Abstract
Simian-human immunodeficiency virus 89.6PD (SHIV89.6PD) was pathogenic after intrarectal inoculation of rhesus macaques. Infection was achieved with a minimum of 2,500 tissue culture infectious doses of cell-free virus stock, and there was no evidence for transient viremia in animals receiving subinfectious doses by the intrarectal route. Some animals experienced rapid progression of disease characterized by loss of greater than 90% of circulating CD4+ T cells, sustained decreases in CD20+ B cells, failure to elicit virus-binding antibodies in plasma, and high levels of antigenemia. Slower-progressing animals had moderate but varying losses of CD4+ T cells; showed increases in circulating CD20+ B cells; mounted vigorous responses to antibodies in plasma, including neutralizing antibodies; and had low or undetectable levels of antigenemia. Rapid progression led to death within 30 weeks after intrarectal inoculation. Plasma antigenemia at 2 weeks after inoculation (P ≤ 0.002), B- and T-cell losses (P ≤ 0.013), and failure to seroconvert (P ≤ 0.005) were correlated statistically with rapid progression. Correlations were evident by 2 to 4 weeks after intrarectal SHIV inoculation, indicating that early events in the host-pathogen interaction determined the clinical outcome.
Simian-human immunodeficiency viruses (SHIV) are recombinant constructs that substitute human immunodeficiency virus type 1 (HIV-1) envelope, tat, and rev genes for the homologous genes in an SIV molecular clone (7, 18). SHIV provides a model for studying immune responses and possible vaccine protection that uses authentic HIV-1 proteins, and yet the constructs retain the ability to infect rhesus macaques. Early SHIV constructs established only limited infections and failed to cause overt disease in macaques (8), but rapid animal-to-animal passages of these viruses evolved pathogenic virus isolates (6, 16). We characterized intrarectal transmission and subsequent disease course with one of these virulent isolates (SHIV89.6PD) to understand how HIV-1 envelope glycoproteins affect transmission efficiency and to study the virulence mechanisms in vivo.
SHIV89.6PD was isolated during a study of rapid serial passage of the nonpathogenic SHIV89.6. SHIV89.6 includes the dualtropic envelope sequences of HIV-189.6 (1) and could be transmitted by intravaginal inoculation of rhesus macaques without causing overt disease (9). Serial passage of this virus in macaques created the virus stocks SHIV89.6P (16) and SHIV89.6PD (10), which are virulent in macaques. Our stock SHIV89.6PD (plasma derived) was transmitted by high-dose intravenous, intrarectal, and intravaginal inoculation of macaques, and substantial and rapid declines in counts of peripheral blood CD4+ T cells occurred frequently (10).
SHIV89.6PD was pathogenic in macaques, even though the intrarectal transmission efficiency was modest. Several markers of infection were highly correlated with outcome; measurements within the first 4 weeks after inoculation predicted accurately the length of survival. There was no evidence for transient viremia after exposure to subinfectious doses, and disease progression was not accelerated with inoculations above the minimal infectious dose. SHIV89.6PD, SHIV89.6P, and other virulent SHIV isolates (5) may be useful for vaccine and pathogenesis studies, because they include HIV-1 envelope glycoprotein genes and lead to rapid disease progression with defined early markers for predicting survival.
Intrarectal inoculation of 2,500 tissue culture infectious doses (TCID) is required for productive SHIV89.6PD infection.
Male (n = 5) and female (n = 5) juvenile rhesus macaques (Maccaca mulatta) bred in captivity were housed at the Wisconsin Regional Primate Research Center (WRPRC) and used in these studies. They were confirmed negative for antibodies to SIV and type D simian retroviruses prior to this study. Macaques were immobilized with ketamine hydrochloride (10 mg/kg of body weight) before all virus inoculation and blood collections. The WRPRC is accredited by the American Academy for Laboratory Animal Care. The Institutional Animal Care and Use Committee approved all animal research protocols.
Ten rhesus macaques were inoculated intrarectally (14) with doses of SHIV89.6PD ranging from 25,000 to 2.5 TCID. The pathogenic SHIV used in these studies was SHIV89.6PD. This virus was derived by passaging the nonpathogenic SHIV89.6 (17) multiple times in macaques and was isolated in CEMx174 cells with plasma from the fourth animal (K542) in this series of passages (10).
Six animals inoculated with 250 TCID or less were negative for all measures of infection for 30 weeks. These animals were then inoculated a second time with 2,500 TCID of virus by the intrarectal route, whereupon all six were persistently infected. Previous intrarectal exposure to low-dose SHIV89.6PD did not cause transient viremia and did not affect subsequent intrarectal virus challenge. We combined data for all 10 infected animals to evaluate markers of disease progression.
Viral burden following intrarectal SHIV89.6PD inoculation.
