Abstract
The V protein of the paramyxovirus Nipah virus (NiV) has been shown to antagonize the interferon (IFN) response in human cells via sequestration of STAT1 and STAT2. This study describes a mutant of the NiV V protein, referred to as V(AAHL), that is unable to antagonize IFN signalling and demonstrates that a single amino acid substitution is responsible for its inactivity. The molecular basis for this was identified as a failure to interact with STAT1 and STAT2. It was also shown that NiV V, but not V(AAHL), was functional as an IFN antagonist in human, monkey, rabbit, dog, horse, pig and bat cells, which suggests that the ability of NiV to block IFN signalling is not a major constraint that prevents this virus from crossing species barriers.
In the last decade, zoonotic outbreaks of respiratory disease and encephalitis affecting humans, horses and pigs in Australia, Malaysia and Singapore have led to the isolation of two novel paramyxoviruses, Hendra virus (HeV) and Nipah virus (NiV) (Chua et al., 2000; Murray et al., 1995; O'Sullivan et al., 1997). However, due to characteristic differences from other paramyxoviruses they have been assigned to a new genus, Henipavirus (Wang et al., 2000). The natural hosts of both HeV and NiV are fruit bats (suborder Megachiroptera) of the genus Pteropus (Chua et al., 2002; Halpin et al., 2000). Neutralizing antibodies to NiV have also been found in an insectivorous bat (suborder Microchiroptera) (Yob et al., 2001). In the initial HeV and NiV outbreaks, the viruses were transmitted from bats to humans by way of intermediate animal hosts, horses and pigs, respectively (Chua et al., 2000). More recent outbreaks of NiV in Bangladesh and India have led to further human deaths and may have been a result of both bat-to-human and human-to-human transmissions (Butler, 2004; Chadha et al., 2006; Enserink, 2004; Hsu et al., 2004).
Similar to other paramyxoviruses, both henipaviruses have the potential to express multiple proteins, P, V, W and C, from the P gene by RNA editing and alternative translational initiation (reviewed by Lamb & Kolakofsky, 2001). The V and/or C proteins of various paramyxoviruses have been demonstrated to antagonize the interferon (IFN) system, part of the innate cellular immune response to viral infection, in several distinct ways (for recent reviews, see Horvath, 2004; Nagai & Kato, 2004; Stock et al., 2005). NiV and HeV antagonize both IFN-α/β and IFN-γ signalling via the binding and sequestration of STAT1 and STAT2 in high-molecular-mass complexes (Rodriguez et al., 2002, 2003). In other paramyxoviruses, the highly conserved cysteine-rich C terminus of the V protein is required to antagonize IFN signalling, but although henipavirus V proteins share this conserved C-terminal domain, it is dispensable for the sequestration of STAT1 and STAT2 by these viruses (Rodriguez et al., 2004; Shaw et al., 2004). The regions of NiV V that interact with STAT1 and STAT2 have been mapped to the N terminus of the protein, from residues 100 to 160 for STAT1 binding and a larger region comprising residues 100–300 for STAT2 binding (Rodriguez & Horvath, 2004; Rodriguez et al., 2004). A similar study by Shaw et al. (2004) identified an overlapping area, residues 50–150, as sufficient for binding of STAT1 (Shaw et al., 2004). These regions are also present in the NiV P and W proteins, both of which have been demonstrated to block IFN-α/β signalling and to bind STAT1 (Rodriguez et al., 2002; Shaw et al., 2004). The P, V and W proteins of NiV, as well as the C protein, which has a sequence distinct from other P gene products as a result of alternative translational initiation, also antagonize the IFN response in chicken cells (Park et al., 2003).
As part of our comparative studies on how viruses circumvent the IFN response in different species, we were looking at the V protein of NiV. To this end, a cDNA encoding the NiV P gene was isolated from a plaque-purified NiV stock held at the Australian Animal Health Laboratory in Geelong, Australia (named NiV-AAHL for this study), which was derived from a human isolate. As the V mRNA is produced by insertion of a non-templated G residue into the P gene transcript at a conserved editing site, we introduced an extra G residue into the cDNA by overlapping PCR and cloned the open reading frame into the mammalian expression vector pEF.plink2 (Didcock et al., 1999). A c-myc epitope tag was fused to the N terminus of NiV V to facilitate detection of the protein. Very surprisingly, given previously published work, IFN signalling assays in Vero cells showed that NiV-AAHL V [referred to as V(AAHL) hereafter] was unable to antagonize either IFN-α/β (Fig. 1a) or IFN-γ signalling (data not shown).
