Abstract
Chronic heat stress (CHS) can negatively affect immune response in animals. In this study we assessed the effects of CHS on host innate immunity and avian influenza virus H5N1 infection in mice. Mice were divided into two groups: CHS and thermally neutral (TN). The CHS treatment group exhibited reduced local immunity in the respiratory tract, including the number of pulmonary alveolar macrophages and lesions in the nasal mucosa, trachea, and lungs. Meanwhile, CHS retarded dendritic cells (DCs) maturation and reduced the mRNA levels of IL-6 and IFN-β significantly (P < .05). After the CHS treatment, mice were infected with H5N1 virus. The mortality rate and viral load in the lungs of CHS group were higher than those of TN group. The results suggest that the CHS treatment could suppress local immunity in the respiratory tract and innate host immunity in mice significantly and moderately increased the virulence in H5N1-infected mice.
1. Introduction
Heat stress can negatively affect an animal's growth performance and the immune competence to some bacterial or viral infection [1–6]. It has been reported that heat stress results in decease of weights of both primary and secondary lymphoid organs, profiles of circulating leukocytes, T cell in the blood, and antibody response to sheep red blood cells (SRBCs) or against Newcastle disease [7–10]. Our previous studies have demonstrated that chronic heat stress condition negatively affects both humoral and cellular responses against foot and mouth disease virus (FMDV) in mice [2]. However, there have been few detailed studies addressing the effects of CHS on the innate immune response as the most immediate defense against viral infection.
The H5N1 subtype of highly pathogenic avian influenza viruses (HPAIVs) causes infections in domestic poultry and humans. It is epidemiologically characterized by wide dissemination and rapid prevalence and is a threat to public health. So far human cases of H5N1 infection in worldwide have increased to 522, including 309 deaths (http://www.who.int/csr/disease/avian_influenza/country/cases_table_2011_02_25/en/index.html). The data from WHO demonstrated that most human cases of H5N1 infection occurred in the tropical and subtropical countries, such as Egypt, Vietnam, and Indonesia, instead of the high latitude countries. (http://www.who.int/csr/disease/avian_influenza/country/cases_table_2011_02_25/en/index.html). In mainland China, the outbreak of H5N1 virus in poultry and human cases mainly occurred in the south of the Yangtze associated with high humidity and temperature, including Guangdong, Guangxi and, Fujian province [11]. It is speculative that high temperature may be associated with human or poultry higher susceptibility to H5N1 virus. It was also reported that the vast temperature changes frequently occurred one week before the avian influenza outbreak in China [12]. Even in winter, heat stress often occurred under conditions of crowding, heating, and without ventilation in poultry. When those flocks are exposed to H5N1 virus, the outbreaks of avian influenza may occur. In this study, we measured the effects of CHS on innate host immunity by detecting local immunity in the respiratory tract, maturation or activation of DCs, and cytokine levels in spleens of the mice under CHS or TN conditions. Then we examined mortality rate, histopathology, and viral loads in lung of CHS mice challenged with H5N1 virus. We demonstrated that heat stress could increase the susceptibility of animals to the highly pathogenic avian influenza virus (HPAIV) H5N1.
2. Materials and Methods
2.1. Virus
The H5N1 influenza virus (A/Chicken/Henan/1/04) used in this study was isolated from infected chicken flocks. This isolate was highly pathogenic on poultry, mouse, and Madin-Darby canine kidney (MDCK) cells. The virus has been adapted in MDCK cells for convenience and propagated in cell culture at 37°C for 48 hours. The viral supernatant was harvested, aliquoted, and stored at −80°C. The viral titers were determined by plaque assay as described previously [13].
2.2. Animals
Female BALB/c mice that were 8–10-weeks-old were obtained from Vital River Laboratories (Beijing, China), while the original breeding pairs were purchased from Charles River (Beijing, China). Mice were raised in independent ventilated cages and received pathogen-free food and water. Experimentation with animals was governed by the Regulations of Experimental Animals of Beijing Authority and approved by the Animal Ethics Committee of the China Agriculture University.
2.3. Chronic Heat Stress Model
Mice were randomly divided into two groups: CHS and TN. Mice in the CHS group were placed in a biological oxygen demand (BOD) incubator for 21 days and subjected to chronic heat exposure for 4 h at a temperature of 38 ± 1°C, simulating high Summer temperatures [14]. Mice in the TN and control groups were kept in an incubator at 24 ± 1°C to simulate room temperature. Mice were sacrificed at various time-points and the lung and spleen from each mouse were collected.
2.4. Viral Challenge and Sample Collection
The virus stocks were diluted in phosphate-buffered saline (PBS). Mice were anesthetized with Zotile (Virbac, France) intramuscular at a dose of 15 mg/kg (body weight) and were then infected intranasally with 50 plaque forming units (PFUs) of H5N1 virus. Mice were sacrificed at various time-points and the lung and spleen from each mouse were collected and stored in liquid nitrogen until required.
