Abstract
Background
Nonalcoholic fatty liver disease (NAFLD) is a growing health issue around the world.
Aim
This study is to investigate whether adult prevalence of NAFLD correlates with national economic status.
Methods
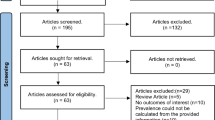
Literature search on PubMed database was conducted to identify eligible records fully published before September 2014. Gross national income (GNI) per capita was chosen to evaluate national economic status. Pearson coefficient, linear regression, and unpaired t test were performed in the statistical analyses.
Results
Twenty-one population-based surveys (seven in East Asia, five in South Asia, three in Middle East, and six in Europe) were included. The pooled prevalence of NAFLD was 24.24 %, and the global prevalence was positively correlated with GNI per capita (r = 0.4782, P = 0.0283). Europe witnessed a higher prevalence (28.04 %) than Middle East (12.95 %, P = 0.0092) and East Asia (19.24 %, P = 0.0083). Male presented a higher prevalence than female (P = 0.019), especially in Europe (P = 0.0132) and in Caucasians (P = 0.0383). Furthermore, male prevalence and rural prevalence individually were correlated with economic status (r = 0.5725, P = 0.0257 and r = 0.7389, P = 0.0060). Lastly, the urban (23.93 %) witnessed a higher prevalence than the rural or the urban + rural (12.65 %, P = 0.0141) in the countries of GNI per capita <$10,000.
Conclusions
This study suggested that countries with higher economic status tend to present a higher prevalence of NAFLD. It is believed to provide a distinctive epidemiologic perspective to global situation of NAFLD.



Similar content being viewed by others
References
Bugianesi E, Leone N, Vanni E, et al. Expanding the natural history of nonalcoholic steatohepatitis: from cryptogenic cirrhosis to hepatocellular carcinoma. Gastroenterology. 2002;123:134–140.
Neuschwander-Tetri BA, Caldwell SH. Nonalcoholic steatohepatitis: summary of an AASLD Single Topic Conference. Hepatology (Baltimore, MD). 2003;37:1202–1219.
Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther. 2011;34:274–285.
Milic S, Stimac D. Nonalcoholic fatty liver disease/steatohepatitis: epidemiology, pathogenesis, clinical presentation and treatment. Dig Dis (Basel, Switzerland). 2012;30:158–162.
Loomba R, Sanyal AJ. The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol. 2013;10:686–690.
Younossi ZM, Stepanova M, Afendy M, et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol. 2011;9:524–530. (quiz e521–e560).
Williams CD, Stengel J, Asike MI, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 2011;140:124–131.
Wagenknecht LE, Scherzinger AL, Stamm ER, et al. Correlates and heritability of nonalcoholic fatty liver disease in a minority cohort. Obesity (Silver Spring, MD). 2009;17:1240–1246.
Fischer GE, Bialek SP, Homan CE, Livingston SE, McMahon BJ. Chronic liver disease among Alaska-Native people, 2003–2004. Am J Gastroenterol. 2009;104:363–370.
Bialek SR, Redd JT, Lynch A, et al. Chronic liver disease among two American Indian patient populations in the southwestern United States, 2000–2003. J Clin Gastroenterol. 2008;42:949–954.
Mendez-Sanchez N, Arrese M, Zamora-Valdes D, Uribe M. Current concepts in the pathogenesis of nonalcoholic fatty liver disease. Liver Int. 2007;27:423–433.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–e34.
Mishra P, Younossi ZM. Abdominal ultrasound for diagnosis of nonalcoholic fatty liver disease (NAFLD). Am J Gastroenterol. 2007;102:2716–2717.
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012.
WorldBank. GNI per capita, Atlas method (current US$). http://data.worldbank.org/indicator/NY.GNP.PCAP.CD.
Wikipedia. List of countries by GNI (nominal, Atlas method) per capita. http://en.wikipedia.org/wiki/List_of_countries_by_GNI_(nominal,_Atlas_method)_per_capita.
Toshikuni N, Tsutsumi M, Arisawa T. Clinical differences between alcoholic liver disease and nonalcoholic fatty liver disease. World J Gastroenterol. 2014;20:8393–8406.
Fan JG. Epidemiology of alcoholic and nonalcoholic fatty liver disease in China. J Gastroenterol Hepatol. 2013;28:11–17.
Fan JG, Saibara T, Chitturi S, Kim BI, Sung JJ, Chutaputti A. What are the risk factors and settings for non-alcoholic fatty liver disease in Asia-Pacific? J Gastroenterol Hepatol. 2007;22:794–800.
Sanyal AJ, American Gastroenterological Association. AGA technical review on nonalcoholic fatty liver disease. Gastroenterology. 2002;123:1705–1725.
Angulo P. GI epidemiology: nonalcoholic fatty liver disease. Aliment Pharmacol Ther. 2007;25:883–889.
Liu CJ. Prevalence and risk factors for non-alcoholic fatty liver disease in Asian people who are not obese. J Gastroenterol Hepatol. 2012;27:1555–1560.
Jamali R, Khonsari M, Merat S, et al. Persistent alanine aminotransferase elevation among the general Iranian population: prevalence and causes. World J Gastroenterol. 2008;14:2867–2871.
