Abstract
Herpesviruses typically establish latent infection in their hosts. The cell(s) responsible for harboring latent virus, in most cases, is not known. Using immunofluorescence and PCR-in situ hybridization (PISH), a technique which combines the sensitivity of PCR with the localization and specificity of in situ hybridization, we provide the first direct evidence that endothelial cells are a major site of murine cytomegalovirus (MCMV) DNA in latently infected animals. These findings are consistent with existing knowledge of the biological behavior of CMV, in particular the transmission of latent CMV by solid organ and bone marrow transplantation, in both human and animal models. In addition, we have localized MCMV DNA in the lung alveolar macrophage and in bone marrow cells. Our findings confirm that bone marrow-derived hematopoietic cells are a site of CMV latency and further suggest that bone marrow may be a reservoir of infected progeny capable of migrating into the circulation and establishing latency in various tissues. These findings provide clearly needed insight into the site of latent infection which is central to an understanding of the mechanisms of reactivation.
One of the most challenging problems in medicine concerns latent viral infections, in particular the specific identification of tissues which harbor these viruses, the ways viruses persist, and the mechanisms by which they are reactivated. Reactivation of latent cytomegalovirus (CMV), a member of the herpesvirus family, is responsible for significant morbidity and mortality in immunocompromised individuals, including recipients of solid organ and bone marrow transplants (20) as well as patients with AIDS (36). Furthermore, CMV has been proposed as an etiological agent in the pathogenesis of certain malignancies (51), insulin-dependent diabetes mellitus (38), and atherosclerosis (32, 41, 50).
The specific site(s) of latency and/or persistence of CMV, in terms of both organ and cell type(s), has remained elusive despite three decades of investigation (23). Animal models of CMV latency have been studied extensively in attempts to characterize latency. In murine CMV (MCMV), both the splenic stroma (43) and, more specifically, the sinusoidal lining cell (34) have been proposed as sites of latent MCMV maintenance, although these findings are indirect and dependent on reactivation of latent virus. With the advent of DNA amplification techniques, MCMV DNA has been determined to be present in most if not all murine organs (12). In addition, several human tissues, including bone marrow, have been found to contain latent CMV (17, 27, 35). Together, these findings suggest that latent virus is harbored in a ubiquitous cell type, explaining the transmission of latent CMV by transplantation in both human and animal models. Both the elusiveness of a specific cellular site for the latent virus and the lack of an in vitro model of latency have compromised the ability to study both viral transcription patterns and the components of the immune system responsible for maintaining latency in the host.
We have previously demonstrated the effectiveness of PCR-in situ hybridization (PISH) for the in situ detection of viral DNA sequences (29, 39, 52). The aim of this study was to use PISH for the localization of MCMV DNA in tissues of latently infected animals and identify the specific cell(s) harboring MCMV during latent infection.
MATERIALS AND METHODS
Animals.
Three-week-old, female, specific-pathogen-free BALB/c mice and pregnant BALB/c mice with 15- to 17-day-old embryos were purchased from Jackson Laboratory, Bar Harbor, Maine. Mice were maintained in isolation cages and fed and watered ad libitum. This study protocol was reviewed and approved by the Northwestern University Institutional Animal Care and Use Committee.
Virus and cell culture.
MCMV (Smith strain, ATCC 194-VR) was purchased from the American Type Culture Collection (Rockville, Md.) and propagated in BALB/c mouse embryo fibroblasts (MEFs). Fibroblasts were prepared from 15- to 17-day BALB/c mouse embryos by trypsinization in 0.25% trypsin–0.125% EDTA and passaged in minimal essential medium with Earle’s salts, 10% fetal calf serum (FCS), and antibiotics (penicillin [100 U/ml] and streptomycin [100 μg/ml]) at 37°C in a humidified chamber with 5% CO2. Large-scale virus propagation was accomplished by infecting 90% confluent monolayers of low-passage (passage 2 to 4) MEFs with virus obtained from clarified supernatants of salivary gland extracts of acutely infected mice. Plaques were visible 11 days after infection, at which time cells and supernatants were harvested, sonicated, and clarified by low-speed centrifugation. Virus was pelleted from the clarified supernatant by centrifugation for 3 h at 18,000 rpm in an SS34 rotor, resuspended in culture medium, sonicated, titered, aliquoted, and stored at −70°C. Titers of 108 to 109 PFU/ml were typically obtained.
Virus infection and establishment of MCMV latency.
Latently infected BALB/c mice were established by intraperitoneal injection with 105 PFU of MCMV purified from infected MEFs. Animals surviving acute infection were maintained for 6 months and analyzed for the presence of serum anti-MCMV antibodies, MCMV DNA, and MCMV IE-1 transcripts. Acutely infected and uninfected animals were maintained as positive and negative controls, respectively.
Plaque assays.
The plaque assay included centrifugal enhancement of infection and omission of the semisolid overlay as previously described (4). MEF cells (2 × 105) were seeded into six-well tissue culture plates (Costar, Cambridge, Mass.) and incubated overnight. Tissue samples obtained from mice ≥6 months after initial MCMV infection were minced and sonicated on ice with an ultrasonic homogenizer (CP-710; Cole Palmer, Chicago, Ill.) for 30 s and stored on ice; 1:10 dilutions of undiluted clarified homogenates from each organ were overlaid on confluent MEF monolayers. Following an initial medium change after 24 h, the cells were maintained in Dulbecco modified Eagle medium with 5% FCS and observed by inverted-phase microscopy (4 to 6 weeks) for cytopathic effects characteristic of CMV infection.
Reactivation of latent virus by spleen explant culture.
Spleens were removed from latently infected mice and minced into 1- by 1-mm fragments. Six fragments were seeded into 75-cm2 dishes containing 90% confluent MEFs in 15 ml of Dulbecco modified Eagle medium supplemented with 10% FCS and 1% antibiotics and incubated at 37°C in a humidified chamber with 5% CO2. Medium supernatant was exchanged and screened for MCMV DNA every fifth day by PCR and Southern blot hybridization.
PCR.
DNA was extracted from tissues of acutely infected, latently infected, or uninfected animals. In initial experiments, MCMV DNA from the IE-1 region was amplified as previously described (1) with primers CH16 and CH17 (18) or MCMV1 and MCMV2 (1) to generate PCR products of 310 or 276 bp, respectively. In later experiments, MCMV DNA from the IE-1 region was amplified by nested PCR. In the first round of amplification, 1 μg of DNA was amplified in standard buffer conditions with 40 pmol of sense primer SY1 (5′TGGATGAGAACCGTGTCTAC3′) and antisense primer SY2 (5′ATATCATCTTGCGTTGTCTT3′) for 20 cycles of 94°C for 30 s, 60°C for 30 s, and 72°C for 30 s to generate a 549-bp product from the MCMV immediate-early region (25) in a reaction volume of 100 μl; 1 μl of this PCR product was reamplified under the same conditions for 30 cycles with internal primers CH17 and CH16 to generate a 310-bp product. β-Actin DNA was amplified by PCR protocol A as described below or PCR protocol B (40 cycles of 94°C for 30 s, 60°C for 30 s, and 72°C for 30 s). PCR products were electrophoretically separated on 2% agarose gels, transferred to nitrocellulose with a Turboblotter system (Schleicher & Schuell, Keene, N.H.), hybridized to a 3′-labeled oligonucleotide CH15 probe (18), and detected by enhanced chemiluminescence (Amersham [Arlington Heights, Ill.] ECL 3′ oligolabeling and detection system).