2.5. Plaque Assay
MDCK cells were cultured in Dulbecco's modified Eagle's medium (DMEM; Hyclone Laboratories) containing 10% FBS (Hyclone Laboratories), 100 U/mL penicillin, and 100 μg/mL streptomycin. The supernatants of mouse lung tissues were diluted 10-fold and added to a monolayer of MDCK cells in semisolid agar that contained 0.5 μg/mL of trypsin TPCK (Sigma-Aldrich, St Louis, MO, USA). Cultures were incubated at 37°C, 5% CO2 for 60–72 hours, fixed, and stained with 1% crystal violet. The plaques were counted and photographed.
2.6. Histopathological and Immunohistochemical Analysis
Tissues were removed and fixed with 4% neutral formalin at room temperature for 48 h. The serial tissue sections were cut to 5 μm thickness after embedding in paraffin. Each slide was stained with hematoxylin and eosin (H&E) and then examined by light microscopy (Olympus CX31). Examination of influenza viral antigen in the tissue samples was performed by immunohistochemical analysis. Sections were incubated in 10% normal goat serum in PBS for 30 minutes to block non-specific binding sites before being reacted with the anti-influenza nucleoprotein mAb (AA5H, Abcam) at 1 : 1000 dilutions in PBS for 2 h. The slides were further incubated with goat anti-mouse IgG conjugated with avidin (Chemicon, USA) for 1 h and followed by an incubation of the biotinlated peroxidase (Victoria, BC, Canada) for additional 1 h. Staining was visualized by the addition of 3,3-diaminobenzidin (DAB, Sigma, St. Louis, Mo., USA ) for 15 min and counterstained with haematoxylin mounted with neutral balsam.
2.7. Quantitative PCR (qPCR)
Total RNA was prepared from 10 mg lung tissue homogenized in Trizol (Invitrogen, Carlsbad, CA, USA) according to the manufacturer's instructions. The DNaseI-treated RNA (0.2 μg) was reverse transcribed into cDNA. Quantification of expression of the hemagglutinin (HA) gene of H5N1 influenza virus was conducted using a Power SYBR Green PCR Master Mix kit (ABI). The following primers were used in the qPCR: forward primer, 5′-CGC AGT ATT CAG AAG AAG CAA GAC-3′; and reverse primer, 5′-TCC ATA AGG ATA GAC CAG CTA CCA-3′. The reaction was run on an ABI 7500 thermal cycler with an initial denaturation step at 95°C for 10 minutes, followed by 40 cycles of 95°C for 15 seconds, 56°C for 30 seconds, and 72°C for 40 seconds. Data analysis was performed using 7500 software v2.0 (ABI). The copy number of the HA gene was calculated using an HA-containing plasmid of known concentration as a standard.
Quantification by qPCR was performed for five other genes: β-actin (primers, 5′-GAG ACC TTC AAC ACC CCG C-3′ and 5′-ATG TCA CGC ACG ATT TCC C-3′), IL-6 (5′-AGC CAG AGT CCT TCA-3′ and 5′-TCT TGG TCC TTA GCC-3′), IL-10 (5′-GGT TGC CAA GCC TTA TCG GA-3′ and 5′-ACC TGC TCC ACT GCC TTG CT-3′), IFN-β (5′-TCC AGC TCC AAG AAA GGA CG-3′ and 5′-GCA TCT TCT CCG TCA TCT CC-3′), and HSP70 (5′-TGA GCA GCC CAT CCT TAG TG-3′ and 5′-ATA GGC ATC CGT CCC TTT GT-3′). Reactions were carried out on an ABI 7500 with initial denaturation at 95°C for 10 min, then 40 cycles of denaturation at 95°C for 15 s, annealing at 50°C for 30 s, and extension at 72°C for 40 s using a Power SYBR Green PCR Master Mix kit. Gene expression was normalized to that of the TN group using the 2−ΔΔCT method with β-actin as an internal standard [15].
2.8. Bronchoalveolar Lavage (BAL) Collection and Pulmonary Alveolar Macrophage (PAM) Counting
At 21 days after exposure to 38 ± 1°C or 24 ± 1°C, the mice were euthanized with a lethal dose of pentobarbital. BAL was collected using 0.8 mL saline twice from the main stem bronchus. The BAL collected from one mouse was pooled centrifuged, and cells were resuspended in 100 mL saline containing 0.1% BSA. Cells were stained with Giemsa, and cell types were identified by morphological criteria. Two hundred cells were examined per slide for the pulmonary alveolar macrophage (PAM) count.
2.9. DC Cell Surface Costimulatory Molecules
Fluorophore-conjugated rat antimouse monoclonal antibodies including anti-MHC-II-PE, anti-CD40-PE, anti-CD80-PE, anti-CD86-PE, anti-CD11c-FITC, and isotype controls were purchased from BDPharMingen (San Diego, CA, USA). CFSE was obtained from Molecular Probes (Eugene, OR, USA). Three mice from each group were sacrificed after exposure to 38 ± 1°C or 24 ± 1°C for 21 days, and single cell suspensions from the spleens at a concentration of 2 × 106 cells/200 μL were blocked with 2 μL Fcγ monoclonal antibody (0.5 μg/mL) for 30 min at 4°C. After rinsing once with PBS, cells were stained with isotype controls, or double stained with anti-CD11c-FITC and anti-CD40-PE, or anti-CD11c-FITC and anti-CD80-PE, or anti-CD11c- FITC and anti-CD86-PE, or anti-CD11c-FITC and anti-MHC-II-PE. The fluorescent intensities were measured with a FACSCalibur and analyzed with Cell Questpro software (BD Biosciences, USA).
