Abstract
Poliovirus live virus vectors are a candidate recombinant vaccine system. Previous studies using this system showed that a live poliovirus vector expressing a foreign antigen between the structural and nonstructural proteins generates both antibody and cytotoxic T-lymphocyte responses in mice. Here we describe a novel in vitro method of cloning recombinant polioviruses involving a hybrid-PCR approach. We report the construction of recombinant vectors of two different serotypes of poliovirus-expressing simian immunodeficiency virus (SIV) antigens and the intranasal and intravenous inoculations of four adult cynomolgus macaques with these poliovirus vectors expressing the SIV proteins p17gag and gp41env. All macaques generated a mucosal anti-SIV immunoglobulin A (IgA) response in rectal secretions. Two of the four macaques generated mucosal antibody responses detectable in vaginal lavages. Strong serum IgG responses lasting for at least 1 year were detected in two of the four monkeys. SIV-specific T-cell lymphoproliferative responses were detected in three of the four monkeys. SIV-specific cytotoxic T lymphocytes were detected in two of the four monkeys. This is the first report of poliovirus-elicited vaginal IgA or cytotoxic T lymphocytes in any naturally infectable primate, including humans. These findings support the concept that a live poliovirus vector is a potentially useful delivery system that elicits humoral, mucosal, and cellular immune responses against exogenous antigens.
The current human immunodeficiency virus (HIV) pandemic has infected more than 30 million people, and the search for an AIDS vaccine continues. Live virus vectors are leading candidates in the hunt for a potential vaccine. Several viral vectors have shown promise in simian immunodeficiency virus (SIV) protection experiments with monkeys, and numerous other live virus vector systems, including our live poliovirus vector, are in earlier testing phases of vaccine development (5, 7, 55).
Poliovirus is an attractive live virus vector for several reasons. The Sabin live poliovirus vaccine is one of the best vaccines in the world. It produces long-lasting immunity (46) and herd immunity (60), it is very safe and easy to experimentally manipulate (32), it is cheap to produce and distribute in developing countries (19), and most importantly, it produces a potent mucosal immune response (42). The capacity of poliovirus to generate a strong mucosal immune response is particularly important given that greater than 90% of HIV-1 infections worldwide occurred via sexual transmission (62). Any strategy to truly control the AIDS pandemic must include a vaccine that prevents sexual transmission of HIV-1.
Natural HIV infections are persistent in virtually all infected individuals, indicating that the human immune system has grave difficulties combating the virus; however, there are several reasons to believe that a strong preexisting mucosal anti-HIV immune response can be protective. Self-limited infections appear to occur, and a vaccine that further tips that balance at the mucosal barrier in the favor of the vaccinee may be able to fully prevent sexually transmitted HIV infections (54). Statistical data both from surveys of individual multiple sexual partners and from surveys tracking individuals exposed to HIV through needle stick injuries indicate that establishment of an HIV infection is a relatively uncommon event (30, 50). Epidemiological estimates indicate that HIV is only moderately infectious as a sexually transmitted disease, being transmitted on average at a rate of 0.1 to 1% per at-risk sexual encounter (30). These statistics are supported by experiments with macaques where naive monkeys were inoculated intravaginally with a low dose of SIV and subsequent PCR analysis transiently detected SIV-infected cells in circulation, without viral persistence or seroconversion (33). A strong anti-HIV mucosal immune response may prevent HIV from completing the pathogenic events necessary to establish a persistent and lethal infection.
The current gold standard for mucosal protection by a candidate AIDS vaccine is the published vaccinia virus-SIV work of J. Benson et al. showing almost 50% protection of macaques against a mucosal (rectal) challenge with the highly virulent SIVmac251 (6). Interestingly, vaccinia virus-SIV was unable to provide protection against an intravenous challenge in this experiment. These challenge experiments suggest that generating local immunity may be as important as other characteristics of the anti-SIV immune response generated by candidate vaccines. This observation is further supported by the fact that though SIV subunit vaccinations have generally been unable to prevent disease following challenge with a virulent SIV strain, direct inoculation of a subunit vaccine into the iliac lymph nodes of macaques provided protection against a rectal mucosal challenge with a virulent SIV (23).
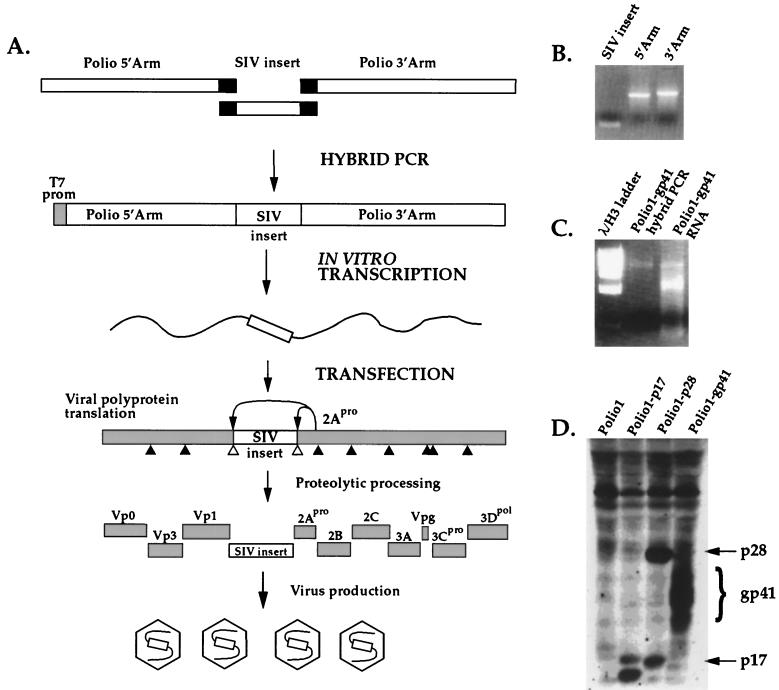
We have previously reported the development of a recombinant poliovirus live virus vector system where we inserted an immunogenic gene fragment of interest at the junction between the capsid proteins and the nonstructural proteins (the P1/P2 junction) in the poliovirus polyprotein reading frame (61). The gene fragment is expressed with the rest of the poliovirus genome as part of the polyprotein and is cleaved away from the polyprotein via the activity of poliovirus-encoded proteases, which cleave at engineered proteolytic sites flanking the gene insert (Fig. 1A). That recombinant poliovirus live-virus vector was tested in mice susceptible to poliovirus infection (48) and demonstrated to elicit strong antibody (61) and cytotoxic T-lymphocyte (CTL) responses (29, 56).
FIG. 1.
In vitro construction of a recombinant poliovirus containing an SIV gene fragment. (A) Strategy schematic. Three PCR fragments were synthesized independently (Polio 5′ Arm, SIV insert, and Polio 3′ Arm) and then joined by a hybrid PCR to generate a full-length poliovirus genome that includes the SIV gene fragment inserted at the P1-P2 junction of the genome. Infectious poliovirus-SIV RNA was generated by in vitro transcription from a T7 promoter. The RNA was transfected into HeLa cells, where viral replication occurs. The viral polyprotein, including the SIV insert, was translated, and the SIV insert was cleaved away from the polyprotein via two 2Apro protease cleavage sites flanking the insert. The virus then continued its replication cycle and produced infectious virions containing the poliovirus genome with the SIV insert. (B) Three independent PCR products, Polio 5′ Arm, SIV insert, and Polio 3′ Arm. (C) Poliovirus-SIV DNA hybrid-PCR product (specifically, Polio1-gp41) and full-length Polio1-gp41 RNA from in vitro transcription. (D) Western blot of a whole cytoplasmic protein extract from HeLa cells infected with Polio1-p17, Polio1-p28, or Polio1-gp41 and probed with SIV antiserum.
Here we describe a novel in vitro method of generating recombinant polioviruses, the construction of recombinant polioviruses of two different serotypes, and the inoculation of cynomolgus macaques with these poliovirus live virus vectors expressing SIV antigens. Both the humoral and cellular immune responses directed against SIV antigens were characterized.
MATERIALS AND METHODS
Recombinant poliovirus construction and DNA procedures.
PCRs to construct the recombinant viruses used recombinant Tth (rTth) polymerase (Perkin-Elmer, Branchburg, N.J.) under conditions recommended by the manufacturer. Poliovirus type 1 (Polio1) cDNA (Mahoney strain) was used as the template DNA to generate the type 1 poliovirus recombinants. The Sabin 2 (Sabin2) cDNA template was generated by infecting HeLa cells with an S0+3 stock (the original Sabin virus isolate passaged three additional times), which was the kind gift of Konstantin Chumakov (Food and Drug Administration, Bethesda, Md.). Total RNA from infected cells was prepared by phenol-chloroform extraction at 9 h postinfection and precipitated with ethanol. Reverse transcription was carried out with Superscript II (Life Technologies, Gaithersburg, Md.) with either random hexamer or oligo(dT) primers. This Sabin2 cDNA was used as template DNA to generate the Sabin2 poliovirus recombinants. SIVmac239 plasmids p239SpSp5′ and p239SpE3′ (obtained from the AIDS Research and Reference Reagent Program, courtesy of Ronald Desrosiers [22]) were used as PCR templates to generate SIV inserts. The 5′ half of the Polio1 genome (Polio 5′ Arm) was amplified with primers 1 and 2, and Polio 3′ Arm was amplified with primers 3 and 4. An EcoRI restriction site was introduced at the P1-P2 junction of Polio 5′ Arm, and a XhoI site was introduced at the P1-P2 junction of Polio 3′ Arm. Proteolytic cleavage sites flanking the restriction sites were designed to be nonhomologous, and a five-glycine linker was introduced upstream of the EcoRI site on the 5′ side of the P1-P2 junction, creating a construct comparable in design to pMov2.11 (61). Restriction enzyme cleavage of the PCR products was done prior to hybrid PCR to generate clean termini at the SIV gene fragment insertion site. When necessary, PCR products were purified by agarose gel electrophoresis and recovered with a Qiagen (Valencia, Calif.) gel extraction kit. Polio1 SIV inserts were generated with primers 5 and 6 (p17), 7 and 8 (gp41), and 9 and 10 (p28). For Sabin2, Polio 5′ Arm was amplified with primers 11 and 12, and Polio 3′ Arm was amplified with primers 13 and 14. Sabin2 inserts were generated with primers 15 and 16 (gp41), 17 and 18 (p17), and 19 and 20 (p28). The Sabin2 insert cloning site was identical to that of Polio1, except the restriction sites were reversed (XhoI at 5′ and EcoRI at 3′).
