by the majority of participants, with 8 patients (9%) having treatment interrupted or discontinued due to drug toxicities. Nearly all drug related adverse events reported were related to amphotericin B, with anaemia being the primary problem, as previously reported [6] (see table 3). Overall, 17 patients (18%) developed DAIDS grade 4 anaemia (Hb < 6.5g/dL) during the first 2 weeks of treatment, with no significant difference between treatment groups. The median fall in Hb from admission to nadir value was 3.1g/dL (IQR 2.1-4.2g/gL with no significant variation across treatment groups. No patients developed DAIDS grade 4 renal impairment, however 8 patients had amphotericin B discontinued (2 only temporarily) due to rises in creatinine, at a median of 9 days (IQR 6-11) into therapy (3 in the standard therapy arm, 3 IFNγ 2-doses and 2 IFNγ 6-doses). Of note three of these patients had concurrent sepsis, and subsequently died. The remaining patients all had full resolution of renal function abnormalities. Rates of neutropaenia, thrombocytopaenia, and other adverse events attributable to flucytosine or IFN-γ were low.
Immune reconstitution syndromes (IRIS)
Cryptococcal IRIS was diagnosed in 14% of patients initiating ART (9 of 65), occurring at a median of 60 days (IQR 24-115 days) post ART initiation, with no significant difference in proportions between treatment groups (table 3). Patients who developed IRIS had lower CD4 counts at the time of initial CM presentation (16 cells/μl vs 36 cells/μl, p=0.06), a less inflammatory CSF at initial CM presentation as evidenced by lower CSF lymphocyte counts (13 ×106/L vs 28 ×106/L, p=0.1) and CSF IFN-γ concentrations (19.9 pg/ml vs 59.4 pg/ml, p=0.1), and a significantly higher baseline fungal burden (5.53 log10CFU/ml CSF vs 5.03 log10CFU/ml CSF, p=0.04) and slower rate of fungal clearance (EFA −0.38 log10CFU/ml/d vs −0.58 log10CFU/ml/d, p=0.04) during initial CM presentation. This was reflected in the significantly higher fungal burden at the end of initial anti-fungal therapy in those who subsequently developed IRIS (1.95 log10CFU/ml CSF versus 0 log10CFU/ml CSF, p=0.006). The median time to ART initiation was exactly the same in patients who did and did not subsequently develop IRIS (a median of 23 days after commencing antifungal therapy).
Long-term outcomes
Patients who survived the initial 10-weeks were followed-up for a median of 1 year, and 97% commenced ART (59 of 61). There were 3 deaths during this period (2 were patients who defaulted ART and regular follow-up, and 1 died of unknown causes at home). At 6 months, 53 (60%) patients were alive, 29 (33%) were dead, and 6 (7%) were lost to follow-up, the median CD4 count was 131 cells/μL (IQR 75-185), and 80% had an undetectable HIV-viral load. By 1-year 30 patients were known to have died (34%), 8 (9%) were lost to follow-up, the median CD4 count was 167 cells/μL (121-222), and 83% of patients had an undetectable HIV-viral load.
Discussion
The addition of short course adjunctive interferon-γ to standard amphotericin B and flucytosine treatment significantly increased the rate of clearance of cryptococcal infection from the CSF of patients with HIV-associated cryptococcal meningitis. Two doses of interferon-γ were as effective as a full two-week course, and the addition of adjunctive interferon-γ was not associated with any increase in drug related adverse events or IRIS. These data confirm the results of an earlier phase two study examining the safety and efficacy of adjunctive interferon-γ, which showed it to be well tolerated, and suggested a trend toward improved combined mycologic and clinical success in interferon-γ recipients [7].
Although this study was not powered to detect mortality differences between treatment arms, overall mortality was lower, but not statistically significant, in interferon-γ treated patients than controls at 2 weeks (14%, 8/57 vs 19%, 6/31) and similar at 10 weeks (30%, 17/57 vs 32%, 10/31), despite a trend towards the control group having higher CD4 cell counts and a lower proportion of patients with abnormal mental status at baseline. Of note, rate of clearance of cryptococci from the CSF, measured by EFA, has been previously shown to be independently associated with mortality in a large combined cohort analysis [22].
The patients in our study had severe cryptococcal disease, with 37% having abnormal mental status, and high fungal burdens at presentation. The mortality of 16% at 2-weeks and 31% at 10-weeks was in keeping with this, and similar to other African cohorts [4-6]. As previously described [17, 22], the key predictors of mortality were high fungal burden and abnormal mental status at presentation. Low weight was also predictive of mortality. In this cohort of patients who had frequent lumbar punctures and aggressive management of raised CSF pressures as per current guidelines [20], baseline CSF opening pressure was not a predictor of mortality, in keeping with what we have previously shown in patients managed according to this study protocol [23]; in fact survivors tended to have higher baseline CSF opening pressures that patients who died.