Fig. 1.
NiV V(AAHL) inhibitory activity is disrupted by a point mutation. (a) Vero cells were transfected with expression vectors for myc-tagged NiV V variants (as indicated) or empty pEF.plink2 expression vector (Ctrl). Cells were also transfected with an IFN-α/β-responsive luciferase reporter plasmid [p(9–27ISRE)4tkΔ(−39)lucter] and a housekeeping-controlled β-galactosidase reporter plasmid (pJATlacZ) (Didcock et al., 1999). Cells were stimulated with 1.8×104 IU IFN-α ml−1 (Roferon-A; Roche Diagnostics) (+) or left untreated (−), and 4–6 h later were lysed and assayed for luciferase and β-galactosidase activity. Luciferase values were normalized to β-galactosidase values and the results are shown as means±sd obtained from five independent transfections. Means of induction factors (induced/uninduced activity) are indicated below the graph. (b) Schematic representation of V(CDC) with STAT1- and STAT2-binding regions. Shaded areas indicate (from left to right) the STAT1-binding region, the nuclear export signal (NES), essential residues interacting with STAT2 (*) and the conserved C-terminal domain (C-term). Numbers above the bar represent amino acid positions. Nucleotide and amino acid differences in V(AAHL) are indicated in open boxes. The P206L mutation (see Fig. 3) is indicated in the filled box. Upper case is used for amino acid residues and lower case for nucleotides.
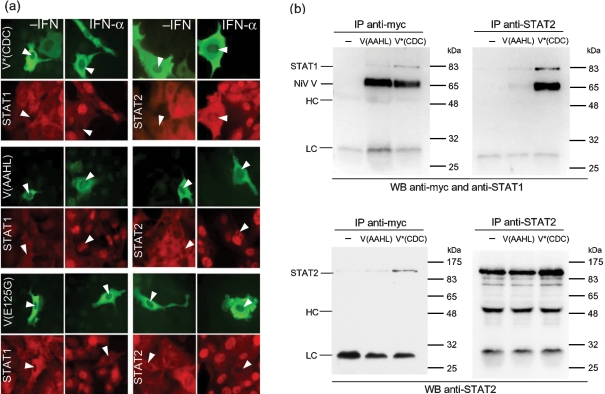
Sequence analysis of the V(AAHL) gene and comparison with the V gene of the reference strain originally published by the CDC group (GenBank accession no. NP_112023; Chua et al., 2000) and termed V(CDC) in this study revealed four nucleotide differences, two of which resulted in changes in the amino acid sequence of the V protein at residues 125 and 280 (Fig. 1b, open boxes). The P sequence from which V(AAHL) had been derived differed from the CDC sequence in the same four nucleotides. As V(CDC) was shown by Rodriguez et al. (2002) to block IFN signalling (Rodriguez et al., 2002), we mutated residues 125 and 280 in V(AAHL) to the equivalent residues in V(CDC). The resulting protein, termed V*(CDC), was able to antagonize both IFN-α/β and IFN-γ signalling in Vero cells (Fig. 1a and data not shown). Subsequently, these two amino acid changes were introduced into V(AAHL) individually, creating V(AAHL)-E125G and V(AAHL)-D280N. As shown in Fig. 1(a), only the mutant containing the E125G mutation was able to block IFN-α/β signalling. V(AAHL)-E125G was also able to antagonize IFN-γ signalling (data not shown). These results indicated that a single amino acid change from glutamic acid (E) to glycine (G) at residue 125 enabled V(AAHL) to block IFN signalling, suggesting that this residue plays a critical role in IFN antagonism by NiV V. Subsequent immunofluorescence experiments showed that constructs containing the E125G mutation, V(AAHL)-E125G and V*(CDC), prevented the nuclear translocation of STAT1 and STAT2 in response to IFN-α (Fig. 2a) and also the nuclear translocation of STAT1 in response to IFN-γ (not shown), as previously demonstrated for V(CDC) (Rodriguez et al., 2002), whilst V(AAHL) did not affect the distribution of STATs. Furthermore, residue 125 lies within the proposed STAT1- and STAT2-binding regions of NiV V (Rodriguez et al., 2004; Shaw et al., 2004), suggesting that the inactivity of V(AAHL) results from defective STAT binding. Indeed, co-immune precipitation experiments showed that the ability of V(AAHL) to bind STAT1 or STAT2 was dramatically reduced, whereas introduction of the glycine at residue 125 in V*(CDC) restored the binding capacity (Fig. 2b). The G374A mutation also causes an amino acid change in the sequence of the C protein. However, although the C protein has been reported to be a weak IFN antagonist, its mode of action is unknown (Park et al., 2003; Shaw et al., 2004) and thus speculation about the possible influence of such a mutation on the function of C cannot be made at present.