Hybrid PCRs were carried out with approximately 200 ng of Polio 5′ Arm template DNA and equimolar amounts of Polio 3′ Arm and the SIV DNA fragment. PCR conditions were as follows: 95°C for 3 min, and then rTth polymerase was added and 11 cycles of PCR were carried out at 95°C for 1 min, 50°C for 1 min, and 72°C for 4 min. Primers 1 and 4 were used to amplify the Polio1 recombinants, and primers 11 and 14 were used to amplify the Sabin2 recombinants.
Full-length viral RNA was generated from hybrid PCR DNA with T7 RNA polymerase and 1 μg of the template in a standard in vitro transcription reaction mixture (10× transcription buffer from Roche Molecular Biochemicals [Indianapolis, Ind.] and 20 U of RNasin [Promega, Madison, Wis.]) at 37°C for 1 h. The presence of full-length RNA was confirmed by agarose gel electrophoresis.
Replication-competent recombinant polioviruses were recovered by transfecting adherent HeLa S3 cells with 5 μg of RNA by the DEAE-dextran method (61), overlaying the monolayer with 1% agar–Dulbecco modified Eagle medium (DMEM) plus 10% newborn calf serum (Life Technologies), incubating the cells at 32°C, and picking individual viral plaques 5 days posttransfection. Individual plaques were then passaged twice on HeLa cells, with the first passage at a multiplicity of infection (MOI) of 0.001 and the second at an MOI of 1, to generate the P2 stocks of 10 to 100 ml of virus used for immunizations.
Viral infections and stocks.
In all experiments, 80%-confluent 10-cm-diameter dishes of HeLa cells containing approximately 5 × 106 cells were used. Dishes were washed with phosphate-buffered saline (PBS), and virus was added at the desired MOI in a volume of 200 μl. Dishes were incubated at room temperature for 15 min to allow viral adsorption, and then 3 ml of medium was added and dishes were incubated at 32°C (5% CO2) until cytopathic effect was visible. Virus was recovered by centrifugation of the cells and medium at 3,000 × g for 5 min followed by three quick freeze-thaw cycles. After recentrifugation, the cleared supernatant containing recombinant poliovirus was transferred to a fresh tube and stored at −20°C.
Neutralization assays were carried out with the desired volume of monkey serum (25 to 90 μl) mixed with 1,000 PFU of the appropriate virus (Polio1 [Mahoney strain] or Sabin2) in a 100-μl total volume (brought to volume with PBS). Serum was incubated with virus for 30 min at room temperature, and then serial dilutions were made and added to HeLa cell dishes for 15 min to allow for viral adsorption. Plates were washed once with PBS before adding 1× DMEM–F12 and 1% agar overlay. Plaque assays were then incubated at 37°C for 2 days (Polio1 assays) or 3 days (Sabin2 assays). Agar overlays were then removed, and plates were stained with a vital dye (0.1% crystal violet, 20% ethanol) to reveal the viral plaques, which were counted. Ninety percent neutralization was established as a 10× reduction in the number of plaques compared to the number of plaques counted on a control plate lacking monkey serum or containing preimmune monkey serum.
RT-PCR.
The presence of the SIV gene fragments in the recombinant polioviruses was confirmed by reverse transcription-PCR (RT-PCR). Total RNA was isolated from cells at 9.5 h postinfection with RNeasy (Qiagen) per the manufacturer’s protocol. cDNA was generated by RT with Superscript II (Life Technologies) and oligo(dT) primers by following the manufacturer’s recommended protocol. PCR was carried out with PfuTurbo (Stratagene, La Jolla, Calif.) with the manufacturer’s recommended reagents and under the following conditions: 95°C for 3 min and then 30 cycles of 95°C for 1 min, 50°C for 1 min, and 72°C for 1 min. PCR products were analyzed on a 1.2% agarose gel buffer. Primers used for Polio1 recombinants were designated primers 21 and 22. Primers for Sabin2 were designated primers 23 and 24.
Western blotting and immunofluorescence.
Expression of the SIV antigens by the recombinant polioviruses was confirmed by Western blotting and immunofluorescence assays. For Western blotting, HeLa cells infected with wild-type or SIV-recombinant polioviruses (MOIs of 1 to 5) were incubated for 9 h at 37°C. Cells were harvested and lysed on ice for 1 min (lysis buffer consisted of 10 mM Tris [pH 7.5], 140 mM NaCl, 5 mM KCl, and 1% NP-40), and nuclei were removed by centrifugation (3). Four micrograms of total lysates was loaded on a sodium dodecyl sulfate–12% polyacrylamide gel and analyzed by immunoblotting. The anti-SIV antiserum used was obtained as a pool of serum from SIV-infected rhesus macaques (Macaca mulatta). Antiserum directed against poliovirus capsid proteins was obtained by inoculating rabbits with purified poliovirus. Horseradish peroxidase-conjugated secondary antibodies (both anti-human and anti-rabbit), and enhanced-chemiluminescence detection kits were obtained from Amersham (Arlington Heights, Ill.).
Western blots were also used to test for monkey anti-poliovirus antibodies. In these experiments, HeLa cells were infected at an MOI of 5 with Polio1 (Mahoney strain) or Sabin2 or left uninfected. Cells were harvested at 5 h (Polio1) or 5.5 h (Sabin2) postinfection and lysed, and nuclei were removed by centrifugation. The protein concentrations were quantified by Bradford assay, and 25 μg of total lysate was run on a sodium dodecyl sulfate–12% polyacrylamide gel before being blotted. Blots were probed with 1:200-diluted monkey serum in TBST (10 mM Tris-HCl [pH 7.5], 150 mM NaCl, 0.1% Tween 20), washed three times, probed with the horseradish peroxidase anti-human antibody (1:2,000 dilution), and then detected by enhanced chemiluminescence. Images were digitally scanned and exported to Photoshop 3.0 and Illustrator 7.0 (Adobe, San Jose, Calif.).
For immunofluorescence assays, adherent HeLa cells infected with wild-type and SIV-recombinant polioviruses (MOI of 0.3) were incubated for 9 h at 37°C. Cells were then fixed with 2% paraformaldehyde and stained with the appropriate primary antibody for 1 h at 25°C in a PBS buffer supplemented with 3% bovine serum albumin and 0.2% saponin buffer. After three PBS washes, cells were stained with secondary antibody for 1 h at 25°C in an identical buffer. Anti-SIV and anti-poliovirus antibodies were as described above. Anti-rabbit immunoglobulin G (IgG) conjugated to Texas Red and anti-monkey IgG conjugated to fluorescein isothiocyanate (FITC) secondary antibodies were obtained from Amersham. Stained cells were visualized for immunofluorescence with a Leica DMLB microscope, and images were captured via a charge-coupled-device camera and exported to Adobe Photoshop 3.0.
Oligonucleotides.
The oligonucleotides used were as follows: 1 (TAATACGACTCACTATAGGTTAAAACAGCTCTGGGGTTGT [S1-T7]), 2 (GAGTTTCTCACGCCGAATTCACCTCCCCCACCTCCGCCATGACCAAAACCGTAAGTCGTTAAGTCCTTGGTGGAGAGGGGTG [RA5′3′]), 3 (GAAATTACCTCGAGGATCTGACCACATATGGATTCGGACACCAAAACAA[RA3′ 5′]), 4 (TTTTTTTTTTTTTTTTTTCTCCGAATTAAAGAAAAATTTACCCC [Mo3′]), 5 (GGAGGTGGGGGAGGTGAATTCGGCGTGAGAAACTCC GTC [Sp175′]), 6 (ATAGTGGGTCCTCGAGGTAATTTCCTCCTCTGCC [Sp173′]), 7 (GGAGGTGGGGGAGGTGAATTCCCATGGCCAAATGCA [Gp41.b5′]), 8 (ATAGTGGGTCAGATCCTCGAGGGAAGAGAACACTGG [Gp41.b3′]), 9 (GGAGGTGGGGGAGGTGAATTCCCAGTACAACAAATAGGT [Sp275′]), 10 (ATAGTGGGTCAGATCCTCGAGCATTAATCTAGCCTTCTG [Sp283′]), 11 (TAATACGACTCACTATAGGTTAAAACAGCTCTGGGGTTG [S2-T7]), 12 (TTTGGCCATGGCTCGAGACCTCCCCCACCTCCGCCATGACCAAAACCATAAGTCGTTAATCCCTTTTC [S25′3′]), 13 (CTCTTCCGAAT TCGAC T TAACGAC T TACGGAT T TGGACACCAAAACAAAGCTGTGTACACAGCTGGCTA [S23′5′]), 14 (TTTTTTTTTTTTTTTTTTTCCCCGAATTAAAGAAAAATTTACCCC [S23′]), 15 (GAAAAGGGATTAACGACTTATGGTTTTGGTCATGGCGGAGGTGGGGGAGGTCTCGAGCCATGGCCAAATGCAAGT [S2gp41.5′], 16 (GTACACAGCTTTGTTTTGGTGTCCAAATCCGTAAGTCGTTAAGTCG AATTCGGAAGAGAACACTG GCCT [S2gp41.3′]), 17 (GAAAAGGGATTAACGACTTATGGTTTTGGTCATGGCGGAGGTGGGGGAGGTCTCGAGGGCGTGAGAAACTCCGTC [S2sp17.5′]),18 (GTACACAGCTTTGTTTTGGTGTCCAAATCCGTAAGTCGTTAAGTCGAATTCGTAATTTCCTCCTCTGCC [S2sp17.3′]), 19 (GAAAAGGGATTAACGACTTATGGTTTTGGTCATGGCGGAGGTGGGGGAG GTCTCGAGCCAGTACAACAAATAGGT [S2sp28.5′]), 20 (GTACACAGCTTTGTTTTGGTGTCCAAATCCGTAAGTCGTTAAGTCGAATTCCATTAA TCTAGCCTTCTG [S2sp28.3′]), 21 (CCTCCAAAATCAGAGTGTATC [P1-3240F]), 22 (GCCCTGGGCTCTTGATTCTGT [P1-3580R]), 23 (CACCTCCAAGATCAGAGTGTA [S2-3240F]), and 24 (ATCGAGTCGGTGCCAAGGGCC [S2-3540R]).