Despite high early mortality, long-term outcomes were good in patients who survived the acute infection. Although ART was initiated early (a median of 23 days post initiation of anti-fungal treatment), the low rates of IRIS seen overall in the cohort, and absence of IRIS deaths, suggest that relatively early ART initiation is safe in patients who receive adequate amphotericin B induction therapy.
It is worth noting that many of the cases of cryptococcal meningitis included in this study could potentially have been prevented had ART been initiated soon after HIV diagnosis, particularly if combined with cryptococcal antigen screening to identify and treat patients with sub-clinical cryptococcal infection [24, 25]. In keeping with previously reported data from South Africa [26], the majority of these ART-naïve patients had been diagnosed with HIV-infection many months before presentation with cryptococcal meningitis but not started treatment. Efforts to improve linkage from testing to care, and quickly establish vulnerable patients on treatment are essential.
The mechanism by which exogenous interferon-γ stimulates more rapid clearance of Cryptococcus from the CSF has not yet been elucidated, but probably results from the direct activation of effector cells such as macrophages [27, 28] and microglial cells [13], stimulating intracellular killing, and favouring protective Th1 [29] rather than detrimental Th2-type immune respones [30]. Cytokines that induce a Th1 response including IL12, and IL-18, and TNF-a have been shown to promote protection through interferon-γ dependent mechanisms [31, 32], and interferon-γ, produced either peripherally or in the CNS, has been shown to stimulate microglial cell activation and anti-cryptococcal activity [13, 33].
This study is the first to demonstrate a clear beneficial biological effect of exogenous interferon-γ in the treatment of an opportunistic infectious disease. Use of a statistically powerful marker of response to therapy (EFA) enabled two dosage schedules to be examined. Very short courses of immunotherapy may be as effective, while being less expensive and more easily implemented, than longer courses - a finding that could have implications for the use of interferon-γ in other infectious diseases, especially where endogenous cytokine responses have been shown to evolve rapidly [16]. At a cost of £66.67 per dose (approximately US$100 – British National Formulary price 2010), a 2-dose course of adjunctive interferon-γ would be economically feasible in many settings. Work is ongoing to identify patient groups in whom adjunctive interferon-γ would be most beneficial, and these results need further validation in clinical endpoint studies. The study highlights the potential role of cytokine immunotherapy with interferon-γ in both cryptococcal meningitis, and the broad range of other opportunistic infections requiring robust Th1 type immunity for effective host defence.
Acknowledgements
JNJ, GM and TB are supported by the Wellcome Trust, London, UK (WT081794 and WT081667). GM also received SATBAT research training that was Fogarty International Center and NIH-funded (NIH/FIC 1U2RTW007373 and 5U2RTW007370). CS received a Fogarty International Center South Africa TB/AIDS Training Award: U2RTW007373 ICORTA. We thank Jara Llenas García and Nicky Longley for assistance with patient recruitment and follow-up.
Funding Wellcome Trust.
Footnotes
Author’s contributions JNJ designed and implemented the study, analysed the data and wrote the manuscript. GM implemented the study and edited the manuscript, KR assisted in study implementation, GNW was the research nurse, TB assisted in study implementation, AW provided laboratory support, CS assisted in study implementation, LGB and RW supervised implementation and critically reviewed the manuscript, TSH conceptualized and designed the study, supervised implementation and helped draft the manuscript. All authors reviewed the final manuscript.
Conflict of Interests None to declare.