2.10. Statistical Analysis
Statistical analysis was performed using one-way ANOVAs with SPSS 12.0 (SPSS Taiwan Corp., Taiwan) and P-values less than .05 were considered statistically significant.
3. Results
3.1. Chronic Heat Stress Reduced Local Immunity in the Respiratory Tract of Mice
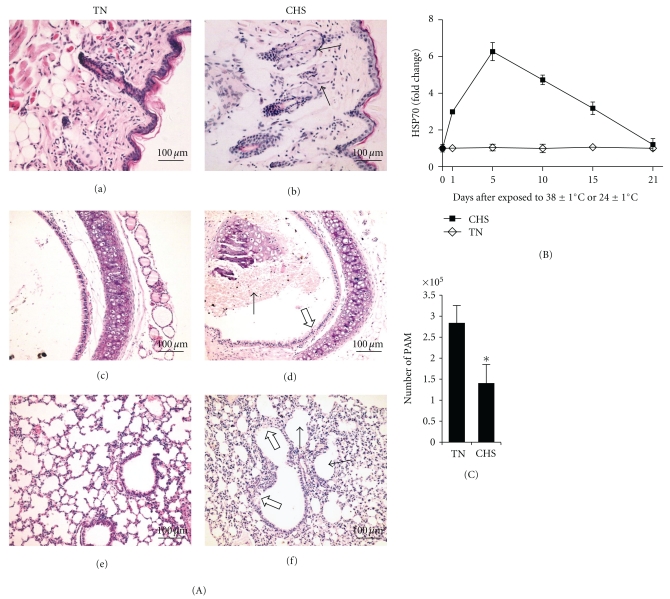
To determine the effect of CHS on local immunity in the respiratory tract of mice, the histopathological changes in the nasal mucosa, trachea, and lungs of the mice in each group after exposure to 38 ± 1°C or 24 ± 1°C for 21 days were examined (Figure 1(a)). The nasal mucosa lesions of mice in the CHS group exhibited sebaceous gland hyperplasia (Figure 1(A)(b)). The tracheal lesions in the CHS mice were characterized by a reduction in tracheal epithelial cells and many erythrocytes had infiltrated the tube cavity of the trachea (Figure 1(A)(d)). Changes in lung pathology included a reduction and necrosis of mucous epithelium cells in the bronchioles and alveolar expansion (Figure 1(A)(f)). In comparison, the nasal mucosa, trachea, and lungs from the TN group exhibited no apparent histological changes (Figures 1(A)(a), (c), and (e)).
Figure 1.
Analysis of the local immunity in the respiratory tract of mice. (A) Representative sections from each group were stained by H&E after exposed to 38 ± 1°C or 24 ± 1°C over 21 days (400×). (a) Normal nasal sections from TN mice. (b) Nasal lesions from CHS mice. Solid arrows indicate sebaceous gland hyperplasia. (c) Normal tracheal sections from TN mice. (d) Tracheal lesions from CHS mice. Solid arrows indicate erythrocytes infiltrated in the tube cavity of the trachea and unshaded arrows indicate the dropout of trachea epithelium cells. (e) Normal lung section from TN mice.(f) Lung lesion from CHS mice. Solid arrows indicate alveolar expansion and unshaded arrows indicate a reduction and necrosis of mucous epithelial cells. (B) The mRNA levels of HSP70 in the lungs were determined by qPCR at various time-points. (C) PAM counting from BAL was performed after exposure to 38 ± 1°C or 24 ± 1°C for 21 days. These results are the mean ± SD values obtained from three distinct animals and are representative of three independent experiments. *indicates P < .05 when compared with the TN group. TN: thermally neutral; CHS: chronic heat stress.
In a previous study, heat stress was characterized by the production of HSPs, especially HSP70 [16]. To determine the mRNA expression of HSP70, we used qPCR analysis. HSP70 expression in the lungs of mice was induced at one day after exposure to 38 ± 1°C, peaking at day 5 and then returned to normal levels at day 21 (Figure 1(B)).
The BAL from the mice following exposure to 38 ± 1°C or 24 ± 1°C for 21 days was collected for PAM counting. The number of PAMs in the CHS group were significantly lower than those in the TN group (Figure 1(C)). These results suggest that CHS can reduce local immunity in the respiratory tract of mice and also inhibit expression of HSP70.