Animals.
All animals used in this study were mature, cycling, female cynomolgus macaques (Macaca fascicularis, referred to as Macaca iris in older literature) from the California Regional Primate Research Center. The animals were housed in accordance with American Association for Accreditation of Laboratory Animal Care standards. When necessary, animals were immobilized with 10 mg of ketamine HCl (Parke-Davis, Morris Plains, N.J.) per kg of body weight, injected intramuscularly. The investigators adhered to the Guide for the Care and Use of Laboratory Animals prepared by the Committee on Care and Use of Laboratory Animals of the Institute of Laboratory Resources, National Resource Council. Prior to use, animals were negative for antibodies to HIV-2, SIV, type D retrovirus, and simian T-cell leukemia virus type 1.
Intranasal inoculations were done in a total volume of 1 ml. The animals were anesthetized and placed in dorsal recumbancy with the head tilted back. One-half milliliter of virus was instilled dropwise into each nostril. The animals were kept in this position for 10 min and then placed in lateral recumbancy until recovery from the anesthesia (21). Intravenous inoculations were administered in the arm in a volume of 1 ml. Five cynomolgus macaques originally received the first series of intranasal inoculations with Polio1-p17 and Polio1-gp41. One monkey developed paralytic disease 3 weeks later and was euthanized; the central nervous system infection of this monkey was most likely via direct infection of the olfactory bulb, which is a specific alternative pathway of poliovirus infection of macaques and irrelevant to this study since it is not a route of infection in humans (10, 36).
Serum antibody and vaginal and rectal lavage antibody responses.
Anti-SIV IgG and IgA responses in vaginal and rectal washes and serum were measured at regular time points during the study. Vaginal and rectal wash samples were collected and analyzed as previously described (27, 34). Briefly, vaginal washes were collected by infusing 6 ml of sterile PBS into the vaginal canal and aspirating the instilled volume. Rectal washes were collected in a comparable manner. Samples were immediately snap-frozen on dry ice and stored at −80°C until analysis. To account for the presence of IgG interfering with and reducing the detection of IgA, sera were first depleted of IgG with protein G-Sepharose beads (Pharmacia Biotech, Uppsala, Sweden) prior to use in the IgA enzyme-linked immunosorbent assay (ELISA). To deplete IgG, 25 μl of a serum sample was incubated with 100 μl of protein G-Sepharose beads for 1 h at 37°C and then at 4°C overnight; next, the protein G-Sepharose was pelleted and the supernatant was collected. Dilution of sample during this process was 1:3. All serum and secretion samples were initially screened for reactivity against whole SIV with 1:100 final dilutions of sera and 1:4 dilutions of vaginal or rectal washes. The change in optical density at 490 nm (ΔOD) between test and control wells was defined as the difference between the mean OD of the sample tested in two antigen-coated wells and the mean OD of the sample tested in two antigen-free control wells. The negative-control OD value was determined from 12 uninfected monkey serum samples and defined stringently as the average OD plus 3 standard deviations. Endpoint titers were determined if the ΔOD of the test sample exceeded the negative-control value by a factor of 2. To then quantify anti-SIV antibody titers, serial fourfold dilutions of duplicate samples of serum, vaginal wash, or rectal wash were tested by ELISA with whole pelleted SIVmac251 (Advanced Biologics Industries, Columbia, Md.). Antibody binding was detected with peroxidase-conjugated goat anti-monkey IgG (Fc) or IgA (Fc) (Nordic Laboratories, San Juan Capistrano, Calif.) and developed with o-phenylenediamine dihydrochloride (Sigma). The endpoint titer was defined as the reciprocal of the last dilution giving a ΔOD greater than 0.1.
Lymphocyte proliferative responses to SIV antigens.
Antigen-specific proliferative responses against SIV Gag and Env proteins were measured in peripheral blood mononuclear cells (PBMCs) from fresh blood samples (31). PBMCs were purified from heparinized blood with Accu-Paque cell separation medium (Accurate Chemical & Scientific Corp., Westbury, N.Y.). The cells were suspended at 2 × 106 per ml in RPMI 1640 medium supplemented with 10% fetal calf serum and plated in triplicate in volumes of 50 μl in a 96-well round-bottomed plate. SIV or control antigens at a concentration of 10, 1.0, and 0.01 μg/ml were added to the cells in 50 μl of complete medium. One hundred microliters of fresh medium was added after 48 h, and the plates were incubated for 5 days at 37°C in a CO2 incubator. The cell cultures were pulsed with [3H]thymidine (1 μCi per well; NEN-DuPont, Wilmington, Del.) overnight prior to harvesting of the cells. The SIV antigens were SIVmac239 p55gag and SIV gp140env (provided by F. Vogel [National Institutes of Health] via Biomolecular Technology, Frederick, Md.). A lysate of the fall armyworm ovary cell line, Sf9, used for the production of baculovirus-expressed p55gag, was used as a negative control for p55gag, and the medium alone was the control for gp140env. The stimulation index was defined as the mean radioactive counts per minute from replicate SIV antigen wells divided by the mean counts per minute from control wells and was considered significant if it was ≥2.0. In a series of preliminary experiments, the proliferative responses to SIV antigens of 10 macaques that had not been exposed to SIV were tested. It was determined that a level of 200 cpm in the negative-control wells was required to eliminate false-positive stimulation indexes (31).
Detection of SIV-specific CTL activity.
The details of culture and detection of bulk, secondary CTL responses have been previously reported (25, 26, 33). Briefly, PBMCs from immunized monkeys were stimulated with 10 μg of concanavalin A (Sigma) per ml and cultured for 14 days in complete medium supplemented with 5% human lymphocyte-conditioned medium (human interleukin 2; Hemagen Diagnostics, Waltham, Mass.). Autologous B cells were transformed with herpesvirus papio (594Sx1055 producer cell line, provided by M. Sharp, Southwest Foundation for Biomedical Research, San Antonio, Tex.) and infected overnight at an MOI of 30 with wild-type vaccinia virus (vvWR) or recombinant vaccinia virus expressing the p55gag (vv-gag) or gp160env (vv-env) of SIVmac239 (provided by L. Giavedoni and T. Yilma, University of California, Davis). The level of vaccinia virus infection of target cells was estimated by indirect immunofluorescence with monkey anti-vaccinia virus antibody and then with fluoresceinated goat anti-human IgG (Vector Laboratories, Burlingame, Calif.). The level of vaccinia virus infection of target cells in this series of experiments was estimated to fall between 5 and 15%.
Target cells were labeled with 50 μCi of 51Cr (Na2CrO4; Amersham Holdings, Arlington Heights, Ill.) per 106 cells. Effector and target cells were added together at multiple effector/target ratios in a 4-h chromium release assay. Specific lysis was considered positive if its level was greater than twofold above that of vvWR targets and if it was at least 10%. For two animals at the time of necropsy (71 weeks postinoculation), a limiting-dilution assay for virus-specific CTL precursors was preformed. The assay was based on previously described methods (21, 26). Briefly, isolated PBMCs or mesenteric lymph node mononuclear cells were diluted 11 times over the range of 10,000 cells per well to 100 cells per well and cultured in replicate plates with 24 wells. The cells were stimulated with concanavalin A (5 μg/ml; Sigma) and supplemented with irradiated human PBMCs as feeder cells at a concentration of 4 × 105/well. The percentages of CD3+ CD8+ T cells were identified by flow cytometry by using double surface immunofluorescence staining with FITC-conjugated anti-human CD3 (Gibco) and phycoerythrin-conjugated anti-human CD8 (Gibco). The cultures were maintained in AIM-V medium (Gibco), supplemented with 20% fetal calf serum and 5% human interleukin 2 (Hemagen Diagnostics). The level of cytolytic activity was measured on day 14, when wells were split three ways and incubated for 5 h with an autologous target cell infected with vvWR, vv-gag, or vv-env, as described above. Positive wells were identified as wells in which cytolysis exceeded that of the negative control (the mean chromium release from wells without effector cells) by 3 standard deviations. Wells containing cells that lysed uninfected autologous targets were eliminated from the calculations. The precursor frequency was determined by chi-square analysis based on maximum likelihood by a computer program provided by R. Miller (University of Michigan, Ann Arbor).
RESULTS
In vitro construction of recombinant polioviruses.
We generated recombinant polioviruses containing SIV gene fragments by a novel in vitro PCR-based approach. Briefly, Polio 5′ Arm and Polio 3′ Arm were amplified as two separate PCR products from Polio1 cDNA (Fig. 1A and B). An SIV gene fragment coding for the Gag protein p17 was amplified from an SIVmac239 plasmid clone and flanked by poliovirus 2Apro cleavage sites plus 45 bp of sequence identity with the 3′ terminus of Polio 5′ Arm and 45 bp of overlap with the 5′ terminus of Polio 3′ Arm. These three separate DNA fragments—Polio 5′ Arm, SIV p17gag, and Polio 3′ Arm—were mixed together and amplified into a single full-length recombinant virus DNA clone by hybrid PCR in which the termini of each overlapping DNA fragment served as a primer for the synthesis of the complementary strands of its neighboring DNA fragment, resulting in the ligation of the three DNA fragments. Further amplification of full-length Polio1-p17 was provided by 10 cycles of standard PCR with 5′ and 3′ primers terminal to the full-length product (see Materials and Methods). This amplified full-length Polio1-p17 recombinant virus DNA contained the p17gag gene fragment (SIV Gag amino acids [aa] 2 to 135) at the P1-P2 junction, between the genes for the structural and nonstructural proteins of the virus. Infectious RNA was then generated by a standard in vitro T7 transcription reaction (Fig. 1C). The transcribed RNA was then transfected into HeLa cells, and virus was recovered. Recovered Polio1-p17 exhibited growth characteristics comparable to those of other recombinant polioviruses we have previously generated (61). Two additional type 1 recombinant polioviruses containing fragments of SIV p28gag (SIV Gag aa 136 to 364) and gp41env (SIV Env aa 523 to 628) were generated by the same in vitro construction technique. Each of the viruses grew to titers of ∼3 × 108 and generated plaques that were 50 to 80% as large as those of wild-type Polio1 (data not shown). Expression of SIV protein in HeLa cells infected with Polio1-p17, Polio1-gp41, and Polio1-p28 was confirmed by Western blotting (Fig. 1D). This SIV protein expression is equimolar to that of each of the endogenous poliovirus proteins, as the single poliovirus open reading frame is initially translated as a polyprotein (Fig. 1A).
