Abstract
Background
Racial disparities in blood pressure (BP) control are well documented but poorly understood; prior studies have only included a limited range of potential explanatory factors. We examined a comprehensive set of putative factors related to blood pressure control, including patients’ clinical and sociodemographic characteristics, beliefs about BP and BP medications, medication adherence, and experiences of discrimination, to determine if the impact of race on BP control remains after accounting for such factors.
Methods & Results
We recruited 806 White and Black patients with hypertension from an urban safety-net hospital. From a questionnaire administered to patients after their clinic visits, electronic medical record and BP data, we assessed an array of patient factors. We then examined the association of patient factors with BP control by modeling it as a function of the covariates using random effects logistic regression.
Blacks indicated worse medication adherence, more discrimination, and more concerns about high BP and BP medications, compared to Whites. After accounting for all factors, race was no longer a significant predictor of BP control.
Conclusions
Results suggest that equalizing patients’ health beliefs, medication adherence, and experiences with care could ameliorate disparities in BP control. Additional attention must focus on the factors associated with race to identify, and ultimately intervene on, the causes of racial disparities in BP outcomes.
Keywords: blood pressure, hypertension, race, disparities
Introduction
Hypertension, which affects over 73 million Americans, is a major risk factor for cardiovascular, cerebrovascular and renal disease 1. It is more frequent among African Americans (AAs) 2, and accounts for a significant portion of racial differences in mortality, through excess cardiovascular morbidity 3. Many patients with hypertension have poorly controlled blood pressure (BP), and AAs are disproportionately represented among this group 4, even after controlling for comorbidities such as diabetes and renal disease 4–7.
The reason for this racial disparity is not well-understood. Many prior studies of BP control have only examined a narrow range of potential etiologic factors -- usually, clinical characteristics and sometimes including selected sociodemographic factors 8, 9. Recently, authors have suggested that patient self-management attitudes and behaviors 10, and other attitudes, beliefs and experiences which might affect medication non-adherence 11, might be potential causal pathways to disparities in chronic disease outcomes such as BP control.
Bosworth and colleagues 12 proposed an organizing framework for the psychosocial and cultural domains they theorized would impact BP control, incorporating Patient characteristics, including age, education, health literacy, and psychological factors such as beliefs and attitudes about health and illness, Social/cultural environmental factors, including culturally linked perceptions of hypertension and therapies for it, and the Medical Environment, including the provider-patient relationship and interactions. The model does not specify causal associations, and perhaps as a result, it has not been tested empirically, so the presence or strength of the hypothesized associations is not known. The model also did not include comorbid conditions. Thus, we sought to extend this work and the model itself by examining the contribution of the previously proposed and additional putative causal factors, in a more diverse sample in a different setting. We hypothesized that after adjusting for a more extensive set of potential confounders, race would no longer be significantly associated with BP control.
Methods
Sample
We identified all White and Black patients ages 21 and older with three separate outpatient diagnoses of hypertension in 2004 in the primary care practices of a northeastern academically affiliated urban safety net tertiary care hospital. We use the term “Black” to refer to patients of African or Caribbean descent. The study was approved by the Institutional Review Board and all subjects gave informed consent.
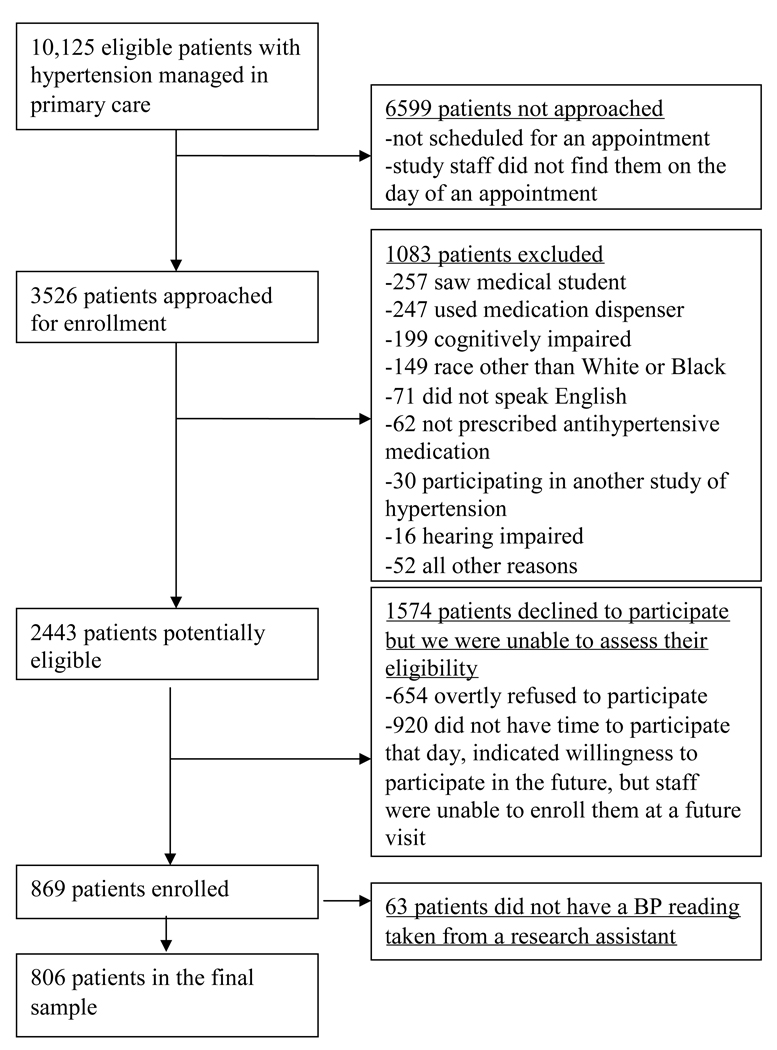
Study staff tracked clinic visits of these 10,125 patients over 19 months (10/2004 to 6/2006), and, as they presented for care, approached 3526 of them to request study participation . Those willing were asked a series of questions and administered a 6-item cognitive screen to determine eligibility 13. However, 654 patients (19% of 3526) overtly refused to participate and 920 patients (26% of 3526) responded that they were unable to participate that day but were potentially willing in the future, all before we were able to assess their eligibility. Subsequently, 1083 patients (55% of the remaining 1952) were excluded, for reasons including cognitive difficulties, hearing impairment, not speaking English, or not being prescribed antihypertensive medications; we enrolled 869 patients. We then applied this 55% exclusion rate to the 1574 non-respondents whose eligibility we had been unable to assess (654 refusers and 920 with no time), and estimated that 708 (45%) would have likely been eligible. Thus, we calculated our participation rate as participants / participants + likely eligible subjects (869 / 869 + 708 = 55%). We subsequently excluded 63 additional patients for whom study staff were unable to obtain BPs, for a final sample of 806 (Figure 1).