Reverse transcription-PCR (RT-PCR).
RNA was extracted from tissues following homogenization in guanidine isothiocyanate. Total cellular RNA was isolated as described previously (9), using cesium trifluoroacetate instead of cesium chloride. Typically, equal amounts of total RNA (1.5 μg) were used to synthesize first-strand cDNA with oligo(dT) primers and Moloney murine leukemia virus reverse transcriptase (GIBCO-BRL, Gaithersburg, Md.) as described previously (18). An aliquot of cDNA was used to amplify β-actin with primers BA-1 and BA-2 (18), and the yield of β-actin was used to subject comparable amounts of cDNA to amplification of MCMV IE-1 RNA. All PCRs were subjected to the hot-start method (10) to minimize primer-primer annealing. After initial denaturation at 94°C for 3 min, MCMV IE-1 cDNA was amplified with primers CH16 and CH17 by PCR protocol A: 35 cycles of denaturation at 94°C for 30 s, annealing at 60°C for 45 s, and extension at 72°C for 60 s, followed by a final 10-min extension at 72°C. Predicted sizes of amplimers are 170 bp for β-actin and 310 and 188 bp for MCMV IE-1 DNA and RNA, respectively. PCR products were analyzed as described above.
Detection of MCMV-specific antibodies.
Immunofluorescent detection of anti-MCMV immunoglobulin was performed on animal serum extracted by the standard clot retraction/centrifugation technique (2). The serum was saved undiluted and as a 1:10 dilution in phosphate-buffered saline (PBS) with 0.1% (vol/vol) Tween 20 for analysis. Second-passage MEFs were infected with MCMV (0.1 PFU/cell) as a source of MCMV antigen. Once the MEFs displayed the cytopathic effects of infection, they were mounted, as cytospins, for assay. The cytospins were fixed in acetone, hydrated through graded alcohols, and blocked with nonimmune goat serum, and test serum was aliquoted over the cells and incubated at 37°C for 30 min. Anti-MCMV immunoglobulin G was detected by a fluorescein isothiocyanate-conjugated goat anti-mouse immunoglobulin G monoclonal antibody (Fisher Biotech, Pittsburgh, Pa.). Negative controls included uninfected MEFs, the omission of test serum, and appropriate isotype controls. Known anti-MCMV serum was used as a positive control.
Tissue processing.
Animals were anesthetized by methoxyflurane (Pitman-Moore, Inc., Mundelein, Ill.) inhalation and sacrificed by cervical dislocation. Whole blood was collected immediately by cardiac puncture, and multiple organs and tissues (including lung, liver, heart, kidney, spleen, and bone marrow) were harvested. These tissues were promptly divided and treated for analysis. Portions collected for plaque assay were homogenized and placed in culture with MCMV-permissive MEFs. Samples dedicated to analysis by PISH were preserved with a nonaldehyde, non-cross-linking tissue fixative (Streck Laboratories, Omaha, Neb.) for in situ preservation of intracellular DNA sequences. Fixed tissues were embedded in paraffin, omitting formalin treatment to prevent DNA cross-linking. Bone marrow specimens were decalcified by 3-day treatment with 0.5 M EDTA prior to embedding.
In situ hybridization.
Standard in situ hybridization was performed by using a modification of the protocol of Haase (16). Modifications included the use of a biotinylated oligonucleotide probe, MCMVP (1), which was detected with a streptavidin-alkaline phosphatase conjugate and nitroblue tetrazolium (NBT)–5-bromo-4-chloro-3-indolylphosphate (X-phosphate) (Boehringer Mannheim Corp., Indianapolis, Ind.).
PISH.
For PISH analysis, 4-μm sections were cut onto a silanized slide (coated with a 3% Elmer’s Glue solution) with a clean, disposable microtome blade. The samples were deparaffinized in xylene and hydrated through graded alcohols. After hydration the samples were washed with PBS and treated with 2.5% bovine serum albumin in reagent-grade water for 20 min at room temperature to inhibit sequestration of the DNA polymerase on the slide and tissues. Sections were digested in proteinase K (20 μg/ml) in lysis buffer (10 mM Tris [pH 8.3], 50 mM KCl, 2.5 mM MgCl2, 0.5% Tween 20, 0.5% Nonidet P-40) for 25 min to 1 h at 37°C, and the slide was then heated to 95°C for 2 min to inactivate the proteinase K. The slides were washed in PBS, dehydrated through graded alcohols, and air dried. IE-1-specific MCMV DNA was amplified by a modified PCR protocol (with primers CH16 and CH17) as described in reference 31. Each section was incubated in 40 μl of a preheated (94°C) PCR mixture consisting of 1× PCR Buffer II (Perkin-Elmer, Norwalk, Conn.), 4.5 mM MgCl2, 0.20 mM dATP, 0.20 mM dCTP, 0.20 mM dGTP, 0.20 mM dTTP–digoxigenin-11-dUTP (9:1) mixture (Boehringer Mannheim), and 1 μM each primer. Digoxigenin-11-dUTP was included in the reaction to anchor the product DNA in situ and prevent positive signal from diffusing into uninfected cells. Subsequently, 1.5 U of Taq DNA polymerase (Perkin-Elmer) in 12.5 μl of reaction mixture was added to initiate the hot-start PCR. Multiple samples were thermocycled by using either a Coy (Detroit, Mich.) TempCycler II Slide Cycler and glass cover slip or the GeneAmp In Situ PCR System 1000 (Perkin-Elmer). The thermocycling profile included 24 cycles of 92°C for 1 min, 56°C for 2 min, and 72°C for 2 min for the denaturing, annealing, and amplification steps, respectively.
Following thermocycling, the sample coverslip or AmpliCover Disc (Perkin-Elmer Cetus, Norwalk, Conn.) was removed, and the PCR mixture was saved for the detection of diffused product DNA. The slides were washed twice for 5 min each time in PBS, and endogenous biotin was blocked in all tissues by using an avidin-biotin blocking kit (Vector Laboratories, Inc., Burlingame, Calif.). Virus-specific product DNA was hybridized in situ with an internally conserved, biotin-labeled (as biotin-dTTP, every 10 to 12 nucleotides) oligonucleotide probe (CH15P [18]). The hybridization buffer (consisting of 50% formamide, 4× SSC [1× SSC is 0.15 M NaCl plus 0.015 M sodium citrate], 1× Denhardt’s solution, 0.1% sodium dodecyl sulfate, and 1 mg of salmon sperm DNA per ml, with a probe concentration of 100 ng/ml) was applied to the sections, which were sealed with a Probe-Clip Press-Seal incubation chamber (Sigma Chemical Co., St. Louis, Mo.). The sections were heated to 95°C for 5 min on the Coy Slide Cycler and incubated overnight at room temperature. Following removal of the incubation chamber, the hybridization buffer was saved for the detection of diffused product DNA and DNA-probe hybrids. The sections were washed once with posthybridization wash buffer (2× SSC, 0.01% sodium dodecyl sulfate, 0.1% bovine serum albumin) and twice with PBS for 5 min and then blocked with 10% sheep serum. Hybridized probe was detected with a streptavidin-alkaline phosphatase conjugate (Boehringer Mannheim). The slides were washed twice with PBS and then incubated for 30 min with NBT (337.5 μg/ml)–X-phosphate (175 μg/ml) in alkaline phosphatase buffer (100 mM Tris, 100 mM NaCl, 50 mM MgCl2 [pH 9.5]) at ambient temperature in the dark. Endogenous alkaline phosphatase was blocked during detection on all sections by the addition of 1× levamisole solution (Zymed Laboratories, Inc., San Diego, Calif.) to the alkaline phosphatase buffer. Slides were then washed in PBS once, counterstained with fast green or aqueous eosin, and mounted by using Aqua-Mount (Lerner Laboratories, Pittsburgh, Pa.). Positive cells yielded a black precipitate.