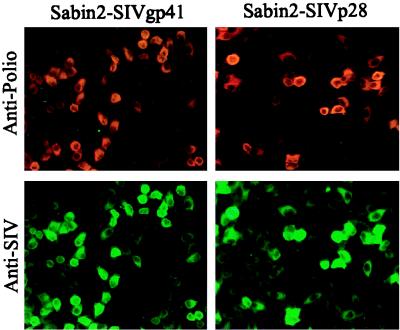
This novel in vitro method for constructing recombinant polioviruses was then used to generate a poliovirus live virus vector with the Sabin2 vaccine strain, which is a type 2 serotype poliovirus and is not neutralized by antibodies directed against Polio1 (36). Sabin2-p17, Sabin2-gp41, and Sabin2-p28 viruses were produced this way, and expression of their respective SIV gene fragments in human HeLa cells was confirmed by Western blotting (data not shown) and fluorescence immunodetection (Fig. 2) (see Materials and Methods). Each of the Sabin2 recombinant viruses grew to titers of ∼5 × 108 and generated plaques that were 50 to 80% as large as those of Sabin2 (data not shown).
FIG. 2.
Expression of SIV proteins in infected human cells. One hundred percent-confluent HeLa cells were infected with Sabin2-gp41 or Sabin2-p28 at an MOI of 0.3. Cells were fixed and colabeled with anti-poliovirus antibodies (Texas Red) and anti-SIV antibodies (FITC; green). One hundred percent of Sabin2-SIVgp41-infected cells expressed the SIV protein, and 100% of Sabin2-SIVp28-infected cells expressed the SIV protein.
Genetic stability can be an issue with live poliovirus vectors (38, 61). Therefore, we quantified the percentages of viruses still expressing SIV protein in immunodetection assays done on the P1 viral stocks. The immunodetection was done at an MOI of 0.3, and greater than 90% of the HeLa cells positive for poliovirus proteins were also positive for SIV proteins (Fig. 2 and data not shown), indicating that the P1 viral stocks were greater than 90% pure. This percentage were confirmed by RT-PCR with primers flanking the P1-P2 junction. Polio1-p17, Polio1-gp41, Sabin2-p17, and Sabin2-gp41 were passaged one additional time (P2) at an MOI of 1 to generate the viral stocks used for immunization of monkeys. RT-PCR of the P2 virus stocks indicated that 60 to 80% of each viral population still contained the full SIV insert.
Monkey immunizations.
Our primary goal was to determine whether these recombinant polioviruses expressing SIV gene fragments stimulated a mucosal anti-SIV immune response at multiple locations in macaques. Cynomolgus macaques (M. fascicularis) are known to be orally and intranasally susceptible to poliovirus, whereas most other Old World primate monkey species are not orally or intranasally susceptible to poliovirus infection and present clinical symptoms only after intracerebral or intraspinal inoculation (9, 10, 12, 51). Therefore, we first titrated poliovirus in a group of cynomolgus monkeys and established that a dose of 106 PFU of Polio1 was the minimal dose necessary to reliably seroconvert 100% of cynomolgus macaques when they are inoculated intranasally (data not shown).
We then designed our recombinant poliovirus immunization as follows: four 2 × 107-PFU intranasal inoculations of a mixture of Polio1-p17 and Polio1-gp41 (one dose every three days), followed 11 weeks later by three 1 × 107-PFU intranasal inoculations of a mixture of Sabin2-p17 and Sabin2-gp41. By using poliovirus live virus vectors derived from two different serotypes (1 and 2), we hoped to avoid vector neutralization problems and increase our ability to boost the immune response against the SIV fragments. The SIV fragments used in these experiments were previously shown to be immunogenic in mice when they were expressed by a recombinant poliovirus; therefore, we had reason to believe that they may be immunogenic in macaques as well (61).
An intravenous booster inoculation was given to all four monkeys 38 weeks into the experiment and will be discussed later.
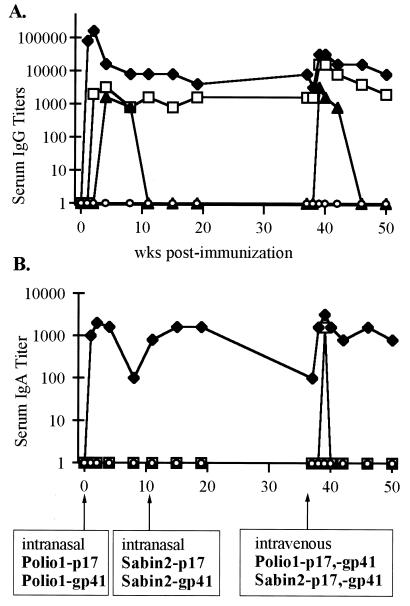
Intranasal immunization induced serum anti-SIV IgG and IgA responses.
The results of ELISAs for serum IgG and IgA responses against SIV are shown in Fig. 3. Three of four monkeys (monkeys 25136, 25137, and 26394) developed strong anti-SIV IgG responses after intranasal inoculation with Polio1-p17 and Polio1-gp41 (Fig. 3A). The second set of intranasal immunizations with Sabin2-p17 and Sabin2-gp41 induced an anamnestic response in two monkeys (monkeys 25136 and 26394) as evidenced by enhanced levels of anti-SIV IgG in sera. Both of these monkeys then maintained a strong long-term anti-SIV IgG response, with titers between 1:1,000 and 1:10,000 (Fig. 3A). In addition to this IgG response, monkey 25136 developed a strong and persistent serum anti-SIV IgA response after intranasal immunization (Fig. 3B).
FIG. 3.
(A) Anti-SIV IgG titers in the sera of poliovirus-SIV-immunized macaques. Four cynomolgus macaques were inoculated intranasally with Polio1-gp41 and Polio1-p17 at week 0. Intranasal inoculations of Sabin2-p17 and Sabin2-gp41 were done at week 11. Intravenous boosts of all four recombinant viruses were done at week 38. Monkeys are labeled as follows: monkey 22701 (○), monkey 25136 (⧫), monkey 25137 (▴), and monkey 26394 (□). (B) Anti-SIV IgA titers in the sera of the poliovirus-SIV-immunized macaques. Symbols are as noted above.
In summary, intranasal immunization with these four recombinant polioviruses elicited anti-SIV IgG in the sera of three of four monkeys and anti-SIV IgA in the serum of one monkey. Therefore, the recombinant polioviruses replicated in vivo and effectively expressed immunogenic SIV antigens.
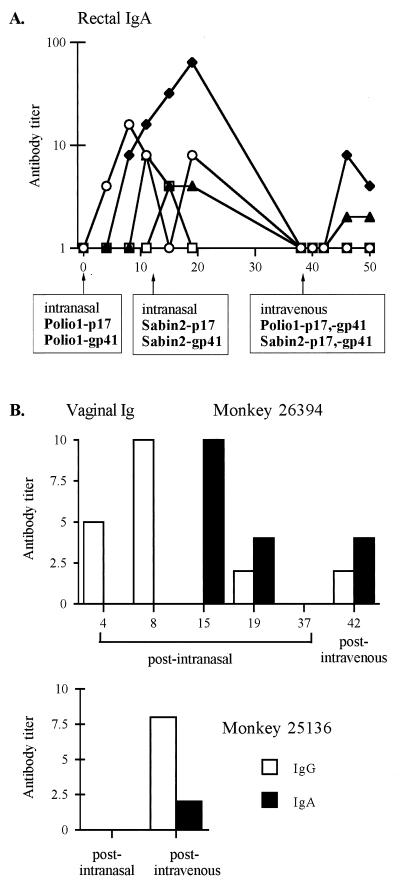
Intranasal immunization induced rectal and vaginal anti-SIV antibody responses.
The common mucosal immune system theory proposes that immunization at one mucosal site will induce immunity detectable in other mucosal sites (40). Looking for evidence of such a broad mucosal response with poliovirus, we measured anti-SIV antibody titers in rectal washes and vaginal secretions after intranasal inoculations with Polio1-p17, Polio1-gp41, Sabin2-p17, and Sabin2-gp41.
Following a single intranasal immunization, three of the four monkeys generated a rectal anti-SIV IgA response, and every monkey tested positive for rectal IgA after both sets of intranasal immunizations (Fig. 4A). One monkey (monkey 26394) had detectable anti-SIV IgA levels in vaginal lavage after the Sabin2-gp41 and Sabin2-p17 intranasal immunizations (Fig. 4B). This monkey also exhibited a vaginal anti-SIV IgG response (Fig. 4B). The vaginal and rectal lavages from the other three monkeys tested negative for anti-SIV IgG in the screening ELISA and were not analyzed further. Thus, intranasal immunization with recombinant polioviruses expressing SIV antigens generated a substantial IgA response in rectal secretions, even though only one monkey tested positive for serum IgA. In contrast, the IgA response to the SIV antigens was more limited in vaginal secretions.
FIG. 4.
(A) Anti-SIV IgA titers in the rectal washes of poliovirus-SIV-immunized macaques. Four cynomolgus macaques were inoculated intranasally with Polio1-gp41 and Polio1-p17 at week 0. Intranasal inoculations of Sabin2-p17 and Sabin2-gp41 were done at week 11. Intravenous boosts of all four recombinant viruses were done at week 38. Monkeys are labeled as follows: monkey 22701 (○), monkey 25136 (⧫), monkey 25137 (▴), and monkey 26394 (□). (B) Anti-SIV antibody titers in the vaginal washes of monkeys 26394 and 25136.
Surprisingly, intranasal immunization induced a pure mucosal anti-SIV antibody response in one monkey. The anti-SIV antibody response of monkey 22701 consisted only of IgA in rectal secretions (Fig. 4A).
All monkeys seroconverted to poliovirus.
