Abstract
Objectives
To estimate, overall and by organism, the incidence of infectious intestinal disease (IID) in the community, presenting to general practice (GP) and reported to national surveillance.
Design
Prospective, community cohort study and prospective study of GP presentation conducted between April 2008 and August 2009.
Setting
Eighty-eight GPs across the UK recruited from the Medical Research Council General Practice Research Framework and the Primary Care Research Networks.
Participants
6836 participants registered with the 88 participating practices in the community study; 991 patients with UK-acquired IID presenting to one of 37 practices taking part in the GP presentation study.
Main outcome measures
IID rates in the community, presenting to GP and reported to national surveillance, overall and by organism; annual IID cases and GP consultations by organism.
Results
The overall rate of IID in the community was 274 cases per 1000 person-years (95% CI 254 to 296); the rate of GP consultations was 17.7 per 1000 person-years (95% CI 14.4 to 21.8). There were 147 community cases and 10 GP consultations for every case reported to national surveillance. Norovirus was the most common organism, with incidence rates of 47 community cases per 1000 person-years and 2.1 GP consultations per 1000 person-years. Campylobacter was the most common bacterial pathogen, with a rate of 9.3 cases per 1000 person-years in the community, and 1.3 GP consultations per 1000 person-years. We estimate that there are up to 17 million sporadic, community cases of IID and 1 million GP consultations annually in the UK. Of these, norovirus accounts for 3 million cases and 130 000 GP consultations, and Campylobacter is responsible for 500 000 cases and 80 000 GP consultations.
Conclusions
IID poses a substantial community and healthcare burden in the UK. Control efforts must focus particularly on reducing the burden due to Campylobacter and enteric viruses.
Keywords: Campylobacter, diarrhoeal disease, epidemiology, infectious diarrhoea, salmonella
Significance of this study.
What is already known about this subject?
Infectious intestinal disease (IID) is a common cause of illness in the community and results in a high burden of consultations to general practice (GP).
Most cases of IID are not reported to national surveillance systems, making it difficult to determine the true burden in the population.
Recent interventions and changes in healthcare delivery may have resulted in changes in disease burden in the community and presenting to primary care; population-based studies are needed to monitor such changes.
What are the new findings?
In the UK, there are up to 17 million cases and 1 million GP consultations due to IID every year.
Although IID incidence in the community appears to have increased since the 1990s, consultations to GP have halved.
Norovirus is the most common recognised cause of IID, accounting for 3 million cases and 130 000 GP consultations annually, while Clostridium difficile, an important pathogen in healthcare settings, is a rare cause of diarrhoea in the community.
How might it impact on clinical practice in the foreseeable future?
Use of recently introduced telephone advice services such as NHS Direct is relatively low and has little impact on the burden of GP consultations for IID. Instead, changes in healthcare use are likely to be behind the decreasing trend in IID-related GP consultations.
Background
The Health Protection Agency recorded 49 880 laboratory-confirmed cases of infectious intestinal disease (IID) due to Campylobacter and 9885 cases of non-typhoidal salmonellosis in England and Wales in 20081 2; rotavirus and norovirus accounted for 13 935 and 6828 reports, respectively.3 4 Most IID is self-limiting, requiring no clinical intervention, but commonly causes high levels of healthcare usage and absenteeism.5 Organisms such as verocytotoxin-producing Escherichia coli (VTEC) and Campylobacter are also associated with long-term, potentially fatal sequelae, including haemolytic uraemic syndrome6 and Guillain–Barré syndrome.7
National statistics underestimate the incidence, because only a fraction of IID presents to health services, and many presenting cases are not investigated further. Reported cases are not a random subset of all cases, as seeking healthcare is related to greater disease severity, recent foreign travel and lower socioeconomic status.8 National statistics can be useful for monitoring trends, but difficult to interpret if there are secular changes in healthcare-seeking behaviour, faecal sampling, diagnostic procedures or surveillance methods. Evaluating control strategies requires accurately estimating population burden and understanding the relationship between national statistics and disease incidence.
In its first 5 years of operation the UK, Food Standards Agency was tasked with reducing food-borne illness by 20%.9 The Second Study of IID in the UK (IID2 Study) was commissioned to assess progress towards this target and determine whether changes in healthcare provision might influence the interpretation of national statistics.
We present results from the IID2 Study, a multicentre longitudinal study to estimate the current incidence of IID in the community, presenting to general practice (GP) and reported to national surveillance.
Methods
The IID2 Study methods are detailed elsewhere.10 Briefly, we conducted the study between 28 April 2008 and 31 August 2009 in a population of 800 000 people served by 88 UK GPs. We recruited practices from the Medical Research Council General Practice Research Framework and Primary Care Research Networks in England, Northern Ireland and Scotland. The number of practices in the four UK countries was proportional to population size. The study comprised a population cohort, a GP presentation study and a national surveillance study.
Population cohort study
We followed up participants from 88 practices weekly for symptoms of diarrhoea and/or vomiting for up to 52 weeks, recruiting throughout the study period. From each practice list, we invited randomly selected individuals to a recruitment interview with the practice study nurse. People were eligible if they did not have: a terminal illness or severe mental incapacity; a recognised, non-infectious cause of diarrhoea or vomiting (precluding determination of onset date and infectious aetiology), such as Crohn's disease, ulcerative colitis, cystic fibrosis or coeliac disease; or a surgical obstruction. Non-English speakers were also excluded.
We asked participants to report weekly, by email or prepaid postcard, whether or not they had experienced diarrhoea and/or vomiting. We asked those reporting symptoms to complete a case questionnaire, enquiring about type and duration of symptoms, healthcare usage and recent travel, and to submit a stool specimen for microbiological examination. We asked them not to report symptoms related to excess alcohol, morning sickness or, among infants, regurgitation.
GP presentation study
In 37 of the 88 participating practices, we asked GPs to refer to the study nurse all patients presenting with IID. The nurse administered a case questionnaire and requested a stool specimen. To assess the degree of under-ascertainment of IID cases in this study (ie, the proportion of all IID cases actually referred and recruited to the study), study nurses searched the computerised practice records monthly, using a predefined list of diagnostic Read codes,11 to identify all IID-related consultations.
National surveillance study
We obtained records of IID cases reported in each UK country over the study period, by organism, from the UK national surveillance centres. Data on sapovirus and non-O157 VTEC were not available, because they are not routinely reported. We excluded national C difficile reports because these are mostly from healthcare settings rather than the community.