Fig. 2.
NiV V(AAHL) does not interact with STAT1 or STAT2. (a) Immunofluorescence. 2fTGH cells were transfected with myc-tagged V(AAHL), V*(CDC) or V(AAHL)-E125G expression constructs and stimulated for 70 min with 1.8×104 IU IFN-α ml−1 (Roferon-A; Roche Diagnostics). Cells were fixed and stained with antibodies against the myc tag (green fluorescence) and against either STAT1 (red fluorescence, left panels) or STAT2 (red fluorescence, right panels) as indicated. (b) Co-immunoprecipitation. 293 cells were transfected with expression constructs encoding STAT1 and STAT2 and either myc-tagged V(AAHL) or V*(CDC). Cells were lysed at 48 h post-transfection and complexes containing the V and STAT proteins were precipitated from the lysates using antibodies against either STAT2 or the myc tag, as indicated above each panel. The precipitates were analysed by Western blotting with antibodies detecting either STAT1 and the myc tag or STAT2, as indicated below the panels. The lower right panel confirms efficient precipitation with the anti-STAT2 antibody in all three lysates. HC, Antibody heavy chain; LC, antibody light chain.
NiV is able to replicate not only in bats, humans and pigs, but also in a number of other species such as hamsters, cats, dogs and horses (Hooper et al., 2001; Middleton et al., 2002; Wong et al., 2003). We analysed the ability of NiV V to antagonize IFN signalling in cells from various species including Tb1 Lu lung epithelial cells from Tadarida brasiliensis (ECACC 90020805), which were of particular interest as the bat population of Southeast Asia is thought to be the reservoir of NiV. [It should be noted that T. brasiliensis is not among the bat species identified as the natural host of NiV. However, in addition to four species of fruit bat, antibodies against NiV have also been found in two insectivorous bats, which are more closely related to T. brasiliensis (Field et al., 2001; Wacharapluesadee et al., 2005; Yob et al., 2001).]
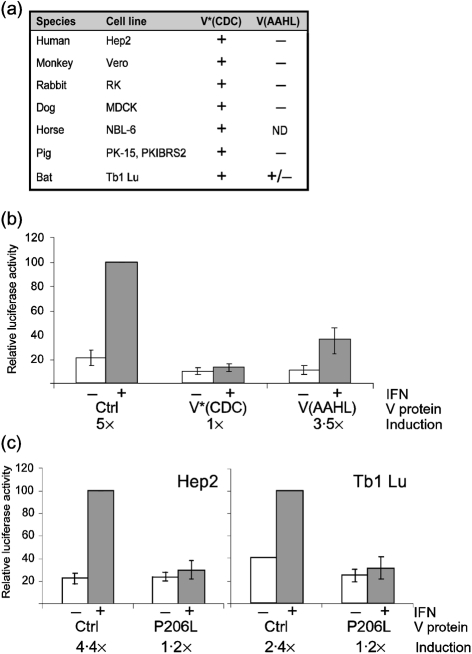
The results from a panel of assays done in cell lines from different species are summarized in Fig. 3(a). V*(CDC) was able to inhibit IFN-α signalling in all species tested, i.e. cells from human, monkey, pig, dog, rabbit, horse and bat. The mutant V(AAHL) was inactive in all species tested except the bat cells, in which it retained some residual activity. A detailed representation of the results obtained in bat Tb1 Lu cells is given in Fig. 3(b). Due to the lack of appropriate tools, such as the sequences of the STAT genes from bat or effective antibodies against bat STAT proteins, we cannot at present provide an experimental explanation for this phenomenon. It might, however, point to a difference in the sequence of bat STAT proteins compared with the other species investigated here.
Fig. 3.