Anti-poliovirus antibodies were detected in the sera of all four monkeys after the intranasal inoculations (Fig. 5A). These antibodies readily detected both type 1 and type 2 polioviruses (Fig. 5A). Three of the four monkeys generated neutralizing antibodies against Polio1 that were detectable after the intranasal inoculations with Polio1-gp41 and Polio1-p17, and these neutralizing antibodies were maintained for at least 3 months (Fig. 5B). Two of the monkeys also developed neutralizing antibodies against Sabin2 (monkeys 22701 and 26394). The strong vaginal anti-SIV IgA response seen in monkey 26394 was detected only after the Sabin2-gp41 and Sabin2-p17 inoculations. Therefore, neutralizing antibodies specific for Polio1 did not prohibit replication of the Sabin2 recombinant viruses in this monkey. Monkey 22701 appears to have generated uncommon cross-neutralizing antibodies after the Polio1-gp41 and Polio1-p17 infections.
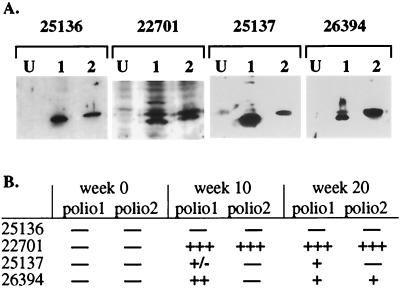
FIG. 5.
All four monkeys generated anti-poliovirus antibodies after the intranasal inoculations. (A) Anti-poliovirus Western blot. Serum from each monkey was taken at 20 weeks postinfection and used to detect poliovirus antigens (primarily Vp1) by Western blotting. Lanes: U, uninfected cell extract; 1, Polio1-infected-cell extract; 2, Polio2-infected-cell extract. (B) Poliovirus neutralizing antibodies. Serum from each monkey was tested for poliovirus neutralizing antibodies by incubation with 1,000 PFU of Polio1 or Sabin2 (Polio2) (see Materials and Methods). +++, 95% neutralization (with 25 μl of serum); ++, 90% neutralization (with 25 μl of serum); +, 50% neutralization (with 25 μl of serum); +/−, 50% neutralization (with 90 μl of serum); −, no neutralizing antibodies detected (with 90 μl of serum).
Intranasal immunization induced anti-SIV T-cell proliferative responses.
Anti-poliovirus helper T-cell immune responses have been reported for humans and mice immunized with the Sabin poliovirus vaccine (14, 28, 57). To determine if immunization of monkeys with our recombinant polioviruses elicited SIV-specific T-helper lymphocytes, the proliferative response of PBMCs was determined following in vitro stimulation with SIV antigens (see Materials and Methods). Data from all four monkeys are shown in Table 1. Two monkeys (monkeys 25137 and 26394) generated an SIV Gag-specific lymphoproliferative response after the intranasal immunizations.
TABLE 1.
Lymphocyte responses to SIV proteins following immunization with poliovirus vectors expressing p17 and gp41
| Monkey | No. of weeks postinoculationa | Lymphoproliferative responseb to:
|
|
|---|---|---|---|
| p55gag | gp140env | ||
| 22701 | 11 (i.n.) | − | − |
| 19 | − | − | |
| 38 (i.v.) | |||
| 40 | − | 2.4 | |
| 42 | 2.2 | 2.2 | |
| 25136 | 11 (i.n.) | − | − |
| 19 | − | − | |
| 38 (i.v.) | |||
| 40 | − | − | |
| 42 | − | − | |
| 25137 | 11 (i.n.) | − | − |
| 19 | 2.4 | − | |
| 38 (i.v.) | |||
| 40 | − | − | |
| 42 | − | − | |
| 26394 | 11 (i.n.) | 8.1 | − |
| 19 | − | 2.0 | |
| 38 (i.v.) | |||
| 40 | ND | ND | |
| 42 | − | − | |
Monkeys were inoculated intranasally with Polio1-gp41 and Polio1-sp17 on day 0. Intranasal boost (i.n.) with Sabin2-gp41 and Sabin2-sp17 was at week 11. Intravenous inoculation (i.v.) with all four viruses was done at week 38.
Proliferation assays were done with PBMCs and purified p55gag or gp140env (see Materials and Methods). Samples giving a proliferative response of <2.0 were considered negative and are indicated by −. ND, not determined.
Intravenous booster immunization induced an anamnestic anti-SIV antibody response in the intranasally primed monkeys.
To augment the humoral and cellular responses generated after intranasal immunization, the monkeys were boosted intravenously with a mixture of all four recombinant polioviruses expressing the SIV antigens p17gag and gp41env. The intravenous boost given 38 weeks after the initial intranasal immunization generated a rapid but transient increase in serum anti-SIV IgG titers in three of the four monkeys (monkeys 25136, 25137, and 26394) and an increase in serum anti-SIV IgA in two of the four monkeys (monkeys 25136 and 26394), with levels soon returning to the pre-intravenous boost levels (Fig. 3).
Following the intravenous boost, monkeys 25136 and 26394 had low but detectable titers of anti-SIV IgA (1:2 to 1:4) in the vaginal lavages collected between 2 and 12 weeks after the intravenous boost (Fig. 4B). Interestingly, monkey 26394 was the same monkey that showed a vaginal IgA response after the intranasal inoculations. Monkeys 25136 and 26394 exhibited not only vaginal anti-SIV IgA responses but also vaginal anti-SIV IgG responses several weeks after the intravenous boost (Fig. 4B).
At the time of the intravenous boost, 9 months after the initial intranasal inoculation, anti-SIV IgA levels were undetectable in the rectal washes of all monkeys. The intravenous immunization resulted in a return of detectable rectal anti-SIV IgA in two of the four animals (monkeys 25136 and 25137), present for at least 3 months after the immunization. As expected, the intravenous boost had no effect on specific IgG levels in rectal washes.
Animal 22701, which made a purely IgA anti-SIV response after the intranasal inoculations, did not produce detectable antibodies after the intravenous boost (Fig. 3 and 4). However, this animal did make notable anti-SIV lymphoproliferative responses to both the p17gag and gp41env antigens after the intravenous boost (Table 1).
Intravenous booster immunization induced anti-SIV CTLs.
CTL responses have not been previously reported for live-poliovirus vaccinations in humans or other primates (60). We have reported the ability of our poliovirus live virus vectors to generate a CTL response against a model antigen (chicken ovalbumin) in mice (29, 56). Additionally, anti-HIV CTLs may be an important part of an AIDS vaccine. Therefore, we were interested in whether our poliovirus vectors expressing SIV proteins would stimulate anti-SIV CTLs in macaques.
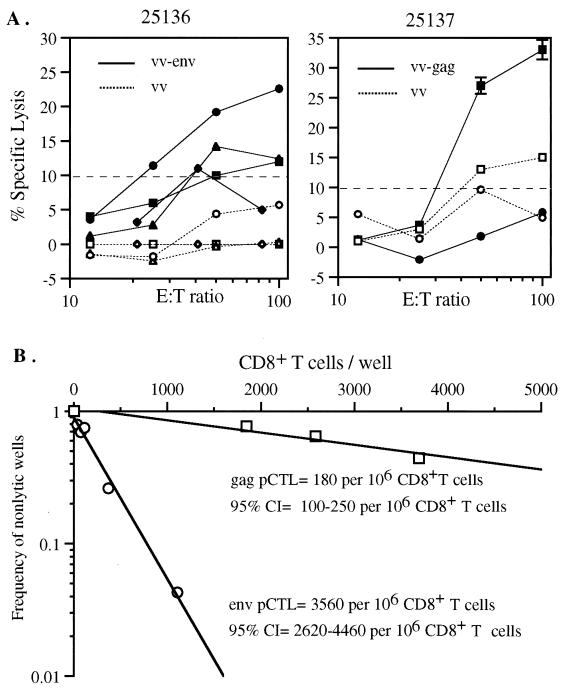
Each monkey was tested at several time points for anti-SIV cytotoxic T cells by a bulk PBMC cytolytic assay. Anti-SIV CTLs specific for Env were consistently detected in monkey 25136 from week 19 through week 42, though it was difficult to obtain greater than 10% specific lysis (Fig. 6A). This was the only monkey with detectable Env-specific CTLs by bulk culture assay. Anti-SIV CTLs specific for Gag were not detected in any monkeys after the two intranasal inoculations. However, after the intravenous booster inoculation, Gag-specific CTLs were detected in monkeys 25137 and 25136 (Fig. 6A and data not shown) by the bulk culture assay. These were the same two monkeys that made substantial rectal IgA and rapid serum IgG responses following the intravenous inoculation (Fig. 3A and 4A).
FIG. 6.
(A) SIV-specific CTLs detected using bulk PBMCs. Monkeys 25136 (left) and 25137 (right) tested positive for SIV-specific CTLs at some time points. Time points: 19 weeks (⧫), 38 weeks (●), 40 weeks (▴), 42 weeks (■). Open symbols represent negative control target cells, and filled symbols indicate Gag-expressing target cells (see Materials and Methods). (B) SIV-specific CTLs detected by limiting dilution assay. Mesenteric lymph nodes from monkey 25137 were tested for Env-specific (○) and Gag-specific (□) CTLs. Calculated precursor frequencies for monkey 25137 were 3,539 Env-specific precursor CTLs per 106 CD8+ T cells (95% confidence interval [CI] of 2,600 to 4,460) and 178 Gag-specific precursor CTLs per 106 CD8+ T cells (95% confidence interval of 100 to 250). Background lysis was subtracted (see Materials and Methods).
At 71 weeks after the initial immunization, all four monkeys were euthanized. Our bulk culture CTL assays appeared to have limited sensitivity; therefore, we tested for the presence of cytotoxic T cells by limiting dilution assay using cells isolated from mesenteric lymph nodes (monkey 26394) and peripheral blood (monkey 25137). PBMCs from monkey 25137 contained T cells with a substantial amount of anti-Env CTL activity (Fig. 6B), giving a calculated Env-specific CTL precursor frequency of 3,539 per 106 CD8+ cells. Gag-specific cytotoxic T cells were detectable at the lower frequency of 178 per 106 CD8+ cells. These data, though striking, are partly inconsistent with the results obtained by bulk culture assay. We were able to detect Gag-specific CTLs in monkey 25137 by bulk culture assay at week 42, which is in agreement with the detection of Gag-specific CTLs by limiting dilution assay at week 71. However, we were unable to detect Env-specific CTLs in monkey 25137 by bulk culture at any time point, whereas we detected a high level of Env-specific CTLs in blood by the limiting dilution assay. The limiting dilution assay is a more sensitive assay, supporting the outgrowth of low frequency antigen-specific precursors, while the bulk culture method is more dependent on initial strong stimulation of the T cells. Env-specific CTLs were not detectable in the mesenteric lymph nodes of monkey 26394, which had no detectable Gag- or Env-specific CTLs at any time point by bulk PBMC culture assay.