Controls for the PISH assay included tissue from uninfected mice, serial sections of slides with positive signal (acutely infected tissues) to which no Taq DNA polymerase or primers were added, the use of nonspecific (human CMV [HCMV]) primers or probe (45), and omission of MCMV-specific probe and/or streptavidin-alkaline phosphatase. More than 80 control slides were tested in parallel under these conditions, and positive cells were not detected in control sections. Sections in which MCMV-positive cells were found were confirmed as positive by examining more than 20 sections. The postamplification PCR mixtures and hybridization buffers were analyzed for diffusion of oligonucleotides by agarose gel electrophoresis and ethidium bromide staining.
Immunohistochemistry.
Immunohistochemistry was performed on the tissue section immediately adjacent (contiguous) to the section found positive for the latent MCMV IE-1 DNA by PISH. Sections were deparaffinized and rehydrated through graded alcohols, washed in PBS, and blocked with serum corresponding to the species in which the primary antibody was raised. The following primary antibodies were used at a dilution of 1:100: rat anti-mouse CD31 (PECAM-1, clone MEC 13.3), specific for endothelial cells (ECs) (55); and rat anti-mouse Mac-3 (clone M3/84), specific for macrophages (PharMingen, San Diego, Calif.) (19, 44). The primary antibodies were detected with biotinylated mouse anti-rat κ light-chain secondary antibody (PharMingen) and a streptavidin-fluorescein isothiocyanate conjugate, or alkaline phosphatase in the case of light microscopic analysis. The isotype control antibodies were purchased from PharMingen. Sections were counterstained with methyl green and eriochrome black and mounted with Aquamount containing 10% triethylenediamine (Sigma). Light microscopic sections were counterstained with metanil yellow (Sigma). Control staining included omission of primary antibody, isotype control antibodies, and identically processed, positive control tissue sections of thymus, lymph nodes, and spleen. Hematoxylin and eosin staining of slides for histological comparison was performed by the standard protocol (11). All images of gels, in situ hybridization, PISH, and immunofluorescence were scanned by using Adobe Photoshop.
RESULTS
Virus infection and establishment of MCMV latency in animal subjects.
Latency for MCMV has been defined as the inability to detect replicating virus in target organs such as salivary gland or spleen 6 months after acute infection (24). Latently infected BALB/c mice were established by intraperitoneal injection of 105 PFU of MCMV (Smith strain), and animals surviving acute infection were maintained for 6 months. All animals were screened for the presence of MCMV-specific antibodies in the serum. Anti-MCMV immunoglobulin was detected in the sera of all infected animals, while uninfected animals were seronegative. Infected animals were also screened for the presence of replicating virus by plaque assays of tissues on permissive MEFs. MCMV plaques were detected by plaque assay of sonicated extracts of organs from acutely infected animals after 6 days in culture but were not detected in extracts from uninfected animals or from mice infected 6 months previously, even after 3 weeks in culture. Mice that had been infected 6 months previously and were seropositive for antibodies against MCMV and negative for viral replication in plaque assays were considered to be latently infected.
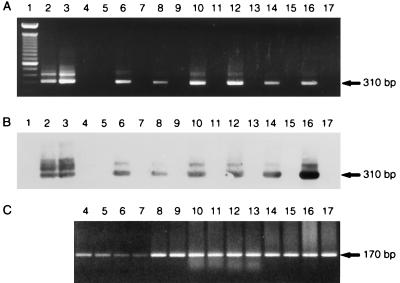
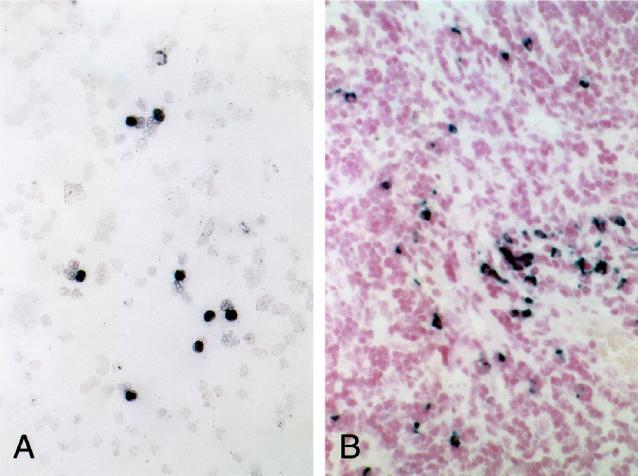
Acutely infected, uninfected, and latently infected mice were then screened for the presence of viral DNA and RNA by PCR analysis of nucleic acid extracted from various tissues. MCMV-specific DNA from the IE-1 region was detected in the heart, spleen, kidney, liver, lung, and bone marrow of all of six latently infected animals but was not detected in tissue from uninfected animals. Figure 1 shows a representative gel of MCMV-specific PCR products amplified from various tissues of one latently infected and one uninfected mouse. The specificity of the amplification product was confirmed by Southern blot hybridization (Fig. 1B). MCMV DNA was not detected in the peripheral blood lymphocytes of either uninfected or latently infected animals, although β-actin sequences could be amplified from all samples from both latently infected and uninfected mice (Fig. 1C).
FIG. 1.
Detection of MCMV DNA in tissues of latently infected mice. (A) Ethidium bromide-stained agarose gel of PCR products amplified by nested PCR (Materials and Methods) from 4 × 104 PFU of virus purified from MEFs infected in vitro (lanes 2 and 3) or from blood (lanes 4 and 5), bone marrow (lanes 6 and 7), heart (lanes 8 and 9), kidney (lanes 10 and 11), liver (lanes 12 and 13), lung (lanes 14 and 15), or spleen (lanes 16 and 17) of latently infected (lanes 4, 6, 8, 10, 12, 14, and 16) or uninfected (lanes 5, 7, 9, 11, 13, 15, and 17) mice. Lane 1, 100-bp ladder. (B) Southern blot of gel in panel A hybridized with probe CH15. (C) Positive control showing amplification of β-actin sequences from DNAs used above with primers BA-1 and BA-2 by PCR protocol B (Materials and Methods).