NHS direct usage
We obtained the number of telephone consultations to NHS Direct (England only) for diarrhoea and vomiting during the study period from the Health Protection Agency Birmingham Regional Surveillance Unit.
Ethics approval
All participants gave signed, informed consent. The North West Research Ethics Committee granted a favourable ethics opinion (07/MRE08/5), and 37 NHS Research Management and Governance organisations for the 88 practices approved the study.
Case definitions
Definite IID was defined as loose stools or clinically significant vomiting lasting less than 2 weeks, in the absence of a known non-infectious cause, preceded by a symptom-free period of 3 weeks. Vomiting was clinically significant if it occurred more than once in a 24 h period and if it incapacitated the patient or was accompanied by other symptoms such as cramps or fever.10 12 Symptomatic people not meeting the case definition because they did not provide a questionnaire or because symptom information was missing were considered possible IID cases. Cases in which the patient reported travel outside the UK in the 10 days before illness onset were excluded.
Microbiological analysis
First, all stool samples were cultured for Campylobacter jejuni/coli, E coli O157, Listeria monocytogenes, Salmonella spp., Shigella spp. and Yersinia spp. They were also examined by ELISA for Clostridium perfringens enterotoxin, C difficile cytotoxins A and B, Cryptosporidium and Giardia, by a commercial PCR test (Cepheid) for C difficile, and by light microscopic examination of a stained smear for Cyclospora and Cryptosporidium. Samples that were immunoassay positive for C difficile toxin or PCR-positive were cultured using National Standard Method BSOP 10, and all isolates were ribotyped.13 Samples from children under 5 years were examined for rotavirus and adenovirus 40/41 by immunoassay.
Next, two nucleic acid extracts were prepared from each stool sample.14–16 Each extract was examined by real-time PCR for C jejuni, C coli, L monocytogenes, Salmonella spp., rotavirus, norovirus, sapovirus, adenovirus, astrovirus, Cryptosporidium, Giardia and E coli (enteroaggregative and VTEC (genes encoding VT1 and VT2)).
Further information on microbiological methods has been published elsewhere.10 For quantitative PCR assays, a cycle threshold value <40 was considered positive for most organisms, with two exceptions: a cycle threshold cut-off value <30 was used to define clinically significant norovirus and rotavirus infection.17 18
In this study, C difficile-associated diarrhoea (CDAD) was defined as symptoms of diarrhoea not attributable to another cause (ie, in the absence of other enteropathogens), but with a positive C difficile toxin assay, in a patient aged >2 years.19
Data analysis
We calculated incidence rates of IID with 95% CIs, overall and by organism. In the cohort study, the denominator was the total person-years at risk among cohort participants. Individuals could contribute multiple episodes of illness. We omitted the first 3 weeks of follow-up to exclude prevalent cases. Participants were followed-up until the 52nd week, or 31 August 2009, or until they dropped out or withdrew for other reasons, whichever occurred earliest. People were ‘dropped out’ after four consecutive non-response weeks.
In the GP presentation study, the denominator in each practice was the practice population on 31 December 2008 multiplied by the time the practice was in the study. For the national surveillance component, the denominator was the UK midyear population at the 2001 census. For the NHS Direct component, the mid-2001 England population was used.
Statistical adjustments
We standardised rates in the cohort study to the UK census age and sex population structure. We adjusted rates in the GP presentation study by an under-ascertainment factor representing the ratio of all cases identified in the practice records to actual cases recruited. We obtained the under-ascertainment factors from a two-level logistic regression model using age group, sex, Read code category, and a random intercept for GP practice to predict the probability of a case being recruited. We grouped the Read codes assigned to each consultation into seven categories: diarrhoea; vomiting; diarrhoea and vomiting; gastroenteritis; organism-specific codes; codes indicating that a stool sample was sent for analysis; and codes for symptoms compatible with IID, for example, ‘gastrointestinal symptoms’. We used the inverse of the predicted ascertainment probabilities obtained from the model as under-ascertainment factors in the incidence calculations.
CIs accounted for clustering of observations within individuals (cohort study) and within practices (GP presentation study).
Imputation of specimen data
We used multiple imputation by chained equations20 to account for missing organism data in participants who did not submit a specimen. We developed separate imputation models for cases in the cohort and GP presentation studies. For each organism, the imputation model included age group, sex and presence or absence of five symptoms (diarrhoea, bloody diarrhoea, vomiting, abdominal pain and fever) as covariates. Overall, we imputed values for 35% of records in the cohort study and 11% of records in the GP presentation study. We combined results from analysis of 20 imputed datasets to produce a point estimate for the rate and 95% CI, accounting for uncertainty in the observed rate and the imputation process.
Reporting ratios
We calculated rate ratios comparing rates in the community, presenting to the GP and reported to national surveillance. We assumed that the rates came from a log-normal distribution with the observed mean and SD. The rate ratios were estimated by simulating 100 000 random draws from each pair of rate distributions. We took the median, 2.5th and 97.5th centiles of the resulting RR distribution as the point estimate and lower and upper 95% confidence limits.
Finally, we applied the estimated rates to the mid-2009 UK population estimate to calculate the annual number of cases and GP consultations associated with each organism.
Multiple imputation was conducted in R 2.11. Analysis of under-ascertainment and analysis of imputed data were performed using the glamm21 and mi22 modules in Stata V.11, respectively.
Results
Participation
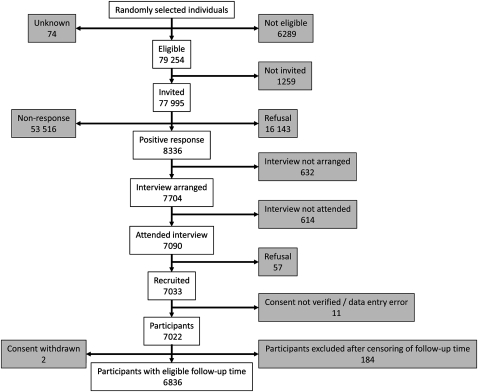
Of 77 995 people invited in the cohort study, 8336 (10.5%) responded positively and 7033 were recruited (9.0%) (figure 1). Some people recruited near the study end date had no eligible follow-up time (n=184), and two people withdrew consent. We analysed data from 6836 participants. Compared with the 2001 census population, cohort participants were more likely to be older, female, employed in managerial and professional occupations, less deprived and in rural areas (online appendix 1). The median follow-up duration was 39 weeks (IQR 27–45 weeks); overall, 86% of the maximum achievable follow-up time to 31 August 2009 was completed. Six hundred and ten (9.5%) participants dropped out, accounting for 219 (4.5%) lost person-years of follow-up.