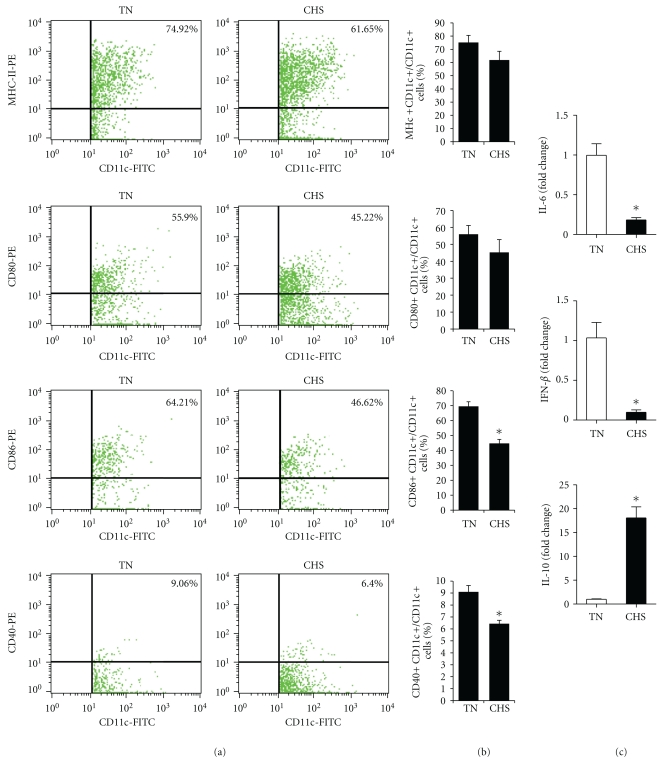
3.2. CHS Weakened the Innate Immunity in Mice
The maturation or activation of DCs is very important for innate immunity and subsequent adaptive immunity. The expression of costimulatory markers CD40, CD86, and CD80 at the DC surface correlated with their capacity to induce or suppress immune responses and the MHC-II expression is important in the initiation of immune response [17]. DC maturation of mice exposed to 38 ± 1°C or 24 ± 1°C for 21 days was determined by FACS (Figures 2(A) and 2(B)). The MHC-II, CD40, CD80 and CD86 expression levels in the CHS group were lower than these of the TN group, especially CD86 and CD40 (P < .05). Previous studies have shown that IL-6, IL-10, and IFN-β played critical roles in the innate immune responses [18–20]. To determine the effect of CHS on the innate immunity associated with cytokine expression in mice, the mRNA levels of IL-6, IL-10, and IFN-β in the spleen after exposure to 38 ± 1°C or 24 ± 1°C were examined. The IL-6 and IFN-β mRNA levels of the CHS group were downregulated significantly compared to the TN group, while IL-10 was significantly upregulated (P < .05) (Figure 2(C)). The mRNA level of TNF-α was also measured, but there was no significant difference between two groups (data not shown). These data suggest that CHS could adversely affect the maturation of DCs and innate immunity in mice.
Figure 2.
Analysis of maturation of DCs and innate immunity associated cytokine expression in mice. (a) Total splenocytes were isolated from the spleen of mice exposed to 38 ± 1°C or 24 ± 1°C over 21 days. Double staining for MHC-II+ CD11c+, CD80+ CD11c+, CD86+ CD11c+, and CD40+ CD11c+ cells was performed. The proportion of double-positive cells in the dot-plot are shown in the upper right corner of the quadrant, with the gate set for CD11c+ cells or events. Data shown are representative of three independent experiments. (b) Summaries of the proportion of MHC-II+ among total CD11c+ cells, CD80+ among CD11c+ cells, CD86+ among CD11c+ cells, and CD40+ among CD11c+ cells. (c) IL-6, IFN-β, and IL-10 mRNA levels from the spleens of mice exposed to 38 ± 1°C or 24 ± 1°C for 21 days were determined by qPCR. These results are the mean ± SD values obtained from three distinct animals and are representative of three independent experiments. * indicates P < .05 when compared with the TN group.
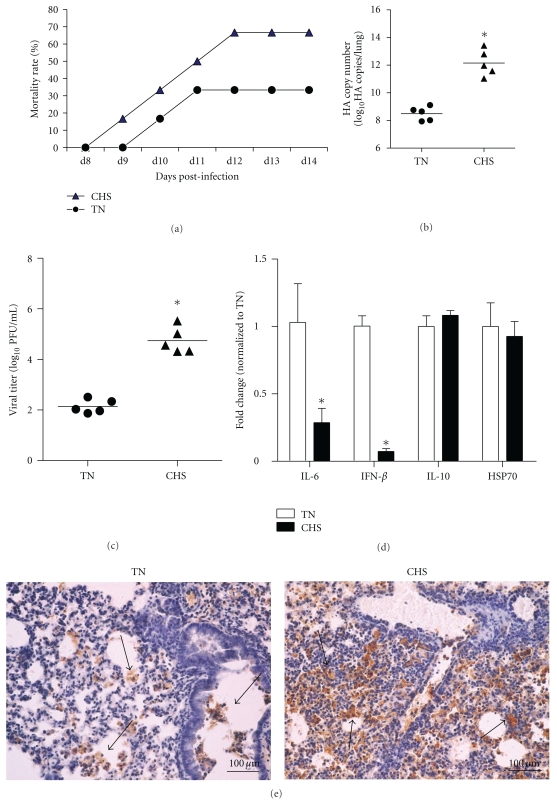
3.3. CHS Increased the Virulence of HPAIV in Infected Mice
To determine whether CHS could impact upon HAPIV H5N1 infection, the mice exposed to 38 ± 1°C or 24 ± 1°C for 21 days were challenged with 50 PFU of H5N1 virus. The lung tissues of five mice per group were collected at Day 3 postinfection for real-time PCR, plaque assay, and histopathogic analysis. Six mice per group were observed for mortality rate for 14 days. Results showed that the mice in the CHS group had a higher mortality rate (67%) than that in TN group (33%) (Figure 3(a)), but not statistically significant by log rank analysis possibly due to the small sample size. To examine the viral load in the lung of the mice infected with the virus, qPCR and plaque assay were performed. Pulmonary viral load in the mice of the CHS group was significantly higher than that of TN group at day 3 postinfection (Figures 3(b) and 3(c)). The H5N1 viral antigen (NP) was detected extensively in the deciduous alveolar cells and mucosal epithelium cells in the lung (Figure 3(e)). Compared with TN group, more H5N1 viral antigen positive cells could be found in the lung of mice after CHS treatment. And the results were consistent with the ones of qPCR and plaque assay.