Figure 1.
Flow chart of patient recruitment.
We evaluated the representativeness of the enrolled cohort, compared to those eligible to be enrolled, using the limited data available on the non-enrolled patients. Enrolled patients were more likely to be White (43% vs. 32%, p<.0001) and were younger (mean age of 59 vs. 65 for non-enrolled patients, p<.0001), but there was no difference in gender distribution from the parent population of eligible patients (not shown).
Measures
Patient Characteristics
Sociodemographic Characteristics & Medical History
Patient sociodemographic characteristics including race (assessed using US Census categories), education, and income were obtained through self-report. To assess patients’ literacy, we utilized the REALM-Short Form 14. We used five separate dichotomous (yes/no) questions to assess insurance status, asking if patients currently have health insurance coverage through Medicare, Medicaid, Medigap, Free Care, or other insurance.
Patients’ clinical data was extracted from the electronic medical record (EMR), including age, gender, height, weight, and hypertension diagnosis. The EMR was searched to obtain diagnoses of comorbid conditions including renal insufficiency, coronary artery disease, peripheral vascular disease, nicotine dependence, hyperlipidemia, diabetes mellitus, congestive heart failure, cerebrovascular disease, and obesity, because these conditions may influence the management of hypertension 15. Obesity was considered a current diagnosis for any patient with an EMR diagnosis or a calculated body mass index of at least 30.
Health Beliefs and Illness Perception
We examined a broad spectrum of patient beliefs and perceptions about high BP and related medications. We used the “Beliefs about Medicines Questionnaire” (BMQ);ten items assess patients’ concerns about present and potential future adverse effects from their medications and eight items measure patients’ beliefs regarding the necessity of their medications; we edited the items to relate responses specifically to BP medicines.16, 17 (items scored on a five point scale: Strongly Agree to Strongly Disagree). Scores were summed within each scale to create an overall scale score (range: 8–40 for the ‘necessity’ scale (Cronbach’s alpha=0.81) and 10–50 for the ‘concerns’ scale (alpha=0.80)). Each score was divided by the number of items to obtain a mean summary score (range 1–5); higher numbers indicated either greater concerns about medications or greater beliefs in their necessity.
We utilized four additional items from our prior work 18 to evaluate the degree of seriousness with which patients perceive hypertension, asking “How serious do you think high BP is, in general?”, “How serious do you think your high BP is, given your current use of medication?”, “If you did not take your BP medications, how likely do you think it would be that your BP would get worse over the next year?” and “If you did not take your BP medications, how likely do you think it is that you would develop other health problems over the next year?” (all scored on a scale of 1–5 (extremely serious to not at all serious for the former two questions; very likely to very unlikely for the latter two)). We also included ten individual items from the “cause” dimension of the “Illness Perception Questionnaire”, to assess illness identity, cause, timeline, consequences, and cure control, to examine patients’ subjective beliefs about the etiology of their high BP (responses on a 5 point scale, range: Strongly Agree - Strongly Disagree) 19.
Perceived Discrimination in Health Care
We included three measures to assess patients’ perceptions of race-based discrimination in the health care setting. We used five questions that were a subset of the Commonwealth Fund 2001 Health Care Quality survey, focusing specifically on the patient’s perception of his/her provider and of encountering discrimination while receiving medical care, in general 20. We created an additional question about the patient’s perception of his/her provider’s understanding of the patient’s cultural background and how it affects his/her health; each item was examined individually. We also included seven dichotomous items from a measure of patients’ perceptions of discrimination in accessing health care 21, counting the number of experiences reported and creating a continuous variable (higher score indicates more experiences of discrimination 21; alpha=0.90).
Medication Adherence & Hypertension Management
To assess medication adherence, we used the Hill-Bone Compliance to High Blood Pressure Therapy Scale, comprised of items scored on a 4 point scale ( “None of the time” to “All of the time”) 22. We included the 9-item adherence sub-scale, which has been validated against BP control, summing the items to create a scale score (range: 9–36; higher scores indicate less adherence (alpha: 0.74)).