Infectious virus was detected in peripheral blood mononuclear cells (PBMC) from all 10 animals by 4 weeks after intrarectal inoculation with the minimal infectious dose (2,500 TCID) or a larger dose. Plasma samples from 8 of 10 animals were positive for SIV p27 antigen by 2 weeks after infection (Table 1). Plasma antigenemia was assessed at 1, 2, 3, 4, 6, and 8 weeks postinoculation (p.i.). We noted only a single positive sampling interval (2 weeks p.i.). The two animals with negative tests may have had a brief spike of p27 in plasma that fell between sample collections. Levels of p27 in plasma varied from <50 to 22,599 pg/ml, with an average of 5,545 pg/ml. Two macaques (r94080 and r92014) had p27 levels just below detection limits, while three macaques (r92069, r94054, and r92058) had levels of p27 greater than 11,000 pg/ml. p27 was not detected later than 2 weeks p.i., and testing was discontinued by 8 weeks p.i.
TABLE 1.
Viral burdens and levels of neutralizing antibody after intrarectal SHIV89.6PD inoculationa
| Animal | Sexe | Virus dose (TCID) | Plasma antigenemiaf | Neutralizing- antibody titerg |
|---|---|---|---|---|
| r92069 | F | 25,000 | 11,631 | <20 |
| r92085 | M | 25,000 | 3,191 | 260 |
| r92058 | M | 2,500 | 22,599 | <20 |
| r94056 | F | 2,500 | 589 | 12,464 |
| r92014b | M | 2,500 | <50 | 900 |
| r94054b | F | 2,500 | 12,665 | <20 |
| r92081c | F | 2,500 | 645 | 35,372 |
| r94080c | M | 2,500 | <50 | 3,165 |
| r94078d | F | 2,500 | 1,560 | <20 |
| r94085d | M | 2,500 | 2,565 | 4,339 |
At 4 weeks after inoculation, all animals were positive for the virus.
Inoculated previously with 250 TCID, intrarectally.
Inoculated previously with 25 TCID, intrarectally.
Inoculated previously with 2.5 TCID, intrarectally.
F, female; M, male.
Tested at 2 weeks after inoculation. Shown are levels of p27 in plasma (in picograms per milliliter).
Tested at peak antiviral antibody response. Shown is the reciprocal of the plasma dilution required to protect 50% of cells from virus-induced killing by SHIV89.6PD.
Rapid loss of greater than 90% of circulating CD4+ T cells in half of infected macaques.
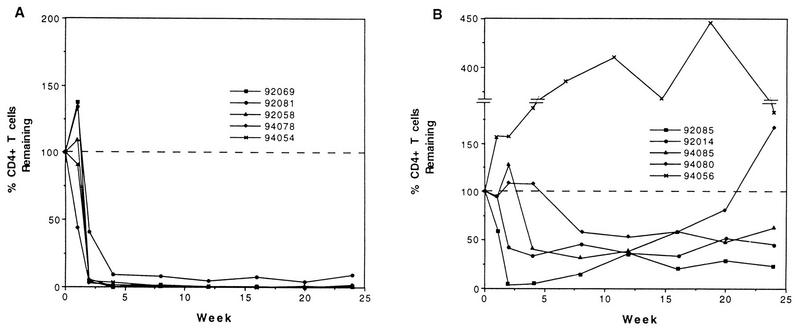
PBMC were purified, and lymphocyte subsets were detected as described previously (15). We collected three samples before infection to measure baseline values. All samples were within the normal range for juvenile rhesus macaques, which is 1,300 ± 420 CD4+ T cells/μl of blood (19a). Nine macaques had decreases in the absolute number of circulating CD4+ T cells following intrarectal SHIV inoculation. CD4+-T-cell loss had two general patterns: (i) rapid and dramatic loss (>90% decrease) and (ii) variable and moderate loss (35 to 80% decrease). Both outcomes were equally represented in our cohort. Five macaques had rapid and dramatic losses of circulating CD4+ cells. Less than 10% of their CD4+ T cells remained by 2 weeks p.i., with the average number of CD4+ cells falling to 65 cells/μl of blood (Fig. 1A). Consistently, these five macaques had less than 10% of their CD4+ T cells remaining over the course of infection, with the absolute number of CD4+ T cells decreasing to undetectable levels. Surprisingly, several animals survived more than 20 weeks with CD4+-T-cell counts below 100 cells/μl of blood.
FIG. 1.
Changes in the number of circulating CD4+ T cells. The percentages of CD4+ T cells remaining for weeks 1 through 24 p.i. were calculated for each animal with the following formulas: percentage of CD4+ T cells remaining (at week x) = 100 + percent change; percent change = 100 × [(number of CD4+ T cells at week x − number of CD4+ T cells at week 0)/(number of CD4+ T cells at week 0)]. Results for five animals with rapid and sustained losses of CD4+ T cells (A) and for five animals with moderate but varying losses of CD4+ T cell (B) are shown.