References
- 1.Jarvis JN, Harrison TS. HIV-associated cryptococcal meningitis. Aids. 2007;21:2119–2129. doi: 10.1097/QAD.0b013e3282a4a64d. [DOI] [PubMed] [Google Scholar]
- 2.Jarvis JN, Boulle A, Loyse A, Bicanic T, Rebe K, Williams A, et al. High ongoing burden of cryptococcal disease in Africa despite antiretroviral roll out. Aids. 2009;23:1181–1185. doi: 10.1097/QAD.0b013e32832be0fc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jarvis JN, Meintjes G, Williams A, Brown Y, Crede T, Harrison TS. Adult meningitis in a setting of high HIV and TB prevalence: findings from 4961 suspected cases. BMC Infect Dis. 2010;10:67. doi: 10.1186/1471-2334-10-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jarvis JN, Meintjes G, Harrison TS. Outcomes of cryptococcal meningitis in antiretroviral naive and experienced patients in South Africa. J Infect. 2010;60:496–498. doi: 10.1016/j.jinf.2010.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bicanic T, Meintjes G, Wood R, Hayes M, Rebe K, Bekker LG, Harrison T. Fungal burden, early fungicidal activity, and outcome in cryptococcal meningitis in antiretroviral-naive or antiretroviral-experienced patients treated with amphotericin B or fluconazole. Clin Infect Dis. 2007;45:76–80. doi: 10.1086/518607. [DOI] [PubMed] [Google Scholar]
- 6.Bicanic T, Wood R, Meintjes G, Rebe K, Brouwer A, Loyse A, et al. High-dose amphotericin B with flucytosine for the treatment of cryptococcal meningitis in HIV-infected patients: a randomized trial. Clin Infect Dis. 2008;47:123–130. doi: 10.1086/588792. [DOI] [PubMed] [Google Scholar]
- 7.Pappas PG, Bustamante B, Ticona E, Hamill RJ, Johnson PC, Reboli A, et al. Recombinant interferon-gamma 1b as adjunctive therapy for AIDS-related acute cryptococcal meningitis. J Infect Dis. 2004;189:2185–2191. doi: 10.1086/420829. [DOI] [PubMed] [Google Scholar]
- 8.Aguirre K, Havell EA, Gibson GW, Johnson LL. Role of tumor necrosis factor and gamma interferon in acquired resistance to Cryptococcus neoformans in the central nervous system of mice. Infect Immun. 1995;63:1725–1731. doi: 10.1128/iai.63.5.1725-1731.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kawakami K, Tohyama M, Teruya K, Kudeken N, Xie Q, Saito A. Contribution of interferon-gamma in protecting mice during pulmonary and disseminated infection with Cryptococcus neoformans. FEMS Immunol Med Microbiol. 1996;13:123–130. doi: 10.1016/0928-8244(95)00093-3. [DOI] [PubMed] [Google Scholar]
- 10.Kawakami K, Qureshi MH, Zhang T, Koguchi Y, Shibuya K, Naoe S, Saito A. Interferon-gamma (IFN-gamma)-dependent protection and synthesis of chemoattractants for mononuclear leucocytes caused by IL-12 in the lungs of mice infected with Cryptococcus neoformans. Clin Exp Immunol. 1999;117:113–122. doi: 10.1046/j.1365-2249.1999.00955.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Uicker WC, Doyle HA, McCracken JP, Langlois M, Buchanan KL. Cytokine and chemokine expression in the central nervous system associated with protective cell-mediated immunity against Cryptococcus neoformans. Med Mycol. 2005;43:27–38. doi: 10.1080/13693780410001731510. [DOI] [PubMed] [Google Scholar]
- 12.Wormley FL, Jr., Perfect JR, Steele C, Cox GM. Protection against cryptococcosis by using a murine gamma interferon-producing Cryptococcus neoformans strain. Infect Immun. 2007;75:1453–1462. doi: 10.1128/IAI.00274-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou Q, Gault RA, Kozel TR, Murphy WJ. Protection from direct cerebral cryptococcus infection by interferon-gamma-dependent activation of microglial cells. J Immunol. 2007;178:5753–5761. doi: 10.4049/jimmunol.178.9.5753. [DOI] [PubMed] [Google Scholar]
- 14.Perfect JR, Granger DL, Durack DT. Effects of antifungal agents and gamma interferon on macrophage cytotoxicity for fungi and tumor cells. J Infect Dis. 1987;156:316–323. doi: 10.1093/infdis/156.2.316. [DOI] [PubMed] [Google Scholar]
- 15.Joly V, Saint-Julien L, Carbon C, Yeni P. In vivo activity of interferon-gamma in combination with amphotericin B in the treatment of experimental cryptococcosis. J Infect Dis. 1994;170:1331–1334. doi: 10.1093/infdis/170.5.1331. [DOI] [PubMed] [Google Scholar]
- 16.Siddiqui AA, Brouwer AE, Wuthiekanun V, Jaffar S, Shattock R, Irving D, et al. IFN-gamma at the site of infection determines rate of clearance of infection in cryptococcal meningitis. J Immunol. 2005;174:1746–1750. doi: 10.4049/jimmunol.174.3.1746. [DOI] [PubMed] [Google Scholar]