Outcome Assessment – BP Control
Research staff assessed patients’ BP using an automatic, portable machine (Omron HEM-907), which was validated according to the international validation protocol and deemed an appropriate instrument for accurate BP measurement 23. We excluded the 7% of patients without a BP reading from study staff. We dichotomized the BP readings to indicate whether each patients’ BP was controlled or not, e.g. when their systolic BP exceeded 140 mm/Hg or their diastolic BP exceeded 90 mm/Hg, according to the Joint National Committee on Hypertension 7 standards at the time of the study, which also specified that for patients with diabetes or renal insufficiency, BP should not exceed 130/80 mmHg 15.
Statistical Analyses
We first examined bivariate associations between race and each of the sociodemographic, clinical, attitudinal, experiential, and medication adherence variables, using chi-square or t-tests, as appropriate. Next, we performed bivariate analyses to determine whether this same set of variables was associated with BP control (yes/no). Finally, BP control was modeled as a function of the covariates using random effects logistic regression. The random effects, which were assumed to be mean-zero Gaussian additive errors on the logit scale, accounted for two levels of clustering: patients within providers and providers within clinics.
We fit six sets of models of increasing numbers of covariates, including only patients with complete data. In the first, we examined the effects of race alone on BP control. Next, we examined the effects of race on BP control, adjusting for age and other sociodemographic characteristics. The third model added medication adherence, the fourth added health beliefs, the fifth added experiences of discrimination, and the sixth added comorbid conditions. Within each model, we chose the subset of additional variables through an ordinary logistic regression stepwise selection procedure, forcing in provider indicators as fixed effects, keeping significant variables from the prior model, and including race in all models. This procedure prevents collinearity and over-parameterization. We used a p-value of 0.05 for variables to enter or be removed from the model. C-statistics and Hosmer-Lemeshow analyses were performed on the models resulting from the stepwise procedure. Each model was then rerun with the random effects terms. All analyses were conducted using SAS 9.1.3 (SAS Institute, Cary, NC) with the exception of the random effects logistic regression, which was conducted using the statistics package R (version 2.8.0 24).
Results
Sociodemographic characteristics of the sample
Most of the sample were Black (57%) or female (65%), with an overall mean age of 59 years. White patients were older (61 years vs. 58), and more likely to have at least a high school education (90% vs. 71%). Black patients were more likely to have insurance coverage through Medicaid or Free Care (42% vs. 22%, 41% vs. 25%, respectively), whereas White patients were more likely to have “other” (private) insurance (59% vs. 35%). There were race differences in combined household family income, with a greater percentage of Blacks earning low incomes of <$20,000 (58% vs. 36% Whites), and being less likely to have a literacy score of 9th grade or higher (48% vs. 84%), (all p’s <0.001; Table 1).
Table 1.
Sociodemographic, clinical, attitudinal, belief and experience variables by race and BP control
| Sociodemographic Characteristics & Medical History |
Overall (%) |
White (%) |
Black (%) |
p-value for race differences |
Controlled BP (%) |
Uncontrolled BP (%) |
p-value for difference by BP control |
|
|---|---|---|---|---|---|---|---|---|
| % White | 43 | n/a | 48** | 36** | 0.0009 | |||
| Mean age | 59 | 61 | 58 | 0.0007 | 59 | 60 | 0.0853 | |
| % male | 35 | 46 | 27 | <0.0001 | 34 | 38 | 0.2919 | |
| Education (% ≥ 12 years) | 79 | 90 | 71 | <0.0001 | 81 | 76 | 0.0521 | |
| % Income < $20k | 48 | 36 | 58 | <0.0001 | 43 | 56 | 0.0003 | |
| Insurance status | ||||||||
| Medicare | 39 | 39 | 40 | 0.6889 | 37 | 43 | 0.0984 | |
| Medigap | 3 | 3 | 2 | .4991 | 2 | 4 | 0.2143 | |
| Medicaid | 33 | 22 | 42 | <0.0001 | 29 | 40 | 0.0012 | |
| Other | 45 | 59 | 35 | <0.0001 | 51 | 38 | 0.0003 | |
| Free Care | 34 | 25 | 41 | <0.0001 | 32 | 37 | 0.1072 | |
| Literacy categories | ||||||||
| ≤3rd grade | 4 | 2 | 5 | 3 | 4 | |||
| 4th–6th grade | 9 | 2 | 14 | 8 | 11 | |||
| 7th–8th grade | 24 | 12 | 33 | 22 | 27 | |||
| ≥9th grade | 63 | 84 | 48 | <0.0001 | 67 | 58 | 0.0884 | |
| % With controlled BP | 58 | 65 | 53 | 0.0009 | n/a | n/a | n/a | |
| Mean systolic BP (mm/Hg) | 131 | 130 | 132 | 0.0277 | n/a | n/a | n/a | |
| Mean diastolic BP (mm/Hg) | 79 | 76 | 81 | <0.0001 | n/a | n/a | n/a | |
| Overall |
White (%) |
Black (%) |
p-value |
Controlled BP (%) |
Uncontrolled BP (%) |
p-value | ||