The results presented here indicate that inoculation of nonhuman primates with poliovirus recombinants results in both humoral and cellular immune responses. The vaccinated monkeys were not challenged with SIV because only two partial SIV proteins constituted our immunization cocktails, and it is likely that a more complex composition of antigens would be required to afford protection. We are currently developing a cocktail of recombinant polioviruses containing most of the SIV proteins, which will be much more suitable for a vaccination and challenge experiment.
DISCUSSION
In this study we constructed a set of poliovirus live virus vectors in vitro that contain SIV antigens. The in vitro PCR-based technique that we describe in this paper should be generally applicable to RNA viruses that are very difficult or impossible to clone into plasmids. We then used these polioviruses expressing SIV antigens to immunize macaques and have characterized the monkeys’ immune responses.
Analyzing the mucosal immune response generated by the live poliovirus vector was a primary goal of this study. High levels of poliovirus neutralizing mucosal IgA are directly correlated with sterilizing immunity against poliovirus (24, 42, 53). These high levels of IgA are produced in human vaccinees inoculated orally with the Sabin live attenuated poliovirus, and the vaccinees make a potent anti-poliovirus IgA response throughout the nasopharyngeal, alimentary, and rectal mucosal surfaces, which persists for several years or more (41–43). Generally, humans secrete the highest anti-poliovirus neutralizing antibody titers in saliva, with moderately lower mucosal antibody titers in both the rectum and the female vagina (43, 45). In the only human Sabin vaccinee who has been tested for vaginal anti-poliovirus antibodies, no IgA was detected (45). Our report here of anti-SIV IgA present in the vaginal secretions of two recombinant poliovirus inoculated monkeys is the first direct evidence of live poliovirus-induced IgA in the vagina (Fig. 4B). Additionally, vaginal anti-poliovirus IgA was detected in other cynomolgus monkeys we have assayed (unpublished results).
We previously reported that a related recombinant poliovirus vector could infect a cynomolgus macaque via the rectal mucosa and generate a rectal IgA response (4). Here we have shown that the immunogenicity of poliovirus in stimulating a mucosal IgA response at multiple locations can be conferred on exogenous sequences expressed by a poliovirus live virus vector inoculated intranasally.
The one monkey exhibiting a purely mucosal anti-SIV antibody response is a fascinating case of local immunity. There have been some published reports in the past that live poliovirus infection can stimulate a purely mucosal immune response (52), but recent Sabin poliovirus vaccine studies have all detected serum IgG in conjunction with mucosal IgA responses in immunized children (13, 59). In fact, we were able to detect some anti-poliovirus, but not anti-SIV, antibodies in the serum of this monkey. Using inactivated poliovirus, Ogra and Karzon (42, 44) and Orga and Orga (45) could induce secretory IgA in the vaginas, uteri, rectums, or nasopharynges of children following high-dose local immunizations, and these children showed no evidence of anti-poliovirus IgG in their sera. However, since those experiments used inactivated poliovirus virions, and expression of the recombinant proteins in our live poliovirus vectors is dependent on replication, the relationship between the two experiments is unclear.
It is worth noting that, though we did not directly test this, the monkeys in our experiment most likely secreted similar or higher levels of IgA in saliva than in the rectum and vagina, since the respiratory tracts of cynomolgus monkeys are much more susceptible to poliovirus infection than their lower alimentary tracts (10–12, 16, 51) and mucosal immunity is normally strongest at the site of inoculation (40). Salivary IgA is not a crucial parameter in the development of a candidate SIV vaccine but may be essential for the development of vaccines against pathogens that replicate in the respiratory tract. We plan to further characterize the breadth of the IgA response stimulated by this live-poliovirus vector in future experiments.
Several of the monkeys made very high IgG responses, indicating that the recombinant polioviruses replicated quite well when they were administered intranasally. Additionally, the booster responses seen in two of the monkeys when the second serotype of recombinant polioviruses was administered indicate that significant cross-neutralization between the serotypes does not occur, as was expected (36) (though one monkey did appear to generate cross-neutralizing anti-poliovirus antibodies, this generally is not seen in human vaccinees). Therefore, we may be able to use all three serotypes of poliovirus as serial vaccine vectors, giving multiple boosts to stimulate a strong and durable immune response, as we saw in monkeys 25136 and 26394 with the use of two serotypes in this study. These two monkeys maintained a high level of anti-SIV IgG in their sera for greater than a year. We note that natural poliovirus infections have been documented to result in persistent IgG neutralizing antibodies for greater than 40 years (46).
Human CD4+ helper T cells specific for poliovirus were first identified several years ago by two separate groups who isolated CD4+ clones specific for capsid protein epitopes from people vaccinated with a Sabin live attenuated poliovirus vaccine (14, 57). However, T cells specific for nonstructural proteins were not identified. In addition, poliovirus-specific T cells have not previously been reported from monkey models. We detected lymphoproliferative responses, indicative of CD4+ helper T cells, specific for SIV antigens in three of the four monkeys (Table 1). Lymphoproliferative responses were detected to both viral SIV inserts, indicating that both the p17gag and gp41env recombinant polioviruses replicated within the monkeys and stimulated antigen-specific helper T-cell responses in this study. The level of the antigen-specific proliferative responses was similar to levels reported in other studies using cynomolgus macaques (35, 39). CD4+ helper T cells are essential for generating a strong antibody response and promoting heavy-chain class switching to IgG and IgA (1). The monkey in which we could not detect any lymphoproliferative response (monkey 25136) was the monkey with the highest long-term anti-SIV IgG and IgA titers. We believe that it may be the case that monkey 25136 produced significant SIV-specific CD4+ cells but that detection was difficult because the majority of SIV-specific CD4+ cells were not circulating in the peripheral blood but were instead locally present in the gut- and bronchus-associated lymphoid tissue or the tonsillar tissue (36, 40). It is worth noting that IgA was detectable in the serum of only one monkey after the intranasal immunizations but that IgA was clearly present in the rectal mucosae of all four monkeys. These results suggest that assays based on peripheral blood samples may be inappropriate and insensitive for measuring mucosal immune responses, whether humoral or cellular. Additionally, the difficulty in identifying a correlate of immunity in the few cases where protection from a virulent SIV challenge has been achieved may indicate that the correlate of SIV immunity is a specific mucosal immune response that may be poorly measured by the standard peripheral blood assays used.
CTL responses are important in several picornavirus infections, including Theiler’s virus (49), hepatitis A virus (63), and coxsackievirus B3 (17) infections. No previous study has identified primate or human cytotoxic T cells (CD8+ T cells) specific for poliovirus, and the role of cell-mediated immunity in resolving poliovirus infections has remained unclear (47). Our laboratory has recently shown that strong CTL responses are elicited by recombinant polioviruses in poliovirus-susceptible mice (mice transgenic for the human poliovirus receptor [48]) (29, 56). In this macaque study we attempted to identify anti-SIV CTLs elicited by our recombinant polioviruses. CTL activity was detectable in two of the four monkeys, by either bulk culture or limiting dilution analysis of PBMCs. Monkey 25136 was consistently positive for anti-SIV Env-specific CTLs beginning at 19 weeks after the first intranasal inoculation; however, it was difficult to detect much greater than 10% specific lysis in these bulk-culture assays. The only other monkey to test positive for CTL activity by bulk culture assay was monkey 25137, and this monkey tested positive for CTLs specific for Gag only at the final time point (42 weeks). Monkey 25137 had a strong Env-specific CTL precursor frequency and a lower frequency of Gag-specific CTL precursors when it was analyzed by limiting dilution assay. However, due to the inconsistency of this data with the bulk culture data, we must consider our CTL results indicative rather than conclusive. We plan to improve the consistency and sensitivity of our cytotoxic T-cell assays for use in future primate experiments.
In summary, after inoculation of macaques with two serotypes of poliovirus live-virus vectors expressing SIV antigens, all of the macaques made a mucosal anti-SIV IgA response (Table 2). Three of four produced strong serum IgG responses, and three of four made a detectable anti-SIV lymphoproliferative response (Table 2). These results are very encouraging for the future development of poliovirus-derived genetically engineered vaccines, as we have shown the poliovirus vector’s ability to stimulate a broad immune response against the desired antigens in a primate model system.
TABLE 2.
Summary of anti-SIV responses after immunization
| Monkey | Serum IgG | Rectal IgA | Vaginal Ig | Helper T cells | CTLs |
|---|---|---|---|---|---|
| 26394 | √ | √ | √ | √ | |
| 25136 | √ | √ | √ | √ | |
| 25137 | √ | √ | √ | √ | |
| 22701 | √ | √ |
When evaluating the data from these recombinant poliovirus immunizations in cynomolgus macaques, it is important to keep in mind that cynomolgus monkeys replicate the virus poorly in comparison with humans and chimpanzees. The 50% infectious dose of the Sabin vaccine in humans is 50 PFU (36), and the standard dose of the Sabin poliovirus vaccine in humans is ∼2 × 107 (2). Cynomolgus macaques are several orders of magnitude less susceptible to poliovirus infection (100% infectious dose, 106 PFU, intranasally) and can be expected to generate significantly smaller immune responses to poliovirus and recombinant polioviruses than humans.
With this cynomolgus monkey data in hand, we believe that we can now plan to make a set of recombinant polioviruses containing the entirity of SIV and carry out a mucosal challenge experiment with macaques to determine whether our poliovirus live-virus vector system can confer protection against a pathogenic SIV challenge. As the recombinant poliovirus system is not limited to SIV vaccine work, we are currently developing multiple additional candidate vaccines that may be well suited to a poliovirus live virus vector system.