- 17.Brouwer AE, Rajanuwong A, Chierakul W, Griffin GE, Larsen RA, White NJ, Harrison TS. Combination antifungal therapies for HIV-associated cryptococcal meningitis: a randomised trial. Lancet. 2004;363:1764–1767. doi: 10.1016/S0140-6736(04)16301-0. [DOI] [PubMed] [Google Scholar]
- 18.National Antiretroviral Treatment Guidelines. National Department of Health; South Africa: 2004. [Google Scholar]
- 19.Southern African HIV Clinicians Society Guidelines for the Prevention, Diagnosis and Management of Cryptococcal Meningitis and Disseminated Cryptococcosis in HIV-infected Patients. Southern African Journal of HIV Medicine. 2007;28:25–35. [Google Scholar]
- 20.Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2010;50:291–322. doi: 10.1086/649858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.NIH Division of Aids Table for Grading the Severity of Adult and Pediatric Adverse Events. (Version 1) 2004 Dec; [Google Scholar]
- 22.Bicanic T, Muzoora C, Brouwer AE, Meintjes G, Longley N, Taseera K, et al. Independent association between rate of clearance of infection and clinical outcome of HIV-associated cryptococcal meningitis: analysis of a combined cohort of 262 patients. Clin Infect Dis. 2009;49:702–709. doi: 10.1086/604716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bicanic T, Brouwer AE, Meintjes G, Rebe K, Limmathurotsakul D, Chierakul W, et al. Relationship of cerebrospinal fluid pressure, fungal burden and outcome in patients with cryptococcal meningitis undergoing serial lumbar punctures. Aids. 2009;23:701–706. doi: 10.1097/QAD.0b013e32832605fe. [DOI] [PubMed] [Google Scholar]
- 24.Jarvis JN, Lawn SD, Vogt M, Bangani N, Wood R, Harrison TS. Screening for Cryptococcal Antigenemia in Patients Accessing an Antiretroviral Treatment Program in South Africa. Clin Infect Dis. 2009;48:856–862. doi: 10.1086/597262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jarvis JN, Lawn SD, Wood R, Harrison TS. Cryptococcal antigen screening for patients initiating antiretroviral therapy: time for action. Clin Infect Dis. 2010;51:1463–1465. doi: 10.1086/657405. [DOI] [PubMed] [Google Scholar]
- 26.Jarvis JN, Meintjes G, Wood R, Harrison TS. Testing but not treating: missed opportunities and lost lives in the South African antiretroviral therapy programme. Aids. 2010;24:1233–1235. doi: 10.1097/QAD.0b013e3283383aeb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Flesch IE, Schwamberger G, Kaufmann SH. Fungicidal activity of IFN-gamma-activated macrophages. Extracellular killing of Cryptococcus neoformans. J Immunol. 1989;142:3219–3224. [PubMed] [Google Scholar]
- 28.Voelz K, Lammas DA, May RC. Cytokine signaling regulates the outcome of intracellular macrophage parasitism by Cryptococcus neoformans. Infect Immun. 2009;77:3450–3457. doi: 10.1128/IAI.00297-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hardison SE, Ravi S, Wozniak KL, Young ML, Olszewski MA, Wormley FL., Jr Pulmonary infection with an interferon-gamma-producing Cryptococcus neoformans strain results in classical macrophage activation and protection. Am J Pathol. 2010;176:774–785. doi: 10.2353/ajpath.2010.090634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arora S, Hernandez Y, Erb-Downward JR, McDonald RA, Toews GB, Huffnagle GB. Role of IFN-gamma in regulating T2 immunity and the development of alternatively activated macrophages during allergic bronchopulmonary mycosis. J Immunol. 2005;174:6346–6356. doi: 10.4049/jimmunol.174.10.6346. [DOI] [PubMed] [Google Scholar]
- 31.Kawakami K, Qureshi MH, Zhang T, Okamura H, Kurimoto M, Saito A. IL-18 protects mice against pulmonary and disseminated infection with Cryptococcus neoformans by inducing IFN-gamma production. J Immunol. 1997;159:5528–5534. [PubMed] [Google Scholar]
- 32.Herring AC, Lee J, McDonald RA, Toews GB, Huffnagle GB. Induction of interleukin-12 and gamma interferon requires tumor necrosis factor alpha for protective T1-cell-mediated immunity to pulmonary Cryptococcus neoformans infection. Infect Immun. 2002;70:2959–2964. doi: 10.1128/IAI.70.6.2959-2964.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aguirre K, Miller S. MHC class II-positive perivascular microglial cells mediate resistance to Cryptococcus neoformans brain infection. Glia. 2002;39:184–188. doi: 10.1002/glia.10093. [DOI] [PubMed] [Google Scholar]