| Nicotine dependence | 7 | 5 | 9 | 0.0839 | 7 | 8 | 0.7303 | |
| Hyperlipidemia | 52 | 60 | 47 | 0.0002 | 52 | 53 | 0.9302 | |
| Diabetes | 33 | 24 | 40 | <0.0001 | 25 | 45 | <0.0001 | |
| Peripheral vascular disease | 5 | 7 | 4 | 0.0383 | 5 | 5 | 0.9918 | |
| Renal insufficiency | 6 | 4 | 7 | 0.0470 | 3 | 10 | <0.0001 | |
| Benign prostatic hypertrophy | 4 | 6 | 2 | 0.0003 | 4 | 2 | 0.1107 | |
| Coronary artery disease | 13 | 19 | 8 | <0.0001 | 14 | 11 | 0.2151 | |
| Obesity | 59 | 52 | 65 | 0.0004 | 58 | 62 | 0.2373 | |
| Congestive Heart Failure | 3 | 1 | 5 | 0.0091 | 2 | 5 | 0.0635 | |
| Cerebrovascular Disease | 5 | 7 | 4 | 0.0382 | 4 | 6 | 0.2162 | |
|
Health Beliefs and Illness Perceptions |
||||||||
| BMQ: Mean necessity of medications (mean score) |
3.7 | 3.7 | 3.7 | 0.1542 | 3.7 | 3.7 | 0.9739 | |
| BMQ: Mean concerns about medications (mean score) |
2.3 | 2.1 | 2.5 | <0.0001 | 2.3 | 2.4 | 0.0407 | |
| How serious do you think high BP is, in general* |
1.5 | 1.5 | 1.5 | 0.4607 | 1.5 | 1.6 | 0.1147 | |
|
How serious do you think your high BP is, given your current use of medication* |
3.0 | 3.3 | 2.8 | <0.0001 | 3.1 | 2.9 | 0.0010 | |
| If you did not take BP meds, likelihood that BP would get worse w/in a year† |
1.5 | 1.4 | 1.5 | 0.1284 | 1.5 | 1.4 | 0.1348 | |
| If you did not take BP meds, likelihood that you would develop other health problems w/in a year† |
1.7 | 1.7 | 1.7 | 0.2307 | 1.7 | 1.7 | 0.4281 | |
| Illness Perceptions Questionnaire Items ‡ | ||||||||
| A germ or virus caused my high BP | 3.9 | 4.2 | 3.7 | <0.0001 | 3.9 | 3.8 | 0.1208 | |
| Diet played a major role in causing my high BP |
2.3 | 2.4 | 2.1 | 0.0017 | 2.2 | 2.3 | 0.6715 | |
| Pollution caused my high BP | 3.7 | 3.8 | 3.5 | 0.0002 | 3.7 | 3.7 | 0.7546 | |
| My high BP is hereditary – it runs in my family |
2.0 | 2.1 | 1.9 | 0.0134 | 2.1 | 2.0 | 0.1877 | |
| It was just by chance that I became ill with high BP |
3.5 | 3.7 | 3.3 | <0.0001 | 3.5 | 3.4 | 0.1876 | |
| Stress was a major factor in causing my high BP |
2.4 | 2.4 | 2.4 | 0.4035 | 2.4 | 2.4 | 0.4737 | |
| My high BP is largely due to my own behavior |
2.7 | 2.7 | 2.8 | 0.3299 | 2.8 | 2.7 | 0.1508 | |
| Other people played a large role in causing my high BP |
3.4 | 3.6 | 3.3 | 0.0010 | 3.4 | 3.3 | 0.2580 | |
| My high BP was caused by poor medical care in the past |
3.9 | 4.1 | 3.7 | <0.0001 | 3.9 | 3.8 | 0.2799 | |
| My state of mind played a major part in causing my high BP |
3.2 | 3.3 | 3.2 | .7686 | 3.3 | 3.2 | 0.4884 | |
| Perceived Discrimination | ||||||||
| Commonwealth Fund Items | ||||||||
| Was there ever a time you would have gotten better medical care if you belonged to a different race or ethnic group? (% yes) |
11 | 1 | 19 | <0.0001 | 12 | 11 | 0.6174 | |
| In the last 2 years, have you ever felt that the doctor or medical staff judged you unfairly or treated you with disrespect because of how well you speak English? (% yes) |
2 | 0 | 4 | 0.0008 | 3 | 2 | 0.3549 | |
| My provider treats me with a great deal of respect and dignity‡ |
1.3 | 1.3 | 1.3 | 0.2509 | 1.3 | 1.3 | 0.5617 | |
| I feel that my provider understands my background and values‡ |
1.5 | 1.4 | 1.5 | 0.0425 | 1.5 | 1.5 | 0.1818 | |
| I often feel as if my provider looks down on me and the way I live my life† |
4.4 | 4.5 | 4.3 | <0.0001 | 4.4 | 4.4 | 0.7828 | |
| New item | ||||||||
| I feel my provider understands my cultural background and how it affects my health‡ |
1.8 | 1.8 | 1.8 | 0.5104 | 1.8 | 1.8 | 0.1044 | |
| Perceived Discrimination Scale (Bird & Bogart) | ||||||||
| Discrimination scale | 0.7 | 0.2 | 1.1 | <0.0001 | 0.7 | 0.7 | 0.9815 | |
| Medication Adherence | 10.5 | 9.9 | 11.0 | <0.0001 | 10.4 | 10.7 | 0.0347 | |
Note: bolded text indicates significant differences; due to rounding, items sum to more than 100%
Higher score=greater belief that high BP is not serious
Higher score=greater belief that statement is unlikely to be true
Higher score=more disagreement with statement
Mean necessity: scale 1–5. Higher score=meds are a necessity
Mean concerns: scale 1–5. Higher score=greater concern about meds
Perceived discrimination scale: Higher score=more experiences of discrimination
Hill Bone Adherence: Higher score indicates less adherence
% White
BP and medical history by race
A greater percentage of White patients had controlled BP (65% vs. 53%), with lower systolic and diastolic BP than Blacks (White SBP 130 mm/Hg vs. 132 mm/Hg; White DBP 76 mm/Hg vs. 81 mm/Hg). White patients were more likely to have hyperlipidemia (60% vs. 47%), peripheral vascular disease (7% vs. 4%), benign prostatic hypertrophy (6% vs. 2%), coronary artery disease (19% vs. 8%), and cerebrovascular disease (7% vs. 4%). Black patients were more likely to have diabetes (40% vs. 24%), renal insufficiency (7% vs. 4%), congestive heart failure (5% vs. 1%) and to be obese (65% vs. 52%, all p’s<0.05).