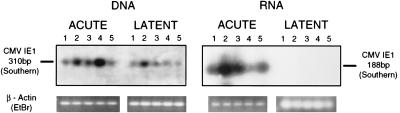
Transcripts from the IE-1 region of the genome are expressed during the early stages of productive infection and, in animals surviving acute infection, are suggestive of persistent rather than latent infection. To determine whether IE-1 transcripts were present in tissues from these mice, RNA extracted from the liver, lung, heart, kidney, and spleen was screened by RT-PCR with oligonucleotide primers specific for the IE-1 region. MCMV IE-1 transcripts were detected in the liver, lung, spleen, kidney, heart, and bone marrow of acutely infected animals. Southern blot hybridization confirmed the specificity of the amplified products. No MCMV IE-1 transcripts were detectable in any organ from six of six latently infected mice or three of three uninfected mice, although β-actin transcripts could be amplified. Figure 2 shows a Southern blot of a representative PCR analysis of DNA and RNA from tissues of an acutely and a latently infected mouse. In this experiment, approximately 5-fold more amplified latent DNA and 10-fold more latent RNA were loaded compared to amplified acute samples (based on the ethidium bromide fluorescence of amplified β-actin bands). In general, the latent samples had 1- to 2-log-fold less IE-1 DNA than the corresponding acute samples.
FIG. 2.
MCMV IE-1 RNA is expressed in acutely infected, but not in latently infected, mice. DNA and RNA were extracted from tissues of acutely infected or latently infected mice and amplified by PCR or RT-PCR, respectively, with IE-1 primers CH16 and CH17, using PCR protocol A (Materials and Methods). PCR products were electrophoretically separated on agarose gels, transferred to nitrocellulose, and hybridized to nonisotopically labeled oligonucleotide CH15 probe. Five times more latent DNA and ten times more latent RNA were loaded than in the corresponding acute samples. Predicted sizes of amplimers are 310 bp for MCMV IE-1 DNA and 188 bp for IE-1 RNA. Lanes 1 to 5 depict lung, liver, kidney, spleen, and heart samples, respectively. No IE-1 transcripts were detected in organs of either uninfected (not shown) or latently infected animals. EtBr, ethidium bromide.
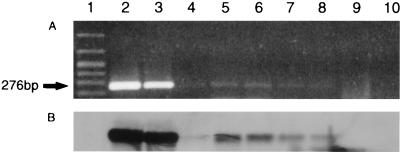
Latent MCMV can be reactivated in vitro by culturing spleen explants in the presence of permissive MEFs. This virus can be recovered from the media and detected by PCR. To demonstrate viral reactivation from our latently infected mice, spleen explants from five latently infected mice were cultured in the presence of MEFs. Cultures were observed for the presence of plaques, and culture medium was harvested every fifth day and screened for the presence of viral DNA by PCR with primers specific for the IE-1 region. No virus was detected in the media at 11 days after explant, but after 16 days in culture, plaques were visible and viral DNA was detected in the media by PCR and Southern blot hybridization (Fig. 3).
FIG. 3.
Reactivation of MCMV from spleen explants of latently infected mice. Supernatants from spleen explants harvested after 16 days of coculture with MEFs were screened for the presence of MCMV IE-1 DNA by PCR protocol B with primers MCMV1 and MCMV2 (1). (A) Ethidium bromide-stained agarose gel of PCR products. Lane 1, 100-bp DNA ladder; lanes 2 to 10, amplification products of MCMV isolated from supernatants of MEFs infected in vitro (lanes 2 and 3), spleen coculture supernatants from five latently infected mice (lanes 4 to 8), and no DNA (lanes 9 and 10). (B) Southern blot of gel shown in panel A.
These data demonstrate that we have established latent MCMV infection in our mice. Despite the presence of viral DNA in many organs in these mice, transcripts from the IE-1 region were not observed, indicating that these mice are in fact latently, rather than persistently, infected. Consistent with these observations, shedding of virus into the media was not detected until 16 days after spleen explant culture. The presence of reactivated virus 16 days after explant indicates that the viral DNA remains biologically viable in cells harboring latent virus.
Cellular localization of MCMV DNA in latently infected tissues.
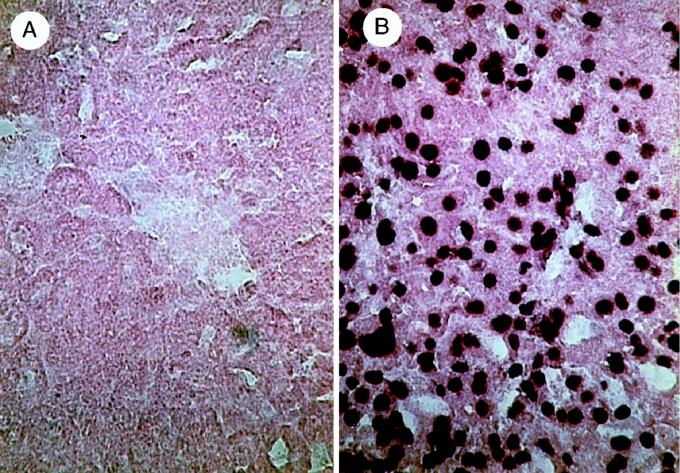
To identify the cell types harboring latent MCMV DNA, we analyzed tissues by standard in situ hybridization without PCR amplification. While MCMV DNA was readily detected in tissues from acutely infected animals, we were unable to detect MCMV DNA in tissues from latently infected animals (Fig. 4), suggesting that the copy number of viral DNA in latently infected cells is below the limits of detection by in situ hybridization. To increase the sensitivity of detection of MCMV DNA, we used PISH analysis on fixed tissue from each organ after having verified the presence of latent MCMV DNA by standard PCR analysis. We have previously demonstrated that this technique is sensitive enough to detect a single copy of intracellular proviral DNA in situ (29, 39, 52).
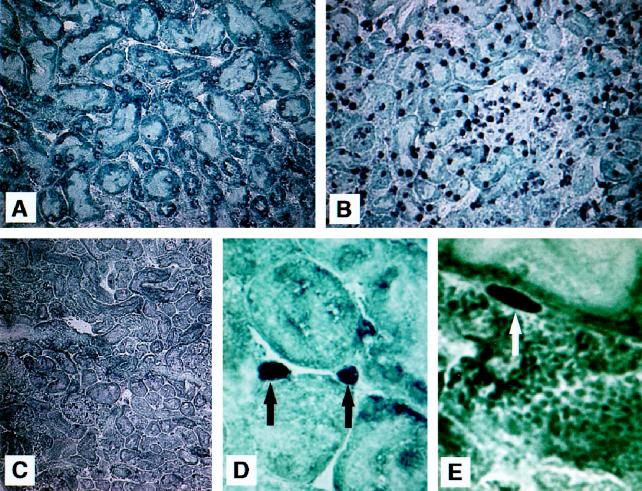
FIG. 4.
In situ hybridization using a biotinylated oligonucleotide probe (without DNA amplification) of liver tissue from latently infected mice showing no detection (A) and acutely infected mice showing widespread detection with a streptavidin-alkaline phosphatase conjugate and NBT–X-phosphate (B).