Figure 1.
Recruitment in the cohort study, Infectious Intestinal Disease 2 Study, UK 2008–9.
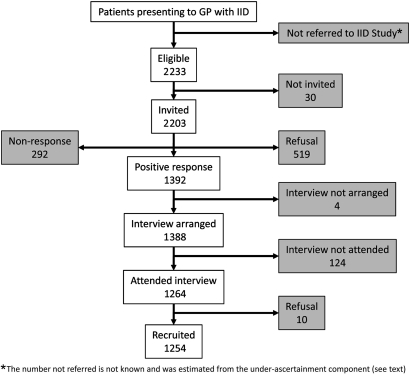
In the GP presentation study, 2233 eligible symptomatic patients were referred and 2203 invited to participate. A total of 1392 people (63.2%) responded positively, and 1254 (56.9%) were recruited (figure 2). We excluded 140 people reporting recent foreign travel, 77 with illness lasting over 2 weeks, and 46 because of missing or inconsistent information on symptoms and/or travel. Ultimately, we analysed data from 991 cases.
Figure 2.
Recruitment in the general practice presentation study, Infectious Intestinal Disease (IID) 2 Study, UK 2008–9.
Rate of overall IID
There were 4658 person-years of follow-up and 1201 definite IID cases in the cohort. The crude IID incidence rate was 258 cases per 1000 person-years. The age- and sex-standardised rate was 274 cases per 1000 person-years (95% CI 254 to 296). When both definite and possible cases were considered, this rose to 523 cases per 1000 person-years (95% CI 497 to 551). There was little evidence that rates varied by socioeconomic characteristics or between urban and rural areas (data not shown).
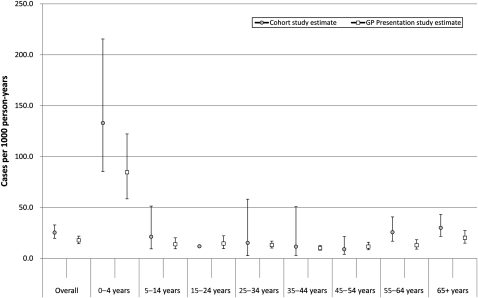
In the under-ascertainment analysis, approximately one case was recruited into the GP presentation study for every six identified in the medical records, although this varied by age group, Read code category and practice. After adjustment for under-ascertainment, there were 5546 IID cases and 312 232 person-years of follow-up, yielding a consultation rate of 17.7 per 1000 person-years (95% CI 14.4 to 21.8). This was lower than that estimated from definite cases in the cohort who reported consulting their GP for their illness (25.3 cases per 1000 person-years, 95% CI 20.7 to 31.3). The age-specific rates of GP consultation in the two studies were similar except for young children and older adults (figure 3). Among children <5 years, the rate was 133 consultations per 1000 person-years in the cohort study (95% CI 92 to 199) and 85 consultations per 1000 person-years in the GP presentation study (95% CI 59 to 122), while among those aged 65 and over, the corresponding rates were 30 consultations per 1000 person-years (95% CI 22 to 42) and 20 consultations per 1000 person-years (95% CI 15 to 27), respectively.
Figure 3.
Age-specific rates of infectious intestinal disease general practice (GP) consultations—estimates from the cohort and general practice presentation studies, Infectious Intestinal Disease 2 Study, UK 2008–9.
Call rates to NHS Direct in England for diarrhoea and vomiting were 6.1 per 1000 person-years, similar to that estimated from cohort study patients in England who reported contacting NHS Direct for their illness (5.5 per 1000 person-years, 95% CI 3.4 to 9.5).
Rates of IID by organism
Rates of IID by organism in the community, presenting to the GP and reported to national surveillance are shown in table 1. For organisms tested by more than one method, rate estimates are presented separately for routine diagnostic methods and for routine and PCR methods combined.
Table 1.
Incidence rates of infectious intestinal disease in the community and presenting to general practice by organism, Infectious Intestinal Disease 2 Study, UK 2008–9
| Organism | Test methods | Community | Presenting to GP | Ratio community/GP | ||||
| Cases* | PY† | Rate‡ (95% CI) | Cases* | PY† | Rate‡ (95% CI) | RR (95% CI) | ||
| Bacteria | ||||||||
| C perfringens | A | 7 | 4658.6 | 1.5 (0.5 to 3.9) | 78 | 312 232 | 0.24 (0.11 to 0.52) | 6.0 (1.7 to 20.9) |
| Campylobacter spp. | A | 43 | 4658.6 | 9.3 (6 to 14.3) | 400 | 312 232 | 1.28 (0.90 to 1.82) | 7.2 (4.1 to 12.7) |
| E | 51 | 4658.6 | 10.9 (7.4 to 15.9) | 693 | 312 232 | 2.22 (1.65 to 2.97) | 4.9 (3 to 7.9) | |
| E coli O157 (VTEC) | A | 1 | 4658.6 | 0.3 (0 to 4.3) | 4 | 312 232 | 0.01 (0.00 to 0.09) | 22.8 (0.9 to 610) |
| Enteroaggregative E coli | D | 28 | 4658.6 | 5.9 (3.4 to 10.2) | 66 | 312 232 | 0.21 (0.11 to 0.41) | 28.4 (11.8 to 68.2) |
| Salmonella spp. | A | 3 | 4658.6 | 0.6 (0.2 to 2.4) | 57 | 312 232 | 0.18 (0.08 to 0.44) | 3.4 (0.7 to 17.4) |
| E | 3 | 4658.6 | 0.6 (0.2 to 2.4) | 56 | 312 232 | 0.18 (0.07 to 0.44) | 3.5 (0.7 to 17.9) | |
| Protozoa | ||||||||
| Cryptosporidium | B | 3 | 4658.6 | 0.7 (0.2 to 2.7) | 65 | 312 232 | 0.20 (0.08 to 0.48) | 3.5 (0.7 to 17.6) |
| C | 6 | 4658.6 | 1.2 (0.4 to 3.9) | 80 | 312 232 | 0.25 (0.11 to 0.58) | 4.9 (1.2 to 20.6) | |
| Giardia | B | 4 | 4658.6 | 0.8 (0.2 to 3) | 29 | 312 232 | 0.09 (0.03 to 0.27) | 9.3 (1.8 to 49.2) |
| C | 9 | 4658.6 | 2.0 (0.7 to 5.6) | 35 | 312 232 | 0.11 (0.05 to 0.26) | 18.2 (4.8 to 69.6) | |
| Viruses | ||||||||
| Adenovirus§ | C | 48 | 4658.6 | 10.2 (6.8 to 15.4) | 265 | 312 232 | 0.84 (0.49 to 1.45) | 12.1 (6.1 to 23.9) |
| Astrovirus | D | 25 | 4658.6 | 5.3 (3 to 9.4) | 127 | 312 232 | 0.40 (0.20 to 0.82) | 13.1 (5.2 to 32.7) |
| Norovirus | D | 219 | 4658.6 | 47.0 (39.1 to 56.5) | 648 | 312 232 | 2.07 (1.44 to 2.99) | 22.7 (15.1 to 34.2) |
| Rotavirus§ | C | 59 | 4658.6 | 12.7 (8.7 to 18.4) | 424 | 312 232 | 1.36 (0.89 to 2.07) | 9.4 (5.3 to 16.5) |
| Sapovirus | D | 121 | 4658.6 | 26.1 (20.1 to 33.8) | 491 | 312 232 | 1.57 (1.08 to 2.29) | 16.6 (10.5 to 26.2) |
Mean number of cases from 20 imputations.