Health Beliefs and Illness Perceptions
Blacks had significantly more concerns about their BP medications than Whites (2.5 vs. 2.1, p<0.0001). White patients were significantly more likely to respond that their BP was less serious given their current use of medications (3.3 vs. 2.8, p<0.0001).
When asked about the causality of high BP, Blacks agreed more with the notion that it is caused by a germ or virus, or that diet, pollution or heredity played a major role in causing BP (Table 1). Blacks were more likely to indicate that it was just by chance that they became ill with hypertension, that other people played a large role in causing their BP, or that high BP was caused by poor medical care in the past.
Perceived discrimination
When asked if there was ever a time they would have gotten better medical care if they belonged to a different race or ethnic group or if they ever felt that a doctor or medical staff judged them unfairly or treated them with disrespect because of how well they spoke English, Blacks were more likely to respond “yes” than Whites (19% vs. 1% and 4% vs. 0%, respectively). While all patients generally agreed that their provider understood their background and values, Black patients agreed less strongly (1.5 vs. 1.4), and though all patients disagreed that their provider looks down on them and the way they live their life, White patients disagreed more strongly (4.5 vs. 4.3). Blacks reported more experiences of discrimination when receiving health care than did Whites (1.1 vs. 0.2, all p’s<0.05).
Medication Adherence
White patients reported better medication adherence than did Black patients (9.9 vs. 11.0, p<0.0001).
Covariates by BP control
A greater proportion of patients with controlled BP were white compared to patients with uncontrolled BP (48% vs. 36%). Patients with uncontrolled BP were more likely to have a household income of <$20,000 (56% vs. 43%), were more likely to have Medicaid (40% vs. 29%) and less likely to have “other” insurance (38% vs. 51%). Patients with uncontrolled BP were more likely to have diabetes (45% vs. 25%) and renal insufficiency (10% vs. 3%), and concerns about their BP medications (2.4 vs. 2.3). Patients with controlled BP were more likely to disagree that their own BP was serious, given their current use of medication (3.1 vs. 2.9) and reported better medication adherence (10.4 vs. 10.7, all p’s<0.05).
Multivariate results
The first model, only adjusted for race, accounting for physician and clinic, indicated that White patients had higher odds of having controlled BP than Blacks (Model 1 b=0.42, p=0.0068; Table 2; c statistic (c) = 0.661, Hosmer and Lemeshow Goodness-of-Fit Test (HL) p=0.4226). The effect of race on BP control persisted in the second model, after adjustment for income (other sociodemographic variables were excluded through the ordinary logistic regression stepwise procedure). The third model added a measure of adherence, which was not significantly related to BP control, so these two latter models had the same results, with race continuing to be a significant predictor of BP control (Models 2 & 3 b=0.37, p=0.0238, Model 2 c=0.691, HL p=0.7127, Model 3 c=0.670, HL p=0.9260). In the fourth model, an item assessing patients’ beliefs that high BP is largely due to one’s own behavior was added, as well as 2 items assessing the degree of seriousness with which patients perceive hypertension (all other attitudinal and experiential factors were excluded through the stepwise procedure). In this model, race was no longer significantly associated with odds of BP control (Model 4, b=0.33, p=0.0531, c=0.713, HL p=0.3932).
Table 2.
Multivariate results modeling controlled blood pressure
| Model 1 | Models 2 & 3 | Model 4 | Model 5 | Model 6 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Co- efficient |
Lower CI, Upper CI† |
Co- efficient |
Lower CI, Upper CI† |
Co- efficient |
Lower CI, Upper CI† |
Co- efficient |
Lower CI, Upper CI† |
Co- efficient |
Lower CI, Upper CI† |
|
| Race (white) | 0.42* | 0.13, 0.71 | 0.37* | 0.06, 0.68 | 0.33 | −0.003, 0.66 | 0.48* | 0.13, 0.83 | 0.32 | −0.03, 0.67 |
| Income | −0.44 | −0.75, −0.13 | −0.37 | −0.68, −0.06 | −0.37 | −0.70, −0.04 | −0.32 | −0.65, 0.01 | ||
| My high BP is largely due to my own behavior‡ |
0.15 | 0.01, 0.29 | 0.17 | 0.03, 0.31 | 0.16 | 0.02, 0.30 | ||||
| How serious do you think high BP is, in general? |
−0.23 | −0.43, −0.03 | −0.24 | −0.44, −0.04 | −0.23 | −0.43, −0.03 | ||||
| How serious do you think your high BP is, given your current use of medication? |
0.18 | 0.04, 0.32 | 0.18 | 0.04, 0.32 | 0.17 | 0.01, 0.33 | ||||
| Would have gotten better medical care if you belonged to different race or ethnic group |
0.56 | 0.05, 1.07 | 0.51 | −0.02, 1.04 | ||||||
| Diabetes | −0.62 | −0.97, −0.27 | ||||||||
| Renal insufficiency |
−1.17 | −1.93, −0.41 | ||||||||
| Benign prostatic hypertrophy |
0.93 | −0.13, 1.99 | ||||||||
p≤ 0.05 (value only reported for race, the only variable forced into all of the stepwise selection procedures)
95% confidence intervals
Higher score=more disagreement with statement
In the fifth model, one item assessing experiences with perceived discrimination in health care was added, specifically, perceptions about whether they would have ever gotten better medical care if they belonged to a different race or ethnic group (other items assessing discrimination were excluded through the stepwise procedure). Race was significant in this model (Model 5, b=0.48, p=0.0074, c=0.708, HL p=0.8660).