The World Health Organization wild poliovirus eradication effort has been wonderfully successful, and it is therefore necessary to address the future viability of a vaccine program based on poliovirus live virus vectors. We are very hopeful that wild-poliovirus infections can be eliminated, and the World Health Organization is well on its way of achieving that goal (18). However, we and others have expressed reservations about the ability to eliminate the Sabin live poliovirus vaccine viruses at any time in the near future (8). We believe that our work with these recombinant polioviruses demonstrates that the Sabin poliovirus vaccine strains should not be cast aside and that they have real potential as vectors for creating novel vaccines against major public health threats. The simple fact that the live poliovirus vaccine is so effective that wild poliovirus eradication is conceivable is a strong argument that we should parlay this knowledge into the development of other vaccines, potentially using the live poliovirus itself as the delivery vector, as we propose.
The Sabin 1 poliovirus vaccine is one of the safest vaccines in existence, with significant side effects seen in fewer that 1 in 10 million individuals. It is notable that our recombinant polioviruses are even further attenuated than the vaccine strains for both mice (7a) and macaques. The wealth of molecular knowledge about poliovirus should allow us to create even safer vaccine strains that, for example, contain modifications in the 5′ untranslated region that prevent neurovirulence and that do not revert to wild type (15, 20). Our poliovirus vector system is also providing valuable groundwork for the development of other positive-strand RNA viral vector systems. Live picornavirus systems based on rhinovirus (58) and mengovirus (64) are under development, and a poliovirus replicon system has also been tested with several model systems (37). Additionally, recombinant flaviviruses, such as one based on the yellow fever virus vaccine strain (30a), may also prove to be valuable vector systems.
ACKNOWLEDGMENTS
We thank Konstantin Chumakov for Sabin virus stocks. We thank M. Sharp for Papio virus stocks.
This work was supported by Public Health Service grant AI36178 to R.A. S.C. is supported by a Howard Hughes predoctoral fellowship.
Footnotes
Dedicated to the memory of Rob Sadler (1963–1999).
REFERENCES
- 1.Abbas A K, Lichtman A H, Pober J S. Cellular and molecular immunology. 3rd ed. Philadelphia, Pa: W. B. Saunders; 1997. [Google Scholar]
- 2.American Hospital Formulary Service. AFHS drug information. Bethesda, Md: American Society of Hospital Pharmacists, SilverPlatter International; 1998. [Google Scholar]
- 3.Andino R, Rieckhof G E, Achacoso P L, Baltimore D. Poliovirus RNA synthesis utilizes an RNP complex formed around the 5′-end of viral RNA. EMBO J. 1993;12:3587–3598. doi: 10.1002/j.1460-2075.1993.tb06032.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andino R, Silvera D, Suggett S D, Achacoso P L, Miller C J, Baltimore D, Feinberg M B. Engineering poliovirus as a vaccine vector for the expression of diverse antigens. Science. 1994;265:1448–1451. doi: 10.1126/science.8073288. [DOI] [PubMed] [Google Scholar]
- 5.Barnett S W, Klinger J M, Doe B, Walker C M, Hansen L, Duliège A M, Sinangil F M. Prime-boost immunization strategies against HIV. AIDS Res Hum Retroviruses. 1998;14(Suppl. 3):S299–S309. [PubMed] [Google Scholar]
- 6.Benson J, Chougnet C, Robert-Guroff M, Montefiori D, Markham P, Shearer G, Gallo R C, Cranage M, Paoletti E, Limbach K, Venzon D, Tartaglia J, Franchini G. Recombinant vaccine-induced protection against the highly pathogenic simian immunodeficiency virus SIV(mac251): dependence on route of challenge exposure. J Virol. 1998;72:4170–4182. doi: 10.1128/jvi.72.5.4170-4182.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buge S L, Richardson E, Alipanah S, Markham P, Cheng S, Kalyan N, Miller C J, Lubeck M, Udem S, Eldridge J, Robert-Guroff M. An adenovirus-simian immunodeficiency virus env vaccine elicits humoral, cellular, and mucosal immune responses in rhesus macaques and decreased viral burden following vaginal challenge. J Virol. 1997;71:8531–8541. doi: 10.1128/jvi.71.11.8531-8541.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7a.Crotty, S., S. Mandl, and R. Andino. Unpublished data.
- 8.Dove A W, Racaniello V R. The polio eradication effort: should vaccine eradication be next? Science. 1997;277:779–780. doi: 10.1126/science.277.5327.779. [DOI] [PubMed] [Google Scholar]
- 9.Faber H, Silverberg R. Experimental airborne infection with poliomyelitis virus. Science. 1941;94:566–568. doi: 10.1126/science.94.2450.566. [DOI] [PubMed] [Google Scholar]
- 10.Faber H K. The pathogenesis of poliomyelitis. 1st ed. Springfield, Ill: Charles C. Thomas; 1955. [Google Scholar]
- 11.Faber H K, Silverberg R J, Dong L. Poliomyelitis in Philippine cynomolgus monkeys after simple feeding. Am J Hyg. 1948;48:94–98. doi: 10.1093/oxfordjournals.aje.a119227. [DOI] [PubMed] [Google Scholar]
- 12.Faber H K, Silverberg R J, Dong L. Poliomyelitis in the cynomolgus monkey. III. Infection by inhalation of droplet nuclei and the nasopharyngeal portal of entry, with a note on this mode of infection in rhesus. J Exp Med. 1944;80:39–57. doi: 10.1084/jem.80.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Faden H, Modlin J, Thoms M L, McBean A M, Ferdon M B, Ogra P L. Comparative evaluation of immunization with live attenuated and enhanced-potency inactivated trivalent poliovirus vaccines in childhood: systemic and local immune responses. J Infect Dis. 1990;162:1291–1297. doi: 10.1093/infdis/162.6.1291. [DOI] [PubMed] [Google Scholar]
- 14.Graham S, Wang E C, Jenkins O, Borysiewicz L K. Analysis of the human T-cell response to picornaviruses: identification of T-cell epitopes close to B-cell epitopes in poliovirus. J Virol. 1993;67:1627–1637. doi: 10.1128/jvi.67.3.1627-1637.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gromeier M, Bossert B, Arita M, Nomoto A, Wimmer E. Dual stem loops within the poliovirus internal ribosomal entry site control neurovirulence. J Virol. 1999;73:958–964. doi: 10.1128/jvi.73.2.958-964.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Howe H A, Bodian D. Poliomyelitis in the cynomolgus monkey following oral inoculation. Am J Hyg. 1948;48:99–106. doi: 10.1093/oxfordjournals.aje.a119228. [DOI] [PubMed] [Google Scholar]
- 17.Huber S A, Job L P, Woodruff J F. Lysis of infected myofibers by coxsackie B3-immune T lymphocytes. Am J Pathol. 1980;98:681–694. [PMC free article] [PubMed] [Google Scholar]
- 18.Hull H F, Aylward R B. Ending polio immunization. Science. 1997;277:780. doi: 10.1126/science.277.5327.780. [DOI] [PubMed] [Google Scholar]
- 19.Hull H F, Ward N A, Hull B P, Milstien J B, de Quadros C. Paralytic poliomyelitis: seasoned strategies, disappearing disease. Lancet. 1994;343:1331–1337. doi: 10.1016/s0140-6736(94)92472-4. [DOI] [PubMed] [Google Scholar]
- 20.Iizuka N, Kohara M, Hagino-Yamagishi K, Abe S, Komatsu T, Tago K, Arita M, Nomoto A. Construction of less neurovirulent polioviruses by introducing deletions into the 5′ noncoding sequence of the genome. J Virol. 1989;63:5354–5363. doi: 10.1128/jvi.63.12.5354-5363.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Imaoka K, Miller C J, Kubota M, McChesney M B, Lohman B, Yamamoto M, Fugihashi K, Someya K, Honda M, McGhee J R, Kiyono H. Nasal immunization of nonhuman primates with simian immunodeficiency virus p55gag and cholera toxin adjuvant induces Th1/Th2 help for virus specific immune responses in reproductive tissues. J Immunol. 1998;161:5952–5958. [PubMed] [Google Scholar]
- 22.Kestler H, Kodama T, Ringler D, Marthas M, Pedersen N, Lackner A, Regier D, Sehgal P, Daniel M, King N, Desrosiers R. Induction of AIDS in rhesus monkeys by molecularly cloned simian immunodeficiency virus. Science. 1990;248:1109–1112. doi: 10.1126/science.2160735. [DOI] [PubMed] [Google Scholar]
- 23.Lehner T, Wang Y, Cranage M, Bergmeier L A, Mitchell E, Tao L, Hall G, Dennis M, Cook N, Brookes R, Klavinskis L, Jones I, Doyle C, Ward R. Protective mucosal immunity elicited by targeted iliac lymph node immunization with a subunit SIV envelope and core vaccine in macaques. Nat Med. 1996;2:767–775. doi: 10.1038/nm0796-767. [DOI] [PubMed] [Google Scholar]
- 24.Lepow M L, Warren R J, Gray N, Ingram V G, Robbins F C. Effect of Sabin type 1 poliomyelitis vaccine administered by mouth to newborn infants. N Engl J Med. 1961;264:1071–1078. doi: 10.1056/NEJM196105252642102. [DOI] [PubMed] [Google Scholar]
- 25.Lohman B L, McChesney M B, Miller C J, McGowan E, Joye S M, Van Rompay K K, Reay E, Antipa L, Pedersen N C, Marthas M L. A partially attenuated simian immunodeficiency virus induces host immunity that correlates with resistance to pathogenic virus challenge. J Virol. 1994;68:7021–7029. doi: 10.1128/jvi.68.11.7021-7029.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lohman B L, Miller C J, McChesney M B. Antiviral cytotoxic T lymphocytes in vaginal mucosa of simian immunodeficiency virus-infected rhesus macaques. J Immunol. 1995;155:5855–5860. [PMC free article] [PubMed] [Google Scholar]
- 27.Lü X, Kiyono H, Lu D, Kawabata S, Torten J, Srinivasan S, Dailey P J, McGhee J R, Lehner T, Miller C J. Targeted lymph-node immunization with whole inactivated simian immunodeficiency virus (SIV) or envelope and core subunit antigen vaccines does not reliably protect rhesus macaques from vaginal challenge with SIVmac251. AIDS. 1997;12:1–10. doi: 10.1097/00002030-199801000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mahon B P, Katrak K, Nomoto A, Macadam A J, Minor P D, Mills K H. Poliovirus-specific CD4+ Th1 clones with both cytotoxic and helper activity mediate protective humoral immunity against a lethal poliovirus infection in transgenic mice expressing the human poliovirus receptor. J Exp Med. 1995;181:1285–1292. doi: 10.1084/jem.181.4.1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mandl S, Sigal L J, Rock K L, Andino R. Poliovirus vaccine vectors elicit antigen-specific cytotoxic T cells and protect mice against lethal challenge with malignant melanoma cells expressing a model antigen. Proc Natl Acad Sci USA. 1998;95:8216–8221. doi: 10.1073/pnas.95.14.8216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mastro T D, Kitayaporn D. HIV type 1 transmission probabilities: estimates from epidemiological studies. AIDS Res Hum Retroviruses. 1998;14(Suppl. 3):S223–S227. [PubMed] [Google Scholar]
- 30a.McAllister, A., A. Arbetman, S. Mandl, and R. Andino. Unpublished data.