Person-years.
Cases per 1000 person-years.
ELISA for adenovirus and rotavirus was conducted in specimens from patients aged <5 years.
A, culture; B, enzyme immunoassay; C, ELISA and/or PCR; D, PCR; E, culture and/or PCR; GP, general practice; VTEC, verotoxin-producing E coli.
Rates in the community
Viruses predominated among IID cases in the community: the estimated rates (cases per 1000 person-years) were 47 for norovirus, 26 for sapovirus, 13 for rotavirus and 10 for adenovirus. The most common bacteria were Campylobacter (11 cases per 1000 person-years) and enteroaggregative E coli (six cases per 1000 person-years). The Salmonella rate was less than one case per 1000 person-years. Based on ELISA, Cryptosporidium and Giardia rates were around one case per 1000 person-years, although PCR-based estimates were slightly higher.
E coli O157 was present in only one sample, and there were no cases of CDAD or L monocytogenes IID in the community cohort.
GP presentation rates
Norovirus was the most common organism among cases presenting to the GP (two consultations per 1000 person-years (table 1)); approximately one in every 23 people with norovirus IID consulted a GP. Rotavirus and sapovirus were also common (∼1.5 consultations per 1000 person-years). One in seven patients with campylobacteriosis consulted their GP, resulting in approximately one consultation per 1000 person-years based on culture diagnostics. Other organisms occurred at rates of less than one consultation per 1000 person-years. Salmonellosis was uncommon (<0.2 consultations per 1000 person-years), although one in three patients consulted their GP.
Only one case of CDAD occurred in the GP presentation study, and no cases of L monocytogenes IID were identified.
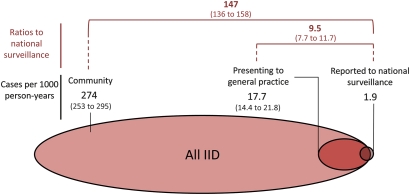
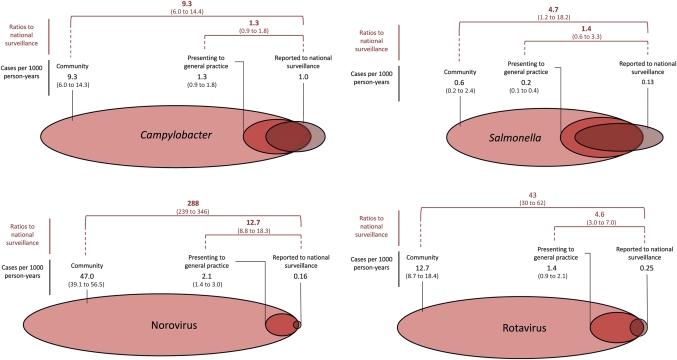
Ratios to national surveillance
Table 2 presents, by organism, the rates of IID in the community and presenting to GP, and the ratios of these rates to those estimated from national surveillance data. Figures 4 and 5 illustrate reporting patterns for all IID and for the four major pathogens, Campylobacter, Salmonella, norovirus and rotavirus. In each diagram, the rates in the community, presenting to GP and reported to national surveillance are represented as ellipses, with the area of each ellipse proportional to the rate.
Table 2.