Inhibition of IFN signalling in cells of different species. (a) Summary of signalling results. IFN-α/β signalling assays were carried out as described. +, Inhibition of signalling; −, failure to inhibit signalling. Results were classified as positive (+) when the induction factor was reduced to 30 % or lower compared with the negative control and the value of the stimulated sample was reduced to 25 % or lower compared with the negative control. (b) Details of the results for Tb1 Lu cells given in (a). Instead of commercial IFN-α, these cells were stimulated with purified and UV-inactivated supernatant from Tb1 Lu cells infected with rSV5VΔC (He et al., 2002), a strong inducer of IFN production. Results are shown as means±sd from six independent transfections. Means of induction factors (induced/uninduced activity) are indicated below the graph. (c) Comparison of inhibition of IFN signalling by NiV V(CDC)-P206L in Hep2 and Tb1 Lu cells. Results are shown as means±sd from six (Hep2) or three (Tb1 Lu) independent transfections. Means of induction factors (induced/uninduced activity) are indicated below the graph.
Single amino acid substitutions affecting IFN sensitivity have been observed in other paramyxoviruses and could reflect the ability of these viruses to cross species barriers (Chatziandreou et al., 2002; Garcin et al., 2002; Young et al., 2001). It was therefore of considerable importance to know whether the G125E mutant was a natural variant that might play a role in the species-specific inhibition of IFN signalling or whether it had been generated during cloning of the V(AAHL) gene. We managed to obtain an earlier passage of the original human isolate of NiV(AAHL), as well as the plaque-purified stock that had been used to generate the V(AAHL) expression plasmid used in this study. We amplified the relevant region of the V genes that contained the position in question (positions 8–569, mRNA sense) by RT-PCR. The sequences obtained from both products had a guanine at position 374, which corresponds to a glycine at position 125 of the amino acid chain, and were thus identical to the sequence published for V(CDC). The most likely explanation for this discrepancy therefore appears to be that V(AAHL) represents a PCR artefact that arose during cloning of the expression plasmid. However, given the observation that the G125E mutation did not completely disrupt the function of the V protein in bat cells, we cannot rule out the possibility that, rather than being coincidental, the mutation might have been present in a small population of virus particles in the original stock. Whatever its origin, the results presented here demonstrate that a single amino acid in the STAT1/2-binding region of NiV V is critical for its ability to bind and prevent the relocalization of STATs in response to IFN stimulation. These findings underscore the importance of the N-terminal region of V for interaction with STATs (Rodriguez et al., 2004; Shaw et al., 2004).
Recently, a number of sequences from NiV isolated from humans and pigs, as well as a single bat isolate, have been added to the database (AbuBakar et al., 2004; Chan et al., 2001; Chua et al., 2000, 2002; Harcourt et al., 2005). There are 0–4 aa changes between the V sequences of the different NiV isolates from Malaysia. The isolate from Bangladesh (GenBank accession no. AAY43918; Harcourt et al., 2005) shows considerable variation (up to 53 aa changes, i.e. ∼10 %, throughout the V protein sequence) compared with the Malayan isolates. However, in all of the NiV V sequences, including the bat isolate, and also in the V sequence of the more distantly related HeV, the glycine at position 125 is conserved, in spite of the overall variability of this sequence. Sequence comparison also revealed a single amino acid difference, at position 206 (indicated as a filled box in Fig. 1b), between the human isolate from Malaysia (the CDC isolate) and the Malaysian bat isolate (GenBank accession no. AAM13407; Chua et al., 2002). Although this mutation (P206L) does not lie within the immediate STAT-binding regions, nor within any other identified motif, the substitution of a proline residue could potentially have a dramatic effect on the functionality of the protein. However, when we introduced the P206L mutation into V*(CDC), the resulting protein V(CDC-P206L) inhibited IFN signalling as efficiently as V*(CDC) in human as well as in bat cells (Fig. 3c).
The ability to circumvent the IFN response is one of many factors that can influence the host range of a virus. In this study, the V protein of wild-type NiV proved to be functional as an antagonist of IFN signalling in cells from seven different species. Although these experiments only considered the functionality of V in vitro, reports on experimental and field infections by other groups confirm that NiV is able to infect and replicate in animals from a broad range of species. Given these observations, the ability of NiV to block IFN signalling does not appear to be a major constraint that prevents this virus from crossing species barriers.
Acknowledgments
The authors would like to thank Georg Kochs for the IFN-responsive reporter plasmid. This work was supported by grants from the BBSRC and Wellcome Trust. K. H. was supported by the DFG (grant no. Ha 3479/1-1).