Figure 3.
Effects of CHS on the virulence of HPAIV in the infected mice. (a) Six mice per group were observed for mortality at 14 days. And the viral load in lungs at day 3 postinfection was determined by real-time PCR (b) and plaque assay (c).(d) The mRNA levels of IL-6, IFN-β, IL-10, and HSP70 in the lung at day 3 postinfection were determined by qPCR. * indicates P < .05 when compared with the TN group. (e) Representative lung sections from each group were stained with immunohistochemical staining with an antiinfluenza NP mAb (400×), and the arrow indicated the NP positive cells.
The multiple functions of inflammation induced by H5N1 infection potentially affect virus clearance from the host. To evaluate the effect of CHS on inflammation in infected mice, expression of cytokines IL-6, IFN-β, and IL-10 in the lung was determined by qPCR at day 3 postinfection. The mRNA levels of IL-6 and IFN-β in the mice of the CHS group were significantly lower than those in the TN group (Figure 3(d)). The soluble cytokine levels in serum of IL-6 and IFN-β were also measured by ELISA, and the results were in similar trend to the mRNA levels (data not shown). The expression of HSP70 at day 3 postinfection was also determined by qPCR. The results did not show significant differences between two groups (Figure 3(d)). These data indicated that CHS could moderately increase the mortality rate and viral load in the lungs of H5N1-infected mice by decreasing IL-6 and IFN-β expression.
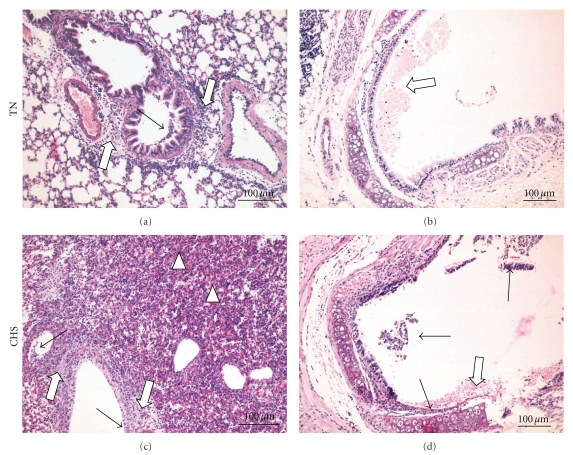
To determine the degree of lung lesion in the infected mice, histopathological changes in the lungs of mice in each group at day 3 postinfection were examined (Figure 4). The lungs of the CHS group mice showed severe alveolitis, peribronchiolitis, and bronchopneumonia, that was characterized by interstitial edema and inflammatory cellular infiltration around small blood vessels, reduction and necrosis of the mucous epithelium of bronchioles, thickening of alveolar walls, and alveolar lumens flooded with edema fluid mixed with exfoliated alveolar epithelial cells, erythrocytes, and inflammatory cells (Figure 4(c)). The trachea of mice in the CHS group exhibited lesions, characterized by exfoliated trachea mucous epithelium cells and a number of erythrocytes and inflammatory cells infiltrated in the tube cavity of the trachea (Figure 4(d)). In mice of the TN group, the lung and trachea lesions were dramatically milder than those observed in the CHS group. The lung lesions in the TN group mice showed peribronchiolitis with interstitial edema and inflammatory cell infiltration around small blood vessels, along with edema and reduction of mucous epithelial cells of the bronchioles (Figure 4(a)). The trachea lesions of mice in the TN group mainly demonstrated erythrocyte infiltration (Figure 4(b)). The results suggested that exposure to 38 ± 1°C for 21 days aggravated lung and trachea lesions in H5N1-infected mice.
Figure 4.
Lung and trachea histopathology following H5N1 infection in mice. Representative lung or trachea sections from each group were stained by H&E (400×). (a) The lung lesions in the TN group of mice showed peribronchiolitis. Solid arrows indicate a reduction in the number of mucous epithelial cells in bronchioles, and unshaded arrows indicate interstitial edema and inflammatory cellular infiltration around small blood vessels and the bronchioles. (b) The tracheal lesions in the TN group of mice. Unshaded arrows indicate erythrocyte infiltration. (c) The lung lesions in the CHS group of mice showed severe alveolitis, peribronchiolitis, and bronchopneumonia. The solid arrows indicate a reduction in necrosis and the number of mucous epithelial cells in bronchioles, with unshaded arrows indicating extreme interstitial edema and vast inflammatory cellular infiltration. Triangles indicate alveolar lumens flooded with edema fluid mixed with exfoliated alveolar epithelial cells, erythrocytes, and inflammatory cells. (d) The tracheal lesions in the CHS group of mice. Solid arrows indicate exfoliation or necrosis of tracheal mucous epithelial cells, and unshaded arrows indicate erythrocytes and inflammatory cellular infiltration in the tube cavity of the trachea.