Incidence rates of infectious intestinal disease (IID) in the community and presenting to general practice by organism, and ratios to national surveillance, IID2 Study, UK 2008–2009
| Organism | Community | Presenting to general practice | Reported to national surveillance | |
| Rate* (95% CI) | Rate* (95% CI) | Rate* (95% CI) | ||
| Bacteria | ||||
| C perfringens | A | 1.5 (0.5 to 3.9) | 0.2 (0.1 to 0.5) | 0.001 (0 to 0.001) |
| Reporting ratio† | 2518.7 (890.7 to 7179.4) | 419.1 (181.9 to 962.8) | 1.0 | |
| Campylobacter | A | 9.3 (6 to 14.3) | 1.3 (0.9 to 1.8) | 0.997 (0.989 to 1.005) |
| Reporting ratio† | 9.3 (6 to 14.4) | 1.3 (0.9 to 1.8) | 1.0 | |
| E coli O157 VTEC | A | 0.3 (0 to 4.3) | 0.0 (0 to 0.1) | 0.042 (0.04 to 0.043) |
| Reporting ratio† | 7.4 (0.5 to 104.4) | – | 1.0 | |
| Salmonella | A | 0.6 (0.2 to 2.4) | 0.2 (0.1 to 0.4) | 0.133 (0.13 to 0.136) |
| Reporting ratio† | 4.7 (1.2 to 18.2) | 1.4 (0.6 to 3.3) | 1.0 | |
| Protozoa | ||||
| Cryptosporidium | B | 0.7 (0.2 to 2.7) | 0.2 (0.1 to 0.5) | 0.086 (0.084 to 0.089) |
| Reporting ratio† | 8.2 (2.1 to 31.7) | 2.3 (1 to 5.6) | 1.0 | |
| Giardia | B | 0.8 (0.2 to 3) | 0.1 (0 to 0.3) | 0.061 (0.059 to 0.063) |
| Reporting ratio† | 14.0 (4 to 49) | 1.5 (0.5 to 4.5) | 1.0 | |
| Viruses | ||||
| Adenovirus | C | 10.2 (6.8 to 15.4) | 0.8 (0.5 to 1.5) | 0.055 (0.053 to 0.057) |
| Reporting ratio† | 184.5 (122 to 279.3) | 15.3 (8.8 to 26.3) | 1.0 | |
| Astrovirus | D | 5.3 (3 to 9.4) | 0.4 (0.2 to 0.8) | 0.003 (0.003 to 0.003) |
| Reporting ratio† | 1763.5 (970.1 to 3218.1) | 135.1 (65.5 to 278.9) | 1.0 | |
| Norovirus | D | 47.0 (39.1 to 56.5) | 2.1 (1.4 to 3) | 0.164 (0.011 to 0.02) |
| Reporting ratio† | 287.6 (239.1 to 346) | 12.7 (8.8 to 18.3) | 1.0 | |
| Rotavirus | C | 12.7 (8.7 to 18.4) | 1.4 (0.9 to 2.1) | 0.296 (0.232 to 0.268) |
| Reporting ratio† | 42.9 (29.5 to 62.4) | 4.6 (3 to 7) | 1.0 | |
Cases per 1000 person-years.
The reporting ratios represent the ratio of rates in the community and presenting to general practice relative to the rate of reports to national surveillance. Enteroaggregative E coli and sapovirus are omitted from this table, as data on these organisms are not routinely collected at national level in all UK countries.
A, culture; B, enzyme immunoassay; C, ELISA and/or PCR; D, PCR; VTEC, verocytotoxin-producing E coli.
Figure 4.
Patterns of reporting to national surveillance for all infectious intestinal disease (IID), UK 2008–9. Black numbers represent the rates (with 95% CIs) in the community, presenting to general practice and reported to national surveillance. Red numbers represent the ratios of incidence in the community and presenting to general practice respective to the incidence of infectious intestinal disease reported to national surveillance (with 95% CIs).
Figure 5.
Patterns of reporting to national surveillance for Campylobacter, Salmonella, norovirus and rotavirus, UK 2008–9. Black numbers represent the rates per 1000 person-years (with 95% CIs) in the community, presenting to general practice and reported to national surveillance. Red numbers represent the ratios of the incidence rates in the community and presenting to general practice compared with infectious intestinal disease reports to national surveillance (with 95% CIs).
The ratios of community and GP presentation rates to national surveillance rates were much higher for viruses than for bacteria and protozoa. For every national surveillance case of norovirus IID, there were 12.7 GP consultations (95% CI 8.8 to 18.3) and 288 community cases (95% CI 239 to 346). The corresponding ratios for rotavirus were one in five (95% CI 3 to 7) and one in 43 (95% CI 30 to 62). By contrast, for every national surveillance case of campylobacteriosis, there were 1.3 GP consultations (95% CI 0.9 to 1.8) and 9.3 community cases (95% CI 6.0 to 14.4). For Salmonella, the corresponding ratios were 1.4 GP consultations (95% CI 0.6 to 3.3) and approximately five community cases (95% CI 1.2 to 18.2). Among the protozoa, 2.3 GP consultations (95% CI 1.0 to 5.6) and 8.2 (95% CI 2.1 to 31.7) community cases occurred for every case of cryptosporidiosis reported to national surveillance. The corresponding figures for giardiasis were somewhat higher, although there was considerable uncertainty in the estimates.
Estimated annual cases and GP presentations
In 2009, there were approximately 16.9 million cases of IID and over 1 million IID-related GP consultations. Campylobacter accounted for over 500 000 cases and approximately 80 000 GP consultations (table 3). Norovirus caused nearly three million sporadic (non-outbreak-related) IID cases and approximately 130 000 GP consultations. The burden from sapovirus was also considerable, with an estimated 1.6 million sporadic cases and nearly 100 000 GP consultations, while rotavirus caused more than 750 000 cases and 80 000 GP consultations.
Table 3.
Estimated annual numbers of infectious intestinal disease (IID) cases in the community and presenting to general practices by organism, IID2 Study, UK 2008–2009
| Organism | Community | Presenting to GP | |||
| Cases | 95% CI | Cases | 95% CI | ||
| Bacteria | |||||
| C perfringens | A | 89 847 | 33 565 to 240 508 | 14 983 | 6981 to 32 157 |
| Campylobacter spp. | A | 571 949 | 369 936 to 884 276 | 78 973 | 55 486 to 112 401 |
| E coli O157 VTEC | A | 18 916 | 1339 to 267 201 | 824 | 120 to 5664 |
| Enteroaggregative E coli | D | 365 297 | 211 351 to 631 374 | 12 893 | 6501 to 25 567 |
| Salmonella spp. | A | 38 606 | 9968 to 149 529 | 11 291 | 4649 to 27 418 |
| Protozoa | |||||
| Cryptosporidium | B | 43 834 | 11 393 to 168 655 | 12 488 | 5232 to 29 805 |
| Giardia | B | 52 434 | 15 022 to 183 020 | 5617 | 1875 to 16 822 |
| Viruses | |||||
| Adenovirus | C | 630 251 | 417 285 to 951 906 | 52 106 | 30 219 to 89 845 |
| Astrovirus | D | 325 642 | 1 82 466 to 581 165 | 24 982 | 12 260 to 50 905 |
| Norovirus | D | 2 905 278 | 2 418 208 to 3 490 451 | 128 022 | 88 784 to 184 600 |
| Rotavirus | C | 783 737 | 539 535 to 1 138 466 | 83 850 | 54 868 to 128 141 |
| Sapovirus | D | 1 610 041 | 1 239 580 to 2 091 219 | 97 024 | 66 661 to 141 217 |
| All IID | 16 935 420 | 15 680 690 to 18 277 944 | 1 096 190 | 891 659 to 1 348 301 | |
A, culture; B, enzyme immunoassay; C, ELISA and/or PCR; D, PCR; VTEC, verocytotoxin-producing E coli.