In the final model, diabetes, renal insufficiency, and benign prostatic hypertrophy were added (other comorbid conditions were excluded during the stepwise procedure in SAS). Here, race was no longer a significant predictor of BP control (Model 6, b=0.32, p=.0876, c=.740, HL p=0.4274).
Discussion
Understanding and ameliorating racial disparities in BP control is a major public health and clinical concern. We hypothesized that after adjusting for an extensive set of potential confounders, race would no longer be significantly associated with BP control, and the results generally supported this notion. While the effects of race persisted after accounting for sociodemographic factors, the inclusion of BP-related attitudes and beliefs rendered race insignificant. However, the introduction of the discrimination variables made race significant again, in a counter-intuitive fashion, although in the final model, with the inclusion of comorbid conditions, race was no longer significant. The finding that patients who agreed with the statement that there was ‘ever a time when they would have gotten better medical care if they had belonged to a different race/ethnic group’ had better BP control is puzzling. We carefully explored this dynamic, ruling out the possibility that race-discrimination interactions were driving it, and finding that even if we removed this variable, another discrimination variable became significant in the same counter-intuitive direction (not shown). The variable was limited by its reference point (e.g. was there ever a time…), so it is possible that patients who felt they were getting bad care in the past had changed clinicians, and are now getting good care, leading to better current BP care and control. It is also possible that another, unmeasured, confounder caused these results.
The study findings are different than Bosworth’s, which indicated that after controlling for a similar range of factors (not including discrimination or comorbid conditions), race remained a significant predictor of BP control, among VA patients in one Southern city 11. They speculated that the results they obtained in that setting, where access to care is assured, might be different than those found elsewhere, and our results in a northeastern urban safety net hospital setting support this notion. Several other studies also controlled for subsets of the factors we included here, but race remained significant 6, 25, 26. Thus, while our findings support Bosworth’s proposed framework as a descriptive model, and the notion that numerous psychosocial, behavioral and experiential factors mediate the relationship between race and BP control11, they indicate that comorbid conditions, whose prevalence varies by race/ethnicity, are also important to account for in models of disparities in BP control.
Several findings have clinical implications. Blacks reported more experiences of discrimination and such experiences may erode overall trust in physicians, their diagnoses, and the therapies they prescribe. Experiences of discrimination in the community setting are generally associated with higher BP 27 29, 30, with less use of chronic disease care 28, and may negatively impact patients’ acceptance of their diagnosis, and beliefs in the necessity of or concerns about the associated therapy, which are foundational to patient adherence to prescribed medications 29. Unequal treatment, documented by us and others 30, 31, may also contribute to disparities in BP outcomes.
Blacks indicated worse medication adherence and more concerns about BP. Each of these is potentially ameliorable through educational or counseling interventions, and our results suggest that addressing these will help address disparities in BP control.
This study was limited by its focus on patients in a single setting and its inclusion of only Black (albeit both African-American and Caribbean born) and White patients. Although we required that participants have three separate outpatient diagnoses of hypertension, our inability to contact or enroll many eligible patients may have biased our sample toward more frequent users. The observational nature of these data limits our ability to form causal inferences, because we were not able to randomize by attitudinal characteristics or ascertain that certain attitudes or experiences preceded BP outcomes in time. Further, our measure of adherence, although internally consistent and previously validated against BP control, was obtained by self-report. However, the large sample, which included women and detailed assessments of the richest array of putative factors examined to date, offsets the limitations.