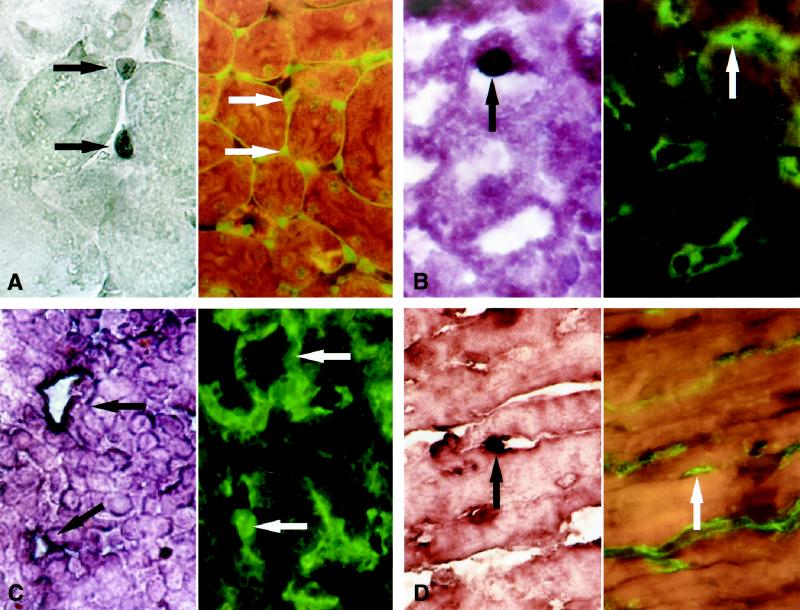
Using PISH, we were able to detect MCMV DNA in kidney sections of both latently and acutely infected mice (Fig. 5B to E). Kidney sections of uninfected control mice were negative (Fig. 5A). The location and morphology of the PCR-positive cells strongly suggested that these cells were peritubular ECs. To demonstrate the presence of ECs surrounding the kidney tubule, immunofluorescence with anti-PECAM-1 antibody was performed on the tissue section immediately adjacent (4 μm) to the section assayed by PISH. PECAM-1 is constitutively expressed at high levels on all continuous endothelial linings in vivo (55). Staining with PECAM-1 antibody clearly shows the presence of ECs in the location of the PCR-positive cells in the kidney and strongly suggests that these PCR-positive cells are ECs (Fig. 6A). A survey of other organs showed that PISH-positive cells were also present in the liver, spleen, and heart (Fig. 6B to D). PECAM-1 staining of adjacent sections was consistent with their identity as ECs. These observations were reproduced in six of six latently infected animals. PCR-positive cells were also detected in cells of the lung alveolar septum of latently infected mice (Fig. 7). However, cells in the adjacent section in the area of the PCR-positive cells were negative for PECAM-1 expression (data not shown). Immunofluorescent staining with Mac-3, a marker for macrophages (19, 44), indicated that the cells in the region of the PCR-positive cells in the lung were macrophages, and thus macrophages are likely to be the cell type harboring latent MCMV in the lung (Fig. 7).
FIG. 5.
PISH series on kidney sections. (A) Uninfected mouse control; (B) acutely infected mouse showing diffuse staining of MCMV; (C) latently infected mouse; (D) cross section of tubule showing peritubular capillary endothelial cells positive for MCMV; (E) sagittal view of tubule showing same as in panel D.
FIG. 6.
PISH detection of MCMV DNA in latently infected mouse tissues. Intracellular MCMV IE-1 amplicon DNA was hybridized in situ with an internally conserved, biotin-labeled oligonucleotide probe which was detected by immunohistochemistry with conventional light microscopic localization. PISH (left) and confirmatory immunohistochemistry using anti-PECAM-1 stain for ECs (right) are presented for tissues in panels A to D. ECs stain green. Black arrows indicate the presence of PISH-positive cells; white arrows indicate PECAM-positive cells that are present in adjacent sections in areas comparable to those where PISH-positive cells are detected. Sections show amplified MCMV DNA kidney vasa recta EC (A), liver (B), spleen (C), and heart capillary EC (D). Positive cells had a variable distribution in capillary beds and a frequency of one to three cells/field when viewed at a magnification of ×400.
FIG. 7.
PISH detection of MCMV DNA in the lung of a latently infected mouse (left). Black arrows indicate PISH-positive cells. Immunofluorescent staining for the macrophage antigen Mac-3 on the adjacent section (right) shows the presence of lung septal macrophages in positions comparable to those detected by PISH analysis, indicating that macrophages are likely to harbor latent MCMV in the lung.
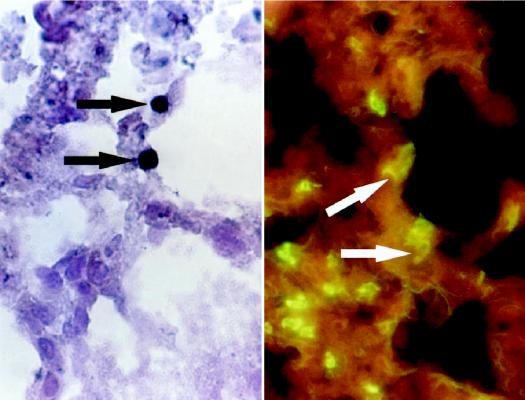
MCMV DNA was also detected in bone marrow samples from latently infected mice. PISH analysis of both cytospin (Fig. 8A) and axial bone marrow (Fig. 8B) sections revealed positive cells, the identities of which have not been determined.
FIG. 8.
PISH detection of MCMV DNA in latently infected bone marrow tissue. MCMV-positive cells stain black. Intracellular MCMV DNA was localized in both bone marrow cytospin preparations (A) and axial sections (B) from latently infected mice.
There was a 100% correlation between PCR organ screening and the detection MCMV DNA by PISH in all tissue samples. Detection of nonspecific product DNA, formed as a result of mispriming and/or polymerase-associated DNA repair, was avoided by the detection of hybridized, target-specific probe. Nonspecific hybridization of the biotinylated oligonucleotide probe was not observed, as shown by lack of staining in uninfected organ sections and sections where either the DNA polymerase was omitted or nonspecific primers were used in the PCR mixture. Digoxigenin-11-dUTP was incorporated into the PCR protocol to prevent diffusion of amplicon DNA into neighboring uninfected cells, and MCMV amplicon sequences were not detected in either the postamplification PCR buffer or the hybridization buffer.
DISCUSSION
In situ PCR and PISH have become valuable tools in the analysis of intracellular DNA and RNA sequences (14, 37, 39). We have used the power and specificity of PISH detection of nucleic acids to identify cells harboring latent MCMV DNA. The location and morphology of the PCR-positive cells in the kidney strongly suggested that these were ECs. While it was not technically possible to confirm this identity definitively by performing immunofluorescent staining on the same section used for PISH, we have used immunofluorescence analysis to show the presence of ECs in adjacent sections in locations in which PCR-positive cells were detected, thus strengthening the conclusion that these are ECs. MCMV-positive cells were also detected by PISH in sections of the liver, spleen, and heart of latently infected mice. PECAM-1 staining of cells in the adjacent section was consistent with these being ECs as well. In contrast, antibody staining of cells on sections adjacent to the PISH-positive sections of the lung suggested that these were macrophages rather than ECs. Of interest, only small vessel or capillary ECs appear to harbor latent viral DNA. The culture and study of ECs to date suggests that there is significant heterogeneity in this cell type with regard to organ type and vessel size (59). Capillary ECs, compared to their arterial and venous counterparts, have been found to exhibit variations in secretory phenotype (49) and in lipoprotein uptake and collagen phenotype (21). In vitro studies using ECs from spleen, kidneys, lungs, and bone marrow have demonstrated that ECs in these areas may phagocytose microorganisms and ingest polystyrene beads (48). In addition, hepatic and splenic sinusoidal endothelia possess gap junctions between adjacent cells and intracellular fenestrae (59), and they store and metabolize serum immunoglobulin (22). Splenic sinusoidal ECs express a unique combination of antigens associated with ECs, T lymphocytes, monocytes, and macrophages (8). Thus, capillary ECs are unique, particularly with regard to phagocytosis and cellular interaction in sinusoidal regions. Furthermore, ECs acutely infected with CMV have recently been found to enlarge and detach from the vessel wall and to enter the bloodstream, causing viral dissemination (15, 40). Although the majority of cells are lysed by the virus, a fraction of these cells become trapped in capillary beds, which may partially explain the demonstration of MCMV DNA in capillary ECs and not in ECs populating larger vessels. Our findings identify the capillary EC as an important site of MCMV DNA in latently infected animals.