- 31.McChesney M B, Collins J R, Lu D, Lü X, Torten J, Ashley R L, Cloyd M W, Miller C J. Occult systemic infection and persistent simian immunodeficiency virus (SIV)-specific CD4+-T-cell proliferative responses in rhesus macaques that were transiently viremic after intravaginal inoculation of SIV. J Virol. 1998;72:10029–10035. doi: 10.1128/jvi.72.12.10029-10035.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Melnick J L. Enteroviruses: polioviruses, coxsackieviruses, echoviruses, and newer enteroviruses. In: Fields B N, Knipe D M, Howley P M, editors. Fields virology. 3rd ed. Vol. 1. Philadelphia, Pa: Lippincott-Raven Publishers; 1996. pp. 655–712. [Google Scholar]
- 33.Miller C J, Marthas M, Torten J, Alexander N J, Moore J P, Doncel G F, Hendrickx A G. Intravaginal inoculation of rhesus macaques with cell-free simian immunodeficiency virus results in persistent or transient viremia. J Virol. 1994;68:6391–6400. doi: 10.1128/jvi.68.10.6391-6400.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miller C J, McChesney M B, Lü X, Dailey P J, Chutkowski C, Lu D, Brosio P, Roberts B, Lu Y. Rhesus macaques previously infected with simian/human immunodeficiency virus are protected from vaginal challenge with pathogenic SIVmac239. J Virol. 1997;71:1911–1921. doi: 10.1128/jvi.71.3.1911-1921.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mills K H G, Kitchin P A, Mahon B P, Barnard A L, Adams S E, Kingsman S M, Kingsman A J. HIV p24-specific helper T cell clones from immunized primates recognize highly conserved regions of HIV-1. J Immunol. 1990;144:1677–1683. [PubMed] [Google Scholar]
- 36.Minor P D. Poliovirus. In: Nathanson N, Ahmed R, editors. Viral pathogenesis. Philadelphia, Pa: Lippincott-Raven; 1997. pp. 555–574. [Google Scholar]
- 37.Morrow C D, Porter D C, Ansardi D C, Moldoveanu Z, Fultz P N. New approaches for mucosal vaccines for AIDS: encapsidation and serial passages of poliovirus replicons that express HIV-1 proteins on infection. AIDS Res Hum Retroviruses. 1994;10(Suppl. 2):S61–S66. [PubMed] [Google Scholar]
- 38.Mueller S, Wimmer E. Expression of foreign proteins by poliovirus polyprotein fusion: analysis of genetic stability reveals rapid deletions and formation of cardioviruslike open reading frames. J Virol. 1998;72:20–31. doi: 10.1128/jvi.72.1.20-31.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nilsson C, Mäkitalo B, Thorstensson R, Norley S, Binninger-Schinzel D, Cranage M, Rud E, Biberfeld G, Putkonen P. Live attenuated simian immunodeficiency virus (SIV)mac in macaques can induce protection against mucosal infection with SIVsm. AIDS. 1998;12:2261–2270. doi: 10.1097/00002030-199817000-00006. [DOI] [PubMed] [Google Scholar]
- 40.Ogra P L. Mucosal immunology. 2nd ed. San Diego, Calif: Academic Press; 1999. [Google Scholar]
- 41.Ogra P L, Fishaut M, Gallagher M R. Viral vaccination via the mucosal routes. Rev Infect Dis. 1980;2:352–369. doi: 10.1093/clinids/2.3.352. [DOI] [PubMed] [Google Scholar]
- 42.Ogra P L, Karon D T. Formation and function of poliovirus antibody in different tissues. Prog Med Virol. 1971;13:156–193. [Google Scholar]
- 43.Ogra P L, Karzon D T. Distribution of poliovirus antibody in serum, nasopharynx and alimentary tract following segmental immunization of lower alimentary tract with poliovaccine. J Immunol. 1969;102:1423–1430. [PubMed] [Google Scholar]
- 44.Ogra P L, Karzon D T. Poliovirus antibody response in serum and nasal secretions following intranasal inoculation with inactivated poliovaccine. J Immunol. 1969;102:15–23. [PubMed] [Google Scholar]
- 45.Ogra P L, Ogra S S. Local antibody response to poliovaccine in the human female genital tract. J Immunol. 1973;110:1307–1311. [PubMed] [Google Scholar]
- 46.Paul J R, Riordan J T, Melnick J L. Antibodies to three different antigenic types of poliomyelitis virus in sera from north Alaskan Eskimos. Am J Hyg. 1951;54:275–285. doi: 10.1093/oxfordjournals.aje.a119485. [DOI] [PubMed] [Google Scholar]
- 47.Plotkin S, Orenstein W, editors. Vaccines. 3rd ed. Philadelphia, Pa: W. B. Saunders Company; 1999. [Google Scholar]
- 48.Ren R B, Costantini F, Gorgacz E J, Lee J J, Racaniello V R. Transgenic mice expressing a human poliovirus receptor: a new model for poliomyelitis. Cell. 1990;63:353–362. doi: 10.1016/0092-8674(90)90168-e. [DOI] [PubMed] [Google Scholar]
- 49.Rossi C P, McAllister A, Tanguy M, Kägi D, Brahic M. Theiler’s virus infection of perforin-deficient mice. J Virol. 1998;72:4515–4519. doi: 10.1128/jvi.72.5.4515-4519.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Royce R A, Seña A, Cates W, Jr, Cohen M S. Sexual transmission of HIV. N Engl J Med. 1997;336:1072–1078. doi: 10.1056/NEJM199704103361507. [DOI] [PubMed] [Google Scholar]
- 51.Sabin A B. Pathogenesis of poliomyelitis. Science. 1956;123:1151–1157. doi: 10.1126/science.123.3209.1151. [DOI] [PubMed] [Google Scholar]
- 52.Sabin A B. Present position of immunization against poliomyelitis with live virus vaccines. Br Med J. 1959;1:663–680. doi: 10.1136/bmj.1.5123.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Savilahti E, Klemola T, Carlsson B, Mellander L, Stenvik M, Hovi T. Inadequacy of mucosal IgM antibodies in selective IgA deficiency: excretion of attenuated poliovirus is prolonged. J Clin Immunol. 1988;8:89–94. doi: 10.1007/BF00917895. [DOI] [PubMed] [Google Scholar]
- 54.Schultz A. Encouraging vaccine results from primate models of HIV type 1 infection. AIDS Res Hum Retroviruses. 1998;14(Suppl. 3):S261–S263. [PubMed] [Google Scholar]
- 55.Schultz A. Using recombinant vectors as HIV vaccines. IAVI Rep. 1998;3:1–4. [Google Scholar]
- 56.Sigal L J, Crotty S, Andino R, Rock K L. Cytotoxic T-cell immunity to virus-infected non-haematopoietic cells requires presentation of exogenous antigen. Nature. 1999;398:77–80. doi: 10.1038/18038. [DOI] [PubMed] [Google Scholar]
- 57.Simons J, Kutubuddin M, Chow M. Characterization of poliovirus-specific T lymphocytes in the peripheral blood of Sabin-vaccinated humans. J Virol. 1993;67:1262–1268. doi: 10.1128/jvi.67.3.1262-1268.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Smith A D, Geisler S C, Chen A A, Resnick D A, Roy B M, Lewi P J, Arnold E, Arnold G F. Human rhinovirus type 14:human immunodeficiency virus type 1 (HIV-1) V3 loop chimeras from a combinatorial library induce potent neutralizing antibody responses against HIV-1. J Virol. 1998;72:651–659. doi: 10.1128/jvi.72.1.651-659.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Smith J W, Lee J A, Fletcher W B, Morris C A, Parker D A, Yetts R, Magrathe D I, Perkins F T. The response to oral poliovaccine in persons aged 16–18 years. J Hyg. 1976;76:235–247. doi: 10.1017/s0022172400055133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sutter R W, Cochi S L, Melnick J L. Live attenuated poliovirus vaccines. In: Plotkin S, Orenstein W, editors. Vaccines. 3rd ed. Philadelphia, Pa: W. B. Saunders; 1999. p. 1230. [Google Scholar]
- 61.Tang S, van Rij R, Silvera D, Andino R. Toward a poliovirus-based simian immunodeficiency virus vaccine: correlation between genetic stability and immunogenicity. J Virol. 1997;71:7841–7850. doi: 10.1128/jvi.71.10.7841-7850.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.UNAIDS and the World Health Organization. Report on the global HIV/AIDS epidemic. Geneva, Switzerland: World Health Organization; 1998. [Google Scholar]
- 63.Vallbracht A, Maier Y, Stierhof D, Wiedmann K H, Flehmig B, Fleischer B. Liver-derived cytotoxic T cells in hepatitis A virus infection. J Infect Dis. 1989;160:209–217. doi: 10.1093/infdis/160.2.209. [DOI] [PubMed] [Google Scholar]
- 64.Van der Ryst E, Nakasone T, Habel A, Venet A, Gomard E, Altmeyer R, Girard M, Borman A M. Study of the immunogenicity of different recombinant Mengo viruses expressing HIV1 and SIV epitopes. Res Virol. 1998;149:5–20. doi: 10.1016/s0923-2516(97)86896-3. [DOI] [PubMed] [Google Scholar]