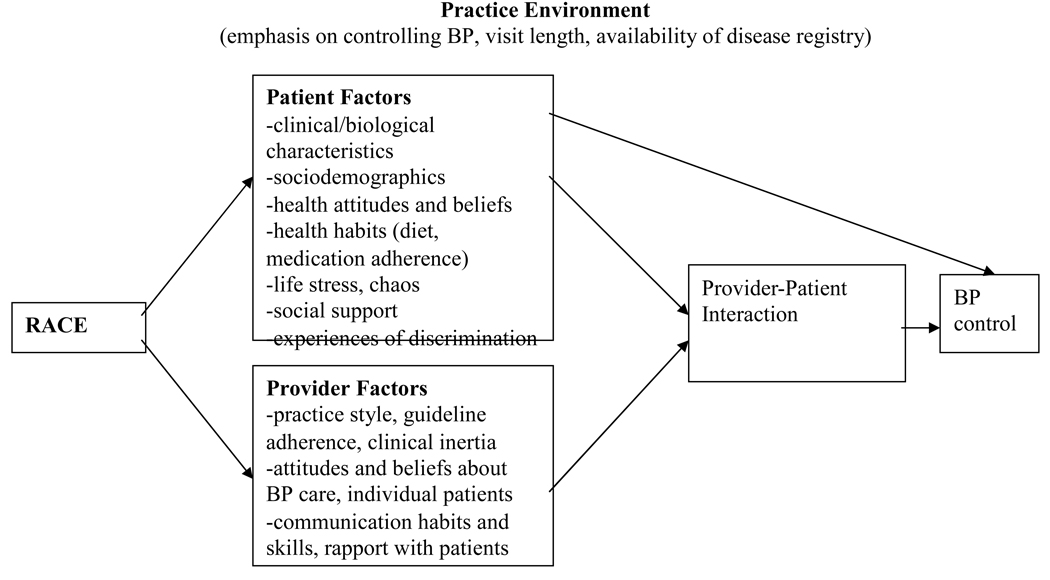
Among the potential causes of disparities in BP control, the etiologic factors could arise from the patient (health beliefs and experiences, medication adherence or self-care behaviors, clinical or biologic factors), the provider (practice style, communication skills, attitudes), the doctor-patient interaction, or the environment. While Bosworth’s model provided an excellent summary of the psychosocial and cultural factors that might be associated with BP control, we propose that a model for racial disparities in BP control should include a wider array of factors and include hypothesized associations (Figure 2). The present results help to demonstrate the effects of a variety of factors on race differences in BP, but we lacked data on other self-care behaviors important to hypertension management (e.g. diet, exercise) to fully address this question. Nor are we able to rule out biologic differences, such as race-linked nitric oxide deficiencies associated with cardiovascular disease 32, or differences in the process of care. Our future work will also examine the effects of racial differences in providers’ therapeutic intensification, which varies by race 33, on BP outcomes. Similar to our prior suggestions for future directions in research on racial differences in invasive cardiac procedure use 31, here we propose additional careful attention by clinicians, researchers and ultimately, policy makers, to a comprehensive array of factors associated with race to identify, and intervene on, the causes of racial disparities in BP outcomes.
Figure 2.
Expanded model of factors leading to disparities in blood pressure control
Acknowledgements
We thank Peter Davidson, MD, and the clinic and research staff for their assistance.
Funding sources: NIH/National Heart, Lung and Blood Institute grant R01 HL072814 (N. Kressin, PI); Dr. Kressin is also supported by a Research Career Scientist award (RCS 02-066-1) from the Health Services Research and Development Service, Department of Veterans Affairs.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: There is no significant financial interest of any author that would affect our research.
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
References
- 1.American Heart Association. [Accessed November 20, 2009];Heart Disease & Stroke Statistics: 2009 Update At-A-Glance. Available at: http://www.americanheart.org/downloadable/heart/1240250946756LS-1982%20Heart%20and%20Stroke%20Update.042009.pdf.
- 2.Wang X, Poole J, Treiber F, Harshfield GA, hanevold C, Snieder H. Ethnic and gender differences in ambulatory blood pressure trajectories: Results from a 15-Year longitudinal study in youth and young adults. Circulation. 2006;114:2780–2787. doi: 10.1161/CIRCULATIONAHA.106.643940. [DOI] [PubMed] [Google Scholar]
- 3.Wong M, Shapiro M, Boscardin W, Ettner S. Contributions of major diseases to disparities in mortality. New England Journal of Medicine. 2002;347:1585–1592. doi: 10.1056/NEJMsa012979. [DOI] [PubMed] [Google Scholar]
- 4.Cushman W, Ford C, Cutler J, Margolis K, Davis B, Grimm R, Black H, Hamilton B, Holland J, Nwachuku C, Papademetriou V, Probstfield J, Wright J, Alderman M, Weiss R, Piller L, Bettencourt J, Walsh W. Success and Predictors of Blood Pressure Control in Diverse North American Settings: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) J Clinical Hypertension. 2002;4:393–404. doi: 10.1111/j.1524-6175.2002.02045.x. [DOI] [PubMed] [Google Scholar]
- 5.Hyman DJ, Pavlik VN. Self-reported hypertension treatment practices among primary care physicians. Archives of Internal Medicine. 2000;160:2281–2286. doi: 10.1001/archinte.160.15.2281. [DOI] [PubMed] [Google Scholar]
- 6.Hajjar I, Kotchen T. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. Journal of the American Medical Association. 2003;290:199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 7.Hicks LS, Fairchild DG, Horng MS, Orav EJ, Bates DW, Ayanian JZ. Determinants of JNC VI guideline adherence, intensity of drug therapy, and blood pressure control by race and ethnicity. Hypertension. 2004;44:429–434. doi: 10.1161/01.HYP.0000141439.34834.84. [DOI] [PubMed] [Google Scholar]
- 8.Fletcher SW, Deliakis J, Schoch WA, Shapiro SH. Predicting blood pressure control in hypertensive patients: an approach to quality-of-care assessment. Medical Care. 1979;27:285–292. doi: 10.1097/00005650-197903000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Wagner EH, James SA, Beresford SA, Strogatz DS, Grimson RC, Kleinbaum DG, Williams CA, Cutchin LM, Ibrahim MA. The Edgecombe County High Blood Pressure Control Program: I. Correlates of uncontrolled hypertension at baseline. Am J Public Health. 1984;74:237–242. doi: 10.2105/ajph.74.3.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heisler M, Faul JD, Hayward RA, Langa KM, Blaum C, Weir D. Mechanisms for racial and ethnic disparities in glycemic control in middle-aged and older Americans in the health and retirement study. Arch Intern Med. 2007;167:1853–1860. doi: 10.1001/archinte.167.17.1853. [DOI] [PubMed] [Google Scholar]
- 11.Bosworth HB, Dudley T, Olsen MK, Voils CI, Powers B, Goldstein MK, Oddone EZ. Racial differences in blood pressure control: potential explanatory factors. Am J Med. 2006;119(70) doi: 10.1016/j.amjmed.2005.08.019. e79-15. [DOI] [PubMed] [Google Scholar]