Discussion
Summary of main findings
This is one of the largest population-based studies of IID to date, comprising over 4500 person-years of community follow-up and over 300 000 person-years of GP follow-up. Few researchers12 23 have investigated the aetiology of IID in the general population so comprehensively. We included a broad panel of organisms using conventional and novel quantitative PCR diagnostics. The greater sensitivity of PCR methods for viral diagnostics allows much more reliable incidence estimates, particularly for norovirus and sapovirus. The results show Campylobacter is the major bacterial IID agent, causing over half a million cases and 80 000 GP consultations annually. Norovirus, commonly thought to cause mild illness in institutional outbreaks, nevertheless accounts for nearly 3 million sporadic cases annually and 130 000 GP consultations.
To our knowledge, this is the first study to report the high population burden of sapovirus, which may partly be due to emergence of a novel sapovirus strain during the study.24 Low population immunity levels may have facilitated its rapid spread. Our estimates also provide a useful baseline for rotavirus burden before the introduction of routine vaccination in the UK, and indicate that C difficile is a very uncommon cause of diarrhoea in the community.
Comparison with other studies
In a previous study,12 limited to England in the mid-1990s, using the same case definition and similar methods, the reported IID rates were 194 community cases and 33.1 GP consultations per 1000 person-years. In our study, the community incidence is ∼40% higher, but GP consultation rates for all the major pathogens have almost halved. This is consistent with data from the Royal College of General Practitioners Weekly Returns Service indicating a threefold decrease in IID-related consultations to its GP network between 1996 and 2008.25 A major change to primary care since the 1990s is the introduction of telephone information and advice services. However, use of services such as NHS Direct in England was low in our study and cannot account for the decline in GP consultations. Instead, increased self-management and perhaps a decrease in the severity of illness from certain pathogens may be responsible.
Our case definition was more sensitive than those used in other studies and may have resulted in milder illness being captured. The effect of varying case definitions will be the subject of more detailed investigation. The Dutch SENSOR Study, which used a definition for IID of three or more loose stools in a 24 h period,23 produced a similar estimate (283 per 1000 person-years) to ours. Approximately 20% of patients in our cohort experienced fewer than three loose stools in a 24 h period, implying that, using comparable definitions, our study would produce somewhat lower estimates of all-cause IID in the community. Nevertheless, using comparable diagnostic methods, rates in the community for Campylobacter, norovirus and rotavirus were similar to those in both the previous IID Study12 26 and the Dutch SENSOR Study.23 By contrast, the incidence of salmonellosis in our study was considerably lower than in those two studies. This reflects a decrease in contamination of poultry products, particularly from Salmonella Enteritidis phage type 4, following the introduction of vaccination of breeder and layer flocks in the mid-1990s.27
We estimate that there are up to 17 million cases of sporadic IID in the UK every year. Studies of IID burden in similar settings using telephone survey methods generally produce incidence estimates two to three times higher.28 The reasons are unclear, but may include differences in case definitions, telescoping of symptoms among telephone survey respondents, and reporting fatigue among cohort participants followed-up for long periods.28 In the IID2 Study, we conducted a parallel telephone survey to study these differences in detail (to be reported elsewhere).
IID-related GP consultation rates vary considerably by study: the SENSOR study rate was half that estimated by us,29 while the rate recently reported in Germany was double.30 These differences are difficult to interpret, but variations in primary care provision and usage between countries may explain them.
Study limitations
Adherence to weekly follow-up in the cohort study was high. Drop-outs accounted for losing <5% of total follow-up time. Nevertheless, ∼10% of those invited were recruited into the study. This is lower than previous studies in England (35%)12 and the Netherlands (42%),23 but similar to recent prospective, population-based UK studies.31 32 Study participants may differ from the general population in terms of IID risk or propensity to report symptoms. We standardised all rates to account for differences in the age and sex structure between the cohort and census populations, and we did not find important differences in IID rates by ethnicity, socioeconomic group, urban–rural residence or area-level deprivation (data not shown).
We based our estimates of community incidence on definite IID cases. These could be conservative, since some cohort participants reporting illness were classified as possible cases because of missing symptom information. If definite and possible cases were considered, the community rate nearly doubled. We used definite cases only because information from them on health service usage agrees with estimates from the GP presentation study and NHS Direct, suggesting that these estimates are more reliable than those based on all definite and possible cases. In addition, our results show a marked decline in community Salmonella incidence, but for Campylobacter, norovirus and rotavirus, for which control measures have not been implemented, our estimates are similar to those reported previously in England12 26 and the Netherlands.23
One in six patients presenting to GP with IID-compatible symptoms was recruited into the GP presentation study, with considerable variation by practice. Although we publicised the study widely in participating practices, some GPs may not have referred patients if they were too busy. To satisfy ethics requirements, invited patients were given a 24 h cooling-off period before providing consent. Some patients were unable or unwilling to return for an interview on another day, and others were no longer interested because their condition had improved. We corrected for under-ascertainment using adjustment factors to account for differences in ascertainment by age group, sex, diagnostic category and practice.
In the cohort study, a third of cases did not provide a stool specimen for microbiological examination, so we used multiple imputation methods to infer missing organism information. Our imputation models included variables most likely to predict the likelihood of infection with different organisms, namely age group and symptom profile, but may not have dealt adequately with missing data if other important factors related to positivity with specific organisms had been omitted.
We used both conventional and quantitative PCR methods for microbial diagnosis. PCR-based methods have greater sensitivity for enteric viruses. For norovirus and rotavirus, however, a substantial fraction of asymptomatic people have evidence of infection using PCR.33 We used previously validated PCR cut-off values to distinguish clinically significant from coincidental infection with norovirus and rotavirus. Similar data do not exist for other organisms, and we opted for a more sensitive threshold. We may have overestimated incidence, particularly for sapovirus, adenovirus and astrovirus, since, in some people, infection may have been coincidental rather than causative. Conversely, we may have underestimated Cryptosporidium and Giardia rates; these organisms often cause illness lasting over 2 weeks, so cases of longer duration may have been excluded.