4. Discussion
In a previous study, we reported that CHS could retard the adaptive immune response by suppressing both humoral and cellular responses [2]. In this study we have demonstrated that CHS can significantly suppress host innate immunity in mice and moderately increase the mortality of H5N1-infected mice. CHS retarded systemic and local innate immune responses significantly, including the number of PAMs, DC maturation, mRNA levels of IL-6, IFN-β, and HSP70, and caused respiratory system lesions. When mice were infected with H5N1 virus after CHS conditioning, the mortality rate and viral load in the lungs increased. Lung histopathology results of infected mice further confirmed that CHS could moderately increase virulence in H5N1-infected mice.
The respiratory mucosa is the first barrier encountered by invading microorganisms. The function and immunity of the respiratory system was closely related to mucosal architecture, PAMs, and other local immune cells or proteins. In the present study, we showed that CHS could reduce local immunity in the respiratory tract of mice by destroying the structural integrity of nasal mucosa, trachea, and lungs and reducing the number of PAMs. The results suggested that CHS could retard the local immunity in respiratory system in mice and rendered them to be susceptible to secondary infection of bacteria or viruses.
Heat stress is often characterized by the production of HSPs. The HSPs, in particular Hsp27, Hsp32, Hsp60, and Hsp70, have an important cytoprotective role during lung inflammation and injury [16], as they can activate the innate immune system, linking innate and adaptive immune responses [21, 22]. Previous studies also indicated that HSPs played an immunoregulatory role in chronic inflammation [23, 24]. The results of the expression of HSP70 under chronic heat stress in this study showed that the HSP70 level increased on day 1, peaked on day 5, decreased from day 10, and appeared to be normal level on day 21 after exposure to 38 ± 1°C, which suggested that the lack of HSP70 may be associated with the suppression of innate immunity by CHS.
The DCs are the most potent antigen presenting cells (APCs), and activation of DCs is a crucial and early event of immune regulation [25]. The expression of costimulatory molecules (CD40, CD86, and CD80) at the DC surface correlated with their capacity to induce or suppress immune responses. The MHC-II molecules expressed on the surface of APCs are important in the initiation of an immune response [17]. In this study, we observed lower levels of expression of MHC-II, CD40, CD80, and CD86 in CHS mice compared to the TN mice, which indicated that CHS weakened antigen processing not only in APCs but also in the co-stimulatory pathway, which in turn leads to lower immune responses. IL-6 and IFN-β play critical roles in the development and maintenance of innate immune responses [18, 19, 26]. IL-10 has been considered to be a suppressive cytokine known to inhibit Th1 cytokine expression [20, 27, 28]. We have shown that CHS downregulates IL-6 and IFN-β expression and upregulates the levels of IL-10. These data further demonstrated that CHS induced lower innate immunity.
The H5N1 influenza virus can cause severe respiratory symptoms in humans with clinical manifestations that include fever, diarrhea, viral pneumonia, encephalitis, and acute respiratory distress syndrome. High levels of proinflammatory cytokines, including TNF-α, IL-6, and CC chemokine ligand 2 (CCL2), have been detected in human cells and mice infected with highly pathogenic H5N1 influenza virus [29, 30]. Generally, a virus-induced cytokine storm has been widely hypothesized to be the main cause of pathology and death during H5N1 infection. There are numerous reports regarding the use of therapeutic agents to control inflammatory responses in influenza infection [31]; however, it is not clear as to whether they are effective in controlling virus replication. Without antiviral agents, knockout mice deficient in TNF-α, TNF-α receptor 1, TNF-α receptor 2, IL-6, chemokine (C-C motif) ligand 2, MIP-1α, and IL-1R or steroid-treated wild-type mice did not have a survival advantage over wild-type mice following influenza virus challenge [32, 33]. On the other hand, type I interferon response that contributes to control of H5N1 virus replication has been demonstrated [34, 35]. The multiple functions of inflammation and cytokines are essential for virus clearance from the host. The antiviral immune response induced by H5N1 virus infection was complicated, involving multiple classes of pattern recognition receptors (PRRs), and different signaling pathways. Although the inflammation is widely suggested to be the main cause of death from H5N1 infection, the results from the knockout mice deficient in single cytokine were insufficient to clarify the complex process. In this study, our results suggested that CHS treatment retarded the innate immunity. This may be one of the underlying causes of increased death rates by H5N1 virus after CHS treatment.
In summary, the data presented here demonstrate that CHS treatment significantly suppressed innate host immunity in mice and increased mortality following H5N1 infection. This study is the first to show that CHS affects systemic and local innate immune responses as well as survival of H5N1-infected in mice. Our results suggest that after a long period of suffering elevated temperatures, the balance in the immune system is destroyed and H5N1 virulence is increased.
Acknowledgments
The authors thank the National Natural Science Foundation of China (Grant no. 31001047) and the Research Fund for the Doctoral Program of Higher Education (Grant no. 20100008120006) for financial support. Y. Jin and Y. Hu Two contributed to the work equally.