We have also found MCMV DNA by PISH in the bone marrow of latently infected mice. CMV can be transmitted by blood transfusion or by bone marrow transplantation, and CMV DNA has been detected in peripheral blood monocytes and in CD34+ hematopoeitic progenitor cells of healthy human seropositive donors (33, 35, 53). HCMV can infect CD34+ bone marrow progenitor cells in vitro (28, 35), but neither monocytes nor CD34+ progenitor cells are permissive for viral replication. MCMV DNA has also been detected in macrophages of latently infected mice (42), and MCMV can be reactivated from latently infected macrophages (7, 42). Thus, hematopoietic progenitors of the monocyte/macrophage lineage have long been suspected to be an important site of CMV latency. Migration of latently infected monocytes and subsequent differentiation into tissue-specific macrophages may serve to disseminate latently infected cells into the periphery. We have provided direct evidence that MCMV DNA is present in bone marrow cells, although the specific identity of these cells has not been determined. We have also detected latently infected macrophages in the lung, which is consistent with cells of the monocyte/macrophage lineage being a site of CMV latency. The lungs, which are rich in macrophages, are known to be a major site of CMV latency, with up to a 10-fold-higher burden of latent viral DNA than in other tissues (3, 27, 30). Unstimulated murine macrophages from latently infected mice are generally nonpermissive for viral replication but become permissive upon stimulation in vitro (7, 42). Reactivation of HCMV is often associated with acute rejection in solid organ transplant recipients (47) and in clinical states associated with high circulating cytokine levels, such as sepsis, trauma, cirrhosis, or graft-versus-host disease (13). These observations suggest that allogeneic stimulation or high levels of cytokines may lead to reactivation of latently infected macrophages.
Thus, we have identified at least two cell types in which MCMV resides during latent infection: the capillary EC in the kidney, liver, and spleen, and the macrophage in the lung. Latently infected bone marrow cells are likely to be the progenitor cells for latently infected macrophages. These findings are consistent with previous analyses and with the transmission of latent CMV by solid organ transplantation in both humans and animals. Given the interactions between endothelial cells and leukocytes (6), it is possible that reactivated virus can be passed from ECs to transmigrating monocytes or vice versa. This theory is supported by a recent study which demonstrated bidirectional transmission of CMV between ECs and monocytes in vitro (56).
The term “latency” is operationally defined as the failure to detect infectious virus despite the presence of the viral genome (23). It is presently unclear whether CMV exists in a truly latent state in some cells, in which no virus particles are produced until the cell receives some external stimulus, or whether it establishes a chronic, persistent infection producing undetectable levels of virus. In the latter case, reactivation of the virus would occur as a result of failure of the immune system to destroy infected cells, whereas in the former, reactivation would occur as a result of a change in the transcriptional program of the latently infected cell (30). Recent data suggest that a truly latent state is established in at least some cells (30, 42). The nature of viral transcripts expressed in latently infected cells remains unclear. Some investigators have reported the presence of IE-1 transcripts, which are expressed in the immediate-early phase of lytic infection, in some organs of latently infected mice, although different investigators report transcripts in different organs (5, 18, 57, 58). Both sense and antisense HCMV IE-1 transcripts with the potential to encode novel proteins are detectable in bone marrow aspirates of healthy seropositive donors (28), raising the possibility that IE-1 transcripts encode negative regulators of productive infection in latently infected cells. Other investigators have reported that HCMV IE-1 transcripts are not detectable in freshly isolated monocytes or CD34+ progenitor cells from healthy seropositive donors but can be induced in monocytes upon differentiation in vitro (33, 54). Differences between human and murine viruses, sensitivity of detection, types of tissue analyzed, and the possibility of viral reactivation make it difficult to reconcile these findings.
We have not detected IE-1 transcripts in tissues from latently infected mice, although latent viral DNA is readily detectable under the conditions that we have used. Although these findings indicate that transcripts associated with lytic infection are not expressed within the limits of sensitivity of our assay, they do not rule out the possibility that other transcripts associated with maintenance of the latent state are expressed. Such transcripts have been identified in cells latently infected with other herpesviruses, such as herpes simplex virus (46) and Epstein-Barr virus (26). CMV latency-associated transcripts could play a role in maintenance of the viral genome, modulation of the immune system, or suppression of host functions required for viral reactivation. Identification of the cell types harboring latent virus suggests targets in which to search for these viral transcripts. In addition, these findings may allow new insights into the biology of CMV through the development of EC models of MCMV latency and reactivation in vitro.