Five other macaques had variable CD4+-T-cell changes (Fig. 1B). One animal (r94056) had increased CD4+-T-cell numbers at all times following SHIV infection. Macaque r94056 had low baseline CD4+-T-cell counts (average of 609 CD4+ T cells/μl of blood for two preinfection samples), but these values were well inside the normal range for juvenile rhesus macaques. By 84 days after SHIV inoculation, the absolute CD4 count for r94056 was increased to 1,882 cells/μl of blood even though the percentage of CD4+ T cells in PBMC (37.1%) was unchanged from the preinfection value of 35.7%. The increase in the absolute count of CD4+ T cells was due mainly to a generalized lymphocytosis, with total, absolute lymphocyte counts rising from the preinfection value of 1,707 lymphocytes/μl of blood to 5,069 lymphocytes/μl of blood by 84 days. The other unique pattern of CD4+-T-cell changes was in animal r92085. An initial drop to <5% CD4+ T cells by 4 weeks p.i. was followed by rising CD4+-T-cell counts that reached 25% of initial CD4+-T-cell counts and remained stable throughout 60 weeks of observation. Three macaques (r92014, r94080, and r94085) had average CD4+ T-cell losses of 57% by 12 weeks p.i. but maintained CD4+-T-cell counts above 450 cells/μl of blood. One of these three macaques experienced CD4+ T-cell increases after the initial CD4+-T-cell loss and ended up with CD4+-T-cell numbers above the starting levels by 24 weeks p.i.
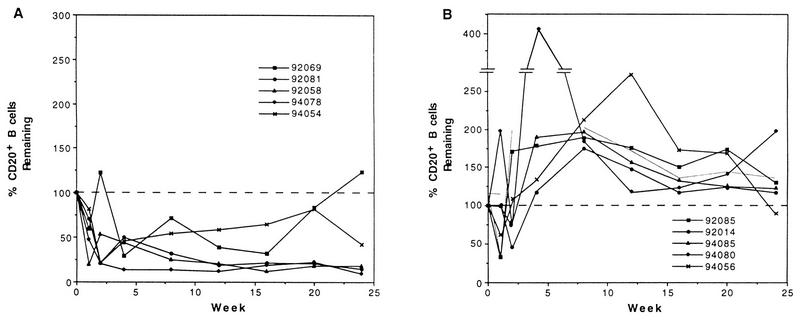
Changes in CD20+ B cells.
Changes in circulating B cells (CD20+ cells) were also related to disease progression (Fig. 2). Figure 2A depicts CD20+-B-cell changes in five macaques that had rapid and dramatic CD4+-T-cell losses. All five of these animals had sustained losses of greater than 50% in circulating B cells. The average percentage of B-cell loss was 63% by 4 weeks p.i., with some animals losing up to 87% of their B cells.
FIG. 2.
Changes in the number of circulating CD20+ B cells. The percentages of CD20+ B cells remaining for weeks 1 through 24 p.i. were calculated for each animal by using week 0 values as 100%. (A) Percentages of B cells remaining in the five animals with rapid and sustained losses of CD4+ T cells; (B) percentages of B cells remaining in the five animals with moderate and variable losses of CD4+ T cells.
Five macaques that did not show dramatic CD4+-T-cell losses had sustained B-cell increases after an initial drop by 1 week p.i. (Fig. 2B). The average B-cell increase was 105% of preinfection levels by 4 weeks after infection. Before SHIV infection, the average number of circulating B cells ± the standard deviation was 1,125 ± 888 cells/μl of blood. Eight weeks after SHIV inoculation, the average B-cell count had decreased to 390 ± 79 cells/μl of blood in the five animals with large CD4+-T-cell losses and had increased to 1,601 ± 1,028 cells/μl of blood in the five animals with moderate CD4+-T-cell losses.
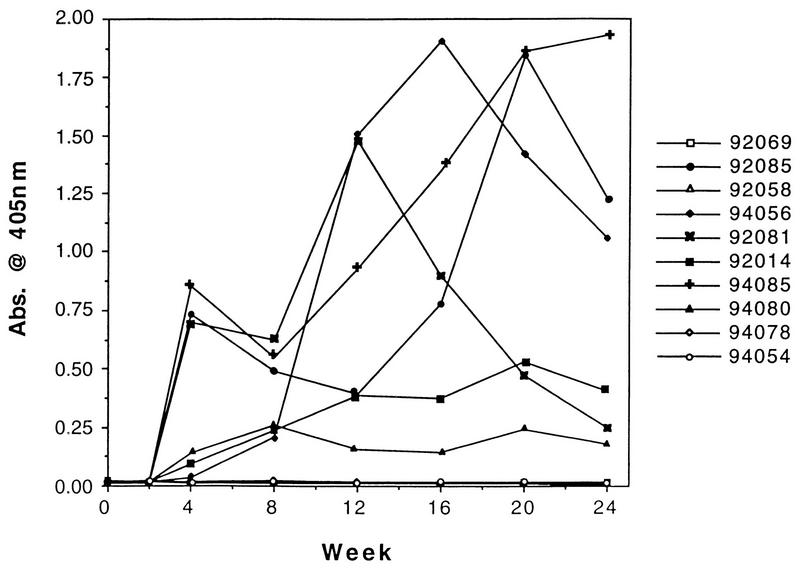
Virus-binding antibodies.