References
- AbuBakar, S., Chang, L.-Y., Ali, A. R. M., Sharifah, S. H., Yusoff, K. & Zamrod, Z. (2004). Isolation and molecular identification of Nipah virus from pigs. Emerg Infect Dis 10, 2228–2230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler, D. (2004). Fatal fruit bat virus sparks epidemics in southern Asia. Nature 429, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chadha, M. S., Comer, J. A., Lowe, L., Rota, P. A., Rollin, P. E., Bellini, W. J., Ksiazek, T. G. & Mishra, A. C. (2006). Nipah virus-associated encephalitis outbreak, Siliguri, India. Emerg Infect Dis 12, 235–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan, Y. P., Chua, K. B., Koh, C. L., Lim, M. E. & Lam, S. K. (2001). Complete nucleotide sequences of Nipah virus isolates from Malaysia. J Gen Virol 82, 2151–2155. [DOI] [PubMed] [Google Scholar]
- Chatziandreou, N., Young, D., Andrejeva, J., Goodbourn, S. & Randall, R. E. (2002). Differences in interferon sensitivity and biological properties of two related isolates of simian virus 5: a model for virus persistence. Virology 293, 234–242. [DOI] [PubMed] [Google Scholar]
- Chua, K. B., Bellini, W. J., Rota, P. A. & 19 other authors (2000). Nipah virus: a recently emergent deadly paramyxovirus. Science 288, 1432–1435. [DOI] [PubMed] [Google Scholar]
- Chua, K. B., Koh, C. L., Hooi, P. S., Wee, K. F., Khong, J. H., Chua, B. H., Chan, Y. P., Lim, M. E. & Lam, S. K. (2002). Isolation of Nipah virus from Malaysian Island flying-foxes. Microbes Infect 4, 145–151. [DOI] [PubMed] [Google Scholar]
- Didcock, L., Young, D. F., Goodbourn, S. & Randall, R. E. (1999). The V protein of simian virus 5 inhibits interferon signalling by targeting STAT1 for proteasome-mediated degradation. J Virol 73, 9928–9933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enserink, M. (2004). Emerging infectious diseases: Nipah virus (or a cousin) strikes again. Science 303, 1121. [DOI] [PubMed] [Google Scholar]
- Field, H., Young, P., Yob, J. M., Mills, J., Hall, L. & Mackenzie, J. (2001). The natural history of Hendra and Nipah viruses. Microbes Infect 3, 307–314. [DOI] [PubMed] [Google Scholar]
- Garcin, D., Marq, J.-B., Strahle, L., le Mercier, P. & Kolakofsky, D. (2002). All four Sendai virus C proteins bind Stat1, but only the larger forms also induce its mono-ubiquitination and degradation. Virology 295, 256–265. [DOI] [PubMed] [Google Scholar]
- Halpin, K., Young, P. L., Field, H. E. & Mackenzie, J. S. (2000). Isolation of Hendra virus from pteropid bats: a natural reservoir of Hendra virus. J Gen Virol 81, 1927–1932. [DOI] [PubMed] [Google Scholar]
- Harcourt, B. H., Lowe, L., Tamin, A. & 11 other authors (2005). Genetic characterization of Nipah virus, Bangladesh, 2004. Emerg Infect Dis 11, 1594–1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He, B., Paterson, R. G., Stock, N., Durbin, J. E., Durbin, R. K., Goodbourn, S., Randall, R. E. & Lamb, R. A. (2002). Recovery of paramyxovirus simian virus 5 with a V protein lacking the conserved cysteine-rich domain: the multifunctional V protein blocks both interferon-β induction and interferon signaling. Virology 303, 15–32. [DOI] [PubMed] [Google Scholar]
- Hooper, P., Zaki, S., Daniels, P. & Middleton, D. (2001). Comparative pathology of the diseases caused by Hendra and Nipah viruses. Microbes Infect 3, 315–322. [DOI] [PubMed] [Google Scholar]
- Horvath, C. M. (2004). Silencing STATs: lessons from paramyxovirus interferon evasion. Cytokine Growth Factor Rev 15, 117–127. [DOI] [PubMed] [Google Scholar]
- Hsu, V. P., Hossain, M. J., Parashar, U. D. & 7 other authors (2004). Nipah virus encephalitis reemergence, Bangladesh. Emerg Infect Dis 10, 2082–2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamb, R. A. & Kolakofsky, D. (2001). Paramyxoviridae: the viruses and their replication. In Fields Virology, 4th edn, pp. 1305–1340. Edited by D. M. Knipe & P. M. Howley. Philadelphia: Lippincott Williams & Wilkins.