REFERENCES
- 1.Abecassis M M, Jiang X, O’Niel M E, Bale J F., Jr Detection of murine cytomegalovirus (MCMV) DNA in skin using the polymerase chain reaction (PCR) Microb Pathog. 1993;15:17–22. doi: 10.1006/mpat.1993.1053. [DOI] [PubMed] [Google Scholar]
- 2.Ausubel F M, et al., editors. Current protocols in molecular biology. New York, N.Y: John Wiley & Sons, Inc.; 1995. p. 11.3.3. [Google Scholar]
- 3.Balthesen M, Messerle M, Reddehase M J. Lungs are a major organ site of cytomegalovirus latency and recurrence. J Virol. 1993;67:5360–5366. doi: 10.1128/jvi.67.9.5360-5366.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balthesen M, Dreher L, Lucin P, Reddehase M J. The establishment of cytomegalovirus latency in organs is not linked to local virus production during primary infection. J Gen Virol. 1994;75:2329–2336. doi: 10.1099/0022-1317-75-9-2329. [DOI] [PubMed] [Google Scholar]
- 5.Bevan I S, Sammons C C, Sweet C. Investigation of murine cytomegalovirus latency and reactivation in mice using viral mutants and the polymerase chain reaction. J Med Virol. 1996;48:308–320. doi: 10.1002/(SICI)1096-9071(199604)48:4<308::AID-JMV3>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 6.Bevilacqua M P. Endothelial leukocyte adhesion molecules. Annu Rev Immunol. 1993;11:767–804. doi: 10.1146/annurev.iy.11.040193.004003. [DOI] [PubMed] [Google Scholar]
- 7.Brautigam A R, Dutko F J, Olding L B, Oldstone M B. Pathogenesis of murine cytomegalovirus infection: the macrophage as a permissive cell for cytomegalovirus infection, replication and latency. J Gen Virol. 1979;44:349–359. doi: 10.1099/0022-1317-44-2-349. [DOI] [PubMed] [Google Scholar]
- 8.Buckley P A, Dickson S A, Walker W S. Human splenic sinusoidal lining cells express antigens associated with monocytes, macrophages, endothelial cells, and T lymphocytes. J Immunol. 1985;134:2310–2315. [PubMed] [Google Scholar]
- 9.Chirgwin J M, Przbyla A E, MacDonald R J, Rutter W J. Isolation of biologically active ribonucleic acid from sources enriched in ribonucleases. Biochemistry. 1979;18:5294–5299. doi: 10.1021/bi00591a005. [DOI] [PubMed] [Google Scholar]
- 10.Chou Q, Russel M, Birch D E, Bloch W. Prevention of pre-PCR mis-priming and primer dimerization improves low-copy-number amplifications. Nucleic Acids Res. 1992;20:1717. doi: 10.1093/nar/20.7.1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clark G. Staining procedures. 4th ed. Baltimore, Md: Williams and Wilkins; 1981. pp. 20–30. [Google Scholar]
- 12.Collins T, Pomeroy C, Jordan M C. Detection of latent cytomegalovirus DNA in diverse organs of mice. J Infect Dis. 1993;168:725–729. doi: 10.1093/infdis/168.3.725. [DOI] [PubMed] [Google Scholar]
- 13.Döcke W D, Prösch S, Fietze E, Kimel V, Zuckermann H, Klug C, Syrbe J, Krüger D H, von Baehr R, Volk H D. Cytomegalovirus reactivation and tumour necrosis factor. Lancet. 1994;343:268–269. doi: 10.1016/s0140-6736(94)91116-9. [DOI] [PubMed] [Google Scholar]
- 14.Embretson J, Zupancic M, Beneke J, Till M, Wolinsky S, Ribas J L, Burke A, Haase A T. Analysis of human immunodeficiency virus-infected tissues by amplification and in situ hybridization reveals latent and permissive infection at single cell resolution. Proc Natl Acad Sci USA. 1993;90:357–361. doi: 10.1073/pnas.90.1.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grefte A, van der Giessen M, van Son W, The T H. Circulating cytomegalovirus (CMV)-infected endothelial cells in patients with an active CMV infection. J Infect Dis. 1993;167:270–277. doi: 10.1093/infdis/167.2.270. [DOI] [PubMed] [Google Scholar]
- 16.Haase A T. Analysis of viral infections by in situ hybridization. J Histochem Cytochem. 1986;34:27–32. doi: 10.1177/34.1.3484488. [DOI] [PubMed] [Google Scholar]
- 17.Hendrix R M G, Wagenaar M, Slobbe R L, Bruggeman C A. Widespread presence of cytomegalovirus DNA in tissues of healthy trauma victims. J Clin Pathol. 1997;50:59–63. doi: 10.1136/jcp.50.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Henry S C, Hamilton J D. Detection of murine cytomegalovirus immediate early 1 transcripts in the spleens of latently infected mice. J Infect Dis. 1993;167:950–954. doi: 10.1093/infdis/167.4.950. [DOI] [PubMed] [Google Scholar]
- 19.Ho M, Springer T A. Tissue distribution, structural characterization, and biosynthesis of Mac-3, a macrophage surface glycoprotein exhibiting molecular weight heterogeneity. J Biol Chem. 1983;258:636–642. [PubMed] [Google Scholar]
- 20.Ho, M. 1994. Advances in understanding cytomegalovirus infection after transplantation. Transplant. Proc. 26(Suppl.1):7–11. [PubMed]
- 21.Irving M G, Roll F J, Huang S, Bissell D M. Characterization and culture of sinusoidal endothelium from normal rat liver: lipoprotein uptake and collagen phenotype. Gastroenterology. 1984;87:1233–1247. [PubMed] [Google Scholar]
- 22.Iwamura S, Enzan H, Saibara T, Onishi S, Yamamoto Y. Hepatic sinusoidal endothelial cell can store and metabolize serum immunoglobulin. Hepatology. 1995;22:1456–1461. [PubMed] [Google Scholar]
- 23.Jordan M C. Latent infection and the elusive cytomegalovirus. Rev Infect Dis. 1983;5:205–215. doi: 10.1093/clinids/5.2.205. [DOI] [PubMed] [Google Scholar]
- 24.Jordan M C, Shanley J D, Stevens J G. Immunosuppression reactivates and disseminates latent murine cytomegalovirus. J Gen Virol. 1977;37:419–423. doi: 10.1099/0022-1317-37-2-419. [DOI] [PubMed] [Google Scholar]
- 25.Keil G M, Ebeling-Keil A, Koszinowski U H. Sequence and structural organization of the murine cytomegalovirus immediate-early gene 1. J Virol. 1987;61:1901–1908. doi: 10.1128/jvi.61.6.1901-1908.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kieff E. Epstein-Barr virus and its replication. In: Fields B N, Knipe D M, Howley D M, et al., editors. Fields virology. 3rd ed. Philadelphia, Pa: Lippincott-Raven Publishers; 1996. pp. 2343–2396. [Google Scholar]
- 27.Koffron A J, Patterson B K, Yan S, Kaufman D B, Fryer J P, Stuart F P, Abecassis M I. Latent human cytomegalovirus: a functional study. Transplant Proc. 1997;29:793–795. doi: 10.1016/s0041-1345(96)00104-2. [DOI] [PubMed] [Google Scholar]
- 28.Kondo K, Xu J, Mocarski E S. Human cytomegalovirus latent gene expression in granulocyte macrophage progenitors in culture and in seropositive individuals. Proc Natl Acad Sci USA. 1996;93:11137–11142. doi: 10.1073/pnas.93.20.11137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Korber B M, Kunstman K J, Patterson B K, Furtado M, McEvilly M M, Levy R, Wolinsky S M. Genetic differences between blood- and brain-derived viral sequences from human immunodeficiency virus type 1-infected patients: evidence of conserved elements in the V3 region of the envelope protein of brain-derived sequences. J Virol. 1994;68:7467–7481. doi: 10.1128/jvi.68.11.7467-7481.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kurz S, Steffens H, Mayer A, Harris J R, Reddehase M J. Latency versus persistence or intermittant recurrences: evidence for a latent state of murine cytomegalovirus in the lungs. J Virol. 1997;71:2980–2987. doi: 10.1128/jvi.71.4.2980-2987.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maniatis T, Fritsch E F, Sambrook J. Molecular cloning: a laboratory manual. Cold Spring Harbor, N.Y: Cold Spring Harbor Laboratory; 1982. [Google Scholar]