Six macaques developed virus-binding antibodies by 4 weeks after infection (Fig. 3). Plasma samples were screened on plates coated with HIV-2 antigens (Sanofi/Pasteur, Chaska, Minn.). Endpoint titers are reciprocals of the last dilution with an absorbance value greater than 0.02 after background subtraction. Three macaques had steady increases in levels of virus-binding immunoglobulin G (IgG) antibody, with peak responses occurring 16 to 20 weeks after infection. Macaque r92085 had a peak response at 16 weeks p.i., with an endpoint titer of 1:25,600. r94056 and r94085 had peak responses at 20 weeks p.i., with endpoint titers at that time of 1:6,400 and 1:25,600, respectively. A single macaque (r92081) had an initial increase of antibodies in plasma that peaked 12 weeks p.i., with an endpoint titer of 1:25,600. Antibodies in r92081 steadily declined to low, but still detectable, levels. Macaques r92014 and r94080 had moderate or low virus-binding IgG antibody responses, but these levels were stable. The endpoint titers for these animals were 1:6,400 and 1:400, respectively, at 20 weeks p.i. The remaining four animals did not produce detectable levels of virus-binding antibodies.
FIG. 3.
Antibody responses in plasma. Macaque sera were tested with an HIV-2 enzyme-linked immunosorbent assay kit for antiviral antibodies. Absorbance values (405 nm) of plasma samples from weeks 0 through 24 p.i. are depicted for each animal. Open symbols represent results with seronegative macaques, and closed symbols represent results with seropositive macaques.
Plasma samples were also tested for HIV-1 env-specific IgG responses in plasma by using enzyme-linked immunosorbent assay plates coated with purified glycosylated gp120 from HIV-1MN (provided by Ribi Immunochem, Hamilton, Mont.). Plasma samples that were positive for virus-binding antibodies (r92014, r92081, r92085, r94056, r94080, and r94085) also reacted with purified HIV-1MN gp120, while plasma samples from all four SIV-seronegative macaques (r92058, r92069, r94054, and r94078) did not react with HIV-1MN gp120. We did not determine strain-specific endpoint titers for envelope responses, because purified HIV-189.6 envelope glycoprotein was not available.
Antibodies that neutralize SHIV89.6P in plasma.
Plasma from peak antiviral antibody responses (those from week 20 were used for all animals except r92081, for which the week 12 sample was used) were tested for the ability to neutralize SHIV89.6P (16) in an MT-2 cell-killing assay as described previously (13, 17). The neutralizing titer reported for each animal in Table 1 is the reciprocal of the plasma dilution required to protect 50% of cells from virus-induced killing. All four macaques that were negative for antibodies against HIV-1 env and SIV structural proteins in plasma were also negative for neutralizing antibodies. Macaques r94056 and r92081 had very high levels of neutralizing antibodies, with titers of 12,464 and 35,372, respectively. The four remaining seropositive macaques had moderate titers of neutralizing antibody ranging from 260 to 4,339.
Clinical outcome.
Four macaques succumbed to disease at 25, 28, 32, and 36 weeks after SHIV89.6PD inoculation. All animals were euthanized on the advice of the veterinarian. Euthanasia was recommended when animals refused food or water, were unreactive to stimuli, or showed some severe distress. Lymphoid tissue pathology and major diagnoses at the time of necropsy provided evidence of advanced disease and supported the euthanasia decisions. Six animals remain alive (two animals at 88 weeks p.i. and four animals at 58 weeks p.i.).
r94054 (female) was euthanized 25 weeks after inoculation with 2,500 TCID. The absolute number of circulating CD4+ T cells decreased to below 100 CD4+ cells/μl of blood within 2 weeks of virus inoculation. This animal had a sustained loss (approximately 70%) of circulating B cells and did not seroconvert before succumbing to disease. At necropsy this animal had lymphoid tissues severely depleted of lymphocytes (in follicles and in paracortex and periarteriolar lymphoid sheaths), edema (severe), cholangiohepatitis, and interstitial pneumonia. Also noted were lymphadenitis and dermatitis associated with cytomegalovirus.
r92058 (male) was euthanized 28 weeks after inoculation with 2,500 TCID. CD4+-T-cell counts dropped to below 10 cells/μl of blood by four weeks p.i. This animal had a sustained decrease (approximately 80% loss) in circulating B cells and remained seronegative. Major diagnoses at necropsy included mild colitis, hepatitis, and lymphocyte depletion in lymphoid tissues.
r92069 (female) was inoculated with 25,000 TCID and was euthanized 32 weeks p.i. CD4+-T-cell numbers decreased to 2 cells/μl of blood four weeks p.i. and remained below 10 cells/μl of blood until the time of necropsy. This animal had a decrease in B-cell numbers (<50% remaining) until 24 weeks p.i., when B-cell numbers increased to above preinfection values. r92069 did not seroconvert. The major diagnoses noted at necropsy were gastritis, interstitial pneumonia, and severe involution of lymphoid tissues.