- Middleton, D. J., Westbury, H. A., Morrissy, C. J., van der Heide, B. M., Russell, G. M., Braun, M. A. & Hyatt, A. D. (2002). Experimental Nipah virus infection in pigs and cats. J Comp Pathol 126, 124–136. [DOI] [PubMed] [Google Scholar]
- Murray, K., Selleck, P., Hooper, P. & 8 other authors (1995). A morbillivirus that caused fatal disease in horses and humans. Science 268, 94–97. [DOI] [PubMed] [Google Scholar]
- Nagai, Y. & Kato, A. (2004). Accessory genes of the paramyxoviridae. a large family of nonsegmented negative-strand RNA viruses, as a focus of active investigation by reverse genetics. Curr Top Microbiol Immunol 283, 197–248. [DOI] [PubMed] [Google Scholar]
- O'Sullivan, J. D., Allworth, A. M., Paterson, D. L., Snow, T. M., Boots, R., Gleeson, L. J., Gould, A. R., Hyatt, A. D. & Bradfield, J. (1997). Fatal encephalitis due to novel paramyxovirus transmitted from horses. Lancet 349, 93–95. [DOI] [PubMed] [Google Scholar]
- Park, M.-S., Shaw, M. L., Muñoz-Jordan, J., Cros, J. F., Nakaya, T., Bouvier, N., Palese, P., García-Sastre, A. & Basler, C. F. (2003). Newcastle disease virus (NDV)-based assay demonstrates interferon-antagonist activity for the NDV V protein and the Nipah virus V, W, and C proteins. J Virol 77, 1501–1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez, J. J. & Horvath, C. M. (2004). Host evasion by emerging paramyxoviruses: Hendra virus and Nipah virus V proteins inhibit interferon signaling. Viral Immunol 17, 210–219. [DOI] [PubMed] [Google Scholar]
- Rodriguez, J. J., Parisien, J.-P. & Horvath, C. M. (2002). Nipah virus V protein evades alpha and gamma interferons by preventing STAT1 and STAT2 activation and nuclear accumulation. J Virol 76, 11476–11483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez, J. J., Wang, L.-F. & Horvath, C. M. (2003). Hendra virus V protein inhibits interferon signaling by preventing STAT1 and STAT2 nuclear accumulation. J Virol 77, 11842–11845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez, J. J., Cruz, C. D. & Horvath, C. M. (2004). Identification of the nuclear export signal and STAT-binding domains of the Nipah virus V protein reveals mechanisms underlying interferon evasion. J Virol 78, 5358–5367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw, M. L., García-Sastre, A., Palese, P. & Basler, C. F. (2004). Nipah virus V and W proteins have a common STAT1-binding domain yet inhibit STAT1 activation from the cytoplasmic and nuclear compartments, respectively. J Virol 78, 5633–5641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stock, N., Goodbourn, S. & Randall, R. E. (2005). The anti-interferon mechanisms of paramyxoviruses. In Modulation of Host Gene Expression and Innate Immunity in Viruses, pp. 115–140. Edited by P. Palese. Dordecht: Springer.
- Wacharapluesadee, S., Lumlertdacha, B., Boongird, K. & 7 other authors (2005). Bat Nipah virus, Thailand. Emerg Infect Dis 11, 1949–1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, L.-F., Yu, M., Hansson, E., Pritchard, L. I., Shiell, B., Michalski, W. P. & Eaton, B. T. (2000). The exceptionally large genome of Hendra virus: support for creation of a new genus within the family Paramyxoviridae. J Virol 74, 9972–9979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong, K. T., Grosjean, I., Brisson, C. & 11 other authors (2003). A golden hamster model for human acute Nipah virus infection. Am J Pathol 163, 2127–2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yob, J. M., Field, H., Rashdi, A. M. & 8 other authors (2001). Nipah virus infection in bats (order Chiroptera) in peninsular Malaysia. Emerg Infect Dis 7, 439–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young, D. F., Chatziandreou, N., He, B., Goodbourn, S., Lamb, R. A. & Randall, R. E. (2001). Single amino acid substitution in the V protein of simian virus 5 differentiates its ability to block interferon signaling in human and murine cells. J Virol 75, 3363–3370. [DOI] [PMC free article] [PubMed] [Google Scholar]