- 32.Melnick J L, Hu C, Burek J, Adam E, BeBakey M E. Cytomegalovirus DNA in aterial walls of patients with atherosclerosis. J Med Virol. 1994;42:170–174. doi: 10.1002/jmv.1890420213. [DOI] [PubMed] [Google Scholar]
- 33.Mendelson M, Monard S, Sissons P, Sinclair J. Detection of endogenous human cytomegalovirus in CD34+ bone marrow progenitors. J Gen Virol. 1996;77:3099–3102. doi: 10.1099/0022-1317-77-12-3099. [DOI] [PubMed] [Google Scholar]
- 34.Mercer J A, Wiley C A, Spector D H. Pathogenesis of murine cytomegalovirus infection: identification of infected cells in the spleen during acute and latent infections. J Virol. 1988;62:987–997. doi: 10.1128/jvi.62.3.987-997.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Minton E J, Tysoe C, Sinclair J H, Sissons J G P. Human cytomegalovirus infection of the monocyte/macrophage lineage in bone marrow. J Virol. 1994;68:4017–4021. doi: 10.1128/jvi.68.6.4017-4021.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mocarski E., Jr . Cytomegalovirus and their replication. In: Fields B N, Knipe D M, Howley D M, et al., editors. Fields virology. 3rd ed. Philadelphia, Pa: Lippincott-Raven Publishers; 1996. pp. 2447–2492. [Google Scholar]
- 37.Nuovo G J. PCR in situ hybridization. Protocols and applications. New York, N.Y: Raven Press; 1994. [Google Scholar]
- 38.Pac C Y, Eun H-M, McArthur R G, Yoon J W. Association of cytomegalovirus infection with autoimmune type I diabetes. Lancet. 1988;1:1–4. doi: 10.1016/s0140-6736(88)92941-8. [DOI] [PubMed] [Google Scholar]
- 39.Patterson B K, Till M, Otto P, Goolsby C, Furtado M R, McBride L J, Wolinsky S M. Detection of HIV-1 DNA and messenger RNA in individual cells by PCR-driven in situ hybridization and flow cytometry. Science. 1993;260:976–979. doi: 10.1126/science.8493534. [DOI] [PubMed] [Google Scholar]
- 40.Percivalle E, Revello M G, Vago L, Morini F, Gerna G. Circulating endothelial giant cells permissive for human cytomegalovirus (HCMV) are detected in disseminated HCMV infections with organ involvement. J Clin Invest. 1993;92:663–670. doi: 10.1172/JCI116635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Persoons M C J, Daemen M J A P, Bruning J H, Bruggeman C A. Active cytomegalovirus infection of arterial smooth muscle cells in immunocompromised rats: a clue to herpesvirus-associated atherogenesis? Circ Res. 1994;75:214–220. doi: 10.1161/01.res.75.2.214. [DOI] [PubMed] [Google Scholar]
- 42.Pollack J L, Presti R M, Paetzold S, Virgin H W. Latent murine cytomegalovirus infection in macrophages. Virology. 1997;227:168–179. doi: 10.1006/viro.1996.8303. [DOI] [PubMed] [Google Scholar]
- 43.Pomeroy C, Hilleren P J, Jordan M C. Latent murine cytomegalovirus DNA in splenic stromal cells of mice. J Virol. 1991;65:3330–3334. doi: 10.1128/jvi.65.6.3330-3334.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ralph P, Ho M, Litcofsky B, Springer T A. Expression and induction in vitro of macrophage differentiation antigens on murine cell lines. J Immunol. 1983;130:108–114. [PubMed] [Google Scholar]
- 45.Rasmussen L, Morris S, Zipeto D, Fessel J, Wolitz R, Dowling A, Merigan T C. Quantitation of human cytomegalovirus DNA from peripheral blood cells of human immunodeficiency virus-infected patients could predict cytomegalovirus retinitis. J Infect Dis. 1995;171:177–182. doi: 10.1093/infdis/171.1.177. [DOI] [PubMed] [Google Scholar]
- 46.Roizman B, Sears A E. Herpes simplex viruses and their replication. In: Fields B N, Knipe D M, Howley D M, et al., editors. Fields virology. 3rd ed. Philadelphia, Pa: Lippincott-Raven Publishers; 1996. pp. 2231–2295. [Google Scholar]
- 47.Rubin R H. The indirect effects of cytomegalovirus infection on the outcome of organ transplantation. JAMA. 1989;261:3607–3609. [PubMed] [Google Scholar]
- 48.Ryan U S. Culture of pulmonary endothelial cells on microcarrier beads. In: Jaffe E A, editor. Biology of the endothelial cell. The Hague, The Netherlands: Martinus Nijhoff; 1984. pp. 34–50. [Google Scholar]
- 49.Sage H, Pritzl P, Bornstein P. Secretory phenotypes of endothelial cells in culture: comparison of aortic, venous, capillary, and corneal endothelium. Arteriosclerosis. 1981;1:427–442. doi: 10.1161/01.atv.1.6.427. [DOI] [PubMed] [Google Scholar]
- 50.Span A H M, Grauls G, Bosman F, Van Boven C P A, Bruggeman C A. Cytomegalovirus infection induces vascular injury in the rat. Atherosclerosis. 1992;93:41–52. doi: 10.1016/0021-9150(92)90198-p. [DOI] [PubMed] [Google Scholar]
- 51.Spector D H, Spector S A. The oncogenic potential of human cytomegalovirus. Prog Med Virol. 1984;29:45–89. [PubMed] [Google Scholar]
- 52.Spira A I, Marx P A, Patterson B K, Mahoney J, Koup R A, Wolinsky S M, Ho D D. Cellular targets of infection and route of viral dissemination after an intravaginal inoculation of simian immunodeficiency virus into rhesus macaques. J Exp Med. 1996;183:215–225. doi: 10.1084/jem.183.1.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Taylor-Wiedeman J, Sissons J G, Borysiewicz L K, Sinclair J H. Monocytes are a major site of persistence of human cytomegalovirus in peripheral blood mononuclear cells. J Gen Virol. 1991;72:2059–2064. doi: 10.1099/0022-1317-72-9-2059. [DOI] [PubMed] [Google Scholar]
- 54.Taylor-Wiedeman J, Sissons P, Sinclair J. Induction of endogenous human cytomegalovirus gene expression after differentiation of monocytes from healthy carriers. J Virol. 1994;68:1597–1604. doi: 10.1128/jvi.68.3.1597-1604.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vecchi A, Garlanda C, Lampugnani M G, Resnati M, Matteucci C, Stoppacciaro A, Schnurch H, Risau W, Ruco L, Mantovani A, Dejana E. Monoclonal antibodies specific for endothelial cells of mouse blood vessels. Their application in the identification of adult and embyonic endothelium. Eur J Cell Biol. 1994;63:247–254. [PubMed] [Google Scholar]
- 56.Waldman W J, Knight D A, Huang F H, Sedmak D D. Bidirectional transmission of infectious cytomegalovirus between monocytes and vascular cells: an in vitro model. J Infect Dis. 1995;171:263–272. doi: 10.1093/infdis/171.2.263. [DOI] [PubMed] [Google Scholar]
- 57.Yu Y, Henry S C, Xu F, Hamilton J D. Expression of a murine cytomegalovirus early-late protein in “latently” infected mice. J Infect Dis. 1995;172:371–379. doi: 10.1093/infdis/172.2.371. [DOI] [PubMed] [Google Scholar]
- 58.Yuhasz S A, Dissette V B, Cook M L, Stevens J G. Murine cytomegalovirus is present in both chronic active and latent states in persistently infected mice. Virology. 1994;202:272–280. doi: 10.1006/viro.1994.1343. [DOI] [PubMed] [Google Scholar]
- 59.Zetter B R. Endothelial cell heterogeneity: influence of vessel size, organ localization, and species specificity on the properties of cultured endothelial cells. In: Ryan U, editor. Endothelial cells. II. Boca Raton, Fla: CRC Press, Inc.; 1988. pp. 63–79. [Google Scholar]