r94078 (female) was inoculated with 2,500 TCID and was euthanized 36 weeks p.i. Circulating CD4+ T cells decreased by greater than 50% by 1 week p.i. r94078 had less than 5% CD4+ T cells remaining by 2 weeks p.i., with absolute numbers of CD4+ T cells below 10 cells/μl of blood from 12 weeks p.i. until the time of necropsy. Follicular involution with normal or expanded paracortex and periarteriolar sheaths was noted for peripheral lymph nodes, thymus, and spleen. Severe depletion of follicles and paracortex in ileocecal and colonic lymph nodes was noted along with pyogranulomatous lymphadenitis. Interstitial pneumonia with multinucleated giant cells was present.
Statistical analysis.
We performed two types of statistical tests to evaluate data on disease progression. The first test assessed differences in survival time as a function of laboratory markers of disease. Individual groups were identified on the basis of CD4 cell count, CD8 cell count, CD20 cell count, level of virus binding antibody, level of neutralizing antibody, and plasma antigenemia. Each marker was used to define two groups within the cohort. Animals with substantial drops in CD4 (Fig. 1A) were grouped separately from animals with moderate drops in CD4 (Fig. 1B). Similar groupings were developed for the other markers of infection. In each case, we divided the cohort into two groups and tested whether there was a statistically significant survival difference. These tests (Table 2) were performed by Kaplan-Meier analysis. Rapid and sustained CD4 loss, CD20 cell loss, a low level of virus-binding antibody, a low level of neutralizing antibody, and a high degree of plasma antigenemia (at 2 weeks) were all predictive of rapid disease progression with shortened survival. Changes in CD8 cells were not correlated with survival. This approach allowed us to identify outcomes that predicted rapid disease progression even at a time when most animals in the study remained alive.
TABLE 2.
Statistical analysis for markers of disease progressiona
| Marker | P value |
|---|---|
| CD4 | 0.013 |
| CD8 | 0.986 |
| CD20 | 0.013 |
| Virus-binding antibody | 0.005 |
| Neutralizing antibody | 0.005 |
| Plasma antigenemia | 0.002 |
Data reflect qualitative correlations with survival times (by Kaplan-Meier analysis).
A second statistical analysis was performed to evaluate correlations among individual markers of disease progression. Quantitative values were compared directly with Pearson’s log rank correlation coefficients, and the values for the comparisons are listed in Table 3). Changes in CD4 cells were positively correlated with either changes in CD8 cells or changes in CD20 cells or levels of virus-binding antibody. Changes in CD8 or CD20 cells were positively correlated with levels of virus-binding antibodies. No other correlations reached statistical significance (P ≤ 0.05). It is interesting that changes in CD4 cell counts were more strongly correlated (0.789, P ≤ 0.01) with levels of virus-binding antibody than were changes in CD20 cell counts (0.659, P ≤ 0.05). Even though this difference is small, the data imply that early changes in CD4 cell populations may be important in the host’s subsequent inability to produce measurable levels of virus-binding antibody. The proportion of CD20 cells remaining by 8 to 24 weeks after inoculation was strongly correlated (P ≤ 0.01) with the level of CD4 cell loss during the acute infection interval from 2 to 4 weeks after inoculation.
TABLE 3.
Quantitative correlations among independent markers of disease progression
| Marker | Correlationa with marker:
|
|||||
|---|---|---|---|---|---|---|
| CD4 | CD8 | CD20 | Virus-binding antibody | Neutralizing antibody | Plasma antigenemia | |
| CD4 | 1.00 | 0.723* | 0.680* | 0.789** | 0.189 | −0.375 |
| CD8 | 1.00 | 0.424 | 0.641* | 0.115 | −0.091 | |
| CD20 | 1.00 | 0.659* | −0.124 | −0.540 | ||
| Virus-binding antibody | 1.00 | 0.468 | −0.488 | |||
| Neutralizing antibody | 1.00 | −0.356 | ||||
Values are Pearson’s correlation coefficients. *, P ≤ 0.05; **, P ≤ 0.01.
DISCUSSION
We characterized intrarectal transmission efficiency and pathogenesis of SHIV89.6PD in rhesus macaques. SHIV89.6PD was transmitted across the rectal mucosa with virus doses of 2,500 and 25,000 TCID. Macaques inoculated with 250 TCID or less showed no signs of either productive or attenuated infection, establishing that the minimum infectious dose lies between 250 and 2,500 TCID. Two patterns of clinical progression were noted, and we observed approximately equal numbers of rapidly or slowly progressing macaques. Rapid progressors succumbed to disease at an average of 30 weeks p.i., and slow progressors survived much longer (two macaques were alive at 88 weeks p.i. and four macaques were alive at 58 weeks p.i.). Markers of disease in slowly progressing macaques were less homogeneous than in rapidly progressing animals.