Eshraghian A, Dabbaghmanesh MH, Eshraghian H, Fattahi MR, Omrani GR. Nonalcoholic fatty liver disease in a cluster of Iranian population: thyroid status and metabolic risk factors. Arch Iran Med. 2013;16:584–589.
Lankarani KB, Ghaffarpasand F, Mahmoodi M, et al. Non alcoholic fatty liver disease in southern Iran: a population based study. Hepat Mon. 2013;13:e9248.
Wikipedia. Demographics. Golestan Province. http://en.wikipedia.org/wiki/Golestan_Province.
Wikipedia. Ethnic groups. Iran. http://en.wikipedia.org/wiki/Iran-Ethnic_groups.
Wikipedia. Religion in Iran. http://en.wikipedia.org/wiki/Religion_in_Iran.
Fan JG, Zhu J, Li XJ, et al. Prevalence of and risk factors for fatty liver in a general population of Shanghai. China J Hepatol. 2005;43:508–514.
Chen CH, Huang MH, Yang JC, et al. Prevalence and risk factors of nonalcoholic fatty liver disease in an adult population of taiwan: metabolic significance of nonalcoholic fatty liver disease in nonobese adults. J Clin Gastroenterol. 2006;40:745–752.
Zelber-Sagi S, Nitzan-Kaluski D, Halpern Z, Oren R. Prevalence of primary non-alcoholic fatty liver disease in a population-based study and its association with biochemical and anthropometric measures. Liver Int. 2006;26:856–863.
Zhou YJ, Li YY, Nie YQ, et al. Prevalence of fatty liver disease and its risk factors in the population of South China. World J Gastroenterol. 2007;13:6419–6424.
Amarapurkar D, Kamani P, Patel N, et al. Prevalence of non-alcoholic fatty liver disease: population based study. Ann Hepatol. 2007;6:161–163.
Bedogni G, Miglioli L, Masutti F, Tiribelli C, Marchesini G, Bellentani S. Prevalence of and risk factors for nonalcoholic fatty liver disease: the Dionysos nutrition and liver study. Hepatology (Baltimore, MD). 2005;42:44–52.
Haring R, Wallaschofski H, Nauck M, Dorr M, Baumeister SE, Volzke H. Ultrasonographic hepatic steatosis increases prediction of mortality risk from elevated serum γ-glutamyl transpeptidase levels. Hepatology (Baltimore, MD). 2009;50:1403–1411.
Mohan V, Farooq S, Deepa M, Ravikumar R, Pitchumoni CS. Prevalence of non-alcoholic fatty liver disease in urban south Indians in relation to different grades of glucose intolerance and metabolic syndrome. Diabetes Res Clin Pract. 2009;84:84–91.
Dassanayake AS, Kasturiratne A, Rajindrajith S, et al. Prevalence and risk factors for non-alcoholic fatty liver disease among adults in an urban Sri Lankan population. J Gastroenterol Hepatol. 2009;24:1284–1288.
Das K, Mukherjee PS, et al. Nonobese population in a developing country has a high prevalence of nonalcoholic fatty liver and significant liver disease. Hepatology (Baltimore, MD). 2010;51:1593–1602.
He S, Bao W, Shao M, et al. Risk factors for non-alcoholic fatty liver disease in a Chinese population. Acta Gastro-Enterol Belgica. 2011;74:503–508.
Pinidiyapathirage MJ, Dassanayake AS, Rajindrajith S, et al. Non-alcoholic fatty liver disease in a rural, physically active, low income population in Sri Lanka. BMC Res Notes. 2011;4:513.
Hou XH, Zhu YX, Lu HJ, et al. Non-alcoholic fatty liver disease’s prevalence and impact on alanine aminotransferase associated with metabolic syndrome in the Chinese. J Gastroenterol Hepatol. 2011;26:722–730.
Caballeria L, Pera G, Rodriguez L, et al. Metabolic syndrome and nonalcoholic fatty liver disease in a Spanish population: influence of the diagnostic criteria used. Eur J Gastroenterol Hepatol. 2012;24:1007–1011.
Wong VW, Chu WC, Wong GL, et al. Prevalence of non-alcoholic fatty liver disease and advanced fibrosis in Hong Kong Chinese: a population study using proton-magnetic resonance spectroscopy and transient elastography. Gut. 2012;61:409–415.
Jeong EH, Jun DW, Cho YK, et al. Regional prevalence of non-alcoholic fatty liver disease in Seoul and Gyeonggi-do. Korea Clin Mol Hepatol. 2013;19:266–272.
Chiloiro M, Caruso MG, Cisternino AM, et al. Ultrasound evaluation and correlates of fatty liver disease: a population study in a Mediterranean area. Metab Syndr Relat Disorders. 2013;11:349–358.
Gruchot M, Graeter T, Oeztuerk S, et al. Fasting time and lipid parameters: association with hepatic steatosis—data from a random population sample. Lipids Health Dis. 2014;13:18.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Jin-Zhou Zhu and Yi-Ning Dai have contributed equally to the work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhu, JZ., Dai, YN., Wang, YM. et al. Prevalence of Nonalcoholic Fatty Liver Disease and Economy. Dig Dis Sci 60, 3194–3202 (2015). https://doi.org/10.1007/s10620-015-3728-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3728-3