Despite extensive microbiological testing, ∼50% and 60% of specimens tested in the GP presentation and cohort studies, respectively, were negative for all the organisms investigated. This is similar to previous studies23 34 and may reflect the role of other organisms for which we did not test, or hitherto unknown pathogens. We excluded patients with known non-infectious causes of IID, and required cases to be symptom-free for the preceding 3 weeks and have illness lasting less than 2 weeks. However, it is possible that a fraction of these stool-negative cases had non-infectious causes such as transient irritable bowel syndrome, either pre-existing or resulting from a prior episode of IID.
The reporting ratios should be interpreted in their epidemiological context. Norovirus cases in national statistics arise primarily from institutional outbreaks, which were not included in our study. We may therefore have overestimated the proportion of sporadic cases in the community captured by national surveillance. For organisms such as Campylobacter, which is uncommonly associated with large outbreaks, the reporting ratio reflects more accurately the ratio of community incidence to national statistics.
Conclusions
The UK burden of IID is substantial, resulting in up to 17 million sporadic cases annually. Despite this, IID-related GP consultations have declined substantially since the 1990s. Changes in healthcare usage, rather than increased use of telephone information and advice services, probably explain this. Tackling Campylobacter is central to the Food Standards Agency's strategy and crucial for reducing food-borne illness burden.35 This involves reducing contamination in poultry, a major source of human infection,36 and promoting safe food preparation to avoid cross-contamination. By contrast, salmonellosis has declined dramatically. C difficile, very important in healthcare settings, appears to be a rare cause of community IID, while enteric viruses account for a large burden of healthcare use and disease in the community. New rotavirus vaccines, if deemed cost-effective for routine immunisation in the UK, show great promise for reducing burden of rotavirus disease in children.37 38 Our study provides contemporaneous baseline estimates of rotavirus burden before introduction of routine immunisation. For norovirus and sapovirus, organisms commonly regarded as mainly causing institutional outbreaks, the large pool of community infection raises important questions about control. Mitigating the impact of these viruses includes scrupulous personal hygiene to avoid person-to-person spread, and protecting shellfish beds against human sewage contamination to reduce food-related norovirus infection. Understanding better the burden of disease that is food-borne, and the relationship between virus circulation in the community and transmission in institutional and healthcare settings, is crucial for developing appropriate control strategies.
Acknowledgments
We thank all the participants, study nurses, general practitioners, practice staff, laboratory, research and administrative staff who took part in the IID2 Study. We are grateful to the Medical Research Council General Practice Research Framework, the Primary Care Research Networks in England and Northern Ireland and the Scottish Primary Care Research Network for assistance with the recruitment of general practices. We thank the UK Food Standards Agency and the Department of Health for funding the research component of the IID2 Study (Project B18021). We also thank the Department of Health, the Scottish Primary Care Research Network, NHS Greater Glasgow and Clyde, NHS Grampian, NHS Tayside, the Welsh Assembly government (Wales Office of Research and Development) and, in Northern Ireland, the Health and Social Care Public Health Agency (HSC Research and Development) for providing service support costs. We thank Julian Gardiner for help with aspects of the analysis.
Footnotes
Funding: This study was funded by the Food Standards Agency and sponsored by University of Manchester. Neither the funder nor the sponsor were involved in the analysis, interpretation or decision to submit for publication.
Correction notice: This article has been corrected since it was published Online First. In the results section of the abstract, the following sentence has been corrected as follows: “Campylobacter was the most common bacterial pathogen, with a rate of 9.3 cases per 1000 person-years in the community, and 1.3 GP consultations per 1000 person-years.”
Competing interests: All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author).
Patient consent: Obtained.
Ethics approval: This study was conducted with the approval of the North West MREC, Stockport PCT, Gateway House, Piccadilly South, Manchester M60 7LP, UK.
Contributors: SJOB, GR, JJG, PRH, DST, CCT and LCR conceived the ideas for the study. All authors participated in its design and coordination. SJOB, GR, JD and LHL led the prospective studies. JJG and DST led the laboratory studies. MRE participated in the national surveillance studies. CCT, LCR and LV led and conducted the analysis. CCT, LCR and SJOB drafted the manuscript. All authors have read and approved the final manuscript. All authors had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis. SJOB is the guarantor of the study.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Health Protection Agency Laboratory Reports of Campylobacter Cases Reported to the Health Protection Agency Centre for Infections England and Wales, 1989-2009, 2010. http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/Campylobacter/EpidemiologicalData/campyDataEw (accessed 15 Apr 2011).
- 2.Health Protection Agency Salmonella in Humans (excluding S. typhi; S. Paratyphi). Faecal and Lower Gastrointestinal Tract Isolates Reported to the Health Protection Agency Centre for Infections. England and Wales, 1990-2009, 2010. http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/Salmonella/EpidemiologicalData/salmDataHuman (accessed 15 Apr 2011).
- 3.Health Protection Agency Rotavirus Laboratory Reports of All Identifications England & Wales, 1986-2009, 2010. http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/Rotavirus/EpidemiologicalData/rota_DataEw (accessed 15 Apr 2011).
- 4.Health Protection Agency Norovirus Laboratory Reports of All Identifications Reported to the Health Protection Agency, Centre for Infections, England and Wales, 1986-2010, 2010. http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/Norovirus/EpidemiologicalData/norovDataEw (accessed 15 Apr 2011).
- 5.Roberts JA, Cumberland P, Sockett PN, et al. The study of infectious intestinal disease in England: socio-economic impact. Epidemiol Infect 2003;130:1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lynn RM, O'Brien SJ, Taylor CM, et al. Childhood hemolytic uremic syndrome, United Kingdom and Ireland. Emerg Infect Dis 2005;11:590–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tam CC, Rodrigues LC, Petersen I, et al. Incidence of Guillain-Barre syndrome among patients with Campylobacter infection: a general practice research database study. J Infect Dis 2006;194:95–7 [DOI] [PubMed] [Google Scholar]
- 8.Tam CC, Rodrigues LC, O'Brien SJ. The study of infectious intestinal disease in England: what risk factors for presentation to general practice tell us about potential for selection bias in case-control studies of reported cases of diarrhoea. Int J Epidemiol 2003;32:99–105 [DOI] [PubMed] [Google Scholar]
- 9.Food Standards Agency Strategic Plan 2001-2006: Putting Consumers First, 2001. http://www.food.gov.uk/multimedia/pdfs/stratplan.pdf (accessed 15 Apr 2011).