Productive SHIV89.6PD infection was evident within 2 weeks after virus doses of 2,500 TCID or higher. The disease progression of animals inoculated with the minimum infectious dose was equivalent to that seen in animals infected with a 10-fold-higher dose, implying that increased doses above the minimum do not accelerate disease progression. Indicators of productive infection included (i) SIV p27 antigen in plasma samples 2 weeks p.i., (ii) PBMC positive for virus isolation 4 weeks p.i., (iii) CD4+-T-cell losses within 2 weeks p.i., and (iv) production of virus-binding antibodies. Rapid progressors had very large decreases in the number of circulating CD4+ T cells, had sustained decreases of up to 80% in circulating CD20+ B cells, did not seroconvert, had high levels of antigenemia, and had shorter survival times after infection. Slow progressors had moderate CD4+-T-cell losses, had increased numbers of circulating B cells, seroconverted to antibodies against SIV structural proteins, had neutralizing antibodies, had no or low levels of antigenemia, and did not succumb to disease. Multiple parameters that predicted rapid progression included a high level of p27 antigenemia in plasma, substantial B- and T-cell losses, and failure to generate an antibody response. These predictive markers were clearly evident by 2 to 4 weeks after virus inoculation, suggesting that virus-host interactions early after infection dictated the eventual outcome. A previous study (23) showed a similar relationship for viral RNA burden in plasma and survival after SIV infection of macaques.
Although we generalized the outcome of infection by describing two different patterns, there was considerable variation, especially among the group of slow progressors. Changes in CD4+ T cells for these macaques ranged from a loss of 73% to a gain of 200%; levels of virus-binding or neutralizing antibodies in plasma and p27 antigenemia in plasma also varied greatly. All slowly progressing macaques had sustained increases in the number of circulating B cells. A unique outcome was observed for macaque r92085. r92085 initially lost more than 90% of circulating CD4+ T cells, yet the animal survived and eventually showed a modest increase in circulating CD4+ T cells. Unlike other macaques with large CD4+-T-cell losses, r92085 did not lose circulating CD20+ B cells and did seroconvert to viral antigens. Perhaps the level of CD4+-T-cell loss in this animal was insufficient to deplete T-cell help that is required to maintain B-cell populations and activities.
Previous studies in our laboratory established strong correlations between the level of antiviral antibody responses and life span after SIV infection of macaques (3). Rapid disease progression has been noted previously in SIV-infected macaques having low levels of antibody in plasma (2) and in HIV-infected individuals without antibody responses to virus (11). This link between antibodies and survival was further substantiated in the present study. The loss of greater than 90% of circulating CD4+ T cells and greater than 50% of CD20+ B cells and the absence of an antibody response all correlated with rapid disease progression (P ≤ 0.013, P ≤ 0.013, and P ≤ 0.005, respectively). Although antibody responses were good indicators of survival in both SIV and SHIV infection, we cannot prove that antibody function was required for survival. The level of antiviral antibodies may reflect indirectly the extent of CD4+-T-cell depletion during acute infection. Increasingly virulent infections may destroy larger portions of the CD4+-T-cell repertoire during the interval of acute infection and thus limit subsequent T-cell-dependent antibody responses. The number of circulating CD4+ T cells correlated more significantly with antiviral antibody responses (P ≤ 0.01) than did the number of B cells (P ≤ 0.05), suggesting that the amounts of CD4+ T cells remaining after acute infection are limiting for virus-specific antibody production. Decreased numbers of B cells may be due to declines in CD4+-T-cell help needed to maintain this population. It is also possible that B cells are sequestered preferentially in lymph nodes or destroyed by an indirect (bystander) mechanism, as was described for HIV-1 infection (4). We have analyzed lymph node biopsies during acute SHIV89.6PD infection of macaques. These tissue samples showed fluctuations of CD4+-T-cell and CD20+-B-cell populations that were similar to the fluctuations in the same populations in peripheral blood (not shown) and argue against preferential sequestration of these cells. Our current hypothesis is that B cells are lost by indirect killing and that this mechanism is proportional to both the magnitude of early virus replication and the consequent level of CD4+-T-cell depletion.
Previously, an attenuated disease progression was noted in macaques inoculated mucosally with low doses of SIV (12, 14). The attenuated disease was designated transient viremia and was characterized by low viral loads, survival greater than 2 years after infection, and resistance to mucosal superinfection (14, 19, 20). Although these low-dose macaques were generally virus isolation negative and did not seroconvert, they did harbor virus, as was evidenced by sporadic detection of viral DNA and the ability to transmit infection via blood transfusions (14, 21). The mechanisms for inducing transient viremia, for containing the disease in these low-dose animals, and for protecting them from mucosal superinfection remain unclear, but they may have an impact on the use of live, attenuated viruses as vaccines. We examined animals inoculated with less than 2,500 TCID for 30 weeks after virus inoculation to look for signs of transient viremia or attenuated infection. No indications were seen of an infectious, but nonpathogenic, viral dose. Animals exposed originally to low doses of SHIV89.6PD were susceptible to intrarectal infection with 2,500 TCID and showed patterns of disease progression similar to those of other animals. Thus, doses of SHIV89.6PD below 250 TCID do not induce attenuated infections. Original studies reporting transient viremia involved mucosal infection of macaques with SIVmac, a heterogeneous virus population that contains defective viruses (12, 14). Low virulence or defective viruses present in biological isolates may be required for transient viremia, and this would account for its absence after inoculation with SHIV89.6PD, a virus stock that is fairly homogeneous and highly pathogenic.