References
- 1.Goligorsky MS. The concept of cellular “fight-or-flight” reaction to stress. American Journal of Physiology. 2001;280(4):F551–F561. doi: 10.1152/ajprenal.2001.280.4.F551. [DOI] [PubMed] [Google Scholar]
- 2.Hu Y, Jin H, Du X, et al. Effects of chronic heat stress on immune responses of the foot-and-mouth disease DNA vaccination. DNA and Cell Biology. 2007;26(8):619–626. doi: 10.1089/dna.2007.0581. [DOI] [PubMed] [Google Scholar]
- 3.Khajavi M, Rahimi S, Hassan ZM, Kamali MA, Mousavi T. Effect of feed restriction early in life on humoral and cellular immunity of two commercial broiler strains under heat stress conditions. British Poultry Science. 2003;44(3):490–497. doi: 10.1080/000071660310001598328. [DOI] [PubMed] [Google Scholar]
- 4.Le Bellego L, van Milgen J, Noblet J. Effect of high temperature and low-protein diets on the performance of growing-finishing pigs. Journal of Animal Science. 2002;80(3):691–701. doi: 10.2527/2002.803691x. [DOI] [PubMed] [Google Scholar]
- 5.Lu Q, Wen J, Zhang H. Effect of chronic heat exposure on fat deposition and meat quality in two genetic types of chicken. Poultry Science. 2007;86(6):1059–1064. doi: 10.1093/ps/86.6.1059. [DOI] [PubMed] [Google Scholar]
- 6.Odongo NE, Alzahal O, Lindinger MI, et al. Effects of mild heat stress and grain challenge on acid-base balance and rumen tissue histology in lambs. Journal of Animal Science. 2006;84(2):447–455. doi: 10.2527/2006.842447x. [DOI] [PubMed] [Google Scholar]
- 7.Liew PK, Zulkifli I, Hair-Bejo M, Omar AR, Israf DA. Effects of early age feed restriction and heat conditioning on heat shock protein 70 expression, resistance to infectious bursal disease, and growth in male broiler chickens subjected to heat stress. Poultry Science. 2003;82(12):1879–1885. doi: 10.1093/ps/82.12.1879. [DOI] [PubMed] [Google Scholar]
- 8.Zulkifli I, Abdulllah N, Azrin NM, Ho YW. Growth performance and immune response of two commercial broiler strains fed diets containing Lactobacillus cultures and oxytetracycline under heat stress conditions. British Poultry Science. 2000;41(5):593–597. doi: 10.1080/713654979. [DOI] [PubMed] [Google Scholar]
- 9.Davison TF, Misson BH, Williamson RA, Rea J. Effect of increased circulating corticosterone in the immature fowl on the blastogenic responses of peripheral blood lymphocytes. Developmental and Comparative Immunology. 1988;12(1):131–144. doi: 10.1016/0145-305x(88)90031-6. [DOI] [PubMed] [Google Scholar]
- 10.Donker RA, Beuving G. Effect of corticosterone infusion on plasma corticosterone concentration, antibody production, circulating leukocytes and growth in chicken lines selected for humoral immune responsiveness. British Poultry Science. 1989;30(2):361–369. doi: 10.1080/00071668908417157. [DOI] [PubMed] [Google Scholar]
- 11.Fang LQ, de Vlas SJ, Liang S, et al. Environmental factors contributing to the spread of H5N1 avian influenza in mainland China. PLoS One. 2008;3(5) doi: 10.1371/journal.pone.0002268. Article ID e2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fang LQ, Cao CX, Chen GS, et al. Studies on the spatial distribution and environmental factors of highly pathogenic avian influenza in Mainland China, using geographic information system technology. Chinese Journal of Epidemiology. 2005;26(11):839–842. [PubMed] [Google Scholar]
- 13.Wu Y, Zhang G, Li Y, et al. Inhibition of highly pathogenic avian H5N1 influenza virus replication by RNA oligonucleotides targeting NS1 gene. Biochemical and Biophysical Research Communications. 2008;365(2):369–374. doi: 10.1016/j.bbrc.2007.10.196. [DOI] [PubMed] [Google Scholar]
- 14.Sinha RK. Electro-encephalogram disturbances in different sleep-wake states following exposure to high environmental heat. Medical and Biological Engineering and Computing. 2004;42(3):282–287. doi: 10.1007/BF02344701. [DOI] [PubMed] [Google Scholar]
- 15.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25(4):402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 16.Wheeler DS, Wong HR. Heat shock response and acute lung injury. Free Radical Biology and Medicine. 2007;42(1):1–14. doi: 10.1016/j.freeradbiomed.2006.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clatza A, Bonifaz LC, Vignali DA, Moreno J. CD40-induced aggregation of MHC class II and CD80 on the cell surface leads to an early enhancement in antigen presentation. Journal of Immunology. 2003;171(12):6478–6487. doi: 10.4049/jimmunol.171.12.6478. [DOI] [PubMed] [Google Scholar]