- 10.O'Brien SJ, Rait G, Hunter PR, et al. Methods for determining disease burden and calibrating national surveillance data in the United Kingdom: the second study of infectious intestinal disease in the community (IID2 study). BMC Med Res Methodol 2010;10:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chisholm J. The Read clinical classification. BMJ 1990;300:1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wheeler JG, Sethi D, Cowden JM, et al. Study of infectious intestinal disease in England: rates in the community, presenting to general practice, and reported to national surveillance. The Infectious Intestinal Disease Study Executive. BMJ 1999;318:1046–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brazier JS, Raybould R, Patel B, et al. Distribution and antimicrobial susceptibility patterns of Clostridium difficile PCR ribotypes in English hospitals, 2007-08. Euro Surveill 2008;13:19000. [DOI] [PubMed] [Google Scholar]
- 14.Boom R, Sol CJ, Salimans MM, et al. Rapid and simple method for purification of nucleic acids. J Clin Microbiol 1990;28:495–503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Green J, Norcott JP, Lewis D, et al. Norwalk-like viruses: demonstration of genomic diversity by polymerase chain reaction. J Clin Microbiol 1993;31:3007–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McLauchlin J, Pedraza-Diaz S, Amar-Hoetzeneder C, et al. Genetic characterization of Cryptosporidium strains from 218 patients with diarrhea diagnosed as having sporadic cryptosporidiosis. J Clin Microbiol 1999;37:3153–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Phillips G, Lopman B, Tam CC, et al. Diagnosing norovirus-associated infectious intestinal disease using viral load. BMC Infect Dis 2009;9:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Phillips G, Lopman B, Tam CC, et al. Diagnosing rotavirus A associated IID: using ELISA to identify a cut-off for real time RT-PCR. J Clin Virol 2009;44:242–5 [DOI] [PubMed] [Google Scholar]
- 19.Department of Health Clostridium difficile Infection: How to Deal with the Problem, 2009. http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_093218.pdf (accessed 15 Apr 2011).
- 20.Rubin DB. Multiple Imputation for Non-Response in Surveys. 2nd edn New Jersey, USA: Wiley-Blackwell, 2004 [Google Scholar]
- 21.Rabe-Hesketh S, Skrondal A, Pickles A. GLLAMM Manual. U.C. Berkeley Division of Biostatistics Working Paper Series. Working Paper 160, 2004. http://www.bepress.com/ucbbiostat/paper160 [Google Scholar]
- 22.Royston P. Multiple imputation of missing values: an update. STATA J 2005;5:1–14 [Google Scholar]
- 23.de Wit MA, Koopmans MP, Kortbeek LM, et al. Sensor, a population-based cohort study on gastroenteritis in the Netherlands: incidence and etiology. Am J Epidemiol 2001;154:666–74 [DOI] [PubMed] [Google Scholar]
- 24.Svraka S, Vennema H, van der Veer B, et al. Epidemiology and genotype analysis of emerging sapovirus-associated infections across Europe. J Clin Microbiol 2010;48:2191–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Royal College of General Practitioners Royal College of General Practitioners Weekly Returns Service Annual Reports, 2008. http://www.rcgp.org.uk/clinical_and_research/rsc/annual_reports.aspx (accessed 15 Apr 2011).
- 26.Phillips G, Tam CC, Conti S, et al. Community incidence of norovirus-associated infectious intestinal disease in England: improved estimates using viral load for norovirus diagnosis. Am J Epidemiol 2010;171:1014–22 [DOI] [PubMed] [Google Scholar]
- 27.Department for Environment Food and Rural Affairs Zoonoses Report United Kingdom 2008, 2008. http://archive.defra.gov.uk/foodfarm/farmanimal/diseases/atoz/zoonoses/documents/report-2008.pdf (accessed 15 Apr 2011).
- 28.Roy SL, Scallan E, Beach MJ. The rate of acute gastrointestinal illness in developed countries. J Water Health 2006;4(Suppl 2):31–69 [DOI] [PubMed] [Google Scholar]
- 29.de Wit MA, Koopmans MP, Kortbeek LM, et al. Etiology of gastroenteritis in sentinel general practices in the netherlands. Clin Infect Dis 2001;33:280–8 [DOI] [PubMed] [Google Scholar]
- 30.Karsten C, Baumgarte S, Friedrich AW, et al. Incidence and risk factors for community-acquired acute gastroenteritis in north-west Germany in 2004. Eur J Clin Microbiol Infect Dis 2009;28:935–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.UK Biobank Co-ordinating Centre UK Biobank: Report of the Integrated Pilot Study, 2006. http://www.ukbiobank.ac.uk/docs/IntegratedPilotReport.pdf (accessed 15 Apr 2011).
- 32.Lamb SE, Lall R, Hansen Z, et al. A multicentred randomised controlled trial of a primary care-based cognitive behavioural programme for low back pain. The Back Skills Training (BeST) trial. Health Technol Assess 2010;14:1–253 [DOI] [PubMed] [Google Scholar]
- 33.Amar CF, East CL, Gray J, et al. Detection by PCR of eight groups of enteric pathogens in 4,627 faecal samples: re-examination of the English case-control Infectious Intestinal Disease Study (1993-1996). Eur J Clin Microbiol Infect Dis 2007;26:311–23 [DOI] [PubMed] [Google Scholar]
- 34.Tompkins DS, Hudson MJ, Smith HR, et al. A study of infectious intestinal disease in England: microbiological findings in cases and controls. Commun Dis Public Health 1999;2:108–13 [PubMed] [Google Scholar]
- 35.Food Standards Agency The Food Standards Agency's Strategy for 2010-2015, 2009. http://www.food.gov.uk/multimedia/pdfs/strategy20102015.pdf (accessed 15 Apr 2011).
- 36.Tam CC, Higgins CD, Neal KR, et al. Chicken consumption and use of acid-suppressing medications as risk factors for Campylobacter enteritis, England. Emerg Infect Dis 2009;15:1402–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jit M, Bilcke J, Mangen MJ, et al. The cost-effectiveness of rotavirus vaccination: comparative analyses for five European countries and transferability in Europe. Vaccine 2009;27:6121–8 [DOI] [PubMed] [Google Scholar]
- 38.Atchison C, Lopman B, Edmunds WJ. Modelling the seasonality of rotavirus disease and the impact of vaccination in England and Wales. Vaccine 2010;28:3118–26 [DOI] [PubMed] [Google Scholar]