The SHIV89.6PD stock did not transmit efficiently via intrarectal inoculation when it was compared to SIVmac. Other chimeric SHIV strains used in mucosal transmission studies to date, such as SHIV89.6, SHIVHXBc2, and SHIVKU-1, have efficiencies of transmission (approximately 2,500 TCID) similar to that of SHIV89.6PD (5, 9, 22). SHIV89.6 and SHIVHXBc2 are relatively nonvirulent, while SHIVKU-1 and SHIV89.6PD are highly virulent. This group of viruses demonstrates the clear distinction between transmission efficiency (modest) and virulence (high). This panel of chimeric SHIV makes it possible to examine independently the determinants of virus transmission and pathogenesis and to define quantitative markers for disease progression that enable this virus to be used for vaccine challenge and therapy studies.
Acknowledgments
This work was supported by WRPRC grant RR00167 and PHS grants AI36643 and AI38491 (C.D.P.).
We gratefully thank Kathy Schell and Kristen Elmer for assistance with flow cytometry.
Footnotes
Publication 37-030 from the Wisconsin Regional Primate Research Center.
REFERENCES
- 1.Collman R, Balliet J W, Gregory S A, Friedman H, Kolson D L, Nathanson N, Srinivasan A. An infectious molecular clone of an unusual macrophage-tropic and highly cytopathic strain of human immunodeficiency virus type 1. J Virol. 1992;66:7517–7521. doi: 10.1128/jvi.66.12.7517-7521.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daniel M D, Letvin N L, Sehgal P K, Hunsmann G, Schmidt D K, King N W, Desrosiers R C. Long-term persistent infection of macaque monkeys with the simian immunodeficiency virus. J Gen Virol. 1987;68:3183–3189. doi: 10.1099/0022-1317-68-12-3183. [DOI] [PubMed] [Google Scholar]
- 3.Dykhuizen, M., J. Mitchen, H. Lardy, D. C. Montefiori, J. Thomsen, and C. D. Pauza. Determinants of disease in the SIV-infected rhesus macaque: characterizing animals with low antibody responses and rapid progression. Submitted for publication. [DOI] [PubMed]
- 4.Finkel T H, Tudor-Williams G, Banda N K, Cotton M F, Curiel T, Monks C, Baba T W, Ruprecht R M, Kupfer A. Apoptosis occurs predominantly in bystander cells and not in productively infected cells of HIV- and SIV-infected lymph nodes. Nat Med. 1995;1:129–134. doi: 10.1038/nm0295-129. [DOI] [PubMed] [Google Scholar]
- 5.Joag S V, Adany I, Li Z, Foresman L, Pinson D M, Wang C, Stephens E B, Raghavan R, Narayan O. Animal model of mucosally transmitted human immunodeficiency virus type 1 disease: intravaginal and oral deposition of simian human immunodeficiency virus in macaques results in systemic infection, elimination of CD4+ T cells, and AIDS. J Virol. 1997;71:4016–4023. doi: 10.1128/jvi.71.5.4016-4023.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Joag, S. V., Z. Li, L. Foresman, E. B. Stephens, L.-J. Zhao, I. Adany, D. M. Pinson, H. M. McClure, and O. Narayan. 1996. Chimeric simian/human immunodeficiency virus that causes progressive loss of CD4+ T cells and AIDS in pig-tailed macaques. 70:3189–3197. [DOI] [PMC free article] [PubMed]
- 7.Li J, Lord C, Haseltine W, Letvin N, Sodroski J. Infection of cynomolgus monkeys with a chimeric HIV-1/SIV that expresses the HIV-1 envelope glycoproteins. J Acquired Immune Defic Syndr. 1992;5:639–646. [PubMed] [Google Scholar]
- 8.Li J T, Halloran M, Lord C I, Watson A, Ranchalis J, Fung M, Letvin N L, Sodroski J G. Persistent infection of macaques with simian-human immunodeficiency viruses. J Virol. 1995;69:7061–7071. doi: 10.1128/jvi.69.11.7061-7067.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lu Y, Brosio P, Lafaile M, Li J, Collman R G, Sodroski J, Miller C J. Vaginal transmission of chimeric simian/human immunodeficiency viruses in rhesus macaques. J Virol. 1996;70:3045–3050. doi: 10.1128/jvi.70.5.3045-3050.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lu, Y., C. D. Pauza, X. Lü, and C. J. Miller. Intravenous, rectal or vaginal inoculation of rhesus macaques with an in vivo-passaged SHIV results in systemic infection and AIDS. Submitted for publication.