- 18.Thornley TB, Phillips NE, Beaudette-Zlatanova BC, et al. Type 1 IFN mediates cross-talk between innate and adaptive immunity that abrogates transplantation tolerance. Journal of Immunology. 2007;179(10):6620–6629. doi: 10.4049/jimmunol.179.10.6620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vanden Bush TJ, Buchta CM, Claudio J, Bishop GA. Cutting edge: importance of IL-6 and cooperation between innate and adaptive immune receptors in cellular vaccination with B lymphocytes. Journal of Immunology. 2009;183(8):4833–4837. doi: 10.4049/jimmunol.0900968. [DOI] [PubMed] [Google Scholar]
- 20.Nakagome K, Dohi M, Okunishi K, et al. In vivo IL-10 gene delivery suppresses airway eosinophilia and hyperreactivity by down-regulating APC functions and migration without impairing the antigen-specific systemic immune response in a mouse model of allergic airway inflammation. Journal of Immunology. 2005;174(11):6955–6966. doi: 10.4049/jimmunol.174.11.6955. [DOI] [PubMed] [Google Scholar]
- 21.Anderson KM, Srivastava PK. Heat, heat shock, heat shock proteins and death: a central link in innate and adaptive immune responses. Immunology Letters. 2000;74(1):35–39. doi: 10.1016/s0165-2478(00)00246-7. [DOI] [PubMed] [Google Scholar]
- 22.Wallin RP, Lundqvist A, More SH, von Bonin A, Kiessling R, Ljunggren HG. Heat-shock proteins as activators of the innate immune system. Trends in Immunology. 2002;23(3):130–135. doi: 10.1016/s1471-4906(01)02168-8. [DOI] [PubMed] [Google Scholar]
- 23.Hirayama E. Relationship of HSP70 to temperature-dependency of influenza viral infection. Yakugaku Zasshi. 2004;124(7):437–442. doi: 10.1248/yakushi.124.437. [DOI] [PubMed] [Google Scholar]
- 24.Van Eden W, Wick G, Albani S, Cohen I. Stress, heat shock proteins, and autoimmunity: how immune responses to heat shock proteins are to be used for the control of chronic inflammatory diseases. Annals of the New York Academy of Sciences. 2007;1113:217–237. doi: 10.1196/annals.1391.020. [DOI] [PubMed] [Google Scholar]
- 25.Weigel BJ, Nath N, Taylor PA, et al. Comparative analysis of murine marrow-derived dendritic cells generated by Flt3L or GM-CSF/IL-4 and matured with immune stimulatory agents on the in vivo induction of antileukemia responses. Blood. 2002;100(12):4169–4176. doi: 10.1182/blood-2002-04-1063. [DOI] [PubMed] [Google Scholar]
- 26.Popko K, Gorska E, Stelmaszczyk-Emmel A, et al. Proinflammatory cytokines Il-6 and TNF-alpha and the development of inflammation in obese subjects. European Journal of Medical Research. 2010;15(2):120–122. doi: 10.1186/2047-783X-15-S2-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang Z, Chen M, Wu R, et al. Suppression of autoimmune diabetes by viral IL-10 gene transfer. Journal of Immunology. 2002;168(12):6479–6485. doi: 10.4049/jimmunol.168.12.6479. [DOI] [PubMed] [Google Scholar]
- 28.Fiorentino DF, Zlotnik A, Vieira P, et al. IL-10 acts on the antigen-presenting cell to inhibit cytokine production by Th1 cells. Journal of Immunology. 1991;146(10):3444–3451. [PubMed] [Google Scholar]
- 29.Szretter KJ, Gangappa S, Lu X, et al. Role of host cytokine responses in the pathogenesis of avian H5N1 influenza viruses in mice. Journal of Virology. 2007;81(6):2736–2744. doi: 10.1128/JVI.02336-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chan MC, Cheung CY, Chui WH, et al. Proinflammatory cytokine responses induced by influenza A (H5N1) viruses in primary human alveolar and bronchial epithelial cells. Respiratory Research. 2005;6 doi: 10.1186/1465-9921-6-135. Article ID 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rainsford KD. Influenza (“Bird Flu”), inflammation and anti-inflammatory/analgesic drugs. Inflammopharmacology. 2006;14(1-2):2–9. doi: 10.1007/s10787-006-0002-5. [DOI] [PubMed] [Google Scholar]
- 32.Salomon R, Hoffmann E, Webster RG. Inhibition of the cytokine response does not protect against lethal H5N1 influenza infection. Proceedings of the National Academy of Sciences of the United States of America. 2007;104(30):12479–12481. doi: 10.1073/pnas.0705289104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carter MJ. A rationale for using steroids in the treatment of severe cases of H5N1 avian influenza. Journal of Medical Microbiology. 2007;56(7):875–883. doi: 10.1099/jmm.0.47124-0. [DOI] [PubMed] [Google Scholar]
- 34.Szretter KJ, Gangappa S, Belser JA, et al. Early control of H5N1 influenza virus replication by the type I interferon response in mice. Journal of Virology. 2009;83(11):5825–5834. doi: 10.1128/JVI.02144-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haasbach E, Droebner K, Vogel AB, Planz O. Low-Dose Interferon Type I Treatment Is Effective Against H5N1 and Swine-Origin H1N1 Influenza a Viruses In vitro and In vivo. doi: 10.1089/jir.2010.0071. Journal of Interferon and Cytokine Research. In Press. [DOI] [PubMed] [Google Scholar]