- 12.Bosworth H, Oddone E. A model of psychosocial and cultural antecedents of blood pressure control. Journal of the National Medical Association. 2002;94:236–248. [PMC free article] [PubMed] [Google Scholar]
- 13.Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Medical Care. 2002;40:771–781. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Arozullah AM, Yarnold PR, Bennett CL, Soltysik RC, Wolf MS, Ferreira RM, Lee S-Y, Costello S, Shakir A, Denwood C, Bryant FB, David T. Development and validation of a short-form, rapid estimate of adult literacy in medicine. Medical Care. 2007;45:1026–1033. doi: 10.1097/MLR.0b013e3180616c1b. [DOI] [PubMed] [Google Scholar]
- 15.Chobanian A, Bakris G, Black H, Cushman W, Green L, Izzo J, Jr., Jones D, Materson B, Oparil S, Wright J, Jr., Rocella E the National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. Journal of the American Medical Association. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed]
- 16.Horne R, Weinman J, Hankins M. The Beliefs about Medicines Questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychology and Health. 1999;14:1–24. [Google Scholar]
- 17.Horne R, Buick D, Fischer M, Leake H, Cooper V, Weinman J. Doubts about the necessity and concerns about adverse effects: identifying the types of beliefs that are associated with non-adherence to HAART. International Journal of STD & AIDS. 2004;15:38–44. doi: 10.1258/095646204322637245. [DOI] [PubMed] [Google Scholar]
- 18.Kressin N, Wang F, Long J, Bokhour B, Orner M, Rothendler J, Clark C, Reddy S, Kozak W, Kroupa L, Berlowitz D. Hypertensive Patients’ Health Beliefs, Process of Care, and Medication Adherence: Is Race Important? Journal of General Internal Medicine. 2007;22:768–774. doi: 10.1007/s11606-007-0165-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weinman J, Petrie KJ, Moss-Mossis R, Horne R. The Illness Perception Questionnaire: a new method for assessing the cognitive representation of illness. Psychology and Health. 1996;11:431–445. [Google Scholar]
- 20.Johnson RL, Saha S, Arbelaez JJ, Beach MC, Cooper LA. Racial and Ethnic Differences in Patient Perceptions of Bias and Cultural Competence in Health Care. Journal of General Internal Medicine. 2004;19:101–110. doi: 10.1111/j.1525-1497.2004.30262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bird ST, Bogart LM. Perceived race-based and socioeconomic status (SES)-based discrimination in interactions with health care providers. Ethnicity and Disease. 2001;11:554–563. [PubMed] [Google Scholar]
- 22.Kim MT, Hill MN, Bone LR, Levine DM. Development and testing of the Hill-Bone Compliance to High Blood Pressure Therapy scale. Progress in Cardiovascular Nursing. 2000;15:90–96. doi: 10.1111/j.1751-7117.2000.tb00211.x. [DOI] [PubMed] [Google Scholar]
- 23.El Assaad MA, Topouchian JA, Darne BM, Asmar RG. Validation of the Omron HEM-907 device for blood pressure measurement. Blood Pressure Monitoring. 2002;7:237–241. doi: 10.1097/00126097-200208000-00006. [DOI] [PubMed] [Google Scholar]
- 24.R: A language environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2008. [computer program]. Version. [Google Scholar]
- 25.Kramer H, Han C, Post W, Goff D, Diez-Roux A, Cooper R, Jinagouda S, Shea S. Racial/ethnic differences in hypertension and hypertension treatment and control in the multi-ethnic study of atherosclerosis (MESA) Am J Hypertens. 2004;17:963–970. doi: 10.1016/j.amjhyper.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 26.Svetkey LP, George LK, Tyroler HA, Timmons PZ, Burchett BM, Blazer DG. Effects of gender and ethnic group on blood pressure control in the elderly. Am J Hypertens. 1996;9:529–535. doi: 10.1016/0895-7061(96)00026-x. [DOI] [PubMed] [Google Scholar]
- 27.Krieger N, Sydney S. Racial discrimination and blood pressure: the CARDIA study of young black and white adults. American Journal of Public Health. 1996;86:1370–1378. doi: 10.2105/ajph.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blanchard J, Lurie N. R-E-S-P-E-C-T: patient reports of disrespect in the health care setting and its impact on care. J Fam Pract. 2004;53:721–730. [PubMed] [Google Scholar]
- 29.Rosenstock I. Why people use health services. Milbank Memorial Fund Q. 1966;44 [PubMed] [Google Scholar]
- 30.Kressin N. Racial Differences in the Use of Invasive Cardiovascular Procedures: Review of the Literature and Prescription for Future Research. Ann Intern Medicine. 2001;135:352–366. doi: 10.7326/0003-4819-135-5-200109040-00012. [DOI] [PubMed] [Google Scholar]
- 31.Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002. Institute of Medicine. [Google Scholar]
- 32.Kalinowski L, Dobrucki IT, Malinski T. Race-specific differences in endothelial function: predisposition of African Americans to vascular diseases. Circulation. 2004;109:2511–2517. doi: 10.1161/01.CIR.0000129087.81352.7A. [DOI] [PubMed] [Google Scholar]
- 33.Manze M, Rose AJ, Orner MB, Berlowitz D, Kressin NR. Society of General Internal Medicine. Miami, FL: 2009. Understanding pathways to disparities in hypertension control: race and treatment intensification. [DOI] [PMC free article] [PubMed] [Google Scholar]