- 11.Michael N L, Brown A E, Voigt R F, Frankel S S, Mascola J R, Brothers K S, Louder M, Birx D L, Cassol S A. Rapid disease progression without seroconversion following primary human immunodeficiency virus type 1 infection—evidence for highly susceptible human hosts. J Infect Dis. 1997;175:1352–1359. doi: 10.1086/516467. [DOI] [PubMed] [Google Scholar]
- 12.Miller C J, Marthas M, Torten J, Alexander N J, Moore J P, Doncel G F, Hendrickx A G. Intravaginal inoculation of rhesus macaques with cell-free simian immunodeficiency virus results in persistent or transient viremia. J Virol. 1994;68:6391–6400. doi: 10.1128/jvi.68.10.6391-6400.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Montefiori D C, Robinson W E, Schuffman S S, Mitchell W M. Evaluation of antiviral drugs and neutralizing antibodies to human immunodeficiency virus by a rapid and sensitive microtiter infection assay. J Clin Microbiol. 1988;26:231–235. doi: 10.1128/jcm.26.2.231-235.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pauza C D, Emau P, Salvato M S, Trivedi P, MacKenzie D, Malkovsky M, Uno H, Schultz K T. Pathogenesis of SIVmac251 after atraumatic inoculation of the rectal mucosa in rhesus monkeys. J Med Primatol. 1993;22:154–161. [PubMed] [Google Scholar]
- 15.Pauza C D, Hinds II P W, Yin C, McKechnie T S, Hinds S B, Salvato M S. The lymphocytosis promoting agent pertussis toxin affects virus burden and lymphocyte distribution in the SIV-infected rhesus macaque. AIDS Res Hum Retroviruses. 1997;13:87–95. doi: 10.1089/aid.1997.13.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reimann K A, Li J T, Veazy R, Halloran M, Park I-W, Karlsson G B, Sodroski J, Letvin N L. A chimeric simian/human immunodeficiency virus expressing a primary patient human immunodeficiency virus type 1 isolate env causes an AIDS-like disease after in vivo passage in rhesus monkeys. J Virol. 1996;70:6922–6928. doi: 10.1128/jvi.70.10.6922-6928.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reimann K A, Li J T, Voss G, Lekutis C, Tenner-Racz K, Racz P, Lin W, Montefiori D C, Lee-Parritz D E, Lu Y, Collman R G, Sodroski J, Letvin N L. An env gene derived from a primary human immunodeficiency virus type 1 isolate confers high in vivo replicative capacity to a chimeric simian/human immunodeficiency virus in rhesus monkeys. J Virol. 1996;70:3198–3206. doi: 10.1128/jvi.70.5.3198-3206.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sakuragi S, Shibata R, Mukai R, Komatsu T, Fukasawa M, Sakai H, Sakuragi J, Kawamura M, Ibuki K, Hayami M. Infection of macaque monkey with a chimeric human and simian immunodeficiency virus. J Gen Virol. 1992;73:2983–2987. doi: 10.1099/0022-1317-73-11-2983. [DOI] [PubMed] [Google Scholar]
- 19.Salvato M S, Emau P, Malkovsky M, Schultz K T, Johnson E, Pauza C D. Cellular immune responses in rhesus macaques infected rectally with low dose simian immunodeficiency virus. J Med Primatol. 1994;23:125–130. doi: 10.1111/j.1600-0684.1994.tb00112.x. [DOI] [PubMed] [Google Scholar]
- 19a.Schenkel, A. R., and C. D. Pauza. Unpublished data.
- 20.Sheng N, Pettit S C, Tritch R J, Ozturk D H, Rayner M M, Swanstrom R, Erickson-Viitanen S. Determinants of the human immunodeficiency virus type 1 p15NC-RNA interaction that affect enhanced cleavage by the viral protease. J Virol. 1997;71:5723–5732. doi: 10.1128/jvi.71.8.5723-5732.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Trivedi P, Horejsh D, Hinds S B, Hinds II P W, Wu M S, Salvato M S, Pauza C D. Intrarectal transmission of simian immunodeficiency virus in rhesus macaques: selective amplification and host responses to transient or persistent viremia. J Virol. 1996;70:6876–6883. doi: 10.1128/jvi.70.10.6876-6883.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Trivedi P, Meyer K K, Streblow D N, Preuninger B L, Schultz K T, Pauza C D. Selective amplification of simian immunodeficiency virus genotypes after intrarectal inoculation of rhesus monkeys. J Virol. 1994;62:7649–7653. doi: 10.1128/jvi.68.11.7649-7653.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Watson A, Ranchalis J, Travis B, McClure J, Sutton W, Johnson P R, Hu S-L, Haigwood N L. Plasma viremia in macaques infected with simian immunodeficiency virus: plasma viral load early in infection predicts survival. J Virol. 1997;71:284–290. doi: 10.1128/jvi.71.1.284-290.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]